Key Points
Question
Is there evidence for the superiority of pharmacological, psychotherapeutic, or combination treatment in treating adults with posttraumatic stress disorder?
Findings
This network meta-analysis including 12 randomized clinical trials comprising 922 participants with 23 comparisons demonstrated similar findings for the 3 approaches at the end of treatment, but long-term benefits of psychotherapeutic and combined treatments were superior to pharmacological treatments across 6 randomized clinical trials that reported follow-up data.
Meaning
The available evidence is sparse and appears not to support the use of pharmacological therapy as first-line treatment for posttraumatic stress disorder; furthermore, this study suggests that direct comparisons reporting long-term outcomes for all 3 types of therapy are needed.
This network meta-analysis compared 12 randomized clinical trials comprising 992 patients to assess the short- and long-term outcomes of psychotherapy, pharmacotherapy, and combination therapies for adults with posttraumatic stress disorder.
Abstract
Importance
Posttraumatic stress disorder (PTSD) is a prevalent mental disorder, with a high risk of chronicity, comorbidity, and functional impairment; PTSD is complicated to treat, and the debate on the best treatment approach is ongoing.
Objective
To examine comparative outcomes and acceptability of psychotherapeutic and pharmacological treatments and their combinations in adults with PTSD.
Data Sources
Embase, MEDLINE, PsycINFO, Cochrane Controlled Trials Register, and PSYNDEX were searched for studies published from January 1, 1980, to February 28, 2018. Reference lists of included studies and of previously published guidelines and systematic reviews were also searched.
Study Selection
Of 11 417 records identified, 12 published randomized clinical trials (RCTs) comprising 922 participants, contributing 23 direct comparisons between psychotherapeutic and pharmacological treatments or their combinations were included.
Data Extraction and Synthesis
Standardized mean differences (SMDs) and odds ratios were aggregated using random-effects network and pairwise meta-analyses. Risk of bias and indirectness was rated for each study, and network confidence was rated using the Confidence in Network Meta-Analysis framework.
Main Outcomes and Measures
The primary outcome was the comparative benefit between 2 treatment approaches to PTSD symptom improvement, and secondary outcome was the comparative acceptability of the treatment approaches, as indicated by patient dropout rates before treatment termination.
Results
No treatment approach was found to be superior at the end of treatment (for all, 95% CI included 0). At the last follow-up, psychotherapeutic treatments showed greater benefit than pharmacological treatments in both network (SMD, −0.83; 95% CI, −1.59 to −0.07) and pairwise (SMD, −0.63; 95% CI, −1.18 to −0.09, 3 RCTs) meta-analyses. No difference was found between combined treatments and psychotherapeutic treatments at long-term follow-up, and combined treatments were associated with better outcomes than pharmacological treatments in the network meta-analysis (SMD, −0.96; 95% CI, −1.87 to −0.04), but not in the pairwise meta-analysis, which included 2 RCTs (SMD, −1.02; 95% CI, −2.77 to 0.72). No evidence was found for differential acceptability of the 3 treatment approaches.
Conclusions and Relevance
These results suggest superiority of psychotherapeutic treatments over pharmacological treatments; network, but not pairwise, meta-analyses suggest superiority of combined treatments over pharmacological treatments in improving PTSD symptom severity in the long term. The scarcity of reported long-term findings hampers definite conclusions and demonstrates the need for robust evidence from large-scaled comparative trials providing long-term follow-up data.
Introduction
Posttraumatic stress disorder (PTSD) is a highly debilitating mental disorder, which is characterized by psychological and behavioral symptoms including re-experiencing of the trauma, avoidance of stimuli associated with the trauma, negative alterations in cognitions and mood, as well as hyperarousal.1 The estimated lifetime prevalence of PTSD among adults is approximately 8%.2,3 Among the 10% to 20% of trauma survivors who develop PTSD,4 the disorder becomes chronic in many cases, leads to considerable disease burden as well as social and occupational impairment, and is associated with a high risk of psychiatric and medical comorbidity, substantial economic and societal costs, and increased risk of suicide.1,5,6,7,8,9
Several beneficial treatments for PTSD are available,10,11,12 including pharmacological treatments13 and a variety of different psychotherapeutic treatment approaches.14,15 A previous network meta-analysis reported that outcome differences between individual psychotherapeutic approaches (eg, cognitive behavioral therapy, prolonged exposure, seeking safety, and eye movement desensitization and reprocessing) are nonsignificant and mostly occur in underpowered studies.15 Accordingly, treatment guidelines typically recommend different types of trauma-focused psychotherapeutic treatments as first-line PTSD treatment.16,17,18,19,20,21 Concerning pharmacological therapies, however, recommendations are inconsistent.22 For instance, the American Psychological Association17 and the International Society for Traumatic Stress Studies16 recommend selective serotonin reuptake inhibitors as possible first-line treatment; but most guidelines, including those of the National Health and Medical Research Council21 and National Institute of Health and Care Excellence,18 conclude that pharmacological treatments should be used as second-line or adjuvant treatment, depending on severity, comorbidity, and patients’ response to psychotherapeutic treatment.22
When it comes to evaluations of the comparative outcomes between psychotherapeutic and pharmacological treatments, some relevant issues must be considered: First, the sustainability of PTSD treatment outcomes needs some attention.23 A meta-analysis comparing outcomes between psychotherapeutic and pharmacological treatments for depressive disorders found psychotherapeutic treatments to be superior to pharmacological treatments in the long term.24 In addition, a recent meta-analysis concerning PTSD showed that trauma-focused psychotherapeutic treatments had greater sustained benefit than pharmacological treatments when both were compared with control treatments.12 Second, previous systematic reviews reported a lack of direct comparisons between psychotherapeutic and pharmacological PTSD treatments.11,12,25,26,27 Accordingly, recent systematic reviews and meta-analyses have been largely based on indirect evidence from studies comparing either psychotherapeutic or pharmacological treatments with control treatments.11,12,26 Particularly when comparing such different treatment approaches as psychotherapeutic and pharmacological treatments, indirect evidence is considered highly problematic.26,28 But when focusing on direct evidence for the comparison between pharmacological and psychotherapeutic PTSD treatments, few studies had previously been identified (eg, a 2013 article by Cuijpers et al25 identified 2 comparative PTSD studies).25 Third, the current debate mainly focused on the comparison between psychotherapeutic and pharmacological monotherapies. Although combination or augmentation treatment strategies have been suggested as promising and exciting new developments,29 it remains uncertain whether benefit increases when combining pharmacological and psychotherapeutic treatments.30 Despite the widespread use of combined treatments in clinical practice, it has been reported repeatedly that systematic evaluations of their outcomes are lacking.26,31,32,33,34,35
We conducted a systematic review to identify all direct comparisons between psychotherapeutic and pharmacological treatments and their combinations in treating PTSD symptoms in adult trauma survivors. We summarized short- and long-term benefit data using network meta-analyses and pairwise meta-analyses.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline36 and was registered with the International prospective register of systematic reviews (PROSPERO identifier CRD42018109767).37
Identification of Studies
The systematic database search was set up in the context of previous 2 projects.14,38 We searched Embase, Medline, PsycINFO, Cochrane Controlled Trials Register, and PSYNDEX for studies published between January 1, 1980, and February 28, 2018 (eAppendix 1 in the Supplement). The search terms included free text as well as controlled vocabulary referring to the intervention, the population, and the type of study. The identification of studies for the present network meta-analysis took place between November 1, 2017, and March 31, 2018. In addition, we screened the references of included studies, all mentioned guidelines, systematic reviews, and meta-analyses11,25,26,27,31 for potentially relevant trials. If the database search identified trial registration records, we checked the corresponding trial register for published results. Two reviewers (J.M. and H.G.) independently screened the full texts of potentially relevant publications using a structured manual. Disagreements were resolved by consensus. The network meta-analyses were conducted between August 9, 2018, and October 3, 2018.
