Abstract
Study Design:
Systematic review and meta-analysis.
Objective:
Compare the clinical and radiographic outcomes of anterior cervical discectomy and fusion (ACDF) with a stand-alone interbody cage versus a conventional cage and anterior cervical plate technique.
Methods:
A systematic Medline search was conducted using PubMed, EMBASE, and Cochrane Library Database of Systematic Reviews. Search terms included “anterior cervical discectomy and fusion,” “cage,” and “bone plates,” or variations thereof. Only studies involving a direct comparison of ACDF with a stand-alone cage versus a cage and plate were included. From the selected studies, we extracted data on patient demographics, comorbidities, surgical risk factors, and pre- and postoperative radiographic findings. A meta-analysis was performed on all outcome measures. The quality of each study was assessed using the Downs and Black checklist.
Results:
Nineteen studies met the inclusion and exclusion criteria. Patients who underwent ACDF with a cage-only technique had significantly lower rates of postoperative dysphagia and adjacent segment disease compared with patients who underwent ACDF with a cage-plate technique. However, patients who underwent ACDF with a cage-plate technique had better radiographic outcomes with significantly less subsidence and better restoration of cervical lordosis. There were no other significant differences in outcomes or postoperative complications.
Conclusions:
ACDF with a cage-only technique appears to have better clinical outcomes than the cage-plate technique, despite radiographic findings of increased rates of subsidence and less restoration of cervical lordosis. Future randomized controlled trials with longer term follow-up are needed to confirm the findings of this meta-analysis.
Keywords: cervical, degenerative disc disease, discectomy, ACDF, fixation
Introduction
Since its initial description by Smith and Robinson1 in 1958, anterior cervical discectomy and fusion (ACDF) has been used for the treatment of cervical degenerative disc disease, radiculopathy, and myelopathy.2–5 Developments in ACDF techniques have led to the introduction and routine application of anterior plate fixation in order to provide additional stability.6 However, there have been reports of complications associated with anterior cervical plates, such as esophageal soft tissue damage, neurovascular injuries, and dysphagia.7,8 To address these complications, stand-alone interbody cages were designed to provide stability and facilitate fusion between cervical vertebrae without necessitating the use of an anterior plate.9 This new technique, however, has its own complications, such as cage subsidence, cervical dislocation, and cervical kyphosis.10 Past studies have compared the 2 techniques, but a general consensus has not yet been reached about the superiority of one technique over the other.
To date, 2 meta-analyses have been published comparing the use of a zero-profile device versus a cage and plate technique in ACDF.11,12 Both studies, however, were limited by a relative paucity of studies—11 and 7, respectively. The primary goal of this study was to perform a systematic review and meta-analysis to compare the clinical and radiographic outcomes of ACDF with a stand-alone interbody cage versus a conventional cage and anterior cervical plate.
Methods
Literature Search
We performed a systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and review recommendations.13,14 A systematic Medline search was conducted using PubMed, EMBASE, and the Cochrane Library Database of Systematic Reviews, using a search strategy with the terms “anterior cervical discectomy and fusion,” “cage,” and “bone plates,” or variations thereof.
Inclusion and Exclusion Criteria
To meet inclusion criteria for this analysis, the study must have directly compared ACDF with a stand-alone cage and ACDF with a cage and anterior cervical plate. Study designs were either prospective or retrospective cohort studies. Only human studies were included. Cadaver studies, basic science studies, and other biomechanical simulation studies were excluded. Review papers and studies conducted using the same data set were excluded as well. Two investigators independently reviewed and assessed the quality of the selected articles. Discrepancies between the 2 reviewers were resolved by discussion and consensus.
Quality Assessment
The quality of each study was independently assessed by two investigators using the Downs and Black checklist, which is a reliable and validated 27-item checklist designed to assess the quality of both randomized controlled trials and nonrandomized studies.15 It consists of questions that evaluate 5 quality domains: reporting, external validity, bias, confounding, and power. Each item on the checklist is scored according to the following method: “Yes” is given a score of 1, and “No” or “Unable to determine” is given a score of 0. Exceptions to this rule are item 5 assessing principal confounders (“Yes” = 2, “Partially” = 1, and “No” = 0) and item 27 assessing power (scored from 0 to 5). In this study, we employed a modified version of the Downs and Black checklist in which item 27 was revised to a binary system in which 1 point was awarded if a power or sample size calculation was performed, and 0 points were awarded if the study did not document a power or sample size calculation. The total score correlates with the quality of the study, with a maximum possible score of 28 in our modified version of the checklist. Only a randomized controlled trial can obtain a full score of 28.
