Abstract
Background—
The Mission: Lifeline STEMI Systems Accelerator program, implemented in 16 US metropolitan regions, resulted in more patients receiving timely reperfusion. We assessed whether implementing key care processes was associated with system performance improvement.
Methods and Results—
Hospitals (n=167 with 23 498 ST-segment–elevation myocardial infarction patients) were surveyed before (March 2012) and after (July 2014) program intervention. Data were merged with patient-level clinical data over the same period. For reperfusion, hospitals were grouped by whether a specific process of care was implemented, preexisting, or never implemented. Uptake of 4 key care processes increased after intervention: prehospital catheterization laboratory activation (62%–91%; P<0.001), single call transfer protocol from an outside facility (45%–70%; P<0.001), and emergency department bypass for emergency medical services direct presenters (48%–59%; P=0.002) and transfers (56%–79%; P=0.001). There were significant differences in median first medical contact-to-device times among groups implementing prehospital activation (88 minutes implementers versus 89 minutes preexisting versus 98 minutes nonimplementers; P<0.001 for comparisons). Similarly, patients treated at hospitals implementing single call transfer protocols had shorter median first medical contact-to-device times (112 versus 128 versus 152 minutes; P<0.001). Emergency department bypass was also associated with shorter median first medical contact-to-device times for emergency medical services direct presenters (84 versus 88 versus 94 minutes; P<0.001) and transfers (123 versus 127 versus 167 minutes; P<0.001).
Conclusions—
The Accelerator program increased uptake of key care processes, which were associated with improved system performance. These findings support efforts to implement regional ST-segment–elevation myocardial infarction networks focused on prehospital catheterization laboratory activation, single call transfer protocols, and emergency department bypass.
Introduction
Primary percutaneous coronary intervention (PCI) is the preferred method of revascularization for acute ST-segment–elevation myocardial infarction (STEMI).1 For patients undergoing primary PCI, clinical guidelines recommend a first medical contact (FMC)-to-device time of <90 minutes for patients presenting to a PCI-capable hospital and <120 minutes for patients presenting to a non-PCI-capable hospital.1 However, ≈30% to 50% of patients are not reperfused within those timeframes.2–5 This cannot be completely explained by inadequate access because 90% of Americans live within 60 minutes of PCI-capable hospitals, and this figure continues to grow at a rate exceeding that of the US population.6–9 The challenges in meeting target reperfusion times are often because of system issues that hinder coordination between emergency medical service (EMS) providers and hospitals and competition among hospitals and integrated physician groups.10
The American Heart Association Mission: Lifeline STEMI Systems Accelerator program was developed and implemented in 16 US metropolitan regions to organize leadership, develop common protocols, and initiate ongoing data collection and timely review to improve the proportion of patients receiving timely coronary intervention.10 This program significantly but modestly increased the overall proportion of patients meeting guideline goals for FMC-to-device times both for patients presenting directly to a PCI-capable hospital and those transferred from non-PCI-capable hospitals.10a
Few studies have compared the impact of multiple STEMI patient flow care processes on reperfusion times.11–14 To our knowledge, no prior studies have determined the specific impact on systems performance of rapidly implementing care processes across multiple heterogeneous STEMI systems as part of a large-scale, national effort. Therefore, the goal of the current study was to (1) determine the uptake of recommended care processes and protocols across hospitals using a pre- and postimplementation survey as part of a large-scale national effort to regionalize STEMI care and (2) determine whether hospitals implementing one of 4 specific key care processes had shorter reperfusion times versus those that did not.
Methods
The STEMI Accelerator intervention was organized and executed between March 2012 and July 2014 in 171 hospitals and 23 809 patients, as previously described.10,14 Each region identified a baseline quarter as the preintervention period, with the remaining quarters considered the postintervention period. Project initiation was conducted on a rolling basis over 6 months, and each region specified a quarter (quarters 3 or 4, 2012; or quarter 1, 2013) as the baseline from which to assess subsequent temporal trends in outcomes. The following 16 of 21 regions that applied for participation in the project met enrollment criteria by the baseline data collection quarter and were included: Atlanta, GA; Columbus, OH; Denver, CO; Hartford, CT; Houston, TX; Kern County, CA; Louisville, KY; New York City, NY; Northern New Jersey; Oklahoma City, OK; Philadelphia, PA; Pittsburgh, PA; St. Louis, MO; San Antonio, TX; Tampa, FL; and Wilkes-Barre/Scranton, PA. All hospitals within participating regions were enrolled in the National Cardiovascular Data Registry ACTION Registry-GWTG program (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With The Guidelines), described in more detail below.15 Each region developed common protocols for STEMI care based on guideline recommendations. A detailed description of the protocol has been published previously.10 All patients with ongoing ischemic symptoms lasting for >10 minutes but <12 hours and who had ECG-diagnosed ST-segment–elevation or left bundle-branch block were included. In cases where the first ECG did not have diagnostic ST-segment–elevation, FMC-to-device time was reset to the time of the first diagnostic ECG.
