Abstract
Purpose
To assess and compare the wetting kinetics of sheathed and unsheathed Schirmer's tear test (STT) strips, and to determine the repeatability of 5-minute wetted length (WL) and basal tear production rate (BTPR).
Methods
Seventeen subjects underwent two sheathed and unsheathed STTs each for both eyes on four visits on separate days. After administration of topical anesthetic, WLs were measured every 30 seconds for 5 minutes, and BTPRs were calculated for sheathed strips. Limits of agreement (LoA), difference-versus-mean plots (DVM), and the coefficient of repeatability (CR) assessed WL and BTPR repeatabilities. Variance estimates were used to calculate sample sizes for future study.
Results
For the unsheathed STT, the mean (SD) difference in WLs between visits was 0.74 (5.05) mm, LoA were [−9.17, 10.64], and CR was 9.17 mm; for the sheathed STT, the mean (SD) intervisit difference was 0.16 (5.94) mm, LoA were [−11.49, 11.8], and CR was 10.53 mm. Eight of 48 sheathed STTs and 20 of 44 unsheathed STTs showed constant WL for the final 90 seconds of the test. The mean (SD) difference between repeated visits for BTPR was approximately 0.0 μL/min, LoA were [−1.82, 1.82], and CR was 1.91 μL/min.
Conclusions
Repeatability of sheathed and unsheathed 5-minute WL and BTPR is inadequate for measuring within-subject changes, but is sufficient for group studies with moderate sample sizes. Constant WL for the final 90 seconds with the eight sheathed STT measurements suggests varying BTPR, whereas constant WL with the unsheathed STT can be explained by balancing evaporation and BTPR.
Translational Relevance
Repeatability of the modified STT is evaluated clinically to establish quantitative BTPRs rather than inference from a strip WL.
Keywords: tear production rate, dry eye, Schirmer strip, modified Schirmer's tear test, wetted length, repeatability, sample size estimation
Introduction
Schirmer's tear test (STT) is one of the most commonly employed clinical tests in dry-eye disease evaluation, treatment, and management. It is thought that inserting a strip of filter paper into the inferior fornix and measuring the length of the wetted portion after 5 minutes provides a direct assessment of tear production rate.1 In clinical practice, use of the STT is hampered by poor repeatability, which has been attributed mainly to a presumed natural variability in tear production rate.2 This assumption, however, may reflect incomplete understanding of what the test actually assesses. Recent studies highlight two issues that contribute to STT performance.3,4
The first issue addresses whether the traditional STT measures only the basal tear production or whether it also measures some degree of residual reflex tearing and/or uptake from the tear meniscus. There are two reported phases during an STT: rapid wetting upon initial insertion, followed by a slower, typically linear, increase with time.4 In the traditional STT without anesthetic, this observation is attributed to rapid initial wetting by reflex tearing upon strip insertion, followed by slower wetting due to basal tear production and diminished reflex tearing.5–8 Li et al.,4 however, observed significant variability in the initial wetting phase even though the eyes had been anesthetized with two drops of proparacaine, an anesthetic that should nullify most or all reflex tearing.9 Based on this observation, the authors argued that in addition to reflex tear production, the initial wetting phase is influenced by the preexisting tear reservoir behind the lower lid.4 Li et al.4 established that the 5-minute wetted length of a Schirmer strip does not always correlate with the basal tear production rate (BTPR). Due to significant inter- and intrapatient variation in the volume of tears held in the tear reservoir, which is likely influenced by ethnicity,10 medication use,11 tasks performed immediately prior to testing (e.g., computer use),12 and diurnal variation,13,14 the BTPR can be assessed only in the second phase, during which a slower linear increase in wetting is observed.
The second issue is that environmental conditions impact wetted length. For example, conducting an STT in low room humidity can lead to excessive evaporation from the wetted Schirmer strip that can contribute to an artificially short wetted length. This is in contrast to the wetted length measured in a high-humidity environment.15 This issue has largely been ignored in clinical practice. In contrast, the mechanistic model of Telles et al.3 estimates BTPR by accounting for the physical forces acting on the strip during wetting imbibition and quantifies the specific impact that evaporation has on wetted length. Based on the calculations of Telles et al.3 and the in vitro studies of Li et al.,4 evaporation can significantly slow wetting dynamics. Li et al.4 recommend that, in addition to application of anesthetic, Schirmer strips be sheathed with transparent plastic tape to inhibit evaporation. We refer to this procedure as the modified STT.3,4
In the current study, after applying anesthetic, we assess whether preventing evaporation from STT strips by sheathing them with plastic tape offers improved repeatability compared with traditional unsheathed strips. We also use the sheathed-strip transient wetted lengths to determine the BTPR, following the work of Li et al.4, and assess its repeatability. An STT with improved accuracy, combined with calculation of BTPR, can provide an important tool in the diagnosis and monitoring of dry-eye disease.
