Abstract
Aim:
Foreign body aspiration is one of the common home accidents that requires urgent diagnosis and treatment, especially in children aged between 1 and 3 years. The type, location, and obstruction level of the aspirated material, age of the patient, and time of diagnosis influence the severity of the clinical picture. In our study, we aimed to evaluate patients who underwent bronchoscopy in our clinic with a diagnosis of foreign body aspiration in light of literature data.
Material and Methods:
The medical records of 87 patients who underwent rigid bronchoscopy with a prediagnosis of foreign body aspiration in Çukurova University, Faculty of Medicine, between January 2016 and August 2018, and were followed up in the pediatric intensive care unit after the procedure were examined retrospectively. The subjects were evaluated in terms of age, sex, primary referal center, time of presentation, symptoms at presentation, physical examination findings, radiologic investigations, type and location of foreign body, and duration of stay in the intensive care unit.
Results:
A total of 87 patients were included in the study. Thirty-seven patients (42.5%) were female. The mean age was found as 33.73±39.44 (range, 5–202) months. The most common (74.7%) symptom at presentation was sudden onset of coughing. The foreign body aspirated was organic in 62.1% of patients. The most common foreign bodies aspirated were peanuts, with a rate of 19.5%. Four adolescent female patients underwent broncoscopy because they aspirated needles they held in their mouths while tying their headscarves. Interestingly, one patient aspirated a stone and one patient aspirated a parasite. The most frequent location of foreign body was the right main bronchus (n=27, 31%).
Conclusion:
In the diagnosis of foreign body aspiration, the most important step is maintaining a high index of suspicion. Foreign body aspiration should be considered in patients who present with cough, respiratory distress or cyanosis, unilaterally diminished breath sounds, ronchi or stridor on physical examination, and air trapping on chest X-ray. Bronchoscopy is life-saving in the presence of any suspicious history suggestive foreign body aspiration or refractory pneumonia, even if a physical examination and radiologic findings are normal, especially in high-risk children between 1–3 years old.
Keywords: Bronchoscopy, child, foreign body aspiration
Abstract
Amaç:
Yabancı cisim aspirasyonu özellikle 1–3 yaş arası çocuklarda acil tanı ve tedavi gerektiren, yaygın ev kazası nedenlerindendir. Aspire edilen materyalin türü, yerleşimi, neden olduğu hava yolu tıkanıklığının düzeyi, olgunun yaşı, tanı süresi kliniğin ciddiyetine etki eder. Çalışmamızda, hastanemizde yabancı cisim aspirasyonu tanısı ile bronkoskopi uygulanan olguları dizin bilgileri ışığında değerlendirmeyi hedefledik.
Gereç ve Yöntemler:
Ocak 2016 – Ağustos 2018 arasında, Çukurova Üniversitesi Tıp Fakültesi’nde yabancı cisim aspirasyonu ön tanısı ile rijid bronkoskopi uygulanıp, işlem sonrası Çocuk Yoğun Bakım Birimi’nde izlediğimiz 87 olgunun tıbbi kayıtları geriye dönük olarak incelendi. Olgular yaş, cinsiyet, ilk başvuru yeri, başvuru süresi, başvuru yakınmaları, fizik bakı bulguları, radyolojik incelemeler, yabancı cismin özelliği ve yerleşim yeri açısından değerlendirildi.
Bulgular:
Çalışmaya toplam 87 olgu alındı. Olguların 37’si kız (%42,5) idi. Ortalama yaş 33,73±39,44 (5–202) ay idi. En sık başvuru yakınması (%74,7) ani başlayan öksürüktü. Aspire edilen yabancı cisim, olguların %62,1’inde organikti. En sık aspire edilen materyal %19,5’lik oran ile fıstıktı. Ergen dört kız olgu eşarp bağlarken ağzında tuttuğu iğneyi aspire ettiği için bronkoskopi yapıldı. İlginç olarak bir olgumuzda taş ve bir olguda parazit aspirasyonu saptadık. En sık yabancı cisim yerleşim yeri 27 (%31) olguda sağ ana bronş idi.
