Abstract
Purpose
To evaluate the efficacy of the functional, keratometric, and refractive postoperative parameters of intracorneal ring segment (ICRS) implantation in keratoconus and its association with collagen cross-linking (CXL), photorefractive keratectomy (PRK), and intraocular lenses (IOLs).
Methods
We conducted a systematic review and meta-analysis on case series published between 2007 and 2017.
Results
We included 95 case series with a total of 4560 patients. We included 64 studies of the ICRS procedure, 20 studies of ICRS+CXL, 9 studies of ICRS+CXL+PRK, and 5 studies of ICRS+IOL. We demonstrated an overall improvement of all parameters in all procedures. Cylinder was decreased with an overall effect size (ES) of −1.15 (−1.36 to −0.95; I2 = 93.7%). Corrected distance visual acuity was improved with an overall ES of 0.89 (0.78 to 1.00; I2 = 81.9%). Maximal keratometry was decreased with an overall ES of 0.98 (0.85 to 1.11; I2 = 78.9%). ICRS+IOL is the best procedure to improve spherical equivalent and uncorrected distance visual acuity (P < 0.05) compared with other procedures. ICRSs versus ICRS+CXL are similar in all parameters except for corrected distance visual acuity. ICRS+CXL+PRK is better than ICRS alone in all parameters except for the correction of spherical equivalent.
Conclusions
Although the quality and strength of the data are questionable, ICRS implantation is an effective strategy to preserve visual function in keratoconic patients. Particularly, ICRS+CXL+PRK could be a low invasive procedure to propose to young keratoconic patients.
Translational Relevance
To propose an overview of postoperative parameters on each ICRS procedure on keratoconus.
Keywords: keratoconus, intracorneal ring, collagen cross liking, intraocular lens, refractive photokeratectomy
Introduction
Keratoconus is a common, asymmetric, and usually bilateral ectatic disease of the cornea characterized by a progressive corneal protrusion, which leads to decreased visual acuity and optical quality.1 The prevalence in the general population is 54 per 100,000,2 ranging from 373 to more than 250 in at-risk population.4,5 Keratoconus often appears during puberty and progresses until the fourth decade of life.2 Several therapeutic choices are available, such as contact lens, corneal collagen cross-linking (CXL), intracorneal ring segment (ICRS) implantation, photorefractive keratectomy (PRK), intraocular lenses (IOLs), and lamellar or penetrating keratoplasty.6,7 Therapeutics may be used on their own or combined in order to improve visual rehabilitation or decrease the progression of ectasia.8 In the past, keratoplasty was the only treatment improving visual acuity if patients were contact lens intolerant.9 However, they induce a lot of complications, such as rejection or endophtalmitis.10 In order to delay keratoplasty, the use of intracorneal rings was proposed in 2000s.11 ICRSs are medical devices made of synthetic material implanted within the corneal stroma, which induce a change in cone geometry.12 They were originally designed to correct mild to moderate myopia.13 ICRS implantation is a reversible, simple surgery and is accepted as a good surgical option for the treatment of keratoconus.14 The use of these implants aims to minimize the spherocylindrical error by modifying the central corneal curvature and inducing a reduction of corneal higher-order aberrations by generating a regularization of the corneal surface.15 However, the lack of guidelines in therapeutic choices and the poor predictability of visual, keratometric, and refractive results are challenges facing ophthalmologists treating keratoconus eyes with ICRS.16
Thus, we aimed to conduct a systematic review and meta-analysis to summarize all studies reporting case series concerning just ICRS implantations or with additional therapeutics in order to find the best procedure for visual rehabilitation and/or stability of the cone. So, we evaluated the change in the six main specific parameters for each procedure.
Methods
Literature Search
We reviewed all case-series studies measuring the efficacy and stability of keratometric, refractive, and functional results of ICRS implantation in keratoconus. ICRS could be realized alone (ICRS) or in association with other procedures such as CXL (ICRS+CXL), CXL and PRK (ICRS+CXL+PRK), and IOL (ICRS+IOL). The PubMed, Cochrane Library, Science Direct, and Embase databases were searched on June 2018 with the following keywords: “intracorneal ring” OR segment OR intacs OR “intrastromal corneal ring” AND keratoconus. The search was limited to the last 10 years, from 2007 to 2017. Articles needed to be written in French or English. No minimal sample size was applied. To be included, articles needed to be case-series studies describing our primary outcome variable, which was the measurement of refractive and/or keratometric and/or functional and/or abberometric parameters. We imposed no limitation on the regional origin or the nature of the control group. Studies needed to be primary research and data had to be useable. In addition, reference lists of all publications that met the inclusion criteria were manually searched to identify any further studies that were not found with the electronic search. The search strategy is presented in Figure 1. One author (CBA) conducted all literature searches and collated the abstracts. Two authors (CBA, FD) separately reviewed the abstracts and, based on the selection criteria, decided the suitability of the articles for inclusion. A third author (BP) was asked to review the articles where consensus on suitability was debated. All authors then reviewed the eligible articles.
Figure 1.
Search strategy.
Quality of Assessment
Although not designed for quantifying the integrity of studies,17 Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria were used to check the quality of the reporting.18 The STROBE Statement consists of a checklist of 22 items, which relate to the title, abstract, introduction, methods, results, and discussion sections of articles. Eighteen items are common to cohort studies, case control studies, and cross-sectional studies, and four are specific to each of the three study designs. Among the 22 items, six are split into several subitems. One point was attributed per item or subitem when the study fulfilled the criteria. The maximum score achievable was 33, which was then converted into a percentage.
Statistical Considerations
Statistical analysis was conducted using Stata software (version 13, StataCorp, College Station, TX).19–22 Baseline characteristics were summarized for each study sample and reported as a mean (standard deviation) and number (%) for continuous and categorical variables, respectively. Heterogeneity in the study results was evaluated by examining forest plots, confidence intervals (CIs), and using formal tests for homogeneity based on the I2 statistic, which is the most common metric for measuring the magnitude of between-study heterogeneity and is easily interpretable. I2 values range between 0% and 100% and are typically considered low for <25%, modest for 25% to 50%, and high for >50%.23 For example, a significant heterogeneity may be due to the variability between the characteristics of the studies, such as those of the participants (age, sex, etc.), the grade of keratoconus, the date of evaluation of parameters following ICRS implantation, and evaluation of parameters. Random effects meta-analyses (DerSimonian and Laird approach) were conducted when data could be pooled.24 P values less than 0.05 were considered statistically significant.
We conducted meta-analysis on variations of six main specific parameters in each procedure. We stratified these meta-analyses by procedure. We described our results by calculating the effect size (ES; standardized mean differences [SMDs]) of the six parameters for each dependent procedure.24 When visual acuity was evaluated with the Snellen or decimal scale, we converted visual acuity into LogMar with the formula: LogMar visual acuity = −Log10 (decimal visual acuity). An ES is defined as a unitless measurement of the effect of ICRS surgery and additional procedures, centered at zero if the procedures did not change parameters before and after surgery. A positive ES denoted improved efficacy. A scale for ES has been suggested with 0.8 reflecting a large effect, 0.5 a moderate effect, and 0.2 a small effect.25
For rigor, funnel plots of these meta-analyses were used to search for potential publication bias. In order to verify the strength of the results, further meta-analyses were then conducted, excluding studies that were not evenly distributed around the base of the funnel.
When possible (sufficient sample size), meta-regressions were proposed to study the relationship between variations of parameters and clinically relevant parameters, such as the grade of keratoconus and when CXL was performed. Results were expressed as regression coefficients and 95% CI.
Results
An initial search produced a possible 2326 articles (Fig. 1). Removal of duplicates and use of the selection criteria reduced the number of articles reporting the evaluation of ICRS in keratoconus to 95 articles.8,14–16,26–116 All articles except three were written in English.30,87,94
Quality of Articles
The assessment of the quality of the 95 studies that were included was performed using the STROBE criteria, with the results varying from 43.8%31 to 93.8%,41,66–68,70,103 with a mean score of 79.7 ± 8.8. Overall, the studies performed best in the methods section and worst in the discussion section. All studies except five mentioned ethical approval.58,83,86,106,115
Method of ICRS Implantation
