We examined smoking and vaping restrictions in homes and cars where children reside and identified parental characteristics associated with the adoption of smoke-free and vape-free policies.
Abstract
Video Abstract
OBJECTIVES:
To determine how smoke-free and vape-free home and car policies differ for parents who are dual users of cigarettes and electronic cigarettes (e-cigarettes), who only smoke cigarettes, or who only use e-cigarettes. To identify factors associated with not having smoke-free or vape-free policies and how often smoke-free advice is offered at pediatric offices.
METHODS:
Secondary analysis of 2017 parental interview data collected after their children’s visit in 5 control practices participating in the Clinical Effort Against Secondhand Smoke Exposure trial.
RESULTS:
Most dual users had smoke-free home policies, yet fewer had a vape-free home policies (63.8% vs 26.3%; P < .01). Dual users were less likely than cigarette users to have smoke-free car (P < .01), vape-free home (P < .001), or vape-free car (P < .001) policies. Inside cars, dual users were more likely than cigarette users to report smoking (P < .001), e-cigarette use (P < .001), and e-cigarette use with children present (P < .001). Parental characteristics associated with not having smoke-free or vape-free home and car policies include smoking ≥10 cigarettes per day, using e-cigarettes, and having a youngest child >10 years old. Smoke-free home and car advice was infrequently delivered.
CONCLUSIONS:
Parents may perceive e-cigarette aerosol as safe for children. Dual users more often had smoke-free policies than vape-free policies for the home. Dual users were less likely than cigarette-only smokers to report various child-protective measures inside homes and cars. These findings reveal important opportunities for intervention with parents about smoking and vaping in homes and cars.
What’s Known on This Subject:
Many parents who smoke have not adopted strictly enforced smoke-free policies for their homes and cars. Most parents who smoke also do not receive advice from child health care providers about keeping their homes and cars smoke free.
What This Study Adds:
This is the first study to examine parents’ rules about prohibiting electronic cigarette and regular tobacco use in homes and cars.
Smoking inside homes and cars when others are present poses a significant health threat; secondhand smoke exposure kills an estimated 41 000 nonsmoking adults and 400 infants per year in the United States.1 Recently, researchers have highlighted additional health risks for people exposed to thirdhand tobacco smoke, which accumulates on surfaces.2–9 Children are especially vulnerable to being exposed to tobacco smoke within their living environments10,11 and have increased risks of asthma,12 leukemia,13 metabolic syndrome,14 sudden infant death syndrome,15 death in adulthood from chronic obstructive pulmonary disease,16 and declines in academic performance.17,18 Recent advances in the understanding of how thirdhand smoke impacts the health of children suggest the need for pediatric health care providers to advocate for strictly enforced smoke-free policies in homes and cars that prohibit smoking even at times when children are not present.19,20
Electronic cigarette (e-cigarette) use has been increasing in the United States among both smokers and nonsmokers.21–23 Moreover, 59% of e-cigarette users are dual users of combustible cigarettes and e-cigarettes.24 Although a comparison between the harmful substances released by cigarettes and e-cigarettes suggests that e-cigarettes are likely safer than cigarettes,25 their overall effect on population health depends on how e-cigarettes are used. When used by people who continue to smoke and when used in the presence of children or inside homes and cars where children live, e-cigarettes may lead to more harm than benefit. Carcinogenetic volatile organic compounds have been detected in the urine of e-cigarette users,26 and e-cigarettes leave deposits of nicotine on surfaces when used inside.27 To protect children from secondhand and thirdhand exposure, parents should adopt strictly enforced policies that prohibit e-cigarette use at all times in homes and cars.28 A recent Internet-based study of US adults revealed that 20% of adults who vape and 30% of cigarette smokers reported prohibiting vaping inside their homes and cars, but it is unknown if this differs for parents who visit pediatric clinics with their children.29 To our knowledge, this is the first study that examines both combusted cigarette use and e-cigarette use in homes and cars where children reside.
Data from a trial testing the Clinical Effort Against Secondhand Smoke Exposure (CEASE) (a pediatric office–based intervention that addresses parental smoking) in 2009–2011 revealed that most pediatricians in usual-care control practices were not asking or advising parent smokers about having smoke-free homes and cars despite large proportions of parents not having strictly enforced smoke-free home and car policies (54% and 24% have strictly enforced smoke-free home and car policies, respectively).30,31 Dissemination of previous research findings through national media,32,33 Web sites,34,35 and pediatrician-focused educational courses36,37 encouraged pediatricians to advise parents to adopt strict smoke-free home and car policies to protect children from exposure to tobacco smoke. We aim to reexamine the prevalence of strictly enforced smoke-free home and car policies and additionally assess the prevalence of strictly enforced home and car policies that prohibit e-cigarette use among a 2017 sample of parents who visited pediatric practices randomly assigned to the control arm of the most recent (2015–2017) CEASE clinical trial.
We examined the prevalence of smoke-free and vape-free homes and cars by whether the parent was smoking, using e-cigarettes, or using both products. Characteristics of parents who lack smoking and vaping policies for their homes and cars were examined. This study also evaluated if pediatricians’ rates of asking and advising about smoke-free homes and cars differed for dual users compared with parents who only smoke or only vape.
