Abstract
Objective:
The purpose of this study was to include youth, parents, researchers, and clinicians in the identification of feasible and acceptable strategies for teen suicide screening in the pediatric emergency department (ED).
Methods:
Concept mapping methodology was used to elicit stakeholder responses.
Results:
Regarding the most important result of suicide screening for teens in the pediatric ED, suicide prevention and education for parents, friends, and community members was rated easiest to implement, while short and long-term follow-up and treatment was rated most important. In terms of successful suicide screening for teens in the pediatric ED, provision of resources and information was rated most feasible, and a safe, friendly, private screening environment was rated most important.
Conclusion:
The concept maps can be used to align suicide risk screening with the priorities and recommendations of pediatric ED stakeholders.
Keywords: suicide screening, youth suicide prevention, pediatric emergency department, concept mapping, multidimensional scaling, cluster analysis
Introduction
Suicide is the second leading cause of death among adolescents 12–17 years old in the United States (Centers for Disease Control and Prevention, 2018), and the adolescent suicide death rate has steadily increased in the last decade (National Center for Health Statistics, 2016). The percentage of hospitalizations and ED visits for mental health conditions has increased over the same period, including a 151% increase in inpatient visits for suicidal ideation, attempts, and self-injury among 10 to 14 year olds (Torio, Encinosa, Berdahl, McCormick, & Simpson, 2015). Estimates from attempts that come to medical attention indicate that for every adolescent death by suicide there are 100 to 200 suicide attempts (Drapeau & McIntosh, 2015). Nationally representative data show 17.2% of high school students have had serious thoughts of attempting suicide and 7.4% have made a suicide attempt in the past 12 months (Centers for Disease Control and Prevention, 2018).
Increased attention to suicide prevention has advanced our understanding of adolescent suicidal ideation and behavior, including the identification of demograpic risk factors, such as sex and race, and psychological risk factors (Bridge, Goldstein, & Brent, 2006). For example, the large majority of youth who attempt or die by suicide have a diagnosable psychiatric disorder (Brent et al., 1988; Brent et al., 1993; Bridge et al., 2006) and the receipt of treatment for an existing psychiatric disorder is predictive of suicidal behavior (Groholt, Ekeberg, & Haldorsen, 2006). Careful attention to previous diagnoses may help identify suicide risk when patients are already engaged with the health system, but such strategies do not go far enough. The Joint Commission has recently emphasized the need to screen for suicide risk in all clinical settings (The Joint Commission, 2016). For 1.5 million children in the United States, the Emergency Department (ED)1 is the only source of medical care (Wilson & Klein, 2000), making it a vital, but historically underutilized (Larkin & Beautrais, 2010) setting for suicide prevention. However, many at-risk youth presenting in EDs do not have previously diagnosed mental health or alcohol and substance abuse concerns (King, O’Mara, Hayward, & Cunningham, 2009), which could alert providers to risk, and adolescents tend not to seek help for mental health conditions or disclose suicidal ideation unless directly questioned on the topic (Ballard et al., 2012; Brent et al., 1986; Michelmore & Hindley, 2012).
Brief, validated screening tools can help overcome these barriers, and studies have shown that ED screening effectively identifies suicide risk (Betz et al., 2016; Fein et al., 2010; King et al., 2009). The goal of screening is not to diagnose suicidality but to identify youth who require further assessment in order to determine actual level of risk. This further assessment might be in the form of a longer validated questionnaire, an in-depth conversation with the health care provider, or a structured evaluation by a mental health professional—or it may be a step-wise series of increasingly detailed assessments aimed at clarifying the patient’s level of suicide risk. Those for whom additional evaluation ultimately reveals elevated suicide risk can then be connected with appropriate services. Ideally, a screening instrument is short enough to administer to every patient and sensitive enough to accurately identify nearly all youth who are experiencing suicidal ideation or who are characterized by elevated suicide risk. Practically, however, an ideal screening instrument must also be specific enough to avoid yielding positive scores for large numbers of youth who are not at risk, thus creating an unmanageable burden for the limited number of health care providers available on any given shift.
One advantage of screening in the ED is that, in contrast to other health care settings, it is often possible for a mental health provider to assess youth who screen positive on brief instruments before they leave the hospital, thus eliminating one barrier to care (Horowitz, Ballard & Pao, 2009). Screening for suicide risk in the ED has been well-accepted by pediatric patients when implemented (Ballard et al., 2012; Horowitz et al., 2010), and while the busy environment of the ED may raise feasibility concerns among clinicians, there is evidence that these perceptions may evolve when screenings are actually implemented (Betz et al., 2015). The current study was conducted to address gaps in the implementation of suicide screening in the ED by understanding the perspectives of relevant stakeholders. The aim of the study was to compare and contrast thoughts about effective screening among patients, researchers, and clinicians in order to inform future implementation of suicide screening in the ED.
Methods
The study employed a mixed method design by using concept mapping (CM). CM is an integrative research method that combines qualitative data collection with quantitative analysis to examine diverse perspectives from a range of stakeholders (Burke et al., 2005; Kane & Trochim, 2007; Trochim, 1989; Vaughn & McLinden, 2016). The method produces a visual concept map that can easily be understood and used by stakeholders to conceptualize a complex problem and develop solutions for addressing it (Rosas & Kane, 2012). For example, CM has been used to prioritize HIV-related strategies in the Black faith community (Szaflarski, Vaughn, McLinden, Wess, & Ruffner, 2015), address obesity and bullying in a low-income, minority/immigrant school (Vaughn, Jacquez & McLinden, 2013), address violence in South African communities (Crawford-Browne & Kaminer, 2012), and reduce substance abuse in distressed African American communities (Windsor & Murugan, 2012).
CM methodology deviates from traditional research approaches, which often lack direct involvement of community members, by offering a structured, visual mapping approach for all stakeholders to be involved in generating, analyzing, and interpreting data from their unique vantage points (Vaughn, Jones, Booth, & Burke, 2017). Furthermore, the involvement of stakeholders as both participants and co-researchers in CM can contribute to the development of interventions, practices, and policies that are more meaningful and culturally relevant to the stakeholder community (Vaughn et al., 2017). Stakeholder engagement is particularly important in suicide-related research due to a historical emphasis on the broad biomedical paradigm and a lack of attention to unique social, ecological, and cultural contexts that can advance suicidology and positively impact target populations (White, Marsh, Kral, & Morris, 2016). Thus, CM was deemed to be a useful method for obtaining diverse stakeholder input and merging quantitative analysis with the richness of qualitative understanding in a visual format to inform the development and implementation of an effective adolescent suicide screening strategy in the pediatric ED setting.
