Abstract
Objective:
To characterize change in physical performance and differential prevalence of low skeletal muscle mass and strength (sarcopenia) and lower 25-hydroxyvitamin D concentrations among older women when they develop urinary incontinence (UI) symptoms.
Methods:
This is a secondary analysis of the Health, Aging, and Body Composition Study. Urinary incontinence symptoms were assessed using validated questions. The Short Physical Performance Battery (SPPB) measured physical performance. Sarcopenia, defined by low muscle mass and strength, was determined using validated cut-offs for gait speed, grip strength, and appendicular skeletal muscle mass. All parameters were evaluated at baseline and year 4. Serum 25-hydroxyvitamin D concentrations were assessed at year 2. The primary outcome was the change in SPPB total scores. Sarcopenia and lower serum 25-hydroxyvitamin D concentrations have been independently associated with poor physical performance and UI, therefore included as secondary outcomes. Univariate and multivariate analyses were used to characterize the associations of change in physical performance from baseline to year 4, incidence of sarcopenia, and lower serum 25-hydroxyvitamin D on the development of UI symptoms.
Results:
Of the 1,583 women enrolled, 910 were excluded (730 had baseline UI; 180 with missing data). Six hundred seventy-three women were continent at baseline; 223 (33%) developed UI symptoms at year 4. Short Physical Performance Battery total scores had a significant decline in among women with incident UI compared to continent women [mean difference [95% CI] continent – incident UI 0.32 [0.04, 0.60], p=0.02. Of subscale measures, standing balance showed the greatest decline at 0.20 [0.05, 0.36], continent - incident UI respectively; p=0.009]. Sarcopenia developed at a higher rate with incident UI (adjusted OR 95% CI: 1.7 [1.0, 2.9]). Low 25-hydroxyvitamin D was not associated with incident UI. [adjusted OR (95% CI) 1.1 (0.7–1.6) and 1.1 (0.7–1.6) for deficient or insufficient compared with sufficient status, respectively].
Conclusions:
We observed a significant decline in standing balance among older women who developed UI symptoms. This decline may be associated with coinciding development of sarcopenia.
Precis:
A greater decline in physical performance and standing balance is associated with the development of urinary incontinence in older, previously continent women.
INTRODUCTION
Urinary incontinence (UI) is a common pelvic floor disorder among women (1) but a geriatric syndrome among women older than 70. Geriatric syndromes are multi-factorial conditions with increasing prevalence with aging. Among older women, UI has been independently associated with mobility impairment (2, 3). Therefore, declining physical performance, also known as functional impairment, and UI are the two most common geriatric syndromes and are often linked (3). Currently, the clinical and biologic factors linking functional impairment and UI in older women are unclear.
The decline in skeletal muscle mass and function defines sarcopenia; a known risk factor for functional impairment in older adults.(4) Low serum 25-hydroxyvitamin D is important in optimizing skeletal muscle function.(5) Sarcopenia and lower serum 25-hydroxyvitamin D concentrations both become more prevalent with aging and impact skeletal muscle health.(5) Consequently, they may influence the linked relationship between functional impairment and UI.
In this secondary analysis, we primarily aim to investigate the longitudinal association between changes in functional impairment and the development of UI in a cohort of older initially well-functioning continent women. Secondarily, we aim to explore the association of sarcopenia and low 25-hydroxyvitamin D serum levels on the development of UI. Characterizing changes in functional impairment among older women who develop UI may provide therapeutic targets to prevent downstream consequences such as falls and permanent loss of independence. We hypothesize that older women who develop UI would have a more significant decline in physical performance, develop sarcopenia, and lower serum 25-hydroxyvitamin D concentrations compared to continent women
MATERIALS AND METHODS
We performed a secondary analysis of the Health, Aging and Body Composition (Health ABC) study, a prospective longitudinal cohort study designed to investigate the associations between body composition, weight-related health conditions, and incident functional impairment in initially well-functioning older adults.(5) Between April 1997 and June 1998, 3,075 community-dwelling, white and black Medicare-eligible adults ages 70–79 years old were recruited at two clinical centers (Pittsburgh, Pennsylvania and Memphis, Tennessee). Enrollment was limited to those reporting no difficulty with walking one-quarter mile, climbing 10 steps, or performing activities of daily living. Adults with life-threatening cancers or who were not planning to stay in the study area for 3 years were excluded. All participants provided written informed consent and all protocols were approved by the Institutional Review Boards at both study sites.
