Abstract
The aim of the study was to evaluate the ability of following biomarkers as diagnostic tools and risk predictors of AAA: C-reactive protein, interleukin-6, pentraxin-3, galectin-3, procollagen type III N-terminal peptide, C-terminal telopeptide of type I collagen, high-sensitive troponin I, and brain natriuretic peptide. Seventy-two patients with an AAA and 100 healthy individuals were enrolled into the study. We assessed individual biomarker performance and correlation between the AAA diameter and biomarker levels, and also, a multivariate logistic regression was used to design a possible predictive model of AAA growth and rupture risk. We identified following four parameters with the highest potential to find a useful place in AAA diagnostics: galectin-3, pentraxin-3, interleukin-6, and C-terminal telopeptide of type I. The best biomarkers in our evaluation (galectin-3 and pentraxin-3) were AAA diameter-independent. With the high AUC and AAA diameter correlation, the high-sensitive troponin I can be used as an independent prognostic biomarker of the upcoming heart complications in AAA patients. Authors recommend to add biomarkers as additional parameters to the current AAA patient management. Main addition value of biomarkers is in the assessment of the AAA with the smaller diameter. Elevated biomarkers can change the treatment decision, which would be done only based on AAA diameter size. The best way how to manage the AAA patients is to create a reliable predictive model of AAA growth and rupture risk. A created multiparameter model gives very promising results with the significantly higher efficiency compared with the use of the individual biomarkers.
Keywords: Abdominal aortic aneurism, Biomarker panel, Pentraxin-3, Galectin-3, Interleukin-6, Procollagen type III N-terminal peptide, C-Terminal telopeptide of type I collagen, High-sensitive troponin I, Brain natriuretic peptide, Multivariate stepwise logistic regression, Multivariate model, Predictive preventive personalized medicine, Patient stratification
Introduction
Abdominal aortic aneurysm (AAA), the enlargement of the abdominal aorta to a diameter at least 3 cm, is a common disease in the western part of the world. The prevalence in overall population ranges between 3 and 7% and is higher in White men and current smokers with the increasing risk with the age [1]. Smoking, White race, male gender, genetic factors, presence of other aneurysms in large vessels, and hypercholesterolemia are named as main risk factors of AAA. Also, modifiable lifestyle-related factors are significantly associated with AAA. Men with active lifestyle (walking or bicycling) have three times lower risk of AAA than men who never do walking or bicycling [2]. The growth rate of AAA is individual. It is estimated that the time to develop AAA of 3 cm or larger is approximately 5 years [3]. The most risky complication is AAA rupture. The mortality associated with ruptured AAA is still high. When including operative mortality, 80–90% of patients with ruptured AAA died [4]. The pathogenesis of AAA is a multifactorial process and is characterized by chronic inflammatory reaction in the aortic wall, particularly in infiltration of tunica media and tunica adventitia by inflammatory cells and extracellular matrix degradation [5]. AAA is usually diagnosed by physical examination, abdominal ultrasound, or computer tomography (CT). However, the speed of growing is individual, and also, the risk of rupture is not just dependent on the size of the aneurysm [6, 7]. Rupture even in small AAA was reported, while large aneurysms remain stable. Stability of the AAA wall depends on its size and the degree of the proteolytic enzyme activity on the enhanced degradation of the extracellular matrix and the related degree of inflammation occurring in the AAA wall [8]. Individual growth rate and multifactorial pathogenesis of AAA do not allow standardized approach to the patients. Individualization of the diagnostic and treatment process is one of the main conditions of future success [9]. The pathological processes in the aortic wall are connected with the production and involvement of various biomarkers. The research of these biomarkers is very extensive worldwide [10]. The aim of our study was to evaluate the individual biomarkers’ performance in AAA diagnostics to correlate the AAA diameter with the age and selected biomarkers, and finally, using multivariate analysis creates the multiparameter model to AAA patient stratification. This model could be used as diagnostic and prognostic tool to identify potentially risky aneurysms, which allow to apply a personalized approach in treatment [11]. The biomarkers were selected as the following—the biomarkers regulating inflammatory response: C-reactive protein (CRP), interleukin-6 (IL-6), pentraxin-3 (PTX-3), and galectin-3; the degradation products of the extracellular matrix: procollagen type III N-terminal peptide (PIIINP) and C-terminal telopeptide of type I collagen (ICTP); and biomarkers of myocardial injury and vascular resistance: high-sensitive troponin I (hsTnI) and brain natriuretic peptide (BNP).
Materials and methods
Study population
A total of 172 participants were enrolled into the study. The patient group comprised 72 patients with the AAA.
Inclusion criterion was the diagnosis of AAA and open surgery or endovascular treatment at the university hospital in Pilsen. Exclusion criteria were malignancy in the anamnesis, infection or autoimmune disease, and renal and hepatic dysfunction. The control group comprised 100 healthy individuals who underwent regular preventive examinations at our university hospital. A summary of the description of patient and control group is shown in Table 1.
Table 1.
Characteristics of the study groups
| Characteristic | Patient group | Control group |
|---|---|---|
| Male | 59 (82%) | 56 (56%) |
| Female | 13 (18%) | 44 (44%) |
| Total | 72 (100%) | 100 (100%) |
| Age, years (min–max) | 56 (36–80) | 53 (32–74) |
| Average size of aneurysm (mm) | 65 | Not applicable |
| Current smoking | 41 (55%) | 46 (46%) |
| Diabetes mellitus | 9 (12%) | 7 (7%) |
| Hypertension | 45 (61%) | 40 (40%) |
| Ischemic heart disease | 21 (29%) | 19 (19%) |
| Peripheral artery disease | 11 (15%) | 5 (5%) |
Serum samples
Blood samples were collected prior to the endovascular treatment or open surgery. Peripheral blood was drawn using VACUETTE® Z Serum Sep tubes (Greiner Bio-One, Kremsmünster, Austria) and allowed to clot. Serum was separated within 3 h of collection by centrifugation at 1700 ×g for 10 min, and all samples were immediately aliquoted and frozen to − 80 °C. Samples were stored under a 24-h monitoring system. Serum samples were thawed only once, just prior to the analysis. Serum levels of PTX-3, IL-6, galectin-3, hsTnl, CRP, BNP, PIIINP, and ICTP were measured for each sample.
Sample analysis
Serum levels of CRP were measured using the chemiluminescent assay with the Maglumi Instrument (Snibe Co., Shenzhen, China). IL-6 and hsTnI were measured using the chemiluminescent ACCESS assays with the UniCel DxI 800 Instrument (Beckman Coulter, Brea, CA, USA). PTX-3 was measured using Simple Plex assay with the Ella System (ProteinSimple, San Jose, CA, USA). Galectin-3 and BNP were measured using the chemiluminescent assays with the Architect 1000i System (Abbott, Libertyville, IL, USA), and PIIINP and ICTP were measured using the radioimmunoassays UniQ PIIINP RIA and ICTP RIA (Orion Diagnostica, Espoo, Finland) with the STRATEC SR 300 Instrument (Stratec Biomedical AG, Birkenfeld, Germany).
