Abstract
The case reported here highlights the importance of examination of functional occlusion along with static occlusion. Any undetected malocclusion during early mixed dentition has potency to alter the growth and function of stomatognathic system. Premature contacts in primary canine region is the most prevalent cause of functional mandibular shift and can lead to TMJ problems for the prevalence of self correction of such malocclusion is very low if not intervened. A case of functional mandibular shift due to faulty canine guidance because of premature contacts is discussed here. Selective grinding of premature contacts and myofunctional exercise resulted in well balanced centric occlusion coinciding with centric relation.
Keywords: Functional occlusion, Functional mandibular shift, Premature contact, Selective grinding
1. Introduction
A posterior cross bite is believed to be transferred from primary to permanent dentition and can have long-term effects on the growth of jaws.1 A unilateral posterior crossbite is usually due to a bilaterally constriction of maxilla or premature contacts during closure.2,3 Innumerable researches and case reports are there in dental literature about the functional shift of mandible due to bilateral constriction of maxilla, giving an illusion of being the only cause. However, premature contacts in primary or in early mixed dentition are probably the most frequent cause of functional crossbites which often goes undetected, for functional occlusion in primary dentition is least commonly discussed topic in publications and text books of pedodontics.
However, irrespective of the cause of posterior crossbite, the prevalence of functional shift of mandible at the primary dentition stage is 8.4% and drops to 7.2% at the mixed dentition stage.3 The frequency of spontaneous self correction ranges from 0% to 9%.3,4 This is very low to justify non intervention. If left untreated, functional crossbite may cause several changes in hard and soft tissues including development of skeletal asymmetries, alteration of soft tissue growth, adaptive changes in the temporomandibular joints (TMJ) and attrition of primary and permanent teeth. Depending upon etiological factors treatment should be done as soon as it is detected to normalize the occlusion and create conditions for normal oro-facial development.2,5,6
The present case report, therefore may prove helpful in recognizing the importance of early detection and treatment of functional crossbite due to premature contacts in developing dentition.
2. Case report
A 6 year old male patient reported to the Department of Pedodontics and Preventive Dentistry, Modern Dental College and Research Centre, Indore, for the routine dental checkup. On extra oral examination a slight facial asymmetry, with chin deviated towards right side, was observed (Fig. 1).The intraoral examination revealed an early mixed dentition with erupting 36 and 46, fused 81 and 82 in mandibular arch and eruption bulge of 16 & 26 in maxilla. Static examination of occlusion showed extended mesial step on left and flush terminal on right side. As 81& 82 were fused having mesio-distal dimension lesser than combined mesio-distal width of 71 & 72, resulting midline shift towards right in relation to maxilla together with mesial shift of 73 & 74 (Fig. 2).
Fig. 1.

Extraoral photograph showing facial asymmetry- chin deviated towards right.
Fig. 2.
Intraoral photograph of static occlusion shows mandibular midline towards right side and anomalous (fused) 81 & 82.
For dynamic stomatognathic system, functional analysis was performed which included examination of TMJ, mandibular positions and movement.5 TMJ showed no clicking sound or tenderness while closing and opening of mouth. Mandibular shift was evaluated by asking patient to close his mouth from maximum opening to maximum intercuspation.7,8 When mouth was wide open, chin- nose midpoints were found coinciding (Fig. 3A) together with mandibular midline got shifted slightly to the left. Nonetheless as patient closed his mouth to habitual occlusion, chin and mandibular midline got shifted to right side, without any premature contact midway of closure of mouth. This was probably because of persistent neuro-muscular feedback that patient got habitual to close his mouth directly into comfortable i.e. habitual occlusion.1,5 This gave us the suspicion of functional occlusion.
Fig. 3.
Functional examination. (A) No mandibular deviation when mouth is wide open. (B) Patient could not stabilize occlusion in first contact, the picture is therefore midway from first contact to full occlusion. Premature contact in 63 and 73 shifted mandible towards right and posterior. Red arrow shows 83 sliding posteriorly on distal facet of 52. (C) Wax bite in habitual occlusion shows perforation (red arrow) in 63 region. Broken red arrow shows erupting bulge of 16 and 26.
