Abstract
Within the current theoretical frameworks used in grief and bereavement research, it remains unclear which individual factors confer risk for specific bereavement-related mental health problems, such as posttraumatic stress disorder (PTSD) and prolonged grief disorder. The present study investigated individual differences in motivational sensitivity and self-regulatory processes in a sample of 326 bereaved individuals who experienced sudden and/or unexpected death losses. We (1) examined associations between behavioral activation system (i.e., orientation to rewarding stimuli) and behavioral inhibition system (orientation to aversive stimuli) sensitivity and bereavement-related mental health problems (i.e., PTSD and prolonged grief symptoms), and (2) explored whether experiential avoidance (i.e., effortful avoidance of internal stimuli) would moderate such associations. Results revealed PTSD was more strongly associated with behavioral inhibition system sensitivity, while prolonged grief symptoms more strongly associated with behavioral activation system sensitivity. In particular, drive sensitivity – a dimension of the behavioral activation system – appeared uniquely associated with prolonged grief symptoms, especially in those who endorsed high experiential avoidance. Findings support a theoretical reconceptualization of prolonged grief as a reward system disorder. This reconceptualization may aid in further understanding mechanisms of bereavement-related mental health problems and related risk factors.
Keywords: bereavement, motivational sensitivity, experiential avoidance, PTSD, prolonged grief, sudden loss
1. Introduction
Surviving the death of a loved one can be one of life’s most painful experiences, often leading to a variety of intense and functionally impairing physical, cognitive, and emotional reactions immediately following the death (Sbarra and Hazan, 2008). Although highly distressing, these reactions will gradually diminish in frequency and intensity for the majority of bereaved persons (Bonanno, 2004). For a subset of bereaved persons, however, acute grief reactions can take a more chronic course, resulting in psychiatric complications such as posttraumatic stress disorder (PTSD; see Atwoli et al., 2017) and prolonged, or complicated, grief disorder (Prigerson et al., 2009). Various labels have been applied to prolonged grief, which is currently called persistent complex bereavement disorder in the DSM-5 and is listed as a condition recommended for further study (American Psychiatric Association [APA], 2013). The World Health Organization, however, has chosen to use the term prolonged grief disorder to describe this syndrome in the ICD-11 (Killikelly and Maercker, 2017). So, for consistency, we use the terms prolonged grief disorder and prolonged grief symptoms throughout this manuscript. Survivors of sudden, unexpected deaths in particular appear to be at especially increased risk for complications in bereavement such as PTSD and prolonged grief (e.g., Djelantik et al., 2017). While these conditions often co-occur (e.g., McDevitt-Murphy et al., 2012; Rheingold and Williams, 2015), PTSD and prolonged grief disorder differ in several important ways and are thought to operate via different neurobiological and psychological processes. For example, PTSD as a condition is associated with dysregulation in stress-related neural circuitry (e.g., de Kloet et al., 2006) and includes symptoms such as intrusive imagery of the death event, avoidance of trauma-related cues, altered mood and cognition, and hypervigilance (APA, 2013), while prolonged grief disorder is associated with simultaneous activation of both pain and reward-related neural circuitry (O’Connor et al., 2008) and includes symptoms such as intense yearning for a deceased loved one, difficulty accepting the loss, and avoidance of the reality of the loss (Prigerson et al., 2009). It remains unclear, however, why some survivors experience bereavement-related PTSD and/or prolonged grief symptoms while others gradually recover after a loss. Better understanding individual differences in self-regulatory processes and motivational sensitivity, or the degree to which individuals desire particular reinforcers and can tolerate aversive stimuli (Reiss and Havercamp, 1996), may shed light on individual factors that confer risk for specific bereavement-related mental health problems like PTSD and prolonged grief.
Reinforcement sensitivity theory (Gray and McNaughton, 2000) suggests that motivational sensitivity is driven by neurobiological systems including the behavioral activation system (orientation to rewarding stimuli) and the behavioral inhibition system (orientation to aversive stimuli). Behavioral activation and behavioral inhibition system sensitivity have each been associated with increased risk for the development of psychopathology. More specifically, behavioral activation system sensitivity is associated with increased risk for problematic externalizing behaviors characterized by the pursuit of reward (e.g., substance use disorders, eating disorders) and behavioral inhibition system sensitivity with increased risk for internalizing behaviors characteristic of mood and anxiety disorders (see Bijttebier et al., 2009, for review). So, temperamental differences in motivational sensitivity likely affect how individuals adjust to stressors like bereavement. Although no research to date has examined associations between motivational sensitivity and prolonged grief symptoms, several studies have established an association between behavioral inhibition system sensitivity and PTSD symptoms among trauma survivors more broadly. For example, Maack et al. (2012) found an association between behavioral inhibition system sensitivity and probable PTSD status in a sample of 291 undergraduates with a lifetime history of trauma exposure. Their analyses further revealed that this association was fully mediated by experiential avoidance. Experiential avoidance describes a self-regulatory process conceptualized as effortful avoidance of aversive internal stimuli, including aversive thoughts, emotions, and/or bodily sensations (e.g., Hayes et al., 1996). As with motivational sensitivity, experiential avoidance has been associated with the development and maintenance of various forms of psychopathology (Chawla and Ostafin, 2007), and evidence suggests that self-regulatory processes like experiential avoidance may interact with motivational sensitivity to increase risk for psychopathology (Bijttebier et al., 2009). So, following trauma exposure, individuals with increased behavioral inhibition system sensitivity may be more likely to avoid internal and external trauma-related stimuli that evoke strong, negative affect, thus increasing risk for PTSD.
