Abstract
Study Design:
Retrospective chart review.
Objective:
To determine the relative cost-effectiveness of spinal anesthesia and general anesthesia for lumbar laminectomy and microdiscectomy surgery performed in an academic versus private practice hospital setting.
Methods:
The authors retrospectively reviewed charts of 188 consecutive patients who underwent lumbar laminectomy or microdiscectomy by a single surgeon from 2012 to 2016 at either an academic or a private practice hospital setting. Intraoperative and postoperative outcomes were recorded and direct variable costs were calculated.
Results:
At the academic institution, the direct cost of a lumbar laminectomy or microdiscectomy surgery under general anesthesia was determined to be 9.93% greater than with spinal anesthesia (P = .040). The greatest difference was seen with operating room costs, in which general anesthesia was associated with 18.74% greater costs than spinal anesthesia (P = .016). There was no significant difference in cost at the private practice hospital setting.
Conclusions:
We conclude that use of spinal anesthesia for lumbar laminectomy leads to less operating room, postanesthesia care unit, and anesthesia times, lower levels of postoperative pain, and no increased rate of other complications compared with general anesthesia at an academic institution as compared to a private practice setting. Spinal anesthesia is 9.93% less expensive than general anesthesia, indicating substantial cost-saving potential. With no sacrifice of patient outcomes and the added benefit of less pain and recovery time, Spinal anesthesia represents a more cost-effective alternative to general anesthesia in lumbar spine surgery in the academic hospital setting.
Keywords: lumbar, laminectomy, discectomy, orthopedic, back pain
Introduction
Lumbar laminectomy and microdiscectomy surgeries may be performed using various anesthetic techniques. General anesthesia has traditionally been preferred, perhaps due to a combination of surgeon preference, anesthesiologist comfort level, and patient perception of the standard of care. However, spinal anesthesia may also be used for these procedures, and recent research has supported its use as an effective alternative to general anesthesia.
Several studies have compared the use of general anesthesia and spinal anesthesia in spinal procedures in terms of perioperative complication rates, hemodynamic parameters, and operative, anesthesia, and recovery times.1-15 A majority of these studies observed fewer complications, more favorable hemodynamic parameters, and shorter anesthetic time spent with spinal anesthesia than with general anesthesia, suggesting that this anesthetic modality may even be a superior alternative to the perceived standard of care.1-11 However, other studies have found no difference in perioperative outcomes between spinal anesthesia and general anesthesia even finding general anesthesia to be superior in some respects, particularly in surgeon satisfaction.14,15
The rate of lumbar spine surgery has been increasing over the past several decades and constitutes a sizeable portion of health care spending in the United States.16 Therefore, in addition to perioperative outcomes, the relative cost of these procedures under spinal anesthesia versus general anesthesia may be of particular interest to providers and administrators seeking to provide more cost-effective care. Two studies were identified that made this comparison in the context of spine surgery, both finding spinal anesthesia to be significantly less costly than general anesthesia.17,18 However, there is a current paucity of research evaluating perioperative outcomes of lumbar laminectomies and microdiscectomies achieved using spinal anesthesia and general anesthesia with direct reference to their relative cost in an academic setting versus private practice setting. Direct comparison of these two anesthetic modalities in terms of both cost and outcomes is necessary to determine their relative cost-effectiveness, which may help guide future discussions of the standard of care. Here we present a retrospective study that seeks to compare the use of spinal anesthesia with general anesthesia in lumbar spine surgery in terms of acute perioperative outcomes and direct cost of the procedure in an academic and a private practice hospital setting.
Materials and Methods
Study Design
In this retrospective chart review, the authors reviewed the electronic medical records of all surgical cases meeting inclusion criteria and consulted with hospital revenue cycle teams to obtain outcomes and cost data, respectively. This data was then analyzed based on anesthetic modality to produce a cost-effectiveness evaluation.
Setting
All procedures took place in either (1) an urban tertiary-care level university-affiliated teaching hospital or in (2) a suburban tertiary-care level private hospital, located in similar demographic areas. Institutional review board approval was obtained from both institutions. All procedures were performed by a single surgeon who relocated from the academic to the private practice hospital setting in 2015.
Patients
Patients were included in this study if they had undergone a lumbar laminectomy or microdiscectomy procedure by a single surgeon from 2012 to 2016. These procedures were considered to be of similar invasiveness and duration, and therefore were analyzed together. Patients undergoing lumbar fusion, vertebroplasty, or repair of iatrogenic dural tear were excluded due to differences in invasiveness and duration. The decision to administer spinal anesthesia vs. general anesthesia was based on individual patient preference after being explained both techniques. Patients with a difficult airway were excluded from receiving spinal anesthesia. The authors obtained a list of all surgical cases by the surgeon in question using institutional databases, and identified eligible patients based on date of surgery and Current Procedural Terminology (CPT) or International Classification of Diseases, 10th Revision (ICD-10) codes.
