Abstract
Objective:
To determine whether a significant number of patients with hyperparathyroidism remain undiagnosed and untreated.
Background:
Failure to diagnose primary hyperparathyroidism and refer patients to surgeons leads to impaired quality of life and increased costs. We hypothesized that many patients with hyperparathyroidism would be untreated due to not considering the diagnosis, inadequate evaluation of hypercalcemia, and under-referral to surgeons.
Methods:
We reviewed administrative data on 682,704 patients from a tertiary referral center between 2011 and 2015, and identified hypercalcemia (>10.5mg/dl) in 10,432. We evaluated whether hypercalcemic patients underwent measurement of parathyroid hormone, had documentation of hypercalcemia/hyperparathyroidism, or were referred to surgeons.
Results:
The mean age of our cohort was 54 years, with 61% females, and 56% Caucasians. Only 3,200 (31%) hypercalcemic patients had parathyroid hormone levels measured, 2,914 (28%) had a documented diagnosis of hypercalcemia, and 880 (8%) had a diagnosis of hyperparathyroidism in the medical record. Only 592 (22%) out of 2,666 patients with classic hyperparathyroidism (abnormal calcium and parathyroid hormone) were referred to surgeons.
Conclusions:
A significant proportion of patients with hyperparathyroidism do not undergo appropriate evaluation and surgical referral. System-level interventions which prompt further evaluation of hypercalcemia and raise physician awareness about hyperparathyroidism could improve outcomes and produce long-term cost savings.
MINI-ABSTRACT
Surgical treatment of hyperparathyroidism significantly improves patients’ quality of life. We found that patients with hyperparathyroidism are frequently undiagnosed and under-treated. Our findings indicate the need for system-level changes to improve detection and treatment of hyperparathyroidism.
BACKGROUND
Failure to diagnose and treat hyperparathyroidism leads to impaired quality of life and increases costs for patients and health systems.1–3,4,5,6 Untreated hyperparathyroidism increases the risk of fractures and kidney stones, is associated with depression and cognitive impairment, and can cause cardiovascular dysfunction that leads to hypertension, stroke, and myocardial infarction.6 The only effective treatment for hyperparathyroidism is parathyroidectomy, which can be performed in an outpatient setting with minimal morbidity and offers a durable cure for 85–95% of patients.6,7
Multiple opportunities exist for healthcare systems to under-diagnose or under-treat hyperparathyroidism. Although surgeons provide the definitive treatment for hyperparathyroidism, the diagnosis is typically made by primary care physicians who then refer to endocrinologists and/or surgeons for further assessment and discussion about treatment. Diagnosing hyperparathyroidism requires a high index of suspicion because symptoms are often nonspecific, and the first indication of disease is usually an elevated calcium on routine laboratory tests.8 Prior work suggests that hyperparathyroidism may be under-diagnosed and under-treated, but these studies used parathyroidectomy as the primary endpoint. They did not distinguish between patients who were untreated due to non-referral to surgeons and those who underwent surgical evaluation but opted not to have surgery.9–11 Not all patients with hyperparathyroidism will decide to have surgery, and surgeons will typically not recommend a procedure when the patient’s health status suggests that risks outweigh benefits. If the purpose of healthcare systems is to take a patient-centered approach to care, then care processes should ideally help patients reach the physician who can help them make informed treatment decisions. When it comes to decisions about parathyroid surgery, surgeons represent the best source of information on risks and benefits. Consequently, we felt that referral to surgeons represents a more useful endpoint than whether patients ultimately undergo parathyroidectomy.
The purpose of this study is to (1) evaluate whether patients with hypercalcemia receive the appropriate biochemical evaluation with assessment of parathyroid hormone (PTH) levels and (2) determine rates of surgical referral and treatment for hyperparathyroidism. We hypothesized that a significant number of patients with hypercalcemia would not have their PTH levels evaluated, and that there would be opportunities to improve rates of referral to surgeons for patients with hyperparathyroidism.
METHODS
Patient Population
Setting:
We used administrative data to review 682,704 consecutive patients seen at the University of Alabama at Birmingham (UAB), a tertiary referral center, from 2011–2015 (Figure 1).
Figure 1.
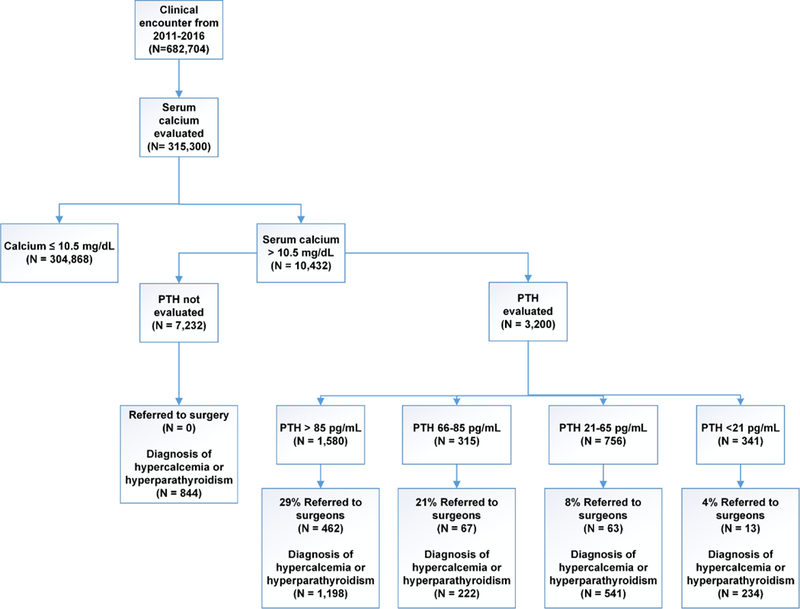
Most patients with hypercalcemia do not receive appropriate evaluation of parathyroid hormone (PTH levels) or referral to surgeons for discussion of treatment options.
