Abstract
Introduction
Eosinophilic granulomatosis with polyangiitis (EGPA) is a subset of antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis with distinct pathophysiological mechanisms, clinical features and treatment responses. Rituximab is a licensed therapy for granulomatosis with polyangiitis and microscopic polyangiitis but there is limited experience of rituximab in EGPA.
Methods
EGPA patients from a tertiary centre who received rituximab for mostly refractory EGPA or in whom cyclophosphamide was contra indicated were studied. A standardised dataset was collected at time of initial treatment and every 3 months for 24 months. Response was defined as a Birmingham Vasculitis Activity Score (BVAS) of 0 and partial response as ≥50% reduction in BVAS from baseline. Remission was defined as a BVAS of 0 on prednisolone dose ≤5 mg.
Results
Sixty-nine patients (44 female) received rituximab between 2003 and 2017. Improvement (response and partial response) was observed in 76.8% of patients at 6 months, 82.8% at 12 months and in 93.2% by 24 months, while relapses occurred in 54% by 24 months, with asthma being the most frequent manifestation. The median BVAS decreased from 6 at baseline to 1 at 6 months, and 0 at 12 and 24 months. Prednisolone dose (mg/day, median) decreased from 12.5 to 7, 7.5 and 5 at 6, 12 and 24 months, respectively. ANCA positive patients had a longer asthma/ear, nose and throat (ENT) relapse-free survival time and a shorter time to remission.
Discussion
Rituximab demonstrated some efficacy in EGPA and led to a reduction in prednisolone requirement, but asthma and ENT relapse rates were high despite continued treatment. The ANCA positive subset appeared to have a more sustained response on isolated asthma/ENT exacerbations.
Keywords: systemic vasculitis, eosinophilic granulomatosis with polyangiitis, ANCA, rituximab, asthma
Key messages.
What is already known about this subject?
Eosinophilic granulomatosis with polyangiitis (EGPA) current management relies on glucocorticoids and immunosuppressive drugs but relapses and high glucocorticoid exposure are frequent. Rituximab is an effective and licensed therapy for granulomatous with polyangiitis/microscopic polyangiitis but there is a paucity of data from EGPA.
What does this study add?
Rituximab was associated with reduced disease activity and prednisolone requirement in EGPA patients, but relapses occurred despite maintenance rituximab.
Antineutrophil cytoplasmic antibodies (ANCA) positive patients had a longer asthma/ear, nose and throat relapse-free survival time and a shorter time to remission after rituximab.
How might this impact on clinical practice?
Rituximab appears to have a useful role in relapsing EGPA patients, although the magnitude of benefit may associate with ANCA status and clinical profile (vasculitic versus eosinophilic).
Introduction
Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare small-vessel vasculitis characterised by eosinophil-rich and necrotising granulomatous inflammation, frequently associated with asthma and eosinophilia.1 The 2012 International Chapel Hill Consensus Conference includes EGPA in the antineutrophil cytoplasmic antibodies (ANCA) associated vasculitis (AAV) group, although only 40% of the patients test positive for ANCA.2 Although yet to be fully elucidated, the pathogenesis of EGPA has some distinctive pathophysiological mechanisms from the other AAV disease phenotypes. These include an increased interleukin (IL)-5 production and consequent increased maturation and survival of eosinophils.3 4 A predominant Th2 response, as levels of Th2 cytokines, such as IL-4 and IL-13, are raised in EGPA.5 Recommendations for EGPA management are often extrapolated from experience in the more common AAV subgroups (granulomatous with polyangiitis (GPA) and microscopic polyangiitis (MPA)), and this approach may not be reliable.6 EGPA has been the subject of few randomised controlled trials. The MIRRA trial of mepolizumab (A Double-blind, Randomised, Placebo-controlled Study to Investigate the Efficacy and Safety of Mepolizumab in the Treatment of Eosinophilic Granulomatosis with Polyangiitis in Subjects Receiving Standard of Care Therapy), a humanised monoclonal antibody that targets IL-5, has been the only industry sponsored trial in EGPA and a positive result led to an approval for EGPA by the Food and Drug Administration (FDA).7 In this trial, mepolizumab led to more accrued weeks of remission than placebo (28% vs 3%) and reduction of the mean daily dose of prednisolone at week 52 (9.2 mg in the mepolizumab group vs 13.5 mg in the placebo group). Based on the long-term observational studies, EGPA patients are subgrouped into those with poor prognostic factors (such as serum creatinine >140 µmol/L; proteinuria >1 g/day; or central nervous system, gastrointestinal or myocardial involvement), in whom cyclophosphamide and glucocorticoids are recommended and those without poor prognostic factors for whom prednisolone with or without an immunosuppressive, such as, azathioprine is recommended.8–10 Despite therapy most patients remain glucocorticoid dependent with a relapsing/remitting course as the glucocorticoid dose is weaned and acquire a high cumulative exposure to glucocorticoids and immunosuppressive agents with their attendant complications. There is a clear need for newer therapies that achieve sustained remission with low or no concomitant glucocorticoids requirement.
Rituximab, an anti‐CD20 B‐cell depleting chimeric monoclonal antibody, has proven efficacy for remission induction and maintenance in GPA and MPA.11–13 The rationale for rituximab in EGPA comes from the presence of ANCA in 40% of the patients, and similarities in the vasculitic features between EGPA and GPA/MPA, which reflect B-cell involvement in disease pathogenesis.2 In distinction from GPA/MPA, EGPA patients suffer non-vasculitic eosinophilic manifestations, including asthma, naso-sinus disease and myocarditis where the rationale for rituximab is weaker.
