Short abstract
Objective/background
This study aimed to review the current evidence on the application of telerehabilitation in occupational therapy practice and its clinical outcomes over the last 10 years.
Methods
A systematic review was performed on studies published in English in the decade 2008 to 2017, retrieved from seven electronic databases (MEDLINE, Cochrane Library, CINAHL, Web of Science, SAGE, Science Direct and EMBASE). Only articles evaluating the use of telerehabilitation to provide occupational therapy services from a distance were included, with no restrictions on pathology, impairment, age, or the nature of occupational therapy intervention.
Results
Fifteen articles (three randomised controlled trials, eight quasi-experimental studies, one trial with single-group post-intervention and three case studies) were reviewed. Despite various study designs and outcome measures, most studies indicated positive therapeutic effects of using telerehabilitation in occupational therapy practice. There is insufficient evidence, however, to confirm that telerehabilitation is more effective than the face-to-face model. Little evidence was shown on the long-term effect and cost efficacy. Only two studies used smartphones in their applications.
Conclusion
Telerehabilitation offers an alternative service delivery model for occupational therapy, not only bridging distance but also offering user-friendly treatment for patients at home. Further research, particularly on the use of the most cutting-edge mobile technology, is needed to determine effectiveness in occupational therapy practice treating various diseases, conditions and impairments and the characteristics of patients, interventions and therapists that lead to the best fit with this alternative and emerging form of service delivery.
Keywords: Telerehabilitation, occupational therapy, systematic review
Introduction
Around 55.4% of occupational therapists deliver services directly through face-to-face treatment in a medical setting (American Occupational Therapy Association, 2010). However, face-to-face occupational therapy (OT) services face challenges. Increasing demand for long-term rehabilitation and a dwindling supply of OT services in rural areas limit clients’ access (Centers for Disease Control and Prevention, 2015; Criss, 2013; Dorsey et al., 2007; Gardner, Bundy, & Dew, 2016). Long traveling times add to the heavy workloads of occupational therapists (Nix & Comans, 2017). Long travel time and distance, complicated service structure and the cost of intensive clinic-based interventions hinder clients’ access (Chen et al., 2013; Gardner et al., 2016; Shimabukuro, Grosse, & Rice, 2008). An alternative service delivery model for OT is needed to overcome these barriers while also improving accessibility and promoting well-being and recovery.
Telerehabilitation (TR) was first used in 1998. It refers to the use of information and communication technologies to provide rehabilitation services at a distance. The technologies used include internet-based media or programs, computers, videoconferencing, telephones, smartphones, applications, data transmission through video and photos or email sent by the healthcare provider and/or the client (Brennan et al., 2010; Kairy, Lehoux, Vincent, & Visintin, 2009; McCue, Fairman, & Pramuka, 2010). TR can be broadly divided into ‘synchronous’ – the provider and patients are connected at the same time, but located at different places, or ‘asynchronous’ – the provider and patients are not connected at the same time but using ‘store-and-forward’ data transmission, which may include video clips, digital photos, virtual technologies and other forms of electronic communication (Cason, Hartmann, Jacobs, & Richmond, 2013). TR is not a new phenomenon since internet communication was developed in the late 1990s; however, technological advances have expanded options including the use of mobile technologies since the introduction of smartphones in the commercial market in the mid-late 2000s. TRs emphasis not only on the use of the internet and telephones, but also other mobile technology, is now possible through the development of wearable sensing technology and its application in clinical practice for some common disorders related to motor rehabilitation, mental health, general health and physiological well-being. This means that monitoring and treatment outcomes can be addressed in the community and out of purely clinical settings. It is becoming increasingly evident that TR can improve access to rehabilitation services, prevent unnecessary delays in the receipt of care (Cason, 2014) and reduce the impact of shortages of rehabilitation professionals in underserved areas (Cason, 2012). Reviews have also found that TR has similar clinical outcomes to in-person interventions (Kairy et al., 2009).
In 2014, the World Federation of Occupational Therapists acknowledged TR as an appropriate service delivery model for OT services. ‘Occupational therapy practitioners use telehealth as a service delivery model to help clients develop skills; incorporate assistive technology and adaptive techniques; modify work, home, or school environments; and create health-promoting habits and routines’ (Cason et al., 2013, p. S69). TR also include tele-evaluation in OT such as the use of low-cost traditional telephone system for conducting phone interview as an alternative for cognitive assessment, wheelchair and assistive device prescription and home modification, etc. (Cason et al., 2013). Patients and caregivers are satisfied and have positive attitudes toward the use of TR in OT services (Cason, 2009; Gardner et al., 2016). Previous reviews of the effectiveness of TR in relation to various pathologies and impairments, healthcare utilisation and cost of rehabilitation use have found that TR has similar clinical outcomes to face-to-face rehabilitation services (Amatya, Galea, Kesselring, & Khan, 2015; Block et al., 2016; Dorstyn, Mathias, & Denson, 2013; Huang et al., 2015; Johansson & Wild, 2011; Kairy et al., 2009; Khan, Amatya, Kesselring, & Galea, 2015; Rogante, Grigioni, Cordella, & Giacomozzi, 2010; Santos et al., 2014). However, to date, no review has been conducted on the effects of TR in OT practice. The aim of this study was to review the current evidence on the application of TR and its clinical outcomes in OT practice.
Methods
Search strategy
Considering the advances in mobile technology over the last 10 years, it was decided to limit the systematic literature search to articles published between January 2008 and October 2017. Studies were identified using seven electronic databases, namely MEDLINE, Cochrane Library, CINAHL, Web of Science, SAGE, Science Direct and EMBASE. The following keywords were used: ‘Telerehabilitation’, ‘Tele-rehabilitation’, ‘Telemedicine’, ‘Telehealth’, ‘eHealth’, or ‘mobile health or mHealth’, and ‘Occupational Therapy’. Additional methods included manual searches of all the reference lists of articles identified as relevant.
Selection criteria
Only studies published in English whose full text was available were selected. All clinical trials evaluating the use of TR to provide OT services from a distance were considered, with no restrictions on pathology, impairment, age or the nature of OT intervention.
Overviews of the application of TR in OT, systematic reviews, meta-analyses, duplicates and studies unavailable in full were excluded. Also excluded were studies examining the development of technology systems, the reliability and validity of assessment, application in continuing professional development and treatment carried out by multidisciplinary teams focusing on the implications of TR in rehabilitation services.
