Via a linkage of health records and traffic data, this longitudinal study suggests that preventable risky behaviors underlie increased crash risk among adolescents with ADHD.
Abstract
OBJECTIVES:
To compare monthly rates of specific types of crashes, violations, and license suspensions over the first years of licensure for drivers with and without attention-deficit/hyperactivity disorder (ADHD).
METHODS:
We identified patients of New Jersey primary care locations of the Children’s Hospital of Philadelphia who were born in 1987–1997, were New Jersey residents, had their last primary care visit at age ≥12 years, and acquired a driver’s license (N = 14 936). Electronic health records were linked to New Jersey’s licensing, crash, and violation databases. ADHD diagnosis was based on International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes. We calculated monthly per-driver rates of crashes (at fault, alcohol related, nighttime, and with peers), violations, and suspensions. Adjusted rate ratios were estimated by using repeated-measures Poisson regression.
RESULTS:
Crash rates were higher for drivers with ADHD regardless of licensing age and, in particular, during the first month of licensure (adjusted rate ratio: 1.62 [95% confidence interval: 1.18−2.23]). They also experienced higher rates of specific crash types: their 4-year rate of alcohol-related crashes was 2.1 times that of drivers without ADHD. Finally, drivers with ADHD had higher rates of moving violations (for speeding, seat belt nonuse, and electronic equipment use) and suspensions. In the first year of driving, the rate of alcohol and/or drug violations was 3.6 times higher for adolescents with ADHD.
CONCLUSIONS:
Adolescents with ADHD are at particularly high crash risk in their initial months of licensure, and engagement in preventable risky driving behaviors may contribute to this elevated risk. Comprehensive preventive approaches that extend beyond current recommendations are critically needed.
What’s Known on This Subject:
In recent studies, it has been established that crash risk is higher among adolescents with attention-deficit/hyperactivity disorder. However, we know little about behavioral mechanisms underlying this risk, and no previous studies have examined risk during the newly licensed period.
What This Study Adds:
This longitudinal study suggests that increased engagement in risky driving behaviors may be an important factor underlying elevated crash risk among adolescent drivers with attention-deficit/hyperactivity disorder. Findings highlight the critical need to develop comprehensive preventive approaches that extend beyond current recommendations.
Attention-deficit/hyperactivity disorder (ADHD) is a common childhood disorder characterized by excessive levels of hyperactivity and impulsivity and/or inattention.1 For the majority of children, ADHD persists into adolescence, when many become licensed to drive.2,3 Skills that are critical in driving, including executive functioning, are frequently impaired in individuals with ADHD.4,5 Indeed, licensing rates among adolescents with ADHD are lower than those among other adolescents.6
Early epidemiological studies suggested an increased crash risk among adolescent drivers with ADHD, but, as described in a previous article,6 they had substantial methodologic limitations.7–11 We recently conducted the first longitudinal examination of crash risk among adolescent drivers with community-identified ADHD; initial analyses revealed that the hazard rate of first-crash involvement was 36% higher among drivers with ADHD compared with that among other adolescents.6 Authors of recent population-based studies of more serious crash-related outcomes (ie, hospital visits) reported similar findings.12,13 However, there have been no studies to examine risk specifically during the newly licensed period (the period of highest lifetime crash risk and thus under the purview of graduated driver licensing [GDL] systems) or crash trajectories as adolescent drivers progress through licensure.
Additionally, research on the specific behavioral mechanisms underlying this elevated crash risk is lacking, limiting the ability to develop evidence-based prevention efforts for novice drivers with ADHD. Examining specific crash types (including single-vehicle crashes, crashes involving alcohol, at-fault crashes, and crashes occurring at night or with peers [2 high-risk driving conditions restricted for newly licensed adolescents under GDL14]), may provide critical insights on driving behaviors that are known to increase the likelihood of crashes or crash-related injuries and may be responsive to targeted intervention. In addition, authors of several previous studies have assessed traffic violations and license suspensions (both frequently used as proxies for risky driving) as well as self-reported risky behaviors (eg, drinking and driving) among these adolescents.7,9–11 However, these studies revealed inconsistent findings and involved samples that were either small or more severely affected.9,10 Moreover, drivers with ADHD have been found to overestimate their driving competence,15 challenging the validity of self-reported measures and highlighting a critical need for studies in which objective traffic safety data are used.
To address these knowledge gaps, we conducted a large retrospective cohort study to compare monthly rates of overall and specific crash types, violations, and suspensions over the initial 4 years of licensure for adolescent drivers with and without ADHD; we hypothesized that rates would be higher among those with ADHD. To do this, we established a cohort of primary care patients at Children’s Hospital of Philadelphia (CHOP) and leveraged a unique linkage of electronic health records (EHRs) and statewide traffic data.
Methods
Study Cohort
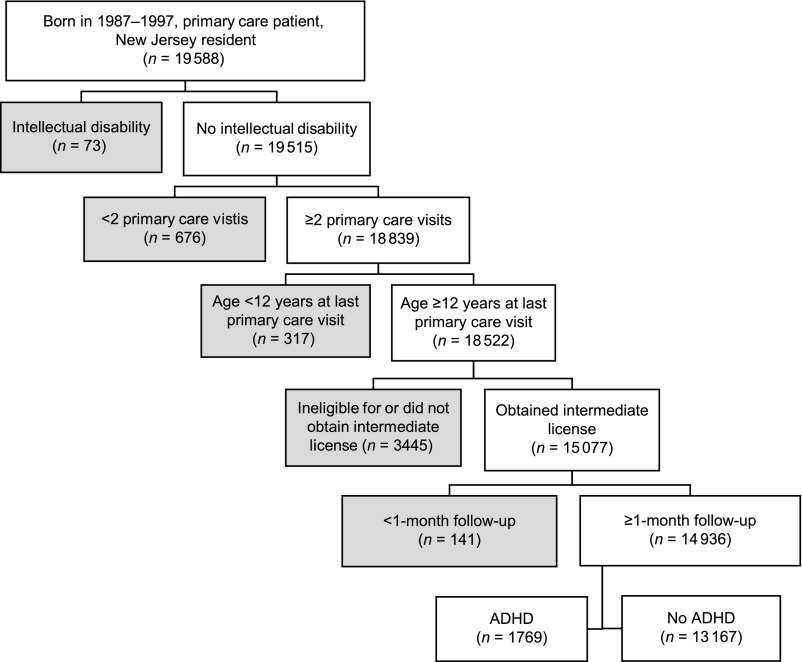
Subjects were identified from the 6 New Jersey primary care practices within the CHOP network, which serves a socioeconomically, ethnically, and racially diverse population. Full details on the study’s design are available elsewhere.6 Briefly, we queried CHOP’s EHR database to select individuals who (1) were born in 1987–1997; (2) were patients at a New Jersey CHOP primary care practice; and (3), to establish New Jersey residency, had a CHOP network visit as a New Jersey resident within 4 years of becoming age eligible to drive (at 16 years) and maintained a New Jersey address through their last CHOP visit. We identified a total of 19 588 individuals. We then excluded individuals with a diagnosed intellectual disability (n = 73); individuals with only 1 primary care visit (n = 676), to minimize ADHD misclassification; and individuals who had their last primary care visit before age 12 years (n = 317), to ensure that individuals were seen at an old enough age to confirm ADHD status.1 The underlying cohort included 18 522 patients. We limited this study to adolescents who obtained an intermediate (initial) driver’s license during the study period and had at least 1 month of post-licensure follow-up (n = 14 936; see Fig 1).
