Abstract
Background—
Pulmonary insufficiency is the nexus of late morbidity and mortality after transannular patch repair of tetralogy of Fallot. This study aimed to establish the feasibility of implantation of the novel Medtronic Harmony transcatheter pulmonary valve (hTPV) and to assess its effect on pulmonary insufficiency and ventricular function in an ovine model of chronic postoperative pulmonary insufficiency.
Methods and Results—
Thirteen sheep underwent baseline cardiac magnetic resonance imaging, surgical pulmonary valvectomy, and transannular patch repair. One month after transannular patch repair, the hTPV was implanted, followed by serial magnetic resonance imaging and computed tomography imaging at 1, 5, and 8 month(s). hTPV implantation was successful in 11 animals (85%). There were 2 procedural deaths related to ventricular fibrillation. Seven animals survived the entire follow-up protocol, 5 with functioning hTPV devices. Two animals had occlusion of hTPV with aneurysm of main pulmonary artery. A strong decline in pulmonary regurgitant fraction was observed after hTPV implantation (40.5% versus 8.3%; P=0.011). Right ventricular end diastolic volume increased by 49.4% after transannular patch repair (62.3–93.1 mL/m2; P=0.028) but was reversed to baseline values after hTPV implantation (to 65.1 mL/m2 at 8 months, P=0.045). Both right ventricular ejection fraction and left ventricular ejection fraction were preserved after hTPV implantation.
Conclusions—
hTPV implantation is feasible, significantly reduces pulmonary regurgitant fraction, facilitates right ventricular volume improvements, and preserves biventricular function in an ovine model of chronic pulmonary insufficiency. This percutaneous strategy could potentially offer an alternative for standard surgical pulmonary valve replacement in dilated right ventricular outflow tracts, permitting lower risk, nonsurgical pulmonary valve replacement in previously prohibitive anatomies.
Keywords: cardiac catheterization, computed tomography, heart valve prosthesis implantation, magnetic resonance imaging, pulmonary valve regurgitation, tetralogy of Fallot
Tetralogy of Fallot (ToF) is the most common form of cyanotic congenital heart disease, accounting for 10% of all congenital heart disease patients. In the United States, the prevalence of ToF is ≈4 to 5 per 10 000 living births.1,2 Surgical repair to reconstruct the right ventricular outflow tract (RVOT) using a transannular patch (TAP) is often required. However, TAP repair always results in pulmonary insufficiency (PI).3,4 Treatment of PI is an important clinical challenge: longstanding PI typically leads to right ventricular (RV) dilatation, ventricular arrhythmias, and heart failure. This adverse remodeling of the RV is a common indication for reintervention, including pulmonary valve replacement (PVR).5,6 Although the need for PVR is well established, no consensus on the optimal timing for PVR exists.7
For the majority of repaired ToF patients, PVR involves open-heart surgery with extensive resection of the dilated RVOT, combined with homograft conduit or bioprosthetic PVR.8,9 However, this standard procedure has recently been challenged following a prospective study that showed no measurable benefit in surgical remodeling of the RVOT when compared with surgical PVR alone.8 If in fact surgical remodeling of the RVOT is not of benefit, a minimally invasive percutaneous approach to PVR could be an equal or superior alternative to surgical PVR. Transcatheter PVR (TCPVR) using the Melody (Medtronic) and Sapien (Edwards) valves has shown promising results, avoiding the risks and complications of open-heart surgery. Although off-label use of these devices in the so-called native outflow tracts has been reported,10–12 for the most part, they are almost exclusively available to patients with preexisting right ventricle-to-pulmonary artery conduits.11,13–16 Patients with distorted, oversized RVOT after TAP repair of ToF (≥ 85% of all ToF patients) are untreatable with most current balloon-expandable devices deployed in the usual pulmonary position, because these valves are too small for secure anchoring in that location.8,17 Self-expanding technology may address this unmet need, as detailed in several recent reports.18–20
This study is the first extensive preclinical evaluation of the Medtronic Harmony transcatheter pulmonary valve (hTPV) in an ovine model of TAP repair that mimics the dilated and distorted RVOT commonly found in patients after TAP repair of ToF.21 The hTPV has evolved from the experimental work of Boudjemline et al22 on the so-called infundibular reducer concept. To date, the hTPV has only been reported in a single human case.18 In this study, we sought to determine whether implantation of the hTPV is feasible, whether it will reduce pulmonary regurgitant fraction (PRF), and whether it will lead to improvements in ventricular volumes in an ovine model of chronic postoperative PI after TAP. The ultimate clinical goal is to provide a novel approach to percutaneous PVR for ToF patients with an oversized RVOT, thereby expanding the indications for percutaneous PVR to include these excluded ToF patients.
Methods
The study protocol was in compliance with the Guide for the Care and Use of Laboratory Animals (US National Institutes of Health publication No. 85–23, revised 1996) and approved by The University of Pennsylvania School of Medicine Institute of Animal Care and Use Committee. Thirteen female Dorsett hybrid sheep were enrolled in the study and underwent baseline cardiac magnetic resonance imaging (MRI), followed by surgical pulmonary valvectomy and TAP repair 4 to 6 weeks after baseline assessment. One month after TAP repair, the hTPV was implanted (n=13) followed by serial MRI and computed tomography (CT) imaging at 1 (n=10), 3 to 5 (n=8), and 6 to 8 month(s) (n=7).