However, preliminary studies have found reductions in T-cell derived IL-5 production with rituximab.14 Also, a strong IgG4 immune response in EGPA, irrespective of the ANCA status, has been described15 and rituximab has proved beneficial for IgG4-related syndromes.16 17 Finally, previous studies have suggested a clinical benefit for rituximab in EGPA, but they were limited by small patient numbers and a short treatment duration.18 19 This study aimed to assess the longer term efficacy and safety of rituximab in EGPA.
Patients and methods
We performed a retrospective study of patients with EGPA treated with rituximab in a single tertiary centre, the Vasculitis and Lupus clinic, Cambridge, UK.
Rituximab treatment protocols
The indications for rituximab in EGPA were either active refractory or frequently relapsing disease, defined according to the patient’s physician assessment or a contraindication to cyclophosphamide. Five patients received a single course of rituximab. The initial treatment protocol consisted, in 64 patients, of two doses of 1000 mg 2 weeks apart, with only five patients receiving a dose of 375 mg/m2/week for 4 weeks. Fifty-nine patients (86%) were retreated every 6 months with a 1000 mg dose, with a minority of the patients (14%) being retreated every 4 (minimum) or 12 (maximum) months. Patients received premedication with intravenous hydrocortisone 100 mg, intravenous chlorpheniramine 10 mg or diphenhydramine 50 mg and oral acetaminophen 1 g before each rituximab infusion; and pneumocystis prophylaxis with sulfamethoxazole/trimethoprim for 6 months.
Data collection
Data collection included baseline demographics, laboratory parameters and Disease Extent Index (DEI)20 at time of first rituximab and every 3 months for 24 months. In the DEI, asthma was considered as a marker for lung involvement. Data about previous immunosuppressive drugs as well as prednisolone doses were collected. A positive ANCA result was recorded if either immunofluorescence or ELISA for either proteinase-3 or myeloperoxidase ANCA were positive from the time of diagnosis to the time of first treatment. Disease activity was assessed using the Birmingham Vasculitis Activity Score (BVAS) V.3.21 In BVAS, symptomatic asthma was scored as ‘wheeze’. Refractory asthma and ear, nose and throat (ENT) disease was defined as asthma or ENT symptoms flares at steroid tapering justifying an increase of the steroid dose and/or a change of immunosuppressive drug.
Treatment outcome and adverse events
The response to therapy was judged clinically by the treating physician. Remission was defined as a BVAS of 0 on a daily prednisolone dose ≤5 mg. Response to treatment was defined as a BVAS of 0 independent of glucocorticoid dose.22 Partial response was defined as a reduction of ≥50% in BVAS compared with the baseline score.
Relapses were defined as a recurrence of signs or symptoms leading to an increase in BVAS and an increase in prednisolone dose by ≥5 mg or institution of intravenous glucocorticoids, intravenous aminophylline or new immunosuppressive agent. An initial remission was not required to have a relapse. Mild hypogammaglobulinaemia was defined as an IgG level between 5 and 6.9 g/L, moderate between 3 and 4.9 g/L and severe if IgG level was <3 g/L. Severe infections were those resulting in hospitalisation, prolongation of existing hospital stays or requiring intravenous antibiotics.
Statistical analyses
Since the usual interval dosing of rtuximab is every 6 months, response, disease activity, prednisolone dose, laboratory tests and infections were considered in the analysis until 6 months after last treatment, and reasons for treatment discontinuation were presented separately. Continuous variables were presented as medians and IQRs unless otherwise stated. Differences in continuous variables were tested by the non-parametric Sign test. Kaplan-Meier curves were used to illustrate the probability of remaining relapse-free according to ANCA status and to evaluate time to remission. A Pearson’s X2 test was applied to evaluate the relationship between categorical variables. A p<0.05 was considered significant for all analyses. Statistical analyses were performed using the Statistical Package for the Social Sciences, SPSS V.22.0 for Windows (IBM). For graphical representations, MedCalc V.18.6 and the BioVinci V.1.3.3 were used.
Results
Between 2003 and 2017, 140 patients with EGPA had been reviewed by the clinic. Seventy-two were treated with rituximab, but only 69 patients were considered for this analysis (table 1). Two were excluded due to follow up in other hospitals, and one because he had received alemtuzumab 1 month before rituximab.
Table 1.
Baseline demographics and clinical characteristics of 69 patients with eosinophilic granulomatosis with polyangiitis treated with rituximab
| Sex Female/Male | 44/25 |
| Age at first rituximab, median (IQR) | 51 (39.5–58.0) |
| ANCA status (historical or at treatment onset), no of patients (%) | |
| Positive (including immunofluorescence) | 24 (34.8) |
| Negative (including immunofluorescence) | 45 (65.2) |
| Positive C-or P-ANCA (only immunofluorescence) | 20 (29.0) |
| PR3-ANCA | 9 (13.0) |
| MPO-ANCA | 16 (23.2) |
| No of prior immunosuppressive therapies: mean±SD; median (IQR) | 2.37±1.46; 2 (1–3) |
| Immunosuppressive drugs prior to rituximab, no of patients (%) | |
| Cyclophosphamide | 34 (49.3) |
| Azathioprine | 46 (66.7) |
| Mycophenolate mofetil | 39 (56.5) |
| Methotrexate | 17 (24.6) |
| Intravenous immunoglobulin | 11 (15.9) |
| Alemtuzumab | 3 (4.3) |
| Etanercept | 1 (1.4) |
| Infliximab | 2 (2.9) |
| Mepolizumab | 1 (1.4) |
| Omalizumab | 1 (1.4) |
| No previous immunosuppressive treatment | 4 (5.8) |
| DEI score at first rituximab treatment, mean±SD | 6±3.1 |
| BVAS at first rituximab, mean±SD; median (IQR) | 7.05 (±5.22); 6.0 (3.0–8.5) |
| Organ involvement according to DEI, no of patients (%) | |
| Lung (including asthma) | 68 (98.6) |
| Ear, nose and throat (ENT) | 61 (88.4) |
| Arthralgia/arthritis | 32 (46.4) |
| Skin | 41 (59.4) |
| Peripheral nervous system | 40 (58.0) |
| Renal | 11 (15.9) |
| Gastrointestinal tract (including biliary system) | 12 (17.4) |
| Heart | 15 (21.7) |
| Eyes | 8 (11.6) |
| Central nervous system | 3 (4.3) |
| Urogenital tract | 2 (2.9) |
| Refractory asthma | 46 (66.6) |
| Refractory ENT disease | 23 (33.3) |
ANCA, anti-neutrophil cytoplasmic antibodies; BVAS, Birmingham Vasculitis Activity Score; DEI, Disease Extent Index; MPO, myeloperoxidase; PR3, proteinase-3.
