Abstract
Adolescents who initiate electronic cigarette (EC) use without having ever used tobacco are more likely than those that have not initiated EC use to try cigarette smoking over time. However, whether rates of EC use coincide with cigarette smoking rates at the population level remains unknown. This study aimed to compare trends in ever, current, and daily use of EC and cigarette smoking among adolescents in Iceland from 2015 to 2018. We analyzed four waves of pooled cross-sectional population-based school survey data with students enrolled in the 8th, 9th and 10th grades in the national Icelandic school system (n = 42,440, boys = 50.1%). Response rates ranged between 83.3% and 86.0%. Findings for 8th, 9th, and 10th grade students, and the combined sample, revealed a consistent pattern: prevalence of cigarette smoking either remained unchanged or decreased minimally over the study period. In the combined sample rates of ever smoking remained between 9 and 10% during the entire study period, whereas the prevalence of daily cigarette smoking was around 1%. The use of EC increased 2- to 3-fold in all age groups. Ever use increased from 12% to roughly 30% in the combined group and daily use increased from about 2% to 6% during the same period. We conclude that the prevalence of adolescent cigarette smoking in Iceland remained mostly unchanged between the years 2015 and 2018, whereas EC use increased exponentially during the same period. The prevalence of EC use now far outweighs cigarette smoking in 8th–10th grade youth in Iceland.
Keywords: Adolescents, Electronic cigarettes, Iceland, Population trends, Primary prevention
Highlights
-
•
Trends in adolescent e-cigarette use and cigarette smoking, 2015–2018, is reported.
-
•
Cigarette smoking remained mostly unchanged during the study period.
-
•
E-cigarette use increased exponentially in all age groups during the study period.
-
•
E-cigarette use now far outweighs cigarette smoking among youth in Iceland.
-
•
Over 40% of 10th grade students have tried e-cigarettes and 10% are daily users.
1. Introduction
On September 12, 2018, the U.S. Food & Drug Administration (FDA) announced a series of actions concerning the marketing and sales of electronic cigarettes (EC) to children and youth, whose use of EC and related products the agency stated had reached “epidemic proportions” (U.S. Food and Drug Administration, 2018). The action represents the largest coordinated enforcement effort in the history of the agency. The principal issues cited by the FDA have been highlighted by many and concern the challenges involving the marketing and selling of EC as a potential harm-reduction mechanism for current tobacco smokers (secondary prevention), while at the same time avoiding an appeal to underaged never-smokers and thus operating as a recruitment tool to a new generation of potential nicotine users (primary prevention) (Farsalinos, 2018; Newton et al., 2018).
From a toxicological perspective, EC are considered a much safer alternative to nicotine delivery compared to tobacco smoking (Alzahrani et al., 2018; Badea et al., 2018; Levy et al., 2018) with significant prospects for improved public health. This is especially important if heavy smokers and chronic relapsers, or both, can be persuaded to switch from tobacco use to EC, although to date most intervention trials and cohort studies have demonstrated minimal efficacy to that end (Farsalinos, 2018; Weaver et al., 2018). A noteworthy exception is a new randomized trial by Hajek and colleagues conducted among British National Health Service users, which is the first to show EC to potentially be more effective for smoking cessation in adults than nicotine-replacement therapy with behavioral support (Hajek et al., 2019). At the same time, reports from several countries have shown a consistent increase in the prevalence of EC use by never-smoking youth with increased prospects for young non-cigarette smoking vapers becoming dependent on nicotine-bearing EC and then developing into regular long-term users with ensuing potential risks of respiratory and cardiac disease (Kristjansson et al., 2017; Goniewicz et al., 2016). In addition, numerous recent longitudinal studies from both the US and the UK have shown that minors who initiate EC use without having ever smoked cigarettes, are significantly more likely than non-users (that neither have used EC nor smoked cigarettes) to initiate tobacco smoking over time (Barrington-Trimis et al., 2016; Best et al., 2018; Conner et al., 2018; Leventhal et al., 2015; Soneji et al., 2017). However, scholars have challenged these findings and largely base their skepticism in the non-validation of the premises of the gateway theory and the lack of measurement into established user patterns by either EC or combustible cigarettes (Etter, 2018; Mayet and Lavagna, 2018). Taken together, reviews (Farsalinos, 2018; Levy et al., 2018) have highlighted the potential promise of EC as a harm-reduction tool for current tobacco smokers, while others (Best et al., 2018; Conner et al., 2018; Soneji et al., 2017) have found EC to be a potential risk factor for tobacco use initiation in minors. Underlining this notion is a new meta-analysis that showed that around 70% of adults that ever try cigarette smoking will develop into daily smokers. Birge et al. (2018) The FDA's response is solely directed at the latter issue, citing concerns over marketing strategies designed to appeal to young people and lack of corporate efforts to curb the sales of EC to never-smoking minors, especially through online mediums (U.S. Food and Drug Administration, 2018).
