Abstract
Being of the male sex has been identified as a risk factor for multiple morbidities associated with preterm birth, including bronchopulmonary dysplasia (BPD). Exposure to inflammatory stress is a well-recognized risk factor for developing BPD. Whether there is a sex difference in pulmonary innate immune TLR4 signaling, lung injury and subsequent abnormal lung development is unknown. Neonatal (P0) male and female mice (ICR) were exposed to systemic LPS (5 mg/kg, IP) and innate immune signaling, and the transcriptional response were assessed (1 and 5 hours), along with lung development (P7). Male and female mice demonstrated a similar degree of impaired lung development with decreased radial alveolar counts, increased surface area, increased airspace area and increased mean linear intercept. We found no differences between male and female mice in the baseline pulmonary expression of key components of TLR4-NFκB signaling, or in the LPS-induced pulmonary expression of key mediators of neonatal lung injury. Finally, we found no difference in the kinetics of LPS-induced pulmonary NFκB activation between male and female mice. Together, these data support the conclusion that the innate immune response to early postnatal LPS exposure and resulting pulmonary sequelae is similar in male and female mice.
Subject terms: Toll-like receptors, Respiratory distress syndrome
Introduction
A growing body of literature supports the hypothesis that many morbidities associated with prematurity are sex-specific1. An increased risk of respiratory morbidity, including bronchopulmonary dysplasia (BPD), has been noted in preterm males2–4. Although genetic, developmental and hormonal differences between male and females have been identified, the mechanisms underlying the increased respiratory morbidity observed in preterm male infants are unclear.
The pathogenesis of BPD is multifactorial. Both clinical and pre-clinical data support a role played by oxidant and inflammatory stress in mediating neonatal lung injury and subsequent abnormal development5–10. Of note, pre-clinical data have begun to unravel the mechanisms underlying sex-type specific responses to neonatal hyperoxia exposure. Compared to female mice, neonatal male mice were more susceptible to early postnatal hyperoxia-induced lung injury and abnormal lung development11. This injury was associated with markers of differential NFκB activity between male and female mice. Work from this same group demonstrated evidence of increased hyperoxia-induced NFκB activity in human umbilical vein endothelial cells derived from female donors12. These data are consistent with previous reports demonstrating that in response to hyperoxia, NFκB activity is protective in the neonatal lung13–16.
Exposure to inflammatory stress injures the developing lung which results in abnormal development. Stimulating the fetal innate immune response with an intraamniotic (IA) injection of LPS during the saccular stage of lung development induces pulmonary inflammation and impairs alveolarization in fetal sheep and rats17–25. In mice, IA LPS during the pseudoglandular (e15) stage of lung development induces inflammation and inhibits distal branching when assessed 48 hours later, and this finding is attenuated by inhibiting the innate immune response26–29, while postnatal LPS exposure during the alveolar stage (PN5) of lung development inhibits alveolarization30,31. However, whether this inflammatory-stress induced injury is sex-specific is unknown.
Previous studies have demonstrated that NFκB signaling protects the neonatal lung against both oxidant and inflammatory stress-induced injury16,31. As stated, pulmonary NFκB activity has been implicated in the attenuated hyperoxia-induced lung injury observed in neonatal female mice and oxygen toxicity observed in HUVEC derived from females11,12. However, these findings may not be applicable to inflammatory stress-induced models of lung injury. The signaling mechanisms leading to NFκB activation following exposure to inflammatory stimuli are distinct from those observed following exposure to oxidant stress. In quiescent cells, NFκB remains sequestered in the cytoplasm bound to members of the IκB family of inhibitory proteins32. Following inflammatory stress, IκB phosphorylation and degradation allow NFκB nuclear translocation and DNA binding33. In contrast, the well-defined NFκB activation cascade that occurs after exposure to inflammatory stress, a definitive pathway has not been established following exposure to oxidant stress34–37. Thus, any sex-type specific differences in response to hyperoxia may not be applicable to injuries following exposure to inflammatory stress.
In this study, we sought to determine whether LPS-induced neonatal lung injury was sex-type specific, and to evaluate the hepatic and pulmonary innate immune response to LPS challenge in the immediate postnatal period. We report that there are no differences in pulmonary injury and abnormal lung development between male and female mice exposed to early postnatal systemic LPS challenge. Furthermore, we demonstrate that pulmonary expression of factors previously implicated in sex differences and lung injury, as well as the key components of TLR4-NFκB signaling are similar in neonatal male and female mice. Together, these data support the conclusion that the innate immune response to early neonatal LPS exposure and the resulting pulmonary sequelae are similar in male and female mice.
Methods
Murine model of endotoxemia
Neonatal (P0, male and female) ICR mice were exposed to LPS (Sigma L2630, 5 mg/kg, IP). The litter was split in half into control and exposed groups. At this point, the best visual determination of sex made in an attempt to equally distribute males and females to control and exposed groups. Sex was confirmed by testing for SRY by qPCR on mRNA isolated from hepatic tissue (see below). All procedures were approved by the IACUC at the University of Colorado (Aurora, CO) and care and handling of the animals was in accord with the National Institutes of Health guidelines for ethical animal treatment.
Lung inflation and collection of pulmonary tissue
For pulmonary mRNA and protein analysis, P0 mice were sacrificed at 1 or 5 hours of LPS exposure with a fatal dose of pentobarbital sodium. Lungs were perfused with normal saline, removed, snap-frozen, and stored at −80 C. For morphometric assessments, mice were exposed to LPS on P0 and sacrificed on P7 and p28 with a fatal dose of pentobarbital sodium. Following perfusion of the lungs with normal saline, the trachea was cannulated with a 24 G angiocath and the lungs were inflation-fixed at 25 cm H2O pressure for 10 minutes with 4% paraformaldehyde. Lungs were paraffin-embedded, and sections were cut (5 µm) and stained with hematoxylin and eosin at the University of Colorado Denver Morphology and Phenotyping Core.
Morphometric analysis
Radial alveolar counts (RAC), and objective measure of alveolar number, were assessed as previously described38,39. Counts were performed on four separate male and female ICR mice for each condition (room air and endotoxemia exposure). The average RAC was obtained from a minimum of 30 perpendicular lines obtained from photomicrographs of 5–10 high-powered fields of two separate sections of lung per animal. Measurements of mean linear intercept (MLI), a measurement of the mean distance in the air spaces, and airspace area (ASA) were performed using the computer-assisted image-analysis program Metamorph Basic (Molecular Devices, Sunnyvale, CA) with custom-designed macros on images captured on an Olympus IX83 microscope (10x, 20x, and 40x objective) and quantified with Metamorph Basic (MolecularDevices Sunnyvale, CA). Ten randomly selected non-overlapping sections per mouse at 40X magnification were assessed.
Isolation of mRNA, cDNA synthesis and analysis of relative mRNA levels by RT-qPCR
Frozen tissue was placed in RLT buffer (Qiagen) and tissue was homogenized using the Bullet Blender (NextAdvance). Pulmonary and hepatic mRNA was collected from homogenized tissue using the RNeasy Mini Kit (Qiagen) according to the manufacturer’s instructions. Initially, tissue RNA was assessed for purity and concentration using the NanoDrop (ThermoFisher Scientific), and cDNA synthesized using the Verso cDNA synthesis Kit (ThermoFisher Scientific). Relative mRNA levels were evaluated by quantitative real-time PCR using exon spanning primers (Table 1), TaqMan gene expression and StepOnePlus Real-Time PCR System (Applied Biosystems). Relative quantitation was performed via normalization to the endogenous control 18S using the cycle threshold (ΔΔCt) method.
Table 1.
List of genes for qPCR analysis.
| Target | Assay ID |
|---|---|
| Bcl2a1 | Mm03646861_mH |
| Bcl2l1 | Mm00437783_m1 |
| Birc3 | Mm01168413_m1 |
| Ccl2 | Mm00441242_m1 |
| Cxcl1 | Mm04207460_m1 |
| Cxcl2 | Mm00436450_m1 |
| Cxcl10 | Mm00445235_m1 |
| Ikbkb | Mm01222247_m1 |
| Il1a | Mm00439620_m1 |
| Il1b | Mm01336189_m1 |
| Il6 | Mm00446190_m1 |
| Il10 | Mm00439614_m1 |
| Il12b | Mm00434174_m1 |
| Myd88 | Mm00440338_m1 |
| Nfkb1 | Mm00476361_m1 |
| Nfkbia | Mm00477798_m1 |
| Nfkbib | Mm00456849_m1 |
| Rel | Mm00485657_m1 |
| Rela | Mm00501346_m1 |
| Serpinb2 | Mm00440905_m1 |
| Sry | Mm00441712_s1 |
| Ticam1 | Mm00844508_s1 |
| Ticam2 | Mm01260003_m1 |
| Tlr4 | Mm00445273_m1 |
| Tnf | Mm00443258_m1 |
| Xiap | Mm01311594_mH |
Isolation of protein and western blot analysis
Frozen pulmonary tissue was homogenized using the Bullet Blender (NextAdvance). Pulmonary whole cell lysates were collected in T-PER (ThermoFisher Scientific) and cytosolic and nuclear extracts were collected in NE-PER (ThermoFisher Scientific). Lysates, cytosolic, and nuclear extracts were electrophoresed on a 4–12% polyacrylamide gel (Invitrogen) and proteins were transferred to an Immobilon membrane (Millipore) and blotted with antibodies (Table 2). Blots were imaged using the LiCor Odyssey imaging system and densitometric analysis was performed using ImageStudio (LiCor). In the figures, cropped images grouped together are from the same gel. No images have been spliced together and no images from separate blots have been grouped together. Full images of all blots are available in the Supplementary Information File.
