Abstract
Objective:
Evidence suggests peer support (PS) is as an effective strategy for enhancing prevention and control of chronic and infectious diseases, including cancer. This systematic scoping review examines the range and variety of interventions on the use of PS across the cancer care continuum.
Method:
We used a broad definition of PS to capture a wide-range of interventions and characterize the current status of the field. Literature searches were conducted using PubMed, SCOPUS, and CINAHL to identify relevant articles published from January 2011 – June 2016. We screened the title and abstracts of 2087 articles, followed by full-text screening of 420 articles, resulting in a final sample of 242 articles of which the most recent 100 articles were reviewed (published June 2014 – May 2016).
Results:
A number of the recent intervention studies focused on breast cancer (32%, breast cancer only) or multiple cancer sites (23%). Although the interventions spanned all phases of the cancer care continuum, only 2% targeted end-of-life care. Seventy-six percent focused on clinical outcomes (e.g., screening, treatment adherence) and 72% on reducing health disparities. Interventions were primarily phone-based (44%) or delivered in a clinic setting (44%). Only a few studies (22%) described the impact of providing PS on peer supporters.
Conclusion:
PS appears to be a widely used approach to address needs across the cancer care continuum, with many opportunities to expand its reach.
Keywords: cancer, community health workers, navigator, oncology, peer support, social support
INTRODUCTION
Cancer is a leading cause of global mortality, accounting for over 8.7 million deaths in 2015 [1]. Over the last decade, substantial progress has been made in regard to prevention, diagnostic, and treatment options for the majority of cancer types [2,3]. However, the burden of cancer related mortality is still rising, particularly in lower-middle income countries where 85% of the world’s population resides [4]. This is due in part to changing demographics, exposure to environmental carcinogens and cancer-causing infectious diseases, and the adoption of lifestyle behaviors that increase cancer risk (e.g., physical inactivity, unsafe reproductive patterns, unhealthy eating, as well as alcohol and tobacco use) [1,4]. Given the breadth of specific cancers and diversity in associated risk factors, effective approaches for cancer control and prevention must be both adaptable and comprehensive.
Despite advances across the cancer care continuum, challenges persist. Studies show that patients have barriers accessing care including screenings and treatment services [5,6]. Patients in rural areas lacking or with small health centers may require travel to receive quality care [7]. Initiating and sustaining a healthy lifestyle becomes a challenge for some during treatment and survivorship [8-10]. Once a person is diagnosed, there are barriers to follow-up. In addition to financial barriers, Palmer et al. notes the need for psychosocial care to reduce fear of recurrence to improve follow-up among African American breast cancer survivors [11]. Research indicates the need for communication to help patients understand the complexities of cancer information to assist with decision making for screening and treatment and during survivorship [12]. Lack of social support, depression, and distress were also indicated in studies as relevant for cancer related outcomes [13-15].
Peer support (PS) is an effective disease prevention and management strategy to enhance linkages to care and attend to the dynamic and evolving conditions of real world environments and circumstances that influence health behavior [16-23]. As used here, PS is defined by the functions and principles that comprise it and not restricted to specific nomenclature commonly used in the reviewed literature (e.g., “community health workers,” “lay health advisors,” and “peer navigators” among others) [24]. By providing individuals assistance for daily management, addressing complex emotional and social issues, linking individuals to resources in clinic and community settings (e.g., navigation of health care systems), and providing ongoing care, peer supporters have effectively addressed diverse health needs and served in a variety of capacities and settings [25-27]. In other words, PS is a strategy for providing help and support to others and is often delivered by non-professionals (i.e., peers).
Across the cancer care continuum, PS has emerged as an important strategy to address many barriers to cancer prevention [28], early detection [29,30], treatment [22,31], and survivorship [31,22]. Peer supporters often work with patients and/or health care providers to address system-level barriers, such as fragmented care, financial constraints, other practical challenges (e.g., transportation, employment concerns, child care), and communication difficulties [32,25]. PS programs in cancer have been shown to increase patient satisfaction; improve psychological adjustment, such as increased hope and decreased emotional distress; and increase skills and knowledge to cope with cancer, such as decision-making [22,31,33]. Despite growing evidence on the effectiveness of PS programs [34], research is needed about how PS is being applied across the cancer care continuum, how PS is being delivered and for whom, and where opportunities exist for extending the reach and scope of PS.
Hence, the purpose of this scoping systematic review of recent literature is to characterize PS usage from primary prevention to end-of-life care among adult populations or families of adults affected by cancer (e.g., family caregivers). Our specific research questions are (as reflected in peer reviewed literature):
What are the areas in which PS is used in cancer prevention, early detection, and care?
To what extent and/or how is PS used to address disparities in cancer care?
Who are the peer supporters? (E.g., What relation do they have to participants? How are they employed?)
What are the characteristics of PS programs?
What are outcomes are examined by PS programs?
METHODS
Scoping systematic reviews are commonly used to convey the breadth and depth of a topic of study, summarize evidence, and identify gaps in existing literature [35]. There are a number of differences between scoping reviews and systematic reviews. First, while systematic reviews are often used to answer a specific question according to a fixed set of a priori factors, scoping reviews use broader approaches (i.e., incorporating a range of evidence) and have broader research questions [36]. As a result, scoping reviews can produce both in-depth and broad results [37]. Second, scoping reviews are designed to provide an overview of existing literature and often incorporate a range of study designs and articles without an assessment of quality [36]. Finally, scoping reviews are typically more iterative than systematic reviews. Search terms can be redefined and steps may be repeated to make sure that the literature is covered in a comprehensive way [37]. Although many scoping reviews are systematic, in some cases, researchers do not place strict limitations at the outset regarding search terms, identification of relevant studies, or study selection [37].
In line with other reviews of this type [38,39], our key steps for completing this review included: 1) identifying our research questions, 2) determining the search strategy, 3) pilot testing and refining our search strategy, 4) using eligibility criteria to select studies through title, abstract and full text review, 5) extracting data from selected articles to answer the research questions, and 6) summarizing the contributions and gaps based on the extracted data and recent literature. We created a written protocol to guide steps for completing the review. All members of the scoping review team had graduate level training, and a sub-group of four members (NB, VC, KE, SK) comprised the leadership team for the review.