Methods
Study Protocol
Subjects were recruited from the University of California, Berkeley and the surrounding community. Both contact lens wearers and non–contact lens wearers were eligible to participate. Subjects with active ocular infection or inflammation were excluded, as were those who elected not to discontinue contact lens wear, use of makeup, artificial tears, and facial lotion for a minimum of 24 hours prior to all study visits. Written informed consent, with a complete description of the goals, risks, benefits, and procedures of the study, was obtained from all participants. This study observed the tenets of the Declaration of Helsinki and was approved by the University of California, Berkeley Committee for Protection of Human Subjects.
The study consisted of four visits: two visits using standard, unsheathed Schirmer strips bilaterally and two visits using sheathed Schirmer strips bilaterally, alternating visits between the two strip types. The type of strip used at the first visit and the eye to have the first strip inserted at each visit were randomized. Visits were separated by a minimum of 24 hours and were scheduled at approximately the same time of day (±2 hours) for each subject to minimize the potential for bias due to possible diurnal variation.13 Subjects were asked to awaken at approximately the same time of day (±1 hour) and to be awake for at least 4 hours prior to every visit.
At the beginning of each visit, room temperature and humidity were measured using a combination digital thermometer and hygrometer (General Tools & Instruments, Secaucus, NJ). For all tests, examination room temperature and relative humidity were held constant at approximately 22°C and 50%, respectively. Anterior ocular health was assessed with slit-lamp biomicroscopy (SL120; Carl Zeiss Meditec, Inc., Jena, Germany) under white light to ensure that there was no active or preexisting ocular pathology (e.g., corneal scars, infiltrates, superficial punctate keratitis). Subjects were acclimated to the ambient room environment for a minimum of 10 minutes prior to insertion of Schirmer strips bilaterally.
To minimize reflex tearing, two drops of 0.5% (wt/vol) proparacaine hydrochloride ophthalmic solution (Akorn Pharmaceuticals, Lake Forest, IL) were administered to each eye sequentially, with a 1-minute interval separating the bilateral applications. The eye previously randomized to have the Schirmer strip inserted also received the first anesthetic drop. If sheathed strips were randomly assigned for that visit, Schirmer strips (Merck Animal Health, Summit, NJ) were sheathed on both sides with water-impermeable transparent tape (One-Arm Bandit Tape Gun; Conros Corporation, North York, Canada) during the period of anesthetic administration. Further details on the sheathing technique can be found in Li et al.4 After drop instillation, the area around the eye was blotted with tissue paper to ensure that no residual fluid on the skin could come into contact with the Schirmer strip and artificially inflate wetted length. After waiting an additional minute for the second anesthetic drop to take effect, subjects were instructed to fixate on a point on the ceiling while a strip was inserted in each eye, and then to close their eyes. A single investigator was responsible for all strip insertions to eliminate interinvestigator variability in insertion technique. With the eyes still closed, subjects were led to the chinrest of the slit lamp and instructed to direct their eyes along the primary gaze axis. Wetted lengths of the millimeter-ruled Schirmer strip were recorded through the slit lamp to within 0.5 mm every 30 seconds for 5 minutes. Finally, after removal of the Schirmer strips, corneal staining type, depth, and extent were graded on the Brian Holden Vision Institute (formerly CCLRU) grading scales16 using sodium fluorescein under cobalt blue illumination and viewed through a 530-nm yellow barrier filter.
In addition to monitoring the wetted lengths of the sheathed STT strips, elimination of evaporative tear loss from the strip permitted calculation of the BTPR in microliters per minute. For standard Schirmer strips, Li et al.4 establish that
 |
where S is the straight-line slope of the measured wetted lengths between 3 and 5 minutes in millimeters per minute. Because of evaporative loss, BTPR is not readily quantified using unsheathed Schirmer strips.
Statistical Analysis
The repeatability of wetted-length measurement with sheathed and unsheathed Schirmer strips was first assessed by limits of agreement (LoA) with a variance estimate corrected for repeated measures, difference-versus-mean (DVM) plots,17 and the coefficient of repeatability (CR).18 The sheathed and unsheathed Schirmer-strip methods were then compared using the methods above and additionally by using multivariable linear mixed-effects models to account for the internal correlations engendered by the repeated-measures study design while statistically adjusting for external factors, including temperature and humidity, both outdoors and inside the examination room; outdoor wind speed (indoor ventilation “wind speed” was assumed to be constant); and time awake before measurement. Variance-component analysis partitioned the total variance of 5-minute wetted lengths into contributions from between-subject variability as well as differences between strips, visits, and eyes, and residual error. To obtain preliminary estimates of the sample variance and to estimate sample sizes necessary for statistical validity, 20 subjects were recruited for this investigation of sheathed Schirmer strips in modified STTs. Sample-size estimates for future larger group comparisons were made for differing wetted lengths and BPTRs, under the assumptions of 95% confidence and 80% power, using a range of between-subject variances from the current study as well as from the literature.19,20
Strip-wetting lengths were discerned only for subjects that exhibited wetted lengths greater than 5 mm after 5 minutes of strip insertion due to length-visibility limitations caused by eyelid concealment.4 For visits that resulted in unobservable wetted lengths at 5 minutes, wetted lengths were imputed to the median of the unobservable region (2.5 mm).
