Abstract
Apathy is a symptom shared among many neurological and psychiatric disorders. However, the underlying neurocircuitry remains incompletely understood. Apathy is one of the core features of behavioural variant frontotemporal dementia (bvFTD), a neurodegenerative disease presenting with heterogeneous combinations of socioaffective symptoms and executive dysfunction. We reviewed all neuroimaging studies of apathy in frontotemporal dementia (FTD) attempting to refine a neurocircuitry model and inform clinical definitions. Levels of apathy have been consistently shown to correlate with the severity of executive dysfunctions across a wide range of diseases, including FTD. Some authors view ‘energisation’—the loss of which is central in apathy—as a core executive function. Apathy in FTD is most robustly associated with atrophy, hypometabolism and/or hypoperfusion in the dorsolateral prefrontal cortex, the anterior and middle cingulate cortex, the orbitofrontal cortex and the medial and ventromedial superior frontal gyri. Data also suggest that abnormalities in connecting white matter pathways and functionally connected more posterior cortical areas could contribute to apathy. There is a lack of consistency across studies due to small samples, lenient statistical thresholds, variable measurement scales and the focus on apathy as a unitary concept. Integrating findings across studies, we revise a neurocircuitry model of apathy divided along three subcomponents (cognition/planning, initiation, emotional-affective/motivation) with specific neuroanatomical and cognitive substrates. To increase consistency in clinical practice, a recommendation is made to modify the bvFTD diagnostic criteria of apathy/inertia. More generally, we argue that bvFTD constitutes a disease model to study the neurocircuitry of complex behaviours as a ‘lesion-based’ approach to neuropsychiatric symptoms observed across diagnostic categories.
INTRODUCTION
Frontotemporal dementia (FTD) is a clinical descriptor for a group of neurodegenerative diseases including both a behavioural variant and language variants (primary progressive aphasia (PPA)). Behavioural variant frontotemporal dementia (bvFTD) is a progressive neurodegenerative disease presenting with a heterogeneous combination of socioaffective symptoms and executive deficits1 due to dysfunction in neuronal networks subserving social cognition, motivation, emotion regulation, decision-making and others.2 While bvFTD is a complex clinical challenge, it constitutes an interesting disease model to understand the neurocircuitry of many human behaviours ascribed to frontal neural systems.
Apathy is one of the six core symptoms of the 2011 International Consensus Criteria for bvFTD (see box 1).1 However, there is still debate about the best definition of apathy, and its boundaries are unclear. The bvFTD diagnostic criteria II.B can be met if the subject has apathy or inertia,1 without specifying the distinction between these concepts. Unsurprisingly, apathy/inertia was found to be the bvFTD criterion with the least inter-rater reliability (mean κ=0.47)3 and specificity.4
Box 1. Clinical diagnostic criteria for behavioural frontotemporal dementia1.
Three of the following behavioural/cognitive symptoms (A–F) must be present to meet criteria:
- Shows progressive deterioration of behaviour and/or cognition by observation or history (as provided by a knowledgeable informant).
- Early1 behavioural disinhibition
- Early apathy or inertia
- Early loss of sympathy or empathy
- Early perseverative, stereotyped or compulsive/ritualistic behaviour
- Hyperorality and dietary changes
- Neuropsychological profile: executive/generation deficits with relative sparing of memory and visuospatial functions.
From Rascovsky et al.1
Apathy is a symptom shared between many neurological and psychiatric disorders including Parkinson’s disease (PD), Alzheimer’s disease (AD), cerebrovascular disease, major depressive disorder (MDD) and schizophrenia. It is one of the most salient behavioural and psychological symptoms of dementia, having been associated with more rapid cognitive and functional decline,5 increased mortality in AD6 and worse outcomes across a number of neurological diagnoses.7,8 Despite the ubiquitous nature of apathy, the underlying neurocircuitry remains incompletely understood. We postulate that bvFTD is an excellent model to study the neurocircuitry of apathy for several reasons. In bvFTD, changes in behaviour are the central clinical feature in the early stage of the disease and arise from neuronal dysfunction associated with measurable cortical atrophy, in contrast to more difficult to localise functional abnormalities in primary psychiatric disorders. Moreover, symptoms are less confounded by other related symptoms such as dysphoria in AD,9 perceptual disturbances in schizophrenia (eg, command hallucinations influencing behaviour) and depressed mood in MDD. In this article, we systematically review FTD neuroimaging studies of apathy attempting to refine a neurocircuitry model of apathy in FTD, postulating that it could serve as a model to understand apathy in other neuropsychiatric disorders. We first provide a brief overview of clinical aspects of apathy.
BACKGROUND
Phenomenology and definitions
We generally think of apathy as a symptom of a disease such as FTD or AD or as a symptom that is an element of a disorder such as MDD, but some authors consider apathy to be a primary neuropsychiatric syndrome in some settings.10 Operationalised criteria for an apathy syndrome were proposed in 1991,10 with lack of motivation compared with a previous baseline being the core symptom. Motivation is defined by the Oxford English Dictionary as the reason(s) an individual behaves in a particular way, as well as the general desire or willingness of someone to do something. Lack of motivation can be evidenced by diminished goal-directed behaviour (eg, lack of initiative), goal-directed cognition (lack of interest in new things) and emotional concomitants of goal-directed behaviour (eg, lack of affective reactivity to evocative events).10 These criteria were revised in 2009, including a 4-week duration criterion (box 2).11 Symptoms are divided into goal-directed behaviour, cognition and emotion, each domain including one example of self-initiated action/cognition/emotion and one related to responsiveness to external stimuli.11 Despite this division into cognitive, affective and action-oriented components, studies have generally found substantial overlap between the three subcomponents.9,12
Box 2. Diagnostic criteria for apathy11.
For a diagnosis of apathy, the patient should fulfil criteria A, B, C and D.
Loss of or diminished motivation in comparison to the patient’s previous level of functioning and which is not consistent with his age or culture. These changes in motivation may be reported by the patient himself or by the observations of others.
- Presence of at least one symptom in at least two of the three following domains for a period of at least 4 weeks and present most of the time.
-
B1:Loss of, or diminished, goal-directed behaviour as evidenced by at least one of the following:
- Loss of self-initiated behaviour (eg, starting conversation, doing basic tasks of day-to-day living, seeking social activities, communicating choices).
- Loss of environment-stimulated behaviour (eg, responding to conversation, participating in social activities).