Search Strategy
A comprehensive and systematic literature search was conducted in MEDLINE/PubMed, Scopus, and CINAHL to identify relevant articles published over the previous five years (January 1, 2011 through June 2, 2016). The literature search included Medical Subject Headings (MeSH), CINAHL Headings and related text and keyword searches, focusing on terms to describe PS roles used in the cancer care continuum. The research team and a cancer information librarian developed the search strategy; the librarian conducted the searches. Details of the search strategy are reported in the supplemental materials. A total of 3,789 articles were identified, of which 2,087 were non-duplicates.
Inclusion and Exclusion Criteria
Studies considered for our review had to include the provision of PS during one or more aspects of the cancer care continuum (prevention through end-of-life). Since our overarching goal was to characterize the application of PS in cancer, we included articles where the qualifications of peer supporters were, and were not, well defined. There was no minimum requirement on the number of interactions between a peer supporter and peer recipient. We included support groups led by a professional if they clearly stated that PS was a program objective, PS groups were led by peers, or some hybrid of the two. We excluded studies where support was provided solely by researchers or health care professionals with post-baccalaureate training serving in an employment capacity, such as nurses, social workers, physicians, dieticians, physical therapists, and mental health professionals (e.g., programs in which Cognitive Behavior Therapy was provided by psychologists or social workers were excluded). We also excluded 1) articles if we could not locate a copy to review, 2) articles in which no English version was available, 3) dissertations, and 4) conference proceedings. Since the goal of this review was to characterize the current field of PS, we included all studies regardless of study design.
Article Selection
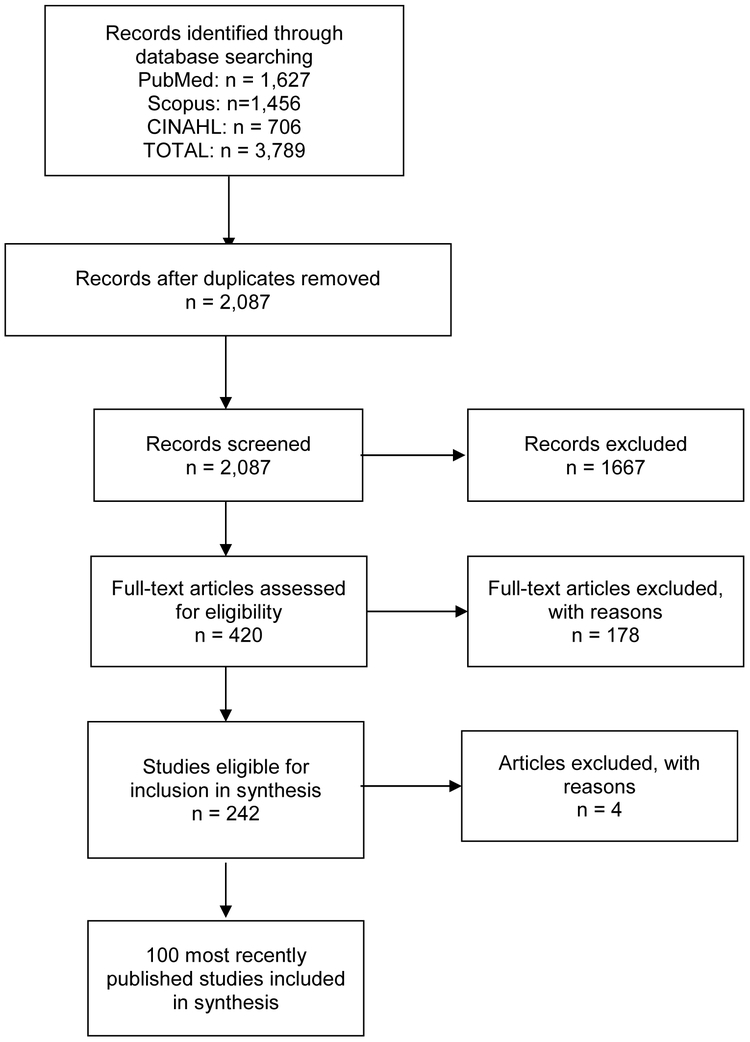
The online software program Covidence [40] was used to complete article screening. Pairs of research team members independently screened all titles and abstracts for inclusion. Titles and abstracts that lacked adequate information to determine inclusion or exclusion underwent a full-text review. A total of 1667 articles were excluded during the initial abstract screening phase. At the full-text review stage, each member of the research team independently reviewed each of the 420 remaining full-text articles for inclusion or exclusion based on the eligibility criteria. An additional 180 articles were excluded during the full text review phase, leaving 242 articles. During the data extraction phase, four additional articles were excluded for eligibility reasons, leaving 238 articles that met all eligibility criteria for inclusion in this study. Consistent with our goal to scope the existing literature to demonstrate the state of PS in cancer and disseminate in-depth and broad results, the study team then selected the 100 most recent articles for data extraction and summarization. This constituted then a broad sample with no apparent bias of the current literature on PS we sought to characterize, representing publication dates over a 2-year period, from June 2014 through May 2016. In addition, narrowing our time frame to the 100 most recent articles facilitated expeditious review of a broad range of literature in an in-depth manner—key goals of scoping reviews [37]. The disposition of articles is shown in Figure 1. A list of all included studies is in the supplemental materials.
Figure 1.
Prisma Flow Diagram
Categorization & Synthesis
Data were collected in the REDCap database [41] using a form that included information about the article citation, study characteristics (e.g., length of program, location, funding, program design), study design and setting, characteristics of study participants, types of cancers and outcomes in selected studies, and characteristics of PS programs. Eleven team members extracted information from the 100 articles. Reliability was assessed by having five members of the research team extract data from a sub-sample of articles assigned to the data extractors. In total, we assessed reliability on 10 articles (10% of the 100 identified articles) [42]. Our overall interrater reliability was 86.8%. Members of the leadership team worked in pairs to resolve conflicts through discussion and consensus and to determine article eligibility, where necessary.
RESULTS
Location and Participant Characteristics
As noted in Table 1, the majority of the PS programs were conducted in the United States (80%) and in urban settings (26%). Most often, programs included individuals from multiple racial/ethnic backgrounds, with a smaller percentage focused only on Black or African American populations (14%) or Latino/Hispanic populations (19%). In addition, most programs focused only on females (50%) or both males and females (39%), with few focusing only on men (7%). Few PS programs (2%) focused specifically on older adults (age 65 or older) and none focused only on younger adults (age 18-24).
Table 1.