Although available data on the prevalence of the use of EC is now routinely included in population surveillance studies among youth (ESPAD group E. Report, 2015; Johnston et al., 2017), some scholars have criticized the definition and reporting use of EC by stating the commonly cited “ever use” to be insufficient to assess potential harm, especially at the population level (Farsalinos, 2018). Several trend analyses of EC use in minors have been published recently but there is a scarcity of high-quality, population-based reports which simultaneously assess trends in ever-, current-, and daily use, in both tobacco smoking and use of EC among specific age groups of adolescents within the same population. For example, Chaffee and colleagues assessed trends in EC use and cigarette smoking from 2011 to 2015 among 6-12th grade youth in the US using 5 waves of the National Youth Tobacco Survey (NYTS) and found a large increase in EC use and around ~4% point decrease in smoking (Chaffee et al., 2017). Another study by Dutra and Glantz (Dutra and Glantz, 2017) also analyzed trend data in ever use and 30-day use of EC and cigarettes from the NYTS from 2004 to 2014 and found a large increase in EC use and either a plateaued trend or minimal decrease in cigarette smoking during the study period. Both NYTS studies are limited to assessing 30 day use and analyse trends in EC and tobacco use by averaging the use by all participants in grades 6 through 12. However, the NYTS 2018 data showed that while e-cigarette use increases in youth, the prevalence of cigarette smoking has slightly increased (see, https://www.cdc.gov/tobacco/data_statistics/surveys/nyts/index.htm).
Analyses that include stratification into subgroups by age and level of use could more accurately reveal how population trends in the use of EC compare to trends in cigarette smoking and vice versa, and thus shedding additional light on the premises of the primary and secondary prevention concerns stated above. By reviewing the current primary prevention literature on the use of EC and its relations to cigarette smoking over time, the question is whether growing population trends in the use of EC should be accompanied by higher rates of tobacco smoking (Barrington-Trimis et al., 2016; Best et al., 2018; Conner et al., 2018; Leventhal et al., 2015; Soneji et al., 2017; Wills et al., 2016). At the same time, by assessing the secondary prevention or harm reduction literature into the use of EC, the assumption can be drawn that increase in prevalence of their use among minors should result in lower population-based rates of cigarette smoking (Newton et al., 2018; Bauld et al., 2017).
To assess these questions we look to Iceland, a small Nordic country renowned for its strong primary substance use prevention efforts among minors (Kristjansson et al., 2016; Sigfusdottir et al., 2009). Iceland represents a compelling case study in these matters for at least two reasons: First, Iceland has seen some of the most dramatic decrease in pan-European adolescent alcohol, tobacco and other drug use over a 20-year period, as evidenced by results from both the European School Project on Alcohol and other Drugs (ESPAD) study and regular local surveillance studies (ESPAD group E. Report, 2015; Kristjansson et al., 2016). Second, despite its primary prevention efforts, the sale and marketing of EC were completely unregulated in Iceland before March 1, 2019, based on laws enacted by the national Parliament in June 2018, which prohibit the sale and marketing of EC to minors under the age of 18. The fact that Iceland has witnessed such a large reduction in rates of tobacco smoking among youth over time, while at the same time operating in a non-regulated environment with regards to sales and marketing of EC, offers an unprecedented opportunity to assess the relationship between the prevalence of cigarette smoking and the use of EC among minors at the population level.