-
B2:Loss of, or diminished, goal-directed cognitive activity as evidenced by at least one of the following:
- Loss of spontaneous ideas and curiosity for routine and new events (ie, challenging tasks, recent news, social opportunities, personal/family and social affairs).
- Loss of environment-stimulated ideas and curiosity for routine and new events (ie, in the person’s residence, neighbourhood or community).
-
B3:Loss of, or diminished, emotion as evidenced by at least one of the following:
- Loss of spontaneous emotion, observed or self-reported (eg, subjective feeling of weak or absent emotions or observation by others of a blunted affect).
- Loss of emotional responsiveness to positive or negative stimuli or events (eg, observer reports of unchanging affect or of little emotional reaction to exciting events, personal loss, serious illness, emotional-laden news).
-
B1:
These symptoms (A–B) cause clinically significant impairment in personal, social, occupational or other important areas of functioning.
The symptoms (A–B) are not exclusively explained or due to physical disabilities (eg, blindness and loss of hearing), to motor disabilities, to diminished level of consciousness or to the direct physiological effects of a substance (eg, drug of abuse, a medication).
From Robert et al.11
Some authors have criticised the emphasis on motivation, suggesting that apathy is best described in behavioural terms by the absence of responsiveness to internal or external stimuli, leading to decreased self-initiated actions.13,14 Levy and Dubois13 suggested redefining apathy more ‘objectively’ as ‘the quantitative reduction of self-generated voluntary and purposeful behaviour’.13 While we agree that a reduction in self-initiated and sustained behaviour is a central feature, we believe that change in the subjective motivation state is a dissociable component. Indeed, some patients with bvFTD report an intact sense of motivation but engage in little productive activity, while others express remarkable indifference but still perform tasks. Integrating these different contributions, Massimo and Evans recently revised the definition of apathy in the context of FTD as being a reduction in goal-directed behaviour stemming from any combination of deficits in initiation, planning and motivation.15
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) does not include operationalised apathy criteria. Apathy is listed as a behavioural disturbance in mild/major neurocognitive disorders, as a symptom of frontotemporal neurocognitive disorder and as a form of personality change due to another medical condition. DSM-5 has adopted a definition of apathy including both subjective motivation changes and reduced observable behaviour, stating that ‘apathy is typically characterised by diminished motivation and reduced goal-directed behaviour, accompanied by decreased emotional responsiveness.’
Comparative terminology
Further challenges arise from the use of different terms to describe related phenomena across disciplines and diseases.16 In psychiatry, apathy has been historically and arbitrarily reserved for disorders with structural abnormalities (eg, dementia, ‘organic personality’), as opposed to idiopathic syndromes. However, symptoms of MDD such as ‘lack of interest’, ‘lack of pleasure’ and ‘lack of energy’ are in part related to apathy. Despite some overlap, patients can have apathy without MDD and vice versa.17,18 The clinical distinction is made based on the presence of these symptoms within a broader negative affective syndrome in depression, including low mood, neurovegetative symptoms, guilt/worthlessness and suicidal thoughts. Whereas anhedonia (reduced experience of pleasure) can be a feature of both depression and apathy,19 it is usually accompanied by distress in the former, as opposed to indifference in the latter. Negative symptoms of schizophrenia also overlap with apathy but are described by distinct terms such as avolition, alogia (impoverishment in thoughts) and asociality. These overlaps across diagnostic categories open the possibility of cross-informative neuroscientific studies.
In neurological nosology, apathy overlaps with abulia and akinetic mutism. Abulia usually implies a poverty of spontaneous movements and speech, in addition to the usual features of apathy.20 Milder forms of abulia have been historically referred to as abulia minor.21 Akinetic mutism is the complete absence of spontaneous behaviour and speech in an individual who appears alert. While akinetic mutism clearly has added descriptive value, we postulate that the distinction between apathy and abulia is not conceptually clear and that the latter term should be eliminated and replaced by a severity specification for apathy.
Neuropsychological perspective
Levels of apathy have been shown to correlate with the severity of executive dysfunctions in a wide range of diseases, including FTD,22,23 AD,24 mild cognitive impairment (MCI),25 PD,26,27 late-life depression28 and psychotic disorders.29,30 It has been most consistently associated with impaired performance on letter fluency (F-A-S),25,28,29,31 Trail Making part B23,28,29 and the Wisconsin card sort test,27,28 independent of depressive symptoms.23–25,27,32 A few studies have also found links between apathy and short-term recall27,32 and social cognition.23
Based on neuropsychological studies and patients with brain lesion, Stuss and Alexander categorised frontal cognitive processes into task setting, monitoring and energisation.14,33 Energisation, defined as the process of initiation and sustaining a response, is particularly relevant to apathy. Deficits in energisation can be measured by, for example, lexical fluency tasks (eg, total number of words produced in a finite period of time)33,34 and have been most consistently associated with lesions of bilateral supplementary motor area (SMA).33 When a clinician is evaluating a patient with suspected apathy, generative tasks such as this may provide the simplest performance-based correlate of the symptom of apathy.
Apathy scales
The most frequently used scale is the Apathy Evaluation Scale (AES), an 18-item scale completed by the patient, caregiver or clinician.16 In dementia, the informant-rated version has the most reliable psychometric properties.35 The Apathy Scale is a briefer version that can be administered with a structured interview. Another scale, the Apathy Inventory, assesses the three dimensions of apathy (behavioural, cognitive, emotional blunting) on a simple one-question frequency/severity Likert scale.36 Apathy is also an item of the Neuropsychiatric Inventory (NPI), graded for both frequency and severity based on nine standard questions after a positive screening item.37 A clinician-rated version including 12 apathy items (NPI-C) was also developed.38 The Frontal Behavioural Inventory (FBI) includes some apathy items (apathy, aspontaneity, emotional flatness, logopenia, personal neglect)39 as part of the ‘negative symptoms’ cluster. The specific apathy item corresponds to the cognitive component (lack of interest). The Frontal Systems Behaviour Scale (FrSBe) is a self-rated or informant-rated scale to assess apathy, disinhibition and executive dysfunction in patients with frontal lobe injuries.40 For a comprehensive review of psychometric properties of scales, see Clarke et al35,41 and Starkstein et al.5,16 Although most measures of apathy involve questionnaires such as these, some investigators have developed performance-based tests such as the Philadelphia Apathy Computerized Test (PACT) to objectively assess apathy along three dimensions: initiation, planning and motivation.42
METHODS
Neuroimaging review
A Pubmed search of all English language original research articles with keywords ‘Frontotemporal Dementia’ AND ‘Apathy’ was conducted through December 2016. We did not include imaging search terms to identify articles of potential interest that did not have imaging component for the general review, in addition to neuroimaging studies that were the focus of the review. The search produced 168 abstracts that were systematically reviewed to identify neuroimaging studies of apathy in FTD across all imaging modalities, excluding case reports. Articles were included in the study if they were either:
Group analyses comparing the neuroimaging correlates of apathy in FTD to other disorders.