Methods
Study Procedure
Parents were approached and asked to participate in an exit interview between April 2017 and October 2017 by research assistants in 5 pediatric primary-care practices that were randomized to the usual-care control arm of a national cluster randomized clinical trial of CEASE. Practices were located in Indiana, North Carolina, Ohio, Tennessee, and Virginia. Additional information about recruitment and eligibility of practices is discussed elsewhere.38 A secondary cross-sectional data analysis was conducted by using these interview data.
Participants
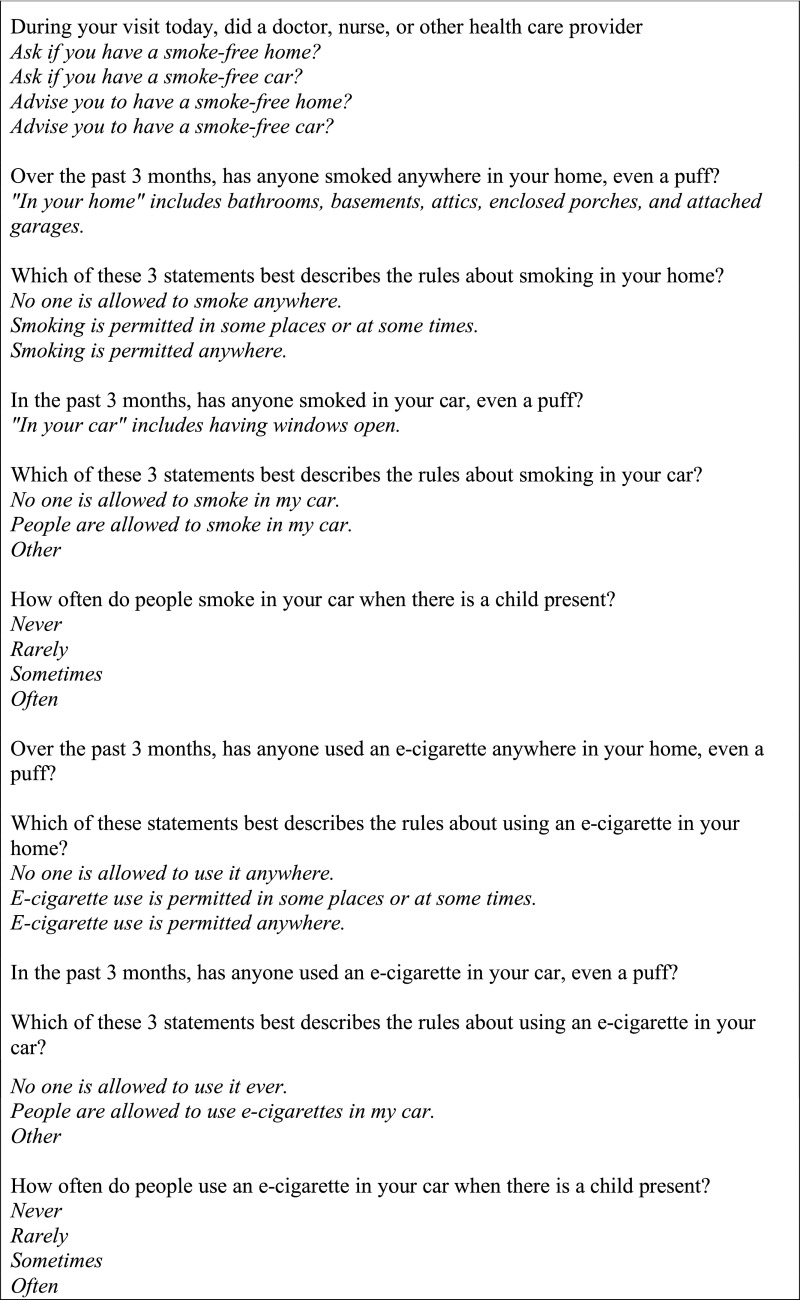
All parents who reported during a screening interview that they were current smokers (had smoked at least 100 cigarettes in their lifetime and had smoked a cigarette, even a puff, in the past 7 days) or former smokers (had not smoked a cigarette in the past 7 days but had smoked a cigarette in the past 2 years) were eligible to participate in an enrollment interview. During this interview, parents were asked about their use of e-cigarettes in the past 30 days, smoking and e-cigarette policies and practices in homes and cars, and whether they were asked or advised at the pediatric visit about having a smoke-free home and a smoke-free car (Fig 1). Eligible parents who agreed to complete the enrollment interview were asked to sign a consent form and were given $5 for participating. Parents who were <18 years old or non-English speaking were not eligible. Institutional review board approval was obtained from Massachusetts General Hospital, the American Academy of Pediatrics, and from pediatric practices (when required).
FIGURE 1.
Questions that were included in the exit enrollment interview.
