Between 2011 and 2015, there was an increase in psychiatric ED visits among youth 6 to 24 years of age in the United States.
Abstract
Video Abstract
BACKGROUND:
Visits to the emergency department (ED) for psychiatric purposes are an indicator of chronic and acute unmet mental health needs. In the current study, we examined if psychiatric ED visits among individuals 6 to 24 years of age are increasing nationwide.
METHODS:
ED data came from the 2011–2015 National Hospital Ambulatory Medical Care Survey, a national survey of ED visits across the United States. Psychiatric ED visits were identified by using the International Classification of Diseases, Ninth Revision and reason-for-visit codes. Survey-weighted logistic regression analyses were employed to examine trends in as well as correlates of psychiatric ED visits. Data from the US Census Bureau were used to examine population rates.
RESULTS:
Between 2011 and 2015, there was a 28% overall increase (from 31.3 to 40.2) in psychiatric ED visits per 1000 youth in the United States. The largest increases in psychiatric ED visits per 1000 US youth were observed among adolescents (54%) and African American (53%) and Hispanic patients (91%). A large increase in suicide-related visits (by 2.5-fold) was observed among adolescents (4.6–11.7 visits per 1000 US youth). Although psychiatric ED visits were long (51% were ≥3 hours in length), few (16%) patients were seen by a mental health professional during their visit.
CONCLUSIONS:
Visits to the ED for psychiatric purposes among youth are rising across the United States. Psychiatric expertise and effective mental health treatment options, particular those used to address the rising suicide epidemic among adolescents, are needed in the ED.
What’s Known on This Subject:
The emergency department (ED) is the national safety net for individuals with chronic and acute mental health issues. Monitoring trends in ED visits is critical because they can signal important changes in population health.
What This Study Adds:
Between 2011 and 2015, psychiatric ED visits among youth in the United States increased. This trend was largely driven by adolescents, and youth of color. An increase in visits related to self-injury and suicide was observed among adolescents.
It is estimated that >1 in 10 youth in the United States has a serious psychiatric disorder.1 Many of these children, however, never receive treatment.2 For those in crisis (eg, suicide ideation, aggression, and psychosis) or without accessible connections to the mental health care system, the emergency department (ED) has become the national safety net because this setting is obligated to treat all patients regardless of day or time, reason for referral, or availability of financial payment. This status as a frontline provider has led EDs to the breaking point, in which EDs are overcrowded and shutting their doors because of lack of financial protections.3
Because the ED is designed as an urgent medical facility, this setting often lacks the resources required to identify and manage psychiatric populations.4,5 Discharge planning is also a challenge because the wait for outpatient psychiatry is long, and inpatient psychiatric beds are a dwindling resource.6–8 As a result, ED mental health visits are associated with long wait times, which are due in part to psychiatric “boarding” (in which a patient waits in the ED for an inpatient bed).9,10
Pediatric ED visits have steadily increased over the last several decades.11–16 The most recent estimates suggest that 5% to 7% of all pediatric ED visits in the United States are related to mental health and/or substance abuse.12,16 This is likely an underestimate because passive mental health reporting, in which providers do not actively screen patients for mental health issues, is the routine procedure in the ED.4,17 The increased presence of pediatric psychiatric visits in the ED has become such a public health problem that it prompted a 2016 joint statement by the American Academy of Pediatrics and the American College of Emergency Physicians.4,18 In that report, the authors provide clinical recommendations regarding best practices when managing youth with mental health issues in the ED.4,18
Less is known about psychiatric ED use among transition-aged adults. Most research has been focused on youth (<17 years of age) or adults (≥18 years), lumping young adults (18–24 years) with older populations who have substantially different mental health profiles.19,20 Investigating psychiatric ED use among young adults is critical because many serious psychiatric disorders emerge in young adulthood, and both mental health and substance abuse–related problems are directly related to the top 3 leading causes of death for young adults (ie, injury, suicide, and homicide).21,22
Understanding psychiatric ED use among youth and young adults is important because the ED is an entryway to the mental health system for many children and families.23 These visits present a unique opportunity to recognize and initiate treatment services for previously unidentified mental health problems.4 The ED is also at the front lines of the nation’s substance abuse and suicide epidemics, which uniquely situates them to intervene in these public health crises.24,25
For the current study, we have 3 aims. First, we provide updated estimates on changes in psychiatric ED visits in the United States (between 2011 and 2015) among youth 6 to 24 years of age. Second, we assessed if there were disparate trends in psychiatric ED visits over time across different age, sex, and racial and/or ethnic groups. Third, we examined correlates of psychiatric ED visits across the different age, sex, and racial and/or ethnic groups. Particular attention was paid to suicidal-attempt and self-injury visits.
Methods
Data for this study primarily came from the 2011–2015 National Hospital Ambulatory Medical Care Survey (NHAMCS).26 The NHAMCS is a cross-sectional national probability survey of ED visits across the United States. Survey sampling weights allow for generalization of NHAMCS estimates to all nonfederal, short-stay, and general hospital EDs across the United States. The weights also account for nonresponse by EDs (those that did not participate in the NHAMCS survey), which averaged 11.9% over the 5-study year period.27
Data for the NHAMCS are collected during a randomly selected 4-week period of the year. Information from patient medical records is abstracted by trained staff members who use standardized forms. All NHAMCS data are deidentified and publicly available, which allows for this study to be exempt from the local institutional review board. Beyond the NHAMCS, the only other data used in this study were retrieved from the US Census Bureau.28 Census data (from 2011 to 2015) were used for calculating population-based rates of psychiatric ED visits per 1000 youth in the United States.
Variables
Identification of Psychiatric ED Visits
The primary study outcome was probability of a psychiatric ED visit. These visits were identified on the basis of the following: (1) diagnoses classified by using the International Classification of Diseases, Ninth Revision codes29 and (2) reason for visit (RFV) (record of the patient’s reason for visiting the ED).
Psychiatric ED visits were identified when any of the 3 RFV or ICD-9 codes were used to identify a psychiatric disorder, psychiatric RFV, or a mental health procedure. Psychiatric diagnoses, RFVs, and procedures were identified by using preestablished criteria by researchers from the National Center for Health Statistics (NCHS).16 Visits were classified as mood (ie, depression, mania and/or hypomania, or anxiety), behavioral (ie, aggression or conduct problems), substance use disorder (SUD), psychosis, or other psychiatric reasons (ie, personality disorder or a mental health procedure). For suicide attempt and intentional self-harm, these visits were identified separately by using RFV (5818.0, 5820.0, and 5820.1) and V codes (V62.84).16
Demographic Characteristics
Demographic variables related to the child included age, US region, sex (male or female) and race and/or ethnicity (a 4-level variable created by the NCHS; see Table 1 for details).
TABLE 1.
