Abstract
Aims:
Endoscopic management of indeterminate strictures and complex stones remains a challenge, for which the latest generation single-operator digital cholangioscope (SpyGlass DS) has shown promising results. We aimed to study the clinical impact of single-operator digital cholangioscope at our tertiary academic center.
Methods:
We retrospectively reviewed all digital cholangioscopies performed from June 2015 to May 2018. Patient characteristics, procedure characteristics, and post-procedural patient outcomes were recorded.
Results:
A total of 50 patients (26 men, average age 61.4 years) underwent 67 procedures. Indications were biliary stones (21/50, 42%), strictures and primary sclerosing cholangitis surveillance (22/50, 46%), and miscellaneous (7/50, 14%). The average procedure time was 82 ± 29 min (99.5 min for stones and 74.2 min for strictures). Stone clearance was achieved in 19/21 (90.47%) cases, with electrohydraulic lithotripsy employed in 16/21 and repeat cholangioscopy necessary in 9/21. Malignant strictures (10) were differentiated from benign (12) in all cases both in patients with primary sclerosing cholangitis (9) and in those without (13), based on visual cholangioscopic features (sensitivity and specificity 100%), single-operator digital cholangioscope–directed biopsies (sensitivity 60% and specificity 100%), and brush cytology (sensitivity 37.5% and specificity 100%). Complications included one post-sphincterotomy bleeding and one post-procedural cholangitis despite antibiotic prophylaxis, but no procedure-related mortality.
Conclusion:
Single-operator digital cholangioscope had a high success rate and a low rate of complications for management of indeterminate strictures and difficult biliary stones. Visual cholangioscopic features of biliary strictures had excellent diagnostic accuracy, and targeted biopsies outperformed brush cytology. Early implementation of cholangioscopy for select indications leads to successful patient outcomes and reduces diagnostic delays, cost, and risks of repeat endoscopic retrograde cholangiopancreatographies.
Keywords: cholangiocarcinoma, cholangioscopy, complex biliary stone, indeterminate biliary stricture, primary sclerosing cholangitis
Introduction
The diagnostic evaluation of indeterminate biliary strictures and the endoscopic management of difficult bile duct stones can be challenging. Current standard of care for evaluation of biliary strictures seen on imaging [magnetic resonance cholangiopancreatography (MRCP), computed tomography (CT), or ultrasound] begins with endoscopic retrograde cholangiopancreatography (ERCP), which utilizes fluoroscopy to create two-dimensional images to localize and characterize the extent of bile duct pathology. Diagnostic options for biliary strictures or lesions include intraductal biopsies and cytology brushings. Although still widely used and inexpensive, ductal cytology brushing is a blind sampling technique that is limited by poor sensitivity and often yields inadequate specimens, which can lead to low diagnostic accuracy.1,2 On the other hand, for the management of difficult biliary stones, successful ductal clearance using balloon sweep or basket retrieval is limited by stone characteristics and location within the biliary tree.3
In the 1970s, conventional peroral cholangioscopy was introduced to aid with diagnosis and treatment by allowing for direct visualization of the biliary system, but was limited by several factors including suboptimal irrigation capabilities, limited maneuverability of the scope, small instrument channel, and the requirement of two endoscopsits.4,5 Due to these limitations and its labor-intensive nature, the ‘mother-baby’ system failed to gain widespread use. In 2006, a single-operator peroral cholangioscopy (SOC) (SpyGlass; Boston Scientific, Natick, MA, USA) was developed, repiquing interest in cholangioscopy as it overcame many of these limitations and offered several improvements over the conventional model, including increased irrigation flow rate, improved steering, and the capability to perform targeted biopsies under direct visualization.3,4,6 These improvements allow for direct sampling of suspicious biliary lesions with the hope of improved accuracy in detecting malignancy.7 The latest digital version of the single-operator cholangioscope (D-SOC) (SpyGlass DS; Boston Scientific) offers additional advantages including sharper image quality and an easier setup process, allowing for both diagnostic and therapeutic benefits.
Thus far, D-SOC has shown significant promise for the evaluation of indeterminate biliary strictures and treatment of difficult bile duct stones. Considering that these results come from high-volume centers of excellence, it remains unclear whether they can be duplicated at other centers. The objective of this descriptive study was to review the indications for D-SOC, the procedural findings and interventions, procedure success rate, and overall impact on clinical management at our tertiary academic center.