Selection Criteria
We included randomized clinical trials (RCTs) reporting comparisons between a psychotherapeutic and a pharmacological treatment or combinations of both with either treatment alone in reducing PTSD symptom severity in adults with PTSD. We defined psychotherapeutic treatments in line with previous work (eAppendix 2 in the Supplement).14,38 For combination psychotherapeutic and pharmacological treatments, we included combination treatments as well as add-on treatment designs, which started with 1 and added the second treatment later. Thus, an active PTSD treatment needed to be present as a comparator in the included studies. If a waiting list or a placebo control was included in a study in addition to the active comparator, we included the additional comparators in the network meta-analyses. We had no language restrictions, and we did not require studies to be double-blind for inclusion, because blinding of therapists and participants is not possible in the context of psychotherapy research.
Outcomes
Our primary outcome was PTSD symptom severity measured on a continuous validated scale. We assessed treatment outcomes immediately after treatment termination and long-term outcomes as indicated by the longest available follow-up assessment. For trials that used more than 1 PTSD scale, we used a predefined hierarchy, which gave precedence to more frequently used scales. Results from intention-to-treat analyses were preferred over results from per-protocol or completer analyses. As secondary outcome, we included the acceptability of PTSD treatments as indicated by patients dropping out of treatment before treatment termination. If no reasons for early termination were provided, we used the total dropout rates per group.
Data Collection
For the effect size calculation, we extracted sample sizes, means, and SDs for each treatment group. If these values were missing, other statistical data that could be converted into means and SDs were extracted. Conversions were calculated according to formulas provided (eg, by Lipsey and Wilson39 and Higgins and Green40). If the sample size was missing in the table of analysis, we used the sample size of the descriptive statistics. We contacted authors of 6 studies from which insufficient information was available. The authors of 1 study provided the relevant data on request.41 Studies were excluded if the missing outcome data could not be calculated, imputed, or obtained from the authors. For the calculation of odds ratios as indicators of treatment acceptability, we extracted the number of dropouts between beginning and end of treatment. If no dropout rates were reported, we used the difference between the number of patients at the beginning and at the end of treatment.
In addition to the data for effect size calculation, characteristics of the included population (eg, type of trauma, mean age of the study sample, PTSD diagnosis, comorbidity, and chronicity of PTSD symptoms), the intervention (eg, number of treatment sessions, dosage of pharmacological treatment), and the study (eg, year of publication) were coded. The Cochrane Risk of Bias (RoB) Assessment Tool was used to assess the quality of the included studies.40 In addition, we used the Confidence in Network Meta-Analysis (CINeMA) framework to assess the quality of the network across studies (a detailed description of rating RoB, indirectness, and network confidence is available in eAppendix 2 in the Supplement).42 Two independent raters (J.M. and H.G.) extracted all data on a standardized form (Microsoft Office Excel 2011) after intensive training in using the coding manual with operational descriptions of each item. Disagreements were solved by consensus.
Data Analysis
For the primary analyses, standardized mean differences (SMDs) between psychotherapeutic and pharmacological treatments and their combinations were calculated first with the end-of-treatment data, and second with the longest follow-up data separately. Negative SMDs indicate the superiority of psychotherapeutic over pharmacological treatments and the superiority of combination treatments over the individual monotherapies. The magnitude of SMD was interpreted as small (0.20 SD), moderate (0.5 SD), or large (0.80 SD).43 Odds ratios were calculated for the dropout rates between start and end of treatment; losses to follow-up were not considered. Odds ratios less than 1 indicate fewer dropouts with psychotherapeutic than with the pharmacological treatment and fewer dropouts with the combination treatment vs the individual monotherapies. We assumed 2-sided P < .05 to indicate statistical significance.
A network was created including 3 jointly randomizable treatments: first, psychotherapeutic PTSD treatments; second, pharmacological PTSD treatments; and third, combinations of psychotherapeutic and pharmacological PTSD treatments. Additional comparators that were present in the included studies (eg, waiting list controls and placebo controls) were included in the network (eAppendix 3 in the Supplement). We assumed that any patient who met all inclusion criteria was likely, in principle, to be randomized to any of the interventions in the synthesis comparator set. We addressed the assumption of transitivity in the network meta-analysis44 by first assessing whether the included interventions were similar across studies using a different design, and then checking whether the distribution of potential moderators was balanced across comparisons.45
We considered random-effects models rather than a fixed-effect model because we assumed that the included studies differed with respect to clinical and other factors. Pairwise SMDs were calculated for the 3 relevant comparisons. In addition, indirect evidence was estimated using the entire network of evidence. To conduct network meta-analyses within a frequentist framework, we used the package netmeta46 version 0.9-7 for the open-source software environment R, version 3.5.1 (R Foundation for Statistical Computing). The R function pairwise transformed the data set to the contrast-based format, which was needed for conducting the network meta-analysis. In addition, we conducted random-effects pairwise meta-analyses for the 3 relevant comparisons.
To reduce heterogeneity between studies, we prioritized the most frequent outcome in our analyses; self-rated outcome scales were used in these analyses only if observer-rated outcomes were not reported. However, because observer-reported outcomes have been shown to overestimate intervention outcomes in psychotherapy outcome research,47 we repeated our primary analyses with a preference for self-rated outcomes, using observer-rated measures only if no self-report scales were reported.
To express heterogeneity between studies, the Q statistic was used.48 Furthermore, τ2 was calculated to estimate variance between studies.49 For the primary outcome, a value of τ2 = 0.04 was considered as low heterogeneity, 0.09 as moderate, and 0.16 as high heterogeneity.50 In addition, we used I2 as an indicator of the amount of observed variance that could be attributed to between-study heterogeneity51 which can roughly be interpreted as follows: 0% to 40%, may not be important; 30% to 60%, may represent moderate heterogeneity; 50% to 90%, may represent substantial heterogeneity; and 75% to 100%, may represent considerable heterogeneity.50 In the network meta-analyses, we assumed a common estimate for the between-study heterogeneity variance across all included comparisons.