This study was determined to be exempt from our Institutional Review Board because data was anonymous and intended to inform the screening strategy within a specific ED screening project, Emergency Department Screen for Teens at Risk for Suicide (ED-STARS). However, all study procedures followed ethical standards and met regulations for research involving humans. We provided participants with the reason for the project and what would be entailed for participation. Participants agreed to participate at each step of the CM process.
We partnered with the Youth Council for Suicide Prevention (YCSP), a youth-centric community-academic research partnership to address the prevalence of adolescent suicide in a midwest region of the U.S.. The current YCSP is comprised of 28 youth who volunteer to design and participate in youth participatory action research suicide prevention projects such as this study. Current YCSP membership includes 28 youth ages 14–18 from 11 different high schools across the region representing various economic and ethnic backgrounds. We partnered with the YCSP to define relevant stakeholders and decide on CM focus prompts (described below).
Study participants:
Using purposeful sampling, we identified relevant stakeholders composed of clinicians and social service providers, clinicians who have worked directly with suicidal youth, researchers focused on suicide-related work, youth members of the YCSP, and parents of YCSP youth who have been to the pediatric ED with their teenager to participate in the study. Purposeful sampling is frequently used in qualitative research to fully understand the phenomenon of interest from individuals who have direct experience with it (Creswell & Plano Clark, 2011). It can be a rigorous sampling technique in mixed methods research (Palinkas et al., 2015). Each stakeholder group was selected based on their unique experiences and collective ability to contribute to a comprehensive examination of suicide screening in the pediatric ED. Although some of the participants occupied more than one role (e.g. clinicians who are researchers and parents), they were categorized and responded to prompts based on their most salient role in suicide prevention efforts. Initial provider and researcher participants were identified through the existing Pediatric Emergency Care Applied Research Network (PECARN), and initial youth and parent participants were identified through the YCSP. Next, these participants were asked to identify additional participants (snowball sampling) similar to them (e.g., other providers or other parents).
Procedure:
Previous methodological assessment has demonstrated the validity and utility of CM in implementation research (Jackson & Trochim, 2002; Rosas & Kane, 2012). CM is accomplished through a six-step process of (1) preparation, (2) idea generation, (3) structuring, (4) representation, (5) interpretation and (6) utilization (Kane & Trochim, 2007). Each step is outlined below to assist the reader with understanding the purpose and how CM was employed in this study.
Step 1: Preparation.
A focus prompt (an incomplete sentence) is intended to focus participants and prompt them to generate ideas about the issue. In order to develop effective strategies for teen suicide screening in the ED based on the priorities and perspectives of relevant stakeholders, the current study included two focus prompts: Prompt 1) I believe the most important result of suicide screening for teens in the ED is….; and Prompt 2) Successful suicide screening for teens in the ED should include….
Step 2: Idea generation (data collection).
After receiving an explanation of the purpose of the study and an overview of CM steps, participants were asked either in person or via email to generate 3–5 ideas in response to each of the two focus prompts.
Step 3: Structuring the ideas.
Using online software (Optimal Workshop Ltd, 2017), a subset of participants from Step 2 sorted the qualitative responses (ideas) to each focus prompt by grouping similar ideas into similar categories for each prompt as recommended by CM scholars (Kane & Trochim 2007). (Trochim & Kane, 2005; Wood & Wood, 2008)Each sorter grouped conceptually similar ideas and named their groups to capture the similarity of ideas (themes). Sorters were prepared for this task by sending them an email with a link to the online software with instructions as to what they were supposed to do.
Step 4: Representation (data analysis).
Multidimensional scaling and hierarchical cluster analysis were performed to illustrate the conceptual similarity of ideas and aggregate the ideas into clusters (Kane & Trochim, 2007). Stakeholders who participated in either Step 2 or 3, provided value ratings of importance and feasibility of implementation (Likert scale 1 to 5) of the resulting clusters in each of the two concept maps. “Pattern Matching” (Kane & Trochim, 2007) compared value ratings across the stakeholder groups for clusters in each concept map.
Step 5: Interpretation.
The research team reviewed the prompt cluster solutions including the ideas and names associated with each cluster during the sorting process. Because there is not an objective best number of clusters, most appropriate cluster solutions balanced sufficient detail with as little overlap as possible. Next, the research team labeled each cluster based on the overall idea themes using the categories suggested by the sorters.
Step 6: Utilization.
The resulting maps will be shared with study participants and the larger PECARN network as recommendations for suicide screening in the pediatric ED. Data analysis: Using R software (R CoreTeam, 2013), sorting data from the respondents for each of the two prompts was first aggregated and analyzed using multidimensional scaling (de Leeuw & Mair, 2009) which creates a map of the ideas with each idea positioned with x,y distance coordinates in a two-dimensional map where ideas in close proximity tend to have similar meaning. Then, hierarchical cluster analysis utilizing Ward’s algorithm (Everitt, 1980) was applied to these coordinates to compute clusters of points that identified similar ideas (Kane & Trochim, 2007). Next, the mean value for each cluster was calculated, and the pattern of results was examined across all stakeholders and within three stakeholder groups (youth, researchers, clinicians) by rank-ordering the final clusters on a ladder graph (vertical number line) for importance and feasibility of implementation for each prompt (termed “pattern matching” as described above).
