Abstract
BACKGROUND:
Despite that physiotherapists (PTs) are supposed to have adequate knowledge of musculoskeletal disorders and the different prevention strategies, they are at high risk of developing work-related musculoskeletal disorders (WRMDs).
AIM:
This study aimed to investigate the prevalence, profile, predictors, and response to WRMDs among Egyptian PTs.
METHODS:
A self-administrated questionnaire was distributed either manually or via e-mail to 564 PTs with at least two years of working experience. Questions elicited information about the personal and occupational history of the respondents in addition to the experience of WRMDs in the past two years.
RESULTS:
Four hundred and fourteen respondents (82.6%) reported WRMDs within the last two years, with the lower back as the most common area affected (68.8%). More than half the PTs (54.8%) who sustained a WRMD reported that their injury took place in a private setting. Significant predictors for WRMDs were age (AOR = 0.78; 95% CI = 0.66, 0.91) and number of years of experience in physiotherapy practice (AOR = 1.26; 95% CI = 1.07, 1.49). In response to the injury, about 73.9% of the respondents stated that they did not officially report their injury and 55.8% of them reported losing a half day or more from their work.
CONCLUSION:
The prevalence of WRMDs among Egyptian physiotherapists is high. Despite socioeconomic and cultural differences between Egypt and other countries, our study findings were consistent with the published reports. Further studies are needed to explore the cultural and psychosocial risk factors of WRMDs.
Keywords: Work-Related Musculoskeletal Disorders, Physiotherapists, Egypt, Prevalence
Introduction
According to the World Health Organization, work-related musculoskeletal disorders (WRMDs) are defined as injuries that include a wide range of inflammatory or degenerative diseases and disorders resulting in pain or functional impairment [1], [2]. They originate from muscles, joints, ligaments, tendons, and bones and last more than three days due to work-related events and conditions [3], [4]. Consequently, WRMDs lead to lost work time, work restrictions, loss of consciousness, career shift or even death [5], [6]. Moreover, these disorders are associated with economic and social burdens, that ultimately impact the quality of life [7].
It is well documented that health care workers are at high risk of musculoskeletal disorders [3]. Despite that nurses have reported the highest rates of WRMDs in different work settings, yet Physiotherapists (PTs) are exposed to the same risk factors [8], [9]. Repetitive tasks, continuous bending, awkward sustained postures, lifting and transferring patients are considered main risk factors, making healthcare providers vulnerable to musculoskeletal injuries [4], [5], [6], [7], [8].
Adding to the complexity, although PTs have adequate knowledge of musculoskeletal injuries and the different prevention strategies, this does not grant them protection from developing WRMDs [5], [9]. Moreover, evidence indicates that PTs tend to work while in pain or with a musculoskeletal injury even while exacerbating their condition. They are also less likely to report their injuries or seek care relying on self-treatment based on their clinical expertise [9].
Previous studies revealed that WRMDs are more common among fresh graduates and young PTs, mostly within the first five years of practice [3], [6]. On the other hand, old aged PTs are less liable to injury as they are more involved in documentary work than manual practice [10]. Most of the previous research revealed that the lower back is the most common area of injury reported among PTs [4], [5], [6], [7], [8].
The prevalence and profile of WRMDs among PTs vary according to the studied population and are influenced by various factors as age, sex, type of clinical setting and practice, years of experience and contact hours with patients. To date, there is lack of information regarding the prevalence of WRMDs among PTs in Egypt. Only two recent studies investigated this problem, one among Egyptian pediatric PTs and the other was limited by a small sample size [3], [11]. Therefore, this study was conducted to determine the prevalence, profile, and predictors of WRMDs among Egyptian PTs in addition to their response to such type of injuries aiming to contribute to the development of effective prevention and control strategies.
Methods
Study design and Participants
A cross-sectional design was used for the current study. Potential participants included all licensed Egyptian PTs working in different practice settings with at least two years of working experience. PTs who were retired or did not practice within the two years before the survey were excluded.
Sample size and technique
Epi Info software, version 7 was used to calculate the sample size. Based on the findings of the study conducted by Al-Eisa et al., [3], the prevalence of WRMDs was assumed to be 77%, with a precision of ± 5%, employing 80% power, 99% confidence interval, and with a design effect of 1.0, the minimal sample size required was 470 participants. Moreover, 20% was added to compensate for possible non- response; the final sample size was estimated to be 564 participants. A systematic random sampling technique was used to select participants from the membership list of the Egyptian Physical Therapy Association after approval of the ethical committee of Faculty of Physical Therapy, Cairo University.
Instrument
The survey instrument was a self-administrated questionnaire based on a previously published instrument by Holder et al., [5]. The questionnaire included two parts composed of predominately closed-ended questions. The first portion elicited information about the personal and occupational history of the participants including questions about sex, age, weight, height, setting, speciality, years of experience and hours of patient contact. The second portion inquired if the participant had experienced any WRMDs in the past two years or not. Respondents who reported WRMDs were asked about the type of injury, specific activities that caused the injury, the body part affected, the type of work setting in which the injury took place and the exacerbating activities. Additionally, they were asked questions related to the immediate and long-term responses to the injury.