Statistical analysis
Statistical Analysis Software release 9.2 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. Basic descriptive statistic parameters are presented: mean, median, minimum, maximum, lower quartile, and upper quartile. Spearman rank correlation coefficient was used to estimate correlation between AAA diameter, biomarkers’ levels, and age. The Wilcoxon test was used to compare distributions of biomarker values between the groups of patients and the group of healthy persons, while a p value of less than 0.05 indicated statistical significance. Receiver operating characteristic (ROC) curves and the area under the curve (AUC) are presented to aid an assessment of the usefulness of selected biomarkers for AAA diagnosis. A multivariate stepwise logistic regression was used whereby the biomarkers (as AAA predictors) were added one-by-one until they achieved statistical significance after addition to the model. The previously added predictors were eliminated if, after the addition of other predictors, they had become statistically non-significant. This ensures that all the predictors, which are in the final logistic regression model, remain statistically significant [12].
Results
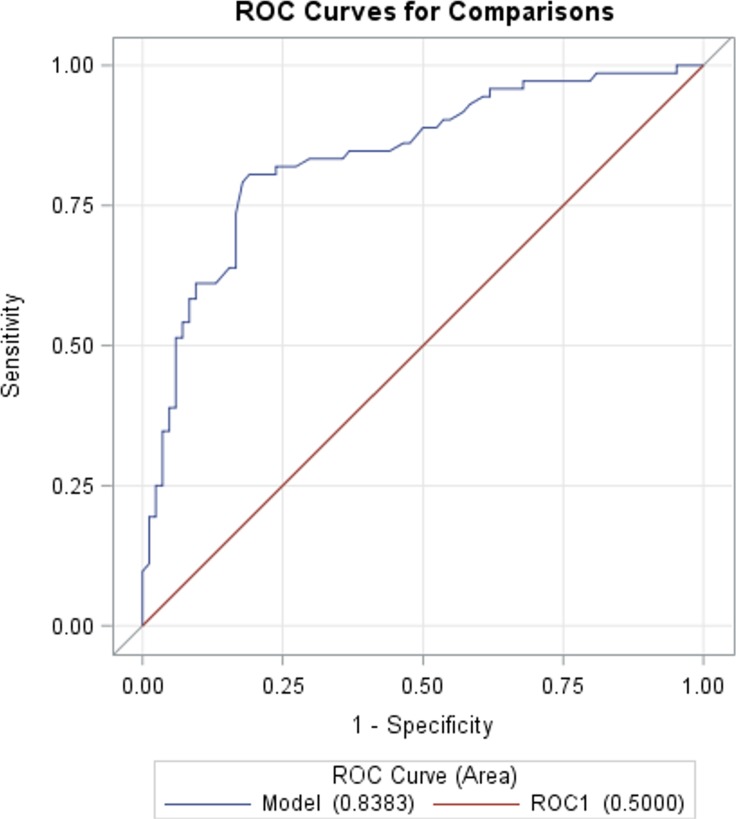
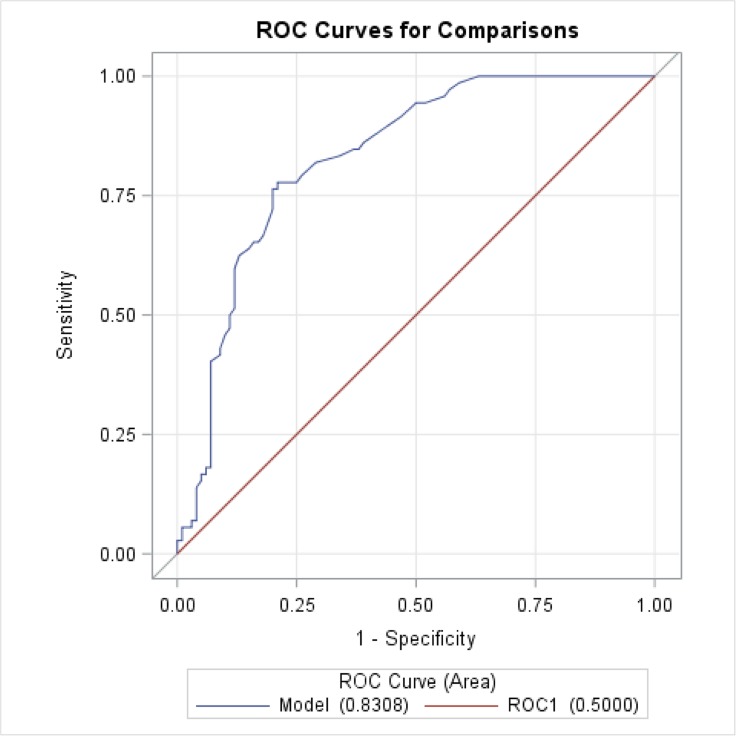
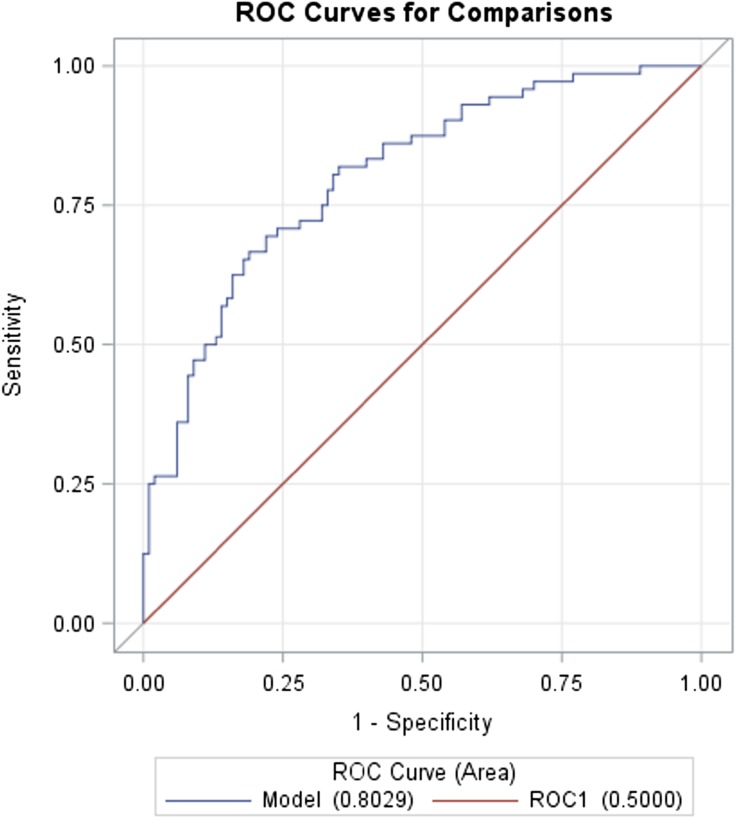
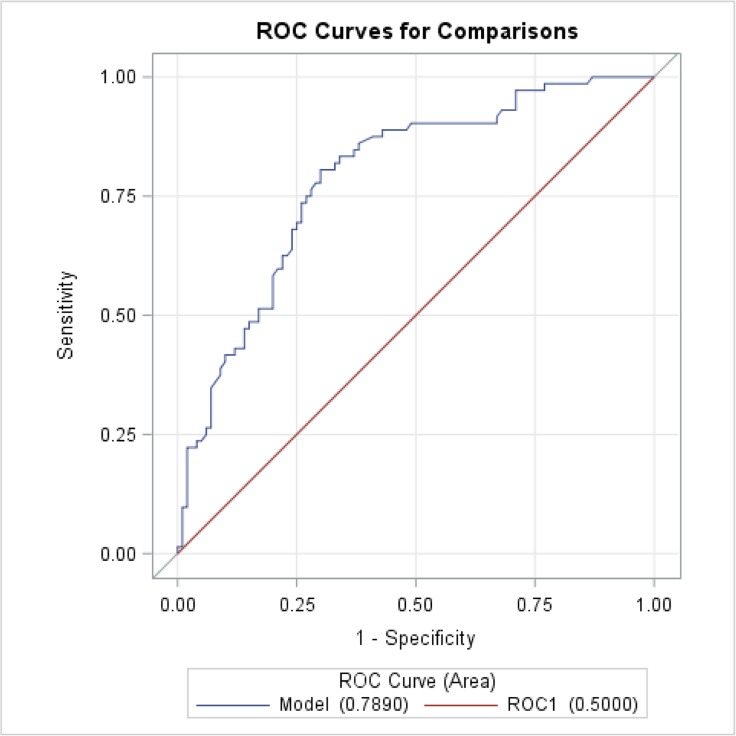
Table 2 shows the results of the comparison of CRP, IL-6, PTX-3, galectin-3, PIIINP, ICTP, hsTnl, and BNP levels in the AAA patient group and in the group of healthy persons. AAA group had statistically significantly higher levels of all the examined biomarkers compared with the control group. We plotted ROC curves and calculated the AUC for each individual biomarker. The values of the AUC are shown in Table 3. The best values were achieved by galectin-3 (AUC = 0.8383), hsTnl (AUC = 0.8306), PTX-3 (AUC = 0.8029), IL-6 (AUC = 0.7890), and ICTP (AUC = 0.7689). The worst value was achieved by CRP (AUC = 0.6014). ROC curves are shown in Figs. 1, 2, 3, 4, 5, 6, 7, 8.
Table 2.
Levels of the selected biomarkers in the AAA group and control group
| Parameter | Status | Mean | Median (min–max) | Lower quartile | Upper quartile | Wilcoxon test p value |
|---|---|---|---|---|---|---|
| CRP (mg/l) | AAA | 5.79 | 1.92 (0.19–100) | 0.81 | 5.16 | 0.0248 |
| Controls | 2.82 | 1.19 (0.13–44.05) | 0.56 | 2.98 | ||
| IL-6 (pg/ml) | AAA | 5.09 | 3.03 (0.58–76.72) | 2.16 | 5.76 | < 0.0001 |