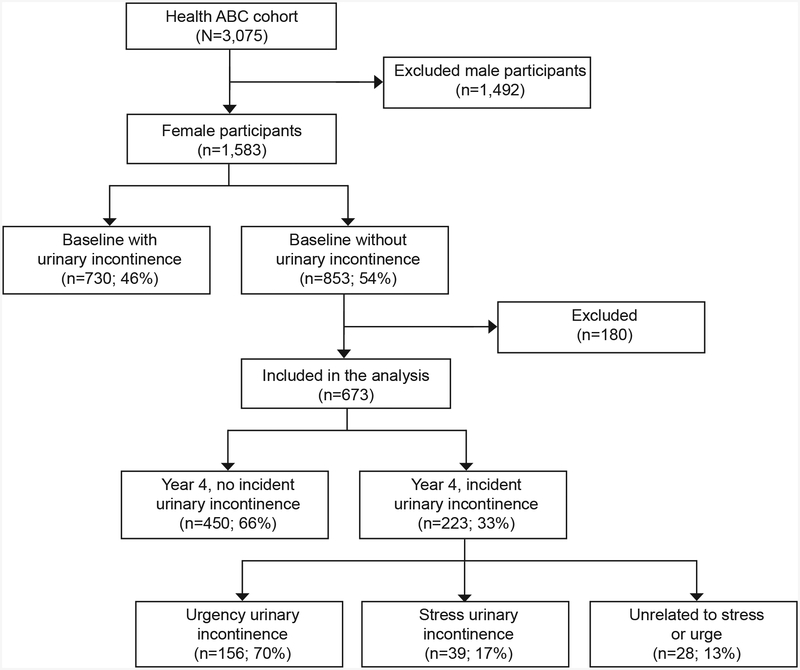
This secondary analysis was restricted to female Health ABC participants (n=1,583). Those with current or past symptoms of UI within 12 months of the baseline evaluation (n=731) and those who were missing follow-up UI data at year 4 (n=180) were excluded leaving an analysis sample of 673 women (Figure 1). At baseline, participants completed questionnaires that included demographic data (age, gender, race, and study site), UI type and severity, and the Center for Epidemiologic Studies-Depression (CES-D) scale.(6) Physical examinations at baseline included height, weight, body composition, and objective performance-based tests of physical function.
Figure 1.
Flow chart of participants. Health ABC, Health, Aging and Body Composition study.
UI type and severity was determined by asking a series of detailed questions modified from other epidemiologic studies. (7) These questions included: “Many people complain that they leak urine unintentionally. In the past 12 months, have you leaked even a small amount of urine?” Incident UI was defined as answering ‘yes’ to this question and this was our primary dependent variable. UI frequency was determined by asking “In the past 12 months, how often have you leaked urine?” Responses were: less than once per month, one or more times per month, one or more times per week, every day, and don’t know. UI type was classified as stress, urgency, or other by asking “In the past 12 months, when does your leakage of urine usually occur?” Choices were 1) ”With an activity like coughing, lifting, standing up or exercises” (stress UI); 2) “When you have the urge to urinate and can’t get to a toilet fast enough (urgency UI); or 3) “You leak urine unrelated to coughing, sneezing, lifting or urge” (other UI). The participants’ choices defined their predominant type of incontinence. (8)
Physical performance was assessed at baseline and at year 4 using the Short Physical Performance Battery (SPPB), the 400-meter fast-paced walk, and the 6-meter usual-paced walk. The SPPB is a standard and robust predictor for disability that includes progressively more challenging standing balance tasks held for 10 seconds each (side-by-side, tandem, and semi-tandem), the faster of two 6-m courses at usual pace, and time to complete five repeated chair stands. (9, 10) Each of the three performance measures was assigned a score ranging from 0 (inability to perform the task) to 4 (the highest level of performance) and summed to create an SPPB score ranging from 0 to 12 (best). The total SPPB score was our primary outcome variable. A low SPPB score (≤ 9) is a strong risk factor of decreased mobility and Activities of Daily Living (ADL) disability in nondisabled older adults. (11) In addition, a small meaningful difference in change in total SPPB score was 0.5.(12) The 400-m walk was assessed as a measurement of exercise tolerance and correlates with measured VO2 peak.(11) The course was 20-m long and marked by cones at each end. Participants were instructed to “cover as much ground as possible” and to “walk as quickly as possible at a pace you can maintain”; time to complete the 400-m walk was recorded.