Age-Related Characteristics of Psychiatric ED Visits Among Youth in the United States
| 6–11 y | 12–17 y | 18–24 y | Overall | |
|---|---|---|---|---|
| Count of total visits (weighted) | 35 497 171 | 39 393 222 | 81 201 713 | 156 092 106 |
| Count of psychiatric ED visits (weighted) | 825 616 | 3 881 608 | 8 434 362 | 13 141 586 |
| Estimated youth in the United States, 2011–2015 | 123 138 640 | 125 212 948 | 154 601 355 | 402 952 943 |
| Psychiatric ED visits, % of all visits (count) | ||||
| 2011 | 2.0 (133 225) | 9.0 (727 111) | 9.4 (1 655 670) | 7.8 (2 516 006) |
| 2012 | 2.0 (132 235) | 8.2 (607 112) | 9.7 (1 575 440) | 7.6 (2 314 787) |
| 2013 | 2.8 (179 852) | 9.4 (675 333) | 9.8 (1 507 892) | 8.1 (2 363 077) |
| 2014 | 2.3 (181 471) | 9.1 (755 863) | 10.7 (1 770 647) | 8.3 (2 707 981) |
| 2015 | 2.5 (198 833) | 13.2 (1 116 189) | 12.5 (1 924 713) | 10.1 (3 239 735) |
| Psychiatric ED visits per 1000 US youth | ||||
| 2011 | 5.4 | 28.9 | 54.0 | 31.3 |
| 2012 | 5.4 | 24.2 | 50.9 | 28.7 |
| 2013 | 7.3 | 27.0 | 48.5 | 29.3 |
| 2014 | 7.3 | 30.2 | 57.0 | 33.5 |
| 2015 | 8.0 | 44.6 | 62.5 | 40.2 |
| Region, % of psychiatric ED visits | ||||
| Northeast | 29.6 | 20.6 | 18.8 | 20.0 |
| Midwest | 22.4 | 25.9 | 24.7 | 25.0 |
| South | 29.3 | 33.9 | 33.7 | 33.5 |
| West | 18.7 | 19.5 | 22.7 | 21.5 |
| Sex,* % | ||||
| Female | 28.4 | 56.7 | 49.7 | 50.0 |
| Male | 71.6 | 43.3 | 50.8 | 50.0 |
| Race, % | ||||
| Non-Hispanic White | 55.7 | 58.6 | 64.3 | 62.1 |
| Non-Hispanic African American | 22.9 | 19.4 | 19.7 | 19.8 |
| Hispanic | 16.5 | 19.8 | 13.8 | 15.8 |
| Non-Hispanic other | 4.9 | 2.1 | 2.1 | 2.3 |
| Insurance,* % | ||||
| Private | 32.2 | 38.6 | 32.5 | 34.3 |
| Public | 56.4 | 52.7 | 38.0 | 43.6 |
| Self-pay | 6.7 | 5.9 | 21.2 | 15.9 |
| Other | 4.6 | 2.8 | 8.3 | 6.4 |
| Visit on a weekend,* % | ||||
| No | 83.5 | 76.7 | 71.9 | 74.0 |
| Yes | 16.5 | 23.3 | 28.1 | 26.0 |
| Arrival time,* % | ||||
| Morning (<11 am) | 18.6 | 20.1 | 32.7 | 28.1 |
| Afternoon (11 am–4 pm) | 28.3 | 31.7 | 29.2 | 29.9 |
| Evening (5 pm–12 am) | 53.0 | 48.2 | 38.0 | 42.0 |
| Urgent,* % | ||||
| No | 34.3 | 21.9 | 33.5 | 30.1 |
| Yes | 65.7 | 78.1 | 66.5 | 69.9 |
| Arrive by ambulance,*% | ||||
| No | 85.9 | 78.7 | 71.2 | 25.6 |
| Yes | 14.1 | 21.3 | 28.8 | 74.4 |
| Length of visit, % | ||||
| <90 min | 18.5 | 17.4 | 21.9 | 20.4 |
| 90–179 min | 25.7 | 28.3 | 28.9 | 28.5 |
| 180–359 min | 36.9 | 30.5 | 28.3 | 29.4 |
| ≥6 h | 18.8 | 23.7 | 21.1 | 21.7 |
| Mental health provider seen,* % | ||||
| No | 84.5 | 75.1 | 87.4 | 83.5 |
| Yes | 15.4 | 24.9 | 12.6 | 16.5 |
| Admit to hospital,* % | ||||
| No | 81.6 | 74.6 | 84.3 | 81.3 |
| Yes or transfer to another hospital | 6.3 | 8.9 | 9.2 | 8.9 |
| Transfer or admit to a psychiatric facility | 12.1 | 16.4 | 6.5 | 9.8 |
| Any psychiatric diagnosis or RFV,*,a % | ||||
| Mood* | 45.4 | 62.7 | 48.5 | 52.5 |
| Behavior* | 42.3 | 19.7 | 8.2 | 13.7 |
| SUD* | 4.5 | 26.6 | 50.7 | 40.6 |
| Psychosis | 6.2 | 5.1 | 7.3 | 6.6 |
| Suicide attempt or self-injury* | 4.2 | 22.7 | 8.9 | 12.7 |
| Other* | 40.8 | 39.7 | 24.8 | 30.2 |
| Count of psychiatric diagnoses or RFVs, mean | 1.39 | 1.53 | 1.39 | 1.42 |
| Primary diagnosis is psychiatric,* % | ||||
| No | 37.9 | 23.3 | 38.9 | 34.2 |
| Yes | 62.1 | 76.7 | 61.1 | 65.8 |
Reflects the presence of any of the listed diagnoses or RFVs.
P < .05.
Visit Characteristics
A host of visit-related descriptors were available. These included insurance type, time of day, day of visit, whether a mental health professional was seen during the visit, whether the patient arrived via ambulance, and urgency of visit (dichotomized as urgent [emergent, immediate, and urgent] versus not [semiurgent and not urgent]). Length of visit was grouped in quartiles. Disposition or whether the visit resulted in a hospitalization was classified as either admission to a medical unit, admission to a psychiatric unit, or other (eg, discharge from the hospital). See Table 1 for details.
Missing Data
Prevalent missing data (>5%) were observed for urgency of visit (22%), race and/or ethnicity (21%), and insurance type (8%). Imputation procedures, conducted by the NCHS,30 were used for race and/or ethnicity only. In the multivariate analyses, a missing data indicator was included for each of these variables (excluding race and/or ethnicity) for the purposes of retaining the full sample.
Analysis
Trends in psychiatric ED visits are reported as proportions (number of psychiatric ED visits over total ED visits) and counts by using the NHAMCS data. Rates (visits per 1000 youth in the United States) and ratios of rates (reflecting percent change) were calculated by using the census data. To address the first study question, a logistic regression model was used to examine changes in the odds of a psychiatric ED visit over time among youth 6 to 24 years of age. For the second study question, separate logistic models were used to test whether there was an increase in the odds of a psychiatric ED visit over time for each individual age, sex, and racial and/or ethnic group (for a total of 9 separate models).
For the third study question, a series of regression models were employed to identify differences in the demographic and visit-related factors associated with age, sex, and race and/or ethnicity. These analyses were limited to psychiatric ED visits only, with the group (age, sex, or race) serving as the outcome variable. For sex, a logistic regression model was employed, whereas a multinomial regression model was used for age and race and/or ethnicity because there were multiple discreet categories. As an example, the relative risk ratio for evening (from the multinomial model; see Table 2) can be interpreted as the relative probability of a psychiatric visit occurring in the evening (rather than the morning), is 2.35 times more likely to occur among children compared with young adults.
TABLE 2.