Table 2.
List of antibodies for Western Blot analysis.
| Antibody | Vendor | Catalog Number |
|---|---|---|
| Anti-IKKA | Cell Signaling Technology | 2682 |
| Anti-IKKB | Cell Signaling Technology | 2370 |
| Anti-NFKB P105/P50 | Abcam | ab32360 |
| Anti-C-REL | Cell Signaling Technology | 12707 |
| Anti-TLR4 | Santa Cruz Biotechnology | sc-293072 |
| Anti-MYD88 | Abcam | ab2064 |
| Anti-P65 | Cell Signaling Technology | 8242 |
| Anti-GAPDH | Cell Signaling Technology | 5174 |
| Anti-IKBA | Cell Signaling Technology | 4814 |
| Anti-IKBB | R&D Systems | AF5225 |
| Anti-P105 | Cell Signaling Technology | 4717 |
| Anti-Calnexin | Enzo Life Sciences | ADI-SPA-860-D |
| Anti-HDAC1 | Cell Signaling Technology | 5356 |
Statistical analysis
For comparison between treatment groups, the null hypothesis that no difference existed between treatment means were tested by Student’s t-test for two groups and two-way ANOVA for multiple groups with potentially interacting variables (sex, duration of exposure), with statistical significance between and within groups determined by means of Bonferroni method of multiple comparisons (Prism, GraphPad Software, Inc). Statistical significance was defined as p < 0.05.
Results
LPS-induced disruption of lung development is similar in male and female mice
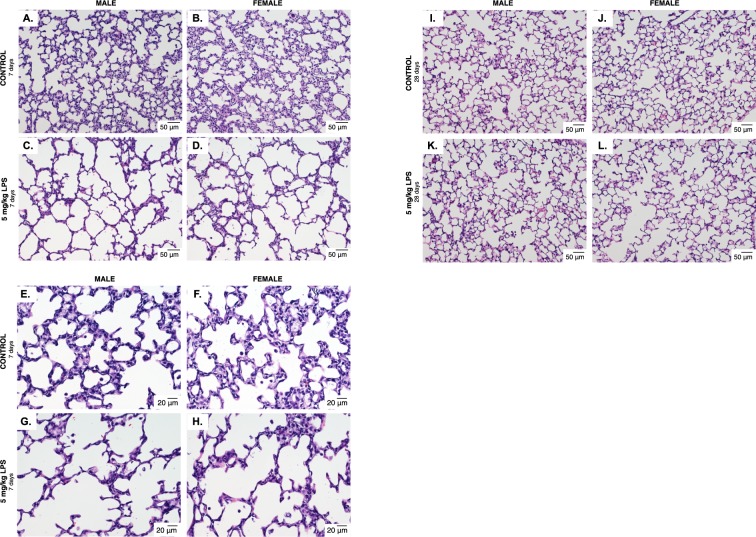
Perinatal systemic LPS exposure results in lung injury and abnormal development17–31. To assess whether the effect of LPS on the developing lung was sex specific, we exposed neonatal (P0) male and female mice to systemic LPS (5 mg/kg, IP). Pups were allowed to recover, and we then assessed lung development on P7 and P28. Both male (Fig. 1A,E) and female (Fig. 1B,F) control mice demonstrated normal and similar lung development at P7 and P28. We found that LPS disrupted lung development of both male (Fig. 1C,G) and female (Fig. 1D,H) neonatal mice, visibly marked by simplified alveolar structure and enlarged airspaces. By P28, LPS-induced abnormalities in lung structure noted at P7 appeared to have attenuated in male and female mice (Fig. 1I–L).
Figure 1.
Early postnatal systemic LPS exposure impairs lung development in male and female mice. Representative hematoxylin and eosin stained photomicrographs of lung tissue from 7 day old (A) male and (B) female control mice, and 7 day old (C) male and (D) female mice exposed to systemic LPS (5 mg/kg, IP, P0). All images were obtained using the 20x objective lens, internal scale bar 50uM. (E) male and (F) female control mice, and 7 day old (G) male and (H) female mice exposed to systemic LPS (5 mg/kg, IP, P0). All images were obtained using the 40x objective lens, internal scale bar 20uM. Representative hematoxylin and eosin stained photomicrographs of lung tissue from 28 day old (I) male and (J) female control mice, and 28 day old (K) male and (L) female mice exposed to systemic LPS (5 mg/kg, IP, P0). All images were obtained using the 20x objective lens, internal scale bar 50uM.
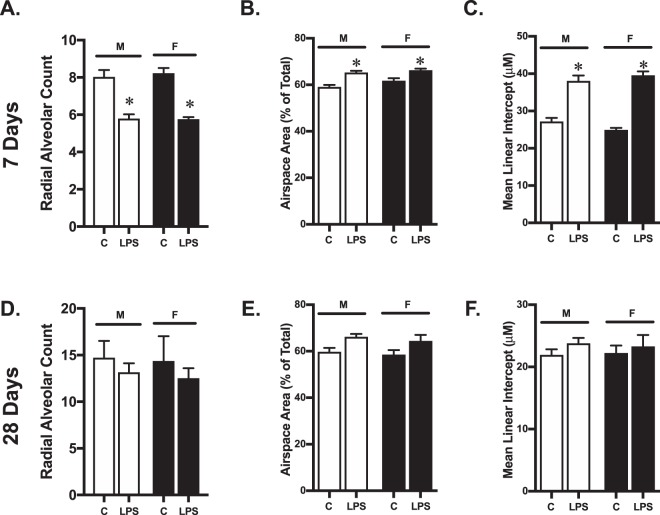
Objective measures of lung development, including RAC (Fig. 2A), airspace area (Fig. 2B), and MLI (Fig. 2C) were not different between control male and female mice at P7. Systemic LPS exposure resulted in decreased RAC (Fig. 2A), increased airspace area (Fig. 2B) and increased MLI (Fig. 2D) in both male and female mice. The degree of injury was similar between male and female mice. Objective measures of lung development, including RAC (Fig. 2D), airspace area (Fig. 2E), and MLI (Fig. 2F) were not different between control male and female mice at P28. The noted differences in lung structure observed at P7 in LPS-exposed male and female mice had attenuated by P28. While LPS-exposed male and female mice showed the similar patterns of changes in RAC (Fig. 2D), airspace area (Fig. 2E) and MLI (Fig. 2F) at P28, these differences were no longer statistically different from controls. Furthermore, no differences were noted between LPS-exposed male and female mice at this time point. These data demonstrate that in ICR mice, abnormal lung development induced by post-natal systemic LPS exposure is not sex-specific, and the resolution of this injury is similar between male and female mice.
Figure 2.
Impaired lung development induced by early postnatal systemic LPS exposure does not differ between male and female mice. (A) Radial alveolar counts, (B) airspace area (C) and mean linear intercept at 7 days of life in male and female control mice (C) or following exposure to systemic LPS (5 mg/kg, IP, P0). (D) Radial alveolar counts, (E) airspace area (F) and mean linear intercept at 28 days of life in male and female control mice (C) or following exposure to systemic LPS (5 mg/kg, IP, P0). Values are means ± SE from 6 individual animals per sex per condition. *p < 0.05 vs. sex-matched unexposed control.
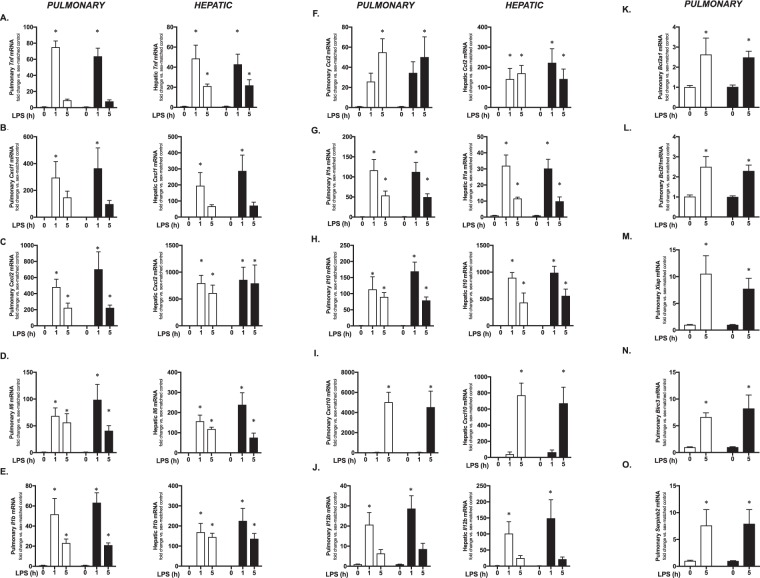
LPS-induced pulmonary and hepatic expression of pro-inflammatory cytokines is similar in male and female mice
A number of different factors have been evaluated for sex-specific differences following neonatal hyperoxia exposure, implicated in TLR4-mediated lung injury26,31,40–46, or have been demonstrated to have sex-specific differences in LPS-induced expression in adult models47–49 (Table 3). Furthermore, although LPS injures the developing lung, the liver is central to the innate immune response to endotoxemia50–64. Thus, we compared the systemic LPS-induced hepatic and pulmonary expression of multiple innate immune regulators between male and female mice at 1 and 5 hours of LPS exposure (Fig. 3A–J). While LPS exposure significantly increased the expression of all genes tested, none were different between male and female mice.