Reperfusion and Outcomes Data
The ACTION Registry-GWTG15 is a voluntary quality improvement registry in the United States that includes consecutive patients admitted to participating hospitals with STEMI or non-STEMI. This program is sponsored by the American College of Cardiology and the American Heart Association. Definitions for data elements of the registry are available at https://www.ncdr.com/webncdr/action/home/datacollection. The National Cardiovascular Data Registry data quality program includes data abstraction training, data quality thresholds for inclusion, site data quality feedback reports, independent auditing, and data validation. An audit of the data has demonstrated chart review agreement in >93% of patients.16 At participating sites, this registry was either approved by an institutional review board or considered quality assurance data and was, therefore, not subject to institutional review board approval based on individual site determinations. The Duke Clinical Research Institute serves as the data coordinating center to analyze deidentified data for research purposes.
Pre- and Postimplementation Survey
American Heart Association Mission: Lifeline coordinators at each participating hospital were contacted via mail or phone to answer a series of questions related to STEMI processes of care and other hospital procedures (Supplement S1 in the Data Supplement). Respondents answered each question at 2 different time points: (1) prior to implementation of STEMI regionalization (preintervention, quarter 1: region-dependent, but typically between July to September or October to December 2012) and (2) after implementation of STEMI regionalization (postintervention, after quarter 7: July to September 2014).
For the purpose of analyzing the relationship between the uptake of 4 key STEMI care processes and reperfusion times, hospitals were stratified according to pre- and postintervention survey responses: (1) hospitals that did not have the care process in place at baseline, but subsequently implemented the existing care process postintervention; (2) hospitals that had an existing care process in place at baseline; and (3) hospitals that did not have the care process in place at baseline and did not implement postintervention. The 4 care processes evaluated were the following:
Prehospital cardiac catheterization laboratory activation for patients presenting directly via EMS to a PCI-capable hospital.
Single call primary PCI transfer protocol for patients presenting to a non-PCI-capable hospital.
Emergency department (ED) bypass for patients presenting directly via EMS to a PCI-capable hospital (bypass was defined as <5 minutes in the ED).
ED bypass for patients transferred from a non-PCI-capable hospital to a PCI-capable hospital (with bypass again defined as <5 minutes in the ED).
Out of 171 STEMI Accelerator PCI-capable hospitals in 16 regions, 167 (97%) hospitals completed and returned the care processes survey. No outcomes data were revealed or known to the investigators until all the survey data were collected. Patient-level data, including reperfusion times, were linked to specific hospitals using American Hospital Association numbers. The overall study flow chart is shown in Figure 1.
Figure 1.

Study flow chart. ED indicates emergency department; FMC, first medical contact; GWTG, Get With The Guidelines; and PCI, percutaneous coronary intervention.
Statistical Analysis
Descriptive statistics for continuous and categorical variables were described as medians (interquartile ranges) and numbers (percentages), respectively. Patient characteristics and process measures were compared by use of the Wilcoxon rank-sum test for 2-group comparisons (the Kruskal–Wallis test was used for comparisons of >2 groups) and Pearson’s χ2 or Fisher’s exact tests as appropriate. A multivariable logistic regression model was used to estimate the adjusted odds ratio and 95% confidence interval for in-hospital mortality outcome based on variables found to be predictive of in-hospital mortality in the ACTION Registry-GWTG risk score17: age, baseline creatinine, systolic blood pressure, initial troponin, heart failure on presentation, cardiogenic shock on presentation, heart rate, and a history of peripheral artery disease. In addition to the above variables, out-of-hospital cardiac arrest, a strong predictor of in-hospital mortality in ACTION-Registry GWTG hospitals,18 was also included in the model. FMC-to-device time data were presented and summarized graphically using mountain plots, which represent a folded-empirical distribution function curve of the data at the 50th percentile (median).19
All statistical tests were conducted at the 0.05 significance level. Statistical analyses were performed with SAS version 9.2 or higher (SAS Institute Inc, Cary, NC). The project was reviewed by the Duke University Institutional Review Board and classified as exempt.