Measures
Research assistants informed parents that the word e-cigarette was a general term being used in this interview to refer to any electronic nicotine-delivery system device, such as vape pens, JUULs, and mods. The prevalence of strictly enforced smoke-free home and car policies and the prevalence of strictly enforced vape-free home and car policies that prohibited the use of e-cigarettes were calculated for parents who were exclusively smoking, exclusively vaping, and both smoking and vaping (dual use). The prevalences of strictly enforced home and car policies were calculated separately for homes and cars and also as composite measures to reflect the prevalence of parents who reported having strictly enforced policies that covered both the home and car. A strictly enforced smoke-free home policy was defined as a parent reporting having rules that no one is allowed to smoke in the home and indicating that no one had smoked in the home in the past 3 months. Similarly, a strictly enforced smoke-free car policy was defined as having rules that no one is allowed to smoke in the car and stating that no one had smoked in the car in the past 3 months. A strictly enforced vape-free home policy prohibiting e-cigarette use was operationalized as having rules that no one is allowed to use an e-cigarette in the home and stating that no one had used an e-cigarette in the home in the past 3 months. A strictly enforced vape-free car policy prohibiting e-cigarette use was operationalized as having rules that no one is allowed to use an e-cigarette in the car and reporting that no one had used an e-cigarette in the car in the past 3 months. Composite variables were created to reflect whether parents (1) had strictly enforced smoke-free policies that covered both the home and car and (2) had strictly enforced vape-free policies that covered both the home and car. The percentages of parents who reported smoking or using an e-cigarette in the car when children were present were calculated among parents who did not have a strictly enforced smoke-free or vape-free policy for the car, respectively.
Statistical Analysis
Proportions were compared, while accounting for clustering by pediatric practice, to determine if the likelihood of home or car smoking, vaping, and policies prohibiting smoking and vaping differed between cigarette-only users, e-cigarette–only users, and dual users. Pearson’s χ2 analyses were used to determine if dual users who smoked and used e-cigarettes were more or less likely to have strictly enforced vape-free policies than strictly enforced smoke-free policies. Pearson’s χ2 analyses also examined if all parents who used e-cigarettes (exclusively or dual users) were more or less likely to have vape-free policies for the home or car when compared with smoke-free policies.
Multivariable logistic regression models using generalized estimating equations to control for clustering by pediatric practice were used to identify factors among enrolled parents associated with not having strictly enforced smoke-free home and car policies and with not having strictly enforced vape-free home and car policies. Proportions were compared, while accounting for clustering by pediatric practice, to determine if child health care clinicians asked and advised cigarette-only users, e-cigarette–only users, and dual users at different rates about keeping homes and cars smoke free.
Results
A total of 4611 parents were screened across the 5 control practices; 943 parents signed a consent form and were enrolled, 439 were eligible but refused enrollment, and 3229 were ineligible for enrollment. Among enrolled parents who reported using a cigarette or an e-cigarette (n = 761), 84.9% (n = 646) used only cigarettes, 4.5% (n = 34) used only e-cigarettes, and 10.6% (n = 81) were dual users of cigarettes and e-cigarettes. Characteristics of enrolled parents who only smoked cigarettes, only used e-cigarettes, and used both cigarettes and e-cigarettes are presented in Table 1.
TABLE 1.
Characteristics of Enrolled Parents by Product Use
| Characteristic | Parent Uses Only Cigarettes (N = 646), n (%) | Parent Uses Only E-cigarettes (N = 34), n (%) | Parent Is Dual User of Cigarettes and E-cigarettes (N = 81), n (%) | P |
|---|---|---|---|---|
| Smoking status | <.001 | |||
| Quit smoking in past 2 y | 0 (0.0) | 34 (100.0) | 0 (0.0) | |
| Currently smokes cigarettes | 646 (100.0) | 0 (0.0) | 81 (100.0) | |
| Age of parent, y | <.05 | |||
| 18–24 | 99 (15.3) | 6 (17.6) | 16 (19.8) | |
| 25–44 | 474 (73.4) | 28 (82.4) | 59 (72.8) | |
| ≥45 | 73 (11.3) | 0 (0.0) | 6 (7.4) | |
| Parent sex | .03 | |||
| Female | 539 (83.4) | 22 (64.7) | 65 (80.2) | |
| Male | 107 (16.6) | 12 (35.3) | 16 (19.8) | |
| Education level | .14 | |||
| No college | 388 (60.1) | 15 (44.1) | 51 (63.0) | |
| Some college or more | 255 (39.5) | 19 (55.9) | 29 (35.8) | |
| Parent race and/or ethnicity | .62 | |||
| Non-Hispanic black or African American | 67 (10.4) | 4 (11.8) | 5 (6.2) | |
| Non-Hispanic white | 540 (83.6) | 28 (82.4) | 70 (86.4) | |
| Hispanic | 8 (1.2) | 1 (2.9) | 3 (3.7) | |
| Other or multiracial | 29 (4.5) | 1 (2.9) | 3 (3.7) | |
| Child insurance status | .50 | |||
| Medicaid | 385 (59.6) | 16 (47.1) | 46 (56.8) | |
| HMO and/or private insurance | 231 (35.8) | 17 (50.0) | 32 (39.5) | |
| Self-pay or other | 26 (4.0) | 1 (2.9) | 2 (2.5) | |
| Reason for visit | .86 | |||
| Sick child | 164 (25.4) | 9 (26.5) | 17 (21.0) | |
| Well child | 398 (61.6) | 21 (61.8) | 55 (67.9) | |
| Other | 84 (13.0) | 4 (11.8) | 9 (11.1) | |
| Parent tobacco use, cigarettes per d | .75 | |||
| ≥10 | 391 (60.5) | 0 (0.0) | 47 (58.0) | |
| <10 | 254 (39.3) | 0 (0.0) | 33 (40.7) | |
| Other household smokers | .08 | |||
| ≥1 | 373 (57.7) | 14 (41.2) | 52 (64.2) | |
| None | 270 (41.8) | 20 (58.8) | 29 (35.8) | |
Missing data were not included. P values are calculated by using the maximum likelihood ratio χ2 test and were calculated for the whole category. HMO, health management organization.