We defined an excellent quality study as a total score of 26 to 28, a high-quality study as a score of 20 to 25, a moderate quality study as a score of 15 to 19, and a poor-quality study as a score of 14 and less. Bucketing scores in this manner is a practice routinely used in the spinal orthopedic literature.16,17 The Down and Black checklist has been shown to have high intrarater, interrater, and test-retest reliability.15 The final results were reviewed and confirmed by a senior investigator.
Data Extraction
For each included study, data was extracted to record study characteristics, patient-specific risk factors, radiographic risk factors, surgical risk factors, and outcome measures. Study characteristics included study design, level of evidence, time of data collection, patient demographics, and duration of follow-up. Patient-specific risk factors included age, smoking status, diabetes, and bone mineral density. Radiographic variables included pre- and postoperative sagittal alignment, segmental angle endpoints, preoperative total intervertebral height, preoperative disk height, and pre- and postoperative anterior intervertebral disk height. Surgical risk factors included single- or multi-level fusion, number of levels fused, specific levels fused, operative time, type of cage, and indication for the procedure.
Outcome measures included length of hospital stay, complications (dysphagia, hoarseness, intraoperative blood loss), radiographical outcomes (total intervertebral height, anterior disk height, posterior disk height, pseudarthrosis rates, mean time to fusion, adjacent segment degeneration (ASD), adjacent disc height, change in adjacent disc height, subsidence, change in kyphosis, postoperative fused segment angle, and patient-reported clinical outcomes (visual analog scale [VAS] for arms and neck, Japanese Orthopedic Association [JOA] score, Neck Disability Index [NDI], Short Form Health Survey [SF-36], and Odom’s scale).
Statistical Analysis
Odds ratios (ORs) were reported as a summary statistic. We tested random-effect models to account for interstudy variation in baseline clinical characteristics and methodology. Chi-square (χ2) tests were used to evaluate heterogeneity between trials. The I2 statistic was used to estimate the percentage of total variation across studies owing to heterogeneity rather than chance, with values greater than 50% considered to be indicative of substantial heterogeneity. The I2 statistic was calculated as I2 = 100% × (Q − df)/Q, with Q defined as Cochrane’s heterogeneity statistic and df defined as degrees of freedom. Subgroup analyses evaluating possible confounding factors were not possible because the raw data was not available. Statistical significance was set to a P value of .05. Review Manager Version 5.3.2 (Cochrane Collaboration, Software Update, Oxford, United Kingdom) was used for all statistical analyses.
Results
Literature Search
Our literature search yielded 455 relevant citations. After initial review of titles and abstracts, 397 references were excluded. After full text review of the remaining 58 articles, 39 were excluded. A total of 19 studies remained that met our inclusion and exclusion criteria and were included in our meta-analysis (Figure 1)7–10,12,18–30. Of the 19 studies, 15 were retrospective cohort studies and 4 were prospective cohort studies. There were no statistically significant differences in patient age, gender, body mass index (BMI), smoking status, or diabetes among the studies (Figure 2). There were no significant differences in follow-up duration between the cage-only and cage-plate groups in any of the included studies (Table 1). Graft material differed among the studies, but within each individual study, the same graft material was used in the cage-only and cage-plate groups. Graft material included β-tricalcium phosphate, demineralized bone matrix, autologous cancellous bone, or recombinant human bone morphogenetic protein–2 (rhBMP-2) with osteophytes. The remaining 4 studies either did not include details on the type of graft used or was a meta-analysis.
Figure 1.
Flowsheet illustrating study selection for this systematic review and meta-analysis.
Figure 2.
Baseline patient demographics and comorbidity variables.
Table 1.