Results
Study participants:
Study participants for data collection in Step 2 (total n = 149) included a purposeful sample of relevant stakeholders (40% clinicians and social service providers, 25% clinicians who have worked with suicidal youth, 11% researchers involved with suicide screening, awareness, and prevention, 11% youth members of the YCSP, 13% parents of YCSP youth or who have been to the pediatric ED with their teenager). Of the 149 participants, 67% were female and ranged in age group (28% 40–49 years; 19% 30–39 years; 15% 14–19 years; 15% 50–59 years). Previous work in CM has shown that there is minimal variation in the final concept map after 20 to 30 sorts (Trochim & Kane, 2005; Wood & Wood, 2008). Thus, a subset of the participants from Step 2 (n = 32 which included 12 (37%) youth, seven providers (22%), six (19%) researchers, and seven (22%) combined clinician/researchers) completed Step 3, the sorting step. The rating step included youth (n = 16; 33%), researchers (n = 16; 33%) and clinicians (n = 16; 33%), who had participated in either Steps 2 or 3. It is common within CM to have different samples for each step of the process (Vaughn & McLinden, 2016).
Idea generation:
Stakeholders generated a total of 501 ideas for Prompt 1 (I believe the most important result of suicide screening for teens in the ED is….) and 428 ideas for Prompt 2 (I believe that successful suicide screening in the ED should include…). In order to ensure completeness, represent diversity of ideas, and yet minimize the response burden for the next sorting step, the research team eliminated redundant ideas that essentially expressed the same idea and chose the 80 unique statements (50 < number of statements ≤ 100) per focus prompt that most clearly represented the overall responses. The final responses were edited for grammar and clarity of expression without altering the original response meaning.
Concept maps:
Prompt 1, the most important result of suicide screening for teens in the ED, has seven clusters (Figure 1). Cluster 2, Short and Long-Term Follow-Up and Treatment, represented the largest percentage of the original responses (26%). Prompt 2, Successful suicide screening in the ED, had a total of six clusters (Figure 2). In this case, Cluster 5, Thorough Risk Assessment, represented the largest percentage of original responses (25%). Stakeholders defined a “thorough risk assessment” as identifying all the factors that might contribute to or prevent a suicide attempt including severity of intent/plan, resiliency factors, risk factors and issues with school, relationships, substance abuse, and bullying.
Figure 1.
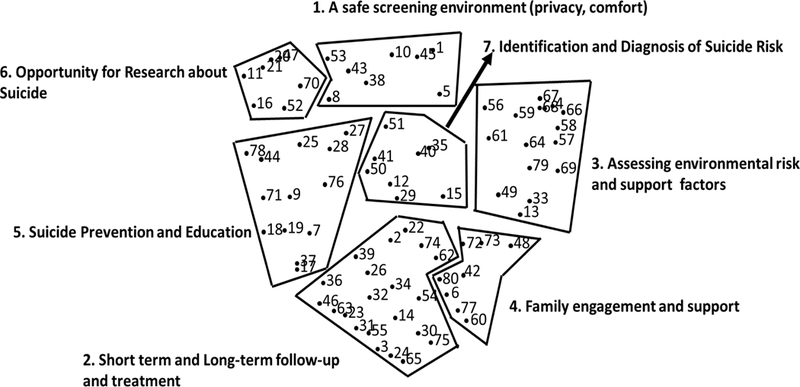
Concept map for Prompt 1 (I believe the most important result of suicide screening for teens in the emergency department is…). Figure 1 illustrates the point map and seven cluster solution for Prompt 1.
Figure 2.
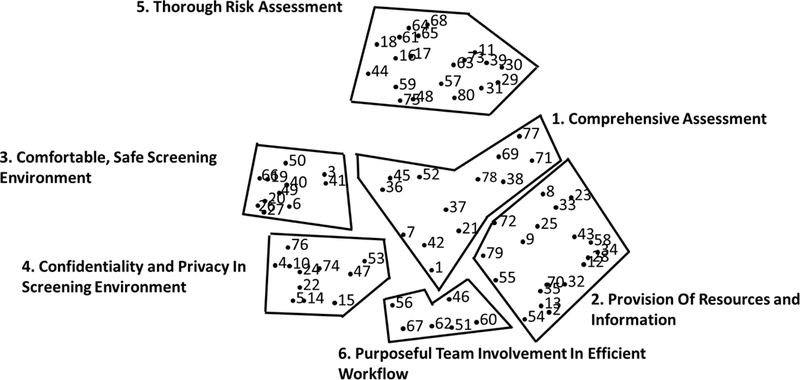
Concept map for Prompt 2 (Successful suicide screening for teens in the emergency department should include…). Figure 2 illustrates the point map and six cluster solution for Prompt 2.
The stress values (a statistic that helps determine how well the point map of ideas represents the data and the strength of the relationship between input matrix and distances on the map) of 0.23 and 0.19 for 80 ideas for each of the prompts indicates a good fit (Kane & Trochim, 2007). A good fit means there is less than 1% chance that the ideas were randomly arranged (Sturrock & Rocha, 2000). The concept maps for Prompts 1 and 2 are shown in Figures 1 and 2 respectively. Table 1 shows an example of responses represented in each of the clusters for the two prompts.
Table 1.