Anesthetic Technique
For spinal anesthesia, a midline approached was used to puncture the dura and deposit local anesthetic, bupivacaine with or without fentanyl, to achieve an adequate sensory level. Subsequently, moderate sedation was achieved with short-acting intravenous agents consisting of a combination of midazolam, fentanyl, and propofol. All patients were given an antiemetic. General anesthesia used a balanced technique with the airway being secured via an endotracheal intubation. The patients were induced with a combination of midazolam, opioid, lidocaine, and a muscle relaxant. The balanced technique consisted of sevoflurane and opioids. All patients were administered an antiemetic prophylactically.
Variables
Patient characteristics included age, sex, body mass index, medical comorbidities, and preoperative diagnosis. Operative characteristics included anesthetic modality, procedure performed, spinal levels operated upon, and discharge status. Intraoperative complications included estimated blood loss (EBL), incidence of dural tear, corneal abrasion, and dental injury. Postoperative complications included nausea/vomiting, urinary retention, pain, opioid requirement, spinal headache, and 30-day readmission rate. Procedural times included operating room (time spent by patient in the operating room [OR]), anesthesia (time spent under anesthesia), surgical (time elapsed from skin incision to closure), and postanesthesia care unit (PACU). PACU time was further subdivided into phase 1 (higher intensity nursing care following the procedure) and phase 2 (lower intensity nursing care before discharge, once the patient has been deemed medically stable). Patients discharged to inpatient floors did not receive phase 2 care, so these patients excluded from calculations of phase 2 time.
Data Collection
All patient data was deidentified and entered into a Microsoft Excel document to which only the authors were permitted access. All clinical outcomes data was obtained from electronic medical records. Specifically, patient characteristics were obtained from hospital intake and preoperative surgical notes, intraoperative complications were obtained from operative notes, and postoperative complications were obtained from PACU nursing notes.
Cost data was obtained from the revenue cycle team of each hospital who were unaffiliated with the authorship and blinded to the study outcome measures. All costs included in this study are listed as net costs to the hospital, or the price that the hospital pays for goods and services, rather than prices billed to the patient or insurers. For the purposes of this study, only costs that are directly attributable to patient care (direct costs) and nonfixed prior to the procedure were included in the analysis. Indirect costs, such as administration, cafeteria, and laundry services, were excluded, as they are unlikely to be affected by anesthetic modality used. Surgeon fee and implantable device costs, although directly related to patient care, were excluded for this same reason. If patients were admitted following the procedure, costs related to hospitalization were excluded, as this would substantially affect the results and may due more to preexisting patient characteristics than acute issues related to anesthetic modality. Costs were categorized based on hospital billing methods, as follows: (1) OR costs, including all OR support staff, medical/surgical supplies, sterilization procedures, and drugs; (2) anesthesia costs, including anesthesiologist fee; and (3) recovery costs, including all PACU support staff, medical/surgical supplies, and drugs. The private hospital included in this study uses private anesthesiologist groups and was unable to provide cost data for anesthesiologist fee. Therefore, anesthesia cost for this surgical site was calculated with the same billing formula used by anesthesiologists in the teaching hospital.
Statistical Analysis
Patients were grouped based on anesthetic modality. Clinical outcomes data from both surgical sites was pooled and analyzed together. However, average direct cost using spinal anesthesia and general anesthesia was calculated separately for each surgical site, as costs were likely to differ between private and teaching hospitals. Mean and standard deviation of general anesthesia and spinal anesthesia groups were calculated for each descriptive parameter recorded. Tests for significance were executed using 2-tailed t tests with assumption of nonsimilar variance for all continuous variables, chi-square tests for all commonly occurring categorical variables, and Fischer exact test for all rarely occurring categorical variables. A P value <.05 was used to establish statistical significance. If patients were administered spinal anesthesia but converted to general anesthesia during the procedure, they were analyzed as having received spinal anesthesia.
Results
A total of 188 patients met inclusion criteria for this study; of these, 97 received spinal anesthesia and 91 received general anesthesia. Only 1 patient experienced a failed spinal anesthesia, which required conversion to general anesthesia. The two groups were similar in terms of age, body mass index, and preoperative diagnosis. However, patients receiving general anesthesia were more likely to be female, have more medical comorbidities, have more spinal levels operated on, and be discharged to a hospital bed than patients receiving spinal anesthesia (Table 1).
Table 1.