Methods
Study design and patients
We retrospectively reviewed all consecutive D-SOC procedures performed by a single experienced endoscopist at our tertiary referral center from June 2015 through May 2018. We used our center’s electronic medical record to collect pre-, intra-, and post-procedural data. The study protocol was approved by our center’s institutional review board. Eligibility criteria for our study included patients 18 years or older and all those referred for cholangiopancreatoscopy for any indication during the study period. Ethical approval was obtained from the UC Davis IRB (IRB ID: 1063005-3), who is the governing board of ethics in research at our institution.
The UC Davis IRB approved a waiver of consent for our study. We request this IRB-approved waiver of consent due to the nature of the study (retrospective chart review) and the minimal risks involved. Data were obtained by chart review, coded, and stored on password-protected storage devices, for which only the primary and coinvestigator had access to.
Single-operator digital cholangioscope system and procedures
All procedures were performed using Olympus TJF-160F or TJF-180F duodenoscopes (Olympus Medical Systems, Tokyo, Japan) and the Boston Scientific SpyGlass DS system. Procedures were performed with CO2 insufflation, under moderate sedation or general anesthesia, in the semiprone swimmer’s position.
When necessary, electrohydraulic lithotripsy (EHL) was performed using the Nortech Autolith system (Northgate Technologies Inc., Elgin, IL, USA) (settings: power 80–100%, rate 15 shots/s, 20 shots per foot pedal depression). Following EHL, stone extraction balloons or baskets were utilized for stone debris clearance. Biliary sphincterotomy, extension of pre-existing sphincterotomy, or sphincteroplasty was done at the discretion of the endoscopist. In the event of incomplete stone extraction during the index procedure, biliary stenting was performed followed by repeat ERCP with stent removal and additional stone clearance within a few weeks to a few months. Duct clearance was confirmed by cholangioscopy or balloon occlusion cholangiogram.
For biliary strictures, we obtained D-SOC-directed biopsies using the SpyBite Biopsy Forceps. Balloon dilation of strictures was performed with 4- to 8-mm dilation balloons. Cytology brushings were obtained with a Boston Scientific cytology brush. Biopsy and cytology specimens were reviewed by experienced gastrointestinal histopathologists and cytopathologists. When indicated, plastic or metal biliary stents were placed. As a general practice, we avoided placing biliary stents in primary sclerosing cholangitis (PSC) patients.
All patients received intravenous Lactated Ringer’s solution and rectal indomethacin post procedure, unless there were contraindications. Patients with biliary strictures, PSC, or known biliary malignancy received periprocedural antibiotic prophylaxis with Levofloxacin 500 mg IV (250 mg IV if renal function was decreased).
Outcomes
Clinical success was defined as the ability to achieve the therapeutic or diagnostic objective based on the procedure indication. For biliary stone cases, a procedure was deemed clinically successful if we were able to achieve stone clearance. For indeterminate strictures, the goal was differentiation of malignant and benign etiologies via D-SOC-directed bile duct examination and biopsy if suspicious lesions were present. Additional endpoints included sensitivity and specificity of visual impression and D-SOC-directed biopsies in diagnosis of indeterminate lesions, as well as the number of D-SOC procedures required to complete the diagnostic or therapeutic objective.
The electronic medical record was also reviewed to identify post-procedural complications. Adverse events were defined as procedural complications resulting in an emergency room visit, hospital admission, prolongation of hospital stay, urgent surgical intervention as a direct consequence of procedural events, and blood loss requiring a transfusion or resulting in a drop in the hemoglobin level of 2 gm/dL or more.
Statistical analysis
Summary statistics included mean, standard deviation, and median.
Results
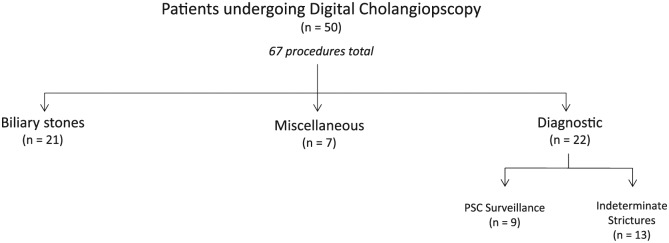
A total of 50 patients [26 men, average age 61.4 years (range 21–90)] underwent 67 D-SOC procedures in the study period. A majority of our patients were White: 58% non-Hispanic White, 14% Asian, 4% African American, and 24% other (Hispanic, Pacific Islander). Baseline patient and procedure indications are summarized in Table 1 and Figure 1. Forty-two (84%) patients had undergone at least one ERCP prior to the index D-SOC case without achieving clinical success as defined above.
