Abstract
Parents of children with developmental delays (DD) report elevated mental health difficulties compared to parents of children with typical development, which appear largely associated with child behavior problems. Latino parents of children with DD may experience heightened risk for poor mental health outcomes due additional stressors associated with minority status. Mindfulness-Based Stress Reduction (MBSR) appears to be efficacious for reducing parenting stress and improving wellbeing in families of children with DD; however, studies have rarely focused on families from racial and ethnic minority backgrounds. The current study employed a mixed-methods, waitlist-control design to examine the efficacy of MBSR for improving parent and child outcomes in Latino and non-Latino families. Results indicate that MBSR is similarly efficacious for Latino and non-Latino families in improving parent mental health (parenting stress, depressive symptomatology, and life satisfaction) and reducing parent-reported child behavior problems. Qualitative analyses further highlight avenues for improving the efficacy of MBSR for Latino families by providing intervention directly in Spanish, rather than using translation services, for Spanish-speaking families. Findings reveal the efficacy of standard MSBR for Latino parents of children with DD and underscore the potential benefits of disseminating this practice to traditionally underrepresented families.
Keywords: Latino, mindfulness, parenting stress, developmental delay, developmental disability, behavior problems
Parents of children with developmental delays (DD) in one or more core domains involving cognition, language, or social-emotional development are at increased risk for experiencing heightened and prolonged parenting stress compared to parents of children with typical development (Baker et al., 2003; Hauser-Cram et al., 2001) and this elevated stress is associated with negative outcomes for parents and children alike. Approximately one-third of parents of children with DD report clinically-elevated parenting stress (Davis & Carter, 2008); however, stress levels may be even greater for parents from racial and ethnic minority backgrounds due to additional stressors associated with minority status (Baum, Garofalo, & Yali, 1999). High levels of parental stress are also associated with other parent mental health concerns including parent depression (Hastings, Daley, Burns, & Beck, 2006) and lower parental well-being (Pisula, 2007). Despite recognition of the importance of addressing parent mental health in families of children with DD, and evidence that families from minority backgrounds may be at greater risk, few studies have focused on related interventions for Latino parents, one of the fastest growing minority demographics in the United States.
Children with DD are particularly vulnerable to developing behavior problems relative to children without DD (Baker, Blacher, Crnic, & Edelbrock, 2002; Emerson & Einfeld, 2010; Merrell & Holland, 1997). Child challenging behaviors appear to account for the relationship between developmental status and parenting stress in families of children with DD (Baker et al., 2002; Hauser-Cram & Warfield, 2001; Herring et al., 2006), and behavior problems are the most consistent predictor of parenting stress in this population (Tervo, 2012; Woodman, 2014). In turn, highly stressed parents of children with DD are significantly more vulnerable to parental depression (Hastings, Daley, Burns, & Beck, 2006), marital conflict (Kersh, Hedvat, Hauser-Cram, & Warfield, 2006), and poorer physical health (Eisenhower, Baker, & Blacher, 2009). Children with DD whose parents are highly stressed are at increased risk for behavior problems (Baker et al., 2003; Neece et al., 2012), poorer social competence (Guralnick, Neville, Connor, & Hammond, 2003; Neece & Baker, 2008), and later comorbid psychopathology (Baker, Neece, Fenning, Crnic, & Blacher, 2010). Targeting parenting stress may therefore represent a critical avenue for enhancing long-term child and family outcomes.
Stress among parents of children with DD has been proposed as an important target for intervention given its association with a variety of other parent mental health outcomes as well as child functioning. Several studies indicate that although there are individual differences in the course of parenting stress over time in families of children with DD, parenting stress generally peaks around the preschool period (i.e., 3–5 years) and decreases over time as a function of reductions in child behavior problems (Crnic, Arbona, Baker, & Blacher, 2009; Neece, Green, & Baker, 2012). Unfortunately, the presence of high levels of parenting stress may also mitigate the efficacy of early interventions designed to reduce child problem behaviors (Eldevik et al., 2009; Robbins, Dunlap, & Plienis, 1991; Strauss et al., 2012). Together, these results suggest that the preschool period may be a particularly impactful time to intervene with parenting stress in families of children with DD.
Although much remains to be learned about parent mental health, child outcomes, and associated stress reduction interventions for the broader population of families of children with DD, even less is known for families from minority backgrounds. To date, research has predominantly included samples characterized white, middle-class status (Cardoso, Padilla, & Sampson, 2010), with relatively limited attention devoted to racial, ethnic, and socioeconomic inclusivity. Studies focused on Latino parents specifically have yielded somewhat mixed results, depending upon the nature of outcomes assessed and the population under investigation. For example, Blacher et al. (1997) examined depressive symptomatology and found that Latina mothers endorsed elevated levels of depressive symptoms relative to national norms, and this was especially the case for Latina mothers of children with intellectual disability. A study of parenting stress revealed that Latina mothers of children with autism spectrum disorder and other developmental disabilities similarly reported clinically-elevated parenting stress, but tended to report less total stress than did non-Hispanic mothers of children with DD (Valicenti-McDermott et al. 2015). Finally, preliminary evidence suggests that interventions for reducing stress may be beneficial for Latino parents of children with DD. Results revealed that those who received a module that targeted depression and stress reported less caregiver burden (Magana et al., 2015), although parental stress was not measured directly. In sum, the relative dearth of research with this at-risk group of parents coupled with existing inconsistent findings suggest a clear need for studies that examine and measure parenting stress specifically among Latino families of children with DD.
The importance addressing parenting stress and related mental health considerations in Latino families is further underscored by evidence that Latino children with DD may be at greater risk for elevated behavior problems relative to non-Latino children, especially early in development (Baker et al., 2010; Flink et al., 2012). Marquis and Baker (2014) examined behavior problems in families of children with and without DD and found that Latina mothers reported higher levels of child internalizing behavior problems at age three relative to other mothers, but differences were no longer significant at child age five. Interestingly, although ethnic-group differences did not emerge in reported externalizing problems after controlling for socioeconomic status, Latina mothers reported a greater decrease in child externalizing behavior problems from age three to five than did other mothers. In contrast, Long et al. (2015) found that Latino children with DD were reported to have higher levels of both internalizing and externalizing problem behaviors compared to non-Latino children ages three to 18 years old. These findings highlight the importance of further clarifying the trajectory of child problem behaviors among Latino children with DD, and also emphasize the need to identify efficacious early intervention strategies to address parent and child outcomes.
Mindfulness-based stress reduction (MBSR, Kabat-Zinn, 2009) is the most well-established, empirically-supported stress-reduction intervention, with over three decades of extensive research demonstrating its efficacy in reducing stress, anxiety, and depression, and promoting overall well-being (Grossman & Nieman, 2004). MBSR was the intervention of choice for the current study because, of the mindfulness interventions that have been developed, MBSR is the most empirically supported approach with the greatest level of support within the DD literature (Bazzano et al., 2015; Chan & Neece, 2018; Dykens, Fisher, Taylor, Lambert, & Miodrag, 2014; Minor, Carlson, Mackenzie, Zernicke, & Jones, 2006; Neece, 2014; Roberts & Neece, 2015; Singh et al., 2006, 2007, 2014). Moreover, consistent with transactional models of family processes, emerging research indicates that MBSR may improve both parent and child outcomes in families of children with DD (Neece, 2014).
However, studies examining the efficacy of MBSR with ethnically and racially diverse samples are sparse. Two uncontrolled studies that included both Spanish- and English-speaking inner-city participants showed improvements in both adult medical and psychological symptoms, as well as self-esteem, following the completion of MBSR (Kabat-Zinn, 1994; Roth & Creaser, 1997). A subsequent controlled study revealed MBSR to be a feasible intervention for Spanish-speaking adults that resulted in significant reduction in physical and mental health symptoms (Roth & Robbins, 2004). Although these studies support initial feasibility and efficacy of MBSR with Latino populations, methodological limitations and a focus on adult outcomes reduce the ability to generalize findings to parents of children with DD.
The current study investigated the efficacy of MBSR for reducing parenting stress and depressive symptoms, and improving life satisfaction among Latino and non-Latino parents of young children with DD.