| Controls | 2.03 | 1.36 (0.18–18.35) | 0.88 | 2.42 | ||
| PTX-3 (pg/ml) | AAA | 7223 | 6545 (1246–18,916) | 4010 | 9453 | < 0.0001 |
| Controls | 3524 | 2872 (708–12,673) | 1727 | 4813 | ||
| Galectin-3 (ng/ml) | AAA | 19.93 | 18.85 (8.00–54.70) | 15.30 | 22.20 | < 0.0001 |
| Controls | 13.21 | 12.95 (5.6–27.10) | 10.70 | 14.70 | ||
| PIIINP (μg/l) | AAA | 5.26 | 4.86 (2.54–10.19) | 4.16 | 6.09 | < 0.0001 |
| Controls | 3.90 | 3.92 (0.12–6.72) | 3.33 | 4.68 | ||
| ICTP (μg/l) | AAA | 5.46 | 4.77 (2.39–15.15) | 3.63 | 6.57 | < 0.0001 |
| Controls | 3.55 | 3.37 (1.75–6.73) | 2.88 | 4.08 | ||
| hsTnl (ng/l) | AAA | 16.30 | 4.90 (1.70–754) | 3.50 | 7.40 | < 0.0001 |
| Controls | 3.25 | 2.25 (0.23–37.30) | 1.40 | 3.35 | ||
| BNP (pg/ml) | AAA | 26.86 | 14.80 (10.00–135) | 10.0 | 27.5 | 0.0128 |
| Controls | 3.55 | 3.37 (1.75–6.73) | 2.88 | 4.08 |
Legend: AAA, abdominal aortic aneurysm; CRP, C-reactive protein; IL-6, interleukin-6; PTX-3, pentraxin-3; PIIINP, procollagen type III N-terminal peptide; ICTP, C-terminal telopeptide of type I collagen; hsTnI, high-sensitive troponin I; BNP, brain natriuretic peptide
Table 3.
AUC values of all tested biomarkers
| Parameter | AUC | 95% confidence limit | |
|---|---|---|---|
| Galectin-3 | 0.8383 | 0.7744 | 0.9022 |
| hsTnl | 0.8308 | 0.7701 | 0.8916 |
| PTX-3 | 0.8029 | 0.7374 | 0.8685 |
| IL-6 | 0.7890 | 0.7209 | 0.8570 |
| ICTP | 0.7689 | 0.6933 | 0.8446 |
| PIIINP | 0.7448 | 0.6664 | 0.8232 |
| BNP | 0.6084 | 0.5244 | 0.6924 |
| CRP | 0.6014 | 0.5149 | 0.6879 |
| Model | 0.9012 | 0.8499 | 0.9526 |
Legend: AUC, area under the curve; hsTnI, high-sensitive troponin I; PTX-3, pentraxin-3; IL-6, interleukin-6; ICTP, C-terminal telopeptide of type I collagen; PIIINP, procollagen type III N-terminal peptide; BNP, brain natriuretic peptide; CRP, C-reactive protein; Model, multivariate stepwise selection model created using galectin-3, PTX-3, IL-6, and ICTP
Fig. 1.
ROC curve of galectin-3. ROC analysis of the galectin-3 ability to separate AAA patients and healthy persons. Galectin-3 proved to be a best individual biomarker to this purpose. Model: galectin-3, AUC = 0.8383
Fig. 2.
ROC curve of hsTnI. ROC analysis of the hsTnI ability to separate AAA patients and healthy persons. hsTnI achieved the second best AUC, and it is a candidate to be used as an independent prognostic biomarker of the upcoming heart complications in AAA patients. Model: hsTnI, high-sensitive troponin I, AUC = 0.8308
Fig. 3.