Table 1.
Baseline patient characteristics and procedure indications.
| Patients, n | 50 |
| Average age (range) | 61.4 (21–90) |
| Average procedure time (range), minutes | 82 (29–234) |
| Sex, n (%) | |
| Male | 26 (52) |
| Female | 24 (48) |
| Race, n (%) | |
| White | 29 (58) |
| Asian | 7 (14) |
| African American | 2 (4) |
| Other | 12 (24) |
| Setting, n (%) | |
| Inpatient | 23 (46) |
| Outpatient | 27 (54) |
| Previous ERCP procedures, n | |
| 0 | 8 |
| 1 | 17 |
| 2 | 10 |
| 3 or more | 15 |
| Procedure indication, n | |
| Biliary stones | 21 |
| Indeterminate biliary strictures | 13 |
| PSC surveillance | 9 |
| Miscellaneous | |
| Palliative biliary decompression | 3 |
| Pancreatic duct stone | 2 |
| Recurrent parasitic hepatobiliary infection | 1 |
| Preoperative planning for cholangiocarcinoma resection | 1 |
ERCP, endoscopic retrograde cholangiopancreatography; PSC, primary sclerosing cholangitis.
Figure 1.
Indications for Cholangioscopy.
PSC, primary sclerosing cholangitis.
Out of 50 patients, 21 (42%) underwent D-SOC for treatment of bile duct stones, 13 (26%) for evaluation of indeterminate biliary strictures, 9 (18%) for PSC surveillance, and 7 (14%) for miscellaneous indications, which included two pancreatic duct stones cases, three patients requiring palliative biliary decompression in setting of known malignancy, one with known cholangiocarcinoma who required preoperative planning for surgical tumor resection, and one patient with AIDS and clonorchis sinensis infection with persistent abnormal liver function tests (LFTs), diarrhea, and failure to thrive (Figure 1).
The average procedure time was 82 ± 29 min. Our clinical success rate was 94% (47/50) as defined by the ability to achieve the therapeutic or diagnostic objective – 90.4% (19/21) for difficult bile duct stones, 50% (1/2) for pancreatic duct stones, 100% (9/9) for PSC surveillance, and 100% (13/13) for indeterminate strictures. All three of our palliative procedures were successful. Patient characteristics, subgrouped by procedure indication, are summarized in Table 2.
Table 2.
Baseline patient and procedure characteristics by indication.
| Biliary stones | Indeterminate strictures | |
|---|---|---|
| Total number of patients | 21 | 22 |
| Average age (range) | 62.5 (29–90) | 59.7 (21–86) |
| Average procedure time (range), minutes | 99.5 (37–234) | 74.2 (29–117) |
| Sex, n (%) | ||
| Male | 7 (33) | 15 (68) |
| Female | 14 (67) | 7 (32) |
| Required EHL, n (%) | 16 (76) | |
| Required repeat SpyGlass, n (%) | 9 (43) | |
| Number of previous ERCP procedures | ||
| 0 | 1 | 5 |
| 1 | 9 | 7 |
| 2 | 7 | 2 |
| 3 or more | 4 | 8 |
EHL, electrohydraulic lithotripsy; ERCP, endoscopic retrograde cholangiopancreatography.
Therapeutic single-operator digital cholangioscope
Of the 21 cases that were performed for bile duct stones, a majority (17/21, 80.9%) were located in the distal common bile duct (CBD), 48% (9/21) in mid CBD, 38% (8/21) in the common hepatic duct, 14.2% (3/21) in the right intrahepatic duct, and one in the cystic duct. We were able to visualize stones via cholangioscopy in all cases. Complete stone clearance was achieved during the index procedures in 12/21 (57%) cases. In the remaining 9/21, one additional cholangioscopy was needed in seven and two needed two or more.
EHL was performed in 16/21 (76%) cases. The 5/21 cases wherein EHL was not used included three cases in which the EHL probe could not be advanced (one due to probe malfunction, one due to a difficult long duodenoscope position, and one case of pyloric stenosis which needed balloon dilation), one pregnant patient wherein D-SOC was utilized to visualize the stone and confirm duct clearance while avoiding use of fluoroscopy, and finally a patient with multiple CBD stones, a body mass index (BMI) of 55, and an abdominal pannus that led to inconclusive magnetic resonance imaging (MRI)/MRCP images, in which D-SOC was used diagnostically to visualize and quantify stone burden in the CBD. Ductal clearance was achieved in four of these five cases by conventional ERCP methods. One patient is due to return for follow-up ERCP for stone clearance.