Methodological quality assessment
The Physiotherapy Evidence Database (PEDro) scale was used to measure quality (Maher, Sherrington, Herbert, Moseley, & Elkins, 2003). All randomised controlled trial (RCT) studies were further rated using the PEDro Scale. PEDro score at 6–10 was considered as a high methodological quality of RCT, but it was not part of the selection criteria for this study.
Results
Study selection
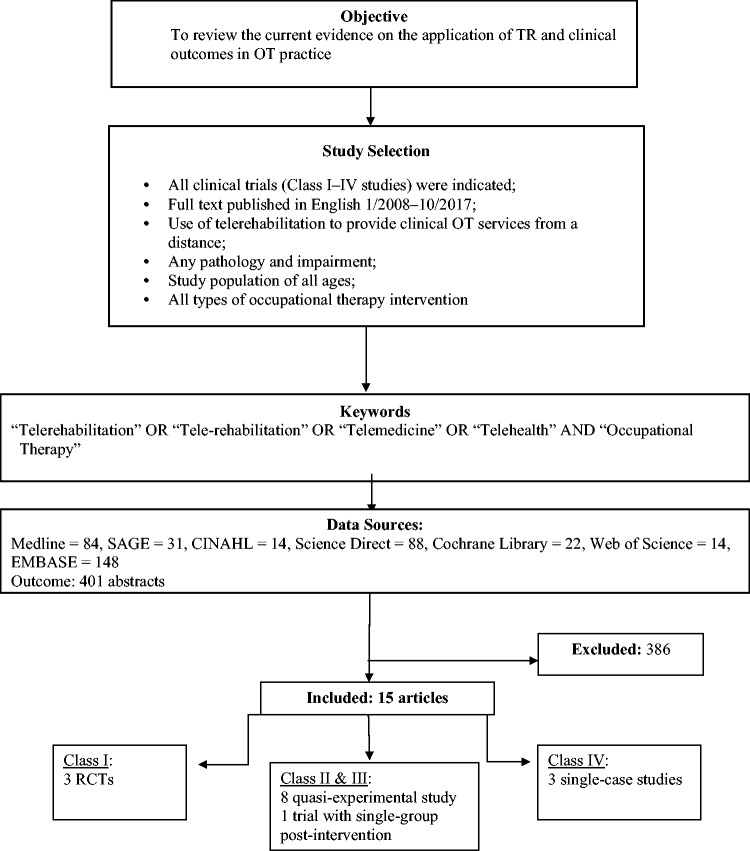
Four hundred one articles were identified from seven databases: MEDLINE (n = 84), SAGE (n = 31), CINAHL (n = 14), Science Direct (n = 88), Cochrane Library (n = 22), Web of Science (n = 14) and EMBASE (n = 148). Only 15 fulfilled all the selection criteria. The other studies were rejected after a review of their titles and abstracts. The main reasons for exclusion were duplication, treatment carried out by multidisciplinary teams focused on the implications of TR in rehabilitation services and absence of TR use for intervention or promotion of well-being (Figure 1).
Figure 1.
Flowchart of the literature review and recruitment process.
TR: telerehabilitation.
Studies’ characteristics
The designs of the 15 selected studies varied, according to the level of evidence by Moore, McQuay, and Gray (1995) with Level 1 indicating the strongest evidence and Level V the weakest evidence, there were eight quasi-experimental studies which were considered as Level III studies (Bergquist, Gehl, Lepore, Holzworth, & Beaulieu, 2008; Breeden, 2016; Criss, 2013; Gibbs & Toth-Cohen, 2011; Golomb et al., 2010; Lawson, Tang, & Feng, 2017; Ng, Polatajko, Marziali, Hunt, & Dawson, 2013; Nix & Comans, 2017), three single-case studies which were Class IV (Boehm, Muehlberg, & Stube, 2015; Hermann et al., 2010; Reifenberg et al., 2017), one trial with single-group post-intervention which belonged to Class III (Yuen & Pope, 2009) and three RCT studies that were Level II (Ferre et al., 2017; Hegel et al., 2011; Linder et al., 2015). As noted above, the RCT studies were further rated using the PEDro scale. The study by Ferre et al. (2017) scored 7 and that by Linder et al. (2015) rated 6 which were considered to be high quality and one (Hegel et al., 2011) was considered to be fair (Table 1).
Table 1.
PEDro scale scores for each study.
| PEDro scale items | Ferre et al. (2017) | Linder et al. (2015) | Hegel et al. (2011) |
|---|---|---|---|
| Eligibility | Yes | Yes | Yes |
| 1. Random allocation | 1 | 1 | 1 |
| 2. Concealed allocation | 1 | 0 | 0 |
| 3. Baseline comparability | 1 | 1 | 1 |
| 4. Blind subjects | 0 | 0 | 0 |
| 5. Blind therapists | 0 | 0 | 0 |
| 6. Blind assessors | 1 | 1 | 0 |
| 7. Adequate follow-up | 0 | 0 | 0 |
| 8. Intention-to-treat analysis | 1 | 1 | 0 |
| 9. Between-group comparisons | 1 | 1 | 1 |
| 10. Point estimated variability | 1 | 1 | 1 |
| Score | 7/10 | 6/10 | 4/10 |
| Quality | High | High | Fair |
PEDro Scale: Physiotherapy Evidence Database Scale; RCT: randomised controlled trial.
Participants’ characteristics
A total of 198 participants were included in this review. Sample size ranged from 1 to 99 participants. One study discussed occupational therapists’ cost effectiveness, and therefore no participants were counted (Nix & Comans, 2017).
The age of participants ranged from two years and six months to over 70. Five studies were conducted with participants aged under 18 (Bergquist et al., 2008; Criss, 2013; Ferre et al., 2017; Gibbs & Toth-Cohen, 2011; Golomb et al., 2010; Reifenberg et al., 2017; Yuen & Pope, 2009), three with elderly aged over 65 (Boehm et al., 2015; Breeden, 2016; Nix & Comans, 2017) and seven studies involved adults aged ≥18 (Bergquist et al., 2008; Hegel et al., 2011; Hermann et al., 2010; Lawson et al., 2017; Linder et al., 2015; Ng et al., 2013; Yuen & Pope, 2009).
