Abstract
This study aimed (1) to estimate the impact of an incremental reduction in excess readmissions on a hospital’s Medicare reimbursement revenue, for hospitals subject to penalties under the Medicare’s Hospital Readmissions Reduction Program and (2) to evaluate the economic case for an investment in a readmission reduction program. For 2,465 hospitals with excess readmissions in the Fiscal Year 2016 Hospital Compare data set, we (1) used the Hospital Readmissions Reduction Program statute to estimate hospital-specific Medicare reimbursement gains per an avoided readmission and (2) carried out a pro forma analysis of investment in a broad-scale readmission reduction program under conservative assumptions regarding program effectiveness and using program costs from earlier studies. For an average hospital, avoiding one excess readmission would result in reimbursement gains of $10,000 to $58,000 for Medicare discharges. The economic case for investments in a readmission reduction effort was strong overall, with the possible exception of hospitals with low excess readmissions.
INTRODUCTION
Medicare’s Hospital Readmissions Reduction Program (HRRP), introduced under the Affordable Care Act and implemented in Fiscal Year (FY) 2013, penalizes hospitals with excess 30-day unplanned readmissions for five applicable conditions - acute myocardial infarction (AMI), heart failure (HF), chronic obstructive pulmonary disease (COPD), pneumonia (PN), and total knee and hip arthroplasty (THA/TKA). Each year, approximately three-quarters of all eligible hospitals are penalized for below-average performance in any of the five applicable conditions. A total of $420 million in HRRP reimbursement penalties was withheld by Medicare in FY 2016 alone, with an average hospital penalty of approximately $160,000, or three-year penalty of close to $0.5 million for an average hospital (MedPAC, 2014). While the program has been credited for a recent nationwide decrease in readmissions for the applicable conditions since the start of the program in FY 2013 (Mellor, Daly, & Smith, 2016; Zuckerman, Sheingold, Orav, Ruhter, & Epstein, 2016), experts have expressed concerns about whether the expected revenue gains from avoiding readmissions are large enough to entice hospitals to invest in further readmission reduction efforts (Axon & Williams, 2011; Berenson, Paulus, & Kalman, 2012; Joynt & Jha, 2013b; van Walraven, Bennett, Jennings, Austin, & Forster, 2011).
Critics of HRRP worry that the cost of readmission prevention, which can involve a substantial financial resource investment (Axon & Williams, 2011; Chollett, Barrett, & Lake, 2011), might discourage readmission prevention efforts by hospitals—meaning hospitals would accept the HRRP penalty rather than engage in readmission prevention efforts. While penalty savings resulting from improved readmission performance may cover all of these costs, it is not clear if that is in fact the case for all hospitals.
The goal of this study was to examine the FY 2016 financial incentives to avoid readmissions under the HRRP for hospitals with readmissions above the risk-adjusted national average on any of the applicable conditions. This study aimed to (1) estimate the expected impact of an incremental reduction in excess readmissions on a hospital’s Medicare reimbursement revenue, and (2) to evaluate the economic case for readmission reduction efforts.
New Contribution
To our knowledge, this is the first study to estimate financial gains that hospitals could expect to accrue if they engage in further readmission avoidance efforts. Our approach is conceptually different from an empirical examination of hospitals’ observed penalty data and readmission performance improvement under the HRRP program (as it has, for example, been reported in (Joynt & Jha, 2013a; Zuckerman et al., 2016)). Shedding light on the financial incentive structure underlying the HRRP is important because uncertainty regarding future payoff from today’s readmission reduction efforts can curtail investment in readmission reduction programs. Additionally, observed readmissions performance and outcomes are subject to selection bias (hospitals that choose to engage in readmission reduction efforts might also be the ones that expect to earn higher financial returns compared to an average hospital), thus potentially overstating financial returns from readmission avoidance.
Our study provides hospitals with an improved understanding of whether further readmission reduction efforts are worth the financial investment they require, and if so whether a broad-scale readmission reduction program could be a viable alternative to risk-prediction and targeted prioritization of high-risk patients. The study also informs Medicare policy whether the HRRP penalties are strong enough to continue to elicit further readmission reduction efforts; or alternatively, whether the incentive structure might need to be tightened to better align hospital revenue-seeking behavior with the socially desirable goal of reducing excess readmissions.
HRRP penalty overview
A hospital’s readmission performance for each of the applicable conditions is determined by the Excess Readmissions Ratio (EXRR). The EXRR is a condition-specific ratio of a hospital’s adjusted number of readmissions for an applicable condition during a prior 3-year performance measurement period (e.g., FY 2012–2014 for the FY 2016 penalty year), called “predicted readmissions”, divided by the risk-adjusted nationwide average performance for that condition over the same period, called “expected readmissions,” where adjustment accounts for variation in patient characteristics and hospital size. Hospitals with more predicted readmissions than expected readmissions (EXRR >1) for any of the applicable conditions are penalized, with the penalty adjustment being applied to each of a hospital’s Medicare discharges in a penalty year. The program does not reward above-average performance (EXRR ≤ 1). Because a hospital’s penalty in any penalty year is assessed based on the hospital’s performance over a prior 3-year measurement period, an avoided readmission in any given year during the measurement period can impact the hospital’s HRRP penalty over a course of a three-year period.
Readmission reduction programs overview
Readmission reduction programs typically include a multi-faceted approach aimed at enhancing the discharge-to-home transition process (transitional care, enhanced discharge, educational interventions, and medication reconciliation activities) (Hansen, Young, Hinami, Leung, & Williams, 2011; Hesselink et al., 2012) (Peikes, Chen, Schore, & Brown, 2009). Some of the widely used readmission prevention interventions are designed to include all patients (i.e., Project RED, (Jack et al., 2009)); while others target a pre-defined category of “high-risk” patients—those with recent hospitalization, multiple chronic conditions, or poor self-health ratings (the Transitional Care Model (TCM), (Naylor et al., 1999)) or those identified as high risk using a proprietary screening tool on hospital admission (Project BOOST, (Hansen et al., 2013)). Existing evidence for efficacy of readmission prevention illustrates an overall 20–30% reduction in readmissions (Coleman, Parry, Chalmers, & Min, 2006; Hansen et al., 2013; Jack et al., 2009; Naylor et al., 1999; Peikes et al., 2009; Tilson & Hoffman, 2012). There is little evidence regarding potential variation on program effectiveness across specific conditions.
Readmission reduction programs have been estimated to cost in the range of $130-$325 per patient discharge (Coleman et al., 2006; Hansen et al., 2013; Jack et al., 2009; Naylor et al., 1999; Peikes et al., 2009). The higher end of the per-discharge cost estimates was reported by programs that include follow-up home visits during the post-discharge period (such as the TCM), and the lower estimates were reported when transition coordination and medication reconciliation were provided by phone (such as Project RED). The studies report only “minimal” upfront capital costs associated with these interventions, possibly limited to the opportunity cost of funds diverted to labor ((Chollett et al., 2011), page 27).
