Abstract
Background.
High resolution manometry (HRM) measures rectoanal pressures in defecatory disorders and fecal incontinence. This study sought to define normal values for rectoanal HRM, ascertain the effects of age and BMI on rectoanal pressures and compare pressures in asymptomatic women with normal and prolonged balloon expulsion time (BET).
Methods.
HRM pressures and BET were measured in 163 asymptomatic healthy participants. Women (96) and men (47) with normal BET were used to estimate normal values and the effects of age/BMI on pressures using a Medtronic 4.2mm diameter rectoanal catheter.
Results.
Age is associated with lower resting pressure, higher rectal pressure during evacuation, and a higher rectoanal gradient during evacuation in women and men. In women, the BET is also inversely correlated with age while the BMI is correlated with a higher threshold volume for discomfort and a longer BET. The anal squeeze pressure increment, squeeze duration, and HPZ length are higher in men than women. The rectoanal gradient during evacuation is also lower (ie, more negative) in asymptomatic women with an abnormal than a normal BET.
Conclusions.
These findings provide an expanded database of normal values for anorectal HRM in men and women. Age and sex affect anal resting and squeeze pressures respectively; rectal pressure during evacuation is also higher in older people. Less than 15% of asymptomatic people have BET greater than 60 seconds, which is associated with manometry features of impaired evacuation.
Keywords: Anorectal manometry, balloon expulsion test, constipation, defecatory disorders, pelvic floor dysfunction
Graphical Abstract
This study provides an expanded database of normal values for anorectal HRM in men and women. Age and sex affect anal resting and squeeze pressures respectively. Less than 15% of asymptomatic people have BET greater than 60 seconds, which is associated with manometry features of impaired evacuation.
BACKGROUND
High resolution anorectal manometry (HRM) is widely used to assess anorectal functions (i.e., anal resting pressure, voluntary contraction of the anal sphincter, rectoanal pressures during evacuation, and rectal sensation) in fecal incontinence (FI) and chronic constipation 1–4. Indeed, manometry and a rectal balloon expulsion test (BET) are recommended first-line tests in these disorders 1, 5–8. There are 3 commercially-available HRM systems manufactured by Medtronic, Sandhill Scientific, and Medical Measurement Systems. For the Medtronic HRM catheter, which is widely used in the United States, values are interpreted by comparison to a relatively small database of normal values in 62 women 9; to our knowledge, there are no published normal values for men 2. A larger database of normal values is necessary because anorectal pressures are significantly affected by age and sex. Also, there is a significant overlap between asymptomatic healthy individuals and patients with defecatory disorders (DD) in rectoanal pressures during evacuation 10, 11.
Some asymptomatic healthy individuals cannot expel the balloon in 60 seconds, which is generally regarded as the upper limit of normal 12, 13. Whether this represents an inability to simulate defecation in an artificial environment or asymptomatic pelvic floor dysfunction is unclear. While increased BMI and bariatric surgery are risk factors for FI 14–16, the effect of increased BMI on rectoanal pressures in asymptomatic healthy people is unknown. Hence, the objectives of this study were to define normal values for rectoanal pressures measured with HRM in men and women, to evaluate the relationship between rectoanal pressures with age and BMI in asymptomatic people, and to compare rectoanal pressures in asymptomatic people with a normal and prolonged BET.
MATERIALS AND METHODS
Study Design
This report is compiled from five research studies in which rectoanal pressures were measured with anorectal high resolution manometry in healthy people at Mayo Clinic, Rochester, MN. The participants consented to participate in these studies that were approved by the Institutional Review Board at Mayo Clinic. The data from some of these studies has been presented previously 8, 9, 17. Data from individual studies were collected from 2008–2010, 2012–2013, 2013–2016, 2014–2017, and 2015–2017 respectively.
Participants
This report include 113 female and 50 male healthy controls aged 18 years and older that were recruited by public advertisement and did not have a clinically-significant systemic (eg, cardiovascular, respiratory, gastrointestinal) disease or symptoms of a functional bowel disorder as assessed by an interview and by a questionnaire. Subjects who had documented anorectal trauma during delivery (i.e., grade 3 or 4 laceration) or any previous anorectal operations including hemorrhoid procedures, were excluded. Of these 113 women and 50 men, respectively 96 and 47 had a normal BET. The mean age and BMI were not significantly different between women (41 ± 16y [Mean ± SD], 25.8±4.5kg/m2) and men (45±16y, 26.4±3.3kg/m2) with a normal BET.
High Resolution Manometry
Rectoanal pressures were measured with Manoscan™ high resolution manometry catheters (currently Medtronic Inc, Minneapolis, MN, USA). These catheters (diameter of 4.2mm) contain 12 circumferential sensors, 2 within the rectal balloon and 10 sensors at 6mm intervals along the anal canal. At each level, 36 circumferential pressure sensors detect pressure over a length of 2.5mm at 35Hz. These pressures are averaged to obtain a single value at each level.
