Abstract
The present longitudinal study examined the relationship between patterns of cigarette smoking and alcohol use during adolescence and illicit drug abuse (DA) and prescription drug abuse (PDA) in early adulthood. The sample consisted of 984 predominantly minority young adults (57% women) who completed (a) six annual surveys as adolescents attending New York City public schools (grades 7 through 12) and (b) a follow-up telephone interview as young adults (mean age = 23). Findings from a series of latent growth models indicated that growth in cigarette smoking and alcohol use during adolescence each independently predicted DA in adulthood. Baseline levels of alcohol use in 7th grade also predicted DA in adulthood. Growth in alcohol consumption during adolescence predicted PDA in young adulthood. Results indicate that an escalation during adolescence in the use of substances that are legal for adults (cigarettes and alcohol) contributes to greater DA and PDA in young adulthood. One implication of these findings is that interventions that can prevent cigarette smoking and alcohol use during adolescence may also reduce DA and PDA in young adults.
Epidemiologic data indicate that prevalence rates of alcohol and substance use, abuse, and disorder in the United States typically reach a peak during the transition from adolescence to adulthood. Peak rates occur as young people often begin to experience new freedoms, such as reaching the legal drinking age and living independently from parents, but have not yet fully taken on responsibilities related to career and family (Bachman, Wadsworth, O’Malley, Johnston, & Schulenberg, 1997). According to the most recent National Survey on Drug Use and Health (NSDUH), participants aged 18 to 25 reported the highest levels of current (past month) binge drinking (39%), heavy drinking (binge drinking five or more times in the past month, 10.9%), and illicit drug use (22.3%) compared to any other age category (Center for Behavioral Health Statistics and Quality, 2016). Furthermore, approximately 1 in 9 young adults (10.9%) aged 18 to 25 had an alcohol use disorder in the past year, more than twice the rate of adults over the age of 26 (5.4%) and over four times the rate of teens aged 12 to 17 (2.5%). Similarly, rates of illicit drug use disorder in the past year were two to three times higher among young adults aged 18 to 25 (7.2%) compared to any other age category.
In addition to the use of alcohol and illegal substances, the misuse and abuse of prescription medications is a national epidemic and major public health issue. Young adults are disproportionately affected by the prescription drug abuse epidemic. According to NSDUH data, 5.1% of young adults aged 18 to 25 misused prescription drugs (pain relievers, 2.4%; stimulants, 2.2%; tranquilizers, 1.7%; and sedatives, 0.2%) in the past month, more than twice the rate of prescription drug misuse among adolescents aged 12 to 17 (2%) or adults older than 26 (2%). The misuse of prescription pain killers and stimulants are most prevalent, and NSDUH findings indicate that an estimated 60% of overall prescription drug misuse is driven by pain relievers, including prescription opioids. The number of opioid prescriptions written by physicians in the U.S. has increased almost 3-fold over the past two decades (Volkow, 2014), coinciding with a rapid escalation in opioid misuse, abuse, addiction, hospitalities, and fatalities (Dart et al., 2015; Netemeyer, Burton, Delaney, & Hijjawi, 2015; Volkow, 2014). An estimated 1 in 4 individuals who are prescribed opiates long-term eventually abuse them, and 10% become addicted (Nelson, Van Ryzin, & Dishion, 2015). Prescription opioid abuse has been found to lead to heroin abuse among some users. Koh (2015) reported that three out of four new heroin users began abusing prescription opioids prior to abusing heroin. In a pattern similar to opioid prescriptions, the number of prescriptions written by physicians in the U.S. for stimulants (including medications for ADHD) has increased almost 5-fold (Safer, 2015) over the past two decades. This has coincided with concurrent increases in abuse and addiction rates, as well as stimulant-related calls to poison control centers, emergency room visits, and sudden deaths (Gould et al., 2009; Setlik et al., 2009).
Taken together, research demonstrates that various forms of drug abuse (DA) and prescription drug abuse (PDA) along with heavy alcohol use are important problems because they contribute to a variety of negative health and behavioral outcomes, particularly among young adults, including work-related problems, unintentional injuries, traffic fatalities, sexual assault, interpersonal aggression and violence, and psychiatric problems (Ellickson, Tucker, & Klein, 2003; Newcomb & Locke, 2005). These behaviors are also associated with a variety of costs to society, including reduced workforce participation, homelessness, and escalating health care, legal, and criminal justice costs (Birnbaum et al., 2011; National Council on Alcoholism and Drug Dependence, 2015).
