Abstract
Ureteritis cystica is a rare benign condition. In this report, we have presented the case of a patient with a left upper back pain. The CT scan showed multiple irregular filling defects in the upper left ureter and the left renal pelvis. During the ureteroscopy, multiple yellow cystic lesions were seen in the proximal part of the left ureter and in the renal pelvis.
The pathology report described cystic structures coated with single line cubic metaplastic epithelium. Ureteritis cystica should be considered in a differential diagnosis, in case of atypical radiological findings. No active treatment is required when confirmed.
Keywords: Ureteritis cystica, Cystitis cystica, Ureter
Introduction
Ureteritis cystica is a rare benign condition that affects the ureter and the renal pelvis. The condition was first reported by Morgagni1 in the 18th century. The first to describe it were Richmond and Robb,2 as a proliferation characterized by multiple cyst and filing defects in the urothelium.
The etiology of the disease is not known, but it is associated with chronic urothelial irritation that can be caused by nephrolithiasis and urinary tract infections.3
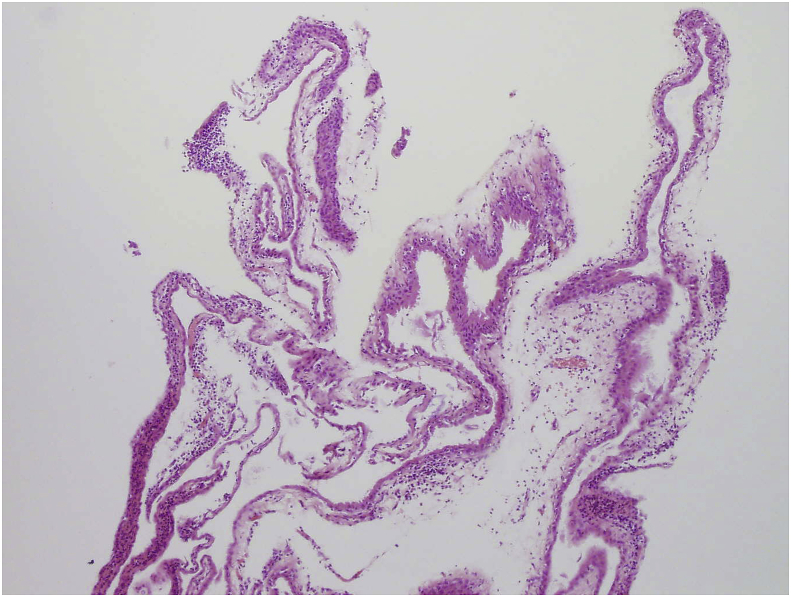
Histologically, there are numerous small submucosal epithelial-lined cysts representing cystic degeneration of the metaplastic epithelium or the submucosal Brunn cell nests. Their walls are transparent macroscopically and the fluid contained within is mucoproteinacous. There is often a surrounding infiltrate of lymphocytes.
Radiographically, the appearance is that of multiple small 2–5 mm smooth, walled, rounded, lucent filling defects projecting into the lumen, usually of the ureter.4 They are most common in the proximal ureter, but can be seen anywhere along the urinary tract: bladder (cystitis cystica) or renal pelvis (pyelitis cystica).
A differential diagnosis of multiple transitional cell tumors, ureteral pseudodiverticula, nonopaque calculi, polyps, papillary tumors, vascular impressions, tuberculosis, iatrogenic gas bubbles, gas-forming microorganisms, and submucosal hemorrhage can be considered with an appropriate clinical correlation.
Case report
A 70-year-old female patient was admitted in office due to left upper back pain which was not severe. The patient had a history of kidney stones. Four and two years ago she passed 4mm and 5mm stone after having severe left flank pain.
A urinalysis was within normal limits. The blood count and serum creatinine were within normal limits. An abdominal roentgenogram showed no abnormal calcifications. Voided urinary cytology was negative for malignant cells.
The ultrasound showed no kidney stones and no dilatation of the renal pelvis. There were multiple renal parapelvic cysts on both kidneys. A CT scan was performed. It confirmed multiple renal parapelvic cysts, up to 2.7 cm in diameter. It also showed multiple irregular filling defects, up to 2mm, in the upper left ureter and the left renal pelvis (Fig. 1). The ureters were not dilated. Many differential diagnosis were considered (multiple transitional cell tumors, papillary tumors, tuberculosis). Our main concern was to rule out malignant lesions so we performed explorative cystoscopy and ureteroscopy. Explorative cystoscopy showed a normal bladder neck. Ureteral orifices were of normal size, shape and position, effluxing clear bilaterally. The bladder mucosa was normal. The left ureteral orifice was easily identified and a ureteroscope was introduced into the ureter.
Fig. 1.
Multiple irregular filling defects in the upper left ureter and the left renal pelvis.