According to the European Working Group on Sarcopenia in Older People (EWGSOP), the definition of sarcopenia includes a person having low muscle mass, low muscle strength, and/or low physical performance. The Foundation for the National Institutes of Health Biomarkers Consortium (FNIH) Sarcopenia Project defines sarcopenia as low muscle mass and weakness. To date, there is no single operational definition of sarcopenia has been universally adopted. Each organization however agree that there are standard cut-offs that can be applied as criteria to define sarcopenia as a condition. Lean muscle mass was assessed using whole-body dual-energy x-ray absorptiometry (DXA) scans performed at baseline and at year 4 (Hologic 4500A, version 8.20a, Waltham, MA). (13, 14) Appendicular skeletal muscle mass index (ASMI) [appendicular lean muscle mass/height (kg/m2)] was calculated by summing the appendicular lean muscle mass in the upper and lower extremities (reported in kg) and dividing it by the height squared (reported in m2). Grip strength (kg) was measured twice in each hand with an isometric Jamar Hydraulic Hand Dynamometer (Jamar, Bolingbrook, Illinois) at baseline and year 4 and the maximum force from 2 trials for the stronger hand was used in the analysis. For longitudinal analyses, the same hand was used unless contraindicated. Gate speed was determined using the 6 meter usual pace walk.
According to the EWGSOP, low muscle mass was defined as ASMI <5.44 kg/m2; low muscle strength was defined as grip strength ≤18 kg; and low physical performance defined as gait speed < 0.8 m/s.(4) While the International Working Group on Sarcopenia (IWGS) used cut-off values of ASMI ≤5.67 kg/m2, gait speed <1 m/s.(15) In addition, the FNIH Sarcopenia group recommends cut-off values of <16 kg for grip strength and <0.512 for ASMI adjusted for BMI. In an effort to prevent exclusion of an important diagnostic criterion, we incorporated 3 standard cut-offs into our comprehensive definition of sarcopenia (16): 1) to define low muscle mass ASMI <5.5 kg/m2 2) to define low physical performance gait speed <1 m/s; and 3) to define low muscle strength a grip strength ≤ 20.5 kg. (4, 17, 18)
Fasting blood samples were collected in the morning after a 12-hour fast, centrifuged, and stored at −80◦C. Serum 25-hydroxyvitamin D was measured at the year 2 clinic visit (1998–1999) with a 2-step radioimmunoassay (25-Hydroxyvitamin D 125I RIA Kit; DiaSorin, Inc., Stillwater, Minnesota) in a laboratory meeting the Vitamin D External Quality Assessment Scheme quality criteria. Total serum 25-hydroxyvitamin D concentrations between 20 to <30 ng/mL defined insufficient status and <20 ng/mL defined deficient status; sufficient status was defined as serum 25-hydroxyvitamin D concentrations ≥ 30 ng/mL (19).
To characterize functional impairment among older women who develop UI, our primary outcome was the change in physical performance determined by the short physical performance battery (SPPB) total and sub-scale scores at baseline and year 4 in women who developed UI at year 4 compared to those who remained continent. To further investigate potential links associating functional impairment and development of UI, we investigated incident sarcopenia and low serum 25-hydroxyvitamin D concentrations because both conditions have been independently associated with functional impairment and UI. Sarcopenia was defined using a strict comprehensive definition and determined at year 4. Incident sarcopenia among women who also developed UI at year 4 was compared to women who remained continent. The prevalence of insufficient and deficient serum 25-hydroxyvitamin D concentrations was determined at year 2 and compared between women who developed UI and those who remained continent.