FIGURE 1.
Flowchart revealing selection of study cohort. Gray boxes reveal individuals who were excluded from the study.
ADHD Classification
We classified subjects as having ADHD if their EHR indicated a 314.x International Classification of Diseases, Ninth Revision, Clinical Modification code either at a CHOP network visit or on the list of known conditions. A total of 1769 subjects were identified; 94% were classified on the basis of visits. We conducted a formal internal validation study of this classification scheme (sensitivity = 0.96; specificity = 0.98).16
Data Linkage
Details on the process and validation of data linkages are available in previous publications.6,17 Briefly, we obtained records for individuals who received a New Jersey license through December 2014 from the New Jersey Motor Vehicle Commission; data included exact dates of licensure, license suspensions and restorations, and traffic violations issued. We also obtained data on all police-reported crashes in New Jersey from January 2004 to December 2014. We conducted a hierarchical deterministic linkage; 98% of New Jersey drivers involved in a crash linked to a licensing record. We then used similar methods to link this licensing-crash database with CHOP EHR data. We estimated the true-match rate (true matches divided by original matches) to be 99.95% and the false nonmatch rate (true matches not found) to be 1.5%.
Driving Outcomes
All subjects acquired an intermediate license in New Jersey, where the minimum licensure age is 17 years. In New Jersey, intermediate drivers licensed at age <21 years can drive independently (without adult supervision) but are restricted from driving between 11:01 pm and 4:59 am, while using electronic equipment, or with >1 peer passenger for the first year. They are also prohibited from driving with any detectable amount of alcohol in their system.18 Notably, New Jersey drivers age <21 years cannot plea bargain a point-carrying moving violation.
Primary crash outcomes for adolescent drivers were defined a priori and included (1) all crashes, reportable to police if an injury or >$500 in property damage occurred19; (2) injury crashes, in which at least 1 person had a moderate or greater severity injury (noted on crash report); (3) at-fault crashes, defined in previous work as those with a crash-contributing driver action (eg, inattention or unsafe speed)20; (4) night crashes, including crashes that occurred during New Jersey’s restricted 11:01 pm to 4:59 am period (late) and between 9:00 pm and 11:00 pm (early), a period also identified to be higher risk21; (5) passenger crashes, previously defined as crashes with only passengers aged 14 to 20 years (peer) or ≥2 passengers of any age (multiple)22; (6) single-vehicle crashes, the majority of which have been shown to involve speeding or traveling too fast for conditions23; and (7) alcohol-related crashes, in which the driver was issued a violation for alcohol use or noted on the crash report to have a blood alcohol content level of ≥0.01 for drivers age <21 years and ≥0.08 for drivers age ≥21 years. We calculated monthly rates per 10 000 driver-months; the numerator was the number of crashes among validly licensed drivers, and person-time was calculated by summing for all drivers the proportion of the month that the driver had a valid license. Average monthly rates for the first 12 and 48 months were estimated. Follow-up time concluded at 48 months after licensure, at death, or at end of the study period, whichever occurred first.
Using similar methods, we calculated the monthly rate of violations issued for (1) all traffic offenses; (2) point-carrying moving violations, which include (a) speeding, (b) careless driving, (c) alcohol and/or drug use, and (d) electronic equipment use; (3) seat belt nonuse; and, (4) for intermediate drivers age <21 years, violation of GDL restrictions (eg, nighttime or passenger restrictions). Finally, exact periods of license suspension were identified; suspension rates were calculated as the number of days in which a driver had a suspended license per year of follow-up since the date of licensure.
Other Variables
Demographic variables were ascertained from the EHR. Two co-occurring conditions that may affect crash risk were categorized via International Classification of Diseases, Ninth Revision, Clinical Modification codes: seizure disorder (345.x) and disruptive behavior disorder (DBD) (312.x or 313.81). DBD was further verified through EHR review by study authors (T.J.P. and B.E.Y.) and trained abstractors; confirmation included ≥3 visits for DBD, independent sources (eg, provider notes), or symptoms consistent with DBD. We used 2010 Census Gazetteer Files and 2007−2011 American Community Survey data to categorize residence zip code at last visit into quintiles of population density and median household income, respectively.24,25
Statistical Analysis
We compared bivariate distributions of demographic and clinical characteristics among drivers with and without ADHD using χ2 and Wilcoxon rank-sum tests. Crash and violation risk within the first 12 and 48 months of licensure were compared by using χ2 statistics; estimates were restricted to drivers followed to the specified post-licensure month. We estimated adjusted rate ratios (adjRRs) and 95% confidence intervals (CIs) using generalized estimating equation models with a log link (ie, Poisson distribution). For models, we accounted for correlation within individual drivers using an independent correlation structure. Potential covariates were chosen a priori on the basis of known or suspected association with ADHD (or its diagnosis) and outcomes, including sex, race and/or ethnicity, insurance payer, DBD and seizure disorders, licensing age (17 years 0 months, 17 years 1 month−17 years 11 months, 18 years, and ≥19 years), primary care practice, and birth year. Models also included indicators for zip code–level household income and population density as well as linear and quadratic terms for month since licensure to control for temporal trends. Analyses of GDL violations were restricted to drivers licensed at age <21 years and only through the first year of licensure. For rarer outcomes (alcohol-related crashes, violations for alcohol and/or drug use [12 months after licensure], and licensure suspension), fully adjusted models failed to converge; thus, models were adjusted only for sex and licensing age. Analyses were conducted in SAS version 9.4 (SAS Institute, Inc, Cary, NC). This study was approved by the CHOP Institutional Review Board.