To deprogram the mandibular muscles, in order to obtain mandibular rest position, three exercises were performed without occlusal contact, each 5 times. Patient was asked to open his mouth wide and to close, while keeping palm of right hand on right side of mandible in order to guard the mandible to close in centric occlusion. This was followed by phonetic and swallowing exercises. The patient was asked to moisten his/her lips, swallow saliva, breathe deeply, and relax his/her jaw with eyes closed.7 Then patient was asked to speak the word ‘Ram’ with lips only slightly meeting at the end of pronunciation.
Following these exercises of 4–5 minutes, patient could produce mandibular rest position without chin and midline deviation. Now again patient was asked to close his mouth slowly from wide open mouth upto occlusal contact. It was revealed that there was premature contact on left canine and, creating a faulty guiding path to mandible to deflect it towards right side, leading to mandibular shift towards right (Fig. 3B). A wax bite was taken in full habitual occlusion, the site of premature contact in that bite was found perforated (Fig. 3C).
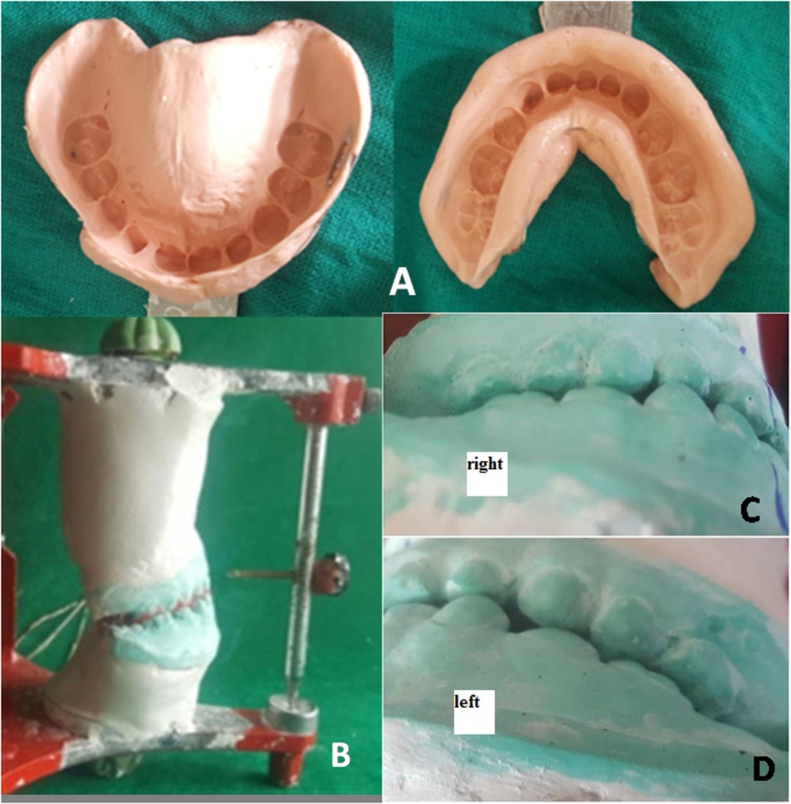
The premature contacts were further confirmed by articulating paper and video, which clearly showed left canine as culprit for mandibular shift. The final diagnosis, ‘functional mandibular shift to right side due to faulty canine guidance on left side’ was established. Same day diagnostic impressions were made (Fig. 4A) and study casts were obtained. Bite was then transferred on the casts and casts mounted on the articulator (Fig. 4B). Casts were evaluated for facets on teeth, maxilla-mandibular vertical, sagittal and transverse relations; Sagittal- a/- posteriorly there was extended mesial step on left compared to right side; b/- anteriorly there was no overjet; Transverse- there was more posterior overjet on left (Fig. 4D) [exposing whole of the maxillary buccal cusps] compared to right side (Fig. 4C, D); Vertical- there was edge to edge bite; Facets- There were light facets on 51, 52 while deeper on 61,62 and 63, where mesial slope of 73 and 74 were occluding respectively.
