Abstract
Background
Frequent consumption of excess amounts of sugar‐sweetened beverages (SSB) is a risk factor for obesity, type 2 diabetes, cardiovascular disease and dental caries. Environmental interventions, i.e. interventions that alter the physical or social environment in which individuals make beverage choices, have been advocated as a means to reduce the consumption of SSB.
Objectives
To assess the effects of environmental interventions (excluding taxation) on the consumption of sugar‐sweetened beverages and sugar‐sweetened milk, diet‐related anthropometric measures and health outcomes, and on any reported unintended consequences or adverse outcomes.
Search methods
We searched 11 general, specialist and regional databases from inception to 24 January 2018. We also searched trial registers, reference lists and citations, scanned websites of relevant organisations, and contacted study authors.
Selection criteria
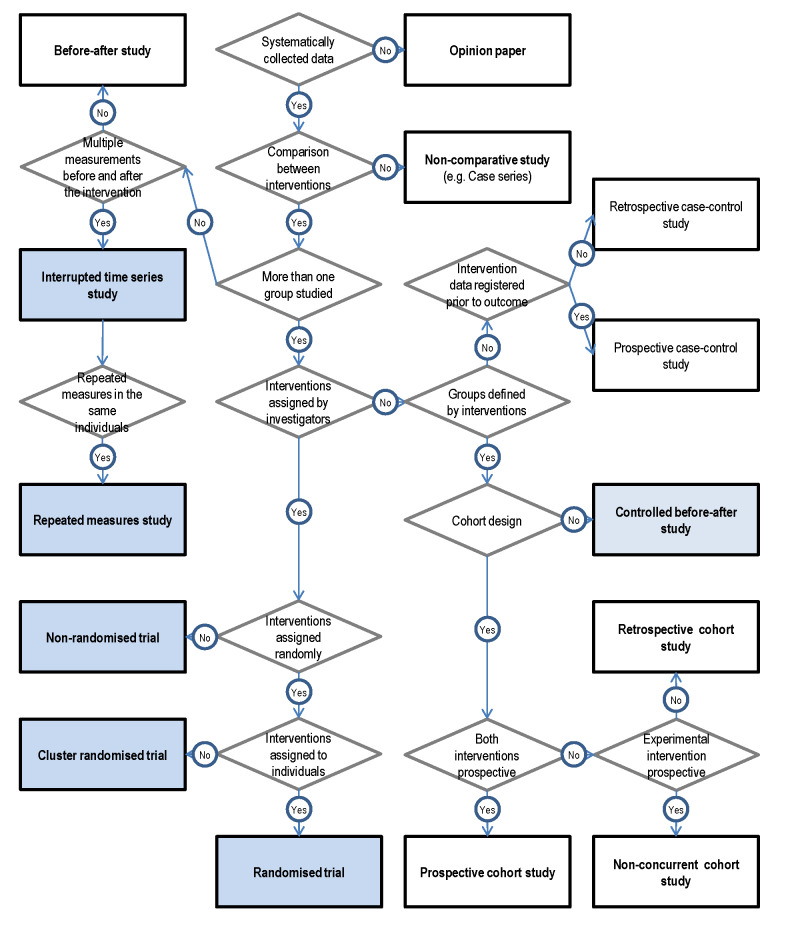
We included studies on interventions implemented at an environmental level, reporting effects on direct or indirect measures of SSB intake, diet‐related anthropometric measures and health outcomes, or any reported adverse outcome. We included randomised controlled trials (RCTs), non‐randomised controlled trials (NRCTs), controlled before‐after (CBA) and interrupted‐time‐series (ITS) studies, implemented in real‐world settings with a combined length of intervention and follow‐up of at least 12 weeks and at least 20 individuals in each of the intervention and control groups. We excluded studies in which participants were administered SSB as part of clinical trials, and multicomponent interventions which did not report SSB‐specific outcome data. We excluded studies on the taxation of SSB, as these are the subject of a separate Cochrane Review.
Data collection and analysis
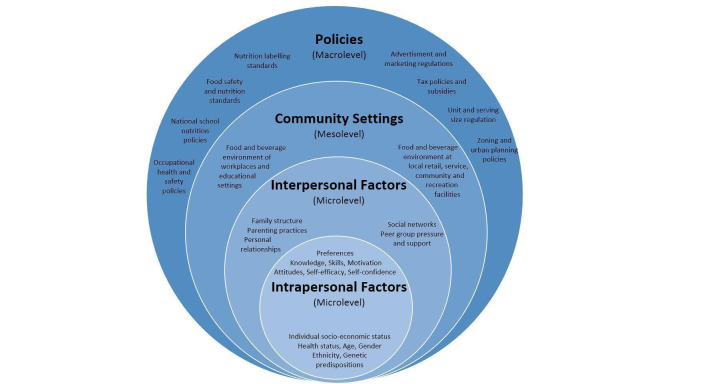
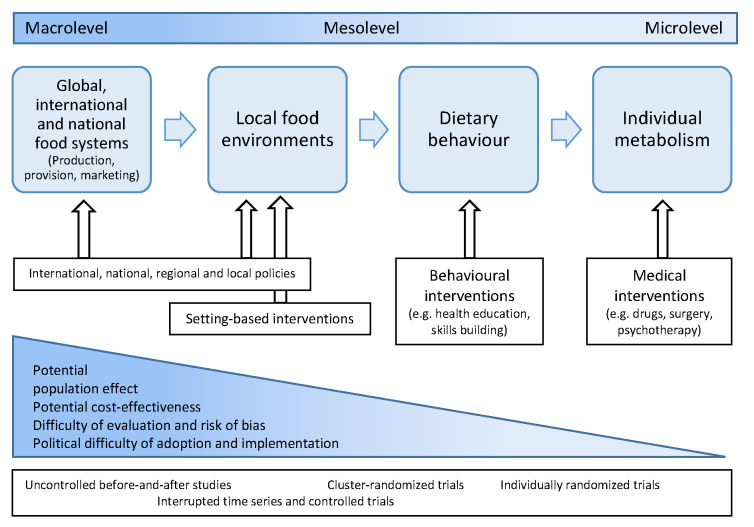
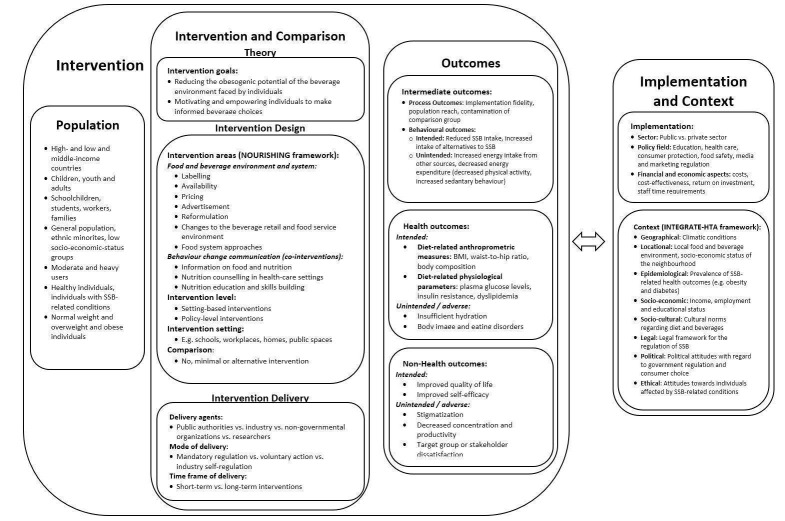
Two review authors independently screened studies for inclusion, extracted data and assessed the risks of bias of included studies. We classified interventions according to the NOURISHING framework, and synthesised results narratively and conducted meta‐analyses for two outcomes relating to two intervention types. We assessed our confidence in the certainty of effect estimates with the GRADE framework as very low, low, moderate or high, and presented ‘Summary of findings’ tables.
Main results
We identified 14,488 unique records, and assessed 1030 in full text for eligibility. We found 58 studies meeting our inclusion criteria, including 22 RCTs, 3 NRCTs, 14 CBA studies, and 19 ITS studies, with a total of 1,180,096 participants. The median length of follow‐up was 10 months. The studies included children, teenagers and adults, and were implemented in a variety of settings, including schools, retailing and food service establishments. We judged most studies to be at high or unclear risk of bias in at least one domain, and most studies used non‐randomised designs. The studies examine a broad range of interventions, and we present results for these separately.
Labelling interventions (8 studies): We found moderate‐certainty evidence that traffic‐light labelling is associated with decreasing sales of SSBs, and low‐certainty evidence that nutritional rating score labelling is associated with decreasing sales of SSBs. For menu‐board calorie labelling reported effects on SSB sales varied.
Nutrition standards in public institutions (16 studies): We found low‐certainty evidence that reduced availability of SSBs in schools is associated with decreased SSB consumption. We found very low‐certainty evidence that improved availability of drinking water in schools and school fruit programmes are associated with decreased SSB consumption. Reported associations between improved availability of drinking water in schools and student body weight varied.
Economic tools (7 studies): We found moderate‐certainty evidence that price increases on SSBs are associated with decreasing SSB sales. For price discounts on low‐calorie beverages reported effects on SSB sales varied.
Whole food supply interventions (3 studies): Reported associations between voluntary industry initiatives to improve the whole food supply and SSB sales varied.
Retail and food service interventions (7 studies): We found low‐certainty evidence that healthier default beverages in children’s menus in chain restaurants are associated with decreasing SSB sales, and moderate‐certainty evidence that in‐store promotion of healthier beverages in supermarkets is associated with decreasing SSB sales. We found very low‐certainty evidence that urban planning restrictions on new fast‐food restaurants and restrictions on the number of stores selling SSBs in remote communities are associated with decreasing SSB sales. Reported associations between promotion of healthier beverages in vending machines and SSB intake or sales varied.
Intersectoral approaches (8 studies): We found moderate‐certainty evidence that government food benefit programmes with restrictions on purchasing SSBs are associated with decreased SSB intake. For unrestricted food benefit programmes reported effects varied. We found moderate‐certainty evidence that multicomponent community campaigns focused on SSBs are associated with decreasing SSB sales. Reported associations between trade and investment liberalisation and SSB sales varied.
Home‐based interventions (7 studies): We found moderate‐certainty evidence that improved availability of low‐calorie beverages in the home environment is associated with decreased SSB intake, and high‐certainty evidence that it is associated with decreased body weight among adolescents with overweight or obesity and a high baseline consumption of SSBs.
Adverse outcomes reported by studies, which may occur in some circumstances, included negative effects on revenue, compensatory SSB consumption outside school when the availability of SSBs in schools is reduced, reduced milk intake, stakeholder discontent, and increased total energy content of grocery purchases with price discounts on low‐calorie beverages, among others. The certainty of evidence on adverse outcomes was low to very low for most outcomes.
We analysed interventions targeting sugar‐sweetened milk separately, and found low‐ to moderate‐certainty evidence that emoticon labelling and small prizes for the selection of healthier beverages in elementary school cafeterias are associated with decreased consumption of sugar‐sweetened milk. We found low‐certainty evidence that improved placement of plain milk in school cafeterias is not associated with decreasing sugar‐sweetened milk consumption.
Authors' conclusions
The evidence included in this review indicates that effective, scalable interventions addressing SSB consumption at a population level exist. Implementation should be accompanied by high‐quality evaluations using appropriate study designs, with a particular focus on the long‐term effects of approaches suitable for large‐scale implementation.
Keywords: Adolescent, Adult, Animals, Child, Humans, Young Adult, Drinking Behavior, Environment, Milk, Social Environment, Artificially Sweetened Beverages, Artificially Sweetened Beverages/supply & distribution, Commerce, Commerce/economics, Controlled Before-After Studies, Controlled Before-After Studies/statistics & numerical data, Drinking Water, Fast Foods, Fast Foods/supply & distribution, Food Supply, Fruit, Fruit/supply & distribution, Interrupted Time Series Analysis, Interrupted Time Series Analysis/statistics & numerical data, Nutritive Value, Product Labeling, Randomized Controlled Trials as Topic, Randomized Controlled Trials as Topic/statistics & numerical data, Schools, Selection Bias, Sugar-Sweetened Beverages, Sugar-Sweetened Beverages/adverse effects, Sugar-Sweetened Beverages/economics, Sugar-Sweetened Beverages/supply & distribution
Plain language summary
Cutting back on sugar‐sweetened beverages: What works?
What are sugar‐sweetened beverages?
Sugar‐sweetened beverages (SSBs) are cold and hot drinks with added sugar. Common SSBs are non‐diet soft drinks, regular soda, iced tea, sports drinks, energy drinks, fruit punches, sweetened waters, and sweetened tea and coffee.
Why are SSBs an important health topic?
Research shows that people who drink a lot of SSBs often gain weight. Drinking a lot of SSBs can also increase the risk of diabetes, heart disease, and dental decay. Doctors therefore recommend that children, teenagers and adults drink fewer SSBs. Governments, businesses, schools and workplaces have taken various measures to support healthier beverage choices.
What is the aim of this review?
We wanted to find out whether the measures taken so far have been successful in helping people to drink fewer SSBs to improve their health. We focused on measures that change the environment in which people make beverage choices. We did not look at studies on educational programmes or on SSB taxes, as these are examined in separate reviews. (We did, however, examine price increases on SSB which were not due to taxes.) We searched for all available studies meeting clearly‐defined criteria to answer this question. This review reflects the state of the evidence up until January 2018.
What studies did we find?
We found 58 studies, which included more than one million adults, teenagers and children. Most studies lasted about one year, and were done in schools, stores or restaurants.
Some studies used methods that are not very reliable. For example, in some studies participants were simply asked how much SSB they drank, which is not very reliable, as people sometimes forget how much SSB they drank. Some of the findings of our review may therefore change when more and better studies become available.
What do these studies tell us?
We have found some evidence that some of the measures implemented to help people drink fewer SSBs have been successful, including the following:
▪ Labels which are easy to understand, such as traffic‐light labels, and labels which rate the healthfulness of beverages with stars or numbers.
▪ Limits to the availability of SSB in schools (e.g. replacing SSBs with water in school cafeterias).
▪ Price increases on SSBs in restaurants, stores and leisure centres.
▪ Children’s menus in chain restaurants which include healthier beverages as their standard beverage.
▪ Promotion of healthier beverages in supermarkets.
▪ Government food benefits (e.g. food stamps) which cannot be used to buy SSBs.
▪ Community campaigns focused on SSBs.
▪ Measures that improve the availability of low‐calorie beverages at home, e.g. through home deliveries of bottled water and diet beverages.
We have also found some evidence that improved availability of drinking water and diet beverages at home can help people lose weight.
There are also other measures which may influence how much SSB people drink, but for these the available evidence is less certain.
Some, but not all studies found that such measures can have effects which were not intended and which may be negative. Some studies reported that profits of stores and restaurants decreased when the measures were implemented, but other studies showed that profits increased or stayed the same. Children who get free drinking water in schools may drink less milk. Some studies reported that people were unhappy with the measures.
We also looked at studies on sugar‐sweetened milk. We found that small prizes for children who chose plain milk in their school cafeteria, as well as emoticon labels, may help children drink less sugar‐sweetened milk. However, this may also drive up the share of milk which is wasted because children choose but do not drink it.
What does this mean in practice?
Our review shows that measures which change the environment in which people make beverage choices can help people drink less SSB. Based on our findings we suggest that such measures may be used more widely. Government officials, business people and health professionals implementing such measures should work together with researchers to find out more about their effects in the short and long term.