METHODS
Data
We used data from the FY 2016 Medicare Final Rule Impact File, FY 2016 Inpatient Prospective Payment System (IPPS) Final Rule Readmissions Supplemental Data File, FY 2016 Tables 2 and 3 Final Rule and Correction Notice (Wage Index Tables) (CMS, 2017), and FY 2016 Medicare’s Hospital Compare database (CMS, 2016b). The Impact File contains hospital characteristics (e.g., bed size) and Medicare add-on payments (e.g., empirical Disproportional Share Hospital (DSH) adjustment, case mix index). The IPPS Data File contains condition-specific payment adjustments (used to calculate the DRG weights). The Final Rule Tables contain hospitals’ wage-index adjusted base operating payments. The Hospital Compare database has condition-specific information about HRRP performance data for FY 2016 (number of discharges, actual, predicted, and expected readmissions, and the EXRR).
Table 2.
Condition-specific Medicare reimbursement revenue gains from preventing one readmission.
| AMI (N=937) |
HF (N=1,409) |
COPD (N=1,356) |
PN (N=1,409) |
THA/TKA (N=718) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Panel 1: HRRP penalty saved from preventing a readmission (1) | ||||||||||
| Mean | 18769.46 | 10627.52 | 9742.24 | 11585.54 | 60369.57 | |||||
| 95%CI | 18280.98 | 19257.95 | 10437.88 | 10817.16 | 9534.52 | 9949.97 | 11338.22 | 11832.85 | 58456.52 | 62282.61 |
| IQ range | 14781.02 | 24214.69 | 10461.27 | 12575.44 | 7614.69 | 12213.8 | 9423.17 | 14472.95 | 51571.91 | 78079.11 |
| Panel 2: Medicare reimbursement revenue foregone on a prevented readmission (2) | ||||||||||
| Mean | 2017.45 | 1329.90 | 1220.343 | 1274.94 | 2121.77 | |||||
| 95%CI | 1990.59 | 2044.32 | 1312.66 | 1347.14 | 1204.75 | 1235.93 | 1259.23 | 1290.66 | 2092.06 | 2151.47 |
| IQ range | 1729.42 | 2169.83 | 1127.20 | 1412.18 | 1042.60 | 1293.36 | 1092.13 | 1345.09 | 1873.99 | 2220.41 |
| Panel 3: Net reimbursement revenue gain per an avoided readmission (3) | ||||||||||
| Mean | 16752.01 | 9297.61 | 8521.90 | 10310.59 | 58247.80 | |||||
| 95%CI | 16266.57 | 17237.44 | 9109.98 | 9485.24 | 8315.26 | 8728.54 | 10063.79 | 10557.39 | 56338.5 | 60157.10 |
| IQ range | 12826.52 | 22219.24 | 9192.18 | 11271.02 | 6395.39 | 11036.73 | 8199.10 | 13288.38 | 49635.87 | 75891.53 |
| n/N (%) (4) | 934/937 (99.7) | 1375/1409 (97.6) | 1327/1356 (97.9) | 1397/1409 (99.1) | 718/718 (100.0) | |||||
| Mean | 117,730.8 | 57,012.33 | 33,680.03 | 44,366.68 | 301,941.8 | |||||
| 95%CI | 20320.74 21249.02 | 48794.75 65229.92 | 27412.27 39947.78 | 38521.00 50212.36 | 274941.7 328942.00 | |||||
| IQ Range | 19,124.47 24,236.5 | 48120.32 71,156.28 | 27,189.23 42,458.36 | 36,458.90 55,458.26 | 461,125.9 350,488.9 | |||||
| n/N (%) | 794/937 (77.3) | 950/1409 (67.4) | 853/1356 (62.9) | 927/1409 (65.8) | 570/718 (79.4) | |||||
The table presents estimates of the means, 95%CIs, and (IQ) interquartile ranges for HRRP penalty savings (Panel 1), forgone reimbursement revenue on prevented re-hospitalization (Panel 2), and the resulting net revenue gains (Panel 3), expected from avoiding one readmission for an HRRP applicable condition, for an average hospital with excess readmissions for that applicable condition.
Notes:
HRRP penalty saved from preventing a readmission (Panel 1): The dollar amount of reimbursement revenue gained from HRRP penalty reduction was calculated using formula (10) in Digital Supplement A. The dollar amount of penalty saved is determined by the impact of an avoided excess readmission on the hospital’s payment for excess readmissions; it accounts for a simultaneous offsetting reduction in the volume of Medicare discharges. See Digital Supplement B Table B.1 for the respective dollar amounts attributable to each of these sources.
Medicare reimbursement revenue foregone on a prevented readmission (Panel 2): Loss of Medicare reimbursement revenue on the avoided readmission was calculated as a hospital’s base operating DRG payment (BOP), minus the direct costs (DC) of hospitalization. Data on hospital costs are not publically available and were imputed here by, first, using a Medicare revenue mark-up of −5% to impute total hospital cost (direct plus indirect) as [BOP / 0.95], and then and assuming that the direct cost represent 80% of the total cost of hospitalization [0.8 × BOP / 0.95]. The loss of revenue was therefore imputed as [BOP – 0.8 × BOP / 0.95]. See Digital Supplement A for more detail.
Net reimbursement revenue gain per an avoided readmission (Panel 3): The total effect of avoiding one readmission on Medicare reimbursement revenue was calculated as revenue gained from readmission avoidance through HRRP penalty savings (Panel 1) minus loss of reimbursement revenue for the avoided readmission (Panel 2).
This row shows the number of hospitals with a positive revenue gain (n) from avoiding a readmission for an applicable condition, as the percentage of all hospitals with excess readmissions (N) for that applicable condition.
The table presents results of a pro forma analysis of expected net earnings from each of the applicable conditions, following a hypothetical readmission-reduction intervention, under four permutations of assumptions regarding the effectiveness and costs of the intervention. Shown are the means, 95% CIs and interquartile (IQ) ranges of the expected net earnings on Medicare discharges for each condition, and the number and percent of hospitals that are expected to see positive net earnings for that condition. Numbers in red represent negative net earnings (the cost of the intervention is expected to exceed the projected Medicare reimbursement revenue gain).
Table 3.