Topical anesthesia was used for all procedures. Surgery was performed by one (references 14–16, 27–37, 39–46, 48, 50–53, 55–57, 59, 60, 62, 63, 65, 66, 70–78, 81–84, 86, 88–94, 98–102, 104–110, 112–116), two (references 8, 26, 38, 47, 49, 58, 61, 67–69, 79, 80, 85, 87, 95, 96, 111), or more54,64,97,103 surgeons using a manual (references 8, 31, 35, 36, 43, 44, 48, 49, 55, 61, 65, 71, 72, 75–78, 81, 83–85, 91, 94, 95, 101, 102, 104, 108, 111, 113, 114) or femtosecond laser-assisted technique (references 14–16, 26–30, 32–34, 37–42, 45–47, 50–54, 56–60, 62–64, 66–70, 72–74, 79, 80, 82, 86–90, 92, 93, 96–100, 103, 105–110, 112, 115, 116) for the creation of the intrastromal pocket. The reference point was a Sinskey hook marking the center of the pupil. Channel depth varied between 70% (references 14–16, 33, 35, 37, 48-54, 63, 65, 66, 70, 80, 82, 83, 87, 88, 90, 92, 95, 98, 99, 102, 103, 105, 108, 109, 111, 113, 114), 75% (references 26, 27, 34, 39, 41, 42, 45, 58, 60, 64, 71, 79, 110), or 80% (references 8, 29, 30, 32, 33, 43, 47, 54–56, 59, 62, 67–69, 72–78, 81, 84, 85, 93, 94, 97, 103, 107, 112) of the thickness at the ring site, which was measured by ultrasonic pachymetry. The degree of the channel was determined using nomograms of specific ICRS used or was a 360-degree15,16,26,32,34,36,39,96 tunnel for inserting the segments. Five ICRS were used: Keraring (Mediphacos, Belo Horizonte, Brazil) (references 8, 16, 27, 28, 31, 32, 36, 41, 42, 47, 54, 55, 58–61, 64, 66, 67, 69, 70, 77, 80, 88, 92, 93, 97–99, 102, 103, 107, 110, 112, 116), Ferrara ring (Ferrara Ophthalmics, Belo Horizonte, Brazil) (references 14, 30, 35, 43, 62, 63, 76, 78, 81, 82, 84, 85, 89, 91, 94, 101, 104), Intacs (Addition Technology, Inc., Des Plaines, IL) (references 16, 26, 33, 37, 39, 40, 45, 46, 48, 49, 52, 53, 56, 58, 65, 71–75, 79, 83, 87, 89, 90, 95, 96, 99, 102, 103, 105, 106, 108, 109, 111, 113–115), CornealRing (Visiontech Medical Optics, Belo Horizonte, Brazil),38,72 and Myoring ICR (Dioptex, GmbH, Linz, Austria).15,32,34,44,57,86,100 The thickness and arc length of segments were also defined by nomograms and topography when several rings could be used, except in two studies evaluating a specific ICRS.36,95 The steepest corneal topographic axis was selected as the incision point in all studies except nine (references 15, 26, 46, 83, 84, 109, 111, 113, 114). Optical zone diameter varied between 5 and 7 mm and was not specified in 36 studies (references 16, 29, 32, 33, 36, 39, 42, 45, 48, 50–52, 54, 58, 62, 64, 65, 72, 75, 85, 86, 89–91, 95, 96, 100, 101, 103, 104, 106, 111, 113–115). When the optical zone was 5 mm (references 15, 27, 30, 31, 34, 35, 43, 44, 53, 57, 59–61, 67–70, 77, 78, 80, 81, 84, 88, 92–94, 103, 107, 110), the inner diameter varied from 4.435,59,60,88,107,110 to 5.4 mm,77 and the outer diameter varied from 5.623,48,49,77,96,99 to 7.0 mm.77 When the optical zone was 6 mm,14,63,71,82,87 the inner diameter varied from 6.014,63,82 to 6.6 mm,87 and the outer diameter varied from 7.08 to 7.5 mm.87 Finally, when the optical zone was 7 mm,83,102,108,109 the inner diameter was 7 mm and the outer diameter was 8.2 mm. One or two rings were inserted depending on the keratoconus grade in 44 studies (references 8, 14, 26–30, 32, 41, 49–51, 53–55, 59–61, 67, 68, 75–77, 80, 82, 84, 85, 87–89, 92–94, 96, 97, 102, 103, 107, 109, 110, 112, 116). In 20 studies, only one ring was systematically set up (references 15, 34–37, 39, 40, 43, 44, 46, 48, 52, 56, 57, 63, 66, 70, 71, 78, 95). In 10 studies, two rings were systematically inserted (references 65, 72, 74, 79, 83, 105, 108, 111, 113, 114). The number of rings inserted was not specified in 21 studies (references 16, 31, 33, 38, 42, 45, 47, 58, 62, 64, 69, 73, 81, 86, 90, 91, 98–101, 104, 106, 115). At the end of the procedure, the incision was sutured using 10-0 nylon (references 26, 37, 46, 48–50, 55, 56, 65, 71, 73, 75, 79, 83, 84, 87, 89, 95, 96, 102, 108, 111, 113). In other studies, the incision was not sutured. Postoperative treatments were antibiotics (quinolone [references 8, 26, 28, 29, 32, 34, 37, 39, 40, 46, 50, 52, 53, 56, 66, 67, 70, 71, 73, 78–80, 84, 85, 88, 89, 91, 96, 98, 99, 101, 104, 111, 116], aminoglycoside [references 14, 15, 30, 31, 35, 41, 43, 50, 51, 55, 59, 60, 63, 64, 68, 69, 74–77, 82, 87, 93, 97, 103, 109, 112], or chloramphenicol [references 35, 36, 42, 62, 65, 72, 81, 83, 88, 92, 102, 107, 108, 110, 113, 114]), steroids (references 14, 15, 26, 28–32, 34–37, 39–43, 46, 48, 50–53, 55–57, 59, 60, 62–85, 87–91, 93, 96–99, 101–104, 107–116), nonsteroid anti-inflammatory,8,28,41,46,85,101,104 and/or artificial tears (references 8, 26, 28, 29, 32, 36, 42, 46, 55, 57, 59, 60, 62, 64, 67, 69–71, 73, 82, 89, 97, 101, 103, 104, 107, 109). Treatments were administrated from 534,37,46,64 to 4536 days after the procedure.
Selection of Patients for ICRS Implantation
Inclusion Criteria
Patients were classified according to the Amsler-Krumeich classification.117 All grades of keratoconus were included in 33 studies (references 15, 16, 30, 33, 41, 43, 45, 49–51, 54, 68, 69, 72, 77, 78, 80, 83, 88, 94, 97–100, 102–106, 111, 112, 115), all grades except grade IV in 22 studies (references 28, 29, 32, 34, 37, 42, 44, 52, 53, 55, 60–62, 76, 82, 87, 90, 92, 93, 101, 107, 110, 114), or all except grade I in eight studies (references 26, 27, 31, 35, 39, 79, 91, 109). Only grade I and II were included in six studies,14,36,47,63,64,82,85 II and III in 11 studies (references 8, 40, 46, 51, 56, 58, 67, 71, 81, 89, 96), III and IV in three studies,70,75,108 and 12 studies did not specify the grade of keratoconus (references 38, 48, 57, 59, 65, 66, 73, 74, 84, 86, 95, 113, 116). Inclusion criteria for ICRS implantation were contact lens intolerance (references 8, 14, 15, 26, 28–33, 35–39, 41–43, 48–51, 55–60, 62–64, 66, 67, 71–82, 84–91, 93, 94, 98, 99, 101–103, 105–108, 110, 111, 114), age of patients (references 26, 34, 36, 37, 45, 84, 107, 108), unsatisfied visual acuity with spectacles (references 15, 28, 29, 31, 32, 37, 38, 41, 44, 52, 53, 59, 61, 67, 73, 76–78, 80, 87, 94, 98, 100, 103, 111), no opacities or scar on central cornea (references 8, 14–16, 26–28, 30–32, 35, 36, 38, 39, 41–46, 48–53, 55–63, 66, 67, 69–71, 73–78, 80, 81, 84–88, 91, 93–95, 98–102, 105–107, 110, 111, 114, 116), and stability of the cone.30,33 Central or thinnest corneal thickness had to be over 330,61,75 350 (references 15, 36, 44, 57, 62, 86, 87, 100, 110, 111), 380,38,116 400 (references 8, 32, 37, 41, 50, 51, 67, 73, 80), or 450 μm.31,76,93 At the ring site insertion, thickness had to be over 300,43,78 400 (references 14, 29, 30, 34, 38, 39, 42, 46, 49, 55–57, 59–61, 63, 66, 70, 71, 74, 75, 82, 84, 91, 94, 96, 105, 107), or 450 μm (references 26–28, 35, 45, 48, 58, 79, 106, 108, 110, 111). When all grades of keratoconus were included, maximal keratometry had to be under 60 (references 8, 26, 27, 37, 43, 49, 93, 106), 63,30,78,101 65 (references 32, 60, 61, 66, 70, 80, 87, 98), 70,31,91 or 75 diopters (D).94
Exclusion Criteria
The main criteria were related to concomitant or a history of specific ocular disease such as dry eye disease (references 32, 36, 42, 49, 56, 67, 73, 80, 85), local infection (herpes) (references 14, 27–29, 31, 32, 41–45, 48, 50, 51, 55, 58, 59, 62, 63, 66, 67, 73, 80–82, 94, 102, 107, 108, 110), retinal disease (macular degeneration, retinal detachment) (references 14, 29, 38, 49, 55, 58, 63, 82), glaucoma,14,29,38,49,58,63,82 ocular inflammation,14,28,29,49,63,82 hydrops (references 28, 30, 43, 62, 70, 78, 80, 91, 94, 101, 107), neuro-ophthalmic disease,14,29 eyelid margin disease,49 affection of anterior segment (cataract, corneal dystrophy) (references 8, 32, 58, 59, 63, 81, 82, 93, 94, 107, 110), or nonspecific ocular disease (references 15, 30, 34, 36, 44, 54, 60, 66–69, 80, 85, 95, 103, 116). Previous corneal surgeries were excluded (references 14, 16, 26, 27, 29, 32, 33, 36–38, 44, 45, 48, 50, 51, 54, 56, 63, 67–69, 80, 82, 91, 97, 102, 108). Patients with concomitant specific systemic disease such as diabetes,38,55 autoimmune disease (references 8, 14, 16, 29, 41, 42, 50, 51, 55, 58, 59, 62, 63, 66, 67, 73, 82, 93, 102), systemic connective tissue disease (references 8, 14, 16, 26, 27, 29, 44, 45, 48, 50, 51, 59, 62, 63, 66, 82, 93, 108, 110), atopy (references 8, 58–60, 66, 70, 78, 93, 101, 107), or nonspecific systemic disease were excluded (references 32, 36, 42, 60, 78, 85, 93, 101). Less frequently, other criteria were cited, such as pregnancy or breastfeeding (references 8, 32, 36, 41, 44, 62, 73, 78, 80, 93, 107), failed follow-up,8,38,56,65,77,81,83,84 endothelial cell count under 2000 cells/mm2 (references 14, 29, 50, 51, 59, 63, 73, 110), hyperopia or emmetropia spherical equivalent,32,38,44 or only one functional eye.67
Method of CXL
Thirty case series used CXL (references 8, 28, 29, 32, 35, 38, 40–42, 44, 45, 50–53, 58–60, 62, 64, 67, 73, 74, 76, 85, 90, 93, 105, 107, 115, 116). Twenty were associated with ICRS insertion (references 8, 28, 29, 35, 38, 44, 45, 53, 58, 62, 67, 74, 76, 85, 93, 105, 107, 115, 116), nine were combined with ICRS insertion and PRK (references 40–42, 50, 52, 60, 64, 73, 90), and two combined CXL with ICRS insertion and phakic IOL (pIOL).51,59 CXL was realized before,67,76,107 simultaneously (references 28, 29, 40, 44, 45, 51–53, 58, 74, 85, 115), or after ICRS insertion.
Most studies (references 35, 38, 40–42, 45, 50–53, 58–60, 62, 64, 67, 73, 74, 76, 85, 90, 93, 95, 107, 116) used the Dresden protocol.118 After topical anesthesia and pilocarpine, 7 to 9 mm of the central corneal epithelium was removed mechanically, with alcohol, or with excimer laser. A mixed 0.1% riboflavin and 20% dextran was instilled every 3 minutes over a 30-minute period until the riboflavin penetrated the cornea. An ultraviolet lamp (370 nm wavelength) was then focused (3 mW/cm2 irradiance) on the apex of the cornea for a total of 30 minutes. During the period of irradiance, the riboflavin solution was applied every 2 to 5 minutes to saturate the cornea.
Variants of the Dresden protocol were used in nine studies (references 8, 28, 29, 40, 44, 74, 105, 115, 116). Two used an accelerated protocol with only 5 minutes of exposure at a higher ultraviolet irradiance (18 mW/cm2).28,29 Three did not remove the epithelium.8,105,115 Among those three studies, one study instilled riboflavin over 12 minutes and then used ultraviolet irradiation for 12 minutes.8 Three studies injected riboflavin into the corneal pocket with 30 minutes of ultraviolet irradiation,44,74,116 and one used topical mixed riboflavin and dextran four times a day for 1 month.67
At the end of the procedure, a soft contact lens was applied. Postoperative treatments were composed of antibiotics (quinolone50,51,76,85,90,93,116 or tobramycin8,35,41,50,51), steroids (references 8, 35, 41, 50, 51, 85, 90, 107, 116), and nonsteroid anti-inflammatories.41,51,76,85,93 Treatments were administrated for 10 to 30 days after the procedure (references 8, 41, 50, 51, 76, 85, 90, 93, 107).