Fig. 4.
Evaluation of premature contacts. (A & B) Impressions made and casts, with wax bite were articulated. (C & D) More posterior overjet on left compared to right side. Also notice extended mesial step on left side.
Evaluation was done on articulator first, to get familiar with pattern of premature contacts in order to minimize the injudicious grinding of teeth in mouth. Since primary dentition was fully developed and patient was in early mixed dentition state, treatment was considered.
2.1. Treatment
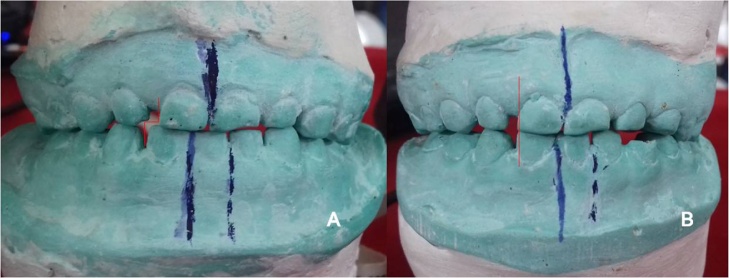
Premature contacts were marked with the help of articulating paper (Fig. 5A). Intraoral premature contact was observed carefully (Fig. 5B) and selective grinding was done slowly (Fig. 5C). Premature contacts were re-evaluated between each grinding.
Fig. 5.
Preventive treatment (selective grinding) (A). Marking premature contacts with the help of articulating paper. (B) Premature contact is shown as dark mark on 63. (C) Selective grinding of dark mark with airotor.
Since functional shift became a learned pattern, patient was closing his mouth in habitual occlusion even after removal of prematurities. Therefore myofunctional exercise was planned. Patient was trained for swallowing and closing his mouth in the right direction. Muscle exercises were explained to patient and to his father as well. Patient was asked to close his mouth while keeping his right hand on right side of mandible to avoid learned deviation of mandible. Patient was recalled after 14 days and examined. Casts and wax bite in habitual occlusion was taken and mounted on the articulator. Mounted casts as compared with the previous one revealed- the mandibular midline got moved towards maxillary midline (Fig. 6A & B) and posterior overjet was corrected. Extra-orally there was improved facial symmetry (Fig. 7A & B series). Functionally, habitual and centric occlusions were coinciding with evenly distributed multipoint contact in the centric occlusion (Fig. 7A, B series).
Fig. 6.
Corrected occlusion- Articulated casts. (A) before selective grinding midline shift towards right. (B) after selective grinding corrected functional shift; step (red arrow) in A turned to straight line in B.
Fig. 7.
Extra and intraoral views- (A) preoperative, (B) after 14 days, (C) after 14 months, raised bite with eruption of first permanent molars.
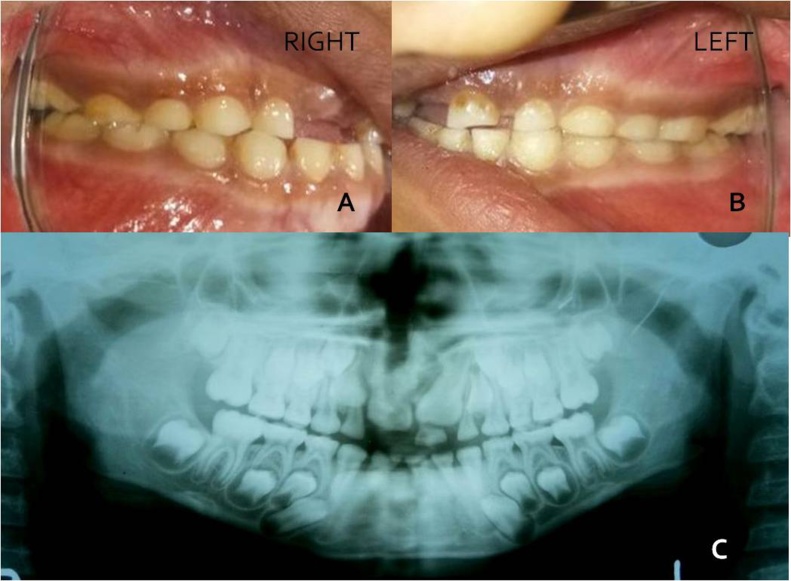
Patient was re-evaluated for stability in developing occlusion after 14 months. There was stable occlusion without functional shift [Figures- 7(A, B, C series) & 8].