Study Location and Sample Participant Characteristics
| Variable | Number of studies (%) |
|---|---|
| Location | |
| International | 16 (16.0) |
| US | 80 (80.0) |
| Both international and US | 2 (2.0) |
| Not reported or unclear | 2 (2.0) |
| Type of location | |
| Rural or frontier | 4 (4.0) |
| Urban | 26 (26.0) |
| Sub-urban | 2 (2.0) |
| Other | 1 (1.0) |
| Multiple types of locations | 4 (4.0) |
| Not applicable (outside of US or unclear) | 20 (20.0) |
| Not reported or unclear | 43 (43.0) |
| Race / Ethnicity (only among US articles) | |
| White | 2 (2.0) |
| Black or African American | 14 (14.0) |
| Asian | 5 (5.0) |
| Pacific Islander or Hawaiian Native | 0 (0) |
| American Indian or Alaska Native | 1 (1.0) |
| Latino / Hispanic | 19 (19.0) |
| Other | 2 (2.0) |
| Multiple races a | 28 (28.0) |
| Not applicable (outside of US) | 20 (20.0) |
| Not reported or unclear | 9 (9.0) |
| Gender | |
| Female | 50 (50.0) |
| Male | 7 (7.0) |
| Both | 39 (39.0) |
| Not reported | 4 (4.0) |
| Age | |
| Focused on young adults (18-24) | 0 (0) |
| Focused on adults, generally | 74 (74.0) |
| Focused on older adults (65+) | 2 (2.0) |
| Not reported or unclear | 24 (24.0) |
Of articles that included multiple races (n=28), most included 3 races (n=12, 12% of all studies) or 4 races (n=10, 10% of all studies).
PS Program Characteristics
Setting.
As shown in Table 2, many PS programs included multiple settings for intervention delivery (23%), with the most common combination being clinic and community-based (9% of all studies). In addition, many used only a community setting (14%) or included a community setting alongside other settings (30%). Few programs were delivered in only a faith-based location (3%) or included a faith-based component (6%).
Table 2.
Program Characteristics
| Variable | Number of studies (%) |
|---|---|
| Program setting for intervention delivery | |
| Clinic | 40 (40.0) |
| Community | 14 (14.0) |
| Faith-based location | 3 (3.0) |
| Home | 6 (6.0) |
| School | 0 (0) |
| University | 0 (0) |
| Worksite | 0 (0) |
| Other a | 3 (3.0) |
| Multiple b | 23 (23.0) |
| Not reported or unclear | 1 (1.0) |
| Not applicable (technology or phone-call based) | 10 (10.0) |
| Modality for intervention delivery | |
| In-person | 60 (60.0) |
| Technology | 2 (2.0) |
| Phone-call | 8 (8.0) |
| Multiple | 29 (29.0) |
| Not reported or unclear | 1 (1.0) |
| Cancer care continuum | |
| Prevention | 6 (6.0) |
| Screening | 37 (37.0) |
| Diagnosis (decision-making) | 4 (4.0) |
| Treatment | 13 (13.0) |
| Survivorship | 9 (9.0) |
| Palliative Care | 0 (0) |
| End-of-life Care c | 0 (0) |
| Multiple continuum foci d | 28 (28.0) |
| Not reported or unclear | 3 (3.0) |
| Cancer type | |
| Breast | 32 (32.0) |
| Prostate | 6 (6.0) |
| Lung e | 2 (2.0) |
| Colorectal | 16 (16.0) |
| Brain | 1 (1.0) |
| Gynecological | 11 (11.0) |
| Liver | 0 (0) |
| Cancer type, continued | |
| Skin | 1 (1.0) |
| Other f | 3 (3.0) |
| Multiple g | 23 (23.0) |
| Not reported or unclear | 5 (5.0) |
| Disparities discussed in stated purpose or hypotheses of program | |
| No | 34 (34.0) |
| Yes | 66 (66.0) |
| Type of disparity | |
| Race / ethnicity | 31 (31.0) |
| Gender | 0 (0) |
| Age | 0 (0) |
| Geographic location | 1 (1.0) |
| Socioeconomic status | 2 (2.0) |
| Other | 1 (1.0) |
| Multiple h | 31 (31.0) |
| Not applicable (disparity not discussed) | 34 (34.0) |
| Peer Training content/curriculum described in article | |
| No | 56 (56.0) |
| Yes | 44 (44.0) |
| Navigation included in program | |
| No | 45 (45.0) |
| Yes | 55 (55.0) |
| Person responsible for initial contact | |
| Peer supporter | 65 (65.0) |
| Recipient | 2 (2.0) |
| Both | 1 (1.0) |
| Not reported or unclear | 32 (32.0) |
| Formal certification requirement for peer supporters | |
| No | 91 (91.0) |
| Yes | 9 (9.0) |
| Use of theory i | |
| No | 27 (27.0) |
| Yes | 29 (29.0) |
| Not reported or unclear | 44 (43.0) |
| Peer supporters discussed as part of health care team | |
| No | 74 (74.0) |
| Yes | 26 (26.0) |
| Spirituality discussed | |
| No | 95 (95.0) |
| Yes | 5 (5.0) |
| Family involved | |
| No | 82 (82.0) |
| Yes, required inclusion | 4 (4.0) |
| Yes, invited inclusion | 14 (14.0) |
| Impacts on peer supporter discussed | |
| No | 96 (96.0) |
| Yes | 4 (4.0) |
Example: mail
The most common combination was 2 settings (n=18). Of these types of setting combinations, the most common combination was clinic-based and community-based (n=9, 9% of all studies).
Note, one article discussed treatment, survivorship, palliative care, and end-of-life care. Another article focused on every point of the continuum.
The most common combination was screening & diagnosis (n=11, 11% of all studies).
Note, 5 articles in total discussed lung cancer. However, 1 of these articles discussed lung cancer and esophageal and 2 of these articles discussed lung cancer and multiple other types of cancer.
Example: esophageal cancer.
The most common type of combination was breast and gynecological (n=9, 9% of all studies).
Most studies focused on two disparities (n=23), while 7 articles of articles focused on 3 disparities and 1 article focused on 5 disparities. The most common type of disparity combination was race/ethnicity and SES (n=17, 17% of all studies).
Variable refers to whether theories, models, or frameworks were seriously and substantively applied in the article (e.g., using constructs in program development, design, or evaluation).
Modality.