Patient Selection:
We identified 315,300 patients who had a serum calcium checked during that time, and our final study cohort consisted of the 10,432 patients with hypercalcemia (at least 1 serum calcium >10.5 mg/dl).
Outcomes
Evaluation and Diagnosis of Hypercalcemia
We searched laboratory records to determine whether patients with hypercalcemia had PTH levels checked and searched medical records to identify whether International Classification of Disease (ICD) 9 or 10 diagnostic codes for either hypercalcemia or hyperparathyroidism were entered.
Referral to Surgeons and Endocrinologists
To ascertain whether patients were referred to surgeons or endocrinologists for evaluation of hyperparathyroidism, we performed a free text search of all notes in the medical record system. We searched for signatures that contained the names of surgeons and endocrinologists employed at UAB during the study period. If patients had a note signed by either a surgeon who performs parathyroidectomies or an endocrinologist, they were considered to have been seen by that physician and were categorized as having been referred to surgery or endocrinology.
Patient Characteristics
Demographic information such as age, gender, and insurance status was obtained from the electronic medical record. Co-morbidities were classified using the Elixhauser method based on ICD-9 or ICD-10 codes in medical records.12 Elixhauser co-morbidities include HIV/AIDS, alcohol abuse, arrhythmia, pulmonary disease, hypertension, heart failure, anemia, diabetes, drug abuse, fluid/electrolyte disorders, hypothyroidism, liver disease, lymphoma, malnutrition/weight loss, cancer, obesity, neurologic disorders, paralysis, ulcers, peripheral vascular disease, psychoses, renal failure, and cardiac valve disorders. A similar process was used to assess whether patients had complications of hyperparathyroidism, including kidney stones, osteoporosis/osteopenia, and fractures.
Statistical Analysis
We used two-tailed t-tests to compare means, chi-square for univariable comparisons of proportions, and multivariable logistic regression to identify independent predictors of (1) checking PTH levels, and (2) odds of referral to surgeons or endocrinologists. An alpha of <0.05 was considered statistically significant. Analyses were performed using SAS ®.
RESULTS
Patient characteristics
We reviewed administrative data on 682,704 consecutive patients from a tertiary referral center between 2011 and 2015, and 315,300 patients had their serum calcium evaluated (Figure 1). Our study population consisted of the 10,432 patients from this cohort who had an elevated serum calcium of >10.5mg/dL. Mean age of the study group was 54±22 years, 61% were women, and 56% were Caucasian (Table 1). The majority of patients (57%) had private commercial insurance, 38% used Medicare or Medicaid, and 57% of encounters occurred in an outpatient setting.
Table 1.
Demographics of patients with elevated calcium from 2011-2015
| Demographics | N = 10,432 N (%) |
|---|---|
| Age in years (mean ±SD) | 54±22 |
| Age Group | |
| 1. <=35 years old | 1,827 (18) |
| 2. 36 to 45 years old | 834 (8) |
| 3. 46 to 55 years old | 1,753 (17) |
| 4. 56 to 65 years old | 2,534 (24) |
| 5. 66 to 75 years old | 2,025 (19) |
| 6. 76 to 85 years old | 1,091 (10) |
| 7. >85 years old | 347 (3) |
| Gender | |
| Female | 6,372 (61) |
| Male | 3,993 (39) |
| Race/Ethnicity | |
| 1. White | 5,825 (56) |
| 2. Black | 4,040 (39) |
| 3. Other | 547 (5) |
| Insurance | |
| 1. Commercial | 5,971 (57) |
| 2. Medicare | 2,875 (28) |
| 3. Medicaid | 1,077 (10) |
| 4. Other/Uninsured/Unknown | 509 (5) |
| Encounter Type | |
| 1. Outpatient | 5,907 (57) |
| 2. Inpatient | 3,066 (29) |
| 3. ER | 809 (8) |
| Any Elixhauser Comorbidity | |
| No | 2,271 (22) |
| Yes | 8,161 (78) |
| Kidney Stone | 267 (3) |
| Fracture | 754 (7) |
| Osteoporosis | 661 (6) |
| Index Elevated Calcium Year 2011 | 1,991 (19) |
| Index Elevated Calcium Year 2012 | 1,866 (18) |
| Index Elevated Calcium Year 2013 | 1,545 (15) |
| Index Elevated Calcium Year 2014 | 2,029 (19) |
| Index Elevated Calcium Year 2015 | 3,001 (29) |
Characteristics of patients who received appropriate biochemical evaluation of hypercalcemia
Only 3,200 (31%) patients with hypercalcemia received an appropriate biochemical workup with evaluation of parathyroid hormone (PTH) levels, while 7,232 (69%) never had their PTH levels checked. Patients who had PTH checked were more likely to be older (mean age 60.7 vs 51.3 years) and female (68% versus 59%) compared to those who did not have PTH evaluated (Table 2). Patients who had PTH evaluated were also more likely to be seen in an outpatient setting, and they were less likely to have Elixhauser co-morbidities (Table 2). Multivariable logistic regression indicated that predictors of appropriate workup for hypercalcemia included age (youngest and oldest patients less likely), female gender, commercial/private insurance, higher calcium levels, the absence of Elixhauser co-morbidities, and the presence of osteoporosis or kidney stones (Figure 2).