Correlation analyses between apathy severity and neuroimaging measures in FTD.
Fourteen articles met the inclusion criteria. Articles were reviewed to extract key findings and determine methodological validity. Reviewing references from the identified articles and a complementary Google Scholar search did not yield additional articles.
RESULTS
Apathy is the most common initial symptom of FTD43 and is present to some degree in almost all patients suffering from bvFTD.9,12 It is more frequent and severe in FTD than in AD12,43 and constitutes a major burden for caregivers.44 Apathy is attributed more predominantly to loss of motivation in FTD, as opposed to dysphoria in AD.9,12
Structural neuroimaging
Most structural imaging studies of apathy have used MRI voxel-based morphometry (VBM) (table 1). In the largest study including only subjects with bvFTD (n=48) or PPA (n=14), FrSBe apathy scores were associated with increased atrophy of the right dorsolateral prefrontal cortex (DLPFC) (p<0.05, whole brain family-wise error correction), with trends of association in the right lateral orbitofrontal cortex (OFC), right anterior cingulate cortex (ACC), right temporoparietal junction (TPJ) and right putamen.22 In a more recent study, Eslinger at al (bvFTD=12, primary non-fluent aphasia (PNFA)=7, semantic dementia (SD)=7) reported an association between AES score and atrophy of the right head of the caudate (including the ventral striatum), right TPJ, the posterior part of the right inferior and middle temporal gyri, left frontal operculum and left anterior insula.23 However, the statistical threshold was lenient (p<0.025, uncorrected, >100 voxels/clusters). In another study (bvFTD=26, PPA=14), NPI apathy was correlated with atrophy in bilateral medial, orbital, inferior and dorsolateral prefrontal areas, in addition to the right middle temporal gyri and right caudate nucleus (p<0.01,false discovery rate corrected after masking areas without atrophy, clusters ≥40 adjacent voxels).44 One study found no difference in basal ganglia volume in subjects with high compared with low NPI apathy.45 Finally, in one of the rare white matter studies, apathy severity was associated with reduced fractional anisotropy (FA) of the temporal part of the uncinate fasciculus.46
Table 1.
Structural neuroimaging studies of apathy in FTD
| Authors | Year | Sample | Apathy scale | Method | Main findings |
|---|---|---|---|---|---|
| Rosen et al47 | 2005 | n=148 (AD, bvFTD, PNFA and SD) | NPI (continuous variable) | MRI–VBM | (1) Apathy in FTD/SD specifically associated with atrophy of right ventromedial superior frontal gyrus (2) Apathy and other neuropsychiatric symptoms associated with atrophy of right-sided frontotemporal areas, including the lateral OFC, MCC, vmSFG (mPFC), caudate head and ventral striatum |
| Zamboni et al22 | 2008 | n=62 (bvFTD and PPA) | FrSBe (continuous variable) | MRI–VBM | (1) Apathy associated with increased atrophy in right DLPFC (2) Trends of association with left DLPFC, right ACC, right LOFC, right temporoparietal junction, right putamen |
| Massimo et al44 | 2009 | n=40 (bvFTD=26, PPA=14) | NPI (continuous variable) | MRI–VBM | Apathy correlated with atrophy in bilateral mPFC, OFC, IFC, DLPFC, right middle temporal and right caudate |
| Links et al45 | 2009 | n=21 (FTD) | Group contrast based on NPI | MRI–Semiautomated volume extraction | No association with basal ganglia |
| Eslinger et al23 | 2012 | n=26 (bvFTD, SD, PNFA) | AES (continuous variable) | MRI–VBM | Apathy associated with higher atrophy in right caudate (ventral striatum), right temporoparietal junction, right posteroinferior and middle temporal gyri and the left anterior insula |
| Powers et al46 | 2014 | n=11 (bvFTD) | NPI (continuous variable) | DTI-FA | Apathy severity associated with reduced FA in the temporal portion of the left uncinate faciculus |
| Massimo et al42 | 2015 | n=18 (bvFTD) | Philadelphia Apathy Computerised Test | MRI-VBM DTI-FA | (1) Initiation deficits associated with decreased GM density in the ACC and reduced FA in the cingulum, inferior longitudinal fasciculus, unicinate fasciculus, corpus callosum (2) Planning deficits associated with decreased GM density in the DLPFC and decreased FA in the superior longitudinal fasciculus (3) Motivation deficits associated with decreased GM in the OFC and ACC and reduced FA in the uncinated fasciculus |
AD, Alzheimer s disease; ACC, anterior cingulate cortex; AES, Apathy Evaluation Scale; bvFTD, behavioural variant frontotemporal dementia; DTI, diffusion tensor imaging; DLPFC, dorsolateral prefrontal cortex; FA, fractional anisotropy; FrSBe, Frontal Systems Behaviour Scale; FTD, frontotemporal dementia; GM, grey matter; IFC, inferior frontal cortex; LOFC, lateral orbitofrontal cortex; mPFC, medial prefrontal cortex; MCC, middle cingulate cortex; NPI, Neuropsychiatric Inventory; OFC, orbitofrontal cortex; PPA, primary progressive aphasia; PNFA, primary non-fluent aphasia; SD, semantic dementia; vmSFG, ventromedial superior frontal gyrus; VBM, voxel-based morphometry.
In a large study of mixed neurodegenerative diseases (n=148), including FTD (bvFTD=39, PNFA=13, SD=23), NPI apathy was associated with VBM atrophy in predominantly right-sided frontotemporal areas, including the lateral OFC, ACC, ventromedial superior frontal gyrus (vmSFG, ie, medial PFC area anterior to the ACC), caudate head and ventral striatum, but there was major overlap with other neuropsychiatric symptoms. When controlling for other variables, apathy was specifically associated with atrophy in the right vmSFG only in the FTD/SD subgroup (less stringent small volume region of interest (ROI) correction).47
Massimo and colleagues recently analysed the grey and white matter correlates of apathy along the three subcomponents of initiation, planning and motivation as measured by the PACT (n=18 bvFTD).42 Impaired initiation was associated with decreased grey matter density in the ACC along with reduced FA in various related white matter tracts (cingulum, inferior longitudinal fasciculus, uncinate fasciculus, corpus callosum). Planning deficits were linked to atrophy in the DLPFC and decreased FA in the superior longitudinal fasciculus. Reduced motivation was associated with decreased grey matter in the OFC and ACC, along with reduced FA in the uncinate fasciculus. These results provide the best support for partially distinct circuits underlying subcomponents of apathy.