Condition-specific expected net earnings (Medicare reimbursement revenue gains net of program costs) from an investment in a readmission reduction program, by applicable condition.
| AMI (n=937) |
HF (n=1,409) |
COPD (n=1,356) |
PN (n=1,409) |
THA/TKA (n=718) |
|
|---|---|---|---|---|---|
| Panel 1: Expected readmission
reduction = 5%; Expected intervention cost = $130 per-discharge | |||||
| Mean | 82,427.02 | 64,325.07 | 42807.83 | 47130.07 | 183566.3 |
| 95%CI | 76,227.78 88,626.26 | 59,604.31 69,045.8 | 39,335.77 46,279.88 | 43,822.46 50,437.67 | 169,490.8 197,641.7 |
| IQ Range | 82,13.45 121,356.12 | 60,457.32 90,004.5 | 36,549.56 71,450.56 | 45,482.12 62,145.36 | 169,458.3 230,456.3 |
| n/N (%) | 779/937 (83.1) | 1140/1409 / (80.9) | 1018/1356 (75.1) | 1070/1409 (75.9) | 606/718 (84.4) |
|
Panel 2: Expected
readmission reduction = 5%;
Expected intervention cost = $325 per-discharge | |||||
| Mean | 25,560.28 | −28,496.73 | −35,793.14 | −27,369.07 | 88,137.39 |
| 95%CI | 21,214.21 29,906.34 | −31,955.3 −25,038.09 | −38,553.1 −33,033.17 | −29,791.26 −24,946.88 | 77,523.07 98,751.71 |
| IQ Range | 21,023.83 32,189.23 | −30,145.25 −10,561.78 | −32,145.39 −23,128.96 | −30,458.36 −25,458.23 | 78,567.91 110,236.96 |
| n/N (%) | 670/937 (71.5) | 303/1409 (21.5) | 125/1356 (9.2) | 215/1409 (15.3) | 549/718 (76.5) |
|
Panel 3: Expected
readmission reduction = 10%; Expected intervention cost = $130 per-discharge | |||||
| Mean | 174,597.6 | 149,834.1 | 112,281 | 118,865.8 | 397,370.7 |
| 95%CI | 19,844.04 20,742.51 | 139,388.9 160,279.3 | 104,325.5 120,236.5 | 111,605 126,126.6 | 366,836.6 427,904.8 |
| IQ Range | 19,568.21 28,125.42 | 130,458.3 175,128.2 | 105,563.1 128,236.9 | 111,230.2 139,123.2 | 360,428.2 450,254.5 |
| n/N (%) | 800/937 (85.3) | 1165/1409 (82.7) | 1071/1356 (79.0) | 1133/1409 (80.4) | 644/718 (89.7) |
|
Panel 4: Expected
readmission reduction =10%;
Expected intervention cost = $325 per-discharge | |||||
| Mean | 117,730.8 | 57,012.33 | 33,680.03 | 44,366.68 | 301,941.8 |
| 95%CI | 20320.74 21249.02 | 48794.75 65229.92 | 27412.27 39947.78 | 38521.00 50212.36 | 274941.7 328942.00 |
| IQ Range | 19,124.47 24,236.5 | 48120.32 71,156.28 | 27,189.23 42,458.36 | 36,458.90 55,458.26 | 461,125.9 350,488.9 |
| n/N (%) | 794/937 (77.3) | 950/1409 (67.4) | 853/1356 (62.9) | 927/1409 (65.8) | 570/718 (79.4) |
The table presents results of a pro forma analysis of expected net earnings from each of the applicable conditions, following a hypothetical readmission-reduction intervention, under four permutations of assumptions regarding the effectiveness and costs of the intervention. Shown are the means, 95% CIs and interquartile (IQ) ranges of the expected net earnings on Medicare discharges for each condition, and the number and percent of hospitals that are expected to see positive net earnings for that condition. Numbers in red represent negative net earnings (the cost of the intervention is expected to exceed the projected Medicare reimbursement revenue gain).
Sample
We included all 2,941 hospitals in the FY 2016 Medicare Impact File and Hospital Compare database and then excluded 476 hospitals that did not have excess readmissions for any of the five applicable HRRP conditions. Among the 2,465 remaining hospitals with excess readmissions for at least one of the applicable conditions, 937 had excess readmissions for AMI, 1,409 had excess readmissions for HF, 1,356 had excess readmissions for COPD, 1,409 had excess readmissions for PN, and 718 had excess readmissions for THA/TKA. Most hospitals had excess readmissions for two or more applicable conditions.
Analysis Methods
Computations for Aim 1.
For each of the applicable conditions for which a hospital had excess readmissions (EXRR>1), condition-specific Medicare reimbursement revenue gains were calculated per one avoided readmission for that condition as the difference of two terms: (a) HRRP penalty savings resulting from an avoided readmission, and (b) Medicare reimbursement revenue foregone due to the avoided readmission.
(a) HRRP penalty savings resulting from an avoided readmission: Because the HRRP statute prescribes an exact method for penalty computation based on a known and observable set of hospital characteristics and performance measures, we used analytical differential calculus methods (in contrast to an empirical approach like regression analysis) to predict HRRP penalty savings for each individual hospital based on a hospital’s own observed data. Knowing the underlying non-stochastic data-generating process for the penalty amount allowed us to perform near-exact analytical computations of the incremental penalty reduction per one avoided readmission for AMI, HF, COPD, and THA/TKA, for each hospital in our sample.
To accomplish this, we represented the HRRP’s statutory process for determination of a hospital’s aggregate HRRP penalty across all Medicare discharges as a mathematical function of condition-specific numbers of readmissions, index discharge volumes, numbers of predicted and expected readmissions, and the wage index-adjusted Medicare base operating DRG payment amounts (we did not include add-on payments in this calculation because the penalty applies only to the base operating DRG payment). We then carried out a first-order differential calculus exercise of this penalty function, taking separate condition-specific first-order derivatives with respect to the number of readmissions for each of the five applicable conditions. These condition-specific first-order derivatives represent the incremental change in a hospital’s annual penalty amount for a one-readmission change in the hospital’s readmissions for the respective applicable condition during the 3-year performance measurement period. (Digital Supplement A provides a detailed explanation and full analytical derivations.) Because an avoided readmission is included in the EXRR assessment for a three-year period, we then calculated condition-specific present values of a three-year stream of future penalty savings, discounted at an annual 4.5% discount rate based on the FY 2016 treasury interest rate (2.3%) and inflation rate (2.2%) (BLS 2017; U.S. Treasury 2016).