Table 2.
Patients with elevated calcium who had parathyroid hormone (PTH) levels evaluated were more likely to be female, have commercial private insurance, and have fewer co-morbidities. There was a variable relationship between age and PTH evaluation.
| Demographics | PTH Workup (N=3,200) |
no PTH Workup (N=7,232) |
p-value |
|---|---|---|---|
| Age in years (mean ± SD) | 60.7 +/− 15.1 | 51.3 +/− 24.5 | <.0001 |
| Age Group | <.0001 | ||
| 1. <=35 years old | 209 ( 6.5) | 1618 (22.4) | |
| 2. 36 to 45 years old | 242 ( 7.6) | 592 ( 8.2) | |
| 3. 46 to 55 years old | 596 (18.6) | 1157 (16.0) | |
| 4. 56 to 65 years old | 907 (28.3) | 1627 (22.6) | |
| 5. 66 to 75 years old | 743 (23.2) | 1282 (17.8) | |
| 6. 76 to 85 years old | 393 (12.3) | 698 ( 9.7) | |
| 7. >85 years old | 110 ( 3.4) | 237 ( 3.3) | |
| Gender | <.0001 | ||
| Female | 2174 (67.9) | 4198 (58.6) | |
| Male | 1026 (32.1) | 2967 (41.4) | |
| Race/Ethnicity | <.0001 | ||
| 1. White | 1818 (56.8) | 4007 (55.4) | |
| 2. Black | 1314 (41.1) | 2746 (38.0) | |
| 3. Other | 68 ( 2.1) | 479 ( 6.6) | |
| Insurance | <.0001 | ||
| 1. Commercial | 2014 (62.9) | 3957 (54.7) | |
| 2. Medicare | 998 (31.2) | 1877 (26.0) | |
| 3. Medicaid | 146 ( 4.6) | 931 (12.9) | |
| 4. Other/Uninsured/Unknown | 42 ( 1.3) | 467 ( 6.5) | |
| Encounter Type | <.0001 | ||
| 1. Outpatient | 2383 (74.5) | 3524 (48.7) | |
| 2. Inpatient | 572 (17.9) | 2494 (34.5) | |
| 3. ER | 147 ( 4.6) | 662 ( 9.2) | |
| Any Elixhauser Comorbidity | <.0001 | ||
| No | 729 (22.8) | 1454 (20.1) | |
| Yes | 2471 (77.2) | 5778 (79.9) | |
| Kidney Stones | 120 ( 3.8) | 147 ( 2.0) | <0.001 |
| Fracture | 216 ( 6.8) | 538 ( 7.4) | 0.2100 |
| Osteoporosis | 302 ( 9.4) | 359 ( 5.0) | <.0001 |
| Year of Index Calcium | |||
| 2011 | 700 (21.9) | 1291 (17.9) | <0.001 |
| 2012 | 618 (19.3) | 1248 (17.3) | |
| 2013 | 575 (18.0) | 970 (13.4) | |
| 2014 | 610 (19.1) | 1419 (19.6) | |
| 2015 | 697 (21.8) | 2304 (31.9) |
Figure 2.
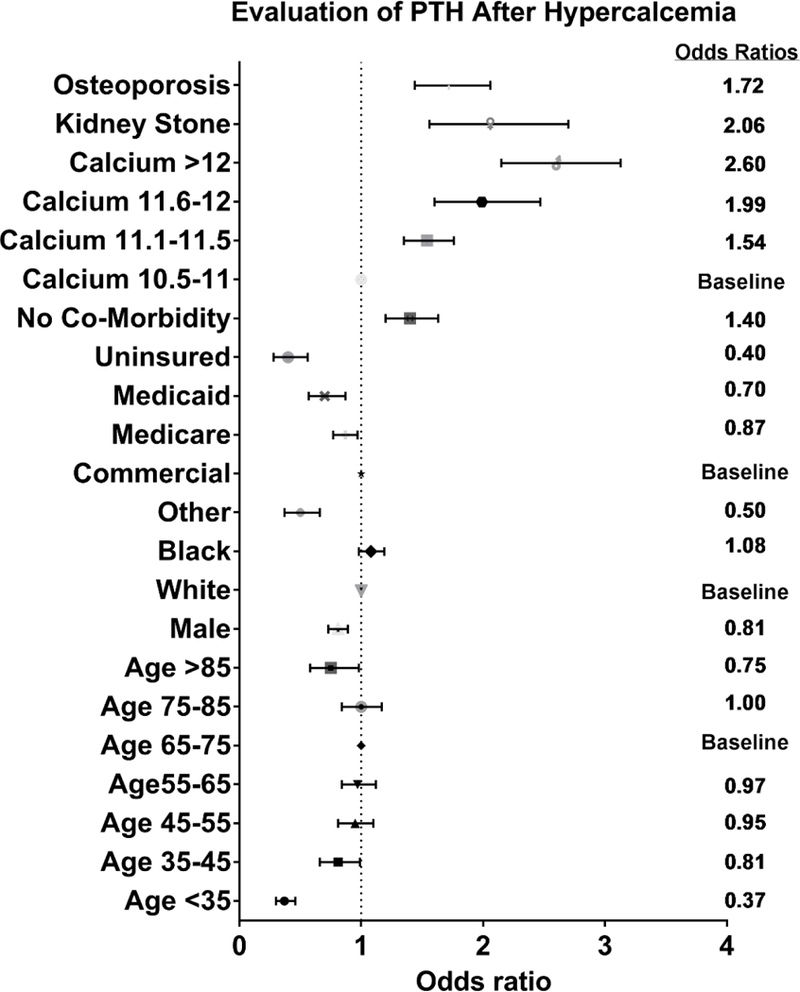
Odds of having parathyroid hormone (PTH) levels evaluated after hypercalcemia vary with age, gender, insurance status, co-morbidity, and calcium level. Odds ratios and 95% confidence intervals shown on the left, with numeric value of odds ratio shown on the right.