The pathologies of the participants varied. They included hemiplegic cerebral palsy (Ferre et al., 2017; Golomb et al., 2010; Reifenberg et al., 2017), stroke (Boehm et al., 2015; Hermann et al., 2010; Lawson et al., 2017; Linder et al., 2015), acquired brain injury (Bergquist et al., 2008), traumatic brain injury (Ng et al., 2013), breast cancer survivors undergoing chemotherapy (Hegel et al., 2011), tetraplegia (Yuen & Pope, 2009), community-dwelling older adults (Breeden, 2016), orthopaedic issues (Nix & Comans, 2017), autism spectrum disorders (Gibbs & Toth-Cohen, 2011) and visual-motor and/or fine motor deficits (Criss, 2013).
All the participants received TR at home, with one exception, who received TR in a community centre (Ng et al., 2013).
Eight studies required the involvement of a significant other (parent or caregiver) in the provision of TR. Their roles included participation in assessment, assisting in treatment implementation and support and monitoring. A summary of participant characteristics is given in Table 2.
Table 2.
Characteristics of the participants recruited to each study.
| Author (Year)(Country) | Application (Model of Care) | Population | Total no. of participants (n) | No. of Experimental gps (n) | No. of Control gps (n) | Aged (y.o.) Mean ± SD | Settings to Received TR | Significant others Required and role |
|---|---|---|---|---|---|---|---|---|
| Criss (2013) (USA) | FM and VP Tx (tele-intervention) | Students with VM and/or FM deficits that impact handwriting skills | 8 | 8 | 0 | 6–11 y.o. (grades 1–6) | Home | Yes (parent)• directing if needed- follow• up on suggestions and Tx |
| Gibbs and Toth-Cohen (2011) (USA) | Sensory diet (tele-consultation) | Children with ASD | 4 | 4 | 0 | 5–12 y.o. | Home | Yes (parent)
|
| Reifenberg et al. (2017) (USA) | Hand function Tx (tele-consultation, tele-monitoring) | Children with spastic haemiparetic CP | 1 | 1 | 0 | 5 y.o. | Home | Yes (parent)
|
| Ferre et al. (2017) (USA) | Hand function Tx (tele-monitoring) | Children with unilateral spastic CP (mild to moderate impairment) | 24 | 12 | 12 | 2 y.o. 6 mo–10 y.o. 1 moTgp: m = 5.2 +2.7Cgp: m = 5.8 + 2.3 | Home | Yes (caregivers)
|
| Nix and Comans (2017) (Australia) | Home modification (tele-intervention) | Patients awaiting discharge home from inpatient medical and orthopaedic ward | NA | NA | NA | Elderly aged over 70 | Three community and rural hospitals | Yes (patient’s family member)
|
| Breeden (2016) (USA) | Home safety education (tele-education) | Community-dwelling older adults | 6 | 0 | 0 | >65 y.o. | Home | No |
| Linder et al. (2015) (USA) | Home-based Robot-assist with Home Exercise Program (tele-monitoring) | Subacute stroke | 99 | 51 | 48 | Tgp: m = 59.4 ± 13.6Cgp: m = 55. 5± 12.6 | Home | Yes (caregiver)
|
| Boehm et al.(2015) (USA) | Energy Conservation with Fatigue Management (tele-education) | Mild to moderate stroke with post-stroke fatigue | 1 | 1 | 0 | 70 y.o. | Home | No |
| Hegel et al. (2011) (USA) | Disability Prevention Program(tele-education) | Breast cancer survivors undergoing chemotherapy | 31 | 15 | 16 | m = 52.6 ± 9.4 y.o. | Home | No |
| Hermann et al. (2010) (USA) | Application of FES to engage in purposeful activity Tx (tele-intervention) | Stroke | 1 | 1 | 0 | 62 y.o. | Home | No |
| Ng et al. (2013) (Canada) | CO-OP Tx (tele-intervention) | Adult with TBI | 3 | 3 | 0 | 34 y.o., 47 y.o., 55 y.o. | 2/3 at Home1/3 community center | Yes (caregiver)
|
| Lawson et al. (2017) (USA) | Upper Limbs Home Program(tele-monitoring) | Chronic Stroke Survivors | 6 | 6 | 0 | m = 53 y.o. | Home | Yes (caregiver)
|
| Golomb et al. (2010)(USA) | Virtual Reality Video Game-based Home Program(tele-monitoring) | Severe hemiplegic CP | 3 | 3 | 0 | m = 14 y.o. | Home | No |
| Yuen and Pope (2009)(USA) | Oral Care Tx(tele-intervention) | Adult with tetraplegia | 2 | 2 | 0 | 42 y.o., 46 y.o. | Home | No |
| Bergquist et al. (2008) (USA) | Cognitive Tx(tele-intervention) | Individuals with ABI with memory impairment | 10 | 10 | 0 | m = 45.5 + 11.4 y.o | Home | No |
n: number; y: years; gp: group; y.o.: years old; VM: visual motor; FM: fine motor; ASD: autism spectrum disorders; CP: cerebral palsy; ax: assessment; tx: training; mo: months; Tgp: telerehabilitation group; Cgp: control group; m: mean; NA: not applicable; TBI: traumatic brain injury; CO-OP: Cognitive Orientation to daily Occupational Performance; ABI: acquired brain injury.
Characteristics of telerehabilitation
The technologies used in the studies are shown in Table 3. A range of hardware and software was used for videoconferencing, training, monitoring and assessment and/or recording.
Table 3.
Summary of studies investigating the use of telerehabilitation in OT practice.