To avoid the initial nonlinear phase contribution from the tear meniscus, BTPR was calculated from the linear slope of the 3-, 4-, and 5-minute wetting lengths from Equation 1.4 Repeatability of the BTPR and the relationships of the BTPR to external factors were assessed using an approach similar to that described above for 5-minute wetted lengths. Wetted-strip lengths <5 mm were unobservable, so BTPR calculation was not possible whenever a subject did not exhibit at least three wetting lengths ≥5 mm recorded from 3 to 5 minutes.4 Readings of completely saturated strips (i.e., wetted lengths of 35 mm) 3 minutes after strip insertion were also excluded from the BTPR determination because no wetting-length dynamics could be assessed.
Results
Of the 20 subjects initially recruited, 17 subjects (5 males and 12 females, mean [SD] age = 34.4 [9.2] years) completed the study. Three subjects completed only the first visit and discontinued participation due to scheduling conflicts. Subject demographics consisted of 12 East Asians, 3 Caucasians, 1 African American, and 1 South Asian. Out of 17 subjects, eight were contact lens wearers and nine were non–contact lens wearers. Of the 136 total readings taken, nine subjects contributed 41 readings that were less than 5 mm in wetted length after 5 minutes of strip insertion. For those subjects, wetting lengths could not be evaluated. Twenty-one of the 41 readings were from unsheathed strips, and 20 were from sheathed strips. Descriptive statistics for all visits are shown in Table 1 for the sheathed and unsheathed Schirmer-strip 5-minute wetted lengths, along with examination room temperature and relative humidity.
Table 1.
Descriptive Statistics for 5-Minute Wetted Lengths (mm) of Unsheathed and Sheathed Schirmer Strips
| Variable |
Minimum |
Maximum |
Median |
Mean |
SD |
| Unsheathed strips | |||||
| Wetted length, mm, visit 1 | 2.5a | 26.0 | 7.5 | 8.9 | 6.81 |
| Exam room temperature, °C, visit 1 | 22.2 | 23.4 | 22.8 | 22.8 | 0.34 |
| Exam room relative humidity, %, visit 1 | 44 | 53 | 49.5 | 48.9 | 2.86 |
| Wetted length, mm, visit 2 | 2.5a | 18.0 | 7.0 | 8.2 | 5.36 |
| Exam room temperature, °C, visit 2 | 21.3 | 23.3 | 22.6 | 22.6 | 0.46 |
| Exam room relative humidity, %, visit 2 | 35 | 57 | 49 | 48.6 | 5.58 |
| Sheathed strips | |||||
| Wetted length, mm, visit 1 | 2.5a | 35.0 | 12.0 | 12.0 | 8.81 |
| Exam room temperature, °C, visit 1 | 21.9 | 23.4 | 22.7 | 22.7 | 0.38 |
| Exam room relative humidity, %, visit 1 | 44 | 54 | 50 | 49.5 | 2.83 |
| Wetted length, mm, visit 2 | 2.5a | 35.0 | 10.5 | 11.9 | 8.18 |
| Exam room temperature, °C, visit 2 | 21.4 | 23.4 | 22.8 | 22.7 | 0.51 |
| Exam room relative humidity, %, visit 2 | 39 | 55 | 50 | 49.1 | 4.57 |
Minimum wetted length was interpolated to the median of unobservable region of the Schirmer strip (2.5 mm).
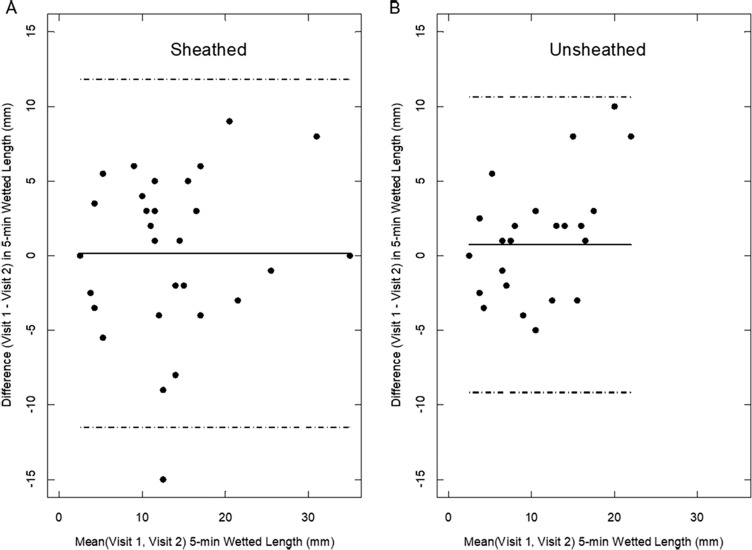
The mean difference between repeat visits in 5-minute wetted length was less than 1 mm for both sheathed and unsheathed Schirmer strips; the two strip types showed comparable repeatabilities. For unsheathed Schirmer strips, the mean (SD) difference was 0.74 (5.05) mm, and for sheathed strips the mean (SD) difference was 0.16 (5.94) mm (Table 2). LoA for unsheathed Schirmer strips were [−9.17, 10.64 mm], and for sheathed strips the LoA were [−11.49, 11.8 mm]. Figure 1 accentuates no dependence of the intervisit difference on the magnitude of the 5-minute wetted length. The CR between visits for unsheathed strips was 9.17 mm, meaning that the difference between two repeated tests lies within 9.17 mm with 95% probability. The CR for sheathed strips was 10.53 mm.