Çıkarımlar:
Yabancı cisim aspirasyonu tanısında en önemli aşama şüphe duymaktır. Öksürük, solunum sıkıntısı ya da morarma ile başvuran, fizik bakısında tek taraflı azalmış akciğer sesleri, ronküs ya da stridor bulunan, akciğer grafisinde hava hapsi olan olgularda yabancı cisim aspirasyonu düşünülmelidir. Fizik bakı ve radyoloji bulguları normal olsa bile yabancı cisim aspirasyonu düşündüren herhangi bir şüpheli öykü, ya da dirençli pnömoni varlığında özellikle riskli grup olan 1–3 yaş arasında bronkoskopi yaşam kurtarıcı olacaktır.
Introduction
Foreign body aspiration (FBA) occurs with a rate of 60–80% in childhood, especially between the ages of 1 and 3 years, though it may be observed in all age groups (1, 2). In children, FBA is a condition that requires urgent assessment and approach, and is the fourth most common cause of mortality related to accidents in children aged under 3 years (3, 4). Sudden-onset coughing and cyanosis are the most common symptoms at presentation. Foreign body aspiration occurs more commonly in boys (5, 6). It may cause significant complications including atelectasis and pneumothorax, depending on th presence of partial or complete obstruction of the airway (7). Clinical prognosis varies depending on the type and localization of the aspirated material, the degree of airway obstruction, the child’s age and time of presentation to a healthcare institution after the event (8). Postero-anterior lung radiography is mostly sufficient for the diagnosis. In the event of delayed diagnosis, the morbidity risk and mortality risk increase. Rigid bronchoscopy is used in the diagnosis and treatment of FBA (9).
In this study, we aimed to evaluate the demographic properties, types, and localizations of foreign bodies and complication rates during and after rigid bronchoscopy in pediatric patients who presented to our hospital because of FBA.
Material and Methods
In this single-center retrospective study, the medical records of 102 patients who underwent rigid bronchoscopy with a prediagnosis of FBA in Çukurova University, Faculty of Medicine, between January 2016 and August 2018 and were followed up in pediatric intensive care unit (PICU) after the procedure were examined retrospectively. Fifteen patients whose records were insufficient were excluded from the study; 87 patients were included in the final analysis. The subjects were evaluated in terms of age, sex, primary referal center, time of presentation, symptoms at presentation, physical examination findings, radiologic investigations, type and location of foreign body, and duration of stay in the PICU and the hospital. The study was conducted in accordance with the Declaration of Helsinki. Approval for the study was obtained from Çukurova University Faculty of Medicine Clinical Researches Ethics Comittee (Date: 08.31.2018, Number: 80).
Statistical analysis
The SPSS software package (version 21.0) was used. Categorical data are summarized as number and percentage, and the numeric data are summarized as mean and standard deviation (median and minimum-maximum, when necessary).
Results
A total of 87 patients were included in the study. Thirty-seven (42.5%) patients were female and the female/male raio was found as 1:1.3. The mean age was found as 33.73±39.44 (range, 5–202) months. The mean time to presentation was found as 6.26±21.22 hours and 31 (35.8%) patients presented to hospital in the first 24 hours. The primary presentation site was an external center in 67 patients (77.1%) and these patients were referred to our hospital with a prediagnosis of FBA. The number of patients who were referred because of treatment-resistant pneumonia and were found to have a foreign body was 2 (2.3%). The mean duration of stay in the PICU was found as 1.8±4.8 (range, 1–40) days, and the mean hospitalization time was 3.7±6.8 (range, 1–51) days.
The most common symptom at presentation was sudden-onset coughing (74.7%). The symptoms and physical examination findings are shown in Table 1. The aspirated foreign body was organic in 62.1% of the patients and inorganic in 12.6%. Foreign body was not found on bronchoscopy in 20 patients (25.3%) (Table 2). The most common aspirated material was a peanut with a rate of 19.5%. Four female adolescents underwent bronchoscopy because they aspirated the needles they held in their mouths while tying their headscarves (Fig. 1). Interestingly, one patient aspirated a stone and one patient aspirated a parasite.
Table 1.
