Abstract
Background:
Caterpillar hump of the right hepatic artery is a rare variation increasing the risk of vascular and biliary injuries during hepatobiliary surgery. The aim of this study is to record the cases of the right hepatic artery forming caterpillar hump in a cohort of patients underwent laparoscopic cholecystectomy and to report a review of the literature systematically conducted.
Methods:
We reviewed clinical and surgical video data of 230 patients with symptomatic cholelithiasis treated with laparoscopic cholecystectomy between January 2016 and August 2017. A systematic literature search in PubMed, Medline, Cochrane and Ovid databases until 30th June 2017 was also performed in accordance with the PRISMA statement.
Results:
Our institutional data indicated that 1.3% of 230 patients presented caterpillar hump right hepatic artery. The systematic review included 16 studies reporting data from a total of 498 human cadavers and 579 patients submitted to cholecystectomy. The overall proportion of surgical patients with the caterpillar hump right hepatic artery was 6.9%.
Conclusions:
Variations of the cystic artery are not just an anatomical dissertation, assuming a very crucial role in surgical strategies to avoid uncontrolled vascular lesions. A meticulous knowledge of the hepatobiliary triangle in association with all elements of ‘Culture of Safety in Cholecystectomy’ is mandatory for surgeons facing more than two structures within Calot's triangle.
Keywords: Calot's triangle variations, caterpillar hump of right hepatic artery, cystic artery variations, laparoscopic cholecystectomy, Moynihan's hump
INTRODUCTION
In the last three decades, minimally invasive cholecystectomy has been widely accepted as the gold standard procedure for the patients with symptomatic cholelithiasis.[1,2,3,4,5,6] However, in spite of excellent visualisation of the surgical field, less wound pain, better cosmesis and early return to daily activities, the laparoscopic approach is associated with a slightly increased risk of iatrogenic biliary injury and arterial haemorrhage.[7,8] Certain variations in biliary as well as vascular anatomy of gallbladder pedicle predispose to iatrogenic nightmares during cholecystectomy.[9] Interestingly, the reported incidence rate of conversion to open surgery due to vascular injuries is approximately 0%–1.9%,[10] with a mortality rate of 0.02%.[11,12] Although several variations in the origin and branching pattern of hepatobiliary triangle arteries have been reported,[1,11,13] the tortuous right hepatic artery configuring an insidious hump represents one of the most considerable and dangerous anomalies. In this extremely rare configuration called caterpillar hump or Moynihan's hump,[14,15] the right hepatic artery runs very close to the gallbladder and cystic duct, forming a U-shaped loop, where the cystic artery starts in exceptionally short fashion.[16] This route consistently predisposes to misidentification as well as vulnerability of vascular structures with inappropriate clipping or uncontrollable bleeding.[17]
On these basis, a meticulous knowledge of hepatobiliary triangle with the possible arterial and biliary variants in association with all elements of the ‘Culture of Safety in Cholecystectomy’ is essential to perform safe surgery and to avoid serious complications.[9,18] The aim of this retrospective study is to record the cases of the right hepatic artery forming caterpillar hump in a cohort of patients underwent surgical therapy for symptomatic cholelithiasis and to report, for the first time, a review of the literature systematically conducted with discussion of the cornerstones in surgical management.
METHODS
Study design and patients
In this retrospective and single-centre study, we retrieved the medical records of all patients who underwent laparoscopic cholecystectomy for symptomatic cholelithiasis (acute or chronic calculous cholecystitis and for biliary colic) who had no evidence of common bile duct stone or intrahepatic duct stone on pre-operative workup between January 2016 and August 2017 at the Department of General, Minimally Invasive and Robotic Surgery, ‘San Matteo degli Infermi’ Hospital, AUSL Umbria 2, Spoleto, Italy. Patients were admitted through outpatient department after completing full diagnostic workup consisted of biochemical tests of liver function as well as systemic inflammation and diagnostic imaging (abdominal ultrasonography). Post-operatively, all patients were checked with biochemical tests (complete blood cell count and liver function tests) at 1 day after surgery. All patients started oral food intake on 1st post-operative day and generally were discharged on 2nd post-operative day. The study was conducted according to the ethical standards of the Helsinki declaration and was approved by the institute's committee on human research. Each patient gave informed written consent.