2. Methods
2.1. Sample and procedures
The data for this study come from the series of annual population-based Youth in Iceland surveys conducted from 2015 to 2018. These surveys are administered to all accessible 8–10 grade students (ages 13–16 years) in Iceland by the Icelandic Centre for Social Research and Analysis (ICSRA) at Reykjavik University. ICSRA's data collection procedures and the survey's theoretical background and history have been described elsewhere (Sigfusdottir et al., 2009; Kristjansson et al., 2013). Data were collected in all or almost all of the country's 144 high schools during February of each year. Consistent with published protocols (Kristjansson et al., 2013), data collection was conducted using anonymous questionnaires and supervised by an individual contact agent in each school using procedures approved by the Icelandic authority overseeing the protection of human research subjects. Students were instructed not to write their names or any other identifying information on the questionnaires. When finished, students were asked to seal their completed questionnaire in an envelope provided and to return the envelope to the supervising agent. Table 1 illustrates the total number of participants and response rates for each year of survey administration.
Table 1.
Annual number of participants and responses rates in the Youth in Iceland surveys, 2015–2018.
| Year | N | Response rate (%) |
|---|---|---|
| 2015 | 10,695 | 84.4 |
| 2016 | 10,738 | 86.0 |
| 2017 | 10,356 | 83.3 |
| 2018 | 10,651 | 84.1 |
| Total | 42,440 | 84.5 |
2.2. Measures
Measures in the Youth in Iceland study have been largely adopted from other international studies, specifically the Monitoring the Future survey in the United States (Johnston et al., 2017) and ESPAD (ESPAD group E. Report, 2015). Two separate questions were used to assess cigarette smoking and use of EC:
-
1)
How often, if ever, in your lifetime have you smoked cigarettes/used electronic cigarettes? Response categories ranged from 1 = “Never” to 7 = “40 times or more”. For the purpose of these analyses this variable was collapsed and recoded into a dichotomized variable with 0 = “Never”, and 1 = “Ever use”.
-
2)
How often have you smoked cigarettes/used electronic cigarettes during the last 30 days? Response categories included; 1 = “Never”, 2 = “Less than once per week”, 3 = “Less than once per day”, 4 = “1-5 times per day”, 5 = “6-10 times per day”, 6 = 11-2-times per day”, and 7 = “More than 20 times per day”. For “current use” this variable was first collapsed into a dichotomized variable and designated with 0 = “Never” and 1 = “Yes, once or more often”. For “daily use” this variable was recoded by merging the first three response categories and code with 0 = “never or less than daily” and the four remaining categories into 1 = “once or more often per day”.
2.3. Analyses
Analyses where stratified by grade, separating 8th, 9th, and 10th grade respondents. First, we ran cross-tabulations for frequency of cigarette smoking and use of EC within cohorts across study years. Then we conducted trend analyses in Mplus using binary logistic regression with maximum likelihood and robust standard errors, adjusting for potential school clustering. The total number of clusters was 153 and average cluster size ranged from 69.6 to 93.5 between the study cohorts. Intraclass correlation coefficient for the outcome variables ranged from non-identified to 3.3% suggesting a minimal school-based variation. Gender was used as a control variable in multivariate analyses (boys = 50.1%).