The majority of programs were delivered using multiple types of modalities (29%). Of those that used only one modality, the most common was in-person (60% of all studies). Few programs were delivered using only technology (i.e., online support groups, apps) (2%) or phone calls (8%). A substantial proportion (33%), however, used a phone component in addition to another modality.
Cancer care continuum.
Twenty-eight percent (28%) of PS programs focused on multiple points along the cancer care continuum. The most commonly addressed was screening, of which 37% focused only on screening and more than half (58%) included a screening component. Points on the continuum that received less attention were treatment (13%) and survivorship (9%). None focused only on palliative care or end-of-life care; however, two studies included palliative care or end-of-life care along with other cancer care continuum foci.
Type of cancers.
Many programs (23%) focused on multiples cancer types. Of these, the most common combination was breast and gynecological (9% of all studies). With regard to specific types of cancer, programs most frequently targeted breast cancer only (32%) or colorectal cancer only (16%). Few programs focused only on lung cancer (2%), however 5% of programs focused on lung cancer plus another cancer type. One percent (1%) of programs focused only on skin cancer and 4% of programs focused on skin cancer plus another cancer type.
Disparities.
Over half of programs (66%) identified a specific disparity to address (e.g., race/ethnicity, gender, age, geographic location, socioeconomic status, etc.). Of these, most addressed disparities involving race/ethnicity (31% of all studies) or multiple disparities, of which the most common combination was race/ethnicity and socioeconomic status (17% of all studies).
Training.
Forty-four percent of articles described the content or curriculum of peer supporters’ training.
Impacts on peer supporters.
Few programs focused on impacts of the PS program on peer supporters (4%). Of those that did, impacts described included a sense of connection (2% of all programs), understanding of cancer (2% of all programs), giving back (1% of all programs), and self-growth (1% of all programs).
Other programmatic characteristics.
Over half of studies (55%) described their intervention as a navigation program. In addition, 9% included a formal requirement for certified peer supporters, 26% noted that peer supporters were part of the health care team, and 18% of programs included a family member.
Study Characteristics
Length of PS contact.
It was difficult to differentiate the length of the overall study and the length of contact between peer supporters and recipients. Approximately half (47%) did not provide enough detail to ascertain how long peer supporters were in contact with recipients (Table 3). For the studies in which data were available (53%), most peer supporters were in contact with recipients for less than 1 month (20% of all studies); the remainder of studies reported contact between 1 month and 6 months (16% of all studies) or greater than 6 months (17% of all studies).
Table 3.
Study Characteristics
| Variable | Number of studies (%) |
|---|---|
| Length of peer support contact | |
| Less than 1 month | 20 (20.0) |
| Between 1 month and less than 6 months | 16(16.0) |
| Greater than 6 months | 17(17.0) |
| Not reported or unclear | 47 (47.0) |
| Study Design | |
| Randomized Controlled Trial | 26 (26.0) |
| Cluster-randomized Randomized Controlled Trial | 6 (6.0) |
| Quasi-experimental | 9 (9.0) |
| Other controlled triala | 2 (2.0) |
| Single group pre-post | 19(19.0) |
| Descriptive or observational | 30 (30.0) |
| Otherb | 4 (4.0) |
| Not reported | 4 (4.0) |
| Study Funding | |
| Federal | 37 (37.0) |
| Private (state or regional foundation) | 4 (4.0) |
| Private (national foundation) | 12(12.0) |
| State / local government | 4 (4.0) |
| Pharmaceutical | 0(0) |
| Other | 3 (3.0) |
| Multiple c | 27 (27.0) |
| Not reported | 13 (13.0) |
| Study Outcomes | |
| Recipient engagement in clinical care | 43 (43.0) |
| Behavioral risk | 2 (2.0) |
| Quality of life | 0(0) |
| Mental health | 0(0) |
| Other psychosocial outcomes d | 8 (8.0) |
| Cancer progression and other clinical outcomes | 0(0) |
| Othere | 4 (4.0) |
| Multiple f | 40 (40.0) |
| Not reported | 3 (43.0) |
Examples: “Cluster-randomized at clinic level, randomized at individual level” and “group-randomized trial with nested cohort design”
Examples: “Simulation” or “multiple types of study designs”
The most common type of funding combination was federal and private (n=11, 11% of all studies).
Examples: appraisal, self-efficacy, social support, attitudes, optimism, intentions, knowledge)
Examples: “cost”, “feasibility or process evaluation outcomes”, “sexual function”, etc.
The most common type of combination was recipient engagement in clinical care and psychosocial outcomes (n=16, 16% of all studies).
Study design and outcomes.
Since the goal of this review was to characterize the current field of PS, we included all studies regardless of study design. Studies were primarily descriptive or observational (30%), randomized controlled trials (26%) or single group pre-post (19%). Studies reported a variety of outcomes, most frequently recipient engagement in clinical care only (43%) or multiple types of outcomes (40%). Eight percent of studies included mental health outcomes in addition to other outcomes and 35% of studies included other psychosocial outcomes alongside other outcomes. However, no study focused only on mental health outcomes and very few focused only on other psychosocial outcomes, such as self-efficacy, social support, attitudes, appraisal, or optimism (8%).
Program Activities and Support
Peer supporters used a variety of tools to engage with recipients, including counseling or motivational interviewing (18% of programs used only counseling or motivational interviewing, while 36% included these alongside other tools), pamphlets (14% used only pamphlets, while 33% included them alongside other tools), or a combination of tools (25%), of which the most common combination was pamphlets and counseling (9%) (see Table 4). Similarly, most programs reported offering multiple types of support to recipients (71%), the most common combination of which was informational, emotional, and behavioral support (18% of all studies). In addition, peer supporters were most likely to interact individually with recipients (65%) or use multiple modes, such as individual and group interactions. While many articles (48%) did not report how peer supporters were affiliated with the PS program, 19% did report that peer supporters were volunteers.
Table 4.