Results
Pre- and Postimplementation Survey
In the 167 hospitals surveyed, uptake of each of the 4 key processes increased after intervention (Figure 2): prehospital activation (62%–91%; P<0.001), single call transfer protocol (45%–70%; P<0.001), and ED bypass for direct presenters (48%–59%; P=0.002) and transfer patients (56%–79%; P=0.001). Uptake of most other care processes also increased after intervention (Supplement S2 in the Data Supplement).
Figure 2.
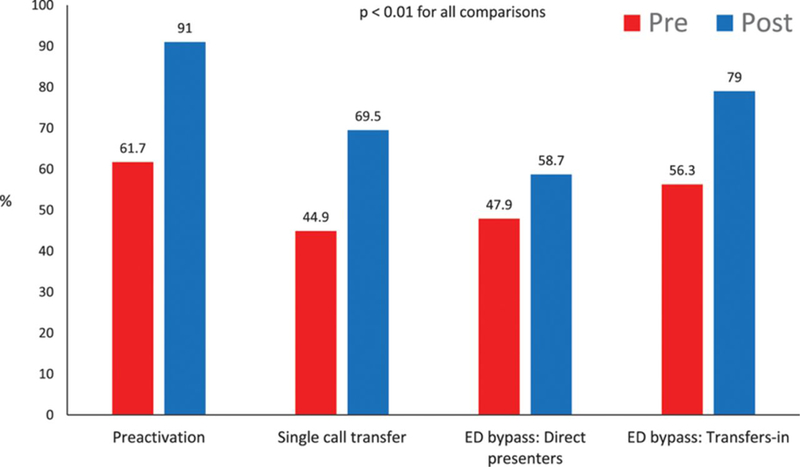
Uptake of 4 key care processes across 167 hospitals during the STEMI accelerator program. ED indicates emergency department; and STEMI, ST-segment–elevation myocardial infarction.
Patient Characteristics and Presentation
Between 2012 quarter 3 and 2014 quarter 1 (7 quarters), 23 809 patients presented with acute STEMI, including 18 267 patients who presented directly to a PCI-capable hospital and 5542 who were transferred from hospitals without PCI capability. Among those presenting to PCI-capable hospitals, 64% (n=11 765) were transported by EMS providers, while 36% (n=6502) arrived by self-transport.14 For the current analysis, overall patient clinical characteristics did not change between quarter 1 and quarter 7 (Table 1), with some exceptions. Compared with quarter 1, patients in quarter 7 were more likely to be male (72.2% versus 70.0%; P=0.044), insured through Medicaid (11.0% versus 9.2%; P=0.03), and considered a reperfusion candidate (96.6% versus 93.9%; P<0.0001), but these patients were less likely to have prior heart failure (2.7% versus 3.5%; P=0.025).
Table 1.
Patient Characteristics for All STEMI Patients: Quarter 1 Versus Quarter 7
| Characteristic | Quarter 1 (N=3477) | Quarter 7 (N=3311) |
P Value |
|---|---|---|---|
| Median age, y | 61.0 (52.0–70.0) | 60.0 (52.0–70.0) | 0.72 |
| Male sex | 2433 (70.0%) | 2391 (72.2%) | 0.044 |
| Race | 0.22 | ||
| White | 2913 (83.8%) | 2724 (82.3%) | |
| Black | 375 (10.8%) | 381 (11.5%) | |
| Other | 189 (5.4%) | 206 (6.2%) | |
| Latino ethnicity | 358 (10.3%) | 323 (9.8%) | 0.47 |
| Insurance | |||
| Private/HMO | 1912 (55.0%) | 1860 (56.2%) | 0.64 |
| Medicaid | 321 (9.2%) | 363 (11.0%) | 0.03 |
| None | 565 (16.2%) | 505 (15.3%) | 0.27 |
| Other | 707 (20.3%) | 632 (19.1%) | 0.2 |
| Prior myocardial infarction | 376 (10.8%) | 416 (12.6%) | 0.11 |
| Prior heart failure | 123 (3.5%) | 90 (2.7%) | 0.02 |
| Prior PCI | 443 (12.7%) | 441 (13.3%) | 1 |
| Prior coronary bypass surgery | 132 (3.8%) | 121 (3.7%) | 0.52 |
| Diabetes mellitus | 919 (26.4%) | 876 (26.5%) | 0.98 |
| Median symptom onset to FMC (minutes) | 69.0 (31.0–172.0) | 68.5 (31.5–167.5) | 0.58 |
| Shock on presentation | 262 (7.5%) | 278 (8.4%) | 0.19 |
| Cardiac arrest | 253 (7.3%) | 267 (8.1%) | 0.25 |
| Heart failure on presentation | 239 (6.9%) | 222 (6.7%) | 0.81 |
| Reperfusion candidate | 3264 (93.9%) | 3200 (96.6%) | <0.0001 |
| Median heart rate on presentation, bpm | 80.0 (66.0–93.0) | 80.0 (66.0–93.0) | 0.21 |
| Median systolic blood pressure, mm Hg | 140.0 (119.0–160.0) | 140.0 (120.0–163.0) | 0.37 |