The observed peak in substance use among young adults is part of a larger normative age-related pattern of substance use across the lifespan that includes initiation or experimental use during adolescence; an increase in the frequency, quantity, and types of substances used through the years of adolescence and into young adulthood; a peak in use during young adulthood; and a gradual decline through the remainder of the adult years (Griffin, 2011; Jackson & Sartor, 2016). While there is a tendency to view early adolescent substance use as experimental, temporary, and social in nature, early onset may heighten the likelihood of heavier and more frequent use that may endure over time, enhancing the risk of developing substance abuse disorders by young adulthood (Chassin, Pitts, & Prost, 2002; Englund, Egeland, Oliva & Collins, 2008; Grant, Stinson, & Harford, 2001; Hingson, Heeren, & Winter, 2006; Mason & Spoth, 2011;). However, less is known about how early onset and escalation of substances that are legal for adults and widely available to youth (i.e., alcohol and cigarettes) may be differentially related to later DA compared to PDA. Finally, most longitudinal studies of substance use during adolescence and the transition to young adulthood have involved predominantly white, suburban, middle class populations; less is known about how early initiation and growth in substance use affect subsequent DA and PDA among urban minority young adults.
The goals of the present study were to address the gap in the extant literature by examining how growth in the use of legal substances (i.e., alcohol and tobacco) during adolescence predicts involvement in DA and PDA during young adulthood in a sample of urban predominantly minority young adults in New York City. A latent growth modeling framework was used to examine both initial levels of substance use (intercept factor) and degree of change over time (growth factor) as predictors of later DA versus PDA.
Methods
Procedures
Participants were part of a large, school-based drug abuse and violence prevention trial. For the present study, only control group participants from the larger study were included in the analysis. Participants completed annual surveys from the seventh through twelfth grade that included demographic information, self-reported academic performance, family structure, and several questions related to substance use frequency and quantity. Data were collected following a detailed protocol used in previous prevention studies (e.g., Botvin et al., 2001). Questionnaires were administered in regular classroom periods by teams of three to five study personnel, and students were informed that their responses would not be made available to school personnel, teachers, or parents. Because participants were of various racial/ethnic backgrounds, efforts were made to recruit a racially and ethnically diverse data collection staff. Unique identification codes were utilized (rather than participants’ names) to permit linkage of surveys over time while preserving confidentiality. Various tracking procedures, including a comprehensive database that documented the progress of tracking and data collection, and annual updates on changes in participants’ contact information from the New York City Board of Education, were used to increase study retention and minimize attrition.
Study participants were followed up via telephone survey six years later as young adults when they were approximately 23 years of age. Recruitment was conducted by mailing a packet of information to individuals who had provided data as adolescents and requesting their participation in a telephone follow-up survey. The packet included a brief description of the continuing study, a 90-day calendar to be used during a scheduled telephone interview, along with $2 and an offer of additional compensation ($40 to $60) upon completion of a phone interview. Participants were provided with a toll-free telephone number to complete the interview. The interview assessed risk behaviors over the past 90 days using timeline follow-back (TLFB) interview procedures. The TLFB interview method is a widely-used assessment procedure that uses calendar-based guided recall to accurately measure alcohol and illicit drug use (Sobell & Sobell, 1992). TLFB procedures have been shown to be psychometrically valid when completed either in person or over the telephone (Sobell, Brown, Leo & Sobell, 1996). As a first step in this procedure, a trained interviewer reviewed a 90-day calendar with the participant, marking on the calendar holidays and significant events (birthdays, anniversaries, illnesses of oneself or close friends and family, or any event that was deemed personally meaningful to the participant), to create “anchor points” for facilitating accurate recall. The interviewer then guided the participant to elicit their day-to-day risk behaviors working backwards over a 90-day period. The length of the telephone interview depended on the degree of engagement in risky behavior and ranged from 20 to 60 minutes. Research protocols and consent procedures for the adolescent and young adult phases of the project were reviewed and approved by the Institutional Review Board at Cornell Medical College.
Sample
The sample included 984 predominantly minority young adults. Of these, 51.1% were Black, 26% were Latino/Hispanic, 5.6% were Asian, 4.9% were White, 1.2% were Native American, and 11.2% were multiracial. The gender composition was 57% female and 43% male. About half (50.1%) of participants were from two-parent households.
