Dr. Editor,
Primary CNSV diagnostic criteria includes: development of a neurological deficit unexplained by other processes; evidence of classic angiographic or histopathologic features of CNSV; and absence of any condition or systemic vasculitis that could elicit those features [1]. Intracerebral Hemorrhage (IH) is an uncommon manifestation in Central Nervous System Vasculitis (CNSV) [2,3]. The relationship between CNSV and Dermatomyositis is uncommon, and that is what makes the early diagnosis and appropriate treatment a challenge. We report a case of Dermatomyositis with bilateral IH and diagnosis of CNSV by angiography.
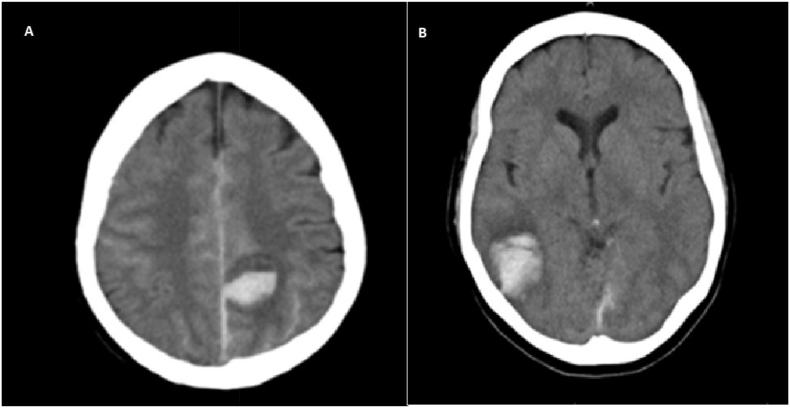
A 59-year-old right-handed woman with personal history of refractory Dermatomyositis, that was diagnosed 10 months prior this event, was admitted to the Emergency Department because of an intense and sudden onset headache on the left side. Before this event, she was treated with two 500 mg dose of Rituximab, receiving currently monthly intravenous gammaglobulins and daily oral 5 mg prednisone. She did not have a history of recent head trauma. On examination, her vital signs were normal. She showed facial erythema in a malar distribution, previously known. Neurological examination revealed no focal deficits. Brain computer tomography (CT) showed a left parietal IH (Fig. 1A). She did not need surgical treatment. The next day, she suffered again from an intense headache on the right side. Under neurological examination, mild left hemiparesia and tactile agnosia in the left extremities were found. A new CT found a righ temporooccipital IH without mass effect (Fig. 1B). A Magnetic Resonance (MRI) showed IH already known.
Fig. 1.
A) Left parietal intracerebral hemorrhage 27 × 16 mm. B) Right temporooccipital intracerebral hemorrhage 32.3 × 28.2 mm.
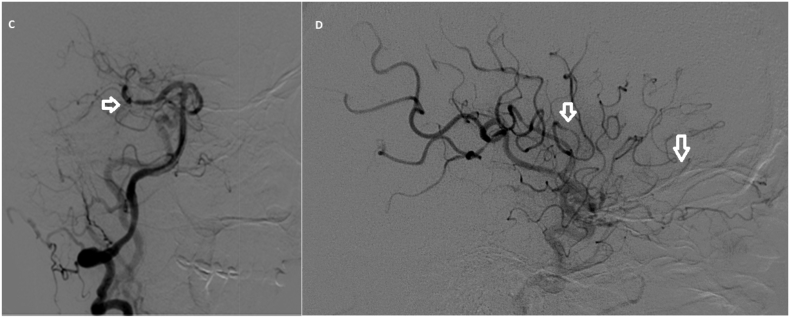
At that time, even if the patient had not previously presented signs of mild cognitive impairment, IH caused by cerebral amyloid angiopathy was considered due to the bilateral distribution. Because of recurrent hemorrhagic strokes in <48 h and previous history of Dermatomyositis, a diagnosis of CNSV was considered. A complete blood count, serum electrolytes, biochemistry (including muscle enzyme levels), serology, cancer biomarkers, and coagulation found no abnormalities. Autoimmunity laboratory tests revealed positive levels of Antinuclear Antibodies (1/320) and elevated levels of antiSSA/Ro antibodies (>100 U/ml) similar to the ones found ten months earlier, when Dermatomyositis was first diagnosed. Autoantibodies associated with inflamatory myopathies were negative. Serum C reactive protein was slightly high (1.06 mg/dl). Cerebral Angiography suggested a diagnostic of CNSV: areas of vascular constriction in the middle cerebral artery territory bilaterally and in the posterior cerebral artery (P2 segment) bilaterally (Fig. 2C and D). A lumbar puncture was not done because of previous CT findings, which indicated a risk of brain herniation due to intracranial hemorrhages size. A brain biopsy was not done. Toracic-abdominal-pelvic CT did not show any hidden cancer. A gynecological review took place with BIRADS 2 finding in the right breast, similar to the previous examination.