ROC curve of PTX-3. ROC analysis of the PTX-3 ability to separate AAA patients and healthy persons. PTX-3 proved to be a potential useful part of the multi parameter predictive model of AAA growth and rupture risk. Model: PTX-3, pentraxin-3, AUC = 0.8029
Fig. 4.
ROC curve of IL-6. ROC analysis of the IL-6 ability to separate AAA patients and healthy persons. IL-6 is the next candidate to be a potential useful part of the multiparameter predictive model of AAA growth and rupture risk. Model: IL-6, interleukin-6, AUC = 0.7890
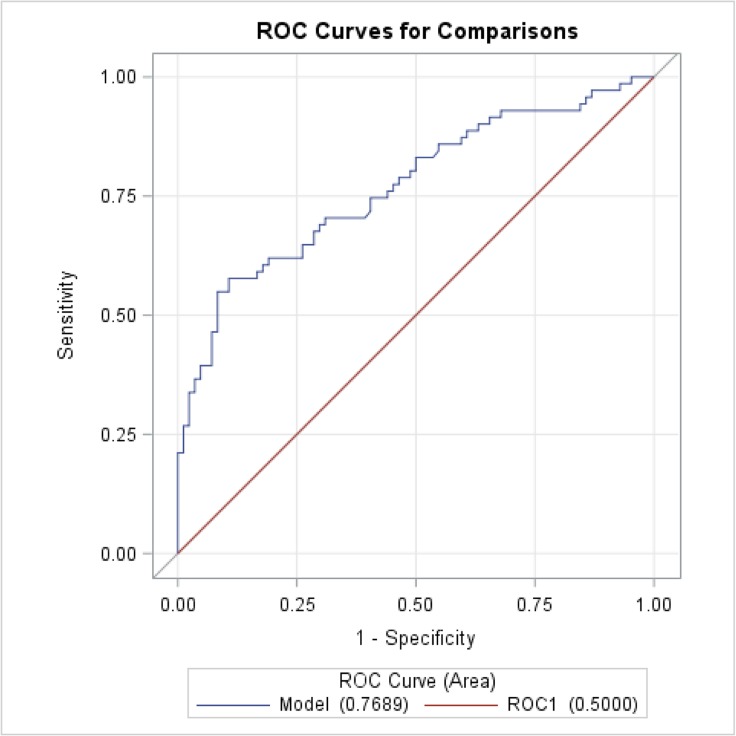
Fig. 5.
ROC curve of ICTP. ROC analysis of the ICTP ability to separate AAA patients and healthy persons. ICTP is the last candidate from our biomarker panel to be a part of the multi parameter predictive model of AAA growth and rupture risk. Model: ICTP, C-terminal telopeptide of type I collagen, AUC = 0.7689
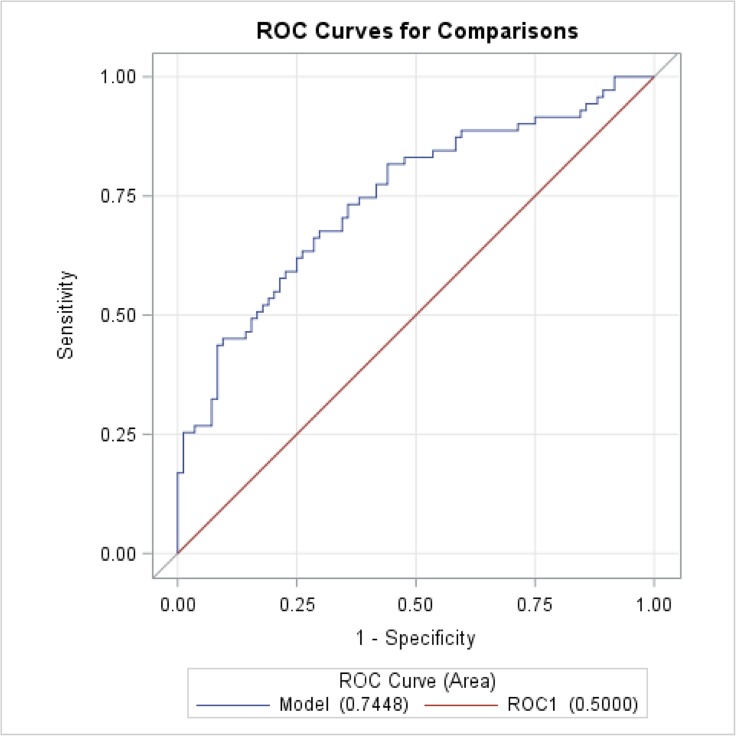
Fig. 6.
ROC curve of PIIINP. ROC analysis of the PIIINP ability to separate AAA patients and healthy persons. Despite relatively satisfied AUC value, PIIINP was not chosen by created multi parameter model of AAA growth and rupture risk. Model: PIIINP, procollagen type III N-terminal peptide, AUC = 0.7448
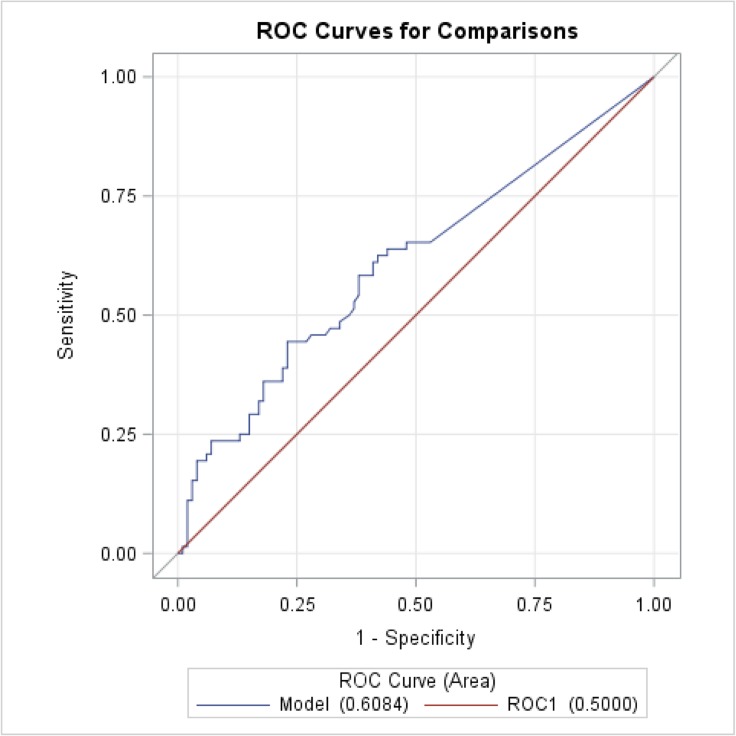
Fig. 7.