Example Responses in Each Cluster for Prompts 1 and 2
| Prompt 1: Most important result of suicide screening for teens in the emergency department |
Prompt 2: Successful suicide screening for teens in the emergency department should include |
|---|---|
| Cluster 1: A safe screening environment (privacy, comfort) 1) For a parent to not be in the room so the teen feels like he/she can say anything 5) Make sure teens know that they are in a safe environment |
Cluster 1: Comprehensive assessment 38) Early intervention 42) A specialist trained in teenage suicide & prevention 21) Multiple doctor reviews 52) Identifying cases not necessarily obvious on initial emergency department screening |
| Cluster 2: Short term and long-term follow-up and treatment 24) Follow-up care for teens who may be suicidal 46) Connection with the health/medical system for future services |
Cluster 2: Provision of resources and information 58) Providing family with emergency contact numbers and resources for follow-up care 70) Ability of parents to monitor, supervise, support, understand |
| Cluster 3: Assessing environmental risk and support factors 68) Finding out if teen has low self-esteem 69) To see what the teens’ family life is like |
Cluster 3: Comfortable, safe screening environment 26) Encouraging honest responses from the patient 27) A friendly questioner |
| Cluster 4: Family engagement and support 42) Not stigmatizing the family if found to be positive 48) Identify family needs |
Cluster 4: Confidentiality and privacy in screening environment 4) A comfortable, low stress environment 5) Not too many people involved in the actual screening (not intimidating) |
| Cluster 5: Suicide prevention and education 7) Giving information to parents 9) Making suicide prevention resources more prominent and known among teens |
Cluster 5: Thorough risk assessment 75) Distinguishing between cries for help and actual attempts (both need help though) 80) Resiliency factors 57) Identification of suicide risk factors 73) Determine severity of intent and plans |
| Cluster 6: Opportunity for research about suicide 20) Gather and track data to develop ideas to prevent teens from getting to this point 21) The more data the easier to approach entities for funding |
Cluster 6: Purposeful team involvement in efficient workflow 46) Team efforts to prevent suicide even in those teens who come in for other issues 51) Buy in from all stakeholders |
| Cluster 7: Identification and diagnosis of suicide risk 12) Identifying potential causes of these thoughts 15) Letting them know that someone will listen to them |
Pattern matching:
The importance and feasibility of the seven clusters from Prompt 1 and the six clusters from Prompt 2 were compared across all combined stakeholders and within each of the three stakeholder groups (youth, researchers, and clinicians). Keeping in mind that all items and clusters are important and to some extent feasible, pattern analysis, visually through ladder graphs, orients stakeholders’ priorities and beliefs about importance and feasibility. For example, with respect to Prompt 1 (The most important result….), across all the stakeholder groups, Cluster 2, Short and Long-Term Follow-Up and Treatment, was rated as most important while Cluster 3, Assessing Environmental Risk and Support Factors, was rated as least important (Figure 3). Cluster 5, Suicide Prevention and Education, was rated as most feasible, and Cluster 2, Short and Long-Term Follow-Up and Treatment, as least feasible (Figure 3).
Figure 3.
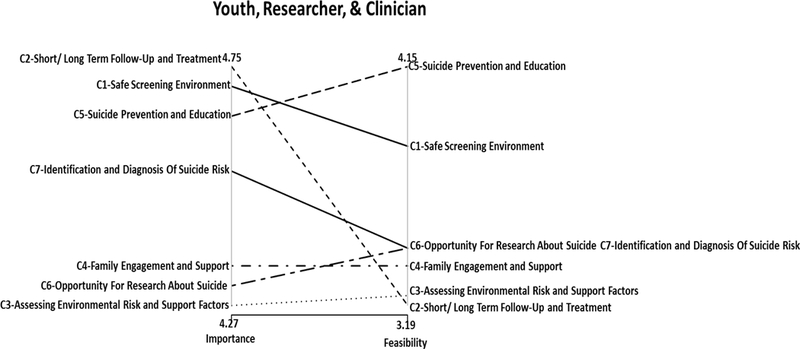
Ladder graph for Prompt 1, all groups. Figure 3 illustrates the pattern matching (importance and feasibility mean ratings) combined across youth, researcher and clinician stakeholder groups for Prompt 1 (I believe the most important result of suicide screening for teens in the emergency department is…). C1-C7 denote names for Clusters 1–7 from the concept map for Prompt 1.
For Prompt 2 (Successful suicide screening….), across all the stakeholder groups, Cluster 3, Comfortable, Safe Screening Environment, was rated as most important. It included ideas such as having a youth-friendly questionnaire that does not include too many questions, building rapport to encourage honest conversation and questionnaire responses, easing into the screening questions by allowing youth ample time to reflect and respond to questions, and conveying to youth that they are important. Cluster 6, Purposeful Team Involvement in Efficient Workflow, was rated as least important (Figure 4) and included ideas such as a simple, straightforward workflow, buy-in from all stakeholders, and team efforts to prevent suicide. Cluster 2, Provision of Resources and Information, was rated as most feasible, and Cluster 5, Thorough Risk Assessment, as least feasible (Figure 4).
Figure 4.
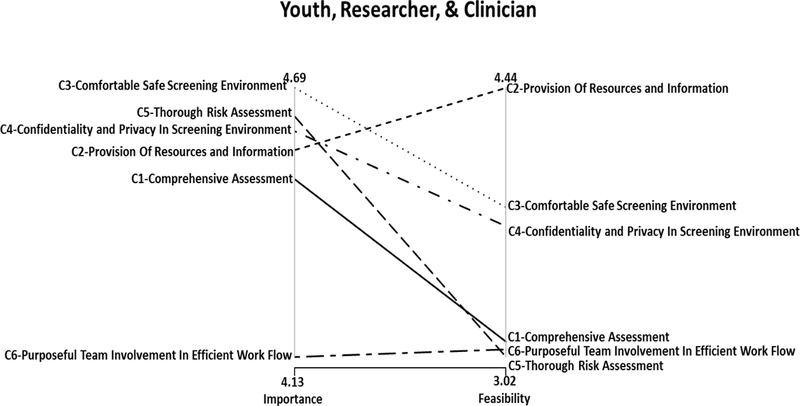
Ladder graph for Prompt 2, all groups. Figure 4 illustrates the pattern matching (importance and feasibility mean ratings) combined across youth, researcher and clinician stakeholder groups for Prompt 2 (Successful suicide screening for teens in the emergency department should include…). C1-C6 denote names for Clusters 1–6 from the concept map for Prompt 2.
Pattern analysis was used to explore the beliefs about importance and feasibility between the three stakeholder groups. For Prompt 1, the biggest differences in agreement were in regard to what was considered most important. Youth rated Cluster 7, Identification and Diagnosis of Suicide Risk, as most important whereas researchers rated Cluster 2, Short and Long-term Follow-up and Cluster 5, Suicide Prevention and Education, and Clinicians rated Cluster 1, A Safe Screening Environment, as most important. Conversely, the most agreement between the different stakeholders was for what is considered most feasible; all three groups agreed that Cluster 5, Suicide Prevention and Education was the most feasible result of pediatric ED suicide screening.
Agreement between stakeholder groups was stronger for Prompt 2 than Prompt 1. Except for researchers’ ratings on what is most important (Cluster 1, Comprehensive Assessment [e.g. conducted by multiple professionals, assessing all youth presenting to the ED for mental health or substance abuse and not just those who present for suicide risk, and early intervention]) and least important (Cluster 5, Thorough Risk Assessment as defined on page 11), there was primarily agreement on importance and feasibility regarding what should be included in successful pediatric ED suicide screening. This included complete agreement between youth, researchers, and clinicians that Cluster 5, Thorough Risk Assessment is least feasible and Cluster 2, Provision of Resources and Information is most feasible. Table 2 displays the pattern analysis for both prompts for comparison within and between the three stakeholder groups.
