Abstract
Background:
Human papillomavirus (HPV) vaccination is expected to reduce HPV-related disease and cancer in the US. However, many parents are hesitant to obtain the vaccine for their children. The purpose of this study is to examine how the reasons for refusing the HPV vaccine vary across regions of the US, across time, and by race/ ethnicity.
Methods:
This study used data on 13–17 year old adolescents collected by the National Immunization Survey – Teen (NIS-Teen) annually between 2008 and 2016. We evaluated the frequencies of parents who did not intend to vaccinate their children in the next year among unvaccinated children. Among these non-intenders, we evaluated how reasons for HPV vaccine hesitancy changed across time, by region of the US, and race/ ethnicity.
Results:
The proportion of non-intenders among unvaccinated decreased from 72% in 2010 to 58% in 2016. The most frequent reason for vaccine hesitancy was that parents felt HPV vaccination was not necessary (22.4%), followed by lack of provider recommendation (16.2%), and lack of knowledge (15.6%). Lack of provider recommendation increased in frequency as a reason for HPV vaccine hesitancy until 2012, then decreased in frequency through 2016. Cost was one reason that was elevated in all regions compared to the Northeast. Black non-intenders were less likely to report safety, costs, or their children’s fear as reasons for not intending to vaccinate their children compared to white non-intenders. Hispanic non-intenders were more likely to report lack of knowledge and that the vaccine is not a school requirement as reasons not to vaccinate their children compared to white non-intenders.
Conclusions:
National advocacy for improving provider recommendation for HPV vaccination likely contributed to a sharp decline in HPV vaccine hesitancy due to lack of provider recommendation. Results indicate the need for multifaceted interventions to increase HPV vaccination.
Background
Human papillomaviruses (HPV) are associated with about 41,000 cases of cancer per year in the United States, and are a source of significant economic costs related to treatment and prevention [1, 2]. Although HPV vaccination can prevent HPV-related cancers and genital warts when administered before exposure, uptake in the US has been modest, and completion of the series inadequate in the target population of both males and females 11–26 years old. In 2016, only 37.5% of 13–17 year old males and 49.5% of 13–17 year old females were up to date on HPV vaccination, and coverage varies widely by location [3]. Although strong healthcare provider recommendation is the most important factor influencing HPV vaccine uptake, parents of adolescents continue to decide that they do not want their children to be vaccinated. Reasons for declining the vaccine have been explored and described by gender of the child [4], but little is known about how these reasons vary across region or by race/ ethnicity.
Interventions aiming to increase HPV vaccination were initially focused on increasing awareness about the vaccine [5]. More recently, interventions have targeted providers to increase recommendation to all eligible patients due to evidence that strong provider recommendation is the most important reason why parents choose to vaccinate their children, even when they were initially hesitant [6–8]. Related research provides evidence that combined provider and community interventions, in addition to removing cost barriers, are effective at increasing uptake of the HPV vaccine series [9, 10]. Nevertheless, vaccination rates remain suboptimal, and parents report several reasons for HPV vaccination hesitancy. Some common reasons that have been cited are that: parents think their children do not need the vaccine, inconsistent provider recommendation, and concerns about effectiveness and safety [11–13]. As interventions are implemented across the US, it is possible that reasons for HPV vaccine hesitancy have changed over time.
It is also unclear how reasons for vaccine hesitancy may vary across race/ ethnicity. For example, more black and Hispanic parents are concerned that vaccinating with the HPV vaccine will make their children think they are being permissive about sexual behavior compared to white parents [14]. Vaccine hesitancy among minority racial/ ethnic groups is particularly of concern, as HPV-related cervical and oral cancers may affect these groups disproportionately. In order to prevent disparities in these cancers from continuing, HPV vaccination needs to be encouraged among all adolescents at the recommended age of 11–12 years old. More information about how vaccine hesitancy varies in these higher-risk groups is needed to better understand which provider responses and interventions are appropriate to address these barriers. The purpose of this study was to examine how parents’ reasons for not vaccinating their children with the HPV vaccine vary by region, over time, and by race/ ethnicity.
Methods
This study used data collected by the National Immunization Survey – Teen (NIS-Teen) annually between 2008 and 2016. The NIS-Teen is a nationally representative telephone survey conducted by the Centers for Disease Control and Prevention (CDC) to determine the vaccination status of 13–17 year old US adolescents. Detailed methods for the NIS-Teen study are available elsewhere [15]. Briefly, the survey is conducted through calls to randomly selected landline and cell phone numbers. Parents refer to their children’s shot cards when available, and children’s health care providers are contacted to verify children’s vaccination status. This study was classified as exempt by the University of Texas Medical Branch Institutional Review Board.
If any of the 3 sources of data (self-report, shot cards, provider report) indicated that the child of responding parents received at least one dose of the HPV vaccine, their data were not included in this study. Participants with no regional information were also excluded from the study. If race/ ethnicity were not reported, then these values were imputed using methods described elsewhere [15].
Parents who answered “not too likely”, “not likely at all”, or “not sure/do not know” to the question, “How likely is it the teen will receive HPV vaccination in the next 12 months?” were considered to be parents who did not intend to vaccinate their children (non-intenders). This question was not available in 2008 and 2009, so parents were categorized as non-intenders only if they gave any reason to the question, “What is the MAIN reason [your teen] will not receive any HPV shots in the next 12 months?” during these years of the survey. Responses were dichotomized into binary outcomes, with 1 = response was selected by respondent and 0 = response was not selected by respondent. Each participant could select more than one reason for not intending to vaccinate their child. All non-intenders selected at least one reason for not intending to vaccinate their child between 2010 and 2016.