Surgical procedure
The patient was positioned in the reverse Trendelenburg left lateral position under general anaesthesia. After establishing a 12-mm Hg pneumoperitoneum using a Veress needle, a four-port technique was used with a 5-mm 30° camera through a 12-mm trocar at the umbilicus to enable the surgeons to exchange instrument for specimen extraction. Three additional 5-mm trocars were placed in the right mid-abdomen: one for the surgeon's left grasper to hold the infundibulum in the left mid-abdomen, one for the surgeon's right hand to use a monopolar hook or Maryland dissector, and one in the xiphoid for assistant surgeon to retract the fundus of the gallbladder cranially over the liver. The dissection started with the assistant retracting the gallbladder fundus over the liver, and the surgeon holding and pulling laterally the infundibulum of the gallbladder with one hand. Using a monopolar hook, the visceral peritoneal reflection was taken down at the neck of the gallbladder. The section of Calot's artery (which connects the cystic artery to the cystic duct) permitted access to the critical safety triangle, set between the gallbladder walls on the right, the cystic duct inferiorly and the cystic artery on the left. The entire fatty dissection of this triangle using monopolar Maryland dissector and the mobilisation of the infundibulum, both anteriorly and posteriorly, allowed visualisation of the liver surface through the triangle, well above Rouviere's sulcus, as described by Strasberg et al.[19] After their identification, the cystic duct and artery were sectioned between proximally and distally placed Hem-o-lok® (Teleflex, Morrisville, NC, USA). In case of tortuous variant of the right hepatic artery configuring an insidious hump running very close to the gallbladder and cystic duct, the short cystic artery was gently hooked, clipped and divided freeing the right hepatic artery from the gallbladder [Figures 1 and 2]. The gallbladder was dissected from the liver bed using a hook and then placed in an Endo Catch™ bag (Covidien, Mansfield, MA, USA) and removed through the 12-mm trocar site. A subhepatic drain was positioned for 1 day.
Figure 1.
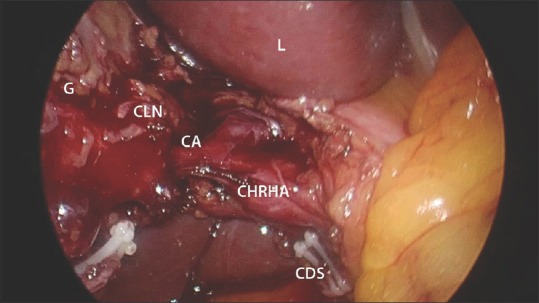
Intra-operative view of the right hepatic artery caterpillar hump. CA: Cystic artery, CDS: Cystic duct stump, G: Gallbladder, CLN: Cystic lymph node, CHRHA: Caterpillar hump right hepatic artery, L: Liver
Figure 2.
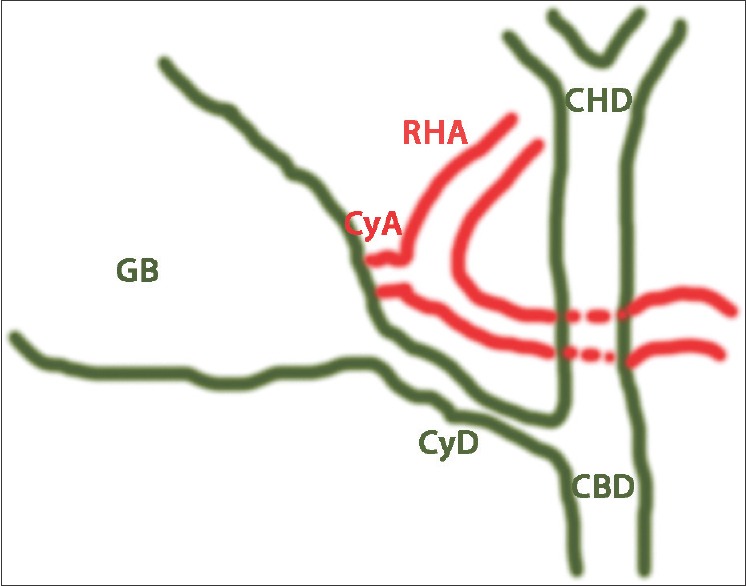
Schematic view of Figure 1. Relevant structures of the hepatic hilum and Calot's triangle are depicted. CyA: Cystic artery, CyD: Cystic duct, CBD: Common biliary duct, CHD: Common hepatic duct, GB: Gallbladder, RHA: Right hepatic artery
Data retrieval
The clinical as well as surgical video data of the eligible patients were retrieved and retrospectively reviewed. Age, sex, pre-operative diagnosis, surgical procedure and outcome of the patients were examined. In addition, perioperative parameters, including the right hepatic artery forming caterpillar hump, operative time, morbidity and length of hospitalisation, were recorded.