Duration of Follow-Up.
| Authors | Year | Duration of Follow-up (Months) | |
|---|---|---|---|
| ACDF Cage Alone | ACDF Cage and Plate | ||
| Han et al | 2016 | 12 | 12 |
| Yun et al | 2016 | 12.77 ± 7.85 | 13.62 ± 9.21 |
| Liu et al | 2016 | 23.3 ± 6.9 | 24.2 ± 6.4 |
| Oh et al | 2013 | 23.4 | 20.6 |
| Wang et al | 2015 | 24.1 ± 7.8 | 23.8 ± 8.2 |
| Ahn et al | 2016 | 25.88 ± 1.95 | 26.14 ± 1.96 |
| Li et al | 2016 | 29.7 ± 6.5 | 30.8 ± 6.6 |
| Song et al | 2009 | 29.9 | 29.9 |
| Shi et al | 2015 | 30.3 | 30.3 |
| Yang et al | 2015 | 30.6 | 33.1 |
| Chen et al | 2016 | 36 | 36 |
| Yan et al | 2014 | 15.32 ± 2.13 | 14.26 ± 2.35 |
| Son et al | 2014 | 6 | 6 |
| Kwon et al | 2016 | 6 | 6 |
| Shao et al | 2015 | Meta-analysis | Meta-analysis |
| Vanek et al | 2013 | 24 | 24 |
| Ji et al | 2015 | 24 | 24 |
| Li et al | 2015 R | 24 | 24 |
| Li et al | 2015 M | 24 | 24 |
Abbreviation: ACDF, anterior cervical discectomy and fusion; R, radiculopathy group; M, myelopathy group.
Quality Assessment
The average modified Downs and Black score of the studies included in this meta-analysis was 18.2 (standard deviation, 2.2; range, 14-22). There were 6 high-quality studies, 12 moderate-quality studies, and 1 poor-quality study.
Perioperative Complications
A summary of all parameters analyzed in this meta-analysis is outlined in Table 2. Seven studies reported rates of dysphagia within 3 months of surgery. Dysphagia was significantly less common in the cage-only group (OR 0.32; P < .01). There was moderate heterogeneity between the studies with an I2 value of 0.45. Eleven studies reported rates of dysphagia after 3 months postoperatively. Dysphagia was significantly less common in the cage-only group as well (OR 0.27; P < .01). There was minimal heterogeneity with an I2 value of 0.08 (Figure 3).
Table 2.
Summary of Clinical and Radiographic Outcomes in the Cage-Only and Cage-Plate Groups.
| Parameter | No. of Patients in Cage Group | No. of Patients in Cage-Plate Group | Mean Difference/Odds Ratioa | Odds Ratio or Mean Difference Used | P | I 2 | Favors | Statistically Significant |
|---|---|---|---|---|---|---|---|---|
| Postoperative Cobb angle | 325 | 339 | −1.44 | Difference | .04 | 0.59 | CP | Yes |
| Postoperative disc height | 96 | 96 | −0.39 | Difference | .003 | 0 | CP | Yes |
| Blood loss | 351 | 362 | −9.90 | Difference | .0001 | 0.82 | Cage | Yes |
| Postoperative dysphagia | 603 | 567 | 0.30 | Odds | .00 001 | 0.22 | Cage | Yes |
| ASD | 263 | 270 | 0.40 | Odds | .003 | 0 | Cage | Yes |
| Subsidence | 443 | 424 | 2.49 | Odds | .0001 | 0.20 | CP | Yes |
| Operation time | 351 | 362 | −1.50 | Difference | .65 | 0.92 | Cage | No |
| Fusion rate | 312 | 310 | 0.56 | Odds | .09 | 0.02 | CP | No |
| Postoperative VAS neck | 240 | 246 | 0.18 | Difference | .28 | 0.81 | CP | No |
| Postoperative VAS arm | 64 | 67 | −0.37 | Difference | .64 | 0.94 | Cage | No |
| Postoperative JOA | 340 | 355 | 0.14 | Difference | .10 | 0 | Cage | No |
| Postoperative NDI | 181 | 187 | 0.11 | Difference | .62 | 0 | CP | No |
| Hospital stay | 98 | 103 | −0.24 | Difference | .52 | 0.47 | Cage | No |
| hoarseness | 86 | 90 | 1.05 | Odds | .96 | 0 | CP | No |
| Kyphotic change | 95 | 103 | 1.34 | Odds | .61 | 0.56 | CP | No |
| Odom E | 214 | 226 | 0.74 | Odds | .26 | 0.38 | Cage | No |
| Odom G | 214 | 226 | 1.15 | Odds | .51 | 0 | CP | No |
| Odom F | 214 | 226 | 1.03 | Odds | .94 | 0.13 | N/A | No |
| Odom P | 214 | 226 | 1.52 | Odds | .52 | 0 | CP | No |
| Postoperative fused segment angle | 87 | 84 | −1.76 | Difference | .09 | 0 | CP | No |
| Postoperative sagittal alignment | 46 | 46 | 5.91 | Difference | .37 | 0.94 | Cage | No |
Abbreviations: CP, cage with anterior plate; ASD, adjacent segment disease; VAS, visual analog scale; JOA, Japanese Orthopedic Association; NDI, neck disability index.