Similarly, Pickett et al. (2011) explored associations between motivational sensitivity and PTSD symptoms in a sample of 851 trauma-exposed female college students (43% of whom identified their most traumatic lifetime event as the sudden death of a loved one) and found an association between behavioral inhibition system sensitivity and PTSD symptoms. Rather than modeling experiential avoidance as a potential mediator, though, experiential avoidance was modeled as a potential moderator of the association between behavioral inhibition system sensitivity and PTSD symptoms. Results indicated that experiential avoidance moderated the association between behavioral inhibition system sensitivity and PTSD symptoms such that individuals high in experiential avoidance and high in behavioral inhibition system sensitivity reported more severe PTSD symptoms than those high in experiential avoidance and low in behavioral inhibition system sensitivity. There was no association observed between behavioral inhibition system sensitivity and PTSD among those low in experiential avoidance. Overall, these studies suggest that behavioral inhibition system sensitivity may serve as an important risk factor in the development of PTSD symptoms among trauma-exposed individuals, including survivors of sudden, traumatic losses, but that self-regulatory mechanisms like experiential avoidance may interact with motivational sensitivity to increase risk for trauma-related psychopathology.
While behavioral inhibition system sensitivity may interact with experiential avoidance to increase risk for PTSD symptoms, much less is known about the association between prolonged grief symptoms, motivational sensitivity, and self-regulatory processes. Unlike PTSD symptoms, there is reason to believe that prolonged grief symptoms may be more strongly associated with behavioral activation system sensitivity than with behavioral inhibition system sensitivity given that behavioral activation system sensitivity is associated with externalizing behaviors characterized by the pursuit of reward. For example, yearning is among the first reactions many grievers experience, and, at least initially, may be partially motivated by positive reinforcement mechanisms (e.g., pictures of a loved one elicit yearning associated with positively reinforcing aspects of the relationship with the deceased; Sbarra and Hazan, 2008). Among grievers with more pronounced prolonged grief symptoms, though, there may be a shift from positive to negative reinforcement in the motivational aspects of yearning, similar to the shift observed in behaviors characteristic of reward system disorders (Hardcastle, 2017). That is, individuals with severe prolonged grief symptoms may experience distress and then yearn for the deceased or seek out reminders of the deceased in an effort to alleviate distress. Thus, a model of prolonged grief disorder as a reward system disorder suggests that aspects of behavioral activation system sensitivity may increase vulnerability to prolonged grief symptoms and that this association is maintained by self-regulatory efforts to avoid negative affect.
The purpose of this study is to examine the association between motivational sensitivity and bereavement-related mental health problems (PTSD and prolonged grief symptoms) among a sample of college students with a history of sudden, unexpected loss. We also sought to explore whether experiential avoidance would moderate the association between motivational sensitivity and PTSD and prolonged grief symptoms. In line with previous research, we hypothesized that experiential avoidance would moderate the association between behavioral inhibition system sensitivity and PTSD symptoms and that experiential avoidance would moderate the association between behavioral activation system sensitivity and prolonged grief symptoms.
2. Method
2.1. Participants
Participants in this study were 326 undergraduate students from a Midwestern university who reported a history of sudden, unexpected death loss as part of a larger research study evaluating exposure to traumatic stress and college adjustment. The sample was primarily female (80.1%) with ages ranging from 18 to 54 years (M = 21.54, SD = 4.75). Participants represented a range of racial backgrounds, with 68.1% identifying as White, 20.2% identifying as African American, 7.7% identifying as Asian, 2.1% identifying as American Indian, and 7.7% identifying as other. In terms of ethnicity, 9.5% of the sample identified as being of Hispanic origin or background. Participants included in the present study endorsed having experienced at least one sudden, unexpected loss. The mean age at the time of loss (or the worst loss in the case of persons endorsing multiple sudden deaths) was 15.24 (SD = 5.08), with a mean of 6.26 (SD = 4.92) years since experiencing the loss. Types of loss endorsed included deaths due to sudden illness (68.4%), suicide or overdose (37.4%), accident (36.8%), murder (16.9%), war/riot/terrorism (2.8%), and natural disaster (1.8%). Note that these percentages add up to greater than 100% because some survivors reported a history of multiple, sudden losses. Participants’ relationships to the deceased varied with 35.3% (n = 115) identifying the deceased as a close friend, 24.2% (n = 79) a grandparent, 24.2% (n = 79) another relative, 8.9% (n = 29) a parent, 1.8% (n = 6) a sibling, .6% (n = 2) a child, and .3% (n =1) a significant other.
2.2. Procedures
All procedures were approved by the university’s Institutional Review Board. Participants were recruited from the Psychology subject pool systems (SONA system) as part of a larger project developed to assess the prevalence of exposure to potentially traumatic events and associations between event characteristics and trauma-related mental health problems during the emerging adulthood period. Before engaging in the study, all individuals provided electronic consent to participate. Surveys were completed in one online session using REDCap, a HIPAA compliant and secure web-based application for data collection (Harris et al., 2009). Surveys took approximately 45 minutes to complete. Participants received research credit for participating in the survey.
2.3. Measures
Loss History.