Biliary stents were placed in 13/21 (61.9%) to ensure continued biliary drainage in the setting of incomplete stone clearance. Stent removal and duct clearance was achieved during follow-up ERCP in all but two cases: one 93-year-old patient with dementia, with an intact gallbladder with stones who was not deemed well tolerated to undergo cholecystectomy, and hence was at risk for recurrent choledocholithiasis, had a fully covered metal stent placed, and did not return for ERCP; another 90-year-old patient with an indwelling biliary plastic stent who has yet to return for repeat ERCP.
Average procedure time for biliary stone cases was 99.5 min (range 37–234).
One case of choledocholithiasis involved a patient with a history of Roux-en-Y gastric bypass who had large stones at the hilum above a biliary stricture requiring a percutaneous approach followed by successful EHL-guided stone fragmentation and ductal clearance in a single session.
Of the two cases performed for pancreatic duct stones, we achieved clinical success in one by EHL fragmentation. A pancreatic duct stricture in the head of pancreas precluded advancement of the D-SOC catheter in the second case. This patient will be referred for extracorporeal shock wave lithotripsy (ESWL) of pancreatic duct stones.
Diagnostic single-operator digital cholangioscope
Diagnostic D-SOC was performed in 22 procedures with 13 patients being evaluated for indeterminate biliary strictures and 9 undergoing PSC surveillance due to worsening LFTs.
SpyBite biopsies were obtained in 10/13 (76.9%) indeterminate biliary strictures based on whether or not suspicious lesions amenable to biopsy were seen on visual exam. Balloon dilatation of stricture was performed in four and stents were placed in eight (61.5%) patients. Of the eight, five had uncovered metal stents placed for palliative intent and have all passed away. One patient had a covered metal stent placed and eventually underwent surgical resection for biliary intraductal papillary mucinous neoplasm (IPMN) that progressed to invasive carcinoma.
Distinction between malignant and benign biliary strictures was successful in all 13 cases based on visual impression, biopsy, and brush cytology. Malignancy was strongly suspected on visual findings in all 10 cases of malignancy, while SpyBite biopsies showed malignant histology in 6/10 (60%) patients and brush cytology confirmed malignancy in 3/8 (37.5%). For evaluation of indeterminate biliary strictures and suspected biliary malignancy, sensitivity and specificity using visual cholangioscopic exam, SpyBite biopsy, and brush cytology were 100% and 100%, 60% and 100%, and 37.5% and 100%, respectively (Table 3).
Table 3.
Performance characteristics of diagnostic modalities for indeterminate biliary strictures.
| Sensitivity (%) | True positive | False negative | |
|---|---|---|---|
| Malignant (10) | |||
| Visual impression | 100 | 10 | 0 |
| D-SOC biopsy | 60 | 6 | 4 |
| Cytology brushing* | 37.5 | 3 | 5 |
| Specificity (%) | True negative | False positive | |
| Benign (12) | |||
| Visual impression | 100 | 12 | 0 |
| D-SOC biopsy | 100 | 5 | 0 |
| Cytology brushing | 100 | 7 | 0 |
D-SOC, single-operator digital cholangioscope.
Cytology brushing was obtained in 8 out of 10 cases of malignant biliary stricture.
In the four malignant cases in which SpyBite biopsy yielded benign histology, the visual impression of D-SOC was strongly suspicious for malignancy. Two of these patients transitioned to palliative care and have since passed away, while the third underwent several cycles of chemotherapy before transitioning to palliative care as well. Of the three cases with a final diagnosis of a benign stricture, SpyBite biopsies were obtained in two cases and showed benign tissue in both. No suspicious lesions amenable to biopsy were seen in the other case(s). Interestingly, one of these patients who had initially presented with imaging concerning for a distal CBD stricture was eventually found to have external biliary compression from a pancreatic mass. This patient ultimately chose palliative care and did not undergo further cancer-directed treatment. For the other two cases, final benign diagnosis has been confirmed based on at least 6 months of follow-up (average 19.2 months) with no clinical evidence (e.g. tumor markers, imaging) of malignancy. With regard to procedure requirements, 7 (53.8%) of the 13 patients only required one D-SOC, while 3 (23.1%) required repeat D-SOC for persistent biliary obstruction requiring stent exchange and eventual metal stent placement. The other three patients required an additional ERCP for plastic stent removal.