Procedures
During the period between April and June 2018, five hundred and sixty-four copies of the questionnaire were distributed either manually at hospitals, clinics, and centres for PTs residing in Cairo and nearby governorates or via email for those living in remote governorates. A cover letter was attached to the questionnaire to explain the purpose of the study and to assure confidentiality. Also, a contact number and an email were provided in case of further inquiries. Participants were asked to complete and return the questionnaire within two weeks. Two reminders were sent to the participants who did not submit their questionnaires after two weeks. The study procedures were carried out by the ethics requirements of the Declaration of Helsinki.
Data analysis
Data were coded, entered and statistically analysed using the Statistical Package for Social Sciences (SPSS) version 21. Qualitative data were expressed as numbers and percentages. Quantitative data were presented as the mean ± Standard Deviation (SD). As the main outcome measures were binary variables namely WRMDs (1 variable), WRMDs according to most frequent body areas affected (6 variables), immediate responses to WRMDs (4 variables) and long term responses to WRMDs (3 variables), 14 multivariate logistic regression models were built to define the significant predictors among the tested independent variables by using binary logistic regression test. The tested independent variables entered in each regression model were sex, age, BMI, physiotherapy practice area, years of experience and contact hours with patients/week. Results were reported as Adjusted Odds Ratio (AOR) and 95% Confidence Interval (CI). A p value less than 0.05 was considered to be statistically significant.
Results
A total of 501 out of 564 questionnaires were completed and returned with a response rate of 88.9%. The mean age of the respondents was 29.9 ± 6.4 years, with a range of 24-63 years, with nearly equal distribution regarding their sex. Estimation of the BMI of the respondents revealed that about two-thirds of the respondents were overweight and obese (63.9%), one third were normal weight, and only 0.6% were underweight. The background characteristics of the respondents are summarised in Table 1.
Table 1.
Background characteristics of the respondents (Total = 501)
| Variables | Number | Per cent | |
|---|---|---|---|
| Sex | |||
| Female | 234 | 47.7 | |
| Male | 267 | 53.3 | |
| Age in years (Mean ± SD)* | 29.9 ± 6.4 | ||
| Weight in Kg (Mean ± SD)* | 77 ± 17.2 | ||
| Height in cm (Mean ± SD)* | 168.8 ± 9.7 | ||
| BMI** (Mean ± SD)* | 26.9 ± 5 | ||
| Physiotherapy practice area | |||
| General | 261 | 52.1 | |
| Specialized | 240 | 47.9 | |
| Years of Experience (Mean ± SD)* | 8.4 ± 6 | ||
| Contact hours with patients/week (Mean ± SD)* | 30.7 ± 20 | ||
Quantitative variables are presented as Mean ± SD;
BMI = Body Mass Index.
Prevalence and Profile of WRMDs
Four hundred and fourteen respondents (82.6%) reported WRMDs within the last two years. Two hundred seventy-seven (66.9%) reported sustaining more than one WRMD.
The respondents reported the highest levels of WRMDs in the lower back (68.8 %), shoulder (40.8%), neck (36.7%), upper back (30.2%), wrist (29%) and knee (27.1%). While the elbow, ankle, and hip were the least reported areas (8%, 7% and 4.6% respectively).
Figure 1 illustrates that the most common types of WRMDs reported by the respondents were muscle strain (44.2%), tendinitis (37.2%) and vertebral disk problem (33.8%). Regarding the activities that caused the WRMDs, the top 3 prevalent activities reported were performing manual therapy techniques (32.6%), maintaining a position for a prolonged period (24.9%) and working when physically fatigued (20.8%) (Table 2).
Figure 1.
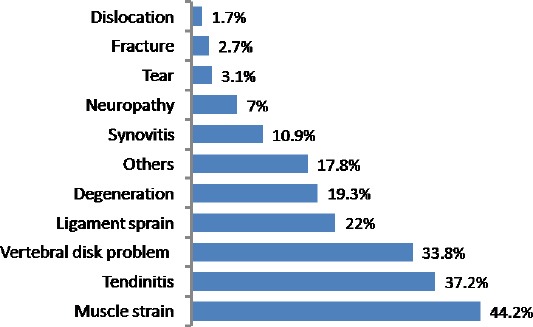
Percent distribution of WRMDs according to the type of injury (Total = 414)*; *Multiple responses were allowed
Table 2.
Frequency of WRMD according to the specific activity that caused the WRMDs (Total = 414)*
| Activity that caused injury | Number | Per cent |
|---|---|---|
| Performing manual therapy techniques | 135 | 32.6 |
| Maintaining a position for a prolonged period | 103 | 24.9 |
| Working when physically fatigued | 86 | 20.8 |
| Performing repetitive tasks | 78 | 18.8 |
| Applying modalities | 72 | 17.4 |
| Bending/ twisting | 72 | 17.4 |
| Lifting heavy equipment or patients | 48 | 11.6 |
| Working in an Awkward/ Cramped Position | 37 | 8.9 |
| Transferring a Patient | 32 | 7.7 |
| Responding to an unanticipated/ Sudden movement by a patient | 24 | 5.8 |
| Slipping/ tripping/ falling | 6 | 1.4 |
*Multiple responses were allowed.