Patient Characteristics.a
| Anesthetic Modality | P | ||
|---|---|---|---|
| Spinal | General | ||
| No. of patients, n | 97 | 91 | — |
| Age (years), mean ± SD | 54.49 ± 2.99 | 54.55 ± 3.44 | .981 |
| Sex (male/female), n | 57/42 | 37/54 | .020 |
| Body mass index (kg/m2), mean ± SD | 29.56 ± 1.17 | 29.91 ± 1.12 | .678 |
| Comorbidities, mean ± SD | 0.97 ± 0.21 | 1.31 ± 0.20 | .026 |
| Preoperative diagnosis (%) | .075 | ||
| Spinal stenosis | 97.9 | 91.2 | |
| Disc displacement | 4.1 | 13.2 | |
| Other | 6.2 | 3.3 | |
| No. of spinal levels, n | 1.26 ± 0.09 | 1.46 ± 0.14 | .014 |
| Discharge to: home/floor, n | 95/2 | 74/17 | <.001 |
a The sum of patients with each preoperative diagnosis exceeds 100% of patients, as several patients in each group carried more than 1 diagnosis. All listed values use 95% confidence intervals as measures of precision.
In terms of intraoperative complications, spinal anesthesia and general anesthesia performed similarly. There were no significant differences between the two groups in terms of EBL or rate of dural tears requiring primary suture closure. There were no incidents of corneal abrasion or dental injury in either group (Table 2). In terms of postoperative complications, both groups experienced similar rates of nausea/vomiting and were administered a similar amount of antiemetic medication. The 2 groups experienced similar rates of urinary retention, postoperative spinal headache, and 30-day readmission rates. The spinal anesthesia group experienced significantly less pain than the general anesthesia group, both immediately postoperatively and on discharge from the PACU. Patients undergoing spinal anesthesia for their lumbar spine procedure were less likely to require postoperative opioids and received fewer doses of opioids than those undergoing general anesthesia. In addition, time elapsed from entering the PACU to first opioid administration was less with general anesthesia. These results indicate that the general anesthesia group experienced more pain, earlier in the postoperative period than the spinal anesthesia group (Table 2).
Table 2.
Procedural Complications.a
| Anesthetic Modality | P | ||
|---|---|---|---|
| Spinal | General | ||
| Intraoperative | |||
| EBL (mL), mean ± SD | 49.33 ± 4.91 | 53.68 ± 5.76 | .261 |
| Dural tear, % | 4.12 | 2.20 | .683 |
| Corneal abrasion, % | 0 | 0 | — |
| Dental injury, % | 0 | 0 | — |
| Postoperative | |||
| Nausea/vomiting, n (%) | 26 (26.80) | 18 (20.22) | .292 |
| Antiemetic medication given (doses)b, mean ± SD | 0.29 ± 0.12 | 0.31 ± 0.14 | .841 |
| Urinary retention, n (%) | 1 (1.10%) | 3 (3.27%) | .356 |
| Initial PACU pain (1-10), mean ± SD | 0.64 ± 0.38 | 3.06 ± 0.69 | <.001 |
| End PACU pain (1-10), mean ± SD | 1.34 ± 0.34 | 2.63 ± 0.53 | <.001 |
| Patients requiring opioids in PACU, n (%) | 52 (53.61) | 74 (81.32) | <.001 |
| Opioids given in PACU (doses),c mean ± SD | 1.13 ± 0.36 | 4.30 ± 0.87 | <.001 |
| Time to first opioid administration (min),d mean ± SD | 80.38 ± 15.97 | 40.73 ± 7.20 | <.001 |
| Spinal headache, n (%) | 4 (4.12%) | 1 (1.10%) | .370 |
| 30-day readmission rate, n (%) | 3.09% | 4.40% | .714 |
Abbreviations: EBL, estimated blood loss; PACU, postanesthesia care unit.
a All listed values use 95% confidence intervals as measures of precision
b One dose of antiemetic medication was considered to be equivalent to: 4 mg ondansetron intravenously, 6.25 mg promethazine intravenously, or 10 mg metoclopramide intraveously.
c One dose of opioid medication was considered to be equivalent to: 2 mg morphine intravenously, 0.25 mg hydromorphone intravenously, 25 μg fentanyl subcutaneously, 5 mg oxycodone orally, 10 mg hydrocodone orally, 50 mg tramadol orally, and 30 mg codeine orally.
d Indicates time elapsed from entering the PACU to first administration of opioid medication.