Pulmonary Valvectomy and TAP
After the animals were anesthetized as described previously,21 a left-sided thoracotomy was performed, followed by incision of the pericardium to expose the RVOT and pulmonary artery (PA; Figure 1A). A partially occluding Satinsky clamp, placed across the RVOT and pulmonary annulus, was used to subtotally obstruct the RVOT. Hereafter, one complete pulmonary valve leaflet was excised by incising the RVOT along its length with the pulmonary annulus at the midpoint of this incision (Figure 1B). An oval Gore-Tex Patch (Gore-Tex Acuseal Cardiovascular Patch; W.L. Gore and Associates, Inc, Flagstaff, AZ), measuring 45 by 25 mm in length and width, respectively, and 0.6 mm thick, was then sutured to the edges of the incised RVOT (Figure 1C). Before the clamp was removed, it was partially released to place additional hemo-static stitches, when necessary, using 6–0 running prolene sutures. Epicardial echocardiography using 2-dimensional color Doppler was performed to confirm PI.
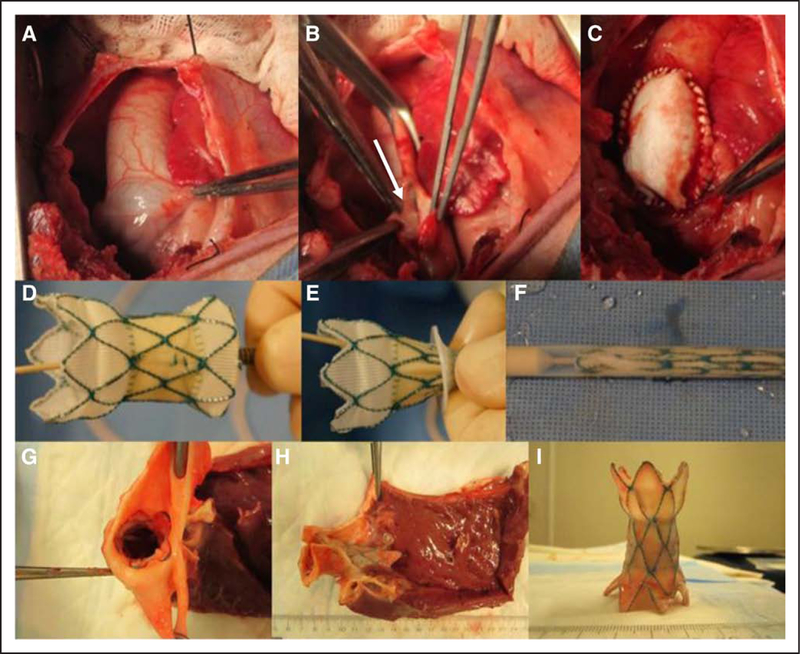
Figure 1.
Photographs of the surgical creation of the ovine pulmonary insufficiency model, followed by transannular patching and Harmony transcatheter pulmonary valve (hTPV) implantation. Intraoperative photographs show the RVOT prevalvectomy (A) and the opened pulmonary artery (PA) with one leaflet of the pulmonary valve being excised (B, arrow). C, Intraoperative picture of transannular patch repair. D, The hTPV in expanded state. E, The hTPV is being loaded into the delivery catheter. F, The hTPV is entirely collapsed into the delivery catheter. G, Picture of the distal PA in the excised heart, showing the hTPV firmly fixed in the PA. H, Photograph shows the device appropriately positioned into the RVOT in situ. I, The hTPV was eventually excised, and valve leaflets were examined. There was no device fracture or erosion. RVOT indicates right ventricular outflow tract.
hTPV Implantation
The hTPV (Medtronic, Minneapolis, MN) consists of a self-expanding nitinol stent with a woven polyester covering and a porcine pericardial valve sewn into its center (proximal diameter=43 mm, valve housing=22 mm, distal diameter=33 mm, length=53 mm; Figure 1D). Baseline angiography was performed, and measurements of the RVOT were made in systole and diastole in the following locations: the pulmonary annulus, the main pulmonary artery (MPA) just proximal to the PA bifurcation, and the length of the MPA (pulmonary annulus to the PA bifurcation). In each animal, the hTPV was crimped onto the 25F delivery system (Figure 1E and 1F). Via the right internal jugular vein, the system was advanced over a guidewire positioned in the distal left PA and positioned for deployment into the MPA. After the device was deployed, angiography was performed to assess the position and function of the device.
Cardiac Imaging Methods
MRI assessments were performed under general anesthesia, using a 3T Siemens Trio scanner (Siemens Healthcare, Malvern, PA) for all scans. A high-fidelity pressure transducer (SPC-350; Millar Instruments Inc, Houston, TX) was inserted percutaneously through the carotid artery into the left ventricle (LV) to allow for both LV pressure monitoring and cardiac-gated image acquisition. After the MRI assessments, each animal was allowed to recover and was then placed back into its housing unit.
Phase-Contrast MRI Methodology
At all time points, phase-contrast MRI acquisition was used to perform flow quantification at the aorta and the MPA and its branches. Imaging parameters were as follows: echo time, 3.5 ms; temporal resolution, 40 ms; flip angle, 25°; and voxel size, 2.0×1.5×5.0 mm (slice thickness). The resulting signal-to-noise ratio was ≈1.0, using signal averaging to improve the signal-to-noise ratio and diminish respiratory artifact. Four-dimensional flow data analysis was performed using a fluid dynamics software package (Ensight; CEI, Apex, NC). Pathlines were computed inside a square volume containing the RVOT. The PRF (%) was calculated as follows: (reverse flow/forward flow)×100.
Ventricular Volume Analysis
High-resolution gradient echo cine short-axis imaging of the ventricles was performed from base to apex. Imaging parameters were specified as an echo time of 2.7 ms; temporal resolution, 31.7 ms; bandwidth, 401 mHz; and voxel size 2.1×2.1×5.0 mm. LV and RV analysis involved contouring the blood pool at end diastole and end systole at each level of the volume data set, resulting in quantification of the end diastolic volume (EDV) and end systolic volume (ESV), respectively (EDV and ESV). The stroke volume was calculated by subtracting the ESV from the EDV; ejection fraction was defined as ([stroke volume/EDV]×100). Indexed volumes were obtained by calculating body surface area using an established conversion formula for sheep: body surface area (m2)=(0.097×weight [kg]0.656).23
Cardiac CT imaging was performed for each animal at each time point to evaluate stent integrity and position using a dual source CT scanner (Definition Flash or Somatom Force; Siemens Healthcare, Malvern, PA). A precontrast prospectively ECG-triggered acquisition was performed for anatomic localization. This was followed by retrospectively ECG-gated helical imaging from the aortic arch through the base of the heart during intravenous injection of iodinated contrast. Images were reconstructed at 20 phases of the cardiac cycle with 0.6-mm slice thickness at 0.4-mm intervals.