3. Results
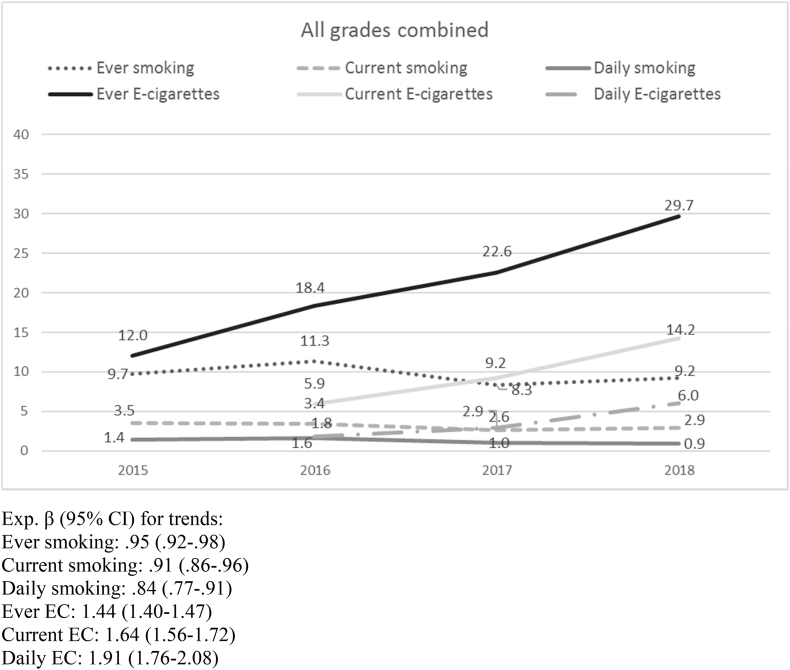
Over 42,000 individual responses encompass the study data base for this analysis. The number of respondents ranged from 10,356 to 10,738 between years of study, or 83.3% to 86.0% of the population in the participating cohorts. Table 2 includes the findings to the trend analyses within and across study cohorts. Among 8th grade students (13–14-year old) no change was observed in ever, current or daily cigarette smoking during the study period. On the other hand, the use of EC increased substantially. For example, ever use rose from almost 7% in 2015 to 18.6% in 2018 and daily use increased from 0.7% to 2.5% over the same period. In 9th grade (14–15-year old) students, the rates of cigarette smoking decreased to a small extent. Correspondingly, ever smoking decreased from 9.5% in 2015 to 8.8% in 2018, and daily smoking went from 1.5% to 0.8% during the same period. On the other hand, the use of EC increased substantially during this time. For example, ever use rose from 12.0% to 30.5% and daily use from 1.7% to 5.6% over the same time period. In 10th grade (15–16-year old) students, rates of cigarette smoking remained unchanged during the study period. Correspondingly, ever smoking was 14.9% in 2015 and 14.4% in 2018 and daily smoking was 2.5% in 2015 and 2.2% in 2018. Similar to 8th and 9th graders, however, the rate of EC use among 10th grade students increased considerably during the study period: ever use went from 17.0% in 2015 to 40.7% in 2018, and daily use increased from 3.0% to 10.2% over the study period. The combined findings for all students (Fig. 1) mirror the overall trend between the study cohorts, i.e., a minimal decrease in cigarette smoking over time versus a large increase in the use of electronic cigarettes.
Table 2.
Population trends in cigarette smoking and use of electronic cigarettes among 8th–10th grade youth in Iceland, 2015–2018.
| 2015% | 2016% | 2017% | 2018% | Exp. β for trend (95% CI) | |
|---|---|---|---|---|---|
| 8th grade students | |||||
| Ever smoking | 4.7 | 6.4 | 3.6 | 4.8 | 0.95 (0.88–1.02) |
| Current smoking | 1.2 | 1.6 | 0.8 | 1.2 | 0.95 (0.82–1.10) |
| Daily smoking | 0.3 | 0.7 | 0.3 | 0.4 | 0.92 (0.73–1.15) |
| Ever E-cigarettes | 6.9 | 9.3 | 12.9 | 18.6 | 1.46 (1.35–1.58) |
| Current E-cigarettes | n/a | 2.9 | 3.9 | 6.9 | 1.62 (1.37–1.91) |
| Daily E-cigarettes | n/a | 0.7 | 1.0 | 2.5 | 2.02 (1.53–2.89) |
| 9th grade students | |||||
| Ever smoking | 9.5 | 10.8 | 8.5 | 8.8 | 0.95 (0.89–0.1.02) |
| Current smoking | 3.7 | 2.7 | 2.8 | 2.2 | 0.84 (0.75–0.95) |
| Daily smoking | 1.5 | 1.2 | 1.2 | 0.8 | 0.81 (0.70–0.95) |
| Ever E-cigarettes | 12.0 | 19.2 | 21.8 | 30.5 | 1.44 (1.37–1.53) |
| Current E-cigarettes | n/a | 5.8 | 9.3 | 13.7 | 1.59 (1.45–1.75) |
| Daily E-cigarettes | n/a | 1.7 | 2.8 | 5.6 | 1.91 (1.65–2.22) |
| 10th grade students | |||||
| Ever smoking | 14.9 | 16.3 | 13.3 | 14.4 | 0.96 (0.91–1.02) |
| Current smoking | 5.7 | 5.8 | 4.2 | 5.4 | 0.95 (0.87–1.03) |
| Daily smoking | 2.5 | 2.7 | 1.7 | 2.2 | 0.85 (0.76–0.94) |
| Ever E-cigarettes | 17.0 | 26.1 | 33.7 | 40.7 | 1.48 (1.41–1.56) |
| Current E-cigarettes | n/a | 8.7 | 14.8 | 22.5 | 1.74 (1.57–1.94) |
| Daily E-cigarettes | n/a | 3.0 | 5.2 | 10.2 | 1.94 (1.73–2.17) |
Fig. 1.