Systematic review method
In addition, a literature search in PubMed, Medline, Cochrane and Ovid databases of all articles published until 30th June, 2017 with the medical subject headings keywords ‘caterpillar hump of right hepatic artery’, ‘Moynihan's hump’, ‘cystic artery variations’, ‘right hepatic artery variations’, ‘aberrant cystic artery’, ‘aberrant right hepatic artery’, ‘vascular variations of gallbladder’, ‘Calot's triangle variations’, ‘cholecystectomy’ was carried out. The keywords were used in all possible combinations to retrieve the maximal number of articles. The bibliography of each selected article was reviewed for other potentially relevant citations. In the case of studies whose results were published more than once, data from the most recent article were considered.
The articles were then screened for the presence of the following inclusion criterion: adult patients with in vivo or post-mortem diagnosis of the right hepatic artery forming caterpillar hump. All types of study designs were included in this study. No exclusion criteria were applied. There were no language restrictions in the selection.
Statistical analysis
The continuous, normally distributed variables are presented as the median and range whereas categorical variables are presented as the number (per cent). All analyses were performed using SPSS 17 software package (SPSS, Inc., Chicago, IL, USA).
RESULTS
Between January 2016 and August 2017, 230 cases of laparoscopic cholecystectomy for symptomatic gallbladder stone were reviewed. About 102 patients (44.4%) were male and 128 (55.6%) were female, with a median age of 61 years (range 16–87). The patients were initially diagnosed with acute calculous cholecystitis (n = 38, 16.5%), biliary colic (n = 152, 66%) and chronic calculous cholecystitis (n = 40, 17.5%). All surgical procedures were performed electively. The median operation time was 62 min (range: 23–181 min).
In three of 230 patients (1.3%; 2 males and 1 female; median age: 61 years [range: 17–64]), the right hepatic artery presented a tortuous configuration arising from proper hepatic artery and coursed behind common hepatic duct. Inside the Calot's triangle, it made a characteristic unique loop with convexity facing upwards and to the right. The U-shaped loop configured an insidious hump running very close to the gallbladder and cystic duct, and the cystic artery resulted in exceptionally short fashion. The median operation time was 87 min (range: 62–181 min).
No conversion to open surgery was registered. The median hospital stay after surgery was 1.7 days (range: 1–4 days). All patients showed excellent post-operative recovery, and no post-operative major complication rate or 30-day mortality was observed.
Systematic review results
The initial search produced 107 studies. By checking the relevant bibliography, two additional articles were included in this study. The titles and abstracts of the records were screened, and after detailed evaluation, 16 studies published between 1976 and 2017 with a study period between 1972 and 2015, fulfilled criteria for eligibility [Table 1]. The included retrospective case–control studies concerned different cohorts of patients except for two studies[16,20] in which the same group may overlap [Figure 3].
Table 1.
