Abstract
BACKGROUND:
Over the past decades, the study of the microenvironment of cancer has supported the hypothesis between inflammation and cancer. Previous studies have demonstrated a promising value of platelet-to-lymphocyte (PLR) and neutrophil-to-lymphocyte ratio (NLR) as a systemic inflammatory response in prostate cancer.
AIM:
To evaluate their pre-biopsy values of PLR and NLR in predicting prostate cancer.
MATERIAL AND METHODS:
This is a diagnostic study with retrospective design. We included all benign prostatic hyperplasia (BPH) and prostate cancer (PCa) patients who underwent prostate biopsy in Adam Malik Hospital between August 2011 and August 2015. We used PSA value above 4 ng/dL as the threshold for the biopsy candidates. The relationship between pre-biopsy variables affecting the percentage of prostate cancer risk was evaluated, including age, prostate-specific antigen (PSA) level, and estimated prostate volume (EPV). The PLR and NLR were calculated from the ratio of related platelets or absolute neutrophil counts with their absolute lymphocyte counts. The values then analysed to evaluate their associations with the diagnosis of BPH and PCa.
RESULTS:
Out of 298 patients included in this study, we defined two groups consist of 126 (42.3%) BPH and 172 PCa (57.7%) patients. Mean age for both groups are 66.36 ± 7.53 and 67.99 ± 7.48 years old (p = 0.64), respectively. There are statistically significant differences noted from both BPH and PCa groups in terms of PSA (19.28 ± 27.11 ng/dL vs 40.19 ± 49.39 ng/dL), EPV (49.39 ± 23.51 cc vs 58.10 ± 30.54 cc), PLR (160.27 ± 98.96 vs 169.55 ± 78.07), and NLR (3.57 ± 3.23 vs 4.22 ± 2.59) features of both BPH and PCa groups respectively (p < 0.05). A Receiver Operating Characteristics (ROC) analysis was performed for PLR and NLR in analysing their value in predicting prostate cancer. The Area Under the Curve (AUC) of PLR is 57.9% with a sensitivity of 56.4% and specificity of 55.6% in the cut-off point of 143 (p = 0.02). The NLR cut-off point of 3.08 gives 62.8% AUC with 64.5% sensitivity and 63.5% specificity. These AUCs were comparable with the AUC of PSA alone (68.5%). We performed logistic regression between PSA, PLR, and NLR with result in the exclusion of PLR if calculated conjunctively. Therefore, NLR has a promising performance in predicting PCa in patients with PSA above 4 ng/dL (OR = 3.2; 95%CI: 1.96-5.11). We found as many as 80 (63.5%) patients with benign biopsy results with negative NLR value in this study.
CONCLUSION:
NLR has promising value in predicting prostate cancer. A further prospective study in validating its diagnostic value was needed.
Keywords: Neutrophil-to-lymphocyte ratio, Platelet-to-lymphocyte ratio, Diagnostic, Prostate cancer
Introduction
Prostate cancer (PCa) is the second most common cancer worldwide. It accounts for more than 15% of cancer in men with ongoing rising clinical relevancies. About 70% of them occurs in the developed country [1], [2]. Trans Rectal Ultrasound Guided procedure of prostate biopsy remains the gold standard in most countries in the diagnosis of prostate cancer. Since the biopsy is mostly office procedure and not only uncomfortable but also associated with significant complications, various non-invasive strategies have been invented to prevent unnecessary biopsy [3].
Serum Prostate Specific Antigen (PSA) has been used as the screening standard for patients in suspicion of prostate cancer. PSA value of more than 4 ng/ml has been considered the threshold to biopsy in most countries [1], [2], [4], [5], [6], [7], [8]. But, recent meta-analyses showed a positive predictive value of PSA above 4 ng/ml is only 25% [6]. Besides, the invasive prostate biopsy may still miss some percentage of cancer, given that up to 20% of men will have prostate cancer in a repeated biopsy [9]. Various imaging and bio-molecular marker have been suggested to increase diagnostic accuracy, but none of these methods is available for widespread use, either due to the availability or even high-cost issues [2], [9].