Further, given the transactional relationship between parenting stress and child behavior problems, we investigated whether MSBR with parents had a collateral benefit of improving parent-reported child behavior problems. The study employed a mixed-method design to examine change in parent and child outcomes using quantitative and qualitative measures. We also examined Latino parents’ recommendations for improving the intervention in order to optimize the efficacy of MBSR for this underrepresented population. Consistent with our previous work (Neece, 2014), we hypothesized that parents in the MBSR treatment group would report significant reductions in parenting stress and depression as well as improvement in life satisfaction compared to parents in the waitlist control. Further, we hypothesized that we would also find significant reduction in parent-reported child behavior problems in the MBSR group relative to the control group. Given the limited research investigating mindfulness interventions with Latino participants, we did not have a priori hypotheses about ethnic-group differences or treatment by ethnic-group interaction effects in predicting parent and child outcomes.
Method
Participants
The current study included 80 participants from the Mindful Awareness for Parenting Stress (MAPS) Project. Participants were parents of children, ages 2.5 to 5 years old, with developmental delay (DD). Families were primarily recruited through the Inland Regional Center, a government agency that provides services for all individuals with developmental disabilities in the Inland Empire region of Southern California. Families with children that met the study’s criteria were identified by the Inland Regional Center’s databases and received information regarding the MAPS Project through a mailing.
Criteria for inclusion were: 1) having a child aged 2.5 to 5 years, 2) child had been determined by Inland Regional Center (or by an independent assessment) to have DD, 3) parent reported more than 10 child behavior problems (the recommended cutoff score for determining risk of behavior problems) on the Eyberg Child Behavior Inventory (ECBI; Robinson, Eyberg, & Ross, 1980), 4) parent was not receiving any form of psychological or behavioral treatment at the time of referral, and 5) participant agreed to participate in the intervention. Exclusion criteria focused on factors that would limit child participation in parent-child interaction tasks that were part of the larger assessment protocol, including physical limitations that prevented child ambulation and the presence of significant cognitive delays due to concerns about task validity (Neece, 2014).
Table 1 depicts the demographics of the current sample. Of the 80 parents participating in the current study, 39 attended the immediate treatment group and 41 were part of the waitlist control group. In the combined sample, 71.25% of the children were boys. Parents identified 25% of the children as White, 47.50% as Latino, 3.75% as Asian, 2.50% as African American, and 21.25% as “Other.” Regarding parent ethnicity, 35.0% of parents reported being White, 46.3% being Latino, 8.8% being Asian, 3.8% being African American, and 6.3% being “Other.” The mean age of the children was 4.18 years. The majority of the participating parents were married (75.0%) and were mothers (96.3%). Families reported a range of annual income, with 25% reporting an annual income below the poverty line for San Bernardino County. Parents completed an average of 14.43 years of school, with a standard deviation of 2.89. In terms of language, 17.5% of the parents were monolingual Spanish speakers. There were no significant demographic differences between the treatment and control groups.
Table 1.
Demographic Characteristics of Participants by Treatment Group and Latino Status
| Treatment Group |
Latino Status |
|||||
|---|---|---|---|---|---|---|
| Treatment N = 39 |
Control N = 41 |
χ2 or t | Latino N = 37 |
Non-Latino N = 43 |
χ2 or t | |
| Children | ||||||
| Gender (% boys) | 66.7 | 75.6 | χ2(1)=0.78 | 75.7 | 67.4 | χ2(1)=66 |
| Mean Age in Years (SD) | 4.01 (0.94) | 4.34 (1.05) | t(78)=1.51 | 4.22 (1.02) | 4.15 (1.01) | t(78)=−.33 |
| Ethnicity (% White) | 28.2 | 32.0 | χ2(1)=0.42 | 0.0 | 46.5 | χ2(1)=22.95*** |
| Participating Parent | ||||||
| Mean Age in Years (SD) | 37.72 (8.38) | 36.76 (6.06) | t(79)=−0.58 | 36.62 (7.18) | 37.73 (7.31) | t(76)=.68 |
| Marital Status (% Married) | 82.1 | 68.3 | χ2(1)=2.02 | 59.5 | 88.4 | χ2(1)=8.87** |
| Mean Grade in School (SD) | 14.72 (3.10) | 14.15 (2.67) | t(100)=−0.89 | 12.97 (2.87) | 15.67 (2.27) | t(78)=4.70*** |
| Family Income (% > $25K) | 84.6 | 65.9 | χ2(1)=3.75 | 59.5 | 88.4 | χ2(1)=8.87** |
p < .01
p < .001
Parents also reported on their child’s current diagnosis. Sixty-four percent of the children in the study were reported to have a diagnosis on the autism spectrum. According to the Gilliam Autism Rating Scale (GARS; Gilliam, 1995), 61.4% of the children were reported to a “very likely” diagnosis of autism and the remaining had a “possible” diagnosis. At intake, 79.4% of children were enrolled in a special education classroom.
Regarding ethnic differences, Latino parents had fewer years of schooling (t = 4.70, p < .001), lower family income (χ2 = 8.87, p < .01), and were less likely to be married (χ2 = 8.87, p < .01) compared to non-Latino parents. Table 1 depicts the demographic differences between the Latino and Non-Latino subsamples.
Procedures
Parents interested in the MAPS Project completed a phone screen to determine the eligibility of the parent. If the parent met inclusion criteria, a baseline assessment was scheduled. At the baseline assessment, participants completed the informed consent followed by an interview to collect demographic information. Parents were then randomly assigned to the immediate treatment or waitlist-control group using simple random assignment (Neece, 2014). Data were collected across two waves of the MAPS Project. In the first wave, 17 parents were part of the immediate treatment group, and 18 parents were part of the waitlist control group; in the second wave, 22 parents were part of the immediate treatment group, and 23 parents were part of the waitlist control group. We had a relatively low attrition rate (n = 17; 21.25%), and parents were considered “drop-outs” if they informed research staff they no longer wished to participate or if they stopped attending MBSR groups and were non-responsive to research staff efforts to contact them. See Figure 1 for recruitment and attrition details.
Figure 1.
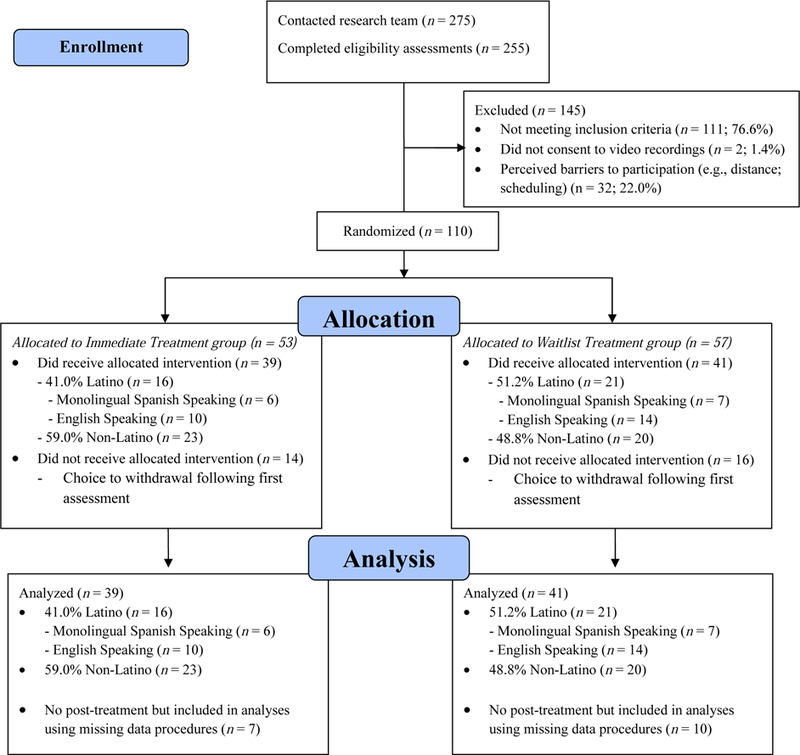
CONSORT Flow Diagram
Parents assigned to the immediate treatment group began MBSR following their baseline assessment and those assigned to the control group began three months after the immediate treatment cohort. The current study utilized standard MBSR (Kabat-Zinn, 2009). Given that this was an initial trial examining the efficacy of MSBR for Latino parents of children with DD, we did not make any modifications to the standard intervention in order to allow direct comparisons with prior MBSR trials and thereby permit us to draw clear conclusions about treatment benefits. The MBSR intervention consisted of three main components: (1) didactic material about the construct of mindfulness, the psychology and physiology of stress and anxiety, and ways that mindfulness can be utilized to facilitate more adaptive responses to challenges and distress, (2) mindfulness exercises during the group meetings and as homework between sessions, and (3) discussion and sharing in pairs and in the larger group (Kabat-Zinn, 2009). The intervention consisted of eight 2-hour weekly sessions, as well as one 6-hour retreat after session six and daily mindfulness tasks with audio CD instruction. Participants were instructed in formal mindfulness practices, including the body scan, sitting meditations, awareness of breath, mindful movements, and yoga. The instructor for the group had over 20 years experiencing practicing mindfulness and teaching MBSR, completed the Advanced MBSR Teacher Training at the University of Massachusetts Medical Center, and had received supervision with senior MBSR teachers through the Center for Mindfulness at the University of Massachusetts Medical Center.