Descriptive statistics (chi-square tests for categorical variables and t-tests for continuous variables) were used to summarize baseline characteristics of the study population by UI status at year 4. Paired t-tests were used to assess (unadjusted) changes in physical function over time within UI group; unadjusted changes in physical function scores were compared between UI groups using an independent t-test. To compare UI groups with respect to changes in physical function scores, analysis of covariance models were fitted to the year 4 physical function score, with predictors including the baseline value of the outcome as well as age, race, body mass index (BMI), co-morbid condition status (diabetes mellitus, hypertension, and cardiovascular disease). McNemar’s test was used to assess within-person changes in sarcopenia status over time by UI group. A logistic model for incident UI was fit with sarcopenia status (or its components) represented by the four states: no sarcopenia at either time point, no sarcopenia at baseline but present at follow-up, sarcopenia at baseline but not at follow-up, and sarcopenia at both time points; the model included the standard set of covariates listed above. Logistic regression was used to assess the impact of baseline sarcopenia and low serum 25-hydroxyvitamin D concentrations on incident UI and sub-type of UI at year 4 after adjustment for age, race, BMI, diabetes, hypertension, and cardiovascular (CVD) disease, site and, season. To account for potential of over-fitting in the model of sarcopenia, we adjusted the analysis to account for age, race, and BMI. We considered the importance of multiple hypothesis testing and have provided the p-values for readers to interpret the statistical relevance of the data individually.
RESULTS:
Between 1997–1998, 3,075 adults were enrolled into the Health ABC study. Of the 1,583 female participants, 910 were excluded from this analysis: 730 reported having UI symptoms at baseline and 180 women had missing data (Figure 1). Compared to included participants, women with baseline UI were more likely to have difficulty with walking (OR 1.48, 95% CI [1.11, 1.95]), to be African-American, and have hypertension. Women with missing data were noted to be less healthy based on the presence of hypertension, diabetes mellitus, and cardiovascular disease to include stroke at baseline compared to our sample. Six hundred seventy-three women were continent at baseline and had follow-up data at year 4. At year 4, 223 (33%) women had incident UI symptoms and 450 (66%) remained continent. Urgency UI was the predominant sub-type (n=156, 70%), followed by stress UI (n=39, 17%), and 13% (n=28) reported UI unrelated to stress or urge. There were few demographic differences between these groups at baseline (Table 1). While more white women developed UI at year 4, the proportion was not statistically different in comparison with black women with incident UI. Women who developed UI had significantly lower number of live births, higher BMI, and higher depressed mood.
Table 1.
Baseline demographic characteristics of women based on incident UI status at Year 4
| Demographic characteristic | Incident UI subjects N=223 |
Continent subjects N=450 |
P-value |
|---|---|---|---|
| Age, mean (SD) | 74.6 (2.9) | 74.2 (2.9) | 0.13 |
| Serum 25(OH)D, mean ± SD (ng/mL) | 24.22±11.5 | 24.61±10.81 | 0.67 |
| Race, N (%) | |||
| White | 112 (52%) | 194 (45%) | |
| Parity, median (IQR) | 2 (2–4) | 3 (2–4) | 0.03 |
| BMI (kg/m2), mean (SD) | 28.3 (5.7) | 27.4 (5.4) | 0.04 |
| Current Estrogen use, N (%) | 84 (39%) | 131 (30%) | 0.86 |
| Depression (CES-D score ≥ 16) N (%) | 11 (5%) | 9 (2%) | 0.04 |
| Anticholinergic use, N (%) |
5 (2%) | 14 (3%) | 0.40 |
| Smoking N (%) |
20 (9%) | 31 (6.9%) | 0.34 |
T-test for continuous variable and chi-square tests for categorical variables
There were no significant differences between SPPB total or subscale scores at baseline among women with incident UI and those without UI symptoms at year 4 (continent subjects). In both groups, there was a decline in SPPB total scores, as well as in standing balance, chair stands, and 6 m usual walk speed subscale scores at year 4 (Table 2). However, we observed a greater decline in SPPB total scores among women who developed UI in comparison to women who remained continent at year 4 after adjusting for baseline physical performance measures and other covariates (12) (Table 3). The primary SPPB subscale driving this difference was the statistically significantly decline in standing balance score among women with UI symptoms compared to those who maintained their continence. Changes in the SPPB chair stand subscale and mobility (the usual (6 m) and fast (400 m) walk speed) were similar between groups. Changes in physical function measures (SPPB total score, standing balance and chair stands subscale scores) based on UI status were similar after adjusting for the presence of baseline sarcopenia or lower 25-hydroxyvitamin D concentrations.