Over the past decades, our study of the microenvironment of cancer has supported Virchow’s hypothesis of the relationship between inflammation and cancer. Inflammatory markers have been associated with more aggressive disease [7], [10]. Study of Cihan et al., in 2013 showed that values of lymphocytes, neutrophils, and white blood cells are significantly lower in PCa patients with statistically significant difference noted in lymphocytes value compared to healthy controls. Their ease of assessment brings the suggestion to use it in combination with other parameters in predicting the diagnosis of prostate cancer [3]. Many follow-up studies had been using neutrophil-to-lymphocyte ratio in fields of predicting diagnosis, prognosis, and recurrence after definitive management [2], [5], [11], [12], [13], [14], [15].
Though small in numbers, previous studies also demonstrated the promising value of platelet-to-lymphocyte (PLR) in prostate cancer. Kaynaret al. found an increased level of PLR in PCa compared with that in benign prostatic hyperplasia (BPH) with PSA value greater than 10 ng/ml [16]. A statistically significant higher PLR in PCa compared to BPH patients was also demonstrated by Yuksel et al., in 2015 [6].
According to our knowledge, there is still no data on the use of NLR and PLR as predictors of PCa in Indonesia. Therefore, this study is conducted to evaluate its pre-biopsy value in predicting PCa.
Material and Methods
Population of Study
This is a diagnostic study with retrospective design. All patients who underwent prostate biopsy in Adam Malik General Hospital between August 2011 and August 2015 were included. Data related to prostate cancer prediction factors were collected, and their relationship with malignant pathology was analysed. The factors included were: age, serum PSA value, and estimated prostate volume (EPV). The routine blood count collected to calculate the NLR and PCR were the recent results right before the biopsy procedure was performed. Histopathology of the biopsy specimen was applied as the gold standard of PCa diagnosis. Patients with irrelevant and incomplete data were excluded from the study.
Variables
Serum PSA was collected from recent laboratory results just before biopsy procedures were performed. We collected EPVs from their initial Trans-Abdominal Ultrasound (TAUS) of the prostate. Prostate was measured in 3-dimensional aspects, and its volume was estimated with the modified ellipsoid formulation in cm3 (0.523 [(length x width x height)]. NLR and PLR value are acquired from the direct division of absolute neutrophil count or platelets count with their absolute lymphocyte count.
Analysis
Input and data analysis was performed using SPSS ver 20.0 software. Data will be divided into two groups according to their histopathology of prostate biopsy, the BPH and PCa group. A pathology of prostatitis will be excluded. Data related to PCa prediction such as routine blood count, NLR, and PLR of each group will be distributed in a frequency table and analysed for their value in predicting biopsy results with bivariate analysis. A p value of < 0.05 (α = 5%) was considered statistically significant. Logistic regression will be performed to multivariate analysed EPV, PSA, NLR, and PLR as predictive factors of prostate biopsy.
Results
Characteristics and Bivariate Analysis
As many as 298 patients consisting of 126 (42.3%) BPH and 172 PCa (57.7%) patients are included in this study. Mean age for both groups are 66.36 ± 7.53 and 67.99 ± 7.48 years old (p = 0.64), respectively. Patients characteristics and laboratory values are shown (Table 1).
Table 1.