| STEMI first diagnosed | 0.81 | ||
| First ECG | 3403 (97.9%) | 3233 (97.6%) | |
| Subsequent | 46 (1.3%) | 50 (1.5%) | |
| Procedures during hospitalization | |||
| PCI | 3096 (89.0%) | 2982 (90.1%) | 0.18 |
| Coronary bypass surgery | 142 (4.1%) | 137 (4.1%) | 0.95 |
| Complications | |||
| In-hospital death | 195 (5.6%) | 198 (6.0%) | 0.51 |
| Stroke | 18 (0.5%) | 26 (0.8%) | 0.17 |
| Cardiogenic shock | 267 (7.7%) | 254 (7.7%) | 1 |
| Congestive heart failure | 212 (6.1%) | 202 (6.1%) | 1 |
| Major bleeding | 152 (4.4%) | 158 (4.8%) | 0.45 |
| Reinfarction | 32 (0.9%) | 24 (0.7%) | 0.42 |
| Not treated | 224 (6.4%) | 229 (6.9%) | 0.44 |
Data presented as n (%) or median (interquartile range). ECG indicates electrocardiogram; FMC, first medical contact-to-device time; HMO, health maintenance organization; PCI, percutaneous coronary intervention; and STEMI, ST-segment–elevation myocardial infarction
Reperfusion Times for Key STEMI Care Processes
There were significant differences in median FMC-to-device times among patients treated at hospitals that implemented preactivation for EMS transport to a PCI-capable hospital compared with nonimplementers (88 minutes for implementers versus 89 minutes for preexisting versus 98 minutes for nonimplementers; P<0.001 for group comparisons; Figure 3A). Similarly, patients treated at hospitals implementing single call transfer protocols at non-PCI-capable hospitals had shorter median FMC-to-device times (112 versus 128 versus 152 minutes; P<0.001). ED bypass was also associated with shorter FMC-to-device times for both direct presenters (84 versus 88 versus 94 minutes; P<0.001) and transfers (123 versus 127 versus 167 minutes; P<0.001; Figure 3B).
Figure 3.

Mountain (folded cumulative distribution at the 50th percentile) plots of first medical contact-to-device times (FMC) according to hospital implementation of prehospital cardiac catheterization activation and single call transfer protocol (A) and emergency department (ED) bypass for patients presenting directly to a percutaneous coronary intervention (PCI)–capable hospital via emergency medical services or those transferred from a non-PCI-capable hospital to a PCI-capable hospital for primary PCI (B). The peak of each mountain plot represents the median reperfusion time (50th percentile, in minutes) for patients in that cohort.
In-Hospital Mortality
After adjustment for 9 variables associated with increased in-hospital mortality (ACTION Risk Score+cardiac arrest), we found no statistically significant difference in mortality between hospitals for any of the 4 key care processes of preactivation, single call transfer protocol, or ED bypass for both direct presenters and transfers (Table 2). However, hospitals that implemented all 4 care processes by the end of the STEMI Accelerator program (or had them preexisting) had numerically lower in-hospital mortality (6.0%) compared with those implementing only 1 (6.2%), 2 (6.3%), or 3 (7.3%) processes (Supplemental S3 in the Data Supplement).
Table 2.