More than half the PTs (54.8%) who sustained a WRMD reported that their injury occurred in a private setting (Figure 2). Seventy-five per cent of the respondents with WRMDs experienced recurrence of symptoms.
Figure 2.
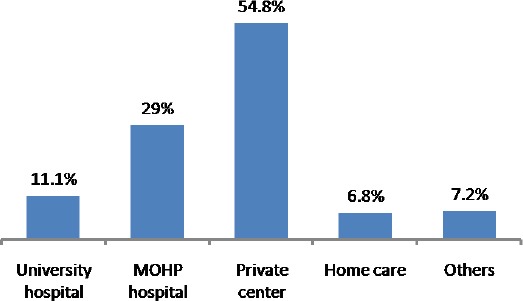
Percent distribution of WRMDs by the type of setting in which the injury occurred (Total = 414); *Multiple responses were allowed
Performing manual therapy techniques (36.5%), maintaining a position for a prolonged period (35.6%) and performing repetitive tasks (21.5%) were the most common activities that caused exacerbation of their symptoms during clinical practice (Table 3).
Table 3.
Exacerbating activity as reported by respondents who experienced a recurrence of symptoms of WRMDs (Total = 312)*
| Exacerbating activity | Number | Per cent |
|---|---|---|
| Performing manual therapy techniques | 114 | 36.5 |
| Maintaining a position for a prolonged period | 111 | 35.6 |
| Performing repetitive tasks | 67 | 21.5 |
| Bending/ twisting | 47 | 15.1 |
| Lifting | 41 | 13.1 |
| Working in an awkward/ cramped Position | 38 | 12.2 |
| Transferring a patient | 27 | 8.7 |
| Squatting | 22 | 7.1 |
| Performing overhead activities | 18 | 5.8 |
| Walking | 13 | 4.2 |
| Climbing stairs | 12 | 3.8 |
| Reaching | 6 | 1.9 |
Multiple responses were allowed
Predictors of WRMDs
Multivariate logistic regression analysis was performed to single out risk factors associated with WRMDs among PTs as shown in Table 4.
Table 4.
Multivariate logistic regression model for factors associated with WRMDs
| Variables | WRMDs | P value* | AOR* (95% CI) | ||
|---|---|---|---|---|---|
| Yes N = 414 |
No N = 87 |
||||
| Sex, n (%) | 0.218 | 1.38 (0.83 - 2.3) | |||
| Female | 196 (83.8) | 38 (16.2) | |||
| Male | 218 (81.6) | 49 (18.4) | |||
| Age in years, mean ± SD | 29.7 ± 6.2 | 31 ± 7.2 | 0.002 | 0.78 (0.67 - 0.91) | |
| BMI**, mean ± SD | 27 ± 5.1 | 26.5 ± 4.7 | 0.155 | 1.04 (0.96 - 1.1) | |
| Physiotherapy practice area, n (%) | 0.722 | 0.92 (0.57 - 1.49) | |||
| General | 213 (81.6) | 48 (18.4) | |||
| Specialized | 201 (83.8) | 39 (16.2) | |||
| Years of Experience, mean ± SD | 8.3 ± 5.9 | 9 ± 6.5 | 0.006 | 1.26 (1.07 - 1.48) | |
| Contact hours with patients/week, mean ± SD | 31.2 ± 20.3 | 28.6 ± 18.8 | 0.102 | 1.01 (0.99 – 1.02) | |
P value, AOR (Adjusted Odds Ratio) and 95% CI (Confidence Interval) obtained by Binary logistic regression test;
BMI = Body Mass Index.
Significant predictors for WRMDs were age (AOR = 0.78; 95% CI = 0.66, 0.91) and number of years of experience in physiotherapy practice (AOR = 1.26; 95% CI = 1.07, 1.49).
Table 5 summarises the results of six multivariate logistic regression models to define risk factors associated with WRMDs according to the most frequent body areas affected.
Table 5.