a Compared with CP as baseline
Figure 3.
Forest plot of differences in dysphagia within and beyond 3 months of anterior cervical discectomy and fusion (ACDF) between the cage-only (Cage) and cage-plate (CP) groups. The cage-only group experienced significantly less dysphagia than the cage-plate group both within and beyond 3 months of surgery.
Twelve studies reported intraoperative blood loss. The cage-only group had an average of 9.90 mL lower intraoperative blood loss (P < .01). There was considerable heterogeneity between the studies with an I2 value of 0.82 (Figure 4).
Figure 4.
Forest plot of differences in estimated blood loss between the cage-only (Cage) and cage-plate (CP) groups. The cage-only group had statistically significant lower blood than the cage-plate group.
There were no statistically significant differences between the 2 groups in terms of duration of operation, postoperative hoarseness, and length of hospital stay.
Radiographic Outcomes
Ten studies reported pre- and postoperative C2-C7 Cobb angles. The cage-only group had a significantly smaller postoperative C2-C7 Cobb angle than the cage-plate group (mean difference 1.44°, P = .04). There was substantial heterogeneity among these studies (I2 = 0.59). There was no significant difference in preoperative Cobb angles between the 2 groups with moderate heterogeneity among studies (I2 = 0.40).
Three studies reported preoperative disc height. There was no significant difference in preoperative disc height between the cage-only and the cage-plate group (P = .46). Two studies reported postoperative disc height, which was significantly lower in the cage-only group (mean difference 0.39 mm, P < .01). For both pre- and postoperative disc height, there was perfect homogeneity among studies (I2 = 0) (Table 1).
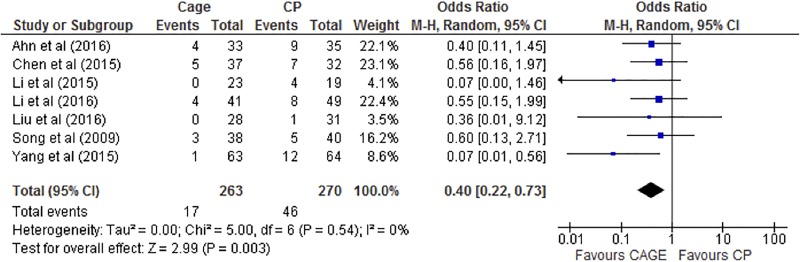
Seven studies reported ASD. The cage-only group had a significantly decreased risk of ASD compared to the cage-plate group (OR 0.40; P < .01). There was perfect homogeneity among studies (I2 = 0) (Table 1, Figure 5).
Figure 5.
Forest plot of differences in adjacent segment disease (ASD) between the cage-only (Cage) and cage-plate (CP) groups. The cage-only group had significantly decreased risk of ASD than the cage-plate group.
Nine studies reported the incidence of subsidence. Most studies measured subsidence within two years of operation, although some did not define a time frame. Furthermore, the parameters used to define “subsidence” differed across studies. Four of the studies defined cage subsidence as either a reduction >3 mm in intervertebral body height or a distance >3 mm between the midpoint of the upper margin of the upper vertebral body and lower margin of the lower vertebral body.8,18,20 Four other studies used a cutoff of 2 mm instead of 3 mm.21,24,31,32 Finally, 1 study defined cage subsidence as a distance >6 mm between the midpoint of the upper margin of the upper vertebral body and lower margin of the lower vertebral body.8,18,20 The cage-only group had a significantly greater risk of cage subsidence than the cage-plate group (OR 2.49; P < .01). There was minimal heterogeneity among these studies (I2 = 0.20) (Table 1).