Before anorectal manometry, each participant received two enemas to ensure the rectal vault was empty before the test. All studies were performed by one of three individuals experienced in performing HRM. With the patient in the left lateral decubitus position, pressures were measured for 20 seconds during each of these maneuvers: at rest, voluntary contraction of the anal sphincters and puborectalis on 3 occasions, simulated evacuation with the catheter balloon empty and then distended with 50cc of water, and a Valsalva maneuver. In order to standardize the Valsalva maneuver, participants used the AlveoSampler (Quintron, Milwaukee, WI, USA), which was attached to a sphygmomanometer. They were encouraged to generate a pressure of 20mmHg during the maneuver. During evacuation, participants were asked to evacuate the catheter as if they were passing a bowel movement. Then, the recto-anal inhibitory reflex and rectal sensation were concurrently assessed by progressively distending the rectal balloon in 20-ml increments from 0 to 200 ml and, if necessary thereafter, in 40 ml increments until a maximum volume of 400 ml. The threshold volumes for first sensation, urge to defecate, and maximum discomfort were recorded. In contrast to the “infinitely compliant” rectal barostat balloons, the balloons used to evaluate sensory thresholds in this research demonstrate variable compliance and were therefore not used to assess rectal compliance.
These parameters were analyzed using commercially available software (Manoview AR v3.0, Medtronic Inc). For rectal pressure, the higher of two rectal balloon pressure measurements during simulated evacuation, was used for the entire study. While the anal pressures are recorded by several, up to 10, sensors, the software has an eSleeve function that reduces the pressures in the anal canal demarcated by the operator to a single value for analysis. At rest and during squeeze, the highest recorded pressure across all sensors was used for analysis. During squeeze, the pressure is averaged across the three squeeze maneuvers to generate the average squeeze pressure. The length of the high pressure zone (HPZ) is the length of the average pressure profile in the resting pressure frame defined as {Rectal Pressure + ([Anal Resting Pressure – Rectal Pressure] *0.25)}. During simulated evacuation, the eSleeve function identifies the most positive (or least negative) difference between rectal and anal pressures, measured over 3 seconds during the twenty seconds (equation 1).
| (1) |
During the assessment of the rectoanal inhibitory reflex and simulated evacuation, anal relaxation (%) is calculated relative to the anal pressure measured over 1.5 seconds before the maneuver (equation 2). The rectoanal inhibitory reflex was considered present if anal relaxation was higher than 25%.
| (2) |
Balloon Expulsion Test
Participants were asked to expel a rectal balloon filled with 50cc of warm water in privacy while seated on a commode. The time (in seconds) required to do so was measured. Patients were given 180 seconds in which to complete this maneuver. Based on a prior study with this technique, values of 60 seconds or less were considered normal 12.
Data and Statistical Analysis
The associations between rectoanal pressures and demographic variables (i.e., age and BMI) were evaluated with Spearman correlation coefficients. Comparative analysis of continuous variables was performed with use of the Mann-Whitney U tests (Wilcoxon rank-sum test) and one-way Kruskal-Wallis tests with Chi-square approximation. Unless stated otherwise, the data are summarized as Mean ± SD. All analyses were performed with JMP Pro version 13.0.0 (SAS Institute, Cary, NC).
RESULTS
Rectoanal Pressures in Women: Relationship with Age, BMI and Parity
The normal values were derived from 96 of 113 women who had a normal rectal BET (less than 60 seconds) (Table 1 and Supplemental Tables 1–4). The anal squeeze pressure increment was lower during the second (−10 ± 2 mmHg, p < 0.001) and third (−9 ± 3 mmHg, p < 0.001) squeeze maneuvers.
Table 1.
Distribution of Anorectal Pressures in Women with a Normal Balloon Expulsion Test
| Variable | Women < 50 years with Normal BET (n = 58) | Women ≥ 50 years with Normal BET (n = 38) | Relationship with BMI a with Normal BET | Relationship with age a with Normal BET | ||
|---|---|---|---|---|---|---|
| Mean ± SD | 10th, 90th percentile | Mean ± SD | 10th, 90th percentile | |||
| Anal resting pressure | 85 ± 22 | 55, 111 | 66 ± 25 | 33, 93 | ns | −0.34 e |
| Anal HPZ length (cm) | 3.3 ± 0.8 | 2.2, 4.3 | 3.6 ± 0.7 | 2.4, 4.6 | ns | ns |
| Anal squeeze pressure, b | 207 ± 56 | 140, 284 | 193 ± 67 | 122, 281 | ns | ns |
| Anal squeeze increment, b,c, | 122 ± 49 | 53, 181 | 126 ± 65 | 49, 218 | ns | ns |
| Anal squeeze duration (s), d | 14 ± 7 | 4, 22 | 13 ± 8 | 3, 23 | ns | ns |
| First sensation (mL) | 39 ± 15 | 20, 60 | 35 ± 12 | 20, 50 | ns | ns |
| Urgency (mL) | 65 ± 22 | 40, 100 | 59 ± 22 | 40, 90 | ns | ns |
| Discomfort (mL) | 104 ± 34 | 60, 150 | 98 ± 28 | 60, 130 | 0.30 e | ns |
| Balloon expulsion time (s) | 13 ± 12 | 2, 26 | 10 ± 12 | 3, 22 | 0.20 f | −0.22 f |
| Simulated evacuation without rectal distention | ||||||
| Rectal pressure | 25 ± 20 | 1, 56 | 37 ± 21 | 11, 69 | ns | 0.27 e |
| Anal pressure | 63 ± 19 | 36, 88 | 64 ± 23 | 35, 97 | ns | ns |
| Rectoanal gradient | −38 ± 25 | −70, −6 | −27 ± 27 | −64, 12 | ns | ns |
| % Anal relaxation | 27 ± 19 | 0, 53 | 9 ± 48 | −30, 49 | ns | ns |
| Simulated evacuation with rectal distention | ||||||
| Rectal pressure | 153 ± 33 | 118, 191 | 182 ± 79 | 137, 218 | ns | 0.28 e |
| Anal pressure | 63 ± 23 | 36, 93 | 64 ± 26 | 39, 103 | ns | ns |
| Rectoanal gradient | 90 ± 41 | 8, 132 | 119 ± 89 | 58, 151 | ns | 0.24 f |
| % Anal relaxation | 17 ± 25 | −2, 46 | 11 ± 26 | −17, 41 | ns | ns |
| Valsalva without rectal distention | ||||||
| Anal Pressure | 125 ± 40 | 72, 188 | 103 ± 45 | 43, 159 | ns | −0.21 f |
Values are mm Hg unless stated otherwise.