Inclusion Criteria for CXL
Progressive keratoconus was required for the cross-linking procedure to be proposed. The evolution of keratoconus was defined as an increase of at least 1.0 D in steepest keratometry (references 35, 40–42, 50, 52, 59, 60, 62, 64, 76, 85, 93, 107, 116) or cylinder35,41,42,62,64,85 or at least 0.5 D in spherical equivalent over the previous 6 months35,41,42,50,64,85,116 or a decrease in visual acuity of at least one line,40,52 more than one change in the prescription for glasses or contact lenses over the past 2 years.52,76
Method of PRK
Nine case series used PRK (references 40–42, 50, 52, 60, 64, 73, 90). All PRK were associated with CXL. Five studies used topography-guided PRK41,42,60,64,73 and four were not topography-guided procedures.40,50,52,90 PRK could be performed simultaneously with ICRS in a same-day procedure40,52 or after ICRS insertion in a two- or three-step procedure.41,42,50,60,64,73,90 When it was a same-day procedure, the intervention started with PRK followed by ICRS insertion and CXL.40,52 In the two-step procedure, PRK and CXL were realized the same day (second step) after ICRS insertion (first step).41,42,60,64,73,90 One study had a three-step procedure with ICRS then PRK followed by CXL on three different days.50 Three excimer lasers were used to perform the PRK: Allegretto 400-Hz (Wavelight Laser Technology AG, Erlangen, Germany),50,60 Visx Star S4 IR laser platform (Abbott Medical Optics, Inc.)40,52,73,90 and Schwind Amaris laser platform (Schwind eye-tech-solution, GmbH, Kleinostheim, Germany).41,42,64 The PRK ablation was performed after removing corneal epithelium. A 650,60,64,90 or 6.5 mm40–42,73 optical zone and a transition zone of less than 1.5 mm was performed with a maximum ablation depth of 50 μm for all procedures. Only two studies used mitomycin.41,42 Antibiotics42 (tobramycin,41,60,64 moxifloxacin,40,52,73,90 or gatifloxacin50), dexamethasone (references 40–42, 50, 52, 60, 64, 73, 90), and diclofenac41,60,64 and contact lenses (references 40–42, 50, 52, 60, 64, 73, 90) were used after the procedure. Treatments were administrated for 1050 to 4550 days after the procedure.
Method of IOL Implantation
Five studies associated IOL and ICRS in a two-step procedure (ICRS then IOL),51,72,113 a three-step procedure (ICRS then CXL then IOL),59 or a one-step procedure (same day ICRS and IOL).49 Delay between ICRS and IOL implantation were at least 6 months in sequential procedures.51,59,72,113 All IOL procedures were performed under general anesthesia.
Two studies used iris-claw pIOL.49,113 For pIOL implantation, patients received eye drops to induce miosis. A 6.5-mm superior clear corneal incision was made, and two side ports were created. The pIOL was then introduced into the anterior chamber and placed in the horizontal lens position. Enclavation of the iris was performed on the nasal and temporal sides. A peripheral iridectomy was made.
Three studies used implantable collamer lenses (ICLs).51,59,72 Iridotomies were performed 1 week before the surgery using a Nd:YAG laser. In the operating room, the horizontal corneal axis was marked while the patient was sitting to avoid potential cyclotorsion. The ICL was sized according to corneal white-to-white distance and anterior chamber depth. A temporal incision was created to inject the ICL. After the insertion of the lens, haptics were placed under the iris. Correct positioning and axis of the ICL was verified.
In all procedures, the main corneal incision was sutured using 10–0 nylon. Antibiotics72,113 (tobramycin)59 and steroids59,72,113 were used after the procedure. This information was not specified in two studies.49,51
Population
Sample Size
A total of 4560 patients were included. Population sizes ranged from 486,90 to 810.78 The number of eyes included ranged from 590 to 1073,78 with a total of 5509 eyes implanted with ICRS.
Gender
The proportion of men varied between 27.565 to 100%.90 Twenty-two studies did not specify the proportion of men (references 8, 14, 16, 46, 47, 53, 58, 64, 67, 69, 70, 74, 77, 85, 86, 88, 93, 94, 101, 104, 113, 114).
Age
The minimal mean age in the included studies was 19.1 ± 10.6 years,16 and the maximal mean age was 45.3 ± 10.6 years.90
Procedure Characterization
ICRS implantation was the only procedure in 3790 eyes of 3139 patients. CXL was associated with ICRS for 1082 eyes of 794 patients. PRK and CXL was performed in 206 eyes of 173 patients. IOL was realized in 65 eyes of 48 patients.
Outcome and Aim of the Studies
The principal aim of the studies included was to evaluate the efficacy and safety of ICRS insertion in keratoconus (references 14–16, 26, 27, 30, 31, 33, 34, 36, 37, 39, 43, 45–48, 54–58, 61, 63, 65, 68–71, 75, 77–84, 86–89, 91, 92, 94, 96, 97, 100–102, 104, 106, 108–112, 114), or the efficacy and safety of ICRS insertion combined with CXL (references 8, 28, 29, 44, 74, 76, 85, 105, 115, 116) or PRK40–42,50,52,60,73,90 or IOL.49,51,59,72,113 Other principal aims were the comparison between ICRS alone or combined with CXL,38,62 the comparison of two types of ICRS,32,95,99 two sequences of the CXL procedure,35,67,93,107 or comparing the outcomes of mechanical versus femtosecond laser-assisted tunnel creation for ICRS in eyes with keratoconus.66,98,103
Study Designs
Eighty-eight studies were single-site (references 8, 14–16, 26–46, 48–53, 55–67, 70–96, 98, 99, 101, 102, 104–116) and seven were multisite.47,54,68,69,97,100,103 The majority of studies came from Europe (41 studies) (references 14, 15, 30, 33, 35, 44, 47, 49, 54, 55, 59–63, 65, 66, 68, 69, 74, 75, 82, 83, 85, 87–89, 92, 94, 97–99, 103, 105–107, 109, 110, 112, 114, 116), followed by the Middle East (30) (references 16, 26, 32, 34, 37, 39, 41, 42, 45, 48, 50, 51, 56–58, 64, 70, 71, 73, 77, 79, 81, 84, 86, 91, 100, 102, 108, 111), South America (13) (references 29, 31, 38, 43, 46, 67, 72, 76, 80, 95, 101, 104), North America (6),40,52,53,90,96,115 and Africa (5).8,27,28,93,113
Parameters and Analysis Conditions
Visual acuity was reported by the Snellen scale (references 14, 45, 54, 59, 62, 78, 79, 82, 86, 99, 103–105, 110), decimal scale (references 27, 30, 33, 48, 58, 73, 74, 77, 81, 93, 94, 101, 102, 108, 112–114), or LogMar (references 8, 15, 16, 26, 28, 29, 31, 32, 34–39, 41–44, 46, 47, 49–53, 55–57, 60, 61, 63–72, 75, 76, 80, 83–85, 87–91, 95–98, 100, 105, 107, 111, 115, 116). Uncorrected distance visual acuity (UDVA) and corrected DVA (CDVA) were evaluated in nearly all studies. Unfortunately, no studies reported whether corrected visual acuity was measured with spectacle or with contact lens.
Refractive parameters (sphere, cylinder, and spherical equivalent) were reported using examination and autorefractometer.
Topographic parameters (Kmin, Kmax, Kmean, and sim K) were measured with different corneal topography: CSO (Costruzione Oftalmici Strumenti, Firenze, Italy) (references 14, 15, 68, 69, 84, 91, 112, 116), Galilei Dual Scheimpflug Analyser (Ziemer Ophthalmic Systems AG),39,79 Keratron Scout (Optikon 2000 SpA, Rome, Italy),76,95,100 Eyesis corneal topographer (Eyesis Vision, Inc.), OPD-Scan (Nidek, Tokyo, Japan),40,87,96 Orbscan (Bausch & Lomb, Orbtek, Inc.) (references 26, 30, 33, 36, 48–51, 54, 55, 58–60, 62, 63, 65, 67–73, 80, 82, 83, 88, 89, 92, 97–99, 102, 106–108, 110, 111), Pentacam (Allegro Oculyzer, Wavelight AG, Erlangen, Germany) (references 16, 27, 28, 34, 35, 37, 43–45, 48–53, 57, 58, 61, 66, 67, 74, 75, 77, 78, 81, 85, 94, 100, 101, 104, 105, 109), and TMS-3 (Tomey Inc., Nagoya, Japan).35,93,103
The date of evaluation of parameters following ICRS implantation corresponded with the date of the last examination after the procedure. Mean date of the last examination was 12.0 ± 18.6 months, ranging from 365,80,91,97,115 to 120 months.30,43
Meta-Analyses and Meta-Regressions on Refractive, Visual and Keratometric Parameters
Spherical Equivalent
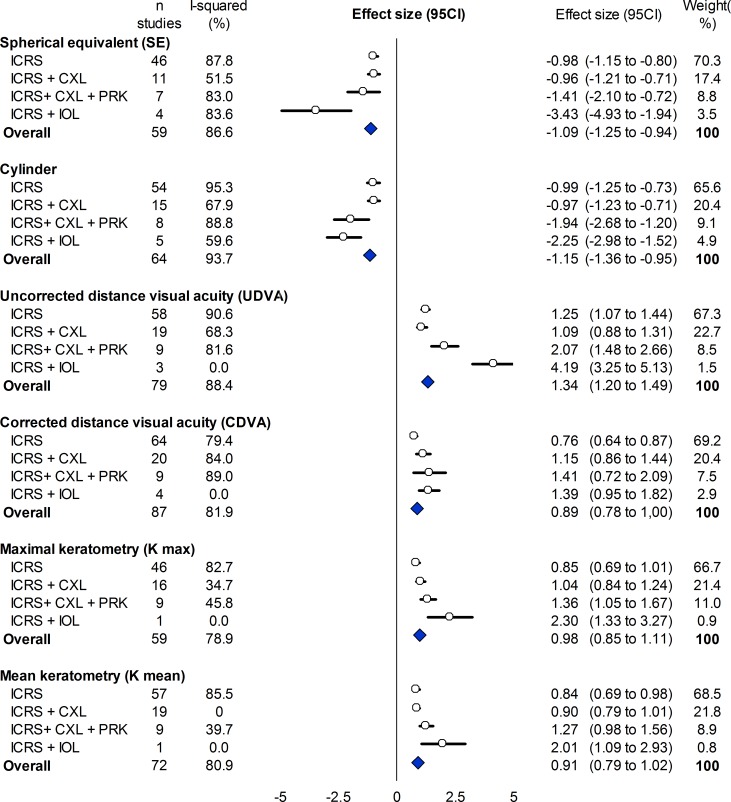
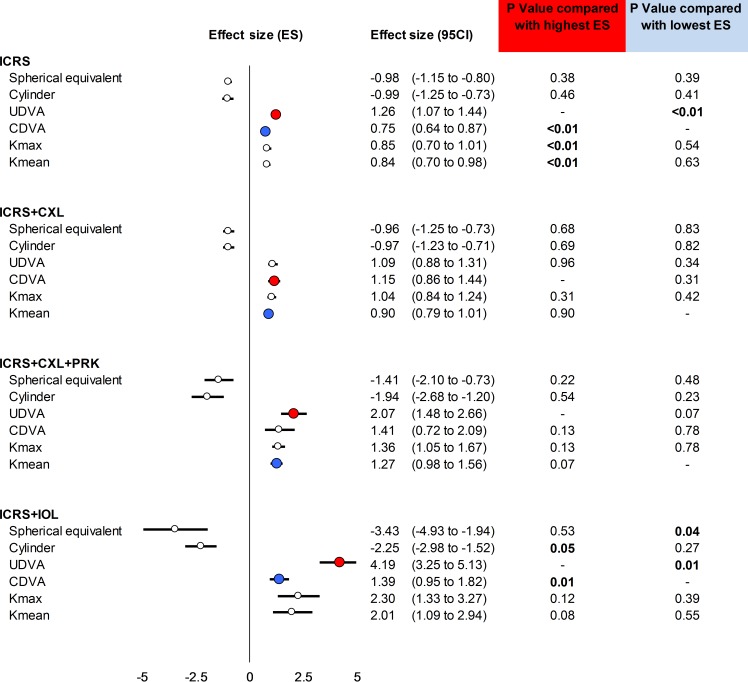
Fifty-nine studies were included (references 14–16, 26, 28, 30, 32, 33, 35–37, 39–41, 45, 46, 48–52, 55, 56, 59–61, 64, 67, 70, 72, 75–77, 79–81, 83–91, 94, 96, 97, 99, 100, 102, 103, 107–112, 114). There was an overall decrease in spherical equivalent with an ES of −1.09 (95% CI, −1.25 to −0.94) as well as a significant decrease for all procedures (ES of −3.43 [−4.93 to −1.94] for ICRS+IOL, −1.41 [−2.10 to −0.72] for ICRS+CXL+PRK, −0.96 [−1.21 to −0.71] for ICRS+CXL, and −0.98 [−1.15 to −0.80] for ICRS) (P < 0.01) (Fig. 2; Supplementary Fig. S1). ICRS+IOL was significantly better than other techniques on spherical equivalent (coefficient of 1.72 [0.24 to 3.20, P < 0.01] versus ICRS+CXL+PRK, 2.12 [0.70 to 3.54, P < 0.01] versus ICRS+CXL, and 2.12 [0.75 to 3.50, P < 0.01] versus ICRS). No significant differences between other techniques were found for spherical equivalent (Fig. 3).
