Abstract
Background
Korea is expected to become an ultra-aged society, in which the elderly population will account for more than 20% of the total population, after 2025. Thus, the social costs due to osteoporotic fractures are expected to increase. Therefore, this study aimed to measure disability weights (DWs) of osteoporosis and osteoporotic fractures in Korea.
Methods
The scenarios were developed to standardize the severity of 6 health statuses: osteoporosis and osteoporotic fractures including wrist, hip, post-hip, vertebral, and post-vertebral fracture. The values for these 6 health statuses were sought via a person trade-off (PTO) approach. We measured the value by PTO and we calculated it to DW of 6 health statuses. Three clinical expertise panels of 33 experts were established, and face-to-face interviews were conducted from July to December 2017.
Results
The distribution of DW varied by panel. DWs ranged from 0.5 (Osteoporosis) to 0.857 (Hip fracture) for Panel 1, 0.091 (Osteoporosis) to 0.5 (Hip fracture) for Panel 2, and 0.091 (Osteoporosis) to 0.726 (Hip fracture) for Panel 3. The final values for the 6 health statuses obtained by pooling all data from 3 panels ranged from 0.286 (Osteoporosis) to 0.750 (Hip fracture). There was no significant difference in rankings for the 6 health statuses among the 3 panels.
Conclusions
Comparing the DW of osteoporotic fracture in this study with other diseases in previous studies, it is predicted that osteoporotic fractures, especially hip fractures, will have a considerable burden of disease.
Keywords: Disability weights, Korea, Osteoporosis, Osteoporotic fractures, Person-Trade-Off
INTRODUCTION
In 2017, Korea became an aged society since the elderly population aged 65 and over exceeded 15% of the total population 2025.[1,2] According to the Health Insurance Review and Assessment Service's report in 2011, osteoporotic fractures have increased by 4% annually among people over 50 years of age, and hip fractures, one of the major causes of elderly mortality, have increased 4-fold in comparison to a decade ago.[3] The report pointed out the seriousness of osteoporotic fractures in the elderly by emphasizing that the social cost was estimated to be more than 1 trillion Korean won.[2]
Since Korea is expected to become an ultra-aged society, in which the elderly population accounts for more than 20% of the total population, after 2025,[2] the social costs due to osteoporotic fractures are expected to increase. However, considering the limited resources for healthcare, it is inevitable to consider the priority of diseases for efficient resource allocation. The high priority of a particular disease for resource allocation means that the disease is highly burdensome to society. Therefore, it is important to study the burden of diseases. Global burden of disease (GBD) studies have been conducted by the World Health Organization (WHO) and a GBD study group (http://www.who.int/healthinfo/global_burden_disease/about/en/) for the last 20 years.
GBD is expressed using Disability-Adjusted Life-Years (DALY), which are constructed using Years of Life Lost and Years Lost Due to Disability following various epidemiological and demographic indicators to comprehensively measure and compare the burden of disease.[4] To calculate Years Lost Due to Disability, it is necessary to have disability weights (DWs) for the specific health status.
Some researchers argued that we should reflect societal judgments of the value of different diseases rather than individual judgments of the disutility of the disease.[5,6] In 1996, the GBD team designed and used person trade-off (PTO) methodology.[7] Through the calculation of disease specific disutility, we can measure the population mean preference value for particular health status. And this weighting is multiplied by the number of years lived in that health status and added to the number of years lost due to that disease. Namely, the burden of disease is affected by disutility.
Fortunately, there have been many studies measuring DALY in a Korean context. Yoon et al.[8] studied GBD on smoking. Lee et al.[9] conducted a study on the priority of chronic degenerative diseases and injuries. Jo et al.[10] and Lee [11] investigated the burden of diseases on alcohol drinking. Studies on global burden of mental diseases, burden of diseases among the elderly, burden of COPD, and burden of enteritis due to climate changes were also conducted in a Korean context by Park et al.,[12] Lee and Kwon,[13] Kim,[14] and Shin et al.,[15] respectively. However, these studies employed the WHO's DW for the examined diseases and did not directly measure them [9,10,11,12,13,14,15] in a Korean population. In addition, some studies attempted to measure DWs applying to similar disease category as in the WHO's GBD research among Korean populations. As GBD studies by the WHO did not specify osteoporosis and osteoporotic fractures for their disease classification system,[16,17] they omitted osteoporosis and osteoporotic fractures in the Korean studies.[18] Therefore, this study aimed to measure DWs of osteoporosis and osteoporotic fractures in Korea.