Results
Twelve percent of the cohort had a diagnosis of ADHD (Table 1). The majority of subjects were long-term CHOP primary care patients and were last seen at a median age of 18.1 years. Drivers with ADHD were licensed a median of 3.6 months later than those without ADHD and were more likely to be male and non-Hispanic white.
TABLE 1.
Demographic and Clinical Characteristics of Study Cohort; Comparing Drivers With and Without ADHD
| ADHD Status | ||||
|---|---|---|---|---|
| Overall (N = 14 936) | ADHD (n = 1769) | No ADHD (n = 13 167) | P (ADHD Versus No ADHD) | |
| Age at licensure, median (IQR), y | 17.1 (17.0–17.6) | 17.3 (17.0–18.0) | 17.0 (17.0–17.6) | <.001 |
| Follow-up time, median (IQR), mo | 48 (31–48) | 48 (28–48) | 48 (32–48) | <.001 |
| Age at last primary care visit, median (IQR), y | 18.1 (16.5–19.1) | 18.3 (17.1–19.6) | 18.1 (16.4–19.1) | <.001 |
| No. CHOP primary care visits, median (IQR) | 21 (11–34) | 27 (16–42) | 20 (11–33) | <.001 |
| Sex, n (%) | <.001 | |||
| Female | 7480 (50.1) | 495 (28.0) | 6985 (53.0) | |
| Male | 7456 (49.9) | 1274 (72.0) | 6182 (47.0) | |
| Race and/or ethnicity, n (%) | <.001 | |||
| Non-Hispanic white | 9620 (64.4) | 1317 (74.4) | 8303 (63.1) | |
| Non-Hispanic black or African American | 2176 (14.6) | 205 (11.6) | 1971 (15.0) | |
| Non-Hispanic other | 2754 (18.4) | 208 (11.8) | 2546 (19.3) | |
| Hispanic | 386 (2.6) | 39 (2.2) | 347 (2.6) | |
| Payer at last visit, n (%) | <.001 | |||
| Private | 13 802 (92.4) | 1681 (95.0) | 12 121 (92.1) | |
| Medicaid or self-pay | 437 (2.9) | 42 (2.4) | 395 (3.0) | |
| Not recorded or not billed | 697 (4.7) | 46 (2.6) | 651 (4.9) | |
| DBD, n (%)a | <.001 | |||
| No | 14 389 (96.3) | 1506 (85.1) | 12 883 (97.8) | |
| Yes | 547 (3.7) | 263 (14.9) | 284 (2.2) | |
| Seizure disorder, n (%) | <.001 | |||
| No | 14 727 (98.6) | 1710 (96.7) | 13 017 (98.9) | |
| Yes | 209 (1.4) | 59 (3.3) | 150 (1.1) | |
| Neighborhood income, n (%), $ | <.001 | |||
| ≤57 226 | 2714 (18.2) | 298 (16.8) | 2416 (18.3) | |
| 57 227–72 857 | 5530 (37.0) | 598 (33.8) | 4932 (37.5) | |
| 72 858–87 222 | 3521 (23.6) | 458 (25.9) | 3063 (23.3) | |
| 87 223–105 888 | 2451 (16.4) | 305 (17.2) | 2146 (16.3) | |
| ≥105 889 | 696 (4.7) | 110 (6.2) | 586 (4.5) | |
| Unknown | 24 (0.2) | 0 (0) | 24 (0.2) | |
| Neighborhood population density, n (%), population per square mile | .14 | |||
| ≤408 | 1811 (12.1) | 236 (13.3) | 1575 (12.0) | |
| 409–1223 | 3950 (26.4) | 472 (26.7) | 3478 (26.4) | |
| 1224–2615 | 5685 (38.1) | 673 (38.0) | 5012 (38.1) | |
| 2616–4876 | 3204 (21.5) | 349 (19.7) | 2855 (21.7) | |
| ≥4877 | 271 (1.8) | 39 (2.2) | 232 (1.8) | |
| Unknown | 15 (0.1) | 0 (0) | 15 (0.1) | |
IQR, interquartile range.
DBD includes conduct disorder and oppositional defiant disorder.