Figure 2.
Meta-analysis of refractive, visual and keratometric parameters in each procedure.
Figure 3.
Meta-regressions concerning the variations of parameters between procedures.
Cylinder
Sixty-four studies were included (references 8, 14, 15, 26, 27, 30, 32, 33, 35, 37, 39, 41, 42, 45–47, 49–53, 56, 57, 59–62, 64, 67–70, 72–77, 79, 81, 84, 86, 88, 89, 91, 93, 94, 96–98, 102–105, 107–116). There was an overall decrease in cylinder with an ES of −1.15 (95% CI, −1.36 to −0.96). As for spherical equivalent, we found a significant decrease in all procedures (P < 0.01) and ICRS+IOL had the highest ES −2.25 (−2.98 to −1.52), followed by ICRS+CXL+PRK −1.94 (−2.68 to −1.20). ICRS and ICRS+CXL were quite similar with −0.99 (−1.25 to −0.73) and −0.97 (−1.23 to −0.71), respectively (Fig. 2; Supplementary Fig. S2).
ICRS+CXL+PRK permitted a significant improvement of cylinder correction compared with other procedures except for the ICRS+IOL procedure (P = 0.02 versus ICRS, and P = 0.05 versus ICRS+CXL). No significant differences for cylinder were found between the other techniques (Fig. 3).
Uncorrected and Corrected Distance Visual Acuity (UDVA and CDVA)
Eighty studies for UDVA (references 8, 14–16, 26–30, 32–37, 39–53, 55–57, 59–68, 70–77, 79, 81, 83–91, 93, 94, 96, 97, 99–105, 107, 109, 111–113, 115, 116) and 88 studies for CDVA were included (references 8, 14–16, 26–53, 55–57, 59–77, 79–91, 93, 94, 96–105, 107–109, 111–113, 115, 116). Both uncorrected and corrected visual acuity was significantly improved in all procedures (P < 0.01). The overall ES was 1.34 (1.20 to 1.49) for UDVA and 0.89 (0.78 to 1.00) for CDVA. ICRS+IOL had the greatest ES for both UDVA and CDVA especially in UDVA 4.19 (3.25 to 5.13). CDVA was greatly increased with the ICRS+CXL+PKR procedure, with an ES of 1.41 (0.72 to 2.09). Respectively, UDVA and CDVA were 1.25 (1.07 to 1.44) and 0.76 (0.64 to 0.87) for ICRS, 1.09 (0.88 to 1.31) and 1.15 (0.86 to 1.44) for ICRS+CXL, 2.07 (1.48 to 2.66) and 1.41 (0.72 to 2.09) for ICRS+CXL+PRK, 4.19 (3.25 to 5.13) and 1.39 (0.95 to 1.82) for ICRS+IOL (Fig. 2; Supplementary Figs. S3, S4). UDVA were significantly improved by ICRS+IOL compared with other procedures (P < 0.05). ICRS+CXL+PRK was also significantly better than other procedures, except ICRS+IOL, for UDVA. ICRS+CXL and ICRS+CXL+PRK were significantly better than ICRS alone for CDVA (P = 0.04 and P = 0.05). There is no significant difference between ICRS+IOL and other procedures for CDVA (Fig. 3).
Maximal and Mean Keratometry (Kmax and Kmean)
Fifty-nine studies for Kmax (references 8, 14–16, 26–28, 30, 32–42, 44, 45, 47, 48, 50–52, 59, 60, 64, 67–70, 73, 75–77, 79–81, 85, 86, 88–90, 93, 94, 96, 97, 99, 101, 103–106, 111, 112, 114, 115) and 72 studies for Kmean were included (references 8, 14–16, 26–28, 30, 32–45, 47, 48, 50–53, 55, 56, 59–62, 64, 66–68, 70, 73–77, 79–81, 83, 85–87, 90, 91, 93, 94, 96, 97, 99, 101–112, 114, 115). They were similarly improved in each procedure with an overall ES of 0.98 (0.85 to 1.11) for Kmax and 0.91 (0.79 to 1.02) for Kmean. Respectively, Kmax and Kmean were 0.85 (0.69 to 1.01) and 0.84 (0.69 to 0.98) for ICRS, 1.04 (0.84 to 1.24) and 0.90 (0.79 to 1.01) for ICRS+CXL, 1.36 (1.05 to 1.67) and 1.27 (0.98 to 1.56) for ICRS+CXL+PRK, 2.30 (1.33 to 3.27) and 2.01 (1.09 to 2.93) for ICRS+IOL (Fig. 2; Supplementary Figs. 5, 6. ICRS+CXL+PRK was significantly better than ICRS alone for Kmax (ratio 0.53 [0.02 to 1.03, P = 0.04]) and Kmean (ratio 0.44 [0.02 to 0.86, P = 0.04]). There was no other significant difference between the procedures for Kmax and Kmean.
Meta-analyses with results expressed in used unity (logMar and diopters) were also computed before and after surgery on each parameter and stratified by each procedure (Table).
Table.
Synthesis of Meta-Analyses With Results Expressed in Used Unity (LogMar and Diopters), Before and After Surgery
| Preoperative |
Last Meet |
|||
| Mean (95% CI) |
Weight % |
Mean (95% CI) |
Weight % |
|
| Spherical Equivalent (Diopters) | ||||
| ICRS | −5.27 (−6.14 to −4.40) | 61.5 | −2.24 (−2.86 to −1.62) | 37.4 |
| ICRS+CXL | −7.29 (−9.01 to −5.58) | 15.9 | −3.18 (−4.60 to −1.76) | 9.8 |
| ICRS+CXL+PKR | −3.12 (−4.66 to −1.59) | 19.8 | −1.00 (−1.84 to −0.15) | 20.5 |
| ICRS+IOL | −12.17 (−16.23 to −8.11) | 2.8 | −0.64 (−1.32 to 0.03) | 32.3 |
| Cylinder (Diopters) | ||||
| ICRS | −4.06 (−4.53 to −3.58) | 44.3 | −2.14 (−2.49 to −1.79) | 46.6 |
| ICRS+CXL | −5.00 (−5.56 to −4.43) | 31.3 | −3.25 (−3.87 to −2.63) | 15.6 |
| ICRS+CXL+PKR | −3.82 (−4.90 to −2.74) | 8.5 | −1.04 (−1.44 to −0.64) | 19.6 |
| ICRS+IOL | −3.18 (−3.97 to −2.38) | 15.9 | −1.43 (−1.87 to −0.99) | 18.3 |
| UDVA (LogMar) | ||||
| ICRS | 0.96 (0.86 to 1.06) | 65.9 | 0.44 (0.38 to 0.50) | 39.4 |
| ICRS+CXL | 0.98 (0.81 to 1.16) | 20.6 | 0.39 (0.30 to 0.48) | 18.2 |
| ICRS+CXL+PKR | 0.97 (0.72 to 1.22) | 10.3 | 0.18 (0.10 to 0.26) | 21.3 |
| ICRS+IOL | 1.43 (0.99 to 1.87) | 3.3 | 0.16 (0.09 to 0.23) | 21.1 |
| CDVA (LogMar) | ||||
| ICRS | 0.28 (0.24 to 0.32) | 68.1 | 0.19 (0.15 to 0.22) | 38.7 |
| ICRS+CXL | 0.46 (0.37 to 0.55) | 13.3 | 0.13 (0.09 to 0.18) | 25.6 |
| ICRS+CXL+PKR | 0.26 (0.12 to 0.40) | 13.4 | 0.07 (0.03 to 0.11) | 28.6 |
| ICRS+IOL | 0.31 (0.17 to 0.45) | 5.2 | 0.15 (0.07 to 0.23) | 7.1 |
| Kmax (Diopters) | ||||
| ICRS | 52.9 (51.6 to 54.1) | 54.7 | 48.7 (47.7 to 49.7) | 49.6 |
| ICRS+CXL | 53.1 (51.4 to 54.8) | 25.6 | 48.5 (47.3 to 49.7) | 33.7 |
| ICRS+CXL+PKR | 49.0 (47.0 to 51.0) | 15.5 | 44.8 (43.0 to 46.6) | 15.3 |
| ICRS+IOL | 56.0 (47.9 to 64.1) | 4.2 | 54.5 (48.5 to 60.5) | 1.4 |
| Kmean (Diopters) | ||||
| ICRS | 51.3 (50.8 to 51.9) | 58.5 | 47.0 (46.1 to 47.8) | 51.7 |
| ICRS+CXL | 50.0 (48.6 to 51.5) | 22.5 | 46.6 (45.3 to 47.9) | 31.2 |
| ICRS+CXL+PKR | 46.7 (45.0 to 48.4) | 14.3 | 43.7 (42.0 to 45.3) | 14.9 |
| ICRS+IOL | 53.1 (47.7 to 58.5) | 4.8 | 54.0 (49.7 to 58.3) | 2.2 |
Comparison of Parameters Between Procedures
ICRS versus ICRS+CXL: The parameters of these procedures only differed for CDVA, in favor of ICRS+CXL (coefficient 0.37 [0.04 to 0.71, P = 0.03]) (Fig. 3).