Measures
The demographic and adolescent substance use measures were derived from widely used instruments that have been used in previous prevention studies with White adolescents and minority adolescents and shown to have good psychometric properties (Botvin, Baker, Dusenbury, Botvin, & Diaz, 1995; Botvin, Griffin, Diaz, & Ifill-Williams, 2001).
Demographics Variables.
Data concerning the characteristics of the participants were collected using survey items assessing gender, race and ethnicity, socioeconomic status (receive free or reduced school lunch), and academic performance. Participants were asked to indicate what grade they generally received, with response options ranging from 1 = “Ds or lower” to 5 = “mostly As.”
Adolescent Cigarette Smoking.
Participants were asked how often they smoke, with response options ranging from 1 = “never” to 9 = “more than once a day.” Participants who reported smoking indicated how much they smoke, from 1 = “not at all” to 8 = “more than two packs a day.” The average of two items was used as an indicator of cigarette smoking.
Adolescent Alcohol Use.
Participants indicated the frequency of (a) drinking alcohol (beer, wine, or hard liquor) and (b) drinking “until you get drunk,” both with response options ranging from 1 = “never” to 9 = “more than once a day.” Participants also indicated how many drinks they consume when they drink, ranging from 1 = “I don’t drink” to 6 = “more than 6 drinks.” The average of three items was used as an indicator of alcohol use.
Young Adult Drug Use.
Survey items to assess drug use among young adults in the present study were taken from the Monitoring the Future young adult follow-up studies (Bachman, Wadsworth, O’Malley, Johnston, & Schulenberg, 1997). DA was assessed by asking participants about their use of any of the following substances in the past three months: cocaine, crack cocaine, methamphetamine, heroin, hallucinogens, LSD, Ecstasy, PCP, or any injection drug use. PDA was assessed by asking participants whether they had used of any of the following pills for non-medical purposes in the past three months: pain killers, amphetamines, sedatives, or tranquilizers.
Data Analysis
Latent growth curve (LGC) modeling was conducted using Mplus (Muthén & Muthén, 2008). Full-information maximum likelihood (FIML) was used to handle missing data. Goodness of fit was assessed using three criteria: chi-square (χ2), Root Mean Square Error of Approximation (RMSEA), and Comparative Fit Index (CFI). Following the recommendations of Hu and Bentler (1998), we set the cutoff for acceptable model fit at RMSEA < .08 and CFI > .90.
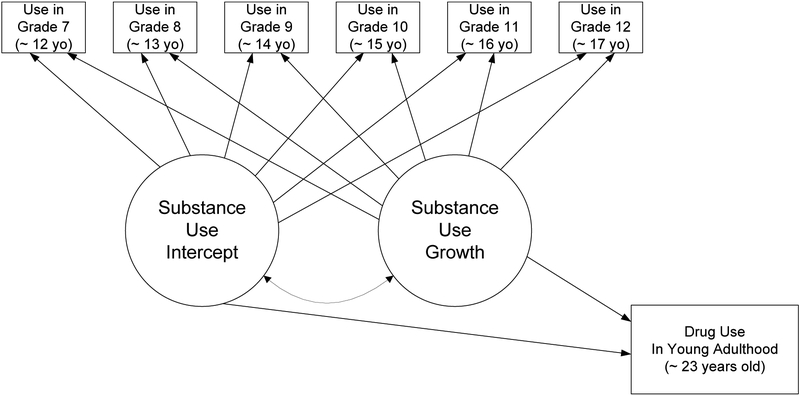
For adolescent alcohol and cigarette use, we first established a model of growth over the course of adolescence, from 7th to 12th grade. Latent factors representing the initial starting point (i.e., the intercept) and rate of change (i.e., the slope) were estimated for the full sample. Variance terms for the intercept and slope, accounting for individual differences in participants’ starting points and rates of change, were also included. After each adolescent substance use trajectory was established, variables indicative of young adult drug use were added, and were predicted by the intercept and slope terms of adolescent substance use (see Figure 1). Young adult DA and PDA were included in separate models. Because males and those with low grades in school are at higher risk for substance use (e.g., Bryant, Schulenberg, O’Malley, Bachman, & Johnston, 2003), gender and grades at baseline were included as exogenous control variables, along with free lunch status as an indicator of socioeconomic status. Race/ethnicity was included as an exogenous control variable, dichotomized to represent Black (the largest racial/ethnic category) vs. non-Black participants. Each control variable was included as a predictor of the slope and intercept of adolescent substance use, as well as the young adult drug use outcome variable, and paths with p < .10 were subsequently trimmed. The analyses resulted in four final models, with one model for adolescent cigarette smoking and a second for adolescent alcohol use, each predicting young adult DA or PDA. Standardized values for regression paths and covariances in the four final models are presented in the results. Non-standardized results are presented for variance and residual variance terms, since standardized variances in Mplus are set at 1.00.