Euthanasia and Postmortem Examinations
A sternotomy was performed under general anesthesia in all animals, after the terminal MRI scan was assessed. After dissecting the heart and great vessels free from adhesions and clamping the great vessels, potassium (100 mEq) was administered into the aortic root to arrest the heart. Finally, the heart was excised and opened to inspect the implant site for erosion and adhesions (Figure 1G through 1I).
Statistical Analysis
Data were analyzed using IBM SPSS Statistics version 22.0 (IBM Corporation, Armonk, NY). After checking for normality, mean values and SDs were calculated for normally distributed continuous variables. Comparison of continuous variables between the different time points were made using paired Student t tests, because all MRI-derived continuous variables were normally distributed, and all studies were on the same subjects. A P value <0.05 was considered to be statistically significant.
Results
A total of 13 female Dorsett hybrid sheep were enrolled in this study. After valvectomy and TAP repair, distorted RVOTs were observed (Table 1; Figure 2), as described previously.21,24 Two of these animals died before hTPV implant because of ventricular fibrillation, which occurred while advancing the delivery system through the right heart. The other animals were successfully implanted with the hTPV (n=11), with 7 animals surviving the entire protocol. Four of the animals were euthanized before completion of the protocol: the first because of aspiration on extubation immediately after successful hTPV implantation; the second, 1 month after hTPV implantation because of severe tricuspid regurgitation likely related to damage to the tricuspid valve because of poor wire positioning necessitating vigorous manipulation of the delivery system while advancing through the RVOT (hTPV was functional at the time of euthanasia); the third, 1 month after hTPV implantation, because of proximal displacement of the device during withdrawal of the tip of the delivery catheter, which lead to failure to thrive; and the fourth, because of carotid pseudoaneurysm causing intractable retching 5 months after hTPV implantation. In 2 of the 7 surviving animals, obstruction of the hTPV with aneurysm of the MPA was observed early during follow-up imaging (at 1 month post-hTPV implantation). The hTPV devices in these 2 animals were nonfunctional, but the animals were clinically asymptomatic and, therefore, permitted to survive. For the purposes of long-term assessment of hTPV function (8-month time point), these animals were analyzed separately. Each animal served as its own control using preoperative baseline data for comparison.
Table 1.
RVOT Dimensions Before hTPV Implantation
| Median±Range | |
|---|---|
| PA in systole, mm | 31.5±3.0 |
| PA in diastole, mm | 27.0±4.0 |
| MPA in systole, mm | 28.5±4.0 |
| MPA in diastole, mm | 26.0±3.0 |
| MPA length, mm | 54.0±4.0 |
hTPV indicates Medtronic Harmony transcatheter pulmonary valve; MPA, main pulmonary artery; PA, pulmonary annulus; and RVOT, right ventricular outflow tract.
Figure 2.
Typical RVOT anatomy at 1-month post-transannular patch repair and pre- Harmony transcatheter pulmonary valve implantation, presented with cine magnetic resonance imaging (A), phase-contrast magnetic resonance imaging (B), and computed tomography (C). The angiogram shows the dimensions of the right ventricular outflow tract (RVOT) (D). For all animals, the diameter of the pulmonary annulus after transannular patch repair ranged between 29 and 32 mm in systole. LV indicates left ventricle; and RV, right ventricle.
Cardiac Imaging Results
Cardiac MRI data at each time point for the 5 surviving animals with functional hTPV are listed in Table 2. Cardiac imaging assessment of the RVOT after successful hTPV implantation is displayed in Figure 3. As Figure 4 shows, PRF at baseline was virtually zero. After valvectomy, mean PRF increased significantly (0.2% versus 40.5%; P=0.001). At 1 month after hTPV implantation, a strong decline in PRF to 8.3% was observed (P=0.011), after which the PRF remained stable (P=ns). PRF at 8 months after hTPV implantation was minimal (PRF=8.6%) but differed significantly from baseline (P=0.042; Figure 4).
Table 2.
Characteristics Female Dorsett Sheep at Each Time Point
| Baseline (n=5) | Postvalvectomy (n=5) | hTPV+1 mo (n=5) | hTPV+5 mo (n=5) | hTPV+8 mo (n=5) | |
|---|---|---|---|---|---|
| Weight, kg | 37.2±2.3 | 40.0±3.6 | 54.2±8.1 | 66.4±10.1 | 73.8±10.5 |
| BSA, m2 | 1.0±0.0 | 1.1±0.1 | 1.3±0.1 | 1.5±0.2 | 1.6±0.2 |
| iRVEDV, mL/m2 | 62.3±7.5 | 93.1±15.3 | 79.4±17.7 | 74.5±12.6 | 65.1±17.9 |
| iRVESV, mL/m2 | 17.0±3.0 | 45.4±20.3 | 46.3±20.0 | 36.1±14.3 | 29.4±13.1 |
| iRVSV, mL/m2 | 45.3±8.6 | 47.7±17.7 | 33.2±2.9 | 38.4±7.0 | 33.4±9.1 |
| RVEF, % | 72.3±7.2 | 51.6±17.0 | 43.7±11.4 | 52.9±13.2 | 56.7±12.5 |
| iLVEDV, mL/m2 | 72.8±13.2 | 64.4±13.8 | 65.6±13.5 | 58.6±14.3 | 50.7±7.3 |
| iLVESV, mL/m2 | 27.3±8.8 | 32.6±17.3 | 30.5±16.9 | 26.6±13.5 | 20.1±5.2 |
| iLVSV, mL/m2 | 45.5±8.0 | 31.7±8.7 | 35.1±3.6 | 32.0±5.4 | 29.2±4.7 |
| LVEF, % | 62.9±8.4 | 51.3±15.2 | 55.4±14.7 | 56.4±11.6 | 58.0±10.4 |
| PRF, % | 0.2±0.5 | 40.5±10.0 | 8.3±2.4 | 10.6±6.6 | 8.6±6.0 |
Values are given in mean±SD. BSA indicates body surface area; hTPV, Harmony transcatheter pulmonary valve; iLVEDV, indexed left ventricular end diastolic volume; iLVESV, indexed left ventricular end systolic volume; iLVSV, indexed left ventricular stroke volume; iRVEDV, indexed right ventricular end diastolic volume; iRVESV, indexed right ventricular end systolic volume; iRVSV, indexed right ventricular stroke volume; LVEF, left ventricular ejection fraction; PRF, pulmonary regurgitant fraction; and RVEF, right ventricular ejection fraction.