Summary of findings
Summary of findings for the main comparison. Interventions to reduce the consumption of SSB compared to no or alternative intervention: impact on SSB intake.
| Interventions to reduce the consumption of SSB compared to no or alternative intervention: impact on SSB intake (additional outcomes reported in Summary of Findings tables 2‐9)a | ||
| Intervention type |
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidenceb |
Impact on direct and indirect measures of SSB intake |
| A Labelling interventions | ||
| A.1 Traffic‐light labelling |
SSB sales (12 months)
42 points‐of‐sale in 2 hospitals in 2 cities 2 ITS studies ⊕⊕⊕⊝ MODERATEc |
Boelsen‐Robinson 2017 (units of red‐labelled beverages sold):−56% (95% CI −67 to −45) Hartigan 2017 (share of red‐labelled beverages among all beverages sold): −25 percentage points (P < 0.001) |
| A.2 Nutritional rating score shelf‐labels |
SSB sales (7 to 11 months) 442 stores from 4 chains in 2 countries 1 ITS and 1 CBA study ⊕⊕⊝⊝ LOW |
Cawley 2015 (units of SSB sold):−27.4% (no P value or CI reported) Hobin 2017 (share of beverages with zero stars (mainly SSB), coefficient estimate): −0.026, P < 0.001 |
| A.3 Menu‐board calorie labelling |
Beverage calories per transaction (4 to 12 months)
353 stores from 4 chains in 6 cities 1 controlled ITS, 2 CBA studies ⊕⊝⊝⊝ VERY LOWd,e |
Bollinger 2011 (beverage calories per transaction): −0.3% (P < 0.01) Elbel 2013 (beverage calories per transaction):No effects (data not shown) Finkelstein 2011 (beverage calories per transaction): +1.7 kcal (95% CI −1.5 to 4.9) |
| A.4 Emoticon labelling |
Sugar‐sweetened milk selection (4 months)
186 students in 2 school cafeterias 1 ITS study ⊕⊕⊝⊝ LOW |
Siegel 2016a (share of students selecting chocolate milk): −16 percentage points (95% CI −27 to −4) |
| B Nutrition standards in public institutions | ||
| B.1 Reduced availability of SSB in schools |
SSB intake (6 to 24 months)
18,238 students in 240 schools 5 CBA studies ⊕⊕⊝⊝ LOW |
Cradock 2011 (total SSB intake): −99 ml/day (95% CI −173 to −26) Whatley Blum 2008 (total SSB intake): −14 ml/day (95% CI −69 to 41) Bauhoff 2014 cohort (share of students consuming any SSB): −4 percentage points (95% CI −10 to 2) Bauhoff 2014 crosssectional (share of students consuming any SSB): −10 percentage points (95% CI −17 to −3) Schwartz 2009 (total intake of beverages excluded by nutrition standards (mainly SSB) in schools):Decrease (ß = −0.23, P < 0.05) |
| B.2 Improved access to drinking water in schools |
SSB intake (3 to 13 months)
11,253 students in 62 schools 1 CBA study, 3 NRCTsf ⊕⊝⊝⊝ VERY LOWd,f,g |
Elbel 2015a (total SSB intake): No statistically significant effect (data not shown) Muckelbauer 2009 (total SSB intake, participants with foreign‐born parents or grandparents): −20 ml/day (95% CI −60 to 20) Muckelbauer 2009 (total SSB intake, participants without foreign‐born parents or grandparents):±0 ml/day (95% CI −60 to 60) Van de Gaar 2014 (total SSB intake): −190 ml/day (95% CI −280 to −100) Visscher 2010 (SSB sales at school):+0.7 ml/day/student (no statistical analyses reported by study authors) |
|
Sugar‐sweetened milk intake (5 years) 1,065,562 students in 1227 schools 1 CBA study ⊕⊝⊝⊝ VERY LOWd |
Schwartz 2016 (sugar‐sweetened milk intake): −3 ml/day (95% CI −5 to −1) | |
| B.3 Small prizes for the selection of healthier beverages in school cafeterias |
Sugar‐sweetened milk selection and purchases (3 to 20 months)
4213 students in 12 schools
(1 RCT and 2 ITS studies)
⊕⊕⊕⊝ MODERATEd (Hendy 2011) ⊕⊕⊝⊝ LOW (Emerson 2017; Siegel 2016b) |
Hendy 2011 (number of meals with unhealthy beverages selected) −3.0 meals/week (P = 0.000) Siegel 2016b (chocolate milk purchases): −0.12 servings/day (P < 0.001) Emerson 2017 (chocolate milk purchases): −0.12 servings/day (P < 0.001) |
| B.4 Improved placement of healthier beverages in school cafeterias | Sugar‐sweetened milk intake (3 to 4 months) 2638 students in 14 schools 1 cluster‐RCT ⊕⊕⊝⊝ LOWd,g | Cohen 2015 (selection and consumption of sugar‐sweetened milk): No statistically significant effect (data not shown) |
| B.5 Fruit provision in schools | SSB intake (9 months to 6 years) 3494 students in 47 schools 1 cluster‐RCT and 1 CBA study ⊕⊝⊝⊝ VERY LOWh,i,j | Da Costa 2014 (SSB intake): Decrease (P = 0.003, data not intelligible to review authors) Øverby 2012 (SSB intake measured with an unhealthy snack frequency score): −1.4 in the free‐fruit provision group, −1.1 in the fruit subscription group, −0.7 in the control group (P = 0.002 for time*group interaction) |
| C Economic tools | ||
| C.1 Price increases on SSB | SSB sales (4 to 12 months) 1 store, 7 leisure centres and 37 restaurants in 29 cities 3 ITS studies ⊕⊕⊕⊝ MODERATEk | Cornelsen 2017 (SSB items sold per customer): −9% (95% CI −15 to −3) Blake 2018 (volume of red‐labelled beverages sold): −28% (95% −32 to −23) Breeze 2018 (volume of SSB sold per attendance): −27% (95% CI −59 to −3) |
| C.2 Financial incentives to purchase low‐calorie beverages implemented through supermarket loyalty cards | SSB intake and sales (3 to 6 months) 1750 customers of 3 supermarket chains 3 RCTs ⊕⊕⊝⊝ LOWd,g |
Ball 2015 (self‐reported SSB intake): +10 ml/day (95% CI 0 to 20)
Ball 2015 (SSB purchases): +55 ml/day (95% CI −7 to 117)
Ni Mhurchu 2010 (energy density of beverages purchased): −0.1 MJ/kg (95% CI −0.4 to 0.2) Franckle 2018 (number of red‐labelled beverages purchased per month): −0.14 beverage items/month (95% CI −0.8 to 0.6) |
| C.3 Price discounts on low‐calorie beverages in community stores | SSB intake (6 months) 8515 inhabitants of 20 remote indigenous communities 1 cluster‐RCT ⊕⊕⊝⊝ LOWd,g | Brimblecombe 2017 (SSB sales): +6% (95% CI −3 to 15) |
| Taxation of SSB | Not included in this review (for a forthcoming Cochrane Review on taxation of SSB see Heise 2016, for existing systematic reviews on taxation of SSB see Backholer 2016, Cabrera Escobar 2013 and Nakhimovsky 2016) | |
| D Advertisement regulation: No studies found | ||
| E Whole food supply interventions | ||
| E.1 Voluntary food and beverage industry initiatives to improve the nutritional quality of the whole food supply | SSB sales and purchases ( 3 to 4 years) 61,126 households and 17 companies 2 controlled ITS and 1 CBA study ⊕⊝⊝⊝ VERY LOWd | Ng 2014a (energy from beverages sold):Decrease: −14 kcal/capita/day in the intervention group compared to −3 kcal/capita/day for national‐brand companies not participating in the pledge, no P value or CI reported) Ng 2014a (SSB sales by companies participating in the Healthy Weight Commitment Foundation Pledge): −7 kcal/per capita/day (no P Value or CIs reported, data for the CG not reported) Ng 2014b (SSB purchases): Increase relative to expected trends (P < 0.001, data shown graphically only) Taillie 2015 (percentage volume of SSB purchased):Decrease (P < 0.01, results shown graphically only) |
| F Retail and food service interventions | ||
| F.1 Healthier default beverages in children's menus in restaurants | SSB sales (6 years) 145 restaurants in 1 theme park 1 ITS study ⊕⊕⊝⊝ LOWc,d | Peters 2016a (share of children's menus served with SSB):−68 percentage points (no P value or CI reported for the pre‐post‐comparison) |
| F.2 In‐store promotion of low‐calorie beverages in supermarkets | SSB sales (6 months) 8 supermarkets from 2 chains 1 cluster‐RCT ⊕⊕⊕⊝ MODERATEg | Foster 2014 (in‐aisle SSB sales per supermarket): −11 l/day (95% CI −63 to 40) Foster 2014 (check‐out cooler SSB sales per supermarket): −2 units/day (95% CI −5 to 1) |
| F.3 Healthier vending machines in workplaces and schools | SSB intake (18 to 24 months) 6 schools and 4 worksites 2 NRCTsf ⊕⊝⊝⊝ VERY LOWd,e,j | Ermetici 2016 (SSB intake, normal‐weight participants): −1.1 times/week (95% CI −1.5 to −0.7) Ermetici 2016 (SSB intake, participants with overweight and obesity): −0.8 times/week (95% CI −1.5 to −0.1) French 2010 (SSB intake): +14 ml/day (P > 0.05) |
| F.4 Urban planning restrictions on new fast‐food outlets | SSB intake frequency (3 to 4 years) 11,821 inhabitants of 1 city and 1 county 1 CBA study ⊕⊝⊝⊝ VERY LOWd,g | Sturm 2015 (SSB intake frequency, measure or scale not reported): −0.9 (P > 0.05) |
| F.5 Restrictions to the number of stores selling SSB in remote communities | SSB sales (8 months) 3 stores in 1 remote community 1 ITS study ⊕⊝⊝⊝ VERY LOWd,g | Minaker 2016 (community‐wide SSB sales, model controlling for the summer peak): CAD −51/day (95% CI −166 to 65) |
| G Action across sectors | ||
| G.1 Trade and investment liberalisation in low‐ and middle‐income countries | SSB sales (4 years) 4 countries 2 controlled ITS studies ⊕⊝⊝⊝ VERY LOWd |
Baker 2016 (annual rate of change in volume sales of SSB per capita): −1.4 percentage points (95% CI −2.5 to −0.4) Baker 2016 (annual rate of change in volume sales of sugar from SSB per capita): −1.0 percentage points (95% CI −1.9 to −0.06) Baker 2016 (annual rate of change in volume sales of sports and energy drinks per capita): +0.3 percentage points (P > 0.05, SE 0.8) Schram 2015 (retail sales of SSB): +13 ml/per capita/day (95% CI 10 to 15) |
| G.2 Government food benefit programs with incentives for buying fruit and vegetables and restrictions on the purchase of SSB | SSB intake (3 to 12 months) 2274 adults and 18,207 children 3 RCTs with 5 comparisons ⊕⊕⊕⊝ MODERATEd | Collins 2016 WIC (intake of sugar from SSB, USD 60 versus no USD benefit/month):−5 g/day (95% CI −8 to −3) Collins 2016 WIC (intake of sugar from SSB, USD 60 versus USD 30 benefit/month): −1 g/day (95% CI −3 to 2) Collins 2016 WIC (intake of sugar from SSB, USD 30 versus no USD benefit/month): −5 g/day (95% CI −8 to −2) Harnack 2016 (SSB intake, incentives + restrictions): −180 ml/day (95% CI −338 to −22) Harnack 2016 (SSB purchases, incentives + restrictions):−0.3 USD/day (95% CI −0.5 to −0.2) Olsho 2016 (energy intake from SSB): −5 kcal/day/person (95% CI −21 to 11) Olsho 2016 (sugar intake from SSB): −1 g/day/person (95% CI −5 to 2) |
| G.3 Government food benefit programmes without incentives for buying fruit and vegetables and restrictions on the purchase of SSB |
SSB intake (3 to 8 months) 25,150 children and 2844 adults 1 RCT with 3 comparisons and 1 CBA study ⊕⊕⊝⊝ LOWd,g (Collins 2016 SNAP) ⊕⊝⊝⊝ VERY LOWd (Waehrer 2015) |
Collins 2016 SNAP (intake of sugar from SSB, USD 60 vs no USD benefit/month):−0.5 g/day (95% CI −2 to 1)
Collins 2016 SNAP (intake of sugar from SSB, USD 60 vs USD 30 benefit/month): +1 g/day (95% CI −1 to 3)
Collins 2016 SNAP (intake of sugar from SSB, USD 30 vs no USD benefit/month): −2 g/day (95% CI −4 to 1) Waehrer 2015 (SSB intake, median): +34 kcal/day (95% CI 7 to 60) |
| G.4 Multi‐component community campaigns focused on SSB | SSB sales (3 years) 32 supermarkets from 6 chains in 2 counties 1 controlled ITS study ⊕⊕⊕⊝ MODERATEc | Schwartz 2017 (SSB sales per product and store): −1.6 l/day (95% CI −2.0 to −1.2) (equivalent to a −20% decrease in the IG and a 0.8% increase in the CG) Schwartz 2017 (sports drinks sales per product and store):−0.4 l/day (95 CI −1.5 to 0.7) Schwartz 2017 (fruit drinks sales per product and store): −1.5 l/day (95% CI −2.0 to −0.9) |
| H Home‐based interventions | ||
| H.1 Improved access to low‐calorie beverages in the home environment | SSB intake (4 to 12 months) 1130 children, teenagers and adults 6 RCTs ⊕⊕⊕⊝ MODERATEd | Albala 2008, Anand 2007, Ebbeling 2006, Ebbeling 2012, Hernández‐Cordero 2014 (SSB intake, pooled effect estimate): −413 ml/day (95% CI −684 to −143) Tate 2012 (energy intake from beverages):−88 kcal/day (95% CI −124 to −51) |
| H.2 Provision of active video‐gaming equipment to teenagers |
SSB intake (10 months)
262 teenagers 1 RCT ⊕⊝⊝⊝ VERY LOWg,l |
Simons 2015 (share of participants consuming more than 1400 ml SSB a week): Decrease (OR 0.71, 95% CI 0.36 to 1.41) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; NRCT: non‐randomised controlled trial; OR: odds ratio; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | ||
aThis 'Summary of Findings' table presents data on effects on direct and indirect measures of SSB intake only. We present data on the remaining primary outcomes (diet‐related anthropometric measures and adverse outcomes) in the additional 'Summary of Findings' tables displayed between the Results and the Discussion section. Data on secondary outcomes are presented narratively in the section on Effects of interventions.
b We assessed the certainty of evidence with GRADE. In GRADE, the certainty of evidence is rated as high, moderate, low or very low. Evidence from randomised controlled trials starts as high‐certainty, and evidence from non‐randomised studies starts as low‐certainty. From there, five factors that can decrease the certainty of evidence (risk of bias, indirectness, inconsistency, imprecision, and publication bias) and three factors can increase the certainty of evidence (magnitude of effect size, direction of plausible confounding, and dose‐response gradient). The certainty of evidence is understood in GRADE as the extent to which one can be confident that the true effect of an intervention lies on one side of a specified threshold, or within a chosen range (Hultcrantz 2017). For the present review, we defined this threshold as difference from the null. Our assessment of the certainty of evidence therefore refers to the existence and the direction of effects, and not to the exact effect sizes reported by individual studies. We report further details in the Methods section, and in the footnotes to the Summary of Findings tables 2‐9.
cUpgraded for magnitude of effect. dDowngraded for risk of bias. eDowngraded for indirectness. fVan de Gaar 2014 and French 2010 were cluster‐RCTs with four units, of which two were allocated by the flip of a coin to the intervention group. Given the small number of randomised units, randomisation may not have been sufficient to attain baseline comparability of the intervention and control groups. We therefore included the two studies as NRCTs in our evidence synthesis. gDowngraded for imprecision. hDowngraded by one level for risk of bias and by one level for imprecision (Da Costa 2014). iDowngraded by one level for risk of bias (Øverby 2012). jDowngraded for probability of publication bias. kUpgraded by one level for dose‐response gradient and magnitude of effect. lDowngraded for probability of publication bias.
