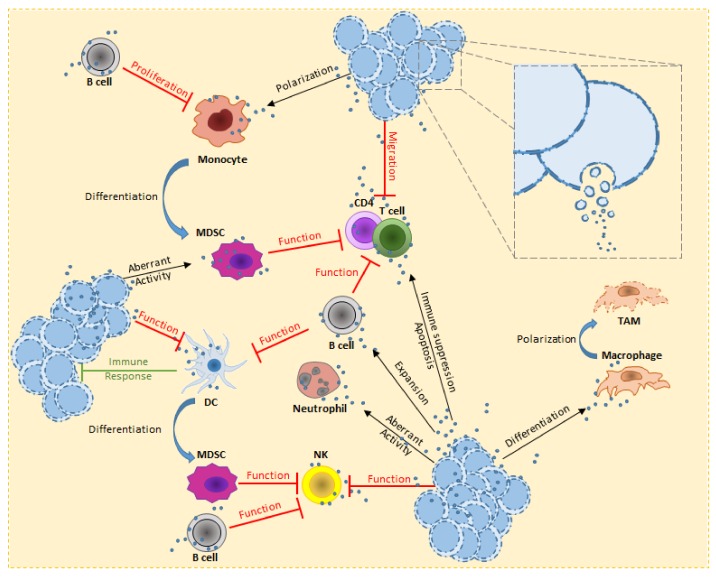
Figure 1.
Overview of hematological malignancy-derived small EV effects on immune cells. In order to escape from the immune system, tumor cells deploy several strategies. TEVs are used to stimulate B cell expansion and activity against several immune cells (e.g., T cells and NK). T cells are known to be affected on the proliferative potential and cytokine production. TEVs directly reduce the T cells migration, leading to up-regulation of receptors involved in immune suppression and or activate pro-apoptotic signals. Alternatively, MDSCs acquire strong immune suppression activity, either from interaction of TEVs or aberrant differentiation from myeloid cells (e.g., monocytes) or immature DCs. Under the effect of TEVs, monocytes polarize towards a pro-tumorigenic form. This leads to pro-inflammatory cytokines release and expression of receptors involved in immune suppression. NK cells have high cytotoxic activity, the tumor uses TEVs to heavily decrease this threat. Furthermore, accumulation of pro-tumorigenic MDSCs also increases this inhibitory effect. TEVs have been reported to stimulate macrophage polarization towards M2 form, this ensure the TME with an increasing pool of TAM which release pro-tumorigenic growth factors, chemokines and cytokines. The consequences of TEV uptake by neutrophils is still under investigation, nevertheless their aberrant activity has been reported to be the cause of CML-like symptoms in vivo experiments. Concerning DCs, it is important to highlight the capacity of TEVs to boost the tumor immune response, transforming the communication through small EVs to a double-edge weapon against the disease.