Table 2.
LoA Between Visits in 5-Minute Wetted Lengths (mm) of Unsheathed and Sheathed Schirmer Strips
| Variable |
Mean Diff |
SD Diff |
LoA |
||
| Lower |
Upper |
Width |
|||
| Unsheathed strips | |||||
| Wetted length Δ (V1−V2) | 0.74 | 5.05 | −9.17 | 10.64 | 19.81 |
| Sheathed strips | |||||
| Wetted length Δ (V1−V2) | 0.16 | 5.94 | −11.49 | 11.81 | 23.30 |
V indicates visit.
Figure 1.
Subject visit difference-versus-mean wetting lengths at 5 minutes for (A) sheathed and (B) unsheathed Schirmer strips. A solid line designates the mean intervisit difference. Dashed lines mark the LoA.
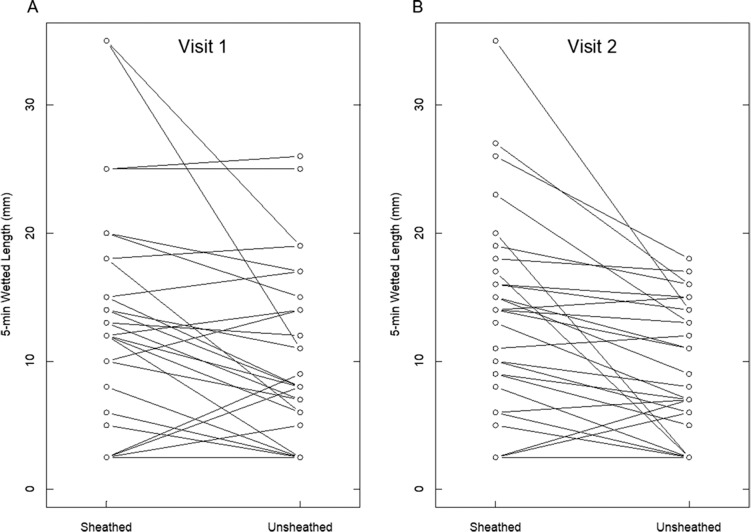
Comparison in Table 3 reveals a mean (SD) difference (sheathed − unsheathed) in wetted length of 3.16 (6.04) mm for the first set of visits (i.e., first sheathed visit compared to first unsheathed visit) and 3.74 (6.54) mm for the second set of visits. LoA between the two types of strips were [−8.67, 14.99 mm] for the first visit and [−9.08, 16.55 mm] for the second visit. DVM plots revealed no dependence of the difference between methods (sheathed versus unsheathed) on the magnitude of the 5-minute wetted length. As seen in Figure 2, sheathing the strips to inhibit evaporation generally increased wetted lengths compared to the unsheathed strips. Large differences between sheathed and unsheathed wetting lengths are evident for the longest 5-minute lengths because longer unsheathed wetted lengths expose more surface area for evaporation. Mixed-effects models of wetted length revealed sheathed strips to average 3.45-mm longer lengths than unsheathed strips (P < 0.001) after accounting for the repeated-measures structure. There was no significant difference between visits (P = 0.539) and no significant effects of indoor or outdoor temperature or indoor or outdoor humidity, outdoor wind speed, or time awake before measurement.
Table 3.
LoA Between Sheathed and Unsheathed Strip 5-Minute Wetted Lengths (mm)
| Variable |
Mean Diff |
SD Diff |
LoA |
||
| Lower |
Upper |
Width |
|||
| Visit 1 | |||||
| Wetted length Δ (S−U) | 3.16 | 6.04 | −8.67 | 14.99 | 23.66 |
| Visit 2 | |||||
| Wetted length Δ (S−U) | 3.74 | 6.54 | −9.08 | 16.55 | 25.62 |
S indicates sheathed, U, unsheathed.
Figure 2.
Five-minute wetting lengths for each subject with sheathed and unsheathed strips on (A) visit 1 and (B) visit 2. Sheathing inhibits evaporation during testing and allows for greater 5-minute wetted lengths on average.
Sample-size estimates for a hypothetical two-group comparison of Schirmer-strip 5-minute wetted lengths are shown in Table 4. As with all such estimates, the larger the variance or the smaller the difference one wishes to detect, the larger is the sample size required. For example, with a sample size of 100 subjects (most efficiently, assuming homoscedasticity, with 50 subjects in each of the groups to be compared21,22), group mean differences as small as 2 mm can be detected with at least 95% confidence and 80% power if the smaller of the variance estimates prevails in the population. If the larger variance estimates prove more accurate, 100 subjects suffice if group mean differences of at least 5 mm are of interest.