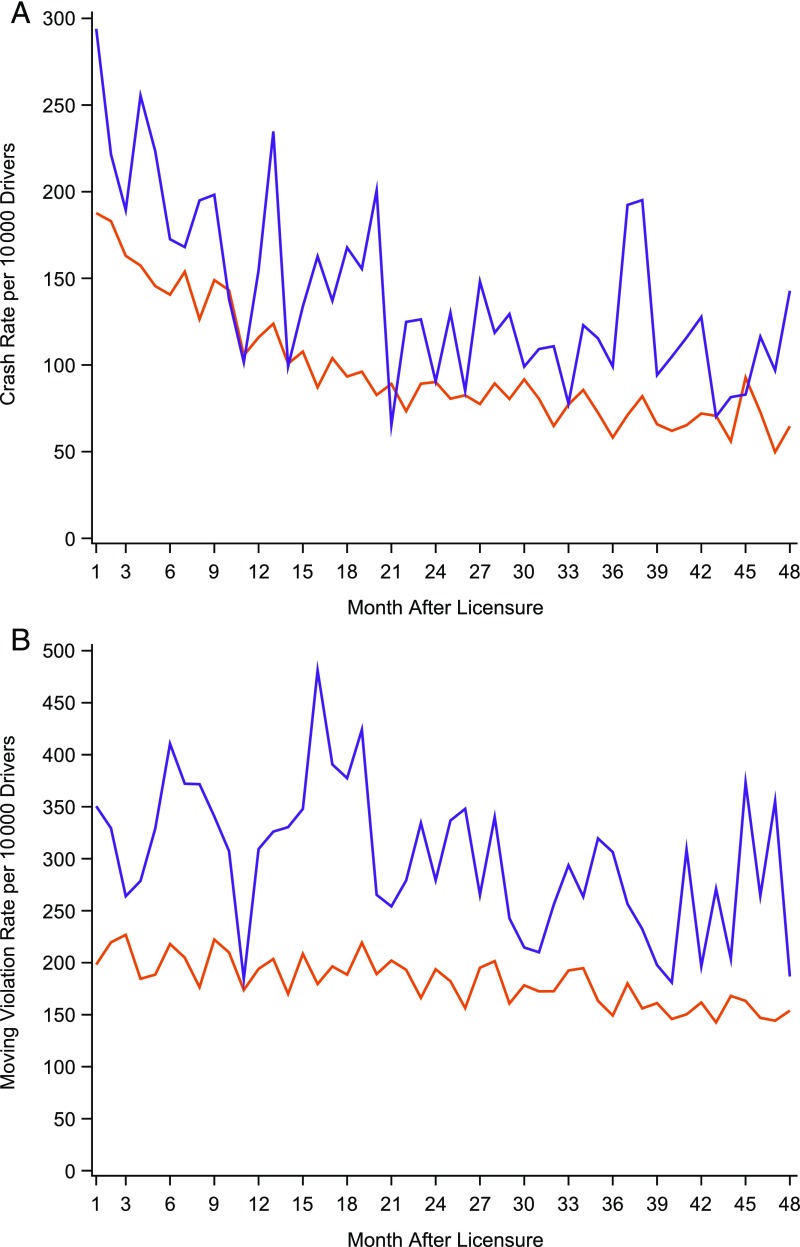
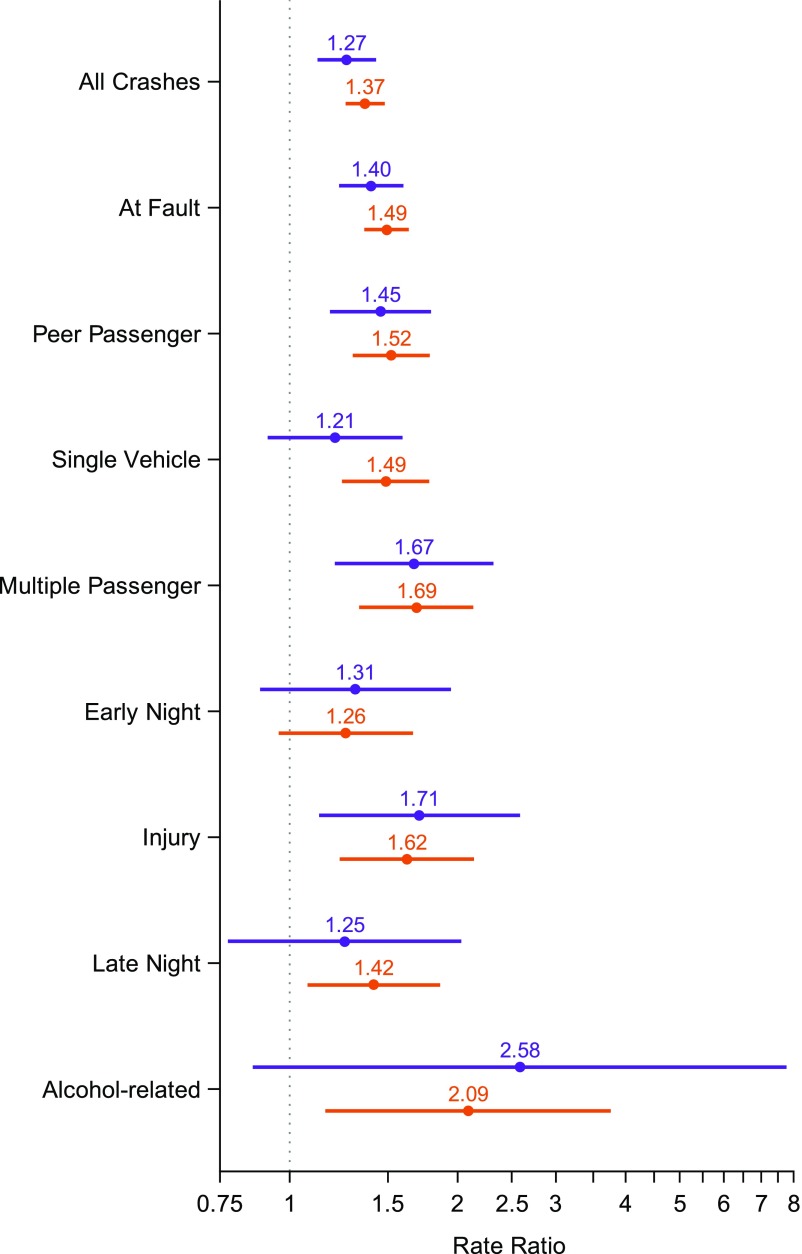
A higher proportion of young drivers with ADHD crashed within the first month (2.8% vs 1.9%; P = .007; not shown), 12 months, and 4 years of licensure (Table 2). The adjusted crash rate in the first month after licensure was 62% higher than that among drivers without ADHD (294.0 vs 187.6 per 10 000 driver-months; adjRR: 1.62 [95% CI: 1.18−2.23]; Fig 2A). After adjusting for potential covariates and temporal trends, the 4-year crash rate of novice adolescent drivers with ADHD was 37% higher than that of drivers without ADHD (95% CI: 1.26−1.48; Fig 3, Supplemental Table 3). In addition, in analyses limited to drivers with ADHD, we found that crash rates of novice drivers who were licensed older versus younger did not differ; for example, there did not appear to be a difference in the 12-month rate for drivers licensed at age ≥18 years and those licensed at age 17 years (adjRR: 1.10 [95% CI: 0.83−1.44]).
TABLE 2.