Results adjusted for type of visit (inpatient, outpatient, emergency room), year of initial calcium, and Elixhauser co-morbidities.
Characteristics of patients with abnormal calcium and PTH who were referred for surgical evaluation
Among the 3,200 patients who had both calcium and PTH evaluated, the chances of surgical referrals decreased for older patients (>75 years old), men, and individuals with Elixhauser co-morbidities. Additionally, the rates of diagnosis (hyperparathyroidism or hypercalcemia) and referral to surgeons varied according to the PTH levels (Figure 1). Patients with PTH levels above the normal values for the assay (>85pg/mL) were correctly diagnosed with either hypercalcemia or hyperparathyroidism 76% of the time, but only 462 (29%) were referred to surgeons (Figure 1). Additionally, among patients with inappropriately high PTH given their calcium levels (normo-hormonal hyperparathyroidism), 21% with PTH 66–85 pg/ml and 8% with PTH 21–65 pg/ml were referred to surgeons. We repeated this analysis for patients who had ≥2 abnormal calcium values and found similar rates of surgical referrals (data not shown). Similarly, hypercalcemia or hyperparathyroidism were correctly diagnosed for 22 patients (70%) in the PTH 66–85 group and 541 (72%) in the PTH 21–65 group. Less than 4% of patients with elevated calcium and PTH <21 pg/mL were referred to surgery, though 234 (69%) were diagnosed with either hypercalcemia or hyperparathyroidism. After adjusting for differences in patient characteristics, both old (OR 0.27 for age >85 years) and young age (OR 0.42 for age <35 years) and male gender (OR 0.78) were associated with lower odds of surgical referral (Figure 3). Patients without any Elixhauser co-morbidities (OR 2.3) and higher calcium levels (OR 1.14–1.85 for calcium >11.1 mg/dL) were more likely to be referred to surgeons.
Figure 3.
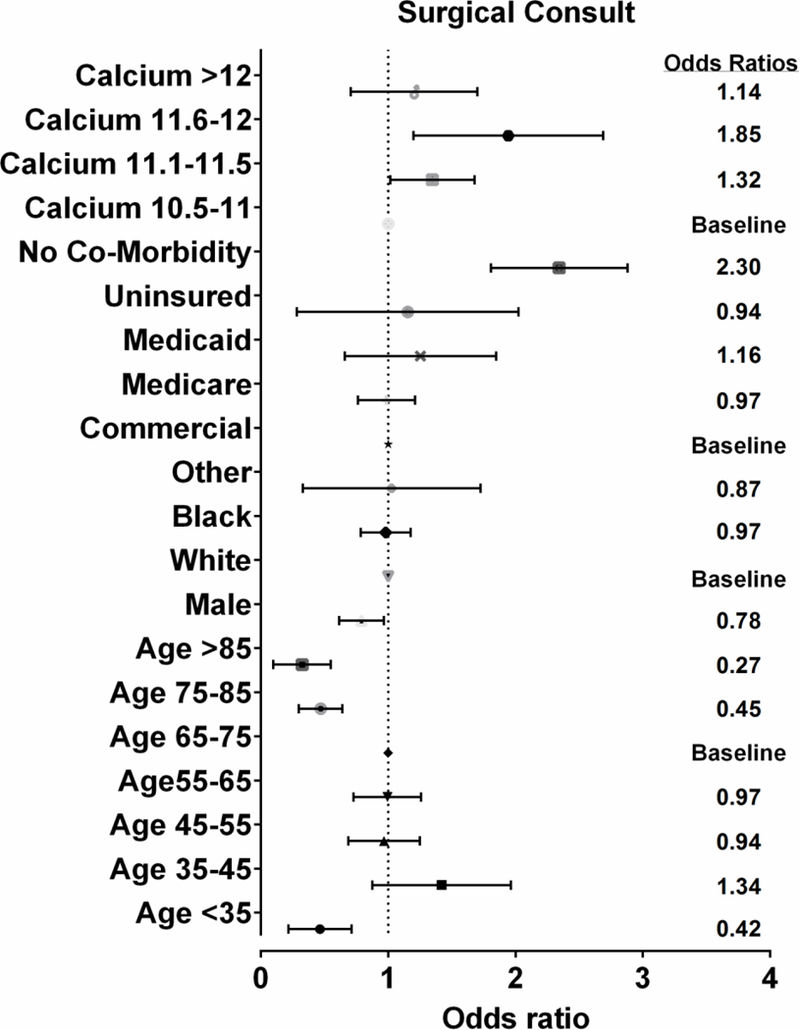
Odds of being referred to surgery after hypercalcemia & evaluation of PTH vary with age, gender, co-morbidity, and calcium level. Odds ratios and 95% confidence intervals shown on the left, with numeric value of odds ratio shown on the right.