METHODS
1. Panel participants
Three clinical expertise panels of 33 experts were established, and face-to-face interviews were conducted from July to December 2017. In order to select panelists, first, we chose the clinical subdivision that most frequently diagnosed osteoporosis and osteoporotic fracture patients. And then, the panelists were recommended by the society of each clinical subdivision. Most of the panelists worked in university hospitals. Panel 1 had 13 orthopedic specialists working at university hospitals, Panel 2 had 10 endocrine physicians working at university hospitals, and Panel 3 had 10 emergency medical specialists. The 3 panels of experts were selected based on their expertise on osteoporosis and fractures as well as their frequency of treating these patients.
2. PTO
DW reflects the social values or preference inherent in each person making up the society.[15] However, as the severity of a disease is assessed differently from person to person, even in the same disease, standardization tools have been devised to measure and apply the values of different individuals' social values. Typical tools include PTO, time trade-off (TTO), Visual Analog Scale, and Standard Gamble.
GBD was measured and compared using PTO by WHO and GBD groups.[16] The GBD group developed a disease classification system consisting of 107 diseases and injuries based on the International Classification of Diseases codes.[16,17] In the evaluation of the DW and its reliability in a Korean setting, Lee et al.[18] suggested a classification of 123 diseases and deliberately selected 16 index diseases to measure DW. However, none of the above studies considered osteoporosis and osteoporotic fractures.
The PTO method places the respondent in the position of a decision maker with a limited budget who must choose from among a series of alternative healthcare interventions.[19] Assuming that only 1 group between W persons in Health Status A and Z number of persons in Health Status B can be treated, and all treated individuals could survive until the same period after treatment, the point where W and Z become indifferent should be detected. This is expressed as follows:
| W(1−U(A))=Z(1−U(B)) |
| (1−U(B))=[W/Z](1−U(A)) |
The PTO technique was first devised by Patrick et al.[20] under the name of “equivalence of numbers technique”. The term PTO was assigned by Nord.[7] It is a method that draws the individual valuation of given health status through a trade-off procedure, which is similar to the TTO technique.
The variables considered in PTO are, first, the number of people who will benefit from the selected health care intervention and, second, the health improvement that the selected health care intervention will bring. So far, most PTO studies [18,19,20,21,22] have been composed of representative valuations of the general population except for the WHO study in 2000 and a study by the Dutch DWs Group conducted in the Netherlands.[21]
3. DW measurements
The scenarios were developed to standardize the severity of 6 health statuses: osteoporosis and osteoporotic fractures including wrist, hip, post-hip, vertebral, and post-vertebral fracture. Through literature reviews, 6 standard health statuses were objectively described and confirmed by the orthopedic specialists on osteoporosis and fractures (Supplementary Appendix 1). Compared to other fractures, vertebral and hip fractures still have difficulties in daily life and complete function recovery even after 6 months of fracture. Thus, vertebral and hip fractures were defined separately after 6 months of fracture. Except for post-vertebral and post-hip fracture, wrist, hip, vertebral fracture are short term case within 1 month after fracture.
Based on these 6 health statuses, the values were sought for PTO 1 and PTO 2.
PTO 1 was to obtain the number of N1 persons by assuming that N1 persons in each health status could match their 1 year of life extension to the equivalent life extension of 1,000 healthy persons. Thus, respondents were asked as decision-makers how many persons (N1) with osteoporosis—for example, living 1 year in their health status—are equivalent to 1,000 healthy persons living 1 year in healthy status. PTO 2 was to get the number of N2 persons who were completely cured from a certain health status and extend their life in perfect health by 1 year.
PTO 1 and PTO 2 were first recorded for 1 and 2 hr and revised after deliberation on the panel members' explanations and discussions. Then, finalized values of PTO 1 and PTO 2 were presented. The PTO 1 and PTO 2 values for each of the 6 health statuses were assigned to the following formula to obtain the DW.