Risk of Crash Involvement, Traffic Violations, and License Suspension Within 12 and 48 Months After Licensure; Comparing Drivers With and Without ADHD
| Within 12 Months Post-Licensure | Within 48 Months Post-Licensure | |||||
|---|---|---|---|---|---|---|
| ADHD (n = 1593) | No ADHD (n = 12 066) | P | ADHD (n = 985) | No ADHD (n = 8089) | P | |
| No. Drivers (%) | No. Drivers (%) | No. Drivers (%) | No. Drivers (%) | |||
| Crashes | ||||||
| All crashes | 316 (19.8) | 1951 (16.2) | <.001 | 461 (46.8) | 2943 (36.4) | <.001 |
| At fault | 259 (16.3) | 1456 (12.1) | <.001 | 370 (37.6) | 2130 (26.3) | <.001 |
| Peer passenger | 113 (7.1) | 664 (5.5) | .01 | 148 (15.0) | 877 (10.8) | <.001 |
| Single vehicle | 57 (3.6) | 312 (2.6) | .02 | 108 (11.0) | 559 (6.9) | <.001 |
| Multiple passenger | 47 (3.0) | 224 (1.9) | .003 | 60 (6.1) | 355 (4.4) | .02 |
| Early night | 29 (1.8) | 172 (1.4) | .22 | 41 (4.2) | 298 (3.7) | .45 |
| Injury | 28 (1.8) | 114 (0.9) | .003 | 42 (4.3) | 219 (2.7) | .006 |
| Late night | 22 (1.4) | 106 (0.9) | .05 | 55 (5.6) | 261 (3.2) | <.001 |
| Alcohol related | 5 (0.3) | 11 (0.1) | .01 | 12 (1.2) | 47 (0.6) | .02 |
| Violations | ||||||
| All violations | 567 (35.6) | 3053 (25.3) | <.001 | 721 (73.2) | 4703 (58.1) | <.001 |
| Moving violations | 427 (26.8) | 2247 (18.6) | <.001 | 619 (62.8) | 3898 (48.2) | <.001 |
| Careless driving | 225 (14.1) | 1193 (9.9) | <.001 | 387 (39.3) | 2094 (25.9) | <.001 |
| Speeding | 135 (8.5) | 663 (5.5) | <.001 | 299 (30.4) | 1750 (21.6) | <.001 |
| Electronic equipment use | 20 (1.3) | 104 (0.9) | .12 | 76 (7.7) | 385 (4.8) | <.001 |
| Alcohol and/or drug use | 17 (1.1) | 31 (0.3) | <.001 | 35 (3.6) | 175 (2.2) | .006 |
| Seat belt nonuse | 105 (6.6) | 461 (3.8) | <.001 | 229 (23.2) | 1334 (16.5) | <.001 |
| GDL restrictionsa | 68 (4.4) | 343 (2.9) | .001 | — | — | — |
| License suspension | 45 (2.8) | 171 (1.4) | <.001 | 168 (17.1) | 813 (10.1) | <.001 |
Risk is estimated among drivers who were followed to the specified post-licensure month. —, not applicable.
Risk of GDL violations (eg, nighttime or passenger restrictions) was limited to drivers licensed before age 21 y (ADHD: n = 1563; no ADHD: n = 11 920) and estimated only for the first 12 mo after licensure.
FIGURE 2.
A, Monthly observed rate per 10 000 driver-months of crash involvement. B, Monthly observed rate per 10 000 driver-months of moving violations. Drivers with and without ADHD were compared over the first 4 years of licensure. Purple lines indicate drivers with ADHD and orange lines indicate drivers without ADHD.
FIGURE 3.
AdjRRs and 95% CIs for crash outcomes; comparing drivers with and without ADHD. Dots indicate the estimated adjRR, and lines indicate the width of the 95% CI from repeated-measures Poisson regression models. Purple dots and lines compare outcomes for 12 months after licensure. Orange dots and lines compare outcomes for 48 months after licensure.
Drivers with ADHD also experienced higher rates of crash subtypes (crashes involving passengers and at-fault, single-vehicle, injury, and alcohol-related crashes; Fig 3, Supplemental Table 3). For example, in the first 48 months after licensure, drivers with ADHD had a 62% higher rate of injury crashes (95% CI: 1.23−2.14) and a 109% higher rate of alcohol-related crashes (95% CI: 1.16−3.76). Notably, these 2 outcomes were rare events; within the 48-month study period, 4.3% of young drivers with ADHD were involved in an injury crash, and 1.2% were involved in an alcohol-related crash (Table 2).