Patients receiving spinal anesthesia almost uniformly spent less time in the various stages of the procedure than patients receiving general anesthesia. The spinal anesthesia group underwent significantly less OR time, surgical time, anesthesia time, and PACU time than the general anesthesia group. When PACU time is subdivided into phase 1 and phase 2 care, the spinal anesthesia group spent significantly less time in phase 1. However, phase 2 times were not significantly different between groups (Table 3).
Table 3.
Time Parameters.a
| Anesthetic Modality | P | ||
|---|---|---|---|
| Spinal | General | ||
| OR time (min) | 138.23 ± 5.25 | 176.44 ± 16.87 | <.001 |
| Surgery time (min) | 84.98 ± 3.97 | 100.58 ± 5.18 | <.001 |
| Anesthesia time (min) | 148.93 ± 5.22 | 178.99 ± 7.33 | <.001 |
| PACU time (total) (min) | 214.00 ± 15.16 | 248.99 ± 26.64 | .0269 |
| Phase 1 | 89.08 ± 9.97 | 123.42 ± 12.32 | <.001 |
| Phase 2 | 131.31 ± 14.19 | 154.40 ± 31.33 | .191 |
Abbreviations: OR, operating room; PACU, postanesthesia care unit.
a All listed values use 95% confidence intervals as measures of precision.
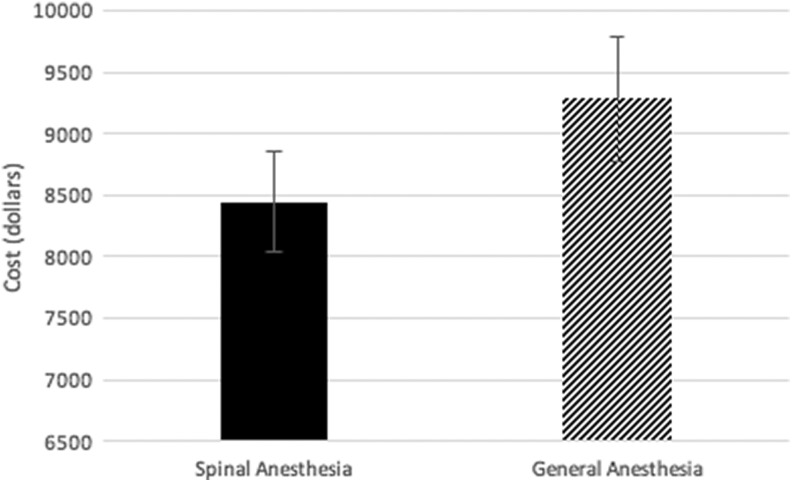
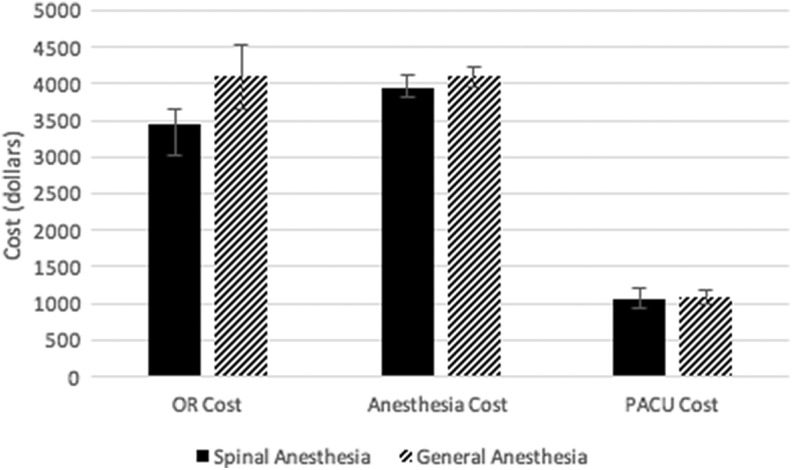
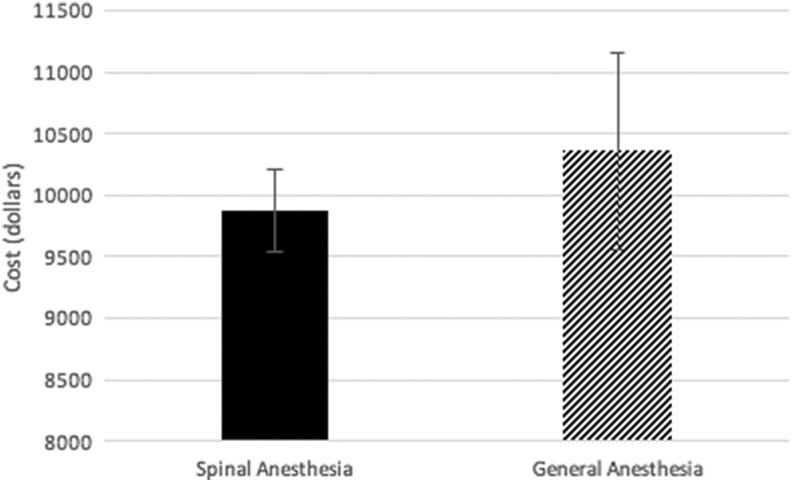
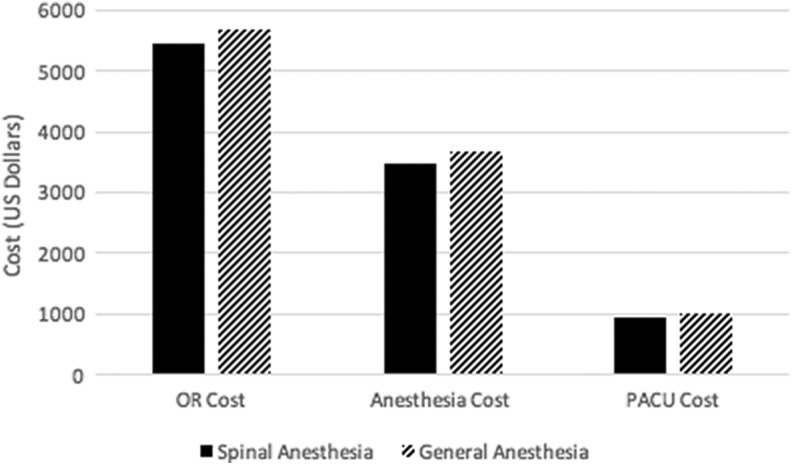
Cost was subdivided by type of anesthesia used as well as location of the surgery. At the academic institution, the direct cost of a lumbar laminectomy or microdiscectomy surgery under general anesthesia was determined to be 9.93% greater than with general anesthesia (P = .040) (Figure 1). The greatest difference was seen with OR costs, in which general anesthesia was associated with 18.74% greater costs than spinal anesthesia (P = .016) (Figure 2). In terms of anesthesia and PACU costs, no significant difference was observed between spinal anesthesia and general anesthesia (Table 4). At the private practice institution, the direct cost was found to be 4.29% greater with general anesthesia than with spinal anesthesia (P = .286) (Figure 3). The spinal anesthesia group had slightly lower costs in terms of OR, anesthesia, and PACU costs, but none of these differences was statistically significant (Table 5; Figure 4).