| Author(Year) | Study design | Description of program technology used | Type of TR | Treatment activities | Treatment regime (Duration per session/frequency/length of intervention) | Outcome measures (Modality in conduct assessment) |
|---|---|---|---|---|---|---|
| Criss (2013) | One gp pretest–posttest quasi-experimental | • Internet-based PC and web camera• Internet-based ax tool: The Print Tool™ | Synchronous | Set up:• Extensive tool kit sent to client’s home in advanceTR:• A variety of interactive activities selection, explanation, demonstration and practice with occupational therapist via web camera• Consultation provided to parent at the end of each session• Parent assisted in guiding and directing if needed, follow-up on suggestions and tx | • 30 min• weekly• 6 wks | • Satisfaction questionnaire administered to parents and students• handwriting performance ax by The Print Tool™(Pretest–posttest tele-ax done at home) |
| Gibbs and Toth-Cohen (2011) | One gp pretest–posttest quasi-experimental | • Website for internet conferencing using webcam• Sessions were archived via website | Synchronous and asynchronous | Set up:• First clinical OT tx conducted in terms of ax, parent education and transfer skillsTR:• Reviews home program, observed parent–child interaction, techniques demonstration, rational explanation via website on sensory diet implementation | First attend clinical OT Tx:• 30 min• weekly• 4 wksFollowed by TR:• 30 min• weekly• 6 wks | • SPM Home form• Parents’ report/interview• OT report through progress notes(Pretest–posttest ax done clinic) |
| Reifenberg et al. (2017) | Pre- and post- single-case study | • Web-based video game: Timocco with videoconferencing• Telepresence robot (Kubi) with back-end control, webcam, iPad and Bluetooth• Data retrieved from the Timocco platform | Synchronous and asynchronous | Set up:• Necessary equipment for GbN and TT shipped to participantTR:• Treatment at home with Timocco, program monitored weekly by researchers• Consultation for participants and parents through TR | Use of Timocco:- 1 h-daily- 8 wksConsultation:• 30 min• weekly• 8 wksProgress monitoring• weekly | • AHA• BOT-2• QUEST• PMAL• PEDI-CAT• PSS-14• GbN performance metrics• Informal questionnaires• parent and child interviews• Session notes(Pretest–posttest ax done in clinic; Time for ax: ∼ Pretest: 2 wks before tx ∼Posttest: 2 wks after tx) |
| Ferre et al. (2017) | RCT: Pretest–posttest control gp | • monitoring via webcam-based software: Adobe Connect• Synchronous and asynchronous | Set up:• Supply and training on BBT and AHA provided to caregivers in advance• Training on caregiver-administrated ax and tx provided in advanceTgp:• Performed H-HABIT tx• supervised and monitored via checking log submission online by occupational therapistCgp• performed intensive tx on lower-limb through Adobe Connect | Training on caregiver-administrated ax and tx:• 1 h• total 2 sessions• TR Tx:• 2 hr• 5 days/week• 9 wks | • BBT• AHA• COPM• (Ax done at home by caregiver; Time for ax: ∼Pretest∼Posttest ∼FU: 6 months after posttest) | |
| Nix and Comans (2017) | Pretest–posttest quasi-experimental | • Smartphone• Video phone calling apps: Skype on PC/tablet | Synchronous and asynchronous | Set up:• The instruction booklet designed to educate patients, families, carers, and new staff on the correct method of measuring a property in development phase• Upgrade staff phones to smartphones with data plan, purchase of tablets in advanceTR:• Pre-discharge home visit conducted through ‘Home Quick’ included Virtual Home Visit/ax with family present and OT present remotely | • One-time home visit• Comparison between two six-month periods(2–8/2013 and2–8/2014) | • No. of OT interventions on acute inpatient wards• Time taken to complete the home visit from time of referral• No. of home visits conducted (Pretest–posttest ax done in situ) |
| Breeden (2016) | One gp pretest–posttest quasi-experimental | • Videoconferencing via web-based VSee software program with PC/iPad• Digital camera or cell phone used for taking photographs sent through email or text message• Sessions were audio/video recorded using Vsee and transcribed using Microsoft Word® | Synchronous and Asynchronous | Set up:• Participant-generated digital photographs were sent to OT prior to each session through email/text messageTR:• Narrative learning about home safety through video conference• A new photo assignment was given based on the discussion for next session | • weekly• 3 wks | • SAFER-HOME v3(Pretest–posttest ax conducted through home visit) |
| Linder et al. (2015) | RCT:Pretest–posttest control gp | • Remote progress monitor via phone call, cellular connection to the Mentor Home™ website• Synchronous and asynchronous | Set up:• Home visit for education conducted before the home programTgp:• Hand Mentor Pro robot-assisted device coupled with HEP• Progress monitored from websites and weekly phone call to FU progressCgp:• HEP• Weekly phone call to FU progress | Tgp:• 3 h (2 h in robot-assisted device, 1 h HEP• 5 days/week• 8 wksCgp:• 3 h on HEP• 5 days/week• 8 wks | • SIS (QoL)• CES–D (Pretest–posttest ax done through home visit) | |
| Boehm et al. (2015) | Pretest–posttest single-case study | • Teleconference through home/office phone | Synchronous | Set up:• The Managing Fatigue course handouts sent before tx beganTR:• Course conducted through phone call made with OT• Client required to complete homework after each phone call | • 1 h• Weekly• 5 wks | • FIS• COPM• Question on perception of teleconferencing delivery (Pretest–posttest ax done via tele-phone) |
| Hegel et al. (2011) | RCT:pretest–posttest control gp | • Telephone | Synchronous | Set up:• Program manual mailed to participants in Tgp in advanceTgp:• Problem solving and OT intervention program through phoneCgp• Attended usual care without problem solving and OT intervention program | Tgp:• weekly• 6 wks | • Satisfaction survey• SF-36• FACT-36• HADS• Healthy activities attendance record(Ax done via mail; Time for ax: ∼ pretest ∼ posttest: 6 wks ∼ FU: 6 wks after posttest) |
| Hermann et al. (2010) | Pretest–posttest single case study | • Logitech Buddy Cams, Skype through PC | Synchronous | Set up:• 1 h education and FES fitting done in laboratory in advanceTR:• Tx supervised by OT on line | 1st wk:• 10 min, with 5 min increased each day for first five days2nd–4th wk:• 30 min• 2 times/week• 4 wks | • FM scale• ARA• COPM(Pretest–posttest ax done in labTime for ax: ∼ pretest: 1 wk before tx ∼ posttest: 1 wk after tx) |