Patients Characteristics and Hematologic Parameters
| Parameters | BPH (n = 126) | PCa (n = 172) | p |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| (Median) | (Median) | ||
| Age (years) | 66.36 ± 7.53 | 67.99 ± 7.48 | 0.64* |
| PSA (ng/dL) | 19.28 ± 27.11 | 40.19 ± 49.39 | < 0.0001* |
| EPV (cm3) | 49.39 ± 23.51 | 58.10 ± 30.54 | 0.02* |
| Hb | 12.99 ± 2.00 (13.20) | 12.95 ± 2.01 (13.10) | 0.754** |
| Leucocytes Count (x103/mm3) | 8.67 ± 3.45 (8.11) | 9.19 ± 3.29 (8.46) | 0.1** |
| Absolute Neutrophil Count (x103/mm3) | 6.09 ± 3.19 (5.45) | 7.54 ± 3.64 (6.92) | < 0.0001** |
| Absolute Lymphocyte Count (x103/mm3) | 2.09 ± 0.83 (2.02) | 2.00 ± 0.76 (1.87) | 0.29** |
| Platelets Count (x103/mm3) | 286.16 ± 112.24 (266) | 311.61 ± 120.81 (294) | 0.049** |
| NLR | 3.57 ± 3.23 (2.54) | 4.22 ± 2.59 (3.67) | < 0.0001** |
| PLR | 160.27 ± 98.96 (128.13) | 169.55 ± 78.07 (151.28) | 0.02** |
T-test
Mann-Whitney Test.
Comparing the laboratory results of both groups, there were statistically significant differences noted from PSA (19.28 ± 27.11 vs 40.19 ± 49.39), EPV (49.39 ± 23.51 vs 58.10 ± 30.54), NLR (3.57 ± 3.23 vs 4.22 ± 2.59), and PLR (160.27 ± 98.96 vs 169.55 ± 78.07) in each bivariate analysis.
NLR, PLR, and PSA
We then performed a Receiver Operating Characteristics (ROC) analysis to define the Area Under Curve (AUC) of NLR and PLR in predicting prostate cancer (Figure 1 and Table 2).
Figure 1.

The ROC Curves of NLR, PLR, and PSA
Table 2.
The AUC of NLR, PLR, and PSA
| Parameters | AUC | p |
|---|---|---|
| NLR | 62.8% | < 0.0001 |
| PLR | 57.9% | 0.02 |
| PSA | 68.5% | < 0.0001 |
The NLR cut-off point of 3.08 gives 62.8% AUC with 64.5% sensitivity and 63.5% specificity. The AUC of PLR is 57.9% with a sensitivity of 56.4% and specificity of 55.6% in the cut-off point of 143 (p = 0.02).
Multivariate Analysis
We performed logistic regression between EPV, PSA, PLR, and NLR with results described in Table 2. We used the cut-off value of NLR (3.08) and PLR (143) as retrieved from ROC analysis before to be included as categorical variables in the regression. PLR was excluded from the regression as it was not statistically significant if analysed conjunctively. Thus, the equation leaves NLR as a single most important systemic inflammatory biomarker in predicting prostate cancer (Table 3).
Table 3.
Multivariate Analysis: Logistic Regression
| Variables | OR | 95% CI | p |
|---|---|---|---|
| EPV | 1.012 | 1.002 – 1.022 | 0.21 |
| NLR (≥ 3.08) | 2.856 | 1.734 – 4.702 | < 0.0001 |
| PLR (≥ 143)* | 1.152 | 0.648 – 2.049 | 0.63 |
| PSA | 1.016 | 1.007 – 1.025 | < 0.0001 |
before excluded in Backward: LR method.
NLR, PLR, and IPCRC: A Subgroup Analysis
We asked for permission from the preceding authors of Indonesian Prostate Cancer Risk Calculator (IPCRC) and calculated its value from 98 randomised patients consist of 45 (45.92%) BPH and 53 (54.08%) PCa.
We found a comparable value between NLR and PLR with IPCRC in predicting prostate cancer (AUC of 75.3%, 67.6%, and 68.4%, respectively) with a statistically significant difference was noted between each value (p < 0.05) as shown in Figure 2 and Table 4.
Figure 2.