We used local as well as global methods to detect inconsistency in the network52 as follows: first locally, using the netsplit command (ie, splitting direct and indirect evidence), and second globally, using the decomp.design command (ie, using the design-by-treatment interaction model). We compared the magnitude of heterogeneity between consistency and inconsistency models to determine how much of the total heterogeneity was explained by inconsistency.
Owing to the small number of included studies, we did not conduct moderator analyses to explain observed heterogeneity. We conducted sensitivity analyses (eAppendix 4 in the Supplement), excluding studies with imputed SDs, studies with high indirectness ratings, studies with inadequate outcome assessment, and studies that reported only short-term findings to test the robustness of the observed results.
Results
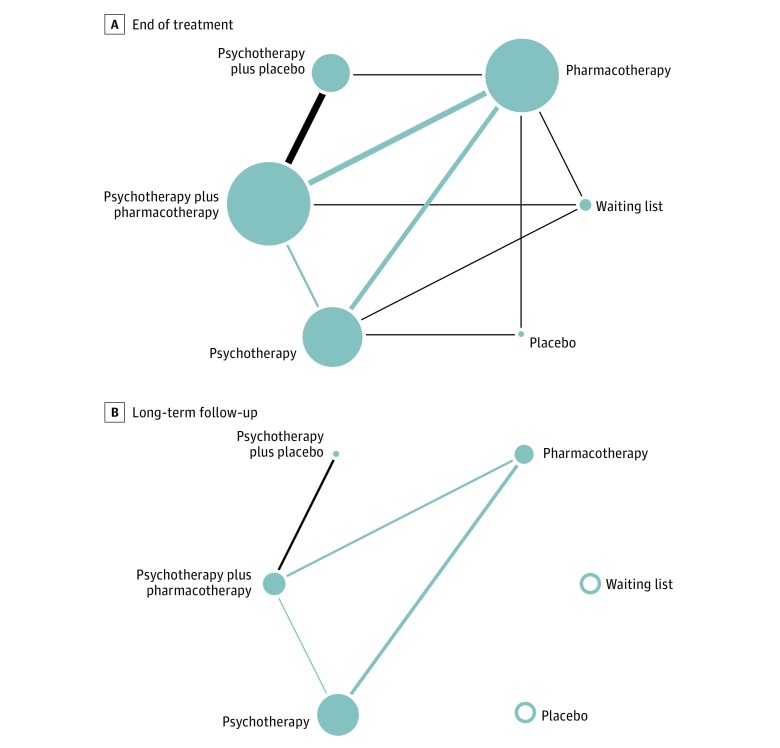
The systematic database search identified 11 416 records.14,38 After the initial screening of titles and abstracts, 46 full-text articles were considered potentially relevant. Twelve published RCTs41,53,54,55,56,57,58,59,60,61,62,63,64 with a total of 922 participants were included in our analyses (eFigure 1 in the Supplement). One study was published in Chinese61 the remaining studies were published in English. For our network meta-analyses at the end of treatment, we used all 12 included studies with 23 comparisons (Figure 1A). Six studies contributed data for the long-term analysis (Figure 1B)41,54,55,56,61,62 The studies that reported only short-term data and those that reported long-term data as well were comparable with respect to most assessed clinical and methodological characteristics (Table; eTable 1 and eTable 2 in the Supplement); only treatment duration appeared somewhat shorter in the studies that provided long-term data compared with the studies that reported short-term data only.
Figure 1. Network of Included Comparisons at the End of Treatment and Follow-up.
The size of the nodes indicates the number of participants per treatment approach. Empty circles indicate the absence of the respective treatment in the network. The thickness of the edges represents the number of comparisons between 2 treatment approaches. Gray lines indicate the 3 comparisons of interest.
Table. Relevant Characteristics of All 12 RCTs Included in the Network Meta-analysis.
| Source | Interventions (No. of Patients Allocated) | Baseline Score, Mean (SD)a | PTSD Severity Measure | Treatment Duration: Weeks/No. of Sessions | Medication Dose, Mean, mg | Dropouts | Trauma Type | Age, Mean, y | Female Sex, % | Blinded Outcome Assessment | Included in Pairwise Meta-analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Trials With Short-term Data Only | |||||||||||
| Buhmann et al,53 2016 | CBT (70) | 3.3 (0.5) | HTQ | 24/12b | NA | 11 | Refugees with mixed trauma | 45.0 | 41.0c | Adequate | A, B, C |
| Sertraline (71) | 3.3 (0.5) | 24/9b | 132.1 | 8 | |||||||
| CBT + sertraline (71) | 3.2 (0.6) | 24/9b + 12b | 132.1 | 10 | |||||||
| Waiting list (68) | 3.3 (0.5) | 24 | NA | 18 | |||||||
| Oehen et al,57 2013 | MDMA + psychotherapy (9) | 66.4 (13.6) | CAPS | NA/3 + 12 | 125.0 + 62.5 | 11 | Mixed trauma | 41.4 | 83.0c | Adequate | NA |
| Active placebo + psychotherapy (5) | 63.4 (7.9) | PDS | NA/3 + 12 | 25.0 + 12.5 | 1 | ||||||
| Rauch et al,64 2018 | Sertraline (71) | 75.5 (15.0) | CAPS | 24 | 25.0 | 13 | Veterans (OEF/OIF/OND) | 34.5 | 13.0 | Unclear | B |
| PE + sertraline (69) | 76.0 (14.2) | 24/13 | 25.0 | 28 | |||||||
| PE + pill placebo (67) | 80.9 (13.2) | 24/13 | NA | 31 | |||||||
| Rothbaum et al,58 2006 | Sertraline + augmentation with PE (34) | 16.1 (10.64) | SIP | 5/2 + 10 | 173.1 | 6 | Mixed trauma | 39.3 | 64.6 | Adequate | C |
| Sertraline (31) | 14.5 (11.65) | 5/2 | 173.1 | 1 | |||||||
| Schneier et al,59 2012 | PE + Paroxetine (19) | 72.6 (12.9) | CAPS | 10/10 + 8 | 32.2 | 6 | Survivors of terrorist attack (World Trade Center 2001) | 50.2 | 54.1 | Adequate | NA |
| PE + pill placebo (18) | 65.4 (12.8) | 10/10 + 8 | 36.8 | 5 | |||||||
| Simon et al,60 2008 | PE + augmentation with paroxetine (11) | 16.1 (8.99) | SPRINT | 10/6 + 5 | 45.8g | 3 | Mixed trauma | 45.6 | 56.0c | Adequate | NA |
| PE + augmentation with placebo (14) | 17.0 (7.65) | 10/6 + 5 | 44.8 | 2 | |||||||
| Trials With Short-term and Long-term Data | |||||||||||