ICRS versus ICRS+CXL+PRK: All parameters were significantly improved in favor of the ICRS+CXL+PRK procedure except for spherical equivalent (Fig. 3).
ICRS+CXL versus ICRS+CXL+PRK: Cylinder and UDVA were significantly improved in favor of ICRS+CXL+PRK (coefficient 0.88 [0.01 to 1.76, P = 0.05] for cylinder and 0.88 [0.21 to 1.54, P = 0.01] for UDVA). Other parameters were not significantly improved (Fig. 3).
ICRS+IOL versus other procedures (ICRS; ICRS+CXL; ICRS+CXL+PRK): UDVA and spherical equivalent were significantly improved in favor of ICRS+IOL compared with all other procedures (P < 0.01). Other parameters did not differ between procedures (Fig. 3).
Comparison Between Parameters Within Procedures
ICRS
A maximum of 64 studies was used to evaluate ICRS insertion (references 8, 14–16, 26, 27, 30–39, 42, 43, 46–48, 53, 55–57, 59, 61–66, 68-71, 73, 75, 77, 79–84, 86–89, 91, 94, 96, 97, 99–104, 108, 109, 111, 112, 115). All parameters were significantly improved by ICRS insertion. The highest ES was found for the improvement of UDVA (ES 1.26 [95% CI, 1.07 to 1.44]), with a significant difference compared with CDVA, Kmax and Kmean (P < 0.01). The lowest ES was found for CDVA 0.75 (0.64 to 0.87), with a significant difference compared with UDVA (P < 0.01) (Fig. 4).
Figure 4.
Meta-regressions concerning the parameters in each procedure.
ICRS+CXL
A maximum of 20 studies was used to evaluate ICRS insertion with CXL (references 8, 15, 28, 29, 35, 38, 44, 45, 50, 51, 60, 62, 67, 74, 76, 85, 93, 105, 107, 115). All parameters were significantly improved by the ICRS+CXL procedure. The highest ES was found for the improvement of CDVA (1.15, 95% CI: 0.86 to 1.44) and the lowest ES for Kmean (0.90, 95% CI: 0.79 to 1.01). There was no significant difference between parameters in this procedure (Fig. 4).
ICRS+CXL+PRK
A maximum of nine studies was used to evaluate ICRS insertion with PRK and CXL (references 40–42, 50, 52, 60, 64, 73, 90). All parameters were significantly improved by ICRS+CXL+PRK insertion. The highest ES was found for the improvement of UDVA (2.07, 1.48 to 2.66) and the lowest ES for Kmean (1.27, 0.98 to 1.56). There was no significant difference between parameters in this procedure (Fig. 4).
ICRS+IOL
A maximum of five studies were used to evaluate ICRS associate with IOL implantation.49,51,59,72,113 All parameters were significantly improved by ICRS insertion. The highest ES was found for the improvement of UDVA (4.19, 3.25 to 5.13), with a significant difference compared with CDVA (P = 0.01) and cylinder (P = 0.05). The lowest ES was found for CDVA (1.39, 0.95 to 1.82) with a significant difference compared with UDVA (P = 0.01) and spherical equivalent (P = 0.04) (Fig. 4).
Funnel plots of all meta-analyses are presented in Supplementary Fig. S7. Further meta-analyses excluding studies that were not evenly distributed around the base of the funnel showed similar results (data not shown).
Metaregressions, Sensitivity Analyses, and Safety
Improvement of all parameters did not differ significantly between grades of keratoconus (Supplementary Fig. S8).
There was no significant difference in the moment of CXL performing in the overall parameters (Supplementary Fig. S9).
Sensitivity analyses taking into account methods of implantation (depth, type of rings—brand and width of ICRS), disease severity (grade), methods to create the intrastromal channel (femtosecond or manual), methods to measure keratometry, patient's gender, and sequence of CXL did not influence results.
Safety of ICRS implantation was reported in Supplementary Table S1. None of the included studies gave information on progression of keratoconus after ICRS implantation.
Discussion
The major findings were an overall improvement of all parameters evaluated with an ES ranging from 0.90 (95% CI, 0.78 to 1.01) for CDVA to 1.36 (95% CI, 1.22 to 1.51) for UDVA. ICRS is a good alternative for visual rehabilitation, and its association with CXL is not pernicious for postoperative results. Combining ICRS+CXL+PRK is less invasive than IOL implantation for young keratoconus patients and seems to be the best procedure leading to a decrease of cylinder (P = 0.02), an increase of CDVA (P = 0.05) and UDVA (P = 0.01), and a decrease in Kmax (P = 0.04) and Kmean (P = 0.04) compared with ICRS only. Even if ICRS+IOL demonstrated high ESs for all parameters, only spherical equivalent (P < 0.01) and UDVA (P < 0.01) had greater improvement, compared with other procedures.
ICRS Only or With CXL
In our study, we demonstrated an improvement in overall parameters in ICRS insertion with or without CXL association. The ICRS procedure must be considered as a good and safe alternative to improve visual rehabilitation and to delay keratoplasty in clear cornea.31 Studies have demonstrated a good stability several years after implantation.30,101 Many clinical studies have shown the effectiveness of CXL to inhibit progression of keratoconus.44 Our study showed that combining CXL with ICRS implantation was not pernicious for refractive, visual, and keratometric results. Interestingly, we found a significant improvement in CDVA for the ICRS+CXL procedure, probably due to an effective stability of the cone allowing a long and good correction of ametropia. Although CXL is known to stop the progression of the protrusion, recent long-term studies have also found a visual rehabilitation by corneal flattening.119 So, CXL must be proposed systematically in progressive keratoconus to stop evolution of the cone. Several CXL protocols have been proposed. The standard protocol is the most used but leads to a greater risk of infection and pain due to epithelium removal.120 Transepithelial-CXL was therefore proposed but results are heterogeneous in terms of biomechanical and functional efficacies.40,44 Finally, riboflavin in intrastromal pockets have been proposed and showed a good stability in the first 24 postoperative months.44,74,116 We did not see any difference in the moment of CXL surgery in the overall parameter, which was in agreement with a recent study.35 Another study found an increase of the CDVA in favor of CXL after ICRS compared with CXL before ICRS.107 So, the best sequence seems to be a one-step procedure with simultaneous ICRS and CXL.
Interest of PRK in the ICRS Procedure
We showed a significant improvement in all parameters except for spherical equivalent with ICRS+CXL+PRK when compared with ICRS alone, demonstrating the interest of associating ICRS and PRK as a safe alternative for correcting minor refractive errors in keratoconus.51,90 PRK is always combined with CXL to stabilize the remaining stromal bed and to avoid progression of ectatic disease in a cornea already weakened by the disease.50 The aim of PRK treatment is to treat part of the refractive error and regularize the cornea rather than fully correct the ametropia,90 which may explain the absence of significant differences in spherical equivalence in our study. The sequence in which the procedure is performed is not consensual. Despite insufficient data precluding further analysis on the best sequence for performing the procedure, a two-step procedure with ICRS first and then simultaneous PRK and CXL seems to be the most common sequence.42,121 The prior use of ICRS induces a corneal flattening and reduces keratometric astigmatism, allowing a controlled PRK treatment with minimal tissue ablation.32 In the second step, PRK followed by CXL seems to be better than CXL followed by PRK.122 This is justified by a decrease of CXL efficacy due to the excimer laser removing impregnated stroma.122
ICRS and IOL
ICRS+IOL demonstrated high ESs for all parameters; however, greater improvement was only seen for spherical equivalent and UDVA compared with other procedures. IOL may be implanted in selected patients with moderate to severe ametropia or with high anisometropia.51,123 In our study, we found a high ES of IOL insertion on spherical equivalent, proving the interest of IOL for ametropia correction. After ICRS insertion, most patients have high residual spherocylindrical refractive errors, which cannot be treated by excimer because of the fragility of the cornea and the high consumption of tissue.49,72 Usually, residual refractive errors are myopia or myopic astigmatism.72,113 In these patients, a pIOL could be proposed but only if ametropia is the reason for the poor visual rehabilitation or if a high anisometropia existed that alters the binocularity.123 IOL must be performed at least 6 months after ICRS implantation to confirm topographic and refractive stabilization after the procedure.59 Combining CXL with pIOL implantation allows a good stability to be ensured, to improve postoperative visual outcomes.120 Two types of pIOL can be proposed: iris claw or posterior chamber collagen copolymer. Both are safe and effective and implants must be determined on a case-by-case basis. Moreover, an important preoperative evaluation is necessary to avoid complications such as endothelial loss, cataract, and keratoconus evolution.124
Limitations
Our study has some limitations. Most studies included few patients and were retrospective. However, we demonstrated the putative role of ICRS in keratoconus and the benefit of additional procedures. Though there were similarities between the inclusion criteria, they were not identical. In particular, all studies did not include all grades of keratoconus and cone types. This may have minimized the differences we reported in different procedures. Moreover, different methods were used to measure keratometry precluding comparability, despite no significant differences between methods in sensitivity analyses. The majority of studies were single site, limiting the generalizability of our results; however, we included the main procedures and a large number of patients from most continents. We found differences in the performing of the techniques, especially for CXL, which could be with or without epithelium removal or with different instillation and irradiation periods, and PRK, which could be topography-guided or not. Data were collected differently in all studies and some data were not useable. Moreover, data were limited for some procedures, such as for ICRS + IOL. The impracticality of blinding interventions is an unavoidable limitation. Last meet was different in all studies, but our analyses took this variable into account. Unfortunately, the lack of details surrounding the disease, such as the results in each grade of keratoconus or the type of cone, precluded further analyses.
Conclusion
Although the quality and strength of the data are questionable, we showed an overall improvement of all parameters in ICRS procedures evaluated in keratoconus. ES ranged from 0.89 (95% CI, 0.78 to 1.00) for CDVA to 1.34 (95% CI, 1.2 to 1.50) for UDVA. Particularly, ICRS+CXL+PRK could be a low invasive procedure to propose to young keratoconic patients. ICRS could be an alternative to improve the visual rehabilitation and can delay other invasive procedures such as keratoplasty.