3. Discussion
In a line with organization of orthodontic service into three basic categories (preventive, interceptive, and corrective), occlusal adjustment through selective grinding done in this case is a preventive orthodontic procedure. Discovering occlusal disharmonies before they have had a chance to create malocclusion is entirely within realm of day to day practice for the discerning, able pedodontist. Routine diagnostic records like, plaster casts, dental radiograph and recording of clinical signs as the patient closed to full occlusion provided many clues of functional shift of mandible which was further augmented with thin articulating paper and soft base plate wax as described by Graber.5
Patients with unilateral posterior crossbite should be observed and diagnosed carefully. Three prevalent reasons are there for unilateral crossbite- presence of premature contact while closing; bilateral maxillary constriction; or true basal skeletal discrepancy between maxilla and mandible. The latter two are often associated with oral habits (thumb sucking and/or tongue thrusting) and atypical soft tissue functional problems (mouth breathing because of severe airway problem).8,9 Presented case was not associated with any oral habits but was a case of absolute premature contact at canine region in fully developed primary dentition. Treatment of functional shifts during eruption of primary teeth is not indicated as premature contacts are transitory and therefore the treatment of these prematurities is considered only when primary teeth have achieved full occlusion.5,6 On careful examination of mounted study casts several findings were revealed. Differences in three dimensional relations between right and left side along with noticeable facets on left side only were suggestive of mandibular shift from left to right side. Anomalous 81 and 82 altered the arch width of mandible and probably created the premature contacts leading to mandibular shift. Little overjet, presence of facets and extended mesial step on left side together with reduced posterior overjet on right compared to left side altogether suggested posterior rotation and translation of right condyle while anterior translation of left condyle of mandible.
Linder and Mooder10 found 97% occurance of lateral forced bites with mandible shift among 76 cases of posterior crossbite, which were also associated with facial asymmetry along with chin deviation towards crossbite side. Seldom only any parent visit dentist for complaint of crossbite. As these functional shifts remain there for long time, there develop delay in periodontal messetric reflex (PMR), an important reflex controlling the jaw movement.11 Asano T et al.11 found that under occlusal hypofunction after electrical stimulation to PDL, the threshold of messetric motor unit responses significantly increased compared to control group.The results indicated that occlusal hypofunction changes in the threshold and latency of the PMR might greatly affect the coordination of mandibular function viz. mastication along with decreased activity of the elevator muscles, especially the masseter. Along with PMR, Bakke 12supposed mechanoreceptor feedback from periosteum of alveolar bone as well.
Troelstrup and Moller13 and Martin et al.7 found functional mandibular lateral shift associated with unilateral posterior cross-bite may persist at rest position i.e. learned pattern of muscular shift to avoid premature contact and to directly occlude in habitual bite. Our patient also showed learned pattern of muscular shift and therefore was occluding his teeth in deviated mandible position only. To evaluate premature contacts, it was necessary to re-train the elevator muscles of mandible. The mandibular muscles were trained by asking patient to open his mouth wide repeatedly, by swallowing and phonetic exercises. The un-deviated rest position of mandible was achieved after 5 min of all these exercises and we could evaluate premature contacts at canine region. Once cuspal interference was removed by selective grinding, habitual occlusion started coinciding with centric occlusion, even rest position of mandible coincided with centric relation. Little muscular exercise of two weeks could correct the lateral functional shift effectively which remain stabilized even after 14 months follow up (Figs. 7 & 8).