To enable monolingual Spanish-speaking parents to participate, a professional translator was utilized in all our MBSR sessions and provided simultaneous translation services via headsets. The translator had over 20 years of experience providing translation in special education settings, as well as having extensive training in MBSR. All didactic materials (audio CDs and MBSR manuals) and questionnaires were offered to participants in both Spanish and English.
Two trained research assistants assessed treatment fidelity each session using a treatment fidelity checklist developed for this project, which quantified the number of items completed as anticipated per the manualized MBSR protocol as well as contact time reported in minutes (see Roberts & Neece, 2015 for details). Inter-rater reliability was high with 95.04% agreement between the two raters. In the immediate treatment group, 73.27% (SD 16.60) of the treatment content items were covered compared to 78.03% in the waitlist-control group 78.03 (SD 9.93; t [34] = −1.046,p = .305). Average contact time for the immediate treatment group was 143.40 (SD 74.68) and 141.75 (SD 76.17) for the waitlist-control group, t [34] = .065, p = .948.
Measures
Demographic data.
Demographic data were collected during an interview with the participating parent.
Parenting Stress Index - Short Form (PSI-SF).
The PSI-SF (Abidin, 1990) is a 36-item measure used to assess parental stress. Items are rated on a 5-point Likert scale ranging from 1 (Strongly Agree) to 5 (Strongly Disagree). The scale contains three subscales: Parental Distress, Parent-Child Dysfunctional Interaction and Difficult Child. The sum of the subscale scores comprises the Total Stress Score. The measure also includes a validity index that measures the level to which parents may be answering in a way that makes them look best. For the current study, we utilized the Parental Distress subscale, as this index measures parenting stress independent of child-behavior problems that are another major outcome in the present investigation. Parents completed the PSI-SF at the initial assessment and at their post-treatment assessment. Internal consistency for the Parental Distress scale of the PSI-SF for the current sample was high (α = .84).
Center for Epidemiological Studies - Depression (CES-D).
The CES-D (Radloff, 1977) was utilized to assess parental depressive symptoms. The scale is made up of 20 items related to mood, cognitive and somatic symptoms associated with depression. Total scores on the CES-D range from 0 to 60, with scores of 16 or above indicating clinical levels of depressive symptoms. The scale includes four subscales: Depressed Affect, Interpersonal Functioning, Positive Affect, and Somatic Symptoms. The total score was employed in the current study to evaluate parental depressive symptoms; internal consistency in the current sample was high (α = .88).
Satisfaction with Life Scale (SWLS).
The SWLS (Diener, Emmons, Larsen, & Griffin, 1985) is a brief, 5-item inventory designed to evaluate one’s overall satisfaction with life. Participants indicate on a 7-point Likert Scale the level at which they agree with five statements, such as “In most ways in my life is close to my ideal”. The measure has demonstrated sufficient psychometric properties (Diener et al., 1985; Pavot & Diener, 1993; Shevlin, Brundsden, & Miles, 1998), as well as strong internal consistency in the present sample (α = .87).
Child Behavior Checklist for ages 1.5–5 (CBCL).
The Child Behavior Checklist for Ages 1 ½ to 5 (CBCL; Achenbach & Rescorla, 2000) was used to assess child behavior problems. Parents rated the degree or frequency of 99 items on a scale of 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true). Each item represents a behavior problem, such as “acts too young for age” and “cries a lot.” In this study, we examined the four narrow-band scales that load onto the internalizing problems subscale (i.e., Emotionally Reactive, Depressed/Anxious, Somatic Complaints, and Withdrawn) and the two narrow-band scales that load onto the externalizing problems subscale (i.e., Attention Problems and Aggressive Behavior). We chose these subscales as our previous studies indicated that parent MBSR had specific effects on these individual child behavior problem sub-scales (Neece, 2014), and we were interested in whether these effects would hold for Latino families as well. In the current sample, internal consistency for the total problem score was excellent (α = .93). The CBCL also shows strong convergent validity with diagnoses based on DSM-IV-TR diagnostic criteria and similar scales measuring child behavior problems (Achenbach & Rescorla, 2000).
Participant Satisfaction Questionnaire.
At the last MSBR session, participants completed a final evaluation form created for this study, which consisted of 11 open-ended questions. These items were designed to elicit overall program and process feedback and to allow participants to express issues or comments that may not have been otherwise addressed.
Data Analyses
The study utilized convergent, evaluative, and expansion mixed-methods design elements (Aarons, Fettes, Sommerfeld, & Palinkas, 2012). The primary analytic strategy involved concurrent data collection with quantitative analysis hypothesis testing and simultaneous qualitative analysis (quant + qual). The evaluative design involved quantitative data to assess outcomes while qualitative data were used to evaluate process (QUAN → qual). Finally, qualitative data were used to explore unanticipated quantitative findings by thematically comparing response from Latino and non-Latino families. Qualitative group comparisons allows for identification of themes and patterns that are unique to one group or shared across both groups (Bernard, Wutich, & Ryan, 2016).
Quantitative Analyses.
As is often the case in clinical trials, particularly those focused on underrepresented populations, some data were missing post-treatment due to participant attrition (n = 17; 21.25%). To handle missing data, we employed an Intent-to-Treat framework (ITT; Chakraborty & Gu, 2009) by using multiple imputation (MI; Enders, 2010) to maximize inclusion of available data. All 17 participants who were lost at post-treatment were included in the quantitative analyses using these missing data analytic procedures. Accordingly, parameters on the following analyses were pooled based on 20 multiply imputed data sets. We examined the presence of outliers using Mahalanobis distance and found no outliers on any of our measures (all p > .001; Tabachnick & Fidell, 2013).
All analyses were conducted using SPSS software and thep-value was set to p < .05 for all tests. Independent sample t-tests were conducted to test for ethnic-group differences in all study variables at baseline. Hierarchical linear regressions were performed to examine whether the effects of MBSR on parental mental health outcomes (i.e., parenting stress, parental depression, and satisfaction with life) and parent-reported child behavior problems varied as a function of parents’ ethnic status (i.e., Latino or non-Latino). Each regression included a post treatment measure of parental mental health or parent-reported child behavior problems as a dependent variable. Additionally, demographic variables listed in Table 1 that had a significant relationship (p < .05) with one or more of the independent variables and one or more of the dependent variables were entered as covariates in the analyses (i.e., marital status for analyses predicting parenting stress and satisfaction with life, as well as family income for the analysis predicting life satisfaction). To control for potential effects of exogenous child intervention, parent report of child in-home intervention services was also entered as a covariate when predicting change in parent-reported child behavior problems. Demographic covariates were entered on Step 1, the pre-treatment score for the relevant parental mental health or parent-reported child behavior problem variable was entered on Step 2, treatment group was entered on Step 3, parents’ Latino status (i.e. Latino vs. non-Latino) was entered on Step 4, and a treatment group x Latino status interaction term was entered on Step 5. By controlling for pre-treatment levels of each variable, we were able to examine how changes in parental mental health were related to treatment group, Latino status, or the interaction between the two.
