Abstract
Purpose
The purpose of this study was to evaluate the disparity between the preoperative target correction amount and the postoperative correction amount in open wedge high tibial osteotomy (OWHTO) in patients divided according to the planned osteotomy gap.
Materials and Methods
Seventy-two patients were divided into two groups (group 1 with the planned opening gap lager than the mean opening gap length of total patients and group 2 with a smaller opening gap). The opening gap was determined according to the target weight bearing line (WBL) ratio on the preoperative whole leg radiograph. Absolute and relative values of the disparity between the target and postoperative WBL ratios were compared between groups in order to clarify whether the disparity was deviated toward over- or under-correction.
Results
The absolute value of disparity between the target and postoperative WBL ratios in group 1 was significantly larger than that in group 2 (6.01%±5.68% vs. 3.32%±3.38%; p=0.02). However, there was no statistically significant difference in relative values between groups (p=0.54).
Conclusions
The postoperative WBL ratio after OWHTO was different from the preoperative target WBL ratio if the planned osteotomy gap was large. This mismatch was not deviated toward one side, either over- or under-correction.
Keywords: Knee, Osteoarthritis, Varus deformity, Osteotomy
Introduction
Medial open wedge high tibial osteotomy (OWHTO) is a good option for treatment of medial unicompartmental osteoarthritis1–3). For successful OWHTO, proper indication, analysis of the deformity, thorough planning, appropriate surgical technique, and postoperative management are mandatory4–6). Among them, thorough planning could be regarded as an essential factor because accurate correction could be obtained through precise planning and proper surgical technique. Several methods, such as those of Hernigou et al.7), Dugdale et al.8), and Miniaci et al.9), have been introduced for preoperative planning using a whole leg radiograph10,11). Recently, the navigation system and digital imaging methods have also been introduced for accurate assessment of the deformity and adjustment in preoperative planning for the real operation11–18). Additionally, the picture archiving and communication system (PACS) and Photoshop are used for direct measurement of the height of the osteotomy gap with high reliability and easy availability6).
Surgeons recommend that the osteotomy gap according to the planned correction amount should be adjusted intraoperatively based on the status of the medial compartment and the goal of the osteotomy in OWHTO19,20). Despite delicate preoperative planning and intraoperative adjustment, the postoperative correction amount could be different from that preoperatively planned21,22) It is because preoperative planning for OWHTO is mostly conducted in 2 dimensions, while correction of the varus deformity is a 3 dimensional task. We observed the tendency of mismatch between the preoperatively planned correction amount and the actual correction amount after OWHTO was more prominent when a large amount of correction was required. We suspected whether this may be due to the limitation of the 2 dimensional planning for the 3 dimensional procedure and associated with the surgical technique itself23).
The purpose of this study was to evaluate the disparity between the preoperative target correction amount and postoperative correction amount in OWHTO of patients divided into two groups according to the planned osteotomy gap. The hypothesis of this study was that the actual correction amount after OWHTO would be different from the preoperatively planned target correction amount if the planned osteotomy gap was large.
Materials and Methods
From March 2014 to January 2015, 72 biplanar OWHTO patients were enrolled in this retrospective analysis. This study was approved by our Institutional Ethics Committee, and the informed consents were obtained from all patients. The mean age of the patients was 57.6±5.5 years and there were 51 females and 21 males. All patients underwent OWHTO for treatment of medial unicompartmental osteoarthritis with a varus deformity. The status of the lateral compartment was checked on preoperative magnetic resonance imaging, physical examination, and intraoperative arthroscopic examination. Exclusion criteria were as follows: (1) secondary, such as post-traumatic arthritis, (2) OWHTO associated with ligament reconstruction, (3) bilateral OWHTO, (4) revision OWHTO, (5) double osteotomy including distal femoral osteotomy, and (6) absence of preoperative and postoperative standing radiograph taken in full extension because of the limitation of more than 5 degrees of extension in the knee joint.