Regions for each of the included participants were calculated using the provided FIPS codes. These codes were changed to states in the US, which were then pooled into one of 4 Census regions, including: Northeast, Midwest, South, and West. Reasons for intent not to vaccinate were also evaluated by race/ethnicity. The races/ ethnicities of the children, which was reported by their parent or guardian (hereafter referred to as “parent”), were examined to determine whether reasons varied between the adolescent’s racial/ ethnic groups. We combined all participants who categorized their children as Hispanic into that group. Non-Hispanics were categorized as “white,” “black,” and “other.” The “other” group included American Indians, Alaska natives, Asians, Native Hawaiians, and Pacific Islanders.
Statistical analyses
We calculated all proportions using weights for the household survey, as provided by the NIS-Teen in the annual datasets. We calculated frequencies for each of the reasons for non-vaccination among non-intenders for each survey year. We charted weighted proportions of reasons which exceeded 5% of the sample in graphs annually between 2008 and 2016 using “smoothing splines.” We also charted the reason, “child is male” across time, as estimates were equal to 0 in the first 2 years due to the timing of guidelines for HPV vaccination among males, and exceeded 5% of the sample between 2010 and 2016. To determine change across time, we calculated unadjusted prevalence ratios comparing 2016 with 2008 for each of the reasons for no intent to vaccinate. We used Joinpoint Regression Program, version 4.6.0.0, to conduct joinpoint regression analyses to determine significant changes during the time period examined. We only conducted these analyses on reasons for not intending to vaccinate which did not have significant differences between 2008 and 2016 estimates. We conducted a sensitivity analysis excluding the 2008 and 2009 years to determine whether our results were the same for 2010 through 2016 as compared to including all data. These analyses were done to ensure that the different methods necessary for inclusion of 2008 and 2009 data did not significantly affect the results. Further, HPV vaccination was not measured for males during those years, which may have also changed the results.
Bivariate analyses were conducted using Rao Scott Chi-Square comparisons of weighted frequencies. Weighted proportions of reasons for not intending to vaccinate were examined by region, across time, and by race/ethnicity. Reasons which were significantly different in bivariate analyses were included as dependent variables in final log-binomial regression models if the counts for all cells were ≥10. We obtained weighted prevalence ratios (PRs) using log-binomial regression to compare reasons for not intending to vaccinate by region and race/ethnicity after controlling for child’s sex, survey year, parent’s education level, region, and poverty level. Finally, we utilized logistic regression models to evaluate potential interactions between region and time for variables which showed significant differences by region and across time to determine whether changes across time were different by region. This analysis allowed us to determine whether the results were due mainly to changes occurring in one particular region of the US. SAS statistical software version 9.4 (Cary, NC) was used to conduct these analyses.
Results
Between 2008 and 2016, the parents of 158,896 females and 173,515 males were surveyed (Supplemental figure 1). In total, 143,721 parents had information on region of residence and provided information on their intention to vaccinate their child. Among participants who were surveyed between 2008 and 2009, we included those that were unvaccinated. Among those with complete information, 89,984 (62.6%) had records provided by their healthcare provider, 26,794 (18.6%) used shot card records, and 26,943 (18.7%) were self-report only. Of those who provided information about intention to vaccinate, 90,866 indicated that they did not intend to vaccinate (non-intenders) their children (63.2%) or responded to a question about why they would not vaccinate their child in the next 12 months in the 2008 and 2009 data. Among the non-intenders, 55% had male children while 51% of parents of unvaccinated children responded for a male adolescent (Table 1). There were differences in the proportion of non-intenders among parents of unvaccinated children by region, race of the adolescent, and the education level of the mother. In addition, the proportion of non-intenders among all parents of unvaccinated children varied over time. The proportion of non-intenders decreased after 2010, from about 72% of unvaccinated in 2010 to 58% of unvaccinated in 2016 (Supplemental figure 2).
Table 1.
Characteristics of participated unvaccinated 13–17-year-old children in NIS-Teen from 2008–2016 (N=143,721).