Qualitative Analyses.
Qualitative data were collected from all participants using open-ended questions on the end-of-program evaluation and were analyzed using content analysis methods. Immersion in and reflection upon the data allowed for identification of recurring and salient themes and patterns. The initial themes were analyzed for summary and interpretation (Berg, 2009; Corbin & Strauss, 2008). After data analysis was completed, two independent raters reviewed the themes to validate the coherence and adequacy of explanatory summaries. The coding was then revised and the themes were finalized.
Results
Independent sample t-tests were conducted for all variables of interest to determine whether any ethnic-group differences existed in the variables at baseline across the treatment groups (see Table 1). No ethnic-group differences were found in parental mental health variables (i.e., PSI-SF, CES-D, and SWLS). Participants reported high levels of parenting stress at baseline, with over half of parents (58%) experiencing “clinical” levels of stress on the Parental Distress subscale of the PSI-SF (greater than the 90th percentile) and 14.8% reported “high” levels of parenting stress (85–89th percentile; Abidin, 1990). Among the CBCL subscales, ethnic-group differences were found only for the Anxious/Depressed subscale wherein Latino parents rated their children as having significantly higher Anxious/Depressed problems (M = 5.27, SD = 2.55) compared to ratings by non-Latino parents (M = 4.05, SD = 2.78, p < .05, d = 0.46). Descriptive statistics at baseline are summarized in Table 2. Data met all necessary assumptions for linear regression. Specifically, examining scatterplots of residuals of each IV with the DVs revealed homoscedasticity of residuals, index plots revealed non-independence of residuals, and the Normal Q-Q plot revealed normality of residuals.
Table 2.
Means and SDs for Variables of Interest at Baseline
| Latino (n = 37) | Non-Latino (n = 43) | t | d | |
|---|---|---|---|---|
| Parental Mental Health | ||||
| PSI-SF | 39.00 (9.17) | 36.32 (7.96) | −1.37 | 0.31 |
| CES-D | 19.51 (9.88) | 17.25 (10.86) | −0.94 | 0.22 |
| SWLS | 20.60 (6.11) | 21.28 (7.14) | 0.44 | −0.10 |
| CBCL Subscales | ||||
| Emotionally Reactive | 5.95 (3.23) | 5.61 (3.56) | −0.44 | 0.10 |
| Anxious/Depressed | 5.27 (2.55) | 4.05 (2.78) | −2.02* | 0.46 |
| Somatic Complaints | 4.32 (2.78) | 4.78 (3.57) | 0.62 | −0.14 |
| Withdrawn | 6.73 (2.64) | 5.68 (2.41) | −1.83† | 0.42 |
| Attention Problems | 5.14 (2.36) | 6.00 (2.56) | 1.55 | −0.35 |
| Aggression | 19.46 (7.05) | 18.41 (7.56) | −0.63 | 0.14 |
Note. PSI-SF = Parenting Stress Index - Short Form. CES-D = Center tor Epidemiological Studies - Depression. SWLS = Satisfaction with Life Scale. CBCL = Child Behavior Checklist.
p < .10.
p < .05
Parental Mental Health Outcomes.
Quantitative Findings.
Results from a series of hierarchical linear regressions indicated a main effect for treatment group, but no main effect for Latino status or the interaction between treatment group and Latino status, for all three parent mental health outcome variables. Specifically, the immediate treatment group reported significant improvement in parenting stress, depressive symptoms, and life satisfaction at post treatment compared to the waitlist-control group. However, these effects did not differ by Latino status, suggesting that Latino parents reported benefited from the MBSR intervention to the same degree as non-Latino parents. Results are presented in Table 3.
Table 3.
Final Models of Parent Mental Health Outcomes Regressed onto Treatment Group, Latino Status, and the Interaction between Treatment Group and. Latino Status
| b | SE | 95% CI (b) | β | sr2 | |
|---|---|---|---|---|---|
| PSI Parental Distress Subscale | |||||
| Step 1: Marital Status | −1.06 | 2.17 | [−5.32, 3.19] | −0.05 | .00 |
| Step 2: Pre-Tx PSI-SF | 0 39*** | 0.12 | [0.16, 0.62] | 0.38 | .13 |
| Step 3:Treatment Group | −7.35** | 2.43 | [−12.13, −2.57] | −0.42 | .09 |
| Step 4: Latino Status | −0.90 | 2.40 | [−5.60, 3.80] | −0.05 | .00 |
| Step 5: Treatment x Latino | 1.03 | 3.36 | [−5.56, 7.62] | 0.05 | .00 |
| CES-D Total Depression Scale | |||||
| Step 1: Pre-Tx CESD | 0.24† | 0.13 | [−0.01, 0.48] | 0.23 | .05 |
| Step 2:Treatment Group | −7.56* | 3.58 | [−14.63, −0.50] | −0.35 | .06 |
| Step 3: Latino Status | 1.86 | 3.12 | [−4.26, 7.98] | 0.09 | .00 |
| Step 4: Treatment x Latino | −3.95 | 4.97 | [−13.74, 5.84] | −0.15 | .00 |
| Satisfaction with Life Total Score | |||||
| Step 1: Marital Status | 1.98 | 1.46 | [−0.90, 4.86] | 0.14 | .02 |
| Step 2: Family Income | −1.15 | 1.23 | [−3.57, 1.27] | −0.09 | .01 |
| Step 3: Pre-Tx SWLS | 0.53*** | 0.09 | [0.35, 0.70] | 0.57 | .28 |
| Step 4:Treatment Group | 3.86* | 1.54 | [0.83, 6.90] | 0.32 | .06 |
| Step 5: Latino Status | 1.11 | 1.63 | [−2.09, 4.30] | 0.09 | .00 |
| Step 6: Treatment x Latino | −1.80 | 2.14 | [−6.00, 2.40] | −0.12 | .01 |
p < .10.
p < .05.
p < .01,
p < .001.
Note. Parameters are pooled based on 20 multiply imputed data sets. PSI-SF = Parenting Stress Index - Short Form. CES-D = Center for Epidemiological Studies - Depression. SWLS = Satisfaction with Life Scale.
Qualitative Findings:
Qualitative analyses of parents’ open-ended responses on the treatment evaluation form yielded two themes related to parental self-perceptions: self-perceptions of stress and self-perceptions of parenting. The themes and sub-themes were common across Latino and non-Latino participants. However, specific codes revealed nuances in the pattern of endorsement by group (see Table 4).
Table 4.
Summary of perceptions regarding the MAPS Project, by participant group.
| Theme Sub-theme |
Code | Latino (n = 20) | Non-Latino (n = 12) |
|---|---|---|---|
| Self-perception of parenting | n (%)a | n (%)a | |
| Changes in parenting | Positive changes in parenting | 18 (94.7) | 11 (91.7) |
| Self-perceptions of stress | |||
| Changes in stress level | Decreased stress levels | 17 (94.4) | 8 (100) |
| Change in response to stress | Mindful responses and improved coping with stress | 20 (95.2) | 8 (88.9) |
| Parents’ perceptions of child | |||
| Parents’ appraisal of child | Increased social skills and improved behavior | 13 (59.1) | 8 (72.7) |
| Noting child attributes | Affirmations | 4 (100) | 0(0) |
| Program Experience | |||
| Most helpful factor | Cognitive skills learned | 0(0) | 8 (66.7) |
| Mind-body connection | 19 (90.4) | 0(0) | |
| Shared experience | 2 (9.5) | 2 (16.7) | |
| Barriers | Schedule/time and health issues | 7 (70.0) | 6 (54.6) |
| Other (language and finances) | 2 (20.0)b | 0(0) | |
| Recommendations | Program in Spanish by Spanish speaking MBSR instructor | 4 (44.4) | 0(0) |
n = code frequency, % = code frequency/total number of codes within sub-theme.
Monolingual Spanish-speakers within the Latino group
Self-perceptions of stress.
Participants were asked what changes, if any, they had noticed in their stress levels. Both Latino and non-Latino participants indicated that their stress levels had decreased. Many participants added qualifiers to express how much their stress levels had changed, and further insightful reflective comments.
“My stress levels greatly decreased in many situations as my approach to these situations changed.” —Non-Latino participant.