1. Preoperative Planning and Intraoperative Adjustment of the Amount of Correction
The weight bearing line (WBL) ratio on the standing whole leg radiograph was used to determine the target amount of correction (postoperative 6 weeks)24). The INFINITT ver. 5.0.9.2 (INFINITT®, Seoul, Korea), which could measure automatically to 2 decimal places, was used for radiological measurements of the WBL ratio. The WBL was drawn from the center of the femoral head to the center of the superior articular surface of the talus. For calculation of the WBL ratio, the denominator was the width of the tibia, as measured using a ruler, and the numerator was the tibial intersection of the WBL (with medial tibial edge at 0% and the lateral tibial edge at 100%).
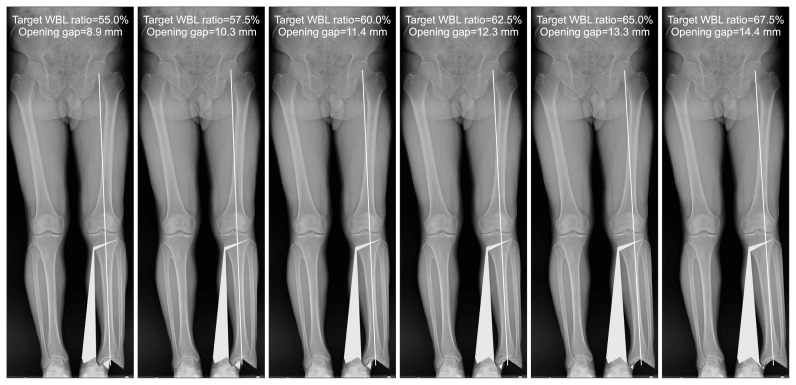
For the preoperative planning, the planned 55.0%, 57.5%, 60.0%, 62.5%, 65.0%, and 67.5% WBLs were drawn in the standing whole leg radiographs. First, a line extending from the center of the hip through the center of the knee and the ankle was drawn24). The second line (osteotomy line) was drawn from the starting point of the osteotomy (4 cm below the joint line) to the tip of the fibular head. The third line connecting the hinge point and the center of the ankle joint was drawn. The fourth line with the same length of the third line was drawn from the hinge point to the first line. The angle between the third and fourth lines was determined as a correction angle. The image was saved as a Joint Photographic Experts Group file and then transferred to Adobe Photoshop ver. 12.0 (AdobeTM, San Jose, CA, USA) and the distal portion of the osteotomy was rotated for correction and saved as a Digital Image Communication in Medicine file. The image was re-transferred to the measuring system and the height of the opening gap at the osteotomy site was measured at each target WBL ratio (Fig. 1).
Fig. 1.
Preoperative target weight bearing line (WBL) ratios (55.0%, 57.5%, 60.0%, 62.5%, 65.0%, and 67.5%) and the heights of opening gap at the osteotomy sites.
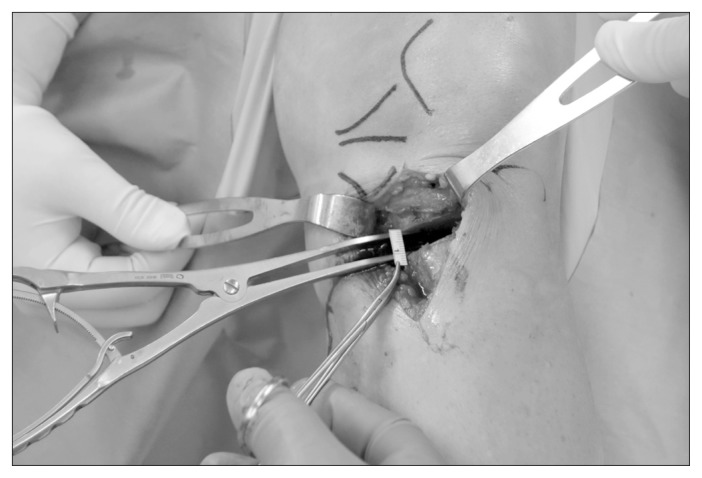
During the surgery, the target WBL ratio was determined according to the status of the medial compartment of the knee joint based on the surgeon’s subjective assessment between 55.0% and 67.5%. The amount of opening gap at the osteotomy site was determined based on the planned osteotomy gap for each WBL ratio (Fig. 1). Lesser amount of correction was performed if cartilage status of the lateral compartment was slightly bad or the osteotomy was performed for protection of the medial compartment after the procedure such as microfracture or meniscal root repair. Larger correction was usually performed if the medial compartment showed the kissing lesion of cartilage or obliteration of the medial joint space. Biplanar osteotomy was performed and distraction was performed at most posterior gap (Fig. 2)25).