The median length of treatment (time between first and last infusion during the follow-up period) was 23 months (IQR 12.5–24.0 months) and the survival rate of rituximab was 84.8% at 12 months and 68.4% at 24 months. During the follow-up period, the median cumulative dose of rituximab was 2 g (IQR 2.0–2.0 g) for induction and 3 g (IQR 2.0–3.0) for maintenance.
Response
Figure 1 describes the percentage of responders, partial responders and non-responders. Patients who discontinued treatment were only considered in the categories until 6 months following last treatment. Moreover, at the time of the analysis, some patients still receiving treatment had insufficient treatment duration to be considered in the analysis at 18 months (5 patients) and at 24 months (10 patients).
Figure 1.
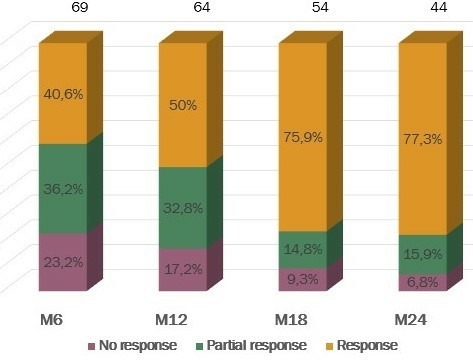
Treatment response by percentage of patients divided by three categories: no response, partial response and response. The total number of patients considered by months are presented over columns.
Five patients received a single course of rituximab. Three had no response and were not followed further, and two, who responded, received maintenance treatment with mycophenolate mofetil and prednisolone or prednisolone alone. Before 12 months, a further five discontinued rituximab due to an insufficient treatment response, and before 18 months, a further five discontinued rituximab with sustained response in four, and an insufficient response in one. The rates of discontinuations due to insufficient response were slightly higher than the rates of discontinuation due to good response.
Response to treatment was achieved in 40.6% of patients by 6 months and this rose to 77.3% by 24 months. Improvement (responses and partial responses) was observed in 76.8% of patients at 6 months, 82.8% at 12 months, in 90.7% at 18 months and in 93.2% by 24 months.
At 6 months, 13.3% and 29.2% of ANCA negative and ANCA positive patients, respectively, were on remission, rising to 23.1% and 34.8% at 12 months, but the differences according to ANCA status were not statistically significant (exact Pearson test 0.19 at 6 months and 0.38 at 12 months).
The median time to remission was shorter in the ANCA positive group than the ANCA negative group (p=0.02), with a median time to remission of 15 months in the former and 24 months in the latter (figure 2).
Figure 2.
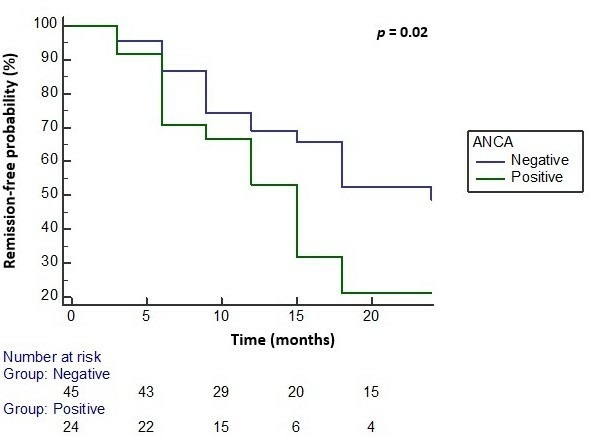
Survival without achieving remission, including vasculitis, asthma and ENT involvement remission. the median time to remission was 15 months in the ANCA positive group and 24 months in the ANCA negative group. Estimation was limited to the largest survival time evaluated (24 months after starting treatment), p=0.02 (log-rank test). ANCA, anti-neutrophil cytoplasmic antibodies; ENT, ear, nose and throat.
The median BVAS at baseline was 6 (IQR 3–8.5) and decreased to 1 (IQR 0–3) at 6 months, to 0 (IQR 0–2) at 12 months and to 0 (IQR 0–0) at 24 months (figure 3). Of the 64 patients who received a second treatment with rituximab at 6 months, only three had a higher BVAS score at 12 months than at baseline and four had no change in BVAS at 12 months. At 24 months, of the 44 patients evaluated, two had the same BVAS as at baseline and none had a higher BVAS. In the two patients with the same BVAS at baseline and 24 months, rituximab treatment allowed prednisolone dose reduction.
Figure 3.