There was no significant difference between the cage-only and cage-plate groups with regards to absolute fusion rate (Figure 6). Independent verification was used to assess radiographic fusion in 10 studies. In comparison, the operating surgeon assessed fusion status in 8 studies. Studies varied slightly in their criteria for assessing fusion. These criteria are outlined in Table 3.
Figure 6.
Forest plot of differences in fusion rate between the cage-only (Cage) and cage-plate (CP) groups. There was no significant difference in fusion rate between the 2 groups.
Table 3.
Criteria for the Assessment of Fusion on Radiographs or CT.
| Study | Year | Fusion Criteria | Imaging Modality |
|---|---|---|---|
| Wang et al Li et al Liu et al | 2015 2016 2016 | (1) Absence of motion between the spinous processes at dynamic lateral radiographs, (2) absence of a radiolucent gap between the graft and endplates, and (3) presence of continuous bridging bony trabeculae at the graft-endplate interface | X-rays and CT |
| Oh et al Song et al Ji et al Chen et al Shi et al | 2013 2009 2015 2016 2015 | (1) <2° movement on lateral flexion/extension views, (2) the presence of bridging trabecular bone between the endplates on anteroposterior/lateral views, (3) the lack of implant failure signs of the anterior plate system, and (4) <50% radiolucency in the perimeter surrounding the cage | X-rays and CT |
| Li et al Li et al | 2015 R 2015 M | (1) <4° of angular motion on flexion and extension radiographs, (2) the presence of bridging trabecular bone between the fused vertebrae, and (3) the absence of any radiolucent zones spanning <50% of the implant-vertebral interface on CT | X-rays and CT |
| Yun et al | 2016 | (1) <10° movement on lateral flexion/extension views, (2) presence of bridging trabecular bone between the end plates on anteroposterior and lateral views, (3) <50% radiolucency in the perimeter surrounding the cage, and (4) no evidence of pullout of the device | X-rays |
| Ahn et al | 2016 | Bridwell fusion grading system. We defined grades 1-2 and motion <2 mm on flexion/extension lateral radiographs as fusion | X-rays and CT |
| Yan et al | 2014 | Continuity of trabecular pattern on CT | CT |
| Son et al Kwon et al Yang et al Han et al | 2014 2016 2015 2016 | Not mentioned | X-rays, MRI, CT |
| Shao et al | 2015 | Meta-analysis | Meta-analysis |
| Vanek et al | 2013 | Assessed based on radiologic stability | Dynamic X-rays |
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; R, radiculopathy group; M, myelopathy group.
Finally, there was no significant difference in kyphotic change between the cage-only and cage-plate groups. Pre- and postoperative fused segment angles and sagittal alignment were not statistically different between the 2 groups.
Patient-Reported Clinical Outcomes
The results of patient-reported clinical outcomes are outlined in Table 1. There were no significant differences in patient-reported outcomes between the cage-only and cage-plate groups, including Odom’s criteria, VAS neck score, VAS arm score, JOA score, and NDI score.
Discussion
ACDF is a well-recognized treatment for cervical disc degeneration, radiculopathy, and myelopathy. ACDF with an anterior cervical plate has been shown to be an effective method of fusion with low pseudarthrosis rates reported for 1- to 2-level fusions.6 However, given the postoperative complications that have been attributed to the presence of an anterior plate, there has been rising interest in the use of techniques such as stand-alone cages that do not require plate fixation. Our systematic review and meta-analysis demonstrated that ACDF with a cage-only technique was associated with decreased incidence of postoperative dysphagia, intraoperative blood loss, and ASD compared with a conventional cage-plate technique. However, a cage-only technique was found to have increased rates of cage subsidence, decreased postoperative disc height, and less restoration of cervical lordosis.