Presentation symptoms and physical examination findings of the patients
| Frequency | Percentage | |
|---|---|---|
| Symptom | ||
| Cough | 65 | 74.7 |
| Respiratory distress | 54 | 62 |
| Cyanosis | 40 | 45.9 |
| Refractory lung infection | 2 | 2.2 |
| Asymptomatic | 10 | 11.4 |
| Physcal examination | ||
| Unilaterally diminished breath sounds | 29 | 33.3 |
| Ronchus | 24 | 27.5 |
| Stridor | 17 | 19.5 |
| Ralles | 5 | 5.7 |
| None | 32 | 36.7 |
Table 2.
Foreign body aspirated
| Frequency | Percentage | |
|---|---|---|
| Organic | 54 | 62,1 |
| Peanut | 17 | 19.5 |
| Sunflower seed | 15 | 17.2 |
| Nut | 6 | 6.8 |
| Carrot | 2 | 2.3 |
| Walnut | 2 | 2.3 |
| Walnut shell | 1 | 1.1 |
| Apple stalk | 1 | 1.1 |
| Plum seed | 1 | 1.1 |
| Almond | 1 | 1.1 |
| Melon seed | 1 | 1.1 |
| Dry bean | 1 | 1.1 |
| Cherry stalk | 1 | 1.1 |
| Sweetcorn | 1 | 1.1 |
| Parasite | 1 | 1.1 |
| Chicken piece | 1 | 1.1 |
| Groundnut | 1 | 1.1 |
| Egg shell | 1 | 1.1 |
| Inorganic | 11 | 12,6 |
| Needle | 4 | 4.5 |
| Marble | 1 | 1.1 |
| Pen point | 1 | 1.1 |
| Carton piece | 1 | 1.1 |
| Parfume cap | 1 | 1.1 |
| Stone | 1 | 1.1 |
| Bead | 1 | 1.1 |
| Toy piece | 1 | 1.1 |
| No foreign body | 22 | 25.3 |
Figure 1.
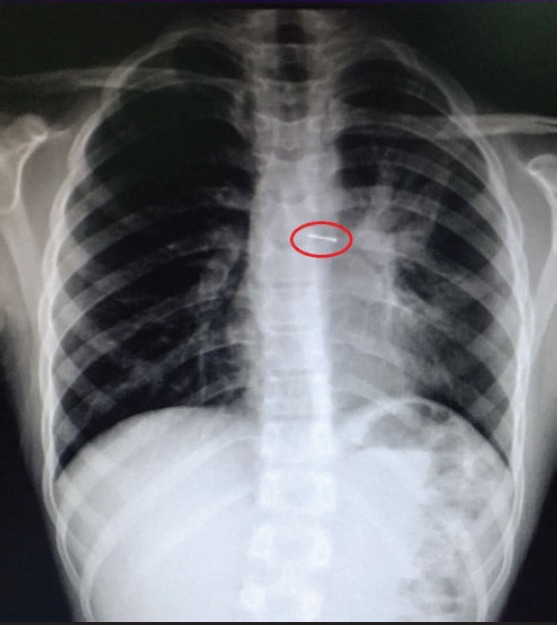
Scarf-pin view on chest graphy
Posteroanterior lung radiography was found to be normal in 41 (47.1%) of the patients. Imaging with computed tomography of the thorax was performed in addition to PA lung radiography in two (2.3%) patients. One of these patients aspirated a piece of carton, the other one was intubated because of treatment-resistant pneumonia in an external center and had bilateral pneumothorax. Rigid bronchoscopy was performed under general anesthesia in all patients. The most common localization of foreign body was the right main bronchus (n=27, 31%). Radiologic imaging findings and foreign body localizations are shown in Table 3.
Table 3.
Radiologic imaging findings and foreign body localizations
| Frequency | Percentage | |
|---|---|---|
| PA-L | ||
| Air trapping | 44 | 50,6 |
| Normal | 41 | 47.1 |
| Atelectasis | 15 | 17.2 |
| Mediastinal shift | 9 | 10.4 |
| Opacity | 4 | 4.6 |
| Pneumothorax | 2 | 2.3 |
| Computed tomography | 2 | 2,3 |
| Bronchoscopy | ||
| Right main bronchus | 27 | 31 |
| None | 22 | 25.3 |
| Left main broncus | 14 | 16.1 |
| Trachea | 9 | 10.3 |
| Esophagus | 6 | 6.9 |
| Both main bronchi | 4 | 4.6 |
| Right main bronchus and trachea | 3 | 3.4 |
| Insufficient information | 2 | 2.3 |
PA-L: Postero-anterior lung radiography
No complications developed and there was no mortality after bronchoscopy in any patients.