Characteristics of included studies
| Author | Study period | Country of origin | Sample size (male/female ratio) | Age (years)a | Caterpillar hump RHA, n (%) | Relationship with CBD | Number of loops | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery | Cadaver | Surgery | Cadaver | Surgery | Cadaver | Anterior | Posterior | One | Two | |||
| El Maksoud[1] | 2014 | Saudi Arabia | 1 female | - | 38 years old | - | 1 | - | 1 | - | 1 | - |
| Kavitha Kamath[13] | 2008-2013 | India | - | 40 (NR) | - | NR | - | 2 (5) | - | 2 (100) | 1 (50) | 1 (50) |
| Jansirani et al.[15] | 2006-2011 | India | - | 60 (NR) | - | NR | - | 3 (5) | 1 (33.4) | 2 (66.6) | 1 (33.4) | 2 (66.6) |
| Al-Sayigh[20] | 2007-2008 | Iraq | 50 (8/42) | - | Range, 20-69 | - | 9 (6) | - | NR | NR | NR | NR |
| Badagabettu et al.[21] | 2012 | India | - | 1 male | - | 60 years old | - | 1 | - | 1 | 1 | - |
| Bergamaschi and Ignjatovic[22] | 1997 | Jugoslavia | - | 90 (47/43) | - | 59 (range, 26-83) | - | 9 (12.9)* | NR | NR | NR | NR |
| Dandekar et al.[23] | NR | India | - | 60 (56/4) | - | NR | - | 8 (13.3) | 4 (50) | 4 (50) | 2 (25) | 6 (75) |
| Eid et al.[24] | NR | Japan | - | 27 (NR) | - | NR | - | 1 (3.7) | 1 | - | 1 | - |
| Johnston and Anson[25] | 1952 | US | - | 35 (NR) | - | NR | - | 1 (2.8) | NR | NR | NR | NR |
| Mugunthan et al.[26] | 2012-2015 | India | - | 60 (NR) | - | Range, 50-80 | - | 2 (3) | 1 (50) | 1 (50) | 2 (100) | - |
| Sangameswaran and Devi[27] | NR | India | - | 60 (NR) | - | NR | - | 2 (3.3) | - | 2 | 2 | - |
| Balija et al.[28] | NR | Croatia | 200 (NR) | - | NR | - | 11 (5.5) | - | NR | NR | NR | NR |
| Bhargava et al.[29] | 2012 | India | 1 female | - | 25 years old | - | 1 | - | NR | NR | NR | NR |
| Dawani et al.[30] | NR | Pakistan | 136 (16/120) | - | 40.9±12.3 (range, 21-71) | - | 8 (5.9) | - | NR | NR | NR | NR |
| Scott-Conner and Hall[31] | 1992 | US | 51 (NR) | - | NR | - | 2 (3.9) | - | NR | NR | NR | NR |
| Benson and Page[32] | 1972-1975 | UK | 140 (NR) | 65 (NR) | NR | NR | 9 (6.4) | 5 (7.6) | NR | NR | NR | NR |
*Data on vascular anomalies were drawn from 70 of the 90 cadavers, aEither mean (SD) or median (range). NR: Not reported, RHA: Right hepatic artery, CBD: Common bile duct, US: United States of America, SD: Standard deviation
Figure 3.
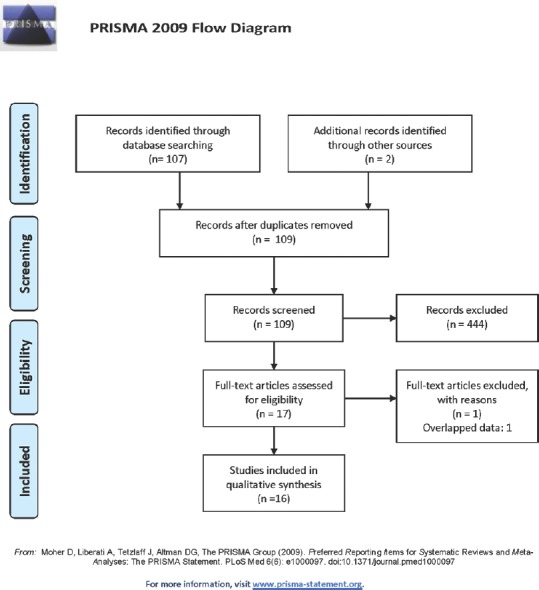
PRISMA flowchart of study selection
Nine studies[13,15,21,22,23,24,25,26,27] reported data from a total of 498 human cadavers used for anatomical dissection purpose ranging from 1[21] to 90[22] specimens per study; six studies[1,20,28,29,30,31] performed the research on a total of 579 patients submitted to cholecystectomy for symptomatic cholelithiasis, ranging from 1[1,29] to 200[28] patients per study [Table 1]. Only the study by Benson and Page[32] involved 140 patients submitted to cholecystectomy and 65 human cadavers as well. The majority of studies were conducted in single Eastern centres (188 cholecystectomies, 32.5% and 308 cadavers, 61.8%) (India, Saudi Arabia, Pakistan, Iraq, Japan),[1,13,15,20,21,22,23,24,26,27,29,30] while the five others were performed in the Western and American Countries (391 cholecystectomies, 67.5% and 190 cadavers, 38.2%) (United Kingdom, Yugoslavia, Croatia, USA).[22,25,28,31,32]
The overall proportion of surgical patients with the caterpillar hump right hepatic artery was 7% (41 patients) ranging from 3.9%[31] to 6.4%[32] patients per study. Similarly, the prevalence of caterpillar variation resulted in 6.8% of human cadavers, ranging from 3%[26] to 13.3%[23] specimens per study.