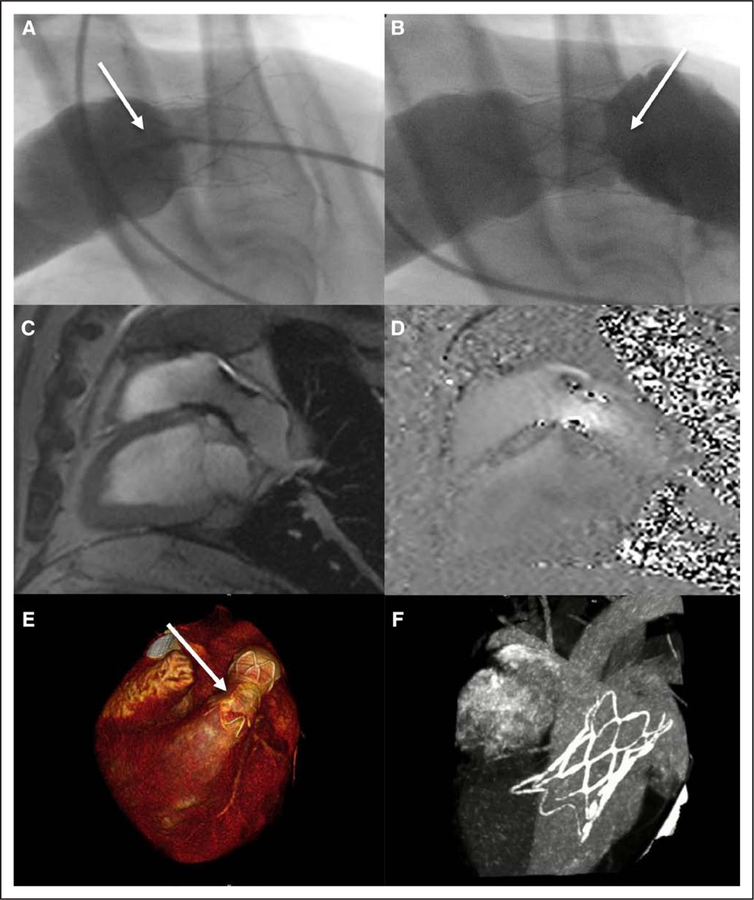
Figure 3.
Imaging of the right ventricular outflow tract after successful Harmony transcatheter pulmonary valve (hTPV) implantation. The angiograms show excellent proximal (A) and distal (B) seal (arrows). Sagittal magnetic resonance imaging (C) and velocity mapping (D) reveal no significant (para)valvular leaking. The hTPV is well positioned (arrow), stable, and no stent fractures were observed (E and F, computed tomography imaging).
Figure 4.
Figure shows means and SE bars. 1: 1 month after Harmony transcatheter pulmonary valve (hTPV) implantation, 5: 3 to 5 months after hTPV implantation, 8: 6 to 8 months after hTPV implantation. PRF indicates pulmonary regurgitant fraction.
Indexed ventricular volume data are displayed for the RV in Figure 5. Compared with baseline, RVEDV showed a significant increase in volume of 49.4% after valvectomy (62.3 versus 93.1 mL/m2; P=0.028). After the hTPV was implanted, RVEDV decreased at each time point, and RVEDV at 8-month follow-up was significantly lower compared with postvalvectomy (65.1 versus 93.1 mL/m2; P=0.045). A similar trend was seen in RVESV, which increased postvalvectomy compared with baseline (17.0 versus 45.4 mL/m2; P=0.043) and decreased over time after hTPV implant.
Figure 5.
Indexed right ventricular volumes at each time point. Figure shows means and SE bars. 1: 1 month after Harmony transcatheter pulmonary valve (hTPV) implantation, 5: 3 to 5 months after hTPV implantation, 8: 6 to 8 months after hTPV implantation. EDV indicates end diastolic volume; and ESV, end systolic volume.
There was no significant difference in either RVEDV or RVESV 8 months after hTPV implantation compared with baseline (P=0.79 and P=0.13, respectively). In the LV, EDV was lower after valvectomy compared with baseline (72.8 versus 64.4 mL/m2; P=0.19). No significant difference in either LVEDV or LVESV was found 8-month post-hTPV implantation compared with baseline (P=0.055 and P=0.24, respectively).
Ventricular ejection fraction dropped in the RV and in the LV after valvectomy (72.3 versus 51.6% and 62.9 versus 51.3%, respectively; both P=ns) but normalized after hTPV with no significant difference at 8 months compared with baseline values (RV ejection fraction P=0.07 and LV ejection fraction P=0.41; Figure 6).
Figure 6.