Table 2.
Pattern Matching (Importance and Feasibility Ratings) within Stakeholder Groups (Youth, Researcher, Clinician) for Prompts 1 and 2
| PROMPT 1 (I believe the most important result of suicide screening for teens in the emergency department is…) | ||||
| MOST IMPORTANT |
LEAST IMPORTANT |
MOST FEASIBLE |
LEAST FEASIBLE |
|
| YOUTH | Cluster 7, Identification and Diagnosis of Suicide Risk | Cluster 6, Opportunity for Research about Suicide* | Cluster 5, Suicide Prevention and Education* | Cluster 3, Assessing Environmental Risk and Support Factors |
| RESEARCHER | Cluster 2, Short Term and Long-Term Follow-Up and Treatment & Cluster 5, Suicide Prevention and Education | Cluster 3, Assessing Environmental Risk and Support factors* | Cluster 5, Suicide Prevention and Education* | Cluster 2, Short Term and Long-Term Follow-Up and Treatment* |
| CLINICIAN | Cluster 1, A Safe Screening Environment (Privacy, Comfort) | Cluster 3, Assessing Environmental Risk and Support Factors & Cluster 6*, Opportunity for Research about Suicide* | Cluster 5, Suicide Prevention and Education* | Cluster 2, Short Term and Long-Term Follow-Up and Treatment* |
| PROMPT 2(Successful suicide screening for teens in the emergency department should include…) | ||||
| MOST IMPORTANT |
LEAST IMPORTANT |
MOST FEASIBLE |
LEAST FEASIBLE |
|
| YOUTH | Cluster 3, Comfortable, Safe Screening Environment* | Cluster 6, Purposeful Team Involvement in Efficient Workflow* | Cluster 2, Provision of Resources and Information* | Cluster 5, Thorough Risk Assessment* |
| RESEARCHER | Cluster 1, Comprehensive Assessment | Cluster 5, Thorough Risk Assessment | Cluster 2, Provision of Resources and Information* | Cluster 5, Thorough Risk Assessment* |
| CLINICIAN | Cluster 3, Comfortable, Safe Screening Environment* | Cluster 6, Purposeful Team Involvement in Efficient Workflow* | Cluster 2, Provision of Resources and Information* | Cluster 5, Thorough Risk Assessment* |
Denotes clusters in which there was agreement on importance and feasibility between at least two of the stakeholder groups.
Note. The emergency department is synonymous with emergency room, emergency ward, or casualty department and describes a medical treatment facility, usually hospital-based, specializing in accident services and delivery of emergency medical care.
Discussion
Across all stakeholder groups, the CM results from this study indicated some level of discrepancy between the strategies stakeholders deemed important as indicators of “successful” screening and practices they viewed as feasible in the pediatric ED. Members of the different stakeholder groups in this study did not agree completely on the strategies that were most important for suicide screening or on the relative feasibility of various approaches, which supports this study’s aim to compare and contrast stakeholder perspectives in order to improve pediatric ED screening. As pediatric EDs seek to expand screening for suicide risk in teens, it is critical to understand what different stakeholders expect during, and as a result of, the screening process. While these differences add to the complexity of developing a successful suicide screening strategy, this initial identification of discrepancies may help to explain previously limited screening practices and lead to insights that can strengthen future screening efforts. Therefore, we discuss the discrepancies below within the context of existing research but also highlight areas of agreement and opportunities for initial implementation.
The current study showed that stakeholders considered follow-up treatment to be the most important result of teen suicide screening in the pediatric ED; however, it was also rated as the least feasible (Prompt 1). Previous studies have shown low rates of follow-up treatment utilization and engagement (Horowitz et al., 2009; Miller, Eckert, & Mazza, 2009) and that compliance varies by diagnosis and parental perceptions of treatment (Burns, Cortell, & Wagner, 2008). Others have also documented a perceived difficulty in accessing mental health services, pessimism about the ability of mental health services to make a difference, difficulties in making referrals, and/or concerns about stigma associated with accessing mental health services (Betz et al., 2016; Gulliver, Griffiths, & Christensen, 2010). Although it has been suggested that mental health interventions be delivered prior to discharge from the ED to mitigate concerns such as these (Horowitz et al., 2009) and this is a standard practice of care in the current study’s ED settings, especially for youth who do not already have ongoing contact with a community-based mental health provider, the current study highlights stakeholder concerns about the feasibility of follow-up treatment in the ED setting. While the current study did not examine exactly why stakeholders believe follow-up treatment is not feasible, the result highlights a need for further research on this stakeholder concern. For example, future research should examine whether feasibility is related the availability of local treatment options, the ability for the ED to link identified youth to treatment, the ability for youth and families to access and adhere to available treatment, or some other unknown reason. Future research may also examine whether the reasons for feasibility of follow-up treatment varies based on other factors.
The delivery of suicide prevention and education was rated by participants in this study as the most feasible result of suicide screening in the ED. Study participants viewed positive screens as opportunities to educate youth and parents about suicide risk, the benefits of ongoing mental health treatment to prevent future suicide risk, and the availability of local treatment programs and related resources. Given the overall participant support for the feasibility of this idea compared to the perceived feasibility of follow-up treatment, pediatric EDs and future research should consider how to improve the provision of suicide prevention and education services and the potential role of this activity as an intermediary in improving follow-up treatment access and adherence.
Regarding what is perceived as a successful indicator for suicide screening in the pediatric ED (Prompt 2), the most identified aspect amongst all stakeholders was a comfortable and safe screening environment, and the most feasible strategy was the provision of resources and information. Least important was purposeful team involvement in efficient workflow and least feasible was a thorough risk assessment (e.g., severity of risk, multiple contributors, resiliency factors, etc.). However, differences amongst the stakeholder groups indicated youth and clinicians found a comfortable, safe screening environment to be more important than the researchers who, not surprisingly, were more interested in a comprehensive assessment, which was represented by responses regarding the involvement of multiple professionals, assessing all youth presenting to the ED for mental health or substance abuse not just those who enter for suicide risk, and early intervention. This discrepancy validates the inclusion of multiple stakeholder groups in the current study, especially those who have directly experienced suicidality, in order to develop effective ED processes. It also highlights the importance of involving stakeholders in problem identification and solutions as recommended by the National Institutes of Health (2011).
