Abstract
Nowadays, dental implants are the best treatment option for tooth loss, but implant placement requires sufficient bone volume. In defect area of alveolar ridge, augmentation is done by various available methods. Utilizing the growth factors such as platelet-rich fibrin (PRF) derived from patient's blood platelets improve treatment outcome. PRF accelerates the wound healing, enhances osteogenic activity as well as regulates the inflammation. Bone grafting, guided bone regeneration, and ridge-split technique promote new bone formation. The aim of this case report is to demonstrate an efficient method of bone augmentation using sticky bone along with PRF membrane, followed by ridge-split technique and engagement of nasal floor to place implant.
Keywords: Dental implant, platelet-rich fibrin membrane, ridge-split technique, sticky bone
INTRODUCTION
As severely resorbed edentulous ridges require implant placement through complex techniques such as bone augmentation and sinus lift. Guided bone regeneration (GBR) and autologous bone graft are the most common techniques for alveolar bone augmentation.[1,2] There should be minimum 2 mm bone around the implant for good dental emergence and correct prosthetic rehabilitation.[3,4] For atrophic ridges, sufficient bone volume is required to place implants. Platelet-rich fibrin (PRF) is a healing biomaterial having potential for bone and soft-tissue regeneration without inflammation.[5] It can be used alone or along with bone graft. Compressed PRF membrane acts as a barrier membrane. Mixing Injectable platelet rich fibrin (IPRF) with the granules of bone graft resulted in the formation of sticky bone. After placing sticky bone, a barrier membrane is used to support the grafted bone to the tissue. Ridge split technique also assists in bone augmentation.[6,7]
The aim of this case report is to present an efficient method of GBR by sticky bone which is obtained by mixing IPRF and bone graft together supported by PRF membrane, followed by split technique.
CASE REPORT
A 22-year-old female patient reported the Outpatient Department of Prosthodontics Unit of Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University. She complained of missing upper right canine. Following a thorough medical history to rule out systemic diseases, clinical and radiographic evaluations were performed. She had undergone routine blood investigations and radiographic evaluation by intraoral periapical radiography radiograph, orthopantomogram, and DentaScan. Radiographic investigations revealed the presence of impacted canine palatally [Figure 1]. First treatment planned was orthodontic treatment, but due to its long course, she denied as her wedding date was planned after 4 months. She was also given another option for temporaries during her marriage, but she denied orthodontic treatment postmarriage. Therefore, the second best treatment option was executed. The tooth was extracted followed by GBR, after 3 months implant placement followed by immediate loading with temporary crown. A written description of risks and benefits of proposed treatment was given followed by written consent.
Figure 1.
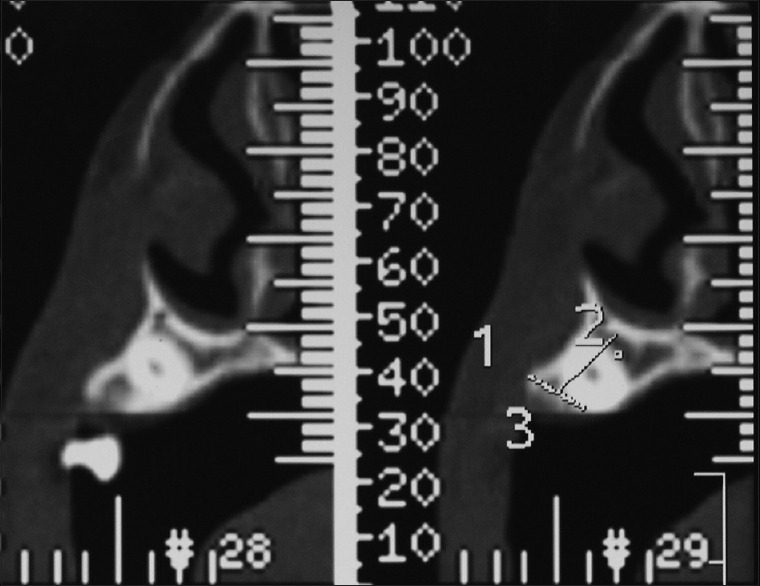
Sagittal sections showing impacted canine
On the day of surgery, antibiotic prophylaxis was administered. The patient was made to rinse 10 ml of Betadine Gargle, followed by extraoral scrubbing with Betadine Scrub. Two percent lignocaine with 1:80,000 adrenaline was administrated for infraorbital nerve block and nasopalatine nerve block to locally anesthetize the surgical site. A crevicular and crestal incision was given at the mid of ridge and full thickness mucoperiosteal flap was reflected. After reflecting flap, impacted canine was extracted atraumatically [Figure 2].