Spearman correlation coefficient
These values are derived from the squeeze maneuver with the highest squeeze pressure
Squeeze increment is (anal squeeze pressure – anal resting pressure)
Average squeeze duration of 3 maneuvers.
p < 0.01
p<0.05; HPZ – high pressure zone. ns – not significant
Among women with a normal BET, age was associated with lower resting pressure (ρ = −0.34, P < 0.01), higher rectal pressure during evacuation with (ρ = 0.28, P < 0.01) and without (ρ = 0.27, P < 0.01) rectal distention, a higher rectoanal gradient with rectal distention during simulated evacuation (ρ = 0.24, P < 0.05), lower anal pressure during the Valsalva maneuver (ρ = −0.21, P < 0.05) and shorter balloon expulsion time (ρ = −0.22, P < 0.05).
Among women with a normal BET, the BMI was correlated with a longer balloon expulsion time (ρ = 0.20, P < 0.05) and a higher threshold volume for maximum discomfort during rectal balloon dilatation (ρ = 0.30, P < 0.01).
Fifty-one (53%) of the women with a normal BET had been pregnant and 48 (49%) had delivered. Among women with a normal BET, 40 had one or more vaginal deliveries (two assisted by forceps) and 13 had delivered at least once by cesarean section. Relative to nulliparous women, parous women were older (47 vs. 34 years, P < 0.001) but demonstrated similar anal resting (P = 0.3) and squeeze pressure (P = 0.05). Parity was not correlated with anal pressure at rest (ρ = −0.04, P = 0.6) or during squeeze (ρ = −0.11, P = 0.3).
Rectoanal Pressures in Men: Relationship with Age and BMI
Table 2 provides the normal values for anal pressures in men with a normal BET. Of the 50 male participants, 3 had a prolonged rectal BET. Among men with a normal BET, age was associated with lower anal resting pressure (ρ = −0.49, P < 0.01), higher rectal pressures during simulated evacuation with (ρ = 0.37, P < 0.05) and without (ρ = 0.39, P < 0.01) rectal distention, and a higher rectoanal gradient (ρ = 0.37, P < 0.05) during simulated evacuation with rectal distention. Similar to women, the anal squeeze pressure increment was lower during the second (−7 ± 4 mmHg, p < 0.05) and third (−10 ± 4 mmHg, p < 0.01) squeeze maneuvers. By contrast to women, BMI was not significantly correlated with any rectoanal parameters (Table 2 and Supplemental Tables 1–4).
Table 2:
Distribution of Anorectal Pressures in 47 Healthy Males with a Normal Balloon Expulsion Test
| Variable | Men with Normal BET (n = 47) | Relationship with BMI a | Relationship with age a | |
|---|---|---|---|---|
| Mean ± SD | 10th, 90th percentile | |||
| Anal resting pressure | 83 ± 25 | 54, 111 | ns | −0.49 e |
| Anal HPZ length (cm) | 3.9 ± 0.8 | 2.9, 4.8 | ns | Ns |
| Anal squeeze pressure b | 257 ± 78 | 164, 366 | ns | Ns |
| Anal squeeze increment b, c | 174 ± 81 | 90, 328 | ns | Ns |
| Anal squeeze duration (s) d | 14 ± 7 | 3, 21 | ns | Ns |
| First sensation (mL) | 44 ± 26 | 20, 72 | ns | Ns |
| Urgency (mL) | 74 ± 34 | 40, 120 | ns | Ns |
| Discomfort (mL) | 123 ± 53 | 60, 212 | ns | Ns |
| Balloon expulsion time (s) | 12 ± 12 | 3, 30 | ns | Ns |
| Simulated evacuation without rectal distention | ||||
| Rectal pressure | 47 ± 36 | 21, 87 | ns | 0.39 e |
| Anal pressure | 105 ± 44 | 55, 152 | ns | Ns |
| Rectoanal gradient | −58 ± 53 | −128, −1 | ns | Ns |
| % Anal relaxation | 5 ± 29 | −32, 44 | ns | Ns |
| Simulated evacuation with rectal distention | ||||
| Rectal pressure | 152 ± 60 | 76, 222 | ns | 0.37 f |
| Anal pressure | 96 ± 43 | 47, 156 | ns | Ns |
| Rectoanal gradient | 56 ± 65 | −36, 143 | ns | 0.37 f |
| % Anal relaxation | −1 ± 32 | −47, 37 | ns | Ns |
| Valsalva without rectal distention | ||||
| Anal Pressure | 173 ± 65 | 104, 258 | ns | Ns |
Values are mm Hg unless stated otherwise.
Spearman correlation coefficient,
These values are derived from the squeeze maneuver with the highest squeeze pressure
Squeeze increment is (anal squeeze pressure – anal resting pressure)
Average squeeze duration of 3 maneuvers.