(b) Medicare reimbursement revenue foregone on an avoided readmission: avoiding a readmission would result in forfeiting the Medicare payment for the avoided hospitalization, while also saving the costs of direct patient care resources (clinician labor, supplies) that would have been used up in caring for the patient had the patient been readmitted. To compute the Medicare payment per discharge for each of the applicable conditions, we used the Medicare base operating payment (from the Final Rule Tables), and multiplied it by the corresponding condition-specific DRG weight (ratio of sum of transfer adjusted DRG relative weights to the number of transfer-adjusted cases). Because Medicare reimbursement also includes supplemental payments (CMS, 2016a), we then multiplied this DRG waged-adjusted base operating payment by the VBP adjustment and then by the sum of hospital-specific Medicare supplemental payment adjustments (empirical DSH, Indirect Medical Education, and low-volume adjustments) and added the uncompensated DSH payment amount (from the Impact File). Because we did not have any hospitalization cost data, we estimated the per discharge cost of hospitalization in relation to the condition- and hospital-specific Medicare payment amount and assuming a patient revenue markup of –5% (MedPAC, 2014). Then, to obtain per-discharge direct patient care costs, we assumed an 80/20 direct-to-indirect cost breakdown (MedPAC, 2016) and subtracted 20% from the estimated per-discharge cost to account for the hospital’s indirect costs (administrative overhead, utilities, depreciation, etc.) incurred regardless of the number of discharges. Finally, the amount of Medicare reimbursement revenue foregone on an avoided readmission for each hospital was calculated by applicable condition as the condition-specific Medicare payment per-discharge, minus the estimated condition-specific direct patient care cost per-discharge, using hospital’s own data. (Digital Supplement A provides a detailed explanation and justification of this approach.)
Computations for Aim 2
To examine a hospital’s economic case for investing in a broad-scale readmission reduction program, we conducted a pro forma net earnings analysis (also known as ex ante cost-benefit analysis) of a hypothetical year-long implementation of a readmission reduction intervention. A broad-scale implementation assumed targeting all patients hospitalized for any of the HRRP applicable condition, regardless of whether or not a hospital had excess readmissions for all conditions. A pro forma analysis assesses the expected financial gain from a project (e.g. expected aggregate Medicare reimbursement revenue gains from an expected reduction readmissions during the implementation year), relative to the expected cost of the project (expected annual cost of the intervention); it is used to assist in decision-making by appraising the costs and benefits of a project that is currently under consideration, but has not yet begun. An economic case for investing in a broad-scale readmission reduction effort condition is supported if the expected net earnings (expected Medicare revenue gain minus expected implementation cost) is positive.
The expected condition-specific Medicare revenue gain from a readmission-reduction intervention was calculated for each hospital by scaling up the condition-specific per-readmission revenue gains from Aim 1 to the expected number of avoided readmissions for that condition at the hospital, assuming a 5% and a 10% reduction in readmission rates following implementation. Although these effect sizes are smaller than the 20–30% reduction in readmissions reported in earlier studies, we chose to be conservative for two reasons—first, derivative calculus methods can be inaccurate in predicting effects of large changes in the independent variable (readmissions) for non-linear functional forms; and second, the earlier studies were published prior to the recently observed nationwide reduction in readmissions, suggesting that incremental effectiveness of readmission reduction efforts at this point in time might be diminished. Using the conservative assumptions of 5% and 10% reductions in readmissions, we computed the corresponding numbers of avoided excess readmissions for each of the applicable conditions, based on each hospital’s own data, and multiplied it by the hospital’s condition-specific Medicare revenue gain per an avoided readmission (penalty saved net of foregone reimbursement from Aim 1), to obtain the amount of Medicare revenue gain from avoiding multiple readmissions for each condition at each hospital.
To compute the cost of a readmission reduction intervention, we used the low ($130) and the high ($325) ends of the per-discharge cost estimates range reported in earlier studies, multiplied by the hospital’s annual discharge volume for each applicable condition. Because the earlier studies report only “minimal” upfront capital costs associated with these interventions, we used the reported program costs as the direct costs of additional clinician labor per-discharge. We did not replicate specific components of the existing transition coordination programs (for example, whether or not the intervention was targeted to specific types of patients, like the CTI, or to all patients, like Project RED). Instead, use chose the more conservative approach by using the cost estimates as a guide for “high” and “low” per-discharge cost for a non-specific broad-scale readmission reduction intervention for all patients.
For each hospital, condition-specific net earning amounts were then computed under each of the four permutations of the assumptions regarding the program effectiveness and per-discharge costs (5%/10% effectiveness × $130/$325 cost). The condition-specific expected net earnings amounts were computed as the difference between the corresponding condition-specific Medicare revenue gain amounts and the program cost amounts. We then computed overall expected net earnings for each hospital, by adding the condition-specific expected net earnings estimates over all five applicable conditions, under the four permutations of effectiveness and cost assumptions. Hospital-level aggregate net earnings were computed across all conditions, by using condition-specific net earnings estimates (from Table 3) for conditions with excess readmissions. For conditions without excess readmissions (for which no HRRP penalty savings from further readmission avoidance can be expected) we only included revenue losses from foregone readmissions and per-discharge intervention costs.
Statistical Analyses
First, we computed descriptive statistics (sample means and ranges) of hospital characteristics (Medicare index discharge volume, number of Medicare readmissions, rates of actual, predicted, and expected readmissions, excess readmission ratio, wage index-adjusted Medicare base operating DRG payment, and Medicare supplemental payments) for the five condition-specific hospital samples (AMI, HF, COPD, PN, THA/TKA) (Table 1).
Table 1.
Condition-Specific Readmissions performance measures and Medicare payment amounts for hospitals with excess readmissions (EXRR>1) from the FY 2016 Hospital Compare Data, N=2,465.
| AMI (N=937) |
HF (N=1,409) |
COPD (N=1,356) |
PN (N=1,409) |
THA/TKA (N=718) |
|
|---|---|---|---|---|---|
| Number of index discharges | |||||
| Mean Range |
244.2 30 1,477 |
382.0 40 3,489 |
328.7 38 2,673 |
320.14 28 2,306 |
461.18 54 2,869 |
| Number of readmissions | |||||
| Mean Range |
47.4 11 279 |
94.1 11 875 |
74.4 11 600 |
61.90 11 402 |
28.19 11 165 |
| Readmission rate, % (1) | |||||
| Mean Range |
20.9 13.4 42.1 |
25.0 18.7 43.9 |
22.7 16.3 36.2 |
19.56 12.9 39.3 |
6.70 4.2 20.7 |
| Predicted readmission rate, % | |||||
| Mean Range |
18.5 13.3 27.9 |
23.3 18.4 33.5 |
21.0 15.5 30.3 |
17.92 12.4 25.9 |
5.77 4.1 9.3 |
| Expected readmission rate, % | |||||
| Mean Range |
17.4 12.6 26.3 |
21.8 17.9 26.8 |
19.9 15.3 25.1 |
16.93 12.1 22.8 |
5.02 3.9 7.5 |
| Excess readmissions ratio | |||||
| Mean Range |
1.06 1.00 1.25 |
1.07 1.00 1.45 |
1.06 1.00 1.32 |
1.06 1.00 1.27 |
1.15 1.00 1.83 |
| Base operating Medicare DRG payment, $ (2) | |||||
| Mean Range |
10,725 9,334 14,186 |
6,801 5,953 9,908 |
6,261 5,480 5,521 |
6,551 5,764 9,594 |
11,665 10,282 15,626 |
| Supplemental Medicare payment, $ (2) | |||||
| Mean Range |
1,848 −135 17,154 |
1,493 −158 19,340 |
1,357 −61.13 14,522 |
1,399 −83 14,768 |
1,442 −144 12,006 |
Notes:
The readmission rate was computed by the authors as the ratio of the number of readmissions to the number of index discharges. Source: https://www.medicare.gov/hospitalcompare/readmission-reduction-program.html.