| Ng et al. (2013) | One gp pretest–posttest quasi-experimental | Videoconferencing using Skype in PC with Logitech™ webcams and noise-cancelling headsets• Session record using Pamela for Skype™ Professional version• Telephone | Synchronous | Set up:• Webcam, headphones and materials provided in advance• One training session on software and hardware set-up use through telephone and videoconference prior to axTR:• Tx provided through videoconference and telephone | • 1 h• Twice a week• 10 wks | • COPM• DEX• MPAI-4-P• QoL• Feedback interview• (Ax done via videoconferencing with participants and telephone with significant others;Time for ax: ∼ pretest ∼ posttest ∼ FU: 3 months) |
| Lawson et al. (2017) | One gp pretest–posttest quasi-experimental | • Mobile app: ARMStrokes through smartphone | Asynchronous | Set up:• App and exercise program installed and selected by OT in advanceTR:• Use of the app was monitored from website. Therapists contacted participants who demonstrated limited use of the app• At wk 3, participants were seen for adjustments | • 6-wk protocol | • ARAT• CAHAI• AM-PAC• MAS• MMT• General fatigue scale (Pretest–posttest ax done in clinic) |
| Golomb et al. (2010) | One gp pretest–posttest quasi-experimental | • Internet-based video game system that included a 5DT 5 Ultra Glove and PlayStation3 and networked to hospital/research centre through DSL modem/router | Asynchronous | Set up:• One time several hour introductory sessions about the games conducted two months in advance• System installed at home by research team in advanceTR:• Performance monitored remotely through website | • 30 min• 5 days/week• 3 months | • Sammons Preston Jamar dynamometer• Pinchometer• BOT• Jebsen Hand Function Test• Remote assessment based on sensor glove reading on finger ROM• DXA• pQCT• fMRI of hand grip task(Pretest–posttest ax done included remotely and clinic) |
| Yuen and Pope (2009) | Trial with post-intervention ax | • Videoconferencing via Acrobat® Connect™ Professional with high-speed internet | Synchronous | • Repeated training, supervised practice of oral hygiene and immediate corrective feedback and positive reinforcement in use of adaptive oral hygiene devices for the participants via videoconferencing | • 20–30 min• weekly• 4 wks | • OHTQ• In-depth interview(Posttest ax done via videoconferencing) |
| Bergquist et al. (2008) | One gp pretest–posttest quasi-experimental | • Internet-based cognitive training through instant messaging system | Synchronous | Set up:• One face-to-face training session on how to use the instant messaging system in advanceTR:• Online cognitive therapy with OTCalendar used to assist in remembering to attend therapy sessions | • weekly• 10 wks | • RBANS• WRAT-3 (Reading sub-test)• Attendance record(Pretest-posttest ax done in clinic) |
n: number; gp: group; tx: training or intervention; min: minutes; ax: assessment; h(s): hour(s); wk(s): week(s); TR: telerehabilitation (program); prog: program; OT: occupational therapy; PC: personal computer; SPM: sensory processing measure; AHA: Assisting Hand Assessment; BOT-2: Bruininks–Oseretsky Test of Motor Proficiency, Second Edition; QUEST: Quality of Upper Extremity Skills Test; PMAL: Pediatric Motor Activity Log; PEDI-CAT: Pediatric Evaluation and Disability Inventory–Computer Adapted Test; PSS-14: Perceived Stress Scale; GbN: game-based neurorehabilitation; TT: telehealth technologies; BBT: Box and Blocks Test; COPM: Canadian Occupational Performance Measure; FU: follow-up; H-HABIT: home-based Hand-arm bimanual intensive therapy; Tgp: telerehabilitation group; Cgp: control group; fx: functional; SAFER-HOME: Safety Assessment for Function and the Environment for Rehabilitation – Health Outcome Measurement and Evaluation; SIS: Stroke Recovery domains of the Stroke Impact Scale; CES–D: Center for Epidemiologic Studies Depression Scale; FIS: Fatigue Impact Scale; MoCA: Montreal Cognitive Assessment; v: version; SF-36: Medical Outcomes Short Form-36; FACT-B: Functional Assessment of Cancer Therapy–Breast Cancer Version; HADS: Hospital Anxiety and Depression Scale; FM scale: Fugl-Meyer Scale; ARA: Action Research Arm Test; FES: Functional Electrical Stimulation; DEX: The Dysexecutive Questionnaire; MPAI-4-P: The Mayo-Portland Adaptability Inventory–4 Participation Index; QoL: The Flanagan’s Quality of Life Scale; app: application; CAHAI: Chedoke Arm and Hand Activity Inventory; AM-PAC: Boston University’s Activity Measure–Post Acute Care Short Form; MAS: Modified Ashworth Scale; MMT: manual muscle tests; DXA: dual-energy X-ray absorptiometry; pQCT: peripheral quantitative computed tomography; fMRI: functional magnetic resonance imaging; ROM: range of motion; OHTQ: Oral Home Telecare Questionnaire; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status; WRAT-3: Wide Range Achievement Test, 3rd ed.; DSL: digital subscriber line.
Table 4.
Summary of results of the included studies.
| Author (Year) |
Results |
||
|---|---|---|---|
| Participants | Other effects | Perception and acceptance on TR | |
| Linder et al. (2015) |
|
|
|
| Ferre et al. (2017) |
|
|
|
| Hegel et al. (2011) |
|
|
|
| Criss (2013) |
|
|
|
| Gibbs and Toth-Cohen(2011) |
|
|
|
| Reifenberg et al. (2017) |
|
|
|
| Nix and Comans (2017) |
|
|
|
| Breeden (2016) |
|
|
|
| Boehm et al. (2015) |
|
|
|
| Hermann et al. (2010) |
|
|
|
| Ng et al. (2013) |
|
|
|
| Lawson et al. (2017) |
|
|
|
| Golomb et al. (2010) |
|
|
|
| Yuen and Pope (2009) |
|
|
|
| Bergquist et al. (2008) |
|
|
|
NA: not mentioned; gp(s): group(s); tx: training or intervention; ax: assessment; TR: telerehabilitation (program); OT: occupational therapy; SPM: sensory processing measure; AHA: Assisting Hand Assessment; BOT-2: Bruininks–Oseretsky Test of Motor Proficiency, 2nd ed.; QUEST: Quality of Upper Extremity Skills Test; PMAL: Pediatric Motor Activity Log; PEDI-CAT: Pediatric Evaluation and Disability Inventory–Computer Adapted Test; PSS-14: Perceived Stress Scale; BBT: Box and Blocks Test; COPM: Canadian Occupational Performance Measure; FU: follow-up; mi: mean improvement; fx: function; Tgp: telerehabilitation group; Cgp: control group; SIS: Stroke Recovery domains of the Stroke Impact Scale; CES–D: Center for Epidemiologic Studies Depression Scale; FIS: Fatigue Impact Scale; SF-36: Medical Outcomes Short Form-36; FACT-B: Functional Assessment of Cancer Therapy–Breast Cancer Version; HADS: Hospital Anxiety and Depression Scale; FM scale: Fugl-Meyer Scale; ARA: Action Research Arm Test; DEX: The Dysexecutive Questionnaire; MPAI-4-P: The Mayo-Portland Adaptability Inventory–4 Participation Index; QoL: The Flanagan’s Quality of Life Scale; DXA: dual-energy x-ray absorptiometry; pQCT: peripheral quantitative computed tomography; fMRI: functional magnetic resonance imaging; CO-OP: Cognitive Orientation to Daily Occupational Performance.