History of sudden, unexpected loss was assessed using six questions from the National Stressful Events Survey (Kilpatrick et al., 2011). This self-administered survey contains 25 closed-ended questions evaluating exposure to potentially traumatic experiences. Six questions assess lifetime history of sudden, unexpected loss, including homicide (“Has a close family member or close friend of yours ever been murdered or killed by a drunk driver?”), fatal accidents (“Has a close family member or close friend of yours ever been killed in a plane crash, car wreck, fire, or other accident?”), suicide and/or drug overdose (“Has a close family member or close friend of yours ever committed suicide or died from an overdose of alcohol or drugs?”), war and/or terrorism-related deaths (“Has a close family member or friend of yours ever been killed in a war, riot, or terrorist attack?”), natural disaster-related deaths (“Has a close family member or friend of yours ever been killed by a natural disaster such as an earthquake or hurricane?”), and sudden, natural death (“Has a close family member or close friend of yours ever died suddenly and unexpectedly due to a heart attack, stroke, or cancer?”). If the participant endorsed multiple types of losses, they were prompted to indicate which death was the worst or most stressful loss for them personally.
Motivational Sensitivity.
The Behavioral Activation System/Behavioral Inhibition System Scale (Carver and White, 1994) is a 24-item, self-report measure based on a Likert scale ranging from 1 (very true for me) to 4 (very false for me). These items measure affective responses to impending reward (behavioral activation system) and punishment (behavioral inhibition system). Behavioral activation system subscales include drive (4 items), which measures a person’s motivation to follow goals in life (e.g., “I go out of my way to get things I want”), fun seeking (4 items), which measures orientation towards excitement seeking (e.g., “I often act on the spur of the moment”), and reward responsiveness (5 items), which measures positive reward reactions (e.g., “When good things happen to me, it affects me strongly”). The behavioral inhibition system subscale (7 items) measures a preoccupation with negative repercussions (e.g., “I worry about making mistakes”). The measure exhibited adequate internal consistency with subscale alphas ranging from .63 to .77 in the present sample.
Experiential Avoidance.
The Brief Experiential Avoidance Questionnaire (Gamez et al., 2014) is a 15-item, self-report measure based on a Likert scale ranging from 1 (strongly disagree) to 6 (strongly agree). Items include questions such as “When unpleasant memories come to me, I try to put them out of my mind” and “I feel disconnected from my emotions”. The measure showed adequate internal consistency (α = .79) in the present study.
PTSD.
The PTSD Checklist (Weathers et al., 2013) is a 20-item, self-report scale of PTSD symptoms. Participants indicate how much they have been bothered by their symptoms over the past month using a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). Questions on the PCL-5 map onto the DSM-5 (APA, 2013) criteria for PTSD. Total scores of 33 or higher indicate a positive screen for PTSD (Bovin et al., 2016). The scale exhibited excellent internal consistency (α = .96) in the present study.
Prolonged Grief.
The Prolonged Grief-13 (Prigerson et al., 2009) is a 13-item self-report measure assessing for prolonged grief symptoms. Part one of the scale examines frequency of symptoms in the past month (e.g., “In the past month, how often have you felt stunned, shocked, or dazed by your loss?”) on a 5-point Likert scale ranging from 1 (not at all) to 5 (several times a day). Part two of the scale assesses the individual’s current feelings toward items (e.g., “Have you had trouble accepting the loss?”) rated on a 5-point Likert scale ranging from 1 (not at all) to 5 (overwhelmingly). In line with previous studies using this instrument with bereaved samples (e.g., Tomarken et al., 2012), a cut-score of 26 was used to establish prolonged grief “caseness.” The scale exhibited good internal consistency with a Cronbach's alpha of .89 in the present study.
3. Results
3.1. Descriptive Statistics and Group Comparisons by Mental Health Screening Status
As shown in Table 1, descriptive statistics and group comparison analyses were run to examine potential differences among participants screening positive for PTSD (35.4%; n = 115) and prolonged grief (14.1%; n = 46) and those screening negative. Comparison analyses were performed to examine differences between demographic variables (i.e., gender, race, and age), mental health variables (i.e., PTSD and prolonged grief symptom severity), motivational sensitivity (i.e., behavioral activation system and behavioral inhibition system subscales), and experiential avoidance. No significant differences were found on demographic variables as a function of PTSD or prolonged grief screening status. In regard to behavioral activation and behavioral inhibition system scale scores, the PTSD positive and negative groups showed significant differences on the behavioral inhibition system scale, with individuals screening positive for PTSD scoring higher on average than those individuals screening negative. Fun seeking scores were significantly different between the prolonged grief disorder positive and negative groups with prolonged grief positive participants scoring higher on average than prolonged grief negative participants. Experiential avoidance scores also differed as a function of mental health screening status, with PTSD positive and prolonged grief positive participants both scoring higher on experiential avoidance than individuals screening negative for each respective condition. In terms of mental health variables, significant differences were found such that individuals screening positive for PTSD scored higher on average for both PTSD and prolonged grief symptom severity compared to the PTSD negative group. Individuals screening positive for prolonged grief also scored higher on both mental health outcome variables than those individuals screening negative for prolonged grief.
Table 1.
