Abstract
Patient: Female, 50
Final Diagnosis: Axial chordoma
Symptoms: Back ache • numbness • urine incontinence • weaknes of lower limbs
Medication: —
Clinical Procedure: —
Specialty: Plastic Surgery
Objective:
Rare disease
Background:
Chordoma is a primary bone tumor that most commonly arises in the sacrococcygeal vertebrae and the spheno-occipital areas. Chordoma is a malignant tumor that should be distinguished from benign notochordal cell tumor (BNCT) of the spine. This report is of a rare case of axial chordoma and describes the challenging approach to diagnosis and management.
Case Report:
A 50-year-old woman presented with a one-year history of a slowly growing swelling in the sacral region. She complained of numbness and progressive weakness in both lower limbs, and urinary incontinence. Computed tomography (CT) imaging showed a large destructive lesion involving the sacrum and coccyx with cranial extension to level S2 and invasion of the right and left S2–S3 neural foramina, sacral nerves, left gluteus maximums muscle, and adjacent subcutaneous tissue. The management approach included the early involvement of a multidisciplinary clinical team. En bloc resection of the tumor through an anterior and posterior approach was performed, and the defect was reconstructed later using bilateral rotational gluteal fascial flaps.
Conclusions:
Axial chordoma is a very rare, locally aggressive, and highly recurrent primary tumor of bone. The clinical management is challenging and requires early involvement of a multidisciplinary team. Following surgical resection, careful selection from limited available reconstructive surgical options is necessary to ensure that the surgical defect is repaired.
MeSH Keywords: Chordoma, Medicine, Surgical Flaps
Background
Chordoma is a primary bone tumor that most commonly arises in the sacrococcygeal vertebrae and the spheno-occipital areas. Chordoma is a malignant tumor that should be distinguished from benign notochordal cell tumor (BNCT) of the spine. The cell or origin of chordoma remains controversial. However, recent studies have suggested that chordoma may arise from BNCT, as both tumors share an anatomic origin. Also, cases of BNCT have been shown to progress to incipient chordoma in two reported cases and into classical chordoma in one case [1,2].
This report is of a rare case of axial chordoma and describes the challenging approach to diagnosis and management.
Case Report
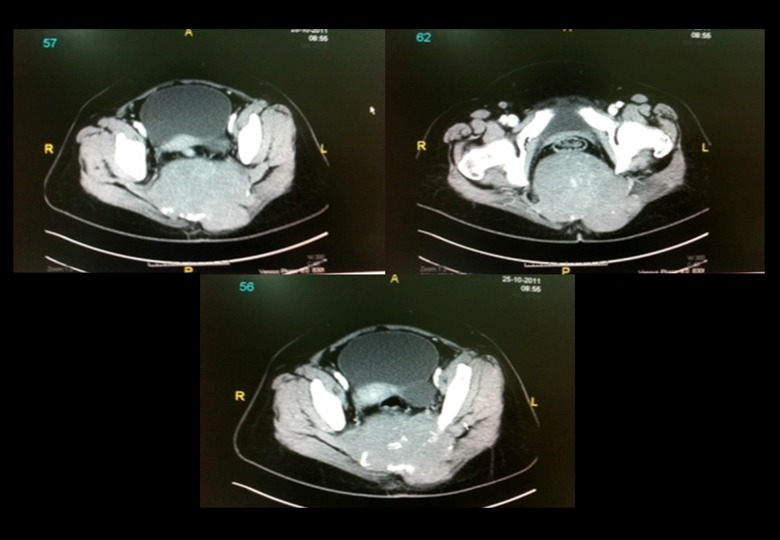
A 50-year-old woman presented with a one-year history of a slowly growing swelling in the sacral region, which she ignored without seeking medical advice. She developed numbness and progressive weakness in both lower limbs, and urinary incontinence. On admission to the hospital, she was found to have a large gluteal mass measuring 15×15 cm, and loss of perineal sensation and anal tone. Computed tomography (CT) imaging showed a large destructive lesion involving the sacrum and coccyx with cranial extension to S2 and invading the right and left S2–S3 neural foramina, sacral nerves, left gluteus maximums muscle, and adjacent subcutaneous tissue (Figure 1). Due to the complex nature of the case, a multidisciplinary clinical approach was taken to her management.