Comparison of Adjusted In-Hospital Mortality for Key Care Processes
| OR (95% CI) | P Value | |
|---|---|---|
| Preactivation | ||
| Preexisting vs implemented | 0.90 (0.71–1.13) | 0.37 |
| Preexisting vs did not implement | 1.26 (0.54–2.92) | 0.6 |
| Implemented vs did not implement | 1.40 (0.59–3.29) | 0.45 |
| Single call transfer | ||
| Preexisting vs implemented | 0.76 (0.47–1.21) | 0.25 |
| Preexisting vs did not implement | 1.26 (0.91–1.76) | 0.17 |
| Implemented vs did not implement | 1.67 (0.99–1.81) | 0.053 |
| ED bypass: directs | ||
| Preexisting vs implemented | 0.87 (0.66–1.14) | 0.31 |
| Preexisting vs did not implement | 0.93 (0.73–1.19) | 0.52 |
| Implemented vs did not implement | 1.07 (0.83–1.38) | 0.59 |
| ED bypass: transfers | ||
| Preexisting vs implemented | 0.85 (0.55–1.3) | 0.46 |
| Preexisting vs did not implement | 1.09 (0.59–2.00) | 0.78 |
| Implemented vs did not implement | 1.28 (0.63–2.60) | 0.45 |
CI indicates confidence interval; ED, emergency department; and OR, odds ratio.
Discussion
The overall goal of this study was to determine the impact of rapidly implementing care processes across multiple heterogeneous STEMI systems as part of a large scale, national effort. We found that after implementation of the STEMI Accelerator program, there was a significant uptake in several care processes. Importantly, we found that hospitals implementing the key care processes of prehospital activation of a cardiac catheterization laboratory, single call transfer protocol from an non-PCI-capable facility, or ED bypass for both direct EMS presenters or transfers had shorter median reperfusion times compared with hospitals that did not implement these processes and comparable reperfusion times compared with hospitals that had the process in place at baseline.
Our work extends that of prior observational studies, which found associations between STEMI care processes and improved reperfusion times, including preactivation of the cardiac catheterization laboratory,20 interfacility transfer for primary PCI,5 and ED bypass.3,4 Some smaller studies have compared the impact of STEMI patient flow care process intervention on outcomes, such as reperfusion times and infarct size.11–13 However, to our knowledge, this is the first study to demonstrate the specific impact on systems performance of rapidly implementing care processes across multiple heterogeneous STEMI systems on such a large-scale basis, involving nearly one quarter of all STEMI patients in the United States during this study time period. Furthermore, by merging hospital-level care process data with patient-level data on reperfusion times, we are able to demonstrate that efforts at implementation were associated with modest reductions in reperfusion times using the most contemporary, guideline-recommended reperfusion metric, FMC-to-device time.
This study has several important implications. First, we show that STEMI systems may be rapidly implemented with data collection, feedback, multidisciplinary team engagement, and importantly, adopting specific key care processes. Second, times to reperfusion in systems implementing processes were comparable to those with preexisting processes. This provides a critical and positive message for regions who have not yet adopted formalized reperfusion protocols, demonstrating that system performance can improve in a timely fashion. As a corollary, our data also demonstrate that hospitals that do not implement key STEMI care processes continue to have the longest reperfusion times. Further, the overall program costs are relatively modest at $USD 1.9 million for the additional resources to implement regionalization across all study regions. This translates into a cost per patient of ≈$USD 80 ($1 900 000/23 809 STEMI patients in Accelerator). We think that this additional expense is fairly modest on a per-patient basis compared with the total cost of a single hospitalization for STEMI patients, recently reported to range from $23 000 to $28 000 based on Nationwide Inpatient Sample data.21 Overall, these data support efforts to optimize STEMI systems, with ongoing focus on the key processes to reduce FMC-to-device times.
There are some limitations. The survey results were reported by representatives in regions, whereby all hospitals were participating in the ACTION Registry-GWTG and, thus, may be at risk for both reporting and selection bias. However, this strategy to assess care process implementation was independent of reperfusion time reporting, which was captured by the ACTION Registry-GWTG; therefore, the findings that care process implementation was associated with shorter reperfusion times are likely robust. We also focused on 4 key care processes and others not studied or yet to be analyzed may be important to reduce reperfusion times. However, these care processes were specifically chosen to be important determinants of system performance3,5,10,20 and highly modifiable at a hospital and regional level; we now extend these findings to a national level. We have limited power to evaluate subgroups based on individual processes because of unmeasured or unmeasurable system factors, as well as a lack of power to reliably assess impact on mortality, which was neutral in this study. With relatively smaller sample sizes and observational data, it may be unrealistic to expect a significant change in overall mortality during a relatively short follow-up period, particularly when some systems of care were already functioning well at baseline.14,22 Finally, we are unable to adequately compare the relative benefit of each care process over another because hospitals may have used >1 care process at a time.