Descriptive statistics for full sample and by PGD and PTSD screening status
| Variables | Full Sample N = 326 n (%) |
PGD + n = 46 n (%) |
PGD − n = 279 n (%) |
χ2 | PTSD + n = 115 n (%) |
PTSD − n = 205 n (%) |
χ2 |
|---|---|---|---|---|---|---|---|
| Gender | .10 | 3.05 | |||||
| Men | 65 (19.9) | 10 (21.7) | 55 (19.7) | 17 (14.8) | 47 (22.9) | ||
| Women | 261 (80.1) | 36 (78.3) | 224 (80.3) | 98 (85.2) | 158 (77.1) | ||
| Race | 1.35 | .25 | |||||
| Non-white | 138 (42.3) | 23 (50) | 114 (40.9%) | 51 (44.3) | 85 (41.5) | ||
| White | 188 (57.7) | 23 (50) | 165 (59.1) | 64 (55.7) | 120 (58.5) | ||
| M (SD) | M (SD) | M (SD) | t | M (SD) | M (SD) | t | |
| Age | 21.54 (4.75) | 21.43 (4.26) | 21.55 (4.84) | −.16 | 21.33 (5.15) | 21.59 (4.53) | −.47 |
| BAS-Drive | 11.35 (2.18) | 11.76 (2.35) | 11.28 (2.16) | 1.39 | 11.62 (2.06) | 11.24 (2.20) | 1.51 |
| BAS-Fun | 11.82 (2.27) | 12.65 (1.82) | 11.68 (2.32) | 2.71** | 12.01 (2.14) | 11.72 (2.34) | 1.10 |
| BAS-Reward | 17.41 (1.98) | 17.41 (2.06) | 17.41 (1.97) | .01 | 17.31 (2.18) | 17.46 (1.83) | −.66 |
| BIS | 21.82 (3.71) | 22.52 (3.49) | 21.71 (3.75) | 1.37 | 23.02 (3.65) | 21.16 (3.60) | 4.42** |
| BEAQ | 52.46 (10.95) | 56.8 (11.79) | 51.75 (10.68) | 2.90** | 57.68 (10.22) | 49.43 (10.27) | 6.90** |
| PCL-5 | 25.83 (18.44) | 42 (16.20) | 23.21 (17.45) | 6.76** | 46.53 (10.94) | 14.22 (9.37) | 27.84** |
| PG-13 | 18.00 (7.25) | 32.65 (4.67) | 15.58 (4.04) | 25.98** | 21.35 (8.86) | 16.09 (5.31) | 5.80** |
Note.
p < .05.
p < .01.
BAS-Drive = Behavioral Activation System-Drive subscale; BAS-Fun = Behavioral Activation System-Fun Seeking subscale; BAS-Reward = Behavioral Activation System-Reward Responsiveness subscale; and BIS = Behavioral Inhibition System subscale; BEAQ = Brief Experiential Avoidance Questionnaire; PCL-5 = PTSD Checklist; PG-13 = Prolonged Grief-13. Cell sizes vary slightly due to missing data.
3.2. Health Outcomes
Associations between demographic variables, behavioral activation system and behavioral inhibition system scale scores, experiential avoidance, and mental health outcomes are presented in Table 2. In terms of behavioral activation system subscales, drive subscale scores were significantly and positively associated with prolonged grief symptoms, and fun seeking subscale scores were positively associated with experiential avoidance. No behavioral activation system subscales were associated with PTSD symptoms. Behavioral inhibition system scores were positively associated with PTSD symptoms and experiential avoidance, but not prolonged grief symptoms. In terms of demographic variables, age was negatively associated with fun seeking and behavioral inhibition system scores. Identifying as White was also positively associated with behavioral inhibition system scores. Because of significant associations with variables of interest, age and race (non-White/White) were included as covariates in regression analyses.
Table 2.
Correlations between demographic variables, motivational sensitivity, experiential avoidance, and mental health outcomes
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | ||||||||
| 2. Race | .06 | -- | |||||||
| 3. BAS-Drive | −.08 | −.07 | -- | ||||||
| 4. BAS-Fun | −.13* | −.03 | .43** | -- | |||||
| 5. BAS-Reward | −.04 | −.07 | .44** | .26** | -- | ||||
| 6. BIS | −.16** | .15** | −.11* | −.06 | .17** | -- | |||
| 7. BEAQ | −.09 | −.02 | .07 | .18** | .09 | .33** | -- | ||
| 8. PCL-5 | −.04 | −.05 | .06 | .10 | .01 | .33** | .42** | -- | |
| 9. PG-13 | −.05 | −.08 | .11* | .09 | −.06 | .04 | .26** | .43** | -- |
Note.
p < .05.
p < .01.
Race was measured using a dichotomous variable where non-white = 0 and white = 1. BAS-Drive = Behavioral Activation System-Drive subscale; BAS-Fun = Behavioral Activation System-Fun Seeking subscale; BAS-Reward = Behavioral Activation System-Reward Responsiveness subscale; and BIS = Behavioral Inhibition System subscale; BEAQ = Brief Experiential Avoidance Questionnaire; PCL-5 = PTSD Checklist; PG-13 = Prolonged Grief-13. Cell sizes vary slightly due to missing data.
3.3. Regression Analyses
A series of multiple regression analyses were used to examine whether experiential avoidance moderated the association between various facets of motivational sensitivity and PTSD and prolonged grief symptoms. As shown in Table 3, behavioral activation system and behavioral inhibition system subscale scores, experiential avoidance scores, and four interaction terms modeling the interaction between experiential avoidance scores and each behavioral activation system and behavioral inhibition system subscale were included as independent variables in each model. PTSD and prolonged grief symptoms were modeled as dependent variables in separate analyses. In the first model, a statistically significant main effect was found for behavioral inhibition system scores and PTSD symptoms where higher behavioral inhibition system scores were associated with more severe PTSD scores. A main effect was also found for experiential avoidance such that higher experiential avoidance scores were associated with more severe PTSD symptoms. Lastly, a main effect was found for reward responsiveness where lower reward responsiveness scores were associated with more severe PTSD scores. No experiential avoidance × behavioral activation/behavioral inhibition system interactions were statistically significant.