| All (N=143,721) |
No intention to vaccinate (n=90,866) |
Unvaccinated (n=52,855) |
P-value | |
|---|---|---|---|---|
| Mean (se) | Mean (se) | Mean (se) | ||
| Age in years of teen | 14.9 (0.01) | 15.0 (0.01) | 14.9 (0.01) | |
| Frequency (w%) | Frequency (w%) | Frequency (w%) | ||
| Sex of adolescent | <0.001 | |||
| Male | 79466 (53.6) | 52095 (55.1) | 27371(51.2) | |
| Female | 64255 (46.4) | 38771 (44.9) | 25484(48.8) | |
| Race of adolescent | <0.001 | |||
| Hispanic | 19117 (18.9) | 9952 (15.3) | 9165 (24.6) | |
| Non-Hispanic White only | 97056 (59.2) | 64385 (63.9) | 32671 (51.7) | |
| Non-Hispanic Only | 15043 (14.0) | 8759 (13.0) | 6284 (15.7) | |
| Non-Hispanic other and multi | 12505 (7.9) | 7770 (7.8) | 4735 (8.0) | |
| Region | <0.001 | |||
| Northeast | 24486 (16.0) | 14983 (15.9) | 9503 (16.2) | |
| Midwest | 31806 (22.7) | 20685 (23.7) | 11121 (21.1) | |
| South | 54292 (38.2) | 33702 (37.9) | 20590 (38.8) | |
| West | 33137 (23.1) | 21496 (22.5) | 11641 (23.9) | |
| Education level of mother | <0.001 | |||
| Less than 12 years | 13393 (13.1) | 6363 (9.5) | 7030 (18.8) | |
| 12 years | 27512 (25.2) | 16855 (24.3) | 10657 (26.6) | |
| More than 12 years, non-college graduate | 41623 (26.4) | 27421 (28.2) | 14202 (23.5) | |
| College graduate | 61193 (35.3) | 40227 (38.0) | 20966 (31.1) |
se = standard error, w% = Percent weighted to account for sampling methods
Among 90,866 non-intenders, the most frequent reason for not intending to vaccinate their child was that parents felt HPV vaccination was not necessary (22.4%), followed by lack of provider recommendation (16.2%), and lack of knowledge (15.6%, Supplemental table 1). Reasons for HPV vaccine refusal did have some significant regional variations in the US. Compared to the Northeast, parents in the Midwest, South, and West were less likely to report “provider did not recommend”, while non-intenders in the South were less likely to report that their child was not the appropriate age, and those in the West were less likely to report safety concerns as a reason for not intending to vaccinate their children (Supplemental table 2). Non-intenders in the Midwest were more likely to report that they had a lack of knowledge about the vaccine compared to parents in the Northeast. Concerns related to time and cost were more likely to be reported in the Midwest, South, and West compared to the Northeast. Non-intenders in the Midwest, South and West were more likely to report that the HPV vaccine was not required for school than parents living in the Northeast, and non-intenders in the West were less likely to report that their child is male as a reason for not intending to vaccinate compared to the Northeast region.
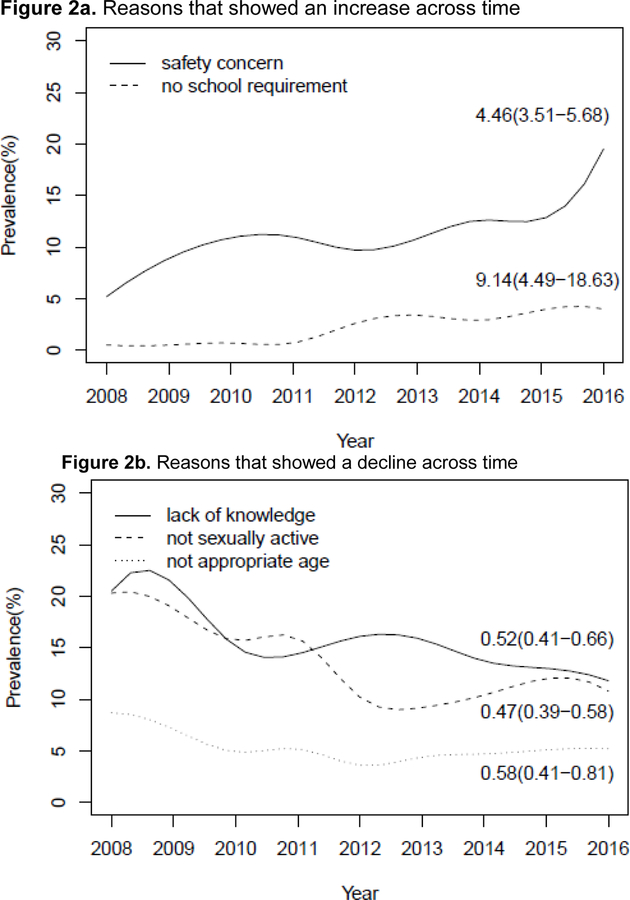
Joinpoint analyses revealed that there were no significant points of change in the frequency of parents who reported that the vaccine was not needed among those who did not intend to vaccinate their children (results not shown). However, we noted a joinpoint in the frequency of non-intenders reporting “provider did not recommend” for the vaccine. Specifically, we found that the prevalence of this reason increased until 2012, when it experienced a sharp decrease in prevalence as a reason for not intending to vaccinate (Figure 1). The prevalence of concerns about safety (PaOR: 4.46, 95% confidence interval (CI): 3.51–5.68) and lack of school entry requirements (PaOR: 9.14, 95% CI: 4.49–18.63) for the HPV vaccine increased significantly as reasons why parents did not intend to vaccinate their children between 2008 and 2016 (Figure 2). Conversely, lack of knowledge about the HPV vaccine, statements that their child was not sexually active, and feeling that their child was not the appropriate age decreased across time. Interactions between region and time were significant for the odds of parents reporting that the vaccine was not recommended (p=0.001) and for parents who felt that safety concerns (p=0.005) kept them from vaccinating their child (supplemental figure 3).
Figure 1.
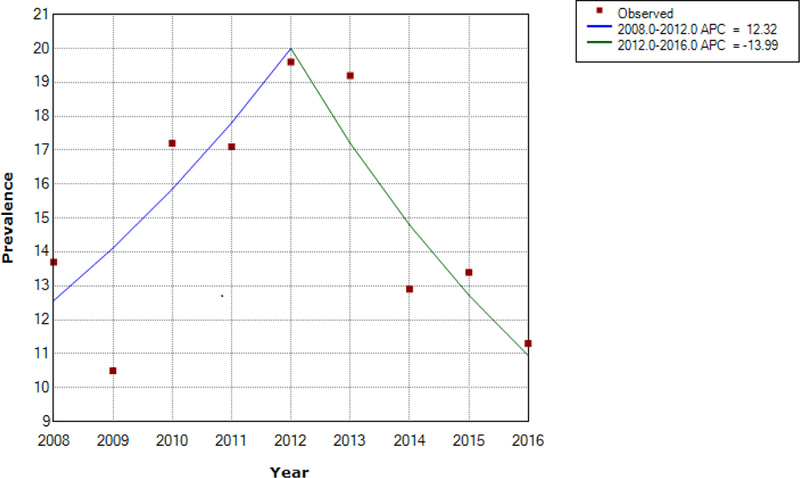
Joinpoint regression analysis of frequency of parents of unvaccinated 13–17 year olds who indicated the HPV vaccine was not recommended as reason for not intending to vaccinate their children (N=90,866)
^ Indicates that the Annual Percent Change (APC) is significantly different from zero at the alpha = 0.05 level. Final Selected Model: 1 Joinpoint.