Participants were also asked what, if anything, changed in how they responded to stress. Mindful responses (awareness of breathing, decreased reactivity, acting with awareness, being present in the moment) and improved coping (insight, application of mindfulness skills) were noted in the responses of Latino and non-Latino participants.
“I am more able to cope with stress after pausing, breathing and then moving forward.”—Latino participant.
“I learned to stop my stressful thoughts, to analyze them… see if they were worth worrying about or not.”—Monolingual Spanish-speaking Latino participant.
Self-perception of parenting.
Participants were asked what changes, if any, they had noticed in their parenting. All participants noted positive changes in their parenting. This included increased patience and calmness, more energy and engagement in parenting, having greater tolerance and understanding, as well as optimism and greater parenting confidence. Parents also expressed having a new awareness of small successes or improvements, rather than dwelling on inadequacies and setbacks.
“I am more calm… I have more patience.”—Monolingual Spanish-speaking Latino participant.
“… being more in-the-moment and savoring my time with him.”—Non-Latino participant.
Child Behavior Problems Outcomes.
Quantitative Findings.
Results from a series of hierarchical linear regressions indicated that there was a significant main effect of treatment group on parent-reported child attention problems, with the immediate treatment group identifying fewer difficulties post-treatment than the waitlist control. Results were marginally significant for problems related to emotional reactivity (p = .052) and withdrawal (p = .06), with the immediate treatment group again reporting fewer behavior problems than the waitlist control at post-treatment. There was also a significant main effect of Latino status in predicting parent-reported attention problems, and Latino status was marginally related to emotionally reactive problems (p = .08). Latino parents reported lower levels of child behavior problems on both subscales at post-treatment compared to non-Latino parents. Finally, the treatment group by Latino status interaction was not a significant predictor of parent-reported child behavior problems. Results are presented in Table 5.
Table 5.
Final Models of Child Behavior Problems Regressed onto Treatment Group, Latino Status, and the Interaction between Treatment Group and Latino Status
| b | SE | 95% CI (b) | β | sr2 | |
|---|---|---|---|---|---|
| Emotionally Reactive | |||||
| Step 1: Behavioral Services | −0.15 | 0.52 | [−1.18, 0.88] | -0.02 | .00 |
| Step 2: Pre-Tx CBCL ER | 0 78*** | 0.08 | [0.62, 0.93] | 0.79 | .60 |
| Step 3:Treatment Group | −1.47† | 0.76 | [−2.96, 0.02] | -0.22 | .03 |
| Step 4: Latino Status | −1.26† | 0.72 | [−2.68, 0.16] | -0.19 | .02 |
| Step 5: Treatment x Latino | 1.71 | 1.08 | [−0.42, 3.83] | 0.21 | .02 |
| Anxious/Depressed | |||||
| Step 1: Behavioral Services | 0.17 | 0.56 | [−0.93, 1.28] | 0.03 | .00 |
| Step 2: Pre-Tx CBCL AD | 0.68*** | 0.11 | [0.45, 0.90] | 0.67 | .42 |
| Step 3:Treatment Group | 0.03 | 0.76 | [−1.47, 1.53] | 0.01 | .00 |
| Step 4: Latino Status | −0.73 | 0.77 | [−2.24, 0.79] | -0.13 | .01 |
| Step 5: Treatment x Latino | −0.10 | 1.08 | [−2.22, 2.03] | -0.01 | .00 |
| Somatic Complaints | |||||
| Step 1: Behavioral Services | −0.45 | 0.52 | [−1.47, 0.56] | -0.08 | .01 |
| Step 2: Pre-Tx CBCL SC | 0.56*** | 0.08 | [0.40, 0.71] | 0.67 | .44 |
| Step 3:Treatment Group | −0.52 | 0.75 | [−2.00. 0.95] | -0.10 | .01 |
| Step 4: Latino Status | −0.29 | 0.69 | [−1.63, 1.06] | -0.05 | .00 |
| Step 5: Treatment x Latino | 0.12 | 1.00 | [−1.84, 2.07] | 0.02 | .00 |
| Withdrawn | |||||
| Step 1: Behavioral Services | −0.66 | 0.69 | [−2.02, 0.71] | -0.11 | .01 |
| Step 2: Pre-Tx CBCL WI | 0.47*** | 0.13 | [0.22, 0.73] | 0.41 | .14 |
| Step 3:Treatment Group | −1.56† | 0.85 | [−3.24, 0.11] | -0.27 | .04 |
| Step 4: Latino Status | 0.00 | 0.87 | [−1.71, 1.70] | 0.00 | .00 |
| Step 5: Treatment x Latino | 0.55 | 1.26 | [−1.92, 3.01] | 0.08 | .00 |
| Attention Problems | |||||
| Step 1: Behavioral Services | −0.09 | −0.45 | [−0.97, 0.80] | -0.02 | .00 |
| Step 2: Pre-Tx CBCL AT | 0.73*** | 0.09 | 0.56, 0.91] | 0.67 | .39 |
| Step 3:Treatment Group | −1 77** | 0.61 | [−2.97, −0.57] | -0.33 | .06 |
| Step 4: Latino Status | −1.18* | 0.60 | [−2.37, −0.003] | -0.22 | .02 |
| Step 5: Treatment x Latino | 1.05 | 0.87 | [−0.65, 2.74] | 0.16 | .01 |
| Aggression | |||||
| Step 1: Behavioral Services | −0.77 | 1.50 | [−3.71, 2.17] | -0.05 | .00 |
| Step 2: Pre-Tx CBCL AG | 0 71*** | 0.11 | [0.51, 0.92] | 0.67 | .40 |
| Step 3:Treatment Group | −1.40 | 2.11 | [−5.56, 2.76] | -0.09 | .00 |
| Step 4: Latino Status | −1.55 | 1.91 | [−5.30, 2.19] | -0.10 | .01 |
| Step 5: Treatment x Latino | 2.18 | 2.87 | [−3.46, 7.82] | 0.11 | .01 |
p < .10.
p < .05.
p < .01.
p < .001.
Note. Parameters are pooled based on 20 multiply imputed data sets. CBCL ER - CBCL Emotionally Reactive. CBCL AD - CBCL Anxious/Depressed, CBCL SC-CBCL Somatic Complaints, CBCL WI-CBCL Withdrawn, CBCL AT-CBCL Attention Problems, CBCL AG-CBCL Aggression
Qualitative Findings.
Qualitative analyses of parents’ open-ended responses on the treatment evaluation form revealed one overarching theme related to parental perceptions of their child, with two sub-themes: parental appraisal of the child and parental acknowledgement of child attributes (see Table 4). The pattern of endorsement for parental appraisal of their child was consistent across both groups whereas affirmation of the child’s attributes was unique to the Latino group.
Parents ‘ perceptions of child.
When asked what changes, if any, parents had noticed in their child over the course of the program, the majority noted increased social skills and improved challenging behavior. Many parents also remarked on their child’s increased communication.
“I noticed that he was more calm, and I saw him be more social with other children his age.”—
Monolingual Spanish-speaking Latino participant.
“His behavior is so much better and others have noticed across the board.”—Non-Latino participant. However, the pattern of endorsement varied between ethnic groups. Non-Latino participants noted increased social skills and improved problem behavior equally, while Latino participants commented on increased social skills more often than improved challenging behavior. Within the Latino group, the monolingual Spanish-speaking Latino participants noted improved challenging behavior more frequently than increased social skills. Some monolingual Spanish-speaking participants also responded with acknowledgements of their child’s attributes with positive affirmations. This striking sub-theme difference that only appeared within the Latino group.
“My son is a love, he’s my good lucky charm, he’s very calm and I know that he’s capable to do a lot more than what I thought.”—Latino participant.
Intervention Process Evaluation.
Parents provided overwhelmingly positive evaluations of the overall treatment. Comparing non-Latino and Latino parents, some differences were noted in terms of participants’ experiences and treatment recommendations (see Table 4). Participants were asked what was most helpful about the program. Latino parents most commonly noted the benefits of learning to utilize the mind-body connection whereas non-Latino parents tended to emphasize the cognitive understanding they developed regarding the stress process and mindfulness attributes. A less common, but salient benefit, noted across groups was a sense of shared experience due to connecting with other parents who have children with DD and similar stressors.