Peer supporter activities, interactions, support, and affiliations
| Variable | Number of studies (%) |
|---|---|
| Tools used by peer supporters | |
| Pamphlets / print materials | 14 (14.0) |
| Videos | 1 (1.0) |
| Counseling / motivational interviewing | 18 (18.0) |
| Support groups | 3 (3.0) |
| Other a | 3 (3.0) |
| Multiple b | 25 (25.0) |
| Not reported | 36 (36.0) |
| Types of support provided by peer supporters | |
| Informational support | 22 (22.0) |
| Emotional support | 3 (3.0) |
| Behavioral support | 1 (1.0) |
| Tangible support | 1 (1.0) |
| Shared activity | 0 (0) |
| Medical appointment support | 0 (0) |
| Other | 0 (0) |
| Multiple c | 71 (71.0) |
| Not reported | 2 (2.0) |
| Types of peer supporter interactions | |
| Individually | 65 (65.0) |
| Group | 9 (9.0) |
| Family | 0 (0) |
| Caregiver | 0 (0) |
| Other d | 3 (3.0) |
| Multiple e | 19 (19.0) |
| Not reported | 6 (6.0) |
| PS affiliations with program | |
| Volunteer | 19 (19.0) |
| Program recipient | 1 (1.0) |
| Regular staff | 17 (17.0) |
| Paid part-time staff / stipend | 6 (6.0) |
| Student | 1 (1.0) |
| Other | 3 (30) |
| Multiple f | 5 (5.0) |
| Not reported | 48 (48.0) |
| PS affiliations with participant | |
| Family member / partner | 0 (0, 0) |
| Friend or buddy | 0 (0, 0) |
| Fellow program recipient | 1 (1.0) |
| Work (co-workers) | 0 (0) |
| Church | 3 (3.0) |
| No connection | 57 (57.0) |
| Other | 4 (4.0) |
| Multiple g | 5 (5.0) |
| Not reported | 30 (30.0) |
Examples include: flip charts, interactive multimedia, and slide presentations.
Most common type of combination of tools was pamphlets and counseling (n=9, 9% of all studies).
Most common type of combination of types of support provided was informational, emotional, and behaviors (n=18, 18% of all studies), followed by tangible support and medical appointments (n=15, 15% of all studies).
Examples include: online interactions.
Most common type of combination of interactions was individual and group (n=9, 9% of all studies).
Most common type of combination of affiliation with program was regular staff and part-time (n=2, 2% of all studies).
Most common type of combination of affiliation with participant was family & friend (n=1, 1% of all studies), family & fellow program recipient (n=1, 1% of all studies), fellow program recipient & other (n=1, 20%), work & church (n=1, 1% of all studies), church & other (n=1, 1% of all studies).
DISCUSSION
The results from this review reflect an extensive and varied breadth of literature reporting on the use of PS across the cancer care continuum. Many PS programs addressed breast and colorectal cancer screening and treatment, which may be driven by incidence rates, public attention to these specific cancer types, funding priorities, and availability of evidence-based screening modalities. Results suggest the need to apply PS strategies to cancer types other than breast and colorectal cancers. In addition, few programs focused solely on men or the provision of PS at late stages in cancer care (i.e., palliative care and end-of-life). Many interventions in this review sought to address racial or ethnic disparities in cancer outcomes. Given the effectiveness of PS interventions in reaching underserved and minority populations [43], continuing to promote PS to address racial disparities across the cancer continuum is warranted. Despite the important, yet challenging, work of peer supporters, few programs examined the positive or negative impact of providing PS on individuals who fill this role. Attention to the wellbeing of peer supporters is essential for both program quality and sustainability.
Types of Cancer
While the volume of peer support appears to be driven by cancers that have received public attention (e.g., breast cancer and colorectal cancer) and where screening modalities are available, this review highlights the need to better disseminate peer support methods and practices to other cancer types, especially those cancers that may carry a stigma, such as lung cancer. Indeed, we found only two papers focused on lung cancer, which is the leading cause of cancer death [1]. Strikingly, this finding aligns with a 2008 systematic review of peer support programs for people with cancer, in which the authors found no examples of peer support programs for lung cancer [22].
Gender
Men in the United States are more likely than women to engage in a number of behaviors that increase their cancer risk26 and die from cancer [44]. However, few PS programs in our review neither focused on men nor the cancers most common among men. Conversely, 50% of studies focused only on women and 32% only on breast cancer – the most common cancer among women. Researchers have argued that gender – which refers to differences that stem from cultural and social origins vs. biological factors – is an important factor to consider when designing health programs [45]. Sensitivity to the influence of gender on behavioral and psychosocial factors across the cancer care continuum could increase the applicability of and engagement in PS programs.
Psychosocial Issues
Our review found that only 35 of the 100 PS programs included psychosocial issues as outcomes. Among eight articles that solely focused on psychosocial study outcomes, none of them covered the cancer care continuum periods of treatment, palliative care, or end-of-life care. The psychosocial challenges associated with a cancer diagnosis and treatment are complex and vary by characteristics of an individual, their families, and environment [46]. Psychosocial issues may include trouble coping with illness, family and social isolation, quality of life concerns, problems with treatment decisions, and end-of-life issues [47]. Research suggests that peer supporters are uniquely positioned to complement formal support provided to patients, given the non-hierarchical, reciprocal relationship between patients and peer supporters [48].
Palliative Care and End-of-Life Care
A striking feature of the review was that only two PS programs addressed palliative or end-of-life care. Indeed, to our knowledge, there are few examples of peer support programs designed to provide palliative or end-of-life care for cancer patients, although some examples exist for other conditions [49], such as end-of-life care for dialysis patients [50]. The distress surrounding pain and symptom management and death and dying are significant issues that impact both cancer patients and their families [51]. Hence, the potential contribution of PS for those with advanced cancer and their families or friends would seem to be substantial, especially given observations of the central contribution of emotional support from PS even when it is not an emphasized part of protocols [25,52]. Opportunities for PS in palliative and end-of-life care could include a) attention to end-of-life issues that otherwise may be avoided until loss is imminent, b) support for family members coming to terms with loved ones’ worsening health, and c) PS for establishing relationships with palliative care providers soon after diagnosis that continue throughout the course of disease.
Addressing Disparities
The majority (66%) of PS programs reviewed focused on at least one historically marginalized population experiencing a disproportionate burden of cancer mortality—most often disparities by race or ethnicity. For these populations, the provision of cancer care can often be inaccessible, overwhelming, unaccepting, or untrustworthy [53,54]. Moreover, the use of PS to address factors that influence disparities is likely based on the idea of increasing patient agency [55] and decreasing social distance within these populations [56]. Approaches to increasing these populations’ agency include patient activation within the clinical environment and patient self-efficacy to manage one’s health. PS may also help address perceived and objective social distance between patients and their care team by decreasing providers’ implicit bias that has been shaped by our nation’s history of structural racism [56]. Future work should continue to examine how patients of color are impacted by PS interventions, and further examine the use of PS programs to address other types of disparities, including those concerning age, gender, and geographic location.