P < 0.01,
P < 0.05; HPZ – high pressure zone. ns – not significant
Comparison of Rectoanal Pressures in Participants with a Normal and an Abnormal Rectal BET
Compared to women with a normal BET, women with an abnormal BET had (i) a lower (p<0.05) rectoanal gradient during evacuation both with (67 ± 37 vs. 101 ± 66 mmHg, P < 0.01) and without (−52 ± 27 vs −34 ± 26 mmHg, P < 0.05) rectal distention (Table 3), (ii) higher anal pressures (78 ± 23 vs 63 ± 21 mmHg, P < 0.05) during simulated evacuation without rectal distention, (iii) lower rectal pressure (138 ± 36 vs 165 ± 58 mmHg, P < 0.05) and less anal relaxation (3 ± 30 vs 14 ± 25 %, P < 0.05) during simulated evacuation with rectal distention, and (iv) higher anal pressure (146 ± 52 vs 116 ± 43 mmHg, P < 0.05) during Valsalva maneuver without rectal distention. In men there were no statistically significant differences between participants with a normal versus prolonged BET.
Table 3:
HRM Parameters in Female Participants with Normal and Abnormal BET
| Variable | Women with Normal BET (n = 96) | Women with Abnormal BET (n = 17) | P Value | ||
|---|---|---|---|---|---|
| Mean ± SD | 10th, 90th percentile | Mean ± SD | 10th, 90th percentile | ||
| Anal resting pressure | 78 ± 25 | 44, 110 | 77 ± 21 | 48, 100 | .83 |
| Anal HPZ length (cm) | 3.4 ± 0.8 | 2.3, 4.5 | 3.5 ± 0.9 | 2.3, 4.7 | .44 |
| Anal squeeze pressure a | 201 ± 61 | 127, 281 | 203 ± 52 | 121, 262 | .80 |
| Anal squeeze increment a, b | 124 ± 56 | 51, 194 | 125 ± 45 | 49, 191 | .69 |
| Anal squeeze duration (s) c | 13 ± 7 | 3, 22 | 14 ± 6 | 4, 21 | >.99 |
| First sensation (mL) | 37 ± 14 | 20, 58 (n = 81) | 44 ± 19 | 20, 76 (n = 15) | .24 |
| Urgency (mL) | 63 ± 22 | 40, 90 (n = 82) | 75 ± 22 | 60, 120 (n = 15) | .03 |
| Discomfort (mL) | 102 ± 31 | 60, 140 (n = 79) | 135 ± 68 | 72, 264 (n = 15) | .12 |
| Balloon expulsion time (s) | 12 ± 12 | 2, 24 | 163 ± 38 | 82, 180 | - |
| Simulated evacuation without rectal distention | |||||
| Rectal pressure | 30 ± 21 | 4, 62 | 27 ± 15 | 9, 52 | .70 |
| Anal pressure | 63 ± 21 | 36, 91 | 78 ± 23 | 40, 110 | .01 |
| Rectoanal gradient | −34 ± 26 | −66, 2 | −52 ± 27 | −84, −12 | .02 |
| Anal relaxation (%) | 20 ± 35 | −16, 50 | 10 ± 30 | −42, 57 | .07 |
| Simulated evacuation with rectal distention | |||||
| Rectal pressure | 165 ± 58 | 124, 197 | 138 ± 36 | 63, 182 | .02 |
| Anal pressure | 63 ± 24 | 38, 98 | 71 ± 21 | 35, 104 | .09 |
| Rectoanal gradient | 101 ± 66 | 45, 138 | 67 ± 37 | 0, 113 | .002 |
| Anal relaxation (%) | 14 ± 25 | −10, 43 | 3 ± 30 | −35, 50 | .046 |
| Valsalva without rectal distention | |||||
| Anal Pressure | 116 ± 43 | 62, 174 | 146 ± 52 | 91, 242 | .046 |
Values are mm Hg unless stated otherwise. HPZ – high pressure zone.
These values are derived from the squeeze maneuver with the highest squeeze pressure
Squeeze increment is (anal squeeze pressure – anal resting pressure)
Average squeeze duration of 3 maneuvers.
Comparison of Rectoanal Pressures in Male and Female Participants with a Normal Rectal BET
Some rectoanal parameters were significantly different between men and women with a normal BET (Table 4, Figures 1–4). Compared to women, in men the high pressure zone was longer (3.9±0.8 vs. 3.4±0.8 cm, P < 0.01), the anal squeeze pressure (257±78 vs. 201±61 mmHg, P < 0.01) and the squeeze increment (174±81 vs. 124±56 mmHg, P < 0.01) were higher, as was the rectal threshold for discomfort (123±53 vs. 102±31 mL, P < 0.05). During simulated evacuation with and without rectal distention, men had higher rectal and anal pressures, less anal relaxation, and a lesser rectoanal gradient than women. During the Valsalva maneuver, the anal pressure was higher in men than in women (173±65 vs. 116±43 mmHg, P < 0.01).