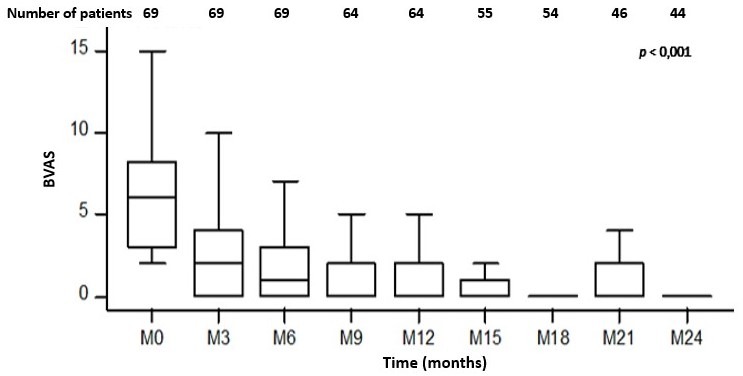
Median (IQR) of the Birmingham Vasculitis Activity Score (BVAS) at baseline and every 3 months (M) from baseline. Baseline: 6.0 (3.0–8.5), N=69 vs 6 months: 1.0 (0.0–3.0), N=69, z=6.9 vs 12 months: 0.0 (0.0–2.0), N=64, z=6.54 vs 18 months: 0 (0.0–0.25), N=54, z=6.49 vs 24 months: 0.0 (0.0–0.0), N=44, z=6.25, p<0.001. Boxes represent IQRs and the median. Lower and upper limits represent the minimum and maximum, respectively.
Prednisolone dose and other concomitant treatments
At baseline, 6, 12, 18 and 24 months, 4.3%, 7.2%, 9.3%, 20.4% and 15.9% were glucocorticoid free, respectively. The median daily dose of prednisolone was 12.5 mg at baseline (IQR 10.0–20.0) and decreased to 7 mg (IQR 5–10.75) at 6 months, to 7.25 mg (IQR 4.75–10.0) at 12 months and to 5 mg (IQR 3.25–10) at 24 months (figure 4). Five patients required treatment with intravenous steroids beyond standard rituximab infusions for asthma in three, skin lesions in one and worsening polyneuropathy in other.
Figure 4.
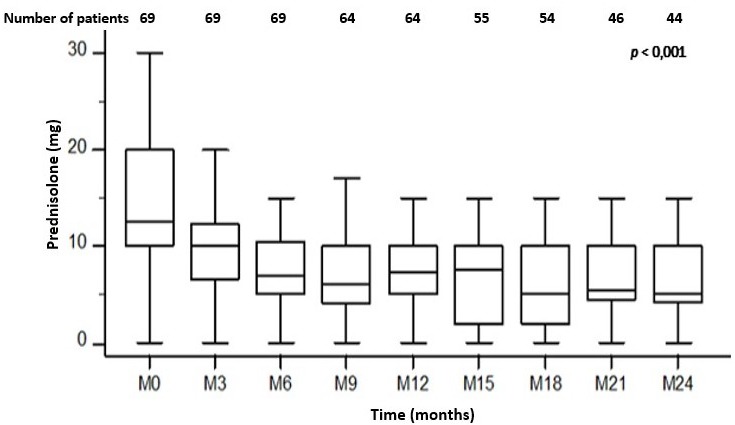
Median (IQR) prednisolone/prednisone dose (mg/day) at baseline, and every 3 months after initial rituximab treatment. Baseline: 12.5 (10.0–20.0), N=69 vs 6 months: 7 (5–10.75), N=69, z=5.58 vs 12 months: 7.25 (IQR 4.75–10.0), N=64, z=4.76 vs 18 months: 5 (2.0–10.0), N=54, z=5.58 vs 24 months: 5 (3.25–10.0), N=44, z=4.8, p<0.001.
Twelve of the 69 patients were treated with a combination of rituximab and an additional immunosuppressive agent. In 11, the immunosuppressive agent was added during rituximab treatment (median of 15 months after starting treatment) in the context of relapsing disease in seven in refractory disease in four. In one, the additional immunosuppressive agent was not suspended when rituximab was initiated nor throughout treatment.
Laboratory tests
No change was observed in C reactive protein, erythrocyte sedimentation rate and eosinophil count throughout the treatment period (table 2). The median value at baseline of these parameters was within the normal ranges. The median IgG level at baseline was 8.07 g/L without major changes at 12 months. However, at 24 months, a median decrease to 6.95 g/L was noted. Hypogammaglobulinaemia rates at baseline, 6 and 12 months were similar (about 15%), but increased to 20.5% and 38.7% at 18 and 24 months, respectively. Rates of mild hypogammaglobulinaemia were 7.3%, 10.6%, 8.3%, 13.6% and 32.3% at 0, 6, 12, 18 and 24 months, respectively. Rates of moderate hypogammaglobulinaemia were 7.3%, 4.5%, 6.7%, 6.8% and 6.5% at 0, 6, 12, 18 and 24 months, respectively. None of the patients developed severe hypogammaglobulinaemia during the evaluated period. During maintenance therapy, no patient received treatment with intravenous immunoglobulin (IG) for recurrent infections or hypogammaglobulinaemia.
Table 2.