Figure 1.
Total costs for site 1 (academic hospital setting). The shown cost values include operating room (OR) and postanesthesia care unit (PACU) time, OR and PACU ancillary personnel, medical and surgical supplies, sterile supplies, pharmaceuticals, and anesthesiologist fee.
Figure 2.
Itemized costs for site 1 (academic hospital setting). The shown values for operating room (OR) cost include OR time, OR ancillary personnel, medical and surgical supplies, sterile supplies, and pharmaceuticals administered in the OR. The values for anesthesia cost include anesthesiologist fee. The values for postanesthesia care unit (PACU) cost include PACU time, PACU ancillary personnel, and pharmaceutical administered in the PACU.
Table 4.
Direct Costs (in $): Site 1 (Academic Hospital Setting).a
| Anesthetic Modality | P | ||
|---|---|---|---|
| Spinal | General | ||
| OR costs | 3453.65 ± 198.22 | 4101.01 ± 437.37 | .016 |
| Anesthesia costs | 3940.80 ± 183.75 | 4100.46 ± 133.84 | .394 |
| PACU costs (total) | 1051.82 ± 146.76 | 1084.32 ± 106.91 | .831 |
| Phase 1 | 755.28 ± 161.99 | 720.64 ± 70.80 | .704 |
| Phase 2 | 296.54 ± 136.66 | 363.68 ± 121.70 | .425 |
| Total costs | 8446.27 ± 411.78 | 9285.78 ± 509.57 | .040 |
Abbreviations: OR, operating room; PACU, postanesthesia care unit.
a All listed values use 95% confidence intervals as measures of precision.
Figure 3.
Total costs for site 2 (private practice hospital setting). The shown cost values include operating room (OR) and postanesthesia care unit (PACU) time, OR and PACU ancillary personnel, medical and surgical supplies, sterile supplies, pharmaceuticals, and anesthesiologist fee.
Table 5.