Multivariate Analysis of Correlates of Psychiatric ED Visits Among Age Groups
| Children | Adolescents | |||
|---|---|---|---|---|
| RRR | 95% CI | RRR | 95% CI | |
| Year | 1.04 | 0.89 to 1.22 | 1.04 | 0.94 to 1.14 |
| Region | ||||
| Northeast | Reference | Reference | Reference | Reference |
| Midwest | 0.56 | 0.29 to 1.09 | 0.99 | 0.67 to 1.45 |
| South | 0.67 | 0.37 to 1.23 | 1.04 | 0.69 to 1.59 |
| West | 0.49* | 0.27 to 0.90 | 0.74 | 0.49 to 1.12 |
| Sex | ||||
| Female | Reference | Reference | Reference | Reference |
| Male | 2.65* | 1.67 to 4.19 | 0.78 | 0.61 to 0.99 |
| Race and/or ethnicity | ||||
| White, non-Hispanic | Reference | Reference | Reference | Reference |
| African American, non-Hispanic | 1.28 | 0.81 to 2.03 | 1.10 | 0.79 to 1.55 |
| Hispanic | 1.27 | 0.64 to 2.52 | 1.74* | 1.22 to 2.47 |
| Other | 2.96 | 0.63 to 13.95 | 1.21 | 0.54 to 2.74 |
| Insurance | ||||
| Private | Reference | Reference | Reference | Reference |
| Public | 1.42 | 0.79 to 2.57 | 1.03 | 0.74 to 1.43 |
| Self-pay | 0.30* | 0.10 to 0.92 | 0.22* | 0.14 to 0.34 |
| Other | 0.48 | 0.14 to 1.70 | 0.26* | 0.12 to 0.54 |
| Visit on a weekend | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.57* | 0.15 to 0.94 | 0.86 | 0.63 to 1.18 |
| Arrival time | ||||
| Morning (<11 am) | Reference | Reference | Reference | Reference |
| Afternoon (11 am–4 pm) | 1.74 | 0.91 to 3.14 | 1.69* | 1.19 to 2.39 |
| Evening (5 pm–12 am) | 2.35* | 1.34 to 4.12 | 2.04* | 1.49 to 2.80 |
| Urgent | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.85 | 0.50 to 1.44 | 1.76* | 1.24 to 2.50 |
| Length of visit | 0.99 | 0.99 to 1.00 | 1.00 | 0.99 to 1.00 |
| Arrive by ambulance | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.39* | 0.21 to 0.75 | 0.71* | 0.54 to 0.93 |
| Mental health provider seen | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 1.06 | 0.32 to 2.11 | 2.08* | 1.46 to 2.96 |
| Admit to hospital | ||||
| No | Reference | Reference | Reference | Reference |
| Yes or transfer to another hospital | 0.58 | 0.31 to 1.11 | 1.06 | 0.67 to 1.69 |
| Transfer or admit to a psychiatric facility | 1.48 | 0.61 to 3.58 | 2.47* | 1.49 to 4.11 |
| Psychiatric diagnosis or RFVa | ||||
| Mood | 0.83 | 0.50 to 1.37 | 1.57* | 1.18 to 2.08 |
| Behavior | 7.64* | 4.62 to 12.62 | 2.53* | 1.79 to 3.56 |
| SUDs | 0.05* | 0.02 to 0.13 | 0.41* | 0.30 to 0.54 |
| Psychosis | 0.57 | 0.22 to 1.47 | 0.67 | 0.44 to 1.02 |
| Suicide attempt or intentional self-injury | 0.47 | 0.19 to 1.14 | 3.19* | 2.27 to 4.48 |
| Other | 1.68* | 1.12 to 2.53 | 1.87* | 1.43 to 2.43 |
| Count of diagnoses and/or RFVs | 0.86 | 0.61 to 1.20 | 1.30* | 1.09 to 1.54 |
| Primary diagnosis is psychiatric | ||||
| No | Reference | Reference | Reference | Reference |
| Yes | 0.96 | 0.61 to 1.51 | 2.21* | 1.66 to 2.93 |
RRR, relative risk ratio.
Reflects the presence of any of the listed diagnoses or RFVs; young adults served as the reference group.
P < .05.
All models used to assess predictors of psychiatric ED visits included year, region, sex, arrival time, weekend (versus weekday), and insurance type as covariates. All other variables (eg, arrival by ambulance, urgency, length of visit, and diagnosis) were examined sequentially in individual models to avoid problems with multicollinearity. All regression models were examined at the visit level (by using the NHAMCS) among those with and/or without psychiatric needs. Whole population data from the census were not included in the models. All analyses were conducted in Stata 15.0 (Stata Corp, College Station, TX) by using the survey sampling weights.
Results
Overall Trends in Psychiatric ED Visits
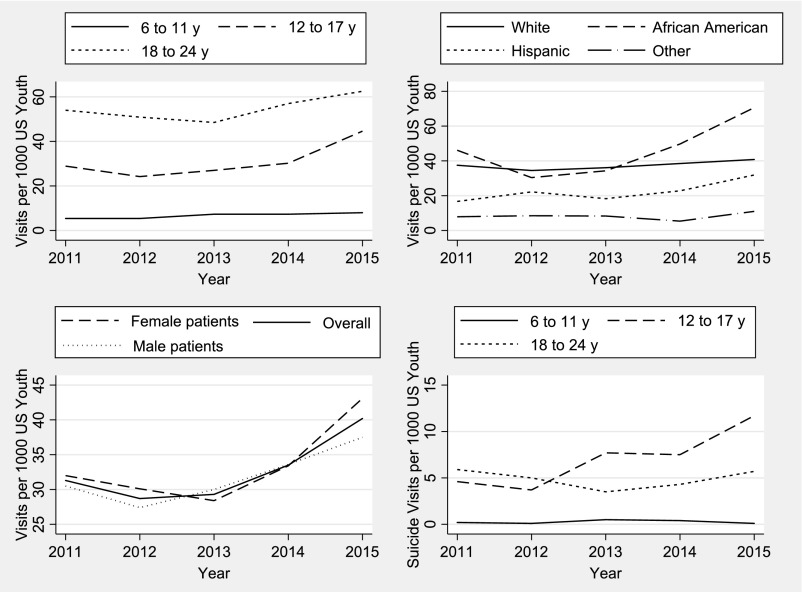
Table 1 displays the 5-year trends in psychiatric ED visits by age group. Overall, there was a significant increase in the odds of a visit over time (odds ratio [OR]: 1.07; 95% confidence interval [CI]: 1.01 to 1.13; P = .01). Shown in Fig 1 and Table 1, increasing rates of psychiatric ED visits among youth in the United States (from 31.3 to 40.2 per 1000; a 28% increase) was also supported.
FIGURE 1.
Age, race, and sex trends in psychiatric and suicide-related ED visits.
Age Trends in Psychiatric ED Visits
For children, there was no significant change over time in the probability of a psychiatric ED visit (OR: 1.05; 95% CI: 0.92 to 1.21; P = .44). There was a rise (5.2–8.0 psychiatric ED visits per 1000 US children; a 53% increase) by using whole population data as the denominator, which do not take into account the increase in ED visits overall.
For adolescents, psychiatric ED visits were much more likely than for children (OR: 4.62; 95% CI: 3.73 to 5.72; P < .001). Young adults were also much more likely to visit the ED for psychiatric purposes compared with children (OR: 4.93; 95% CI: 3.99 to 6.10; P < .001), although there was no difference when compared with adolescents (OR: 1.07; 95% CI: 0.92 to 1.23; P = .37). Notably, young adults had the highest overall population rates.
The probability of a psychiatric ED visit significantly increased over time for adolescents (OR: 1.11; 95% CI: 1.02 to 1.21; P = .01) and young adults (OR: 1.08; 95% CI: 1.01 to 1.15; P = .03). By using census data, a larger increase was observed for adolescents (28.9–44.6 psychiatric ED visits per 1000 youth in the United States; a 54% increase) than for young adults (54.0–62.4 per 1000 youth in the United States; a 15% increase). See Table 1 for details.
Race and/or Ethnicity Trends in Psychiatric ED Visits
Table 3 reveals trends in psychiatric ED visits across racial and ethnic groups. No significant change in the odds of a psychiatric ED visit was observed over time for the white group (OR: 1.03; 95% CI: 0.97 to 1.10; P = .31). However, a significant increase was observed among those in the African American (OR: 1.16; 95% CI: 1.03 to 1.30; P = .01) and Hispanic groups (OR: 1.12; 95% CI: 1.01 to 1.24; P = .02). Both of these findings remained significant even after adjusting for insurance status. No difference was found among the “other” race group (OR: 1.06, 95% CI: 0.84 to 1.35, P = .59). The census data supported increasing rates among African American (46.1–70.6 per 1000 youth, a 53% increase) and Hispanic patients (16.7–31.9, a 91% increase), whereas these rates remained flat among non-Hispanic white patients (37.5–40.8; a 9% increase) and rare among all in the “other” racial category (7.9–11.0; a 39% increase).