Rounded to a whole number.
For Aim 1, we calculated condition-specific sample means and 95% confidence intervals (CIs) for (a) the Medicare reimbursement revenue gained from HRRP penalty reduction, (b) Medicare reimbursement revenue foregone on the prevented readmission, and the total Medicare reimbursement revenue gain (a minus b) from an avoided readmission (Table 2). Condition-specific CIs depended on several sources of variation: the hospital’s number of index discharges, actual, predicted, and expected readmissions, the hospital’s total volume of index discharges and readmissions across all applicable conditions, and the hospitals condition-specific Medicare payments.
For Aim 2, we first computed condition-specific expected net earnings means and 95% CIs from a hypothetical intervention under the four permutations of assumptions regarding intervention effectiveness and costs, for all hospitals with excess readmissions for the specific applicable condition; we also calculated the proportion of these hospitals expected to have positive net earnings for that condition (Table 3). We then stratified the sample into 4 subgroups by the number of applicable conditions for which hospitals had excess readmissions—one (n=732), two (n=686) , three (n=583), and four or more (n=464)—and computed overall hospital-level net earnings means and 95% CI (Figure 1) and the proportion of hospitals with positive expected net earnings within each subgroup (Figure 2).
Figure 1. Hospital-level average expected net earnings (Medicare reimbursement revenue gain net of program costs) from an investment in a broad-scale readmission reduction program, by the number of conditions with EXRR>1.
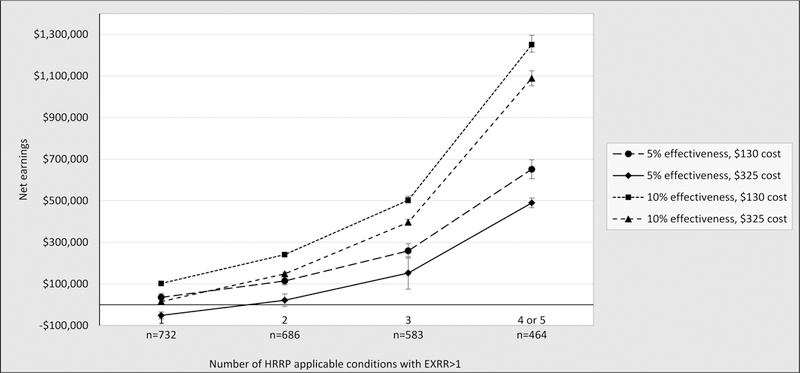
Broad-scale implementation assumes targeting all patients hospitalized for any of the HRRP applicable condition, regardless of whether or not a hospital has excess readmissions for all conditions. The numbers are computed across all conditions, by using condition-specific net earnings estimates from Table 3 for conditions with excess readmissions, and only revenue losses from forgone readmissions and intervention costs for conditions without excess readmissions for which no HRRP penalty savings from further readmission avoidance can be expected. As in Table 3, four permutations of assumptions regarding the effectiveness and costs of the intervention are used. We display the means and 95% CIs of the expected net earnings from a broad-scale readmission reduction intervention. Points located below the x-axis represent negative expected net earnings (the cost of the intervention is expected to exceed the projected overall Medicare reimbursement revenue gain).
Figure 2. Proportion of hospitals with expected net earnings (Medicare reimbursement revenue gain net of program costs) from an investment in a broad-scale readmission reduction program, by the number of applicable conditions with EXRR>1.
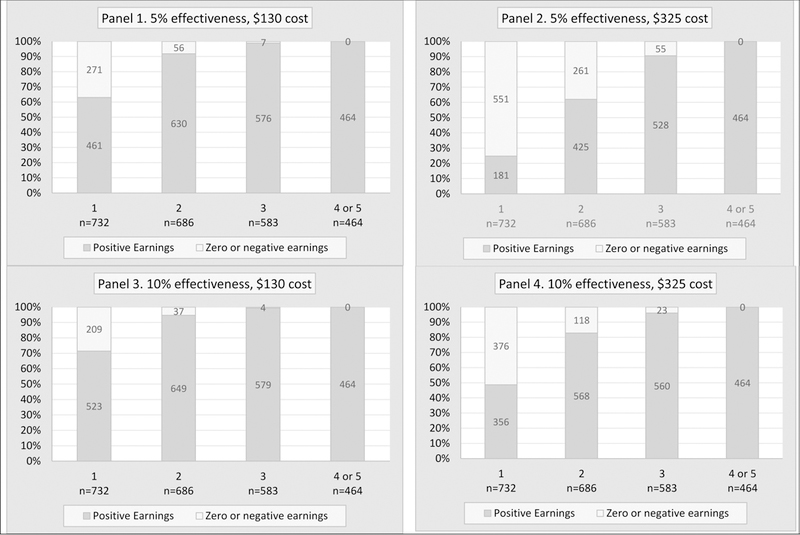
Broad-scale implementation assumes targeting all patients hospitalized for an HRRP applicable condition, regardless of whether or not a hospital has excess readmissions for all conditions. The numbers are computed across all conditions, by using condition-specific net earnings estimates from Table 3 for conditions with excess readmissions, and only revenue losses from forgone readmissions plus intervention costs for conditions without excess readmissions for which no HRRP penalty savings from further readmission avoidance can be expected. As in Table 3, four permutations of assumptions regarding the effectiveness and costs of the intervention are used. As in Table 3, the number and percentage of hospitals with positive the expected net earnings from a broad-scale readmission reduction intervention.
RESULTS
Descriptive Results
Over the three-year performance measurement period (FY 2012 – FY 2014), hospitals had 224 index discharges for AMI, 382 for HF, 323 for COPD, 320 for PN, and 461 for THA/TKA, with considerable variation across hospitals (Table 1). Average readmission rates were between 20% and 25% for AMI, HF, COPD, and PN; the average readmission rate for THA/TKA was considerably lower, at 6.7%. Predicted readmission rates were about 1.5 percentage points lower than the actual readmission rates for AMI, HF, COPD, and PN, and about 1 percentage point lower for THA/TKA, due to Medicare’s risk-adjustment for patient mix and hospital size. Because our sample was restricted to relatively poorly performing hospitals (EXRR>1), expected readmission rates were lower than both the corresponding actual and predicted readmission rates. Average wage index-adjusted base operating DRG payments ranged from ~$6,500 (HF, COPD, and PN) to more than $10,000 (AMI and THA/TKA).