Table 2 displays the smoking and e-cigarette behaviors and policies for the home and car among enrolled parents who used only cigarettes, used only e-cigarettes, and were dual users. Dual users were less likely than cigarette-only users to have a strictly enforced smoke-free car policy (25.0% vs 42.3%; P < .01), a vape-free home policy (26.3% vs 72.7%; P < .001), and a vape-free car policy (23.9% vs 65.8%; P < .001). Dual users were more likely than cigarette-only users to report anyone smoking inside the car (72.2% vs 56.0%; P < .001) and anyone using an e-cigarette inside the car (62.5% vs 8.4%; P < .001). Among parents without a strictly enforced policy prohibiting e-cigarette use in the car, dual users were more likely than cigarette-only users to report someone has used an e-cigarette in the car with a child present (55.6% vs 26.8%; P < .001). Dual users (22.2%) were less likely than cigarette-only users (37.5%) and less likely than e-cigarette–only users (48.4%) to have strictly enforced smoke-free policies that covered both the home and car (P = .02).
TABLE 2.
Smoking and E-cigarette Behavior and Policies for the Home and Car Among Enrolled Parents
| Variable | Parent Uses Only Cigarettes (N = 646), n (%) | Parent Uses Only E-cigarettes (N = 34), n (%) | Parent Is Dual User of Cigarettes and E-cigarettes (N = 81), n (%) | P |
|---|---|---|---|---|
| Anyone smoked in home (past 3 mo) | 224 (34.8) | 6 (17.6) | 26 (32.1) | .13 |
| Strictly enforced smoke-free home policy | 393 (61.1) | 25 (73.5) | 51 (63.0) | .35 |
| Anyone smoked in car (past 3 mo) | 327 (56.0)a | 7 (22.6)b | 52 (72.2)c | <.001 |
| Strictly enforced smoke-free car policy (if no) | 247 (42.3)a | 18 (58.1)a | 18 (25.0)b | <.01 |
| People smoke in car when children are present | 187 (58.6)a | 1 (9.1)b | 26 (52.0)a | .03 |
| Strictly enforced smoke-free policy for both home and car | 219 (37.5)a | 15 (48.4)a | 16 (22.2)b | .02 |
| Anyone used e-cigarette in home (past 3 mo) | 69 (10.7)a | 24 (70.6)b | 50 (61.7)b | <.001 |
| Strictly enforced vape-free home policy | 402 (72.7)a | 8 (23.5)b | 21 (26.3)b | <.001 |
| Anyone used e-cigarette in car (past 3 mo) | 49 (8.4)a | 24 (77.4)b | 45 (62.5)b | <.001 |
| Strictly enforced vape-free car policy (if no) | 340 (65.8)a | 6 (19.4)b | 17 (23.9)b | <.001 |
| People use e-cigarette in car when children are present | 40 (26.8)a | 14 (56.0)b | 30 (55.6)b | <.001 |
| Strictly enforced vape-free policy for both home and car | 308 (60.5)a | 6 (19.4)b | 15 (21.1)b | <.001 |
Missing data were not included. Car items are limited to parents who reported that they have a car. Each superscript letter denotes categories whose column proportions do not differ significantly from each other at the .05 level.
Pearson’s χ2 analysis revealed that most dual users had a strictly enforced smoke-free home policy, yet fewer had a strictly enforced vape-free home policy (63.8% vs 26.3%; P < .01). When dual users and e-cigarette–only users were combined into a single group, most of these parents had a strictly enforced smoke-free home policy, and significantly fewer had a strictly enforced vape-free home policy (66.7% vs 25.4%; P = .03). Similarly, the combined group of dual users and e-cigarette–only users were more likely to have a strictly enforced smoke-free car policy than a strictly enforced vape-free car policy (35.3% vs 22.5%; P < .001).