ROC curve of BNP. ROC analysis of the BNP ability to separate AAA patients and healthy persons. AUC value of BNP was the second worst in our evaluation. BNP did not meet our criteria for the ability to be the biomarker for AAA diagnostics. Model: BNP, brain natriuretic peptide, AUC = 0.6084
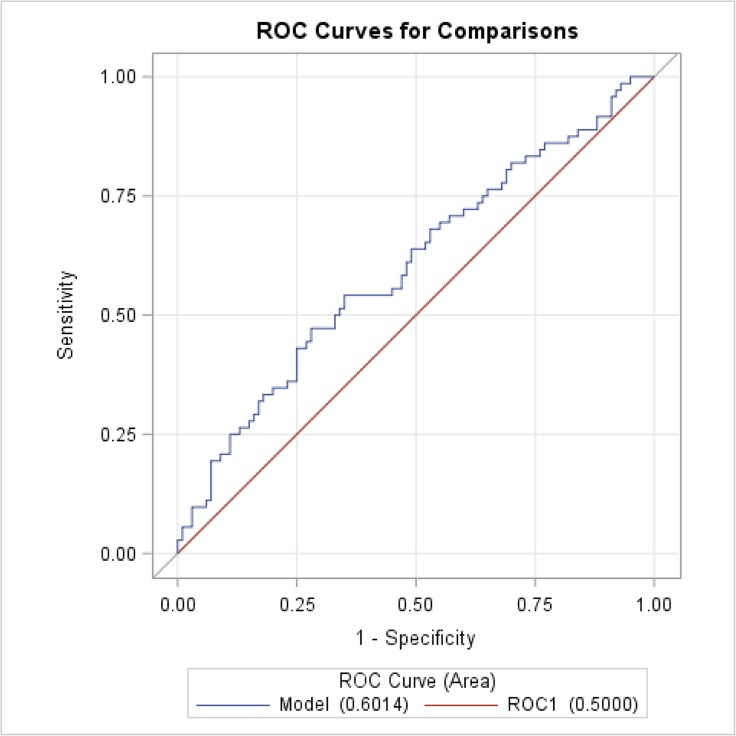
Fig. 8.
ROC curve of CRP. ROC analysis of the CRP ability to separate AAA patients and healthy persons. AUC value of CRP was the worst in our evaluation. CRP did not meet our criteria for the ability to be the biomarker for AAA diagnostics. Model: CRP, C-reactive protein, AUC = 0.6014
Table 4 shows the correlation between the AAA diameter and biomarkers. The correlation with statistical significance was observed in the case of CRP, hsTnl, IL-6, PIIINP, and ICTP. Galectin-3, PTX-3, BNP, and age did not correlate with the AAA diameter.
Table 4.
Correlation of AAA diameter with the biomarker levels
| Item | Spearman correlation coefficient | p value |
|---|---|---|
| CRP | 0.3210 | 0.0060 |
| hsTnI | 0.3197 | 0.0062 |
| IL-6 | 0.3152 | 0.0070 |
| PIIINP | 0.2896 | 0.0143 |
| ICTP | 0.2879 | 0.0149 |
| BNP | 0.1393 | 0.2429 |
| age | 0.1231 | 0.3028 |
| PTX-3 | 0.1131 | 0.3440 |
| Galectin-3 | 0.0031 | 0.9791 |
Legend: CRP, C-reactive protein; PTX-3, pentraxin-3; IL-6, interleukin-6; PIIINP, procollagen type III N-terminal peptide; ICTP, C-terminal telopeptide of type I collagen; hsTnI, high-sensitive troponin I; BNP, brain natriuretic peptide
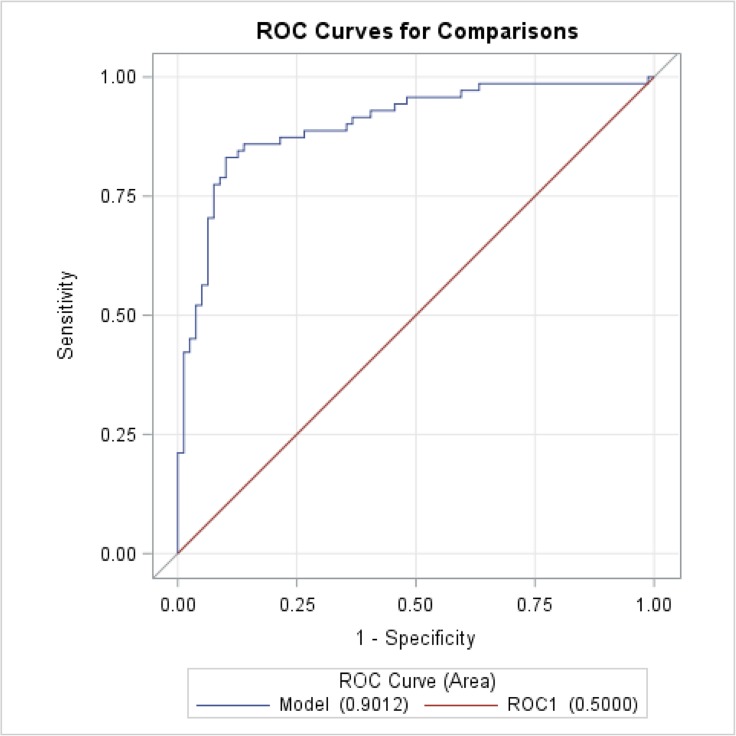
When multivariate stepwise logistic regression was applied, the following four biomarkers were selected as the best predictors of AAA: galectin-3, PTX-3, IL-6, and ICTP. We created a multivariate model (AUC = 0.9012, Fig. 9) with the significantly higher efficiency compared with the use of the individual biomarkers only (p < 0.0001).
Fig. 9.
ROC curve of multi parameter model. ROC analysis of the multi parameter model ability to separate AAA patients and healthy persons. AUC value of this model was statistically significantly higher compared with the individual biomarkers. This result showed that the right way for the future in AAA diagnostics is the shift from single parameter assessment to multi parameter systematic model. Model: multiparameter model, multivariate stepwise selection model created using galectin-3, PTX-3, IL-6, and ICTP, AUC = 0.9012
Discussion
Recently, a large number of studies have been published that analyze various biomarkers in patients with AAA [2, 8, 13, 14]. We summarized our data, which will be discussed in following text in Tables 2 and 3.
Inflammatory biomarkers
The most common focus is the effort to detect signs of an inflammatory reaction occurring in the wall of the aorta as a potential reason for the aortic wall instability and hence an increased risk of rupture of the aneurysm. Being one of the basic inflammatory markers [15], CRP is a frequently investigated parameter in connection with AAA. CRP is long-established and used as a reliable non-specific inflammatory marker with an important place in inflammatory diagnostics. However, with regard to AAA, the use of CRP is limited. In our study, CRP correlates with the AAA diameter but achieved the worst AUC value (AUC = 0.6014), and we cannot recommend its use as an AAA marker. Inflammation cells, like activated macrophages, monocytes, or eosinophils, produce many kinds of cytokines. There are many studies available on this topic. However, the conclusions regarding the usefulness of individual cytokines are controversial [13]. IL-6 was confirmed as one of the most significant markers. There is a hypothesis that IL-6 is directly produced by an AAA [16]. In our study, IL-6 was higher in the AAA group with a strong statistical significance (p < 0.0001) compared with the healthy group, achieved a good AUC value (AUC = 0.7890), and also correlated with the AAA diameter. This is in concordance with previously published studies our own team’s included [15, 17].