Summary of findings 2. Labelling compared to no intervention.
| A Labelling compared to no intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| A.1 Traffic‐light labelling | |
|
SSB sales (12 months)
42 points‐of‐sale in 2 hospitals in 2 cities 2 ITS studies ⊕⊕⊕⊝ MODERATEa |
Boelsen‐Robinson 2017 (units of red‐labelled beverages sold):−56% (95% CI −67 to −45) Hartigan 2017 (share of red‐labelled beverages among all beverages sold): −25 percentage points (P < 0.001) |
|
Revenueb (12 months)
42 points‐of‐sale in 2 hospitals in 2 cities 2 ITS studies ⊕⊕⊝⊝ LOW |
Boelsen‐Robinson 2017 (total vending machine revenue):−21% (95% CI −29 to −12) Hartigan 2017 (monthly revenue from beverages): Increase (from USD 34,624 at baseline to USD 35,390 during the intervention, no statistical analyses shown) |
| A.2 Nutritional rating score shelf‐labels in supermarkets | |
|
SSB sales (7 to 11 months) 442 stores from 4 chains in 2 countries 1 ITS and 1 CBA study ⊕⊕⊝⊝ LOW |
Cawley 2015 (units of SSB sold):−27.3% (no P value or CI reported) Hobin 2017 (share of beverages with zero stars (mainly SSB), coefficient estimate): −0.026, P < 0.001 |
|
Revenueb (7 to 11 months)
442 stores from 4 chains in 2 countries 1 ITS and 1 CBA study ⊕⊕⊝⊝ LOW |
Cawley 2015 (total unit sales): −4.9% (95% CI −9.7 to 0.07) Hobin 2017 (total revenue, coefficient estimate):+0.042, P < 0.01 |
|
Compensatory consumptionb (7 to 11 months)
442 stores from 4 chains in 2 countries 1 ITS and 1 CBA study ⊕⊕⊝⊝ LOW |
Cawley 2015 (number of zero‐star rated items sold per week in the average food and beverage category): −3183 units/week (95% CI −5454 to −913). Hobin 2017 (average star rating of all products sold, coefficient estimate): +0.01 (P < 0.001). |
| A.3 Menu‐board calorie labelling in chain restaurants and cafés | |
|
Beverage calories per transaction (4 to 12 months)
353 stores from 4 chains in 6 cities 1 controlled ITS, 2 CBA studies ⊕⊝⊝⊝ VERY LOWc,d |
Bollinger 2011 (beverage calories per transaction): −0.3% (P < 0.01) Elbel 2013 (beverage calories per transaction):No effects (data not shown) Finkelstein 2011 (beverage calories per transaction): +1.7 kcal (95% CI −1.5 to 4.9) |
|
Revenueb (11 months)
316 stores from 1 chain in 2 cities 1 controlled ITS ⊕⊝⊝⊝ VERY LOWc,e |
Bollinger 2011 (total store revenue, regression coefficient):+0.005, P > 0.05 |
|
Fast‐food restaurant visits* (4 months)
23 stores from 2 chains in 2 cities (1 CBA study) ⊕⊝⊝⊝ VERY LOWc,e |
Elbel 2013 (number of fast‐food restaurant visits): +0.9 visits/week (P = 0.07) |
|
Compensatory consumption* (4 to 12 months)
353 stores from 4 chains in 6 cities and counties 1 controlled ITS and 2 CBA studies ⊕⊝⊝⊝ VERY LOWc |
Bollinger 2011 (calories from foods and beverages per transaction):−6.0% (95%CI −6.2 to −5.8) Elbel 2013 (calories from foods and beverages per transaction):−3.8 kcal/transaction (95% CI −125 to 119) Finkelstein 2011 (calories from foods and beverages per transaction):+18.5 kcal/transaction (95% CI −11 to 48) |
| A.4 Emoticon labelling in school cafeterias | |
|
Sugar‐sweetened milk (4 months)
186 students in 2 schools 1 ITS study ⊕⊕⊝⊝ LOW |
Siegel 2016a (share of students selecting chocolate milk): −16 percentage points (−27 to −4) |
|
Total milk selection* (4 months)
186 students in 2 schools 1 ITS study ⊕⊝⊝⊝ VERY LOWf |
Siegel 2016a (share of students selecting any milk):+2 percentage points (no statistical analyses shown) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; NRCT: non‐randomised controlled trial; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages. | |
aUpgraded for magnitude of effect: We judged the effects on beverage sales to be large, and unlikely to have arisen by chance or through bias. bOutcomes included as potential adverse outcomes. cDowngraded for risk of bias: We judged Elbel 2013 and Finkelstein 2011 to be at unclear risk of bias in several domains. In both studies, calories per transaction were substantially lower in the intervention group than in the control group at baseline, and in Finkelstein 2011 the study authors hypothesise that differences in baseline outcome measurements may explain the lack of observed effects. In Finkelstein 2011 the control restaurants were located in counties adjacent to the county where the intervention was implemented. Restaurants in the intervention and control groups may have been frequented by the same customers, leading to contamination, which would have biased results towards null. Elbel 2013 reports only the non‐significance of effects observed for the outcome of interest to this review (calories from beverages per transaction), and may have been underpowered to detect effects for this outcome, which was not the primary outcome of the study. dDowngraded for indirectness: All three studies report only indirect measures of SSB intake, namely beverage calories per transaction. Moreover, the only study at low risk of bias, (Bollinger 2011), was implemented in a specific setting – Starbucks cafés in New York City – and the generalisability of its results to other settings may be limited. eDowngraded for imprecision: The 95% CI is large and includes zero. fDowngraded for imprecision: The study reports that no statistically significant effects were observed without providing an exact effect estimate, P value or 95% CI.
Summary of findings 3. Nutrition standards in public institutions compared to no intervention.
| B Nutrition standards compared to no intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| B.1 Reduced availability of SSB in schools | |
|
SSB sales (6 to 24 months)
18,238 students in 240 schools 5 CBA studies ⊕⊕⊝⊝ LOW |
Cradock 2011 (total SSB intake):−99 ml/day (95% CI −173 to −26) Whatley Blum 2008 (total SSB intake): −14 ml/day (95% CI −69 to 41) Bauhoff 2014 cohort (share of students consuming any SSB): −4 percentage points (95% CI −10 to 2) Bauhoff 2014 crosssectional (share of students consuming any SSB):−10 percentage points (95% CI −17 to −3) Schwartz 2009 (total intake of beverages excluded by nutrition standards [mainly SSB]):Decrease (ß = −0.23, P < 0.05) |
| Compensatory SSB intake outside school ‐ high schoolsa (36 months) 8146 households in 46 school districts 1 controlled ITS ⊕⊕⊝⊝ LOW | Lichtman‐Sadot 2016 (purchases outside school, high‐school‐aged children): +36 ml/day (95% CI 13 to 60) |
| Compensatory SSB intake outside school ‐ other school typesa (6 to 36 months) 11,331 households in 51 school districts (Huang 2012 and Lichtman‐Sadot 2016), 495 students in 6 schools (Schwartz 2009) 2 CBA studies and 1 controlled ITS ⊕⊝⊝⊝ VERY LOWb | Huang 2012 (SSB purchases outside school, school‐aged children): −13 ml/day (95% CI −137 to 112) Lichtman‐Sadot 2016 (SSB purchases outside school, middle‐school‐aged children): −20 ml/day (95% CI −50 to 10) Lichtman‐Sadot 2016 (SSB purchases outside school, elementary‐school‐aged children):−2 ml/day (95% CI −47 to 44) Schwartz 2009 (consumption of beverages excluded by nutrition standards outside school, middle‐school‐aged children): Decrease (ß = −0.18, P < 0.05) |
| Body dissatisfaction and dieting behavioura (12 months) 495 students in 6 schools 1 CBA study ⊕⊝⊝⊝ VERY LOWc | Schwartz 2009 (body dissatisfaction and dieting behaviour): No statistically significant effects (data not shown) |
| B.2 Improved access to drinking water in schools | |
|
SSB sales (3 to 13 months)
11,253 students in 62 schools 1 CBA study, 3 NRCTsd ⊕⊝⊝⊝ VERY LOWd,e,f |
Elbel 2015a (total SSB intake): No statistically significant effect (data not shown) Muckelbauer 2009 (total SSB intake, participants with foreign‐born parents or grandparents):−20 ml/day (95% CI −60 to 20) Muckelbauer 2009 (total SSB intake, participants without foreign‐born parents or grandparents):±0 ml/day (95% CI −60 to 60) Van de Gaar 2014 (total SSB intake): −190 ml/day (95% CI −280 to −100) Visscher 2010 (SSB sales at school):+0.7 ml/day/student (no statistical analyses reported by study authors) |
|
Sugar‐sweetened milk intake (5 years) 1,065,562 students in 1227 schools 1 CBA study ⊕⊝⊝⊝ VERY LOWg |
Schwartz 2016 (sugar‐sweetened milk intake): −3 ml/day (95% CI −5 to −1) |
| Body weight (10 months to 5 years) 1,069,521 students at 1231 schools 1 NRCT, 1 CBA study and 1 cluster RCT ⊕⊝⊝⊝ VERY LOWh,i | Muckelbauer 2009 (z‐BMI): −0.00 (95% CI −0.04 to 0.04) Muckelbauer 2009 (share of students with overweight or obesity): Decrease (OR 0.69, 95% CI 0.48 to 0.99) Schwartz 2016 (z‐BMI): −0.02 (95% CI −0.03 to −0.00) Schwartz 2016 (share of students with overweight or obesity): −1.2 percentage points (95% CI −1.9 to −0.5) for boys, and −0.6 percentage points (95% CI −1.3 to 0.1) for girls Van de Gaar 2014 (share of students with overweight or obesity): Increase (OR 1.27, 95% CI 0.78 to 2.07) |
| Total milk intake* (10 months to 5 years) 1,066,947 students in 1246 schools 1 CBA study and 1 NRCT ⊕⊝⊝⊝ VERY LOWj | Elbel 2015a (number of milk‐taking events per 100 students): −4 events (P = 0.24, 10 months follow‐up) Schwartz 2016 (total milk sales): −3 ml/day (95% CI −6 to −1) |
| B.3 Small prizes for the selection of healthier beverages in school cafeterias | |
|
Sugar‐sweetened milk selection and purchases (3 to 20 months)
4213 students in 12 schools
1 RCT and 2 ITS studies
⊕⊕⊕⊝ MODERATEk (Hendy 2011) ⊕⊕⊝⊝ LOW (Emerson 2017; Siegel 2016b) |
Hendy 2011 (number of meals with unhealthy beverages selected)−3.0 meals/week (P = 0.000) Siegel 2016b (chocolate milk purchases): −0.12 servings/day (P < 0.001) Emerson 2017 (chocolate milk purchases): −0.12 servings/day (P < 0.001) |
| Total milk purchasesa (3 to 13 months) 3961 students in 11 schools 2 ITS studies ⊕⊕⊝⊝ LOW | Siegel 2016b (total milk purchases): −0.03 servings/day (P < 0.001) Emerson 2017 (total milk purchases): +0.04 servings/day (P < 0.001) |
| Food wastea (follow‐up not reported) 96 students in 1 school 1 ITS study ⊕⊝⊝⊝ VERY LOWl | Siegel 2016b (share of total milk selected but not consumed): +5 percentage points (P = 0.275) |
| B.4 Improved placement of healthier beverages in school cafeterias | |
| Sugar‐sweetened milk intake (3 to 4 months) 2638 students in 14 schools 1 cluster‐RCT ⊕⊕⊝⊝ LOWm,n | Cohen 2015 (selection and consumption of sugar‐sweetened milk): No statistically significant effect (data not shown) |
| White milk intake* (3 to 4 months) 2638 students in 14 schools 1 cluster‐RCT ⊕⊕⊝⊝ LOWm,n | Cohen 2015 (selection and consumption of white milk): No statistically significant effect (data not shown) |
|
Stakeholder discontenta (3 to 4 months)
2638 students in 14 schools
1 cluster‐RCT ⊕⊝⊝⊝ VERY LOWo |
Cohen 2015 reports that the intervention "met with substantial resistance from teachers, who were concerned that younger students were having trouble accessing the less prominently displayed sugar‐sweetened milk" |
| B.5 Fruit provision in schools | |
| SSB consumption (9 months to 6 years) 3494 students in 47 schools 1 cluster‐RCT and 1 CBA study ⊕⊝⊝⊝ VERY LOWp,q,r,s | Da Costa 2014 (SSB intake): Decrease (P = 0.003, data not intelligible to review authors) Øverby 2012 (SSB intake measured with a unhealthy snack frequency score):−1.4 in the free‐fruit provision group, −1.1 in the fruit subscription group, −0.7 in the control group (P = 0.002 for time*group interaction) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; N/A: not assessed; NRCT: non‐randomised controlled trial; OR: odds ratio; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | |
aOutcomes included as potential adverse outcomes. bDowngraded for imprecision: The CIs reported by Lichtman‐Sadot 2016 for elementary and middle schools, as well as those reported by Huang 2012 for all school types considered together are large and include zero. cDowngraded for risk of bias and imprecision: In Schwartz 2009, participants were not blinded and data were self‐reported. Results are shown graphically and narratively only, and the study authors note that the survey that was used to assess this outcome may not have been sensitive enough to detect changes. dClassification of study design: Van de Gaar 2014 included four schools, two of which were chosen by the flip of a coin to serve as intervention schools. Given the small number of randomised units, randomisation may not have been sufficient to attain baseline comparability of the intervention and control groups. We therefore included Van de Gaar 2014 as a NRCT in our evidence synthesis. eDowngraded for risk of bias: We judged all four studies contributing data to this outcome to be at high or unclear risk of bias in at least one domain. In Elbel 2015a, Muckelbauer 2009 and Van de Gaar 2014 participants were not blinded, and outcome data were self‐reported. In Visscher 2010 and Van de Gaar 2014 baseline differences between the intervention and control groups may have affected effect estimates. Muckelbauer 2009 and Van de Gaar 2014 report substantial attrition and performed per protocol analyses. fDowngraded for imprecision: The CIs reported by Muckelbauer 2009 for SSB intake are large and include zero. Elbel 2015a reports that no effects were observed, without providing quantitative outcome data, and Visscher 2010 does not report an overall effect estimate but only unadjusted means for individual schools and study periods. gDowngraded for risk of bias: Our main concern with Schwartz 2016 was that due to its stepped‐wedge design underlying temporal trends may have influenced the results. hDowngraded for risk of bias: In Muckelbauer 2009 and Van de Gaar 2014 baseline differences between intervention and control groups and incomplete outcome data may have affected effect estimates. iDowngraded for imprecision: The CIs reported by Van de Gaar 2014 for the share of students with overweight or obesity, and by Muckelbauer 2009 for z‐BMI are large and include zero, as does the CI reported by Schwartz 2016 for the share of female students with overweight or obesity. jDowngraded for risk of bias:Schwartz 2016 used a stepped‐wedge design, and underlying temporal trends may have influenced results. kDowngraded for risk of bias: We judged Hendy 2011 to be at high or unclear risk of bias in several domains. Attrition was substantial (32%) and analyses were per protocol. Only healthy beverage selection was recorded directly, and effect estimates for unhealthy beverage selection are based on the assumption that the share of children not having any beverage for lunch was approximately 1% and therefore negligible (effect estimates for unhealthy beverage selection are not reported in the study’s published report, but were calculated by us based on the above information, which was provided to us by the study’s corresponding author). lDowngraded for imprecision: For food waste, Hudgens 2017 (a secondary publication to Siegel 2016b) reports that P > 0.05 (no exact P value or CI reported). mDowngraded for risk of bias: We judged Cohen 2015 to be at unclear risk of bias in several domains. For beverage intake baseline outcome measurements are not reported for the intervention and control groups separately; relevant baseline differences may have existed. The study does not report if observers were blinded to the intervention or control status of the schools. nDowngraded for imprecision: For sugar‐sweetened and plain low‐fat milk intake Cohen 2015 only reports that no significant effects were observed, but does not provide an effect estimate, an exact P value or a CI. The study may have been underpowered to detect changes in beverage intake, which was not the primary focus of the study. oEvidence on this outcome is not based on a systematic study design, but is derived from anecdotal evidence. We therefore judged it to be of very low certainty. pDowngraded by on level for risk of bias (Da Costa 2014): In Da Costa 2014, participants were not blinded, the outcomes were self‐reported, and the behavioural co‐intervention in particular may have introduced social desirability bias. Attrition was high (54%) and dropouts differed from those remaining in the study. Baseline characteristics differed substantially between intervention and control groups, and it is not clear if these were taken into account in the analyses on which the study's conclusions about SSB intake are based. The study does not report if clustering at the school level was taken into account in the analyses. We therefore downgraded the level of evidence by one level for risk of bias. qDowngraded for imprecision (Da Costa 2014):Da Costa 2014 reports that the intervention resulted in a significant reduction in SSB intake, but does not provide an effect estimate. rDowngraded by one level for risk of bias (Øverby 2012): In Øverby 2012, participants were not blinded and the outcomes were self‐reported. Study authors note that contamination is likely, as some control schools started to organise fruit provision schemes independently of the intervention during the study phase. Study authors note that schools self‐selected to the intervention group, and that this may have lead to baseline differences between the intervention and control groups. sDowngraded for publication bias: We found a number of studies on school fruit provision programmes that did not report effects on SSB intake, even though overall dietary intake was assessed. Publication and reporting bias seems possible.