Figure 2.
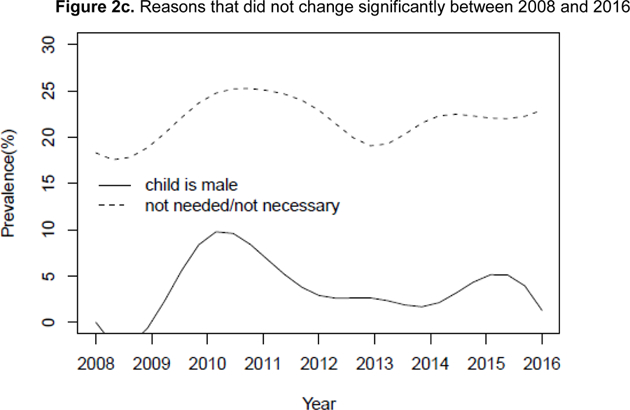
Spline-smoothed line graphs showing change across time for reasons parents do not intend to vaccinate among 13–17 year old children of non-intenders (2008–2016) (N=90,866)
There were several differences observed in bivariate analyses between race/ ethnicity and reasons for not intending to vaccinate (Table 2). Reasons for not intending to vaccinate that varied by racial/ ethnic group included: the HPV vaccine is not needed or not necessary, it was not recommended, lack of knowledge, their child is not sexually active, safety concerns or side effects, child is not the appropriate age, their child is male, family or parental decision, cost, not a school requirement, their child is fearful, and that the shot should be administered for college. Sensitivity analyses revealed no differences when data from 2008 and 2009 were removed.
Table 2.
Parent reasons for no intent for HPV vaccination among 13–17 year old adolescents by race/ethnicity (2008–2016) (N=90,866)
| Total (N=90,866) |
Non-Hispanic White only (n= 64,385) |
Hispanic (n= 9,952) |
Non-Hispanic Black only (n= 8,759) |
Non-Hispanic Other race (n= 7,770) |
P-value | |
|---|---|---|---|---|---|---|
| Freq (w%) | Freq (w%) | Freq (w%) | Freq (w%) | Freq (w%) | ||
| Not needed or not necessary | 19903 (22.4) | 14481 (22.9) | 1853 (19.8) | 1927 (23.4) | 1642 (21.3) | 0.0003 |
| Provider did not recommend | 13837 (16.2) | 9384 (15.1) | 1660 (18.7) | 1381 (16.5) | 1412 (20.0) | <0.001 |
| Lack of knowledge | 12802 (15.6) | 8411 (14.1) | 1767 (20.0) | 1479 (17.7) | 1145 (16.2) | <0.001 |
| Teen is not sexually active | 12199 (13.7) | 9043 (14.6) | 1111 (10.2) | 1085 (13.3) | 960 (13.0) | <0.001 |
| Safety concerns | 9736 (10.8) | 7122 (11.4) | 1020 (9.9) | 870 (9.8) | 724 (9.3) | 0.001 |
| Not appropriate age/ provider indicated could vaccinate at older age | 4554 (5.1) | 3357 ( 5.5) | 468 (4.6) | 344 (4.1) | 385 (4.6) | 0.003 |
| Child is male | 4002 (5.1) | 3053 (5.5) | 312 (3.3) | 354 (4.9) | 283 (4.8) | <0.001 |
| Family/parental decision | 2798 (3.2) | 1966 (3.1) | 267 (2.8) | 353 (4.3) | 212 (3.1) | 0.001 |
| More info/new vaccine | 2038 (2.3) | 1517 (2.5) | 183 (2.1) | 201 (2.3) | 137 (1.8) | 0.28 |
| Other reason | 1610 (1.8) | 1119 (1.8) | 192 (1.9) | 159 (1.8) | 140 (1.6) | 0.92 |
| Costs or underinsured | 1458 (1.8) | 1035 (1.7) | 221 (2.7) | 82 (1.2) | 120 (1.6) | <0.001 |
| Not a school requirement | 1566 (1.8) | 1028 (1.6) | 220 (2.5) | 159 (1.8) | 159 (2.3) | 0.002 |
| Child fearful | 977 (1.2) | 737 (1.3) | 99 (1.2) | 59 (0.5) | 82 (1.2) | 0.01 |
| Child should make decision | 891 (1.1) | 587 (1.0) | 140 (1.4) | 89 (1.2) | 75 (0.9) | 0.17 |
| Don’t believe in immunizations | 744 (0.9) | 545 (0.9) | 77 (0.7) | 74 (1.2) | 48 (0.6) | 0.07 |
| No doctor or doctor’s visit not scheduled | 754 (0.9) | 548 (0.8) | 94 (0.9) | 66 (1.1) | 46 (0.7) | 0.46 |
| Handicapped/special needs/illness | 616 (0.6) | 454 (0.7) | 71 (0.6) | 45 (0.5) | 46 (0.6) | 0.42 |
| Religion/orthodox | 529 (0.6) | 410 (0.7) | 49 (0.5) | 22 (0.3) | 48 (0.7) | 0.18 |
| Already planned | 17 (0.5) | 12 (0.3) | 0 | 2 (0.6) | 3 (3.1) | NA |
| Concern about increasing sexual activity | 378 (0.4) | 284 (0.4) | 37 (0.3) | 27 (0.2) | 30 (0.3) | 0.08 |
| Effectiveness concern | 284(0.3) | 217 (0.3) | 32 (0.3) | 22 (0.3) | 13 (0.2) | 0.60 |
| Already up-to date | 175 (0.2) | 109 (0.2) | 27 (0.2) | 23 (0.3) | 16 (0.3) | 0.21 |
| College shot | 68 (0.1) | 57 (0.1) | 4 (0.02) | 2 (0.001) | 5 (0.1) | 0.01 |
| Time | 84 (0.1) | 55 (0.1) | 16(0.1) | 6 (0.1) | 7 (0.03) | 0.49 |
| Vaccine not available in provider’s office | 113 (0.1) | 70 (0.1) | 19 (0.1) | 6 (0.1) | 18 (0.1) | 0.96 |
| Already sexually active | 31 (0.1) | 19 (0.1) | 5 (0.03) | 4 (0.1) | 3 (0.1) | 0.79 |
| No ob/gyn | 24 (0.04) | 20 (0.04) | 4 (0.07) | 0 | 0 | NA |