Results adjusted for type of visit (inpatient, outpatient, emergency room), year of initial calcium, and Elixhauser co-morbidities.
A similar analysis to assess rates of referral to medical endocrinologists (Table 4 and Figure 4) identified only 385 out of 3,200 (12%) patients who were referred to endocrinologists after both calcium and PTH were evaluated. The only factor in our model that predicted the likelihood of an endocrine referral was male gender (OR 0.64). Age, race/ethnicity, insurance status, and serum calcium were not significant predictors.
Table 4.
Likelihood of referral to endocrinology after evaluation of calcium and PTH is less likely in men, and in patients with co-morbidities.
| Demographics | Endocrinology consultation (N=385) |
No endocrinology consultation (N=2,815) |
p-value |
|---|---|---|---|
| Age in years (mean ± SD) | 62.0 +/− 13.6 | 60.6 +/− 15.2 | 0.0800 |
| Age Group | 0.1679 | ||
| 1. <=35 years old | 20 ( 5.2) | 189 ( 6.7) | |
| 2. 36 to 45 years old | 22 ( 5.7) | 220 ( 7.8) | |
| 3. 46 to 55 years old | 62 (16.1) | 534 (19.0) | |
| 4. 56 to 65 years old | 117 (30.4) | 790 (28.1) | |
| 5. 66 to 75 years old | 104 (27.0) | 639 (22.7) | |
| 6. 76 to 85 years old | 50 (13.0) | 343 (12.2) | |
| 7. >85 years old | 10 ( 2.6) | 100 ( 3.6) | |
| Gender | <.0001 | ||
| Female | 310 (80.5) | 1864 (66.2) | |
| Male | 75 (19.5) | 951 (33.8) | |
| Race/Ethnicity | 0.4534 | ||
| 1. White | 224 (58.2) | 1594 (56.6) | |
| 2. Black | 156 (40.5) | 1158 (41.1) | |
| 3. Other | 5 ( 1.3) | 63 ( 2.2) | |
| Insurance | 0.5196 | ||
| 1. Commercial | 243 (63.1) | 1771 (62.9) | |
| 2. Medicare | 114 (29.6) | 884 (31.4) | |
| 3. Medicaid | 23 ( 6.0) | 123 ( 4.4) | |
| 4. Other/Uninsured/Unknown | 5 ( 1.3) | 37 ( 1.3) | |
| Encounter Type | <.0001 | ||
| 1. Outpatient | 340 (88.3) | 2043 (72.6) | |
| 2. Inpatient | 25 ( 6.5) | 547 (19.4) | |
| 3. ER | 17 ( 4.4) | 130 ( 4.6) | |
| Any Comorbidity | <.0001 | ||
| No | 137 (35.6) | 642 (22.8) | |
| Yes | 248 (64.4) | 2173 (77.2) | |
| Kidney Stone | 16 ( 4.2) | 104 ( 3.7) | 0.6549 |
| Fracture | 12 ( 3.1) | 204 ( 7.2) | 0.0024 |
| Osteoporosis | 29 ( 7.5) | 273 ( 9.7) | 0.1728 |
| Year of Index Calcium | 0.008 | ||
| 2011 | 106 (27.5) | 594 (21.1) | |
| 2012 | 77 (20.0) | 541 (19.2) | |
| 2013 | 75 (19.5) | 500 (17.8) | |
| 2014 | 58 (15.1) | 552 (19.6) | |
| 2015 | 69 (17.9) | 628 (22.3) |
Figure 4.