Figure 1.
General Growth Model: Adolescent Substance Use and Young Adult Illicit and Prescription Drug Abuse
Results
Lifetime alcohol use was reported by almost one-in-four (23.6%) 7th graders, which increased in subsequent years to 29.7% (8th graders), 38% (9th graders), 49% (10th graders), 53.3% (11th graders) and almost two-in-three (64.3%) reported ever drinking as high school seniors. Lifetime cigarette smoking was reported by 14% of 7th graders, 16% of 8th graders, 18.6% of 9th graders, 22.2% of 10th graders, 22.7% of 11th graders, and 23.2% high school seniors. Thus, prevalence of lifetime alcohol use was substantially higher than that of cigarette smoking among 7th graders and this difference continued to widen throughout the secondary school years. When assessed as young adults, 22% of participants reported marijuana use in the past three months, 2.5% reported DA other than marijuana in the past three months, and 1.7% reported PDA in the past three months.
Illicit Drug Abuse.
The final model with adolescent cigarette use predicting young adult DA had acceptable fit with the data, χ2(37) = 127.97, p < .001, RMSEA = .05 (90% CI [.04, .06]), CFI = .90. The mean estimate for the slope was marginally statistically significant (μS = .19, p = .06), indicating a trend towards significant overall growth in smoking during secondary school. There was significant residual variance in both the intercept and slope terms (ψI= .26, p < .001, and ψS = .07, p < .001), indicating significant unexplained variability in participants’ initial cigarette use, as well as in the rate at which cigarette use changed over time. The covariance between the intercept and slope terms was statistically significant (r = −.31, p < .001), indicating that participants who started with higher cigarette use tended to have less steep (i.e., smaller) increases in cigarette use over time. Baseline grades and Black race were significant predictors of the slope (B = −.10, p = .01, and B = −.13, p < .001), such that participants with lower baseline grades and non-Black participants reported significantly greater increases in cigarette use. The intercept term was not a significant predictor of DA (B = .06, p = .15), whereas the slope was a significant predictor (B = .10, p = .01). Participants who reported greater increases in cigarette use had significantly higher levels of young adult DA.
The final model with adolescent alcohol use predicting young adult DA had acceptable fit with the data, χ2(36) = 134.87, p < .001, RMSEA = .05 (90% CI [.04, .06]), CFI = .90. The slope of alcohol use was statistically significant, μS = .77, p < .001, such that participants experienced significant increases in alcohol use from 7th to 12th grade on average. There was also significant residual variance in both the intercept and slope terms, ψI= .26, p < .001, and ψS = .05, p < .001, indicating significant unexplained variation in participants’ initial levels of and rates of change in alcohol use over adolescence. The covariance between the intercept and slope terms was significant (r = −.18, p = .005), such that participants with higher 7th grade alcohol use had less steep increases in alcohol use over adolescence. Gender and Black race were significant predictors of the slope term (B = .12, p = .005, and B = −.14, p = .001, respectively), such that males and non-Black participants had steeper increases in alcohol use. Both the intercept and slope of alcohol use were significant predictors of DA (B = .11, p = .009, and B = .12, p = .005, respectively). Participants who began with higher alcohol use and who experienced steeper increases in alcohol use over adolescence reported significantly higher DA as young adults.
Prescription Drug Abuse.
The fit statistics for the final model with adolescent cigarette use predicting young adult PDA were χ2(31) = 176.12, p < .001, RMSEA = .07 (90% CI [.06, .08]), CFI = .85. Although findings indicated that slope of cigarette use was a significant predictor of PDA (B = .14, p = .01), we did not further examine this model because the CFI is not considered an acceptable fit.