TABLE 3.
Race- and Ethnicity-Related Characteristics of Psychiatric ED Visits Among Youth in the United States
| Non-Hispanic White | Non-Hispanic African American | Hispanic | Non-Hispanic Other | |
|---|---|---|---|---|
| Count of total visits (weighted) | 75 572 719 | 35 939 326 | 27 564 070 | 3 874 405 |
| Count of psychiatric ED visits (weighted) | 8 162 101 | 2 607 369 | 2 074 122 | 297 994 |
| Estimated youth in the United States, 2011–2015 | 217 594 589 | 56 413 412 | 92 679 177 | 36 265 765 |
| Psychiatric ED visits, % of all visits (count)* | ||||
| 2011 | 9.3 (1 629 561) | 6.3 (519 859) | 5.7 (309 237) | 6.2 (57 349) |
| 2012 | 9.3 (1 499 311) | 4.9 (342 599) | 6.5 (411 193) | 7.1 (61 684) |
| 2013 | 9.8 (1 576 000) | 5.9 (387 165) | 6.1 (339 747) | 7.9 (60 165) |
| 2014 | 10.1 (1 682 520) | 6.0 (562 364) | 7.2 (423 844) | 5.5 (39 253) |
| 2015 | 10.3 (1 774 709) | 10.8 (795 382) | 9.1 (590 101) | 8.9 (79 543) |
| Psychiatric ED visits per 1000 US youth | ||||
| 2011 | 37.5 | 46.1 | 16.7 | 7.9 |
| 2012 | 34.5 | 30.4 | 22.2 | 8.5 |
| 2013 | 36.1 | 34.3 | 18.3 | 8.3 |
| 2014 | 38.5 | 49.7 | 22.8 | 5.4 |
| 2015 | 40.8 | 70.6 | 31.9 | 11.0 |
| Region,* % of all psychiatric ED visits | ||||
| Northeast | 19.8 | 19.4 | 21.1 | 24.1 |
| Midwest | 28.1 | 26.8 | 11.8 | 19.3 |
| South | 32.7 | 44.0 | 24.7 | 24.8 |
| West | 19.4 | 9.8 | 43.1 | 31.8 |
| Youth, % | ||||
| 6–11 | 5.6 | 7.2 | 6.6 | 13.6 |
| 12–17 | 27.9 | 28.9 | 37.1 | 27.6 |
| 18–24 | 66.5 | 63.9 | 56.3 | 58.8 |
| Sex, % | ||||
| Female | 51.8 | 47.3 | 47.6 | 45.3 |
| Male | 48.2 | 52.7 | 52.4 | 54.6 |
| Insurance,* % | ||||
| Private | 41.7 | 18.6 | 22.6 | 40.4 |
| Public | 37.5 | 54.3 | 56.0 | 35.6 |
| Self-pay | 15.1 | 19.7 | 14.6 | 9.4 |
| Other | 5.7 | 7.4 | 6.8 | 14.5 |
| Visit on a weekend,* % | ||||
| No | 73.4 | 74.5 | 76.8 | 69.1 |
| Yes | 26.6 | 25.5 | 23.2 | 30.9 |
| Arrival time,* % | ||||
| Morning (<11 am) | 29.4 | 26.6 | 25.2 | 27.4 |
| Afternoon (11 am–4 pm) | 28.7 | 31.5 | 32.7 | 26.9 |
| Evening (5 pm–12 am) | 41.9 | 41.9 | 42.1 | 45.7 |
| Urgent* | ||||
| No | 28.3 | 37.5 | 27.8 | 32.4 |
| Yes | 71.7 | 62.4 | 72.2 | 67.6 |
| Length of visit, % | ||||
| <90 min | 20.9 | 20.5 | 17.3 | 25.7 |
| 90–179 min | 30.6 | 25.9 | 25.0 | 16.5 |
| 180–359 min | 28.3 | 28.4 | 35.6 | 27.9 |
| ≥6 h | 20.2 | 25.2 | 22.1 | 29.9 |
| Arrive by ambulance,* % | ||||
| No | 24.0 | 28.2 | 27.4 | 36.0 |
| Yes | 76.0 | 71.8 | 72.5 | 64.0 |
| Mental health provider seen, % | ||||
| No | 82.7 | 84.6 | 84.5 | 92.1 |
| Yes | 17.3 | 15.4 | 15.5 | 8.0 |
| Admit to hospital, % | ||||
| No | 80.5 | 81.8 | 84.0 | 80.3 |
| Yes or transfer to another hospital | 9.8 | 7.6 | 6.5 | 13.0 |
| Transfer or admit to a psychiatric facility | 9.7 | 10.6 | 9.5 | 6.8 |
| Psychiatric diagnoses or RFV,*,a % | ||||
| Mood | 54.0 | 47.4 | 51.6 | 63.4 |
| Behavior* | 11.9 | 18.6 | 16.9 | 6.7 |
| SUD* | 43.7 | 37.1 | 35.6 | 24.1 |
| Psychosis | 6.2 | 9.3 | 5.7 | 2.7 |
| Suicide attempt or self-injury | 12.9 | 11.4 | 12.8 | 20.2 |
| Other | 29.7 | 33.0 | 27.5 | 36.4 |
| Count of psychiatric diagnoses or RFVs, mean* | 1.45 | 1.45 | 1.37 | 1.33 |
| Primary diagnosis is psychiatric,* % | ||||
| No | 32.8 | 35.2 | 37.9 | 37.7 |
| Yes | 67.2 | 64.8 | 62.1 | 62.3 |
Reflects the presence of any of the listed diagnoses or RFVs.
P < .05.
Sex Trends in Psychiatric ED Visits
Table 4 reveals trends in psychiatric ED visits stratified by sex. There was a slight increase in the probability over time for female patients (OR: 1.08; 95% CI: 1.01 to 1.16; P = .02). No significant time trends were observed for male patients (OR: 1.06; 95% CI: 0.99 to 1.13; P = .08). The probability of a psychiatric ED visit was increased in male patients compared with female patients (OR: 1.30; 95% CI: 1.17 to 1.45). Rates per 1000 youth also increased slightly more for female patients (32.0–43.1; a 34% increase) than for male patients (30.5–37.5; a 23% increase).
TABLE 4.