Nine patients underwent D-SOC for surveillance of strictures in setting of PSC with worsening LFTs. The primary objective in six (66.7%) cases was to rule out cholangiocarcinoma. The other three patients were having symptoms concerning for cholangitis, so D-SOC was primarily done to evaluate for biliary obstruction and perform therapeutic intervention (e.g. balloon dilatation, stent placement) if necessary, with an additional goal to evaluate for cholangiocarcinoma. SpyBite biopsies were performed in five (55.6%) cases. Balloon dilatation was performed in five cases and two patients required a plastic stent, one of which was removed and the other remained in place as the patient passed away.
Distinction between malignant and benign strictures was successful in all nine PSC cases, based on visual impression and SpyBite pathology. In the two patients with a final malignant diagnosis, SpyBite biopsies and brush cytology showed suspicious findings in one case and were non-diagnostic in the other. However, malignancy was strongly suspected on visual exam in both cases. Of the seven cases with a benign diagnosis, SpyBite specimens yielded benign histology in three. No SpyBite biopsies were obtained in four cases as there was no suspicious lesion or mass to biopsy. For PSC surveillance, sensitivity and specificity of visual exam, biopsy, and brush cytology were 100% and 100%, 50% and 100%, and 50% and 100%, respectively. With regard to procedure requirements, six (66.7%) patients only required one SpyGlass procedure, while three required one additional ERCP, with one patient in this group requiring SpyGlass with EHL for stone fragmentation and clearance. Average clinical follow-up time for these patients was 26.3 months (range 8–35) with no clinical evidence of malignancy.
For the malignant strictures, with and without PSC, we observed similar cholangioscopic findings that were suspicious for malignancy, which are summarized in Table 4.
Table 4.
Frequency of cholangioscopic features of malignancy.
| Visual finding | All malignancies (n = 10) | Indeterminate biliary strictures (n = 8) | PSC (n = 2) |
|---|---|---|---|
| Vascular lakes (increased vascularity) | 9/10 | 7/8 | 2/2 |
| Irregular mucosa/nodularity | 6/10 | 5/8 | 1/2 |
| Luminal narrowing | 6/10 | 6/8 | 0/2 |
| Tumor vessel | 5/10 | 5/8 | 0/2 |
| Mucosal lesion | 4/10 | 2/8 | 0/2 |
PSC, primary sclerosing cholangitis.
Adverse events were seen in two cases (4%). Our complications included the following: (1) post-sphincterotomy bleeding, which resolved with epinephrine injection and stent placement for continued biliary drainage and tamponade of bleeding, and (2) post-procedural cholangitis. The first patient was admitted to the hospital for observation and hemoglobin monitoring as she was in her second trimester of pregnancy. She did not require any transfusions and was discharged 2 days later. The second patient was admitted to the hospital 2 days after his procedure with cholangitis, despite periprocedural antibiotics. He received intravenous (IV) antibiotics and was discharged without complications (Table 5).
Table 5.
Yield of diagnostic modalities in malignant biliary strictures.
| Visual impression | D-SOC biopsy | Brush cytology | |
|---|---|---|---|
| PSC – cholangiocarcinoma | 2/2 | 1/2 | 1/2 |
| Cholangiocarcinoma | 4/4 | 2/4 | 1/4 |
| Gallbladder carcinoma | 1/1 | 0/1 | 0/1 |
| Rectal cancer metastases | 1/1 | 0/1 | 1/1 |
| Biliary IPMN | 2/2 | 2/2 | n/a |
| 10/10 | 6/10 | 3/8 |
D-SOC, single-operator digital cholangioscope; IPMN, intraductal papillary mucinous neoplasm; n/a, not available; PSC, primary sclerosing cholangitis.
Discussion
Difficult bile duct stones and indeterminate biliary stricture evaluation were the most common indications for D-SOC in our study, consistent with other reported series.8–10 While balloon and basket stone extraction has a reported success rate of 86–95%,4 large stones (>15 mm), impacted stones, and stones located above biliary stricture reduce chances of success. Different modalities such as mechanical lithotripsy, large balloon papillary dilation, EHL, and laser lithotripsy (LL) have been traditionally employed for these types of stones. With the ease of setup and superior image quality, there has been a renewed interest in D-SOC for management of difficult CBD stones.
In the largest published D-SOC series of 407 patients with difficult stones, Brewer Gutierrez and colleagues11 reported an overall success rate of 97.3%, with ductal clearance achieved in 77.4% with a single session. Smaller series by Navaneethan and colleagues10 (n = 31) and Ogura and colleagues8 (n = 13) have reported 100% success.