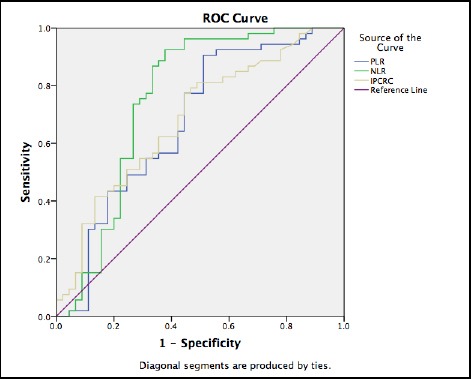
The ROC Curves of PLR and IPCRC Score
Table 4.
The AUC of NLR, PLR, and IPCRC
| Parameters | AUC | p |
|---|---|---|
| NLR | 75.3% | < 0.0001 |
| PLR | 67.6% | 0.003 |
| IPCRC | 68.5% | 0.002 |
Discussion
The body response to cancer parallels with inflammation and wound healings. In 1863, Rudolf Virchow noted leucocytes in neoplastic tissues and suggested a connection between inflammation and cancer. He suggested that the “lymphoreticular infiltrate” reflected the origin of cancer at sites of chronic inflammation. Tumour-infiltrating lymphocytes may contribute to cancer growth and spread, and the immunosuppression associated with malignant disease. In his review in 2001, Balkwill et al., still mention the theory of “Tumours: wounds that do not heal” [10] previously showed by Dvorak in 1986 [10]. This theory showed how wound healing and tumour stroma formation share many important features. Wound healing is usually self-limiting, but tumours secrete a vascular permeability factor, vascular endothelial growth factor (VEGF), that can lead to persistent extravasation of fibrin and fibronectin and continuous generation of the extracellular matrix. Platelets in wounds are a critical source of cytokines, especially transforming growth factor β (TGF-β) and VEGF. Platelet release of such factors may also play an important role in angiogenesis. Also, malignant cells themselves secrete proinflammatory cytokines [10].
Though inflammatory markers such as lymphocytes were mentioned in previous studies, not all markers are incoherent with every cancer. Leucocytes, mainly lymphocytes, is the most prominent marker in many cancers, but not in PCa. Study of Cihan Y, et al. showed that patient with PCa had a lower level of lymphocytes, neutrophils, and a higher level of monocytes with a significant difference in lymphocyte count, compared to healthy controls [3]. McDonald et al., also found that lymphocytes count is significantly lower in patients with elevated PSA compared with patients with PSA below 4 ng/ml [4]. Though this study found that the absolute lymphocyte counts of PCa patients are lower, the difference was not statistically significant compared with a benign group (2.09 ± 0.83 vs 2.00 ± 0.76; p = 0.23).
As supported by previous studies, we calculated the NLR values of both groups and found a significant difference of the value between PCa and BPH groups (4.22 ± 2.59 vs 3.57 ± 3.23; p < 0.0001). Gokce et al., in a larger population, also found the same significant results of the difference between both groups (p = 0.002). McDonald et al., in his study, found a correlation between increasing PSA and NLR value (ORmultiv = 1.14; 95% CI, 1.03-1.26), after adjustment for age, smoking, body mass index, education, race, co-morbidities, and use of medications [4]. These findings are also coherent with the recent study of Oh JJ et al., and Kawahara et al., in 2015 [5], [9].
In this study, though we found a significant difference of platelets count with no statistical difference in lymphocyte count between both groups, the ratio of PLR value gives the event more significant difference (p = 0.02). A similar result of this study also showed by Yuksel et al., where a significant intergroup statistical difference was found for PLR (p = 0.041) but not for lymphocyte count (p > 0.05) [6]. This also supported by the study of Li et al., who found a statistical difference of PLR value in PCa and normal/BPH patient (p < 0.05).