““I am aware when I start to feel stress and I am abele to not explode but I’m able to breath and think.” Latino participant.
“Being able to focus more and learn how to be aware of the good moments and put the bad ones in the proper perspective.”— Non-Latino participant.
Participants reported experiencing minimal barriers to accessing and persisting in treatment. Of those parents who noted some difficulties with treatment engagement, the most common obstacles noted by both Latino and non-Latino participants related to scheduling considerations, time commitments, and personal or family health issues. Monolingual Spanish-speaking Latino participants also identified barriers related to language and the financial cost of transportation. Both monolingual and bilingual Latino participants expressed a preference to have the program delivered in Spanish by a Spanish-speaking MBSR instructor rather than through translation.
Discussion
The current study employed a mixed-methods design to examine the efficacy of MBSR for improving parent mental health and reducing parental perceptions of child behavior problems in Latino and non-Latino families of children with DD. Given the dearth of research examining MBSR for Latino participants, we also examined Latino parents’ recommendations for improving this intervention in future research and clinical delivery.
Findings suggest that MBSR was similarly efficacious in improving parent mental health outcomes for Latino and non-Latino parents. Both Latino and non-Latino parents reported similarly high levels of stress and depressive symptoms at baseline, suggesting a critical need for treatment across groups, and average levels of satisfaction with life (Diener, 2006). There were no ethnic-group differences in parent outcomes (parenting stress, depressive symptoms, and satisfaction with life) according to either quantitative or qualitative analyses, suggesting that MBSR generally appears equally effective in improving parent-reported outcomes regardless of ethnicity. Although previous studies have tested MBSR with multi-lingual samples (English and Spanish; Roth & Creaser, 1997) and a monolingual Spanish-speaking sample (Roth and Robbins, 2004), no study to our knowledge has employed a non-Latino control group to investigate the relative efficacy of MSBR in improving parent mental health outcomes. Given evidence that Latino parents of children with DD may experience high levels of stress and psychological distress, this study supports previous findings that MBSR is effective in reducing stress and depression, and promoting overall well-being (Chiesa & Serretti, 2009), and provides empirical evidence that MBSR may be just as effective in reducing parent mental health difficulties for a growing population in the United States that has historically been underrepresented in the research literature. By testing intervention efficacy across populations, as opposed to assuming universality, this investigation further advances models of culturally-competence service delivery (Campinha-Bacote, 2002).
Results also suggest that participation in MBSR was associated with reduction in aspects of parent-reported child behavior problems. Parents in the immediate treatment group reported fewer child attention problems posttreatment than did parents in the waitlist control group; trends were observed for reported child problems related to emotional reactivity and withdrawal. These changes in parent-reported child behavior problems map onto the goals of mindfulness interventions which help parents to slow down, notice impulses before they act, really listen to their children, and come to a more relaxed and peaceful state of mind when they interact with their children (Neece, 2014; Singh, et al., 2006; 2010). Increased present-moment awareness may alter parental perceptions and interpretations of child behavior, which may in turn contribute to improved in-the-moment responding. Parenting behaviors play a particularly important role in the development of social and emotional competence in children with DD (Baker, Fenning, Crnic, Baker, & Blacher, 2007; Baker et al., 2010), and growing evidence suggests that MBSR may enhance positive parenting behaviors in families of children with DD (Sanner & Neece, 2018). It will be important for future research to further examine the effects of MBSR on parenting as a potential mechanism for improving child outcomes. Given that parents are not blind to their own participation in treatment, adopting a multi-method approach that includes measurement of child behavior based on observation and external ratings will be especially important in teasing apart the mechanisms of effect.
Regarding ethnic-group differences in parent-reported child behavior problems, Latino parents reported higher levels of child depressed/anxious behavior at baseline, which is consistent with literature suggesting a tendency toward greater reporting of internalizing, particularly somatic, symptoms in this ethnic group (Weiss, Goebel, Page, Wilson, & Warda, 1999). However, there was no evidence of differential change in this dimension over the course of the intervention. Indeed, results for parent-reported child behavior outcomes were similar in directionality and magnitude across our Latino and non-Latino samples with one exception. Latino parents perceived their children to experience a greater decrease in attention problems from pre- to post-treatment than did non-Latino parents. It may be that the effect of MBSR on parent mental health has particularly valuable cascading effects for Latino families in the domain of child attention. Health disparities are prominent for Latino families, and research indicates that Latino children are less likely to receive child mental health services compared to other groups with minority status (Zimmerman, 2005). Although we controlled for parent-reported child participation in behavioral intervention, it is possible that MBSR may result in broader impact for Latino families in the absence of other services. Differences in reported child attention problems may also reflect ethnic-group variation in parental perceptions of child challenges (Yeh, Hough, McCabe, Lau, & Garland, 2004), and it will be important to attend to these considerations, as well as possible measurement biases (Gross et al., 2006), in future investigations. On the whole, given that ethnic-group differences emerged for only one index of parent-reported child problems, caution is warranted in interpreting these findings and further investigation and replication is required.
Qualitative analyses generally converged with our quantitative results suggesting similar improvements in parent mental health and parent-reported child behavior outcomes across Latino and non-Latino participants. However, our qualitative results revealed some ethnic-group differences with regard to participants’ experience in the group in addition to some important suggestions for future research and clinical endeavors using MBSR with Latino families. Interestingly, in reflecting on the benefits of the MBSR intervention, Latino parents emphasized the use the mind-body connection, while non-Latino parents most appreciated having a deeper understanding of the stress process and mindfulness attributes. Latino parents’ attention to the mind-body connection is consistent with research suggesting greater focus on somatic components of distress and a tendency for affective states to significantly influence assessments of health status in Latino individuals (Angel & Guarnaccia, 1989). Therefore, future research and clinical efforts that utilize MBSR with Latino participants may benefit from further emphasizing the mind-body connection in the didactics, formal mindfulness practices, discussions, and assigned home practices. With regard to recommendations for future MBSR groups with Latino participants, the most consistent suggestion from Latino parents was to offer the intervention in Spanish rather than using translation services. This recommendation is in line with research indicating that offering interventions in the participants’ primary language is preferable to providing translation services in terms of maximizing participant engagement and minimizing methodological biases (Barnier & Weksel, 2004).
Limitations and Future Research Directions
Although our findings were promising, these results must be considered within the context of several study limitations that have implications for future research. First, the non-Latino group was heterogeneous, comprising participants of White, African-American, Asian and other backgrounds. Further, our Latino group was also very heterogeneous and comprised parents from several different Latino descents (e.g. Mexican, Guatemalan, Nicaraguan, and others). It should also be noted that the current sample all resided in the Inland Empire Region of Southern California and, therefore, the current findings may not generalize to Latino and non-Latino parents outside this region. Future studies with larger samples are necessary to examine potential subgroup differences. Second, our findings relied solely on parent-report data to measure both parental outcomes and child behavior problems. This was important given our emphasis on parent perceptions. However, reporting biases may have influenced results. Subsequent studies would therefore benefit from the use of observational measures and additional reports of child behavior problems (e.g. from teachers), as well as biomarkers of parent stress. Third, our results only employed data immediately following treatment. Therefore, the maintenance of the treatment effects over time is unknown and future studies should include follow-up assessments. Fourth, although the current study controlled for child participation in behavioral intervention, detailed data regarding intensity, duration, as well as other types of child interventions were not available, which restricted our ability to address the unique effects of MBSR on parent-reported child behavior problems. Finally, further research is needed to investigate potential mediators of MSBR on parent and child outcomes. Transactional associations between parent mental health and child behavior problems are well documented (Neece et al., 2012; Woodman, 2014), and the extent to which MBSR may influence underlying processes needs to be elucidated in subsequent studies. The mechanisms through which therapeutic change occurs is important because understanding why a given treatment works serves as a basis for maximizing its effects and ensuring that the critical features of the treatment are generalized to clinical practice (Kazdin, 2000; Kazdin & Nock, 2003). Moreover, future studies should also investigate cultural and ethnic factors that may moderate mediation models, as previous studies have indicated that parental beliefs about disability, parenting practices, and child outcomes may vary cross-culturally (Lynch & Hanson, 2004; Walker-Barnes & Mason, 2001).