Table 2.
Unadjusted baseline and year 4 physical performance measures [means (SE)] based on UI status at year 4.
| Physical performance measure | Incident UI subjects N=223 Mean (SE) |
Continent subjects N=450 Mean (SE) |
Test for difference in changes by UI status** | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Year 4 | P-value* | Baseline | Year 4 | P-value* | ||
| SPPB score (0–12) | 9.82 (0.10) | 9.18 (0.15) | < 0.001 | 9.96 (0.07) | 9.58 (0.10) | <0.0001 | 0.08 |
| Standing balance score (0–4) | 3.66 (0.06) | 3.39 (0.07) | 0.002 | 3.63 (0.04) | 3.59 (0.05) | 0.31 | 0.03 |
| Chair stands (0–4) | 2.21 (0.08) | 1.95 (0.08) | 0.001 | 2.35 (0.05) | 2.14 (0.06) | <0.0001 | 0.54 |
| 6 m usual walk speed (m/sec) | 1.13 (0.01) | 1.04 (0.02) | <0.0001 | 1.14 (0.01) | 1.06 (0.01) | <0.0001 | 0.63 |
| 400 m fast walk (m/sec) |
1.20 (0.02) | 1.19 (0.02) | 0.0003 | 1.20 (0.01) | 1.22 (0.01) | 0.26 | 0.12 |
Paired t-test (unadjusted)
Independent t-test (unadjusted) of differences in change scores between UI and non-UI
Table 3.
Adjusted mean difference (non-UI - UI) and 95% CI in physical performance at year 4 based on incident UI status at year 4.
| Year 4 physical performance measures | Incident UI subjects N=223 Mean (SE) |
Continent subjects N=450 Mean (SE) |
DIFF [95% CI] (non-incident – incident) | Test for significant difference in means at year 4 p-value |
|---|---|---|---|---|
| SPPB score (0–12) | 9.2 (0.1) | 9.5 (0.1) | 0.32 [0.04, 0.60] | 0.02 |
| Standing balance score (0–4) | 3.32 (0.08) | 3.52 (0.07) | 0.20 [0.05, 0.36] | 0.009 |
| Chair stands score (0–4) | 1.98 (0.09) | 2.09 (0.07) | 0.11 [−0.05, 0.28] | 0.18 |
| 6-m usual walk speed (m/sec) | 1.03 (0.02) | 1.04 (0.02) | 0.01 [−0.02, 0.05] | 0.44 |
| 400-m fast walk speed (m/sec) | 1.17 (0.02) | 1.20 (0.02) | 0.03 [−0.01, 0.06] | 0.14 |
Models adjusted for baseline physical performance measure, age, race, BMI, and baseline presence of diabetes, hypertension, and cardiovascular disease
The presence of sarcopenia was similar among both groups at baseline and change in sarcopenia status from baseline was not associated with incident UI (Table 4). After excluding women with baseline sarcopenia (n=334), a greater proportion of women with incident UI concurrently developed sarcopenia based on the composite definition (37% incontinent vs. 27% continent, p=0.06) at year 4. After controlling for age, race, and BMI, women with incident UI had a 1.7 greater odds (95% CI: 1.0, 2.9) of developing sarcopenia compared to those who didn’t develop UI. However, incident sarcopenia was not independently associated with a specific type of UI (urgency or stress UI), p=0.36 controlling for race and BMI.
Table 4.