Table 3.
References used to identify innate immune target genes implicated in TLR4 mediated lung injury and sex differences.
| Gene Name | Model Evaluated - Reference | ||
|---|---|---|---|
| Hyperoxia-induced neonatal lung injury | TLR4-mediated developing lung injury | Sex difference in adult models following LPS exposure | |
| Tnf | 11 | 27, 31 | 47, 48 |
| Cxcl1 | 11 | 40 | |
| Cxcl2 | 11 | 31 | |
| Il1b | 11 | 27, 41, 42, 43, 44 | 48 |
| Il6 | 11 | 47, 48 | |
| Ccl2 | 11 | 26,31 | |
| Il1a | 45 | 48 | |
| Il10 | 47 | ||
| Cxcl10 | 31, 46 | ||
| Il12b | 49 | ||
Figure 3.
Systemic LPS-induced pulmonary and hepatic gene expression is not different between neonatal male and female mice. Fold induction of pulmonary and hepatic expression of (A) Tnf, (B) Cxcl1, (C) Cxcl2, (D) Il6, (E) Il1b and (F) Ccl2, (G) Il1a, (H) Il10, (I) Cxcl10, (J) Il12b, (K) Bcl2a1, (L) Bcl2l1, (M) Xiap, (N) Birc3, (O) Serpinb2, in neonatal (P0) male (white bars) and female (black bars) following exposure to systemic LPS (5 mg/kg IP, 1–5 hours). Genes were selected based on previous reports linking them to LPS-induced lung injury or sex-specific differences in expression (see Table 1). All values are normalized to sex-specific control mice. Values are means ± SE from 6 individual animals per sex per condition. *p < 0.05 vs. sex-matched unexposed control.
Additionally, the expression of anti-apoptotic factors has previously been identified as a key mediator or neonatal lung injury13,16,43. Therefore, we tested whether there was sex-specific pulmonary expression of antiapoptotic factors previously demonstrated respond to systemic LPS exposure in the neonatal period43. We did not test these genes at the early time point (1 hour) as we reasoned that detecting any differences in the induction of the anti-apoptotic program if present would occur at later hours of exposure. We found no difference in the induction of pulmonary expression of Bcl2a1 (Fig. 3K), Bcl2l1 (Bcl-XL, Fig. 3L), Xiap (Fig. 3M), Birc3 (Fig. 3N) or Serpinb2 (PAI-2, Fig. 3O) at 5 hours of LPS-exposure in male and female mice. Thus, we found that exposure to systemic LPS induced expression of all genes tested, but this expression did not differ between male and female mice. These data are consistent with a similar degree of LPS-induced lung injury observed between male and female neonatal mice.
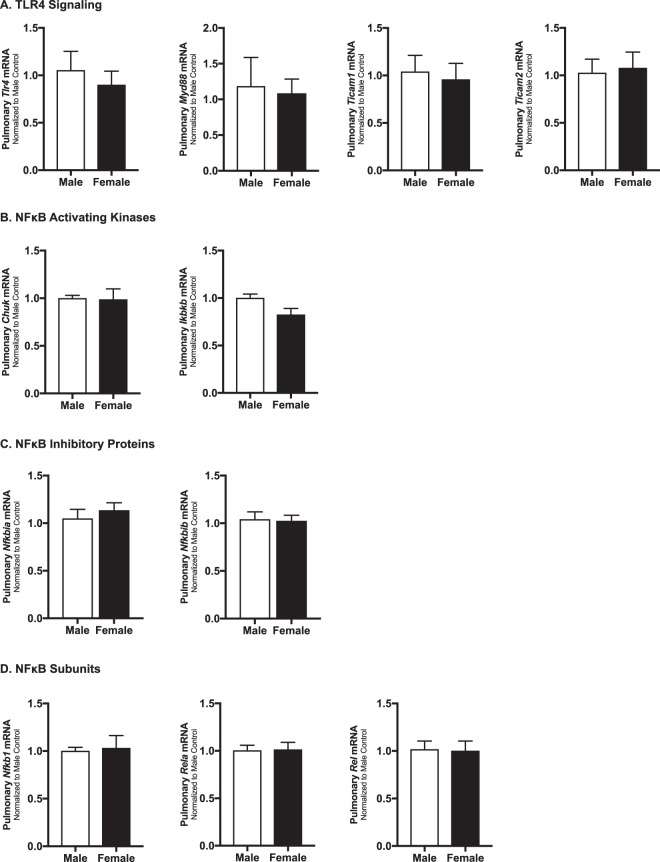
Baseline pulmonary expression of key TLR4 signaling proteins does not differ between male and female neonatal mice
Previous reports have demonstrated that there are no sex differences in TLR4 expression in the adult rat lung65, or in murine macrophage66. However, TLR4 expression in the lung is developmentally regulated67, and neonatal TLR4 expression is sex specific in other organs68. Furthermore, whether pulmonary expression of key mediators of TLR4 signaling is sex-specific is unknown. Thus, we evaluated neonatal pulmonary expression of key mediators of TLR4 signaling (Fig. 4A: TLR4, Myd88, Ticam1, Ticam2), NFκB activating kinases (Fig. 4B: Chuk, Ikbkb), NFkB inhibitory proteins (Fig. 4C: Nfkbia, Nfkbib), and NFκB subunits (Fig. 4D: Nfkb1, Rela, Rel) in the absence of LPS exposure. We found no differences in the pulmonary expression of these key components of TLR4 signaling between male and female mice.
Figure 4.
Baseline pulmonary mRNA expression of key components of TLR4 signaling is not different between neonatal male and female mice. Neonatal (P0) male (white bars) and female (black bars) baseline pulmonary expression of (A) TLR4 signaling: TLR4, Myd88, Ticam1, and Ticam2 (B) NFκB activating kinases: Chuk, Ikbkb (C) NFκB inhibitory proteins: Nfkbia, Nfkbib (D) NF-κB subunits: Nfkb1, Rela, and Rel. All values are normalized to male mice. Values are means ± SEM from 6 individual animals per sex.
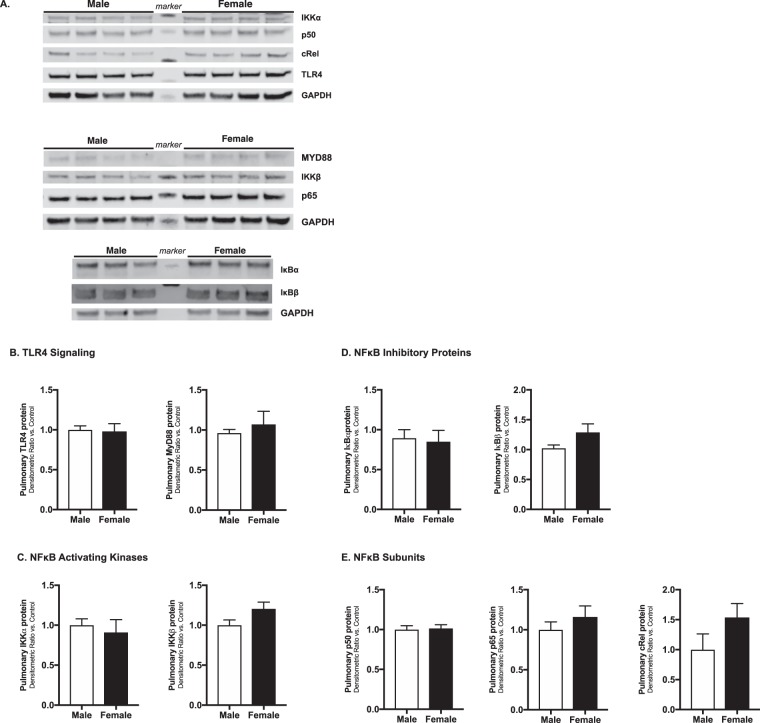
Furthermore, we assessed pulmonary protein expression of key components of TLR4 signaling (Fig. 5A,B: TLR4 and Myd88), NFκB activating kinases (Fig. 5A,C: IKKα and IKKβ), NFκB inhibitory proteins (Fig. 5A,D: IκBα, IκBβ), and NFκB subunits (Fig. 5A,E: p50, p65 and cRel) in the absence of LPS exposure. We found no differences in the pulmonary expression of these key components of TLR4 signaling between male and female mice. These data demonstrate that at baseline, prior to any LPS exposure, pulmonary expression of these key mediators of LPS-induced TLR4 signaling is not different between male and female mice.