Multivariate logistic regression models for factors associated with WRMDs according to most frequent body areas affected
| Variables | Lower back | Shoulder | Neck | Upper back | Knee | Wrist | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P value | AOR 95% CI | P value | AOR 95% CI | P value | AOR 95% CI | P value | AOR 95% CI | P value | AOR 95% CI | P value | AOR 95% CI | |
| Sex (Female/ Male) | 0.416 | 0.85 (0.57 - 1.26) | 0.004 | 1.83 (1.21 - 2.78) | 0.058 | 1.5 (0.99 - 2.28) | 0.168 | 1.37 (0.88 - 2.14) | 0.688 | 0.91 (0.57 - 1.45) | 0.005 | 1.93 (1.22 - 3.07) |
| Age in years | 0.001 | 0.81 (0.72 - 0.92) | 0.009 | 0.84 (0.74 - 0.96) | 0.118 | 0.9 (0.79 - 1.03) | 0.148 | 0.9 (0.79 - 1.04) | 0.246 | 0.92 (0.79 - 1.06) | 0.452 | 0.95 (0.82 - 1.09) |
| BMI** | 0.472 | 1.01 (0.98 - 1.06) | 0.051 | 1.04 (1 - 1.08) | 0.561 | 1.01 (0.97 - 1.06) | 0.552 | 0.99 (0.94 - 1.03) | 0.069 | 1.04 (0.99 - 1.09) | 0.538 | 1.01 (0.97 - 1.06) |
| Physiotherapy practice area (General/ Specialized) | 0.556 | 1.12 (0.77 - 1.62) | 0.708 | 1.08 (0.73 - 1.58) | 0.350 | 0.83 (0.56- 1.23) | 0.715 | 1.08 (0.71 - 1.64) | 0.775 | 0.94 (0.61 - 1.45) | 0.978 | 1.01 (0.66 - 1.54) |
| Years of Experience | 0.007 | 1.2 (1.05 - 1.37) | 0.016 | 1.19 (1.03 - 1.36) | 0.170 | 1.1 (0.96 - 1.27) | 0.170 | 1.11 (0.96 - 1.29) | 0.344 | 1.08 (0.92 - 1.26) | 0.668 | 1.03 (0.89 - 1.2) |
| Contact hours with patients/week | 0.03 | 1.01 (1 – 1.02) | 0.364 | 1.01 (0.99 - 1.02) | 0.654 | 0.99 (0.99 – 1) | 0.392 | 1.01 (0.99 – 1.02) | 0.181 | 1.01 (0.99 – 1.02) | 0.009 | 1.02 (1 – 1.03) |
*P value, AOR (Adjusted Odds Ratio) and 95% CI (Confidence Interval) obtained by binary logistic regression test;
BMI = Body Mass Index.
These prediction models revealed that female PTs had an increased risk of WRMDs in the shoulder (AOR = 1.83; 95% CI = 1.21, 2.78), and wrist (AOR = 1.93; 95% CI= 1.22, 3.07) than their male counterparts. Older ages were associated with a decreased risk of WRMDs in the lower back (AOR = 0.81; 95% CI = 0.72, 0.92) and shoulder (AOR = 0.84; 95% CI = 0.74, 0.96), meanwhile, the number of experience years was associated with increased risk of WRMDs in the lower back (AOR = 1.2; 95% CI = 1.05, 1.37) and shoulder (AOR = 1.19; 95% CI = 1.03, 1.36). The number of hours in contact with patients per week was associated with increased risk of WRMDs in the lower back (AOR = 1.01; 95% CI = 1, 1.02) and wrist (AOR = 1.02; 95% CI = 1, 1.03).
Immediate and long-term response to WRMDs
As an immediate response to the injury, most of the respondents (73.9%) stated that they did not officially report their injury, and only about one third (38.6%) consulted a physician for their injury. Meanwhile, the vast majority of the PTs with WRMDs (95.4%) received treatment and more than half the respondents (55.8%) reported losing half day or more from their work as a result of injury (Table 6).
Table 6.
Immediate and long term responses to the injury as reported by the respondents who sustained a WRMD (Total = 414)*
| Type of response | Response | Number | Per cent |
|---|---|---|---|
| Immediate response | Officially reported the injury | 108 | 26.1 |
| Consulted a physician | 160 | 38.6 | |
| Lost half day or more of work as an immediate effect of the injury | 231 | 55.8 | |
| Received treatment | 395 | 95.4 | |
| Long term response | Alteration of working habits | 300 | 72.5 |
| Limitation of contact time with patients | 170 | 41.1 | |
| Considering changing their job | 163 | 39.4 |
Multiple responses were allowed.
Regarding the long-term response to WRMDs, more than two-thirds of the respondents (72.5 %) indicated that they had altered their working habits as a response to their injury (Table 6). A variety of coping strategies were used by PTs who altered their working habits, changing working position frequently, using improved body mechanics and taking more breaks during the workday were the most common stated coping strategies (55%, 35%, and 31.7% respectively). While nearly half the respondents indicated that they had not limited their contact time with the patients nor considered changing their job in response to the WRMDs. (41.1% and 39.4% respectively) (Table 6).
Multivariate logistic regression analysis was performed to identify the significant predictors for each response (4 immediate and three long terms) as the dependent variable. Results from these prediction models revealed that PTs working in general practice were less likely to officially report their injury and consult physician than specialists (AOR = 0.58; 95% CI = 0.37, 0.92 and AOR = 0.55; 95% CI = 0.36, 0.84 respectively). In terms of gender, female PTs were more likely to consult a physician and alter their working habits in response to WRMDs (AOR = 1.83; 95% CI = 1.17, 2.87 and AOR = 1.62; 95% CI = 1, 2.6 respectively) compared to male PTs. Additionally, increased BMI was independently associated with the likelihood of consulting a physician for the injury (AOR = 1.05; 95% CI = 1, 1.1).
Discussion
The purpose of this study was to investigate the prevalence and profile of WRMDs among physiotherapists in Egypt and to identify their causes and risk factors. What makes our study unique is the large sample size and the high response rate. Out of 564 questionnaires, 501 were returned with a response rate of 88.9%. In previous studies, however, the response rate was 53% in Australia [12], 58% in Nigeria [13], 59% in Turkey [6], and 75% in the United Kingdom [14]. Compared to the previous studies, the achieved high response rate may be explained by the increased perception and awareness among physiotherapists in Egypt about the value of participating in research activities.