Supplementary Material
Acknowledgments
Disclosure: C. Benoist d'Azy, None; B. Pereira, None; F. Chiambaretta, None; F. Dutheil, None
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Romero-Jimenez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: a review. Cont Lens Anterior Eye. 2010;33:157–166. doi: 10.1016/j.clae.2010.04.006. quiz 205. [DOI] [PubMed] [Google Scholar]
- 3.Hwang S, Lim DH, Chung TY. Prevalence and incidence of keratoconus in South Korea: a nationwide population-based study. Am J Ophthalmol. 2018;192:56–64. doi: 10.1016/j.ajo.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP. Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol. 2017;175:169–172. doi: 10.1016/j.ajo.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Torres Netto EA, Al-Otaibi WM, Hafezi NL, et al. Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia. Br J Ophthalmol. 2018;102:1436–1441. doi: 10.1136/bjophthalmol-2017-311391. [DOI] [PubMed] [Google Scholar]
- 6.Henein C, Nanavaty MA. Systematic review comparing penetrating keratoplasty and deep anterior lamellar keratoplasty for management of keratoconus. Cont Lens Anterior Eye. 2017;40:3–14. doi: 10.1016/j.clae.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Parker JS, van Dijk K, Melles GR. Treatment options for advanced keratoconus: a review. Surv Ophthalmol. 2015;60:459–480. doi: 10.1016/j.survophthal.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Elsaftawy HS, Ahmed MH, Saif MY, Mousa R. Sequential intracorneal ring segment implantation and corneal transepithelial collagen cross-linking in keratoconus. Cornea. 2015;34:1420–1426. doi: 10.1097/ICO.0000000000000600. [DOI] [PubMed] [Google Scholar]
- 9.Olson RJ, Pingree M, Ridges R, et al. Penetrating keratoplasty for keratoconus: a long-term review of results and complications. J Cataract Refract Surg. 2000;26:987–991. doi: 10.1016/s0886-3350(00)00430-2. [DOI] [PubMed] [Google Scholar]
- 10.Sharif KW, Casey TA. Penetrating keratoplasty for keratoconus: complications and long-term success. Br J Ophthalmol. 1991;75:142–146. doi: 10.1136/bjo.75.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 12.Vega-Estrada A, Alio JL. The use of intracorneal ring segments in keratoconus. Eye Vis (London, England) 2016;3:8. doi: 10.1186/s40662-016-0040-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burris TE. Intrastromal corneal ring technology: results and indications. Curr Opin Ophthalmol. 1998;9:9–14. doi: 10.1097/00055735-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez-Vega Cueto L, Lisa C, Poo-Lopez A, et al. Intrastromal corneal ring segment implantation in 409 paracentral keratoconic eyes. Cornea. 2016;35:1421–1426. doi: 10.1097/ICO.0000000000000978. [DOI] [PubMed] [Google Scholar]
- 15.Alio JL, Pinero DP, Daxer A. Clinical outcomes after complete ring implantation in corneal ectasia using the femtosecond technology: a pilot study. Ophthalmology. 2011;118:1282–1290. doi: 10.1016/j.ophtha.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Haddad W, Fadlallah A, Dirani A, et al. Comparison of 2 types of intrastromal corneal ring segments for keratoconus. J Cataract Refract Surg. 2012;38:1214–1221. doi: 10.1016/j.jcrs.2012.02.039. [DOI] [PubMed] [Google Scholar]
- 17.da Costa BR, Cevallos M, Altman DG, Rutjes AW, Egger M. Uses and misuses of the strobe statement: bibliographic study. BMJ Open. 2011;1:e000048. doi: 10.1136/bmjopen-2010-000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (strobe): explanation and elaboration. Ann Intern Med. 2007;147:W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 19.Ollier M, Jr, Chamoux A, Naughton G, Pereira B, Dutheil F. Chest computed tomography screening for lung cancer in asbestos occupational exposure: a systematic review and meta-analysis. Chest. 2014;145:1339–1346. doi: 10.1378/chest.13-2181. [DOI] [PubMed] [Google Scholar]
- 20.Benoist d'Azy C, Pereira B, Naughton G, Chiambaretta F, Dutheil F. Antibioprophylaxis in prevention of endophthalmitis in intravitreal injection: a systematic review and meta-analysis. PLoS One. 2016;11:e0156431. doi: 10.1371/journal.pone.0156431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Courtin R, Pereira B, Naughton G, et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis. BMJ Open. 2016;6:e009675. doi: 10.1136/bmjopen-2015-009675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lanhers C, Pereira B, Naughton G, et al. Creatine supplementation and lower limb strength performance: a systematic review and meta-analyses. Sports Med. 2015;45:1285–1294. doi: 10.1007/s40279-015-0337-4. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Citrome L, Magnusson K. Paging Dr Cohen, Paging Dr Cohen... An effect size interpretation is required STAT!: visualising effect size and an interview with Kristoffer Magnusson. Int J Clin Pract. 2014;68:533–534. doi: 10.1111/ijcp.12435. [DOI] [PubMed] [Google Scholar]
- 26.Zare MA, Mehrjardi HZ, Afarideh M, Bahrmandy H, Mohammadi SF. Visual, keratometric and corneal biomechanical changes after intacs SK implantation for moderate to severe keratoconus. J Ophthalmic Vis Res. 2016;11:17–25. doi: 10.4103/2008-322X.180698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Israel M, Yousif MO, Osman NA, Nashed M, Abdelfattah NS. Keratoconus correction using a new model of intrastromal corneal ring segments. J Cataract Refract Surg. 2016;42:444–454. doi: 10.1016/j.jcrs.2015.11.044. [DOI] [PubMed] [Google Scholar]
- 28.Ibrahim O, Elmassry A, Said A, et al. Combined femtosecond laser-assisted intracorneal ring segment implantation and corneal collagen cross-linking for correction of keratoconus. Clin Ophthalmol. 2016;10:521–526. doi: 10.2147/OPTH.S97158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gordillo CH, Grandin JC, Zaldivar R, Zaldivar R, Lotfi AC. Efficacy of intrastromal corneal ring segments combined with flash collagen cross-linking in keratoconus. Cornea. 2017;36:144–147. doi: 10.1097/ICO.0000000000001104. [DOI] [PubMed] [Google Scholar]
- 30.Gauthier AS, Friot M, Montard R, Saleh M, Delbosc B. [Femtosecond-assisted ferrara intrastromal corneal ring implantation for treatment of keratoconus: functional outcomes at one year] J Fr Ophtalmol. 2016;39:428–436. doi: 10.1016/j.jfo.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Beniz LA, Queiroz GH, Queiroz CF, et al. Intrastromal corneal ring segments delay corneal grafting in patients with keratoconus. Arq Bras Oftalmol. 2016;79:30–32. doi: 10.5935/0004-2749.20160009. [DOI] [PubMed] [Google Scholar]
- 32.Al-Tuwairqi WS, Osuagwu UL, Razzouk H, AlHarbi A, Ogbuehi KC. Clinical evaluation of two types of intracorneal ring segments (ICRS) for keratoconus. Int Ophthalmol. 2017;37:1185–1198. doi: 10.1007/s10792-016-0385-2. [DOI] [PubMed] [Google Scholar]
- 33.Vega-Estrada A, Alio JL, Plaza-Puche AB. Keratoconus progression after intrastromal corneal ring segment implantation in young patients: five-year follow-up. J Cataract Refract Surg. 2015;41:1145–1152. doi: 10.1016/j.jcrs.2014.08.045. [DOI] [PubMed] [Google Scholar]
- 34.Mohebbi M, Hashemi H, Asgari S, Bigdeli S, Zamani KA. Visual outcomes after femtosecond-assisted intracorneal myoring implantation: 18 months of follow-up. Graefes Arch Clin Exp Ophthalmol. 2016;254:917–922. doi: 10.1007/s00417-015-3231-8. [DOI] [PubMed] [Google Scholar]
- 35.Liu XL, Li PH, Fournie P, Malecaze F. Investigation of the efficiency of intrastromal ring segments with cross-linking using different sequence and timing for keratoconus. Int J Ophthalmol. 2015;8:703–708. doi: 10.3980/j.issn.2222-3959.2015.04.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jadidi K, Mosavi SA, Nejat F, et al. Intrastromal corneal ring segment implantation (keraring 355 degrees) in patients with central keratoconus: 6-month follow-up. J Ophthalmol. 2015;2015:916385. doi: 10.1155/2015/916385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hashemi H, Amanzadeh K, Miraftab M, Asgari S. Femtosecond-assisted intrastromal corneal single-segment ring implantation in patients with keratoconus: a 12-month follow-up. Eye Contact Lens. 2015;41:183–186. doi: 10.1097/ICL.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 38.Ferenczy PA, Dalcegio M, Koehler M, et al. Femtosecond-assisted intrastromal corneal ring implantation for keratoconus treatment: a comparison with crosslinking combination. Arq Bras Oftalmol. 2015;78:76–81. doi: 10.5935/0004-2749.20150021. [DOI] [PubMed] [Google Scholar]
- 39.Fahd DC, Alameddine RM, Nasser M, Awwad ST. Refractive and topographic effects of single-segment intrastromal corneal ring segments in eyes with moderate to severe keratoconus and inferior cones. J Cataract Refract Surg. 2015;41:1434–1440. doi: 10.1016/j.jcrs.2014.10.037. [DOI] [PubMed] [Google Scholar]
- 40.Elbaz U, Shen C, Lichtinger A, et al. Accelerated versus standard corneal collagen crosslinking combined with same day phototherapeutic keratectomy and single intrastromal ring segment implantation for keratoconus. Br J Ophthalmol. 2015;99:155–159. doi: 10.1136/bjophthalmol-2014-304943. [DOI] [PubMed] [Google Scholar]
- 41.Al-Tuwairqi WS, Osuagwu UL, Razzouk H, Ogbuehi KC. One-year clinical outcomes of a two-step surgical management for keratoconus-topography-guided photorefractive keratectomy/cross-linking after intrastromal corneal ring implantation. Eye Contact Lens. 2015;41:359–366. doi: 10.1097/ICL.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 42.Zeraid FM, Jawkhab AA, Al-Tuwairqi WS, Osuagwu UL. Visual rehabilitation in low-moderate keratoconus: intracorneal ring segment implantation followed by same-day topography-guided photorefractive keratectomy and collagen cross linking. Int J Ophthalmol. 2014;7:800–806. doi: 10.3980/j.issn.2222-3959.2014.05.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Torquetti L, Ferrara G, Almeida F, et al. Intrastromal corneal ring segments implantation in patients with keratoconus: 10-year follow-up. J Refract Surg. 2014;30:22–26. doi: 10.3928/1081597X-20131217-02. [DOI] [PubMed] [Google Scholar]