Functional neuroimaging (table 2)
Table 2.
Functional neuroimaging studies of apathy in FTD
| Authors | Year | Sample | Apathy scale | Method | Main findings |
|---|---|---|---|---|---|
| Franceschi et al51 | 2005 | n=18 (bvFTD) | Group contrast based on NPI | FDG-PET | (1) Apathy associated with hypometabolism of bilateral DLPFC, mPFC (MCC, SMA), frontal pole/anterior OFC, insula (2) Apathy and disinhibition associated with hypometabolism of bilateral insula and thalamus |
| Peters et al50 | 2006 | n=41 (bvFTD) | NPI (continuous variable and group contrast) | FDG-PET | (1) No association with NPI apathy as a continuous variable (2) Subjects with predominant apathy (n=13) had hypometabolism in posterior mOFC (gyrus rectus) compared with controls |
| Le Ber et al49 | 2006 | n=17 (bvFTD) vs 28 age-matched controls | Group contrast based on clinical assessment | SPECT | Apathy associated with predominant hypoperfusion in vmSFG, ACC, MCC, pre-SMA/SMA and DLPFC |
| McMurtray et al48 | 2006 | n=74 (bvFTD) | Single item 5-point Likert scale (continuous variable) | SPECT | Apathy associated with frontal hypoperfusion |
| Schroeter et al52 | 2011 | n=54 (AD, FTD, MCI, SCI, others) | NPI (continuous variable) | FDG-PET | (1) Apathy specifically associated to hypometabolism of VTA and left inferior and middle temporal gyri (2) Apathy, disinhibition and eating disorders associated with mPFC/ACC/MCC (BA 9, 10, 24, 32, 33) and left anterior SFG (BA 9, 10) |
| Farb et al53 | 2012 | n=16 (bvFTD, SD) vs 16 age-matched controls | FBI | fMRI intrinsic connectivity | (1) Apathy associated with PFC hyperconnectivity (2) Apathy associated with increased angular gyrus connectivity in bvFTD only |
| Day et al54 | 2013 | n=15 (bvFTD, SD) | FBI | fMRI | (1) No correlation between severity of apathy and resting state activity (2) Left insula integrity could predict short-term worsening of apathy |
AD, Alzheimer’s disease; ACC, anterior cingulate cortex; bvFID, behavioural variant frontotemporal dementia; BA, Brodmann area; DLPFC, dorsolateral prefrontal cortex; FDG-PET, fluorodeoxy glucose positron emission tomography; FBI, Frontal Behaviour Inventory; FTD, frontotemporal dementia; fMRI, functional MRI; mPFC, medial prefrontal cortex; MCC, middle cingulate cortex; MCI, mild cognitive impairment; NPI, Neuropsychiatric Inventory; OFC, orbitofrontal cortex; PFC, prefrontal cortex; SD, semantic dementia; SPECT, single-photon emission CT; SCI, subjective cognitive impairment; SMA, supplementary motor area; vmSFG, ventromedial superior frontal gyrus; VTA, ventral tegmental area.
Using single-photon emission computed tomography (SPECT), McMurtray et al. (2006) reported that apathy (single item Likert scale) was associated with bilateral frontal hypoperfusion, as opposed to temporal hypoperfusion for “hypomania-like” behaviors.48 Sample size was relatively large (n=74 bvFTD), but hypoperfusion was assessed with a semiquantitative method with poor anatomical resolution. Le Ber et al compared 17 subjects with a predominant apathetic bvFTD to 28 age-matched controls and reported the strongest degree of hypoperfusion in medial SFG, ACC, middle cingulate cortex (MCC), pre-SMA/SMA and DLPFC.49 The authors do not mention controlling for disease severity, so these findings may not be specific to apathy.
Using fluorodeoxyglucose positron emission tomography (FDG-PET), Peters et al did not find correlation between NPI apathy score and metabolism in 41 bvFTD subjects.50 When comparing the 13 subjects with predominant apathy to controls using a more lenient statistical threshold (p<0.001, uncorrected, masking hypometabolic areas in non-apathetic subjects), there was hypometabolism in the posterior medial OFC (gyrus rectus). Franceschi et al compared 12 subjects with predominantly apathetic bvFTD to 24 age-matched controls and 6 disinhibited bvFTD.51 The apathetic subjects unsurprisingly showed widespread differences with controls, while compared with disinhibited subjects controlling for disease duration (p<0.01, uncorrected) they had less uptake in bilateral DLPFC, medial PFC and insula. The disinhibited subgroup had predominant hypometabolism in posterior OFC, inferior temporal cortex, ACC, hippocampus/amygdala and nucleus accumbens.51
In an FDG-PET study of a mixed sample of early dementia, MCI and subjective cognitive concerns (13/54 with FTD), apathy, disinhibition and abnormal eating were all associated with hypometabolism of the ACC, MCC, medial PFC and the left anterior and medial SFG.52 Controlling for age and dementia severity (but not diagnosis), NPI apathy was specifically associated with hypometabolism in the left medial, inferior temporal gyri and the ventral tegmental area, a crucial node of the dopaminergic system.52
Two studies have used fMRI intrinsic connectivity. In a small sample (n = 8 bvFTD+8 SD) independent component analysis, there was an association between apathy and increased dorsal PFC connectivity, even when controlling for atrophy.53 In bvFTD subjects only, increased right angular gyrus connectivity, a central node of the default mode network, was also linked to apathy.53 Of note, the FBI negative symptoms score was used as a proxy of apathy; however, this subscale includes unrelated items (eg, apraxia, aphasia). Another study from the same group in 15 subjects (5 bvFTD+10 SD) found no association between baseline resting state fMRI and FBI negative symptoms score.54 Authors reported that fractional amplitude of low-frequency fluctuation (a measure of network integrity) in the left insula predicted worsening of apathy, but this finding is difficult to interpret given the very short 8-week time frame.