Table 3 presents the adjusted odds ratios for characteristics associated with not having strictly enforced smoke-free policies for the home and car or strictly enforced vape-free policies for the home and car among enrolled parents who smoke. Parents were more likely to not have a strictly enforced smoke-free policy for the home and car if they had not attended college, smoked ≥10 cigarettes per day, had ≥1 additional household smoker, had used an e-cigarette in the past 30 days, and their youngest child was ≥5 years old. Parents were more likely to not have a strictly enforced vape-free policy prohibiting e-cigarette use in the home and car if they had not attended college, were between 18 and 24 years old, smoked ≥10 cigarettes per day, had used an e-cigarette in the past 30 days, or their youngest child was >10 years old.
TABLE 3.
Multivariable Logistic Regression Models Using Generalized Estimating Equations Showing the Adjusted Odds of Not Having Strictly Enforced Home and Car Policies Among Enrolled Parents Who Smoke
| Variable | Not Having Strictly Enforced Smoke-Free Policies Prohibiting Smoking in the Home and Car (n = 643), Adjusted OR (95% CI) | Not Having Strictly Enforced Vape-Free Policies Prohibiting E-cigarette Use in the Home and Car (n = 567), Adjusted OR (95% CI) |
|---|---|---|
| Parent age, y | ||
| 18–24 | 1.49 (0.68–3.28) | 3.93 (1.77–8.71) |
| 25–44 | 1.19 (0.64–2.22) | 1.82 (0.95–3.47) |
| ≥45 | Reference | Reference |
| Age of youngest child, y | ||
| >10 | 2.83 (1.55–5.16) | 2.56 (1.43–4.56) |
| 5–10 | 1.61 (1.04–2.49) | 1.47 (0.94–2.30) |
| <5 | Reference | Reference |
| Parent sex | ||
| Female | Reference | Reference |
| Male | 1.17 (0.73–1.86) | 1.03 (0.64–1.65) |
| Education level | ||
| No college | 1.66 (1.16–2.38) | 1.47 (1.01–2.13) |
| Some college or more | Reference | Reference |
| Parent race and/or ethnicity | ||
| Non-Hispanic black or African American | 0.50 (0.18–1.44) | 0.42 (0.15–1.14) |
| Non-Hispanic white | 0.94 (0.37–2.37) | 1.18 (0.52–2.68) |
| Hispanic | 0.43 (0.09–2.14) | 0.27 (0.04–1.81) |
| Other | Reference | Reference |
| Child insurance status | ||
| Medicaid | 1.59 (0.64–3.98) | 1.06 (0.44–2.55) |
| HMO and/or private insurance | 1.28 (0.51–3.25) | 0.90 (0.37–2.20) |
| Self-pay or other | Reference | Reference |
| Reason for visit | ||
| Sick child | 0.81 (0.43–1.53) | 0.83 (0.44–1.55) |
| Well child | 0.84 (0.47–1.50) | 0.77 (0.44–1.35) |
| Other | Reference | Reference |
| Parent tobacco use, cigarettes per d | ||
| ≥10 | 2.39 (1.66–3.43) | 1.71 (1.17–2.49) |
| <10 | Reference | Reference |
| Other household smokers | ||
| ≥1 | 1.74 (1.21–2.49) | 1.44 (0.99–2.08) |
| None | Reference | Reference |
| E-cigarette use in past 30 d | ||
| Used | 2.54 (1.35–4.75) | 7.49 (3.86–14.54) |
| Did not use | Reference | Reference |
List-wise deletion was used; analyses were limited to parents who had a car. CI, confidence interval; HMO, health management organization; OR, odds ratio.
Table 4 shows the percentage of enrolled parents who reported being asked about or advised to have smoke-free homes and cars at the time of their children’s visit to the pediatric office that day. Parents who smoke were approximately half as likely to be asked if they have a smoke-free home than parents who reported exclusively using e-cigarettes. Parents who smoke only cigarettes were significantly less likely than dual users to be asked and advised about having smoke-free homes and cars.
TABLE 4.
Rates of Enrolled Parents Being Asked About or Advised to Have Smoke-Free Homes and Cars at the Pediatric Visit
| Variable | Parent Uses Only Cigarettes (N = 646), n (%) | Parent Uses Only E-cigarettes (N = 34), n (%) | Parent Is Dual User of Cigarettes and E-cigarettes (N = 81), n (%) | P |
|---|---|---|---|---|
| Asked if you have a smoke-free home | 142 (22.0)a | 14 (41.2)b | 26 (32.5)b | <.01 |
| Advised to have a smoke-free home | 95 (14.8)a | 9 (26.5)a,b | 23 (28.8)b | <.01 |
| Asked if you have a smoke-free car | 87 (14.9)a | 8 (25.8)a,b | 20 (28.2)b | <.01 |
| Advised to have a smoke-free car | 74 (12.6)a | 7 (22.6)a,b | 21 (29.6)b | <.01 |
Missing data were not included. Car items are limited to parents who reported that they have a car. Each superscript letter denotes categories whose column proportions do not differ significantly from each other at the.05 level.