Direct Costs (in $): Site 2 (Private Practice Hospital Setting).a
| Anesthetic modality | P | ||
|---|---|---|---|
| Spinal | General | ||
| OR costs | 5469.74 ± 283.98 | 5693.29 ± 647.33 | .542 |
| Anesthesia costs | 3468.15 ± 105.75 | 3664.17 ± 224.99 | .136 |
| PACU costs (total)b | 938.47 ± 74.43 | 1005.13 ± 176.90 | .504 |
| Total costs | 9876.36 ± 335.97 | 10 362.59 ± 802.59 | .286 |
Abbreviations: OR, operating room; PACU, postanesthesia care unit.
a All listed values use 95% confidence intervals as measures of precision.
b The private hospital in this study did not incorporate phase 2 PACU care into cost.
Figure 4.
Itemized costs based on location of care for site 2 (private practice hospital setting). The shown values for operating room (OR) cost include OR time, OR ancillary personnel, medical and surgical supplies, sterile supplies, and pharmaceuticals administered in the OR. The values for anesthesia cost include anesthesiologist fee. The values for postanesthesia care unit (PACU) cost include PACU time, PACU ancillary personnel, and pharmaceutical administered in the PACU.
Discussion
The key finding of this study was lower postoperative pain and opioid usage, shorter operative and recovery times, and cost savings seen by using spinal anesthesia over general anesthesia for lumbar laminectomy and microdiscectomy surgery in the academic hospital setting versus the private practice setting. These findings are largely in accordance with prior research comparing these two anesthetic modalities in lumbar spine procedures in academic hospital settings.1-6 Although induction is typically more rapid with general anesthesia, time required to assess patient responsiveness and respiratory function prior to extubation leads to a net increase in anesthesia time.5 Some studies have observed greater blood loss with general anesthesia than with spinal anesthesia, but others, including the present study, have found no difference.7 If a true difference exists, it may be in part due to a drop in systemic vascular resistance caused by spinal anesthesia–induced sympathetic blockade.19 This is the same mechanism proposed by Sadrolsadat et al15 for the increased incidence of nausea/vomiting seen among spinal anesthesia patients in that study. Our results similarly show greater incidence of nausea/vomiting with spinal anesthesia, although the difference was not significant. Perhaps any primary effect of increased nausea/vomiting seen with spinal anesthesia is offset by increased postoperative opioid pain medication requirements of general anesthesia patients—a known side effect of which is nausea/vomiting.
Significantly increased postoperative pain and opioid administration with general anesthesia over spinal anesthesia has been consistently observed in recent research.1,3,5-7 This may be caused by a direct inhibitory effect exerted by local anesthetic on nociceptive fibers. Pain fibers are smaller and thus generally more susceptible to local anesthetic than larger motor fibers; therefore, the analgesic effect of spinal anesthesia often outlasts the motor blockade.13
Iatrogenic urinary retention and dural tear both represent incidents of neural injury to which spinal anesthesia patients are theoretically at greater risk.21 Urinary retention has been hypothesized to be the result of either mechanical nerve root injury during spinal administration or excess duration of block, leading to delayed discharge or prompt readmission.20 Dural tear is a surgical complication that may be provoked by excessive patient movement during surgery. A potential concern among surgeons is that although patients are sedated under spinal anesthesia, movement of the upper extremities is possible and may become excessive if sedation is too light.14 Nonetheless, our results show no significant differences between spinal anesthesia and general anesthesia groups in terms of these complications.
Because spinal anesthesia appears to be similar or superior to general anesthesia in terms of clinical outcomes, a discussion of cost is clinically relevant. Variation exists between the 2 surgical sites of this study, in terms of both cost values and methods of documenting and calculating procedural costs. Therefore, separate cost analyses of spinal anesthesia and general anesthesia groups were performed for each site to avoid this confounding factor. Our results show that use of spinal anesthesia is associated with roughly 4% to 10% lower costs than general anesthesia. This is a more modest cost savings than calculated by prior research investigating this topic. Agarwal et al17 found that spinal anesthesia was associated with a 41.1% reduction in direct costs of lumbar laminectomies and discectomies at an academic hospital setting. However, nearly half of the observed effect was attributable to hospitalization costs. In the present study, hospital admission costs were considered a potential confounder due to indirect association with use of general anesthesia and were therefore excluded from analysis. At both sites of this study, OR costs constituted the bulk of the observed difference in direct costs, which is consistent with previous findings.17,18
Although both hospitals mentioned in this study observed lower costs with spinal anesthesia than with general anesthesia, this difference was only significant at the large academic hospital setting. This discrepancy may be due in part to different cost calculation methods, materials used, or operative, anesthesia, and nursing practices at each hospital. Given that OR costs are the largest cost component at each hospital, any difference in practices affecting this metric is likely responsible. Therefore, it appears that the teaching environment may contribute to increased operative costs with general anesthesia relative to spinal anesthesia, as this difference is not as dramatic in the purely private setting. Future research in the private hospital setting is needed to investigate cost-influencing factors using spinal anesthesia versus general anesthesia in greater detail, as this setting constitutes an immense portion of health care spending in the United States.