Comparing with the older fiberoptic cholangioscopy, Mizrahi and colleagues9 reported 83% stone clearance with D-SOC using EHL compared to 58% with the older version.
When comparing EHL with LL, Brewer Gutierrez and colleagues11 reported 96.7% success with EHL and 99% with LL, but LL was shown to reduce procedure duration (49.9 versus 73.9 min on average).
Buxbaum and colleagues12 compared D-SOC with LL to mechanical lithotripsy without cholangioscopy for stones larger than 1 cm, and reported 93% success with LL compared with 67% with mechanical lithotripsy.
We report 90.47% success for ductal clearance in our series (19/21) by utilizing EHL in 16/21 cases. While this is lower than the other reported series of D-SOC, the two cases of incomplete clearance were older patients aged 93 and 90 years, one of whom is unlikely to return for repeat ERCP and has a fully covered metal biliary stent in place. The other patient is due to return for repeat ERCP.
Within the indeterminate biliary stricture and PSC surveillance groups, with the combined use of cholangioscopic exam, targeted biopsies, and brush cytology, we were able to differentiate malignant from benign strictures in all 22 cases, 9 of whom had underlying PSC.
Overall, we had greater success differentiating between malignant and benign strictures using cholangioscopic exam compared with targeted biopsies. The cholangioscopic findings that we found to be most suspicious with malignancy included an increase in vascularity or vascular lakes, irregular mucosa or nodularity, tumor vessels, and luminal narrowing, with similar findings reported in the literature (see images).4,6,10
Furthermore, targeted SpyBite biopsies outperformed brush cytology with higher sensitivity (60 versus 30%). The limited sensitivity of targeted biopsies may be related to inherent tumor characteristics, post-inflammatory (e.g. recent infection) or stent-related mucosal changes, and the absence of established guidelines for the sampling technique.
Recent studies of D-SOC have consistently shown that visual impression based on cholangioscopic views outperform D-SOC-directed biopsies when it comes to sensitivity in diagnosing benign versus malignant biliary strictures, while biopsy findings are more specific. Turowski and colleagues conducted a multicenter trial of D-SOC of 117 biliary stenosis cases suspicious for malignancy. Visual exam was found to be 95.5% sensitive and 94.5% specific in differentiating benign from malignant etiology, while D-SOC-guided biopsies had a sensitivity of 57.7% and a specificity of 100%.13 Ogura and colleagues8 performed D-SOC in 32 cases of indeterminate biliary stricture and 7 with focal bile duct wall thickness, and reported an overall accuracy of visual findings of 93%, with a sensitivity of 83% and a specificity of 89%, compared with an overall accuracy of 89% with forceps biopsies, with a sensitivity of 80% and a specificity of 100%. Navaneethan and colleagues conducted a multicenter study of D-SOC that included 44 cases of biliary strictures. They reported a sensitivity of 90% and a specificity of 95.8% for visual impression, compared with a relatively high sensitivity of 85% for biopsy with a specificity of 100%. They utilized an on-site cytopathologist which may explain the higher sensitivity of SOC-directed biopsies in differentiating benign and malignant biliary strictures.10
In 2011, Draganov and colleagues14 performed a prospective paired cohort study showing that SOC-guided biopsies with mini-forceps (SpyBite) had higher sensitivity and better accuracy compared with the traditional ERCP-based sampling techniques of cytology brushing and intraductal biopsy. Review of the literature and similar studies on SOC for the evaluation of indeterminate biliary strictures shows that visual assessment via SOC has a higher sensitivity for the diagnosis of malignancy compared with targeted biopsies and tissue diagnosis, but higher false positives (i.e. decreased specificity).3 In a retrospective cohort study of 88 patients, who underwent SOC for diagnostic and therapeutic reasons by Tieu and colleagues,15 they also found that most cancers were diagnosed based on visual appearance, rather than biopsy. Furthermore, a negative tissue diagnosis, in the setting of suspected malignancy based on clinical presentation and imaging, did not deter decision to pursue surgical exploration.15 However, it is also important to consider the costs and risks associated with unnecessary surgery for benign strictures. We did not have any false-positive cases in our series, and with superior image quality of D-SOC compared with the older fiberoptic version and with adequate training of endoscopists, it is less likely to happen.