Figure 1.
Transverse computed tomography (CT) images of the sacrum and coccyx in a 50-year-old woman with axial chordoma. Computed tomography (CT) images show extensive destruction of the sacrum and coccyx, and tumor invasion of the right and left S2–S3 neural foramina, sacral nerves, left gluteus maximums muscle, and adjacent subcutaneous tissue.
The patient was taken to the operating room and, in conjunction with colorectal and plastic surgery specialists, she underwent a low sacral vertebral amputation and en bloc resection of the tumor. An en bloc resection was performed with an anterior and posterior approach, because of local invasion of the large bowel. Following surgical resection, histopathology confirmed a completely excised chordoma with negative surgical resection margins.
In the plastic surgery ward, when patient’s condition allowed, bilateral rotational gluteal fascial flaps were raised, one flap was de-epithelialized and embedded in the cavity and the other epithelized flap was sutured on top of the de-epithelialized flap.
Discussion
Chordoma was first described in 1857 by Virchow in et al. [3], who described the origin of chordoma as being from notochord remnant that usually involute during the tenth week of gestation. Notochord remnants that remain in the nucleus pulposus of the cartilaginous discs, might explain the anatomic predilection for chordoma in the axial skeleton, clivus, and sacral regions. Chordoma is a rare tumor that affects adults over the age of 40 years and has an incidence of 0.5 per million in the European population [5]. The prevalence of primary chordoma is 1–8% of all primary malignant tumors of bone, but chordoma represents 20% of all primary bone malignancy of the spine [4]. The most common site of chordoma is the axial skeleton in 32.8% of the cases, followed by the sacrum in 29.2%, and few cases of primary chordoma have been reported in the extra-axial bone and soft tissue.
Chordoma is a slowly growing malignant tumor that tends to locally infiltrate bone and adjacent soft tissues and has a high chance of recurrence after surgical excision, which increases when the tumor invades into the neural foramina [6], and also results in a challenge for the surgeon to ensure complete excision. Chordoma has the potential to transform into high-grade sarcomas in 5% of patients [6]. Although chordoma is generally locally invasive, this tumor has the ability to metastasize late in the disease course in around 37% of the cases [7–9]. The malignant characteristics of chordoma results in a reported mean overall survival of 6.29 years [10].
Furukawa et al. [11] reported the use of the gluteus maximus adipomuscular turnover or sliding flap for repair of sacral defects following surgical excision of chordoma. The advantages of using the gluteus maximus muscle are its bulk, proximity to the defect, and good blood supply [12–16]. However, the use of a gluteus flap is not available in all cases because this flap can be invaded by the tumor, which will limit the options for postoperative coverage and cosmesis.
In this case, the gluteus maximums muscles, as well as the superior and inferior gluteal pedicles, were invaded and replaced by the tumor, leaving minimal reconstructive options for covering the gluteal and sacral defect with exposed wires. One of the available options was to raise the latissimus dorsi muscle as a free flap to create a subcutaneous vascular conduit to microsurgically connect both the artery and vein of the muscle flap to the femoral artery and vein in an end-to-side anastomosis. However, this procedure is very extensive and may be too prolonged, considering the general condition of the patient. Therefore, in this case, two fascial flaps were raised and arranged in a stacked fashion and provided adequate thickness to cover the deep surgical defect. Also, this surgical approach was not associated with donor morbidity and resulted in good aesthetic and reconstructive outcome.
Conclusions
Axial chordoma is a very rare, locally aggressive, and highly recurrent primary tumor of bone. As this case has shown, the clinical management is challenging and requires early involvement of a multidisciplinary team. Following surgical resection, careful selection from limited available reconstructive surgical options is necessary to ensure that the surgical defect is repaired.
Footnotes
Conflict of interest
None.