| Frommberger et al,54 2004d | CBT (10) | 70.5 (7.2) | CAPS | 12/12 | 28.0 | 2 | Survivors of serious unintentional injury and sexual or nonsexual violence | 42.7 | 57.1 | Inadequate | A |
| Paroxetine (11) | 65.0 (13.4) | PSS | 12/12 | NA | 3 | ||||||
| Hien et al,55 2015d | Seeking safety + sertraline (32) | 65.5 (20.3) | CAPS | 12/12 | 50.0-200.0 | 4 | Mixed trauma | 42.4 | 81.2 | Adequate | NA |
| Seeking safety + placebo (37) | 59.5 (18.97) | 12/12 | NA | 8 | |||||||
| Mithoefer et al,56 2011e | MDMA + psychotherapy (15) | 79.2 (23.6) | CAPS | NA/2 + 8 | 125.0 (+ 62.5) | 2 | Mixed trauma | 40.4 | 85.0c | Adequate | NA |
| Pill placebo + psychotherapy (8) | 79.6 (22.0) | IES-R | NA/2 + 8 | 125.0 (+ 62.5) | 0 | ||||||
| Popiel et al,41 2015f | PE (114) | 32.6 (9.7) | PDS | 12/10 to 12 | NA | 25 | Survivors of motor vehicle collisions | 37.7 | 76.3 | Adequate | A, B, C |
| Paroxetine (57) | 34.9 (8.42) | 12/5 | 20.0 | 34 | |||||||
| PE + Paroxetine (57) | 31.5 (9.76) | 12/15 to 17 | 20.0 | 31 | |||||||
| Su et al,61 2007g | ET + fluoxetine (10) | 16.5 (2.97) | PCL | 12/7 | NA | 0 | NA | 29.0 | 60.0 | Adequate | C |
| Fluoxetine (10) | 17.6 (2.97) | 12/NA | NA | 0 | |||||||
| van der Kolk et al,62 2007f | EMDR (29) | 69.4 (12.07) | CAPS | 8/8 | NA | 5 | Mixed trauma | 36.1 | 83.0 | Adequate | A |
| Fluoxetine (30) | 73.7 (13.4) | 8/8 | 30.0 | 4 | |||||||
| Pill placebo (29) | 70.3 (13.0) | 8/NA | NA | 3 | |||||||
Abbreviations: A, studies included in the pairwise meta-analysis between psychotherapeutic and pharmacological treatment; B, studies included in the pairwise meta-analysis on the combination treatment compared with psychotherapeutic treatment; C, studies included in the pairwise meta-analysis on the combined treatment compared with pharmacological treatments; CAPS, Clinician Administered PTSD Scale67; CBT, cognitive behavioral therapy; EMDR, eye movement desensitization and reprocessing; ET, exposure therapy; HTQ, Harvard Trauma Questionnaire68; IES-R, Impact of Event Scale-Revised69; MDMA, 3,4-methylenedioxymethamphetamine; NA, not applicable; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OND, Operation New Dawn; PCL, PTSD Checklist70; PDS, Posttraumatic Diagnostic Scale71; PE, prolonged exposure therapy; PTSD, posttraumatic stress disorder; PSS, Posttraumatic Stress Scale72; SIP, Structured Interview for PTSD73; RCT, randomized clinical trial; SPRINT, short PTSD rating interview.74
No significant differences were found between baseline scores in a network meta-analysis.
Mean number of treatment sessions.
Data are only available for participants who completed the treatment: 20 in Mithoefer et al56; 12 in Oehen et al57; 23 in Simon et al60; and 128 in Buhmann et al.53
Participants could choose to continue medication after the end of treatment until follow-up assessment.
Pharmacological treatment was ended but participants were offered 1 additional medication session.
Participants discontinued pharmacological treatment during a 2-week period.
No information regarding medication continuation between end of treatment and follow-up.
Risk of bias was considered low in 3 studies, moderate in 8, and high in 1 (eTable 1 in the Supplement). The network meta-analyses relied mostly on evidence with moderate RoB and with low to moderate indirectness (eFigures 2 and 3 in the Supplement). The only study with high RoB reported both short- and long-term data. Confidence in the network meta-analyses was considered high for all 3 relevant comparisons at the end of treatment and moderate to high at follow-up (eTable 3 in the Supplement).
Short-term Findings
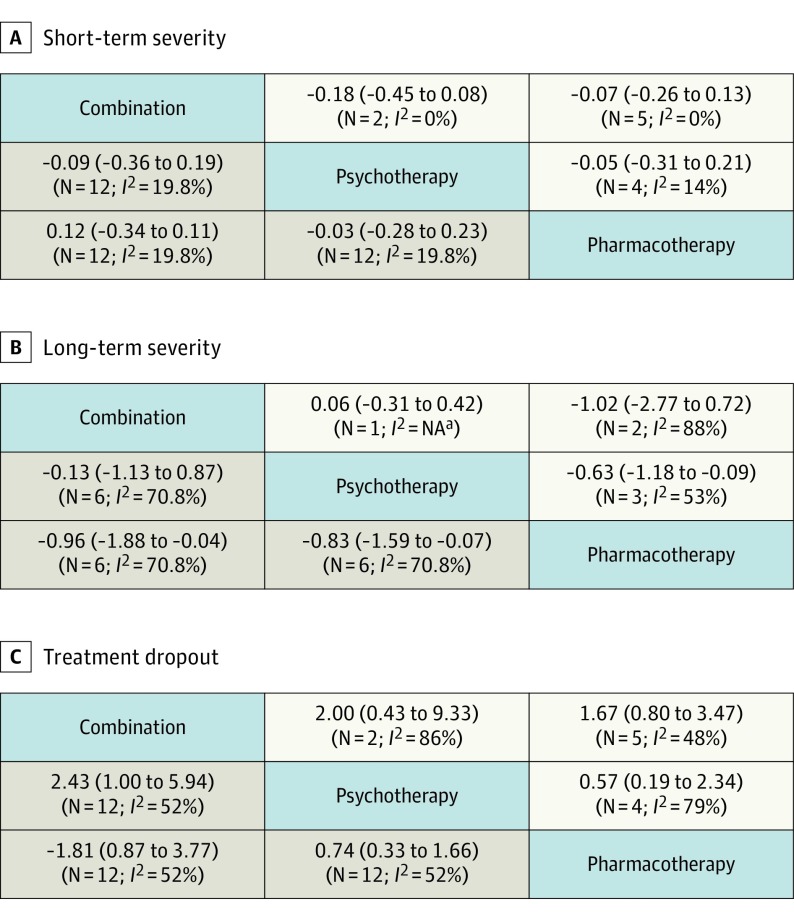
At the end of treatment, the comparative benefit between pharmacological and psychotherapeutic treatments and their combinations showed no significant superiority of any treatment approach (Figure 2A). The amount of overall heterogeneity in the analysis was small (τ2 = 0.02). We found no indication of inconsistency either within (Q = 9.58; df = 5; P = .09) or between (Q = 5.37; df = 7; P = .61) designs. Sensitivity analyses confirmed the robustness of the SMDs and contributed to explaining heterogeneity and inconsistency (eTable 4 in the Supplement). Pairwise meta-analyses confirmed the lack of superiority of either approach at the end of treatment (Figure 2A) (eAppendix 5 in the Supplement). Heterogeneity was low in all 3 pairwise comparisons (all, τ2<0.02).