Sex-Related Characteristics of Psychiatric ED Visits Among Youth in the United States
| Female Sex | Male Sex | |
|---|---|---|
| Count of total visits (weighted) | 87 687 560 | 68 404 546 |
| Count of psychiatric ED visits (weighted) | 6 582 345 | 6 559 241 |
| Estimated youth in the United States, 2011–2015 | 196 847 905 | 206 105 038 |
| Psychiatric ED visits*, % of all visits (count) | ||
| 2011 | 6.9 (1 259 925) | 8.9 (1 256 081) |
| 2012 | 6.9 (1 184 067) | 8.6 (1 130 720) |
| 2013 | 6.7 (1 122 287) | 10.0 (1 240 790) |
| 2014 | 7.4 (1 320 195) | 9.4 (1 387 786) |
| 2015 | 9.5 (1 695 871) | 11.0 (1 543 864) |
| Psychiatric ED visits per 1000 US youth | ||
| 2011 | 32.0 | 30.5 |
| 2012 | 30.1 | 27.4 |
| 2013 | 28.4 | 30.0 |
| 2014 | 33.4 | 33.6 |
| 2015 | 43.1 | 37.5 |
| Region,* % of all psychiatric ED visits | ||
| Northeast | 18.8 | 21.3 |
| Midwest | 24.8 | 25.1 |
| South | 37.8 | 29.2 |
| West | 18.8 | 24.5 |
| Youth,* y, % | ||
| 6–11 | 3.6 | 9.0 |
| 12–17 | 33.4 | 25.6 |
| 18–24 | 63.0 | 65.4 |
| Race, % | ||
| Non-Hispanic white | 64.2 | 60.0 |
| Non-Hispanic African American | 18.7 | 20.9 |
| Hispanic | 15.0 | 16.6 |
| Non-Hispanic other | 2.1 | 2.5 |
| Insurance, % | ||
| Private | 34.1 | 34.5 |
| Public | 46.4 | 40.6 |
| Self-pay | 14.5 | 17.0 |
| Other | 5.0 | 7.9 |
| Visit on a weekend, % | ||
| No | 73.4 | 74.6 |
| Yes | 26.5 | 25.4 |
| Arrival time, % | ||
| Morning (<11 am) | 28.2 | 28.1 |
| Afternoon (11 am–4 pm) | 31.6 | 28.1 |
| Evening (5 pm–12 am) | 40.2 | 43.8 |
| Urgent, % | ||
| No | 31.7 | 28.4 |
| Yes | 68.2 | 71.6 |
| Length of visit, % | ||
| <90 min | 20.8 | 19.9 |
| 90–179 min | 28.4 | 28.5 |
| 180–359 min | 29.5 | 29.4 |
| ≥6 h | 21.2 | 22.2 |
| Arrive by ambulance, % | ||
| No | 25.4 | 25.9 |
| Yes | 74.6 | 74.1 |
| Mental health provider seen, % | ||
| No | 82.5 | 84.5 |
| Yes | 17.4 | 15.4 |
| Admit to hospital, % | ||
| No | 81.9 | 80.7 |
| Yes or transfer to another hospital | 7.4 | 10.4 |
| Transfer or admit to a psychiatric facility | 10.7 | 8.9 |
| Psychiatric diagnosis or RFV,*,a % | ||
| Mood* | 59.1 | 45.9 |
| Behavior | 12.1 | 15.3 |
| SUD* | 37.1 | 44.2 |
| Psychosis* | 5.1 | 8.2 |
| Suicide attempt or self-injury | 14.6 | 10.9 |
| Other | 30.1 | 30.3 |
| Count of psychiatric diagnoses or RFVs, mean | 1.44 | 1.44 |
| Primary diagnosis is psychiatric, % | ||
| No | 35.1 | 33.4 |
| Yes | 64.9 | 66.6 |
Reflects the presence of any of the listed diagnoses or RFVs
P < .05
Correlates of Psychiatric ED Visits
Age Group
Child and visit-related characteristics of psychiatric ED visits across age groups are shown in Table 1. In the multivariate analyses (Table 2), children and adolescents were both less likely to have self-pay insurance, arrive by ambulance, and have an SUD diagnosis compared with young adults. Children visiting the ED were also less likely to live in the West and have a visit on the weekend compared with young adults. Both children and adolescents were more likely to have an evening visit; and adolescents only were more likely to have an afternoon visit and less likely to have the “other” insurance type (all P < .05).
Adolescents who visited the ED were more likely to be Hispanic, have an urgent visit, see a mental health provider, and be transferred or admitted to a psychiatric facility compared with young adults. In terms of diagnoses, adolescents were more likely to have a primary psychiatric diagnosis related to the visit along with an increasing number of diagnoses. Adolescents were also more likely to have a mood, behavioral, suicide, and other diagnosis or RFV compared with young adults (all: P < .05). Children were far more likely to have a behavioral diagnosis or RFV and slightly more likely to have an “other” diagnosis. See Table 2 for details.
Race and/or Ethnicity
Characteristics of psychiatric ED visits across racial and/or ethnic groups are shown in Table 3. In the multivariate analyses (Table 5), white patients served as the reference group. African American patients were less likely to have a visit in the Western region of the United States, have a visit that was deemed urgent, and present with an SUD. They were more likely to have an insurance type other than private and have a behavioral problem coded as a diagnosis or RFV. Hispanic patients were less likely to have a visit occur in the Midwest and had a fewer number of diagnoses coded for their visit, whereas they were more likely to have a visit in the Western part of the United States and have public or self-pay insurance. The only significant difference for the “other” racial group was that they were less likely to have an SUD associated with their visit (all: P < .05).
TABLE 5.
Multivariate Analysis of Correlates of Psychiatric ED Visits Among Racial and Ethnic Groups
| African American | Hispanic | Other | ||||
|---|---|---|---|---|---|---|
| RRR | 95% CI | RRR | 95% CI | RRR | 95% CI | |
| Year | 1.14* | 1.03 to 1.27 | 1.10 | 0.98 to 1.24 | 1.00 | 0.77 to 1.30 |
| Age group, y | ||||||
| 6–11 | Reference | Reference | Reference | Reference | Reference | Reference |
| 12–17 | 0.86 | 0.50 to 1.46 | 1.37 | 0.68 to 2.76 | 0.43 | 0.08 to 2.40 |
| 18–24 | 0.77 | 0.49 to 1.21 | 0.78 | 0.38 to 1.58 | 0.35 | 0.07 to 1.73 |
| Region | ||||||
| Northeast | Reference | Reference | Reference | Reference | Reference | Reference |
| Midwest | 0.93 | 0.52 to 1.69 | 0.35* | 0.20 to 0.61 | 0.59 | 0.15 to 2.39 |
| South | 1.45 | 0.85 to 2.50 | 0.73 | 0.41 to 1.27 | 0.65 | 0.23 to 1.77 |
| West | 0.49* | 0.26 to 0.95 | 2.11* | 1.31 to 3.41 | 1.35 | 0.66 to 2.81 |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 1.26 | 0.99 to 1.61 | 1.15 | 0.83 to 1.59 | 1.08 | 0.58 to 2.01 |
| Insurance | ||||||
| Private | Reference | Reference | Reference | Reference | Reference | Reference |
| Public | 3.36* | 2.23 to 5.05 | 2.72* | 1.85 to 4.00 | 0.97 | 0.35 to 2.72 |
| Self-pay | 2.99* | 1.81 to 4.92 | 2.42* | 1.48 to 3.93 | 0.77 | 0.28 to 2.07 |
| Other | 2.93* | 1.56 to 5.50 | 1.84 | 0.91 to 5.02 | 2.68 | 0.98 to 4.53 |
| Visit on a weekend | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.01 | 0.72 to 1.42 | 0.87 | 0.59 to 1.26 | 1.31 | 0.65 to 2.63 |
| Arrival time | ||||||
| Morning (<11 am) | Reference | Reference | Reference | Reference | Reference | Reference |
| Afternoon (11 am–4 pm) | 1.00 | 0.69 to 1.44 | 1.13 | 0.73 to 1.77 | 0.97 | 0.41 to 2.31 |
| Evening (5 pm–12 am) | 1.01 | 0.73 to 1.42 | 1.06 | 0.72 to 1.56 | 1.10 | 0.53 to 2.31 |
| Urgent | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 0.67* | 0.45 to 0.97 | 0.89 | 0.39 to 2.01 | 0.94 | 0.41 to 2.14 |
| Length of visit | 1.13 | 0.99 to 1.28 | 1.08 | 0.96 to 1.21 | 0.98 | 0.71 to 1.36 |
| Arrive by ambulance | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.30 | 0.94 to 1.80 | 1.23 | 0.85 to 1.75 | 1.88 | 0.85 to 4.16 |
| Mental health provider seen | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 0.87 | 0.61 to 1.23 | 0.81 | 0.55 to 1.19 | 0.38 | 0.13 to 1.13 |
| Admit to hospital | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes or transfer | 0.80 | 0.52 to 1.24 | 0.69 | 0.40 to 1.20 | 1.35 | 0.50 to 3.64 |
| Psychiatric facility | 0.97 | 0.58 to 1.63 | 0.69 | 0.42 to 1.11 | 0.66 | 0.22 to 1.96 |
| Psychiatric diagnosis or RFVa | ||||||
| Mood | 0.77 | 0.58 to 1.02 | 0.91 | 0.67 to 1.22 | 1.62 | 0.73 to 3.64 |
| Behavior | 1.60* | 1.09 to 2.34 | 1.34 | 0.87 to 2.06 | 0.41 | 0.14 to 1.23 |
| SUDs | 0.74* | 0.56 to 0.97 | 0.73 | 0.52 to 1.01 | 0.39* | 0.20 to 0.69 |
| Psychosis | 1.38 | 0.89 to 2.50 | 0.78 | 0.44 to 1.41 | 0.42 | 0.15 to 1.13 |
| Suicide attempt or self-injury | 0.91 | 0.56 to 1.42 | 0.82 | 0.55 to 1.23 | 1.82 | 0.88 to 3.74 |
| Other | 1.17 | 0.87 to 1.57 | 0.80 | 0.55 to 1.16 | 1.33 | 0.68 to 2.62 |
| Count of diagnoses and/or RFVs | 0.94 | 0.78 to 1.15 | 0.75* | 0.60 to 0.94 | 0.80 | 0.37 to 1.71 |
| Primary diagnosis is psychiatric | 0.93 | 0.69 to 1.27 | 0.76 | 0.52 to 1.11 | 1.44 | −0.01 to 2.5 |
RRR, relative risk ratio.