Fig. 2.
The height of the opening gap was adjusted according to the preoperative plan and intraoperative status of the medial compartment.
All patients were divided into 2 groups according to the correction amount (group 1 with an opening gap larger than the mean height of the opening gap of total patients and group 2 with an opening gap smaller than the mean height of the opening gap of total patients). The difference between the preoperative target WBL ratio and postoperative WBL ratio measured at 6 weeks after surgery was compared between groups (Fig. 3). For clarification of under- or over-correction, relative and absolute valued were used in the comparison. Correlation analysis was also performed to evaluate the inaccuracy according to the amount of correction.
Fig. 3.

Radiographs of a 59-year-old male showing a difference of 5.3% between the preoperative target weight bearing line (WBL) ratio and postoperative WBL ratio (65.0%–59.7%).
2. Statistical Analysis
Statistical analysis was conducted using PASW Statistics ver. 18.0 (IBM Corp., Armonk, NY, USA). Student’s t-test was used to compare between groups. Pearson’s correlation analysis was performed to evaluate the accuracy of the preoperative planning according to the correction degree. The statistical significance was set at p<0.05. Two orthopedic surgeons measured all parameters twice with a 2–3 week interval. The reliability of the measurements was assessed by examining the intra-rater and inter-rater reliability using the intra-class correlation coefficient.
Results
The inter- and intra-observer reliabilities for the measurement of the WBL ratio were satisfactory and the mean values were 0.89 (range, 0.82 to 0.94) and 0.92 (range, 0.88 to 0.97), respectively.
The mean target WBL ratio was 62.5%±1.8% (range, 55.0% to 67.5%). The mean opening gap at the osteotomy site was 10.8±3.2 mm (range, 6 to 18 mm). This mean opening gap of 10.8 mm divided all patients into two groups (34 patients in group 1 and 38 patients in group 2). Preoperative demographics of the two groups are shown in Table 1.
Table 1.
Preoperative Demographics
| Group 1 | Group 2 | p-value | |
|---|---|---|---|
| No. of patients | 34 | 38 | |
| Age (yr) | 56.9±4.7 | 58.1±5.5 | 0.392a) |
| BMI (kg/m2) | 27.6±3.1 | 26.7±4.2 | 0.294a) |
| Sex (male/female) | 10/24 | 11/27 | 0.965b) |
| Side (left/right) | 16/18 | 18/20 | 0.979b) |
| Varus alignment (°) | 8.6±2.4 | 7.2±1.8 | 0.046a) |
| MPTA (°) | 85.1±2.7 | 85.9±2.4 | 0.387a) |
| Posterior tibial slope (°) | 9.2±1.2 | 10.1±2.7 | 0.247a) |
Values are presented as number only or mean±standard deviation. The statistical significance was set at p<0.05.
Group 1: opening gap larger than the mean height of the opening gap of total patients, Group 2: opening gap smaller than the mean height of the opening gap of total patients.
BMI: body mass index, MPTA: medial proximal tibial angle.
Derived from Student’s t-test.
Derived from Pearson chi-square test.