The global proportion of caterpillar hump right hepatic artery including in vivo as well as post-mortem cases was 6.9% (75 vascular anomalies on a total of 1077 cases).
Only eight articles[1,13,15,21,23,24,26,27] reported the relationship between the caterpillar hump and the common bile duct as well as the characteristics of loop configuration. The tortuous artery was found to route anteriorly to the common hepatic duct in 40% of cases and posteriorly in 60%, representing the posterior presentation the more common anatomical route. Furthermore, in 55% of cases, the vascular variation was reported in a single-loop fashion and in 45% the vascular humps were noted in a double-loop configuration.
DISCUSSION
From the introduction of open gallbladder surgery up to laparoscopic cholecystectomy, surgeons have been highly interested in the anatomy of the hepatobiliary triangle to perform a safe surgical procedure, and a great number of papers have been published to shed lights on this issue. Anatomic variations in and around the hepatobiliary triangle (biliary tree and cystic artery) are frequent[32,33] accounting for 20%–50% of the patients. As a consequence, the position and possible variations of the cystic artery are not only an anatomical dissertation but also assuming a very crucial role in surgical strategies, especially in laparoscopic settings, to avoid uncontrolled vascular lesions that usually lead to conversion.[28,32,33,34,35]
Furthermore, the route of cystic artery is difficult to establish before surgery, and it can be recognised only after careful dissection of Calot's triangle and the gallbladder.[23,28]
The incidence of caterpillar or Moynihan's hump of the right hepatic artery in previous reports ranged between 3% and 13.3%.[1,13,15,20,21,22,23,24,25,27,28,29,30,31,32] Its incidence in the present study was 1.3%, which is more or less comparable to the literature data. The aetiology of the caterpillar hump is still not well known. Taylor CR[36] theorised that the elongation as well as the tortuosity of the artery could be attributed to architectural distortion with corkscrewing of intrahepatic branches of hepatic artery in patients with cirrhosis of the liver. However, neither clinical nor statistical correlation has been demonstrated for this hypothesis. Furthermore, none of our three patients with caterpillar hump was affected by hepatic cirrhosis. Benson and Page[32] proposed the suggestive explanation that the anomaly might be represent a pure artefact produced by traction during cholecystectomy. Nevertheless, the similar incidence of caterpillar hump right hepatic artery in both the operative and cadaver groups (7% vs. 6.9%, respectively) indicated that a significant vascular anomaly is unlikely due to surgical manoeuvres. Another fascinating hypothesis can be explained on the basis of embryonic development.[37,38] According to Miyaki,[39] the embryonic liver is supplied by three segmental arteries arising from the dorsal aorta. The branch from the middle segmental artery develops to a proper hepatic artery arising from the common hepatic artery and the other two become two accessory hepatic arteries arising from the left gastric and superior mesenteric arteries. Since the artery arising from the left gastric artery can persist in 25% of cases and the other persists in 18.3%, it could be postulated that the partial or complete persistence of the arterial supply of foetal liver could sustain the caterpillar hump of the right hepatic artery. Of note, it must be highlighted that the incidence of persistence of accessory hepatic artery from superior mesenteric artery (18.3%) is not too far from the global incidence of caterpillar hump (6.9%).