DISCUSSION
Although there are considerable variations between studies, some patterns seem to emerge. Atrophy, hypometabolism and hypoperfusion localise predominantly to the DLPFC,22,42,44,49,51 ACC/MCC,22,42,47,49,51 OFC22,42,44,47,50,51 and medial SFG.44,47,49 Other areas less consistently implicated included the ventromedial SFG,47 pre-SMA/SMA,49,51 insula23,51 and temporal areas,23,44,52 with possibly a right-sided predominance in structural imaging studies.22,47 The lack of consistency across studies is not surprising given the small samples and the often lenient statistical thresholds. The most statistically robust structural correlations were found in the right DLPFC22 and right vmSFG (the medial area rostral to the ACC),47 which are associated with executive dysfunctions.22,23
These results partially overlap with findings in AD that have most consistently linked apathy to the ACC and OFC, but less with the MCC, vmSFG, SMA, ventrolateral PFC and DLPFC.55,56 Studies in PD have suggested a possible reduction in cathecholaminergic transmission in the mesolimbic pathway as one of the causes of apathy.57–59 This dovetails with the finding of VTA hypometabolism on FDG-PET in a mixed sample of neurodegenerative disease, although this is an isolated finding requiring replication.52
Levy and Dubois proposed a frontostriatal neurocircuitry model of the three subcomponents of apathy. Cognitive features were attributed to damage in the DLPFC and connections to the ‘cognitive territory’ of basal ganglia (dorsal caudate nucleus); emotional-affective aspects to the vmPFC/OFC and connections to the ‘limbic territories’ of the basal ganglia (ventral striatum and ventral pallidum); and behavioural/auto-activation deficits to the ACC, MCC and medial SFG and connection to both cognitive and limbic basal ganglia territories. Although there is overlap between these components,9,12 this model was partly supported by findings from Massimo and Evans15 linking planning to the DLPFC, initiation to the ACC and motivation to the ACC/OFC.42
We agree in large parts with the biological plausibility of this model,13 with a few additional updates as illustrated in figure 1A. DLPFC atrophy is predominantly related to the cognitive component (planning) and associated with deficits in set-shifting, task setting and abstraction. Neuronal loss in the dorsomedial frontal areas (ACC, MCC, medial SFG, SMA) is most likely linked to the initiation component and to energisation deficits. The SMA/pre-SMA was not included in the original Levy and Dubois model, but this is potentially an important area given its role in energisation33,60 and intentional movement planning.61 Finally, dysfunction in ventral prefrontal areas (SgACC, medial and lateral OFC) would be predominantly responsible for the emotional/affective components (subjective motivation) and accompanying problems in social cognition tests. The anterior insula could also have a role in the subjective motivation state across all subcomponents23 given its role in the perception of emotionally significant stimuli, integration of interoceptive inputs and close connections with prefrontal structures.62
Figure 1.
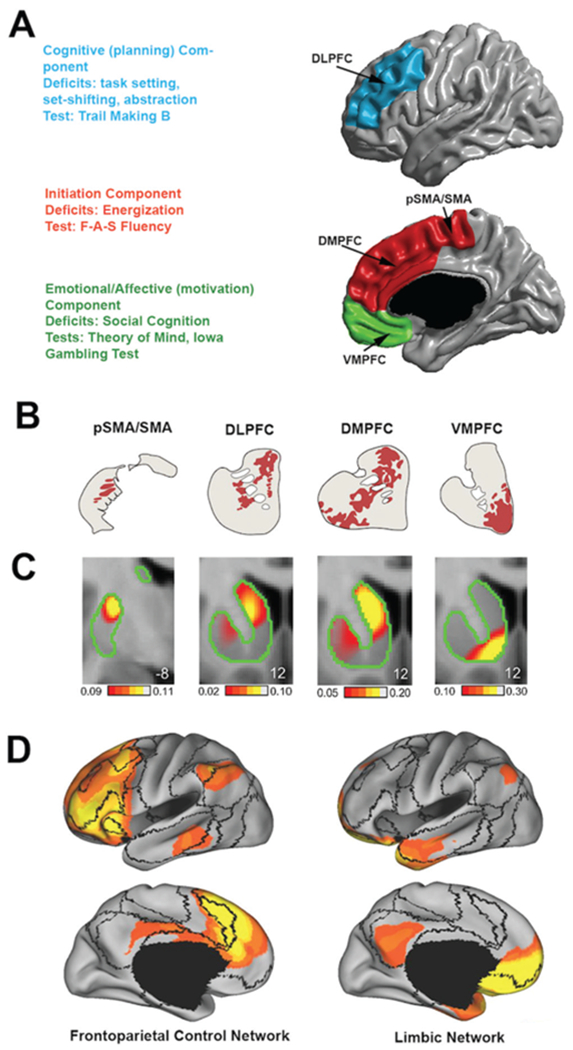
Neurocircuitry model of the three components of apathy and associated cognitive deficits. (A) Hypothesised main neuroanatomical areas related to three subcomponents of apathy and associated cognitive deficits. (B) Striatal connections of key cortical nodes based on monkey tract tracing. pSMA/SMA has main connections with the medial putamen, DLPFC and DMPFC to dorsal caudate and VMPFC to ventral caudate (nucleus accumbens). (C) Resting state fMRI intrinsic connectivity of key cortical nodes with the striatum in humans corroborating anatomical findings in monkeys. (D) Main resting state intrinsic connectivity networks associated with cortical nodes and related striatal connections. DLPFC, DMPFC and pSMA/SMA are mainly integrated as part of the frontoparietal control network. The VMPFC is integrated within the limbic network. (B–D) Adapted with permission from Choi et al.63 Organisation of the human striatum estimated by intrinsic functional connectivity. DLPFC, dorsolateral prefrontal cortex; pSMA/SMA, presupplementary motor area/supplementary motor area; DMPFC, dorsal medial prefrontal cortex; fMRI, functional MRI; pSMA, presupplementary motor area; VMPFC, ventromedial prefrontal cortex.
These cortical areas have specific anatomical connections and functional correlations with the striatum (figure 1B,C).63 Lesions/dysfunction in these striatal areas (and possibly in their thalamic nuclei) could lead to similar symptoms to their cortical counterparts, as supported by the presence of apathy in neuro-degenerative diseases with predominant subcortical involvement (eg, PD, Huntington’s disease) and subcortical strokes.