Summary of findings 4. Economic tools compared to no or alternative intervention.
| C Economic tools compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| C.1 Price increases on SSB | |
| SSB sales (4 to 12 months) 1 store, 7 leisure centres and 37 restaurants in 29 cities 3 ITS studies ⊕⊕⊕⊝ MODERATa | Cornelsen 2017 (SSB items sold per customer): −9% (95% CI −15 to −3) Blake 2018 (volume of red‐labelled beverages):−28% (95% CI −32 to −23) Breeze 2018 (volume of SSB sold per attendance): −27% (95% CI −59 to −3) |
| Total beverage sales and revenueb (4 to 12 months) 1 convenience store and 7 leisure centres 2 ITS studies ⊕⊕⊝⊝ LOW | Blake 2018 (total revenue from beverage sales): −10% (95% CI −14 to −7) Breeze 2018 (total cold beverage unit sales): −5% (P > 0.05) |
| Stakeholder discontentb (4 months) 1 convenience store 1 ITS study ⊕⊕⊝⊝ LOW | Blake 2018 reports that "[t]he issue of customer complaints was a strong sub‐theme from the qualitative interviews of store and hospital staff. (…) [O]ngoing concerns about customer perceptions of the store and the long‐term impact on the business were expressed by all staff interviewees” |
| C.2 Financial incentives to purchase low‐calorie beverages implemented through supermarket loyalty cards | |
| SSB sales (3 to 6 months) 1750 customers of 3 supermarket chains 3 RCTs ⊕⊕⊝⊝ LOWc,d |
Ball 2015 (self‐reported SSB intake): +10 ml/day (95% CI 0 to 20)
Ball 2015 (SSB purchases): +55 ml/day (95% CI −7 to 117)
Ni Mhurchu 2010 (energy density of beverages purchased): −0.1 MJ/kg (95% CI −0.4 to 0.2) Franckle 2018 (number of red‐labelled beverages purchased per month): −0.14 beverage items/month (95% CI −0.8 to 0.6) |
| Purchases of less‐healthy products (6 months) 1028 customers of 1 supermarket chain 1RCT ⊕⊕⊝⊝ LOWc,d | Ni Mhurchu 2010 (purchases of less‐healthy products, including foods and beverages): +0.07 kg/week (95% CI −0.15 to 0.29) |
| C.3 Price discounts on low‐calorie beverages in community stores | |
| SSB sales (6 months) 8515 inhabitants of 20 remote indigenous communities 1 cluster‐RCT ⊕⊕⊝⊝ LOWe,f | Brimblecombe 2017 (SSB sales): +6% (95% CI −3 to 15) |
| Total energy content of grocery purchasesb (6 months) 8515 inhabitants of 20 remote indigenous communities 1 cluster‐RCT ⊕⊕⊝⊝ LOWe,f | Brimblecombe 2017 reports that "[t]here have been concerns that total calories purchased might increase with price subsidies on healthy foods thereby potentially negating health gains. Our findings add to this evidence because we observed increases (albeit non‐significant) in the volume of other food purchases and increases in energy and sodium (due to its ubiquity in the food supply) during and after the price discount. Similar increases in purchases were observed for both healthy and less healthy food groups" |
| Taxation of SSB | |
| Not included in this review (for a forthcoming Cochrane Review on taxation of SSB see Heise 2016, for existing systematic reviews on taxation of SSB see Backholer 2016, Cabrera Escobar 2013 and Nakhimovsky 2016) | |
| CI: Confidence interval; ITS: interrupted‐time‐series study; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | |
aUpgraded by one level for dose‐response gradient and magnitude of effect: For effects on SSB sales we noticed a dose‐response gradient, and deemed the magnitude of the effect to be large for the two studies in which a relatively larger price increase was applied. bOutcomes included as potential adverse outcomes. cDowngraded for risk of bias: In Ball 2015, Ni Mhurchu 2010 and Franckle 2018 participants were not blinded, and outcome data were either self‐reported or assessed through loyalty cards, which may have been used selectively by the participants. Ball 2015 notes that SSB purchases were highly variable at baseline, with the highest values in the control group, and that the observed effects may be explained by a regression to the mean. dDowngraded for imprecision: The 95% CIs of the primary outcome measure of interest to this review reported by Ball 2015, Franckle 2018 and Ni Mhurchu 2010 are large and include zero. eDowngraded for risk of bias:Brimblecombe 2017 used a stepped‐wedge design, and all stores received the intervention, but at different time points. The study does not report if stores receiving the intervention later (i.e. serving as controls for longer) differed from those receiving it earlier with regard to baseline outcome measurements and other characteristics. We therefore judged the study to be at unclear risk of bias for baseline differences between intervention and control groups. fDowngraded for imprecision: The CIs reported by Brimblecombe 2017 for beverage sales are large and include zero.
Summary of findings 5. Advertisement regulation compared to no or alternative intervention.
| D Advertisement regulation compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| We found no eligible studies on advertisement regulation | |
Summary of findings 6. Whole food supply interventions compared to no or alternative intervention.
| E Whole food supply interventions compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| E.1 Voluntary food and beverage industry initiatives to improve the whole food supply | |
| SSB sales (3 to 4 years) 61,126 households and 17 companies 2 controlled ITS and 1 CBA study ⊕⊝⊝⊝ VERY LOWa | Ng 2014a (energy from beverages sold):Decrease: (−14 kcal/capita/day in the intervention group compared to −3 kcal/per capita/day for national‐brand companies not participating in the pledge; no P value or CI reported) Ng 2014a (SSB sales by companies participating in the Healthy Weight Commitment Foundation Pledge): −7 kcal/per capita/day (no P Value or CIs reported, data for the CG not reported) Ng 2014b (SSB purchases): Increase relative to expected (P < 0.001, data shown graphically only) Taillie 2015 (percentage volume of SSB purchased):Decrease (P < 0.01, results shown graphically only) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; SSB: sugar‐sweetened beverages | |
aDowngraded for risk of bias: In Ng 2014a and Ng 2014b it seems possible that relevant baseline differences between the intervention and control groups existed and affected results. In Ng 2014a, Ng 2014b and Taillie 2015, contamination is likely, as a number of other food and beverage companies in the USA announced similar initiatives during the study period, as noted by the study authors in Taillie 2015, and were possibly included in the control groups of the three studies. This would have biased observed effects towards null. In the ITS analyses reported by Taillie 2015 and Ng 2014b, observed effects may have been affected by changes not attributable to the intervention, such as shifts in public attitudes and macroeconomic changes, as pointed out by the authors of both studies.
Summary of findings 7. Retail and food service interventions compared to no or alternative intervention.
| F Retail and food service interventions compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| F.1 Healthier default beverages in children's menus in restaurants | |
| SSB sales (6 years) 145 restaurants in 1 theme park 1 ITS study ⊕⊕⊝⊝ LOWa,b | Peters 2016a (share of children's menus served with SSB): −68 percentage points |
| F.2 In‐store promotion of low‐calorie beverages in supermarkets | |
| SSB sales (6 months) 8 supermarkets from 2 chains 1 cluster‐RCT ⊕⊕⊕⊝ MODERATEc | Foster 2014 (in‐aisle SSB sales per supermarket): −11 l/day (95% CI −63 to 40) Foster 2014 (check‐out cooler SSB sales per supermarket): −2 units/day (95% CI −5 to 1) |
| F.3 Healthier vending machines in workplaces and schools | |
| SSB sales (18 to 24 months) 6 schools and 4 worksites 2 NRCTsd ⊕⊝⊝⊝ VERY LOWd,e,f | Ermetici 2016 (SSB intake, normal weight participants): −1.1 times/week (95% CI −1.5 to −0.7) Ermetici 2016 (SSB intake, participants with overweight and obesity): −0.8 times/week (95% CI −1.5 to −0.1) French 2010 (SSB intake): +14 ml/day (P > 0.05) |
| Total revenueg (5 months) 1 worksite 1 cluster‐RCT ⊕⊕⊝⊝ LOWh | Hua 2017 reports that "the control machines and machines that had product guidelines and price changes both had small but significant decreases in revenue (‐$156.10 and ‐$593.55, respectively; P < 0.05)." |
| F.4 Urban planning restrictions on new fast‐food outlets | |
| SSB intake (3 to 4 years) 11,821 inhabitants of 1 city and 1 county 1 CBA study ⊕⊝⊝⊝ VERY LOWi,j | Sturm 2015 (SSB intake frequency, measure or scale not reported): −0.9 (P > 0.05) |
| F.5 Restrictions on the number of stores selling SSB in remote communities | |
| SSB sales (8 months) 3 stores in 1 remote community 1 ITS study ⊕⊝⊝⊝ VERY LOWk,l | Minaker 2016 (community‐wide SSB sales, model controlling for the summer peak): CAD −51 /day (95% CI −166 to 65) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; NRCT: non‐randomised controlled trial; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | |
aDowngraded for risk of bias: In Peters 2016a, data for the first three years post‐intervention are missing, and the point of analysis is therefore not the point of intervention. Study authors note that data were provided by the Walt Disney company based on the understanding that only certain outcomes are reported. Effect estimates may have been affected by missing data, and reporting may have been selective. bUpgraded for magnitude of effect: We judged the observed effect size to be large, and unlikely to have arisen by chance or due to bias. We upgraded the level of evidence by one level for this reason.Downgraded for imprecision: For all outcomes except effects on check‐out cooler bottled water sales the CIs are large and include zero. dClassification of study design: In French 2010, two out of four bus garages were selected to serve as intervention sites by the toss of a coin. Given the small number of randomised units, randomisation may not have been sufficient to attain baseline comparability of the intervention and control groups, and the study does not report baseline characteristics other than baseline outcome measurements separately for the intervention and control groups. We therefore included French 2010 as a NRCT in our evidence synthesis. eDowngraded for risk of bias: In Ermetici 2016 and French 2010, participants were not blinded, and outcome data are self‐reported in both studies. In Ermetici 2016, schools were allocated to the intervention and control groups based on pre‐existing co‐operation with the researchers, which may have led to unobserved baseline differences. In French 2010, survey participants were redrawn each time from the study population, and the method used for the selection (40 participants were enrolled at each garage on a first‐come‐first‐served basis) does not guarantee representativeness. fDowngraded for publication bias: We note that data on SSB sales were collected, but not reported in a standard way by Hua 2017. Publication bias seems possible. gOutcomes included as potential adverse outcomes. hDowngraded by two levels for risk of bias:Hua 2017 does not report baseline characteristics other than baseline outcome measurements, and differences in baseline characteristics between intervention and control groups may have influenced results. Baseline outcome measurements differed substantially across vending machines, and the study does not report if this was taken into account in the analyses. All vending machines were located on the same university campus, and contamination seems likely. iDowngraded for risk of bias: We judged Sturm 2015 to be at high or unclear risk of bias in several domains. There were substantial differences in baseline outcome measurements and in demographic and socio‐economic characteristics between the intervention and control groups, which may have affected the effect estimates. Moreover, given the potential mobility of residents between the different parts of Los Angeles, contamination seems possible. jDowngraded for imprecision: Sturm 2015 reports that effects on SSB intake did not reach statistical significance at the 5% level (P > 0.05, no CI or exact P value reported). kDowngraded for risk of bias: We judged Minaker 2016 to be at low risk of bias in most domains. However, the study authors note that the follow‐up period was relatively short and did not include a summer season, which limited the study’s ability to control for seasonality. lDowngraded for imprecision: The CI reported by Minaker 2016 is large and includes zero.
Summary of findings 8. Action across sectors compared to no or alternative intervention.
| G Action across sectors compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| G.1 Trade and investment liberalisation in low‐ and middle‐income countries | |
| SSB sales ( 4 years) 4 countries 2 controlled ITS studies ⊕⊝⊝⊝ VERY LOWa | −Baker 2016 (annual rate of change in volume sales of SSB per capita): −1.4 percentage points (95% CI −2.5 to −0.4) Baker 2016 (annual rate of change in volume sales of sugar from SSB per capita): −1.0 percentage points (95% CI −1.9 to −0.06) Baker 2016 (annual rate of change in volume sales of sports and energy drinks per capita): +0.3 percentage points (P > 0.05, SE 0.8) Schram 2015 (retail sales of SSB): +13 ml/capita/day (95% CI 10 to 15) |
| G.2 Government food benefit programmes with incentives and restrictions | |
| SSB intake (3 to 12 months) 2274 adults and 18,207 children 3 RCTs with 5 comparisons ⊕⊕⊕⊝ MODERATEb | Collins 2016 WIC (intake of sugar from SSB, USD 60 versus no USD benefit/month):−5 g/day (95% CI −8 to −3) Collins 2016 WIC (intake of sugar from SSB, USD 60 versus USD 30 benefit/month): −1 g/day (95% CI −3 to 2) Collins 2016 WIC (intake of sugar from SSB, USD 30 versus no USD benefit/month): −5 g/day (95% CI −8 to −2) Harnack 2016 (SSB intake, incentives + restrictions): −180 ml/day (95% CI −338 to −22) Harnack 2016 (SSB purchases, incentives + restrictions):USD −0.3/day (95% CI −0.5 to −0.2) Olsho 2016 (energy intake from SSB): −5 kcal/day/person (95% CI −21 to 11) Olsho 2016 (sugar intake from SSB): −1 g/day/person (95% CI −5 to 2) |
|
Stigma (9 ‐ 11 months)
2009 adults 1 RCT N/A |
Olsho 2016 reports that “the (…) evaluation found no evidence of increased stigma associated with rebate use. This may be because in most settings [the project] was implemented automatically via electronic cash registers.” |
|
Alcoholic beverage intakec (9 ‐ 11 months)
2009 adults 1 RCT ⊕⊕⊝⊝ LOWd |
Olsho 2016 (alcoholic beverage intake): +0.08 drinks/day (95% CI 0.01 to 0.15) |
| G.3 Government food benefit programmes without incentives and restrictions | |
| SSB intake (3 months) 25,150 children 1 RCT with 3 comparisons ⊕⊕⊝⊝ LOWe,f | Collins 2016 SNAP (intake of sugar from SSB, USD 60 vs no USD benefit/month):−0.5 g/day (95% CI −2 to 1) Collins 2016 SNAP (intake of sugar from SSB, USD 60 vs USD 30 benefit/month): +1 g/day (95% CI −1 to 3) Collins 2016 SNAP (intake of sugar from SSB, USD 30 vs no USD benefit/month): −2 g/day (95% CI −4 to 1) |
|
SSB intake (8 months)
2844 adults 1 CBA study ⊕⊝⊝⊝ VERY LOWg |
Waehrer 2015 (SSB intake, median): +34 kcal/day (95% CI 7 to 60) |
| G.4 Multi‐component community campaigns focused on SSB | |
| SSB sales (3 years) 32 supermarkets from 6 chains in 2 counties 1 controlled ITS study ⊕⊕⊕⊝ MODERATEh | Schwartz 2017 (SSB sales per product and store): −1.6 l/day (95% CI −2.0 to −1.2) (equivalent to a −20% decrease in the intervention group and a 0.8% increase in the control group) Schwartz 2017 (sports drinks sales per product and store):−0.4 l/day (95 CI −1.5 to 0.7) Schwartz 2017 (fruit drinks sales per product and store): −1.5 l/day (95% CI −2.0 to −0.9) |
| CBA: Controlled‐before‐after study; CI: Confidence interval; ITS: interrupted‐time‐series study; NRCT: non‐randomised controlled trial; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | |
aDowngraded for risk of bias: Study authors of Baker 2016 and Schram 2015 note that there were relevant baseline differences between intervention and control countries, which may have affected the results. In Schram 2015 in particular, differences in baseline outcome measurements were large, approximately five times the size of the observed intervention effect. In Baker 2016 study authors note that the intervention may have had regional effects affecting the control country. In both studies study authors note that factors not attributable to the intervention may have differentially affected outcome measures in the intervention and control countries. bDowngraded for risk of bias: In Collins 2016wic, Harnack 2016 and Olsho 2016 participants were not blinded, and SSB intake data is self‐reported. Harnack 2016 also assessed SSB purchasing data based on grocery receipts, which may have been turned in selectively by participants, as noted by the study authors. cOutcomes included as potential adverse outcomes. dDowngraded by two levels for risk of bias: In Olsho 2016, study authors note that reported effects on alcoholic beverage intake may have been driven by several outliers in the second follow‐up assessment, who reported more than eight alcoholic drinks in the prior 24 hours. Participants were not blinded and outcomes self‐assessed. eDowngraded for risk of bias: In Collins 2016 SNAP participants were not blinded, and SSB intake data is self‐reported. fDowngraded for imprecision: Collins 2016 SNAP reports three comparisons (USD 60 vs no USD, USD 60 vs USD 30, and USD 30 vs no USD monthly benefit), and the 95% CI for all three comparisons include zero. gDowngraded for risk of bias: In Waehrer 2015, baseline outcome measurements as well as demographic and socio‐economic characteristics of participants differed substantially between the intervention and control groups. Study authors note that the control group may have included a substantial number of individuals receiving SNAP benefits at some time point during the study phase, and that this may have biased the results towards null. hUpgraded for magnitude of effect: We judged the effects on beverage sales to be large, and unlikely to be arisen by chance or through bias.