Table 4:
HRM Parameters in all Participants Stratified by Normal or Abnormal BET
| Variable | Women with Normal BET (n = 96) | Women with Abnormal BET (n = 17) | Men with Normal BET (n = 47) | Men with Abnormal BET (n = 3) | P Value |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Anal resting pressure | 78 ± 25 | 77 ± 21 | 83 ± 25 | 78 ± 18 | .13 |
| Anal HPZ lengtd (cm) | 3.4 ± 0.8 | 3.5 ± 0.9 | 3.9 ± 0.8 | 4.0 ± 0.5 | <.001 |
| Anal squeeze pressure a | 201 ± 61 | 203 ± 52 | 257 ± 78 | 206 ± 46 | <.001 |
| Anal squeeze increment a, b | 124 ± 56 | 125 ± 45 | 174 ± 81 | 128 ± 33 | <.001 |
| Anal squeeze duration (s) c | 13 ± 7 | 14 ± 6 | 14 ± 7 | 16 ± 2 | .53 |
| First sensation (mL) | 37 ± 14 | 44 ± 19 | 44 ± 26 | 40 ± 0 | .33 |
| Urgency (mL) | 63 ± 22 | 75 ± 22 | 74 ± 34 | 60 ± 0 | .06 |
| Discomfort (mL) | 102 ± 31 | 135 ± 68 | 123 ± 53 | 130 ± 46 | .049 |
| Balloon expulsion time (s) | 12 ± 12 | 163 ± 38 | 12 ± 12 | 180 ± 0 | .89 |
| Simulated evacuation without rectal distention | |||||
| Rectal pressure | 30 ± 21 | 27 ± 15 | 47 ± 36 | 30 ± 18 | <.001 |
| Anal pressure | 63 ± 21 | 78 ± 23 | 105 ± 44 | 109 ± 42 | <.001 |
| Rectoanal gradient | −34 ± 26 | −52 ± 27 | −58 ± 53 | −80 ± 24 | .02 |
| Anal relaxation (%) | 20 ± 35 | 10 ± 30 | 5 ± 29 | −6 ± 35 | <.001 |
| Simulated evacuation with rectal distention | |||||
| Rectal pressure | 165 ± 58 | 138 ± 36 | 152 ± 60 | 172 ± 9 | .82 |
| Anal pressure | 63 ± 24 | 71 ± 21 | 96 ± 43 | 78 ± 58 | <.001 |
| Rectoanal gradient | 101 ± 66 | 67 ± 37 | 56 ± 65 | 94 ± 52 | <. 001 |
| Anal relaxation (%) | 14 ± 25 | 3 ± 30 | −1 ± 32 | 11 ± 41 | .003 |
| Valsalva without rectal distention | |||||
| Anal Pressure | 116 ± 43 | 146 ± 52 | 173 ± 65 | 115 ± 111 | <.001 |
Values are mm Hg unless stated otherwise. HPZ – high pressure zone.
These values are derived from the squeeze maneuver with the highest squeeze pressure
Squeeze increment is (anal squeeze pressure – anal resting pressure).
Average squeeze duration of 3 maneuvers.
Figure 1. Resting Anal Pressure in Men and Women with Normal Balloon Expulsion Time.
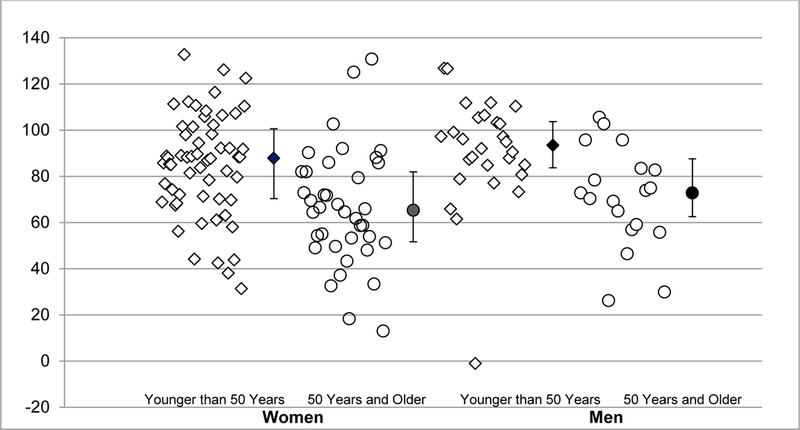
Individual values are represented by unfilled diamonds (younger than 50 years) and circles (50 years and older). The median and interquartile range is denoted by the filled symbols.
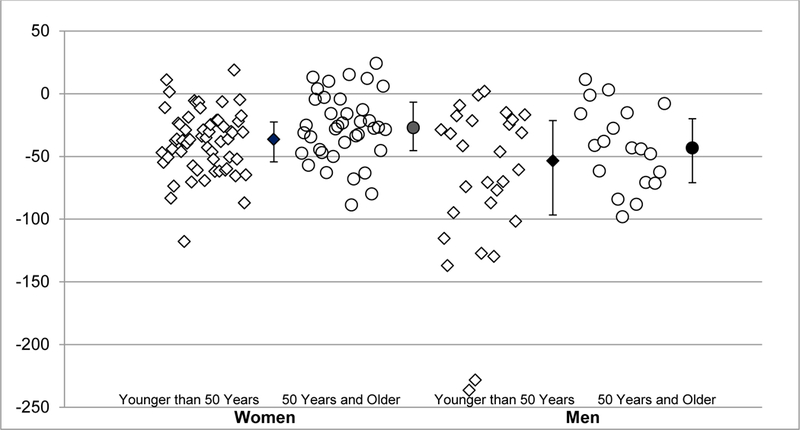
Figure 4. Rectoanal Gradient with Rectal Balloon Distention in Men and Women with Normal Balloon Expulsion Time.
Individual values are represented by unfilled diamonds (younger than 50 years) and circles (50 years and older). Themedian and interquartile range is denoted by the filled symbols. The rectoanal gradient is lower (P < 0.001) in men than women.