Reflects the presence of any of the listed diagnoses or RFVs; non-Hispanic white patients served as the reference group.
P < .05.
Sex
Differences between male and female patients, in terms of demographic and visit-related characteristics of psychiatric ED visits, are shown in Table 4. In the multivariate models (Table 6), male patients were more likely to be younger and visit the ED for an SUD or psychosis compared with female patients. On the other hand, psychiatric ED visits were less likely to occur in the South among male patients.
TABLE 6.
Multivariate Analysis of Correlates of Psychiatric ED Visits Across Youth Sex
| Female Sex | Male Sex | ||
|---|---|---|---|
| OR | 95% CI | ||
| Year | Reference | 0.97 | 0.91 to 1.05 |
| Age group, y | |||
| 6–11 | Reference | Reference | Reference |
| 12–17 | Reference | 0.29* | 0.18 to 0.49 |
| 18–24 | Reference | 0.38* | 0.54 to 0.60 |
| Region | |||
| Northeast | Reference | Reference | Reference |
| Midwest | Reference | 0.95 | 0.74 to 1.21 |
| South | Reference | 0.67* | 0.51 to 0.87 |
| West | Reference | 1.20 | 0.92 to 1.80 |
| Race and/or ethnicity | |||
| White, non-Hispanic | Reference | Reference | Reference |
| African American, non-Hispanic | Reference | 1.26 | 0.99 to 1.61 |
| Hispanic | Reference | 1.14 | 0.83 to 1.58 |
| Other | Reference | 1.09 | 0.58 to 2.05 |
| Insurance | |||
| Private | Reference | Reference | Reference |
| Public | Reference | 0.81 | 0.62 to 1.06 |
| Self-pay | Reference | 1.17 | 0.78 to 1.78 |
| Other | Reference | 1.53 | 0.99 to 2.40 |
| Visit on a weekend | |||
| No | Reference | Reference | Reference |
| Yes | Reference | 0.94 | 0.77 to 1.67 |
| Arrival time | |||
| Morning (<11 am) | Reference | Reference | Reference |
| Afternoon (11 am–4 pm) | Reference | 0.89 | 0.67 to 1.19 |
| Evening (5 pm–12 am) | Reference | 1.09 | 0.84 to 1.42 |
| Urgent | |||
| No | Reference | Reference | Reference |
| Yes | Reference | 1.25 | 0.97 to 1.61 |
| Length of visit | Reference | 1.00 | 0.99 to 1.00 |
| Arrive by ambulance | |||
| No | Reference | Reference | Reference |
| Yes | Reference | 0.99 | 0.79 to 1.22 |
| Mental health provider seen | |||
| No | Reference | Reference | Reference |
| Yes | Reference | 0.89 | 0.70 to 1.13 |
| Admit to hospital | |||
| No | Reference | Reference | Reference |
| Yes or transfer to another hospital | Reference | 1.54 | 1.08 to 2.20 |
| Transfer or admit to a psychiatric facility | Reference | 0.90 | 0.65 to 1.25 |
| Psychiatric diagnosis or RFV | |||
| Mood | Reference | 0.60 | 0.48 to 75 |
| Behavior | Reference | 1.28 | 0.91 to 1.78 |
| SUDs | Reference | 1.41* | 1.13 to 1.75 |
| Psychosis | Reference | 1.70* | 1.11 to 2.61 |
| Suicide attempt or intentional self-injury | Reference | 0.75 | 0.52 to 1.06 |
| Other | Reference | 1.02 | 0.79 to 1.33 |
| Count of diagnoses and/or RFVs | Reference | 1.03 | 0.89 to 1.20 |
| Primary diagnosis is psychiatric | |||
| No | Reference | Reference | Reference |
| Yes | Reference | 1.14 | 0.91 to 1.43 |
P < .05
Suicidal-Attempt or Self-Injurious Visit
Changes in the proportion of suicide-related visits (overall and within psychiatric visits) over time are shown in Table 7; population-based rates are also provided. Overall, there was an increase in the probability of a suicidal, self-injurious visit among adolescents only (OR: 1.27; 95% CI: 1.10 to 1.48; P < .01); there was no increase over time for children or young adults (both: P > .80). There was also no significant increase in the probability of a suicide-related visit for female (OR: 1.11; 95% CI: 0.97 to 1.27) or male patients (OR: 1.15; 95% CI: 0.96 to 1.37) when examined separately. When whole population rates were employed, similar increases were observed among female (4.4–6.7 per 1000 US youth; a 52% increase) and male patients (3.2–5.1; a 59% increase). Racial and/or ethnic trends were not examined because of small sample sizes.
TABLE 7.
Trends in ED Visits Related to Suicidal Attempts and/or Self-Injury
| 2011 | 2012 | 2013 | 2014 | 2015 | Overall | |
|---|---|---|---|---|---|---|
| All ED visits, % | ||||||
| 6–11 y | <0.1 | <0.1 | 0.2 | 0.1 | <0.1 | <0.1 |
| 12–17 y* | 1.4 | 1.3 | 2.7 | 2.3 | 3.5 | 2.2 |
| 18–24 y | 1.3 | 1.0 | 0.7 | 0.8 | 1.1 | 0.9 |
| Female patients | 1.0 | 1.0 | 1.1 | 1.0 | 1.5 | 1.1 |
| Male patients | 0.9 | 0.7 | 1.1 | 1.1 | 1.5 | 1.0 |
| Overall* | 0.9 | 0.8 | 1.1 | 1.0 | 1.5 | 1.7 |
| Psychiatric visits only, % | ||||||
| 6–11 y | 4.2 | 2.4 | 7.3 | 5.3 | 1.7 | 4.2 |
| 12–17 y* | 15.8 | 15.5 | 28.7 | 24.8 | 26.2 | 22.7 |
| 18–24 y | 10.9 | 9.9 | 7.1 | 7.6 | 9.1 | 8.9 |
| Female patients | 13.6 | 13.8 | 15.9 | 13.9 | 15.5 | 14.6 |
| Male patients | 10.4 | 7.9 | 11.0 | 10.6 | 13.5 | 10.9 |
| Overall | 12.0 | 10.9 | 13.3 | 12.2 | 14.5 | 12.7 |
| Visits per 1000 US youth | ||||||
| 6–11 y | 0.2 | 0.1 | 0.5 | 0.4 | 0.1 | 0.3 |
| 12–17 y | 4.6 | 3.7 | 7.7 | 7.5 | 11.7 | 7.1 |
| 18–24 y | 5.9 | 5.0 | 3.5 | 4.3 | 5.7 | 4.8 |
| Female patients | 4.4 | 4.1 | 4.5 | 4.6 | 6.7 | 4.9 |
| Male patients | 3.2 | 2.2 | 3.3 | 3.6 | 5.1 | 3.5 |
| Overall | 3.7 | 3.2 | 3.9 | 4.1 | 5.8 | 4.2 |
P < .05.