The final model with adolescent alcohol use predicting young adult PDA had acceptable fit with the data, χ2(37) = 136.51, p < .001, RMSEA = .05 (90% CI [.04, .06]), CFI = .90. Again, the slope term was statistically significant (μS = .77, p < .001), there was significant residual variance in both the slope and intercept terms (ψI= .26, p < .001, and ψS = .05, p < .001), the covariance between the intercept and slope was significant (r = −.18, p = .005), and gender and Black race were significant predictors of the slope (B = .12, p = .005, and B = −.13, p = .001, respectively), such that males and non-Black participants had steeper increases in alcohol use. While the intercept of adolescent alcohol use was not a significant predictor of young adult PDA (B = .03, p = .50), the slope of adolescent alcohol use was a significant predictor of young adult PDA (B = .10, p = .02).
Discussion
Research and theory suggest that the early onset of substance use during adolescence leads to the greater likelihood of substance abuse in later adolescence and young adulthood. However, few studies have investigated the long-term consequences of adolescent alcohol and tobacco use (substances that are legal for adults) on illicit drug abuse (DA) among urban minority young adults, and whether these predictive patterns are similar for PDA in this population. In the present study, a series of latent growth models were used to examine how alcohol and tobacco use onset and escalation during adolescence predicted later involvement in both DA and PDA in a sample of predominantly minority young adults. In analyses controlling for gender, academic performance, eligibility for free school lunch, and race/ethnicity, we found that participants who reported greater increases in cigarette smoking and alcohol use had significantly higher levels of young adult DA. Initial baseline levels of alcohol use also predicted DA in young adulthood. We also found that participants who reported greater increases in alcohol use during adolescence had significantly higher levels of PDA in young adulthood.
These findings are important because they support and extend previous research showing that there is a developmental progression in substance use. For example, early use of one substance has been shown to increase the risk of crossing over to the use of other substances, progressing from the use of alcohol and/or tobacco to multiple forms of illicit drug abuse later in adolescence and young adulthood. Additionally, both alcohol and marijuana have been positively correlated with increased rates of smoking and marijuana use, high-risk drinking, illicit substance use other than marijuana, polysubstance use, and the nonmedical use of prescription drugs (Ellickson et al., 2003; King, Nguyen, Kosterman, Bailey, & Hawkins, 2012; Chassin et al. 2002; Mason & Spoth, 2011; Ohannessian et al., 2015; Cohn et al., 2015; Duncan, Gau, Farmer, Seely, Kosty, & Lewenson, 2015; Moss et al., 2014; Passarotti, Crane, Hedeker, & Mermelstein, 2015; Zhang, Brook, Leukefeld, & Brook, 2016).
Early substance use has not only been demonstrated to lead to continued and crossover substance use, but it has also been associated with numerous adverse social consequences. These include poor academic performance and school dropout, delinquent behavior, violence and aggression, and other associated health risk behaviors (Ellickson et al., 2003; King et al., 2012; Chassin et al. 2002; Mason & Spoth, 2011; Ohannessian et al., 2015; Cohn et al., 2015; Duncan et al., 2015; Moss et al., 2014; Passarotti et al., 2015; Zhang et al., 2016). The current findings are important because they not only demonstrate that patterns of adolescent substance use are linked to subsequent young adult DA, but the association is also significant in terms of PDA, a major epidemic in the U.S.
The finding that adolescent substance use predicts young adult substance use in urban predominantly minority young adults is also an important finding. A variety of studies examining racial and ethnic differences in substance use and abuse have consistently reported higher frequency and quantity of substance use among non-minority (i.e., White) adolescents (Stone et al., 2012; Chen & Jacobson, 2012; Malone et al., 2012; Keyes et al., 2014). Black youth, on the other hand, have been shown to initiate substance use later than both White and Hispanic youth. However, NSDUH data show that Black young adults have the highest rate of past month DA compared to both White and Hispanic young adults. Black individuals may not reach peak levels of substance use until between the 20s to early 30s (Chen & Jacobson, 2012). One explanation for this delayed peak in use is that, compared to non-Black adolescents, Black late initiators may be more likely to continue using drugs, rather than “mature out” of use. This, in turn, could leave them at a greater risk of developing substance use disorders (Stone et al. 2012; Finlay, White, Mun, Cronley, & Lee, 2012; Chen & Jacobson, 2012) as well as greater social and legal problems (e.g., arrest and incarceration) related to substance use (Keyes et al., 2014), relative to non-Black young adults (Pacek, Malcolm, & Martins, 2012).