Despite our limitations, the implications of this study are significant. This study highlights that MBSR, a widely-used intervention with strong empirical support, is a promising intervention for Latino families of children with DD. This intervention was efficacious in improving significant parent mental health problems that are common among families of children with DD, and Latino families more specifically. Furthermore, MBSR was shown to have a collateral benefit in reducing parent-reported child behavior problems across populations. By providing scientific evidence suggesting the efficacy of MBSR for Latino families of children with DD, this study underscores the value of engaging diverse populations in treatment research and highlights the importance of disseminating this approach to families historically underrepresented in the service delivery system.
Footnotes
Compliance with Ethical Standards: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
All authors declare that they have no conflicts of interest.
References
- Aarons GA, Fettes DL, Sommerfeld DH, & Palinkas L (2012). Mixed methods for implementation research: Application to evidence-based practice implementation and staff turnover in community based organizations providing child welfare services. Child Maltreatment, 17(1), 67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abidin RR (1990). Parenting stress index-short form. Charlottesville, VA: Pediatric Psychology Press. [Google Scholar]
- Achenbach TM , & Rescorla LA (2000). ASEBA preschool forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families. [Google Scholar]
- Angel R, & Guarnaccia PJ (1989). Mind, body, and culture: somatization among Hispanics. Social Science & Medicine, 28(12), 1229–1238. [DOI] [PubMed] [Google Scholar]
- Baker BL, Blacher J, Crnic KA, & Edelbrock C (2002). Behavior problems and parenting stress in families of three-year-old children with and without developmental delays. American Journal on Mental Retardation, 107(6), 433–444. [DOI] [PubMed] [Google Scholar]
- Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, & Low C (2003). Pre-school children with and without developmental delay: Behaviour problems and parenting stress over time. Journal of Intellectual Disability Research, 47(4–5), 217–230. doi: 10.1046/j.1365-2788.2003.00484.x [DOI] [PubMed] [Google Scholar]
- Baker BL, Neece CL, Fenning RM, Crnic KA, & Blacher J (2010). Mental disorders in five-year-old children with or without developmental delay: Focus on ADHD. Journal of Clinical Child & Adolescent Psychology, 39(4), 492–505. doi: 10.1080/15374416.2010.486321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, Crnic KA, Baker BL, & Blacher J (2007). Prediction of social skills in 6-year-old children with and without developmental delays: Contributions of early regulation and maternal scaffolding. American Journal on Mental Retardation, 112(5), 375–391. [DOI] [PubMed] [Google Scholar]
- Barnier BG, & Weksel D (2004). U.S. Patent No. 6,690,932. Washington, DC: U.S. Patent and Trademark Office. [Google Scholar]
- Baum A, Garofalo JP, & Yali A (1999). Socioeconomic status and chronic stress: Does stress account for SES effect on health? Annals of the New York Academy of Sciences, 896(1), 131–144. [DOI] [PubMed] [Google Scholar]
- Bazzano A, Wolfe C, Zylowska L, Wang S, Schuster E, Barrett C, & Lehrer D (2015). Mindfulness based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: A community-based approach. Journal of Child and Family Studies, 24(2), 298–308. [Google Scholar]
- Berg BL (2009). Qualitative research methods for the social sciences. Boston: Allyn and Bacon [Google Scholar]
- Bernard HR, Wutich A, & Ryan GW (2016). Analyzing qualitative data: Systematic approaches. Los Angeles: SAGE publications. [Google Scholar]
- Blacher J, Lopez S, Shapiro J, & Fusco J (1997). Contributions to depression in Latina mothers with and without children with retardation: Implications for caregiving. Family Relations, 325–334. [Google Scholar]
- Board of Supervisors County of San Bernardino. (2010). San Bernardino County Community Indicators Report 2010.
- Campinha-Bacote J (2002). The process of cultural competence in the delivery of healthcare services: A model of care. Journal of Transcultural Nursing, 13(3), 181–184. [DOI] [PubMed] [Google Scholar]
- Cardoso JB, Padilla YC, & Sampson M (2010). Racial and ethnic variation in the predictors of maternal parenting stress. Journal of Social Service Research, 36(5), 429–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty H, & Gu H (2009). A mixed model approach for intent-to-treat analysis in longitudinal clinical trials with missing values RTI Press Publication No. MR-0009–0903. Research Triangle Park, NC: RTI International; Retrieved from http://www.rti.org/rtipress. [PubMed] [Google Scholar]
- Chan N, & Neece CL (2018). Mindfulness-based stress reduction for parents of children with developmental delays: A follow-up study. Evidence-Based Practice in Child and Adolescent Mental Health, 3(1), 16–29. [Google Scholar]
- Chiesa A, & Serretti A (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. The Journal of Alternative and Complementary Medicine, 15(5), 593–600. [DOI] [PubMed] [Google Scholar]
- Corbin J , & Strauss A (2008). Basics of qualitative research: Techniques and procedures for developing grounded theory. Los Angeles: Sage Publications, Inc. [Google Scholar]
- Crnic K, Arbona AP, Baker B, & Blacher J (2009). Mothers and fathers together: Contrasts in parenting across preschool to early school age in children with developmental delays. International Review of Research in Mental Retardation, 37, 3–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crnic KA, Gaze C, & Hoffman C (2005). Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behaviour at age 5. Infant & Child Development, 14(2), 117–132. doi: 10.1002/icd.384 [DOI] [Google Scholar]
- Davis NO, & Carter AS (2008). Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. Journal of Autism and Developmental Disorders, 38(7), 1278–1291. [DOI] [PubMed] [Google Scholar]
- Diener ED (2006). Understanding scores on the satisfaction with life scale. Retrieved from https://internal.psychology.illinois.edu/~ediener/Documents/Understanding%20SWLS%20Scores.pdf.