Postoperative dysphagia is the most common complication of ACDF.33 While the exact mechanism of dysphagia following ACDF is unknown, several hypotheses have been proposed. Fountas et al33 suggested that esophageal injury, soft tissue edema, hematoma, and adhesion formation around the anterior cervical plate may be potential contributors to the development of dysphagia. Lee et al noted a positive correlation between the thickness of the plate and the rate of postoperative dysphagia.34 In addition, Fogel and McDonnell demonstrated in their meta-analysis that removal of an anterior plate and lysis of associated esophageal adhesions significantly reduced rates of both immediate and chronic postoperative dysphagia in patients who had previously undergone ACDF.35
In this meta-analysis, the association between the conventional cage-plate technique and higher rates of dysphagia does not come as a surprise, but it is important to note that almost half of the studies included individually reported no significant difference in dysphagia between cage-only and cage-plate cohorts.8,18,21,24,27 By pooling together the results from these studies, statistical power was increased and we found strong evidence that the stand-alone cage technique is associated with lower rates of dysphagia compared to the conventional cage-plate technique. This suggests that use of a stand-alone cage could potentially reduce rates of postoperative dysphagia by as much as 5-fold, which in turn, could have a significant impact on patient comfort and satisfaction.
The cage-only technique was also associated with a statistically significant lower intraoperative blood loss. However, given that average blood loss during an ACDF is relatively low, this difference is likely not clinically significant.
ACDF with a cage-only technique was found to be superior to the conventional cage-plate technique with regards to the incidence of ASD. Biomechanical studies have demonstrated that ACDF with a conventional cage-plate technique affects the mechanical properties of intervertebral disks at adjacent levels to the fusion. There is increased stress and mobility in adjacent segments after fusion, which potentially contributes to accelerated ASD.19,36 ASD is associated with accelerated disc degeneration as well as sagittal malalignment, which may necessitate additional treatment months to years after the index operation.9,37
The higher rate of ASD seen with the cage-plate technique has been attributed to surgical factors such as proximity of the plate to the adjacent intervertebral disk.5 However, if stand-alone cages have at least equivalent outcomes to the conventional cage-plate technique, then one of the major proposed benefits in favor of the cage-only technique is a theoretical reduction in the rate of ASD due to the absence of an anterior plate. In this meta-analysis, we indeed found a significantly decreased rate of ASD in the cage-only group. Again, it is notable that only 1 of the 6 studies included in the analysis reported a decreased rate of ASD with the cage-only technique. However, with the increased power from pooled data, the cage-only technique was found to be associated with a 2- to 3-fold decrease in the rate of ASD, which may potentially reduce later-onset complications after the index operation.19
One of the major concerns of ACDF with a stand-alone cage is the potential increase in the rate of cage subsidence. Our pooled results did demonstrate a significantly increased rate of subsidence in the cage-only group, but as noted previously, there was variability among studies in terms of the definitions of “subsidence.” Unfortunately, this makes it difficult to truly assess the difference in cage subsidence between the cage-only and cage-plate groups. Studies have reported that cage subsidence may cause local cervical kyphosis and hypermobility in the posterior cervical region.19 However, it is also important to note that a previously published systematic review found that cage subsidence following ACDF does not affect clinical outcomes or fusion rates.37 Therefore, the clinical significance of higher rates of radiographic cage subsidence in the cage-only group in this meta-analysis is unclear and should be further examined in future studies.
This meta-analysis also found that the cage-only technique was associated with less restoration of cervical lordosis compared to the cage-plate technique. Loss of cervical lordosis has been associated with postoperative pain and functional disability.10 In additional, sagittal alignment plays an important role in the distribution of stress across fixation devices.23 Loss of cervical lordosis is a theoretical risk factor for ASD as cervical kyphosis accelerates degenerative changes of the cervical spine by increasing biomechanical stress on the anterior portion of the vertebral bodies of adjacent segments.10 Our pooled results in this meta-analysis demonstrated that the cage-plate technique resulted in significantly greater sagittal Cobb angles (ie, greater cervical lordosis) than the stand-alone cage technique. Of the 9 studies included, only 1 study independently reported a significant difference in postoperative cervical lordosis between the 2 groups.10 While previous studies have shown that loss of cervical lordosis is associated with poorer clinical outcomes, we did not find worse clinical outcomes in the cage-only group.31 This may be due to the fact that the clinical sequelae resulting from loss of cervical lordosis may take years to develop and thus, were not captured in the relatively short-term follow-up time period of the included studies.