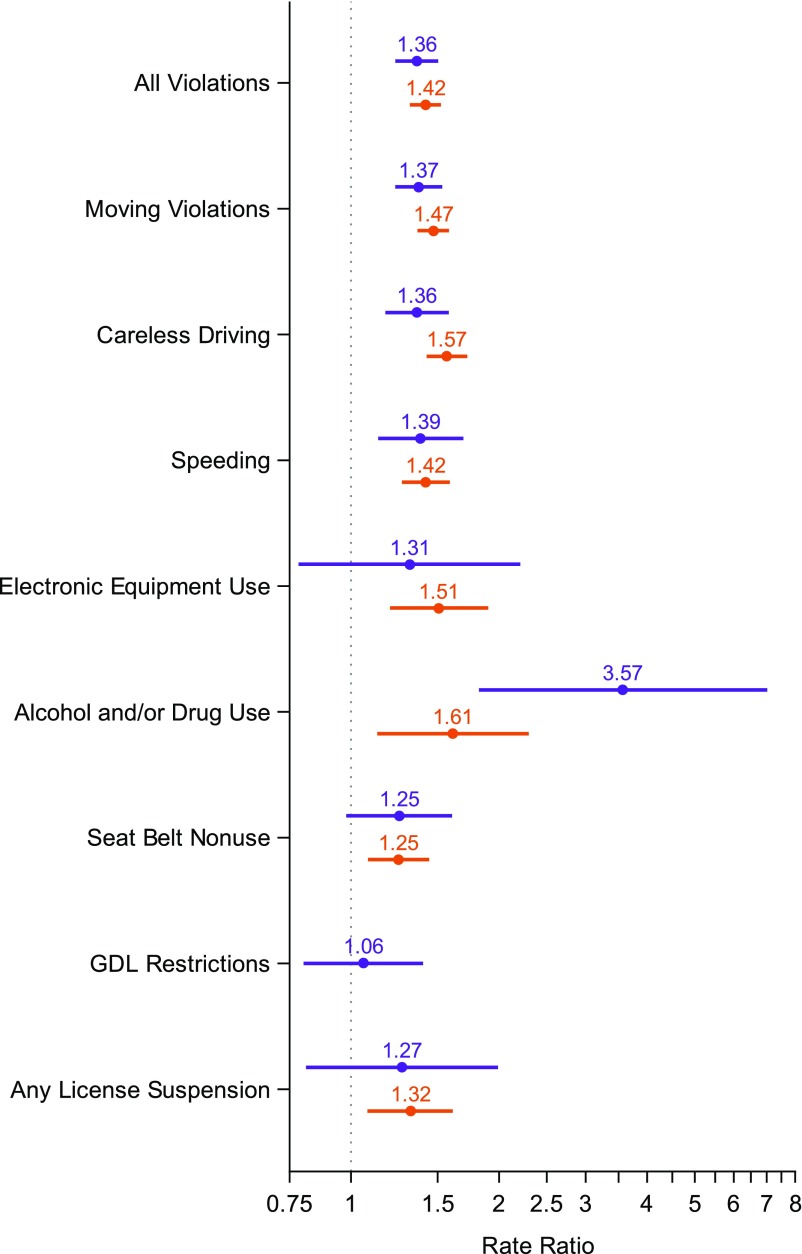
Among drivers with ADHD, 35.6% were issued a traffic violation, and 26.8% were issued a moving violation within their first year of driving (compared with 25.3% and 18.6%, respectively, among drivers without ADHD; Table 2). Rates of moving violations were consistently higher for drivers with ADHD over the study period (at 48 months adjRR: 1.47 [95% CI 1.36−1.58]; Figs 2B and 4). Similarly, rates for specific violations, including careless driving and speeding, were higher among drivers with ADHD. Violation rates for other risky driving behaviors were also elevated, including for alcohol and/or drug violations, which were an estimated 3.57 and 1.61 times higher over the first year and over 4 years of licensure, respectively. GDL violations did not appear to be elevated among those with ADHD (adjRR: 1.06 [95% CI: 0.80−1.40]). Finally, 17.1% of drivers with ADHD and 10.1% of drivers without ADHD had their license suspended at least once in the 4-year period, with average suspension rates of 13.5 and 7.0 days per driver-year, respectively (adjRR: 1.32 [95% CI: 1.08−1.61]; Table 2, Fig 4, Supplemental Table 3).
FIGURE 4.
AdjRRs and 95% CIs for violation and license suspension outcomes; comparing drivers with and without ADHD. Dots indicate the estimated adjRR, and lines indicate the width of the 95% CI from repeated-measures Poisson regression models. Purple dots and lines compare outcomes for 12 months after licensure. Orange dots and lines compare outcomes for 48 months after licensure.
Discussion
With this study, we provide the first longitudinal assessment of crash, violation, and suspension risk among adolescent drivers with ADHD. Findings indicate that adolescent drivers with ADHD have a moderately increased crash risk, a finding consistent with several recent population-based studies of adolescent and adult drivers with ADHD12,13 but lower than estimates in early small studies of adolescents more severely affected.11 In addition, with our study, we uniquely identify the early licensure period as a time of particularly high risk and the potential contribution of preventable factors to increased risk. These findings both offer important implications for families and for professionals working with them and highlight the need to develop comprehensive preventive approaches to reduce these adolescents’ crash risk.
First, this study suggests that risky driving behaviors may underlie elevated crash risk of adolescent drivers with ADHD. Their risk of alcohol-related crashes (albeit low on an absolute scale) remained considerably higher over time, and the relative risk of several risky driving–related crash types was comparatively higher than that of all crash types. In addition, drivers with ADHD had a higher risk of violations for speeding, seat belt nonuse, alcohol and/or drug use, and electronic equipment use. This is consistent with literature revealing that individuals with ADHD are more likely to engage in risk-taking behaviors such as risky sexual activity and substance abuse.26,27 Importantly, many risky driving behaviors may be amenable to change. Although medication may improve driving performance for drivers with ADHD28,29 (and thus is a primary recommendation to families30), there is not firm evidence that medication reduces adolescents’ engagement in certain risky behaviors.31 In addition, there are serious medication adherence issues in adolescence, and our previous study revealed that few adolescents with ADHD are medicated at the time of licensure and detected no differences in crash risk by medication status at licensure.6,32 Thus, novel nonpharmacologic preventive approaches that capitalize on adolescents’ desire for independence and that incorporate skill-training approaches for ADHD (which reveal evidence of effectiveness33) should be strongly considered to promote safe driving. Research suggests that risky behaviors among adolescents with ADHD may be mediated by suboptimal decision-making.34,35 As such, approaches may include training teenagers in decision-making skills in the context of driving and parent training to promote independent, responsible driving behavior. In addition, shared decision-making involving the health care provider, parent, and adolescent (strongly affirmed by the Institute of Medicine) is recommended for the development of intervention plans that balance best provider practices with the goals and preferences of adolescents and their families.36 Additional research is needed to shape shared decision-making practices for youth with ADHD as they learn to drive. Finally, vehicles are increasingly equipped with advanced safety features specifically designed to reduce young drivers’ risk (eg, preset speed limits). Future studies to investigate the effect of these features on driving behaviors, and further, how adolescents interact with these features, are needed.
Second, in this study, we reported that crash risk is particularly heightened in the initial month of licensure and is elevated for novice drivers regardless of age at licensure. Our finding of a 62% increased rate for adolescent drivers with ADHD in their first month of driving reveals that they may be at their most vulnerable just after licensure. This is of particular concern because in general, teenagers are at their highest risk during the first 6 to 12 months after licensure.37,38 Although parents of adolescents with ADHD are frequently guided to delay licensure,30 our results reveal that (contrary to the general population of adolescent drivers38) those with ADHD who delay licensure do not experience a lower crash risk once licensed. This finding may have important implications. In the vast majority of US states, adolescents who delay licensure until age ≥18 years are licensed outside the protective benefits of a GDL system (the most proven intervention to reduce young drivers’ crash risk39). Thus, providers may encourage families inquiring about readiness to drive to seek the assistance of a certified driving rehabilitation specialist (educator specializing in training drivers with medical conditions) during the learner’s permit phase and to adopt GDL-like household rules for teenagers who are not under GDL purview.