- Diener ED, Emmons RA, Larsen RJ, & Griffin S (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Fisher MH, Taylor JL, Lambert W, & Miodrag N (2014). Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics, 134(2), e454–e463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenhower AS, Baker BL, & Blacher J (2009). Children’s delayed development and behavior problems: Impact on mothers’ perceived physical health across early childhood. Social Science & Medicine, 68(1), 89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, & Cross S (2009). Meta-analysis of early intensive behavioral intervention for children with autism. Journal of Clinical Child & Adolescent Psychology, 38(3), 439–450. [DOI] [PubMed] [Google Scholar]
- Emerson E, & Einfeld S (2010). Emotional and behavioural difficulties in young children with and without developmental delay: a bi-national perspective. Journal of Child Psychology and Psychiatry, 51(5), 583–593. [DOI] [PubMed] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. Guilford Press. [Google Scholar]
- Flink IJ, Jansen PW, Beirens TM, Tiemeier H, van IJzendoorn MH, Jaddoe VW, … & Raat H (2012). Differences in problem behaviour among ethnic minority and majority preschoolers in the Netherlands and the role of family functioning and parenting factors as mediators: The Generation R Study. BMC Public Health, 12(1), 1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilliam JE (1995). Gilliam Autism Rating Scale: GARS. Pro-ed. [Google Scholar]
- Gross D, Fogg L, Young M, Ridge A, Cowell JM, Richardson R, & Sivan A (2006). The equivalence of the Child Behavior Checklist/1 1/2–5 across parent race/ethnicity, income level, and language. Psychological Assessment, 18(3), 313. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. [DOI] [PubMed] [Google Scholar]
- Guralnick M, Neville B, Connor R, & Hammond M (2003). Family factors associated with the peer social competence of young children with mild delays. American Journal on Mental Retardation, 108(4), 272–287. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Daley D, Burns C, & Beck A (2006). Maternal distress and expressed emotion: Cross-sectional and longitudinal relationships with behavior problems of children with intellectual disabilities. American Journal on Mental Retardation, 111, 48–61. [DOI] [PubMed] [Google Scholar]
- Hauser-Cram P, Warfield ME, Shonkoff JP, Krauss MW, Sayer A, & Upshur CC (2001). Children with disabilities: A longitudinal study of child development and parent well-being. Monographs of the Society for Research in Child Development, i–126. [PubMed] [Google Scholar]
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, & Einfeld S (2006). Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. Journal of Intellectual Disability Research, 50(12), 874–882. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1994, September). Catalyzing movement towards a more contemplative/sacred-appreciating/non-dualistic society. In Meeting of the Working Group. [Google Scholar]
- Kabat-Zinn J , & Hanh TN (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta. [Google Scholar]
- Kazdin AE (2000). Psychotherapy for children and adolescents: Directions for research and practice. Oxford University Press. [Google Scholar]
- Kazdin AE, & Nock MK (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44(8), 1116–1129. [DOI] [PubMed] [Google Scholar]
- Kersh J, Hedvat TT, Hauser-Cram P, & Warfield ME (2006). The contribution of marital quality to the well-being of parents of children with developmental disabilities. Journal of Intellectual Disability Research, 50, 883–893. [DOI] [PubMed] [Google Scholar]
- Long KA, Kao B, Plante W, Seifer R, & Lobato D (2015). Cultural and child-related predictors of distress among Latina caregivers of children with intellectual disabilities. American Journal on Intellectual and Developmental Disabilities, 120(2), 145–165. [DOI] [PubMed] [Google Scholar]
- Lynch EW, & Hanson MJ (2004). Steps in the right direction: Implications for service providers. Developing cross-cultural competence: A guide for working with children and their families, 449–466. [Google Scholar]
- Magana S, Li H, Miranda E, & Paradiso de Sayu R (2015). Improving health behaviours of Latina mothers of youths and adults with intellectual and developmental disabilities. Journal of Intellectual Disability Research, 59(5), 397–410. [DOI] [PubMed] [Google Scholar]
- Marquis WA, & Baker BL (2014). An examination of Anglo and Latino parenting practices: Relation to behavior problems in children with or without developmental delay. Research in developmental disabilities, 35(2), 383–392. [DOI] [PubMed] [Google Scholar]
- Merrell KW, & Holland ML (1997). Social-emotional behavior of preschool-age children with and without developmental delays. Research in Developmental Disabilities, 18(6), 393–405. [DOI] [PubMed] [Google Scholar]
- Minor HG, Carlson LE, Mackenzie MJ, Zernicke K, & Jones L (2006). Evaluation of a mindfulness-based stress reduction (MBSR) program for caregivers of children with chronic conditions. Social Work in Health Care, 43(1), 91–109. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The role of the family context in the development of emotion regulation. Social Development, 16(2), 361–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neece CL (2014). Mindfulness-based stress reduction for parents of young children with developmental delays: Implications for parental mental health and child behavior problems. Journal of Applied Research in Intellectual Disabilities, 27(2), 174–186. [DOI] [PubMed] [Google Scholar]
- Neece C, & Baker B (2008). Predicting maternal parenting stress in middle childhood: The roles of child intellectual status, behaviour problems and social skills. Journal of Intellectual Disability Research, 52(12), 1114–1128. doi: 10.1111/j.1365-2788.2008.01071.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neece CL, Green SA, & Baker BL (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. doi: 10.1352/1944-7558-117.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavot W, & Diener E (1993). Review of the satisfaction with life scale. Psychological Assessment, 5(2), 164. [Google Scholar]
- Pisula E (2007). A comparative study of stress profiles in mothers of children with autism and those of children with Down’s syndrome. Journal of Applied Research in Intellectual Disabilities, 20, 274–278. [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Robbins FR, Dunlap G, & Plienis AJ (1991). Family characteristics, family training, and the progress of young children with autism. Journal of Early intervention, 15(2), 173–184. [Google Scholar]
- Roberts LR, & Neece CL (2015). Feasibility of mindfulness-based stress reduction intervention for parents of children with developmental delays. Issues in Mental Health Nursing, 36(8), 592–602. [DOI] [PubMed] [Google Scholar]
- Robinson EA, Eyberg SM, & Ross AW (1980). The standardization of an inventory of child conduct problem behaviors. Journal of Clinical Child Psychology, 9(1), 22–29. doi: 10.1080/15374418009532938 [DOI] [Google Scholar]
- Roth B, & Robbins D (2004). Mindfulness-based stress reduction and health-related quality of life: Findings from a bilingual inner-city patient population. Psychosomatic Medicine, 66(1), 113–123. [DOI] [PubMed] [Google Scholar]
- Roth B, & Creaser T (1997). Mindfulness meditation-based stress reduction: Experience with a bilingual inner-city program. The Nurse Practitioner, 22(3), 150–178. [PubMed] [Google Scholar]
- Sanner CM and Neece CL (2018). Parental distress and child behavior problems: Parenting behaviors as mediators. Journal of Child and Family Studies, 27(2), 591–601. doi: 10.1007/s10826-017-0884-4 [DOI] [Google Scholar]
- Shevlin M, Brunsden V, & Miles JNV (1998). Satisfaction with life scale: Analysis of factorial invariance, mean structures and reliability. Personality and Individual Differences, 25(5), 911–916. [Google Scholar]
- Singh NN, Lancioni GE, Winton AS, Fisher BC, Wahler RG, Mcaleavey K, … & Sabaawi M (2006). Mindful parenting decreases aggression, noncompliance, and self-injury in children with autism. Journal of Emotional and Behavioral Disorders, 14(3), 169–177. [Google Scholar]
- Singh NN, Lancioni GE, Winton AS, Karazsia BT, Myers RE, Latham LL, & Singh J (2014). Mindfulness-based positive behavior support (MBPBS) for mothers of adolescents with autism spectrum disorder: Effects on adolescents’ behavior and parental stress. Mindfulness, 5(6), 646–657. [Google Scholar]
- Singh NN, Lancioni GE, Winton AS, Singh J, Curtis WJ, Wahler RG, & McAleavey KM (2007). Mindful parenting decreases aggression and increases social behavior in children with developmental disabilities. Behavior Modification, 31(6), 749–771. [DOI] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Winton AS, Singh J, Singh AN, Adkins AD, & Wahler RG (2010). Training in mindful caregiving transfers to parent-child interactions. Journal of Child and Family Studies, 19(2), 167–174. [Google Scholar]
- Strauss K, Vicari S, Valeri G, D’Elia L, Arima S, & Fava L (2012). Parent inclusion in early intensive behavioral intervention: The influence of parental stress, parent treatment fidelity and parent-mediated generalization of behavior targets on child outcomes. Research in Developmental Disabilities, 33(2), 688–703. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2013). Using multivariate statistics (6th edition).Boston: Allyn & Bacon. [Google Scholar]
- Tervo RC (2012). Developmental and behavior problems predict parenting stress in young children with global delay. Journal of child neurology, 27(3), 291–296. [DOI] [PubMed] [Google Scholar]
- Valicenti-McDermott M, Lawson K, Hottinger K, Seijo R, Schechtman M, Shulman L, & Shinnar S (2015). Parental stress in families of children with autism and other developmental disabilities. Journal of Child Neurology, 30(13), 1728–1735. [DOI] [PubMed] [Google Scholar]
- Walker-Barnes CJ, & Mason CA (2001). Ethnic differences in the effect of parenting on gang involvement and gang delinquency: A longitudinal, hierarchical linear modeling perspective. Child Development, 72(6), 1814–1831. [DOI] [PubMed] [Google Scholar]
- Weiss SJ, Goebel P, Page A, Wilson P, & Warda M (1999). The impact of cultural and familial context on behavioral and emotional problems of preschool Latino children. Child Psychiatry and Human Development, 29(4), 287–301. [DOI] [PubMed] [Google Scholar]
- Woodman AC (2014). Trajectories of stress among parents of children with disabilities: A dyadic analysis. Family Relations, 63(1), 39–54. [Google Scholar]
- Yeh M, Hough RL, McCabe K, Lau A, & Garland A (2004). Parental beliefs about the causes of child problems: Exploring racial/ethnic patterns. Journal of the American Academy of Child & Adolescent Psychiatry, 43(5), 605–612. [DOI] [PubMed] [Google Scholar]
- Zimmerman FJ (2005). Social and economic determinants of disparities in professional help γ seeking for child mental health problems: Evidence from a national sample. Health Services Research, 40(5p1), 1514–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]