Summary of findings 9. Home‐based interventions compared to no or alternative intervention.
| H Home‐based interventions compared to no or alternative intervention in children, youth and adults: impact on primary outcomes | |
|
Outcomes (follow‐up) No. of clusters or participants No. of studies Certainty of Evidence |
Impact |
| H.1 Improved access to low‐calorie beverages in the home environment | |
| SSB intake (4 to 12 months) 1130 children, teenagers and adults 6 RCTs ⊕⊕⊕⊝ MODERATEa | Albala 2008, Anand 2007, Ebbeling 2006, Ebbeling 2012, Hernández‐Cordero 2014 (SSB intake, pooled effect estimate): −413 ml/day (95% CI −684 to −143) Tate 2012 (energy intake from beverages):−88 kcal/day (95% CI −124 to −51) |
|
Body weight (6 to 12 months ‐ comparison with no intervention, teenagers)
320 teenagers 2 RCTs ⊕⊕⊕⊕ HIGH |
Ebbeling 2006 (BMI):−0.14 kg/m2 (95% CI −0.54 to 0.26) Ebbeling 2012 (BMI): −0.57 kg/m2 (95% CI −1.12 to −0.01) |
|
Body weight and waist circumference (6 to 9 months ‐ comparison with general weight‐loss counselling, adults)
558 adults 2 RCTs ⊕⊕⊝⊝ LOWb,c |
Hernández‐Cordero 2014 (BMI):−0.17 kg/m2 (95% CI −0.6 to 0.2)
Tate 2012 and Hernández‐Cordero 2014 (pooled analysis, body weight in kg): −1.11 kg (95% CI −3.56 to 1.34) Tate 2012 and Hernández‐Cordero 2014 (pooled analysis, waist circumference): −0.83 cm (95% CI −3.65 to 1.98) |
| Adverse outcomes (3 to 12 months) 653 children, teenagers and adults 4 RCTs N/Ad | Albala 2008, Ebbeling 2006 and Ebbeling 2012 report that no serious adverse effects related to study participation were observed Hernández‐Cordero 2014 reports that "[t]wenty‐two participants from the IG group reported an adverse event during the intervention. The most common adverse events reported were tiredness, nausea, stress, or frequent urge to urinate" |
| H.2 Provision of active video‐gaming equipment to teenagers | |
|
SSB sales (10 months)
262 teenagers 1 RCT ⊕⊝⊝⊝ VERY LOWe,f,g |
Simons 2015 (share of participants consuming more than 1400 ml SSB a week): Decrease (OR 0.71, 95% CI 0.36 to 1.41) |
|
Injuriesh (10 months)
262 teenagers 1 RCT N/Ad |
Simons 2015 reports that at 10 months "1/5 of the intervention group reported having experienced an injury (the most frequently mentioned injuries were bruises or strained muscles/tendons) while playing the Move video games" |
| CI: Confidence interval; N/A: not assessed; OR: odds ratio; RCT: randomised controlled trial; SSB: sugar‐sweetened beverages | |
aDowngraded for risk of bias: Participants were not blinded, and beverage intake data are self‐reported in all studies contributing data to this outcome. bDowngraded for risk of bias: In Hernández‐Cordero 2014 authors note that contamination is likely, and would have biased results towards null. In Tate 2012 SSB intake and BMI were inclusion criteria and assessed, but are not reported for the main three‐arm comparison. cDowngraded for imprecision: The CIs reported by Hernández‐Cordero 2014 and Tate 2012 for body weight outcomes are large and include zero. dDue to the heterogeneity of definitions and assessment methods used for adverse outcomes by the studies contributing data to the outcome, we did not assess the certainty of evidence with GRADE for this outcome. eDowngraded by one level for risk of bias: In Simons 2015, participants were not blinded, and outcomes are self‐reported only. Data on SSB consumption are presented only in dichotomised form (share of participants consuming more or less than 1400 ml of SSB a week), and this is not mentioned in the trial register entry or the published protocol. fDowngraded for imprecision: The CI reported by Simons 2015 for SSB intake is large and includes zero. We therefore downgraded the level of evidence by one for imprecision. gDowngraded for probability of publication bias: Most studies comparing active and non‐active video gaming do not report effects on SSB intake. Across‐studies reporting bias seems possible. hOutcomes included as potential adverse outcomes.
Background
Please see Appendix 1 for a list of common abbreviations used throughout this review.
Description of the condition
Sugar‐sweetened beverages and health
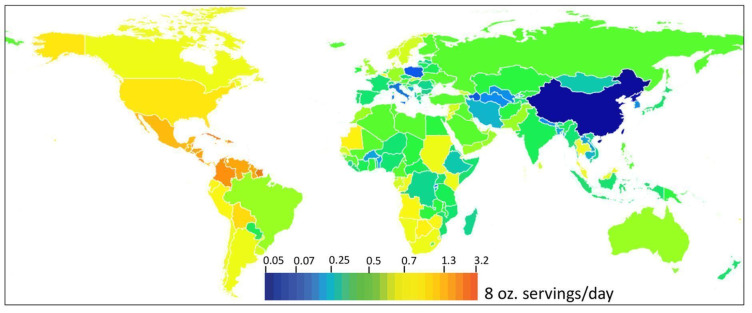
Dietary and diet‐related risk factors are a major cause of death and disease worldwide. It was estimated that in 2016, 10% of the global burden of disease could be attributed to diets of poor nutritional content (Gakidou 2017; IHME 2018). Among the various dietary risk factors sugar‐sweetened beverages (SSBs) have recently received particular attention. Frequent consumption of SSB has been linked to an increased risk for a number of adverse health outcomes. There is evidence for a causal role of SSB in the development of overweight and obesity from randomised controlled trials in children and youth (De Ruyter 2014; Ebbeling 2012) and systematic reviews of observational and intervention studies (Hu 2013; Malik 2013; Luger 2017; Vartanian 2007). Moreover, systematic reviews of observational studies have found positive associations between SSB intake and type 2 diabetes (Imamura 2015; Malik 2010a; Malik 2010b; Vartanian 2007), cardiovascular disease (Huang 2014; Malik 2010a; Vos 2016), and dental caries (Bleich 2018; Vartanian 2007).
Definition of sugar‐sweetened beverages
In the broadest sense, the term SSB is used for liquids with added caloric sweeteners (USDA 2015a, USDA 2015b). Contrary to the literal meaning of the term SSB, alcoholic beverages with added sugars and sugar‐sweetened milk are generally not included in the definitions used in the literature (AAP 2015; Bleich 2018; Gakidou 2017; Singh 2015). Following this convention, we define SSBs for the purposes of this review as non‐alcoholic, non‐dairy beverages with added caloric sweeteners. This definition includes, but is not limited to, carbonated soft drinks (sodas), fruit juices with less than 100% fruit content and added sugars, sugar‐sweetened energy and sports drinks, sugar‐sweetened vitamin waters and flavoured water, and sugar‐sweetened coffee and tea beverages. The definition covers both ready‐to‐drink beverages and beverages prepared by consumers from syrups, concentrates or powder, or by adding sugar to beverages such as tea and coffee. Interventions targeting sugar‐sweetened milk are included in this review, but are considered as a separate category.
The pathophysiology of sugar‐sweetened beverage consumption
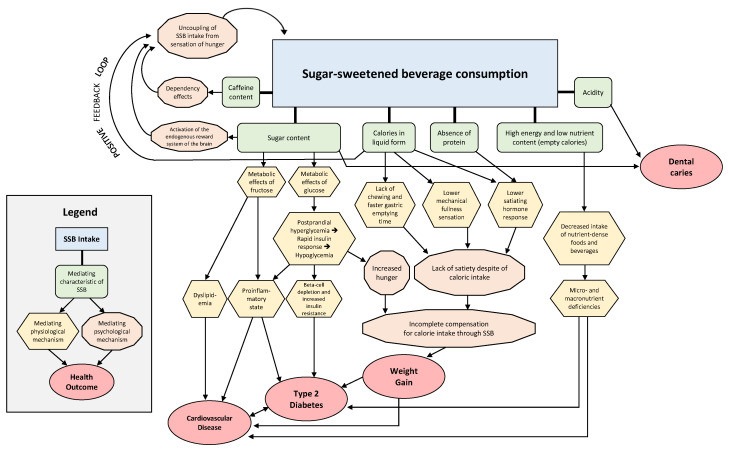
A number of physiological and psychological mediating mechanisms are discussed as explanations for the negative health outcomes linked to SSBs. With regard to the causal role of SSB in weight gain, it has been shown that individuals incompletely compensate for energy consumed as SSB (Malik 2010a; Wolf 2008). Incomplete caloric compensation refers to the following phenomenon: when SSBs are added to a diet, energy intake from other sources is generally reduced by an amount smaller than the amount obtained from the SSB consumed. Two mechanisms may be responsible for this phenomenon: the inability of SSBs to induce feelings of satiety equivalent to their caloric content, and the tendency of individuals to consume SSB regardless of hunger and satiety.
A number of factors may contribute to this bi‐directional uncoupling of SSB consumption from normal feelings of hunger and satiety:
The lack of chewing and the lower orosensory response, as well as the faster gastric emptying time and lower mechanical fullness sensations associated with liquids as compared to solid foods (Cassady 2012; Poppitt 2015).
The limited capacity of liquid calories to induce a satiating hormone response, including an attenuated release of glucagon‐like peptide 1, and a lower ghrelin suppression, compared to solid calories (Cassady 2012).
The lower fullness sensation and satiating hormone response to SSB as compared to isocaloric beverages containing milk or other sources of protein (Maersk 2012; Poppitt 2015).
The central nervous response to sugar, in particular its capacity to activate the endogenous reward system of the brain (Johnson 2009; Poppitt 2015).
The caffeine content of many SSBs, which can induce dependence effects (Keast 2015).
The reduced perception of sweetness, and of the sugar and caloric content of chilled foods and beverages.
The relatively high glycaemic index (GI) and glycaemic load (GL) of SSBs, as compared to beverages without added sugars and unprocessed foods, which can result in postprandial hyperglycaemia, a subsequent rapid insulin response followed by a marked drop in plasma glucose levels and concomitant increased hunger (Ludwig 2002; Malik 2010a).
The positive association of SSB with type 2 diabetes and cardiovascular disease seems to be mediated largely through adiposity, which is a known risk factor for these conditions (Malik 2015). However, it has been argued that additional direct causal pathways may exist (Imamura 2015; Malik 2010a; Malik 2015). More specifically, highly processed dietary sugars, as they are present in SSB, may have adverse metabolic effects above and beyond their caloric content (Johnson 2009; Malik 2015; Vos 2016). The sugars most commonly used in SSB are either sucrose (a disaccharide made up of equal parts of glucose and fructose) or high‐fructose corn syrup, which consists of glucose and fructose in monomeric form, with a fructose content ranging from 42% to 55% (Johnson 2009). The degree to which sucrose and high‐fructose corn syrup are used in SSB varies by product and geographic region (Nestle 2015).
SSBs constitute a source of empty calories, i.e. they contain energy but no micro‐ and macronutrients except water and sugars. SSB consumption can therefore lead to a reduced intake of micro‐ and macronutrients through alternative beverages as well as through solid foods, even under conditions of incomplete caloric compensation (Vartanian 2007). To achieve healthy dietary patterns, nutrient needs must be met without exceeding energy needs (USDA 2015b). Dietary guidelines therefore recommend reducing the intake of energy‐dense but nutrient‐poor foods and beverages, such as SSB, and replacing them with foods and beverages that provide relevant amounts of nutrients and relatively few calories (Hauner 2012; USDA 2015b). Potential causal pathways between SSB consumption and adverse health outcomes are shown in Figure 1.
1.
Physiological and psychological mechanisms linking SSB intake with adverse health outcomes.
Alternatives to sugar‐sweetened beverages
Plain water has been the most commonly used source of hydration for the largest part of the evolution of the human species (Wolf 2008). In the context of obesity and obesity‐related diseases, increased consumption of drinking water has been linked to a reduced total energy intake among certain populations (Daniels 2010; Muckelbauer 2013). This effect of drinking water on energy intake may be due to a concomitantly reduced intake of caloric beverages, and possibly also to a reduced intake of solid foods when water is consumed with or before meals, even though this second effect is disputed (Daniels 2010; Muckelbauer 2013). Current dietary guidelines therefore recommend drinking water as a preferred alternative to SSB (DGE 2015; USDA 2015b).
Further recommended alternatives to SSB are low‐fat or fat‐free milk, including fortified soy beverages (USDA 2015a; USDA 2015b). Tea and coffee are also recommended by the Dietary Guidelines for Americans 2015 ‐ 2020 as alternatives to SSB for the general public (USDA 2015b), but caffeine intake from coffee, tea and other sources should be limited to moderate amounts among children, adolescents and women who are pregnant or considering pregnancy (USDA 2015a).
Beverages containing non‐nutritive sweeteners (NNSs) are not generally recommended by dietary guidelines as preferred alternatives to SSB (Borges 2017; DGE 2015; USDA 2015a; USDA 2015b). NNSs, also known as low‐calorie, low‐energy or artificial sweeteners, are chemically diverse compounds with no or minimal caloric content and a sweet taste of varying intensity (Fitch 2012). In cross‐sectional and cohort studies frequent consumption of beverages with NNS was associated with adverse health outcomes similar to those associated with SSB, including an increased risk of obesity and type 2 diabetes (Borges 2017; Imamura 2015). However, most RCTs directly comparing beverages sweetened exclusively with NNS versus SSB have shown results favouring the former for weight gain (Miller 2014). Moreover, available prospective studies indicate that after adjustment for possible confounders consumption of beverages with NNS is associated with a lower risk of diabetes than consumption of equal amounts of SSB (Greenwood 2014). Furthermore, safety reviews by regulatory and scientific bodies have generally found NNS to be safe at the levels consumed by most populations (Fitch 2012; USDA 2015a). In much of the literature, the term 'diet beverages' is used to denote beverages that contain NNS; depending on the context, the term may refer to beverages sweetened exclusively with NNS, or include beverages that contain NNS in addition to caloric sweeteners. In this review, we follow this convention, but try to specify whenever possible if the term refers to beverages sweetened exclusively with NNS, or to beverages containing NNS and caloric sweeteners, or to both types of beverages.
Full‐fat milk and 100% fruit juice are both relevant sources of essential nutrients and are relatively energy‐dense. Excessive amounts of these beverages can therefore contribute to a positive energy balance. Consequently, current dietary guidelines recommend limiting intake of 100% fruit juice among children and adolescents to moderate amounts (Auerbach 2018; USDA 2015b), and preferring low‐fat or fat‐free milk to full‐fat milk (USDA 2015b). Moreover, full‐fat milk is relatively high in saturated fat (USDA 2015a). By contrast, beverages prepared by adding varying amounts of 100% fruit juice to carbonated or uncarbonated water without adding additional caloric sweeteners are generally considered acceptable alternatives to SSB (AAP 2015; DGE 2015).
Sugar‐sweetened milk constitutes another grey area. While dietary guidelines generally recommend choosing unsweetened milk (USDA 2015b), it remains controversial whether or not sugar‐sweetened milk should be targeted in public health interventions (AAP 2015; EU 2018; Patel 2018). It has been argued that limits on the consumption of sugar‐sweetened milk could decrease overall milk intake, and thus overall dietary quality (AAP 2015; Hanks 2014; Patel 2018). Based on feedback from members of our Review Advisory Group (listed in Appendix 2) we therefore consider interventions targeting sugar‐sweetened milk as a separate category, and consider effects on total milk intake as a potential adverse outcome. Appendix 3 provides an overview on all beverage categories considered in this review, and relevant definitions.
Sugar‐sweetened beverage consumption patterns
SSB consumption varies considerably by geographic location, gender, age and socio‐economic status. Based on a systematic review and pooled analysis of dietary surveys, global mean adult daily SSB consumption was estimated at 137 mL (95% confidence interval (CI) 88 mL to 211 mL) in 2010 (Singh 2015). Mean daily SSB consumption is higher in upper‐middle income countries (189 mL) and lower‐middle income countries (140 mL) than in high‐income (121 mL) and low‐income (83 mL) countries, with substantial variation within regions (see Figure 2) (Singh 2015). Consumption is generally higher in younger age groups, among males, and in the Americas as compared with other world regions (Singh 2015).
2.
Estimated SSB consumption by country in 2010 (an 8 oz. serving is equivalent to approximately 237 ml). Reproduced with permission from Singh 2015.
Over the past decades, consumption of SSB has increased substantially in most countries, with decreases observed in some but not all countries beginning around 2000 (Bleich 2015; Gakidou 2017; Malik 2010a; Popkin 2016). Among the populations with the highest intake, SSBs constitute a substantial source of energy (Malik 2010a). It is estimated that in Mexico in 2012, SSB accounted for 7% of total energy intake among children, youth, and adults (Stern 2014). For the USA, mean SSB consumption was estimated to account for 8% of total energy intake among youth in 2010, and for 6.9% of total energy intake for adults (Kit 2013). In the USA, consumption levels have been shown to be particularly high among ethnic minority and socio‐economically disadvantaged groups (Ogden 2011), but have declined substantially since the beginning of the century (Bleich 2018).
The increase in the consumption of SSB observed over the past decades, and SSB consumption in general, have been attributed to a number of factors. Positive associations, which may or may not indicate causal relationships, have been shown for the following factors:
Exposure to advertisements and other forms of marketing (Andreyeva 2011; Hennessy 2015).
Availability of SSB in schools and in other educational settings (Mazarello Paes 2015; Verloigne 2012).
Increases in unit and serving sizes (Flood 2006; Mantzari 2017).
Low relative and absolute prices (Jones 2014).
Television watching and other screen‐based activities (Mazarello Paes 2015).
Low household and individual income, and insecure employment status (Mazarello Paes 2015; Verloigne 2012).
Availability and regular visits to fast‐food restaurants serving SSB (Mazarello Paes 2015).