Population trends in cigarette smoking and use of electronic cigarettes, combined for 8th–10th grade youth in Iceland, 2015–2018.
4. Discussion
Findings from this population-level comparative study of trends over time in cigarette smoking and the use of EC by 13–16-year-old adolescents in Iceland can be summarized as follows: the rates of cigarette smoking in all categories among 8th grade students remained unchanged over the study period, whereas a large increase was observed in use of EC across all categories. In 9th grade students, ever use of cigarettes remained unchanged over time but current (i.e., 30-day) use and daily use decreased minimally. In 10th grade students, rates of cigarettes smoking did not change for ever- and current use, but minimal change was observed in daily smoking. At the same time, the use of EC increased two- to three-fold across all categories. When all groups of respondents are combined, a minimal decrease in cigarette smoking over time was observed while use of EC either doubled or tripled over the study period. Across all cohorts the prevalence of use of EC now far exceeds cigarette smoking.
It is well established that both tobacco smoking and other forms of tobacco use are harmful to health. However, the results of this study call attention to the use of EC and the primary and secondary prevention functions that their use may play in contemporary society's efforts to mitigate the use of tobacco. Similar to our findings, use of EC among youth has been reported to have increased considerably in many countries and now far exceeds the number of youth who smoke cigarettes or use other forms of tobacco in many of them (ESPAD group E. Report, 2015; Kristjansson et al., 2017; Yoong et al., 2018). This, according to many primary prevention advocates, is disconcerting because although use of EC is less physically harmful than tobacco smoking (Pokhrel et al., 2015; Green et al., 2018), the primary function of EC is to a) socially and behaviorally mimic the experience of cigarette smoking, and b) physically deliver nicotine to the user (although non-nicotine EC are available) (Ayers et al., 2017; Tindle and Freiberg, 2016). With this in mind, it should be noted that EC were originally invented and marketed as a harm-reduction tool for tobacco smokers (Berridge, 2014). On the other hand, although several longitudinal studies have shown that youth who initiate EC use without having ever smoked cigarettes are significantly more likely than youth who have never used EC nor other forms of tobacco to begin using tobacco over time (Best et al., 2018; Conner et al., 2018; Leventhal et al., 2015; Goldenson et al., 2017; Barnett et al., 2015), the results from this trend analysis do not support the conclusion that greater population levels of EC use lead to rising levels of cigarette smoking among youth. The exponential increase in population trends in the use of EC among youth in Iceland appears largely to be separate from, or in addition to, tobacco use, at least when cigarette smoking is taken into consideration, although a minimal decrease was observed in cigarettes smoking in the combined group. It is of course possible that the change in cigarette smoking is due to the availability of ECs; however, the decrease is very minimal compared to the large increase in EC use. Concerns over a looming increase in cigarette smoking use among youth as a result of increased use of EC therefore appear without foundation. On the other hand, given that the sale and marketing of EC in Iceland was completely unregulated during the entire study period and that EC have been readily available for youth, as well as the fact that research results have shown that EC are commonly marketed directly at them (Kornfield et al., 2015; Pokhrel et al., 2015), a separate but related concern is the potential increase in nicotine addicted youth and young people in Iceland, as a result of the large increase in the prevalence of use of EC in the country. This increase in prevalence of current and daily EC use among never smoking youth is disconcerting because as EC users grow older they may be likely to initiate cigarette smoking or other tobacco use because of nicotine dependence stemming from their EC use.