Table 3.
Regression analyses modeling associations between demographics, motivational sensitivity, experiential avoidance, and mental health outcomes
| Variable | β | t | P |
|---|---|---|---|
| PCL | |||
| Age | .04 | .79 | .43 |
| Non-white vs. White | −.10 | −1.86 | .06 |
| BAS-Drive | .10 | 1.54 | .12 |
| BAS-Fun | .06 | .98 | .33 |
| BAS-Reward | −.12 | −2.04 | .04 |
| BIS | .27 | 4.69 | <.01 |
| BEAQ | .31 | 5.6 | <.01 |
| BEAQ × BAS-Drive | .04 | .56 | .57 |
| BEAQ × BAS-Fun | −.04 | −.74 | .46 |
| BEAQ × BAS-Reward | −.01 | −.21 | .83 |
| BEAQ × BIS | .07 | 1.37 | .17 |
| PG-13 | |||
| Age | −.02 | −.31 | .76 |
| Non-white vs. White | −.07 | −1.32 | .19 |
| BAS Drive | .16 | 2.34 | .02 |
| BAS Fun | .01 | .21 | .83 |
| BAS Reward | −.16 | −2.51 | .01 |
| BIS | .01 | .08 | .94 |
| BEAQ | .23 | 3.85 | <.01 |
| BEAQ × BAS-Drive | .15 | 2.16 | .03 |
| BEAQ × BAS-Fun | −.10 | −1.74 | .08 |
| BEAQ × BAS-Reward | −.01 | −.16 | .88 |
| BEAQ × BIS | .07 | 1.24 | .22 |
Note. BAS-Drive = Behavioral Activation System-Drive subscale; BAS-Fun = Behavioral Activation System-Fun Seeking subscale; BAS-Reward = Behavioral Activation System-Reward Responsiveness subscale; and BIS = Behavioral Inhibition System subscale; BEAQ = Brief Experiential Avoidance Questionnaire; PCL-5 = PTSD Checklist; PG-13 = Prolonged Grief-13. Cell sizes vary slightly due to missing data.
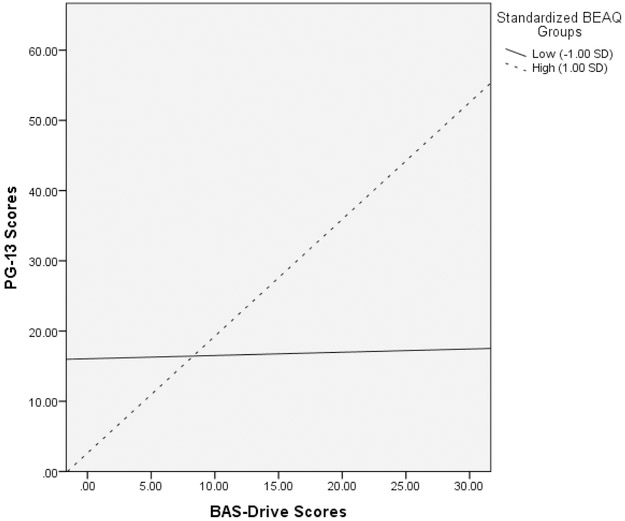
In terms of prolonged grief scores, a main effect was found between reward responsiveness and prolonged grief symptoms such that lower reward responsiveness scores were associated with more severe prolonged grief symptoms. A statistically significant experiential avoidance x drive interaction also emerged. The experiential avoidance × fun seeking interaction term was marginally associated with prolonged grief symptoms. A simple slopes analysis was conducted to probe the experiential avoidance × drive interaction. As depicted in Figure 1, results indicated that drive sensitivity was significantly and positively associated with prolonged grief symptoms among participants high in experiential avoidance (B = 1.37, β = .19, p = .009) but not among participants low in experiential avoidance (B = −.00, β = .00, p = .999). A simple slopes analysis was also conducted to probe the marginally significant experiential avoidance × reward responsiveness interaction. Results indicated that reward responsiveness was not associated with prolonged grief symptoms among participants high in experiential avoidance (B = −.22, β = −.03, p = .654) or participants low in experiential avoidance (B = −.96, β = −.13, p = .087).
Figure 1.
Associations between BAS-Drive sensitivity and PGD symptoms at high and low levels of EA.
Note. PG-13 = Prolong Grief-13 total scores; BAS-Drive = Behavioral Activation System-Drive subscale; BEAQ = Brief Experiential Avoidance Questionnaire.
4. Discussion
Researchers have long known that self-regulatory processes such as experiential avoidance may combine with other personal characteristics like motivational sensitivity to increase risk for mental health problems (e.g., Bijttebier et al., 2009). To our knowledge, this study is the first to explore how motivational sensitivity, experiential avoidance, and the interaction between the two, are uniquely and differentially associated with PTSD and prolonged grief symptoms in a large sample of individuals with a history of sudden loss. Consistent with our hypotheses, PTSD symptoms were more strongly associated with behavioral inhibition system sensitivity, while behavioral activation system sensitivity, and drive sensitivity in particular, was more uniquely associated with prolonged grief symptoms. This association appeared to be strongest among those individuals high in experiential avoidance.