Figure 2.
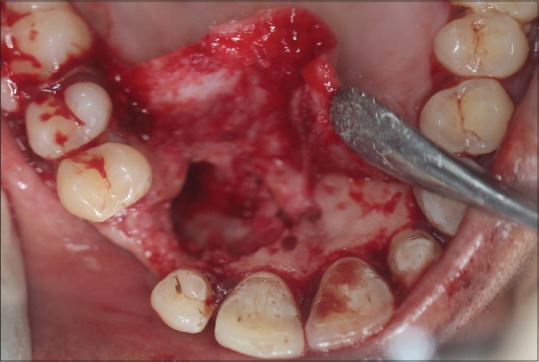
Defect created after extraction of impacted canine
Blood sample was taken from the patient's forearm and collected into three silica-coated red cap tube and 1 noncoated orange cap tube of 10 ml each. Blood in red cap tube was used to make PRF membrane by spinning in centrifuge (Choukron DUO Quatro, France) at 1300 rpm for 8 min, while blood in noncoated orange cap tube was used to prepare IPRF by spinning at 700 rpm for 3 min. IPRF was mixed with granules of xenograft bone (Bio Tiss, Cerabone granulate, natural bovine bone, particle size – 0.5–1 mm) to form sticky bone (stable fibrin bone graft). As sticky bone is a stable fibrin bone graft it has its own body and is easy to handle and can be moulded into desired shape [Figure 3]. PRF layer obtained from red cap tube was allowed to compress to achieve a membrane-like shape. The compressed PRF membrane will act as a barrier membrane. Sticky bone was adapted at the defect site and compressed PRF membrane was placed as barrier membrane. Flaps were approximated and interrupted suture was given. The patient was prescribed antibiotics, analgesics, anti-inflammatory, and chlorhexidine mouth rinses for 5 days and recalled after 7 days for suture removal.
Figure 3.
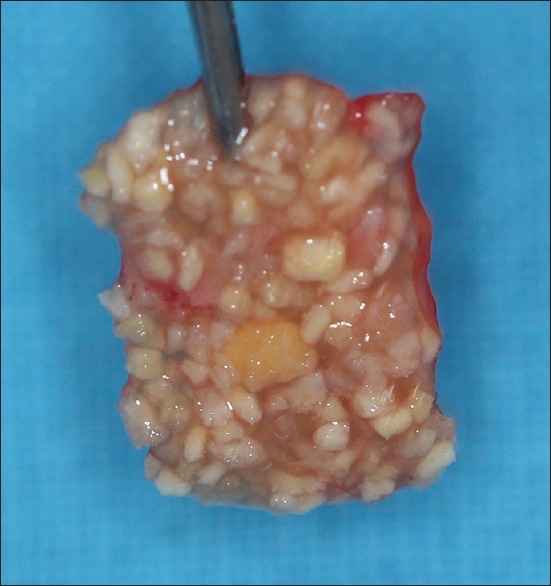
Sticky bone
After 3 months, the patient was clinically evaluated and radiographical investigation was repeated to evaluate changes. As it was evident in the computed tomography scan [Figure 4], predictable bone formation was observed. Surgical reentry was made. Clinically, ridge width was still thin crestally, so ridge-split technique was introduced into the procedure using disc to place two vertical incisions connected with a horizontal incision. After ridge splitting, osteotomy was done to place implant of size 3.5 × 11.5 (Touareg™, ADIN) [Figure 5]. Nasal floor was also engaged to enhance cortical bony support as immediate loading was planned. Additional bone graft was applied over the deficient bone and healing abutments were screwed. Flaps were approximated and sutured.
Figure 4.