The few studies on white matter support the idea that apathy could also stem from lesions in pathways connecting these corticostriatal areas to each other and to wider networks (figure 1D).63–65 Indeed, apathy was related to FA of the uncinate fasciculus, which is a key white matter tract connecting the limbic system to the OFC.42,46 The main intrinsic connectivity network related to the DLPFC, dorsal medial PFC and pre-SMA/SMA is the frontoparietal executive control network, while the ventral medial PFC is integrated as part of a wider limbic network.63,66 These long-range connections could explain a more minor contribution to apathy of posterior areas with functional connections to the PFC. Indeed, a few studies in FTD have suggested associations between apathy and the TPJ or lateral temporal areas.22,23,44 Although this remains to be tested, the severity of the different domains of apathy could evolve over time within a single patient as the disease propagates from core frontomedial deficits to more lateral frontal and temporal areas.67
It is important to note that the networks involved in this model are closely related to other core behavioural symptoms of bvFTD. Indeed, Shroeter et al and Rosen et al have demonstrated the significant overlap of cerebral regions across behavioural symptoms. For example, the dorsomedial PFC circuitry plays a key role in theory of mind,68 and the anterior insula is part of the salience functional network, which has been shown to be disrupted in the stages of the disease.69 However, not all regions involved in executive dysfunction, such as the inferior frontal area, overlap with the neurocircuitry of apathy.70
A few factors contribute to our limited understanding of the neurocircuitry of apathy. First, there remains some debate regarding the optimal definition of apathy. Although lack of motivation was identified as the central component of the syndrome,11 observable lack of initiation and sustainability of goal-directed actions are also core features in our opinion. Indeed, patients with FTD are often unable to communicate a subjective lack of motivation or may report a normal degree of subjective motivation while not engaging in any productive behaviour. The wording in the 2011 bvFTD criteria1 and DSM-5 is not consistent with this current definition of apathy. Indeed, ‘inertia’, if interpreted as a lack of behavioural initiative/auto-activation, is a subcomponent of apathy, not a separate symptom. Consequently, we suggest the modification in box 3 to the bvFTD diagnostic criteria.
Box 3. Recommended modifications to bvFTD diagnostic criteria B.
B. Early apathy (one of the following symptoms (B.1–B.2) must be present):
-
B.1.
Loss of motivation.
-
B.2.
Diminished initiation and/or performance to completion of goal-directed behaviour.
Some patients with bvFTD and many with SD may have excessive motivation for compulsive non-productive interests or rituals but neglect day-to-day productive activities. In our view, some of these patients do not exhibit what we would describe as apathy—in fact, they may keep themselves quite ‘busy’—but they have developed a relatively narrow set of activities to which they assign value. This could be viewed as a form of perseveration, which may involve executive dysfunction, semantic memory loss or other deficits that deserve further investigation but should not be viewed as apathy. The currently available scales do not capture these subtleties that are frequently seen in FTD. Even more problematic is the potential confusion between concepts such as depression and apathy.17 For example, a careful assessment for depression has been shown to markedly reduce the identified prevalence of apathy in PD.71 Confusing depression and apathy also has therapeutic consequences if patients do not receive adequate treatment for their mood disorders. Given the subtleties of teasing out apathy from depressive and cognitive factors, apathy in FTD should be assessed with information provided by caregivers23 but rated by an experienced clinician. Non-professional caretakers do not have experience with a large number of patients; therefore, ratings can be influenced by recall bias, culture, beliefs, expectations and social desirability.38
From a methodological standpoint, we believe that it is important to control for disease severity in statistical analyses since apathy tends to increase as the disease progresses. In terms of imaging methodology, no published neuroimaging studies of the correlates of apathy have used surface-based cortical thickness analyses, which could provide better anatomical precision for the cortex. As the number of studies on this topic grows, meta-analytic approaches could be useful to clarify a specific circuitry for the different behavioural symptoms of FTD.67 In addition, multimodal network approaches combining structural and functional connectivity could provide further insight into this behavioural problem.
In conclusion, the field should keep working toward more precise definitions of symptom domains such as apathy, and these constructs should be validated by multimodal methods of neuroscientific inquiry, across different diagnostic classes, factoring in the variation of traits within healthy individuals (eg, normal variations in motivation). This research should be integrated within the framework of the Research Domain Criteria (RDoC) to study neuropsychiatric symptoms in terms of neurocircuitry regardless of diagnostic category (eg, studying apathy as a combination of deficits in approach motivation and arousal systems). We argue that bvFTD represents an excellent population for RDoC investigations because neuropsychiatric symptoms are central to the disease and arise from readily measurable neuronal atrophy. However, the generalisability of the neurocircuitry model of apathy in bvFTD proposed in this article should be tested in other psychiatric and neurological disorders to determine if the neurocircuitry is similar in all conditions. Finally, the hope is to reach the point where the diagnostic criteria for apathy could be revised to fit with our understanding of the underlying neurocircuitry abnormalities, providing a more robust foundation for the development of treatments including neuromodulation approaches such as rTMS and tDCS, in addition to pharmacological approaches.
Acknowledgments
Funding Dr Ducharme receives salary funding from the Fonds de Recherche du Québec - Santé. Authors would like to thank The Sidney R Baer, Jr Foundation for their support.