Table 4.
Sample-Size Estimates for Comparing 5-Minute Wetted Lengths Between Two Groups
| Source |
Variance, σ2 |
Minimum Difference of Interest, mm |
||||
| 1 |
2 |
3 |
5 |
10 |
||
| Smallest σ2 from literature (Lee, 1988)20 | 19.536 | 308 | 78 | 36 | 14 | 4 |
| Smallest σ2, current study (2018) | 22.279 | 350 | 88 | 40 | 14 | 4 |
| Largest σ2 current study (2018) | 94.743 | 1488 | 372 | 166 | 60 | 16 |
| Largest σ2 from literature (Lira, 2011)19 | 112.36 | 1764 | 442 | 196 | 72 | 18 |
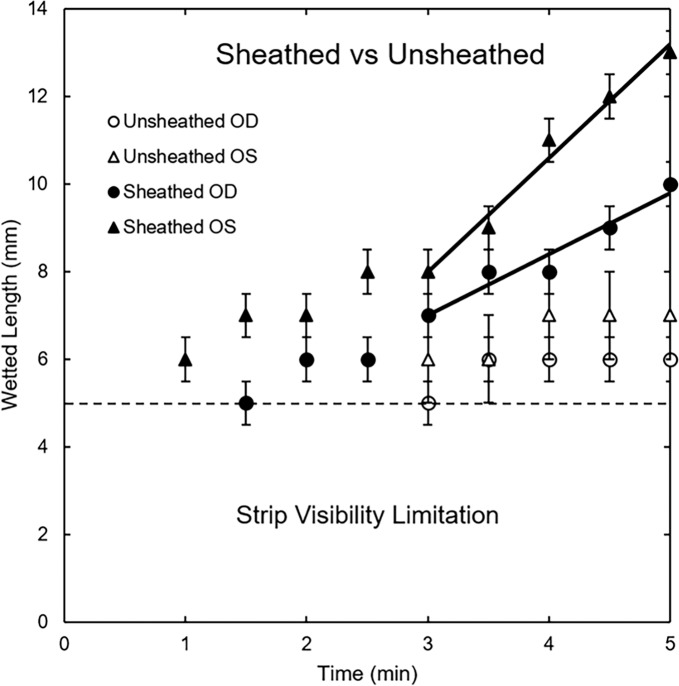
Figure 3 graphs transient wetting lengths as a function of time for one subject with sheathed (closed symbols) and unsheathed (open symbols) strips. Here again, sheathed data evidence longer wetting lengths because evaporation is precluded. Sheathed Schirmer-strip wetted lengths continued to increase linearly for both eyes, allowing calculation of BTPRs; that is, slopes of the solid straight lines drawn for the last 2 minutes of the sheathed STTs give BTPRs from Equation 1.4 Conversely, the unsheathed wetted lengths flattened in time and did not sensibly increase for the last 90 seconds for either eye. BTPRs cannot be directly assessed when Schirmer strips are exposed to the environment. Wetted lengths also could not be assessed below the dashed horizontal line due to visibility limitations.
Figure 3.
Wetting-length dynamics for right and left eyes of subject 15. Closed symbols reflect sheathing. Open symbols correspond to unsheathed strips. Slopes of the straight lines drawn after 3 minutes give the BTPR. Wetted lengths cannot be assessed below the dashed horizontal line due to visibility limitation. BTPRs are not available for unsheathed strips because of evaporation. Error bars represent the precision of the Schirmer-strip markings.
Due to evaporation loss, flattening of the wetted lengths occurred in 45% of unsheathed strips. Upon excluding data for completely wetted Schirmer strips (one subject, three readings), 20 out of 44 (45%) of unsheathed Schirmer strip readings had no change in wetted length for the final 90 seconds. Interestingly, 8 out of 48 (17%) of sheathed Schirmer-strip readings also showed similar behavior. This result cannot be explained by evaporation as for unsheathed STTs. Moreover, all eight of these sheathed readings had wetted lengths of ≤10 mm at 5 minutes, while only 11 out of 20 unsheathed Schirmer strip readings with no change in wetted length had wetted lengths of ≤10 mm at 5 minutes.