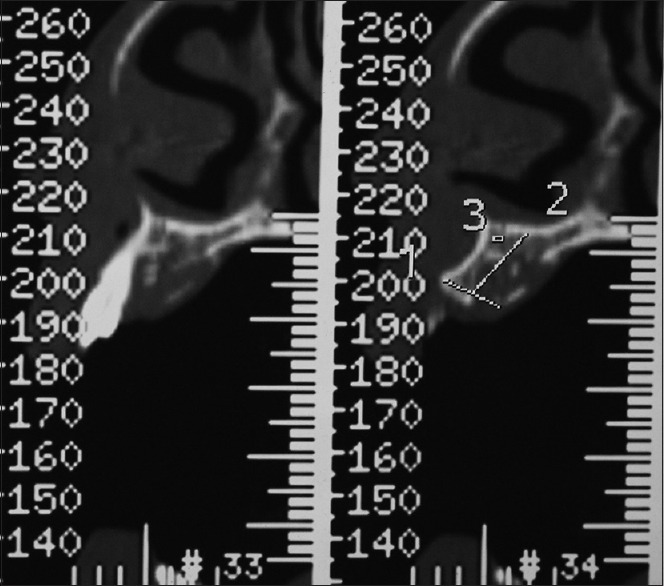
Sagittal sections showing bone formation
Figure 5.

Ridge split and implant placement
Impression was made with open-tray impression coping and temporary crown was fabricated on the cast obtained from impression. Temporary crown was seated and immediately was loaded without occlusal contact in centric, eccentric, and protruded position [Figure 6].
Figure 6.

Occlusal contact in centric occlusion
DISCUSSION
Bone can be augmented by various methods such as distraction osteogenesis, use of various barrier membranes for GBR, particulate grafting material, onlay block graft, ridge-split technique, and the future application of molecules to stimulate bone formation rate and their various combinations.
Distraction osteogenesis is a long-standing phenomenon that involves the filling of new bone in the gap defect created when two parts of the bone are separated slowly under tension. It includes latency phase, distraction phase, and consolidation phase of different time durations to complete the process of bone augmentation and thus a long-duration process which is one of its limitations. Due to more complications in cases of small ridge defects of 1 or 2 missing teeth, it is not indicated for short-span edentulous areas.
GBR is based on the principal of providing space over a defect so that osteogenic cells can grow and prevent the growth of undesired cells into the maintained space where blood clot is protected and gingival connective tissue is excluded to preserve the growth of osteogenic cells. Depending on resorption, there are two types of barrier membranes used, bioresorbable or nonresorbable where bioresorbable is further categorized into synthetic and natural. Commercially available nonresorbable membranes are expanded polytetrafluoroethylene (ePTFE), titanium-reinforced ePTFE, high-density PTFE, or titanium mesh, whereas bioresorbable barrier membranes are synthetic polymeric forms and natural forms are collagen and connective tissue. As resorbable membranes are good treatment options, because there is no need for second surgery for the removal of membranes and they exhibit less soft-tissue exposure complications as compared to nonresorbable membranes. In general, membranes must be used in combination with a bone graft material to maximize the regenerative outcomes.[8]
Autograft, allograft, xenograft, and alloplast all have reported success alone or in combination for particulate bone augmentation. Although autograft is the best bone graft available due to its osteogenic, osteoconductive, and osteoinductive properties and biocompatibility, due to the second surgical-site morbidity, inadequate bone volume, and potential resorption, in some clinical situations, other grafts also offer overall good results. A combination of autograft and allograft/xenograft offers good results by extracting advantages of both grafts used. As allografts are osteoconductive only, they provide scaffold, there is no osteogenic and osteoinductive activity and due to chances of cross infection, it is less preferred in comparison with autograft, but its easy availability and sufficient bone volume allow it as the second option after autograft. Another method of bone augumentation is onlay block graft technique in which block graft is stabilized over recipient bed. Recipient bed is decorticated by intramarrow penetration which leads to optimal neovascularization of block graft. Block stabilization and intimate contact with well prepared recipient bed is imperative which is done by fixation screw, but their removal requires a second stage surgry.