Ejection fraction for the right ventricle (RV) and left ventricle (LV). Figure shows means and SE bars. 1: 1 month after Harmony transcatheter pulmonary valve (hTPV) implantation, 5: 3 to 5 months after hTPV implantation, 8: 6 to 8 months after hTPV implantation. LVEF indicates left ventricular ejection fraction; and RVEF, right ventricular ejection fraction.
Four-Dimensional Flow MRI
Time-resolved 3-dimensional phase-contrast MRI (4-dimensional flow) enabled evaluation of the complex blood flow patterns throughout the heart, using pathline visualization during diastole and systole (Figure 7). After valvectomy was performed, pulmonary regurgitation could clearly be seen, causing a turbulent diastolic flow directed to the apical portion of the RV (Figure 7C). Improvement in pulmonary regurgitation and in 4-dimensional flow parameters was observed after hTPV implant (Figure 7E).
Figure 7.
Four-dimensional flow visualization showing flow dynamics in the right ventricular (RV) outflow tract at baseline (A and B), postvalvectomy (C and D) and 8 months after Harmony transcatheter pulmonary valve (hTPV) implantation (E and F). Cardiac phases are indicated late diastole (A, C, E) and late systole (B, D, F). Severe regurgitation crashing into the RV wall was observed during diastole after valvectomy (C, thick arrow), compared with almost zero regurgitation at baseline (A, dotted arrow) and little regurgitation at 8-month post-hTPV (E, dashed arrow). Velocity scale score in m/s. LPA indicates left pulmonary artery; MPA, main pulmonary artery; RPA, right pulmonary artery; and RV, right ventricular.
ECG-Gated Cardiac CT Scan
Stent integrity and position were evaluated using serial ECG-gated cardiac CT imaging. The devices remained in stable position with no evidence of stent fracture. Two devices were clotted with associated large aneurysm of the MPA easily visualized by CT 1 month after implant (Figure 8). In these particular animals, incomplete proximal seal of the device permitted antegrade perivalvular flow and aneurysm development of the MPA. Because the animals remained asymptomatic, we suspect that occlusion of the device happened over time. Because the lumen of the device became progressively occluded, perivalvular channels likely formed and matured, which served as the only source for blood flow from the RV to the PA. Development of these channels enabled the animals to survive the entire protocol despite stenosis and subsequent occlusion of the hTPV. Of note, one of the devices that developed clot and subsequently became occluded had been used previously in a failed implant procedure. Thus, it was previously exposed to blood and stored in glutaraldehyde solution, which perhaps made subacute thrombosis and occlusion more likely. There was no evidence of hTPV erosion on the CT scan, which was consistent with postmortem examinations in all animals.
Figure 8.
Harmony transcatheter pulmonary valve (hTPV) with occluded lumen and aneurysm formation in 1 animal. A, Angiogram showing perivalvular channels (arrow); B, cardiac magnetic resonance imaging displaying the right ventricular outflow tract with visible flow outside the stent, as indicated by the thick arrow; C, computed tomography showing perivalvular channels around the hTPV (arrow); D, postmortem examination of the stent showing occlusion of the valve, the arrow points out the occluded leaflets of the hTPV.
Discussion
Pulmonary insufficiency is the major cause of long-term morbidity after ToF repair,25 and PVR remains the most common indication for reoperation in these patients.4,5 Although TCPVR has advanced during the past years, current devices are still not applicable for the majority of ToF patients (≥85%) because of size limitations.8,17 Therefore, these patients have no option except surgical PVR, which incurs the inconveniences and risks inherent to open-heart surgery. This presents clinicians charged with the care of these patients with a management dilemma as they try to balance the immediate risks of surgery against the insidious long-term risks associated with chronic volume loading of the right heart. The encouraging news is that TCPVR continues to evolve, and as these technologies expand and diversify, the population eligible for TCPVR will expand in kind.
The Medtronic hTPV is a representative of the next phase of TCPVR, being designed for implantation into dilated, non-RVPA conduit outflow tracts—found in the majority of patients after successful ToF repair. Thus, the hTPV and similar devices hold promise for thousands of patients worldwide. This promise can only become a reality if the device functions as intended in a varied and anatomically complex group of patients.
The purpose of this study was to investigate TCPVR using the self-expanding hTPV in an ovine model that mimics the anatomic complexity encountered clinically in human patients. The aim was both to create a model of PI consistent with ToF after TAP repair and to test the effect of the hTPV on pulmonary regurgitation and ventricular function in the short, intermediate, and long term.
Ovine Model of PI
Consistent with previous studies, the current report demonstrates that postoperative RVOT dysfunction mimicking repaired ToF can be reliably modeled.21,24 In the present animal cohort, we demonstrated a negligibly small PRF at baseline and uniform, circular pulmonary valve annuli. After TAP surgery, the RVOTs became asymmetrically distorted and dilated, and the PRF increased substantially to a mean of 40.5%. This is anatomically and physiologically consistent with anatomies and PRFs reported in humans late after TAP repair of ToF (43±10%26; 39.7±5.7%27). Commensurate with the moderate-to-severe PI, the RVEDV increased significantly over time, simulating the dilated RV commonly encountered clinically.
hTPV Implant Procedure and Survival
Although there was an early learning curve resulting in 2 cases of intractable ventricular fibrillation before hTPV implantation, in most of the animals, the hTPV procedure was straight-forward from a right internal jugular approach using the 25F delivery system. In all but one of the remaining cases, the hTPV was implanted into the intended location, at the level of the pulmonary valve annulus. In that one animal, the device was initially implanted as intended but migrated proximally on withdrawal of the delivery system.