Discussion
In the current study, we found that psychiatric visits to the ED among youth 6 to 24 years of age are increasing across the United States. The largest rise in such visits were found among adolescents and youth of color. It should be noted that the findings were heavily driven by 2015, in which the largest increase in visits was observed. Nevertheless, these data reflect a continuation of historical trends in pediatric psychiatric ED visits12,16 and are in line with recent increases in inpatient psychiatric hospitalizations.31 Ultimately, it is unclear if the findings represent a change in identification (by providers) or reporting (by patients or family members) of mental health in the ED, a shift in the epidemiology of psychiatric disorders in the United States, or fluctuations in referral patterns or service-seeking behavior.
This study unmistakably reveals that adolescents are a population with urgent mental health needs. Not only were their visits the most acute, but their probability of suicidal attempt and/or self-harm increased as well. The latter is consistent with the national trends in suicide ideation.22 Surprisingly, only 37% of visits involving adolescents who visited the ED for a suicidal attempt and/or self-injury resulted in a mental health provider being seen. In the same vein, only 16% of all psychiatric ED visits resulted in a mental health provider being seen. This is not the first study to identify this gap (for suicide-related or general psychiatric ED visits), which is likely due to the limited access of mental health providers in the ED.4,5 With the growing presence of mental health in this setting, coupled with the length of these visits, this finding represents a missed opportunity for screening and treatment planning. Nevertheless, there are promising efforts to increase the availability of expertise within the ED, notably through the use of telemedicine or other mobile health technologies and linkages to treatment afterward.32–34 Data from this study support the continued funding and effort of these initiatives.
The rise in psychiatric ED visits among youth of color is an important finding from this study. Again, this finding was heavily driven by 2015. Although there were no visit-related differences (eg, time of day, arrival type, and urgency), there were several known demographic (eg, insurance type and geographic location) and diagnostic (eg, SUDs) differences between racial and ethnic groups.35 Future research is needed to unpack these findings, particularly among African American youth who had less urgent visits.
A few sex-related differences were identified in this study. Although there was no difference in time trends, male patients were slightly more likely to visit the ED for psychiatric reasons, which departs from previous pediatric research.11 This discrepancy is likely due to the inclusion of young adults, who had the highest proportion of substance use–related ED visits. In this study and others, male patients are known to have increased rates of substance abuse compared with female patients.35 Surprisingly, female patients were not significantly more likely to visit the ED for suicide or self-injury, a finding that may be partly due to the small samples sizes given the rarity of these visits.36 This finding supports the need for suicide prevention and interventions efforts among male patients as well as female patients, who could be overlooked.
Although many researchers and clinicians look to the outpatient mental health system to prevent psychiatric ED visits, there is mixed evidence to suggest that a connection to mental health providers can reduce such visits.37,38 For instance, a recent systematic review revealed little to no evidence that engagement in outpatient, primary care, or community and/or school-based mental health services impacted ED use.37 One explanation may be that providers themselves may be sending children to the ED during times of crisis, as reflected by a recent national survey that revealed that 60% of child and adolescent psychiatrists recommended that parents take their child to the ED during times of crisis.39 Although the ultimate goal is to link youth with appropriate sources of care outside of the ED (particularly because these visits have been linked to iatrogenic outcomes,40 poor follow-up,41 and repeat visits42), the ED will likely have to play a continued role in treating both acute and chronic mental health issues in the future. As such, this study supports the continued effort to outfit EDs with the expertise to identify and treat mental health problems, to investigate novel approaches to crisis intervention (eg, mobile crisis centers, peer crisis services, crisis stabilization beds, and telemedicine crisis services),43,44 or to design new models of urgent mental health care that are accessible (particularly in the evening).
There are several study limitations that require mentioning. First, there were missing data across a few variables, namely visit acuity and race and/or ethnicity, although the latter was imputed by the NCHS.30 The inability to confirm diagnostic validity is another limitation because consistent application of diagnostic criteria may systematically vary (across providers and over time) in unknown ways. These limitations are offset by the nationally representative sample, in-depth analysis across numerous variables, and novel findings that have important implications to both policy and practice.
Conclusions
Psychiatric ED visits among young people increased nationally, most notably in 2015. The largest increases were observed among adolescents and youth of color, whereas young adults had the highest overall population rates. Visits related to suicidal attempt and self-injury also increased among adolescents. These data support the continued funding and deployment of evidenced-based interventions that can effectively reach families and young adults during times of crisis.