Laboratory data at entry (time of first rituximab infusion), at 12 and 24 months
| Entry, median (IQR) (N=69) |
12 months (N=64) |
24 months (N=44) |
|
| IgG, g/L | 8.07 (6.66–9.66) | 7.9 (6.04–8.77) z=0.452, p=0.651 | 6.95 (5.76–8.52) z=2.84, p<0.005 |
| Total peripheral eosinophil count, x109/L | 0.26 (0.11–0.77) | 0.21 (0.10–0.55) z=0.62, p=0.53 | 0.22 (0.13–0.34) z=0, p=1.00 |
| C reactive protein, mg/L | 4.00 (3.00–9.00) | 4.00 (3.00–8.00) Z=3.2, p=0.75 |
4.00 (2.00–8.00) z=0, p=1.000 |
| Erythrocyte sedimentation rate, mm/hour | 9.00 (6.00–19.50) | 8.00 (5.00–14.00) z=2.96, p<0.005 | 7.00 (5.50–12.00) z=−2.46, p=0.01 |
Relapses
During the first 24 months after starting treatment, 54% of the patients suffered at least one relapse on treatment. 29.7% of these relapses occurred after achieving remission, and thus were considered as having relapsing disease. The mean number of relapses per patient was 0.9±1.27. Relapses were mainly driven by asthma, with 43.5% of the patients suffering at least one asthma relapse (table 3). ENT relapses were the second most frequent, followed by joint and skin manifestations. Skin involvement was usually described as erythematous maculopapular without purpura but was not systematically recorded and not confirmed by skin biopsy. None of the 11 patients with renal disease relapsed during treatment with rituximab. Only one patient presented with neurological features, suggestive of worsening polyneuropathy. Central nervous system vasculitis was not reported.
Table 3.
Manifestations driving relapse during rituximab treatment
| Manifestations driving relapse, mean relapses/person (% persons who suffered at least one relapse) | |
| Asthma/lung | 0.68±1.13 (43.5) |
| ENT | 0.17±0.38 (17.4) |
| Skin | 0.26±0.8 (13.0) |
| Kidney | 0 (0) |
| Heart | 0.03±0.169 (2.9) |
| Joint | 0.16±0.41 (14.5) |
| Digestive | 0.03±0.17 (2.9) |
| Neurological | 0.01±0.12 (1.4) |
ENT, ear, nose and throat.
Regarding isolated asthma/ENT relapses (figure 5), ANCA negative patients had a shorter relapse-free survival time compared with ANCA positive patients, (p=0.04), but no difference was seen between both groups regarding vasculitis relapses (figure 6).
Figure 5.
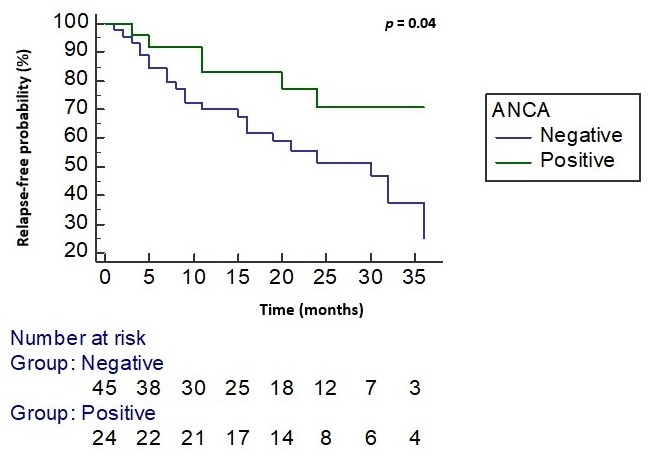
Kaplan-Meier curve representing isolated asthma/ENT relapse-free survival (months) after starting rituximab. Estimation was limited to the largest survival time evaluated (36 months after starting treatment), p=0.04 (log-rank test). ANCA, antineutrophil cytoplasmic antibodies; ENT, ear, nose and throat.
Figure 6.
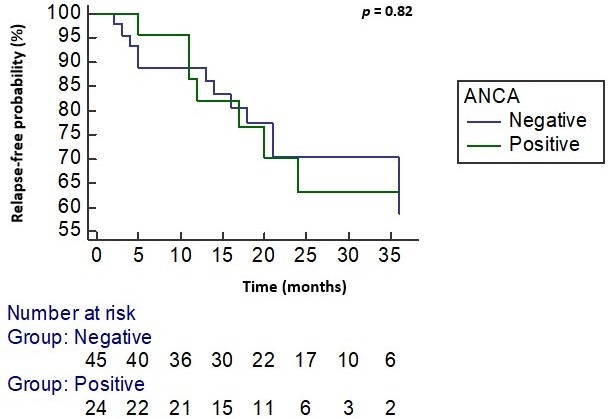
Kaplan-Meier curve representing vasculitis relapse-free survival (months) after starting rituximab (log-rank test). Estimation was limited to the largest survival time evaluated (36 months after starting treatment), p=0.82 (log-rank test). ANCA, antineutrophil cytoplasmic antibodies.
Severe infections and mortality
In the first 24 months from baseline, 11 patients (16%) suffered at least one severe infection during treatment, with four (5.8%) of them suffering two severe infections and one (1.4%) suffering three severe infections. Severe infections were observed in 12.32 per 100 patients-year. In some of these, treatment was delayed, but infection was not associated with treatment withdrawal. Infections were mainly localised to the respiratory tract, corresponding to 71% of all severe infections (table 4). No opportunistic infections were reported. Deaths of any cause did not occur during the first 24 months of follow-up.
Table 4.
Type of severe infections reported during rituximab treatment
| Type of infections, N (%) | |
| Respiratory tract | 12 (71) |
| Urogenital tract | 3 (17.6) |
| Mastoiditis | 1 (5.9) |
| Cellulitis | 1 (5.9) |
Discussion
We have analysed the efficacy and safety of rituximab in a cohort of 69 patients with EGPA. The rates of positive responses and the corticosteroid sparing effect seen after rituximab strengthens the argument for a useful therapeutic effect of this drug.