There are several limitations to this study. First, there was significant heterogeneity across studies for some of the parameters analyzed in this meta-analysis. Only 5 of the studies included were prospective studies, while most of the remaining 17 studies were observational in nature and therefore, more susceptible to selection bias. Second, the number of studies analyzed for each outcome measure varied widely. The heterogeneous nature of the studies created imbalances in the amount of data available for each outcome variable. Additionally, 9 of the studies reviewed included outcomes from multiple surgeons, which may introduce bias as estimated blood loss; operation time and fusion rates can vary from surgeon to surgeon. Furthermore, the operating surgeon assessed radiographic fusion in 8 studies, which is another potential source of bias. Finally, our literature search only included studies from select databases and excluded studies that were not published in English, which may have potentially overlooked some studies with relevant data.
In conclusion, ACDF with a stand-alone cage technique is associated with a reduced incidence of postoperative dysphagia and decreased risk of ASD. The cage-alone technique was also associated with less restoration of normal cervical lordosis, but this did not seem to have short-term clinical significance. Long-term outcomes remain unclear as the studies included in this meta-analysis had relatively short-term follow-up. In summary, the cage-only technique appears to have better short-term clinical outcomes than the conventional cage-plate technique, despite radiographic findings of greater cage subsidence and less restoration of cervical lordosis. More randomized controlled trials with longer-term follow-up are needed to determine whether the findings of this meta-analysis hold up in the long-term.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 2. Maharaj MM, Mobbs RJ, Hogan J, Zhao DF, Rao PJ, Phan K. Anterior cervical disc arthroplasty (ACDA) versus anterior cervical discectomy and fusion (ACDF): a systematic review and meta-analysis. J Spine Surg. 2015;1:72–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Phan K, Kim JS, Lee NJ, Kothari P, Cho SK. Relationship between ASA scores and 30-day readmissions in patients undergoing anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2017;42:85–91. [DOI] [PubMed] [Google Scholar]
- 4. Di Capua J, Somani S, Kim JS, et al. Predictors for patient discharge destination after elective anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2017;42:1538–1544. [DOI] [PubMed] [Google Scholar]
- 5. Lu VM, Zhang L, Scherman DB, Rao PJ, Mobbs RJ, Phan K. Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J. 2017;26:546–557. [DOI] [PubMed] [Google Scholar]
- 6. Song KJ, Lee KB. A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci. 2006;13:181–187. [DOI] [PubMed] [Google Scholar]
- 7. Wang Z, Jiang W, Li X, et al. The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J. 2015;24:148–154. [DOI] [PubMed] [Google Scholar]
- 8. Chen Y, Chen H, Wu X, Wang X, Lin W, Yuan W. Comparative analysis of clinical outcomes between zero-profile implant and cages with plate fixation in treating multilevel cervical spondylotic myelopathy: a three-year follow-up. Clin Neurol Neurosurg. 2016;144:72–76. [DOI] [PubMed] [Google Scholar]
- 9. Liu Y, Wang H, Li X, et al. Comparison of a zero-profile anchored spacer (ROI-C) and the polyetheretherketone (PEEK) cages with an anterior plate in anterior cervical discectomy and fusion for multilevel cervical spondylotic myelopathy. Eur Spine J. 2016;25:1881–1890. [DOI] [PubMed] [Google Scholar]
- 10. Kwon WK, Kim PS, Ahn SY, et al. Analysis of associating factors with C2-7 sagittal vertical axis after two-level anterior cervical fusion: comparison between plate augmentation and stand-alone cages. Spine (Phila Pa 1976). 2017;42:318–325. [DOI] [PubMed] [Google Scholar]
- 11. Duan Y, Yang Y, Wang Y, et al. Comparison of anterior cervical discectomy and fusion with the zero-profile device versus plate and cage in treating cervical degenerative disc disease: a meta-analysis. J Clin Neurosci. 2016;33:11–18. [DOI] [PubMed] [Google Scholar]