Medicare revenue gain per an avoided readmission (Aim 1)
The condition-specific HRRP penalty savings from an avoided readmission (Panel 1, Table 2) were roughly equivalent—between $9,742 and $11,586—for HF, COPD, and PN. Penalty savings were substantially greater for AMI and THA/TKA— $18,769 and nearly $60,369, respectively. Across the five applicable conditions, reimbursement revenue foregone on an avoided readmission was small by comparison to the HRRP penalty saving, amounting to $1,220-$2,122 (or 11–12% of penalty saved) for AMI, HF, COPD, and PN, and $2,017 (less than 3% of penalty saved) for THA/TKA (Panel 2, Table 2). Accounting for foregone reimbursement, Medicare reimbursement revenue gains per avoided readmission were $16,752 (AMI), $9,298 (HF), $8,522 (COPD), $10,311 (PN), and $58,248 (THA/TKA), with more than 97 percent of hospitals expected to see positive total reimbursement revenue gains, net of revenue loss from avoiding an excess readmission.
Economic case for readmission avoidance (Aim 2)
Depending on the assumptions regarding program costs and effectiveness, an adoption of a readmission reduction program was expected to generate a positive financial benefit, net of program costs, of $25,560–$174,598 from reducing excess readmissions for AMI and $88,138–$394,371 from reducing excess readmissions for THA/TKA, over a three-year penalty period following the year during which the readmission reduction program was in place (Table 3). Expected net earnings ranges were lower for HF (up to $149,834), COPD (up to $112,281), and PN (up to $118,866). A combination of very low program effectiveness (5% reduction in readmissions) and high program costs ($325 per discharge) led to negative expected net earnings (or losses) of –$27,369 to –$35,793 for 9–22% of hospitals with excess readmissions for HF, PN, or COPD.
Aggregated across all five applicable conditions, hospitals with excess readmissions for two or more applicable conditions were expected to see positive net earnings under all assumptions, ranging from $21,546 (low effectiveness and high cost) to about $240,556 (high effectiveness and low cost) for hospitals with excess readmissions for exactly two applicable conditions, and from about $489,400 to $1,250,446 for hospitals with excess readmissions for four or more applicable conditions (Figure 1). Hospitals with excess readmissions for only one applicable condition had small positive expected net earnings ($35,304 to $102,002) under the low cost assumption, and non-significant ($14,970, p=0.52) or negative (–$60,000, p<0.001) expected net earnings under the high cost assumption (Figure 1). Among hospitals with excess readmissions for two, three, four or more applicable conditions, the majority had positive expected net earnings, ranging from 62% of hospitals with excess readmissions for exactly two conditions under the least favorable assumptions on program cost and effectiveness, and increasing to 90%—100% as the number of conditions with excess readmissions increased and assumptions on program cost and effectiveness improved (Figure 2).
Sensitivity Analyses
We conducted sensitivity analyses to examine the robustness of the results to hospital baseline readmissions performance, hospital size, and to assumptions regarding the Medicare revenue markup and the break-down of direct-to-indirect hospitalization costs. (Tables B3–B6 in Digital Supplement B). We found significantly lower projected Medicare revenue gains from readmissions avoidance for hospitals that perform close to the national benchmark (the first EXRR quintile), relative to hospitals in the higher EXRR quintiles (Table B3, Panel 2). Smaller hospitals had slightly lower financial gains from readmission avoidance relative to larger hospitals (this was likely due to the HRRP’s adjustment that stabilizes, or “shrinks”, the number of predicted readmissions for smaller hospitals to avoid undue penalties from small fluctuations in readmissions, thus partly muting their financial incentives to reduce excess readmissions) (Table B3, Panel 3; also Table B4 shows performance adjustments by hospital size). Various assumptions regarding the size of the Medicare reimbursement markup did not change the results notably, although lower (more negative) reimbursement markups produced smaller estimates of foregone reimbursement revenue from readmission avoidance, thus contributing to greater incentives and higher projected net earnings from readmission avoidance efforts (Table B5, Panel 2). The share of direct cost in the total cost of hospitalization mattered substantially—compared to our assumption of the 80/20 relative shares of direct-to-indirect costs, a 50/50 split would results in up to a 40% lower projected net revenue gains (HRRP penalty savings net of foregone readmission revenue) per an avoided readmission (Table B5, Panel 3). This is because an avoided readmission results in direct cost savings that partially offset the loss of reimbursement revenue; therefore, the smaller the share of direct costs in total hospitalization costs, the larger is the loss of revenue from an avoided readmission. However, in a final sensitivity analysis, where we replicated the pro-forma analyses of hospital-level net earnings from a broad-scale implementation of a readmission reduction program under the alternative cost breakdown assumptions, the finding of a positive economic case for hospitals with excess readmissions (EXRR>1) for two or more applicable conditions, or at least one applicable condition with the EXRR exceeding the first percentile (EXRR>1.02), held (Table B6).
DISCUSSION
This study was a novel application of differential calculus methods to policy evaluation and analysis where a non-stochastic data-generating process could be analytically derived from the HRRP’s statutory language. Because in social sciences, the underlying data-generating model is rarely known or directly observable, researchers frequently resort to regression analyses as a way of deducing the relationship of interest (in this case, the amount of penalty reduction per an avoided readmission) from a reduced-form association between the two variables, while treating both variables as stochastic or random. Although it is intuitive and computationally rather straightforward, the stochastic inference approach is subject to model misspecification (incorrect functional form) and various type of bias (selection bias, suppression bias, omitted variable bias, etc.). Taking advantage of the known underlying data-generating process (the HRRP statute), we were able to carry out near-exact calculations (to the first order of approximation) of the incremental change in HRRP penalty per an avoided readmission for an applicable condition for individual hospitals, without model specification concerns and other biases associated with the stochastic approach. The study’s novel approach allowed us, for the first time, to shed light on the entire hospital-level financial incentive structure underlying the HRRP statute (Aim 1) and to examine the projected economic case for an investment in readmission reduction efforts under a number of scenarios (Aim 2).