Exposure to and consumption of other energy‐dense, micronutrient‐poor foods both at and out of home (Mazarello Paes 2015; Verloigne 2012).
Unawareness or disbelief in the association of SSB consumption and weight gain (Park 2014).
Mistrust in the safety of tap water (Onufrak 2014).
Unfavourable parenting practices, including parental consumption of SSB, access to SSB at home, irregular family dinners, and overly permissive and pressuring parenting styles (Mazarello Paes 2015; Verloigne 2012).
Description of the intervention
Various interventions intended to reduce SSB intake and its effects on health have been implemented so far. Two approaches can be distinguished, which can be implemented separately or jointly (CDC 2015; Roberto 2015; WCRFI 2015):
Environmental interventions, targeting the environment, physical, socio‐economic, socio‐cultural or legal, in which individuals make food and beverage choices.
Behavioural interventions, targeting the dietary preferences, knowledge, attitudes, motivations, skills and abilities of individuals, as well as their subjective perception of social norms on food and beverage consumption.
The difference between environmental and behavioural interventions is not always clear‐cut. Interventions such as marketing regulations may aim to influence individual preferences by altering the environment encountered by individuals. In this review, we classify interventions as environmental when they aim to alter the food and beverage environment in a permanent way. We consider interventions that alter the food and beverage environment temporarily with the aim of influencing individual preferences (e.g. a one‐off public media campaign) to be behavioural interventions.
In this review, we only consider behavioural interventions when they are part of larger interventions that also include environmental components, as several systematic reviews focusing on behavioural interventions to reduce the consumption of SSB have already been published (Abdel Rahman 2017; Vargas‐Garcia 2017; Vercammen 2018). In addition, we exclude taxation, as a Cochrane Review on taxation of SSB is ongoing (Heise 2016), and several systematic reviews and meta‐analyses on SSB taxes have been published (Backholer 2016; Cabrera Escobar 2013; Nakhimovsky 2016).
To categorise included studies by intervention area we used the NOURISHING framework, which has been developed by the World Cancer Research Fund International to classify nutrition interventions (WCRFI 2015). It is consistent with the intervention categories used in the World Health Organization (WHO) Global Action Plan for the Prevention and Control of Non‐Communicable Diseases 2013 – 2020 (WHO 2013) and the INFORMAS food environment benchmarking network (INFORMAS 2015). It distinguishes seven environmental and policy intervention areas (including the food system), and three behavioural intervention areas (see Text‐body table 1 below).
| Text‐body table 1: The NOURISHING Framework | ||
| Short name (our wording used in this review) | Intervention area (wording used in the NOURISHING framework) | Examples |
| Environmental interventions | ||
| Labelling interventions | Nutrition label standards and regulations on the use of claims and implied claims on foods | Nutrient lists on food packages, front‐of‐package traffic‐light‐labelling, shelf and menu board calorie labels |
| Nutrition standards in public institutions | Offer healthy foods and set standards in public institutions and other specific settings | School nutrition policies, nutrition standards in health facilities |
| Economic tools | Use economic tools to address food affordability and purchase incentives | Targeted subsidies, price promotions at point of sale, health‐related food taxes (not covered by this review) |
| Advertisement regulation | Restrict food advertising and other forms of commercial promotion | Restrictions on advertising to children that promotes unhealthy diets |
| Whole food supply interventions | Improve the nutritional quality of the whole food supply | Reformulation to reduce sugar content and energy density of processed foods, portion size limits |
| Retail and food service interventions | Set incentives and rules to create a healthy retail and food service environment | Incentives for shops to locate in underserved areas, planning restrictions on food outlets, in‐store promotions |
| Action across sectors | Harness the food supply chain and actions across sectors to ensure coherence with health | Health‐in‐all policies, governance structures for multi‐sectoral engagement |
| Behavioural interventions (included in this review only when implemented as co‐intervention besides an environmental intervention) | ||
| Awareness raising interventions | Inform people about food and nutrition through public awareness | Dissemination of dietary guidelines, public information campaigns |
| Counselling interventions | Nutrition advice and counselling in healthcare settings | Nutrition advice for at‐risk individuals, guidelines for health professionals on nutrition interventions |
| Skill‐building interventions | Give nutrition education and skills | Cooking skills on education curricula, health literacy programmes |
Interventions can also be classified by their level of implementation (CDC 2015):
Policy interventions, which are adopted and implemented at the level of geographically‐defined political or administrative units, such as supra‐national organisations, states, regions or municipalities. Alternative terms include jurisdiction‐based or macro‐level interventions.
Setting‐based interventions, which are adopted and implemented within individual settings, such as schools, work sites, local retail, food service or recreational facilities. Synonyms are community interventions, or meso‐level interventions.
Some interventions may be implemented either within individual settings or at a policy level, or they may target both levels at the same time. Examples include bans on the sale of SSB in schools, which may be mandated by a local school director for his or her individual school, or by national legislation as part of a national school nutrition policy. Similarly, interventions such as labelling are often first evaluated by trials within specific settings, e.g. an individual shop or restaurant, before they are implemented at a policy level, e.g. as part of national regulation. In this review, we classify interventions as policy level when they are implemented at the level of a geographically‐defined political or administrative unit. We classify all other interventions as setting‐based interventions, regardless of whether or not the intervention in question is suitable for implementation at a policy level.
How the intervention might work
All environmental nutrition interventions ultimately aim to change human food and beverage intake by providing conducive environments at different levels. A theoretical framework commonly used to conceptualise the effects of such interventions is the social‐ecological model. It postulates that dietary behaviour is influenced by a host of individual and environmental factors, which can interact to create complex, multi‐layered systems (see Figure 3) (CDC 2015; Peeters 2018; Swinburn 2011). Environmental interventions generally target the macro‐ and meso‐level, i.e. policies and settings. Behavioural interventions generally target the micro‐level, i.e. interpersonal factors such as social norms and networks of social support, and intrapersonal factors such as personal preferences, attitudes and skills (see Figure 3).
3.
Socio‐ecological model of food and beverage intake. Adapted fromCDC 2015.
Environmental interventions targeting the macro‐ and meso‐level are generally considered to have a larger potential population effect, and more likely to be cost‐effective and equitable when compared to micro‐level interventions (Gortmaker 2015; Peeters 2018; Roberto 2015; Swinburn 2011). At the same time, it is more difficult to achieve political consensus about their implementation, and to evaluate them with rigorous scientific study designs (Swinburn 2011) (See Figure 4).
4.
Determinants of diet‐related health outcomes and related interventions. Adapted from Swinburn 2011.
How a given intervention will work also depends on a number of collateral factors, such as the characteristics of the target population, the delivery mechanisms, implementation aspects and further contextual factors (Rutter 2017). The intervention is thus nested in a complex system, as illustrated by the system‐based logic model shown in Appendix 4, which we developed for this systematic review and which guided our data extraction, analysis and interpretation.
Public health and health promotion interventions can have unintended consequences, including boomerang effects and other adverse outcomes (Byrne 2011; Lorenc 2014; O'Dea 2005). A number of adverse outcomes of interventions targeting SSBs are conceivable. Interventions focused on reducing SSB intake may lead to decreased fluid intake and dehydration, in particular in settings where access to safe drinking water is limited. Insufficient hydration has been documented for a number of populations and has been linked to diverse negative health outcomes (Kenney 2015). Moreover, caffeine has been shown to improve concentration among certain populations, such as shift workers (Ker 2010; Liira 2014), which suggests that a decrease in the consumption of caffeinated SSB might have the potential to decrease productivity and safety among certain occupational groups. Alcoholic beverages are a potential substitute for SSB, which has led to the concern that interventions targeting SSB may lead to increased alcohol consumption (Quirmbach 2018), while it has also been shown that consuming SSB with a high caffeine content, such as energy drinks, with alcohol may increase the urge to drink alcohol compared to drinking alcohol alone (McKetin 2014).
Furthermore, nutrition interventions targeting specific foods or beverages may lead to adverse compensatory behaviour, such as increased consumption of alternative but similarly unhealthy foods and beverages (Byrne 2011). Nutrition interventions may increase stigmatisation of overweight and obese individuals, including internalised stigma (Lorenc 2014; MacLean 2009), as well as stigmatisation of disadvantaged groups who are perceived as practising unhealthy lifestyles (Byrne 2011; O'Dea 2005). Furthermore, nutrition interventions may exacerbate body image and eating disorders, including unhealthy weight control and dieting practices, and psychosocial distress (Byrne 2011; O'Dea 2005; Ramos Salas 2015). Given the popularity of SSBs, we can assume that many people enjoy their consumption. It has therefore been suggested that limits on SSB may have the potential to decrease the quality of life of targeted populations. Finally, policy interventions in particular can have repercussions on the society and economy as a whole (Powell 2014).
Why it is important to do this review
Many global, regional and national policy initiatives call for action to reduce intake of added sugars (European Commission 2007; FAO/WHO 2014; Public Health England 2015; USDA 2015a; WHO 2013; WHO‐EURO 2014), for which SSBs are the most important source among many population groups (Drewnowski 2014). Environmental interventions show particular promise to be effective and cost‐effective at a population level (Gortmaker 2015; Roberto 2015; Swinburn 2011). A systematic synthesis of the available evidence in this field will help policy‐makers, regulators, health promotion authorities and professionals, and other relevant stakeholders to identify and implement suitable interventions in their own constituencies.
Objectives
To assess the effects of environmental interventions (excluding taxation) on the consumption of sugar‐sweetened beverages and sugar‐sweetened milk, diet‐related anthropometric measures and health outcomes, and on any reported unintended consequences or adverse outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We considered the following study types, as recommended by the Cochrane Effective Practice and Organisation of Care (EPOC) Group (EPOC 2013a), using the definitions proposed by EPOC:
Randomised controlled trials (RCTs): Experimental studies in which people are allocated to different interventions using methods that are random. This includes both individually‐randomised controlled trials, in which the randomisation occurs at the level of individuals, and cluster‐randomised controlled trials (cluster‐RCTs), in which the randomisation occurs at the level of clusters of individuals, e.g. study groups or study sites.
Non‐randomised controlled trials (NRCTs): Experimental studies in which people (individuals or clusters of individuals) are allocated to different interventions using methods that are not random.
Controlled before‐after (CBA) studies: Studies in which observations are made before and after the implementation of an intervention, both in a group that receives the intervention and in a control group that does not. Unlike in NRCTs, the allocation to the intervention and control groups is not determined by the investigators, but by nature or by other factors outside the control of the investigators.
Interrupted‐time‐series (ITS) studies: Studies that use observations at multiple time points before and after an intervention (the ‘interruption’). The design attempts to detect whether the intervention has had an effect greater than any underlying trend over time.
Repeated measures studies (RMS): An ITS study where measurements are made in the same individuals at each time point.
For the exact classification of study designs we used the algorithm provided by EPOC (see Appendix 5). We included only study designs that satisfy the following criteria specified by EPOC (EPOC 2013a):
For cluster‐RCTs, NRCTs and CBA studies: studies with at least two intervention and two control sites.
For ITS and RMS: a clearly defined point in time when the intervention occurred and at least three data points before and three data points after the intervention.
We interpreted the term ‘intervention and control site’ to apply to the level of implementation of the intervention, rather than to the level of allocation. This distinction matters for studies such as Muckelbauer 2009, which included 32 schools located in two cities, of which one city served as control. Further details are provided in the section Differences between protocol and review.
We included both studies that collected data on individual participants, and studies based on data not linked to individual participants, such as sales or transaction data.
We included randomised and non‐randomised cross‐over trials if they satisfied the criteria specified by EPOC for their respective study design.
The inclusion of evidence from non‐randomised controlled and uncontrolled study designs in systematic reviews is controversial (EPOC 2013a). While non‐randomised study designs are commonly used for the evaluation of public health interventions, cluster‐randomisation is feasible for most setting‐based interventions which are of relevance to this review. Even though NRCTs, CBA studies, ITS studies and RMSs are generally at higher risk of bias than RCTs, we decided to include these non‐randomised study designs in order to cover a broader set of study populations, interventions types, and intervention contexts.
Types of participants
Any participants, including adults, adolescents and children, regardless of their weight and health status and their country of residence.
Types of interventions
We consider interventions that are intended to reduce, or have potential effects on the consumption of SSB and sugar‐sweetened milk, or their adverse effects on health, implemented at an environmental level. Where these included behavioural (individual‐level) components as well as environmental components, this was clearly documented. We did not include stand‐alone behavioural interventions. We excluded studies on taxation, as a separate Cochrane Review on taxation to reduce the consumption of SSB is ongoing (Heise 2016). We did, however, include studies on other types of economic instruments, such as subsidies, price discounts and price increases not due to taxation.
We considered both ready‐to‐drink SSB and SSB prepared from syrups, concentrates or powder, or by adding sugar to beverages such as tea and coffee. We also included interventions that use diet beverages as a substitute for SSB, or in which the energy content of SSB is reduced by substituting caloric sweeteners with NNS through reformulation. Appendix 3 presents a list of all beverage categories included in this review and relevant definitions.
We excluded the following:
Studies conducted in laboratory or virtual settings, as the results may not be generalisable to real‐world environments.
Studies with a follow‐up period of less than 12 weeks, as the effects of environmental interventions may peter out due to habituation, which may limit their long‐term public health impact. In this review, we define the follow‐up period as the time span between the start of the intervention and the last outcome assessment.
Very small studies with fewer than 20 individuals in each of the intervention or control groups, as the results may not be generalisable.
Studies in which participants are administered SSB or alternatives to SSB as part of clinical trials on the physiological effects of SSB consumption, as these studies provide only limited evidence on the feasibility and effectiveness of public health interventions aimed at reducing SSB intake among free‐living individuals outside controlled research settings. This includes studies in which participants consume predefined amounts of beverages under supervision, or in which participants received predefined amounts of SSB for consumption at home.
Studies of interventions that combine intervention components targeting SSB consumption with intervention components targeting other dietary behaviours or physical activity, if these do not report beverage‐specific outcome measures, as it would be difficult to attribute effects to the environmental or policy intervention of interest. During the screening process we documented which studies we had excluded for this reason.
The comparison was no intervention, minimal or alternative interventions, such as behavioural intervention only.
Types of outcome measures
Based on structured feedback from our Review Advisory Group (see Appendix 2) , we identified a set of outcome measures that reflects short‐ and long‐term health and non‐health, and intended and unintended outcomes (see Text‐body table 2 below). To meet inclusion criteria, studies must report at least one primary outcome. We used the reporting of primary outcomes as an inclusion criterion, as we expected to find a large number of studies on environmental interventions potentially influencing SSB consumption levels. Including such studies regardless their reporting on SSB consumption would not have been feasible. We discuss implications of this decision in the paragraph on reporting bias in the section on Overall completeness and applicability of evidence. Definitions of direct and indirects measures of SSB intake used by included studies are shown in Table 10.
1. Direct and indirect measures of SSB intake.
| Additional table 1: Direct and indirect measures of SSB intake |
Albala 2008
|
Anand 2007
|
Baker 2016
|
Ball 2015
|
Bauhoff 2014 cohort and Bauhoff 2014 crosssectional
|
Blake 2018
|
Boelsen‐Robinson 2017
|
Bollinger 2011
|
Breeze 2018
|
Brimblecombe 2017
|
Cawley 2015
|
Cohen 2015
|
Collins 2016 SNAPandCollins 2016 WIC
|
Cornelsen 2017
|
Cradock 2011
|
Da Costa 2014
|
Ebbeling 2006
|
Ebbeling 2012
|
Elbel 2013
|
Elbel 2015a
|
Emerson 2017
|
Ermetici 2016
|
Finkelstein 2011
|
Foster 2014
|
Franckle 2018
|
French 2010
|
Harnack 2016
|
Hartigan 2017
|
Hendy 2011
|
Hernández‐Cordero 2014
|
Hobin 2017
|
Hua 2017
|
Huang 2012
|
Lichtman‐Sadot 2016
|
Minaker 2016
|
Muckelbauer 2009
|
Ng 2014a
|
Ng 2014b
|
Ni Mhurchu 2010
|
Olsho 2016
|
Øverby 2012
|
Peters 2016a
|
Schram 2015
|
Schwartz 2009
|
Schwartz 2016
|
Schwartz 2017
|
Siegel 2016a
|
Siegel 2016b
|
Simons 2015
|
Sturm 2015
|
Taillie 2015
|
Tate 2012
|
Van de Gaar 2014
|
Visscher 2010
|
Waehrer 2015
|
Whatley Blum 2008
|
OR: odds ratio; SE: standard error; SSB: sugar‐sweetened beverages
| Text‐body table 2: Primary and secondary outcomes | |
| Outcomes | Examples |
| Primary outcomes | |
| Direct and indirect measures of SSB intake | The amount of SSB consumed or purchased in ml/day/person, energy intake from SSB and total energy intake in kcal/day/person |
| Diet‐related anthropometric measures and health outcomes | Body mass index (BMI), age‐ and sex‐standardised body mass index (BMI z‐scores (zBMI)), waist circumference, waist‐to‐hip ratio, body weight change, incidence and prevalence of overweight and obesity, body composition or total body fat, incidence and prevalence of pre‐diabetes and diabetes, insulin resistance, blood lipids and blood pressure, incidence of dental caries and other indicators of oral health |
| Any reported adverse outcomes or unintended consequences | Compensatory behaviour, reduced fluid intake and dehydration, reduced intake of essential nutrients, body image changes, unhealthy dietary practices, unhealthy weight control, perceived reduction of freedom of choice and other forms of target group and stakeholder dissatisfaction, negative effects on employment or other adverse economic consequences |
| Secondary outcomes | |
| Measures of financial and economic viability | Costs, cost effectiveness, return on investment, and staff time requirements |
| Diet‐related psychosocial variables | Perceived dietary self‐efficacy, general self‐efficacy, health‐related and general quality of life |
| Target group perceptions of the intervention | Satisfaction with the intervention, satisfaction with the way the intervention was implemented, support for the continuation of the intervention |
| Consumption of beverages other than SSB | The amount of beverages other than SSB consumed or purchased in ml/day/person |
Search methods for identification of studies
We performed searches in the following databases:
-
Health:
MEDLINE
Embase (Excerpta Medica dataBASE)
CENTRAL (Cochrane Central Register of Controlled Trials)
-
Multidisciplinary:
Scopus
Google Scholar
Social Science Citation Index
Public health, health promotion and occupational health databases:
BiblioMap (EPPI‐Centre database of health promotion research)
TRoPHI (EPPI‐Centre Trials Register of Promoting Health Interventions)
-
Nutrition:
eLENA (WHO e‐Library of Evidence for Nutrition Actions)
-
Sources for grey literature:
openGrey (formerly openSIGLE)
-
Unpublished studies:
ClinicalTrials.gov
ICTRP (International Clinical Trials Registry Platform)
-
Databases with a regional focus:
LILACS
SciELO Citation Index
We used the Ovid search interface for MEDLINE, Embase and CENTRAL.