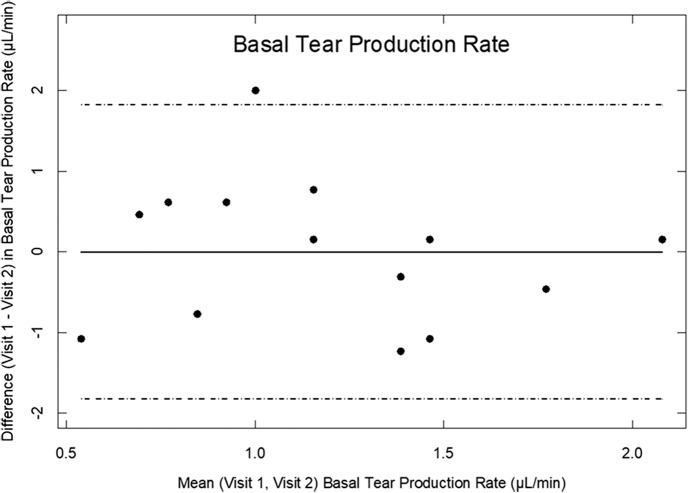
For 22 sheathed readings, wetting lengths did not exceed 5 mm for at least three of the last observed times. Accordingly, BTPRs could not be quantified for these readings, giving a total of 46 quantifiable BTPRs. Of the 32 eyes with measureable BTPRs, 14 eyes had BTPRs available for repeatability analyses. These are graphed in Figure 4. Sheathed BTPRs ranged from 0 to 2.16 μL/min, with a grand mean (SD) of 1.19 (0.61) μL/min. Results stratified on visits were nearly identical (Table 5). The CR for BTPR was 1.91 μL/min, meaning that repeated BTPR measurements on the same subject, under the same conditions, and by the same observer, fall within 1.91 μL/min with 95% probability. Employing the variance estimate corrected for repeated measures,17 the LoA for BTPR were [−1.82, 1.82] μL/min, with a mean difference of <0.001 ≈ 0 μL/min. There was no dependence of the intervisit difference on the magnitude of the tear production rate (Fig. 4). Furthermore, there were no significant relationships between BTPR and external factors, including indoor or outdoor temperature or outdoor humidity, outdoor wind speed, or time awake before measurement. Indoor humidity was around 50% and did not influence BTPR. BTPRs are not available for unsheathed strips because of evaporation loss.
Figure 4.
Subject visit DVM BTPRs for sheathed Schirmer strips. A solid line indicates the mean intervisit difference in BTPR. Dashed lines mark the LoA.
Table 5.
Descriptive Statistics for BTPR (μL/min) From Dynamic Wetted Lengths of Sheathed Schirmer Strips
| BTPR |
Min |
Max |
Median |
Mean |
SD |
| Visit 1 | 0.00 | 2.16 | 1.23 | 1.19 | 0.57 |
| Visit 2 | 0.00 | 2.00 | 1.16 | 1.19 | 0.67 |
Sample-size estimates for a hypothetical two-group comparison of BTPR are shown in Table 6. As with all such estimates, the larger the variance or the smaller the difference one wishes to detect, the larger is the sample size required. In this case, because there is currently no understanding as to what a clinically meaningful difference in BTPR might be, we estimated sample sizes required to detect differences of 5%, 10%, 15%, 20%, and 25% of the maximum BTPR observed (2.156 μL/min, which to our knowledge, is very close to the only published estimate of the maximum BTPR of 2.2 μL/min23,24). Confidence and power were set at 95% and 80%, respectively, and variance estimates from current study data were used. In a hypothetical two-group comparison of BTPR, 100 total subjects sufficed to detect a difference in mean BTPR as small as 10% (i.e., 0.2156 μL/min, see Table 6). Should the variance in the hypothetical two-group study prove to be closer to our largest, unpartitioned total-variance estimate, 100 subjects are sufficient to detect a difference in mean BTPR as small as 15% (i.e., 0.3234 μL/min, see Table 6). The actual BTPR in microliters per minute, or percent change in BTPR, for clinical concern remains to be determined.
Table 6.
Sample-Size Estimates for Comparing BTPR Between Two Groups
| Source |
Variance (σ2) |
Minimum Difference of Interest, μL/min |
||||
| 0.1078 |
0.2156 |
0.3234 |
0.4312 |
0.5390 |
||
| Smaller (V2) between-subject σ2 | 0.0928 | 126 | 32 | 14 | 8 | 6 |
| Larger (V1) between-subject σ2 | 0.1250 | 170 | 44 | 20 | 12 | 8 |
| Total unpartitioned σ2 | 0.3722 | 504 | 126 | 56 | 32 | 22 |
Discussion
For anesthetized eyes, sheathed and unsheathed Schirmer-strip wetted-length methodologies yield similar repeatabilities based on DVM plots, LoA, and the CR. Subject awake time prior to measurement, room temperature, outdoor temperature, outdoor relative humidity, and outdoor wind speed had no significant effect on wetted-length dynamics of the strips. Similar repeatability performance of sheathed and unsheathed strip wetted length suggests little reason to sheath Schirmer strips. However, wetted-length dynamics (Fig. 3) and the method-comparison analysis clearly demonstrate reduction of wetting lengths with unsheathed Schirmer strips due to evaporation. Out of 11 eyes (eight subjects) that had average unsheathed wetted lengths between 5 and 10 mm at 5 minutes, seven eyes (five subjects) had sheathed wetted lengths greater than 10 mm at 5 minutes. In traditional STT, a wetted length between 5 and 10 mm at 5 minutes post insertion is considered equivocal for aqueous-deficient dry eye.25 Therefore, evaporation is a significant factor in traditional STTs for patients with <10-mm wetted length at 5 minutes. Most importantly, sheathing the Schirmer strip allows quantification of tear production rates; BTPR is not necessarily correlated with 5-minute wetted lengths.