w% = Percent weighted to account for sampling methods, Freq = Frequency
We found some racial/ ethnic differences in reasons for not intending to vaccinate their children persisted after controlling for the child’s sex, survey year, mother’s education level, region, and poverty level (Table 3). A higher prevalence of Hispanic non-intenders reported the vaccine was not recommended, lack of knowledge, and that the vaccine is not a school requirement as reasons for deciding not to vaccinate their children compared to parents of white children. A lower prevalence of Hispanics noted that it was not needed or that their child was not male compared to parents of white children. A higher prevalence of non-Hispanic black non-intenders cited it was not recommended, lack of knowledge, or that it was a family or parental decision as reasons for not intending to vaccinate their children. However, a lower prevalence reported that safety, that their child was not the appropriate age, costs, or their children’s fear as reasons for not intending to vaccinate their children compared to white non-intenders. The most notable differences were observed between white and “other” non-intenders. A higher prevalence of parents of children who did not identify as Hispanic, black, or white reported that the vaccine was not recommended or that they had a lack of knowledge as reasons for not intending to vaccinate their children compared to white non-intenders. However, a lower prevalence of the same group had safety concerns as a reason not to vaccinate compared to white non-intenders. These results were the same in sensitivity analyses which removed 2008 and 2009 from the analyses.
Table 3.
Adjusted* log-binomial models of reasons for not intending to HPV vaccinate children by race/ethnicity among adolescents aged 13–17 (2008 to 2016) (N=90,866)
| Non-Hispanic White only (n= 64,385) |
Hispanic (n= 9,952) |
Non-Hispanic Black only (n= 8,759) |
Non-Hispanic Other race (n= 7,770) |
|
|---|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Not needed or not necessary (22.4) | Reference | 0.89 (0.82, 0.97) | 1.05 (0.98, 1.13) | 0.94 (0.87, 1.02) |
| Not recommended (16.2) | Reference | 1.16 (1.06, 1.27) | 1.10 (1.01, 1.20) | 1.33(1.22, 1.45) |
| Lack of knowledge (15.6) | Reference | 1.29 (1.18, 1.40) | 1.21 (1.11, 1.32) | 1.15 (1.03, 1.27) |
| Not sexually active (13.7) | Reference | 0.76 (0.67, 0.85) | 0.91 (0.82, 1.01) | 0.91 (0.82, 1.01) |
| Safety concern/side effects (10.8) | Reference | 0.96 (0.85, 1.09) | 0.83 (0.75, 0.93) | 0.81 (0.71, 0.92) |
| Not appropriate age | Reference | 0.91 (0.76, 1.10) | 0.80 (0.67, 0.96) | 0.85 (0.72, 1.01) |
| Child is male | Reference | 0.71 (0.58, 0.86) | 0.93 (0.78, 1.10) | 1.02 (0.83, 1.25) |
| Family/parental decision | Reference | 1.05 (0.83, 1.33) | 1.42 (1.18, 1.72) | 1.03 (0.80, 1.32) |
| Costs | Reference | 1.14 (0.89, 1.45) | 0.56 (0.40, 0.79) | 0.84 (0.61, 1.15) |
| Child fearful | Reference | 0.76 (0.48, 1.20) | 0.37 (0.25, 0.56) | 0.83 (0.55, 1.24) |
| Not a school requirement | Reference | 1.38 (1.07, 1.78) | 1.20 (0.91, 1.60) | 1.36 (0.97, 1.92) |
Controlled for gender of child, year of enrollment, mother’s education level, region, poverty level
aPR=Adjusted Prevalence ratio, 95% CI=95% confidence interval
Discussion
Overall, this study found that common reasons non-intenders do not vaccinate their children have changed in frequency over time. For example, we found that reasons related to knowledge about the vaccine, child is not yet sexually active, and child is not the appropriate age, decreased as reasons why non-intenders do not vaccinate their children. Several interventions addressing lack of knowledge have been implemented, and the decrease in frequency of lack of knowledge as a reason for not intending to vaccinate across time demonstrates the success of increasing awareness of the HPV vaccine [10].