One limitation of this study is selection bias evidenced by demographic differences between the two groups. On average, the general anesthesia group carried a greater number of medical comorbidities and had more spinal levels operated upon than the spinal anesthesia group. Sicker patients undergoing more extensive procedures may be at greater risk of respiratory compromise. Prone positioning enhances these risks, so securing the airway via endotracheal intubation may be preferable in select patients.22 A common limitation of case-control studies is restriction of outcome measures to those routinely recorded. A frequently cited factor influencing the choice of anesthetic method is surgeon/patient satisfaction, but there is a current lack of consensus in the literature regarding this topic. Several randomized controlled trials have found higher surgeon satisfaction scores with lumbar spine procedures under spinal anesthesia than general anesthesia.4-6 However, Kahveci et al14 and Sadrolsadat et al15 conducted randomized controlled trials of 80 and 100 patients, respectively, and came to opposite conclusions, citing unfamiliarity and patient wakefulness as sources of dissatisfaction with spinal anesthesia. Few studies have measured patient satisfaction with anesthesia for spine procedures, but to our knowledge have found positive results with spinal anesthesia.6,13 Earlier discharge and postoperative pain found in the current study could potentially be associated with higher patient satisfaction when undergoing spinal anesthesia. However, patient anxiety, discomfort during anesthesia administration, and residual effects may also affect satisfaction, and would be difficult to predict without formal evaluation of this measure. Although reported satisfaction is inherently subject to individual biases, it remains an important factor in choice of anesthesia, and should be investigated in future prospective trials.
A common deterrent to performing any procedure under spinal anesthesia is concern that unforeseen events may prolong the surgery lead to premature resolution of anesthesia. This is a valid concern, but the risk of premature resolution of anesthesia is directly related to variation in surgical times. Therefore, this risk can be mitigated through precision of surgical times. It should be noted that the surgery/anesthesia team in this study began performing these procedures under spinal anesthesia only after enough cases were completed under general anesthesia to attain what was considered an acceptable level of precision. The authors recommend performing at least 20 to 30 lumbar laminectomies or microdiscectomies before initiating the use of spinal anesthesia.
Conclusions
The present findings show that the use of spinal anesthesia in lumbar laminectomy and microdiscectomy procedures is associated with less time spent in the OR, PACU, and under anesthesia than with general anesthesia, as well as less postoperative pain and opioid requirement in the academic hospital setting. However, no difference was observed between groups in terms of blood loss, intraoperative dural tear, nausea/vomiting, urinary retention, spinal headache, and 30-day readmission rate. Additionally, use of general anesthesia was associated with 4.29% to 9.93% greater costs than the use of spinal anesthesia, for a total direct cost savings of $423.41 to $838.48 per procedure. With no sacrifice of patient outcomes and the added benefit of less pain and recovery time, we conclude that spinal anesthesia represents a more cost-effective alternative to general anesthesia in lumbar spine surgery.
Acknowledgments
The authors would like to acknowledge the following contributors, without whom this study would not have been possible: Lavana Ragavan, Performance Improvement Manager, Montefiore Medical Center, Bronx, NY 10 461 and Gladys Attanasio, Assistant Vice President of Revenue Cycle, St John’s Riverside Hospital, Yonkers, NY 10 701.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Jellish WS, Thalji Z, Stevenson K, Shea J. A prospective randomized study comparing short- and intermediate-term perioperative outcome variables after spinal or general anesthesia for lumbar disk and laminectomy surgery. Anesth Analg. 1996;83:559–564. [DOI] [PubMed] [Google Scholar]
- 2. McLain RF, Bell GR, Kalfas I, Tetzlaff JE, Yoon HJ. Complications associated with lumbar laminectomy: a comparison of spinal versus general anesthesia. Spine (Phila Pa 1976). 2004;29:2542–2547. [DOI] [PubMed] [Google Scholar]