Strengths of this study include its longitudinal nature, use of objective measures of outcomes, ability to account for potential covariates (sex, licensing age, time since licensure, and co-occurring conditions), and increased generalizability to the general population of adolescents with ADHD by using a community-identified cohort. A primary limitation is that diagnoses relied on assessment by primary care providers; however, we previously validated ADHD diagnosis codes with high sensitivity and specificity.16 Nevertheless, our sample may more appropriately be characterized as individuals with a lifetime history of ADHD because diagnoses occurred before adolescence and because some individuals may not have had ADHD-related impairments at the time of licensure.40 Additionally, driving exposure was not directly measured. Several previous studies found that those with ADHD reported driving more miles8,41; however, these studies were limited in the authors’ assessment of exposure (eg, usual driving at time of survey) and reliance on self-reports, which might have been subject to positive illusory bias.15 In our analyses, we accounted for time since licensure, a proxy for exposure and itself critically important given that crash risk declines over the initial years of driving. In this study, we also used crash and violation events as proxies for engagement in risky driving behavior; future studies in which naturalistic driving methodologies are used would provide additional crucial insights.42 Adolescents with ADHD may be less likely than adolescents without ADHD to leave the state for postsecondary education43,44; this may lead to an overestimation of true rate ratios. However, rates were elevated in the 12-month period after licensure, before most subjects completed high school. In addition, generalizability may be limited as a result of New Jersey’s licensing age (the oldest in the United States) and high urbanization. Finally, the 12% prevalence of ADHD in our study cohort was higher than estimates of 8% to 9% ever diagnosed for New Jersey children45; this may be influenced by CHOP’s reputation and corresponding care-seeking behavior of parents.
Conclusions
Adolescent drivers with ADHD are at particularly high crash risk in their initial months of licensure, and engagement in preventable risky driving behaviors likely underlies this increased risk. Prospective studies to objectively measure risky driving behaviors among novice drivers with ADHD and examine the extent to which these behaviors mediate driving outcomes are vital to inform prevention strategies. The development of comprehensive preventive approaches to reduce crash risk is critically needed.
Acknowledgments
We thank the New Jersey Department of Transportation, the New Jersey Motor Vehicle Commission, the New Jersey Office of Information Technology, and Children’s Hospital of Philadelphia Department for Biomedical Informatics for their assistance in providing data. We thank Melissa R. Pfeiffer, MPH, for her work on the New Jersey Traffic Safety Outcomes data warehouse. Drs Curry and Metzger had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- adjRR
adjusted rate ratio
- CHOP
Children’s Hospital of Philadelphia
- CI
confidence interval
- DBD
disruptive behavior disorder
- EHR
electronic health record
- GDL
graduated driver licensing
Footnotes
Dr Curry conceptualized and designed the study, drafted the initial manuscript, and critically reviewed and revised the manuscript; Dr Metzger led data collection and analysis and critically reviewed and revised the manuscript; Mrs Carey and Drs Power and Yerys participated in data analysis and interpretation and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health (awards R01HD079398 and R21HD092850; principal investigator: Dr Curry). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Yerys was part of a single consultation meeting with Aevi Genomic Medicine about development of a novel treatment of attention-deficit/hyperactivity disorder; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: American Psychiatric Association; 2013 [Google Scholar]
- 2.Mannuzza S, Klein RG. Long-term prognosis in attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2000;9(3):711–726 [PubMed] [Google Scholar]
- 3.Winston FK, Senserrick TM. Competent independent driving as an archetypal task of adolescence. Inj Prev. 2006;12(suppl 1):i1–i3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barkley RA. ed. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 4th ed. New York, NY: The Guilford Press; 2014 [Google Scholar]
- 5.Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57(11):1336–1346 [DOI] [PubMed] [Google Scholar]
- 6.Curry AE, Metzger KB, Pfeiffer MR, Elliott MR, Winston FK, Power TJ. Motor vehicle crash risk among adolescents and young adults with attention-deficit/hyperactivity disorder. JAMA Pediatr. 2017;171(8):756–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodward LJ, Fergusson DM, Horwood LJ. Driving outcomes of young people with attentional difficulties in adolescence. J Am Acad Child Adolesc Psychiatry. 2000;39(5):627–634 [DOI] [PubMed] [Google Scholar]
- 8.Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98(6, pt 1):1089–1095 [PubMed] [Google Scholar]
- 9.Nada-Raja S, Langley JD, McGee R, Williams SM, Begg DJ, Reeder AI. Inattentive and hyperactive behaviors and driving offenses in adolescence. J Am Acad Child Adolesc Psychiatry. 1997;36(4):515–522 [DOI] [PubMed] [Google Scholar]
- 10.Thompson AL, Molina BS, Pelham W Jr, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. J Pediatr Psychol. 2007;32(7):745–759 [DOI] [PubMed] [Google Scholar]
- 11.Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3- to 5-year follow-up survey. Pediatrics. 1993;92(2):212–218 [PubMed] [Google Scholar]
- 12.Redelmeier DA, Chan WK, Lu H. Road trauma in teenage male youth with childhood disruptive behavior disorders: a population based analysis. PLoS Med. 2010;7(11):e1000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang Z, Lichtenstein P, D’Onofrio BM, Sjölander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry. 2014;71(3):319–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams AF. Graduated driver licensing (GDL) in the United States in 2016: a literature review and commentary. J Safety Res. 2017;63:29–41 [DOI] [PubMed] [Google Scholar]