In addition, we searched the websites of key organisations in the area of health, health promotion and nutrition, including the following:
EU platform for action on diet, physical activity and health (ec.europa.eu/health/ph_determinants/life_style/nutrition/platform/database/dsp_search.cfm).
U.S. Centers for Disease Control and Prevention (www.cdc.gov/nutrition/data‐statistics/sugar‐sweetened‐beverages‐intake.html).
Rudd Center for Food Policy and Obesity (www.uconnruddcenter.org/publications).
Harvard TH Chan School of Public Health Obesity Prevention Source (www.hsph.harvard.edu/obesity‐prevention‐source).
World Obesity (www.worldobesity.org/what‐we‐do/policy‐prevention).
We handsearched reference lists of included studies and previously published reviews, and contacted the corresponding author of included studies and previously published reviews as well as the members of the Review Advisory Group to identify additional studies. We also conducted a citing studies search with Scopus, i.e. we searched for studies that have cited included studies and previously published reviews. The studies used for these forward and backward citation searches are provided in Appendix 6.
Our search strategy was based on three search sets, namely a beverage search set (including terms related to SSB and low‐calorie alternatives to SSB as well as to nutritive and non‐nutritive sweeteners); an intervention search set (including terms on intervention areas, intervention types and study designs); and an outcome search set (including terms on outcome measures). We conducted searches in English, but considered studies published in English, French, Spanish, Italian or German for inclusion. We applied no restriction based on the year or format of publication. The full search strategies are shown in Appendix 7, Appendix 8 and Appendix 9. We updated searches to 24 January 2018. We included ScieELO, Google Scholar, Open Grey and Bibliomap in our original search (conducted on 27 ‐ 28 June 2016), but not in our 2018 search update.
We conducted targeted searches to identify secondary publications reporting on eligible studies. Secondary publications included published protocols, baseline assessments reported in separate publications, follow‐up publications, publications in other languages, comments and corrections. We handsearched reference lists of eligible studies for this purpose, and conducted searches on PubMed and Google.
Data collection and analysis
Selection of studies
After removal of duplicate studies, we performed a multistage screening process to select those studies which met the inclusion criteria:
Two review authors (from PvP, JMS, JB, LKB, LMP or SP) independently assessed all titles and abstracts, removing those which were clearly not relevant. We resolved disagreement by discussion, and where necessary by consulting a third review author.
In the second step, two review authors (from PvP, JMS, JB, LKB, LMP, or SP) independently assessed all full texts selected in the first step. We resolved disagreement by discussion, and where necessary by consulting a third review author.
We used EndNote and Zotero to collect and de‐duplicate studies, and Rayyan for title and abstract screening. Rayyan is a web‐based application for facilitating citation screening for systematic reviews (Ouzzani 2016). At the full‐text screening stage we used Excel to document reasons for exclusion.
Data extraction and management
Two review authors (from PvP, JMS, JB, LKB, LMP, SP, or CH) independently extracted study characteristics and study data to the data extraction form. The two review authors resolved inconsistencies between them by discussion, and where necessary by consulting a third review author. PvP entered the final agreed data into Review Manager 5, and JMS checked them. In case of uncertainties, they consulted a third review author.
Based on our logic model (see Appendix 4), we extracted and categorised data on the study population, intervention goals, intervention areas, level and setting, comparison, delivery agents, mode of delivery, and time frame of delivery, as well as on primary and secondary outcomes and on intervention context and implementation, including equity considerations.
A sufficiently detailed description of intervention characteristics is necessary for a meaningful interpretation of intervention outcomes. We therefore used the Template for Intervention Description and Replication (TIDieR) framework to extract relevant data (Hoffmann 2014).
The effectiveness and the potential for unintended consequences of public health interventions are often highly dependent on the broader context in which they are implemented. We therefore extracted contextual data, using the categories defined by the Context and Implementation of Complex Interventions (CICI) framework (Pfadenhauer 2017).
Large social gradients in SSB consumption have been observed (Ogden 2011). There is also evidence that the recent decreases in average SSB consumption noted in some countries, such as the USA, have mainly been driven by decreases in consumption among relatively privileged social groups (Bleich 2015). This suggests that recent attempts to curb SSB consumption may have reached disadvantaged groups to a lesser extent, a phenomenon seen with many public health and health promotion interventions (Armstrong 2011). We therefore examined whether included studies allow conclusions about different outcomes for groups with varying levels and forms of disadvantage, as recommended by the Cochrane‐Campbell Equity Working Group (Tugwell 2010). We used the PROGRESS‐Plus framework for this purpose, which distinguishes nine domains in which social disadvantage may exist: place of residence, race or ethnicity, occupation, gender, religion, education, socio‐economic status, social capital, as well as other factors of potential relevance to equity consideration, such as disability or disease (Cochrane Campbell Methods Group 2011; Evans 2003; O'Neill 2014).
On a global scale, the highest SSB consumption levels have been reported for upper‐ and lower‐middle‐income countries (Singh 2015). However, most studies eligible for inclusion were from high‐income countries. We therefore paid special attention to issues of transferability and applicability of our conclusions to low‐ and middle‐income countries, extracting, reporting and discussing contextual data concerning this issue, including data on resource needs.
We extracted both data on the number of participants allocated, and on the number of participants included in analyses, and report the latter in our ‘Summary of Findings’ tables. For repeat cross‐sectional studies, we extracted both the number of participants at baseline and at follow‐up, and report the smaller of the two figures in our ‘Summary of Findings’ tables. The total number of participants, as reported in the Abstract, in the Results and the Discussion section, is based on the figures reported in the ‘Summary of Findings’ tables. We found two studies using partially overlapping data sets (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional). To avoid double counting of participants we included only the number of participants reported for Bauhoff 2014 cohort in our calculation of the total number of participants.
We provide the full data extraction form in Appendix 10. We had piloted this form, using a selection of studies that would clearly be included to ensure that it allows accurate and reliable extraction of relevant data.
Assessment of risk of bias in included studies
Two review authors (from PvP, JMS, JB, LKB, LMP, SP, or CH) independently assessed risks of bias of included studies, with the EPOC‐adapted Cochrane 'Risk of bias' tool (EPOC 2013b; EPOC 2015; Higgins 2017a). They resolved inconsistencies by discussion, and where necessary by consulting a third review author.
The EPOC‐adapted Cochrane 'Risk of bias' tool has been validated, and is commonly used in Cochrane and non‐Cochrane reviews. It includes four criteria that are applied to all study designs, five criteria that are applied only to controlled study designs (RCTs, NRCTs, CBA studies, and controlled ITS studies), and three criteria that are applied only to ITS studies and RMSs (EPOC 2015). Text‐body table 3 below specifies these criteria, and the study designs to which they are applied.
| Text‐body table 3: Criteria for the assessment of the risk of bias of included studies | |||
| Criterion | RCTs, cluster RCTs, NRCTs and CBA studies | ITS studies and RMS without control group | Controlled ITS studies |
| Random sequence generation (selection bias) | √ | ‐ | √ |
| Allocation concealment (selection bias) | √ | ‐ | √ |
| Similarity of baseline outcome measurements (selection bias) | √ | ‐ | √ |
| Similarity of other baseline characteristics (selection and performance bias) | √ | ‐ | √ |
| Incomplete outcome data (attrition bias) | √ | √ | √ |
| Blinding (performance and detection bias) | √ | √ | √ |
| Contamination (performance bias) | √ | ‐ | √ |
| Selective reporting (reporting bias) | √ | √ | √ |
| Independence of the intervention from other changes (performance bias) | ‐ | √ | √ |
| Prespecification of the intervention effect (detection bias) | ‐ | √ | √ |
| Intervention effects on data collection (detection bias) | ‐ | √ | √ |
| Other potential sources of bias | √ | √ | √ |
For each of these criteria, one of the following assessments is given:
Low risk of bias: plausible bias unlikely to alter the results
Unclear risk of bias: plausible bias that raises some doubt about the results
High risk of bias: plausible bias that seriously weakens confidence in the results
We used Review Manager 5 to apply the EPOC‐adapted Cochrane 'Risk of bias' tool, and to document results with traffic‐light‐coded 'Risk of bias' tables (EPOC 2013b). In applying the tool we followed the relevant instructions as provided by EPOC (EPOC 2015) and the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017a), applying judgement by the content and methods experts in our review team.
For cluster‐RCTs, we addressed failure to take the correlated nature of within‐cluster data into account in the analysis within the domain ‘Other potential sources of bias’ (Higgins 2017b). For multi‐arm and cross‐over trials, we considered potential sources of bias specific to these study designs as recommended by Cochrane guidance (Higgins 2017b).
We assessed risk of bias due to lack of blinding for subjective and objective outcomes separately. We did not assess risk of bias due to incomplete outcome data separately for different outcomes, as the number of studies for which this would have been relevant was limited. We assessed risk of bias for primary outcomes only.
Conflicts of interests by study authors can introduce further sources of bias not captured by standardised assessment tools (Lundh 2017). For studies on SSB, two potential sources of bias relating to conflicts of interest have been discussed: financial or other links to the food and beverage industry (Bes‐Rastrollo 2013; Litman 2018; Mozaffarian 2017), and ‘white hat bias’ introduced by the zeal to achieve ends perceived as righteous, as well as by anti‐corporate feelings, which might be present in researchers without industry links (Cope 2009). In this review, we extracted and documented any conflicts of interest, as well as funding sources reported in primary studies. We present data on conflicts of interest and funding in the section on Included studies. We did not consider conflicts of interest and funding as a separate domain in our risk of bias assessment, but used these data to inform our judgement in the domain of selective outcome reporting, where appropriate. This includes cases in which confidentiality agreements between study authors and data providers or industry partners limited reporting, as discussed by Ball 2015, Cawley 2015 and Peters 2016a. Details are provided in the section on Characteristics of included studies. Due to the heterogeneity of included studies we did not do sensitivity analyses based on conflicts of interest or funding.
We did not do a summary risk of bias assessment on the level of studies. We took risks of bias of studies into account in our assessment of the overall certainty of the evidence. Due to the small number of studies within each intervention category, we decided not to conduct stratified or sensitivity analyses based on risks of bias.
Measures of treatment effect
We extracted all measures of treatment effect for the primary and secondary outcomes prespecified in our protocol. We extracted both adjusted and unadjusted results, but preferred to use adjusted results for our evidence synthesis. For continuous outcome measures we used the mean difference (MD) as our preferred measure of treatment effect. We included 95% confidence intervals (CIs) when these were reported by primary studies, or when they could be calculated based on data reported in primary studies. Appendix 11 provides details on included studies reporting multiple statistical models, data sources, comparisons or outcome measures.
We used SI units (i.e. the metric system) to report results, except for energy, which we report in calories. We converted values reported in primary studies where necessary. Appendix 12 provides details on conversion factors used in this review, which we derived from primary studies or the general literature.
Some studies report several alternative measures for the same group of outcomes, such as prevalence of overweight and mean BMI as diet‐related anthropometric measures, and self‐reported SSB consumption and SSB purchasing data as direct and indirect measures of SSB intake. Some studies report effect estimates for several time points. In our protocol, we did not indicate any preferences to follow in such cases. We therefore extracted and reported all available outcome data. The results presented in the abstract, the plain language summary and the main ‘Summary of findings’ table are based either on the outcome prespecified as primary by the study in question, or alternatively on the most conservative effect estimate reported (for studies which did not prespecify primary outcomes). For studies reporting data at several time points we used data for the last follow‐up assessment conducted during the intervention phase. In some cases we assessed the individual case and selected the data considered to be most valid and relevant to our primary analysis. We provide further details in Appendix 11.
Definition of minimal patient‐relevant differences
In our protocol, we did not define minimal patient‐relevant differences, i.e. thresholds for the clinical or public‐health relevance of reported effect sizes. For population‐level public health interventions, any difference from the null may be potentially relevant, in particular for low‐cost or cost‐neutral interventions. We therefore used the difference from the null as the threshold for the potential public health relevance. Accordingly, our narrative synthesis and our assessment of the certainty of evidence focuses on the existence and direction of effects, and not on the effect size. We did, however, document any cases in which reported effect sizes were small, and may arguably be of limited practical relevance. This was the case for two studies (Bollinger 2011; Visscher 2010), which we discuss in the Results section.
Unit of analysis issues
We documented when included studies used cluster designs but did not report if this was taken into account in the analysis. For studies with more than two intervention or control groups, we combined groups to create a single pair‐wise comparison. Where this was not feasible we included two or more comparisons, as specified by Cochrane guidance (Higgins 2017b).
Dealing with missing data
In cases where missing data on study characteristics or outcome measures precluded study inclusion or limited the use of a study at further stages of the review, we contacted the corresponding author. Appendix 13 provides further details on the cases in which we contacted study authors, and on the information received. For registered but unpublished trials, we contacted the corresponding investigator to request relevant data. When studies did not report outcomes based on intention‐to‐treat analyses, we considered this as a source of bias within the domain ‘Missing data’ of the EPOC‐adapted Cochrane ‘Risk of bias’ tool. We extracted both data on the total number of participants recruited, enrolled or allocated, and on the number of participants included in analyses. Participant numbers reported in the review refer to the number of participants included in analyses, unless stated otherwise.
Assessment of heterogeneity
We assessed methodological and clinical heterogeneity with tables documenting the following characteristics of the included studies:
Implementation level.
Intervention area.
Use of behavioural co‐interventions.
Setting (e.g. schools, workplaces, shops, restaurants).
Population (e.g. age group, weight and health status, baseline SSB consumption, occupational status).
Methods (outcome measures, outcome assessment).
Mode of delivery (by permanent staff of the setting or institution in which the intervention took place, or by members of the research group or staff contracted by the research team).
Type of SSB or alternative to SSB targeted by the intervention (e.g. SSB, sugar‐sweetened milk, beverages with NNS, beverages without added sweeteners).
For those studies assessing the impacts of a given intervention category (as defined by the NOURISHING framework) on comparable outcomes (e.g. measures of SSB consumption) in the same population group (e.g. individuals below or above 18 years of age), thus making pooling through meta‐analysis feasible, we assessed statistical heterogeneity graphically with forest plots by examining the extent to which confidence intervals overlap, and statistically with the I2 statistic. We considered an I2 value greater than 50% to indicate substantial statistical heterogeneity, and considered it statistically significant if the P value for the Chi2 test is less than 0.1. Statistical heterogeneity was documented but did not have direct consequences for meta‐analysis. For one intervention type and one outcome measure (effects of price increases on SSB on SSB sales) we conducted a post hoc subgroup analysis (not prespecified in our protocol) according to the level of the price increase, i.e. the intensity of the intervention. We did this in order to assess if a dose‐response gradient existed. We created forest plots and I2 calculations using Review Manager 5. We present summary data on study population characteristics, intervention implementation and context in the section on Included studies, and discuss implications in the section on Overall completeness and applicability of evidence.