Discussion
FBA is among the causes of common home accidents for children. Patients typically present with a history of sudden-onset coughing and respiratory distress while feeding or playing with toys. It occurs more commonly in children, especially those aged below three years and in boys because of insufficiency in swallowing and gag reflexes and being restless while eating (10, 11). In our study, the mean age and the female/male ratio were found to be compatible with the literature data.
It is thought that aspirated foreign bodies vary by the countries’ nutritional habits and sociocultural and religious characteristics (12). Sunflower, pumpkin, and watermelon seeds are the most commonly aspirated foreign bodies in Egypt, Turkey, and Greece, whereas bone is reported to be aspirated most commonly in South Asia and China (13). In recent years, adolescent female patients aspirating needles being held in their mouths while speaking at the same time have been reported with an increasing frequency in muslum communities. This condition has recently been named as ‘scarf pin-related Hijab syndrome’ in the literature (14). In our study, 57.4% of the aspirated foreign bodies were organic and the most commonly aspirated material was peanut (19.5%), followed by sunflower seeds (17.2%). Scarf pin-related Hijab syndrome was found in 4 adolescent patients, the oldest was aged 16 years.
One of our patients was a three-year-old male patient who started to cough suddenly while running in the park and vomited after telling her mother that he swallowed something. Bronchoscopy was performed because his cough had a resistant course. Parasitic larvae were observed in both bronchi and lavage was performed. The patient needed bronchoscopic lavage three times and administration of intravenous antibiotherapy. Again, interestingly, stone aspiration was observed in one of our patients.
The diagnosis can be made by having a suspicion with a detailed history and physical examination and supportive radiologic findings in patients who are in the risk group and with removal of a foreign body on rigid broncgoscopy. However, it should be kept in mind that patients may be asymptomatic or physical examination and radiologic findings may be negative. In our study, 11.4% of patients were asymptomatic, physical examination findings and breath sounds were found to be natural in 36.7% of patients, and PA-lung radiography was found to be normal in 47.1% of patients.
In our study, the most common (74.7%) symptom at presentation was sudden-onset coughing, which is compatible with the literature (6). In our literature screening, there were studies that reported the most common physical examination finding to be unilateral diminished breath sounds or ronchi; however, there were also studies that reported the most common physical examination finding to be normal breath sounds (15, 16). The most commonly reported radiologic findings included air trapping, atelectasis, and mediastinal shift (17). In our patients, the most common lung auscultation finding was unilaterally diminished breath sounds (33.3%), and the most common radiologic finding was unitalteral air trapping on PA-lung radiography (50.6%).
In pediatric patients who present with chronic cough and lung infection that is unresponsive to appropriate treatment or frequently recurring lung infection, FBA should always be kept in mind in the differential diagnosis (18). Two patients in our study were referred because of treatment-refractory pneumonia. One of these patients was a 10-month-old patient who was referred on the eigth day of treatment for refractory pneumonia. He had bilateral pneumothorax, and was intubated and ventilated with high peak pressures on a mechanical ventilator. FBA was not predominantly considered because of the age group, but a detailed history revealed that he had an older borther aged four years who had given a sunflower seed to the patient. Subsequently, bronchoscopy was performed and a sunflower seed was removed from the right main bronchus. In the follow-up, pneumothorax regressed, extubation was attempted, but subglottic stenosis related to prolonged intubation developed and tracheostomy was performed in the patient who could not tolerate extubation. The patient was decannulated after nine months. Similarly, the second patient was a 14-month-old patient who was admitted to the PICUt because of treatment-refractory pneumonia. In the follow-up, he was intubated because of hypoxia and hypercarbia. In the detailed history taken from the family, it was learned that the patient had cyanosis while eating a cherry. He was extubated with high-flow nasal cannula oxygen support after a piece cherry was removed with rigid bronchoscopy.