Our multivariate analysis revealed that not only EPV and PSA, but NLR was also an independent biomarker in predicting prostate biopsy (OR 2.856; 95%CI 1.734 – 4.702). PLR was excluded in the analysis as it is not significant statistically in the concurrent analysis. Same results were stated in Kawahara et al. who found that not only free to total PSA ratio (HR = 3.13) but also NLR (HR = 2.21) was an independent risk factor for prostate cancer [5]. In another study of Oh JJ et al., in their multivariate analyses, a higher NLR was significantly associated with prostate cancer detection after adjusting for other factors (OR = 1.372, p = 0.038). An increased accuracy noted from 0.712 to 0.725 in the addition of NLR (p = 0.005) in the multivariate model for prostate cancer detection [9]. Thus, we can conclude that NLR is increasing in prostate cancer.
IPCRC has been widely used in Indonesia as a clinical calculator to predict the diagnosis of PCa. In a subgroup analysis, we compared the NLR and PLR value with IPCRC and analysed their AUC with ROC analysis and found a comparable result of NLR with IPCRC. NLR surprisingly has a comparable AUC with IPCRC (75.3% vs 68.5%). From these findings, we can conclude that further validation is mandatory. Increasing NLR can be part of the calculation in predicting prostate cancer.
In conclusion, NLR is thus likely elevated in patients with prostate cancer. Accordingly, NLR, with or without combination with PSA, may function as a new systemic inflammatory biomarker in predicting prostate biopsy results. To be applied as routine testing and to selectively decide candidates for prostate biopsy in a patient with PSA value more than 4 ng/ml, further prospective trial and validation is mandatory.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.GLOBOCAN. Prostate Cancer:Estimated Incidence, Mortality, and Prevalence Worldwide in 2012. IARC; 2012. [Google Scholar]
- 2.Gokce MI, Hamidi N, Suer E, Tangal S, Huseynov A, Ibis A. Evaluation of neutrophil-to-lymphocyte ratio prior to prostate biopsy to predict biopsy histology:Results of 1836 patients. Canadian Urological Association journal =Journal de l'Association des urologues du Canada. 2015;9(11-12):E761–5. doi: 10.5489/cuaj.3091. https://doi.org/10.5489/cuaj.3091 PMid:26600880 PMCid:PMC4639422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cihan YB, Arslan A, Ergul MA. Subtypes of white blood cells in patients with prostate cancer or benign prostatic hyperplasia and healthy individuals. Asian Pacific journal of cancer prevention:APJCP. 2013;14(8):4779–83. doi: 10.7314/apjcp.2013.14.8.4779. https://doi.org/10.7314/APJCP.2013.14.8.4779 PMid:24083743. [DOI] [PubMed] [Google Scholar]
- 4.McDonald AC, Vira MA, Vidal AC, Gan W, Freedland SJ, Taioli E. Association between systemic inflammatory markers and serum prostate-specific antigen in men without prostatic disease - the 2001-2008 National Health and Nutrition Examination Survey. The Prostate. 2014;74(5):561–7. doi: 10.1002/pros.22782. https://doi.org/10.1002/pros.22782 PMid:24435840 PMCid:PMC4380881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawahara T, Fukui S, Sakamaki K, Ito Y, Ito H, Kobayashi N, et al. Neutrophil-to-lymphocyte ratio predicts prostatic carcinoma in men undergoing needle biopsy. Oncotarget. 2015;6(31):32169–76. doi: 10.18632/oncotarget.5081. https://doi.org/10.18632/oncotarget.5081 PMid:26359354 PMCid:PMC4741667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuksel OH, Urkmez A, Akan S, Yldirim C, Verit A. Predictive Value of the Platelet-To-Lymphocyte Ratio in Diagnosis of Prostate Cancer. Asian Pacific journal of cancer prevention:APJCP. 2015;16(15):6407–12. doi: 10.7314/apjcp.2015.16.15.6407. https://doi.org/10.7314/APJCP.2015.16.15.6407 PMid:26434851. [DOI] [PubMed] [Google Scholar]