In addition to the evaluation of indeterminate biliary strictures and management of choledocholithiasis, there are several ‘miscellaneous’ indications for which SOC has proven to be useful. A case series by Woo and colleagues16 showed that cholangioscopy-assisted guidewire placement in patients with anastomotic biliary strictures following living donor liver transplant (LDLT) was both well tolerated and useful when conventional methods were not successful. We had one case of choledocholithiasis in a patient with a history of LDLT and an anastomotic biliary stricture that failed conventional ERCP for which we successfully used D-SOC to visualize and fragment stones for clearance. We also utilized D-SOC via a percutaneous biliary sheath to perform EHL for stone fragmentation in a patient with altered anatomy due to prior Roux-en-Y gastric bypass surgery.17
Overall, the procedures in our study were well tolerated with a low rate of adverse events, and no procedure-related mortality. We encountered two complications (2/67, 0.03%) – a case of cholangitis and a post-sphincterotomy bleeding. Our procedure complication rate was similar to that seen in previous studies.4,5
While D-SOC equipment can be expensive, a cost analysis study done at two large hospitals in Belgium with the goal to estimate the economic impact of SOC for difficult stones and indeterminate strictures reported a reduction in the number of procedures by 27–31% and a decrease in costs by 5–11%.18 A majority of our cases had undergone prior unsuccessful conventional ERCPs and were able to achieve diagnostic or therapeutic success with D-SOC, thereby avoiding repeat ERCPs.
Study limitations
Our study had several limitations. It is a single-center, single-endoscopist study that analyzed 50 patients retrospectively. It did not include a control group to compare diagnostic and therapeutic success rates and adverse events. However, most of our findings regarding the utility of D-SOC, indications, and adverse events resemble other similar studies. In addition, with regard to the diagnosis of malignancy based on visual impression on cholangioscopy, there is no formal classification system or guidelines to eliminate subjective bias.
Future directions
Current D-SOC limitations include challenges with endoscopic access, whether it is because of altered anatomy or body habitus, and stone characteristics or location (e.g. intrahepatic stones, impacted stones). Furthermore, D-SOC-directed tissue sampling guidelines – size, number, and location of targeted biopsy samples that are considered sufficient to confidently assess indeterminate biliary lesions – and validated criteria for visual diagnosis of malignancy are not well established and further studies need to be done.5,19,20 What also remains a challenge is determining the appropriate biopsy location in individuals with preexisting biliary disease (e.g. PSC), post-inflammatory states, or post-biliary stenting, as they often have underlying mucosal abnormalities that may confound visual examination.5,20 Additional studies would be helpful to determine sampling guidelines and can improve the sensitivity of targeted biopsies in detecting malignancy.
In conclusion, digital cholangioscopy had a 100% success rate in differentiating malignant and benign etiologies of indeterminate strictures and 90.4% success in clearance of difficult biliary stones, with a low rate of adverse events. D-SOC for select indications leads to successful patient outcomes and reduced diagnostic delays, cost, and risks of repeat ERCPs. Widespread use of cholangioscopy remains limited due to a variety of factors including cost, endoscopic expertise/skill, and lack of clear indications or guidelines for its use. With newer generation cholangioscopes and further studies, this is likely to improve.
Footnotes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iDs: Stephanie Yan  https://orcid.org/0000-0002-7414-4432
https://orcid.org/0000-0002-7414-4432
Sooraj Tejaswi  https://orcid.org/0000-0001-6615-3155
https://orcid.org/0000-0001-6615-3155
Contributor Information
Stephanie Yan, Department of Internal Medicine, University of California Davis School of Medicine, Sacramento, CA, USA.
Sooraj Tejaswi, Division of Gastroenterology and Hepatology, Department of Internal Medicine, University of California Davis School of Medicine, Sacramento, CA, USA.