Radio-opaque foreign bodies can be detected with direct radiography. Findings including atelectasis and difference in aeration may be found on direct radiography due to radioluscent foreign bodies. In asymptomatic patients with a suspicion of aspiration who have normal lung radiography and no auscultation findings, CT of the thorax may be used for the diagnosis (6). In our study, CT was needed as additional imaging in only two patients. However, when we consider that we were able to make a diagnosis with history, physical examination, and PA-lung radiography in 98% of patients in our study and the radiation exposure caused by CT, we think that routine use of CT is not necessary, despite its high sensitivity and specificity.
The left main bronchus is connected with the trachea with a sharper angle compared with the right main bronchus. This anatomic characteristic predisposes FBA in the right main bronchus (19). In our patients, foreign bodies were removed most commonly from the right main bronchus (31%), in accordance with the literature data.
The low number of patients and the presence of patients whose data could not be accessed because of insufficiencies in file records are among the limiting factors of our study. We think that prospective studies with larger patient groups will be more helpful.
In conclusion, FBA should primarily be prevented. However, the most important step in the diagnosis of FBA is having a suspicion. In the presence of sudden-onset coughing, which was also the most common symptom at presentation in our study, FBA is a diagnosis that should always be kept in mind in children. Poor clinical prognosis, which progressed as subglottic stenosis developing as a complication of prolonged intubation, resulting in tracheostomy in one of our patients who was admitted to the PICU because of treatment-refractory pneumonia and underwent bronchoscopy with a suspicion of FBA, shows the importance of detailed history and suspicion. Considering that lung radiography was found to be normal in 47% of patients with FBA in our study, bronchoscopy is lifesaving in terms of diagnosis and treatment, especially in children aged between 1 and 3 years in presence of any suspicious history suggestive of FBA or pneumonia that does not respond to appropriate antibiotherapy.
Footnotes
Ethics Committee Approval: Ethical approval for this study was received from the Çukurova University Faculty of Medicine Clinical Research Ethics Committee.
Informed Consent: No informed consent received.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - N.A., A.Y.; Design - N.A., A.Y., D.Y., Ö.Ö.; Supervision - D.,Y. Ö.Ö., S.K.; Data Collection and/or Processing - N.A., A.Y.; Analysis and/or Interpretation - N.A. A.Y., D.Y.; Literature Review - N.A., D.Y.; Writing - N.A., D.Y.; Critical Review - D.Y., Ö.Ö.H.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Etik Komite Onayı: Bu çalışma için etik komite onayı Çukurova Üniversitesi Tıp Fakültesi Klinik Araştırmalar Etik Kurulu’ndan alınmıştır.
Hasta Onamı: Hasta onamı alınmadı.
Hakem Değerlendirmesi: Dış bağımsız.
Yazar Katkıları: Fikir - N.A., A.Y.; Tasarım - N.A., A.Y., D.Y., Ö.Ö.; Denetleme - D.,Y. Ö.Ö., S.K.; Veri Toplanması ve/veya İşlemesi - N.A., A.Y.; Analiz ve/veya Yorum - N.A. A.Y., D.Y.; Literatür Taraması - N.A., D.Y.; Yazıyı Yazan - N.A., D.Y.; Eleştirel İnceleme - D.Y., Ö.Ö.H.
Çıkar Çatışması: Yok.
Mali Destek: Yok.