The neutral mortality results may also be related to secular trends demonstrating increasing mortality risk in contemporary STEMI populations,23,24 which could then offset gains in patients with shorter reperfusion times (survivor–cohort effect).25 We found numeric (but not statistically significant) increases in both shock (7.5%–8.4%) and cardiac arrest (7.3%–8.1%) at presentation between quarters 1 and 7, suggestive of a temporal increase in risk among STEMI patients within our study (Table 1). While we were unable to demonstrate a mortality benefit associated with shorter reperfusion times at the population level, the benefit of shorter reperfusion times to decrease mortality at the individual patient level is still clear.26 As discussed earlier, our study may be underpowered to show a mortality benefit in our population or longer follow-up may be required to demonstrate the impact of implementing such care processes. We did find a numerically lower in-hospital mortality among hospitals that had implemented all 4 care processes by the end of the Accelerator program, compared with those that had implemented 1 to 3 processes (Supplement S3 in the Data Supplement). However, a dose–response trend was not observed between number of processes and mortality; therefore, these results should be interpreted with caution.
In conclusion, this study found that the rapid uptake of several care processes occurred during STEMI Accelerator implementation across multiple STEMI systems within the United States. The implementation of key care processes (preactivation, single call transfer, ED bypass for both direct EMS presenters and transfers) was associated with improved reperfusion times. Efforts to optimize STEMI systems should continue and with a focus of these key care processes.
Supplementary Material
WHAT IS KNOWN
Few studies have compared the impact of multiple ST-segment–elevation myocardial infarction (STEMI) patient flow care processes on reperfusion times.
No prior studies have determined the specific impact on system performance of rapidly implementing care processes across multiple heterogeneous STEMI systems at a national level.
WHAT THE STUDY ADDS
Through the American Heart Association STEMI Systems Accelerator Project, the first effort to regionalize STEMI care nationally, we found that hospitals implementing key care processes (preactivation, single call transfer, emergency department bypass for both direct emergency medical service presenters and transfers) had shorter reperfusion times compared with hospitals that did not implement these processes.
Our results support efforts to continue to optimize STEMI systems, with a focus on these key care processes.
Acknowledgments
We dedicate this article to the late Dr Lee Garvey, whose expertise, passion, and wisdom have been essential to this work We thank Morgan deBlecourt for her editorial contributions, which were provided as part of her regular duties as an employee of the Duke Clinical Research Institute.
Sources of Funding
The Regional Systems of Care Demonstration Project: Mission: Lifeline STEMI Systems Accelerator is supported by the ACTION Registry-Get With The Guidelines and education and research grants by The Medicines Company, Abiomed, Inc, Philips Healthcare, and AstraZeneca. Dr Fordyce received support from the University of British Columbia Clinician Investigator Program.
Footnotes
Disclosures
Dr Jollis reported research grants from The Medicines Company, Astra Zeneca, Medtronic Foundation, Philips Healthcare, and Abiomed, Inc. Dr Berger reported research grants from Janssen, The Medicines Company, Astra Zeneca, Lilly, and Sanofi and consultant from Janssen and Medicure. Dr Dauerman reported consultant from Medtronic, Boston Scientific, Daiichi Sankyo, and The Medicines Company and research grants from Medtronic and Abbott Vascular. Dr Garvey reported research support and advisory board member: Philips Healthcare. Dr Sherwood reported honoraria from Boehringer Ingelheim, education grant from AstraZeneca, and project grant from Gilead Sciences. Dr Wilson reported consultant: Medical Advisory Board: Boston Scientific Corporation.
Dr Granger is available at https://dcri.org/about-us/conflict-of-interest. The other authors report no conflicts.
Contributor Information
Christopher B. Fordyce, Division of Cardiology, University of British Columbia, Vancouver, Canada; Duke Clinical Research Institute, Durham, NC