.......... [22]
The consistency of PTO 1 and PTO 2 was emphasized in the GBD study.[23,24] However, Mansley and Elbasha [22] argued that it was difficult to meet the consistency of PTO 1 and 2 in practice and recommended asking only PTO 1 because there was a gap of social value for recovery. In this study, we examined both PTO 1 and 2 from 33 specialists, but only PTO 1 was used to derive the results; PTO 2 was used to identify consistency and provide opportunities for revision through discussion. However, as Mansley and Elbasha [22] asserted, it was very difficult to identify consistency. The PTO survey form used in this study can be found in Supplementary Appendix 2.
4. Analysis
The results of the PTO valuations were converted by linear transformation into a 0 to 1 scale ranging from no disability (0) to extreme disability (1). The median was calculated as the DW for each health status. Interquartile range (IQR) was calculated for distribution of DWs measured by each panel member. The quartiles represent the values corresponding to each rank when the values are divided into 4 quarters after being collected from the lowest to the highest order. The IQR is the range between the first quartile and the third quartile. It can be expresses as follows.
| IQR=3rd quartile–1st quartile |
The Spearman's rank correlation among the 3 panels was tested to check the agreement of the order of disability weighing judgment. This rank correlation coefficient is usually expressed as ρ, and the formula to calculate it is as follows.
Where D is the difference between the 2 ranks of each observation, and n is the number of observations. All statistical analyses were performed using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA).
5. Ethical statements
The study protocol was approved by the Institutional Review Board (IRB) of Mokwon University, Daejeon, Korea (IRB no. 2017AA0706).
RESULTS
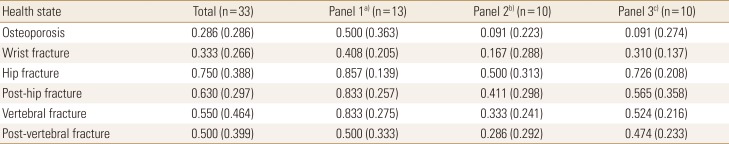
As shown in Table 1, median values of the DW for 6 health statuses including osteoporosis and wrist, vertebral, post-vertebral, post-hip, and hip fractures according to 3 panels were calculated.
Table 1. Disability weights for 6 health states related to osteoporosis and osteoporotic fractures.
The data is presented as mean (interquartile range).
a)Orthopedic surgeon. b)Endocrinologist. c)Emergency medical specialist.
The distribution of DWs varied by panel. DW ranged from 0.5 (Osteoporosis) to 0.857 (Hip fracture) for Panel 1, 0.091 (Osteoporosis) to 0.5 (Hip fracture) for Panel 2, and 0.091 (Osteoporosis) to 0.726 (Hip fracture) for Panel 3. In fact, the final values for 6 health statuses were obtained by pooling all data from the 3 panels and ranged from 0.286 (Osteoporosis) to 0.750 (Hip fracture).
Health statuses listed in order from highest to lowest DW by health status were hip fracture, post-hip fracture, vertebral fracture, wrist fracture, post-vertebral fracture, and osteoporosis for Panel 1. For Panels 2 and 3, the order was similar: hip fracture, post-hip fracture, vertebral fracture, post-vertebral fracture, wrist fracture, and osteoporosis.
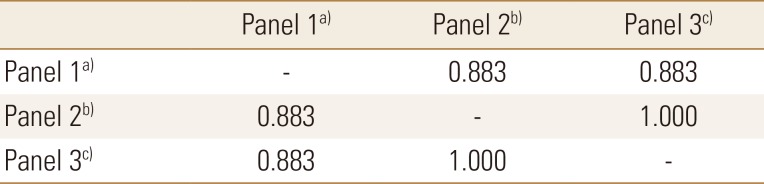
As shown in Table 2, the Spearman's rank correlation among 3 panels was tested, and the result showed a significant correlation among 3 panels (ρ=0.883; P=0.05). This means that there was no significant change in ranking 6 health statuses among the 3 panels.
Table 2. Inter-panel correlations.
a)Orthopedic surgeon. b)Endocrinologist. c)Emergency medical specialist.
DISCUSSION
This study is the first attempt to measure the DWs for osteoporosis and osteoporotic fractures in Korea. DWs were surveyed by 3 panels composed of 13 orthopedic surgeons, 10 endocrine physicians, and 10 emergency medical specialists. Although there were significant differences in the observed DWs among the panels, the calculated median values of DWs were in the following order: osteoporosis, 0.286; and wrist, 0.333; vertebral, 0.550; post-vertebral, 0.500; post-hip, 0.630; and hip, 0.750 fractures. As expected, this study indicates that that hip fractures, including post-hip fractures, most substantially affect patients with osteoporosis from the perspective of physicians caring for them.