Figure 5.
Baseline pulmonary protein expression of key components of TLR4 signaling is not different between neonatal male and female mice. (A) Representative Western blots and (B) densitometric analysis showing male (white bars) and female (black bars) neonatal (P0) pulmonary expression of (A,B) key components of TLR4 signaling: TLR4 and Myd88; (A,C) NFκB activating kinases: IKKα and IKKβ; (A,D) NFκB inhibitory proteins: IκBα, IκBβ; and (A,E) NFκB subunits: p50, p65 and cRel. GAPDH as loading control. Values first normalized to GAPDH, and then to male control. Values shown as means ± SEM from 6 individual animals per sex.
Cytosolic pulmonary activation of canonical NFκB signaling induced by systemic LPS exposure does not differ between male and female neonatal mice
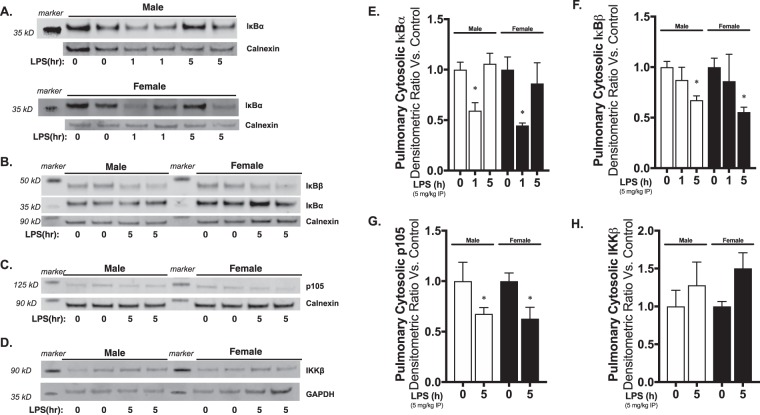
It is well known that canonical NFκB signaling proceeds following TLR4 activation69. In order for NFκB complexes to translocate to the nucleus, degradation of the cytosolic NFκB inhibitory proteins IκBα, IκBβ and p105 must occur33. Previous studies of sex-specific differences in neonatal lung injury have invoked differences in NFκB signaling11,12. Thus, we sought to assess whether the first step penultimate step of NFκB nuclear translocation differed between sexes in the lungs of neonatal mice exposed to systemic LPS. We found similar patterns of IκBα degradation (Fig. 6A,B,E), IκBβ degradation (Fig. 6B,F) and p105 degradation (Fig. 6C,G) in the lungs of male and female neonatal mice exposed to systemic LPS. These data demonstrate similar kinetics of cytosolic TLR4-NFκB signaling in the lungs of neonatal male and female mice exposed to systemic LPS.
Figure 6.
Pulmonary cytosolic IκB degradation in response to systemic LPS is not different between neonatal male and female mice. Representative Western blots of pulmonary cytosolic extracts showing (A,B) IκBα and IκBβ, (C) p105 and (D) IKKβ in neonatal (P0) male and female mice following exposure to systemic LPS (5 mg/kg IP, 1–5 hours). Calnexin as loading control. Densitometric analysis of (E) IκBα, (F) IκBβ, (G) p105 and (F) IKKβ in pulmonary cytosolic extracts form neonatal male and female mice following exposure to systemic LPS (5 mg/kg IP, 1–5 hours). All values first normalized to loading control, then to unexposed, sex-specific control. Values shown as means ± SEM from 6 individual animals per sex per time point. *p < 0; 0.05 vs. control.
Previous studies have implicated differential regulation of the NFκB activating kinase IKKβ in the pathogenesis of sex differences in neonatal hyperoxic lung injury11,12. Thus, we assessed pulmonary IKKβ protein expression in the lungs of neonatal male and female mice following exposure to systemic LPS. Consistent with previous reports, we found no differences in baseline IKKβ expression between male and female neonatal mice (Fig. 6D,H)11. Furthermore, we found that exposure to systemic LPS did not alter total IKKβ levels in either male or female mice (Fig. 6D,H).
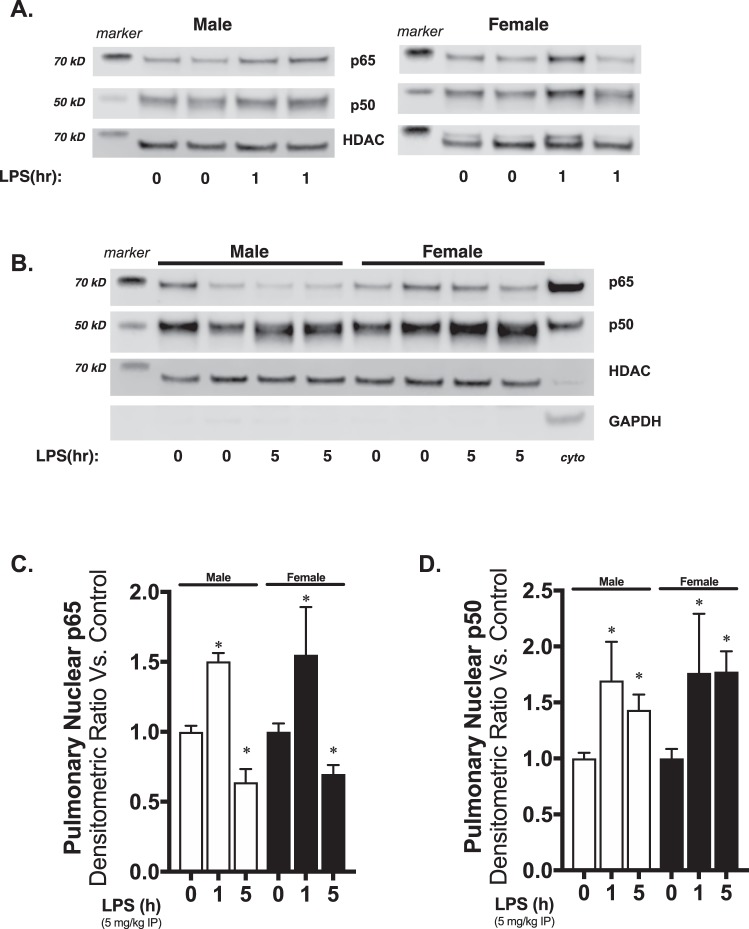
Nuclear translocation of NFκB subunits induced by systemic LPS exposure does not differ between male and female neonatal mice
In our final comparison of LPS-induced pulmonary TLR4 signaling in neonatal male and female mice, we assessed nuclear translocation of the key NFκB subunits p65 and p50. At early time points, we found significantly elevated nuclear p50 and p65 in both male and female LPS-exposed mice (Fig. 7A,C,D). At later time points, p65 levels were significantly lower than baseline, while p50 remained elevated in both male and female mice (Fig. 7B–D). Of note, previous studies have shown that NFκB activity and nuclear translocation of NFκB is oscillatory following innate immune stimulation70–76. Thus, the observed dynamic changes in nuclear NFκB subunits demonstrates that oscillatory NFκB activity is similar between LPS-exposed male and female mice. Thus, the similarities between male and female mice demonstrate the absence of difference in pulmonary TLR4 signaling and subsequent NFκB activation following exposure to systemic LPS.
Figure 7.
Pulmonary nuclear translocation of the NFκB subunits p65 and p50 in response to systemic LPS is not different between neonatal male and female mice. Representative Western blots of pulmonary nuclear extracts showing (A) p65 and p50 in neonatal (P0) male and female mice following 1 hours of systemic LPS exposure (5 mg/kg IP), and (B) p65 and p50 following 5 hours of systemic LPS exposure (5 mg/kg IP). Cyto = cytosolic positive control. HDAC as nuclear loading control. GAPDH shown as evidence of purity of nuclear extract. Densitometric analysis of (C) p65, (D) p50 in pulmonary nuclear extracts form neonatal (P0) male and female mice following exposure to systemic LPS. All values first normalized to loading control, then to unexposed, sex-specific control. Values shown as means ± SEM from 6 individual animals per sex per time point. *p < 0; 0.05 vs. control.
Discussion
We found that in response to early postnatal systemic LPS challenge, there was no difference in pulmonary injury and abnormal lung development between male and female mice. Following systemic LPS exposure on P0 mice, both males and females demonstrated evidence of abnormal lung development with decreased radial alveolar counts, increased airspace area and increased mean linear intercept. The deviations from control were similar in LPS-exposed male and female mice, indicating a lack of sex difference in terms of lung injury in response to systemic LPS exposure. Because previous reports have demonstrated sex differences in hyperoxia-induced neonatal lung injury and abnormal development, we sought to assess pulmonary expression of factors previously implicated in sex differences and lung injury, as well as the key components of TLR4-NFκB signaling in male and female mice. We found no differences in the pulmonary expression of key mediators of lung injury or apoptosis between LPS-exposed male and female neonatal mice. Furthermore, we found no difference between male and female mice in the baseline pulmonary expression of key mediators of TLR4-NFκB signaling, or in the kinetics of LPS-induced NFκB activation as assessed by cytosolic IκB inhibitory degradation and nuclear translocation of activating NFκB subunits. Together, these phenotypic, transcriptional, and mechanistic data support the conclusion that the innate immune response to early postnatal LPS exposure and resulting pulmonary sequelae are similar in male and female mice.