Fourteen studies required initial preparation prior to implementation of intervention. Seven required the supply of necessary tools, equipment or handouts in advance and/or training on how to set up the equipment through tele-media (Boehm et al., 2015; Criss, 2013; Ferre et al., 2017; Hegel et al., 2011; Ng et al., 2013; Nix & Comans, 2017; Reifenberg et al., 2017). Eight studies required in-person sessions conducted either in clinics or in participants’ homes for set up and training on the use of equipment (Bergquist et al., 2008; Breeden, 2016; Ferre et al., 2017; Gibbs & Toth-Cohen, 2011; Golomb et al., 2010; Hermann et al., 2010; Lawson et al., 2017; Linder et al., 2015). One study (Nix & Comans, 2017) mentioned upgrading staff phones to smartphones with data plans.
The applications of TR in OT practice were diverse. They were applied in intervention or training (Bergquist et al., 2008; Boehm et al., 2015; Criss, 2013; Ferre et al., 2017; Ng et al., 2013; Yuen & Pope, 2009), consultation (Nix & Comans, 2017), education (Breeden, 2016; Gibbs & Toth-Cohen, 2011), prevention programme (Hegel et al., 2011) and use of assistive technology (Golomb et al., 2010; Hermann et al., 2010; Lawson et al., 2017; Linder et al., 2015; Reifenberg et al., 2017).
Intervention regime and length of study
Frequency, duration and length of intervention varied among the 15 studies. Eight performed TR on a weekly basis, two studies did so twice a week, three involved participation five times a week and one study was performed on a daily basis. In terms of the duration of each session, five studies involved sessions of 30 min, three studies were 1 h, one study was 2 h and one study was 3 h. Four studies did not specify duration (Bergquiset et al., 2008; Breeden, 2016; Hegel et al., 2011; Lawson et al., 2017). The length of intervention ranged from three weeks to three months. One study performed a one-time home visit for home modification (Nix & Comans, 2017).
Only three studies followed-up with their participants, after six months, at six weeks and three months after active intervention was completed (Ferre et al., 2017; Hegel et al., 2011; Ng et al., 2013).
Types of outcome measures
The outcome measures used included both standardised and non-standardised assessments of cognitive function, motor function, functional performance and quality of life (QoL). Satisfaction level, attendance records, therapists’ progress notes, bone dexterity and brain imaging results were also considered as outcome measures. One study (Nix & Comans, 2017) used the total number of interventions conducted as an outcome measure.
The outcome measures were assessed by investigators, occupational therapists, caregivers and participants. One study (Ferre et al., 2017) trained caregivers to conduct standardised assessments at home. In terms of modalities in conducting the assessment, six studies were assessed in clinics, four used tele-evaluation, two studies required OT performed during home visits and one was delivered by mail. Two studies (Golomb et al., 2010; Reifenberg et al., 2017) involved both remote and clinical assessment.
Effects of telerehabilitation in OT practice
Among the RCT studies, significant improvement in the TR group relative to the control group was found in functional performance among children with unilateral cerebral palsy, and in QoL and emotional status among breast cancer survivors undergoing chemotherapy. Greater improvement among TR groups than control groups was shown in dexterity for children with cerebral palsy and carry-out effects on emotional state for breast cancer survivors. Linder et al. (2015) found that both TR and control groups showed significant improvement in QoL among stroke survivors. One study found equal improvement in satisfaction with occupational performance in both groups (Ferre et al., 2017). There was no difference in the effects on bimanual performance and engaging in healthy activities (Ferre et al., 2017; Hegel et al., 2011).
For Level III–IV studies, all the studies demonstrated that applying TR to deliver OT services was feasible for various pathologies and age groups. Three studies (Hermann et al., 2010; Ng et al., 2013) showed significant improvement in functional performance. Five indicated positive effects in the improvement of participants’ occupational performance (Boehm et al., 2015; Criss, 2013; Gibbs & Toth-Cohen, 2011; Lawson et al., 2017; Yuen & Pope, 2009), increased carryover of home programs (Gibbs & Toth-Cohen, 2011; Hegel et al., 2011), increased motivation (Lawson et al., 2017; Reifenberg et al., 2017; Yuen & Pope, 2009), enhanced home safety (Breeden, 2016), enhanced hand function (Golomb et al., 2010; Hermann et al., 2010; Lawson et al., 2017; Reifenberg et al., 2017), improved cognitive function (Bergquist et al., 2008) and reduced parental stress (Gibbs & Toth-Cohen, 2011; Reifenberg et al., 2017). Ng et al. (2013) showed a significant carry-on effect of reduced impact of executive dysfunction on daily life among participants with traumatic brain injury.
Six studies measured the satisfaction of participants, parents and/or caregivers (Boehm et al., 2015; Criss, 2013; Hegel et al., 2011; Linder et al., 2015; Ng et al., 2013; Yuen & Pope, 2009). All participants and caregivers expressed satisfaction with the quality of their program and had a positive perception of TR. Two participants and one caregiver preferred face-to-face intervention if given the choice (Boehm et al., 2015; Ng et al., 2013). One study (Nix & Comans, 2017) indicated a significant increase in total OT intervention, including an increase in the number of patients seen earlier following referral and an increase in the number of inpatient intervention visits conducted.
Discussion
Study design
Little research has been conducted on the effectiveness of telerehabilitation in OT practice. According to the PEDro scale, only two of the RCTs (Ferre et al., 2017; Linder et al., 2015) reviewed in this study had good methodological quality. Twelve articles were one-group pretest–posttest quasi-experimental studies, single-group studies with-post intervention or case studies, designs which are indicative of low evidence.
Effects of telerehabilitation in OT practice
Two of the RCT studies found that TR groups had better effects than control groups and one study showed comparable improvement in both groups. However, there is insufficient evidence to confirm that the effects of TR are more effective than the face-to-face model due to the inadequate number of RCTs.
The use of TR in OT practice is feasible and has positive effects in improving various functions among different pathologies and age groups. However, the majority of the changes in most of the standardised assessments in Class II–IV studies did not exceed the minimum level for clinically important difference. It is difficult to generalise the results.
Only three studies (Ferre et al., 2017; Hegel et al., 2011; Ng et al., 2013) conducted follow-up evaluations. Only one (Nix & Comans, 2017) investigated all interventions with the same level of staffing in place after the application of TR. But this study did not provide enough evidence to make conclusive comments on long-term effects or cost efficiency. This could serve as a reference for future studies.