The findings of this study indicate that Egyptian physiotherapists are at high risk of developing WRMDs in the workplace. On average, 82.6% of respondents reported at least one WRMD within the last two years, and 66.9% reported sustaining more than one WRMD (Table 1). By looking at the published rates of WRMDs and compare them to our findings, it is valid to say that WRMDs among physiotherapists in Egypt is high and needs further attention. It has been documented that WRMDs among physiotherapists have many burdens, including pain and distress, cost, decreased working hours, and potential disability [14], [15], [16]. Notably, muscle strain, tendinitis, and vertebral disk problem were the most repeatedly mentioned WRMDs types among our respondents (44.2%, 37.2%, 33.8%, respectively) (Table 1).
Consisting with the literature, our respondents reported the highest levels of WRMDs in the lower back (68.8 %), followed by shoulders (40.8%), neck (36.7%), and knees (27.1%). Although lower back pain (LBP) is the most common complaint among physiotherapists in the workplace in many countries [12], [17], [18], the high prevalence found in our study (68.8%) is alarming because it is among the highest in the published data. For instance, in Canada Mierzejewski and Kumar (1997) reported a prevalence of (49%) of LBP among physiotherapists [19]. Similar rates have been reported at (45%) in the USA [8], 35% in Australia [12], 38% in Greece [20], and 26% in Turkey [6]. In the Middle East, although there is a dearth of such research, the literature review identified three relevant studies [10], [21], [22]. In Shehab et al., (2003) study, 70% of physiotherapists who practice physiotherapy in the State of Kuwait reported LBP [21]. However, a recent study in the State of Kuwait documented a dramatic decrease in the prevalence of LBP from 70% in 2003 to 32% in 2010 [10], yet still similar to the international records. In Saudi Arabia, a recent study conducted an online survey targeted members of the Saudi Physical Therapy Association. They reported that 89% of participants had a work-related LBP [22]. In our study, however, nearly 70% of the participants reported LBP, which is among the highest published rates up-to-date. By combining our findings with past research, it is valid to conclude that LBP among physiotherapists in Egypt poses a significant population health problem. Despite a tremendous burden of LBP on individuals, it has been linked to psychological distress [23], and physical disability [24]. Consequently, LBP may negatively affect the productivity of physiotherapists and the overall efficiency of physiotherapy practice in Egypt.
Apart from LBP, this study, as in other studies, revealed that other parts of the body could be influenced by WRMDs [6], [25]. In this study, more than 40% of respondents reported shoulder pain, 36.7% reported neck pain, and 27.1% suffered from knee problems. Although the past research was focused on LBP and the evidence of WRMDs in other areas of the body is limited, our findings seem to be in line with the published rates [15], [26]. Interestingly, nearly one-third (27.1%) of the respondents reported knee problems. This is a striking finding of our study because it is much higher than the published rates in previous studies. In Salik and Özcan’s (2004) study, about 8% of surveyed physiotherapists reported knee problems [6]. Similarly, Anyfantis and Biska (2018) reported that 6% [20], and Cromie et al., (2000) reported that 11.2% of participants had knee problems [18]. The high prevalence of knee problems reported in our study may be explained, in part, by the fact that almost two-thirds (63.9%) of the respondents were overweight and obese. Obesity was documented by many authors as a risk factor for many musculoskeletal problems, including LBP, hip, and knee problems [27], [28], [29].
In our study, the mean age of the respondents was (29.9 ± 6.4). This is an important finding because it confirms the link between work-experience and vulnerability to WRMDs. This finding goes by other studies stating that WRMDs typically occur in physiotherapists between the ages of 20 to 40 years [18], [30]. One explanation of this prevalence in young age may be due to lack of experience, lack of professional training, or limited prophylactic and/or coping strategies. It can also be referred to other cultural or socioeconomic factors in the early career years. This increased prevalence of WRMDs among the younger physiotherapists is problematic because such burdens can increase with age [31]. Effective interventions that prevent WRMDs, such as educational programs, improving the infrastructure, and seeking assistance from other healthcare staff in physically-demanding tasks (e.g., patient transfer) are suggested strategies to subsidise WRMDs [17].
In this study, we also collected data on the most common activities that caused WRMDs in clinical settings (Table 3). Similar to the previously published data, our analyses showed that (32.6%) of the participants developed their injury during performing manual therapy techniques, followed by (24.9%) due to maintaining a position for a prolonged period, and (20.8%) while working when physically fatigued. Past studies have shown consistent correlations between biomechanical factors, such as awkward posture, manual therapy practices, repeated movement and lifting heavy objects, and the development of WRMDs [5], [32]. Campo et al., (2008) conducted a 1-year prospective study with physiotherapists to investigate the risk factors of WRMDs in the USA. They found that patient repositioning and transfers were the main risk factors for WRMDs [17]. Salik and Özcan (2004) identified the main causes of WRMDs as patient positioning and transfer, repeated movements, lifting heavy objects, and working when fatigued [6]. Two studies highlighted the risk of staying in the same position for a long time, manual therapy practices, and repeating the same movement on the musculoskeletal system of physiotherapists [8], [12]. In our study, the top exacerbating activity was performing manual therapy technique. This can be explained by the fact that manual therapy is common in Egypt, and the number of days treated patients usually exceeds the number of physiotherapists in a given clinical facility. Thus, most of the physiotherapists work when they are exhausted, and this adds extra loads on their body and exacerbate their musculoskeletal pain.