To contextualize these findings, scores on relevant symptom measures suggest that our sample was comparable to other samples of trauma-exposed and bereaved college students (e.g., Eddinger and McDevitt-Murphy, 2017; Maccallum et al., 2015). Similar to findings from other college student samples, behavioral inhibition system sensitivity was also associated with PTSD symptoms (e.g., Maack et al., 2012; Pickett et al., 2011) but not with prolonged grief symptoms. Facets of behavioral activation system sensitivity, however, were associated with prolonged grief in bivariate analyses, such that drive sensitivity was positively associated with prolonged grief symptoms. Interestingly, bereaved participants screening positive for prolonged grief evidenced higher scores on the fun seeking sensitivity scale than individuals screening negative for prolonged grief. No statistically significant correlation emerged between fun seeking and prolonged grief symptoms, though, so additional research is needed to better understand the association between fun seeking and prolonged grief symptoms.
Consistent with previous research (e.g., Maack et al., 2012; Pickett et al., 2011), behavioral inhibition system sensitivity and experiential avoidance were both associated with PTSD symptoms even after adjusting for demographic variables and other facets of motivational sensitivity. In contrast to previous research, experiential avoidance did not appear to moderate the association between behavioral inhibition system sensitivity and PTSD symptoms. These contrasting findings may be due to several factors, including the use of different assessment instruments across studies and sample differences (all of the participants in this study identified a history of sudden, unexpected loss). Nevertheless, these findings join with other studies to suggest that motivational sensitivity to aversive stimuli and efforts to avoid aversive stimuli independently increase risk for PTSD symptoms.
While behavioral inhibition system sensitivity was uniquely associated with PTSD symptoms, our findings further revealed that aspects of behavioral activation system sensitivity were associated with both PTSD and prolonged grief symptoms. More specifically, in multivariate analyses, lower reward responsiveness was uniquely associated with greater PTSD and prolonged grief symptom severity. These findings are consistent with previous research linking PTSD with blunted reward expectancies and satisfaction (e.g., Hopper et al., 2008), although, to our knowledge, this is one of the first studies linking diminished reward responsiveness with prolonged grief severity. In the case of PTSD symptoms, these findings intuitively make sense in that contemporary models of PTSD argue that heightened arousal to threat (perhaps at least partially driven by elevated behavioral inhibition system sensitivity) increases the threshold at which individuals will respond to pleasant, rewarding stimuli, thus increasing the likelihood of behavioral withdrawal and restricted positive affect characteristic of PTSD-related changes in mood and cognition (see Litz and Gray, 2002). Although a distinct syndrome from PTSD, it is worth noting that prolonged grief also includes similar symptoms of behavioral withdrawal and restricted affect (e.g., emotional numbing, feeling that life is unfulfilling and meaningless; Prigerson et al., 2009). Thus, bereaved individuals with inhibited reward responsiveness may be less responsive to reinforcement derived from restoration-oriented activities such as engaging in pleasant activities, developing new relationships, etc., after the death of a loved one (Stroebe and Schut, 1999), leading to the avoidance and restricted positive affect characteristic of prolonged grief.
Having mentioned that behavioral withdrawal and avoidance are features of both PTSD and prolonged grief, it is not surprising then that experiential avoidance was associated with both PTSD and prolonged grief symptoms, as has been demonstrated in other studies with traumatically and suddenly bereaved samples (Nam, 2016; Pickett et al., 2011). As hypothesized, experiential avoidance also moderated the association between drive sensitivity and prolonged grief symptoms in our sample such that greater drive sensitivity was associated with greater prolonged grief symptoms among those high in experiential avoidance but not those low in experiential avoidance. As a specific facet of the behavioral activation system, the drive scale assesses the extent to which an individual persists in the pursuit of desired goals, and data from experimental research has shown that bereaved individuals with prolonged grief disorder evidence greater approach-related tendencies when confronted with grief-related stimuli compared to individuals without prolonged grief disorder (Maccallum et al., 2015). To some extent, such approach tendencies are likely a normal response to separation and loss. Indeed, in the context of acute loss, responses are often characterized by active protest and “search behaviors” that seek to bring about reunion with the lost loved one (Sbarra and Hazan, 2008). While these behaviors often give way to more passive despair, active proximity seeking in the form of seeking out comforting reminders of the lost love one may continue among those individuals with more sensitive drive systems who may be more likely to remain steadfast in their pursuit of reconnection with their lost loved one. Our findings suggest that this may be especially true among individuals high in experiential avoidance.
Taken together these findings provide initial support for theoretical conceptualizations of prolonged grief disorder as a reward system disorder where individuals with greater drive sensitivity continue seeking out positively reinforcing reminders of the lost attachment with the deceased loved one, especially when such yearning and proximity seeking occurs in the context of avoiding negative affect. Whether the association between drive sensitivity and prolonged grief symptoms can be more specifically explained by subsequent increases in yearning and proximity seeking behavior, though, remains an important topic worthy of future investigation. While we believe that these findings support theoretical conceptualizations of prolonged grief disorder as a reward system disorder, we should mention here that this reward system disorder conceptualization of prolonged grief is far from universally accepted within the bereavement field. This conceptualization is only one of several alternative conceptualizations of prolonged grief, and there even remains considerable resistance to the idea that prolonged grief reactions like yearning and proximity seeking can be “disordered” regardless of their intensity and duration given that these are fully expected and natural responses to the loss of a loved one. In light of these ongoing debates, we hope this conceptualization in some way helps advance our field by shedding light on who is most likely to experience severe prolonged grief reactions and why they may be most vulnerable to the unremitting pain of prolonged grief.