The tortuous artery may route anteriorly or posteriorly to the common hepatic duct,[23] representing the posterior presentation the more common anatomical variation with 60% of incidence.[15,23] Accordingly, in all three patients with caterpillar hump of the current study, the arterial trunk passed dorsally to the common hepatic duct. Due to its tortuous course as well as the closeness to the gallbladder and common hepatic duct, this variant of the right hepatic artery may be injured with catastrophic consequences unless it is carefully dissected during cholecystectomy.[13] Furthermore, it may be mistaken to be the cystic artery and inadvertently ligated during surgical manoeuvres.[13,15,16,20,29] It must be highlighted that an atypically large cystic artery requires careful exploration of the hepatobiliary triangle as it may represent a Moynihan's hump right hepatic artery.[15,28]
Vascular variation is reported more commonly in a single-loop fashion (55% of cases), and in the present study, all vascular humps were noted in a single-loop configuration. It is interesting to note that in double-looped hump, cystic artery usually arises from the distal loop in an extremely short fashion, even if the origin from proximal loop is reported as well, with the long cystic artery crossing the tortuous right hepatic artery to reach gallbladder.[13,15,29] In the present study, the cystic artery arose from the convexity single-looped right hepatic artery resulting in exceptionally short fashion. Obviously, the cystic artery shortness could invariably lead to vascular injuries during cholecystectomy,[21,29] with the possible unfortunate sequence of events, both for its accidentally avulsion from the right hepatic artery due to excessive traction applied to the gallbladder and for right hepatic artery injury during its dissection and ligation.[13,15,20,30]
On these basis, a meticulous knowledge of hepatobiliary triangle with the possible arterial variant in association with all elements of the ‘Culture of Safety in Cholecystectomy’ is essential to perform safe surgery and to avoid serious complications.[9,18] To this aim, the separation of the lower part of the gallbladder from the cystic plate, the hepatobiliary triangle cleaning from the fat and fibrous tissue and the visualisation of 2 and only 2 structures attached to the gallbladder, may help surgeons to understand the potential for aberrant anatomy in all cases and to avoid complications with Moynihan's hump of right hepatic artery.[9,13,15,29]
This study has some limitations, which have to be pointed out. The retrospective nature of the study and the recruitment from a single Italian centre do not allow us to draw definite conclusions, pointing to biases associated with that. In addition, the methodology for caterpillar hump right hepatic artery detection is not standardised among the studies. Future high-quality, large-scaled reports will be of interest helping future researches on this field. However, this is the largest datasets presented on this subject.
CONCLUSION
Even with the above-mentioned limitations, this study shows that right hepatic artery is subject to rare anatomical variations in its course that increase the risk of vessel ligation or injury during laparoscopic cholecystectomy. Thus, a thorough knowledge of the right hepatic arterial anatomy and its variations is mandatory for surgeons facing more than two structures within Calot's triangle during surgical procedures to avoid fatal intra- and post-operative complications performing a safe and uneventful laparoscopic cholecystectomy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.El Maksoud W. Variant right hepatic artery forming Moynihan's hump, travelling through the gall bladder bed and enter the liver in unusual anterior location. Pak J Surg. 2014;30:196–8. [Google Scholar]