The question of why the population-level increase in the use of EC among youth has not led to greater rates of cigarette smoking in Iceland, however, warrants distinct attention. This is especially relevant because, as stated earlier, many studies have found that the use of EC is longitudinally linked to greater odds of cigarettes smoking use over time among youth that never had smoked prior to EC use initiation. The most sensible explanation for this discrepancy is the strong primary prevention efforts that have been implemented both nationally and by municipalities and in school communities of Iceland (the latter commonly labelled The Icelandic Model of Primary Substance Use Prevention) over the last 20 years, which has seen the prevalence of use of tobacco, alcohol and other drugs decrease dramatically in the country (Kristjansson et al., 2016; Sigfusdottir et al., 2009; Kristjansson et al., 2010), Presumably this emphasis has led to a consistent norm among youth that cigarette smoking and other tobacco use is harmful and should be avoided at all costs, whereas norms surrounding the potential harm of EC are less developed in the society. Although norms around ECs and cigarette smoking were not observed in this study, several investigations have shown that adolescents commonly perceive EC to be less harmful than smoked tobacco (Pokhrel et al., 2015; Thrasher et al., 2016). To this end, our findings support the notion that youth in Iceland appear to approve of the less harmful EC without feeling the need to initiate smoking as a result. At least presently, strong negative norms around youth cigarette smoking appear unchanged despite the rising use of EC. Despite the fact that EC are not harmless, an important future question for Iceland is whether the dramatic increase in EC use among its youth will lead to a change in norms around smoking and/or other tobacco use, as has been suggested by several scholars (Choi et al., 2017; Fairchild et al., 2014).
This study has three notable limitations as well as two major strengths. First, our data collection procedures do not separate nicotine-containing from non-nicotine-containing EC. Thus, we are unable to know if youth refer their responses to nicotine-bearing EC or not when answering questions about their use of EC. Second, we did not measure or include other forms of tobacco use, such as hookah, snuff or chewing tobacco, in the analyses. Future studies should incorporate measures that include poly-tobacco use as well as use of EC. Third, because of the lack of available measures, our analyses were limited to solely modeling gender as a demographic control variable; a preferred approach would have included factors such as SES-variables and family structure. Considering the strengths, first, our study utilized a large, population-based sample and we achieved high response rates. Second, given the large sample, we were able to collapse the analyses into subgroups based on ever, current (i.e. 30-day), and daily cigarette smoking and use of EC.
In conclusion, population rates of adolescent cigarette smoking in Iceland remained largely unchanged between the years 2015 and 2018, whereas the use of EC increased exponentially over the same period. Unlike the assumptions to be drawn from the results of many international longitudinal studies, the increased prevalence of use of EC among youth in Iceland has not coincided with a corresponding increase in rates of cigarette smoking. The large population-level increase in rates of youth use of EC in Iceland now far exceeds subsequent rates of cigarette smoking in the population, with the primary mode of nicotine delivery among youth being EC.
References
- Alzahrani T., Pena I., Temesgen N., Glantz S.A. Association between electronic cigarette use and myocardial infarction. Am. J. Prev. Med. 2018;55(4):455–461. doi: 10.1016/j.amepre.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers J.W., Leas E.C., Allem J.P. Why do people use electronic nicotine delivery systems (electronic cigarettes)? A content analysis of Twitter, 2012-2015. PLoS One. 2017;12(3):8. doi: 10.1371/journal.pone.0170702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badea M., Luzardo O.P., Gonzalez-Antuna A. Body burden of toxic metals and rare earth elements in non-smokers, cigarette smokers and electronic cigarette users. Environ. Res. 2018;166:269–275. doi: 10.1016/j.envres.2018.06.007. [DOI] [PubMed] [Google Scholar]