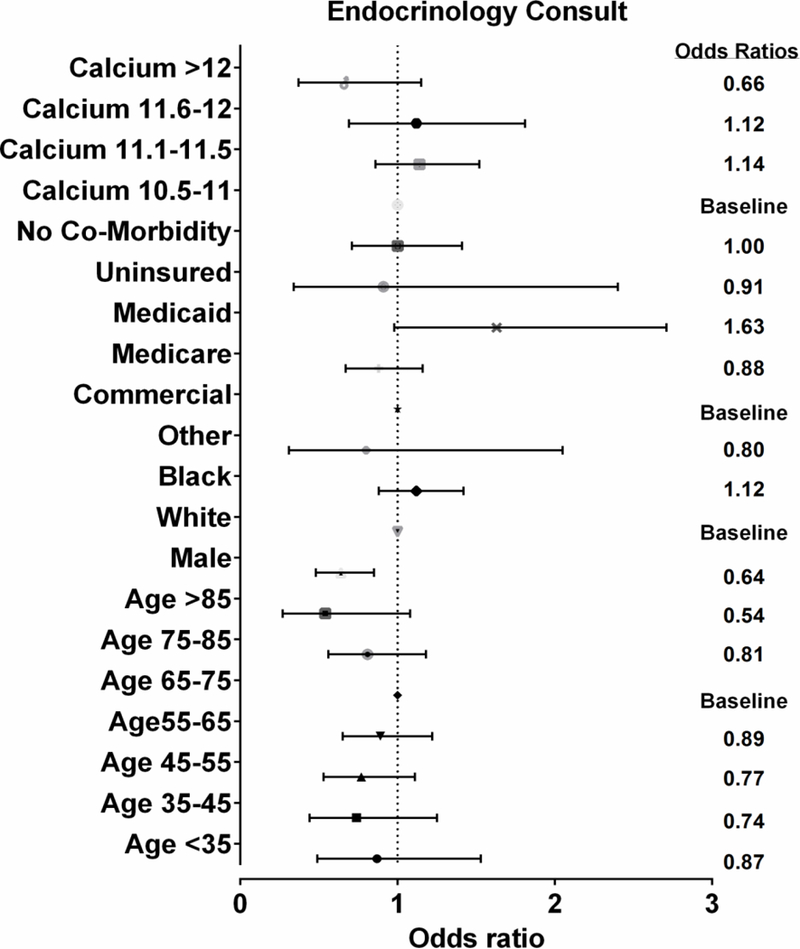
Odds of being referred to endocrinology after hypercalcemia & evaluation of PTH vary with gender but not age, co-morbidity, or calcium level. Odds ratios and 95% confidence intervals shown on the left, with numeric value of odds ratio shown on the right.
Results adjusted for type of visit (inpatient, outpatient, emergency room), year of initial calcium, and Elixhauser co-morbidities.
DISCUSSION
Our primary finding was that very few patients with hypercalcemia undergo evaluation of PTH levels to identify the underlying etiology, and an even smaller minority with both abnormal calcium and PTH are referred to surgeons to discuss treatment. Although not all patients with hyperparathyroidism need or desire surgery, the most appropriate healthcare provider to discuss risks and benefits of parathyroidectomy is a surgeon. Unfortunately, we found that 71% of patients with clear hyperparathyroidism (abnormal calcium and PTH) never see a surgeon to discuss treatment options. Additionally, >80% of patients with inappropriately high PTH in the setting of hypercalcemia, who might also benefit from surgery, never receive a surgical referral. Parathyroidectomy is a low-risk procedure that can improve quality of life, enhance bone health, and reduce risk of kidney stones. Our analysis identified considerable opportunity health systems to improve the diagnosis and treatment of hyperparathyroidism, given how many patients miss the opportunity to even discuss the benefits of surgery.
Our findings expand upon earlier work that explored diagnosis and treatment of hyperparathyroidism. Yeh et al. used administrative data from Kaiser Permanente in California to determine whether patients with primary hyperparathyroidism were undergoing parathyroidectomy when they met consensus recommendations for surgery. In this group of patients who would be expected to have high rates of surgery, only 39–51% actually had parathyroidectomy.9 They looked at individual criteria for surgery and found that patients with nephrolithiasis were more likely to undergo surgery, but that significant bone density changes did not increase the odds of surgery. The study indicated that rates of parathyroidectomy remained low even when patients clearly met indications for surgery, but the authors were unable to determine whether patients discussed parathyroidectomy with a surgeon and opted not to have the operation, or were deemed too high risk by their surgeon. Press et al. reviewed medical records at the Cleveland clinic for patients with elevated calcium and estimated that 43% of hypercalcemic patients were likely to have hyperparathyroidism and should undergo further evaluation and referral to endocrine surgeons.10 Their study illustrates the importance of following up an abnormal calcium with a detailed history and measurement of PTH levels. The commentary on this article astutely noted that despite mounting evidence on the benefits of parathyroidectomy, little practice change has occurred at the level of primary care physicians to improve detection and increase surgical referrals.13
Many potential explanations exist for low rates of diagnosis and treatment of hyperparathyroidism that could be addressed by clinical interventions. Primary care physicians are increasingly overwhelmed by a growing number of laboratory alerts, clinical messages, and paperwork.14 It would be relatively easy to miss or ignore an isolated abnormal laboratory value, such as a high calcium, that arises during an otherwise routine assessment. Alternatively, the abnormal calcium might be noted but deemed low priority as it is rarely immediately life-threatening. Patients also may see different physicians at subsequent office visits, particularly at an academic center with resident involvement. In the current busy clinical environment, there may be insufficient time to review all previous laboratory values and the need to follow up on a previously high calcium may be missed.