Previous studies have suggested that adolescent ED patients, with both psychiatric and non-psychiatric complaints, support the asking of brief suicide screening questions in the ED and appreciate talking with a healthcare professional who can connect them to mental health resources (Ballard, Stanley, Horowitz, Cannon, & Bridge, 2013; Horowitz et al., 2010). Results from the current study suggest ED screening would be most supported by youth and clinicians if a safe, private area is available. Furthermore, it may be conducive for sharing prevention and education information that encourages help-seeking and long-term treatment utilization.
The primary aim of suicide screening is to identify risk so youth can be appropriately treated. The view that thorough risk assessment was the least feasible by all three stakeholder groups as an indicator of successful suicide screening in the ED supports goals of programs currently under development to develop a rapid screen to facilitate triage (King, Horwitz, Czyz, & Lindsay, 2017; Turecki & Brent, 2016). Through the larger multi-site ED-STARS study, we are currently in the process of developing an optimal screen that can be disseminated nationwide to enhance ED capacity to identify and effectively triage youth at acute risk for suicide attempts (National Institute of Mental Health, 2014; NIH RePORTER Research Portfolio Online Reporting Tools). Once implemented, additional study of perceptions of thorough risk assessment feasibility would be useful for the field, including whether feasibility refers to a readily available risk assessment tool or the feasibility of administering it in the ED.
It is worth noting again that youth thought the most important result of suicide screening in the pediatric ED is the identification and diagnosis of suicidal risk. However, this was not of equal importance to clinicians and researchers even though research has indicated screening may be especially useful for identifying youth with an elevated risk of suicide (King et al., 2009), and that even a single mental health assessment in the general population ED has been associated with a reduced risk of repeat suicidal behavior (Kapur et al., 2013). Clinicians and researchers also expressed pessimism and/or disinterest about assessment of environmental risks and supports, even though these factors are especially relevant in affecting risk for adolescents (Stanley et al., 2013). While the results of the current study cannot conclusively state why there was a discrepancy in importance among the stakeholder groups, it is important to acknowledge that clinician and researcher participants were heavily involved in the development and utilization of ED suicide screening, so their intense focus on the process may have led them to assume that, by definition, screening involves identification and diagnosis of suicide risk. Conversely, youth may have responded with a more direct indicator of a successful screening strategy because they do not necessarily know whether this is occurring in the ED. Despite the current study’s important first step in comparing and contrasting stakeholder perspectives, additional research that utilizes prompts developed by professionals may be warranted to determine the continuation of these discrepancies.
The primary aim of suicide risk screening is to identify risk so youth can be appropriately treated, suggesting the importance of the availability of effective treatments for adolescents and families. (King et al., 2017; Turecki & Brent, 2016)
Limitations:
As with all research there were limitations to the current study. Even though PECARN was used to recruit researcher and clinician participants, the generalizability of findings is limited by the use of snowball sampling with youth and parents who were primarily drawn from one U.S. hospital. The inclusion of community stakeholders who have direct experience with the study topic is a strength of the CM method, but the present study findings may have been limited by stakeholder representation from a single region, including youth who may be less racially and economically diverse than those served by the study EDs. Furthermore, although parents were initially involved in responding to the focus prompts, we were not able to recruit parents to continue in the subsequent phases perhaps because of the time and response burden to participate in the structuring and rating phases (Vaughn et al., 2017). Although it was intentional to capture successful suicide screening strategies in the pediatric ED by assessing it from two vantage points, the two focus prompts used in this study were similar and may have led to some duplication of ideas. One was about successful suicide screening and the other was the most important result of suicide screening. The similarity of focus prompts could have resulted in overlapping of generated ideas as stakeholders may have interpreted the successful strategies as the important results of screening. This might have also led them to infer “successful” in terms of feasibility of implementation and not necessarily on screening at-risk youth and help with prevention.
Conclusion
ED visits provide an excellent opportunity to screen and assess suicide risk among youth who otherwise may not receive needed treatment and/or services to prevent future suicide attempts. The multi-stakeholder approach utilized in this study was a major strength in that it allowed youth, parents, researchers and healthcare professionals to pool their collective wisdom to identify successful suicide screening practices and results in the pediatric ED. The concept maps can be used to align suicide risk screening and implementation efforts with the priorities and recommendations of ED stakeholders, which are based on significant lived experience. CM is a concrete method that can be transferred to other contexts to engage multiple stakeholders toward identification of priority health issues and develop a community-driven intervention to address these issues. Using such an integrated approach can lead to purposeful participation from a committed and motivated team of individuals driven by a common cause.
Acknowledgments
Funding Source: This research was funded by the National Institute for Mental Health, Award 1U01MH104311–01.
CK receives royalties from Guilford Press for Teen Suicide Risk: A Practitioner Guide to Screening, Assessment and Care Management (2013).
DB has received funding personally from UpToDate, Healthwise, and the Klingenstein Third Generation Foundation for consulting. DB receives royalties from eRT Inc. and Guilford Press.
Footnotes
Conflicts of Interest:
LV reports no conflict of interest.
CS reports no conflict of interest.
RLG reports no conflict of interest.
SB reports no conflict of interest.
JGP reports no conflict of interest.
Ethical Approval and Consent: This study was determined to be exempt from the Institutional Review Board. All study procedures followed ethical standards and participants agreed to participate at each step of the concept mapping process including the rating survey.
The emergency department (ED) is synonymous with emergency room, emergency ward, or casualty department and describes a medical treatment facility, usually hospital-based, specializing in accident services and delivery of emergency medical care.
Contributor Information
Lisa M. Vaughn, Division of Emergency Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH USA.
Cijy Elizabeth Sunny, Educational Studies, University of Cincinnati, Cincinnati, OH USA.
Robin Lindquist-Grantz, Institute for Policy Research, University of Cincinnati, Cincinnati, OH USA.
Cheryl King, Department of Psychiatr, University of Michigan, Ann Arbor, Michigan USA.