DISCUSSION
This is the largest study of rectoanal pressures measured with HRM in healthy people. Seventeen of 113 asymptomatic women (15%) and three of 50 men (6%) had a BET greater than 60 seconds, which is the upper limit of normal for comparable balloons 12, 18–20. This proportion is comparable to previous studies in which approximately 10% of healthy participants could not expel a 50 ml balloon filled with water 18 or artificial stool from the rectum 21. Because the BET is highly specific for diagnosing pelvic floor dysfunction documented with defecography 20, 22, the participants with an abnormal BET were not included in the consideration of normal values. Among women, the rectoanal gradient during evacuation was also lower (ie, more negative) in asymptomatic women with an abnormal BET, which suggests that the inability to expel the balloon was not isolated to the BET; these participants were either unable to replicate defecation in the test environment or have asymptomatic pelvic floor dysfunction. Because rectoanal pressures during evacuation are different in women with a normal and abnormal BET, the normal values in this report are only based on men and women with a normal BET.
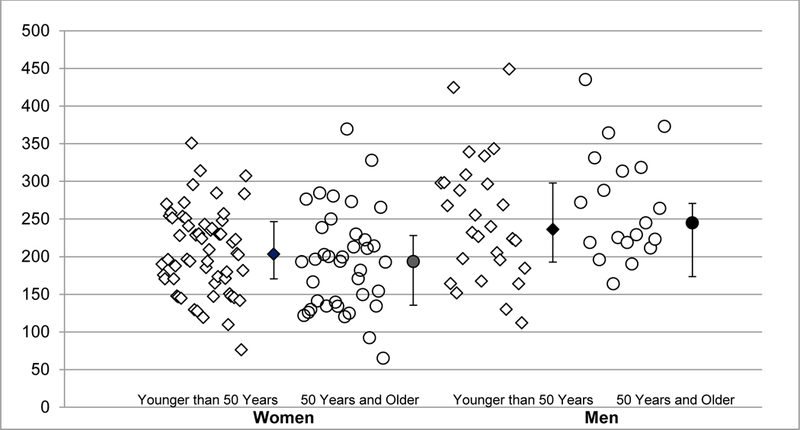
While the normal values are presented separately for younger and older women, only some rectoanal parameters, notably the anal resting pressure, the BET, rectal pressure and the rectoanal gradient during evacuation were associated with age. Among women, the normal values for rectoanal pressures are similar to our previous report 9. However, the anal squeeze pressure and increment were respectively 201 ± 6 mmHg and 124 ± 6 mmHg (mean ± SEM), which is higher than the corresponding values of 164 ± 7 mmHg and 85 ± 7 mmHg published previously. Similar to previous studies, the rectoanal gradient during evacuation without rectal distention was negative, which contradicts the supposition that this gradient should be positive in asymptomatic healthy people 2. Because the normal values for the rectoanal gradient were derived from healthy people with a normal BET, it is unlikely that these data are biased by people with asymptomatic pelvic floor dysfunction. In this study, the lower tenth percentile value for rectoanal gradient without rectal distention was −70mmHg in women younger than 50 years and −64mmHg in women 50 years and older. Only when the gradient is more negative than these values is it abnormal. Several potential explanations for a negative gradient (ie, test performance in the left lateral position or an empty rectum or catheter displacement) are also applicable to non-HRM 23. Indeed, by contrast to non-HRM, the topographic display in HRM allows the operator to steady the catheter and reduce catheter displacement. In addition, similar to esophageal HRM catheters, impingement or bending of the anorectal catheter may artefactually increase the measured pressure, thereby predisposing to a negative rectoanal gradient 24.
Confirming previous studies with HRM and non-HRM, the anal resting pressure was lower in older women (Figure 1) 9, 10. Indeed, the Spearman correlation coefficient for this comparison in the present study (ie, −0.34) was similar to prior studies i.e., −0.47 with HRM and −0.44 with non-HRM. During simulated evacuation with rectal distention, the rectoanal gradient was more conducive to normal evacuation in older than younger women in this study, similar to our prior report 9. By contrast, while age is associated with neurogenic or myogenic injury of the external anal sphincter evaluated with electromyography 25, neither the anal squeeze pressure nor the squeeze duration were correlated with age in this study. These findings suggests that age has more pronounced effects on internal than external anal sphincter function in men and women.
Similar to women with FI, the rectal threshold volume for discomfort was correlated with BMI in healthy women 16; the BET was also correlated with BMI in this study. However, the BMI was not associated with these parameters in men, either due to a type II error or because among men, the distribution of BMI values was tighter. By contrast, among 54 healthy Koreans, anal resting pressure was modestly correlated with BMI, even after adjusting for age, sex, and vaginal deliveries 26. In that study, the rectal pressure during evacuation without rectal distention was also correlated with BMI before but not after adjusting for age, sex, and vaginal deliveries. Taken together, these observations suggest that BMI has relatively modest effects on rectoanal functions and as observed previously, with anorectal motion evaluated with MRI 27. By contrast to urinary incontinence, which is clearly associated with BMI, the association between increased BMI and FI before bariatric surgery is variable and weak 28. The severity of FI is comparable in obese and non-obese patients 16. By comparison to non-obese FI patients, decreased stool consistency and a history of cholecystectomy are the major risk factors for FI 16.