Hussein R. Al-Khalidi, Duke Clinical Research Institute, Durham, NC
James G. Jollis, University of North Carolina, Chapel Hill
Mayme L. Roettig, Duke Clinical Research Institute, Durham, NC
Joan Gu, Duke Clinical Research Institute, Durham, NC
Akshay Bagai, St. Michael’s Hospital, University of Toronto, ON, Canada
Peter B. Berger, Northwell Health, Great Neck, NY
Claire C. Corbett, New Hanover Regional Medical Center, Wilmington, NC
Harold L. Dauerman, of Vermont College of Medicine, Burlington
Kathleen Fox, Duke Clinical Research Institute, Durham, NC
J. Lee Garvey, Department of Emergency Medicine, Carolinas Medical Center, Charlotte, NC.
Timothy D. Henry, Cedars-Sinai Heart Institute, Los Angeles, CA
Ivan C. Rokos, UCLA–Olive View Medical Center, Los Angeles, CA
Matthew W. Sherwood, Duke Clinical Research Institute, Durham, NC
B. Hadley Wilson, Sanger Heart & Vascular Institute, Carolinas Medical Center, Charlotte, NC
Christopher B. Granger., Duke Clinical Research Institute, Durham, NC
References
- 1.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 2.Dauerman HL, Bates ER, Kontos MC, Li S, Garvey JL, Henry TD, Manoukian SV, Roe MT. Nationwide analysis of patients with ST-segment-elevation myocardial infarction transferred for primary percutaneous intervention: findings from the American Heart Association Mission: Lifeline Program. Circ Cardiovasc Interv. 2015;8:e002450. [DOI] [PubMed] [Google Scholar]
- 3.Bagai A, Al-Khalidi HR, Muñoz D, Monk L, Roettig ML, Corbett CC, Garvey JL, Wilson BH, Granger CB, Jollis JG. Bypassing the emergency department and time to reperfusion in patients with prehospital ST-segment-elevation: findings from the reperfusion in acute myocardial infarction in Carolina Emergency Departments project. Circ Cardiovasc Interv. 2013;6:399–406. doi: 10.1161/CIRCINTERVENTIONS.112.000136. [DOI] [PubMed] [Google Scholar]
- 4.Bagai A, Jollis JG, Dauerman HL, Peng SA, Rokos IC, Bates ER, French WJ, Granger CB, Roe MT. Emergency department bypass for ST-Segment-elevation myocardial infarction patients identified with a prehospital electrocardiogram: a report from the American Heart Association Mission: lifeline program. Circulation. 2013;128:352–359. doi: 10.1161/CIRCULATIONAHA.113.002339. [DOI] [PubMed] [Google Scholar]
- 5.Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle BL, Xian Y, Garvey JL, Mears G, Corbett CC, Peterson ED, Glickman SW. The impact of a statewide pre-hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–612. [DOI] [PubMed] [Google Scholar]
- 6.Langabeer JR, Henry TD, Kereiakes DJ, Dellifraine J, Emert J, Wang Z, Stuart L, King R, Segrest W, Moyer P, Jollis JG. Growth in percutaneous coronary intervention capacity relative to population and disease prevalence. J Am Heart Assoc. 2013;2:e000370. doi: 10.1161/JAHA.113.000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah RU, Henry TD, Rutten-Ramos S, Garberich RF, Tighiouart M, Bairey Merz CN. Increasing percutaneous coronary interventions for ST-segment elevation myocardial infarction in the United States: progress and opportunity. JACC Cardiovasc Interv. 2015;8(1pt B):139–146. doi: 10.1016/j.jcin.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Nallamothu BK, Bates ER, Wang Y, Bradley EH, Krumholz HM. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 9.Concannon TW, Nelson J, Kent DM, Griffith JL. Evidence of systematic duplication by new percutaneous coronary intervention programs. Circ Cardiovasc Qual Outcomes. 2013;6:400–408. doi: 10.1161/CIRCOUTCOMES.111.000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagai A, Al-Khalidi HR, Sherwood MW, Muñoz D, Roettig ML, Jollis JG, Granger CB. Regional systems of care demonstration project: Mission: Lifeline STEMI Systems Accelerator: design and methodology. Am Heart J. 2014;167:15–21.e3. doi: 10.1016/j.ahj.2013.10.005.10a. Jollis JG, Al-Khalidi HR, Roettig ML, Berger PB, Corbett CC, Dauerman HL, Fordyce CB, Fox K, Garvey JL, Gregory T, Henry TD, Rokos IC, Sherwood MW, Suter RE, Wilson BH, Granger CB;Mission: Lifeline STEMI Systems Accelerator Project. Regional systems of care demonstration project: American Heart Association Mission: Lifeline STEMI Systems Accelerator. Circulation. 2016;134:365–374. doi: 10.1161/CIRCULATIONAHA.115.019474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glickman SW, Lytle BL, Ou FS, Mears G, O’Brien S, Cairns CB, Garvey JL, Bohle DJ, Peterson ED, Jollis JG, Granger CB. Care processes associated with quicker door-in-door-out times for patients with ST-elevation-myocardial infarction requiring transfer: results from a statewide regionalization program. Circ Cardiovasc Qual Outcomes. 2011;4:382–388. [DOI] [PubMed] [Google Scholar]