Equally important, research shows that physiotherapists are reluctant to talk about their pain due to WRMDs [9]. Interestingly, more than half the surveyed physiotherapists (54.8%) who sustained a WRMD reported that their injury occurred in a private setting, and 20% of them were working when physically fatigued. Furthermore, the majority of respondents (73.9%) stated that they did not report their injury, and only about one third (38.6%) consulted a physician for treatment (Table 2). This finding is important because it reflects the cultural and socioeconomic dimensions of WRMDs. The clinical culture of healthcare facilities, as well as the culture of physiotherapists themselves, may play an essential role in admitting any pain caused by patient care. As documented in previous research, more than half of the respondents did not report their WRMDs to their employers [9]. It is a common sense that physiotherapists in Egypt work in both the public and private sectors. Therefore, they usually experience heavy workloads [33]. Our survey revealed that more than half the respondents (55.8%) reported losing half a day or more from their work as a result of injury (Table 6). Because some of the hidden pains are disabling in the long run, this claim deserves further exploration because it may potentially lead to loss of experienced physiotherapists.
Regarding the long-term response to WRMDs, our analyses indicated that the majority of the respondents (72.5%) stated that they had changed their working habits as a response to their injury (Table 6). Several coping strategies were used by physiotherapists who modified or changed their working habits. For example, about 55% of respondents reported changing working position frequently during treatment sessions, 35% used improved body mechanics, and 31.7% had more breaks during the workday. Noteworthy, nearly 40% of surveyed physiotherapists considered leaving the profession due to WRMDs, which is higher to what has been found in the literature. Although Campo et al., (2008) reported the lowest rate of leaving the profession at less than 1%, others reported similar to our findings [17]. For example, Cromie et al., (2000) documented that one in six physiotherapists changed or left the profession due to WRMDs [18]. Anyfantis and Biska (2018) reported that 32% of the recruited physiotherapists considered changing the profession [20]. Contrarily, Alrowayeh et al., (2010) reported no changes in work habits nor desire to leave the profession among the surveyed physiotherapists in their study. This inconsistency among studies is perhaps due to cultural and socioeconomic factors [10]. In this study, we performed multivariate logistic regression analyses to see if there are associations between risk factors, such as age, gender, working hours and years of work experience, and WRMDs as shown in Table 4. Age and the number of years of experience in physiotherapy practice were identified as significant predictors for WRMDs. Our analyses also revealed that female physiotherapists are at an increased risk of WRMD in the upper limbs (mainly in the shoulder and wrists) than their male colleagues. The latter was proven true by many authors [6], [26], [34].
Limitations: This study has some limitations. As all cross-sectional designs, the findings can only recognise risk factors. Second, the self-administered questionnaire could have some recall bias. Participants may forget to mention all incidents of WRMDs. Also, since the physiotherapy job market in Egypt is extremely competitive, it is possible that some respondents underestimated or even hide their injury to show that they are fit and competence for the job. Finally, since we did not ask about the physical activity level of our participants, it is possible that athletes vs non-athletes physiotherapists experience WRMDs at different levels and frequencies.
In conclusion, this study reveals that the WRMDs among Egyptian physiotherapists is high and similar to their counterparts elsewhere. Despite socioeconomic and cultural differences between Egypt and other countries, our study showed relatively consistent findings to the published reports. Further research that focuses on cultural and psychosocial dimension may provide valuable insight into other issues and risk factors of WRMDs among physiotherapists in Egypt.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.World Health Organization. Identification and control of work-related diseases. Geneva: The Organization;Technical Report Series. No. 714; 1985. [PubMed] [Google Scholar]
- 2.Milhem M, Kalichman L, Ezra D, Alperovitch-Najenson D. Work-related musculoskeletal disorders among physical therapists:A comprehensive narrative review. International journal of occupational medicine and environmental health. 2016;29(5):735–47. doi: 10.13075/ijomeh.1896.00620. https://doi.org/10.13075/ijomeh.1896.00620 PMid:27518884. [DOI] [PubMed] [Google Scholar]