Discussion
Among enrolled parents, only 37.5% of smokers and 22.2% of dual users had strictly enforced smoke-free policies in both the home and car. Given the extensive scientific knowledge that has accumulated over decades about the health consequences of exposure to tobacco smoke,39 these findings represent a major public health shortfall. Only 14.8% of parents who used only cigarettes said they were advised to have a smoke-free home and 12.6% were advised to have a smoke-free car during their visit to their children’s doctor’s office. Limited pediatrician engagement on these issues reveals a continued unmet need in health care settings for screening and advising parents who smoke to protect children in homes and cars.
Significant discrepancies in the likelihood of protecting children from different tobacco product exposures were noted. Dual users were less likely to have a smoke-free car policy and less likely to have vape-free policies for the home and car than parents who only smoked cigarettes. Additionally, dual users were more likely to report people had vaped inside the car when children were present compared with parents who exclusively smoked cigarettes. These results suggest clinical interventions, such as CEASE, should identify parents who are dual users and enhance counseling about the importance of keeping living spaces completely free from both smoking and vaping.20,27
Cigarettes and e-cigarettes were frequently being used in parents’ cars, and significant percentages of parents reported smoking or vaping in cars with children present. As of June 2017, 8 US states have passed legislation prohibiting smoking in cars with children, yet many of the laws do not specifically mention vaping.40 Our findings suggest that legislation should consider including prohibitions against vaping, too, because many children are being exposed inside cars. A California study revealed that legislation prohibiting smoking in a car with a child lowered children’s tobacco smoke exposure and improved health outcomes.41
This study showed that approximately 20% of parents who used e-cigarettes (either exclusively or as a dual user) had strictly enforced vape-free policies for the home and car. This compares similarly with a recent nationally representative study of US adults that found that approximately 20% of adults who vape had rules against the use of vaping products in their homes and cars.29 The percentages of cigarette smokers who allowed vaping in their homes and cars were markedly different between the parents interviewed in this study and US adults who participated in the Internet-based study. Approximately 60% of enrolled parents who only smoke reported prohibiting vaping in homes and cars compared to 30% of adult smokers in the Internet-based study who reported having rules against vaping in their homes and cars.29 Identifying how parents who smoke perceive the risk of vaping in the home and car differently than nonparents should be examined in future research.
Results suggest a perception may exist among many parents that e-cigarette aerosol is safe for their children because the majority of dual users had a strictly enforced smoke-free home policy (63.8%), whereas a statistically significant lower percentage of these parents had a strictly enforced vape-free home policy (26.3%). When we examined this issue by combining dual users and e-cigarette users into a single group of e-cigarette users, we found the majority had a strictly enforced smoke-free home policy (66.7%), yet significantly fewer had a strictly enforced vape-free home policy (25.4%). A greater percentage of the combined dual users and e-cigarette users group had strictly enforced smoke-free car policies (35.3%) compared with strictly enforced vape-free car policies (22.5%). Pediatric health care providers should address these apparent misperceptions about e-cigarette aerosol with parents. E-cigarette use has been proposed by some advocates as a potential risk-reduction strategy compared with smoking combusted tobacco. This study suggests that dual users of both traditional cigarettes and e-cigarettes are less likely to protect children with smoke-free (22.2% vs 37.5%; P = .02) as well as vape-free (21.1% vs 60.5%; P < .001) policies for the home and car compared with parents who smoke only cigarettes. These results highlight the enhanced need for child health care providers to be prepared to assist parents with issues related to traditional smoking and assist parents who vape.
Having a youngest child ≥5 years old was associated with a reduced likelihood of having a strictly enforced smoke-free policy for the home and car. Having a youngest child >10 years old was associated with a reduced likelihood of having a strictly enforced vape-free policy for the home and car. Because parents are more likely to protect younger children from their smoking and vaping inside homes and cars, additional efforts should be made within pediatric practices to also encourage parents with older children to protect them with smoke-free and vape-free home and car policies. Younger parents (≥18 and ≤24 years old) were more likely to lack a home and car policy that prohibits vaping compared with older parents. Marketing of vaping products, such as JUUL and other e-cigarettes, have been heavily targeted to young people and may be influencing their decisions42 and attitudes43 about vaping in homes and cars when they become parents.
A limitation of our analysis is that the exit interview only contained items related to asking and advising about smoking and did not include similar items about vaping. Additional limitations include the use of parental self-report data that may not necessarily reflect the true incidence of cigarette and e-cigarette use in homes and cars. Results that compare groups of parents with major differences in sample sizes should be interpreted cautiously.
Conclusions
The findings presented in this study could be used to broaden tobacco control recommendations to include guidance for addressing e-cigarettes in the pediatric health care setting. Parents who were dual users of cigarettes and e-cigarettes were more likely to have strictly enforced smoke-free policies than vape-free policies for the home, suggesting that some may believe exposure to vaping inside the home is safe for children. Additionally, parents who dual use cigarettes and e-cigarettes were less likely to have strictly enforced smoke-free policies for the car and vape-free policies in the home and car than parents who only use traditional cigarettes. The large percentages of parents who have not adopted smoke-free and vape-free homes and cars and the low percentages of parents who are asked or advised about keeping homes and cars smoke free when attending pediatric practices reveals the continued unmet need to implement interventions that will promote safe homes and cars for children.