These results are interesting because clinical studies have reported sex-specific pulmonary implications following preterm delivery. While an increased risk of developing bronchopulmonary dysplasia (BPD) has been reported in males2–4, an increased incidence in persistent lung function following exposure to chorioamnionitis has been reported in in former preterm female neonates77. Importantly, not all studies agree that males have worse long-term respiratory morbidities following preterm birth78. These results argue for a better understanding of the mechanisms underlying the pulmonary response to various oxidant and inflammatory stressors encountered in the neonatal period and following preterm delivery.
Various pre-clinical models of neonatal lung injury exist6,9. Neonatal hyperoxia exposure is a well-established model that induces consistent and significant lung injury. Importantly, Lingappan and colleagues demonstrated that neonatal hyperoxia-induced lung injury was worse in male compared to female mice11. Of note, hyperoxic exposure was associated with evidence of increased NFκB activation in female mice, with increased levels of the active phosphorylated p65 in females and lower levels of the activating kinase IKKβ in males. These findings are consistent with previous reports demonstrating a protective effect of pulmonary NFκB signaling following hyperoxia exposure13,14,16.
Exposing the canalicular and saccular stage of lung to LPS consistently results in inflammation, injury and abnormal development across multiple species17–31. Similar to hyperoxia-induced pulmonary NFκB activity, LPS-induced NFκB activity plays some protective role in the neonatal lung31. While NFκB controls the expression of multiple likely injurious pro-inflammatory cytokines and chemokines, complete inhibition of LPS-induced NFκB activation exacerbates neonatal lung injury31. However, while pulmonary NFκB signaling has been implicated in the attenuated injury observed in female neonatal mice following hyperoxia exposure11,12,79, these results may not apply to lung injury and subsequent abnormal development following exposure to LPS. Importantly, NFκB activity following exposure to inflammatory stimuli results from signaling events that are likely independent from those leading to activation following exposure to oxidant stress. With exposure to inflammatory stress (eg. LPS-induced TLR4 activation), the IκB inhibitory proteins are phosphorylated and degraded, allowing NFκB nuclear translocation and DNA binding32,33. While the NFκB activation cascade occurring after exposure to inflammatory stress is well defined, the definitive pathway that occurs following exposure to oxidant stress remains debatable34–37. Therefore, the well-characterized sex-type specific differences in response to hyperoxia in the neonatal period may not be applicable to injury following exposure to inflammatory stress.
Previous studies have demonstrated that there are sex-specific differences in the innate immune response that are dynamic over the life course80–82. Multiple studies have interrogated whether there are sex-specific differences in TLR4 innate immune signaling in adults. The results of these studies are decidedly mixed, and these mixed results are likely related to differences in study design, dose of LPS used, the model organism used, the maturational stage of the organism, and whether the exposure was performed on cells in culture or in vivo. Proinflammatory cytokine (TNFα, IL-1β) levels were higher in LPS-exposed whole blood, neutrophils, and peripheral blood mononuclear cells obtained from healthy human male volunteers compared to female83–86, and LPS-induced IL-1β expression was higher in macrophages isolated from adult male mice compared to female66. In contrast to these findings, some studies have demonstrated a more robust response to LPS in adult female rodents and cells derived from adult females when compared to males. For example, in response to IV LPS challenge, adult female human volunteers demonstrate a more robust proinflammatory response compared to males87,88. Similarly, pro-inflammatory cytokine expression is higher in LPS-exposed adult female mice89 and macrophages isolated from adult female mice90 compared to males. Finally, it has even been published that there are no differences in circulating TNFα and IL-1β in male and female adult mice following IP LPS challenge91.
However, whether any of these findings guide our understanding of neonatal period is unclear. Significant progress has been made in determining differences between the neonatal and adult response to LPS challenge and TLR4 stimulation. While important differences between adults and neonates have been identified, most of the studies comparing early life TLR4 responsiveness have not evaluated for sex differences92–100. Furthermore, in the scant data that are available, reports are not consistent. Levels of LPS-stimulated cord blood IL-1β and IL-6 secretion are higher in males compared to females101. In contrast to this finding, no difference in LPS-stimulated cytokine levels were noted from LPS-exposed monocytes obtained from cord blood of preterm male and female neonates102. Following early neonatal IP LPS challenge in rats, systemic cytokine levels were not different between males and females, although mortality was higher in males103. Our data adds to this literature, and supports the conclusion that in response to early neonatal systemic LPS challenge, the acute innate immune response and early pulmonary sequelae in male and female mice are more similar than they are dissimilar.
Given our growing appreciation of the differences between male and female innate immunity, it is important to question our results and query the existing literature to better understand these findings. Given the known influence of sex hormones on the innate immune response82, studies have been done examining sex-specific differences in pre- and post-pubertal mice. Following IP LPS challenge, circulating levels of TNFα, IL-6, and IL-10 were not different between pre-pubertal male and female mice47. In contrast, post-pubertal mice demonstrated a sex difference, with circulating levels being higher in males compared to females47. The influence of sex hormones is further highlighted by the finding that pre-pubertal female mice are resistant to LPS-induced mortality comparted to post-pubertal females104. Human data support these findings, as levels of IL-1β, IL-6, and TNFα were not different between LPS-exposed male and female whole blood samples105. Of note, macrophage TLR4 expression is responsive to sex hormone levels106,107. In the current study, we did not assess our mice for sex hormone levels. However, previous studies have shown that there is a testosterone surge in male mice shortly after delivery, with levels returning to baseline and no longer different from females by 4–6 hours of life108,109. Furthermore, serum estrogen levels are similar in male and female neonatal rats110. Thus, it is possible that the confluence of the developing innate immune system and relatively similar levels of sex hormones present in the early neonatal period obviate the sex differences reported with post-pubertal LPS challenge.
There are important limitations to the current study. Here, we used systemic LPS challenge to stimulate the TLR4 mediated innate immune response. There are limitations to using endotoxemia as a clinically relevant model111. Namely, LPS challenge is a single exposure to a sterile stimulus. While it is very useful to interrogate TLR signaling, because there is no ongoing bacterial presence as there is with an active infection, the conclusions that can be drawn are limited. Thus, while these studies represent a first step, more work must be done using more complex models to interrogate sex-differences in the innate immune response. Additionally, we assessed the transcriptional response at 1 and 5 hours after exposure to systemic LPS. It is quite likely that significant changes occur before the one-hour time point, and beyond the 5 hour time point. One important remaining area to investigate is sex-differences in the factors controlling resolution of inflammation112. Importantly, we did not assess any markers of the mechanisms responsible for the resolution of inflammation. It is possible that while male and female neonatal mice have similar acute responses to LPS-induced TLR4 signaling, the time course to resolution and the factors controlling that process are different. How these mechanisms may affect the developing lung, and whether this occurs in a sex-specific manner, is unknown. Along these lines, we assessed lung morphometrics at 7 and 28 days following a single, early postnatal innate immune stimulus. While lungs of both LPS-exposed male and female mice are abnormal at postnatal day 7, it appears that the lungs are recovering by the 28 day time point. At this point, the abnormalities noted in RAC, airspace area, and mean linear intercepts at P7 in LPS-exposed male and female mice have attenuated. Thus, while the lung is recovering, it is not known if the mechanisms underlying that recovery are sex specific, or how the recovering lung would respond to a second injurious exposure. Additionally, it is unknown whether there are sex-specific differences in lung function, as only morphometrics were assessed here.
In conclusion, we found that following early postnatal systemic LPS challenge, both male and female neonatal mice demonstrated evidence of pulmonary injury and abnormal lung development. Objective markers showed that lung development was similarly impaired in LPS-exposed male and female mice. We interpret these data to support a lack of sex difference in terms of lung injury in response to systemic LPS exposure. Importantly, male and female pulmonary expression of key member of TLR4-NFκB signaling cascade was similar, as was the LPS-induced expression of pro-inflammatory and apoptotic mediators of lung injury. Lastly, the kinetics of LPS-induced pulmonary TLR4-NFκB signaling was similar in male and female neonatal mice. We speculate that in the early postnatal period, the pulmonary innate immune response to TLR4 stimulation is more similar than dissimilar in male and female mice. These results have implications for treatment strategies aimed at attenuating lung injury and abnormal development following exposure to inflammatory stress following preterm delivery.
Supplementary information
Acknowledgements
This work was supported by NIH Grant R01HL132941 to CJW.
Author Contributions
C.W. and S.M. conception and design of research; L.N., O.C., R.D., J.S., S.M. and C.W. performed experiments; L.N., O.C., R.D., J.S., S.M. and C.W. analyzed data; L.N., O.C., R.D., J.S., S.M. and C.W. interpreted results of experiments; L.N., O.C., R.D., S.M. and C.W. edited and revised manuscript; L.N., O.C., R.D., J.S., S.M. and C.W. approved final version of manuscript; L.N., S.M. and C.W. prepared figures; C.W. drafted manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-44955-0.