- 3.Al-Eisa E, Buragadda S, Shaheen AA, Ibrahim A, Melam GR. Work related musculoskeletal disorders:causes, prevalence and response among egyptian and saudi physical therapists. Middle-East Journal of Scientific Research. 2012;12(4):523–9. [Google Scholar]
- 4.Abaraogu UO, Ezema CI, Nwosu CK. Job stress dimension and work-related musculoskeletal disorders among southeast Nigerian physiotherapists. International Journal of Occupational Safety and Ergonomics. 2017;23(3):404–9. doi: 10.1080/10803548.2016.1219476. https://doi.org/10.1080/10803548.2016.1219476 PMid:27486916. [DOI] [PubMed] [Google Scholar]
- 5.Holder NL, Clark HA, DiBlasio JM, Hughes CL, Scherpf JW, Harding L, Shepard KF. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Physical therapy. 1999;79(7):642–52. doi: 10.1093/ptj/79.7.642. https://doi.org/10.1093/ptj/79.7.642 PMid:10416574. [DOI] [PubMed] [Google Scholar]
- 6.Salik Y, Özcan A. Work-related musculoskeletal disorders:a survey of physical therapists in Izmir-Turkey. BMC musculoskeletal disorders. 2004;5(1):27. doi: 10.1186/1471-2474-5-27. https://doi.org/10.1186/1471-2474-5-27 PMid:15315712 PMCid:PMC516038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahimi F, Kazemi K, Zahednejad S, López-López D, Calvo-Lobo C. Prevalence of Work-Related Musculoskeletal Disorders in Iranian Physical Therapists:A Cross-sectional Study. Journal of manipulative and physiological therapeutics. 2018;41(6):503–7. doi: 10.1016/j.jmpt.2018.02.003. https://doi.org/10.1016/j.jmpt.2018.02.003 PMid:30098820. [DOI] [PubMed] [Google Scholar]
- 8.Bork BE, Cook TM, Rosecrance JC, Engelhardt KA, Thomason ME, Wauford IJ, Worley RK. Work-related musculoskeletal disorders among physical therapists. Physical therapy. 1996;76(8):827–35. doi: 10.1093/ptj/76.8.827. https://doi.org/10.1093/ptj/76.8.827 PMid:8710962. [DOI] [PubMed] [Google Scholar]
- 9.Darragh AR, Huddleston W, King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am J Occup Ther. 2009;63(3):351–62. doi: 10.5014/ajot.63.3.351. https://doi.org/10.5014/ajot.63.3.351 PMid:19522144. [DOI] [PubMed] [Google Scholar]
- 10.Alrowayeh HN, Alshatti TA, Aljadi SH, Fares M, Alshamire MM, Alwazan SS. Prevalence, characteristics, and impacts of work-related musculoskeletal disorders:a survey among physical therapists in the State of Kuwait. BMC musculoskeletal disorders. 2010;11(1):116. doi: 10.1186/1471-2474-11-116. https://doi.org/10.1186/1471-2474-11-116 PMid:20540724 PMCid:PMC2905326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atia DT, Abdelazeim FH, Radwan H. Impact of work-related musculoskeletal disorders on Egyptian pediatric physical therapists:one-year follow-up study. Trends in Applied Sciences Research. 2015;10(3):175. https://doi.org/10.3923/tasr.2015.175.182. [Google Scholar]
- 12.West DJ, Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Australian Journal of Physiotherapy. 2001;47(3):179–86. doi: 10.1016/s0004-9514(14)60265-8. https://doi.org/10.1016/S0004-9514(14)60265-8. [DOI] [PubMed] [Google Scholar]
- 13.Adegoke BO, Akodu AK, Oyeyemi AL. Work-related musculoskeletal disorders among Nigerian physiotherapists. BMC musculoskeletal disorders. 2008;9(1):112. doi: 10.1186/1471-2474-9-112. https://doi.org/10.1186/1471-2474-9-112 PMid:18710570 PMCid:PMC2535595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glover W, McGregor A, Sullivan C, Hague J. Work-related musculoskeletal disorders affecting members of the Chartered Society of Physiotherapy. Physiotherapy. 2005;91(3):138–47. https://doi.org/10.1016/j.physio.2005.06.001. [Google Scholar]
- 15.Glover W. Lifting the Lid on Work-related Ill-health and Musculoskeletal Injury:CSP embarks on large-scale member study. Physiotherapy. 2003;89(7):394–5. https://doi.org/10.1016/S0031-9406(05)60072-7. [Google Scholar]
- 16.Nordin NA, Leonard JH, Thye NC. Work-related injuries among physiotherapists in public hospitals:a Southeast Asian picture. Clinics. 2011;66(3):373–8. doi: 10.1590/S1807-59322011000300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campo M, Weiser S, Koenig KL, Nordin M. Work-related musculoskeletal disorders in physical therapists:a prospective cohort study with 1-year follow-up. Physical Therapy. 2008;88(5):608–19. doi: 10.2522/ptj.20070127. https://doi.org/10.2522/ptj.20070127 PMid:18276935 PMCid:PMC2390722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cromie JE, Robertson VJ, Best MO. Occupational injuries in PTs. Physical therapy. 2000;80(5):529–30. https://doi.org/10.1093/ptj/80.4.336 PMid:10758519. [PubMed] [Google Scholar]