The outcomes in our study were analysed until 6 months after last rituximab, corresponding to our usual interval dosing of the drug and the expected duration of the treatment effect. Although rituximab may have a prolonged effect on the disease beyond 6 months, we aimed to look at the effect of the treatment only during the period of administration to avoid potential bias related to other treatments, as some of the patients who failed to respond were later exposed to other treatments. Most followed the 6 months repeat dose rituximab regimen for 24 months with nine (13%) discontinuing the drug due to an insufficient response and six (8.7%) due to a good treatment response.
Reductions in disease activity, as measured by BVAS, followed treatment with rituximab. At 6 months, 41% of the patients achieved a response and 36% achieved a partial response. Response rates, however, tended to increase in our cohort until 24 months, with 77% of the patients achieving a response.
The rates of remission seen in our study were lower than that seen following Rituximab in GPA/MPA, which range from 64% to 75% at 6 months.23 24 ANCA positive patients had a shorter time to remission compared with the ANCA negative subgroup. Higher remission rates were seen in the ANCA positive group. ANCA positivity has previously been associated with a higher remission rate at 12 months in EGPA after rituximab.18 This may suggest that ANCA positive EGPA patients may have a phenotype more similar to GPA and MPA and may benefit more from B-cell depletion therapies.
Rituximab permitted prednisolone dose reductions with the median daily prednisolone at baseline of 12.5 mg/day falling to 7.25 at 12 months and to 5 mg at 24 months. However, only a few patients were steroid free. Eleven patients required addition of another immunosuppressive during follow-up, which may overestimate the efficacy of rituximab. However, these results are still encouraging as EGPA patients are frequently exposed to high doses of prednisolone and susceptible to related complications. For instance, in a large French study, 236 out of 280 EGPA patients required long-term high prednisolone doses (mean dose 12.9±12.5 mg/day).25
We did not observe any change with treatment in the C reactive protein, erythrocyte sedimentation rate and peripheral eosinophil counts. This is likely due to the fact that the median values at time of first treatment were within the normal ranges, as a result of high previous prednisolone doses and other concomitant immunosuppression, as these were mainly refractory and relapsing patients. A reduction of IgG levels was seen by 18 months and worsened by 24 months, although, 20.5% of the patients had low levels at baseline reflecting prior therapy. The susceptibility of AAV patients to rituximab-induced hypogammaglobulinaemia has been noted in other studies.26
We found a high rate of relapses during treatment with rituximab, with about half of the patients relapsing during the evaluation period, much higher than seen with similar repeat dose rituximab maintenance dosing in GPA/MPA populations.27 However, our cohort was mainly relapsing and/or refractory patients and, in other EGPA populations, relapse rates as high as 81.1% have been reported.28 ANCA positivity was associated with longer asthma/ENT relapse-free survival time and a shorter time to remission after rituximab. Whether this represents a drug effect or reflects the natural history of the disease, with ANCA positive patients having more frequent asthma and/or ENT flares than ANCA negative patients, could not be assessed in our study. No difference was found regarding vasculitis relapse-free survival time between ANCA positive and ANCA negative patients. Interestingly, other studies have showed higher relapse-free survival rates for ANCA negative patients when treatment modality was not considered,25 29 even though other studies failed to show any difference.2 28 30 This may indicate a greater benefit of rituximab in the treatment of ANCA positive patients. In a smaller study, treatment response to rituximab was independent of ANCA status.19
The relapses in our cohort were mainly driven by asthma, followed by ENT disease. Of note, asthma relapses were only included if they were associated with change in treatment, in line with EGPA task force recommendations which recognise that transient loss of asthma control with, for example, a viral infection are common and do not necessarily require therapeutic changes.31 Renal flares were not observed in any patient during treatment with rituximab. Moreover, skin flares were usually described as erythematous and not vasculitic with purpura. This suggests that rituximab may be better in preventing vasculitis-mediated relapses, rather than preventing eosinophilic mediated relapses.
The rate of infections in our study was similar to the rate of infections in other studies of patients with AAV treated with rituximab.32 It is important to note that the infective risk will have been reduced by avoiding concurrent rituximab and immunosuppressive treatment and the prednisolone reduction that was seen after rituximab. In a smaller study comprising 14 patients with EGPA treated with rituximab, none of the patients developed a major infection during the first 36 months after the first treatment, although only three patients were retreated with rituximab after induction.19
Alternative treatment options for refractory EGPA have included intravenous IG, plasma exchange and alpha-interferon with support only from small observational studies.33 34 Mepolizumab led to clinically useful effects in around three-quarters of patients in the MIRRA trial with particular benefit shown for the non-vasculitic eosinophilic manifestations of asthma and naso-sinus disease.7 The greater success of rituximab for the ANCA positive EGPA subgroup and failure to control asthma relapses points to a differentiation compared with mepolizumab and the potential for personalisation of therapy according to these parameters. A recent genome-wide association study of EGPA revealed genetic and clinical differences between the ANCA positive and the ANCA negative subsets, supporting different pathogenesis between these subsets and consequently different therapeutic strategies.35
Our study was limited by its retrospective nature, with the potential for missing data and inaccurate BVAS assessment. BVAS itself is a semiobjective tool that has not been thoroughly validated in EGPA, although has appeared to perform well in previous EGPA studies. The relatively short follow-up after last rituximab means that we have not been able to report in detail on the longer term efficacy benefits and safety risks of rituximab. However, over time the difference between discontinuation rates due to insufficient response compared with discontinuation rates due to response was low, therefore, we would not expect this to impact our conclusions. The glucocorticoid sparing effect is difficult to evaluate without a control group. Lastly, there was some heterogeneity in the rituximab treatment schedules. However, in a previous study, no differences in treatment responses were observed between patients who received rituximab 375 mg/m2/week for 4 weeks or those who received rituximab two doses of 1 g at 2-week intervals, but no data were available regarding relapses.18 While the dose regimen may not influence the results, a scheduled rituximab-maintenance treatment may reduce the relapse rate compared with rituximab given on demand for relapses, as suggested recently by an Italian study.36 The strengths of this study are presenting a long-term data in the largest sample size of patients with EGPA treated with rituximab and the lack of selection bias, due to evaluation of a complete cohort of EGPA patients. We also present the first concise data on relapses in patients treated with rituximab.