David Brent, Psychiatry, Pediatrics, and Epidemiology, University of Pittsburgh School of Medicine, Western Psychiatric Institute and Clinic, Pittsburgh, PA USA.
Stephanie Boyd, Division of Emergency Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH USA.
Jacqueline Grupp-Phelan, Pediatric Emergency Medicine, UCSF Benioff Children’s Hospital, San Francisco, CA USA.
References
- Alderman EM, Avner J, & Racine A (2012). Adolescents’ use of the emergency department: does source of primary care make a difference? Journal of Primary Care & Community Health, 3(1), 36–41. 10.1177/2150131911413595 [DOI] [PubMed] [Google Scholar]
- Ballard ED, Bosk A, Snyder D, Bridge JA, Wharff EA, Teach SJ, & Horowitz L (2012). Patients’ opinions about suicide screening in a pediatric emergency department. Pediatric Emergency Care, 28(1), 34. doi: 10.1097/PEC.0b013e31823f2315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard ED, Stanley IH, Horowitz LM, Cannon EA, & Bridge JA (2013). Asking youth questions about suicide risk in the pediatric emergency department: results from a qualitative analysis of patient opinions. Clinical Pediatric Emergency Medicine, 14(1), 20–27. 10.1016/j.cpem.2013.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Arias SA, Miller M, Barber C, Espinola JA, Sullivan AF, . . . Boudreaux ED (2015). Change in emergency department providers’ beliefs and practices after use of new protocols for suicidal patients. Psychiatric Services, 66(6), 625–631. 10.1176/appi.ps.201400244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Wintersteen M, Boudreaux ED, Brown G, Capoccia L, Currier G, . . . Stanley B (2016). Reducing suicide risk: challenges and opportunities in the emergency department. Annals of Emergency Medicine, 68(6), 758–765. 10.1016/j.annemergmed.2016.05.030 [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Camargo CA, Arias SA, Sullivan AF, Allen MH, Goldstein AB, . . . Miller IW (2016). Improving suicide risk screening and detection in the emergency department. American Journal of Preventive Medicine, 50(4), 445–453. 10.1016/j.amepre.2015.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Kalas R, Edelbrock C, Costello AJ, Dulcan MK, & Conover N (1986). Psychopathology and its relationship to suicidal ideation in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 25(5), 666–673. 10.1016/S0002-7138(09)60292-2 [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, & Zelenak JP (1988). Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Archives of General Psychiatry, 45(6), 581–588. doi: 10.1001/archpsyc.1988.01800300079011 [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, . . . Baugher M (1993). Psychiatric risk factors for adolescent suicide: a case-control study. Journal of the American Academy of Child and Adolescent Psychiatry, 32(3), 521–529. 10.1097/00004583-199305000-00006 [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, & Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47(3‐4), 372–394. doi: 10.1111/j.1469-7610.2006.01615.x [DOI] [PubMed] [Google Scholar]
- Burke JG, O’Campo P, Peak GL, Gielen AC, McDonnell KA, & Trochim WM (2005). An introduction to concept mapping as a participatory public health research method. Qualitative Health Research, 15(10), 1392–1410. 10.1177/1049732305278876 [DOI] [PubMed] [Google Scholar]
- Capoccia L, & Labre M (2015). Caring for adult patients with suicide risk: A consensus-based guide for emergency departments. Retrieved from http://www.sprc.org/edguide [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Youth Risk Behavior Surveillance - United States, 2017. Retrieved from https://www.cdc.gov/mmwr/volumes/67/ss/ss6708a1.htm
- Crawford-Browne S, & Kaminer D (2012). The use of concept mapping in engaging women to identify the factors that influence violence. Journal of Psychology in Africa, 22(4), 527–535. 10.1080/14330237.2012.10820564 [DOI] [Google Scholar]
- Creswell JW, & Plano Clark V (2011). Designing and conducting mixed methods research, 2nd edition Los Angeles: Sage. [Google Scholar]
- de Leeuw J, & Mair P (2009). Multidimensional scaling using majorization: SMACOF in R. Journal of Statistical Software, 31(3), 1–30. doi: 10.1016/j.csda.2009.01.002 [DOI] [Google Scholar]
- Drapeau CW, & McIntosh JL (2015). USA suicide 2014: Official final data. Washington, DC: American Association of Suicidology, dated December 22, 2015. [Google Scholar]
- Everitt B (1980). Cluster analysis, 2nd ed London: Halsted. [Google Scholar]
- Fein JA, Pailler ME, Barg FK, Wintersteen MB, Hayes K, Tien AY, & Diamond GS (2010). Feasibility and effects of a Web-based adolescent psychiatric assessment administered by clinical staff in the pediatric emergency department. Archives of Pediatrics and Adolescent Medicine, 164(12), 1112–1117. doi: 10.1001/archpediatrics.2010.213 [DOI] [PubMed] [Google Scholar]
- Groholt B, Ekeberg Ø, & Haldorsen T (2006). Adolescent suicide attempters: What predicts future suicidal acts? Suicide and Life-Threatening Behavior, 36(6), 638–650. [DOI] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, & Christensen H (2010). Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry, 10(1), 113 10.1186/1471-244X-10-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz L, Ballard E, Teach SJ, Bosk A, Rosenstein DL, Joshi P, & Dalton ME (2010). Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department: a good time to talk? Pediatric Emergency Care, 26(11), 787. doi: 10.1097/PEC.0b013e3181fa8568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Ballard ED, & Pao M (2009). Suicide screening in schools, primary care and emergency departments. Current Opinion in Pediatrics, 21(5), 620. doi: 10.1097/MOP.0b013e3283307a89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, & Trochim WM (2002). Concept mapping as an alternative approach for the analysis of open-ended survey responses. Organizational Research Methods, 5(4), 307–336. 10.1177/109442802237114 [DOI] [Google Scholar]
- Kane M, & Trochim WMK (2007). Concept mapping for planning and evaluation. Thousand Oaks, CA: Sage [Google Scholar]