One implication from these findings is that interventions demonstrated to prevent tobacco and alcohol use among adolescents and/or reduce the escalation of use may also reduce DA and PDA and their negative consequences in young adulthood. This is particularly important because young adulthood has become extended in time in recent years, with an increasing number of young people choosing to delay career, marriage, and childrearing into their late twenties and beyond. This translates into an extended period during which young adults may engage in social activities (e.g., socializing with friends at bars and clubs), that may place them at higher risk for heavier levels of alcohol and drug use (Settersten, 2012; Silva, 2010). Implementation of effective preventive interventions during adolescence not only may decrease DA and PDA among young adults; it may also help young adults navigate their way through the extended transition from adolescence to the responsibilities of adulthood.
Strengths of the current study include the focus on an understudied population of urban, predominantly minority economically disadvantaged individuals, followed from early adolescence into young adulthood. The study expands upon previous research by focusing on an understudied population, differentiating between young adult DA and PDA, and by focusing on early alcohol and tobacco use, substances that are legal for adults and widely available to teens. Several limitations should be noted. First, the prevalence rates of DA and PDA within the past three months at the young adult assessment were low, and the retention rates over the course of the study were approximately 55%. The findings may not generalize to higher risk youth, who typically drop out of cohort studies more than lower risk youth. Our assessment of race and ethnicity was limited in that it did not allow for us to examine the racial backgrounds of participants who reported that they were Hispanic or Latino. An additional limitation is that because our follow-up assessment occurred when participants were in their early twenties, we were not able to examine any delayed patterns of substance use onset, escalation, or cessation that have been observed in samples of predominantly minority young adults in their later 20s and 30s (Thomas & Price, 2016).
In summary, findings indicated that early onset of alcohol and tobacco use among urban minority teens leads to greater drug involvement and the potential for multiple negative consequences in young adulthood. Future research is needed to extend these findings further into the adult years. Because the onset and escalation of alcohol and cigarette use during adolescence may increase the risk for later DA and PDA, the findings also indicate that universal efforts for preventing youth alcohol and tobacco use have the potential to play a critical role in reducing DA and PDA during adulthood. Research is needed to determine the extent to which preventive interventions implemented during adolescence can decrease DA and PDA among young adults from a variety of racial/ethnic and socioeconomic backgrounds, as well as those from other demographic subgroups.
Table 1.
Latent Growth Models Predicting Illicit Drug Use in Young Adulthood
| Outcome: Illicit Drug Use in Young Adulthood | ||||
|---|---|---|---|---|
| Prediction Model: | CFI | RMSEA | Intercept β | Slope β |
| Cigarette Smoking in Secondary School | .90 | .05 | .06 | .10** |
| Alcohol Use in Secondary School | .90 | .05 | .11** | .12*** |
Note: Bold numbers indicate adequate model fit statistics;
Significance of intercept and slope terms in each model,
p < 05;
p < .01;
p < .001
Table 2.