Presence of sarcopenia and its components at baseline and year 4 based on incident UI status at year 4.
| Sarcopenia determinants | Incident UI N=218 |
Non-Incident UI N=444 |
Overall p-value** | ||||
|---|---|---|---|---|---|---|---|
| Baseline N=218 |
Year 4 N=218 |
P-value* | Baseline N=444 |
Year 4 N=441 |
P-value* | ||
| Sarcopenia* | 54% (109/203) |
67% (136/203) |
0.0005 | 50% (208/416) |
61% (253/416) |
<0.0001 | 0.16 |
| ASMI < 5.5 kg/m2 | 15% (27/176) |
19% (34/176) |
0.16 | 20% (74/379) |
23% (88/379) |
0.012 | 0.93 |
| Grip Strength < 20.5 kg | 19% (41/218) |
25% (55/218) |
0.93 | 19% (82/441) |
21% (91/441) |
0.31 | 0.26 |
| Walking speed < 1m/s | 28% (60/217) |
41% (90/217) | 0.26 | 25% (109/444) |
36% (161/144) |
<0.0001 | 0.39 |
McNemar’s test of agreement (unadjusted)
Test of the relationship between changes in sarcopenia (and its components) and incident UI, adjusted for age, race, BMI, study site, diabetes status, hypertension status, and CVD status
Mean serum 25-hydroxyvitamin D concentrations at year 2 did not differ among women who developed UI versus those remaining continent at year 4 (Table 1). Specifically, the proportions of women with sufficient, insufficient, and deficient vitamin D status were similar among women with incident UI (34% deficient, 34% insufficient and 33% sufficient). Further, when we examined the association between 25-hydroxyvitamin D status and the odds of developing UI, 25-hydroxyvitamin D status was not significantly associated with incident UI [OR (95% CI): 1.1 (0.7, 1.6) and 1.1 (0.7, 1.6) for deficient vs insufficient/sufficient and insufficient vs. sufficient 25-hydroxyvitamin D status, respectively], adjusting for age, race, BMI, depression, site, and the season. Vitamin D status was also not independently associated with the developed of sub-types of UI (urgency or stress UI), p=0.39 controlling for race and BMI. Serum 25-hydroxyvitamin D concentrations were explored as a continuous variable and the lack of significant association remained.
Discussion
In this Health ABC longitudinal cohort of older initially well-functioning, continent women, we observed a significant decline in physical performance, specifically standing balance among in women who developed UI symptoms. The observation of a greater deterioration in physical performance scores among women with incident UI exceeded the minimally important change.(12) Declining skeletal muscle mass and strength, also known as sarcopenia was more prevalent among older women with incident UI. In addition, there was a higher risk of concomitant development of sarcopenia with incident UI. This finding may be a link between the decline in overall physical performance and standing balance observed in this cohort.
Standing balance depends on skeletal muscle function of the trunk, pelvic floor, as well as the lower extremities. The prospective observation of a significant decline in standing balance with incident UI confirms previous observations in cross-sectional studies. Fritel and colleagues assessed UI and motor-related physical abilities and reported that balance and gait impairments were independently associated with urgency UI.(20) They also demonstrated that walking speed and balance scores were lower with increasing severity of UI.(20) These data collaboratively may implicate poor standing balance as a potential clinical factor linking functional impairment and incident UI in women.
The role of sarcopenia as a potential link between functional impairment and development of UI in older women is under explored. Sarcopenia may impact skeletal muscle health important for urethral continence and physical performance. (21) Our data aligns with a previous analysis of the Health ABC cohort of women with baseline UI that reported greater odds of persistent or new onset of stress UI in women who had a ≥ 5% decrease in grip strength over 3 years.(22) In addition, the odds of persistent or new onset of stress UI was lower if women had a ≥ 5% increase in appendicular lean mass over 3 years. Collectively, this data supports the concept that markers of sarcopenia may be important clinical predictors for older women with UI.
We previously reported that low 25-hydroxyvitamin D [< 30 ng/mL] concentrations was more prevalent among women with UI symptoms and was associated with a greater negative impact of UI on daily life. (23) However, in this cohort, serum 25-hydroxyvitamin D status was not associated with the development of UI. In a previous Health ABC analysis, insufficient serum 25-hydroxyvitamin D was associated with poor physical performance over 4 years (5). Similar to our report, it was not associated with a greater decline in physical performance.(5) This study has three major strengths. First is the longitudinal, prospective design that provides unique opportunity to follow initially well-functioning women over time to observe objective changes in physical performance coincident with UI onset. Second, we analyzed a large ethnically-diverse cohort of women which increases the generalizability of our results. Third, we applied standardized collection of robust data on UI, physical performance, and sarcopenia measures at baseline and year 4 permitting more precise identification of the focal areas of functional impairment and determination of sarcopenia status.. The observational nature of the study is a limitation as causality cannot be determined regarding changes in physical performance or sarcopenia status and incident UI. The relationship between serum 25-hydroxyvitamin D concentrations and UI was not confirmed. It is possible that the single measurement at year 2 may explain this. However, it is standard practice to allow a single measurement of serum 25-hydroxyvitamin D to determined vitamin D status as the serum concentration remains stable without aggressive high dose supplementation. The exclusion of subjects, particularly men and women with baseline UI may weaken this analysis. However, in order to specifically target incident UI in women, these exclusions were necessary. Finally, the analysis was unable to definitively explore exactly when the onset of UI symptoms developed in this population because this was not the primary aim of the Health ABC study.