Our data indicates that “age” and “child is not sexually active” have decreased in frequency as reasons not to vaccinate across time. This is promising, because HPV vaccine series completion is lower among adolescents who initiate at older ages compared to those who initiate at an earlier age, which could potentially limit the effectiveness of the vaccine at the population-level [16]. However, the observed decrease in frequency of non-intenders responding that their child is not sexually active or is not the appropriate age as reasons for not intending to vaccinate reflects improved educational outreach and evidence that the vaccine is not associated with increased sexual behavior [17, 18].
Conversely, safety concerns related to the HPV vaccine increased as a reason not to vaccinate across the time period examined. Efforts of vaccination opponents have promulgated worries about the vaccine’s safety and attempted to increase concerns about the vaccine promoting sexual promiscuity [19]. Although face-to-face interventions may improve HPV vaccination uptake in populations with high lack of awareness about the vaccine, areas with high levels of vaccine hesitancy due to worries about safety may be more difficult to address [20]. Our results illustrate the lingering effect of efforts to discredit the HPV vaccine.
Other reasons for not intending to vaccinate that may not have easy interventions, such as not believing in the vaccine or religious reasons, comprised an extremely small proportion of the parents who did not intend to vaccinate their children. The most common reason, which was belief that the vaccine is not needed, is potentially difficult to address as well. It is possible that this response may represent a personal conviction of the children’s’ parents about the HPV vaccine, but it is also possible that it could be addressed through improving knowledge. Patient education is known to increase vaccination even when used alone as an intervention [10]. More research is needed to improve the understanding about why parents feel that their children do not need the vaccine, and to help understand how these reasons have changed over time. Interventions to address these reasons need to be adaptable in responding to changes in population beliefs and behaviors in order to achieve long-term success [11].
The results from this study also demonstrated a response to increased national awareness of the need for strong provider recommendation. Provider recommendation has been highly associated with HPV vaccine acceptability and uptake in the US, and physician recommendation has been shown to have had the greatest impact on HPV vaccine uptake [21, 22]. Sustained efforts by professional organizations, such as the American Academy of Pediatrics and American Academy of Family Physicians, to encourage their members to provide strong recommendations to their patients have had an impact on provider HPV vaccine communication strategies [23]. The sharp decline in prevalence of “provider did not recommend” as a reason for declining the vaccine after 2012 combined with the downward trend in the prevalence of non-intenders among unvaccinated adolescents after 2010 may have been at least partially attributed to increased provider recommendation to patients in the US.
Many of the common reasons for no intent to vaccinate varied by race/ethnicity. In particular, it is concerning that provider recommendation is one of these. Prevalence ratios indicate that this reason was particularly high among those who were in the “Non-Hispanic Other” race/ethnicity category. It is possible that providers who predominantly serve patients from ethnic backgrounds other than Hispanic or black need education about strongly recommending the vaccine, or may have difficulty communicating with these patients due to language or cultural barriers [24–28]. It is also concerning that disparity in prevalence of the lack of knowledge as a reason to not vaccinate adolescents among racial/ethnic minorities was found. Hispanic and black women suffer a disproportionate incidence of cervical cancer compared to white women, and black women have lower 5-year survival after diagnosis [29–31]. These disparities may remain if HPV vaccination is not recommended early enough. Increased provider education and culturally appropriate community and patient level interventions may be useful in addressing the more prevalent reasons for not intending to vaccinate adolescents among these groups [14, 32, 33]. Additionally, the differences observed indicate that there may be a need to target interventions by race/ ethnicity.
It was particularly interesting that some reasons for vaccine hesitancy were less likely to be mentioned among parents of black adolescents compared to parents of white adolescents, after controlling for demographics and socioeconomic status. Black parents had lower likelihood of citing safety concerns, cost, and that their child was fearful of the vaccine compared to parents of white adolescents. In the early post-licensure years after the vaccine was introduced to the US, cost was one of the common barriers to HPV vaccination that was cited [34]. Since then, the Affordable Care Act and Vaccines for Children program have ensured that costs would no longer be a barrier, and may have contributed to recent findings that vaccine initiation is higher among adolescent minorities compared to white adolescents [35].
Our findings were similar to a recent published study which found significantly decreased frequencies in reasons for not intending to vaccinate for all reasons except “not needed,” “lack of knowledge,” “not recommended,” and “not appropriate age [4].” Similar to our findings, concern about safety and side effects were increased among non-intenders as a reason for not vaccinating in 2016 compared to 2010 [4]. While the previous study compared results between 2 time periods – 2010 and 2016 – our study considered changes during the entire observed time period using joinpoint analyses for those outcomes that had no differences between 2008 and 2016. Thus, we were able to report the strong increase in prevalence of reporting that the vaccine had not been recommended among non-intenders, followed by a significant decrease after 2012. This was an important finding, as it demonstrates the importance of education programs focused on increasing provider recommendation.
There were some differences in reasons why parents do not intend to vaccinate by region, but most were small and unlikely to impact regional programs focused on increasing HPV vaccination. However, it appeared that cost was one reason that was elevated in all regions compared to the Northeast. Campaigns that are focused on helping parents to understand that the HPV vaccine is covered under the Vaccines for Children program could improve vaccination in those regions, particularly in the South, which has higher rates of HPV-related cancers, and lower rates of HPV vaccination.