References:
- 1.Yamaguchi T, Yamato M, Saotome K. First histologically confirmed case of a classic chordoma arising in a precursor benign notochordal lesion: Differential diagnosis of benign and malignant notochordal lesions. Skeletal Radiol. 2002;31:413–18. doi: 10.1007/s00256-002-0514-z. [DOI] [PubMed] [Google Scholar]
- 2.Yamaguchi T, Watanabe-Ishiiwa H, Suzuki S, et al. Incipient chordoma: A report of two cases of early-stage chordoma arising from benign notochordal cell tumors. Mod Pathol. 2005;18(7):1005–10. doi: 10.1038/modpathol.3800378. [DOI] [PubMed] [Google Scholar]
- 3.Stewart MJ. Malignant sacrococcygeal chordoma. J Pathol Bacteriol. 1922;25:40–62. [Google Scholar]
- 4.Rosenberg AE. Pathology of chordoma and chondrosarcoma of the axial skeleton. In: Harsh G, editor. Chordomas and chondrosarcomas of the skull base and spine. New York, NY: Thieme Medical Publishers; 2003. pp. 8–15. [Google Scholar]
- 5.Eriksson B, Gunterberg B, Kindblom LG. Chordoma: A clinicopathological and prognostic study of a Swedish National series. Acta Orthop Scand. 1981;52:49–58. doi: 10.3109/17453678108991758. [DOI] [PubMed] [Google Scholar]
- 6.Al-Adnani M, Cannon SR, Flanagan AM. Chordomas do not express CD10 or renal cell carcinoma (RCC) antigen: An immunohistochemical study. Histopathology. 2005;47:536–37. doi: 10.1111/j.1365-2559.2005.02131.x. [DOI] [PubMed] [Google Scholar]
- 7.Badwal S, Pal L, Basu A, et al. Multiple synchronous spinal extraosseous intradural chordomas: Is it a distinct entity? Br J Neurosurg. 2006;20:99–103. doi: 10.1080/02688690600682614. [DOI] [PubMed] [Google Scholar]
- 8.Bergh P, Kindblom LG, Gunterberg B, et al. Prognostic factors in chordoma of the sacrum and mobile spine: A study of 39 patients. Cancer. 2000;88:2122–34. doi: 10.1002/(sici)1097-0142(20000501)88:9<2122::aid-cncr19>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 9.McPherson CM, Suk K, McCutcheon IE, et al. Metastatic disease from spinal chordomas: A 10-year experience. J Neurosurg Spine. 2006;5:277–80. doi: 10.3171/spi.2006.5.4.277. [DOI] [PubMed] [Google Scholar]
- 10.McMaster ML, Goldstein AM, Bromley CM, et al. Chordoma: Incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control. 2001;12:1–11. doi: 10.1023/a:1008947301735. [DOI] [PubMed] [Google Scholar]
- 11.Furukawa H, Yamamoto Y, Igawa HH, et al. Gluteus maximus adipomuscular turnover or sliding flap in the surgical treatment of extensive sacral chordomas. Plast Reconstr Surg. 2000;105:1013–16. doi: 10.1097/00006534-200003000-00026. [DOI] [PubMed] [Google Scholar]
- 12.Ramirez OM, Swartz WM, Futrell JW. The gluteus maximus muscle: Experimental and clinical considerations relevant to reconstruction in ambulatory patients. Br J Plast Surg. 1987;40:1–10. doi: 10.1016/0007-1226(87)90002-6. [DOI] [PubMed] [Google Scholar]
- 13.Parkash S, Banerjee S. The total gluteus maximus rotation and other gluteus maximus musculocutaneous flaps in the treatment of pressure ulcers. Br J Plast Surg. 1986;39:66–71. doi: 10.1016/0007-1226(86)90006-8. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez OM, Hurwitz DJ, Futrell JW. The expansive gluteus maximus flap. Plast Reconstr Surg. 1984;74:757–68. doi: 10.1097/00006534-198412000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Ramirez OM, Orlando JC, Hurwitz DJ. The sliding gluteus maximus myocutaneous flap: Its relevance in ambulatory patients. Plast Reconstr Surg. 1984;74:68–75. doi: 10.1097/00006534-198407000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Hagerty RC, Gould WL. The split gluteus maximus muscle turnover flap. Plast Reconstr Surg. 1995;96:1459–62. doi: 10.1097/00006534-199511000-00040. [DOI] [PubMed] [Google Scholar]