- 2.Ferreres AR, Asbun HJ. Technical aspects of cholecystectomy. Surg Clin North Am. 2014;94:427–54. doi: 10.1016/j.suc.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Tebala GD, Innocenti P, Ciani R, Zumbo A, Fonsi GB, Bellini P, et al. Identification of gallbladder pedicle anatomy during laparoscopic cholecystectomy. Chir Ital. 2004;56:389–96. [PubMed] [Google Scholar]
- 4.Tebala GD. Three-port laparoscopic cholecystectomy by harmonic dissection without cystic duct and artery clipping. Am J Surg. 2006;191:718–20. doi: 10.1016/j.amjsurg.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 5.Kamitani S, Tsutamoto Y, Hanasawa K, Tani T. Laparoscopic cholecystectomy in situ s inversus totalis with “inferior” cystic artery: A case report. World J Gastroenterol. 2005;11:5232–4. doi: 10.3748/wjg.v11.i33.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hüscher CG, Lirici MM, Di Paola M, Crafa F, Napolitano C, Mereu A, et al. Laparoscopic cholecystectomy by ultrasonic dissection without cystic duct and artery ligature. Surg Endosc. 2003;17:442–51. doi: 10.1007/s00464-002-9068-3. [DOI] [PubMed] [Google Scholar]
- 7.De Silva WM, Sivananthan S, De Silva D, Fernando N. Biliary tract injury during cholecystectomy: A retrospective descriptive review of clinical features, treatment and outcome. Ceylon Med J. 2006;51:132–6. doi: 10.4038/cmj.v51i4.1141. [DOI] [PubMed] [Google Scholar]
- 8.Targarona EM, Marco C, Balagué C, Rodriguez J, Cugat E, Hoyuela C, et al. How, when, and why bile duct injury occurs. A comparison between open and laparoscopic cholecystectomy. Surg Endosc. 1998;12:322–6. doi: 10.1007/s004649900662. [DOI] [PubMed] [Google Scholar]
- 9.Strasberg SM, Brunt LM. The critical view of safety: Why it is not the only method of ductal identification within the standard of care in laparoscopic cholecystectomy. Ann Surg. 2017;265:464–5. doi: 10.1097/SLA.0000000000002054. [DOI] [PubMed] [Google Scholar]
- 10.Thompson JE, Jr, Bock R, Lowe DK, Moody WE., 3rd Vena cava injuries during laparoscopic cholecystectomy. Surg Laparosc Endosc. 1996;6:221–3. [PubMed] [Google Scholar]
- 11.Ding YM, Wang B, Wang WX, Wang P, Yan JS. New classification of the anatomic variations of cystic artery during laparoscopic cholecystectomy. World J Gastroenterol. 2007;13:5629–34. doi: 10.3748/wjg.v13.i42.5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC, et al. Complications of laparoscopic cholecystectomy: A national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 13.Kavitha Kamath B. An anatomical study of Moynihan's hump of right hepatic artery and its surgical importance. [Last accessed on 2018 Mar 30];Anat Soc India. 2016 65:S65–7. Available from: https://www.infona.pl/resource/bwmeta1.element.elsevier-4082da5e-b99a-3079-b79a-8feb6399ef7e . [Google Scholar]
- 14.Flint ER. Abnormalities of the right hepatic, cystic, and gastroduodenal arteries, and of the bile-ducts. [Last accessed on 2017 Oct 12];Br J Surg. 1923 10:509–19. Available from: http://www.doi.wiley.com/10.1002/bjs.1800104011 . [Google Scholar]
- 15.Jansirani D, Mugunthan N, Phalgunan V, Deep S. Caterpillar hump of right hepatic artery: Incidence and surgical significance. [Last accessed on 2017 Oct 12];Natl J Clin Anat. 2012 1:121–4. Available from: http://www.scopemed.org/?mno=24466 . [Google Scholar]
- 16.Hamza M, Jaffar A, Hassan H. Vascular and gallbladder variations in laparoscopic cholecystectomy. Med J Babylon. 2008;5:119–34. [Google Scholar]
- 17.Hafeez Bhatti AB, Dar FS, Zia H, Rafique MS, Khan NY, Salih M, et al. Prognostication of learning curve on surgical management of vasculobiliary injuries after cholecystectomy. Int J Hepatol 2016. 2016 doi: 10.1155/2016/2647130. 2647130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liška V, Pálek R, Třeška V, Glanc D, Svobodová M. Analysis of complications and clinical and pathologic factors in relation to the laparoscopic cholecystectomy. Rozhl Chir. 2014;93:123–31. [PubMed] [Google Scholar]
- 19.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25. [PubMed] [Google Scholar]
- 20.Al-Sayigh HA. The incidence of cystic artery variation during laparoscopic surgery 121. Med J Babylon. 2010;7:389–403. [Google Scholar]