The difference of the absolute value between the target WBL ratio and postoperative WBL ratio was statistically significant between both groups (p=0.02). However, there was no statistically significant difference in relative values between both groups (p=0.54). Detailed differences between the target WBL ratio and postoperative WBL ratio are listed in Table 2.
Table 2.
Difference between Preoperative Target WBL Ratio and Postoperative WBL Ratio
| Group | Difference (%) | p-value | |
|---|---|---|---|
| Absolute value of difference in WBL ratio | 1 | 6.01±5.68 | 0.02 |
| 2 | 3.32±3.38 | ||
| Relative value of difference in WBL ratio | 1 | 2.13±8.10 | 0.54 |
| 2 | 1.19±4.62 |
Values are presented as mean±standard deviation. The statistical significance was set at p<0.05.
Group 1: opening gap larger than the mean height of the opening gap of total patients, Group 2: opening gap smaller than the mean height of the opening gap of total patients.
WBL: weight bearing line.
In the correlation analysis of absolute values, the correlation coefficient was 0.35, showing statistical significance (p<0.01). However, in the correlation analysis of relative values, the correlation coefficient was 0.11, showing no statistical significance (p=0.38).
Discussion
The principal finding of this study was that the difference between the target and postoperative WBL ratios showed statistical significance only in the absolute values, not in the relative values. Moreover, the differences in absolute values between the target and postoperative WBL ratios in group 1 were significantly larger than those in group 2. It could imply that disparity between the preoperative target WBL ratio and the postoperative WBL ratio could occur if the amount of correction was large. However, it was not deviated toward the side of either over- or under-correction.
Preoperative planning of OWHTO is performed for determination of the length of the opening gap for acquisition of the target valgus angle. Pape and Rupp11) reported that the difference of 10 mm in height of the osteotomy gap corresponds to the change of 8°–10° angulation in the alignment. The Fujisawa point26) is most commonly used and 62% point of the WBL ratio corresponds to the valgus angulation of 1°–3°. However, the target point should differ according to the status of the medial compartment. Our intraoperative target WBL ratio was variable according to the status of the medial compartment, but the mean target WBL ratio was similar to the Fujisawa point26).
Medial contracture and lateral laxity are usually encountered in the knee joint during OWHTO. Lateral subluxation of the proximal tibia is also commonly observed in the knee joint. Therefore, the medial collateral ligament is released or resected for prevention of high pressure on the medial compartment27). Based on our experience, it was assumed that the different ligament tension between the medial and lateral sides and tibial subluxation would be possible causes of the mismatch between the preoperatively planned and postoperative WBL ratios because the tendency was more prominent if the deformity was severer requiring a greater correction.
Postoperative limb alignment can be planned based on the anatomical alignment, mechanical alignment, or WBL ratio prior to OWHTO. Additionally, many surgeons still use an intraoperative radiopaque line such as the Bovie cable under the fluoroscopic guidance. However, previous studies reported significant differences among the methods. In a recent study, the cable-based method resulted in more unacceptable corrections than did the PACS image-based preoperative planning. It would be due to differences in the mechanical axis between radiographs taken in preoperative standing position and those obtained in supine position, which have been reported to be over 3 degrees. In this study, axial pressure was applied to the foot sole during intraoperative adjustment of the target axis, in which weight bearing was simulated in the supine position. Despite the effort, postoperative activity of muscles around the knee joint may have caused the difference between the intraoperative target alignment and the postoperative alignment.
Recently introduced digital planning software, such as mediCAD (Hectec GmbH, Landshut, Germany) and PreOPlan (Synthes, Zuchwil, Switzerland), has improved inter-rater reliability and correctness in preoperative planning and measurement of the limb alignment10). In this study, we did not use any planning program for preoperative planning, but PACS and Adobe Photoshop ver. 12.0 were used. PACS software was reported to have higher inter- and intra-observer reliability for evaluation of the lower extremity alignment28). However, the difference between the preoperative target amount of correction and postoperative amount of correction was noted in this study. This difference may have been caused by the fact that the planning was only performed based on the 2 dimensional evaluation of the WBL ratio, whereas correction of deformities involved 3 dimensional procedures based on the coronal and sagittal planes23,29). In the future, a 3 dimensional planning method would be required because the deformity of lower extremity is 3 dimensional.