In terms of clinical implications, this study suggests that bereaved persons with severe prolonged grief symptoms may benefit from interventions that promote goal disengagement and reengagement efforts. The ability to adjust one’s goals and reengage with other new goals, especially when one’s current goals are unattainable, has been associated with overall psychological well-being (e.g., Wrosch et al., 2003). Thus, helping bereaved persons with prolonged grief identify and reengage with new life goals following the death of a loved one may help promote overall recovery and psychological well-being, especially for those survivors that continue to experience intense yearning and proximity-seeking behaviors with the goal of restoring a relationship with a lost loved one as they were before the death. Recognizing the need to help bereaved persons identify and pursue new life goals, researchers have demonstrated that interventions such as behavioral activation that seek to help reengage bereaved persons in personally meaningful and pleasant activities are effective in the treatment of prolonged grief symptoms (e.g., Acierno et al., 2012; Papa, et al., 2013). These findings may shed light on possible mechanisms of action underlying such interventions.
Despite the important contribution made by this study, there are several limitations worth mentioning. First, these data are cross-sectional and based on self-reported symptoms and perceptions of motivational sensitivity and experiential avoidance. Thus, we cannot draw firm conclusions about causation from our data as it may well be the case that scores on measures of motivational sensitivity and experiential avoidance are influenced by greater symptom severity rather than vice versa. Second, we did not specifically test whether yearning and proximity-seeking effectively mediate the association between drive sensitivity and prolonged grief symptoms among those bereaved individuals high in experiential avoidance, although this is an important area for future work. Third, revised conceptualizations of reinforcement sensitivity theory have proposed a third neurobiological system – the fight-flight-freeze system – along with the behavioral activation and behavioral inhibition systems (Gray and McNaughton, 2000). Although our assessment of motivational sensitivity only included scales assessing the two original behavioral activation and behavioral inhibition systems, future studies may benefit from assessing motivational sensitivity using the revised reinforcement sensitivity model. Fourth, because we did not assess for Criterion A for PTSD, we cannot be sure that PTSD symptoms were directly attributable to the respondent’s history of sudden loss over and above other potentially traumatic events. Nevertheless, evidence from epidemiological studies suggest that sudden losses throughout the lifespan increase risk for PTSD and other psychiatric disorders, even after controlling for exposure to other, potentially traumatic events (Keyes et al., 2014). So, even in cases where the index trauma might have involved a traumatic incident unrelated to the death of a loved one, it seems likely that PTSD symptom severity could at least be exacerbated by experiences like the sudden death of a loved one. Lastly, data were collected from a college student sample, and the extent to which these data generalize to community-based samples of sudden loss survivors is unclear. Despite these limitations, this study helps shed light on key individual differences that may help predict how an individual will respond to the sudden loss of a loved one.
Highlights.
Individual differences in motivational sensitivity may help explain differential risk for complications in bereavement, such as posttraumatic stress and prolonged grief.
Experiential avoidance was associated with more severe PTSD and prolonged grief symptoms.
Experiential avoidance moderated the association between drive sensitivity and prolonged grief symptoms, where drive sensitivity was uniquely associated with prolonged symptoms among those high, but not low, in experiential avoidance.
Experiential avoidance and behavioral inhibition system sensitivity were both uniquely associated with PTSD symptoms, but did not interact to predict more severe PTSD symptoms.
Acknowledgments
Funding
Manuscript preparation was supported by NIH Loan Repayment Award L30 MH104802. (PI: Williams).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acierno R, Rheingold A, Amstadter A, Kurent J, Amelia E, Resnick H, … Lejuez C, 2012. Behavioral activation and therapeutic exposure for bereavement in older adults. Am. J. Hosp. Palliaiat. Me 29, 13–25. doi: 10.1177/1049909111411471 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Atwoli L, Stein DJ, King A, Petukhova M, Aguilar-Gaxiola S, Alonso J,…Kessler RC, 2017. Posttraumatic stress disorder associated with unexpected death of a loved one: Cross-national findings from the World Mental Health Surveys. Depress. Anxiety 34, 315–326. doi: 10.1002/da.22579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bijttebier P, Beck I, Claes L, Vandereycken W, 2009. Gray's Reinforcement Sensitivity Theory as a framework for research on personality–psychopathology associations. Clin. Psychol. Rev 29, 421–430. doi: 10.1016/j.cpr.2009.04.002 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, 2004. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol 59, 20–28. doi: 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM, 2016. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in Veterans. Psychol. Assessment 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Carver CS, White TL, 1994. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J. Pers. Soc. Psychol 67, 319–333. doi: 10.1037/0022-3514.67.2.319 [DOI] [Google Scholar]
- Chawla N, Ostafin B, 2007. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. J. Clin. Psychol 63, 871–890. doi: 10.1002/jclp.20400 [DOI] [PubMed] [Google Scholar]