Removal of functional interferences has been shown to be useful only in patients under the age of 5, with success rates ranging from 27% to 64%.4,14,15 Lateral forced bites in primary dentition, is very easy to treat as less time in re-training of elevator muscles of mandible is required and further harm to permanent dentition is prevented by eliminating possibility of any grinding on permanent teeth. In a study of 76, 4-year-old children with posterior crossbite, Linder et al.15 reported 50% correction after functional grinding. The greatest chance of correction after selective grinding occurred when the maxillary intercanine width was at least 3.3 mm greater than the corresponding mandibular intercanine width.15,16Myers et al.17 determined whether functional posterior crossbites in children of 5-9 years of age influenced the position of the mandibular condyle and also assessed the affect of crossbite correction on condylar position. They found significant differences in vertical and horizontal joint space measurement between crossbite and noncrossbite side prior to treatment, which was found nonsignificant after crossbite correction. Fourteen months follow up of patient showed extra and intraoral mid line correction, normal articulation of TMJ on both side and balanced growth of jaws (Fig. 8A–C).
Fig. 8.
(A & B) stabilizing corrected shift with proper intercuspation of erupting first permanent molars. (C) orthopentogram shows properly articulated right and left condyles.
Delay in correction of functional shifts in primary dentition, may guide the erupting permanent dentition to intercuspate in functionally shifted mandibular position, which in turn may establish facial asymmetry and TMJ pathosis.18 Wattanachai et al.19 tested the effect of mechanical stress from a functional lateral shift of mandible on expression of two main condylar cartilage extracellular matrix components by evaluation of immunoreactivity through expression of type II collagen and aggrecan and found that compared to control group the contralateral condyles (opposite side of lateral shift) showed significantly increased immunoreactivity
of the experimental groups from 7 to 14 days. While on the ipsilateral condyles (same side of lateral shift), the immunoreactive areas were significantly decreased. They concluded that a functional lateral shift of the mandible modulated the condylar cartilage extracellular matrix differently on each side of the condyle, which affected condylar morphology, growth, biomechanical properties, and even the susceptibility of the condylar cartilage to pathogenesis.
In primary dentition the tooth guidance usually requires less spot grinding as compared to permanent dentition with established occlusal relationship. In primary dentition inclined planes are not as deep and in conjunction with growth and development, the adjustment of mandible and TMJ to a new position is comparatively easy. In the mixed dentition, greater care must be exercised to avoid removing too much tooth material from permanent teeth. In the permanent dentition even greater dependence must be placed on articulated study models, and careful plan must be exercised before instituting the actual grinding procedure.5
Since a “high” or premature contacts can cause a deflection of the mandible during closure, calling for certain proprioceptive responses and a learned pattern of activity, the elimination of such learned pattern permits the re-direction of the forces toward normal path of closure and centric relationship.5,6 The commonly missed evaluation i.e. the functional evaluation during orthodontic examination should be practiced in routine examination for complete preventive therapy. A dentist should not only concentrate on problems related to chief complaint but also to overall growing structures in orofacial region to maintain the normal growth and development of stomatognathic system.
4. Conclusion
This paper emphasized the importance of early detection, correction and possible complications of functional mandibular shift. Among many reasons of functional mandibular shift, occlusal prematurities are the one quite frequent in primary dentition which should be carefully evaluated. One should not wait until a frank malocclusion developes. The occlusal dynamics should be a part of routine examination along with the static one in young child patients. A few moments of selective grinding may prevent countless not only hours of orthodontic mechanotherapy but also the myofunctional problems later on.