This study had several strengths. It was conducted using a repeated cross-sectional nationally representative data set, which means that it was representative of the US. Further, many of the participants reviewed shot cards or had provider records for their children’s HPV vaccination status, which reduced recall bias for self-report of vaccination. However, our study did have some limitations. During the 2008 and 2009 years, we observed much lower frequencies of non-intenders among unvaccinated adolescents compared to the subsequent years. This could be due to the vaccine being relatively new to the market, but was more likely due to differences in the measurement of non-intenders during that period.
In conclusion, many of the reasons that parents do not intend to vaccinate their adolescent children can be addressed through intervention programs, as a low frequency of participants cited personal beliefs (family decision or religion), which may not be as amenable to intervention. Although the results from this study improve understanding of the reasons that the vaccine is refused, the most effective interventions need to be multifaceted, and work at several levels, in order to increase the HPV vaccination rates in the US [36]. This study also demonstrates that intervening on a common reason (lack of provider recommendation) for not intending to vaccinate children with the HPV vaccine can be successful when awareness and specific recommendations to address the issue on a national level are made.
Supplementary Material
Supplemental figure 1. Flow chart of NIS-Teen participants included, 2008–2016
Supplemental figure 2. Proportion of HPV vaccine non-intenders among unvaccinated 13–17 year olds across time, 2008–2016 (N=143,721)
Supplemental figure 3. Changes in prevalence of “not recommended” and “safety concern/side effects” as reasons for not intending to vaccinate with the HPV vaccine across time by region, NIS-Teen (2008–2016)
Acknowledgments
Funding
E.L. Fuchs is a Scholar supported by a research career development award (K12HD052023: Building Interdisciplinary Research Careers in Women’s Health Program –BIRCWH; Principal Investigator: Berenson) from the Office of Research on Women’s Health (ORWH), the Office of the Director (OD), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) at the National Institutes of Health. The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Research Data Center, the National Center for Health Statistics, or the Centers for Disease Control and Prevention. The sponsors did not have any role in the study design, collection, analysis, and interpretation of the data or any other aspect of this study or manuscript.
Footnotes
Conflicts of interest:
The authors have no conflicts of interest to report.
Contributor Information
Jacqueline M. Hirth, Department of Obstetrics & Gynecology, Center for Interdisciplinary Research in Women’s Health, University of Texas Medical Branch.
Erika L. Fuchs, Center for Interdisciplinary Research in Women’s Health, Department of Obstetrics & Gynecology, University of Texas Medical Branch.
Mihyun Chang, Center for Interdisciplinary Research in Women’s Health, Department of Obstetrics & Gynecology, University of Texas Medical Branch.
Maria E. Fernandez, Health Promotion and Behavioral Sciences, Director, Center for Health Promotion and Prevention Research, University of Texas Health Science Center at Houston.
Abbey B. Berenson, Department of Obstetrics & Gynecology, Director, Center for Interdisciplinary Research in Women’s Health, University of Texas Medical Branch.
References
- [1].Chesson HW, Blandford JM, Gift TL, Tao G, Irwin KL. The estimated direct medical cost of sexually transmitted diseases among American youth, 2000. Perspectives on Sexual and Reproductive Health 2004;36:11–9. [DOI] [PubMed] [Google Scholar]
- [2].Centers for Disease Control and Prevention (CDC). Cancers associated with human papillomavirus by state, 2010–2014 Atlanta, GA: 2018. [Google Scholar]
- [3].Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2016. MMWR Morb Mortal Wkly Rep 2017;66:874–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Beavis A, Krakow M, Levinson K, Rositch AF. Reasons for Lack of HPV Vaccine Initiation in NIS-Teen Over Time: Shifting the Focus From Gender and Sexuality to Necessity and Safety. Journal of Adolescent Health 2018;63:652–6. [DOI] [PubMed] [Google Scholar]
- [5].Fu LY, Bonhomme L-A, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: A systematic review. Vaccine 2014;32:1901–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Smith P, Stokley S, Bednarczyk R, Orenstein W, Omer S. HPV vaccination coverage of teen girls: The influence of health care providers. Vaccine 2016;34:1604–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Dorell C, Yankey D, Kennedy A, Stokley S. Factors That Influence Parental Vaccination Decisions for Adolescents, 13 to 17 Years Old: National Immunization Survey–Teen, 2010. Clinical Pediatrics 2012;52:162–70. [DOI] [PubMed] [Google Scholar]
- [8].Shay LA, Baldwin AS, Betts AC, Marks EG, Higashi RT, Street RL, et al. Parent-Provider Communication of HPV Vaccine Hesitancy. Pediatrics 2018;141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Niccolai LM, Hansen CE. Practice- and community-based interventions to increase human papillomavirus vaccine coverage: A systematic review. JAMA Pediatrics 2015;169:686–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Human Vaccines & Immunotherapeutics 2016;12:1566–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gilkey MB, Calo WA, Marciniak MW, Brewer NT. Parents who refuse or delay HPV vaccine: Differences in vaccination behavior, beliefs, and clinical communication preferences. Human Vaccines & Immunotherapeutics 2017;13:680–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among us adolescents: A systematic review of the literature. JAMA Pediatrics 2014;168:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Thompson EL, Rosen BL, Vamos CA, Kadono M, Daley EM. Human Papillomavirus Vaccination: What Are the Reasons for Nonvaccination Among U.S. Adolescents? Journal of Adolescent Health 2017;61:288–93. [DOI] [PubMed] [Google Scholar]
- [14].Galbraith KV, Lechuga J, Jenerette CM, Moore LTCAD, Palmer MH, JB Hamilton. Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: A literature review. Social Science & Medicine 2016;159:116–26. [DOI] [PubMed] [Google Scholar]
- [15].Centers for Disease Control and Prevention (CDC). National Immunization Surveys (NIS) In: Centers for Disease Control and Prevention (CDC), editor. p. https://www.cdc.gov/vaccines/imz-managers/nis/about.html.