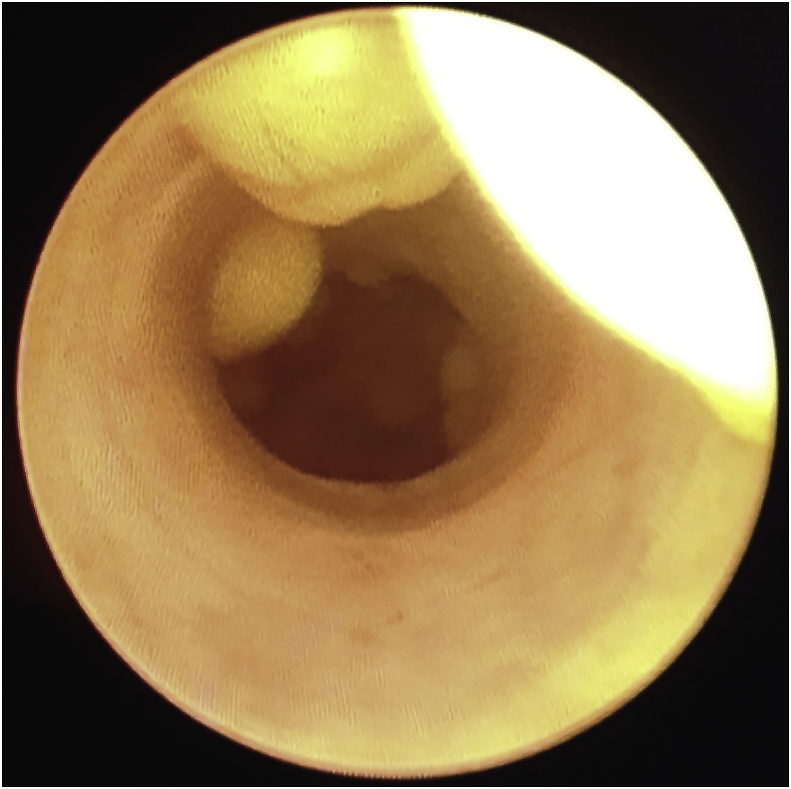
During the ureteroscopy, multiple yellow cystic lesions were seen in the proximal part of the left ureter and in the left renal pelvis (Fig. 2). One of the cysts was punctured. Milky and cloudy fluid drained from the cyst. The material was collected for cytological evaluation. The second cyst was punctured and its wall was collected for pathological evaluation.
Fig. 2.
Yellow cystic lesions in the proximal part of the left ureter. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The pathology report described cystic structures coated with single line cubic metaplastic epithelium most consistent with cystitis cystica (Fig. 3).
Fig. 3.
Cystic structures coated with single line cubic metaplastic epithelium.
Discussion
Ureteritis cystica is a rare benign condition that affects the ureter and the renal pelvis. It is usually detected incidentally on a CT or an MR scan during imaging for other reasons, like an unexplained finding of filling defects in the ureters.5 The most common location of cystic lesions is the proximal ureter but they can be found at any level of the urothelium.
In this case, the renal pelvis was also affected with the proximal ureter. The patient had a history of kidney stones. The CT scan was performed because of the upper back pain. It is possible that the cause of the flank pain might have been an undiagnosed ureteral stone which had been spontaneously expelled prior to radiographic workup rather than the cystic leasons themselves and the diagnosis of urethritis cystica was an incidental finding. The diagnosis was confirmed by ureteroscopy and the pathological report.
In case of recurrent flank pain in this patient that is not severe and with no ultrasound dilatation of renal calycs we would treat her with non-steroidal anti-inflammatory drugs.
Since the patient has kidney stone history in case of recurrent flank pain that is severe and non-responsive to analgesic therapy we would perform non-contrast low dose CT scan to rule out ureteral/renal stone.
Urethritis cystica is associated with chronic urothelial irritation that can be caused by nephrolithiasis (as was in our case) and urinary tract infections. There are no guidelines for the management of ureteritis cystica apart from the treatment of the underlying cause.
Conclusion
Ureteritis cystica should be considered as a differential diagnosis in case of atypical radiological findings. No active treatment is required when confirmed.
Declarations
Consent for publication: Written informed consent for publication of clinical details and images was obtained from the patient.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1.Morgagni J.B. William Cooke Translation; 1822. De sedibus et causis morborum per anatomen indagatis libri quinque; pp. 316–411. [Google Scholar]
- 2.Richmond H.G., Robb W.A. Adenocarcinoma of the ureter secondary to ureteritis cystica. Br J Urol. 1967;39:359–363. doi: 10.1111/j.1464-410x.1967.tb09816.x. [DOI] [PubMed] [Google Scholar]
- 3.Kilic S., Sargin S.Y., Gunes A. A rare condition: the ureteritis cystica. A report of two cases and review of literature. M.T. Altinok İnönü Üniversitesi Tıp Fakültesi Dergisi. 2003:87–89. [Google Scholar]
- 4.Rothschild J.G., Wu G. Ureteritis cystica: a radiologic pathologic correlation. Journal of Clinical Imaging Science. 2011;23 doi: 10.4103/2156-7514.80375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menendez V., Sala X., Alvarez-Vijande R. Cystic pyeloureteritis: review of 34 cases. Radiologic aspects and differential diagnosis. Urology. 1997;50:31. doi: 10.1016/S0090-4295(97)00205-7. [DOI] [PubMed] [Google Scholar]