Fig. 2.
C) Vascular constriction in cerebral posterior artery (P2 segment). D) Areas of vascular constriction in cerebral middle artery.
She was treated with methylprednisolone (1 g/day for three days), and ciclofosfamide (500 mg every fifteen days) plus daily oral 10 mg prednisone. She recovered completely within three weeks, Modified Rankin score at discharge: 0. A new brain MRI including Gradient-Echo sequence was done three months after first hospital admission and there were no new radiological findings and did not show any Amyloid-Beta deposition. No new neurological or systemic events happened in the one year follow-up.
Dermatomyositis is known as a type of inflammatory myopathy. Whilst other rheumatologic illnesses such as Systemic Lupus Erythematosus frequently affect the central nervous system, Dermatomyositis does not [4].
Literature review found only eight cases which reported a relationship between Juvenile Dermatomyositis and CNSV [[5], [6], [7], [8], [9]]. The clinical course and prognostic was different from our case. As far as we know, there is only one case report of association between CNSV and refractory Dermatomiositis in adults [10]. Because of that, the possibility of other connective tissue diseases apart from Dermatomyositis was also considered in a differential diagnosis in our case, although no systemic sign or symptom were found; and there were no laboratory findings which supported this idea.
In addition, IH is not a common manifestation of CNSV [2,3]. Due to these considerations, a wide differential diagnoses of recurrent IH over two days without prior brain trauma was discused.
In this case, the good clinical response to immunosuppressant therapy permits us to establish a relationship between IH, CNSV and refractory Dermatomyositis. This would be the first case reported with these characteristics. Hence CNSV should be considered when assessing patients with Dermatomyositis and neurological deficits. Prompt diagnosis and inmunosuppressant treatment may be essential for a good outcome in such patients.
Disclosure of conflicts of interest
Authors do not have any conflicts of interest to disclose. All listed authors have seen and approved the submission.
References
- 1.Hajj-Ali R.A., Calabrese L.H. Central nervous system vasculitis. Curr. Opin. Rheumatol. 2009;21:10–18. doi: 10.1097/bor.0b013e32831cf5e6. [DOI] [PubMed] [Google Scholar]
- 2.Pomper M.G., Miller T.J., Stone J.H. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. Am. J. Neuroradiol. 1999;20:75–80. [PubMed] [Google Scholar]
- 3.Salvarani C., Brown R.D.J., Calamia K.T. Primary central nervous system vasculitis: analysis of 101 patients. Ann. Neurol. 2007;62:442–451. doi: 10.1002/ana.21226. [DOI] [PubMed] [Google Scholar]
- 4.Dutra L.A., de Souza A.W., Grinberg-Dias G. Central nervous system vasculitis in adults: an update. Autoimmun. Rev. 2017;16:123–131. doi: 10.1016/j.autrev.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Gotoff S.P., Smith R.D., Sugar O. Dermatomyositis with cerebral vasculitis in a patient with agammaglobulinemia. Am. J. Dis. Child. 1972;123:53–56. doi: 10.1001/archpedi.1972.02110070103015. [DOI] [PubMed] [Google Scholar]
- 6.Jimenez C., Rowe P.C., Keene D. Cardiac and central nervous system vasculitis in a child with dermatomyositis. J. Child. Neurol. 1994;9:297–300. doi: 10.1177/088307389400900315. [DOI] [PubMed] [Google Scholar]
- 7.Falcini F., Trapani S., Ermini M. Systemic vasculitis in juvenile dermatomyositis: a fatal case. Clin. Exp. Rheumatol. 1995;13:531–532. [PubMed] [Google Scholar]
- 8.Ramanan A.V., Sawhney S., Murray K.J. Central nervous system complications in two cases of juvenile onset dermatomyositis. Rheumatology. 2001;40:1293–1298. doi: 10.1093/rheumatology/40.11.1293. [DOI] [PubMed] [Google Scholar]
- 9.Elst E.F., Kamphuis S.S., Prakken B.J. Severe central nervous system involvement in juvenile dermatomyositis. J Rheumatol. 2003;30:2059–2063. [PubMed] [Google Scholar]
- 10.Regan M., Haque U., Pomper M. Central nervous system vasculitis as a complication of refractory dermatomyositis. J Rheumatol. 2001;28:207–211. [PubMed] [Google Scholar]