- De Kloet CS, Vermetten E, Geuze E, Kavelaars A, Heijnen CJ, Westenberg HG, 2006. Assessment of HPA-axis function in posttraumatic stress disorder: Pharmacological and non-pharmacological challenge tests, a review. J. Psychiat. Res 40, 550–567. doi: 10.1016/j.jpsychires.2005.08.002 [DOI] [PubMed] [Google Scholar]
- Djelantik AMJ, Smid GE, Kleber RJ, Boelen PA, 2017. Symptoms of prolonged grief, post-traumatic stress, and depression after loss in a Dutch community sample: A latent class analysis. Psychiat. Res 247, 276–281. doi: 10.1016/j.psychres.2016.11.023 [DOI] [PubMed] [Google Scholar]
- Eddinger JR, McDevitt-Murphy ME, 2017. A confirmatory factor analysis of the PTSD Checklist 5 in veteran and college student samples. Psychiat. Res 255, 219–224. doi: 10.1016/j.psychres.2017.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gámez W, Chmielewski M, Kotov R, Ruggero C, Suzuki N, Watson D, 2014. The brief experiential avoidance questionnaire: Development and initial validation. Psychol. Assessment 26, 35–45. doi: 10.1037/a0034473 [DOI] [PubMed] [Google Scholar]
- Gray JA, McNaughton N, 2000. The neuropsychology of anxiety (2nd ed.). New York, NY: Oxford University Press. [Google Scholar]
- Hardcastle VG, 2017. Pain, chronic pain, and suffering In Solomon M, Simon JR, and Kincaid H (Eds.), The Routledge companion to philosophy of medicine (pp. 124–133). New York, NY: Routledge. [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, 2009. Research Electronic Data Capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform 42, 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K, 1996. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. J. Consult. Clin. Psych 64, 1152–1168. doi: 10.1037/0022-006X.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Hopper JW, Pitman RK, Su Z, Heyman GM, Lasko NB, Macklin ML, Orr SP, Lukas SE, Elman I, 2008. Probing reward function in posttraumatic stress disorder: Expectancy and satisfaction with monetary gains and losses. J. Psychiatr. Res 42, 802–807. doi: 10.1016/j.jpsychires.2007.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear MK, 2014. The burden of loss: Unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am. J. Psychiatry 171, 864–871. doi: 10.1176/appi.ajp.2014.13081132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killikelly C, Maercker A, 2017. Prolonged grief disorder for ICD-11: The primacy of clinical utility and international applicability. Eur. J. Psychotraumatol 8, 1476441. doi: 10.1080/20008198.2018.1476441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Baber B, Guille C, Gros K The National Stressful Events Web Survey (NSES-W). Medical University of South Carolina, Charleston, SC, 2011. [Google Scholar]
- Litz BT, Gray MJ, 2002. Emotional numbing in posttraumatic stress disorder: Current and future research directions. Aust. Nz. J. Psychiat 36, 198–204. doi: 10.1046/j.1440-1614.2002.01002.x [DOI] [PubMed] [Google Scholar]
- Maack DJ, Tull MT, Gratz KL, 2012. Experiential avoidance mediates the association between behavioral inhibition and posttraumatic stress disorder. Cognitive. Ther. Res 36, 407–416. doi: 10.1007/s10608-011-9362-2 [DOI] [Google Scholar]
- Maccallum F, Sawday S, Rinck M, Bryant RA, 2015. The push and pull of grief: Approach and avoidance in bereavement. J. Behav. Ther. Exp. Psy 48, 105–109. doi: 10.1016/j.jbtep.2015.02.010 [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Neimeyer RA, Burke LA, Williams JL, Lawson K, 2012. The toll of traumatic loss in African Americans bereaved by homicide. Psychol. Trauma 4, 303–311. doi: 10.1037/a0024911 [DOI] [Google Scholar]
- Nam I, 2016. Suicide bereavement and complicated grief: Experiential avoidance as a mediating mechanism. J. Loss. Trauma 4, 325–334. doi: 10.1080/15325024.2015.1067099 [DOI] [Google Scholar]
- O’Connor MF, Wellisch DK, Stanton AL, Eisenberger NI, Irwin MR, Lieberman MD, 2008. Craving love? Enduring grief activates brain’s reward center. NeuroImage. 42, 969–972. doi: 10.1016/j.neuroimage.2008.04.256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papa A, Sewell MT, Garrison-Diehn C, Rummel C, 2013. A randomized open trial assessing the feasibility of behavioral activation for pathological grief responding. Behav. Ther 44, 639–650. doi: 10.1016/j.beth.2013.04.009 [DOI] [PubMed] [Google Scholar]
- Pickett SM, Bardeen JR, Orcutt HK, 2011. Experiential avoidance as a moderator of the relationship between behavioral inhibition system sensitivity and posttraumatic stress disorder. J. Anxiety. Disord 25, 1038–1045. doi: 10.1016/j.janxdis.2011.06.013 [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, … Maciejewski PK, 2009. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS. Med 6, e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, Havercamp S, 1996. The sensitivity theory of motivation: Implications for psychopathology. Behav. Res. Ther 34, 621–632. doi: 10.1016/0005-7967(96)00041-1 [DOI] [PubMed] [Google Scholar]
- Rheingold AA, Williams JL, 2015. Survivors of homicide: mental health outcomes, social support, and service use among a community-based sample. Violence. Victims 30, 870–883. doi: 10.1177/0269758016684421 [DOI] [PubMed] [Google Scholar]
- Sbarra DA, Hazan C, 2008. Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Pers. Soc. Psychol. Rev 12, 141–167. doi: 10.1177/1088868308315702 [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H, 1999. The dual process model of coping with bereavement: Rationale and description. Death. Stud 23, 197–224. doi: 10.1080/074811899201046 [DOI] [PubMed] [Google Scholar]
- Tomarken A, Roth A, Holland J, Ganz O, Schachter S, Rose G,…Nelson CJ, 2012. Examining the role of trauma, personality, and meaning in young prolonged grievers. Psycho-Oncol. 21, 771–777. doi: 10.1002/pon.1983 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP, 2013. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at http://www.ptsd.va.gov. [Google Scholar]
- Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS, 2003. Adaptive self-regulation of unattainable goals: Goal disengagement, goal reengagement, and subjective well-being. Pers. Soc. Psychol. B 29, 1494–1508. doi: 10.1177/0146167203256921 [DOI] [PubMed] [Google Scholar]