The findings of Aim 1 show that the HRRP penalty offers positive financial incentives to reduce readmissions—just one fewer readmission is estimated to result in an average future financial gain of $8,500-$58,000, net of a revenue loss from the avoided readmission. Nearly all hospitals (close to 100%) stand to receive additional reimbursement revenue if they continue to reduce excess readmissions (Table 2). The largest incremental financial gain per an avoided readmission is in the prevention readmissions for THA/TKA discharges, followed by AMI, and then PN, HF, and COPD. This is not surprising considering that, due to smaller readmission rates for THA/TKA, avoiding one readmission for THA/TKA improves a hospital’s EXRR for this condition to a greater extent than for any of the other conditions. The high base operating DRG payment for these procedures relative to the other applicable conditions further elevates the HRRP revenue gains from avoiding THA/TKA readmissions above the other conditions. Relatively greater penalty savings for AMI similarly reflect fewer readmissions and higher base operating Medicare DRG payments relative to HF, COPD, and PN. However, while these revenue gains provide evidence of positive incentives within the HRRP statute, costs and effectiveness of readmission prevention efforts must also be considered before we can gauge whether the HRRP’s incentive structure is sufficiently robust to induce actual changes in hospitals’ readmission prevention performance.
Our findings of Aim 2 suggest a positive economic case for investment in transitional care or enhanced discharge programs for the majority hospitals (60%−100%) under most assumptions regarding program cost and effectiveness, with higher-effectiveness and lower-cost assumptions leading to more favorable findings (Table 3). Even under the conservative assumption of a 5–10% reduction in readmissions following a hypothetical intervention, an average hospital with excess readmissions was predicted to retain up to $110,000–$175,000 by reducing excess readmissions for AMI, HF, COPD, and PN, and up to $400,000 for reducing readmissions for THA/TKA, after recouping the program’s annual costs. Given that the average HRRP penalty for FY 2016 was $160,000 (MedPAC, 2016), our findings point to the potential of a successful readmission reduction effort to largely eliminate the penalty for an average hospital performing below the national benchmark.
The choice of a prevention program could, however, impact the economic case for investment in readmission reduction within each particular organization. Comparing the net earnings estimates across the different sets of assumptions regarding program cost and effectiveness (Table 3) show that a combination of very low effectiveness and high per-discharge costs was projected to result in small or even negative net earnings from program implementation (reimbursement gains barely recouping or falling short of recouping program costs) for HF, COPD, and PN patients. We also found that the hospital’s own cost structure, specifically the greater relative share of indirect (facility, equipment) versus direct (labor, supplies) per-discharge cost, could amplify the negative impact of forgone reimbursement revenue from avoided readmissions. Implementation of readmission prevention programs can pose challenges to these organizations, depending on approaches taken, the specific conditions targeted by the intervention, and the skill with which the intervention is implemented (Hesselink et al., 2012; Kripalani, Theobald, Anctil, & Vasilevskis, 2014; Leppin et al., 2014; Mitchell, Weigel, Laurens, Martin, & Jack, 2017). The potential losses under the worst-case scenario (around $30,000 annual earnings shortfall) are, however, negligible relative to an average hospital’s budget, and they might be well worth it in terms of improved patient satisfaction and organizational reputation effects. Nevertheless, hospitals will need to individually assess their organizational readiness and financial ability to engage in successful prevention strategies. Finding a favorable balance between effectiveness and cost may result in a positive economic case from readmissions reduction efforts for most organizations.
Results of analyses stratified by the number of conditions for which a hospital has excess readmissions (Figures 1) revealed that the HRRP provides a strong economic case for poorly performing organizations to invest in broad-scale implementation of readmission reduction programs, with $500,000 to $1.25 million projected net earnings (after recouping program costs) annually for hospitals with excess readmissions for most or all applicable conditions. In sensitivity analyses, these estimates were higher for larger hospitals whose performance estimates were less likely to be adjusted for small hospital size. The strong financial incentives for large poorly performing hospitals is important because, with few exceptions, these organizations contribute the majority of all excess readmissions and healthcare costs (Joynt & Jha, 2013a).
The economic case for investing in readmission reduction programs was, however, weaker for hospitals performing close the nationwide average on most or all targeted conditions. Our estimates showed that the Medicare reimbursement gains per an avoided readmission for these hospitals were much lower than average, thus potentially eliminating their case for investing in broad-scale readmissions prevention efforts. However, to the extent that these relatively better-performing hospitals may be able to target a subset of Medicare patients at a high risk for poor post-hospitalization outcomes—rather than implementing readmission reduction programs broadly for all Medicare discharges—readmissions prevention could generate a positive financial return. Development and refinement of risk-prediction models for readmissions can facilitate such targeting (Kansagara et al., 2011).
The economic case for hospitals may change in the future, given upcoming changes to the HRRP. Recent legislation (P.L. 114–255, 2016) stipulates that, beginning in FY 2019, CMS will compare a hospital’s readmissions performance not to all other hospitals, as is currently done, but only to hospitals with similar proportions of dually eligible patient populations. Under this new policy, one would expect the variation in performance across hospitals within each new assessment category (of dually eligible patient populations) to be smaller than currently observed and lower the penalties observed for many poorly performing hospitals, reducing their incentives to invest in readmission prevention. On the other hand, the projected roll-out of the bundled payment model would largely cut (or completely eliminate) payments for readmissions within a 30 day period after an index discharge (CMS, 2018a), thus strengthening the economic case for readmission prevention efforts, especially if the Medicare reimbursement markup continues to follow the current downward trend (MedPAC, 2018). Additionally, as the number of applicable conditions subject to the HRRP performance assessment increases (CMS, 2018b), so will the economic case for broad-scale readmission reduction programs.
Our study had several limitations. First, we were unable to adjust the net earnings analyses for potential differences in condition-specific implementation costs or effectiveness; however, because the program costs are limited to labor costs (clinician time), these cost differences are likely to be small. We also did not examine potential economies of scale that may arise if these programs have upfront costs or if resource-constrained hospitals need to hire additional clinical staff to manage the increased workload; such economies of scale may disadvantage smaller hospitals by increasing their per-discharge program costs; however, because upfront costs are reported to be negligible, and because additional clinical staff can shift effort between transition coordination activities and other clinical tasks, efficiency losses in smaller hospitals, and economies of scale, are likely to be minimal. Second, we assumed that readmissions cost, and are reimbursed, at the same rate as an index Medicare discharge (MedPAC, 2013); however, if readmissions cost more or are reimbursed at a lower rate than index discharges, our estimates may be conservative. Third, improved readmission performance could have positive reputational effects and could increase demand for hospital services and private reimbursement rates, not measured in this study; this would also make our results conservative. Fourth, as readmission rates decline, it may become more difficult and costly to further lower readmissions; however, we used conservative assumptions for effectiveness and costs of readmission reduction interventions. Last but not least, penalty reductions are estimated for incremental changes in readmissions and may not be accurate for large readmission reductions. Given the assumptions and limitations, the estimates presented in this study are intended to serve only as a guide to hospitals interested in addressing readmissions. Hospitals will need to individually track the costs and results of any readmission prevention efforts, to assess whether such efforts—when weighed against financial penalties avoided—result in a continuing positive economic case.