- Barnett T.E., Soule E.K., Forrest J.R., Porter L., Tomar S.L. Adolescent electronic cigarette use associations with conventional cigarette and hookah smoking. Am. J. Prev. Med. 2015;49(2):199–206. doi: 10.1016/j.amepre.2015.02.013. [DOI] [PubMed] [Google Scholar]
- Barrington-Trimis J.L., Urman R., Leventhal A.M. E-cigarettes, cigarettes, and the prevalence of adolescent tobacco use. Pediatrics. 2016;138(2) doi: 10.1542/peds.2015-3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauld L., MacKintosh A.M., Eastwood B. Young people's use of E-cigarettes across the United Kingdom: findings from five surveys 2015-2017. Int. J. Environ. Res. Public Health. 2017;14(9):12. doi: 10.3390/ijerph14090973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge V. Electronic cigarettes and history. Lancet. 2014;383(9936):2204–2205. doi: 10.1016/s0140-6736(14)61074-6. [DOI] [PubMed] [Google Scholar]
- Best C., Haseen F., Currie D. Relationship between trying an electronic cigarette and subsequent cigarette experimentation in Scottish adolescents: a cohort study. Tob. Control. 2018;27(4):373–378. doi: 10.1136/tobaccocontrol-2017-053691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birge M.D.S., Miler J.A., Hajek P. What proportion of people who try one cigarette become daily smokers? A meta-analysis of representative surveys. Nicotine Tob. Res. 2018;20(12):1427–1433. doi: 10.1093/ntr/ntx243. [DOI] [PubMed] [Google Scholar]
- Chaffee B.W., Couch E.T., Gansky S.A. Trends in characteristics and multi-product use among adolescents who use electronic cigarettes, United States 2011-2015. PLoS One. 2017;12(5):19. doi: 10.1371/journal.pone.0177073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K., Grana R., Bernat D. Electronic nicotine delivery systems and acceptability of adult cigarette smoking among Florida youth: renormalization of smoking? J. Adolesc. Health. 2017;60(5):592–598. doi: 10.1016/j.jadohealth.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner M., Grogan S., Simms-Ellis R. Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study. Tob. Control. 2018;27(4):365–372. doi: 10.1136/tobaccocontrol-2016-053539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra L.M., Glantz S.A. E-cigarettes and national adolescent cigarette use: 2004–2014. Pediatrics. 2017;139(2) doi: 10.1542/peds.2016-2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter J.F. Gateway effects and electronic cigarettes. Addiction. 2018;113(10):1776–1783. doi: 10.1111/add.13924. [DOI] [PubMed] [Google Scholar]
- Fairchild A.L., Bayer R., Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco "endgame". N. Engl. J. Med. 2014;370(4):293–295. doi: 10.1056/NEJMp1313940. [DOI] [PubMed] [Google Scholar]
- Farsalinos K. E-cigarettes: an aid in smoking cessation, or a new health hazard? Ther. Adv. Respir. Dis. 2018;12:20. doi: 10.1177/1753465817744960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenson N.I., Leventhal A.M., Stone M.D., McConnell R.S., Barrington-Trimis J.L. Associations of electronic cigarette nicotine concentration with subsequent cigarette smoking and vaping levels in adolescents. JAMA Pediatr. 2017;171(12):1192–1199. doi: 10.1001/jamapediatrics.2017.3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz M.L., Leigh N.J., Gawron M. Dual use of electronic and tobacco cigarettes among adolescents: a cross-sectional study in Poland. Int. J. Public Health. 2016;61(2):189–197. doi: 10.1007/s00038-015-0756-x. [DOI] [PubMed] [Google Scholar]
- Green L.W., Fielding J.E., Brownson R.C. The debate about electronic cigarettes: Harm minimization or the precautionary principle. In: Fielding J.E., Brownson R.C., Green L.W., editors. Annual Review of Public Health, Vol 39. vol 39. Annual Reviews; Palo Alto: 2018. pp. 189–191. [DOI] [PubMed] [Google Scholar]
- ESPAD group E. Report . 2015. Results from the European School Survey Project on Alcohol and Other Drugs. Luxembourg: European Monitoring Centre for Drugs and Drug Addiction. 2016. [Google Scholar]
- Hajek P., Phillips-Waller A., Przulj D. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N. Engl. J. Med. 2019;380(7):629–637. doi: 10.1056/NEJMoa1808779. [DOI] [PubMed] [Google Scholar]
- Johnston L.D., O'Malley P.M., Miech R.A., Bachman J.G., Schulenberg J.E. Institute for Social Research, University of Michigan; Ann Arbor: 2017. Monitoring the Future National Survey Results on Drug Use, 1975–2016: Overview, Key Findings on Adolescent Drug Use. [Google Scholar]