Glossary
- CI
confidence interval
- ED
emergency department
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- OR
odds ratio
- RFV
reason for visit
- SUD
substance use disorder
Footnotes
Dr Kalb designed the study, drafted the initial manuscript, and conducted the analyses on the publicly available data set; Drs Stapp, Ballard, Keefer, and Riley and Ms Holingue reviewed and revised the manuscript and provided important intellectual content, including conceptualization of the study design, fit of the current study within the literature, and approach to the analyses; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded, in part, by the National Institute of Mental Health Intramural Research program. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Williams NJ, Scott L, Aarons GA. Prevalence of serious emotional disturbance among U.S. children: a meta-analysis. Psychiatr Serv. 2018;69(1):32–40 [DOI] [PubMed] [Google Scholar]
- 2.Costello EJ, He JP, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey-Adolescent. Psychiatr Serv. 2014;65(3):359–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine IOM report: the future of emergency care in the United States health system. Acad Emerg Med. 2006;13(10):1081–1085 [DOI] [PubMed] [Google Scholar]
- 4.Chun TH, Mace SE, Katz ER; American Academy of Pediatrics; Committee on Pediatric Emergency Medicine; American College of Emergency Physicians; Pediatric Emergency Medicine Committee . Executive summary: evaluation and management of children and adolescents with acute mental health or behavioral problems. Part I: common clinical challenges of patients with mental health and/or behavioral emergencies. Pediatrics. 2016;138(3):e20161571. [DOI] [PubMed] [Google Scholar]
- 5.Dolan MA, Mace SE; American Academy of Pediatrics, Committee on Pediatric Emergency Medicine; American College of Emergency Physicians, Pediatric Emergency Medicine Committee . Pediatric mental health emergencies in the emergency medical services system. Pediatrics. 2006;118(4):1764–1767 [DOI] [PubMed] [Google Scholar]
- 6.Cama S, Malowney M, Smith AJB, et al. Availability of outpatient mental health care by pediatricians and child psychiatrists in five U.S. cities. Int J Health Serv. 2017;47(4):621–635 [DOI] [PubMed] [Google Scholar]
- 7.Bishop TF, Seirup JK, Pincus HA, Ross JS. Population of US practicing psychiatrists declined, 2003-13, which may help explain poor access to mental health care. Health Aff (Millwood). 2016;35(7):1271–1277 [DOI] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration Behavioral Health, United States, 2012. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013 [PubMed] [Google Scholar]
- 9.Gallagher KAS, Bujoreanu IS, Cheung P, et al. Psychiatric boarding in the pediatric inpatient medical setting: a retrospective analysis. Hosp Pediatr. 2017;7(8):444–450 [DOI] [PubMed] [Google Scholar]
- 10.Wharff EA, Ginnis KB, Ross AM, Blood EA. Predictors of psychiatric boarding in the pediatric emergency department: implications for emergency care. Pediatr Emerg Care. 2011;27(6):483–489 [DOI] [PubMed] [Google Scholar]
- 11.Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr. 2015;167(4):905–910 [DOI] [PubMed] [Google Scholar]
- 12.Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Acad Emerg Med. 2014;21(1):25–30 [DOI] [PubMed] [Google Scholar]
- 13.Sills MR, Bland SD. Summary statistics for pediatric psychiatric visits to US emergency departments, 1993-1999. Pediatrics. 2002;110(4). Available at: www.pediatrics.org/cgi/content/full/110/4/e40 [DOI] [PubMed] [Google Scholar]
- 14.Mahajan P, Alpern ER, Grupp-Phelan J, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Epidemiology of psychiatric-related visits to emergency departments in a multicenter collaborative research pediatric network. Pediatr Emerg Care. 2009;25(11):715–720 [DOI] [PubMed] [Google Scholar]
- 15.Grupp-Phelan J, Harman JS, Kelleher KJ. Trends in mental health and chronic condition visits by children presenting for care at U.S. emergency departments. Public Health Rep. 2007;122(1):55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon AE, Schoendorf KC. Emergency department visits for mental health conditions among US children, 2001-2011. Clin Pediatr (Phila). 2014;53(14):1359–1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott EG, Luxmore B, Alexander H, Fenn RL, Christopher NC. Screening for adolescent depression in a pediatric emergency department. Acad Emerg Med. 2006;13(5):537–542 [DOI] [PubMed] [Google Scholar]
- 18.Chun TH, Mace SE, Katz ER; American Academy of Pediatrics, Committee on Pediatric Emergency Medicine; American College of Emergency Physicians, Pediatric Emergency Medicine Committee . Executive summary: evaluation and management of children with acute mental health or behavioral problems. Part II: recognition of clinically challenging mental health related conditions presenting with medical or uncertain symptoms. Pediatrics. 2016;138(3):e20161574. [DOI] [PubMed] [Google Scholar]
- 19.Hampton LM, Daubresse M, Chang HY, Alexander GC, Budnitz DS. Emergency department visits by adults for psychiatric medication adverse events. JAMA Psychiatry. 2014;71(9):1006–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11(2):193–195 [PubMed] [Google Scholar]
- 21.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Vital Statistics System; National Center for Health Statistics; Centers for Disease Control and Prevention . 10 Leading Causes of Death by Age Group, United States - 2015. Atlanta, GA: Centers for Disease Control and Prevention; 2017 [Google Scholar]
- 23.Gill PJ, Saunders N, Gandhi S, et al. Emergency department as a first contact for mental health problems in children and youth. J Am Acad Child Adolesc Psychiatry. 2017;56(6):475–482.e4 [DOI] [PubMed] [Google Scholar]
- 24.Miller IW, Camargo CA Jr, Arias SA, et al. ; ED-SAFE Investigators . Suicide prevention in an emergency department population: the ED-SAFE study. JAMA Psychiatry. 2017;74(6):563–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winstanley EL, Mashni R, Schnee S, Miller N, Mashni SM. The development and feasibility of a pharmacy-delivered opioid intervention in the emergency department. J Am Pharm Assoc. 2017;57(suppl 2):S87–S91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Ambulatory health care data. Available at: https://www.cdc.gov/nchs/ahcd/index.htm. Accessed July 1, 2018
- 27.Centers for Disease Control and Prevention National Hospital Ambulatory Medical Care Survey: 2011 emergency department summary tables. Available at: https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed January 28, 2019
- 28.United States Census Bureau Download center - a step-by-step guide to downloading data. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/download_center.xhtml. Accessed October 1, 2018
- 29.Center for Disease Control and Prevention ICD-9-CM Official Guidelines for Coding and Reporting. Atlanta, GA: Centers for Disease Control and Prevention; 2011 [Google Scholar]
- 30.National Center for Health Statistics; Centers for Disease Control and Prevention Notices for NAMCS and NHAMCS public use data file users. Available at: https://www.cdc.gov/nchs/ahcd/notice.htm. Accessed July 1, 2018
- 31.Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Psychiatric disorders and trends in resource use in pediatric hospitals. Pediatrics. 2016;138(5):e20160909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mroczkowski MM, Havens J. The state of emergency child and adolescent psychiatry: raising the bar. Child Adolesc Psychiatr Clin N Am. 2018;27(3):357–365 [DOI] [PubMed] [Google Scholar]
- 33.Narasimhan M, Druss BG, Hockenberry JM, et al. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatr Serv. 2015;66(11):1167–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newton AS, Hartling L, Soleimani A, Kirkland S, Dyson MP, Cappelli M. A systematic review of management strategies for children’s mental health care in the emergency department: update on evidence and recommendations for clinical practice and research. Emerg Med J. 2017;34(6):376–384 [DOI] [PubMed] [Google Scholar]
- 35.Center for Behavioral Health Statistics and Quality Key Substance Use and Mental Health Indicators in the United States: Results From the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016 [Google Scholar]
- 36.Ballard ED, Cwik M, Van Eck K, et al. Identification of at-risk youth by suicide screening in a pediatric emergency department. Prev Sci. 2017;18(2):174–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirkland SW, Soleimani A, Newton AS. Review: the impact of pediatric mental health care provided outpatient, primary care, community and school settings on emergency department use – a systematic review. Child Adolesc Ment Health. 2018;23(1):4–13 [DOI] [PubMed] [Google Scholar]
- 38.Frosch E, dosReis S, Maloney K. Connections to outpatient mental health care of youths with repeat emergency department visits for psychiatric crises. Psychiatr Serv. 2011;62(6):646–649 [DOI] [PubMed] [Google Scholar]
- 39.Kalb LG, Stuart EA, Mandell DS, Olfson M, Vasa RA. Management of mental health crises among youths with and without ASD: a national survey of child psychiatrists. Psychiatr Serv. 2017;68(10):1039–1045 [DOI] [PubMed] [Google Scholar]
- 40.Coyle TN, Shaver JA, Linehan MM. On the potential for iatrogenic effects of psychiatric crisis services: the example of dialectical behavior therapy for adult women with borderline personality disorder. J Consult Clin Psychol. 2018;86(2):116–124 [DOI] [PubMed] [Google Scholar]
- 41.Bridge JA, Marcus SC, Olfson M. Outpatient care of young people after emergency treatment of deliberate self-harm. J Am Acad Child Adolesc Psychiatry. 2012;51(2):213–222.e1 [DOI] [PubMed] [Google Scholar]
- 42.Leon SL, Cloutier P, Polihronis C, et al. Child and adolescent mental health repeat visits to the emergency department: a systematic review. Hosp Pediatr. 2017;7(3):177–186 [DOI] [PubMed] [Google Scholar]
- 43.Substance Abuse and Mental Health Services Administration Crisis Services: Effectiveness, Cost-Effectiveness, and Funding Strategies. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014 [Google Scholar]
- 44.Sunderji N, de Bibiana JT, Stergiopoulos V. Urgent psychiatric services: a scoping review. Can J Psychiatry. 2015;60(9):393–402 [DOI] [PMC free article] [PubMed] [Google Scholar]