The most likely reason for the comparable repeatability of the sheathed-versus-unsheathed methodologies is that the single testing site had nearly constant room temperature and humidity for all subjects and all visits. Unsheathed STT strips, therefore, did not have sufficient variability in evaporative flux to display wider LoA. Buckmaster and Pearce15 found that a relative humidity difference of 60% resulted in a significant difference in 5-minute wetted length but that a difference of 30% did not. Within a constant environment such as a single, climate-controlled examination room, sheathing STT strips, although representative of BTPR, does not improve repeatability. However, for unbiased comparison between different testing sites or between different regions of the world, environmental differences can play an important role. We recommend sheathing Schirmer strips foremost to maintain consistent repeatability by minimizing or eliminating the effects of external factors and to obtain quantitative BTPRs, for example, in microliters per minute.
Eight of 48 sheathed Schirmer-strip readings showed no change in wetted length for the final 90 seconds, indicating a change in the BTPR to 0 μL/min. This observation has not been reported previously and was not observed in the majority of the current study data that shows constant BTPR for each STT.3,4 Li et al.4 showed in vitro that sheathing effectively eliminates the impact of environmental factors, making the abovementioned anomaly difficult to explain unless BTPR diminishes in time during STT for some subjects. It is interesting that seven subjects involved in these eight readings exhibited Schirmer-strip wetted lengths between 5 and 10 mm at 5 minutes post insertion, which is within the range of debate for aqueous-deficient dry eye.25 In the case of unsheathed STTs, approximately half of the measurements showing no change in wetted length for the final 90 seconds produced wetted lengths >10 mm, resulting in a larger wetted surface area and enhanced evaporative loss. For unsheathed STT strips, wetting length that slows to a constant value is attributed to a balance between evaporation and BTPR. Therefore, wetted lengths >10 mm using unsheathed strips do not necessarily indicate normal BTPRs. This provides an explanation for why traditional STT results correlate poorly with other clinical signs and symptoms.26 Further studies are necessary to examine the relationships between aqueous-deficient dry eye and BTPR and with changes in that rate over time, especially for subjects whose STT strips wet within the range of 5 to 10 mm.
There are limitations to our study. Due to the visibility limitation for wetted lengths <5 mm, subjects who had less than 5 mm of wetting at 5 minutes post strip insertion were assigned the median wetted length of the nonobservable region, or 2.5 mm. This approximation led to nearly identical 5-minute wetted lengths, as did assigning 5 or 0 mm for nonobserved wetted lengths (i.e., the largest or smallest they could be, respectively, without being observed). This approximation, however, had no bearing on production rate analysis since BTPR could not be determined for these test outcomes. Additionally, without at least three measurable wetted lengths at 3-, 4-, and 5-minute time points for each trial, the BTPR was not assessable. Although the BTPR is not calculable in these situations, patients exhibiting the abovementioned wetting behavior would be classified as aqueous-deficient dry eye by existing STTs.25 Due to the limitations outlined above, only 14 repeated intrasubject BTPRs were obtained. Additional data are warranted for better population estimates of BTPR and for a fuller assessment of repeatability, taking into account a wider range of testing conditions.
Even after sheathing to minimize or eliminate external environmental effects, sheathed Schirmer-strip 5-minute wetted lengths and BTPRs exhibited relatively poor repeatability. Because the same operator performed the tests in an identical environment, and because theory and in vitro studies validate Schirmer-strip wetting kinetics,3,4 this observation strongly supports the hypothesis that individuals exhibit substantial day-to-day variability in tear production.2 Although the unsheathed STTs from our single testing site under controlled conditions exhibited repeatability similar to the modified STTs, sheathing the strips carries the distinct advantage that BTPR can be directly estimated (from Equation 1 following the procedure of Li et al.4 to eliminate the effects of evaporation and variability in the preexisting lower-lid tear reservoir volume). It is important that modified STT results can be compared without bias across different testing environments.
Acknowledgments
Supported by the Roberta J. Smith Foundation (MCL).