- 12.Ranasinghe I, Turnbull F, Tonkin A, Clark RA, Coffee N, Brieger D. Comparative effectiveness of population interventions to improve access to reperfusion for ST-segment-elevation myocardial infarction in Australia. Circ Cardiovasc Qual Outcomes. 2012;5:429–436. doi: 10.1161/CIRCOUTCOMES.112.965111. [DOI] [PubMed] [Google Scholar]
- 13.Jones WS, Clare RM, Chiswell K, Perera D, French JK, Kumar AS, Blaxill J, Pijls N, Mills J, Ohman EM, Patel MR. The impact of processes of care on myocardial infarct size in patients with ST-segment elevation myocardial infarction: observations from the CRISP-AMI trial. Clin Cardiol. 2015;38:25–31. doi: 10.1002/clc.22349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherwood MW, Al-Khalidi HR, Jollis JG, Roettig ML, Berger PB, Corbett CC, Dauerman HL, Fox K, Garvey JL, Henry TD, Rokos IC, Wilson BH, Granger CB. Developing regional STEMI systems of care: final results of the Mission: Lifeline STEMI Accelerator Study. Circulation. 2014;130:2111. [Google Scholar]
- 15.Peterson ED, Roe MT, Rumsfeld JS, Shaw RE, Brindis RG, Fonarow GC, Cannon CP. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network) a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–499. [DOI] [PubMed] [Google Scholar]
- 16.Messenger JC, Ho KK, Young CH, Slattery LE, Draoui JC, Curtis JP, Dehmer GJ, Grover FL, Mirro MJ, Reynolds MR, Rokos IC, Spertus JA, Wang TY, Winston SA, Rumsfeld JS, Masoudi FA; NCDR Science and Quality Oversight Committee Data Quality Workgroup. The National Cardiovascular Data Registry (NCDR) Data Quality Brief: the NCDR Data Quality Program in 2012. J Am Coll Cardiol. 2012;60:1484–1488. doi: 10.1016/j.jacc.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 17.Chin CT, Chen AY, Wang TY, Alexander KP, Mathews R, Rumsfeld JS, Cannon CP, Fonarow GC, Peterson ED, Roe MT. Risk adjustment for in-hospital mortality of contemporary patients with acute myocardial infarction: the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) registry-Get With The Guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. 2011;161:113–122.e2. [DOI] [PubMed] [Google Scholar]
- 18.Kontos MC, Scirica BM, Chen AY, Thomas L, Anderson ML, Diercks DB, Jollis JG, Roe MT; NCDR. Cardiac arrest and clinical characteristics, treatments and outcomes among patients hospitalized with ST-elevation myocardial infarction in contemporary practice: a report from the National Cardiovascular Data Registry. Am Heart J. 2015;169:515–522.e1. doi: 10.1016/j.ahj.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Monti KL. Folded empirical distribution function curves—mountain plots. Am Stat. 1995;49:342–345. [Google Scholar]
- 20.Diercks DB, Kontos MC, Chen AY, Pollack CV, Wiviott SD, Rumsfeld JS, Magid DJ, Gibler WB, Cannon CP, Peterson ED, Roe MT. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161–166. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal S, Garg A, Parashar A, Jaber WA, Menon V. Outcomes and resource utilization in ST-elevation myocardial infarction in the United States: evidence for socioeconomic disparities. J Am Heart Assoc. 2014;3:e001057. doi: 10.1161/JAHA.114.001057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Henry TD, Jacobs AK, Granger CB. Regional systems of care for ST-elevation myocardial infarction: do they save lives? Am Heart J. 2013;166:389–391. doi: 10.1016/j.ahj.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 23.Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. [DOI] [PubMed] [Google Scholar]
- 24.Fordyce CB, Cairns JA, Singer J, Lee T, Park JE, Vandegriend RA, Perry M, Largy W, Gao M, Ramanathan K, Wong GC. Evolution and impact of a regional reperfusion system for ST-elevation myocardial infarction. Can J Cardiol. 2016;32:1222–1230. doi: 10.1016/j.cjca.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 25.Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 26.Nallamothu BK, Normand SL, Wang Y, Hofer TP, Brush JE, Messenger JC, Bradley EH, Rumsfeld JS, Krumholz HM. Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385:1114–1122. doi: 10.1016/S0140-6736(14)61932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