- 21.Badagabettu SN, Sirasanagandla SR, Kumar N, Shetty SD. Hepatosplenic trunk associated with tortuous course of right hepatic artery forming caterpillar hump. N Am J Med Sci. 2012;4:376–8. doi: 10.4103/1947-2714.99525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergamaschi R, Ignjatovic D. More than two structures in calot's triangle. A postmortem study. Surg Endosc. 2000;14:354–7. doi: 10.1007/s004640000154. [DOI] [PubMed] [Google Scholar]
- 23.Dandekar U, Dandekar K, Chavan S. Right hepatic artery: A cadaver investigation and its clinical significance. Anat Res Int 2015. 2015 doi: 10.1155/2015/412595. 412595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eid N, Ito Y, Otsuki Y. Right hepatic artery forming caterpillar hump, perforating calot's triangle into the cystic plate and associated with a variant branching pattern of the parent vessel. J Hepatobiliary Pancreat Sci. 2015;22:402–3. doi: 10.1002/jhbp.231. [DOI] [PubMed] [Google Scholar]
- 25.Johnston EV, Anson BJ. Variations in the formation and vascular relationships of the bile ducts. Surg Gynecol Obstet. 1952;94:669–86. [PubMed] [Google Scholar]
- 26.Mugunthan N, Kannan R, Jebakani CF, Anbalagan J. Variations in the origin and course of right hepatic artery and its surgical significance. J Clin Diagn Res. 2016;10:AC01–4. doi: 10.7860/JCDR/2016/22126.8428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sangameswaran K, Devi MR. Surgical importance of caterpillar (Moynihan) hump of right hepatic artery. [Last accessed on 2017 Jun 04];Int J Anat Res. 2017 5:3672–5. Available from: https://www.ijmhr.org/IntJAnatRes/IJAR.2017.136 . [Google Scholar]
- 28.Balija M, Huis M, Nikolic V, Stulhofer M. Laparoscopic visualization of the cystic artery anatomy. World J Surg. 1999;23:703–7. doi: 10.1007/pl00012372. [DOI] [PubMed] [Google Scholar]
- 29.Bhargava G, Singh H, Singh H, Gupta R. Moynihan's hump of right hepatic artry: A case report. CIBTech J Surg. 2014;3:42–4. [Google Scholar]
- 30.Dawani S, Sandhya A, Rasul S, Ali M. Frequency of common anatomical variations in the extrahepatic biliary tract in patients undergoing elective cholecystectomy introduction. Pak J Surg. 2013;29:61–5. [Google Scholar]
- 31.Scott-Conner CE, Hall TJ. Variant arterial anatomy in laparoscopic cholecystectomy. Am J Surg. 1992;163:590–2. doi: 10.1016/0002-9610(92)90563-7. [DOI] [PubMed] [Google Scholar]
- 32.Benson EA, Page RE. A practical reappraisal of the anatomy of the extrahepatic bile ducts and arteries. Br J Surg. 1976;63:853–60. doi: 10.1002/bjs.1800631105. [DOI] [PubMed] [Google Scholar]
- 33.Cimmino PT, Bocchetti T, Izzo L. Anatomo-surgical considerations in laparoscopic cholecystectomy. G Chir. 1992;13:149–51. [PubMed] [Google Scholar]
- 34.Ramirez-Flores R. A new anatomic guide for safe ligation of the cystic artery. Surg Gynecol Obstet. 1955;100:633–5. [PubMed] [Google Scholar]
- 35.Hugh TB, Kelly MD, Li B. Laparoscopic anatomy of the cystic artery. Am J Surg. 1992;163:593–5. doi: 10.1016/0002-9610(92)90564-8. [DOI] [PubMed] [Google Scholar]
- 36.Taylor C. Cirrhosis Imaging. 2015. [Last accessed 2018 Mar 30]. Available from: https://emedicine.medscape.com/article/366426-overview .
- 37.Bhardwaj N. Anomalous origins of hepatic artery and its significance for hepatobiliary surgery. [Last accessed on 2017 Oct 14];Anat Soc India. 2010 59:173–6. Available from: http://www.sciencedirect.com/science/article/pii/S0003277810800206?via%3Dihub . [Google Scholar]
- 38.Abdullah SS, Mabrut JY, Garbit V, De La Roche E, Olagne E, Rode A, et al. Anatomical variations of the hepatic artery: Study of 932 cases in liver transplantation. Surg Radiol Anat. 2006;28:468–73. doi: 10.1007/s00276-006-0121-0. [DOI] [PubMed] [Google Scholar]
- 39.Miyaki T. Patterns of arterial supply of the human fetal liver. The significance of the accessory hepatic artery. Acta Anat (Basel) 1989;136:107–11. doi: 10.1159/000146806. [DOI] [PubMed] [Google Scholar]