Figure 2. Comparative Outcomes and Acceptability.
Results on the comparative benefit and acceptability from network meta-analyses (gray) and pairwise meta-analyses (white). To make network and pairwise meta-analysis results directly comparable, estimates are presented as column vs row for the network meta-analyses, and row vs column for the pairwise meta-analyses. A and B illustrate standardized mean difference (SMD) (95% CI); C, odds ratio (OR) (95% CI). Standardized mean differences less than 0 and ORs less than 1 indicate superiority of psychotherapy over pharmacological treatment and of combined treatment over either approach alone. NA indicates not applicable.
aNo I2 statistic could be estimated because no meta-analysis could be performed (ie, only 1 study was available).
Long-term Findings
At the longest available follow-up, psychotherapeutic treatments were significantly more beneficial than pharmacological treatments (SMD, −0.83; 95% CI, −1.59 to −0.07) and the combined treatments were slightly but not significantly superior to psychotherapeutic treatment alone (SMD, −0.13; 95% CI, −1.12 to 0.87), but the combined treatments were significantly more beneficial than pharmacological treatments alone (SMD, −0.96; 95% CI, −1.87 to −0.04) (Figure 2B). At the last available follow-up, we found high overall heterogeneity (τ2 = 0.33). This finding was mainly explained by inconsistency between designs (Q = 10.64; df = 2; P = .005). After detaching single designs in the full design-by-treatment interaction model inconsistency was reduced but still significant (τ2 = 0.11; Q = 6.04; df = 2; P = .05). Sensitivity analyses confirmed the magnitude of the SMDs but did not explain heterogeneity or inconsistency (eTable 4 in the Supplement). The pairwise meta-analyses (Figure 2B) confirmed the statistically significant superiority of psychotherapeutic over pharmacological treatments at the last available follow-up (SMD, −0.63; 95% CI, −1.18 to −0.09), as well as a large but nonsignificant benefit of combined treatments over pharmacological treatment alone (SMD, −1.02; 95% CI, −2.77 to 0.72). No significant difference between psychotherapeutic and combined treatments was reported in 1 pairwise comparison (SMD, 0.06; 95% CI, −0.31 to 0.42). Heterogeneity was moderate to large in the pairwise meta-analyses at the last available follow-up.
Findings Favoring Self-reported Outcomes
The network meta-analysis favoring self-reported short-term outcomes confirmed the findings based on the preference for observer-rated outcomes with an SMD of −0.10 (95% CI, −0.39 to 0.18) in favor of psychotherapeutic over pharmacological treatments, an SMD of −0.04 (95% CI, −0.35 to 0.26) for the comparisons between combination treatment and psychotherapeutic treatment, and an SMD of −0.14 (95% CI, −0.39 to 0.10) in favor of the combination treatment over pharmacological treatment (eTable 4 in the Supplement).
The network meta-analysis favoring self-reported long-term outcomes confirmed the findings based on the preference for observer-rated outcomes with an SMD of −0.84 (95% CI, −1.57 to −0.11) in favor of psychotherapeutic over pharmacological treatments, an SMD of −0.11 (95% CI, −1.06 to 0.84) for the comparisons between combination treatment and psychotherapeutic treatment, and an SMD of −0.95 (95% CI, −1.83 to −0.07) in favor of the combination treatment over pharmacological treatment (eTable 4 in the Supplement).
Acceptability
With respect to the comparative acceptability of the 3 treatment approaches, we found slightly lower dropout rates in psychotherapeutic treatments than in the pharmacological and combined treatments, but the differences were not statistically significant, because all 95% CIs included 1.00. The detailed data are presented in Figure 2C. We found evidence for between-study heterogeneity (τ2 = 0.40), and for inconsistency; in particular, estimates significantly differed between designs (Q = 21.90; df = 7; P = .003). The pairwise meta-analyses confirmed the results from our network meta-analysis (Figure 2C). Again, heterogeneity was observed in all 3 comparisons (all, τ2>0.29).
Discussion
Our meta-analytic study addresses the comparative benefit and acceptability of psychotherapeutic and pharmacological PTSD treatments and their combinations in adult trauma survivors. Our results indicate that there is no superiority of any treatment approach at the end of treatment; however, we found evidence for the superiority of psychotherapeutic over pharmacological treatments, and of combined treatments over pharmacological treatments alone at the last available follow-up. With regard to treatment acceptability, we did not find significant differences between the 3 treatment approaches. This finding diverged from previous meta-analyses showing a significantly higher dropout rate for pharmacological compared with psychotherapeutic treatments.65,66
Our results confirm the recommendations of many treatment guidelines, that psychotherapeutic treatments should be preferred as first-line treatments,22 and we found limited evidence to recommend pharmacological treatments as monotherapies, when sustained and long-term symptom improvement is intended. For the superiority of the combination of psychotherapeutic and pharmacological treatments over pharmacological treatment alone, we found some evidence: both meta-analytic approaches showed large SMDs in favor of the combined treatment; but owing to low power, the findings were not statistically significant in the pairwise meta-analysis. Thus, our study reflects the advantage of network meta-analysis compared with pairwise meta-analysis in achieving greater precision of treatment benefit estimates owing to a formal combination of direct and indirect evidence in a single analysis. The resulting increase in statistical power is especially relevant when few studies are available for each of a number of possible comparisons, as in the present study.
The differences in findings at the end of treatment and at long-term follow-up highlight the necessity to include long-term follow-up data when evaluating the comparative benefit of treatments, because the treatment outcomes at the end of treatment may differ fundamentally from long-term findings. Thus, focusing on results at the end of treatment and founding treatment recommendations on short-term data only, as done for instance in previous meta-analyses,25 may lead to false conclusions.
This is the first meta-analysis to our knowledge to combine the available evidence on the comparative benefit between psychotherapeutic and pharmacological PTSD treatments and their combinations in a single analysis. Previous meta-analyses mainly relied on indirect comparisons, which are particularly problematic when comparing 2 diverging treatment approaches across studies, such as psychotherapies and pharmacotherapies. Here, differences in methodology could be profound, for instance in blinding of participants, personnel, and outcome assessors.11,26,27 Accordingly, we did not include 2-arm comparisons between psychotherapeutic treatment and waiting list control patients or between pharmacological treatments and placebos, because they have been shown to lead to overestimations of the active treatment benefits75,76,77,78,79 and would not add much new information to what is already known from previous meta-analyses on indirect comparisons. Thus, the inclusion of comparative studies only, but studies on all 3 different treatment approaches (ie, psychotherapeutic and pharmacological treatments as well as their combinations) at once in 1 network meta-analysis constitutes a relevant advantage compared with the existing meta-analyses.