Impact on Peer Supporter
Only four articles [57-60] reported how peer supporters were impacted by their involvement in a PS program. Methodological issues, such as insufficient sample size of peer supporters or a general lack of focus on the impact of participation on those in the PS role could explain this gap. A focus on the impact of PS provision is warranted given the potential for both positive and negative impacts [61]. Offering PS may provide psychosocial benefits for those in the peer supporter role. Conversely, the psychological and emotional burden of guiding others who are struggling through illness might be tremendous, potentially worsening or contributing to health problems among peer supporters [62]. For peer supporters going through or recovering from their own health issues, the demands of their position may worsen or create new health problems [62]. Of the four studies that did examine the impact on peer supporters, self-growth and giving back were the most common impacts reported [57-60]. Findings from non-cancer related PS programs have shown improvements in confidence, self-esteem, and mental health among peer supporters [63]. Future work should examine the clinical, psychological, and emotional impact of PS programs on people providing PS across the cancer continuum and identifying approaches to improve self-care.
Study Limitations
Although meta-analysis typically errs on the side of exclusion in order to increase precision in statistical analysis, our scoping systematic review errs on the side of inclusion in order to capture the breadth of recent articles. One limitation of a scoping review, however, is our inability to determine the effectiveness of PS interventions across the cancer care continuum. Instead, this review details the implementation and content of such interventions. Additionally, although we single-coded the majority of included papers, the high percent-agreement from our reliability sample provides confidence in our overall conclusions. Moreover, given that we limited our review to the most recently published 100 studies, our findings are influenced by the speed of review and publishing (which differs by journal) as well as publication bias, the tendency for publication of studies with positive results. However, many published systematic reviews include fewer than 100 papers and limiting our sample allowed us to answer our research questions with comprehensive, in-depth findings. Finally, we did not assess quality of studies. Scoping reviews do not typically assess quality of studies [37,35] since they are not designed to weigh evidence or assess quality of evidence [36].
Clinical Implications
Individuals and their families face numerous challenges at each phase of the cancer care continuum. In addition to social workers and mental health professionals, peer supporters may be an alternative resource for cancer patients and their families who experience social or mental health distress. More broadly, they may promote engagement in all phases of the continuum, help patients understand and adhere to treatment and management plans, and also assist families and facilitate the support they provide. In the literature on PS in cancer care, it appears that peer supporters are underutilized in a number of important areas, including interventions targeting lung cancer, involving men, and focusing on palliative care and end-of-life issues. Future research should examine expanding the provision of PS across the cancer continuum, particularly as it relates to the gaps identified in this review, and assess and address the impact of providing PS.
Supplementary Material
Acknowledgments
Funding. Preparation of this manuscript was supported by Peers for Progress, Chapel Hill, NC; the Cancer Health Disparities Training Program (2T32CA128582-06) and UNC Center for Health Equity Research (for author KRE); the National Cancer Institute (NCI) Geographical Management of Cancer Health Disparities Programs, Region 1-South, (3P30CA138313-07S2); and the Lineberger Comprehensive Cancer Center (P30 CA016086) through an NCI Administrative Supplement to Strengthen NCI - Supported Community Outreach Capacity through Community Health Educators (CHEs) of the National Outreach Network (NON).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Research involving Human Participants. This research did not involve human participants.
Informed Consent. Since this research did not involve human participants, informed consent was not required.
Data. The authors have control of all primary data and would allow the journal to review the data if requested.
References
- 1.Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabe E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castaneda-Orjuela C, Catala-Lopez F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, TT GH, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Soreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabares-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M (2017) Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA oncology 3 (4):524–548. doi: 10.1001/jamaoncol.2016.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, Bannon F, Ahn JV, Johnson CJ, Bonaventure A, Marcos-Gragera R, Stiller C, Azevedo e Silva G, Chen WQ, Ogunbiyi OJ, Rachet B, Soeberg MJ, You H, Matsuda T, Bielska-Lasota M, Storm H, Tucker TC, Coleman MP (2015) Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 385 (9972):977–1010. doi: 10.1016/s0140-6736(14)62038-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, Jemal A, Cho H, Anderson RN, Kohler BA, Eheman CR, Ward EM (2014) Annual Report to the Nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer 120 (9):1290–1314. doi: 10.1002/cncr.28509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vineis P, Wild CP (2014) Global cancer patterns: causes and prevention. Lancet 383 (9916):549–557. doi: 10.1016/s0140-6736(13)62224-2 [DOI] [PubMed] [Google Scholar]
- 5.Sabatino SA, White MC, Thompson TD, Klabunde CN (2015) Cancer screening test use-United States, 2013. MMWR Morbidity and mortality weekly report 64 (17):464–468 [PMC free article] [PubMed] [Google Scholar]
- 6.Freeman HP, Chu KC (2005) Determinants of cancer disparities: barriers to cancer screening, diagnosis, and treatment. Surgical Oncology Clinics 14 (4):655–669 [DOI] [PubMed] [Google Scholar]
- 7.Butow PN, Phillips F, Schweder J, White K, Underhill C, Goldstein D (2012) Psychosocial well-being and supportive care needs of cancer patients living in urban and rural/regional areas: a systematic review. Support Care Cancer 20 (1): 1–22 [DOI] [PubMed] [Google Scholar]
- 8.Coups EJ, Ostroff JS (2005) A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med 40 (6):702–711 [DOI] [PubMed] [Google Scholar]