References
- 1.O’Driscoll D. N., McGovern M., Greene C. M. & Molloy E. J. Gender disparities in preterm neonatal outcomes. Acta Paediatr (2018). [DOI] [PubMed]
- 2.Townsel CD, Emmer SF, Campbell WA, Hussain N. Gender Differences in Respiratory Morbidity and Mortality of Preterm Neonates. Front Pediatr. 2017;5:6. doi: 10.3389/fped.2017.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farstad T, Bratlid D, Medbo S, Markestad T. Norwegian Extreme Prematurity Study G. Bronchopulmonary dysplasia - prevalence, severity and predictive factors in a national cohort of extremely premature infants. Acta Paediatr. 2011;100:53–8. doi: 10.1111/j.1651-2227.2010.01959.x. [DOI] [PubMed] [Google Scholar]
- 4.Binet ME, et al. Role of gender in morbidity and mortality of extremely premature neonates. Am J Perinatol. 2012;29:159–66. doi: 10.1055/s-0031-1284225. [DOI] [PubMed] [Google Scholar]
- 5.Balany J, Bhandari V. Understanding the Impact of Infection, Inflammation, and Their Persistence in the Pathogenesis of Bronchopulmonary Dysplasia. Front Med (Lausanne). 2015;2:90. doi: 10.3389/fmed.2015.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berger J, Bhandari V. Animal models of bronchopulmonary dysplasia. The term mouse models. Am J Physiol Lung Cell Mol Physiol. 2014;307:L936–47. doi: 10.1152/ajplung.00159.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins RD, et al. Bronchopulmonary Dysplasia: Executive Summary of a Workshop. J Pediatr. 2018;197:300–8. doi: 10.1016/j.jpeds.2018.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: A review of pathogenesis and pathophysiology. Respir Med. 2017;132:170–7. doi: 10.1016/j.rmed.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nardiello C, Mizikova I, Morty RE. Looking ahead: where to next for animal models of bronchopulmonary dysplasia? Cell Tissue Res. 2017;367:457–68. doi: 10.1007/s00441-016-2534-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Dong W. Oxidative stress and bronchopulmonary dysplasia. Gene. 2018;678:177–83. doi: 10.1016/j.gene.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Lingappan K, Jiang W, Wang L, Moorthy B. Sex-specific differences in neonatal hyperoxic lung injury. Am J Physiol Lung Cell Mol Physiol. 2016;311:L481–93. doi: 10.1152/ajplung.00047.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Lingappan K. Differential sex-specific effects of oxygen toxicity in human umbilical vein endothelial cells. Biochem Biophys Res Commun. 2017;486:431–7. doi: 10.1016/j.bbrc.2017.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenna S, et al. Sustained hyperoxia-induced NF-kappaB activation improves survival and preserves lung development in neonatal mice. Am J Physiol Lung Cell Mol Physiol. 2014;306:L1078–89. doi: 10.1152/ajplung.00001.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Michaelis KA, et al. IkappaBbeta-mediated NF-kappaB activation confers protection against hyperoxic lung injury. Am J Respir Cell Mol Biol. 2014;50:429–38. doi: 10.1165/rcmb.2013-0303OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright CJ, Zhuang T, La P, Yang G, Dennery PA. Hyperoxia-induced NF-kappaB activation occurs via a maturationally sensitive atypical pathway. Am J Physiol Lung Cell Mol Physiol. 2009;296:L296–306. doi: 10.1152/ajplung.90499.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang G, Abate A, George AG, Weng YH, Dennery PA. Maturational differences in lung NF-kappaB activation and their role in tolerance to hyperoxia. J Clin Invest. 2004;114:669–78. doi: 10.1172/JCI200419300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lambermont VA, et al. Effects of intra-amniotic lipopolysaccharide exposure on the fetal lamb lung as gestation advances. Pediatr Res. 2014;75:500–6. doi: 10.1038/pr.2014.3. [DOI] [PubMed] [Google Scholar]
- 18.Tang JR, et al. Moderate postnatal hyperoxia accelerates lung growth and attenuates pulmonary hypertension in infant rats after exposure to intra-amniotic endotoxin. Am J Physiol Lung Cell Mol Physiol. 2010;299:L735–48. doi: 10.1152/ajplung.00153.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi CW, et al. Bronchopulmonary dysplasia in a rat model induced by intra-amniotic inflammation and postnatal hyperoxia: morphometric aspects. Pediatr Res. 2009;65:323–7. doi: 10.1203/PDR.0b013e318193f165. [DOI] [PubMed] [Google Scholar]
- 20.Willet KE, et al. Antenatal endotoxin and glucocorticoid effects on lung morphometry in preterm lambs. Pediatr Res. 2000;48:782–8. doi: 10.1203/00006450-200012000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Cheah FC, et al. Airway inflammatory cell responses to intra-amniotic lipopolysaccharide in a sheep model of chorioamnionitis. Am J Physiol Lung Cell Mol Physiol. 2009;296:L384–93. doi: 10.1152/ajplung.90547.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kallapur SG, et al. Recruited inflammatory cells mediate endotoxin-induced lung maturation in preterm fetal lambs. Am J Respir Crit Care Med. 2005;172:1315–21. doi: 10.1164/rccm.200506-1007OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kallapur SG, et al. Vascular changes after intra-amniotic endotoxin in preterm lamb lungs. Am J Physiol Lung Cell Mol Physiol. 2004;287:L1178–85. doi: 10.1152/ajplung.00049.2004. [DOI] [PubMed] [Google Scholar]
- 24.Willet KE, et al. Intra-amniotic injection of IL-1 induces inflammation and maturation in fetal sheep lung. Am J Physiol Lung Cell Mol Physiol. 2002;282:L411–20. doi: 10.1152/ajplung.00097.2001. [DOI] [PubMed] [Google Scholar]
- 25.Kallapur SG, Willet KE, Jobe AH, Ikegami M, Bachurski CJ. Intra-amniotic endotoxin: chorioamnionitis precedes lung maturation in preterm lambs. Am J Physiol Lung Cell Mol Physiol. 2001;280:L527–36. doi: 10.1152/ajplung.2001.280.3.L527. [DOI] [PubMed] [Google Scholar]
- 26.Miller JD, Benjamin JT, Kelly DR, Frank DB, Prince LS. Chorioamnionitis stimulates angiogenesis in saccular stage fetal lungs via CC chemokines. Am J Physiol Lung Cell Mol Physiol. 2010;298:L637–45. doi: 10.1152/ajplung.00414.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prince LS, Okoh VO, Moninger TO, Matalon S. Lipopolysaccharide increases alveolar type II cell number in fetal mouse lungs through Toll-like receptor 4 and NF-kappaB. Am J Physiol Lung Cell Mol Physiol. 2004;287:L999–1006. doi: 10.1152/ajplung.00111.2004. [DOI] [PubMed] [Google Scholar]
- 28.Benjamin JT, et al. NF-kappaB activation limits airway branching through inhibition of Sp1-mediated fibroblast growth factor-10 expression. J Immunol. 2010;185:4896–903. doi: 10.4049/jimmunol.1001857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prince LS, Dieperink HI, Okoh VO, Fierro-Perez GA, Lallone RL. Toll-like receptor signaling inhibits structural development of the distal fetal mouse lung. Dev Dyn. 2005;233:553–61. doi: 10.1002/dvdy.20362. [DOI] [PubMed] [Google Scholar]
- 30.Hou Y, et al. Activation of the nuclear factor-kappaB pathway during postnatal lung inflammation preserves alveolarization by suppressing macrophage inflammatory protein-2. Am J Physiol Lung Cell Mol Physiol. 2015;309:L593–604. doi: 10.1152/ajplung.00029.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alvira CM, Abate A, Yang G, Dennery PA, Rabinovitch M. Nuclear factor-kappaB activation in neonatal mouse lung protects against lipopolysaccharide-induced inflammation. Am J Respir Crit Care Med. 2007;175:805–15. doi: 10.1164/rccm.200608-1162OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghosh S, Hayden M. New regulators of NF-kappaB in inflammation. Nat Rev Immunol. 2008;8:837–48. doi: 10.1038/nri2423. [DOI] [PubMed] [Google Scholar]
- 33.Hayden M, Ghosh S. Shared principles in NF-kappaB signaling. Cell. 2008;132:344–62. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 34.Janssen-Heininger Y, Poynter M, Baeuerle P. Recent advances towards understanding redox mechanisms in the activation of nuclear factor kappaB. Free Radic Biol Med. 2000;28:1317–27. doi: 10.1016/S0891-5849(00)00218-5. [DOI] [PubMed] [Google Scholar]