Limitations
Our study has some limitations. First, we identified few (12) comparative RCTs for the short-term analyses, and fewer (6) RCTs for our long-term analyses. Although this limited evidence showed consistent results in the short term, conclusions are constrained with respect to long-term findings. Second, we combined psychotherapeutic as well as pharmacological treatments and the combined treatments each in 1 node. This approach was chosen because previous network meta-analyses reported only nonsignificant differences between the included psychotherapeutic treatment approaches (ie, cognitive behavioral therapy, prolonged exposure, seeking safety, and eye movement desensitization and reprocessing),14 as well as between the 3 selective serotonin reuptake inhibitors that were used as monotherapies in our included studies (ie, paroxetine hydrochloride, fluoxetine hydrochloride, and sertraline hydrochloride).13 Nevertheless, the combined nodes may have contributed to heterogeneity and inconsistency. However, at the end of treatment, indicators of heterogeneity and inconsistency were small, and only in the long-term data did we find significant heterogeneity and inconsistency. The identified substantial superiority of psychotherapeutic over pharmacological PTSD treatments in our network meta-analysis might be overestimated and must be confirmed by high-quality direct comparison studies. For the moment, the statistically and clinically80 significant moderate superiority based on the pairwise meta-analysis with moderate heterogeneity appears more valid. Third, the included studies varied in several dimensions. The observed heterogeneity between studies was very small at the end of treatment in the pairwise meta-analyses, indicating that the observed variations were not associated with treatment outcome. In addition, we conducted several sensitivity analyses, which confirmed the robustness of the reported pattern of findings. Nevertheless, particularly our less-consistent long-term findings await confirmation from large-scale comparative RCTs preferably including all 3 treatment approaches and reporting long-term data.
Conclusions
Despite the relatively small number of identified studies, our meta-analyses suggest a consistent pattern of equivalent treatment at the end of treatment across a number of sensitivity analyses including self-reported and observer-reported outcomes, and suggest that no urgent need for further evidence on short-term outcomes. But, to our knowledge, our meta-analyses using long-term data are the first to empirically confirm the typical recommendation of psychotherapeutic treatments as first-line treatments. Based on a comprehensive aggregation of all available direct comparisons, our results suggest clinically significant inferiority of pharmacological monotherapies in the long term. The evidence base for long-term outcomes, however, was unsatisfactory, with few direct comparison studies, and most studies being underpowered.
eAppendix 1. Search Terms
eAppendix 2. Addition to Methods
eAppendix 3. Additional Results (Main Analyses)
eAppendix 4. Sensitivity Analyses
eAppendix 5. Pairwise Meta-analyses
eFigure 1. Flowchart
eFigure 2. Risk of Bias Assessment
eFigure 3. Indirectness
eTable 1. Risk of Bias for Each Included Study
eTable 2. Indirectness for Each Included Study
eTable 3. Confidence in Network Meta-analysis (CINEMA) Rating
eTable 4. Comparisons of Results Across Different Network Models
References
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.de Vries G-J, Olff M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. J Trauma Stress. 2009;22(4):259-267. doi: 10.1002/jts.20429 [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169-184. doi: 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norris FH, Slone LB. The epidemiology of trauma and PTSD In: Friedman MJ, Keane TM, Resick PA, eds. Handbook of PTSD: Science and Practice. New York: Guilford Press; 2007:78-98. [Google Scholar]
- 5.Frayne SM, Seaver MR, Loveland S, et al. Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med. 2004;164(12):1306-1312. doi: 10.1001/archinte.164.12.1306 [DOI] [PubMed] [Google Scholar]
- 6.Krysinska K, Lester D. Post-traumatic stress disorder and suicide risk: a systematic review. Arch Suicide Res. 2010;14(1):1-23. doi: 10.1080/13811110903478997 [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(suppl 5):4-12. [PubMed] [Google Scholar]
- 8.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- 9.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655-679. doi: 10.1016/j.euroneuro.2011.07.018 [DOI] [PubMed] [Google Scholar]
- 10.Stein DJ, Cloitre M, Nemeroff CB, et al. Cape Town consensus on posttraumatic stress disorder. CNS Spectr. 2009;14(1)(suppl 1):52-58. [PubMed] [Google Scholar]
- 11.Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiatry. 2013;74(6):e541-e550. doi: 10.4088/JCP.12r08225 [DOI] [PubMed] [Google Scholar]
- 12.Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016;33(9):792-806. doi: 10.1002/da.22511 [DOI] [PubMed] [Google Scholar]
- 13.Cipriani A, Williams T, Nikolakopoulou A, et al. Comparative efficacy and acceptability of pharmacological treatments for post-traumatic stress disorder in adults: a network meta-analysis. Psychol Med. 2018;48(12):1975-1984. doi: 10.1017/S003329171700349X [DOI] [PubMed] [Google Scholar]
- 14.Gerger H, Munder T, Gemperli A, et al. Integrating fragmented evidence by network meta-analysis: relative effectiveness of psychological interventions for adults with post-traumatic stress disorder. Psychol Med. 2014;44(15):3151-3164. doi: 10.1017/S0033291714000853 [DOI] [PubMed] [Google Scholar]
- 15.Frost ND, Laska KM, Wampold BE. The evidence for present-centered therapy as a treatment for posttraumatic stress disorder. J Trauma Stress. 2014;27(1):1-8. doi: 10.1002/jts.21881 [DOI] [PubMed] [Google Scholar]
- 16.Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd ed New York, NY: Guilford Press; 2009. [Google Scholar]
- 17.American Psychological Association Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. https://www.apa.org/about/offices/directorates/guidelines/ptsd.pdf. Published February 24, 2017. Accessed May 2, 2019.