In the field of inflammatory markers, many new molecules have recently been introduced. We focused on two of them: PTX-3 and galecin-3. PTX-3 is a glycoprotein, a member of the pentraxin family. It is produced by a variety of cells, such as monocytes, macrophages, dendritic cells, endothelial cells, and fibroblasts in response to an inflammatory stimulus. It is one of the acute phase proteins and is close to CRP. Its role has been studied in connection with acute aortic dissection or acute coronary syndrome. Very little is currently known about the association between the AAA and serum levels of PTX-3 [18, 19]. We proved statistically significantly higher serum levels of PTX-3 in patients with an AAA (p < 0.0001) with a high AUC value (AUC = 0.8029). To our knowledge, only one study reported PTX-3 expression in the tissue of AAA [20]. Based on our results, we can assume that PTX-3 plays an important role in the pathogenesis of AAA and seems to be a potentially new AAA diameter independent biomarker.
Galectin-3 is a member of the family of lectins. It is produced by activated macrophages and is involved in cell adhesion, proliferation, angiogenesis, and apoptosis [21]. Galectin-3 has previously been investigated in connection with inflammation and risk of the cardiovascular diseases and mortality [22]. Data regarding the relation of galetin-3 to AAA are rare. Recent studies show a positive correlation between galectin-3 levels and AAA incidence. In the general population, systemic galectin-3 concentrations are elevated years before the identification of AAA incidence [23]. Increased galectin-3 levels were associated with AAA progression, while galectin-3 inhibition decreased experimental AAA development. In addition, galectin-3 serum levels were associated with the need for surgical repair, independently of other potential diagnostic factors [24]. In our study, we observed statistically significantly higher serum levels of galectin-3 in patients with an AAA (p < 0.0001) with the highest AUC value (AUC = 0.8383). This finding proved an important role of galectin-3 in the AAA pathogenesis and the ability of this molecule to be a good marker of inflammation and increased systemic vascular resistance in AAA. Similarly to PTX-3, galectin-3 seems to be AAA diameter independent. We did not prove any correlation with the AAA diameter in case of both above mentioned biomarkers.
Collagen degradation products
Another group of biochemical markers, which are very often studied in connection with AAA pathogenesis, is the extracellular matrix degradation products, collagen, and elastin, respectively. Collagen, as an important component of this matrix, appears to be a key element in the process of AAA development and progression. If collagen degradation prevails over the synthesis, the irreversible destruction of the aortic wall is started. This situation can directly lead to the expansion and subsequent rupture of an AAA [25]. In our work, we decided to analyze PIIINP and ICTP. We understand these two collagen degradation products to be an indicator of collagenolysis. In the available literature, there are a number of studies of these parameters in patients with AAA [13, 22]. Certain works had shown that PIIINP is able to predict further development and the eventual necessity for intervention in a small AAA [26, 27]. Also, the association of PIIINP with congenital cardiovascular disorders has been proved [24]. In our study, we found statistically significantly elevated PIIINP in AAA patients (p < 0.0001) as well as ICTP (p < 0.0001). The AUC values for PIIINP (AUC = 0.7448) and ICTP (AUC = 0.7689) were still acceptable for possible clinical use. PIIINP and ICTP correlated with the AAA diameter.
Biomarkers of cardiac injury and vascular resistance
The last two biomarkers in our study were hsTnI and BNP, which were primarily connected with cardiac injury and increased vascular resistance [13, 28]. A new generation of high-sensitive troponins (hsTn) opens up a new field of indication for these types of biomarkers [29]. In our work, we used newly introduced hsTnI kit, and to our knowledge, it is the first use in this indication, which was published. We observed statistically significantly elevated hsTnI levels in AAA patients (p < 0.0001), and hsTnI also reached the high AUC value (AUC = 0.8303) when ROC analysis was done and also correlated with the AAA diameter. hsTnI seems to be an independent sign of the cardial risk and can early selected the patients we have to focused on in this regard. In the case of BNP, recent studies describe increased BNP in patients who later developed AAA [30]. In our study, BNP levels were also statistically significantly higher in the group of AAA patients (p < 0.0213); however, its AUC value was the second worst in our evaluation (AUC = 0.6084), and BNP also did not correlate with the AAA diameter.
Correlation between biomarkers and AAA diameter
Looking at our data, it is visible that the relation between concentration of biomarkers and AAA diameter will not provide reliable information, which can be used in the decision about following treatment procedure. Two biomarkers, which have the best ability to separate AAA patients and healthy persons (PTX-3 and galectin-3), achieved the worst correlation coefficient with the AAA diameter. CRP achieved the best correlation coefficient, but according to the AUC value, it is very unspecific. Age is considered as one of the main risk factor of AAA development. Therefore, we also correlated age of AAA patients with AAA diameter, but in concordance with the literature findings, it is without a positive result [31]. We recommend to assess AAA diameter and biomarker activity as two independent parameters with the addition of the biomarker levels to the current system of AAA evaluation, which is based on AAA diameter.
Multiparameter model
The rapid development of various diagnostic technologies is driving the shift from single parameter model to multiparameter systematical model. This way allows us to better interpretation of the results, which accelerates predictive, preventive, and personalized medicine (PPPM) practice allowing prediction of response with substantially increased accuracy, stratification of particular patients, and eventual personalization of medicine [32]. Using experience from our previous research [11] and other relevant studies [33, 34] as the last step of our eight biomarker panel evaluation, we selected the best candidates for use in clinical practice. For this reason, multivariate stepwise logistic regression was used, and the following four biomarkers were selected as the best predictors of AAA: galectin-3, pentraxin-3, IL-6, and ICTP. We created a multivariate model (AUC = 0.9012) with the significantly higher efficiency compared with the use of the individual biomarkers (p < 0.0001).
Conclusions and expert recommendations
AAA patients are currently followed up using an imaging techniques and AAA diameter scanning. Our data together with the literature evidences show that blood biomarkers have important information, which allows us better stratify patient and individualize the treatment procedures.
We identified following four parameters with the highest potential to find a useful place in AAA diagnostics: galectin-3, PTX-3, IL-6, and ICTP.
We created a multivariate model with the significantly higher efficiency compared with use of the individual biomarkers.
The best biomarkers in our evaluation (galectin-3 and PTX-3) were AAA diameter independent.
With the high AUC and AAA diameter correlation, the hsTnI can be used as an independent prognostic biomarker of the upcoming heart complications in AAA patients.
We recommend to add biomarker levels as additional parameters to the current algorithm of AAA patient management.
The main addition value of biomarkers we see in the assessment of the AAA with the smaller diameter. Elevated biomarker levels can work as a warning signal and can changed the treatment decision, which would be done only based on AAA diameter size.