We conclude that, in a real-world tertiary vasculitis clinic setting rituximab was associated with decreases in EGPA disease activity and prednisolone requirement. However, the asthma and ENT relapse rates were high despite repeat rituximab dosing and the development of hypogammaglobulinaemia a safety concern. The ANCA positive subset appeared to have a more sustained response on isolated asthma/ENT exacerbations.
Acknowledgments
We thank the support of the medical and nursing staff of the vasculitis and lupus service at Addenbrooke’s Hospital, Cambridge.
Footnotes
Contributors: All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: DJ has received research grants from Roche/Genentech and consulting fees from Astra-Zeneca, Celgene, Chemocentryx, CSL, GSK, Insmed and Sanofi/Genzyme.
Patient consent for publication: Not required.
Ethics approval: According to the UK National Health Service Research Ethics Committee guidelines, ethics approval was not required for an anonymised retrospective study; all treatment decisions were made prior to our evaluation.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request. Data may be obtained from a third party and are not publicly available.
References
- 1.Sunderkötter CH, Zelger B, Chen K-R, et al. Nomenclature of cutaneous vasculitis: dermatologic addendum to the 2012 revised international chapel Hill consensus Conference Nomenclature of vasculitides. Arthritis Rheumatol 2018;70:171–84. 10.1002/art.40375 [DOI] [PubMed] [Google Scholar]
- 2.Sinico RA, Di Toma L, Maggiore U, et al. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in Churg-Strauss syndrome. Arthritis Rheum 2005;52:2926–35. 10.1002/art.21250 [DOI] [PubMed] [Google Scholar]
- 3.Terrier B, Bièche I, Maisonobe T, et al. Interleukin-25: a cytokine linking eosinophils and adaptive immunity in Churg-Strauss syndrome. Blood 2010;116:4523–31. 10.1182/blood-2010-02-267542 [DOI] [PubMed] [Google Scholar]
- 4.Jakiela B, Szczeklik W, Plutecka H, et al. Increased production of IL-5 and dominant Th2-type response in airways of Churg-Strauss syndrome patients. Rheumatology 2012;51:1887–93. 10.1093/rheumatology/kes171 [DOI] [PubMed] [Google Scholar]
- 5.Dallos T, Heiland GR, Strehl J, et al. CCL17/thymus and activation-related chemokine in Churg-Strauss syndrome. Arthritis Rheum 2010;62:3496–503. 10.1002/art.27678 [DOI] [PubMed] [Google Scholar]
- 6.Yates M, Watts RA, Bajema IM, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis 2016;75:1583–94. 10.1136/annrheumdis-2016-209133 [DOI] [PubMed] [Google Scholar]
- 7.Wechsler ME, Akuthota P, Jayne D, et al. Mepolizumab or placebo for eosinophilic granulomatosis with polyangiitis. N Engl J Med 2017;376:1921–32. 10.1056/NEJMoa1702079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen P, Pagnoux C, Mahr A, et al. Churg-Strauss syndrome with poor-prognosis factors: a prospective multicenter trial comparing glucocorticoids and six or twelve cyclophosphamide pulses in forty-eight patients. Arthritis Rheum 2007;57:686–93. 10.1002/art.22679 [DOI] [PubMed] [Google Scholar]
- 9.Samson M, Puéchal X, Mouthon L, et al. Microscopic polyangiitis and non-HBV polyarteritis nodosa with poor-prognosis factors: 10-year results of the prospective CHUSPAN trial. Clin Exp Rheumatol 2017;35 Suppl 103:176–84. [PubMed] [Google Scholar]
- 10.Puéchal X, Pagnoux C, Baron G, et al. Adding azathioprine to remission-induction glucocorticoids for eosinophilic granulomatosis with polyangiitis (Churg-Strauss), microscopic polyangiitis, or polyarteritis nodosa without poor prognosis factors: a randomized, controlled trial. Arthritis Rheumatol 2017;69:2175–86. 10.1002/art.40205 [DOI] [PubMed] [Google Scholar]
- 11.Jones RB, Tervaert JWC, Hauser T, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med 2010;363:211–20. 10.1056/NEJMoa0909169 [DOI] [PubMed] [Google Scholar]
- 12.Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med 2010;363:221–32. 10.1056/NEJMoa0909905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guillevin L, Pagnoux C, Karras A, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med 2014;371:1771–80. 10.1056/NEJMoa1404231 [DOI] [PubMed] [Google Scholar]
- 14.Pepper RJ, Fabre MA, Pavesio C, et al. Rituximab is effective in the treatment of refractory Churg-Strauss syndrome and is associated with diminished T-cell interleukin-5 production. Rheumatology 2008;47:1104–5. 10.1093/rheumatology/ken175 [DOI] [PubMed] [Google Scholar]
- 15.Vaglio A, Strehl JD, Manger B, et al. IgG4 immune response in Churg-Strauss syndrome. Ann Rheum Dis 2012;71:390–3. 10.1136/ard.2011.155382 [DOI] [PubMed] [Google Scholar]
- 16.Carruthers MN, Topazian MD, Khosroshahi A, et al. Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis 2015;74:1171–7. 10.1136/annrheumdis-2014-206605 [DOI] [PubMed] [Google Scholar]