Acknowledgments
We especially appreciate the efforts of the American Academy of Pediatrics practices and practitioners.
Glossary
- CEASE
Clinical Effort Against Secondhand Smoke Exposure
- e-cigarette
electronic cigarette
Footnotes
This trial has been registered at www.clinicaltrials.gov (identifier NCT01882348).
Mr Drehmer conceptualized and designed the analysis, coordinated and supervised data collection, conducted the data analyses, and drafted and revised the manuscript; Dr Nabi-Burza made a substantial contribution to the conception and design of the analysis, assisted with coordinating and supervising data collection, and made intellectual contributions to the editing of the manuscript; Dr Winickoff conceived of and conducted the larger trial as principal investigator, made substantial intellectual contributions to the conception and design of the study, and critically reviewed the manuscript; Drs Hipple Walters, Ossip, Levy, Rigotti, and Klein made substantial intellectual contributions to the conception and design of the study, interpretation of data, and editing of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Health (grant R01-CA127127). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Not related to this article, Dr Rigotti receives royalties from UpToDate, Inc, is an unpaid consultant to Pfizer regarding smoking cessation, and is a paid consultant to Achieve Life Sciences regarding an investigational smoking-cessation aid; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.US Department of Health and Human Services The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014 [Google Scholar]
- 2.Hang B, Wang Y, Huang Y, et al. Short-term early exposure to thirdhand cigarette smoke increases lung cancer incidence in mice. Clin Sci (Lond). 2018;132(4):475–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matt GE, Quintana PJ, Destaillats H, et al. Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environ Health Perspect. 2011;119(9):1218–1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramírez N, Özel MZ, Lewis AC, Marcé RM, Borrull F, Hamilton JF. Exposure to nitrosamines in thirdhand tobacco smoke increases cancer risk in non-smokers. Environ Int. 2014;71:139–147 [DOI] [PubMed] [Google Scholar]
- 5.Martins-Green M, Adhami N, Frankos M, et al. Cigarette smoke toxins deposited on surfaces: implications for human health. PLoS One. 2014;9(1):e86391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hang B, Sarker AH, Havel C, et al. Thirdhand smoke causes DNA damage in human cells. Mutagenesis. 2013;28(4):381–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sleiman M, Gundel LA, Pankow JF, Jacob P III, Singer BC, Destaillats H. Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards. Proc Natl Acad Sci USA. 2010;107(15):6576–6581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacob P III, Benowitz NL, Destaillats H, et al. Thirdhand smoke: new evidence, challenges, and future directions. Chem Res Toxicol. 2017;30(1):270–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hang B, Snijders AM, Huang Y, et al. Early exposure to thirdhand cigarette smoke affects body mass and the development of immunity in mice. Sci Rep. 2017;7:41915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matt GE, Quintana PJ, Hovell MF, et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob Control. 2004;13(1):29–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hovell MF, Zakarian JM, Matt GE, et al. Counseling to reduce children’s secondhand smoke exposure and help parents quit smoking: a controlled trial. Nicotine Tob Res. 2009;11(12):1383–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jin Y, Seiber EE, Ferketich AK. Secondhand smoke and asthma: what are the effects on healthcare utilization among children? Prev Med. 2013;57(2):125–128 [DOI] [PubMed] [Google Scholar]
- 13.Metayer C, Dahl G, Wiemels J, Miller M. Childhood leukemia: a preventable disease. Pediatrics. 2016;138(suppl 1):S45–S55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moore BF, Clark ML, Bachand A, Reynolds SJ, Nelson TL, Peel JL. Interactions between diet and exposure to secondhand smoke on metabolic syndrome among children: NHANES 2007-2010. J Clin Endocrinol Metab. 2016;101(1):52–58 [DOI] [PubMed] [Google Scholar]
- 15.Royal College of Physicians Passive Smoking and Children. A Report by the Tobacco Advisory Group. London, United Kingdom: Royal College of Physicians; 2010. https://cdn.shopify.com/s/files/1/0924/4392/files/passive-smoking-and-children.pdf?15599436013786148553. Accessed October 5, 2018 [Google Scholar]
- 16.Diver WR, Jacobs EJ, Gapstur SM. Secondhand smoke exposure in childhood and adulthood in relation to adult mortality among never smokers. Am J Prev Med. 2018;55(3):345–352 [DOI] [PubMed] [Google Scholar]
- 17.Chen R, Clifford A, Lang L, Anstey KJ. Is exposure to secondhand smoke associated with cognitive parameters of children and adolescents?–a systematic literature review. Ann Epidemiol. 2013;23(10):652–661 [DOI] [PubMed] [Google Scholar]
- 18.Ho SY, Lai HK, Wang MP, Lam TH. Exposure to secondhand smoke and academic performance in non-smoking adolescents. J Pediatr. 2010;157(6):1012–1017.e1 [DOI] [PubMed] [Google Scholar]