- Kapur N, Steeg S, Webb R, Haigh M, Bergen H, Hawton K, . . . Cooper J (2013). Does clinical management improve outcomes following self-harm? Results from the multicentre study of self-harm in England. PloS One, 8(8), e70434 10.1371/journal.pone.0070434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Horwitz A, Czyz E, & Lindsay R (2017). Suicide Risk Screening in Healthcare Settings: Identifying Males and Females at Risk. Journal of Clinical Psychology in Medical Settings, 24(1), 8–20. doi: 10.1007/s10880-017-9486-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, O’Mara RM, Hayward CN, & Cunningham RM (2009). Adolescent suicide risk screening in the emergency department. Academic Emergency Medicine, 16(11), 1234–1241. 10.1111/j.1553-2712.2009.00500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin G, & Beautrais A (2010). Emergency Departments Are Underutilized Sites for Suicide Prevention. Crisis, 31(1), 1–6. doi: 10.1027/0227-5910/A000001 [DOI] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, . . . Marusic A (2005). Suicide prevention strategies: a systematic review. Journal of the American Medical Association, 294(16), 2064–2074. doi: 10.1001/jama.294.16.2064 [DOI] [PubMed] [Google Scholar]
- Michelmore L, & Hindley P (2012). Help‐seeking for suicidal thoughts and self‐harm in young people: A systematic review. Suicide and Life‐Threatening Behavior, 42(5), 507–524. 10.1111/j.1943-278X.2012.00108.x [DOI] [PubMed] [Google Scholar]
- Miller DN, Eckert TL, & Mazza JJ (2009). Suicide prevention programs in the schools: A review and public health perspective. School Psychology Review, 38(2), 168. [Google Scholar]
- National Center for Health Statistics. (2016). Increase in suicide in the United States, 1999–2014. [Google Scholar]
- National Institute of Mental Health. (2014). Personalized screen to ID suicidal teens in 14 ERs. Retrieved from https://www.nimh.nih.gov/news/science-news/2014/personalized-screen-to-id-suicidal-teens-in-14-ers.shtml
- National Institutes of Health (2011). Principles of community engagement. Washington, DC: CTSA Community Engagement Key Function Committee Task Force on the Principles of Community Engagement. [Google Scholar]
- NIH RePORTER Research Portfolio Online Reporting Tools. Emergency department screen for teens at risk for suicide (ED-STARS). Retrieved from https://projectreporter.nih.gov/project_info_description.cfm?aid=8755416&icde=21651658
- Optimal Workshop Ltd. (2017). Optimal Sort [online card sorting software]. Retrieved from https://www.optimalworkshop.com/optimalsort
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health and Mental Health Services Research, 42(5), 533–544. doi: 10.1007/s10488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- R CoreTeam. (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Online: http://www.R-project.org.
- Rosas SR, & Kane M (2012). Quality and rigor of the concept mapping methodology: a pooled study analysis. Evaluation and Program Planning, 35(2), 236–245. 10.1016/j.evalprogplan.2011.10.003 [DOI] [PubMed] [Google Scholar]
- Stanley IH, Snyder DJ, Westen S, Ballard ED, Teach SJ, Kapetanovic S, . . . Horowitz LM (2013). Self-reported recent life stressors and risk of suicide in pediatric emergency department patients. Clinical Pediatric Emergency Medicine, 14(1), 35–40. 10.1016/j.cpem.2013.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szaflarski M, Vaughn LM, McLinden D, Wess Y, & Ruffner A (2015). Using concept mapping to mobilize a Black faith community to address HIV. International Public Health Journal, 7(1), 117. [PMC free article] [PubMed] [Google Scholar]
- The Joint Commission. (2016). Sentinel Event Alert 56: Detecting and treating suicide ideation in all settings Retrieved from https://www.jointcommission.org/sea_issue_56/ [PubMed]
- Torio CM, Encinosa W, Berdahl T, McCormick MC, & Simpson LA (2015). Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Academic Pediatrics, 15(1), 19–35. 10.1016/j.acap.2014.07.007 [DOI] [PubMed] [Google Scholar]
- Trochim WM (1989). An introduction to concept mapping for planning and evaluation. Evaluation and Program Planning, 12(1), 1–16. 10.1093/intqhc/mzi038 [DOI] [Google Scholar]
- Trochim WMK, & Kane M (2005). Concept mapping: an introduction to structured conceptualization in health care. International Journal for Quality in Health Care, 17(3), 187–191. 10.1093/intqhc/mzi038 [DOI] [PubMed] [Google Scholar]
- Turecki G, & Brent DA (2016). Suicide and suicidal behaviour. The Lancet, 387(10024), 1227–1239. 10.1016/S0140-6736(15)00234-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn L, & McLinden D (2016). Concept mapping Handbook of methodological approaches to community-based research: Qualitative, quantitative, and mixed methods, Oxford University Press, Oxford, UK, 305–314. [Google Scholar]
- Vaughn LM, Jacquez F, & McLinden D (2013). The use of concept mapping to identify community-driven intervention strategies for physical and mental health. Health Promotion Practice, 14(5), 675–685. 10.1177/1524839912462871 [DOI] [PubMed] [Google Scholar]
- Vaughn LM, Jones JR, Booth E, & Burke JG (2017). Concept mapping methodology and community-engaged research: a perfect pairing. Evaluation and Program Planning, 60, 229–237. 10.1016/j.evalprogplan.2016.08.013 [DOI] [PubMed] [Google Scholar]
- White J, Marsh I, Kral MJ, & Morris J (2016). Introduction: Rethinking Suicide In White J, Marsh I, Kral MJ, & Morris J (Eds.), Critical suicidology: Transforming suicide research and research for the 21st century. Vancouver, BC: University of British Columbia Press. [Google Scholar]
- Wilson KM, & Klein JD (2000). Adolescents who use the emergency department as their usual source of care. Archives of Pediatrics and Adolescent Medicine, 154(4), 361–365. doi: 10.1001/archpedi.154.4.361 [DOI] [PubMed] [Google Scholar]
- Windsor LC, & Murugan V (2012). From the individual to the community: Perspectives about substance abuse services. Journal of Social Work Practice in the Addictions, 12(4), 412–433. 10.1080/1533256X.2012.728115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JR, & Wood LE (2008). Card sorting: current practices and beyond. Journal of Usability Studies, 4(1), 1–6. [Google Scholar]