Participants and caregivers were satisfied and had positive attitudes toward the use of TR in OT services. The findings noted in this review are similar to those in previous studies on clients’ perception and acceptance of the application of TR in OT (Cason, 2009; Gardner et al., 2016), rehabilitation services (Bragadottir, 2008; Johansson & Wild, 2011; Kairy et al., 2009; Wakeford, 2002) and speech-language pathologists (Dunkley, Pattie, Wilson, & McAllister, 2010). Very few participants and caregivers expressed a preference for face-to-face intervention over TR. The client and caregiver characteristics that lead to the best fit with TR service delivery can be investigated further.
Feasibility
Bergquist et al. (2008) reported that clients with acquired brain injury involving memory impairment were able to participate in internet-based cognitive rehabilitation independently. However, due to the small sample size, caution should be taken against overgeneralising.
The studies indicate that it is necessary to provide initial preparation or training prior to OT intervention through TR, and to upgrade staff equipment and technical support in order to provide a successful service. Considering the popularity and affordability of smartphones, it is surprising that only two studies applying smartphone and/or applications were found (Lawson et al., 2017; Nix & Comans, 2017). The keyword ‘mobile technology’ brought up various articles that examine the development of smartphone applications for use in TR. But it may be necessary to await the development of more advanced technology to examine the effects of smartphone use in TR for OT practice. One study used the Skype app (Nix & Comans, 2017), but none used wearable devices for measurements or quantitative (such as kinematic data) and qualitative (such as video filming) feedback, or Bluetooth connection and data synchronising with smartphones.
There has been no discussion of the barriers to the development of TR related to legal uncertainty and malpractice insurance, cost effectiveness, data privacy and security or the reimbursement of services/payment related to TR.
Treatment regime
Because OT intervention is devised according to the client-specific functional strengths, needs and impairments, all the studies used different protocols, which is why no exact comparison of the intensity and length of the treatment regimes can be made. Further reviews could extend focus to the use of TR for different client-specific functional strengths, needs and impairments in OT practice.
Outcome measures
Most of the outcome measures used were questionnaires on tele-evaluation. Caregivers were trained to administer a standardised assessment in Ferre et al. (2017). Although the reliability of caregiver-administered assessments was examined at baseline, the reliability of the posttest and six-month follow-up were not assessed. Further research is needed to determine which OT assessments are appropriate for TR and the test–retest reliability of caregiver-administered standardised assessment.
Limitations
Limitations in the studies’ design included small sample size, inadequate control groups, and inadequate follow-up and report outcomes in the short term. It is difficult to confirm whether the effects of TR are comparable to or more effective than in-person intervention. The results serve as proof of principle that the application of TR in OT practice is an alternative service delivery model.
Four of 15 articles were retrieved through manual search (Ferre et al., 2017; Golomb et al., 2010; Lawson et al., 2017; Yuen & Pope, 2009). An overall lack of standardisation in the terminology used in OT and TR is noted and it is hard to identify relevant studies.
Conclusion
This systematic review shows that using TR in OT practice has positive therapeutic effects. TR offers an alternative service delivery model. Further trials with larger samples and more comprehensive follow-ups are needed. It is particularly important that more research is conducted on the use of cutting-edge mobile technology to determine its effectiveness in TR for various pathologies and impairments, its cost efficacy and the characteristics of clients, interventions and therapists leading to the best fit for this alternative form of service delivery.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Amatya B., Galea M. P., Kesselring J., Khan F. (2015). Effectiveness of telerehabilitation interventions in persons with multiple sclerosis: A systematic review. Multiple Sclerosis and Related Disorders, 4(4), 358–369. [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2010). Workforce trends in occupational therapy. Retrieved from http:www.aota.org/-/media/Corporate/Files/EducationCareers/Prospective/Workforce-trends-in-OT.PDF
- Bergquist T., Gehl C., Lepore S., Holzworth N., Beaulieu W. (2008). Internet-based cognitive rehabilitation in individuals with acquired brain injury: A pilot feasibility study. Brain Injury, 22(11), 891–897. [DOI] [PubMed] [Google Scholar]
- Block V. A. J., Pitsch E., Tahir P., Cree B. A. C., Allen D. D., Gelfand J. M. (2016). Remote physical activity monitoring in neurological disease: A systematic review. PLoS One, 11(4), 1–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm N., Muehlberg H., Stube J. E. (2015). Managing poststroke fatigue using telehealth: A case report. American Journal of Occupational Therapy, 69(6), 6906350020 pp1–7. doi:10.5014/ajot.2015.016170 [DOI] [PubMed] [Google Scholar]
- Bragadottir H. (2008). Computer-mediated support group intervention for parents. Journal of Nursing Scholarship, 40, 32–38. [DOI] [PubMed] [Google Scholar]
- Breeden L. E. (2016). Occupational therapy home safety intervention via telehealth. International Journal of Telerehabilitation, 8(1), 29–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan D., Tindall L., Theodoros D., Brown J., Campbell M., Christiana D., Smith D., Lee A. (2010). A blueprint for telerehabilitation guidelines. International Journal of Telerehabilitation, 2(2), 31–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cason J. (2009). A pilot telerehabilitation program: Delivering early intervention services to rural families. International Journal of Telerehabilitation, 1(1), 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cason J. (2012). Telehealth opportunities in occupational therapy through the Affordable Care Act. American Journal of Occupational Therapy, 66, 131–136. [DOI] [PubMed] [Google Scholar]
- Cason J. (2014). Telehealth: A rapidly developing service delivery model for occupational therapy. International Journal of Telerehabilitation, 6(1), 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cason J., Hartmann K., Jacobs K., Richmond T. (2013). Telehealth. American Journal of Occupational Therapy, 67, S69–S90. doi:10.5014/brhoffm.2013.67S69 [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Stroke facts and statistics. Retrieved from https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_stroke.htm