- 17.Ebbo M, Grados A, Samson M, et al. Long-term efficacy and safety of rituximab in IgG4-related disease: data from a French nationwide study of thirty-three patients. PLoS One 2017;12:e0183844 10.1371/journal.pone.0183844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammad AJ, Hot A, Arndt F, et al. Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Ann Rheum Dis 2016;75:396–401. 10.1136/annrheumdis-2014-206095 [DOI] [PubMed] [Google Scholar]
- 19.Thiel J, Troilo A, Salzer U, et al. Rituximab as induction therapy in eosinophilic granulomatosis with polyangiitis refractory to conventional immunosuppressive treatment: a 36-month follow-up analysis. J Allergy Clin Immunol Pract 2017;5:1556–63. 10.1016/j.jaip.2017.07.027 [DOI] [PubMed] [Google Scholar]
- 20.de Groot K, Gross WL, Herlyn K, et al. Development and validation of a disease extent index for Wegener's granulomatosis. Clin Nephrol 2001;55:31–8. [PubMed] [Google Scholar]
- 21.Mukhtyar C, Lee R, Brown D, et al. Modification and validation of the Birmingham vasculitis activity score (version 3). Ann Rheum Dis 2009;68:1827–32. 10.1136/ard.2008.101279 [DOI] [PubMed] [Google Scholar]
- 22.Hellmich B, Flossmann O, Gross WL, et al. EULAR recommendations for conducting clinical studies and/or clinical trials in systemic vasculitis: focus on anti-neutrophil cytoplasm antibody-associated vasculitis. Ann Rheum Dis 2007;66:605–17. 10.1136/ard.2006.062711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones RB, Ferraro AJ, Chaudhry AN, et al. A multicenter survey of rituximab therapy for refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2009;60:2156–68. 10.1002/art.24637 [DOI] [PubMed] [Google Scholar]
- 24.Specks U, Merkel PA, Seo P, et al. Efficacy of remission-induction regimens for ANCA-associated vasculitis. N Engl J Med 2013;369:417–27. 10.1056/NEJMoa1213277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comarmond C, Pagnoux C, Khellaf M, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): clinical characteristics and long-term followup of the 383 patients enrolled in the French vasculitis Study Group cohort. Arthritis Rheum 2013;65:270–81. 10.1002/art.37721 [DOI] [PubMed] [Google Scholar]
- 26.Besada E, Koldingsnes W, Nossent JC. Long-term efficacy and safety of pre-emptive maintenance therapy with rituximab in granulomatosis with polyangiitis: results from a single centre. Rheumatology 2013;52:2041–7. 10.1093/rheumatology/ket257 [DOI] [PubMed] [Google Scholar]
- 27.Smith RM, Jones RB, Guerry M-J, et al. Rituximab for remission maintenance in relapsing antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2012;64:3760–9. 10.1002/art.34583 [DOI] [PubMed] [Google Scholar]
- 28.Durel C-A, Berthiller J, Caboni S, et al. Long-term followup of a multicenter cohort of 101 patients with eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Arthritis Care Res 2016;68:374–87. 10.1002/acr.22686 [DOI] [PubMed] [Google Scholar]
- 29.Baldini C, Della Rossa A, Grossi S, et al. [Churg-Strauss syndrome: outcome and long-term follow-up of 38 patients from a single Italian centre]. Reumatismo 2009;61:118–24. [DOI] [PubMed] [Google Scholar]
- 30.Sablé-Fourtassou R, Cohen P, Mahr A, et al. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med 2005;143:632–8. 10.7326/0003-4819-143-9-200511010-00006 [DOI] [PubMed] [Google Scholar]
- 31.Groh M, Pagnoux C, Baldini C, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) (EGPA) consensus Task Force recommendations for evaluation and management. Eur J Intern Med 2015;26:545–53. 10.1016/j.ejim.2015.04.022 [DOI] [PubMed] [Google Scholar]
- 32.Calich AL, Puéchal X, Pugnet G, et al. Rituximab for induction and maintenance therapy in granulomatosis with polyangiitis (Wegener's). Results of a single-center cohort study on 66 patients. J Autoimmun 2014;50:135–41. 10.1016/j.jaut.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 33.Danieli MG, Cappelli M, Malcangi G, et al. Long term effectiveness of intravenous immunoglobulin in Churg-Strauss syndrome. Ann Rheum Dis 2004;63:1649–54. 10.1136/ard.2003.015453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seeliger B, Förster M, Happe J, et al. Interferon-α for induction and maintenance of remission in eosinophilic granulomatosis with polyangiitis: a single-center retrospective observational cohort study. J Rheumatol 2017;44:806–14. 10.3899/jrheum.160907 [DOI] [PubMed] [Google Scholar]
- 35.Lyons P, Peters J, Alberici F, et al. Genetically distinct clinical subsets, and associations with asthma and eosinophil abundance, within eosinophilic granulomatosis with polyangiitis. bioRxiv 2018. [Google Scholar]
- 36.Emmi G, Rossi GM, Urban ML, et al. Scheduled rituximab maintenance reduces relapse rate in eosinophilic granulomatosis with polyangiitis. Ann Rheum Dis 2018;77:952–4. 10.1136/annrheumdis-2017-211897 [DOI] [PubMed] [Google Scholar]