There are some limitations that should be considered. First, this study was a retrospective study with a small number of patients; hence, a selection bias could have occurred. Second, only one planning method was used to assess the accuracy of planning; however, the reliability of the planning method was verified in previous research6). Third, the WBL ratio was examined only at the postoperative 6 weeks and serial change was not assessed. Serial assessment of the WBL ratio after OWHTO may have altered the distribution of two groups. Finally, the degree of preoperative varus deformity might have critically impacted the amount of opening gap at the osteotomy site. However, the difference in preoperative varus deformity was not considered in the classification of patient groups.
Conclusions
The postoperative WBL ratio after OWHTO was different from the preoperative target WBL ratio if the planned osteotomy gap was large. This mismatch was not deviated toward one side of either over- or under-correction.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90:1193–7. doi: 10.1302/0301-620X.90B9.20688. [DOI] [PubMed] [Google Scholar]
- 2.Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia--early results in 92 cases. Injury. 2003;34(Suppl 2):B55–62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Schröter S, Gonser CE, Konstantinidis L, Helwig P, Albrecht D. High complication rate after biplanar open wedge high tibial osteotomy stabilized with a new spacer plate (Position HTO plate) without bone substitute. Arthroscopy. 2011;27:644–52. doi: 10.1016/j.arthro.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Han SB, Bae JH, Lee SJ, Jung TG, Kim KH, Kwon JH, Nha KW. Biomechanical properties of a new anatomical locking metal block plate for opening wedge high tibial osteotomy: uniplane osteotomy. Knee Surg Relat Res. 2014;26:155–61. doi: 10.5792/ksrr.2014.26.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fan JC. Open wedge high tibial osteotomy: cause of patellar descent. J Orthop Surg Res. 2012;7:3. doi: 10.1186/1749-799X-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee YS, Lee BK, Lee SH, Park HG, Jun DS, Moon DH. Effect of foot rotation on the mechanical axis and correlation between knee and whole leg radiographs. Knee Surg Sports Traumatol Arthrosc. 2013;21:2542–7. doi: 10.1007/s00167-013-2419-x. [DOI] [PubMed] [Google Scholar]
- 7.Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–54. doi: 10.2106/00004623-198769030-00005. [DOI] [PubMed] [Google Scholar]
- 8.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;(274):248–64. [PubMed] [Google Scholar]
- 9.Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. 1989;(246):250–9. [PubMed] [Google Scholar]
- 10.Schröter S, Ihle C, Mueller J, Lobenhoffer P, Stöckle U, van Heerwaarden R. Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg Sports Traumatol Arthrosc. 2013;21:189–96. doi: 10.1007/s00167-012-2114-3. [DOI] [PubMed] [Google Scholar]
- 11.Pape D, Rupp S. Preoperative planning for high tibial osteotomies. Oper Tech Orthop. 2007;17:2–11. doi: 10.1053/j.oto.2006.09.007. [DOI] [Google Scholar]
- 12.Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:197–205. doi: 10.1007/s00167-012-2122-3. [DOI] [PubMed] [Google Scholar]
- 13.Bae DK, Yoon KH, Song SJ, Shin MC, Noh JH. Navigation versus radiographic measurements in the open-wedge high tibial osteotomy using computer assisted surgery (CAS) J Korean Orthop Assoc. 2008;43:301–7. doi: 10.4055/jkoa.2008.43.3.301. [DOI] [Google Scholar]