The best way how to manage the AAA patients is to create a reliable predictive model of AAA growth and rupture risk. Our multiparameter model gives very promising results, and we will focus on the confirmation of current results on the larger group of patients.
Abbreviations
- AAA
abdominal aortic aneurysm
- AUC
area under the curve
- BNP
brain natriuretic peptide
- CRP
C-reactive protein
- hsTnI
high-sensitive troponin I
- ICTP
C-terminal telopeptide of type I collagen
- IL-6
interleukin-6
- PIIINP
procollagen type III N-terminal peptide
- PTX-3
pentraxin-3
- ROC
receiver operating characteristic
- SAS
Statistical Analysis Software
Funding information
This study was supported by the Grant of the Czech Health Research Council No.15-32727A.
Compliance with the ethical standards
Competing interests
The authors declare that they have no competing interests.
Ethical approval
All investigations conformed to the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all the participants. The study was approved by the responsible Ethical Committee of the University Hospital in Pilsen on August 12, 2014.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tang W, Yao L, Roetker NS, Alonso A, Lutsey PL, Steenson CC, Lederle FA, Hunter DW, Bengtson LG, Guan W, Missov E, Folsom AR. Lifetime risk and risk factors for abdominal aortic aneurysm in a 24-year prospective study: the ARIC study (atherosclerosis risk in communities) Arterioscler Thromb Vasc Biol. 2016;36:2468–2477. doi: 10.1161/ATVBAHA.116.308147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stackelberg O, Wolk A, Eliasson K, Hellberg A, Bersztel A, Larsson SC, Orsini N, Wanhainen A, Björck M. Lifestyle and risk of screening-detected abdominal aortic aneurysm in men. J Am Heart Assoc. 2017;6:e004725. doi: 10.1161/JAHA.116.004725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oliver-Williams C, Sweeting MJ, Turton G, Parkin D, Cooper D, Rodd C, Thompson SG, Earnshaw JJ, Gloucestershire and Swindon Abdominal Aortic Aneurysm Screening Programme Lessons learned about prevalence and growth rates of abdominal aortic aneurysms from a 25-year ultrasound population screening programme. Br J Surg. 2018;105:68–74. doi: 10.1002/bjs.10715. [DOI] [PubMed] [Google Scholar]
- 4.de Jesus-Silva SG, de Oliveira VR, de Moraes-Silva MA, Krupa AE, Cardoso RS. Risk factors and short and medium-term survival after open and endovascular repair of abdominal aortic aneurysms. J Vasc Bras. 2018;17:201–207. doi: 10.1590/1677-5449.011717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang W, Yao L, Hoogeveen RC, Alonso A, Couper DJ, Lutsey PL, Steenson CC, Guan W, Hunter DW, Lederle FA, Folsom AR. The association of biomarkers of inflammation and extracellular matrix degradation with the risk of abdominal aortic aneurysm: the ARIC study. Angiology. 2018;70:130–140. doi: 10.1177/0003319718785278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ying AJ, Affan ET. Abdominal aortic aneurysm screening: a systematic review and meta-analysis of efficacy and cost. Ann Vasc Surg. 2019;54:298–303.e3. doi: 10.1016/j.avsg.2018.05.044. [DOI] [PubMed] [Google Scholar]
- 7.van Schaik TG, Yeung KK, Verhagen HJ, de Bruin JL, van Sambeek MRHM, Balm R, Zeebregts CJ, van Herwaarden JA, Blankensteijn JD, Grobbee DE, Blankensteijn JD, Bak AAA, Buth J, Pattynama PM, Verhoeven ELG, van Voorthuisen AE, Blankensteijn JD, Balm R, Buth J, Cuypers PWM, Grobbee DE, Prinssen M, van Sambeek MRHM, Verhoeven ELG, Baas AF, Hunink MG, van Engelshoven JM, Jacobs MJHM, de Mol BAJM, van Bockel JH, Balm R, Reekers J, Tielbeek X, Verhoeven ELG, Wisselink W, Boekema N, Heuveling LM, Sikking I, Prinssen M, Balm R, Blankensteijn JD, Buth J, Cuypers PWM, van Sambeek MRHM, Verhoeven ELG, de Bruin JL, Baas AF, Blankensteijn JD, Prinssen M, Buth J, Tielbeek AV, Blankensteijn JD, Balm R, Reekers JA, van Sambeek MRHM, Pattynama P, Verhoeven ELG, Prins T, van der Ham AC, van der Velden JJIM, van Sterkenburg SMM, ten Haken GB, Bruijninckx CMA, van Overhagen H, Tutein Nolthenius RP, Hendriksz TR, Teijink JAW, Odink HF, de Smet AAEA, Vroegindeweij D, van Loenhout RMM, Rutten MJ, Hamming JF, Lampmann LEH, Bender MHM, Pasmans H, Vahl AC, de Vries C, Mackaay AJC, van Dortmont LMC, van der Vliet AJ, Schultze Kool LJ, Boomsma JHB, van Dop HR, de Mol van Otterloo JCA, de Rooij TPW, Smits TM, Yilmaz EN, Wisselink W, van den Berg FG, Visser MJT, van der Linden E, Schurink GWH, de Haan M, Smeets HJ, Stabel P, van Elst F, Poniewierski J, Vermassen FEG. Long-term survival and secondary procedures after open or endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 2017;66:1379–1389. doi: 10.1016/j.jvs.2017.05.122. [DOI] [PubMed] [Google Scholar]
- 8.Schermerhorn ML, Cronenwett JL. The UK small aneurysm trial. J Vasc Surg. 2001;33:443. doi: 10.1067/mva.2001.111985. [DOI] [PubMed] [Google Scholar]
- 9.Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation—EPMA position paper 2016. EPMA J. 2016;7:23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohno T, Aoki H, Ohno S, Nishihara M, Furusho A, Hiromatsu S, Akashi H, Fukumoto Y, Tanaka H. Cytokine profile of human abdominal aortic aneurysm: involvement of JAK/STAT pathway. Ann Vasc Dis. 2018;11:84–90. doi: 10.3400/avd.oa.17-00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kucera R, Smid D, Topolcan O, Karlikova M, Fiala O, Slouka D, Skalicky T, Treska V, Kulda V, Simanek V, Safanda M, Pesta M. Searching for new biomarkers and the use of multivariate analysis in gastric cancer diagnostics. Anticancer Res. 2016;36:1967–1971. [PubMed] [Google Scholar]