- 7.Sidaway P. Prostate cancer:Platelet-to-lymphocyte ratio predicts prostate cancer prognosis. Nature reviews Urology. 2015;12(5):238. doi: 10.1038/nrurol.2015.69. https://doi.org/10.1038/nrurol.2015.69 PMid:25823375. [DOI] [PubMed] [Google Scholar]
- 8.Li F, Hu H, Gu S, Chen X, Sun Q. Platelet to lymphocyte ratio plays an important role in prostate cancer's diagnosis and prognosis. International journal of clinical and experimental medicine. 2015;8(7):11746–51. [PMC free article] [PubMed] [Google Scholar]
- 9.Oh JJ, Kwon O, Lee JK, Byun SS, Lee SE, Lee S, et al. Association of the neutrophil-to-lymphocyte ratio and prostate cancer detection rates in patients via contemporary multi-core prostate biopsy. Asian Journal of Andrology. 2015 doi: 10.4103/1008-682X.164198. https://doi.org/10.4103/1008-682X.164198 PMid:26470836 PMCid:PMC5109892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balkwill F, Mantovani A. Inflammation and cancer:back to Virchow? Lancet (London, England) 2001;357(9255):539–45. doi: 10.1016/S0140-6736(00)04046-0. https://doi.org/10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 11.Gazel E, Tastemur S, Acikgoz O, Yigman M, Olcucuoglu E, Camtosun A, et al. Importance of neutrophil/lymphocyte ratio in prediction of PSA recurrence after radical prostatectomy. Asian Pacific journal of cancer prevention:APJCP. 2015;16(5):1813–6. doi: 10.7314/apjcp.2015.16.5.1813. https://doi.org/10.7314/APJCP.2015.16.5.1813 PMid:25773829. [DOI] [PubMed] [Google Scholar]
- 12.Kwon YS, Han CS, Yu JW, Kim S, Modi P, Davis R, et al. Neutrophil and Lymphocyte Counts as Clinical Markers for Stratifying Low-Risk Prostate Cancer. Clinical genitourinary cancer. 2016;14(1):e1–e8. doi: 10.1016/j.clgc.2015.07.018. https://doi.org/10.1016/j.clgc.2015.07.018 PMid:26341038 PMCid:PMC5767465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee H, Jeong SJ, Hong SK, Byun SS, Lee SE, Oh JJ. High preoperative neutrophil-lymphocyte ratio predicts biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. World journal of urology. 2015 doi: 10.1007/s00345-015-1701-6. https://doi.org/10.1007/s00345-015-1701-6 PMid:26449784. [DOI] [PubMed] [Google Scholar]
- 14.Maeda Y, Kawahara T, Kumano Y, Ohtaka M, Kondo T, Mochizuki T, et al. The Neutrophil-to-Lymphocyte Ratio before Repeat Prostate Needle Biopsy for Predicting Prostate Cancer. Urologia internationalis. 2015 doi: 10.1159/000442895. https://doi.org/10.1159/000442895 PMid:26669562. [DOI] [PubMed] [Google Scholar]
- 15.Zhang GM, Zhu Y, Ma XC, Qin XJ, Wan FN, Dai B, et al. Pretreatment Neutrophil-to-Lymphocyte Ratio:A Predictor of Advanced Prostate Cancer and Biochemical Recurrence in Patients Receiving Radical Prostatectomy. Medicine. 2015;94(41):e1473. doi: 10.1097/MD.0000000000001473. https://doi.org/10.1097/MD.0000000000001473 PMid:26469891 PMCid:PMC4616804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaynar M, Yildirim ME, Gul M, Kilic O, Ceylan K, Goktas S. Benign prostatic hyperplasia and prostate cancer differentiation via platelet to lymphocyte ratio. Cancer biomarkers :section A of Disease markers. 2015;15(3):317–23. doi: 10.3233/CBM-150458. https://doi.org/10.3233/CBM-150458 PMid:25586096. [DOI] [PubMed] [Google Scholar]