Footnotes
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 2011;134:2456–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seeley WW, Zhou J, Kim EJ. Frontotemporal dementia: what can the behavioral variant teach us about human brain organization? Neuroscientist 2012;18:373–85. [DOI] [PubMed] [Google Scholar]
- 3.Lamarre AK, Rascovsky K, Bostrom A, et al. interrater reliability of the new criteria for behavioral variant frontotemporal dementia. Neurology 2013;80:1973–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris JM, Gall C, Thompson JC, et al. Sensitivity and specificity of FTDC criteria for behavioral variant frontotemporal dementia. Neurology 2013;80:1881–7. [DOI] [PubMed] [Google Scholar]
- 5.Starkstein SE, Jorge R, Mizrahi R. The prevalence, clinical correlates and treatment of apathy in alzheimer’s disease. The European Journal of Psychiatry 2006;20:96–106. [Google Scholar]
- 6.Spalletta G, Long JD, Robinson RG, et al. Longitudinal neuropsychiatric predictors of death in alzheimer’s disease. J Alzheimers Dis 2015;48:627–36. [DOI] [PubMed] [Google Scholar]
- 7.Jorge RE, Starkstein SE, Robinson RG, et al. Can J Psychiatry 2010;55:350–4. [DOI] [PubMed] [Google Scholar]
- 8.Wee N, Kandiah N, Acharyya S, et al. Baseline predictors of worsening apathy in Parkinson’s disease: a prospective longitudinal study. Parkinsonism Relat Disord 2016;23:95–8. [DOI] [PubMed] [Google Scholar]
- 9.Chow TW, Binns MA, Cummings JL, et al. Apathy symptom profile and behavioral associations in frontotemporal dementia vs dementia of alzheimer type. Arch Neurol 2009;66:888–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marin RS. Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci 1991;3:243–54. [DOI] [PubMed] [Google Scholar]
- 11.Robert P, Onyike CU, Leentjens AF, et al. Proposed diagnostic criteria for apathy in Alzheimer’s disease and other neuropsychiatric disorders. Eur Psychiatry 2009;24:98–104. [DOI] [PubMed] [Google Scholar]
- 12.Derouesné C, Lacomblez L, Fiori N, et al. L’apathie dans la démence frontemporale et la maladie d’Alzheimer: existe-t-il des profils distincts? Gériatrie et Psychologie Neuropsychiatrie du Vieillissement 2012;10:107–15. [DOI] [PubMed] [Google Scholar]
- 13.Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb Cortex 2006;16:916–28. [DOI] [PubMed] [Google Scholar]
- 14.Stuss DT, Van Reekum R, Murphy KJ. Differentiation of states and causes of apathy Borod JC, ed. The neuropsychology of emotion. New York, NY: Oxford University Press, Inc, 2000:340–63. [Google Scholar]
- 15.Massimo L, Evans LK. Differentiating subtypes of apathy to improve person-centered care in frontotemporal degeneration. J Gerontol Nurs 2014;40:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starkstein SE, Leentjens AF. The nosological position of apathy in clinical practice. J Neurol Neurosurg Psychiatry 2008;79:1088–92. [DOI] [PubMed] [Google Scholar]
- 17.Starkstein SE, ingram L, Garau ML, et al. On the overlap between apathy and depression in dementia. J Neurol Neurosurg Psychiatry 2005;76:1070–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levy ML, Cummings JL, Fairbanks LA, et al. Apathy is not depression. J Neuropsychiatry Clin Neurosci 1998;10:314–9. [DOI] [PubMed] [Google Scholar]
- 19.Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev 2011;35:537–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vijayaraghavan L, Krishnamoorthy ES, Brown RG, et al. Abulia: a delphi survey of British neurologists and psychiatrists. Mov Disord 2002;17:1052–7. [DOI] [PubMed] [Google Scholar]
- 21.Fisher CM. Honored guest presentation: abulia minor vs. agitated behavior. Clin Neurosurg 1983;31:9–31. [DOI] [PubMed] [Google Scholar]
- 22.Zamboni G, Huey ED, Krueger F, et al. Apathy and disinhibition in frontotemporal dementia: insights into their neural correlates. Neurology 2008;71:736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eslinger PJ, Moore P, Antani S, et al. Apathy in frontotemporal dementia: behavioral and neuroimaging correlates. Behav Neurol 2012;25:127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McPherson S, Fairbanks L, Tiken S, et al. Apathy and executive function in Alzheimer’s disease. J Int Neuropsychol Soc 2002;8:373–81. [DOI] [PubMed] [Google Scholar]
- 25.Zahodne LB, Tremont G. Unique effects of apathy and depression signs on cognition and function in amnestic mild cognitive impairment. Int J Geriatr Psychiatry 2013;28:50–6. [DOI] [PubMed] [Google Scholar]
- 26.Zgaljardic DJ, Borod JC, Foldi NS, et al. Relationship between self-reported apathy and executive dysfunction in nondemented patients with Parkinson disease. Cogn Behav Neurol 2007;20:184–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Varanese S, Perfetti B, Ghilardi MF, et al. Apathy, but not depression, reflects inefficient cognitive strategies in Parkinson’s disease. PLoS One 2011;6:e17846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feil D, Razani J, Boone K, et al. Apathy and cognitive performance in older adults with depression. Int J Geriatr Psychiatry 2003;18:479–85. [DOI] [PubMed] [Google Scholar]
- 29.Konstantakopoulos G, Ploumpidis D, Oulis P, et al. Apathy, cognitive deficits and functional impairment in schizophrenia. Schizophr Res 2011;133:193–8. [DOI] [PubMed] [Google Scholar]
- 30.Faerden A, Vaskinn A, Finset A, et al. Apathy is associated with executive functioning in first episode psychosis. BMC Psychiatry 2009;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faerden A, Nesvåg R, Barrett EA, et al. Assessing apathy: the use of the Apathy Evaluation Scale in first episode psychosis. Eur Psychiatry 2008;23:33–9. [DOI] [PubMed] [Google Scholar]
- 32.Butterfield LC, Cimino CR, Oelke LE, et al. The independent influence of apathy and depression on cognitive functioning in Parkinson’s disease. Neuropsychology 2010;24:721–30. [DOI] [PubMed] [Google Scholar]
- 33.Stuss DT, Alexander MP. is there a dysexecutive syndrome? Philos Trans R Soc Lond B Biol Sci 2007;362:901–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stuss DT, Alexander MP, Hamer L, et al. The effects of focal anterior and posterior brain lesions on verbal fluency. J Int Neuropsychol Soc 1998;4:265–78. [PubMed] [Google Scholar]
- 35.Clarke DE, Reekum R, Simard M, et al. Apathy in dementia: an examination of the psychometric properties of the apathy evaluation scale. J Neuropsychiatry Clin Neurosci 2007;19:57–64. [DOI] [PubMed] [Google Scholar]
- 36.Robert PH, Clairet S, Benoit M, et al. The apathy inventory: assessment of apathy and awareness in Alzheimer’s disease, Parkinson’s disease and mild cognitive impairment. Int J Geriatr Psychiatry 2002;17:1099–105. [DOI] [PubMed] [Google Scholar]