- [16].Beachler DC, Gonzales FA, Kobrin SC, Kreimer AR. HPV vaccination initiation after the routine-recommended ages of 11–12 in the United States. Papillomavirus Research 2016;2:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Rysavy MB, Kresowik JDK, Liu D, Mains L, Lessard M, Ryan GL. Human Papillomavirus Vaccination and Sexual Behavior in Young Women. Journal of Pediatric and Adolescent Gynecology 2014;27:67–71. [DOI] [PubMed] [Google Scholar]
- [18].Mullins TLK, Widdice LE, Rosenthal SL, Zimet GD, Kahn JA. Risk perceptions, sexual attitudes, and sexual behavior after HPV vaccination in 11–12 year-old girls. Vaccine 2015;33:3907–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Whelan AM. Lowering the Age of Consent: Pushing Back against the Anti-Vaccine Movement. The Journal of Law, Medicine & Ethics 2016;44:462–73. [DOI] [PubMed] [Google Scholar]
- [20].Kaufman J, Ryan R, Walsh L, Horey D, Leask J, Robinson P, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database of Systematic Reviews 2018. [DOI] [PMC free article] [PubMed]
- [21].Zimet GD. Improving adolescent health: Focus on HPV vaccine acceptance. J Adolesc Health 2005;37. [DOI] [PubMed] [Google Scholar]
- [22].Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, et al. Parents’ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open 2018;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hswen Y, Gilkey MB, Rimer BK, Brewer NT. Improving physician recommendations for HPV vaccination: The role of professional organizations. Sexually transmitted diseases 2017;44:42–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Lee H, Kim D, Kiang PN-c, Cooley ME, Shi L, Thiem L, et al. Awareness, knowledge, social norms, and vaccination intentions among Khmer mother–daughter pairs. Ethnicity & Health 2018:1–13. [DOI] [PubMed]
- [25].Kim M, Lee H, Kiang P, Kim D. Human Papillomavirus: A qualitative study of Korean American female college students’ attitudes toward vaccination. Clinical Journal of Oncology Nursing 2017;21:e239–e47. [DOI] [PubMed] [Google Scholar]
- [26].Hopfer S, Garcia S, Duong HT, Russo JA, Tanjasiri SP. A Narrative Engagement Framework to Understand HPV Vaccination Among Latina and Vietnamese Women in a Planned Parenthood Setting. Health Education & Behavior 2017;44:738–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yzer M, Rhodes K, McCann M, Harjo J, Nagler RH, LoRusso SM, et al. Effects of cultural cues on perceptions of HPV vaccination messages among parents and guardians of American Indian youth. Preventive Medicine 2018;115:104–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Schmidt-Grimminger D, Frerichs L, Black Bird AE, Workman K, Dobberpuhl M, Watanabe-Galloway S. HPV Knowledge, Attitudes, and Beliefs Among Northern Plains American Indian Adolescents, Parents, Young Adults, and Health Professionals. Journal of Cancer Education 2013;28:357–66. [DOI] [PubMed] [Google Scholar]
- [29].Henley SJ, Singh SD, King J, Wilson RJ, O’Neil ME, Ryerson AB. Invasive Cancer Incidence and Survival — United States, 2013. MMWR Morb Mortal Wkly Rep 2017;66:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, et al. Human Papillomavirus–Associated Cancers — United States, 2008–2012. MMWR Morb Mortal Wkly Rep 2016;65:661–6. [DOI] [PubMed] [Google Scholar]
- [31].Singh GK, Jemal A. Socioeconomic and Racial/Ethnic Disparities in Cancer Mortality, Incidence, and Survival in the United States, 1950–2014: Over Six Decades of Changing Patterns and Widening Inequalities. Journal of Environmental and Public Health 2017;2017:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, et al. Interventions to Improve HPV Vaccine Uptake: A Systematic Review. Pediatrics 2016;138. [DOI] [PubMed] [Google Scholar]
- [33].Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers’ human papillomavirus vaccine knowledge. Human Vaccines & Immunotherapeutics 2015;11:1331–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: A systematic review. Preventive Medicine 2014;58:22–32. [DOI] [PubMed] [Google Scholar]
- [35].Agénor M, Pérez AE, Peitzmeier SM, Borrero S. Racial/ethnic disparities in human papillomavirus vaccination initiation and completion among U.S. women in the post-Affordable Care Act era. Ethnicity & Health 2018:1–15. [DOI] [PubMed]
- [36].Beavis AL, Levinson KL. Preventing Cervical Cancer in the United States: Barriers and Resolutions for HPV Vaccination. Frontiers in Oncology 2016;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental figure 1. Flow chart of NIS-Teen participants included, 2008–2016
Supplemental figure 2. Proportion of HPV vaccine non-intenders among unvaccinated 13–17 year olds across time, 2008–2016 (N=143,721)
Supplemental figure 3. Changes in prevalence of “not recommended” and “safety concern/side effects” as reasons for not intending to vaccinate with the HPV vaccine across time by region, NIS-Teen (2008–2016)