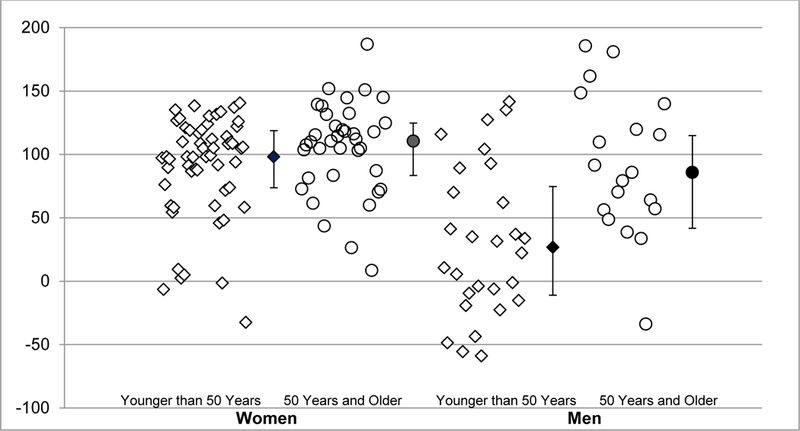
Confirming a previous study, the anal squeeze but not resting pressure was higher in men than women 18. Indeed, the anal squeeze pressure increment, squeeze duration, and HPZ length were higher in men than in women. During simulated evacuation without rectal distention, both anal and rectal pressures were higher in men than women. However, the rectoanal gradient was lower (i.e., more negative) in men than women because sex-related differences in anal pressures were higher than corresponding differences in rectal pressure.
This study was conducted using standardized techniques in a large cohort of asymptomatic participants. Because the commercially-available software program for analyzing HRM has been modified over time, we reanalyzed the studies using the latest version of the software. Recognizing that the accuracy of pressure measurements may be reduced by pressure drift 29, the studies were carefully inspected to ensure that thermal compensation was performed at atmospheric pressure. Consistent with the literature, we considered 60 seconds as the upper limit of normal expulsion time for this balloon 12, 18–20. For a Foley catheter balloon, the normal balloon expulsion time is longer, i.e., up to 120 seconds 30. A recent study that compared the expulsion time for 3 balloons in 44 healthy people observed that the 10–90th percentile range for balloon expulsion time was 2–18 seconds for a party balloon, 1–20 seconds for a commercial balloon, and 4–180 seconds for a Foley catheter. Moreover, “using a cut-off of 120 seconds for the Foley catheter would still incorrectly classify 10/40 healthy subjects” 31.
However, there are potential weaknesses. Assessment of the effects of age and BMI on anorectal functions and BET may have been limited by sample size. Although there was no significant increase in individual’s maximum sphincter pressure, anal squeeze increment, or squeeze duration between the first and final maneuvers (data not shown), it is possible that intra-procedural coaching, which was not used in these studies, could have influenced the test results. In one study, coaching improved the test accuracy 32. Absent anorectal imaging, it is conceivable that asymptomatic individuals had occult disturbances (eg, rectal intussusception) of unclear, if any, clinical significance. It is conceivable that the observed normal values may be affected by other obstetric variables (e.g., birthweight), which were not evaluated, among women who had children in the study.
In summary, these findings provide normal values for rectoanal pressures measured with HRM in women and men. The BET is longer than 60 seconds in 15% of asymptomatic healthy females and 6% of asymptomatic healthy males. In men and women with a normal BET, age is correlated with lower resting anal pressure and a rectoanal pressure profile that is more conducive to evacuation; the BET was also shorter in older than younger women. By comparison with age, the relationship between BMI and rectoanal pressures is modest.
Supplementary Material
Figure 2. Anal Squeeze Pressures in Men and Women with Normal Balloon Expulsion Time.
Individual values are represented by unfilled diamonds (younger than 50 years) and circles (50 years and older) The median and interquartile range is denoted by the filled shapes. The squeeze pressure is higher (P < 0.001) in men than women.
Figure 3. Rectoanal Gradient without Rectal Balloon Distension in Men and Women with Normal Balloon Expulsion Time.
Individual values are represented by unfilled diamonds (younger than 50 years) and circles (50 years and older). The median and interquartile range is denoted by the filled symbols. The rectoanal gradient is lower (P = 0.02) in men than women.
KEY POINTS.
Among healthy men and women, older people have a lower anal resting pressure and higher rectal pressure during evacuation.
Anal squeeze pressure and duration are higher in men than women. Increased BMI is associated with a longer BET in women.
Compared to women with a normal BET, women with an abnormal BET had a lower (more negative or less positive) rectoanal gradient during evacuation.
ACKNOWLEDGEMENTS
• NO analyzed and reviewed the data and authored the manuscript
• SG and AM reviewed the data
• SC, MS, DP, and KF collected data in multiple studies
• AEB designed the study, analyzed the data and authored the manuscript
• All authors reviewed and approved the final submitted version.
FUNDING
This work was supported in part by USPHS NIH Grant P01 DK78924.
Footnotes
DISCLOSURES
AEB holds patents for a portable anorectal manometry device and an anorectal catheter fixation device which have been licensed respectively to Medspira Inc and Medronic Inc.