In conclusion, we observed a significant decline in objectively measured physical performance specifically standing balance among older women when they developed UI. Poor standing balance among women with UI may implicate unique clinical sub-type of pelvic floor muscle dysfunction. Sarcopenia is prevalent among older women who develop UI. Its presence reflects poor skeletal muscle health, and may be a clinical predictor linking functional impairment and UI in older women, two common and linked geriatric syndromes. The concomitant presentation of these linked geriatric syndromes is largely under-recognized, but is clinically important as it may impact management of UI in older women.
Erekson and colleagues found that older women with daily UI had a 3.3 greater odds of functional difficulties or dependence and 1.8 greater odds of lower mobility compared to continent older women in a cross-sectional analysis.(3) Our data aligns with this finding as we report a clinically important decline in SPPB scores among women who developed UI symptoms. This was not observed among women who remained continent. Further, Dargent-Molina and colleagues reported an independent association between the timed 6-m walk with urgency and stress UI in a prospective cohort. (24) Contrary to this study, we did not observe significant changes in walking speed associated with incidence of UI.
Acknowledgements:
The authors thank Karen Klein, MA for her editorial assistance, supported by the Wake Forest Clinical and Translational Science Institute (UL1 TR001420; PI: McClain).
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
Supported by the National Institute on Aging (contracts N01-AG-6–2101, N01-AG-6–2103, and N01-AG-6–2106); NIA grants R01 G028050; and the Wake Forest Older Americans Independence Center (P30 AG021332).
Footnotes
Presented at PFD Week 2016 the American Urogynecology Association’s national meeting, September 27- October 1, 2016, at the Colorado Convention Center in Denver, Colorado.
REFERENCES
- 1.Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, Markland AD. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstetrics and gynecology. 2014;123(1):141–8. Epub 2014/01/28. doi: 10.1097/aog.0000000000000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. Jama. 1995;273(17):1348–53. Epub 1995/05/03. [PubMed] [Google Scholar]
- 3.Erekson EA, Ciarleglio MM, Hanissian PD, Strohbehn K, Bynum JP, Fried TR. Functional Disability and Compromised Mobility Among Older Women With Urinary Incontinence. Female pelvic medicine & reconstructive surgery. 2014. Epub 2014/09/05. doi: 10.1097/spv.0000000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahat G, Tufan A, Tufan F, Kilic C, Akpinar TS, Kose M, Erten N, Karan MA, Cruz-Jentoft AJ. Cut-off points to identify sarcopenia according to European Working Group on Sarcopenia in Older People (EWGSOP) definition. Clinical nutrition. 2016. doi: 10.1016/j.clnu.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Houston DK, Tooze JA, Neiberg RH, Hausman DB, Johnson MA, Cauley JA, Bauer DC, Cawthon PM, Shea MK, Schwartz GG, Williamson JD, Tylavsky FA, Visser M, Simonsick EM, Harris TB, Kritchevsky SB. 25-hydroxyvitamin D status and change in physical performance and strength in older adults: the Health, Aging, and Body Composition Study. American journal of epidemiology. 2012;176(11):1025–34. Epub 2012/11/03. doi: 10.1093/aje/kws147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.L R. The CES-D Scale: a self-report depression scale for research in the general population.. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 7.Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourology and urodynamics. 2000;19(2):137–45. [DOI] [PubMed] [Google Scholar]
- 8.Jackson RA, Vittinghoff E, Kanaya AM, Miles TP, Resnick HE, Kritchevsky SB, Simonsick EM, Brown JS. Urinary incontinence in elderly women: findings from the Health, Aging, and Body Composition Study. Obstetrics and gynecology. 2004;104(2):301–7. Epub 2004/08/05. doi: 10.1097/01.AOG.0000133482.20685.d1. [DOI] [PubMed] [Google Scholar]