- 44.Studeny P, Krizova D, Stranak Z. Clinical outcomes after complete intracorneal ring implantation and corneal collagen cross-linking in an intrastromal pocket in one session for keratoconus. J Ophthalmol. 2014;2014:568128. doi: 10.1155/2014/568128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shetty R, D'Souza S, Ramachandran S, Kurian M, Nuijts RM. Decision making nomogram for intrastromal corneal ring segments in keratoconus. Indian J Ophthalmol. 2014;62:23–28. doi: 10.4103/0301-4738.126170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sanchez-Thorin JC, Navarro PI. Single-segment intacs severe keratoconus 80% stromal depth insertion with a femtosecond laser for asymmetric keratoconus: a case series. Asia Pac J Ophthalmol (Phila) 2014;3:23–26. doi: 10.1097/APO.0b013e318299068a. [DOI] [PubMed] [Google Scholar]
- 47.Pena-Garcia P, Alio JL, Vega-Estrada A, Barraquer RI. Internal, corneal, and refractive astigmatism as prognostic factors for intrastromal corneal ring segment implantation in mild to moderate keratoconus. J Cataract Refract Surg. 2014;40:1633–1644. doi: 10.1016/j.jcrs.2014.01.047. [DOI] [PubMed] [Google Scholar]
- 48.Hashemian MN, Zare MA, Mohammadpour M, et al. Outcomes of single segment implantation of conventional intacs versus intacs SK for keratoconus. J Ophthal Vis Res. 2014;9:305–309. doi: 10.4103/2008-322X.143359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ferreira TB, Guell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30:336–341. doi: 10.3928/1081597X-20140319-01. [DOI] [PubMed] [Google Scholar]
- 50.Dirani A, Fadlallah A, Syed ZA, et al. Non-topography-guided photorefractive keratectomy for the correction of residual mild refractive errors after ICRS implantation and CXL in keratoconus. J Refract Surg. 2014;30:266–271. doi: 10.3928/1081597X-20140320-05. [DOI] [PubMed] [Google Scholar]
- 51.Dirani A, Fadlallah A, Khoueir Z, et al. Visian toric icl implantation after intracorneal ring segments implantation and corneal collagen crosslinking in keratoconus. Eur J Ophthalmol. 2014;24:338–344. doi: 10.5301/ejo.5000384. [DOI] [PubMed] [Google Scholar]
- 52.Yeung SN, Low SA, Ku JY, et al. Transepithelial phototherapeutic keratectomy combined with implantation of a single inferior intrastromal corneal ring segment and collagen crosslinking in keratoconus. J Cataract Refract Surg. 2013;39:1152–1156. doi: 10.1016/j.jcrs.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 53.Yeung SN, Ku JY, Lichtinger A, et al. Efficacy of single or paired intrastromal corneal ring segment implantation combined with collagen crosslinking in keratoconus. J Cataract Refract Surg. 2013;39:1146–1151. doi: 10.1016/j.jcrs.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 54.Vega-Estrada A, Alio JL, Brenner LF, et al. Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive, and aberrometric impairment. Am J Ophthalmol. 2013;155:575–584. doi: 10.1016/j.ajo.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 55.Tunc Z, Helvacioglu F, Sencan S. Evaluation of intrastromal corneal ring segments for treatment of keratoconus with a mechanical implantation technique. Indian J Ophthalmol. 2013;61:218–225. doi: 10.4103/0301-4738.109519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kotb AM, Hantera M. Efficacy and safety of intacs SK in moderate to severe keratoconus. Middle East Afr J Ophthalmol. 2013;20:46–50. doi: 10.4103/0974-9233.106386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jabbarvand M, Salamatrad A, Hashemian H, Mazloumi M, Khodaparast M. Continuous intracorneal ring implantation for keratoconus using a femtosecond laser. J Cataract Refract Surg. 2013;39:1081–1087. doi: 10.1016/j.jcrs.2013.02.054. [DOI] [PubMed] [Google Scholar]
- 58.Ganesh S, Shetty R, D'Souza S, Ramachandran S, Kurian M. Intrastromal corneal ring segments for management of keratoconus. Indian J Ophthalmol. 2013;61:451–455. doi: 10.4103/0301-4738.116065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Coskunseven E, Sharma DP, Jankov MR, 2nd, et al. Collagen copolymer toric phakic intraocular lens for residual myopic astigmatism after intrastromal corneal ring segment implantation and corneal collagen crosslinking in a 3-stage procedure for keratoconus. J Cataract Refract Surg. 2013;39:722–729. doi: 10.1016/j.jcrs.2012.11.027. [DOI] [PubMed] [Google Scholar]
- 60.Coskunseven E, Jankov MR, 2nd, Grentzelos MA, et al. Topography-guided transepithelial PRK after intracorneal ring segments implantation and corneal collagen CXL in a three-step procedure for keratoconus. J Refract Surg. 2013;29:54–58. doi: 10.3928/1081597X-20121217-01. [DOI] [PubMed] [Google Scholar]
- 61.Carballo J, Puell MC, Cuina R, Vazquez JM, Benitez-del-Castillo JM. Changes in visual function under mesopic and photopic conditions after intrastromal corneal ring segment implantation for different stages of keratoconus. J Cataract Refract Surg. 2013;39:393–402. doi: 10.1016/j.jcrs.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 62.Cakir H, Pekel G, Perente I, Genc S. Comparison of intrastromal corneal ring segment implantation only and in combination with collagen crosslinking for keratoconus. Eur J Ophthalmol. 2013;23:629–634. doi: 10.5301/ejo.5000250. [DOI] [PubMed] [Google Scholar]
- 63.Alfonso JF, Fernandez-Vega Cueto L, Baamonde B, et al. Inferior intrastromal corneal ring segments in paracentral keratoconus with no coincident topographic and coma axis. J Refract Surg. 2013;29:266–272. doi: 10.3928/1081597X-20130318-06. [DOI] [PubMed] [Google Scholar]
- 64.Al-Tuwairqi W, Sinjab MM. Intracorneal ring segments implantation followed by same-day topography-guided PRK and corneal collagen CXL in low to moderate keratoconus. J Refract Surg. 2013;29:59–63. doi: 10.3928/1081597X-20121228-04. [DOI] [PubMed] [Google Scholar]
- 65.Tu KL, Batterbury M, Kaye SB. Intrastromal corneal ring segments: effect of relationship between alignment and topographic keratometric meridians. J Cataract Refract Surg. 2012;38:1432–1439. doi: 10.1016/j.jcrs.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 66.Sogutlu E, Pinero DP, Kubaloglu A, Alio JL, Cinar Y. Elevation changes of central posterior corneal surface after intracorneal ring segment implantation in keratoconus. Cornea. 2012;31:387–395. doi: 10.1097/ICO.0b013e31822481df. [DOI] [PubMed] [Google Scholar]
- 67.Renesto Ada C, Melo LA, Jr, Sartori Mde F, Campos M. Sequential topical riboflavin with or without ultraviolet a radiation with delayed intracorneal ring segment insertion for keratoconus. Am J Ophthalmol. 2012;153:982–993. doi: 10.1016/j.ajo.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 68.Pinero DP, Alio JL, Barraquer RI, Michael R. Corneal biomechanical changes after intracorneal ring segment implantation in keratoconus. Cornea. 2012;31:491–499. doi: 10.1097/ICO.0b013e31821ee9f4. [DOI] [PubMed] [Google Scholar]
- 69.Pena-Garcia P, Vega-Estrada A, Barraquer RI, Burguera-Gimenez N, Alio JL. Intracorneal ring segment in keratoconus: a model to predict visual changes induced by the surgery. Invest Ophthalmol Vis Sci. 2012;53:8447–8457. doi: 10.1167/iovs.12-10639. [DOI] [PubMed] [Google Scholar]
- 70.Ozerturk Y, Sari ES, Kubaloglu A, et al. Comparison of deep anterior lamellar keratoplasty and intrastromal corneal ring segment implantation in advanced keratoconus. J Cataract Refract Surg. 2012;38:324–332. doi: 10.1016/j.jcrs.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 71.Niknam S, Shamshiri M, Shahrzad SS, et al. Treatment of moderate to severe keratoconus with 6-mm intacs SK. Int J Ophthalmol. 2012;5:513–516. doi: 10.3980/j.issn.2222-3959.2012.04.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Navas A, Tapia-Herrera G, Jaimes M, et al. Implantable collamer lenses after intracorneal ring segments for keratoconus. Int Ophthalmol. 2012;32:423–429. doi: 10.1007/s10792-012-9582-9. [DOI] [PubMed] [Google Scholar]
- 73.Kremer I, Aizenman I, Lichter H, Shayer S, Levinger S. Simultaneous wavefront-guided photorefractive keratectomy and corneal collagen crosslinking after intrastromal corneal ring segment implantation for keratoconus. J Cataract Refract Surg. 2012;38:1802–1807. doi: 10.1016/j.jcrs.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 74.Kilic A, Kamburoglu G, Akinci A. Riboflavin injection into the corneal channel for combined collagen crosslinking and intrastromal corneal ring segment implantation. J Cataract Refract Surg. 2012;38:878–883. doi: 10.1016/j.jcrs.2011.11.041. [DOI] [PubMed] [Google Scholar]
- 75.Khan MI, Injarie A, Muhtaseb M. Intrastromal corneal ring segments for advanced keratoconus and cases with high keratometric asymmetry. J Cataract Refract Surg. 2012;38:129–136. doi: 10.1016/j.jcrs.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 76.Henriquez MA, Izquierdo L, Jr, Bernilla C, McCarthy M. Corneal collagen cross-linking before ferrara intrastromal corneal ring implantation for the treatment of progressive keratoconus. Cornea. 2012;31:740–745. doi: 10.1097/ICO.0b013e318219aa7a. [DOI] [PubMed] [Google Scholar]
- 77.Gharaibeh AM, Muhsen SM, AbuKhader IB, et al. Keraring intrastromal corneal ring segments for correction of keratoconus. Cornea. 2012;31:115–120. doi: 10.1097/ICO.0b013e3182215a15. [DOI] [PubMed] [Google Scholar]
- 78.Ferrara G, Torquetti L, Ferrara P, Merayo-Lloves J. Intrastromal corneal ring segments: Visual outcomes from a large case series. Clin Exp Ophthalmol. 2012;40:433–439. doi: 10.1111/j.1442-9071.2011.02698.x. [DOI] [PubMed] [Google Scholar]
- 79.Fahd DC, Jabbur NS, Awwad ST. Intrastromal corneal ring segment sk for moderate to severe keratoconus: a case series. J Refract Surg. 2012;28:701–705. doi: 10.3928/1081597X-20120921-05. [DOI] [PubMed] [Google Scholar]
- 80.Coimbra CC, Gomes MT, Campos M, et al. Femtosecond assisted intrastromal corneal ring (ISCR) implantation for the treatment of corneal ectasia. Arq Bras Oftalmol. 2012;75:126–130. doi: 10.1590/s0004-27492012000200011. [DOI] [PubMed] [Google Scholar]
- 81.Ameerh MA, Hamad GI, Ababneh OH, et al. Ferrara ring segments implantation for treating keratoconus. Int J Ophthalmol. 2012;5:586–590. doi: 10.3980/j.issn.2222-3959.2012.05.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alfonso JF, Lisa C, Merayo-Lloves J, Fernandez-Vega Cueto L, Montes-Mico R. Intrastromal corneal ring segment implantation in paracentral keratoconus with coincident topographic and coma axis. J Cataract Refract Surg. 2012;38:1576–1582. doi: 10.1016/j.jcrs.2012.05.031. [DOI] [PubMed] [Google Scholar]