- 37.Cummings JL, Mega M, Gray K, et al. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994;44:2308. [DOI] [PubMed] [Google Scholar]
- 38.de Medeiros K, Robert P, Gauthier S, et al. The neuropsychiatric inventory-clinician rating scale (NPI-C): reliability and validity of a revised assessment of neuropsychiatric symptoms in dementia. Int Psychogeriatr 2010;22:984–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kertesz A, Nadkarni N, Davidson W, et al. The Frontal Behavioral inventory in the differential diagnosis of frontotemporal dementia. J Int Neuropsychol Soc 2000;6:460–8. [DOI] [PubMed] [Google Scholar]
- 40.Malloy P, Grace J. A review of rating scales for measuring behavior change due to frontal systems damage. Cogn Behav Neurol 2005;18:18–27. [DOI] [PubMed] [Google Scholar]
- 41.Clarke DE, Ko JY, Kuhl EA, et al. Are the available apathy measures reliable and valid? A review of the psychometric evidence. J Psychosom Res 2011;70:73–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Massimo L, Powers JP, Evans LK, et al. Apathy in frontotemporal degeneration: neuroanatomical evidence of impaired goal-directed behavior. Front Hum Neurosci 2015;9:611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shinagawa S, ikeda M, Fukuhara R, et al. initial symptoms in frontotemporal dementia and semantic dementia compared with Alzheimer’s disease. Dement Geriatr Cogn Disord 2006;21:74–80. [DOI] [PubMed] [Google Scholar]
- 44.Massimo L, Powers C, Moore P, et al. Neuroanatomy of apathy and disinhibition in frontotemporal lobar degeneration. Dement Geriatr Cogn Disord 2009;27:96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Links KA, Chow TW, Binns M, et al. Apathy is not associated with basal ganglia atrophy in frontotemporal dementia. Am J Geriatr Psychiatry 2009;17:819–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Powers JP, Massimo L, McMillan CT, et al. White matter disease contributes to apathy and disinhibition in behavioral variant frontotemporal dementia. Cogn Behav Neurol 2014;27:206–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosen HJ, Allison SC, Schauer GF, et al. Neuroanatomical correlates of behavioural disorders in dementia. Brain 2005;128:2612–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMurtray AM, Chen AK, Shapira JS, et al. Variations in regional SPECT hypoperfusion and clinical features in frontotemporal dementia. Neurology 2006;66:517–22. [DOI] [PubMed] [Google Scholar]
- 49.Le Ber i, Guedj E, Gabelle A, et al. Demographic, neurological and behavioural characteristics and brain perfusion SPECT in frontal variant of frontotemporal dementia. Brain 2006;129:3051–65. [DOI] [PubMed] [Google Scholar]
- 50.Peters F, Perani D, Herholz K, et al. Orbitofrontal dysfunction related to both apathy and disinhibition in frontotemporal dementia. Dement Geriatr Cogn Disord 2006;21:373–9. [DOI] [PubMed] [Google Scholar]
- 51.Franceschi M, Anchisi D, Pelati O, et al. Glucose metabolism and serotonin receptors in the frontotemporal lobe degeneration. Ann Neurol 2005;57:216–25. [DOI] [PubMed] [Google Scholar]
- 52.Schroeter ML, Vogt B, Frisch S, et al. Dissociating behavioral disorders in early dementia-An FDG-PET study. Psychiatry Res 2011;194:235–44. [DOI] [PubMed] [Google Scholar]
- 53.Farb NA, Grady CL, Strother S, et al. Abnormal network connectivity in frontotemporal dementia: evidence for prefrontal isolation. Cortex 2013;49:1856–73. [DOI] [PubMed] [Google Scholar]
- 54.Day GS, Farb NA, Tang-Wai DF, et al. Salience network resting-state activity: prediction of frontotemporal dementia progression. JAMA Neurol 2013;70:1249–53. [DOI] [PubMed] [Google Scholar]
- 55.Robert G, Lozachmeur C, Le Jeune F, et al. [Apathy neural bases in neurodegenerative disorders]. Rev Neurol 2012;168:605–19. [DOI] [PubMed] [Google Scholar]
- 56.Theleritis C, Politis A, Siarkos K, et al. A review of neuroimaging findings of apathy in Alzheimer’s disease. Int Psychogeriatr 2014;26:195–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Remy P, Doder M, Lees A, et al. Depression in Parkinson’s disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 2005;128:1314–22. [DOI] [PubMed] [Google Scholar]
- 58.Thobois S, Ardouin C, Lhommée E, et al. Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: predictors and underlying mesolimbic denervation. Brain 2010;133:1111–27. [DOI] [PubMed] [Google Scholar]
- 59.Benoit M, Robert PH. imaging correlates of apathy and depression in Parkinson’s disease. J Neurol Sci 2011;310:58–60. [DOI] [PubMed] [Google Scholar]
- 60.Chapados C, Petrides M. impairment only on the fluency subtest of the Frontal Assessment Battery after prefrontal lesions. Brain 2013;136(Pt 10):2966–78. [DOI] [PubMed] [Google Scholar]
- 61.Fried i, Mukamel R, Kreiman G. internally generated preactivation of single neurons in human medial frontal cortex predicts volition. Neuron 2011;69:548–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Craig AD. How do you feel--now? The anterior insula and human awareness. Nat Rev Neurosci 2009;10:59–70. [DOI] [PubMed] [Google Scholar]
- 63.Choi EY, Yeo BT, Buckner RL. The organization of the human striatum estimated by intrinsic functional connectivity. J Neurophysiol 2012;108:2242–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schmahmann JD, Pandya DN. Disconnection syndromes of basal ganglia, thalamus, and cerebrocerebellar systems. Cortex 2008;44:1037–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cacciari C, Moraschi M, Di Paola M, et al. White matter microstructure and apathy level in amnestic mild cognitive impairment. J Alzheimers Dis 2010;20:501–7. [DOI] [PubMed] [Google Scholar]
- 66.Damoiseaux JS, Rombouts SA, Barkhof F, et al. Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci U S A 2006;103:13848–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schroeter ML, Laird AR, Chwiesko C, et al. Conceptualizing neuropsychiatric diseases with multimodal data-driven meta-analyses - the case of behavioral variant frontotemporal dementia. Cortex 2014;57:22–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Amodio DM, Frith CD. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci 2006;7:268–77. [DOI] [PubMed] [Google Scholar]
- 69.Zhou J, Seeley WW. Network dysfunction in Alzheimer’s disease and frontotemporal dementia: implications for psychiatry. Biol Psychiatry 2014;75:565–73. [DOI] [PubMed] [Google Scholar]
- 70.Schroeter ML, Vogt B, Frisch S, et al. Executive deficits are related to the inferior frontal junction in early dementia. Brain 2012;135:201–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Starkstein SE. Apathy in Parkinson’s disease: diagnostic and etiological dilemmas. Mov Disord 2012;27:174–8. [DOI] [PubMed] [Google Scholar]