- 9.Ligibel J (2012) Lifestyle factors in cancer survivorship. J Clin Oncol 30 (30):3697–3704 [DOI] [PubMed] [Google Scholar]
- 10.Pinto BM, Trunzo JJ (2005) Health behaviors during and after a cancer diagnosis. Cancer 104 (S11):2614–2623 [DOI] [PubMed] [Google Scholar]
- 11.Palmer NRA, Weaver KE, Hauser SP, Lawrence JA, Talton J, Case LD, Geiger AM (2015) Disparities in Barriers to Follow-up Care between African American and White Breast Cancer Survivors. Support Care Cancer 23 (11):3201–3209. doi: 10.1007/s00520-015-2706-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blank T, Graves K, Sepucha K, Llewellyn-Thomas H (2006) Understanding treatment decision making: contexts, commonalities, complexities, and challenges. Ann Behav Med 32 (3):211–217 [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez-Saenz de Tejada M, Bilbao A, Bare M, Briones E, Sarasqueta C, Quintana J, Escobar A (2016) Association of social support, functional status, and psychological variables with changes in health-related quality of life outcomes in patients with colorectal cancer. Psycho-Oncology 25 (8): 891–897 [DOI] [PubMed] [Google Scholar]
- 14.Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W (2014) Optimism, social support, and mental health outcomes in patients with advanced cancer. Psycho-Oncology 23 (3):299–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunault P, Champagne AL, Huguet G, Suzanne I, Senon JL, Body G, Rusch E, Magnin G, Voyer M, Réveillère C (2016) Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non-metastatic breast cancer patients. Psycho-Oncology 25 (5):513–520 [DOI] [PubMed] [Google Scholar]
- 16.Swider SM (2002) Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs 19 (1): 11–20 [DOI] [PubMed] [Google Scholar]
- 17.Andrews JO, Felton G, Wewers ME, Heath J (2004) Use of community health workers in research with ethnic minority women. J Nurs Scholarsh 36 (4):358–365 [DOI] [PubMed] [Google Scholar]
- 18.Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L Jr., Zhang X, Satterfield D (2007) Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med 32 (5):435–447. doi: 10.1016/j.amepre.2007.01.011 [DOI] [PubMed] [Google Scholar]
- 19.Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, Jack L Jr., Satterfield DW (2006) Effectiveness of community health workers in the care of persons with diabetes. Diabet Med 23 (5):544–556. doi: 10.1111/j.1464-5491.2006.01845.x [DOI] [PubMed] [Google Scholar]
- 20.Colella TJ, King KM (2004) Peer support. An under-recognized resource in cardiac recovery. Eur J Cardiovasc Nurs 3 (3):211–217. doi: 10.1016/j.ejcnurse.2004.04.001 [DOI] [PubMed] [Google Scholar]
- 21.Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, Walker DG, Bhutta Z (2007) Achieving child survival goals: potential contribution of community health workers. The Lancet 369 (9579):2121–2131 [DOI] [PubMed] [Google Scholar]
- 22.Hoey LM, Ieropoli SC, White VM, Jefford M (2008) Systematic review of peer-support programs for people with cancer. Patient Educ Couns 70 (3):315–337. doi: 10.1016/j.pec.2007.11.016 [DOI] [PubMed] [Google Scholar]
- 23.Postma J, Karr C, Kieckhefer G (2009) Community health workers and environmental interventions for children with asthma: a systematic review. J Asthma 46 (6):564–576. doi: 10.1080/02770900902912638 [DOI] [PubMed] [Google Scholar]
- 24.Fisher EB, Ballesteros J, Bhushan N, Coufal MM, Kowitt SD, McDnough M, Parada H, Robinette J, Tang P, Urlaub D, Sokol R (2015) Key features of peer support in chronic disease prevention and management. Health Aff (Millwood) 9. doi: 10.1377/hlthaff.2015.0365 [DOI] [PubMed] [Google Scholar]
- 25.Fisher EB, Ayala GX, Ibarra L, Cherrington A, Elder JP, Tang TS, Heisler M, Safford M, Simmons D (2015) Contributions of peer support to health, health care, and prevention: Papers from Peers for Progress. Ann Fam Med 13(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher EB, Boothroyd RI, Elstad EA, Hays L, Henes A, Maslow GR, Velicer C (2017) Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews. Clinical Diabetes and Endocrinology 3. doi: 10.1186/s40842-017-0042-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fisher EB, Coufal MM, Parada H, Robinette JB, Tang PY, Urlaub DM, Castillo C, Guzman-Corrales LM, Hino S, Hunter J (2014) Peer Support in health care and prevention: Cultural, organizational, and dissemination issues. Annu Rev Public Health 35:363–383 [DOI] [PubMed] [Google Scholar]
- 28.Ancker JS, Carpenter KM, Greene P, Hoffmann R, Kukafka R, Marlow LAV, Prigerson HG, Quillin JM (2009) Peer-to-peer communication, cancer prevention, and the internet: Workgroup discussion of peer-to-peer communication about primary and secondary prevention, Society of Behavioral Medicine, San Diego, CA, March 26, 2008. J Health Commun 14 (0 1):38–46. doi: 10.1080/10810730902806760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whop LJ, Valery PC, Beesley VL, Moore SP, Lokuge K, Jacka C, Garvey G (2012) Navigating the cancer journey: a review of patient navigator programs for Indigenous cancer patients. Asia-Pacific Journal of Clinical Oncology 8 (4) [DOI] [PubMed] [Google Scholar]
- 30.Maxwell AE, Jo AM, Crespi CM, Sudan M, Bastani R (2010) Peer navigation improves diagnostic follow-up after breast cancer screening among Korean American women: results of a randomized trial. Cancer Causes Control 21 (11): 1931–1940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meyer A, Coroiu A, Korner A (2015) One-to-one peer support in cancer care: a review of scholarship published between 2007 and 2014. European journal of cancer care 24 (3):299–312 [DOI] [PubMed] [Google Scholar]
- 32.Ayala GX, Ibarra L, Cherrington AL, Parada H, Horton L, Ji M, Elder JP (2015) Puentes hacia una mejor vida (Bridges to a better life): Outcome of a diabetes control peer support intervention. Ann Fam Med 13 Suppl 1:S9–17. doi: 10.1370/afm.1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campbell HS, Phaneuf MR, Deane K (2004) Cancer peer support programs—do they work? Patient Educ Couns 55 (1):3–15 [DOI] [PubMed] [Google Scholar]
- 34.Nesta Health Lab & National Voices (2015) Peer support: What is it and does it work? https://www.nationalvoices.org.uk/sites/default/files/public/publications/peer_support_-_what_is_it_and_does_it_work.pdf. Accessed Nov 20, 2017
- 35.Levac D, Colquhoun H, O'Brien KK (2010) Scoping studies: advancing the methodology. Implementation science : IS 5:69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB (2015) Guidance for conducting systematic scoping reviews. International journal of evidence-based healthcare 13 (3): 141–146. doi: 10.1097/xeb.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 37.Arksey H, O'Malley L (2005) Scoping studies: towards a methodological framework. International journal of social research methodology 8 (1): 19–32 [Google Scholar]