Disclosure: Y.H. Kim, None; A.D. Graham, None; W. Li, None; C.J. Radke, None; M.C. Lin, None
References
- 1.Casser L, Fingeret M, Woodcome T. Atlas of Primary Eyecare Procedures 2nd ed. Maidenhead, UK: McGraw-Hill Education;; 1997. [Google Scholar]
- 2.Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004;23:272–285. doi: 10.1097/00003226-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Telles R, Li W, Dursch TJ, Lin MC, Radke CJ. Human tear-production rate from closed-eye Schirmer-strip capillary dynamics. Colloids Surf A Physicochem Eng Asp. 2017;521:61–68. [Google Scholar]
- 4.Li S, Kim YH, Li W, Lin MC, Radke CJ. Human lacrimal production rates from modified Schirmer-tear test. Optom Vis Sci. 2018;95:343–348. doi: 10.1097/OPX.0000000000001196. [DOI] [PubMed] [Google Scholar]
- 5.Holly FJ, Lamberts DW, Esquivel ED, et al. Kinetics of capillary tear flow in the Schirmer strip. Curr Eye Res. 1982;2:57–70. doi: 10.3109/02713688208998380. [DOI] [PubMed] [Google Scholar]
- 6.Holly FJ. Lacrimation kinetics as determined by a Schirmer-type technique. In: Sullivan DA, editor. In Lacrimal Gland, Tear Film, and Dry Eye Syndromes. New York, NY: Plenum Press;; 1994. pp. 543–548. [DOI] [PubMed] [Google Scholar]
- 7.Beebe WE, Esquivel ED, Holly FJ. Comparison of lacrimation kinetics in dry eye patients and normal. Curr Eye Res. 1988;7:419–425. doi: 10.3109/02713688809031792. [DOI] [PubMed] [Google Scholar]
- 8.Holly FJ, Laukaitis SJ, Esquivel ED. Kinetics of lacrimal secretion in normal human subjects. Curr Eye Res. 1984;3:897–910. doi: 10.3109/02713688409167207. [DOI] [PubMed] [Google Scholar]
- 9.Li N, Deng X-G, He M-F. Comparison of the Schirmer I test with and without topical anesthesia for diagnosing dry eye. Int J Ophthalmol. 2012;5:478–481. doi: 10.3980/j.issn.2222-3959.2012.04.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakamoto R, Bennett ES, Henry VA, et al. The phenol red thread tear test: a cross-cultural study. Invest Ophthalmol Vis Sci. 1993;34:3510–3514. [PubMed] [Google Scholar]
- 11.Kuriki R, Hata T, Nakayama K, et al. Changes in tear volume and ocular symptoms of patients receiving oral anticancer drug S-1. J Pharm Health Care Sci. 2018;4:3. doi: 10.1186/s40780-018-0100-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kojima T, Ibrahim OMA, Wakamatsu T, et al. The impact of contact lens wear and visual display terminal work on ocular surface and tear functions in office workers. Am J Ophthalmol. 2011;152:933–940.e2. doi: 10.1016/j.ajo.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 13.Srinivasan S, Chan C, Jones L. Apparent time-dependent differences in inferior tear meniscus height in human subjects with mild dry eye symptoms. Clin Exp Optom. 2007;90:345–350. doi: 10.1111/j.1444-0938.2007.00174.x. [DOI] [PubMed] [Google Scholar]
- 14.Yokoi N, Bron AJ, Tiffany JM, Maruyama K, Komuro A, Kinoshita S. Relationship between tear volume and tear meniscus curvature. Arch Ophthalmol. 2004;122:1265–1269. doi: 10.1001/archopht.122.9.1265. [DOI] [PubMed] [Google Scholar]
- 15.Buckmaster F, Pearce EI. Effects of humidity on tests of tear production. Clin Sci. 2016;35:754–758. doi: 10.1097/ICO.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 16.Terry RL, Schnider CM, Holden BA, et al. CCLRU standards for success of daily and extended wear contact lenses. Optom Vis Sci. 1993;70:234–243. doi: 10.1097/00006324-199303000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–582. doi: 10.1080/10543400701329422. [DOI] [PubMed] [Google Scholar]
- 18.Vaz S, Falkmer T, Passmore AE, Parsons R, Andreou P. The case for using the repeatability coefficient when calculating test-retest reliability. PLoS One. 2013;8:e73990. doi: 10.1371/journal.pone.0073990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lira M, Oliveira ME, Franco S. Comparison of the tear film clinical parameters at two different times of the day. Clin Exp Optom. 2011;94:557–562. doi: 10.1111/j.1444-0938.2011.00647.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee JH, Hyun PM. The reproducibility of the Schirmer test. Kor J Ophthalmol. 1988;2:5–8. doi: 10.3341/kjo.1988.2.1.5. [DOI] [PubMed] [Google Scholar]
- 21.Atkinson AC, Donev AN. Optimum Experimental Designs. Oxford, UK: Oxford Science Publications;; 1992. [Google Scholar]
- 22.Wong WK, Zhu W. Optimum treatment allocation rules under a variance heterogeneity model. Stat Med. 2008;27:1–20. doi: 10.1002/sim.3318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishima S, Gasset A, Klyce SD, Baum JL. Determination of tear volume and tear flow. Invest Ophthalmol Vis Sci. 1966;5:264–276. [PubMed] [Google Scholar]
- 24.Prabha JL. Tear secretion–a short review. J Pharm Sci Res. 2014;6:155–157. [Google Scholar]
- 25.The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Workshop (2007) Ocul Surf. 2007;5:75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 26.Feldman F, Wood M. Evaluation of the Schirmer tear test. Can J Ophthalmol. 1979;14:257–259. [PubMed] [Google Scholar]