- 15.Fabiano GA, Schatz NK, Hulme KF, et al. Positive bias in teenage drivers with ADHD within a simulated driving task. J Atten Disord. 2018;22(12):1150–1157 [DOI] [PubMed] [Google Scholar]
- 16.Gruschow SM, Yerys BE, Power TJ, Durbin DR, Curry AE. Validation of the use of electronic health records for classification of ADHD status [published online ahead of print October 1, 2016]. J Atten Disord. 10.1177/1087054716672337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curry AE, Pfeiffer MR, Localio R, Durbin DR. Graduated driver licensing decal law: effect on young probationary drivers [published correction appears in Am J Prev Med. 2014;47(1):103]. Am J Prev Med. 2013;44(1):1–7 [DOI] [PubMed] [Google Scholar]
- 18.New Jersey Motor Vehicle Commission Initial license. Available at: https://www.state.nj.us/mvc/license/initiallicense.htm. Accessed December 12, 2017
- 19.New Jersey Motor Vehicle Commission NJTR-1 form field manual. 2011. Available at: www.state.nj.us/transportation/refdata/accident/pdf/NJTR-1Field_Manual.pdf. Accessed May 1, 2015
- 20.Curry AE, Pfeiffer MR, Myers RK, Durbin DR, Elliott MR. Statistical implications of using moving violations to determine crash responsibility in young driver crashes. Accid Anal Prev. 2014;65:28–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayhew D, Williams A, Pashley C; Traffic Injury Research Foundation A new GDL framework: evidence base to integrate novice driver strategies. Available at: http://trid.trb.org/view.aspx?id=1358954. Accessed February 16, 2016
- 22.Curry AE, Metzger KB, Williams AF, Tefft BC. Comparison of older and younger novice driver crash rates: informing the need for extended Graduated Driver Licensing restrictions. Accid Anal Prev. 2017;108:66–73 [DOI] [PubMed] [Google Scholar]
- 23.Carney C, McGehee DV, Harland K, Weiss M, Raby M Using naturalistic driving data to assess the prevalence of environmental factors and driver behaviors in teen driver crashes. 2015. Available at: https://www.aaafoundation.org/using-naturalistic-driving-data-assess-prevalence-environmental-factors-and-driver-behaviors-teen. Accessed April 6, 2015
- 24.United States Census Bureau 2010 census gazetteer files. 2010. Available at: www.census.gov/geo/maps-data/data/gazetteer2010.html. Accessed April 5, 2018
- 25.United States Census Bureau ACS demographic and housing estimates: 2007-2011 American Community Survey 5-year estimates. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_11_5YR_DP05&prodType=table. Accessed April 5, 2018
- 26.Molina BS, Pelham WE Jr. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol. 2003;112(3):497–507 [DOI] [PubMed] [Google Scholar]
- 27.Sarver DE, McCart MR, Sheidow AJ, Letourneau EJ. ADHD and risky sexual behavior in adolescents: conduct problems and substance use as mediators of risk. J Child Psychol Psychiatry. 2014;55(12):1345–1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Surman CBH, Fried R, Rhodewalt L, Boland H. Do pharmaceuticals improve driving in individuals with ADHD? A review of the literature and evidence for clinical practice. CNS Drugs. 2017;31(10):857–866 [DOI] [PubMed] [Google Scholar]
- 29.Chang Z, Quinn PD, Hur K, et al. Association between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA Psychiatry. 2017;74(6):597–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Resource Center on ADHD Teens with ADHD and driving. Available at: https://chadd.org/for-parents/teens-with-adhd-and-driving/. Accessed February 28, 2018
- 31.Humphreys KL, Eng T, Lee SS. Stimulant medication and substance use outcomes: a meta-analysis. JAMA Psychiatry. 2013;70(7):740–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Molina BS, Hinshaw SP, Swanson JM, et al. ; MTA Cooperative Group . The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2018;47(2):157–198 [DOI] [PubMed] [Google Scholar]
- 34.Shoham R, Sonuga-Barke EJ, Aloni H, Yaniv I, Pollak Y. ADHD-associated risk taking is linked to exaggerated views of the benefits of positive outcomes. Sci Rep. 2016;6:34833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pollak Y, Oz A, Neventsal O, Rabi O, Kitrossky L, Maeir A. Do adolescents with attention-deficit/hyperactivity disorder show risk seeking? Disentangling probabilistic decision making by equalizing the favorability of alternatives. J Abnorm Psychol. 2016;125(3):387–398 [DOI] [PubMed] [Google Scholar]
- 36.Institute of Medicine Initial National Priorities for Comparative Effectiveness Research. Washington, DC: The National Academies Press; 2009 [Google Scholar]
- 37.Chapman EA, Masten SV, Browning KK. Crash and traffic violation rates before and after licensure for novice California drivers subject to different driver licensing requirements. J Safety Res. 2014;50:125–138 [DOI] [PubMed] [Google Scholar]
- 38.Curry AE, Pfeiffer MR, Durbin DR, Elliott MR. Young driver crash rates by licensing age, driving experience, and license phase. Accid Anal Prev. 2015;80:243–250 [DOI] [PubMed] [Google Scholar]
- 39.Curry AE, Foss RD, Williams AF. Graduated driver licensing for older novice drivers: critical analysis of the issues. Am J Prev Med. 2017;53(6):923–927 [DOI] [PubMed] [Google Scholar]
- 40.Cherkasova M, Sulla EM, Dalena KL, Pondé MP, Hechtman L. Developmental course of attention deficit hyperactivity disorder and its predictors. J Can Acad Child Adolesc Psychiatry. 2013;22(1):47–54 [PMC free article] [PubMed] [Google Scholar]
- 41.Barkley RA, Murphy KR, Dupaul GI, Bush T. Driving in young adults with attention deficit hyperactivity disorder: knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc. 2002;8(5):655–672 [DOI] [PubMed] [Google Scholar]
- 42.Klauer C, Ollendick T, Ankem G, Dingus T Improving driving safety for teenagers with attention deficit and hyperactivity disorder (ADHD). Available at: https://vtechworks.lib.vt.edu/bitstream/handle/10919/79137/ADHD STSCE Report_Final.pdf?sequence=1&isAllowed=y. Accessed February 28, 2018
- 43.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45(2):192–202 [DOI] [PubMed] [Google Scholar]
- 44.Kuriyan AB, Pelham WE Jr, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention State-based prevalence data of parent reported ADHD diagnosis by a health care provider. Available at: https://www.cdc.gov/ncbddd/adhd/prevalence.html. Accessed May 11, 2018