References
- 1. Lee JG. Brush cytology and the diagnosis of pancreaticobiliary malignancy during ERCP. Gastrointest Endosc 2006; 63: 78–80. [DOI] [PubMed] [Google Scholar]
- 2. Fritcher EG, Kipp BR, Halling KC, et al. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology 2009; 136: 2180–2186. [DOI] [PubMed] [Google Scholar]
- 3. Navaneethan U, Hasan MK, Lourdusamy V, et al. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: a systematic review. Gastrointest Endosc 2015; 82: 608.e2–614.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen YK, Parsi MA, Binmoeller KF, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc 2011; 74: 805–814. [DOI] [PubMed] [Google Scholar]
- 5. Ramchandani M, Reddy DN, Gupta R, et al. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: a single-center, prospective study. Gastrointest Endosc 2011; 74: 511–519. [DOI] [PubMed] [Google Scholar]
- 6. Woo YS, Lee JK, Oh SH, et al. Role of SpyGlass peroral cholangioscopy in the evaluation of indeterminate biliary lesions. Dig Dis Sci 2014; 59: 2565–2570. [DOI] [PubMed] [Google Scholar]
- 7. Manta R, Frazzoni M, Conigliaro R, et al. SpyGlass single-operator peroral cholangioscopy in the evaluation of indeterminate biliary lesions: a single-center, prospective, cohort study. Surg Endosc 2013; 27: 1569–1572. [DOI] [PubMed] [Google Scholar]
- 8. Ogura T, Imanishi M, Kurisu Y, et al. Prospective evaluation of digital single-operator cholangioscope for diagnostic and therapeutic procedures (with videos). Dig Endosc 2017; 29: 782–789. [DOI] [PubMed] [Google Scholar]
- 9. Mizrahi M, Khoury T, Wang Y, et al. ‘Apple Far from the Tree’: comparative effectiveness of fiberoptic single-operator cholangiopancreatoscopy (FSOCP) and digital SOCP (DSOCP). HPB 2018; 20: 285–288. [DOI] [PubMed] [Google Scholar]
- 10. Navaneethan U, Hasan MK, Kommaraju K, et al. Digital, single-operator cholangiopancreatoscopy in the diagnosis and management of pancreatobiliary disorders: a multicenter clinical experience (with video). Gastrointest Endosc 2016; 84: 649–655. [DOI] [PubMed] [Google Scholar]
- 11. Brewer Gutierrez OI, Bekkali NLH, Raijman I, et al. Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Clin Gastroenterol Hepatol 2018; 16: 918.e1–926.e1. [DOI] [PubMed] [Google Scholar]
- 12. Buxbaum J, Sahakian A, Ko C, et al. Randomized trial of cholangioscopy-guided laser lithotripsy versus conventional therapy for large bile duct stones (with videos). Gastrointest Endosc 2018; 87: 1050–1060. [DOI] [PubMed] [Google Scholar]
- 13. Turowski F, Hugle U, Dormann A, et al. Diagnostic and therapeutic single-operator cholangiopancreatoscopy with SpyGlassDS: results of a multicenter retrospective cohort study. Surg Endosc 2018; 32: 3981–3988. [DOI] [PubMed] [Google Scholar]
- 14. Draganov PV, Chauhan S, Wagh MS, et al. Diagnostic accuracy of conventional and cholangioscopy-guided sampling of indeterminate biliary lesions at the time of ERCP: a prospective, long-term follow-up study. Gastrointest Endosc 2012; 75: 347–353. [DOI] [PubMed] [Google Scholar]
- 15. Tieu AH, Kumbhari V, Jakhete N, et al. Diagnostic and therapeutic utility of SpyGlass® peroral cholangioscopy in intraductal biliary disease: single-center, retrospective, cohort study. Dig Endosc 2015; 27: 479–485. [DOI] [PubMed] [Google Scholar]
- 16. Woo YS, Lee JK, Noh DH, et al. SpyGlass cholangioscopy-assisted guidewire placement for post-LDLT biliary strictures: a case series. Surg Endosc 2016; 30: 3897–3903. [DOI] [PubMed] [Google Scholar]
- 17. Du L, D’Souza P, Thiesen A, et al. Percutaneous transhepatic cholangioscopy for indeterminate biliary strictures using the SpyGlass system: a case series. Endoscopy 2015; 47: 1054–1056. [DOI] [PubMed] [Google Scholar]
- 18. Deprez PH, Garces Duran R, Moreels T, et al. The economic impact of using single-operator cholangioscopy for the treatment of difficult bile duct stones and diagnosis of indeterminate bile duct strictures. Endoscopy 2018; 50: 109–118. [DOI] [PubMed] [Google Scholar]
- 19. Tamada K, Kurihara K, Tomiyama T, et al. How many biopsies should be performed during percutaneous transhepatic cholangioscopy to diagnose biliary tract cancer? Gastrointest Endosc 1999; 50: 653–658. [DOI] [PubMed] [Google Scholar]
- 20. Xie C, Aloreidi K, Patel B, et al. Indeterminate biliary strictures: a simplified approach. Expert Rev Gastroenterol Hepatol 2018; 12: 189–199. [DOI] [PubMed] [Google Scholar]