Conflict of interest
None
References
- 1.Nerder P.H., Bakke M., Solow B. The functional shift of mandible in unilateral posterior cross bite and adaptation of temperomandibular joints:a pilot study. Eur J Orthod. 1999;21:155–166. doi: 10.1093/ejo/21.2.155. [DOI] [PubMed] [Google Scholar]
- 2.Sudhakar N., Dinesh S. Unilateral posterior crossbite - shoot it at sight. A review. J Dent Med Sci. 2013;12(4):47–50. [Google Scholar]
- 3.Kutin G., Hawes R.R. Posterior cross-bites in the deciduous and mixed dentitions. Am J Orthod. 1969;56(5):491–504. doi: 10.1016/0002-9416(69)90210-3. [DOI] [PubMed] [Google Scholar]
- 4.Thilander B., Wahlund S., Lennartsson B. The effect of early interceptive treatment in children with posterior crossbite. Eur J Orthod. 1984;6(1):25–33. doi: 10.1093/ejo/6.1.25. [DOI] [PubMed] [Google Scholar]
- 5.Premkumar S. 4th ed. Elsevier; 2009. Graber’s textbook of orthodontics: basic principles and practice. [Google Scholar]
- 6.Profit W.R., Fields H.W. 3rd ed. Harcourt Private limited; New Delhi: 2000. Contemporary orthodontics. [Google Scholar]
- 7.Martin C., Palma J.C., Alaman J.M., Lopez- Quinones J.M., Alarcon J.A. Longitudinal evaluation of sEMG of masticatory muscles and kinematics of mandible changes in children treated for unilateral cross-bite. J Electromyogr Kinesiol. 2012;22(4):1–8. doi: 10.1016/j.jelekin.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Binder R. Correction of posterior crossbites: diagnosis and treatment. Pediatr Dentr. 2004;26(3):266–272. [PubMed] [Google Scholar]
- 9.Bell R.A. A review of maxillary expansion in relation to rate of expansion and patient’s age. Am J Orthod. 1982;81(1):32–37. doi: 10.1016/0002-9416(82)90285-8. [DOI] [PubMed] [Google Scholar]
- 10.Lindner A., Modeer T. Relation between sucking habit and dental characteristics in preschool children with unilateral crossbite. Scand J Dent Res. 1989;97(3):278–283. doi: 10.1111/j.1600-0722.1989.tb01613.x. [DOI] [PubMed] [Google Scholar]
- 11.Asano T., Zeredo J.L., Tada K., Soma K. Periodontal massetric reflex is changed by periodontal sensory modification during occlusal hypofunction in rats. J Med Dent Sci. 2007 [PubMed] [Google Scholar]
- 12.Bakke M. Mandible elevator muscles: physiology action, and effect of dental occlusion. Scand J Dent Res. 1993;101:314–331. doi: 10.1111/j.1600-0722.1993.tb01127.x. [DOI] [PubMed] [Google Scholar]
- 13.Troelstrup B., Moller E. Electromyography of the temporalis and messetormuscles in children with unilateral crossbie. Scand J Dent Res. 1970;78:425–430. doi: 10.1111/j.1600-0722.1970.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 14.Kurol J., Bergland L. Longitudinal study and cost–benefit analysis of the effect of early treatment of posterior crossbites in the primary dentition. Eur J Orthod. 1992;14(3):173–179. doi: 10.1093/ejo/14.3.173. [DOI] [PubMed] [Google Scholar]
- 15.Lindner A. Longitudinal study of the effect of early interceptive treatment in 4-year old children with unilateral cross-bite. Scand J Dent Res. 1989;97(5):432–438. doi: 10.1111/j.1600-0722.1989.tb01457.x. [DOI] [PubMed] [Google Scholar]
- 16.Keneddy D., Matthew O. Unilateral posterior crossbite with mandibular shift: a review. J Can Dent Assoc. 2005;71(8):569–573. [PubMed] [Google Scholar]
- 17.Myers D.R., Barenie J.T., Bell R.A., Williamson E.H. Condylar position in children with functional posterior crossbite: before and after crossbite correction. Pediatr Dent. 1980;2(3):190–194. [PubMed] [Google Scholar]
- 18.Sharma D.S., Saadia M. Evaluation of functional occlusion. In Textbook of Pedodontics. 3rd ed. Tandon S editor. Paras publication. Hyderabad, India 2017-18, section 9, chapter 56, pp-884. (in press).
- 19.Wattannachai T., Yonemista Y., Kenoko S., Soma K. Functional lateral shift of the mandible: effects on the expression of ECM in rat tempoeromandibular cartilage. Angle Orthod. 2009;7:652–659. doi: 10.2319/080808-417.1. [DOI] [PubMed] [Google Scholar]