Combination approach where block graft or particulate graft is used along with barrier membrane maximizes the regenerative outcomes. Filling the defect area with sticky bone and covering it with autologous PRF membrane accelerates the bone formation and wound healing. As sticky bone has its own body and can be easily molded into the required shape, thus offers easy handling and also prevents dispersion. Use of PRF membrane as a barrier membrane over the sticky bone increases new bone formation due to the availability of growth factor enriched surrounding, thus leaving a positive effect on tissue healing.[9]
For horizontal bone augmentation, ridge splitting is one of the best options available. It is used for expansion of insufficient residual ridge width along with adequate height provided buccal and lingual cortex are not fused, and there is some intervening cancellous bone present. During split-crest technique, for optimal primary stability, implants are placed apical to osteotomic vertical cuts. The primary advantage of this technique is reduced treatment time and reduced tissue morbidity due to lack of the second surgical donor site.
Nasal floor engagement increases cortical anchorage. Pal et al. analyzed immediate implantation is slightly better than delayed implantation as gingival and bone conditions are slightly better.[10] The approach depends on the extent of defect and procedure to be carried out. Depending on the extent of defect and clinical situations which varies according to the patient, treatment plans are made. Cumulative effect of sticky bone with PRF membrane followed by ridge-split technique and engaging nasal floor results into favorable implant placement with good cortical support and immediate loading.
CONCLUSION
It can be said that in thin atrophic ridges, bony defects of ridges where implant placement is impossible, by utilizing sticky bone supported by autologous PRF membrane followed by ridge-split technique and engaging nasal floor, the implant can be placed with immediate temporary loading in the anterior region. The proposed treatment is very technique sensitive, requires good clinical handling. Long-term studies and researches are further needed to arrive on a definitive conclusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cortese A, Pantaleo G, Amato M, Howard CM, Pedicini L, Claudio PP. Platelet-rich fibrin (PRF) in implants dentistry in combination with new bone regenerative flapless technique: Evolution of the technique and final results. Open Med (Wars) 2017;12:24–32. doi: 10.1515/med-2017-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soni R, Singh A, Vivek R, Baranwal HC, Chaturvedi TP, Srivastava A. Immediate implant placement in mandibular anterior region with dehiscence. J Dent Implant. 2013;3:177–80. [Google Scholar]
- 3.Meloni SM, De Riu G, Pisano M, Dell’aversana Orabona G, Piombino P, Salzano G, et al. Computer-assisted implant surgery and immediate loading in edentulous ridges with dental fresh extraction sockets. Two years results of a prospective case series study. Eur Rev Med Pharmacol Sci. 2013;17:2968–73. [PubMed] [Google Scholar]
- 4.Sammartino G, Pantaleo G, Nuzzolo P, Amato M, Riccitiello F. Minimally invasive approaches to optimize block grafting: A case report. J Oral Implantol. 2016;42:176–9. doi: 10.1563/aaid-joi-D-14-00076. [DOI] [PubMed] [Google Scholar]
- 5.Cortese A, Pantaleo G, Borri A, Caggiano M, Amato M. Platelet-rich fibrin (PRF) in implant dentistry in combination with new bone regenerative technique in elderly patients. Int J Surg Case Rep. 2016;28:52–6. doi: 10.1016/j.ijscr.2016.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mestas G, Alarcón M, Chambrone L. Long-term survival rates of titanium implants placed in expanded alveolar ridges using split crest procedures: A systematic review. Int J Oral Maxillofac Implants. 2016;31:591–9. doi: 10.11607/jomi.4453. [DOI] [PubMed] [Google Scholar]
- 7.Waechter J, Leite FR, Nascimento GG, Carmo Filho LC, Faot F. The split crest technique and dental implants: A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017;46:116–28. doi: 10.1016/j.ijom.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 8.McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007;78:377–96. doi: 10.1902/jop.2007.060048. [DOI] [PubMed] [Google Scholar]
- 9.Kökdere NN, Baykul T, Findik Y. The use of platelet-rich fibrin (PRF) and PRF-mixed particulated autogenous bone graft in the treatment of bone defects: An experimental and histomorphometrical study. Dent Res J (Isfahan) 2015;12:418–24. doi: 10.4103/1735-3327.166188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pal US, Dhiman NK, Singh G, Singh RK, Mohammad S, Malkunje LR. Evaluation of implants placed immediately or delayed into extraction sites. Natl J Maxillofac Surg. 2011;2:54–62. doi: 10.4103/0975-5950.85855. [DOI] [PMC free article] [PubMed] [Google Scholar]