There are also several reasons why patients with hyperparathyroidism may not be referred for surgical evaluation. Primary care physicians may assume that surgeons have no role to play unless patients meet some of the consensus criteria for surgery, including a history of kidney stones, bone changes, elevated creatinine, etc.6 Although these guidelines are meant to help with the decision to operate, it seems reasonable that patients would benefit from evaluation by an expert who could discuss the risks and benefits of surgery and fully engage with patients in making treatment decisions. Indeed, the recent American Association of Endocrine Surgery guidelines emphasize the importance of referring patients to surgical experts for discussion of treatment options.6 Additionally, busy primary care physicians may be falsely reassured when they check PTH levels and the results fall within the “normal” range for the assay. Classic hyperparathyroidism consists of elevated calcium and PTH, but normo-hormonal hyperparathyroidism is also a recognized entity where PTH is inappropriately high in the setting of elevated calcium, even though the PTH value falls within the general parameters of “normal”.15 Normo-hormonal hyperparathyroidism can be a difficult diagnosis even for experts, and many non-specialists could easily miss the diagnosis and leave patients untreated.15
It is also important to acknowledge that patients may not be interested in surgery when they have reasonable quality of life and are not experiencing significant symptoms. At the same time, surgeons may not recommend an operation for patients who are high risk and likely to derive little benefit from parathyroidectomy. We consider it important to emphasize that regardless of patient co-morbidity or symptoms, a surgeon is still the optimal person to have an informed discussion about risks and benefits of parathyroidectomy. Surgeons are more likely than medical specialists to understand the risks of surgery and to effectively determine how their skill level and patients’ health status intersect to determine operative risk. Surgeons are also well equipped to address questions about operative technique and postoperative recovery that are important for patients to make informed decisions. In short, patients with hyperparathyroidism are likely to gain valuable information and insight from talking to surgeons even if they ultimately decide not to have surgery. If nothing else, it will ensure that patients are aware of treatment options, and they may reconsider the value of surgery at a later date, or if their disease progresses.
Our study provides a detailed picture of deficiencies in the clinical approach to hypercalcemia and hyperparathyroidism, but several limitations should be acknowledged. The number of patients is substantial, but they are all derived from a single institution’s health system. UAB draws patients from a wide geographic area and maintains excellent follow up, but it is entirely possible that some individuals received evaluation and treatment at other institutions and this was not captured by our analysis. Our mean follow up was 16 months, however, which suggests that most patients were seen in the UAB system long enough to undergo appropriate evaluation and referral. We also found that patients with ≥2 abnormal calcium values had similarly low rates of surgical referral, which suggests that loss to follow up is unlikely to explain our findings. Additionally, the approach to hyperparathyroidism and hypercalcemia at UAB may not be representative of practice patterns nationally. We feel that this is unlikely, however, given similar results found in other health systems.9,10 Finally, any retrospective study involving administrative data is subject to error related to coding of co-morbidity and other demographic data.
In summary, we found strong evidence for a need to change how health systems approach diagnosis and treatment of hypercalcemia and hyperparathyroidism. There is a significant opportunity to improve patient outcomes by earlier detection and treatment of a problem that can impact multiple organ systems and greatly impair quality of life. Although this study did not examine the impact of under-diagnosis and under-treatment on health outcomes (mortality, clinic visits, hospitalization, use of medications, and costs of care), it would be reasonable to expect that delays in diagnosis could affect these outcomes. Future work can further elaborate the health implications of failure to diagnose and treat hyperparathyroidism in a timely fashion. Changing the approach to hypercalcemia and hyperparathyroidism will require interventions that affect multiple levels of care. Engaging with primary care providers to increase awareness of hyperparathyroidism and the benefits of modern surgical approaches to the disease are important. At the same time, it will be necessary to engage with patients to ensure they are active participants in the process and are able to advocate for effective diagnosis and treatment. Finally, automated processes that ensure appropriate laboratory evaluations and referrals can reduce error by minimizing the risk of missed laboratory values or misdiagnosis of hyperparathyroidism. The combination of systems changes and stakeholder engagement is more likely to succeed than focusing on one component to the exclusion of others.16 This will better enable hospitals and providers to care for patients with a frequently overlooked diagnosis.
Table 3.
Likelihood of referral to surgery after evaluation of calcium and PTH is less likely in older patients, male gender, and in patients with co-morbidities.
| Demographics | Surgical consultation (N=609) |
No surgical consultation (N=2,591) |
p-value |
|---|---|---|---|
| Age in years (mean ± SD) | 60.2 +/− 12.5 | 60.9 +/− 15.6 | 0.2842 |
| Age Group | <.0001 | ||
| 1. <=35 years old | 19 ( 3.1) | 190 ( 7.3) | |
| 2. 36 to 45 years old | 59 ( 9.7) | 183 ( 7.1) | |
| 3. 46 to 55 years old | 117 (19.2) | 479 (18.5) | |
| 4. 56 to 65 years old | 195 (32.0) | 712 (27.5) | |
| 5. 66 to 75 years old | 163 (26.8) | 580 (22.4) | |
| 6. 76 to 85 years old | 48 ( 7.9) | 345 (13.3) | |
| 7. >85 years old | 8 ( 1.3) | 102 ( 3.9) | |
| Gender | <.0001 | ||
| Female | 456 (74.9) | 1718 (66.3) | |
| Male | 153 (25.1) | 873 (33.7) | |
| Race/Ethnicity | 0.2421 | ||
| 1. White | 363 (59.6) | 1455 (56.2) | |
| 2. Black | 236 (38.8) | 1078 (41.6) | |
| 3. Other | 10 ( 1.6) | 58 ( 2.2) | |
| Insurance | 0.4647 | ||
| 1. Commercial | 399 (65.5) | 1615 (62.3) | |
| 2. Medicare | 176 (28.9) | 822 (31.7) | |
| 3. Medicaid | 25 ( 4.1) | 121 ( 4.7) | |
| 4. Other/Uninsured/Unknown | 9 ( 1.5) | 33 ( 1.3) | |
| Encounter Type | <.0001 | ||
| 1. Outpatient | 538 (88.3) | 1845 (71.2) | |
| 2. Inpatient | 40 ( 6.6) | 532 (20.5) | |
| 3. ER | 28 ( 4.6) | 119 ( 4.6) | |
| Any Elixhauser Comorbidity | <.0001 | ||
| No | 259 (42.5) | 520 (20.1) | |
| Yes | 350 (57.5) | 2071 (79.9) | |
| Kidney Stone | 25 ( 4.1) | 95 ( 3.7) | 0.6082 |
| Fracture | 19 ( 3.1) | 197 ( 7.6) | <.0001 |
| Osteoporosis | 43 ( 7.1) | 259 (10.0) | 0.0258 |
| Year of Index Calcium | |||
| 2011 | 121 (19.9) | 579 (22.3) | 0.14 |
| 2012 | 122 (20.0) | 496 (19.1) | |
| 2013 | 129 (21.2) | 446 (17.2) | |
| 2014 | 107 (17.6) | 503 (19.4) | |
| 2015 | 130 (21.3) | 567 (21.9) |
Acknowledgments
Funding Source: This work was supported by an AHRQ mentored career development award (K12 HS023009-03) for Dr. Balentine.