- 9.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. The New England journal of medicine. 1995;332(9):556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pahor M, Blair SN, Espeland M, Fielding R, Gill TM, Guralnik JM, Hadley EC, King AC, Kritchevsky SB, Maraldi C, Miller ME, Newman AB, Rejeski WJ, Romashkan S, Studenski S Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. The journals of gerontology Series A, Biological sciences and medical sciences. 2006;61(11):1157–65. Epub 2006/12/15. [DOI] [PubMed] [Google Scholar]
- 11.Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, Harris T, Health ABCSG. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56(10):M644–9. [DOI] [PubMed] [Google Scholar]
- 12.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society. 2006;54(5):743–9. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 13.Visser M, Fuerst T, Lang T, Salamone L, Harris TB. Validity of fan-beam dual-energy X-ray absorptiometry for measuring fat-free mass and leg muscle mass. Health, Aging, and Body Composition Study--Dual-Energy X-ray Absorptiometry and Body Composition Working Group. Journal of applied physiology. 1999;87(4):1513–20. [DOI] [PubMed] [Google Scholar]
- 14.Salamone LM, Fuerst T, Visser M, Kern M, Lang T, Dockrell M, Cauley JA, Nevitt M, Tylavsky F, Lohman TG. Measurement of fat mass using DEXA: a validation study in elderly adults. Journal of applied physiology. 2000;89(1):345–52. [DOI] [PubMed] [Google Scholar]
- 15.Lee WJ, Liu LK, Peng LN, Lin MH, Chen LK, Group IR. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. Journal of the American Medical Directors Association. 2013;14(7):528 e1–7. doi: 10.1016/j.jamda.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 16.McLean RR, Kiel DP. Developing consensus criteria for sarcopenia: an update. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2015;30(4):588–92. doi: 10.1002/jbmr.2492. [DOI] [PubMed] [Google Scholar]
- 17.Yu S, Appleton S, Chapman I, Adams R, Wittert G, Visvanathan T, Visvanathan R. An anthropometric prediction equation for appendicular skeletal muscle mass in combination with a measure of muscle function to screen for sarcopenia in primary and aged care. Journal of the American Medical Directors Association. 2015;16(1):25–30. doi: 10.1016/j.jamda.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Woo J, Leung J, Morley JE. Validating the SARC-F: a suitable community screening tool for sarcopenia? Journal of the American Medical Directors Association. 2014;15(9):630–4. doi: 10.1016/j.jamda.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine S. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism. 2011;96(7):1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 20.Fritel X, Lachal L, Cassou B, Fauconnier A, Dargent-Molina P. Mobility impairment is associated with urge but not stress urinary incontinence in community-dwelling older women: results from the Ossebo study. BJOG : an international journal of obstetrics and gynaecology. 2013;120(12):1566–72. Epub 2013/06/12. doi: 10.1111/1471-0528.12316. [DOI] [PubMed] [Google Scholar]
- 21.Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C. Effects of PFM rehabilitation on PFM function and morphology in older women. Neurourology and urodynamics. 2013;32(8):1086–95. Epub 2013/01/30. doi: 10.1002/nau.22370. [DOI] [PubMed] [Google Scholar]
- 22.Suskind AM, Cawthon PM, Nakagawa S, Subak LL, Reinders I, Satterfield S, Cummings S, Cauley JA, Harris T, Huang AJ, Health ABCS. Urinary Incontinence in Older Women: The Role of Body Composition and Muscle Strength: From the Health, Aging, and Body Composition Study. Journal of the American Geriatrics Society. 2017;65(1):42–50. doi: 10.1111/jgs.14545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parker-Autry CY, Markland AD, Ballard AC, Downs-Gunn D, Richter HE. Vitamin D status in women with pelvic floor disorder symptoms. International urogynecology journal. 2012;23(12):1699–705. doi: 10.1007/s00192-012-1700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Breart G. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348(9021):145–9. [DOI] [PubMed] [Google Scholar]