- Chen C. L., Kang L. J., Hong W. H., Chen F. C., Chen H. C., Wu C. Y. (2013). Effect of therapist-based constraint-induced therapy at home on motor control, motor performance and daily function in children with cerebral palsy: A randomized controlled study. Clinical Rehabilitation, 27(3), 236–245. [DOI] [PubMed] [Google Scholar]
- Criss M. J. (2013). School-based telerehabilitation in occupational therapy: Using telerehabilitation technologies to promote improvements in student performance. International Journal of Telerehabilitation, 5(1), 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey E. R., Constantinescu R., Thompson J. P., Biglan K. M., Holloway R. G., Kieburtz K., Tanner C. M. (2007). Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology, 68(5), 384–386. [DOI] [PubMed] [Google Scholar]
- Dorstyn D., Mathias J., Denson L. (2013). Applications of telecounselling in spinal cord injury rehabilitation: A systematic review with effect sizes. Clinical Rehabilitation, 27(12), 1072–1083. [DOI] [PubMed] [Google Scholar]
- Dunkley C., Pattie L., Wilson L., McAllister L. (2010). A comparison of rural speech-language pathologists’ and residents’ access to and attitudes towards the use of technology for speech-language pathology service delivery. International Journal of Speech-Language Pathology, 12(4), 333–343. [DOI] [PubMed] [Google Scholar]
- Ferre C. L., Brandão M., Surana B., Dew A. P., Moreau N. G., Gordon A. M. (2017). Caregiver‐directed home‐based intensive bimanual training in young children with unilateral spastic cerebral palsy: A randomized trial. Developmental Medicine & Child Neurology, 59(5), 497–504. [DOI] [PubMed] [Google Scholar]
- Gardner K., Bundy A., Dew A. (2016). Perspectives of rural carers on benefits and barriers of receiving occupational therapy via information and communication technologies. Australian Occupational Therapy Journal, 63(2), 117–122. [DOI] [PubMed] [Google Scholar]
- Gibbs V., Toth-Cohen S. (2011). Family-centered occupational therapy and telerehabilitation for children with Autism Spectrum Disorders. Occupational Therapy in Health Care, 25(4), 298–314. [DOI] [PubMed] [Google Scholar]
- Golomb M. R., McDonald B. C., Warden S. J., Yonkman J., Saykin A. J., Shirley B., Burdea G. C. (2010). In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Archives of Physical Medicine and Rehabilitation, 91(1), 1–8.e1. [DOI] [PubMed] [Google Scholar]
- Hegel M. T., Lyons K. D., Hull J. G., Kaufman P., Urquhart L., Li Z., Ahles T. A. (2011). Feasibility study of a randomized controlled trial of a telephone‐delivered problem-solving: Occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psycho‐Oncology, 20(10), 1092–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann V. H., Herzog M., Jordan R., Hofherr M., Levine P., Page S. J. (2010). Telerehabilitation and electrical stimulation: An occupation-based, client-centered stroke intervention. American Journal of Occupational Therapy, 64(1), 73–81. [DOI] [PubMed] [Google Scholar]
- Huang K., Liu W., He D., Huang B., Xiao D., Peng Y., Huang D. (2015). Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: A systematic review and meta-analysis. European Journal of Preventive Cardiology, 22(8), 959–971. [DOI] [PubMed] [Google Scholar]
- Johansson T., Wild C. (2011). Telerehabilitation in stroke care: A systematic review. Journal of Telemedicine and Telecare, 17(1), 1–6. [DOI] [PubMed] [Google Scholar]
- Kairy D., Lehoux P., Vincent C., Visintin M. (2009). A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disability and Rehabilitation, 31(6), 427–447. [DOI] [PubMed] [Google Scholar]
- Khan F., Amatya B., Kesselring J., Galea M. (2015). Telerehabilitation for persons with multiple sclerosis. The Cochrane Database of Systematic Reviews, 4 Retrieved from http://www.cochrane.org/CD010508/MS_telerehabilitation-for-persons-with-multiple-sclerosis [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson S., Tang Z., Feng J. (2017). Supporting stroke motor recovery through a mobile application: A pilot study. American Journal of Occupational Therapy, 71(3), 1–5. [DOI] [PubMed] [Google Scholar]
- Linder S. M., Rosenfeldt A. B., Bay R. C., Sahu K., Wolf S. L., Alberts J. L. (2015). Improving quality of life and depression after stroke through telerehabilitation. American Journal of Occupational Therapy, 69(2), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher C. G., Sherrington C., Herbert R. D., Moseley A. M., Elkins M. (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical Therapy, 83(8), 713–721. [PubMed] [Google Scholar]
- McCue M., Fairman A., Pramuka M. (2010). Enhancing quality of life through telerehabilitation. Physical Medicine and Rehabilitation Clinics of North America, 21(1), 195–205. [DOI] [PubMed] [Google Scholar]
- Moore A., McQuay H., Gray J. A. M. (1995). Evidence-based everything. Bandolier, 1(12), 1. [Google Scholar]
- Ng E. M. W., Polatajko H. J., Marziali E., Hunt A., Dawson D. R. (2013). Telerehabilitation for addressing executive dysfunction after traumatic brain injury. Brain Injury, 27(5), 548–564. [DOI] [PubMed] [Google Scholar]
- Nix J., Comans T. (2017). Home quick: Occupational therapy home visits using mHealth, to facilitate discharge from acute admission back to the community. International Journal of Telerehabilitation, 9(1), 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reifenberg G., Gabrosek G., Tanner K., Harpster K., Proffitt R., Persch A. (2017). Feasibility of pediatric game-based neurorehabilitation using telehealth technologies: A case report. American Journal of Occupational Therapy, 71(3), 1–8. [DOI] [PubMed] [Google Scholar]
- Rogante M., Grigioni M., Cordella D., Giacomozzi C. (2010). Ten years of telerehabilitation: A literature overview of technologies and clinical applications. Neurorehabilitation, 27(4), 287–304. [DOI] [PubMed] [Google Scholar]
- Santos M. T. N. D., Moura S. C. D. O., Gomes L. M. X., Lima A. H., Moreira R. S., Silva C. D., Guimaraes E. M. P. (2014). Telehealth application on the rehabilitation of children and adolescents. Revista Paulista de Pediatria, 32(1), 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimabukuro T., Grosse S., Rice C. (2008). Medical expenditures for children with an autism spectrum disorder in a privately insured population. Journal of Autism and Developmental Disorders, 38(3), 546–552. [DOI] [PubMed] [Google Scholar]
- Wakeford L. (2002). Using telehealth technology to provide services to children with special needs. OT Practice, 7(21), 12–16. [Google Scholar]
- World Federation of Occupational Therapists. (2014). World Federation of Occupational Therapists’ position statement on telehealth. International Journal of Telerehabilitation, 6(1), 37–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen H. K., Pope C. (2009). Oral home telecare for adults with tetraplegia: A feasibility study. Special Care in Dentistry, 29(5), 204–209. [DOI] [PubMed] [Google Scholar]