- 19.Kuschner WG, Reddy S, Mehrotra N, Paintal HS. Electronic cigarettes and thirdhand tobacco smoke: two emerging health care challenges for the primary care provider. Int J Gen Med. 2011;4:115–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drehmer JE, Walters BH, Nabi-Burza E, Winickoff JP. Guidance for the clinical management of thirdhand smoke exposure in the child health care setting. J Clin Outcomes Manag. 2017;24(12):551–559 [PMC free article] [PubMed] [Google Scholar]
- 21.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013. Nicotine Tob Res. 2015;17(2):228–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arrazola RA, Singh T, Corey CG, et al. ; Centers for Disease Control and Prevention (CDC) . Tobacco use among middle and high school students - United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–385 [PMC free article] [PubMed] [Google Scholar]
- 23.McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, Klein JD. Trends in electronic cigarette use among U.S. Adults: use is increasing in both smokers and nonsmokers. Nicotine Tob Res. 2015;17(10):1195–1202 [DOI] [PubMed] [Google Scholar]
- 24.QuickStats: cigarette smoking status* among current adult E-cigarette users,† by age group - National Health Interview Survey,§ United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(42):1177. [DOI] [PubMed] [Google Scholar]
- 25.Rigotti NA. Balancing the benefits and harms of e-cigarettes: a national academies of science, engineering, and medicine report. Ann Intern Med. 2018;168(9):666–667 [DOI] [PubMed] [Google Scholar]
- 26.Rubinstein ML, Delucchi K, Benowitz NL, Ramo DE. Adolescent exposure to toxic volatile organic chemicals from E-cigarettes. Pediatrics. 2018;141(4):e20173557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goniewicz ML, Lee L. Electronic cigarettes are a source of thirdhand exposure to nicotine. Nicotine Tob Res. 2015;17(2):256–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walley SC, Jenssen BP; Section on Tobacco Control . Electronic nicotine delivery systems. Pediatrics. 2015;136(5):1018–1026 [DOI] [PubMed] [Google Scholar]
- 29.Gentzke AS, Homa DM, Kenemer JB, Gomez Y, King BA. Rules to prohibit the use of electronic vapor products inside homes and personal vehicles among adults in the U.S., 2017. Prev Med. 2018;114:47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ossip DJ, Chang Y, Nabi-Burza E, et al. Strict smoke-free home policies among smoking parents in pediatric settings. Acad Pediatr. 2013;13(6):517–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nabi-Burza E, Regan S, Drehmer J, et al. Parents smoking in their cars with children present. Pediatrics. 2012;130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salamon M. Many smokers light up with kids in car, study says. HealthDay November 12, 2012. Available at: https://medicalxpress.com/news/2012-11-smokers-kids-car.html. Accessed July 25, 2018
- 33.Kemp C. Children held captive in smoky vehicles. AAP News May 1, 2011. Available at: www.aappublications.org/content/early/2011/05/01/aapnews.20110501-1. Accessed October 1, 2018
- 34.AAP Pediatric research in office settings. Available at: https://www.aap.org/en-us/professional-resources/Research/PROS/Pages/Pediatric-Research-in-Office-Setting.aspx. Accessed October 5, 2018
- 35.AAP Parents who smoke often expose children to tobacco smoke in their cars. Available at: https://www.healthychildren.org/English/news/Pages/Parents-Who-Smoke-Often-Expose-Children-to-Tobacco-Smoke-in-Their-Cars.aspx. Accessed July 25, 2018
- 36.Winickoff JP, Dempsey JH, Friebely J, Hipple B, Lazorick S EQIPP: Eliminate Tobacco Use and Exposure. 2011. Available at: www.pedialink.org/cme/eqipptc. Accessed September 27, 2012
- 37.Drehmer J, Hipple B, Murphy S, Winickoff JP EQIPP: Eliminating Tobacco Use and Exposure to Secondhand Smoke. 2014. Available at: https://eqipp.aap.org. Accessed January 1, 2017
- 38.Walters BH, Ossip DJ, Drehmer JE, et al. Clinician telephone training to reduce family tobacco use: analysis of transcribed recordings. J Clin Outcomes Manag. 2016;23(2):79–86 [PMC free article] [PubMed] [Google Scholar]
- 39.Office on Smoking and Health The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2006 [PubMed] [Google Scholar]
- 40.Public Health Law Center U.S. prohibitions on smoking in cars with children. 2017. Available at: www.publichealthlawcenter.org/sites/default/files/resources/Prohibitions-Chart-Smoking-With-Children-Cars-2017.pdf. Accessed July 25, 2018
- 41.Patel M, Thai CL, Meng YY, et al. Smoke-free car legislation and student exposure to smoking. Pediatrics. 2018;141(suppl 1):S40–S50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cruz TB, McConnell R, Low BW, et al. Tobacco marketing and subsequent use of cigarettes, e-cigarettes and hookah in adolescents [published online ahead of print May 28, 2018]. Nicotine Tob Res. doi: 10.1093/ntr/nty107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hébert ET, Vandewater EA, Businelle MS, Harrell MB, Kelder SH, Perry CL. Real time assessment of young adults’ attitudes toward tobacco messages. Tob Regul Sci. 2018;4(1):644–655 [DOI] [PMC free article] [PubMed] [Google Scholar]