In a 2013 GBD study which was conducted for the general population, DWs of each fracture were reported as follows: 0.111 (short term) to 0.005 (long term) for vertebral fractures, 0.035 for humerus fractures, and 0.050 (short term) to 0.055 (long term) for ankle fractures.[25,26] The 2013 GBD study showed that the DW value for most health statuses was smaller than that of a 2010 GBD study since the number of respondents from Western Europe was greater in 2013 than in 2010.[25,26,27] On the other hand, The Australian Burden of Disease and Injury study, which was conducted for the health care professionals assigned a DW of 0.372 to short-term cases of hip fracture.[28] The CHANCES is a consortium of 14 cohorts from Europe and the USA that was established in 2010 for an elderly population health study. In this study, they used the DWs proposed by the National Osteoporosis Foundation which was conducted for the experts, assigning a weight of 0.468 related to hip fracture.[29]
In our study, the DWs were estimated to be higher than in previous studies. We think this is because the panels who consider osteoporosis and related fractures most seriously owing to their specialty valued high. In addition, despite our effort for the thorough explanation, there is a possibility that the panels overestimate about osteoporotic fractures.
Among studies conducted in a Korean context, Do et al. [30] did not include osteoporosis and fractures but demonstrated DWs in low birth weight, 0.256; hepatitis B and C, 0.344; diabetes mellitus, 0.394; epilepsy, 0.433; rheumatic heart disease, 0.616; ischemic heart disease, 0.727; and stomach cancer, 0.847. Referring to this study, osteoporosis had higher DW than low birth weight and lower than hepatitis B and C, and wrist fracture had similar DW to hepatitis B and C. Hip fracture had a higher burden than rheumatic heart disease and ischemic heart disease but lower than stomach cancer.
Our study has limitations. First, the panels were made up entirely of medical professionals, as in previous studies.[11,16,21] Some studies did not limit respondents to medical doctors for the DW surveys, and public view was also worth adopting.[24,27] Second, the results of this study showed higher values than those of other countries. As the questionnaires in this study did not included other serious diseases such as cancer, there might be a bias to overestimate the given health statuses. Also, since the panels were composed to medical experts who mainly treat osteoporosis and fractures, their weights for these diseases might be biased. Despite these limitations, the present study was the first attempt to measure the DWs for osteoporosis and fractures in Korea. Further studies are necessary to validate our study results in the future. In addition, this study may instigate DW measurements for GBD studies in Korea.
CONCLUSIONS
This study was the first to measure the DW of osteoporosis and osteoporotic fractures in Korea using a PTO approach. The findings can be used to derive the disability adjusted life years of osteoporosis and osteoporotic fractures in a Korean context. Comparing the DW of osteoporotic fracture in this study with other diseases in previous studies, it is predicted that osteoporotic fractures, especially hip fractures, will be a significant burden of disease in Korea.
Acknowledgments
Authors appreciated the panels who participated in our survey for their effort to understand and give valuable information for our study.
Footnotes
Funding: This study was funded by Amgen Korea.