The protocol was intended for long-term survival, and as such, we encountered morbidities in 4 of the implanted animals over time, some of which were noncardiac, all of which required euthanasia in keeping with humane practices. Seven animals survived the entire protocol, with 5 of those having securely positioned, competent, functional hTPV at 8 months. In those animals, hTPV implant resulted in a significant reduction of PRF, improvements in RV and LV volumes, and preserved ventricular function. These results are comparable to findings in human patients after appropriately timed surgical PVR.5 Interestingly, the small amount of pulmonary regurgitation (8.6%) present 8 months after hTPV implantation was explained by incomplete sealing of the proximal end of the hTPV. For the most part, this was inconsequential. However, in 2 animals, large perivalvular channels developed over time, associated with aneurysm formation in the MPA and occlusion of the hTPV lumen. It is unclear whether there is a cause and effect relationship between hTPV occlusion and aneurysm formation; however, we suspect that the primary issue was clot formation on the hTPV leaflets resulting in a relative stenosis, which encouraged more flow around the hTPV with subsequent opening of a large perivalvular channel as the device pulled away from the MPA at its distal end. Of note, one of these animals was at risk for thrombus formation because the hTPV device had been previously exposed to sheep blood, because it was used in one of the cases, where ventricular fibrillation occurred. We think that the finding of aneurysm development highlights the importance of obtaining a tight seal between the RVOT and the proximal aspect of the hTPV at the time of implantation. Given the anatomic variability of ToF patients, successful self-expanding devices such as the hTPV will likely need to be available in a variety of diameters and lengths, as previously noted by others,17 to facilitate adequate sealing. On the basis of this observation, we think that matching the device to the individual anatomy of the patient seems crucial for optimal outcome, especially with regard to the proximal seal placement.
MRI and CT Findings
The primary end points for this study were MRI and CT findings over time, and in the 5 long-term surviving animals with functional hTPVs, the results were encouraging. The hTPV devices remained in stable position, with no device fractures and no erosions. There were no significant differences in ventricular volume data between baseline and 8 months after hTPV (Figure 5). Importantly, a significant decrease in RVEDV was observed at 8-month follow-up compared with the initial increase in RVEDV after valvectomy (65.1 versus 93.1 mL/m2; P=0.045), indicating improvements of RV volumes after hTPV implantation. Theoretically, improvements in RV volume are related to improvements at the cardiomyocyte level and could indicate RV remodeling. In addition, both RV and LV functions were preserved in the long term after hTPV implantation (Figure 6). On the basis of these findings, it is reasonable to predict that if timed appropriately, hTPV implant will lead to the same reverse ventricular remodeling demonstrated in ToF patients with appropriately timed surgical PVR,28 although without the need for sternotomy and cardiopulmonary bypass.
Four-Dimensional Flow MRI Visualization
Pathline visualization of the created pulmonary regurgitation in our animal models, using time-resolved 3-dimensional phase-contrast MRI, revealed interesting findings. During diastole, a turbulent regurgitant flow was observed forcefully crashing into the apical RV. This could potentially cause damage to the regional cardiomyocytes in the RV wall. Longstanding regurgitant flow crashing into the same region of the RV could lead to local adverse remodeling, resulting in heterogeneous RV dilatation and dysfunction. However, pathological examination of the suspected tissue is ongoing, so for now this observation should be considered speculative. The phenomenon of regional wall motion abnormalities in the RV in ToF patients was described earlier by Kowalik et al,29 showing increased RV regional deformation in patients with significant pulmonary regurgitation after ToF repair. Histological examination of RV tissue in ovine models of PI after ToF repair may be an interesting focus for future studies.
Limitations
Despite our ability to model complex RVOT dysfunction, animal models do not completely reflect the complexities of congenital heart disease in humans. Pulmonary trunk anatomy, RVOT morphology, and RV characteristics 1 month after TAP in our model unavoidably differ from the situation in human patients. However, despite these limitations, we were able to demonstrate the dramatic effect that PI has on the myocardium and importantly that implant of the Harmony valve reverses those changes.
In addition, because of the small number of surviving animals, there was limited power, and the statistical analyses reported should be considered preliminary. Only 7 animals survived the entire protocol. Five of these had functioning hTPV devices, and only those animals were, therefore, considered in the final analysis of ventricular size and function. The 2 other surviving animals were excluded from this analysis, because their hTPV devices were found to be occluded early in follow-up and, therefore, nonfunctional. These animals were instructive in their own way, because they demonstrate the challenge and importance of obtaining appropriate sealing of catheter-based heart valves.
Conclusions
Implantation of the Medtronic hTPV significantly reduced pulmonary valve regurgitation, facilitated RV volume improvements, and preserved RV and LV function in an ovine model of PI after ToF repair at a follow-up time of 8 months. This percutaneous strategy could potentially offer an exciting alternative for standard surgical PVR and is, in contrast to currently available percutaneous PVR, potentially applicable for the majority of ToF patients with oversized RVOTs. Our experience with this percutaneous PVR strategy suggests the potential for lower risks, as compared with the risks of open-heart surgery, because the procedure and technique mature and become more established over time.
The availability of percutaneous PVR strategies in these patients also may have the potential to shift the timing of PVR toward earlier intervention. Matching the device to the anatomy of the individual patient is critical for optimal outcome. Development of novel percutaneous devices is rapidly evolving, and further investigation of these strategies, both preclinical and clinical, is necessary to treat the entire complex population of postoperative ToF patients.
WHAT IS KNOWN
Transcatheter pulmonary valve replacement is an effective alternative to open-heart surgery in some patients with right ventricular out flow tract dysfunction after the repair of tetralogy of Fallot. However, transcatheter pulmonary valve replacement is not applicable to the majority of patients after transannular patch.
The Medtronic Harmony transcatheter pulmonary valve (hTPV) was designed for catheter-based valve replacement in transannular patch patients. Typically, these patients have significantly dilated, distorted, nonuniform right ventricular outflow tracts.
WHAT THE STUDY ADDS
This study tested the effect of implantation of the novel Medtronic hTPV on pulmonary insufficiency and ventricular function in an ovine model of chronic postoperative pulmonary insufficiency after trans-annular patch.