REFERENCES
- 1.Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology 2013;144:218–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee TH, Bharucha AE. How to Perform and Interpret a High-resolution Anorectal Manometry Test. Journal of neurogastroenterology and motility 2016;22:46–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basilisco G, Bharucha AE. High-resolution anorectal manometry: An expensive hobby or worth every penny? Neurogastroenterology & Motility 2017;29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carrington EV, Scott SM, Bharucha A, et al. Expert consensus document: Advances in the evaluation of anorectal function. Nature Reviews Gastroenterology & Hepatology 2018;15:309–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bharucha AE, Locke GR, Pemberton JH. AGA Practice Guideline on Constipation: Technical Review. Gastroenterology 2013;144:218–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao SS, Bharucha AE, Chiarioni G, et al. Functional Anorectal Disorders. Gastroenterology 2016;25:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wald A, Bharucha AE, Cosman BC, et al. ACG Clinical Guidelines:Management of Benign Anorectal Disorders. American Journal of Gastroenterology 2014;109:1141–57. [DOI] [PubMed] [Google Scholar]
- 8.Bharucha AE, Stroetz R, Feuerhak K, et al. A novel technique for bedside anorectal manometry in humans. Neurogastroenterology and Motility 2015:1504–1508. [DOI] [PMC free article] [PubMed]
- 9.Noelting J, Ratuapli SK, Bharucha AE, et al. Normal Values For High-Resolution Anorectal Manometry In Healthy Women: Effects Of Age And Significance Of Rectoanal Gradient. American Journal of Gastroenterology 2012;107:1530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fox JC, Fletcher JG, Zinsmeister AR, et al. Effect of aging on anorectal and pelvic floor functions in females. Diseases of the Colon & Rectum 2006;49:1726–35. [DOI] [PubMed] [Google Scholar]
- 11.Grossi U, Carrington EV, Bharucha AE, et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 2016;65:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ratuapli S, Bharucha AE, Harvey D, et al. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterology and Motility 2013;25:e813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ratuapli S, Bharucha AE, Noelting J, et al. Phenotypic Identification and Classification of Functional Defecatory Disorders Using High Resolution Anorectal Manometry Gastroenterology 2013;144:314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bharucha AE, Zinsmeister AR, Schleck CD, et al. Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population-based case-control study in women. Gastroenterology 2010;139:1559–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberson EN, Gould JC, Wald A. Urinary and Fecal Incontinence after Bariatric Surgery. Digestive Diseases and Sciences 2010;55:2606–2613. [DOI] [PubMed] [Google Scholar]
- 16.Brochard C, Venara A, Bodere A, et al. Pathophysiology of fecal incontinence in obese patients: A prospective case-matched study of 201 patients. Neurogastroenterology & Motility 2017;29. [DOI] [PubMed] [Google Scholar]
- 17.Chakraborty S, Feuerhak K, Muthyala A, et al. Effects of Alfuzosin, an Alpha-1 Alphadrenergic Antagonist on Anal Pressures and Bowel Habits, in Women With and Without Defecatory Disorders. Clinical Gastroenterology & Hepatology 2018;18:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao SS, Hatfield R, Soffer E, et al. Manometric tests of anorectal function in healthy adults. American Journal of Gastroenterology 1999;94:773–83. [DOI] [PubMed] [Google Scholar]
- 19.Mazor Y, Prott G, Jones M, et al. Anorectal physiology in health: a randomized trial to determine the optimum catheter for the balloon expulsion test. Neurogastroenterol and Motility 2019;31. [DOI] [PubMed] [Google Scholar]
- 20.Minguez M, Herreros B, Sanchiz V, et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62. [DOI] [PubMed] [Google Scholar]
- 21.Wald A, Jafri F, Rehder J, et al. Scintigraphic studies of rectal emptying in patients with constipation and defecatory difficulty. Digestive Diseases and Sciences 1993;38:353–8. [DOI] [PubMed] [Google Scholar]
- 22.Prichard DO, Lee T, Parthasarathy G, et al. High-resolution Anorectal Manometry for Identifying Defecatory Disorders and Rectal Structural Abnormalities in Women. Clinical Gastroenterology & Hepatology 2017;15:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sauter M, Heinrich H, Fox M, et al. Toward more accurate measurements of anorectal motor and sensory function in routine clinical practice: validation of high-resolution anorectal manometry and Rapid Barostat Bag measurements of rectal function. Neurogastroenterology and Motility 2014;26:685–95. [DOI] [PubMed] [Google Scholar]
- 24.Babaei A, Szabo A, Yorio SD, et al. Pressure exposure and catheter impingement affect the recorded pressure in the Manoscan 360TM system. Neurogastroenterology & Motility 2018;09:09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bharucha AE, Daube J, Litchy W, et al. Anal sphincteric neurogenic injury in asymptomatic nulliparous women and fecal incontinence. American Journal of Physiology-Gastrointestinal & Liver Physiology 2012;303:G256–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee HJ, Jung KW, Han S, et al. Normal values for high-resolution anorectal manometry/topography in a healthy Korean population and the effects of gender and body mass index. Neurogastroenterology and Motility 2014;26:529–37. [DOI] [PubMed] [Google Scholar]
- 27.Tirumanisetty P, Prichard D, Fletcher JG, et al. Normal values for assessment of anal sphincter morphology, anorectal motion, and pelvic organ prolapse with MRI in healthy women. Neurogastroenterology & Motility 2018;30:e13314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bharucha AE. Incontinence-An Underappreciated Problem In Obesity And Bariatric Surgery. Digestive Diseases and Sciences 2010;55:2428–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parthasarathy G, McMaster J, Feuerhak K, et al. Determinants and clinical impact of pressure drift in manoscan anorectal high resolution manometry system. Neurogastroenterology & Motility 2016;28:1433–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiarioni G, Kim SM, Vantini I, et al. Validation of the Balloon Evacuation Test: Reproducibility and Agreement With Findings From Anorectal Manometry and Electromyography. Clinical Gastroenterology and Hepatology 2014;12:2049–54. [DOI] [PubMed] [Google Scholar]
- 31.Mazor Y, Prott G, Jones M, et al. Anorectal physiology in health: A randomized trial to determine the optimum catheter for the balloon expulsion test. Neurogastroenterol Motil 2019:e13552. [DOI] [PubMed]
- 32.Heinrich H, Fruehauf H, Sauter M, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterology and Motility 2013;25:e163. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