Latent Growth Models Predicting Prescription Drug Abuse in Young Adulthood
| Outcome: Prescription Drug Abuse in Young Adulthood | ||||
|---|---|---|---|---|
| Prediction Model: | CFI | RMSEA | Intercept β | Slope β |
| Cigarette Smoking in Secondary School | .85 | .07 | .03 | .14*** |
| Alcohol Use in Secondary School | .90 | .05 | .03 | .10* |
Note: Bold numbers indicate adequate model fit statistics;
Significance of intercept and slope terms in each model,
p < 05;
p < .01;
p < .001
Acknowledgments
This paper was supported by grants from the National Institute on Drug Abuse (R01 DA023890) and National Institute on Alcoholism and Alcohol Abuse (R21 AA016531) to the first author. Correspondence should be addressed to Kenneth W. Griffin, PhD, Department of Healthcare Policy & Research, Weill Cornell Medical College, 402 East 67th Street, New York, NY 10065; kgriffin@med.cornell.edu
References
- Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD, & Schulenberg JE (1997). Smoking, drinking, and drug use in young adulthood: The impacts of new freedoms and new responsibilities Psychology Press.Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, & Roland CL (2011). Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Medicine, 12(4), 657–667. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Dusenbury L, Botvin EM, & Diaz T (1995) Long-term follow-up results of a randomized drug abuse prevention trial in a White middle-class population. Journal of the American Medical Association, 273, 1106–1112. [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW, Diaz T, & Ifill-Williams M (2001). Drug abuse prevention among minority adolescents: One-year follow-up of a school-based preventive intervention. Prevention Science, 2, 1–13. [DOI] [PubMed] [Google Scholar]
- Bryant AL, Schulenberg JE, O’Malley PM, Bachman JG, & Johnston LD (2003). How academic achievement, attitudes, and behaviors relate to the course of substance use during adolescence: A 6‐year, multiwave national longitudinal study. Journal of Research on Adolescence, 13(3), 361–397. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). 2015 National Survey on Drug Use and Health: Detailed Tables Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Chassin L, Pitts SC, & Prost J (2002). Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. Journal of Consulting & Clinical Psychology, 70 (1), 67–78. [PubMed] [Google Scholar]
- Chassin L, Pitts SC, & Prost J (2002). Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. Journal of Consulting & Clinical Psychology, 70(1), 67–78. [PubMed] [Google Scholar]
- Chen P, & Jacobson KC (2012). Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health, 50, 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, & Mermelstein R (2015). The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addictive Behaviors, 48, 79–88. [DOI] [PubMed] [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, & Green JL (2015). Trends in opioid analgesic abuse and mortality in the United States. New England Journal of Medicine, 372(3), 241–248. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Gau JM, Farmer RF, Seeley JR, Kosty DB, & Lewinsohn PM (2015). Comorbidity and temporal relations of alcohol and cannabis use disorders from youth through adulthood. Drug & Alcohol dependence, 149, 80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, Tucker JS, & Klein DJ (2003). Ten-year prospective study of public health problems associated with early drinking. Pediatrics, 111(5, Pt. 1), 949–955. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Tucker JS, & Klein DJ (2003). Ten-year prospective study of public health problems associated with early drinking. Pediatrics, 111(5, Pt. 1), 949–955. [DOI] [PubMed] [Google Scholar]
- Englund MM, Egeland B, Oliva EM, & Collins WA (2008). Childhood and adolescent predictors of heavy drinking and alcohol use disorders in early adulthood: a longitudinal developmental analysis. Addiction, 103, 23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay AK, White HR, Mun EY, Cronley CC, & Lee C (2012). Racial differences in trajectories of heavy drinking and regular marijuana use from ages 13 to 24 among African-American and White males. Drug & Alcohol Dependence, 121, 118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould MS, Walsh BT, Munfakh JL, Kleinman M, Duan N, Olfson M, Greenhill L, & Cooper T (2009). Sudden death and use of stimulant medications in youths. American Journal of Psychiatry, 166, 992–1001. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, & Harford TC (2001). Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. Journal of Substance Abuse, 13, 493–504. [DOI] [PubMed] [Google Scholar]
- Griffin KW (2011). Substance use across the lifespan. In Finkel M (Ed.) Public Health in the 21st Century Vol. 2: Disease Management (pp. 351–370). Santa Barbara, CA: Praeger. [Google Scholar]
- Jackson KM, & Sartor CE (2016). The natural course of substance use and dependence In Sher KJ (Ed.), The Oxford Handbook of Substance Use and Substance Use Disorders. Oxford University Press [Google Scholar]
- Hermos JA, Winter MR, Heeren TC, & Hingston RW (2008). Early age-of-onset drinking predicts prescription drug misuse among teenagers and young adults: Results from a national survey. Journal of Addiction Medicine, 2, 22–30. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, & Winter MR (2006). Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatric & Adolescent Medicine, 160, 739–746. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3, 424–453. [Google Scholar]