Footnotes
Disclaimers: None of the authors have any conflicts of interest to report. All authors approved the final version of the manuscript. The authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Zanocco KA, Wu JX, Yeh MW. Parathyroidectomy for asymptomatic primary hyperparathyroidism: A revised cost-effectiveness analysis incorporating fracture risk reduction. Surgery.161(1):16–24. [DOI] [PubMed] [Google Scholar]
- 2.Aliabadi-Wahle S, Kelly TL, Rozenfeld Y, et al. Treatment Strategies for Primary Hyperparathyroidism: What Is the Cost? The American Surgeon. 2014;80(11):1146–1151. [PubMed] [Google Scholar]
- 3.Weber T, Eberle J, Messelhäuser U, et al. Parathyroidectomy, elevated depression scores, and suicidal ideation in patients with primary hyperparathyroidism: Results of a prospective multicenter study. JAMA Surgery. 2013;148(2):109–115. [DOI] [PubMed] [Google Scholar]
- 4.Cheng S-P, Lee J-J, Liu T-P, et al. Quality of Life After Surgery or Surveillance for Asymptomatic Primary Hyperparathyroidism: A Meta-Analysis of Randomized Controlled Trials. Medicine. 2015;94(23):e931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brito K, Edirimanne S, Eslick GD. The extent of improvement of health-related quality of life as assessed by the SF36 and Paseika scales after parathyroidectomy in patients with primary hyperparathyroidism – A systematic review and meta-analysis. International Journal of Surgery.13:245–249. [DOI] [PubMed] [Google Scholar]
- 6.Wilhelm SM, Wang TS, Ruan DT, et al. The american association of endocrine surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surgery. 2016;151(10):959–968. [DOI] [PubMed] [Google Scholar]
- 7.Lou I, Balentine C, Clarkson S, Schneider DF, Sippel RS, Chen H. How Long Should We Follow Patients After Apparently Curative Parathyroidectomy? Surgery. 2017;161(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bilezikian JP, Cusano NE, Khan AA, Liu JM, Marcocci C, Bandeira F. Primary hyperparathyroidism. Nat Rev Dis Primers. 2016;2:16033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeh MW, Wiseman JE, Ituarte PH, et al. Surgery for primary hyperparathyroidism: are the consensus guidelines being followed? Ann Surg. 2012;255(6):1179–1183. [DOI] [PubMed] [Google Scholar]
- 10.Press DM, Siperstein AE, Berber E, et al. The prevalence of undiagnosed and unrecognized primary hyperparathyroidism: A population-based analysis from the electronic medical record. Surgery. 2013;154(6):1232–1238. [DOI] [PubMed] [Google Scholar]
- 11.Wu B, Haigh PI, Hwang R, et al. Underutilization of Parathyroidectomy in Elderly Patients with Primary Hyperparathyroidism. The Journal of Clinical Endocrinology and Metabolism. 2010;95(9):4324–4330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 13.Sippel RS. Under-recognition of the benefits of parathyroidectomy leads to underdiagnosis of the disease. Surgery. 2013;154(6):1230–1231. [DOI] [PubMed] [Google Scholar]
- 14.Singh H, Spitzmueller C, Petersen NJ, Sawhney MK, Sittig DF. Information overload and missed test results in electronic health record–based settings. JAMA Internal Medicine. 2013;173(8):702–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Applewhite MK, White MG, Tseng J, et al. Normohormonal primary hyperparathyroidism is a distinct form of primary hyperparathyroidism. Surgery.161(1):62–69. [DOI] [PubMed] [Google Scholar]
- 16.Damschroder LJ, Goodrich DE, Robinson CH, Fletcher CE, Lowery JC. A systematic exploration of differences in contextual factors related to implementing the MOVE! weight management program in VA: A mixed methods study. BMC Health Services Research. 2011;11(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]