- 12.Golubnitschaja O, Costigliola V, EPMA General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2012;3:14. doi: 10.1186/1878-5085-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Urbonavicius S, Urbonaviciene G, Honoré B, Henneberg EW, Vorum H, Lindholt JS. Potential circulating biomarkers for abdominal aortic aneurysm expansion and rupture—a systematic review. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2008;36:273–280. doi: 10.1016/j.ejvs.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Groeneveld ME, Meekel JP, Rubinstein SM, Merkestein LR, Tangelder GJ, Wisselink W, Truijers M, Yeung KK. Systematic review of circulating, biomechanical, and genetic markers for the prediction of abdominal aortic aneurysm growth and rupture. J Am Heart Assoc. 2018;7:e007791. doi: 10.1161/JAHA.117.007791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindberg S, Zarrouk M, Holst J, Gottsäter A. Inflammatory markers associated with abdominal aortic aneurysm. Eur Cytokine Netw. 2016;27:75–80. doi: 10.1684/ecn.2016.0381. [DOI] [PubMed] [Google Scholar]
- 16.Dawson J, Cockerill GW, Choke E, Belli A-M, Loftus I, Thompson MM. Aortic aneurysms secrete interleukin-6 into the circulation. J Vasc Surg. 2007;45:350–356. doi: 10.1016/j.jvs.2006.09.049. [DOI] [PubMed] [Google Scholar]
- 17.Treska V, Topolcan O, Pecen L. Cytokines as plasma markers of abdominal aortic aneurysm. Clin Chem Lab Med. 2000;38:1161–1164. doi: 10.1515/CCLM.2000.178. [DOI] [PubMed] [Google Scholar]
- 18.Arao K, Fujiwara T, Taniguchi Y, Jinnouchi H, Sasai H, Matsumoto M, Funayama H, Ako J, Momomura SI. Implications of pentraxin 3 levels in patients with acute aortic dissection. Heart Vessel. 2015;30:211–217. doi: 10.1007/s00380-014-0470-2. [DOI] [PubMed] [Google Scholar]
- 19.Zhou Q, Chai X-P, Fang Z-F, Hu X-Q, Tang L. Association of plasma pentraxin-3 levels on admission with in-hospital mortality in patients with acute type a aortic dissection. Chin Med J. 2016;129:2589–2595. doi: 10.4103/0366-6999.192785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sawada H, Naito Y, Oboshi M, Soyama Y, Nishimura K, Eguchi A, Ando T, Okuhara Y, Morisawa D, Iwasaku T, Hirotani S, Mano T, Mitsuno M, Miyamoto Y, Masuyama T. Increment of pentraxin3 expression in abdominal aortic aneurysm. Int J Cardiol. 2015;195:281–282. doi: 10.1016/j.ijcard.2015.05.177. [DOI] [PubMed] [Google Scholar]
- 21.Papaspyridonos M, McNeill E, de Bono JP, Smith A, Burnand KG, Channon KM, Greaves DR. Galectin-3 is an amplifier of inflammation in atherosclerotic plaque progression through macrophage activation and monocyte chemoattraction. Arterioscler Thromb Vasc Biol. 2008;28:433–440. doi: 10.1161/ATVBAHA.107.159160. [DOI] [PubMed] [Google Scholar]
- 22.Leone M, Iacoviello M. The predictive value of plasma biomarkers in discharged heart failure patients: role of galectin-3. Minerva Cardioangiol. 2016;64:181–194. [PubMed] [Google Scholar]
- 23.Fashanu OE, Folsom AR, Oyenuga A, Ballantyne CM, Lutsey PL, Tang W. Galectin-3 and the incidence of abdominal aortic aneurysm: the atherosclerosis risk in communities (ARIC) study. Am J Cardiovasc Dis. 2017;7:114–121. [PMC free article] [PubMed] [Google Scholar]
- 24.Fernandez-García C-E, Tarin C, Roldan-Montero R, Martinez-Lopez D, Torres-Fonseca M, Lindhot JS, Vega de Ceniga M, Egido J, Lopez-Andres N, Blanco-Colio LM, Martín-Ventura JL. Increased galectin-3 levels are associated with abdominal aortic aneurysm progression and inhibition of galectin-3 decreases elastase-induced AAA development. Clin Sci Lond Engl. 2017;1979:2707–2719. doi: 10.1042/CS20171142. [DOI] [PubMed] [Google Scholar]
- 25.Martufi G, Gasser TC. Turnover of fibrillar collagen in soft biological tissue with application to the expansion of abdominal aortic aneurysms. J R Soc Interface. 2012;9:3366–3377. doi: 10.1098/rsif.2012.0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindholt JS, Heickendorff L, Vammen S, Fasting H, Henneberg EW. Five-year results of elastin and collagen markers as predictive tools in the management of small abdominal aortic aneurysms. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2001;21:235–240. doi: 10.1053/ejvs.2001.1329. [DOI] [PubMed] [Google Scholar]
- 27.Ormezzano O, Baguet J-P, Thony F, Blin D, Chavanon O, Toussaint B, Trocmé C, Vanzetto G, Faure P. Aminoterminal propeptide of type III procollagen (PIIINP) is associated with ascending aortic aneurysm growth rate. Int J Cardiol. 2010;145:379–380. doi: 10.1016/j.ijcard.2010.02.051. [DOI] [PubMed] [Google Scholar]
- 28.Tambyraja AL, Dawson ARW, Murie JA, Chalmers RTA. Cardiac troponin I predicts outcome after ruptured abdominal aortic aneurysm repair. Br J Surg. 2005;92:824–827. doi: 10.1002/bjs.4995. [DOI] [PubMed] [Google Scholar]
- 29.Li G, Wu X-W, Lu W-H, Cheng J, Wu X-Y, Ai R, Zhou ZH, Tang ZZ, Liao YH. High-sensitivity cardiac troponin T: a biomarker for the early risk stratification of type-A acute aortic dissection? Arch Cardiovasc Dis. 2016;109:163–170. doi: 10.1016/j.acvd.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Acosta S, Gottsäter A, Engström G, Melander O, Zarrouk M, Nilsson PM, Smith JG. B-type natriuretic peptide for prediction of incident clinically significant abdominal aortic aneurysm: a population-based prospective study. Vasc Med Lond Engl. 2018;23:46–51. doi: 10.1177/1358863X17745150. [DOI] [PubMed] [Google Scholar]
- 31.Taimour S, Zarrouk M, Holst J, Melander O, Engström G, Smith JG, Gottsäter A. No relation between biomarkers at age 47–49 and aortic diameter after 14–19 years of follow-up—a population-based study. Vasa. 2017;46:291–295. doi: 10.1024/0301-1526/a000632. [DOI] [PubMed] [Google Scholar]
- 32.Lu M, Zhan X. The crucial role of multiomic approach in cancer research and clinically relevant outcomes. EPMA J. 2018;9:77–102. doi: 10.1007/s13167-018-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng T, Zhan X. Pattern recognition for predictive, preventive, and personalized medicine in cancer. EPMA J. 2017;8:51–60. doi: 10.1007/s13167-017-0083-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Golubnitschaja O, Polivka J, Jr, Yeghiazaryan K, Berliner L. Liquid biopsy and multiparametric analysis in management of liver malignancies: new concepts of the patient stratification and prognostic approach. EPMA J. 2018;9:271–285. doi: 10.1007/s13167-018-0146-6. [DOI] [PMC free article] [PubMed] [Google Scholar]