- 18.National Institute for Health and Care Excellence Post-traumatic stress disorder: management. 2005; https://www.nice.org.uk/guidance/cg26. [PubMed]
- 19.Institute of Medicine Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC: National Academies Press; 2008. [Google Scholar]
- 20.World Health Organization Guidelines for the management of conditions specifically related to stress. 2013; https://www.who.int/mental_health/emergencies/stress_guidelines/en/. [PubMed]
- 21.Forbes D, Creamer M, Phelps A, et al. Australian guidelines for the treatment of adults with acute stress disorder and post-traumatic stress disorder. Aust N Z J Psychiatry. 2007;41(8):637-648. doi: 10.1080/00048670701449161 [DOI] [PubMed] [Google Scholar]
- 22.Forbes D, Creamer M, Bisson JI, et al. A guide to guidelines for the treatment of PTSD and related conditions. J Trauma Stress. 2010;23(5):537-552. doi: 10.1002/jts.20565 [DOI] [PubMed] [Google Scholar]
- 23.Stein DJ, Ipser J, McAnda N. Pharmacotherapy of posttraumatic stress disorder: a review of meta-analyses and treatment guidelines. CNS Spectr. 2009;14(1)(suppl 1):25-31. [PubMed] [Google Scholar]
- 24.Imel ZE, Malterer MB, McKay KM, Wampold BE. A meta-analysis of psychotherapy and medication in unipolar depression and dysthymia. J Affect Disord. 2008;110(3):197-206. doi: 10.1016/j.jad.2008.03.018 [DOI] [PubMed] [Google Scholar]
- 25.Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF III. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. 2013;12(2):137-148. doi: 10.1002/wps.20038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huhn M, Tardy M, Spineli LM, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry. 2014;71(6):706-715. doi: 10.1001/jamapsychiatry.2014.112 [DOI] [PubMed] [Google Scholar]
- 27.Jonas DE, Cusack K, Forneris CA, et al. Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). AHRQ Comparative Effectiveness Reviews. 2013;92. https://www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed]
- 28.Linde K, Rücker G, Schneider A, Kriston L. Questionable assumptions hampered interpretation of a network meta-analysis of primary care depression treatments. J Clin Epidemiol. 2016;71:86-96. doi: 10.1016/j.jclinepi.2015.10.010 [DOI] [PubMed] [Google Scholar]
- 29.Pratchett LC, Daly K, Bierer LM, Yehuda R. New approaches to combining pharmacotherapy and psychotherapy for posttraumatic stress disorder. Expert Opin Pharmacother. 2011;12(15):2339-2354. doi: 10.1517/14656566.2011.604030 [DOI] [PubMed] [Google Scholar]
- 30.Pull CB. Combined pharmacotherapy and cognitive-behavioural therapy for anxiety disorders. Curr Opin Psychiatry. 2007;20(1):30-35. doi: 10.1097/YCO.0b013e3280115e52 [DOI] [PubMed] [Google Scholar]
- 31.Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2010;7(7):CD007316. doi: 10.1002/14651858.CD007316.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stewart CL, Wrobel TA. Evaluation of the efficacy of pharmacotherapy and psychotherapy in treatment of combat-related post-traumatic stress disorder: a meta-analytic review of outcome studies. Mil Med. 2009;174(5):460-469. doi: 10.7205/MILMED-D-04-1507 [DOI] [PubMed] [Google Scholar]
- 33.Black DW. Efficacy of combined pharmacotherapy and psychotherapy versus monotherapy in the treatment of anxiety disorders. CNS Spectr. 2006;11(10)(suppl 12):29-33. doi: 10.1017/S1092852900025827 [DOI] [PubMed] [Google Scholar]
- 34.Marshall RD, Cloitre M. Maximizing treatment outcome in post-traumatic stress disorder by combining psychotherapy with pharmacotherapy. Curr Psychiatry Rep. 2000;2(4):335-340. doi: 10.1007/s11920-000-0078-3 [DOI] [PubMed] [Google Scholar]
- 35.Kuzma JM, Black DW. Integrating pharmacotherapy and psychotherapy in the management of anxiety disorders. Curr Psychiatry Rep. 2004;6(4):268-273. doi: 10.1007/s11920-004-0076-y [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gerger H, Merz J Comparative efficacy and acceptability of pharmacological and psychological treatments and their combination for adults with posttraumatic stress disorder: a network meta-analysis. PROSPERO International Prospective Register of Systematic Reviews. 2018. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=109767.
- 38.Gerger H, Munder T, Barth J. Specific and nonspecific psychological interventions for PTSD symptoms: a meta-analysis with problem complexity as a moderator. J Clin Psychol. 2014;70(7):601-615. doi: 10.1002/jclp.22059 [DOI] [PubMed] [Google Scholar]
- 39.Lipsey MW, Wilson DB. Practical Meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 40.Higgins JPT, Green S Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 ed. http://www.cochrane-handbook.org. Updated March 2011. Accessed May 2, 2019.
- 41.Popiel A, Zawadzki B, Pragłowska E, Teichman Y. Prolonged exposure, paroxetine and the combination in the treatment of PTSD following a motor vehicle accident. A randomized clinical trial—the “TRAKT” study. J Behav Ther Exp Psychiatry. 2015;48:17-26. doi: 10.1016/j.jbtep.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 42.Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLoS One. 2014;9(7):e99682. doi: 10.1371/journal.pone.0099682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 44.Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods. 2012;3(2):80-97. doi: 10.1002/jrsm.1037 [DOI] [PubMed] [Google Scholar]
- 45.Jansen JP, Naci H. Is network meta-analysis as valid as standard pairwise meta-analysis? it all depends on the distribution of effect modifiers. BMC Med. 2013;11:159. doi: 10.1186/1741-7015-11-159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rücker G, Schwarzer G, Krahn U, König J netmeta: Network meta-analysis using frequentist methods. R package version 0.9-8. 2018. https://CRAN.R-project.org/package=netmeta.