- Keyes KM, Vo T, Wall MM, Caetano R, Suglia SF, Martins SS, Galea S & Hasin D (2015). Racial/ethnic differences in use of alcohol, tobacco, and marijuana: Is there a cross-over from adolescence to adulthood? Social Science & Medicine, 124, 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Vo T, Wall MM, Caetano R, Suglia SF, Martins SS, Galea S & Hasin D (2015). Racial/ethnic differences in use of alcohol, tobacco, and marijuana: Is there a cross-over from adolescence to adulthood? Social Science & Medicine, 124, 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Nguyen HV, Kosterman R, Bailey JA, & Hawkins JD (2012). Co‐occurrence of sexual risk behaviors and substance use across emerging adulthood: evidence for state‐and trait‐level associations. Addiction, 107(7), 1288–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh H (2015). Community approaches to the opioid crisis. JAMA, 314(14), 1437–1438. [DOI] [PubMed] [Google Scholar]
- Lessem JM, Hopher CJ, Haberstick BC, Timberlake D, Ehringer MA, Smolen A, & Hewitt JK (2006). Relationship between adolescent marijuana use and young adult illicit drug use. Behavior Genetics, 36, 498–506. [DOI] [PubMed] [Google Scholar]
- Malone PS, Northrup TF, Masyn KE, Lamis DA & Lamont AE (2012). Initiation and persistence of alcohol use in United States Black, Hispanic, and White male and female youth. Addictive Behaviors, 37, 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA and Spoth RL (2011). Longitudinal associations of alcohol involvement with subjective well-being in adolescence and prediction to alcohol problems in early adulthood. Journal of Youth & Adolescence, 40(9), 1215–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2008). Mplus (Version 5.1). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Council on Alcoholism and Drug Dependence, Inc. (2015). Facts about drugs: Costs to society. Retrieved from https://www.ncadd.org/about-addiction/faq/facts-about-drugs
- Nelson SE, Van Ryzin MJ, & Dishion TJ (2015). Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Development & Psychopathology, 27(1), 253–277. [DOI] [PubMed] [Google Scholar]
- Netemeyer R, Burton S, Delaney B, & Hijjawi G (2015). The legal high: Factors affecting young consumers’ risk perceptions and abuse of prescription drugs. Journal of Public Policy & Marketing, 34(1), 103–118. [Google Scholar]
- Newcomb MD, & Locke T (2005). Health, social, and psychological consequences of drug use and abuse (pp. 45–59). In Sloboda Z (Ed.), Epidemiology of Drug Abuse. New York: Springer. [Google Scholar]
- Ohannessian CM, Finan LJ, Schulz J, & Hesselbrock V (2015). A long-term longitudinal examination of the effect of early onset of alcohol and drug use on later alcohol abuse. Substance Abuse, 36(4), 440–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacek LR, Malcolm RJ, & Martins SS (2012). Race/ethnicity differences between alcohol, marijuana, and co‐occurring alcohol and marijuana use disorders and their association with public health and social problems using a national sample. American Journal on Addictions, 21(5), 435–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passarotti AM, Crane NA, Hedeker D, & Mermelstein RJ (2015). Longitudinal trajectories of marijuana use from adolescence to young adulthood. Addictive Behaviors, 45, 301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DJ (2016). Recent trends in stimulant usage. Journal of Attention Disorders, 20(6), 471–477. [DOI] [PubMed] [Google Scholar]
- Setlik J, Bond GR, & Ho M (2009). Adolescent prescription ADHD medication abuse is rising along with prescriptions for these medications. Pediatrics, 124(3), 875–880. [DOI] [PubMed] [Google Scholar]
- Settersten RA Jr (2012). The contemporary context of young adulthood in the USA: From demography to development, from private troubles to public issues In Booth A, Brown SL, Landale MS, Manning WD & McHale SM (Eds.), Early adulthood in a family context (pp. 3–26). Springer: New York [Google Scholar]
- Silva JM (2012). Constructing adulthood in an age of uncertainty. American Sociological Review, 77, 505–522. [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug & Alcohol Dependence, 42, 49–54. [DOI] [PubMed] [Google Scholar]
- Sobell LC; Sobell MB (1992). Timeline follow-back: A technique for assessing self-reported alcohol consumption (pp. 207–224). In Measuring alcohol consumption; Litten R, Allen J, Eds.; Humana Press: Rockville, MD. [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37(7), 747–775. [DOI] [PubMed] [Google Scholar]
- Thomas YF, & Price LN (2016). Drug use trajectories among minority youth. New York: Springer. [Google Scholar]
- Volkow ND (2014, May 14). America’s addiction to opioids: Heroin and prescription drug abuse. In testimony to Senate Caucus on International Narcotics Control. Retrieved from https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse.
- Zhang C, Brook JS, Leukefeld CG, & Brook DW (2016). Trajectories of marijuana use from adolescence to adulthood as predictors of unemployment status in the early forties. The American Journal on Addictions, 25(3), 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]