References
- 1.Darrow DH, Hollinger LD. Foreign bodies in the larynx, trachea, and bronchi. In: Bluestone CD, Stool S, Kenna MA, editors. Pediatric Otolaryngology. Philadelphia: W.B. Saunders; 1996. pp. 1390–401. [Google Scholar]
- 2.Haliloglu M, Ciftci AO, Oto A, et al. CT virtual bronchoscopy in the evaluation of children with suspected foreign body aspiration. Eur J Radiol. 2003;48:188–92. doi: 10.1016/S0720-048X(02)00295-4. [DOI] [PubMed] [Google Scholar]
- 3.Özdemir Ç, Demirel B, Akar T, et al. Ankara'da yabancıcisim aspirasyonu sonucu ölen olguların değerlendirilmesi. Adli Tıp Dergisi. 2006;20:24–8. [Google Scholar]
- 4.Rodríguez H, Passali GC, Gregori D, et al. Management of foreign bodies in the airway and oesophagus. Int J Pediatr Otorhinolaryngol. 2012;76(Suppl 1):S84–91. doi: 10.1016/j.ijporl.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Sahin A, Meteroglu F, Eren S, et al. Inhalation of foreign bodies in children:experience of 22 years. J Trauma Acute Care Surg. 2013;74:658–63. doi: 10.1097/TA.0b013e3182789520. [DOI] [PubMed] [Google Scholar]
- 6.Mapelli E, Sabhaney V. Stridor and drooling in infants and children. In: Tintinalli JE, Stapczynski J, Ma O, editors. Tintinalli's emergency medicine:A comprehensive study guide. 8th ed. New York: McGraw-Hill Education; 2015. [Google Scholar]
- 7.Tokar B, Ozkan R, Ilhan H. Tracheobronchial foreign bodies in children:importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol. 2004;59:609–15. doi: 10.1016/j.crad.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Eren S, Balci AE, Dikici B, et al. Foreign body aspiration in children:experience of 1160 cases. Ann Trop Paediatr. 2003;23:31–7. doi: 10.1179/000349803125002959. [DOI] [PubMed] [Google Scholar]
- 9.Thatte NM, Guglani L, Turner DR, et al. Retrieval of endobronchial foreign bodies in children:involving the cardiaccatheterization lab. Pediatrics. 2014;134:e865–9. doi: 10.1542/peds.2013-3069. [DOI] [PubMed] [Google Scholar]
- 10.Committee on Injury, Violence, and Poison Prevention. Prevention of choking among children. Pediatrics. 2010;125:601–7. doi: 10.1542/peds.2009-2862. [DOI] [PubMed] [Google Scholar]
- 11.Rizk H, Rassi S. Foreign body inhalation in the pediatric population:lessons learned from 106 cases. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:169–74. doi: 10.1016/j.anorl.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Wiseman NE. The diagnosis of foreign body aspiration in childhood. J Pediatr Surg. 1984;19:531–5. doi: 10.1016/s0022-3468(84)80097-4. [DOI] [PubMed] [Google Scholar]
- 13.Salih AM, Alfaki M, Alam-Elhuda DM. Airway foreign bodies:A critical review for a common pediatric emergency. World J Emerg Med. 2016;7:5–12. doi: 10.5847/wjem.j.1920-8642.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baram A, Kakamad FH, Bakir DA. Scarf pin-related hijab syndrome:A new name for an unusual type of foreign bodyaspiration. J Int Med Res. 2017;45:2078–84. doi: 10.1177/0300060517711086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraga Ade M, Reis MC, Zambon MP, et al. Foreign body aspiration in children:clinical aspects, radiological aspects and bronchoscopic treatment. [Article in English, Portuguese] J Bras Pneumol. 2008;34:74–82. doi: 10.1590/s1806-37132008000200003. [DOI] [PubMed] [Google Scholar]
- 16.Baram A, Sherzad H, Saeed S, et al. Tracheobronchial Foreign Bodies in Children:The Role of Emergency Rigid Bronchoscopy. Glob Pediatr Health. 2017;4:2333794X17743663. doi: 10.1177/2333794X17743663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liang J, Hu J, Chang H, et al. Tracheobronchial foreign bodies in children - a retrospective study of 2,000 cases in Northwestern China. Ther Clin Risk Manag. 2015;11:1291–5. doi: 10.2147/TCRM.S86595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Öncü S, Güzel A, Paksu Ş, et al. Tekrarlayan Akciğer Enfeksiyonunda OlasıBir Tanı:YabancıCisim Aspirasyonu. J Pediatr Emerg Intensive Care Med. 2014;1:53–6. [Google Scholar]
- 19.Ahmed AO, Shuiabu IY. Inhaled foreign bodies in a paediatric population at AKTH Kano-Nigeria. Niger Med J. 2014;55:77–82. doi: 10.4103/0300-1652.128178. [DOI] [PMC free article] [PubMed] [Google Scholar]