- 47.Cuijpers P, Li J, Hofmann SG, Andersson G. Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: a meta-analysis. Clin Psychol Rev. 2010;30(6):768-778. doi: 10.1016/j.cpr.2010.06.001 [DOI] [PubMed] [Google Scholar]
- 48.Cochran WG. The comparison of percentages in matched samples. Biometrika. 1950;37(3-4):256-266. doi: 10.1093/biomet/37.3-4.256 [DOI] [PubMed] [Google Scholar]
- 49.Higgins JP. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37(5):1158-1160. doi: 10.1093/ije/dyn204 [DOI] [PubMed] [Google Scholar]
- 50.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-analysis. Chichester, UK: John Wiley & Sons; 2009. doi: 10.1002/9780470743386 [DOI] [Google Scholar]
- 51.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Efthimiou O, Debray TP, van Valkenhoef G, et al. ; GetReal Methods Review Group . GetReal in network meta-analysis: a review of the methodology. Res Synth Methods. 2016;7(3):236-263. doi: 10.1002/jrsm.1195 [DOI] [PubMed] [Google Scholar]
- 53.Buhmann CB, Nordentoft M, Ekstroem M, Carlsson J, Mortensen EL. The effect of flexible cognitive-behavioural therapy and medical treatment, including antidepressants on post-traumatic stress disorder and depression in traumatised refugees: pragmatic randomised controlled clinical trial. Br J Psychiatry. 2016;208(3):252-259. doi: 10.1192/bjp.bp.114.150961 [DOI] [PubMed] [Google Scholar]
- 54.Frommberger U, Stieglitz RD, Nyberg E, et al. Comparison between paroxetine and behaviour therapy in patients with posttraumatic stress disorder (PTSD): a pilot study. Int J Psychiatry Clin Pract. 2004;8(1):19-23. doi: 10.1080/13651500310004803 [DOI] [PubMed] [Google Scholar]
- 55.Hien DA, Levin FR, Ruglass LM, et al. Combining seeking safety with sertraline for PTSD and alcohol use disorders: a randomized controlled trial. J Consult Clin Psychol. 2015;83(2):359-369. doi: 10.1037/a0038719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Doblin R. The safety and efficacy of +/−3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study. J Psychopharmacol. 2011;25(4):439-452. doi: 10.1177/0269881110378371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oehen P, Traber R, Widmer V, Schnyder U. A randomized, controlled pilot study of MDMA (± 3,4-methylenedioxymethamphetamine)-assisted psychotherapy for treatment of resistant, chronic post-traumatic stress disorder (PTSD). J Psychopharmacol. 2013;27(1):40-52. doi: 10.1177/0269881112464827 [DOI] [PubMed] [Google Scholar]
- 58.Rothbaum BO, Cahill SP, Foa EB, et al. Augmentation of sertraline with prolonged exposure in the treatment of posttraumatic stress disorder. J Trauma Stress. 2006;19(5):625-638. doi: 10.1002/jts.20170 [DOI] [PubMed] [Google Scholar]
- 59.Schneier FR, Neria Y, Pavlicova M, et al. Combined prolonged exposure therapy and paroxetine for PTSD related to the World Trade Center attack: a randomized controlled trial. Am J Psychiatry. 2012;169(1):80-88. doi: 10.1176/appi.ajp.2011.11020321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Simon NM, Connor KM, Lang AJ, et al. Paroxetine CR augmentation for posttraumatic stress disorder refractory to prolonged exposure therapy. J Clin Psychiatry. 2008;69(3):400-405. doi: 10.4088/JCP.v69n0309 [DOI] [PubMed] [Google Scholar]
- 61.Su H, Wang JT, Lou ZS, Lu HT. Cognitive-exposure therapy for post-traumatic stress disorder. J Clin Rehab Tissue Engineering Res. 2007;11(39):7783-7786. [Google Scholar]
- 62.van der Kolk BA, Spinazzola J, Blaustein ME, et al. A randomized clinical trial of eye movement desensitization and reprocessing (EMDR), fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: treatment effects and long-term maintenance. J Clin Psychiatry. 2007;68(1):37-46. doi: 10.4088/JCP.v68n0105 [DOI] [PubMed] [Google Scholar]
- 63.Rauch S. Randomized Trial of Sertraline, Prolonged Exposure, and Their Combination for Post-traumatic Stress Disorder (PTSD) in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF). ClinicalTrialsgov. 2018. https://clinicaltrials.gov/ct2/show/results/NCT01524133?term=Rauch&cond=PTSD&rank=2. Accessed May 8, 2019.
- 64.Rauch SAM, Kim HM, Powell C, et al. Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2018;76(2):117-126. doi: 10.1001/jamapsychiatry.2018.3412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van Etten ML, Taylor S. Comparative efficacy of treatments for post-traumatic stress disorder: a meta-analysis. Clin Psychol Psychother. 1998;5(3):126-144. doi: [DOI] [Google Scholar]
- 66.Swift JK, Greenberg RP, Tompkins KA, Parkin SR. Treatment refusal and premature termination in psychotherapy, pharmacotherapy, and their combination: a meta-analysis of head-to-head comparisons. Psychotherapy (Chic). 2017;54(1):47-57. doi: 10.1037/pst0000104 [DOI] [PubMed] [Google Scholar]
- 67.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8(1):75-90. . doi: 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- 68.Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180(2):111-116. . doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- 69.Weiss D, Marmar C. The Impact of Event Scale-Revised In: Wilson JP, Keane TM, eds. Assessing Psychological Trauma and PT-SD. New York, NY: Guliford Press; 1997. [Google Scholar]
- 70.Weathers FW, Huska JA, Keane TM. PCL-C for DSM-IV. Boston, MA: National Center for PTSD-Behavioral Science Division; 1991. [Google Scholar]
- 71.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9(4):445-451. doi: 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- 72.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress. 1993;6(4):459-473. doi: 10.1002/jts.2490060405 [DOI] [Google Scholar]
- 73.Davidson JR, Malik MA, Travers J. Structured interview for PTSD (SIP): psychometric validation for DSM-IV criteria. Depress Anxiety. 1997;5(3):127-129. . doi: [DOI] [PubMed] [Google Scholar]
- 74.Connor KM, Davidson JR. SPRINT: a brief global assessment of post-traumatic stress disorder. Int Clin Psychopharmacol. 2001;16(5):279-284. doi: 10.1097/00004850-200109000-00005 [DOI] [PubMed] [Google Scholar]
- 75.Cuijpers P, Cristea IA. How to prove that your therapy is effective, even when it is not: a guideline. Epidemiol Psychiatr Sci. 2016;25(5):428-435. doi: 10.1017/S2045796015000864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Furukawa TA, Noma H, Caldwell DM, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatr Scand. 2014;130(3):181-192. doi: 10.1111/acps.12275 [DOI] [PubMed] [Google Scholar]
- 77.Sinyor M, Levitt AJ, Cheung AH, et al. Does inclusion of a placebo arm influence response to active antidepressant treatment in randomized controlled trials? results from pooled and meta-analyses. J Clin Psychiatry. 2010;71(3):270-279. doi: 10.4088/JCP.08r04516blu [DOI] [PubMed] [Google Scholar]
- 78.Salanti G, Chaimani A, Furukawa TA, et al. Impact of placebo arms on outcomes in antidepressant trials: systematic review and meta-regression analysis. Int J Epidemiol. 2018;47(5):1454-1464. doi: 10.1093/ije/dyy076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Papakostas GI, Fava M. Does the probability of receiving placebo influence clinical trial outcome? a meta-regression of double-blind, randomized clinical trials in MDD. Eur Neuropsychopharmacol. 2009;19(1):34-40. doi: 10.1016/j.euroneuro.2008.08.009 [DOI] [PubMed] [Google Scholar]
- 80.Stefanovics EA, Rosenheck RA, Jones KM, Huang G, Krystal JH. Minimal clinically important differences (MCID) in assessing outcomes of post-traumatic stress disorder. Psychiatr Q. 2018;89(1):141-155. doi: 10.1007/s11126-017-9522-y [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Search Terms
eAppendix 2. Addition to Methods
eAppendix 3. Additional Results (Main Analyses)
eAppendix 4. Sensitivity Analyses
eAppendix 5. Pairwise Meta-analyses
eFigure 1. Flowchart
eFigure 2. Risk of Bias Assessment
eFigure 3. Indirectness
eTable 1. Risk of Bias for Each Included Study
eTable 2. Indirectness for Each Included Study
eTable 3. Confidence in Network Meta-analysis (CINEMA) Rating
eTable 4. Comparisons of Results Across Different Network Models