- 14.Hankemeier S, Hufner T, Wang G, Kendoff D, Zeichen J, Zheng G, Krettek C. Navigated open-wedge high tibial osteotomy: advantages and disadvantages compared to the conventional technique in a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2006;14:917–21. doi: 10.1007/s00167-006-0035-8. [DOI] [PubMed] [Google Scholar]
- 15.Lee DH, Nha KW, Park SJ, Han SB. Preoperative and postoperative comparisons of navigation and radiologic limb alignment measurements after high tibial osteotomy. Arthroscopy. 2012;28:1842–50. doi: 10.1016/j.arthro.2012.05.881. [DOI] [PubMed] [Google Scholar]
- 16.Schröter S, Günzel J, Freude T, Ateschrang A, Stöckle U, Albrecht D. [Precision in the planning of open wedge HTO]. Z Orthop Unfall. 2012;150:368–73. doi: 10.1055/s-0032-1314957. German. [DOI] [PubMed] [Google Scholar]
- 17.Akamatsu Y, Mitsugi N, Mochida Y, Taki N, Kobayashi H, Takeuchi R, Saito T. Navigated opening wedge high tibial osteotomy improves intraoperative correction angle compared with conventional method. Knee Surg Sports Traumatol Arthrosc. 2012;20:586–93. doi: 10.1007/s00167-011-1616-8. [DOI] [PubMed] [Google Scholar]
- 18.Gebhard F, Krettek C, Hüfner T, Grützner PA, Stöckle U, Imhoff AB, Lorenz S, Ljungqvist J, Keppler P AO CSEG. Reliability of computer-assisted surgery as an intraoperative ruler in navigated high tibial osteotomy. Arch Orthop Trauma Surg. 2011;131:297–302. doi: 10.1007/s00402-010-1145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852–61. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20:366–72. doi: 10.1016/j.arthro.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Yoon SD, Zhang G, Kim HJ, Lee BJ, Kyung HS. Comparison of cable method and miniaci method using picture archiving and communication system in preoperative planning for open wedge high tibial osteotomy. Knee Surg Relat Res. 2016;28:283–8. doi: 10.5792/ksrr.16.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim HJ, Lee HJ, Shin JY, Park KH, Min SG, Kyung HS. Preoperative planning using the picture archiving and communication system technique in high tibial osteotomy. J Orthop Surg (Hong Kong) 2017;25 doi: 10.1177/2309499016684701. 2309499016684701. [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Park J, Shin JY, Park IH, Park KH, Kyung HS. More accurate correction can be obtained using a three-dimensional printed model in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2018;26:3452–8. doi: 10.1007/s00167-018-4927-1. [DOI] [PubMed] [Google Scholar]
- 24.Lee YS, Lee BK, Kwon JH, Kim JI, Reyes FJ, Suh DW, Nha KW. Serial assessment of weight-bearing lower extremity alignment radiographs after open-wedge high tibial osteotomy. Arthroscopy. 2014;30:319–25. doi: 10.1016/j.arthro.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 25.Lee YS, Moon GH. Comparative analysis of osteotomy accuracy between the conventional and devised technique using a protective cutting system in medial open-wedge high tibial osteotomy. J Orthop Sci. 2015;20:129–36. doi: 10.1007/s00776-014-0663-7. [DOI] [PubMed] [Google Scholar]
- 26.Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 27.Jung WH, Takeuchi R, Chun CW, Lee JS, Ha JH, Kim JH, Jeong JH. Second-look arthroscopic assessment of cartilage regeneration after medial opening-wedge high tibial osteotomy. Arthroscopy. 2014;30:72–9. doi: 10.1016/j.arthro.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA, Pavlov H. Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc. 2011;19:1693–8. doi: 10.1007/s00167-011-1467-3. [DOI] [PubMed] [Google Scholar]
- 29.Kim HJ, Park J, Park KH, Park IH, Jang JA, Shin JY, Kyung HS. Evaluation of accuracy of a three-dimensional printed model in open-wedge high tibial osteotomy. J Knee Surg. 2018 doi: 10.1055/s-0038-1669901. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]