- 83.Tu KL, Sebastian RT, Owen M, Batterbury M, Kaye SB. Quantification of the surgically induced refractive effect of intrastromal corneal ring segments in keratoconus with standardized incision site and segment size. J Cataract Refract Surg. 2011;37:1865–1870. doi: 10.1016/j.jcrs.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 84.Sedaghat M, Zarei-Ghanavati M. Vertical versus oblique implantation of intrastromal corneal ring segments for keratoconus. J Cataract Refract Surg. 2011;37:161–165. doi: 10.1016/j.jcrs.2010.07.026. [DOI] [PubMed] [Google Scholar]
- 85.Saelens IE, Bartels MC, Bleyen I, Van Rij G. Refractive, topographic, and visual outcomes of same-day corneal cross-linking with ferrara intracorneal ring segments in patients with progressive keratoconus. Cornea. 2011;30:1406–1408. doi: 10.1097/ICO.0b013e3182151ffc. [DOI] [PubMed] [Google Scholar]
- 86.Mahmood H, Venkateswaran RS, Daxer A. Implantation of a complete corneal ring in an intrastromal pocket for keratoconus. J Refract Surg. 2011;27:63–68. doi: 10.3928/1081597X-20100212-11. [DOI] [PubMed] [Google Scholar]
- 87.Madar J, Proust H, Matonti F, et al. [New therapeutic approach of keratoconus with intracorneal ring segments aided by femtosecond laser (tecnolas perfect vision): indications, operating technique and results] J Fr Ophtalmol. 2011;34:2–9. doi: 10.1016/j.jfo.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 88.Kubaloglu A, Sari ES, Cinar Y, et al. Intrastromal corneal ring segment implantation for the treatment of keratoconus. Cornea. 2011;30:11–17. doi: 10.1097/ICO.0b013e3181e2cf57. [DOI] [PubMed] [Google Scholar]
- 89.Kaya V, Utine CA, Karakus SH, Kavadarli I, Yilmaz OF. Refractive and visual outcomes after intacs vs ferrara intrastromal corneal ring segment implantation for keratoconus: a comparative study. J Refract Surg. 2011;27:907–912. doi: 10.3928/1081597X-20110906-03. [DOI] [PubMed] [Google Scholar]
- 90.Iovieno A, Legare ME, Rootman DB, et al. Intracorneal ring segments implantation followed by same-day photorefractive keratectomy and corneal collagen cross-linking in keratoconus. J Refract Surg. 2011;27:915–918. doi: 10.3928/1081597X-20111103-03. [DOI] [PubMed] [Google Scholar]
- 91.Hamdi IM. Preliminary results of intrastromal corneal ring segment implantation to treat moderate to severe keratoconus. J Cataract Refract Surg. 2011;37:1125–1132. doi: 10.1016/j.jcrs.2010.12.048. [DOI] [PubMed] [Google Scholar]
- 92.Gorgun E, Kucumen RB, Yenerel NM. Influence of intrastromal corneal ring segment implantation on corneal biomechanical parameters in keratoconic eyes. Jpn J Ophthalmol. 2011;55:467–471. doi: 10.1007/s10384-011-0057-8. [DOI] [PubMed] [Google Scholar]
- 93.El-Raggal TM. Sequential versus concurrent kerarings insertion and corneal collagen cross-linking for keratoconus. Br J Ophthalmol. 2011;95:37–41. doi: 10.1136/bjo.2010.179580. [DOI] [PubMed] [Google Scholar]
- 94.Ancele E, Malecaze F, Arne JL, Fournie P. [Predictive factors for successful ferrara intracorneal ring segment implantation in keratoconus] J Fr Ophtalmol. 2011;34:513–520. doi: 10.1016/j.jfo.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 95.Abad JC, Arango J, Tobon C. Comparison of astigmatism correction using shorter arc length 90 degrees/120 degrees asymmetric intacs severe keratoconus versus 150 degrees single-segment intacs severe keratoconus in asymmetric keratoconus. Cornea. 2011;30:1201–1216. doi: 10.1097/ICO.0b013e3182182bc6. [DOI] [PubMed] [Google Scholar]
- 96.Sansanayudh W, Bahar I, Kumar NL, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–113. doi: 10.1016/j.jcrs.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 97.Pinero DP, Alio JL, Teus MA, Barraquer RI, Uceda-Montanes A. Modeling the intracorneal ring segment effect in keratoconus using refractive, keratometric, and corneal aberrometric data. Invest Ophthalmol Vis Sci. 2010;51:5583–5591. doi: 10.1167/iovs.09-5017. [DOI] [PubMed] [Google Scholar]
- 98.Kubaloglu A, Sari ES, Cinar Y, et al. Comparison of mechanical and femtosecond laser tunnel creation for intrastromal corneal ring segment implantation in keratoconus: prospective randomized clinical trial. J Cataract Refract Surg. 2010;36:1556–1561. doi: 10.1016/j.jcrs.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 99.Kubaloglu A, Cinar Y, Sari ES, et al. Comparison of 2 intrastromal corneal ring segment models in the management of keratoconus. J Cataract Refract Surg. 2010;36:978–985. doi: 10.1016/j.jcrs.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 100.Daxer A, Mahmoud H, Venkateswaran RS. Intracorneal continuous ring implantation for keratoconus: one-year follow-up. J Cataract Refract Surg. 2010;36:1296–1302. doi: 10.1016/j.jcrs.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 101.Torquetti L, Berbel RF, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009;35:1768–1773. doi: 10.1016/j.jcrs.2009.05.036. [DOI] [PubMed] [Google Scholar]
- 102.Shetty R, Narayana KM, Mathew K, et al. Safety and efficacy of intacs in Indian eyes with keratoconus: an initial report. Indian J Ophthalmol. 2009;57:115–119. doi: 10.4103/0301-4738.44517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pinero DP, Alio JL, El Kady B, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009;116:1675–1687. doi: 10.1016/j.ophtha.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 104.Ferrara P, Torquetti L. Clinical outcomes after implantation of a new intrastromal corneal ring with a 210-degree arc length. J Cataract Refract Surg. 2009;35:1604–1608. doi: 10.1016/j.jcrs.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 105.Ertan A, Karacal H, Kamburoglu G. Refractive and topographic results of transepithelial cross-linking treatment in eyes with intacs. Cornea. 2009;28:719–723. doi: 10.1097/ICO.0b013e318191b83d. [DOI] [PubMed] [Google Scholar]
- 106.Dauwe C, Touboul D, Roberts CJ, et al. Biomechanical and morphological corneal response to placement of intrastromal corneal ring segments for keratoconus. J Cataract Refract Surg. 2009;35:1761–1767. doi: 10.1016/j.jcrs.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 107.Coskunseven E, Jankov MR, 2nd, Hafezi F, et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35:2084–2091. doi: 10.1016/j.jcrs.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 108.Shetty R, Kurian M, Anand D, et al. Intacs in advanced keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 109.Ertan A, Kamburoglu G. Intacs implantation using a femtosecond laser for management of keratoconus: comparison of 306 cases in different stages. J Cataract Refract Surg. 2008;34:1521–1526. doi: 10.1016/j.jcrs.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 110.Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year results of intrastromal corneal ring segment implantation (keraring) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008;145:775–779. doi: 10.1016/j.ajo.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 111.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: safety and efficacy. J Cataract Refract Surg. 2007;33:1886–1891. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 112.Shabayek MH, Alio JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114:1643–1652. doi: 10.1016/j.ophtha.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 113.El-Raggal TM, Abdel Fattah AA. Sequential intacs and verisyse phakic intraocular lens for refractive improvement in keratoconic eyes. J Cataract Refract Surg. 2007;33:966–970. doi: 10.1016/j.jcrs.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 114.Colin J, Malet FJ. Intacs for the correction of keratoconus: two-year follow-up. J Cataract Refract Surg. 2007;33:69–74. doi: 10.1016/j.jcrs.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 115.Chan CC, Sharma M, Wachler BS. Effect of inferior-segment intacs with and without c3-r on keratoconus. J Cataract Refract Surg. 2007;33:75–80. doi: 10.1016/j.jcrs.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 116.Alio JL, Toffaha BT, Pinero DP, Klonowski P, Javaloy J. Cross-linking in progressive keratoconus using an epithelial debridement or intrastromal pocket technique after previous corneal ring segment implantation. J Refract Surg. 2011;27:737–743. doi: 10.3928/1081597X-20110705-01. [DOI] [PubMed] [Google Scholar]
- 117.Krumeich JH, Daniel J, Knulle A. Live-epikeratophakia for keratoconus. J Cataract Refract Surg. 1998;24:456–463. doi: 10.1016/s0886-3350(98)80284-8. [DOI] [PubMed] [Google Scholar]
- 118.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 119.Goldich Y, Marcovich AL, Barkana Y, et al. Clinical and corneal biomechanical changes after collagen cross-linking with riboflavin and uv irradiation in patients with progressive keratoconus: results after 2 years of follow-up. Cornea. 2012;31:609–614. doi: 10.1097/ICO.0b013e318226bf4a. [DOI] [PubMed] [Google Scholar]
- 120.Esteve-Taboada JJ, Dominguez-Vicent A, Ferrer-Blasco T, Alfonso JF, Montes-Mico R. Posterior chamber phakic intraocular lenses to improve visual outcomes in keratoconus patients. J Cataract Refract Surg. 2017;43:115–130. doi: 10.1016/j.jcrs.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 121.Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided prk for treatment of keratoconus. J Refract Surg. 2009;25:S812–S818. doi: 10.3928/1081597X-20090813-10. [DOI] [PubMed] [Google Scholar]
- 122.Lin DT, Holland S, Tan JC, Moloney G. Clinical results of topography-based customized ablations in highly aberrated eyes and keratoconus/ectasia with cross-linking. J Refract Surgery. 2012;28:S841–S848. doi: 10.3928/1081597X-20121005-06. [DOI] [PubMed] [Google Scholar]
- 123.Alio JL, Pena-Garcia P, Abdulla GF, Zein G, Abu-Mustafa SK. Comparison of iris-claw and posterior chamber collagen copolymer phakic intraocular lenses in keratoconus. J Cataract Refract Surg. 2014;40:383–394. doi: 10.1016/j.jcrs.2013.07.052. [DOI] [PubMed] [Google Scholar]
- 124.Moshirfar M, Imbornoni LM, Ostler EM, Muthappan V. Incidence rate and occurrence of visually significant cataract formation and corneal decompensation after implantation of verisyse/artisan phakic intraocular lens. Clin Ophthalmol. 2014;8:711–716. doi: 10.2147/OPTH.S59878. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.