We demonstrated that hTPV implantation is feasible, significantly reduced pulmonary regurgitant fraction, and improved ventricular function in an ovine model.
This preclinical work suggests that the Harmony valve holds promise as an alternative to surgical valve replacement for patients with larger right ventricular outflow tracts experiencing pulmonary valve insufficiency.
Acknowledgments
Sources of Funding
This study was supported by The Children’s Hospital of Philadelphia internal funding, and philanthropic support was received from Mr Richard Seidel and family. Medtronic supplied the devices free of charge for this study.
Footnotes
Disclosures
Dr Gillespie serves as a consultant to Medtronic, the manufacturer of the hTPV device. Dr Litt receives research funding from Siemens Healthcare for unrelated projects. The other authors report no conflicts.
References
- 1.Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet 2009;374:1462–1471. doi: 10.1016/S0140-6736(09)60657-7. [DOI] [PubMed] [Google Scholar]
- 2.Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998–2005. J Pediatr 2008;153:807–813. doi: 10.1016/j.jpeds.2008.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luijten LW, van den Bosch E, Duppen N, Tanke R, Roos-Hesselink J, Nijveld A, van Dijk A, Bogers AJ, van Domburg R, Helbing WA. Long-term outcomes of transatrial-transpulmonary repair of tetralogy of Fallot. Eur J Cardiothorac Surg 2015;47:527–534. doi: 10.1093/ejcts/ezu182. [DOI] [PubMed] [Google Scholar]
- 4.Al Habib HF, Jacobs JP, Mavroudis C, Tchervenkov CI, O’Brien SM, Mohammadi S, Jacobs ML. Contemporary patterns of management of tetralogy of Fallot: data from the Society of Thoracic Surgeons Database. Ann Thorac Surg 2010;90:813–819, discussion 819. doi: 10.1016/j.athoracsur.2010.03.110. [DOI] [PubMed] [Google Scholar]
- 5.Ferraz Cavalcanti PE, Sá MP, Santos CA, Esmeraldo IM, de Escobar RR, de Menezes AM, de Azevedo OM Jr, de Vasconcelos Silva FP, Lins RF, Lima Rde C. Pulmonary valve replacement after operative repair of tetralogy of Fallot: meta-analysis and meta-regression of 3,118 patients from 48 studies. J Am Coll Cardiol 2013;62:2227–2243. doi: 10.1016/j.jacc.2013.04.107. [DOI] [PubMed] [Google Scholar]
- 6.Geva T. Indications and timing of pulmonary valve replacement after tetralogy of Fallot repair. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2006;9:11–22. doi: 10.1161/CIRCULATIONAHA.113.005878. [DOI] [PubMed] [Google Scholar]
- 7.O’Byrne ML, Glatz AC, Mercer-Rosa L, Gillespie MJ, Dori Y, Goldmuntz E, Kawut S, Rome JJ. Trends in pulmonary valve replacement in children and adults with tetralogy of Fallot. Am J Cardiol 2015;115:118–124. doi: 10.1016/j.amjcard.2014.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geva T, Gauvreau K, Powell AJ, Cecchin F, Rhodes J, Geva J, del Nido P. Randomized trial of pulmonary valve replacement with and without right ventricular remodeling surgery. Circulation 2010;122(suppl 11):S201–S208. doi: 10.1161/CIRCULATIONAHA.110.951178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oosterhof T, Meijboom FJ, Vliegen HW, Hazekamp MG, Zwinderman AH, Bouma BJ, van Dijk AP, Mulder BJ. Long-term follow-up of homo-graft function after pulmonary valve replacement in patients with tetralogy of Fallot. Eur Heart J 2006;27:1478–1484. doi: 10.1093/eurheartj/ehl033. [DOI] [PubMed] [Google Scholar]
- 10.Boshoff DE, Cools BL, Heying R, Troost E, Kefer J, Budts W, Gewillig M. Off-label use of percutaneous pulmonary valved stents in the right ventricular outflow tract: time to rewrite the label? Catheter Cardiovasc Interv 2013;81:987–995. doi: 10.1002/ccd.24594. [DOI] [PubMed] [Google Scholar]
- 11.Meadows JJ, Moore PM, Berman DP, Cheatham JP, Cheatham SL, Porras D, Gillespie MJ, Rome JJ, Zahn EM, McElhinney DB. Use and performance of the Melody Transcatheter Pulmonary Valve in native and postsurgical, nonconduit right ventricular out-flow tracts. Circ Cardiovasc Interv 2014;7:374–380. doi: 10.1161/CIRCINTERVENTIONS.114.001225. [DOI] [PubMed] [Google Scholar]
- 12.Gillespie MJ, Rome JJ, Levi DS, Williams RJ, Rhodes JF, Cheatham JP, Hellenbrand WE, Jones TK, Vincent JA, Zahn EM, McElhinney DB. Melody valve implant within failed bioprosthetic valves in the pulmonary position: a multicenter experience. Circ Cardiovasc Interv 2012;5:862–870. doi: 10.1161/CIRCINTERVENTIONS.112.972216. [DOI] [PubMed] [Google Scholar]
- 13.Eicken A, Ewert P, Hager A, Peters B, Fratz S, Kuehne T, Busch R, Hess J, Berger F. Percutaneous pulmonary valve implantation: two-centre experience with more than 100 patients. Eur Heart J 2011;32:1260–1265. doi: 10.1093/eurheartj/ehq520. [DOI] [PubMed] [Google Scholar]
- 14.Guccione P, Milanesi O, Hijazi ZM, Pongiglione G. Transcatheter pulmonary valve implantation in native pulmonary outflow tract using the Edwards SAPIEN™ transcatheter heart valve. Eur J Cardiothorac Surg 2012;41:1192–1194. doi: 10.1093/ejcts/ezr130. [DOI] [PubMed] [Google Scholar]