Conclusion
Overall, readmission prevention efforts may “pay for themselves”— hospitals generally have a strong financial incentive to avoid readmissions, even when accounting for prevention costs and lost patient revenue from fewer hospital admissions. The incentive is strongest for poorly performing hospitals with high rates of excess readmissions or excess readmissions for several conditions subject to penalties under HRRP. Broad-scale readmission reduction programs are likely to generate positive economic returns for most hospitals, although risk-prediction and targeting may be necessary for organizations with fewer excess readmissions.
Of interest to policy makers, the HRRP’s incentive structure appears to be strong overall but decaying closer to the national performance benchmark; building in rewards for better than average performance, as it is done in the Hospital Value Based Purchasing, could strengthen incentives for all hospitals and help promote a sustained downward trend in repeat hospitalizations.
Supplementary Material
Contributor Information
Olga Yakusheva, Department of Systems, Populations and Leadership, University of Michigan School of Nursing.
Geoffrey J. Hoffman, Department of Systems, Populations and Leadership, University of Michigan School of Nursing.
References:
- Axon RN, & Williams MV (2011). Hospital readmission as an accountability measure. JAMA, 305(5), 504–505. doi: 10.1001/jama.2011.72 [DOI] [PubMed] [Google Scholar]
- Berenson RA, Paulus RA, & Kalman NS (2012). Medicare’s readmissions-reduction program--a positive alternative. N Engl J Med, 366(15), 1364–1366. doi: 10.1056/NEJMp1201268 [DOI] [PubMed] [Google Scholar]
- Chollett D, Barrett A, & Lake T (2011). Reducing hospital readmissions in New York state: A simulation analysis of alternative payment incentives. Retrieved from http://nyshealthfoundation.org/uploads/resources/reducing-hospital-readmissions-payment-incentives-september-2011.pdf
- CMS. (2016a). FY 2016 Final Rule, Correction Notice and Consolidated Appropriations Act of 2016 Tables. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2016-IPPS-Final-Rule-Home-Page-Items/FY2016-IPPS-Final-Rule-Tables.html
- CMS. (2016b). Hospital Compare Data Archive. Retrieved from: https://data.medicare.gov/data/archives/hospital-compare
- CMS. (2017). FY 2016 Final Rule and Correction Notice Data Files. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2016-IPPS-Final-Rule-Home-Page-Items/FY2016-IPPS-Final-Rule-Data-Files.html
- CMS. (2018a). Bundled Payments for Care Improvement (BPCI) Initiative: General Information. Retrieved from https://innovation.cms.gov/initiatives/bundled-payments/
- CMS. (2018b). Hospital Readmissions Reduction Program (HRRP) Archives.
- Coleman EA, Parry C, Chalmers S, & Min SJ (2006). The Care Transitions Intervention: Results of a randomized controlled trial. Arch Intern Med, 166(17), 1822–1828. doi: 10.1001/archinte.166.17.1822 [DOI] [PubMed] [Google Scholar]
- Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, Maynard G, … Williams MV (2013). Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med, 8(8), 421–427. doi: 10.1002/jhm.2054 [DOI] [PubMed] [Google Scholar]
- Hansen LO, Young RS, Hinami K, Leung A, & Williams MV (2011). Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med, 155(8), 520–528. doi: 10.7326/0003-4819-155-8-201110180-00008 [DOI] [PubMed] [Google Scholar]
- Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, … Wollersheim H (2012). Improving patient handovers from hospital to primary care: A systematic review. Ann Intern Med, 157(6), 417–428. doi: 10.7326/0003-4819-157-6-201209180-00006 [DOI] [PubMed] [Google Scholar]
- Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, … Culpepper (2009). A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med, 150(3), 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joynt KE, & Jha AK (2013a). Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA, 309(4), 342–343. doi: 10.1001/jama.2012.94856 [DOI] [PubMed] [Google Scholar]
- Joynt KE, & Jha AK (2013b). A path forward on Medicare readmissions. N Engl J Med, 368(13), 1175–1177. doi: 10.1056/NEJMp1300122 [DOI] [PubMed] [Google Scholar]
- Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, & Kripalani S (2011). Risk prediction models for hospital readmission: A systematic review. JAMA, 306(15), 1688–1698. doi: 10.1001/jama.2011.1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripalani S, Theobald CN, Anctil B, & Vasilevskis EE (2014). Reducing hospital readmission: Current strategies and future directions. Annual Review of Medicine, 65, 471–485. doi: 10.1146/annurev-med-022613-090415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, … Montori VM(2014). Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern Med, 174(7), 1095–1107. doi: 10.1001/jamainternmed.2014.1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MedPAC. (2013). Report to Congress: Medicare and the health care delivery system. Retrieved from Washington, DC:
- MedPAC. (2014). Report to the Congress: Medicare payment policy. Retrieved from Washington, DC: http://www.medpac.gov/documents/reports/mar14_ch03_appendix.pdf?sfvrsn=0
- MedPAC. (2016). Chapter 3: Hospital inpatient and outpatient services. Retrieved from Washington DC:
- MedPAC. (2018). Report to the Congress: Medicare Payment Policy. Retrieved from http://www.medpac.gov/docs/default-source/reports/mar18_medpac_entirereport_sec.pdf?sfvrsn=0
- Mellor J, Daly M, & Smith M (2016). Does It pay to penalize hospitals for excess readmissions? Intended and unintended consequences of Medicare’s Hospital Readmissions Reductions Program. Health Economics, n/a-n/a. doi: 10.1002/hec.3382 [DOI] [PubMed] [Google Scholar]
- Mitchell SE, Weigel GM, Laurens V, Martin J, & Jack BW (2017). Implementation and adaptation of the Re-Engineered Discharge (RED) in five California hospitals: A qualitative research study. BMC Health Serv Res, 17(1), 291. doi: 10.1186/s12913-017-2242-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, & Schwartz JS (1999). Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA, 281(7), 613–620. [DOI] [PubMed] [Google Scholar]
- 21st Century Cures Act, PL 114–255, C.F.R. (2016).
- Peikes D, Chen A, Schore J, & Brown R (2009). Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA, 301(6), 603–618. doi: 10.1001/jama.2009.126 [DOI] [PubMed] [Google Scholar]
- Tilson S, & Hoffman G (2012). Addressing Medicare Hospital Readmissions. Retrieved from https://pdfs.semanticscholar.org/f60a/bba1dd06804ef6393bfb12b3e74ab0ad28d2.pdf
- van Walraven C, Bennett C, Jennings A, Austin PC, & Forster AJ (2011). Proportion of hospital readmissions deemed avoidable: A systematic review. CMAJ, 183(7), E391–402. doi: 10.1503/cmaj.101860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, & Epstein AM (2016). Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. doi: 10.1056/NEJMsa1513024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