- 19.Mierzejewski M, Kumar S. Prevalence of low back pain among physical therapists in Edmonton, Canada. Disability and Rehabilitation. 1997;19(8):309–17. doi: 10.3109/09638289709166544. https://doi.org/10.3109/09638289709166544 PMid:9279486. [DOI] [PubMed] [Google Scholar]
- 20.Anyfantis ID, Biska A. Musculoskeletal disorders among Greek physiotherapists:Traditional and emerging risk factors. Safety and health at work. 2018;9(3):314–8. doi: 10.1016/j.shaw.2017.09.003. https://doi.org/10.1016/j.shaw.2017.09.003 PMid:30370163 PMCid:PMC6130005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shehab D, Al-Jarallah K, Moussa MA, Adham N. Prevalence of low back pain among physical therapists in Kuwait. Medical Principles and Practice. 2003;12(4):224–30. doi: 10.1159/000072288. https://doi.org/10.1159/000072288 PMid:12966194. [DOI] [PubMed] [Google Scholar]
- 22.Alghadir A, Zafar H, Iqbal ZA, Al-Eisa E. Work-related low back pain among physical therapists in Riyadh, Saudi Arabia. Workplace health &safety. 2017;65(8):337–45. doi: 10.1177/2165079916670167. https://doi.org/10.1177/2165079916670167 PMid:28121518. [DOI] [PubMed] [Google Scholar]
- 23.Shaw WS, Hartvigsen J, Woiszwillo MJ, Linton SJ, Reme SE. Psychological distress in acute low back pain:a review of measurement scales and levels of distress reported in the first 2 months after pain onset. Archives of physical medicine and rehabilitation. 2016;97(9):1573–87. doi: 10.1016/j.apmr.2016.02.004. https://doi.org/10.1016/j.apmr.2016.02.004 PMid:26921683. [DOI] [PubMed] [Google Scholar]
- 24.Gouveia N, Rodrigues A, Eusébio M, Ramiro S, Machado P, Canhão H, Branco JC. Prevalence and social burden of active chronic low back pain in the adult Portuguese population:results from a national survey. Rheumatology international. 2016;36(2):183–97. doi: 10.1007/s00296-015-3398-7. https://doi.org/10.1007/s00296-015-3398-7 PMid:26661091. [DOI] [PubMed] [Google Scholar]
- 25.Rossettini G, Rondoni A, Schiavetti I, Tezza S, Testa M. Prevalence and risk factors of thumb pain in Italian manual therapists:An observational cross-sectional study. Work. 2016;54(1):159–69. doi: 10.3233/WOR-162289. https://doi.org/10.3233/WOR-162289 PMid:27061697. [DOI] [PubMed] [Google Scholar]
- 26.Islam M, Habib M, Hafez M, Nahar N, Lindstrom-Hazel D, Rahman M. Musculoskeletal complaints among physiotherapy and occupational therapy rehabilitation professionals in Bangladesh. Work. 2015;50(3):379–86. doi: 10.3233/WOR-151994. [DOI] [PubMed] [Google Scholar]
- 27.Lievense AM, Bierma-Zeinstra SM, Verhagen AP, Van Baar ME, Verhaar JA, Koes BW. Influence of obesity on the development of osteoarthritis of the hip:a systematic review. Rheumatology. 2002;41(10):1155–62. doi: 10.1093/rheumatology/41.10.1155. https://doi.org/10.1093/rheumatology/41.10.1155 PMid:12364636. [DOI] [PubMed] [Google Scholar]
- 28.Manek NJ, Hart D, Spector TD, MacGregor AJ. The association of body mass index and osteoarthritis of the knee joint:an examination of genetic and environmental influences. Arthritis &Rheumatism:Official Journal of the American College of Rheumatology. 2003;48(4):1024–9. doi: 10.1002/art.10884. https://doi.org/10.1002/art.10884 PMid:12687544. [DOI] [PubMed] [Google Scholar]
- 29.Østbye T, Dement JM, Krause KM. Obesity and workers'compensation:results from the Duke Health and Safety Surveillance System. Archives of internal medicine. 2007;167(8):766–73. doi: 10.1001/archinte.167.8.766. https://doi.org/10.1001/archinte.167.8.766 PMid:17452538. [DOI] [PubMed] [Google Scholar]
- 30.Rugelj D. Low back pain and other work-related musculoskeletal problems among physiotherapists. Applied ergonomics. 2003;34(6):635–9. doi: 10.1016/S0003-6870(03)00059-0. https://doi.org/10.1016/S0003-6870(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 31.Iqbal Z, Alghadir A. Prevalence of work-related musculoskeletal disorders among physical therapists. Med Pr. 2015;66(4):459–69. doi: 10.13075/mp.5893.00142. https://doi.org/10.13075/mp.5893.00142 PMid:26536963. [DOI] [PubMed] [Google Scholar]
- 32.Warren G. Moving and handling:reducing risk through assessment. Nursing Standard (2014+) 2016;30(40):49. doi: 10.7748/ns.30.40.49.s45. https://doi.org/10.7748/ns.30.40.49.s45 PMid:27275915. [DOI] [PubMed] [Google Scholar]
- 33.Elden NM, Rizk HI, Wahby G. Improving Health System in Egypt:Perspectives of Physicians. Egyptian Journal of Community Medicine. 2016;34(1) https://doi.org/10.21608/ejcm.2016.646. [Google Scholar]
- 34.Falavigna A, Teles AR, Mazzocchin T, de Braga GL, Kleber FD, Barreto F, Santin JT, Barazzetti D, Lazzaretti L, Steiner B, Beckenkamp NL. Increased prevalence of low back pain among physiotherapy students compared to medical students. European Spine Journal. 2011;20(3):500–5. doi: 10.1007/s00586-010-1646-9. https://doi.org/10.1007/s00586-010-1646-9 PMid:21136121 PMCid:PMC3048232. [DOI] [PMC free article] [PubMed] [Google Scholar]