- 15.Zahn EM, Hellenbrand WE, Lock JE, McElhinney DB. Implantation of the melody transcatheter pulmonary valve in patients with a dysfunctional right ventricular outflow tract conduit early results from the U.S. Clinical trial. J Am Coll Cardiol 2009;54:1722–1729. doi: 10.1016/j.jacc.2009.06.034. [DOI] [PubMed] [Google Scholar]
- 16.Kenny D, Hijazi ZM, Kar S, Rhodes J, Mullen M, Makkar R, Shirali G, Fogel M, Fahey J, Heitschmidt MG, Cain C. Percutaneous implantation of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position: early phase 1 results from an international multicenter clinical trial. J Am Coll Cardiol 2011;58:2248–2256. doi: 10.1016/j.jacc.2011.07.040. [DOI] [PubMed] [Google Scholar]
- 17.Schievano S, Coats L, Migliavacca F, Norman W, Frigiola A, Deanfield J, Bonhoeffer P, Taylor AM. Variations in right ventricular outflow tract morphology following repair of congenital heart disease: implications for percutaneous pulmonary valve implantation. J Cardiovasc Magn Reson 2007;9:687–695. doi: 10.1080/10976640601187596. [DOI] [PubMed] [Google Scholar]
- 18.Schievano S, Taylor AM, Capelli C, Coats L, Walker F, Lurz P, Nordmeyer J, Wright S, Khambadkone S, Tsang V, Carminati M, Bonhoeffer P. First-in-man implantation of a novel percutaneous valve: a new approach to medical device development. EuroIntervention 2010;5:745–750. doi: 10.4244/EIJV5I6A122. [DOI] [PubMed] [Google Scholar]
- 19.Promphan W, Prachasilchai P, Siripornpitak S, Qureshi SA, Layangool T. Percutaneous pulmonary valve implantation with the Venus P-valve: clinical experience and early results. Cardiol Young 2016;26:698–710. doi: 10.1017/S1047951115001067. [DOI] [PubMed] [Google Scholar]
- 20.Cao QL, Kenny D, Zhou D, Pan W, Guan L, Ge J, Hijazi ZM. Early clinical experience with a novel self-expanding percutaneous stent-valve in the native right ventricular outflow tract. Catheter Cardiovasc Interv 2014;84:1131–1137. doi: 10.1002/ccd.25544. [DOI] [PubMed] [Google Scholar]
- 21.Robb JD, Harris MA, Minakawa M, Rodriguez E, Koomalsingh KJ, Shuto T, Dori Y, Gorman RC, Gorman JH 3rd, Gillespie MJ. An ovine model of pulmonary insufficiency and right ventricular outflow tract dilatation. J Heart Valve Dis 2012;21:247–252. [PMC free article] [PubMed] [Google Scholar]
- 22.Boudjemline Y, Agnoletti G, Bonnet D, Sidi D, Bonhoeffer P. Percutaneous pulmonary valve replacement in a large right ventricular outflow tract: an experimental study. J Am Coll Cardiol 2004;43:1082–1087. doi: 10.1016/j.jacc.2003.10.037. [DOI] [PubMed] [Google Scholar]
- 23.Berman A Effects of body surface area estimates on predicted energy requirements and heat stress. J Dairy Sci 2003;86:3605–3610. doi: 10.3168/jds.S0022-0302(03)73966-6. [DOI] [PubMed] [Google Scholar]
- 24.Robb JD, Harris MA, Minakawa M, Rodriguez E, Koomalsingh KJ, Shuto T, Shin DC, Dori Y, Glatz AC, Rome JJ, Gorman RC, Gorman JH 3rd, Gillespie MJ. Melody valve implantation into the branch pulmonary arteries for treatment of pulmonary insufficiency in an ovine model of right ventricular outflow tract dysfunction following tetralogy of Fallot repair. Circ Cardiovasc Interv 2011;4:80–87. doi: 10.1161/CIRCINTERVENTIONS.110.959502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gregg D, Foster E. Pulmonary insufficiency is the nexus of late complications in tetralogy of Fallot. Curr Cardiol Rep 2007;9:315–322. doi: 10.1007/BF02938380. [DOI] [PubMed] [Google Scholar]
- 26.Lee C, Lee CH, Kwak JG, Kim SH, Shim WS, Lee SY, Jang SI, Park SJ, Kim YM. Factors associated with right ventricular dilatation and dysfunction in patients with chronic pulmonary regurgitation after repair of tetralogy of Fallot: analysis of magnetic resonance imaging data from 218 patients. J Thorac Cardiovasc Surg 2014;148:2589–2595. doi: 10.1016/j.jtcvs.2014.07.051. [DOI] [PubMed] [Google Scholar]
- 27.O’Meagher S, Ganigara M, Munoz P, Tanous DJ, Chard RB, Celermajer DS, Puranik R. Right ventricular outflow tract enlargement prior to pulmonary valve replacement is associated with poorer structural and functional outcomes, in adults with repaired tetralogy of Fallot. Heart Lung Circ 2014;23:482–488. doi: 10.1016/j.hlc.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Therrien J, Siu SC, McLaughlin PR, Liu PP, Williams WG, Webb GD. Pulmonary valve replacement in adults late after repair of tetralogy of Fallot: are we operating too late? J Am Coll Cardiol 2000;36:1670–1675. doi: 10.1016/S0735-1097(00)00930-X. [DOI] [PubMed] [Google Scholar]
- 29.Kowalik E, Kowalski M, Różański J, Kuśmierczyk M, Hoffman P. The impact of pulmonary regurgitation on right ventricular regional myocardial function: an echocardiographic study in adults after total repair of tetralogy of Fallot. J Am Soc Echocardiogr 2011;24:1199–1204. doi: 10.1016/j.echo.2011.08.008. [DOI] [PubMed] [Google Scholar]