Conflict of interest: No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIAL
Six health states in accordance with major fractures
Person trade-off (PTO)1,2
References
- 1.Lee JW, Kim DH, Cho DH. Reducing suicide of the elderly and futures of aged society. Future Res. 2017;2:99–123. [Google Scholar]
- 2.Ha YC, Kim TY, Lee A, et al. Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int. 2016;27:2603–2609. doi: 10.1007/s00198-016-3576-9. [DOI] [PubMed] [Google Scholar]
- 3.Kim J, Lee E, Kim S, et al. Economic burden of osteoporotic fracture of the elderly in South Korea: a national survey. Value Health Reg Issues. 2016;9:36–41. doi: 10.1016/j.vhri.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Kirk MD, Pires SM, Black RE, et al. World Health Organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: a data synthesis. PLoS Med. 2015;12:e1001921. doi: 10.1371/journal.pmed.1001921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nord E. An alternative to QALYs: the saved young life equivalent (SAVE) BMJ. 1992;305:875–877. doi: 10.1136/bmj.305.6858.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nord E, Richardson J, Macarounas-Kirchmann K. Social evaluation of health care versus personal evaluation of health states. Evidence on the validity of four health-state scaling instruments using Norwegian and Australian surveys. Int J Technol Assess Health Care. 1993;9:463–478. doi: 10.1017/s0266462300005390. [DOI] [PubMed] [Google Scholar]
- 7.Nord E. The person-trade-off approach to valuing health care programs. Med Decis Making. 1995;15:201–208. doi: 10.1177/0272989X9501500302. [DOI] [PubMed] [Google Scholar]
- 8.Yoon SJ, Ha BM, Kang JW, et al. Estimation of attributable burden due to premature death from smoking in Korea. Korean J Prev Med. 2001;34:191–199. [Google Scholar]
- 9.Lee TJ, Kim J, Sung J. Estimation of disability-adjusted life years of major cardiovascular diseases in Korea. Korean Health Econ Rev. 2002;8:91–106. [Google Scholar]
- 10.Jo J, Lee TY, Lee SG, et al. Alcohol-related years of potential life lost in Korea. J Korean Soc Health Stat. 2003;28:40–56. [Google Scholar]
- 11.Lee JK. Measuring the burden of diseases due to alcohol consumption in Korea [master's thesis] Seoul: Seoul National University; 2004. [Google Scholar]
- 12.Park JH, Yoon SJ, Lee HY, et al. Estimating the burden of psychiatric disorder in Korea. J Prev Med Public Health. 2006;39:39–45. [PubMed] [Google Scholar]
- 13.Lee CE, Kwon S. Differences in the burden of disease of the elderly by socioeconomic status. Korean J Health Policy Adm. 2008;18:1–22. [Google Scholar]
- 14.Kim SJ. Burden of disease due to COPD [master's thesis] Seoul: Sookmyung Women's University; 2009. [Google Scholar]
- 15.Shin HS, Yun S, Jeong JW, et al. The impacts of climate change and age factors on the food-borne disease. Health Soc Welf Rev. 2015;35:186–210. [Google Scholar]
- 16.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 17.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee JK, Yoon SJ, Do YK, et al. Disability weights for diseases in Korea. Korean J Prev Med. 2003;36:163–170. [Google Scholar]
- 19.Wittrup-Jensen K, Pedersen KM. An empirical assessment of the person trade-off: Valuation of health, framing effects, and estimation of weights for fairness. Odense, DK: Syddansk Universitet; 2008. [Google Scholar]
- 20.Patrick DL, Bush JW, Chen MM. Methods for measuring levels of well-being for a health status index. Health Serv Res. 1973;8:228–245. [PMC free article] [PubMed] [Google Scholar]
- 21.Stouthard MEA, Essink-Bot ML, Bonsel GJ. Disability weights for diseases: a modified protocol and results for a Western European region. Eur J Public Health. 2000;10:24–30. [Google Scholar]
- 22.Mansley EC, Elbasha EH. Preferences and person trade-offs: forcing consistency or inconsistency in health-related quality of life measures. Health Econ. 2003;12:187–198. doi: 10.1002/hec.707. [DOI] [PubMed] [Google Scholar]
- 23.Burden of Disease Unit, Harvard School of Public Health. Measuring disability weights for a national burden of disease study using the person-trade-off method: a revised protocol. Cambridge, MA: Harvard School of Public Health; 1996. [Google Scholar]
- 24.Murray CJL, Lopez AD, editors. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: Summary. Geneva, CH: World Health Organization; 1996. [Google Scholar]
- 25.Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3:e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 26.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 28.Bertram M, Norman R, Kemp L, et al. Review of the long-term disability associated with hip fractures. Inj Prev. 2011;17:365–370. doi: 10.1136/ip.2010.029579. [DOI] [PubMed] [Google Scholar]
- 29.Papadimitriou N, Tsilidis KK, Orfanos P, et al. Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health. 2017;2:e239–e246. doi: 10.1016/S2468-2667(17)30046-4. [DOI] [PubMed] [Google Scholar]
- 30.Do YK, Yoon SJ, Lee JK, et al. Disability weights for the korean burden of disease study: focused on comparison with disability weights in the Australian burden of disease study. J Prev Med Public Health. 2004;37:59–71. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Six health states in accordance with major fractures
Person trade-off (PTO)1,2