- 12. Shao H, Chen J, Ru B, et al. Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res. 2015;10:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Phan K, Mobbs RJ. Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg. 2015;1:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Theis J, Gerdhem P, Abbott A. Quality of life outcomes in surgically treated adult scoliosis patients: a systematic review. Eur Spine J. 2015;24:1343–1355. [DOI] [PubMed] [Google Scholar]
- 17. Steiger F, Becker HJ, Standaert CJ, et al. Surgery in lumbar degenerative spondylolisthesis: indications, outcomes and complications. A systematic review. Eur Spine J. 2014;23:945–973. [DOI] [PubMed] [Google Scholar]
- 18. Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976). 2009;34:2886–2892. [DOI] [PubMed] [Google Scholar]
- 19. Ahn SS, Paik HK, Chin DK, Kim SH, Kim DW, Ku MG. The fate of adjacent segments after anterior cervical discectomy and fusion: the influence of an anterior plate system. World Neurosurg. 2016;89:42–50. [DOI] [PubMed] [Google Scholar]
- 20. Han SY, Kim HW, Lee CY, Kim HR, Park DH. Stand-alone cages for anterior cervical fusion: are there no problems? Korean J Spine. 2016;13:13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yun DJ, Lee SJ, Park SJ, et al. Use of a zero-profile device for contiguous 2-level anterior cervical discectomy and fusion: comparison with cage with plate construct. World Neurosurg. 2017;97:189–198. [DOI] [PubMed] [Google Scholar]
- 22. Li Y, Hao D, He B, Wang X, Yan L. The efficiency of zero-profile implants in anterior cervical discectomy fusion: a prospective controlled long-term follow-up study. J Spinal Disord Tech. 2015;28(10):398–403. [DOI] [PubMed] [Google Scholar]
- 23. Li Z, Zhao Y, Tang J, et al. A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J. 2017;26(4):1129–1139. [DOI] [PubMed] [Google Scholar]
- 24. Shi S, Liu ZD, Li XF, Qian L, Zhong GB, Chen FJ. Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: a preliminary clinical study. Spine J. 2015;15(9):1973–1980. [DOI] [PubMed] [Google Scholar]
- 25. Oh JK, Kim TY, Lee HS, et al. Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. J Spinal Disord Tech. 2013;26:415–420. [DOI] [PubMed] [Google Scholar]
- 26. Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS. Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative dyphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 2014;56(2):103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vanek P, Bradac O, Delacy P, Lacman J, Benes V. Anterior interbody fusion of the cervical spine with Zero-P spacer: prospective comparative study-clinical and radiological results at a minimum 2 years after surgery. Spine (Phila Pa 1976). 2013;38(13):E792–E797. [DOI] [PubMed] [Google Scholar]
- 28. Ji GY, Oh CH, Shin DA, et al. Stand-alone cervical cages versus anterior cervical plates in 2-level cervical anterior interbody fusion patients: analysis of adjacent segment degeneration. J Spinal Disord Tech. 2015;28(7):E433–E438. [DOI] [PubMed] [Google Scholar]
- 29. Yan D, Li J, Zhang Z, et al. Anterior cervical discectomy and fusion with the zero-profile implant system for cervical spondylotic myelopathy. Techniques in Orthopaedics. 2014;29(1):49–53. [Google Scholar]
- 30. Yang H, Chen D, Wang X, Yang L, He H, Yuan W. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg. 2015;135(8):781–787. [DOI] [PubMed] [Google Scholar]
- 31. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 1999;12(1):50–56. [PubMed] [Google Scholar]
- 32. Pinder EM, Sharp DJ. Cage subsidence after anterior cervical discectomy and fusion using a cage alone or combined with anterior plate fixation. J Orthop Surg (Hong Kong). 2016;24(1):97–100. [DOI] [PubMed] [Google Scholar]
- 33. Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complication. Spine (Phila Pa 1976). 2007;32(21):2310–2317. [DOI] [PubMed] [Google Scholar]
- 34. Lee CH, Hyun SJ, Kim MJ, et al. Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, an cage plus plating. J Spinal Disord Tech. 2013;26(2):112–118. [DOI] [PubMed] [Google Scholar]
- 35. Fogel GR, McDonnell MF. Surgical treatment of dysphagia after anterior cervical interbody fusion. Spine J. 2005;5(2):140–144. [DOI] [PubMed] [Google Scholar]
- 36. Park JB, Cho YS, Riew KD. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005;87(3):558–563. [DOI] [PubMed] [Google Scholar]
- 37. Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech. 2014;27(1):1–10. [DOI] [PubMed] [Google Scholar]