- 35.Rahman A, Fazal F. Blocking NF-kappaB: an inflammatory issue. Proc Am Thorac Soc. 2011;8:497–503. doi: 10.1513/pats.201101-009MW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sawyer CC. Child mortality estimation: estimating sex differences in childhood mortality since the 1970s. PLoS Med. 2012;9:e1001287. doi: 10.1371/journal.pmed.1001287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morgan MJ, Liu ZG. Crosstalk of reactive oxygen species and NF-kappaB signaling. Cell Res. 2011;21:103–15. doi: 10.1038/cr.2010.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Emery JL, Mithal A. The number of alveoli in the terminal respiratory unit of man during late intrauterine life and childhood. Archives of disease in childhood. 1960;35:544–7. doi: 10.1136/adc.35.184.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooney TP, Thurlbeck WM. The radial alveolar count method of Emery and Mithal: a reappraisal 2–intrauterine and early postnatal lung growth. Thorax. 1982;37:580–3. doi: 10.1136/thx.37.8.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jia H, et al. Pulmonary Epithelial TLR4 Activation Leads to Lung Injury in Neonatal Necrotizing Enterocolitis. J Immunol. 2016;197:859–71. doi: 10.4049/jimmunol.1600618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nold MF, et al. Interleukin-1 receptor antagonist prevents murine bronchopulmonary dysplasia induced by perinatal inflammation and hyperoxia. Proc Natl Acad Sci USA. 2013;110:14384–9. doi: 10.1073/pnas.1306859110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liao J, et al. The NLRP3 inflammasome is critically involved in the development of bronchopulmonary dysplasia. Nat Commun. 2015;6:8977. doi: 10.1038/ncomms9977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McKenna S, Butler B, Jatana L, Ghosh S, Wright CJ. Inhibition of IkappaBbeta/NFkappaB signaling prevents LPS-induced IL1beta expression without increasing apoptosis in the developing mouse lung. Pediatr Res. 2017;82:1064–72. doi: 10.1038/pr.2017.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stouch AN, et al. IL-1beta and Inflammasome Activity Link Inflammation to Abnormal Fetal Airway Development. J Immunol. 2016;196:3411–20. doi: 10.4049/jimmunol.1500906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benjamin JT, et al. Cutting Edge: IL-1alpha and Not IL-1beta Drives IL-1R1-Dependent Neonatal Murine Sepsis Lethality. J Immunol. 2018;201:2873–8. doi: 10.4049/jimmunol.1801089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stouch AN, et al. IkappaB kinase activity drives fetal lung macrophage maturation along a non-M1/M2 paradigm. J Immunol. 2014;193:1184–93. doi: 10.4049/jimmunol.1302516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kuo SM. Gender Difference in Bacteria Endotoxin-Induced Inflammatory and Anorexic Responses. PLoS One. 2016;11:e0162971. doi: 10.1371/journal.pone.0162971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li P, et al. Mice deficient in IL-1 beta-converting enzyme are defective in production of mature IL-1 beta and resistant to endotoxic shock. Cell. 1995;80:401–11. doi: 10.1016/0092-8674(95)90490-5. [DOI] [PubMed] [Google Scholar]
- 49.Wilcoxen SC, Kirkman E, Dowdell KC, Stohlman SA. Gender-dependent IL-12 secretion by APC is regulated by IL-10. J Immunol. 2000;164:6237–43. doi: 10.4049/jimmunol.164.12.6237. [DOI] [PubMed] [Google Scholar]
- 50.Jenne CN, Kubes P. Immune surveillance by the liver. Nat Immunol. 2013;14:996–1006. doi: 10.1038/ni.2691. [DOI] [PubMed] [Google Scholar]
- 51.Gao B, Jeong WI, Tian Z. Liver: An organ with predominant innate immunity. Hepatology. 2008;47:729–36. doi: 10.1002/hep.22034. [DOI] [PubMed] [Google Scholar]
- 52.Racanelli V, Rehermann B. The liver as an immunological organ. Hepatology. 2006;43:S54–62. doi: 10.1002/hep.21060. [DOI] [PubMed] [Google Scholar]
- 53.Mathison JC, Ulevitch RJ. The clearance, tissue distribution, and cellular localization of intravenously injected lipopolysaccharide in rabbits. J Immunol. 1979;123:2133–43. [PubMed] [Google Scholar]
- 54.Praaning-van Dalen DP, Brouwer A, Knook DL. Clearance capacity of rat liver Kupffer, Endothelial, and parenchymal cells. Gastroenterology. 1981;81:1036–44. [PubMed] [Google Scholar]
- 55.McCuskey RS, McCuskey PA, Urbaschek R, Urbaschek B. Species differences in Kupffer cells and endotoxin sensitivity. Infect Immun. 1984;45:278–80. doi: 10.1128/iai.45.1.278-280.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Freudenberg N, et al. The role of macrophages in the uptake of endotoxin by the mouse liver. Virchows Arch B Cell Pathol Incl Mol Pathol. 1992;61:343–9. doi: 10.1007/BF02890437. [DOI] [PubMed] [Google Scholar]
- 57.Ge Y, Ezzell RM, Tompkins RG, Warren HS. Cellular distribution of endotoxin after injection of chemically purified lipopolysaccharide differs from that after injection of live bacteria. J Infect Dis. 1994;169:95–104. doi: 10.1093/infdis/169.1.95. [DOI] [PubMed] [Google Scholar]
- 58.Nakao A, et al. The fate of intravenously injected endotoxin in normal rats and in rats with liver failure. Hepatology. 1994;19:1251–6. doi: 10.1002/hep.1840190525. [DOI] [PubMed] [Google Scholar]
- 59.Takeuchi M, et al. The localization of lipopolysaccharide in an endotoxemic rat liver and its relation to sinusoidal thrombogenesis: light and electron microscopic studies. Pathol Res Pract. 1994;190:1123–33. doi: 10.1016/S0344-0338(11)80438-3. [DOI] [PubMed] [Google Scholar]
- 60.Yasui M, et al. Immunohistochemical detection of endotoxin in endotoxemic rats. Hepatogastroenterology. 1995;42:683–90. [PubMed] [Google Scholar]
- 61.Ge Y, et al. Relationship of tissue and cellular interleukin-1 and lipopolysaccharide after endotoxemia and bacteremia. J Infect Dis. 1997;176:1313–21. doi: 10.1086/514127. [DOI] [PubMed] [Google Scholar]
- 62.Shao B, et al. A host lipase detoxifies bacterial lipopolysaccharides in the liver and spleen. J Biol Chem. 2007;282:13726–35. doi: 10.1074/jbc.M609462200. [DOI] [PubMed] [Google Scholar]
- 63.Shao B, Munford RS, Kitchens R, Varley AW. Hepatic uptake and deacylation of the LPS in bloodborne LPS-lipoprotein complexes. Innate Immun. 2012;18:825–33. doi: 10.1177/1753425912442431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Deng M, et al. Lipopolysaccharide clearance, bacterial clearance, and systemic inflammatory responses are regulated by cell type-specific functions of TLR4 during sepsis. J Immunol. 2013;190:5152–60. doi: 10.4049/jimmunol.1300496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Du XH, Yao YM, Li R, Shen CA, Yin HN. [Influence of sexual difference on expression of Toll-like receptor 4 and myeloid differential protein-2 mRNA in the lung in septic rats] Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2005;17:726–8. [PubMed] [Google Scholar]
- 66.Marriott I, Bost KL, Huet-Hudson YM. Sexual dimorphism in expression of receptors for bacterial lipopolysaccharides in murine macrophages: a possible mechanism for gender-based differences in endotoxic shock susceptibility. J Reprod Immunol. 2006;71:12–27. doi: 10.1016/j.jri.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 67.Harju K, Glumoff V, Hallman M. Ontogeny of Toll-like receptors Tlr2 and Tlr4 in mice. Pediatr Res. 2001;49:81–3. doi: 10.1203/00006450-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 68.Roberts BJ, Dragon JA, Moussawi M, Huber SA. Sex-specific signaling through Toll-Like Receptors 2 and 4 contributes to survival outcome of Coxsackievirus B3 infection in C57Bl/6 mice. Biol Sex Differ. 2012;3:25. doi: 10.1186/2042-6410-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kawasaki T, Kawai T. Toll-like receptor signaling pathways. Front Immunol. 2014;5:461. doi: 10.3389/fimmu.2014.00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sakai J, et al. Lipopolysaccharide-induced NF-kappaB nuclear translocation is primarily dependent on MyD88, but TNFalpha expression requires TRIF and MyD88. Sci Rep. 2017;7:1428. doi: 10.1038/s41598-017-01600-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zambrano S, De Toma I, Piffer A, Bianchi ME, Agresti A. NF-kappaB oscillations translate into functionally related patterns of gene expression. Elife. 2016;5:e09100. doi: 10.7554/eLife.09100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoffmann A, Baltimore D. Circuitry of nuclear factor kappaB signaling. Immunol Rev. 2006;210:171–86. doi: 10.1111/j.0105-2896.2006.00375.x. [DOI] [PubMed] [Google Scholar]
- 73.Covert MW, Leung TH, Gaston JE, Baltimore D. Achieving stability of lipopolysaccharide-induced NF-kappaB activation. Science. 2005;309:1854–7. doi: 10.1126/science.1112304. [DOI] [PubMed] [Google Scholar]
- 74.Barken D. Comment on "Oscillations in NF- B Signaling Control the Dynamics of Gene Expression". Science. 2005;308(5718):52a–52a. doi: 10.1126/science.1107904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nelson DE, et al. Oscillations in NF-kappaB signaling control the dynamics of gene expression. Science. 2004;306:704–8. doi: 10.1126/science.1099962. [DOI] [PubMed] [Google Scholar]
- 76.Hoffmann A, Levchenko A, Scott ML, Baltimore D. The IkappaB-NF-kappaB signaling module: temporal control and selective gene activation. Science. 2002;298:1241–5. doi: 10.1126/science.1071914. [DOI] [PubMed] [Google Scholar]