- 38.Gorman JR, Standridge D, Lyons KS, Elliot DL, Winters-Stone K, Julian AK, Weprin J, Storksdieck M, Hayes-Lattin B (2017) Patient-centered communication between adolescent and young adult cancer survivors and their healthcare providers: Identifying research gaps with a scoping review. Patient Educ Couns doi: 10.1016/j.pec.2017.08.020 [DOI] [PubMed] [Google Scholar]
- 39.Tucker CA, Martin MP, Jones RB (2017) Health information needs, source preferences and engagement behaviours of women with metastatic breast cancer across the care continuum: protocol for a scoping review. BMJ open 7 (2):e013619. doi: 10.1136/bmjopen-2016-013619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Covidence systematic review software [computer program] (2017). Melbourne, Australia. [Google Scholar]
- 41.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics 42 (2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hartling L, Hamm M, Milne A, Vandermeer B, Santaguida P, Ansari M, Tsertsvadze A, Hempel S, Shekelle P, Dryden D (2012) Validity and inter-rater reliability testing of quality assessment instruments. Agency for Healthcare Research and Quality (US) https://www.ncbi.nlm.nih.gov/books/NBK92293. Accessed Nov 27, 2017 [PubMed] [Google Scholar]
- 43.Sokol R, Fisher E (2016) Peer support for the hardly reached: A systematic review. Am J Public Health 106 (7):1308. doi: 10.2105/AJPH.2016.303180a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF (2011) Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomarkers Prev 20 (8): 1629–1637. doi: 10.1158/1055-9965.epi-11-0246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Griffith DM, Gunter K, Allen JO (2011) Male gender role strain as a barrier to African American men's physical activity. Health Educ Behav 38 (5):482–491. doi: 10.1177/1090198110383660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Institute of Medicine (US) Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting (2008) Meeting psychosocial health needs. The psychosocial needs of cancer patients in cancer care for the whole patient. National Academies Press (US), Washington (DC) [Google Scholar]
- 47.American Cancer Society (2015) Counseling services you may need. https://www.cancer.org/treatment/treatments-and-side-effects/emotional-side-effects/distress/counseling-services.html. Accessed Nov 27, 2017
- 48.Embuldeniya G, Veinot P, Bell E, Bell M, Nyhof-Young J, Sale JE, Britten N (2013) The experience and impact of chronic disease peer support interventions: a qualitative synthesis. Patient Educ Couns 92 (1):3–12. doi: 10.1016/j.pec.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 49.Herber OR, Johnston BM (2013) The role of healthcare support workers in providing palliative and end-of-life care in the community: a systematic literature review. Health & social care in the community 21 (3):225–235 [DOI] [PubMed] [Google Scholar]
- 50.Perry E, Swartz J, Brown S, Smith D, Kelly G, Swartz R (2005) Peer mentoring: a culturally sensitive approach to end-of-life planning for long-term dialysis patients. Am J Kidney Dis 46 (1): 111–119 [DOI] [PubMed] [Google Scholar]
- 51.Bevans M, Sternberg EM (2012) Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA 307 (4):398–403. doi: 10.1001/jama.2012.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kowitt SD, Urlaub D, Guzman-Corrales L, Mayer M, Ballesteros J, Graffy J, Simmons D, Cummings DM, Fisher EB (2015) Emotional support for diabetes management: An international cross-cultural study. Diabetes Educ 41 (3). doi: 10.1177/0145721715574729 [DOI] [PubMed] [Google Scholar]
- 53.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H (2009) Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol 27 (31):5160–5167. doi: 10.1200/jco.2009.22.9773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guadagnolo BA, Cina K, Helbig P, Molloy K, Reiner M, Cook EF, Petereit DG (2009) Medical mistrust and less satisfaction with health care among Native Americans presenting for cancer treatment. J Health Care Poor Underserved 20 (1):210–226. doi: 10.1353/hpu.0.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O'Hair D, Villagran MM, Wittenberg E, Brown K, Ferguson M, Hall HT, Doty T (2003) Cancer survivorship and agency model: implications for patient choice, decision making, and influence. Health Commun 15 (2):193–202. doi: 10.1207/s15327027hc1502_7 [DOI] [PubMed] [Google Scholar]
- 56.Street R, Epstein RM (2008) Key interpersonal functions and health outcomes: Lessons from theory and research on clinician-patient communication In: Glanz K, Rimer BK, Viswanath K (eds) Health behavior and health education: theory, research, and practice. John Wiley & Sons. [Google Scholar]
- 57.Huntingdon B, Schofield P, Wolfowicz Z, Bergin R, Kabel D, Edmunds J, Penberthy S, Juraskova I (2016) Toward structured peer support interventions in oncology: a qualitative insight into the experiences of gynaecological cancer survivors providing peer support. Support Care Cancer 24 (2):849–856. doi: 10.1007/s00520-015-2853-z [DOI] [PubMed] [Google Scholar]
- 58.Mirrielees JA, Breckheimer KR, White TA, Denure DA, Schroeder MM, Gaines ME, Wilke LG, Tevaarwerk AJ (2015) Breast cancer survivor advocacy at a university hospital: Development of a peer support program with evaluation by patients, advocates, and clinicians. J Cancer Educ doi: 10.1007/s13187-015-0932-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mollica MA, Nemeth LS, Newman SD, Mueller M, Sterba K (2014) Peer navigation in African American breast cancer survivors. Patient Relat Outcome Meas 5:131–144. doi: 10.2147/prom.s69744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rafie C, Ayers A, Cadet D, Quillin J, Hackney MH (2015) Reaching hard to reach populations with hard to communicate messages: Efficacy of a breast health research champion training program. J Cancer Educ 30 (3):599–606. doi: 10.1007/s13187-014-0720-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rebeiro Gruhl KL, LaCarte S, Calixte S (2016) Authentic peer support work: challenges and opportunities for an evolving occupation. Journal of mental health (Abingdon, England) 25 (1):78–86. doi: 10.3109/09638237.2015.1057322 [DOI] [PubMed] [Google Scholar]
- 62.Miyamoto Y, Sono T (2012) Lessons from Peer Support Among Individuals with Mental Health Difficulties: A Review of the Literature. Clin Pract Epidemiol Ment Health 8:22–29. doi: 10.2174/1745017901208010022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schwartz CE, Sendor M (1999) Helping others helps oneself: response shift effects in peer support. Soc Sci Med 48 (11):1563–1575 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.