- 3. McLain RF, Kalfas I, Bell GR, Tetzlaff JE, Yoon HJ, Rana M. Comparison of spinal and general anesthesia in lumbar laminectomy surgery: a case-controlled analysis of 400 patients. J Neurosurg Spine. 2005;2:17–22. [DOI] [PubMed] [Google Scholar]
- 4. McLain RF, Tetzlaff JE, Bell GR, Uwe-Lewandrowski K, Yoon HJ, Rana M. Microdiscectomy: spinal anesthesia offers optimal results in general patient population. J Surg Orthop Adv. 2007;16:5–11. [PubMed] [Google Scholar]
- 5. Attari M, Mirhosseini S, Honarmand A, Safavi MR. Spinal anesthesia versus general anesthesia for elective lumbar spine surgery: a randomized clinical trial. J Res Med Sci. 2011;16:524–529. [PMC free article] [PubMed] [Google Scholar]
- 6. Dagher C, Naccache N, Narchi P, Hage P, Antakly MC. Regional anesthesia for lumbar microdiscectomy [in French]. J Med Liban. 2002;50:206–210. [PubMed] [Google Scholar]
- 7. De Rojas JO, Syre P, Welch WC. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: a review of the modern literature. Clin Neurol Neurosurg. 2014;119:39–43. doi:10.1016/j.clineuro.2014.01.016 [DOI] [PubMed] [Google Scholar]
- 8. Demeril CB, Kalayci M, Ozkocak I, Altunkaya H, Ozer Y, Acikgoz B. A prospective randomized study comparing perioperative outcome variables after epidural of general anesthesia for lumbar disc surgery. J Neurosurg Anesthesiol. 2003;15:185–192. [DOI] [PubMed] [Google Scholar]
- 9. Tetzlaff JE, Dilger JA, Kodsy M, al-Bataineh J, Yoon HJ, Bell GR. Spinal anesthesia for elective lumbar spine surgery. J Clin Anesth. 1998;10:666–669. [DOI] [PubMed] [Google Scholar]
- 10. Ulutas M, Secer M, Taskapilioglu O, et al. General versus epidural anesthesia for lumbar microdiscectomy. J Clin Neurosci. 2015;22:1309–1313. [DOI] [PubMed] [Google Scholar]
- 11. Singeisen H, Hodel D, Schindler C, Frey K, Eichenberger U, Hausmann ON. Significantly shorter anesthesia time for surgery of the lumbar spine: process analytical comparison of spinal anesthesia and intubation narcosis [in German]. Anaesthesist. 2013;62:632–638. doi:10.1007/s00101-013-2204-8 [DOI] [PubMed] [Google Scholar]
- 12. Chen HT, Tsai CH, Chao SC, et al. Endoscopic discectomy of L5-S1 disc herniation via an interlaminar approach: prospective controlled study under local and general anesthesia. Surg Neurol Int. 2011;2:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hassi N, Badaoui R, Cagny-Bellet A, Sifeddine S, Ossart M. Spinal anesthesia for disk herniation and lumbar laminectomy. Apropos of 77 cases [in French]. Cah Anesthesiol. 1995;43:21–25. [PubMed] [Google Scholar]
- 14. Kahveci K, Doger C, Ornek D, Gokcinar D, Aydemir S, Ozay R. Perioperative outcome and cost-effectiveness of spinal versus general anesthesia for lumbar spine surgery. Neurol Neurochir Pol. 2014;48:167–173. doi:10.1016/j.pjnns.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 15. Sadrolsadat SH, Mahdavi AR, Moharari RS, et al. A prospective randomized trial comparing the technique of spinal and general anesthesia for lumbar disk surgery: a study of 100 cases. Surg Neurol. 2009;71:60–65. doi:10.1016/j.surneu.2008.08.003 [DOI] [PubMed] [Google Scholar]
- 16. Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976). 2006;31:2707–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Agarwal P, Pierce J, Welch WC. Cost analysis of spinal versus general anesthesia for lumbar diskectomy and laminectomy spine surgery. World Neurosurg. 2016;89:266–271. doi:10.1016/j.wneu.2016.02.022 [DOI] [PubMed] [Google Scholar]
- 18. Walcott BP, Khanna A, Yanamadala V, Coumans JV, Peterfreund RA. Cost analysis of spinal and general anesthesia for the surgical treatment of lumbar spondylosis. J Clin Neurosci. 2015;22:539–543. doi:10.1016/j.jocn.2014.08.024 [DOI] [PubMed] [Google Scholar]
- 19. Modig J. Beneficial effects on intraoperative and postoperative blood loss in total hip replacement when performed under lumbar epidural anesthesia: an explanatory study. Acta Chir Scand Suppl. 1989;550:95–103. [PubMed] [Google Scholar]
- 20. Bjerregaard LS, Bogø S, Raaschou S, et al. Incidence of and risk factors for postoperative urinary retention in fast-track hip and knee arthroplasty. Acta Orthop. 2015;86:183–188. doi:10.3109/17453674.2014.972262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baldini G, Bagry H, Aprikian A, Carli F. Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology. 2009;110:1139–1157. [DOI] [PubMed] [Google Scholar]
- 22. Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008;100:165–183. [DOI] [PubMed] [Google Scholar]