- Kornfield R., Huang J., Vera L., Emery S.L. Rapidly increasing promotional expenditures for e-cigarettes. Tob. Control. 2015;24(2):110–111. doi: 10.1136/tobaccocontrol-2014-051580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjansson A.L., James J.E., Allegrante J.P., Sigfusdottir I.D., Helgason A.R. Adolescent substance use, parental monitoring, and leisure-time activities: 12-year outcomes of primary prevention in Iceland. Prev. Med. 2010;51(2):168–171. doi: 10.1016/j.ypmed.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Kristjansson A.L., Sigfusson J., Sigfusdottir I.D., Allegrante J.P. Data collection procedures for school-based surveys among adolescents: the youth in Europe study. J. Sch. Health. 2013;83(9):662–667. doi: 10.1111/josh.12079. [DOI] [PubMed] [Google Scholar]
- Kristjansson A.L., Sigfusdottir I.D., Thorlindsson T., Mann M.J., Sigfusson J., Allegrante J.P. Population trends in smoking, alcohol use and primary prevention variables among adolescents in Iceland, 1997-2014. Addiction. 2016;111(4):645–652. doi: 10.1111/add.13248. [DOI] [PubMed] [Google Scholar]
- Kristjansson A.L., Mann M.J., Sigfusson J. Prevalence of e-cigarette use among adolescents in 13 eastern European towns and cities. Public Health. 2017;147:66–68. doi: 10.1016/j.puhe.2017.02.005. [DOI] [PubMed] [Google Scholar]
- Leventhal A.M., Strong D.R., Kirkpatrick M.G., Unger J.B., Sussman S., Riggs N.R., Stone M.D., Khoddam R., Samet J.M., Audrian-McGovern J. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy D.T.B.R., Lindblom E.N., Goniewicz M.L., Meza R., Holford T.R., Yuan Z., Luo Y., O'Connor R.J., Niaura R., Abrams D.B. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob. Control. 2018;27(1):18–25. doi: 10.1136/tobaccocontrol-2017-053759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayet A., Lavagna C. Electronic cigarettes: harm reduction tool or new substance use behavior? Addiction. 2018;113(10):1786–1788. doi: 10.1111/add.14220. [DOI] [PubMed] [Google Scholar]
- Newton J.N., Dockrell M., Marczylo T. Making sense of the latest evidence on electronic cigarettes. Lancet. 2018;391(10121):639–642. doi: 10.1016/S0140-6736(18)30202-2. [DOI] [PubMed] [Google Scholar]
- Pokhrel P., Fagan P., Kehl L., Herzog T.A. Receptivity to ecigarette marketing, harm perceptions, and e-cigarette use. Am. J. Health Behav. 2015;39:121–131. doi: 10.5993/AJHB.39.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigfusdottir I.D., Thorlindsson T., Kristjansson A.L., Roe K.M., Allegrante J.P. Substance use prevention for adolescents: the Icelandic model. Health Promot. Int. 2009;24(1):16–25. doi: 10.1093/heapro/dan038. [DOI] [PubMed] [Google Scholar]
- Soneji S.B.-T.J., Wills T.A., Leventhal A.M., Unger J.B., Gibson L.A., Yang J., Primack B.A., Andrews J.A., Miech R.A., Spindle T.R., Dick D.M., Eissenberg T., Hornik R.C., Dang R., Sargent J.D. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J.F., Abad-Vivero E.N., Barrientos-Gutierrez I. Prevalence and correlates of E-cigarette perceptions and trial among early adolescents in Mexico. J. Adolesc. Health. 2016;58(3):358–365. doi: 10.1016/j.jadohealth.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle H.A., Freiberg M.S. Editorial commentary: nicotine in electronic cigarettes: cardiovascular harm reduction, not elimination. Trends Cardiovasc. Med. 2016;26(6):524–525. doi: 10.1016/j.tcm.2016.03.013. [DOI] [PubMed] [Google Scholar]
- U.S. Food & Drug Administration; 2018. FDA takes new steps to address epidemic of youth e-cigarette use, including a historic action against more than 1,300 retailers and 5 major manufacturers for their roles perpetuating youth access. [press release]
- Weaver S.R., Huang J.D., Pechacek T.F., Heath J.W., Ashley D.L., Eriksen M.P. Are electronic nicotine delivery systems helping cigarette smokers quit? Evidence from a prospective cohort study of US adult smokers, 2015-2016. PLoS One. 2018;13(7):25. doi: 10.1371/journal.pone.0198047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills T.A., Sargent J.D., Knight R., Pagano I., Gibbons F.X. E-cigarette use and willingness to smoke: a sample of adolescent non-smokers. Tob. Control. 2016;25(E1):E52–E59. doi: 10.1136/tobaccocontrol-2015-052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoong S.L., Stockings E., Chai L.K. Prevalence of electronic nicotine delivery systems (ENDS) use among youth globally: a systematic review and meta-analysis of country level data. Aust. N. Z. J. Public Health. 2018;42(3):303–308. doi: 10.1111/1753-6405.12777. [DOI] [PubMed] [Google Scholar]