- 77.Jones MH, et al. Chorioamnionitis and subsequent lung function in preterm infants. PLoS One. 2013;8:e81193. doi: 10.1371/journal.pone.0081193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kotecha SJ, Lowe J, Kotecha S. Does the sex of the preterm baby affect respiratory outcomes? Breathe (Sheff). 2018;14:100–7. doi: 10.1183/20734735.017218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Coarfa C, et al. Sexual dimorphism of the pulmonary transcriptome in neonatal hyperoxic lung injury: identification of angiogenesis as a key pathway. Am J Physiol Lung Cell Mol Physiol. 2017;313:L991–L1005. doi: 10.1152/ajplung.00230.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.O’Driscoll DN, Greene CM, Molloy EJ. Immune function? A missing link in the gender disparity in preterm neonatal outcomes. Expert Rev Clin Immunol. 2017;13:1061–71. doi: 10.1080/1744666X.2017.1386555. [DOI] [PubMed] [Google Scholar]
- 81.Jaillon, S., Berthenet, K. & Garlanda, C. Sexual Dimorphism in Innate Immunity. Clin Rev Allergy Immunol (2017). [DOI] [PubMed]
- 82.Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626–38.. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 83.Imahara SD, Jelacic S, Junker CE, O’Keefe GE. The influence of gender on human innate immunity. Surgery. 2005;138:275–82. doi: 10.1016/j.surg.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 84.Asai K, et al. Gender differences in cytokine secretion by human peripheral blood mononuclear cells: role of estrogen in modulating LPS-induced cytokine secretion in an ex vivo septic model. Shock. 2001;16:340–3. doi: 10.1097/00024382-200116050-00003. [DOI] [PubMed] [Google Scholar]
- 85.Moxley G, et al. Sexual dimorphism in innate immunity. Arthritis Rheum. 2002;46:250–8. doi: 10.1002/1529-0131(200201)46:1<250::AID-ART10064>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 86.Aomatsu M, Kato T, Kasahara E, Kitagawa S. Gender difference in tumor necrosis factor-alpha production in human neutrophils stimulated by lipopolysaccharide and interferon-gamma. Biochem Biophys Res Commun. 2013;441:220–5. doi: 10.1016/j.bbrc.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 87.van Eijk LT, et al. Gender differences in the innate immune response and vascular reactivity following the administration of endotoxin to human volunteers. Crit Care Med. 2007;35:1464–9. doi: 10.1097/01.CCM.0000266534.14262.E8. [DOI] [PubMed] [Google Scholar]
- 88.Wegner A, et al. Inflammation-induced pain sensitization in men and women: does sex matter in experimental endotoxemia? Pain. 2015;156:1954–64. doi: 10.1097/j.pain.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Trentzsch H, Stewart D, De Maio A. Genetic background conditions the effect of sex steroids on the inflammatory response during endotoxic shock. Crit Care Med. 2003;31:232–6. doi: 10.1097/00003246-200301000-00036. [DOI] [PubMed] [Google Scholar]
- 90.Scotland RS, Stables MJ, Madalli S, Watson P, Gilroy DW. Sex differences in resident immune cell phenotype underlie more efficient acute inflammatory responses in female mice. Blood. 2011;118:5918–27. doi: 10.1182/blood-2011-03-340281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Everhardt Queen A, Moerdyk-Schauwecker M, McKee LM, Leamy LJ, Huet YM. Differential Expression of Inflammatory Cytokines and Stress Genes in Male and Female Mice in Response to a Lipopolysaccharide Challenge. PLoS One. 2016;11:e0152289. doi: 10.1371/journal.pone.0152289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Corbett NP, et al. Ontogeny of Toll-like receptor mediated cytokine responses of human blood mononuclear cells. PLoS One. 2010;5:e15041. doi: 10.1371/journal.pone.0015041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang JP, Yang Y, Levy O, Chen C. Human neonatal peripheral blood leukocytes demonstrate pathogen-specific coordinate expression of TLR2, TLR4/MD2, and MyD88 during bacterial infection in vivo. Pediatr Res. 2010;68:479–83. doi: 10.1203/PDR.0b013e3181f90810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nguyen M, et al. Acquisition of adult-like TLR4 and TLR9 responses during the first year of life. PLoS One. 2010;5:e10407. doi: 10.1371/journal.pone.0010407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Levy O, et al. Selective impairment of TLR-mediated innate immunity in human newborns: neonatal blood plasma reduces monocyte TNF-alpha induction by bacterial lipopeptides, lipopolysaccharide, and imiquimod, but preserves the response to R-848. J Immunol. 2004;173:4627–34. doi: 10.4049/jimmunol.173.7.4627. [DOI] [PubMed] [Google Scholar]
- 96.Yan SR, et al. Role of MyD88 in diminished tumor necrosis factor alpha production by newborn mononuclear cells in response to lipopolysaccharide. Infect Immun. 2004;72:1223–9. doi: 10.1128/IAI.72.3.1223-1229.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Forster-Waldl E, et al. Monocyte toll-like receptor 4 expression and LPS-induced cytokine production increase during gestational aging. Pediatr Res. 2005;58:121–4. doi: 10.1203/01.PDR.0000163397.53466.0F. [DOI] [PubMed] [Google Scholar]
- 98.Pedraza-Sanchez S, Hise AG, Ramachandra L, Arechavaleta-Velasco F, King CL. Reduced frequency of a CD14+ CD16+ monocyte subset with high Toll-like receptor 4 expression in cord blood compared to adult blood contributes to lipopolysaccharide hyporesponsiveness in newborns. Clin Vaccine Immunol. 2013;20:962–71. doi: 10.1128/CVI.00609-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goriely S, et al. A defect in nucleosome remodeling prevents IL-12(p35) gene transcription in neonatal dendritic cells. J Exp Med. 2004;199:1011–6. doi: 10.1084/jem.20031272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Upham JW, et al. Development of interleukin-12-producing capacity throughout childhood. Infect Immun. 2002;70:6583–8. doi: 10.1128/IAI.70.12.6583-6588.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kim-Fine S, et al. Male gender promotes an increased inflammatory response to lipopolysaccharide in umbilical vein blood. J Matern Fetal Neonatal Med. 2012;25:2470–4. doi: 10.3109/14767058.2012.684165. [DOI] [PubMed] [Google Scholar]
- 102.Sharma AA, et al. Hierarchical maturation of innate immune defences in very preterm neonates. Neonatology. 2014;106:1–9. doi: 10.1159/000358550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kosyreva AM. The Sex Differences of Morphology and Immunology of SIRS of Newborn Wistar Rats. Int Sch Res Notices. 2014;2014:190749. doi: 10.1155/2014/190749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Joachim R, Suber F, Kobzik L. Characterising Pre-pubertal Resistance to Death from Endotoxemia. Sci Rep. 2017;7:16541. doi: 10.1038/s41598-017-16743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Casimir GJ, et al. Gender differences and inflammation: an in vitro model of blood cells stimulation in prepubescent children. J Inflamm (Lond). 2010;7:28. doi: 10.1186/1476-9255-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rettew JA, Huet YM, Marriott I. Estrogens augment cell surface TLR4 expression on murine macrophages and regulate sepsis susceptibility in vivo. Endocrinology. 2009;150:3877–84. doi: 10.1210/en.2009-0098. [DOI] [PubMed] [Google Scholar]
- 107.Rettew JA, Huet-Hudson YM, Marriott I. Testosterone reduces macrophage expression in the mouse of toll-like receptor 4, a trigger for inflammation and innate immunity. Biol Reprod. 2008;78:432–7. doi: 10.1095/biolreprod.107.063545. [DOI] [PubMed] [Google Scholar]
- 108.Poling MC, Kauffman AS. Sexually dimorphic testosterone secretion in prenatal and neonatal mice is independent of kisspeptin-Kiss1r and GnRH signaling. Endocrinology. 2012;153:782–93. doi: 10.1210/en.2011-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Corbier P, Edwards DA, Roffi J. The neonatal testosterone surge: a comparative study. Arch Int Physiol Biochim Biophys. 1992;100:127–31. doi: 10.3109/13813459209035274. [DOI] [PubMed] [Google Scholar]
- 110.Rhoda J, Corbier P, Roffi J. Gonadal steroid concentrations in serum and hypothalamus of the rat at birth: aromatization of testosterone to 17 beta-estradiol. Endocrinology. 1984;114:1754–60. doi: 10.1210/endo-114-5-1754. [DOI] [PubMed] [Google Scholar]
- 111.Fink MP. Animal models of sepsis. Virulence. 2014;5:143–53. doi: 10.4161/viru.26083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sugimoto MA, Sousa LP, Pinho V, Perretti M, Teixeira MM. Resolution of Inflammation: What Controls Its Onset? Front Immunol. 2016;7:160. doi: 10.3389/fimmu.2016.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.