Assessment of reporting biases
We did not find more than 10 studies within the same intervention category and assessing comparable outcomes in the same population group, and therefore did not use funnel plots to assess the risk of reporting bias, or perform statistical tests of asymmetry (Sterne 2017). We discuss potential reporting biases in the sections on ‘Potential biases in the review process’ and Implications for research.
Data synthesis
We synthesised results from all studies within a given intervention category (as defined by the NOURISHING framework) narratively and with ‘Summary of findings’ tables. In line with our definition of minimal patient‐relevant differences (see above) and our assessment of the certainty of evidence (see below), our narrative synthesis focuses on the existence and the direction of effects, and not on the effect size. We present one main 'Summary of findings' table (Table 1), which provides an overview of effects for the main primary outcome (direct and indirect measures of SSB intake) for all intervention types. We created an effect direction plot to present the results shown in the main ‘Summary of Findings’ table in graphical form. The effect direction plot has been developed for the visual display of non‐standardised effects across multiple outcome domains (Thomson 2013). We took the decision to include an effect direction plot after the publication of our protocol. We present additional 'Summary of findings' tables for each of the eight intervention areas, which provide data on effects for all three primary outcomes as defined in our protocol. We took the decision to restrict the main 'Summary of findings' table to direct and indirect measures of SSB intake after the publication of our protocol. We decided to restrict the main 'Summary of findings' table to direct and indirect measures of SSB intake due to the large number of intervention types, which made it impractical to present data on all intervention types and all primary outcomes in one table.
We conducted meta‐analyses in Review Manager 5 for all intervention types for which we found two or more studies using the same study designs, and reporting comparable outcome measures. The decision which studies and which outcome measures were sufficiently homogeneous to allow for meaningful meta‐analysis required judgement by the review authors, and was taken based on discussions between the content and methods experts in the review team. Because of high heterogeneity in intervention delivery, setting and study population, we used the random‐effects model. We used the results of our risk of bias assessment as input to our assessment of the certainty of evidence, but did not incorporate it otherwise into data synthesis.
Certainty of evidence
We used the GRADE system to rate the body of evidence for all primary outcomes. In GRADE, the certainty of evidence can be understood as the extent to which one can be confident that the true effect of an intervention lies on one side of a specified threshold, or within a chosen range (Hultcrantz 2017). Based on our assumption that for the interventions considered in this review even small effect sizes can be relevant when interventions are implemented at a population level, and in line with relevant GRADE guidance (Hultcrantz 2017), we defined this threshold as difference from the null. Accordingly, our assessment of the certainty of evidence refers to the existence and the direction of effects, and not to the exact effect sizes reported by individual studies. In conducting our assessment of the certainty of evidence, we followed GRADE guidance, and applied judgement by the content and methods experts in our review team. We present the results of and our reasoning behind our assessment in the 'Summary of findings' tables.
Within the GRADE approach, the certainty of evidence is assessed based on a number of factors which can decrease or increase the level of evidence. Traditionally, evidence from RCTs starts as high‐certainty evidence in GRADE, and evidence from all other study designs starts as low‐certainty.
There are four possible levels of evidence:
High‐certainty: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate‐certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low‐certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low‐certainty: Any estimate of effect is uncertain.
There are five factors that can lead to a downgrading of the level of evidence. If one of these factors is found to exist, it is classified either as serious (downgrading by one level) or as very serious (downgrading by two levels):
Risk of bias of individual studies (limitations in the design and implementation of available studies, suggesting high likelihood of bias).
Indirectness of evidence (indirect population, intervention, control, outcomes).
Unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses).
Imprecision of results (wide confidence intervals).
High probability of publication bias.
There are three factors increasing the certainty of evidence, each of which can lead to an upgrading of the level of evidence:
Large magnitude of effect (upgrading by one or two levels).
All plausible confounding would reduce a demonstrated effect or suggest a spurious effect when results show no effect (upgrading by one level).
Dose‐response gradient (upgrading by one level).
In our GRADE assessment, we considered cluster‐RCTs in which the number of randomised units was four or fewer as equivalent to NRCTs, given that randomisation may be insufficient to achieve baseline comparability of the intervention and control groups when the number of randomised units is small. This rule, which we defined post hoc, applied to two studies in our review (French 2010; Van de Gaar 2014).
One review author (PvP) conducted the GRADE assessments, and a second review author (JMS) checked them. Assessements on which the two review authors disagreed, or for which they found that a third opinion would be helpful, were discussed within the review team.
Results
Description of studies
Results of the search
The study flow diagram is shown in Figure 5, and search logs are shown in Appendix 7. We updated the searches to 24 January 2018. Through database as well as forward and backward citation searches we identified 14,488 unique records. Of these, we excluded 13,458 at title and abstract stage, leaving 1030 full‐texts to be assessed for eligibility. Overall, 58 studies, presented in 118 records (including 39 records identified through targeted searches for secondary publications), met our inclusion criteria and were included in our narrative evidence synthesis. We found 24 studies with more than one record, and two records reporting on more than one study (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Collins 2016 SNAP; Collins 2016 WIC). The section Included studies shows how records relate to studies, and details of the two records reporting on more than one study are provided in Appendix 11 and in the section on Effects of interventions.
5.

Study flow diagram.
Included studies
In this section we provide a summary overview of key characteristics of the included studies. We provide brief narrative summaries of each of the 58 included studies in the sub‐sections ‘Description of studies contributing data to this comparison’ in the section on Effects of interventions. Further details are provided in the tables of Characteristics of included studies.
Study design, sample size and follow‐up
We included 16 RCTs with individual randomisation, 6 cluster‐RCTs, 3 NRCTs, 14 CBA studies, 11 ITS studies without control group and 8 ITS studies with control group. Thirty‐seven studies collected data on individual participants, and 21 studies were based on sales data or other types of data not linked to individual participants, and did not report participant numbers. The studies reporting participant numbers included a total of 1,180,096participants, and the number of participants ranged from 93 to 1,065,562, with a median of 1032. The combined length of intervention and follow‐up ranged from three months to six years, and the median length was 10 months.
Interventions
We found studies on a large variety of intervention types. Following our protocol, we classified these according to the NOURISHING framework (see Text‐body table 1). The NOURISHING framework covers the following seven environmental intervention areas: labelling interventions, nutrition standards in public institutions, economic tools, advertisement and marketing regulation, whole food supply interventions, retail and food service interventions, and intersectoral approaches. Besides these, we introduced an eighth intervention area for interventions implemented in the home environment (see Differences between protocol and review for further details). Following our protocol, we further stratified interventions within each of the eight intervention areas by mode of delivery, setting, and population, resulting in 24 different intervention types. Text‐body table 4 provides an overview on these. A more detailed description of the interventions examined in this review is provided in the section on Effects of interventions.
| Text‐body table 4: Studies included in this review by intervention area and intervention type | ||
| Intervention area | Intervention type | Studies |
| A. Labelling interventions | A.1 Traffic light labelling | 2 ITS studies (Boelsen‐Robinson 2017; Hartigan 2017) |
| A.2 Nutritional rating score shelf‐labels in supermarkets | 1 ITS and 1 CBA study (Cawley 2015; Hobin 2017) | |
| A.3 Menu board calorie labelling in chain restaurants and cafés | 1 controlled ITS and 2 CBA studies (Bollinger 2011; Elbel 2013; Finkelstein 2011) | |
| A.4 Emoticon labelling in school cafeterias | 1 ITS study (Siegel 2016a) | |
| B. Nutrition standards in public institutions | B.1 Reduced availability of SSB in schools | 6 CBA and 1 controlled ITS study (Bauhoff 2014 cohort; Bauhoff 2014 crosssectionall; Cradock 2011; Huang 2012; Lichtman‐Sadot 2016; Schwartz 2009; Whatley Blum 2008) |
| B.2 Improved access to drinking water in schools | 2 CBA studies, 2 NRCTs and 1 cluster‐RCT (Elbel 2015a; Muckelbauer 2009; Schwartz 2016; Van de Gaar 2014; Visscher 2010) | |
| B.3 Small prizes for the selection of healthier beverages in school cafeterias | 1 RCT and 2 ITS studies (Hendy 2011; Siegel 2016b; Emerson 2017) | |
| B.4 Improved placement of healthier beverages in school cafeterias | 1 cluster‐RCT (Cohen 2015) | |
| B.5 Fruit provision in schools | 1 cluster‐RCT and 1 CBA study (Øverby 2012; Da Costa 2014) | |
| C. Economic tools | C.1 Price increases on SSB | 3 ITS studies (Blake 2018; Breeze 2018; Cornelsen 2017) |
| C.2 Financial incentives to purchase low‐calorie beverages implemented through supermarket loyalty cards | 3 RCTs (Ball 2015; Franckle 2018; Ni Mhurchu 2010) | |
| C.3 Price discounts on low‐calorie beverages in community stores | 1 cluster‐RCT (Brimblecombe 2017) | |
| C.4 Taxation of SSB | Not covered by this review | |
| D. Advertisement regulation | No studies found | ‐ |
| E. Whole food supply interventions | E.1 Voluntary food and beverage industry initiatives to improve the nutritional quality of the whole food supply | 2 controlled ITS and 1 CBA study (Ng 2014a; Ng 2014b; Taillie 2015) |
| F. Retail and food service interventions | F.1 Healthier default beverages in children’s menus in restaurants | 1 ITS study (Peters 2016a) |
| F.2 In‐store promotion of low‐calorie beverages in supermarkets | 1 cluster‐RCT (Foster 2014) | |
| F.3 Healthier vending machines in workplaces and schools | 2 cluster‐RCTs and 1 NRCT (Ermetici 2016; Hua 2017; French 2010) | |
| F.4 Urban planning restrictions on new fast‐food outlets | 1 CBA study (Sturm 2015) | |
| F.5 Restrictions to the number of stores selling SSB in remote communities | 1 ITS study (Minaker 2016) | |
| G. Action across sectors | G.1 Trade and investment liberalisation in low‐ and middle‐income countries | 2 controlled ITS studies (Baker 2016; Schram 2015) |
| G.2 Government food benefit programmes with incentives and restrictions | 3 RCTs (Collins 2016 WIC; Harnack 2016; Olsho 2016) | |
| G.3 Government food benefit programmes without incentives and restrictions | 1 RCT and 1 CBA study (Collins 2016 SNAP; Waehrer 2015) | |
| G.4 Multi‐component community campaigns focused on SSB | 1 controlled ITS study (Schwartz 2017) | |
| H. Home‐based interventions | H.1 Improved access to low‐calorie beverages in the home environment | 6 RCTs (Albala 2008; Anand 2007; Ebbeling 2006; Ebbeling 2012; Hernández‐Cordero 2014; Tate 2012) |
| H.2 Provision of active video gaming equipment to teenagers | 1 RCT (Simons 2015) | |
Participants
The studies in this review included a broad range of participants. Twelve studies included only children, seven studies included only teenagers, eight studies included children and teenagers, nine studies included only adults, and 22 studies included participants of all ages. Four studies included only individuals with overweight and obesity. Twelve studies reported the baseline prevalence of overweight and obesity among participants. Among these, baseline prevalence of overweight and obesity ranged from 23% to 100%, with a median of 39%. Seven studies reported baseline BMI among participants. Among these, mean baseline BMI ranged from 21 to 38 kg/m2, and the median baseline BMI was 30 kg/m2. Four studies included only participants with a high baseline consumption of SSB. Among the remaining studies, baseline consumption of SSB varied considerably, as reported in the tables of Characteristics of included studies.
Context and implementation
The interventions were implemented in the following settings: schools (20 studies), supermarkets and other retailing establishments (12 studies), participants’ homes (7 studies), restaurants and cafés (6 studies), and other settings (13 studies). Thirty‐eight studies were conducted in the USA, four in Australia, three in the Netherlands, two each in Canada and the UK, and one each in the following countries: Brazil, Chile, Germany, Italy, Mexico, New Zealand, Norway, Peru, and Vietnam. The mode of implementation was as follows: pilot trials by researchers with or without the co‐operation of other actors (29 studies), mandatory government regulation or government programmes (16 studies), government pilot projects (4 studies) and voluntary industry action (9 studies). Thirty‐five studies were implemented at the level of individual settings, such as schools or restaurants, and 23 interventions were implemented at a policy level, i.e. at the level of political jurisdictions such as states or municipalities. The interventions were implemented between 2001 and 2017, and the studies published between 2006 and 2018.
Outcome measures
Fifty‐seven studies report direct or indirect measures of SSB intake, using the following data sources: self‐reported SSB intake (24 studies), electronic sales data (22 studies), data on beverage production and sales provided by market research firms (eight studies), observations by trained observers (three studies), grocery and restaurant receipts collected from participants (two studies), and administrative data bases on beverage deliveries to schools (one study). Eight studies report anthropometric measures which could be included in the analyses reported in this review, including mean BMI (six studies), prevalence of overweight and obesity (two studies), and body weight (two studies). Seven studies report effect estimates for anthropometric measures which we did not include in the analyses reported in this review, as the respective interventions were not focused on beverages, but included, among others, intervention components on nutrition in general and physical activity (Anand 2007; Bauhoff 2014 crosssectional; Bauhoff 2014 cohort; Hendy 2011; Ermetici 2016; Sturm 2015; Simons 2015). We did not include these effect estimates, as they may have been confounded by the non‐beverage‐specific intervention components.
Funding and conflicts of interest
We document funding sources and conflicts of interest reported by primary studies in the Characteristics of included studies tables. Fifty‐four of 58 studies report their source of funding, including public sources (42 studies), philanthropic/not‐for‐profit private sources (23 studies), and industry/private for‐profit sources (4 studies). Forty‐five of 58 studies include in their published reports statements on conflicts of interest. Twenty‐seven studies report that study authors had no conflicts of interests to declare. In 18 studies, data were provided by private for‐profit companies or public administrative bodies implementing the intervention. Seven studies were co‐authored by employees of the private companies or administrative bodies implementing the intervention, and in five studies funding or in‐kind contributions were provided by private companies with a commercial interest in the outcome of the study.
Excluded studies
Of the 14,488 unique records identified in the searches, we excluded 13,458 records at the title and abstract screening stage, without documenting reasons for exclusion. At this stage, we excluded only studies that were obviously irrelevant for this review. We excluded 951 studies at the full‐text screening stage, documenting reasons for exclusion. We excluded most studies for multiple reasons. Based on the first reason that led to exclusion, these included:
372 studies with ineligible study designs;
146 studies not reporting any of our predefined primary outcomes;
17 studies not meeting the predefined minimum sample size;
55 studies not meeting the predefined minimum combined length of intervention and follow‐up;
6 studies not implemented in real‐world settings;
309 studies without a direct, clearly‐defined environmental intervention component;
21 studies in which participants were administered predefined amounts of SSB or alternatives to SSB as part of clinical studies;
24 studies not meeting the EPOC criteria for included study designs;
1 study on taxation of SSB.
We report details on a subset of excluded studies in the section Characteristics of excluded studies. These include studies for which the reason for exclusion may not be obvious or unambiguous, and for which exclusion required judgement by the review authors.
Ongoing studies
We conducted trial register searches to identify ongoing studies, and found 10 studies which we judged likely to meet our eligibility criteria upon completion. These include four studies on improved availability of drinking water in schools (Kajons 2018; NCT02996422; NCT03069274; NCT03181971), two studies on improved availability of low‐calorie beverages in the home environment (NCT02877823; NCT0306927), and one study each on reduced availability of SSB and improved availability of drinking water in schools (Oi 2018), reduced availability of SSB in workplaces (NCT03431051), price increases on SSB (NCT02914821) and the removal of SSB from supermarket checkout coolers (NCT03518151). We provide details of these studies in the section Characteristics of ongoing studies. Trial register searches may, however, provide only an incomplete picture of ongoing research in the field, given that only a small proportion of all studies included in this review were registered.
Risk of bias in included studies
We assessed all included studies for their risks of bias, i.e. the risk of systematic errors in the reported effects. A low risk of bias implies a high internal validity, meaning that effects reported in a given study are likely to be close to the true effects.
We judged two studies to be at low risk of bias in all domains (Boelsen‐Robinson 2017; Cornelsen 2017), two studies to be at low risk of bias in all domains for objective outcomes (Albala 2008; Ebbeling 2006), and 11 studies to be at either low or unclear risk of bias in all domains (Blake 2018; Boelsen‐Robinson 2017; Breeze 2018; Brimblecombe 2017; Cawley 2015; Cohen 2015; Cornelsen 2017; Foster 2014; Minaker 2016; Ni Mhurchu 2010; Siegel 2016a). We judged all remaining studies to be at high risk of bias in at least one domain. Figure 6 and Figure 7 provide an overview of the risks of bias in included studies. Further details are provided in the following sections, as well as in the 'Risk of bias' tables in the section Characteristics of included studies.
6.
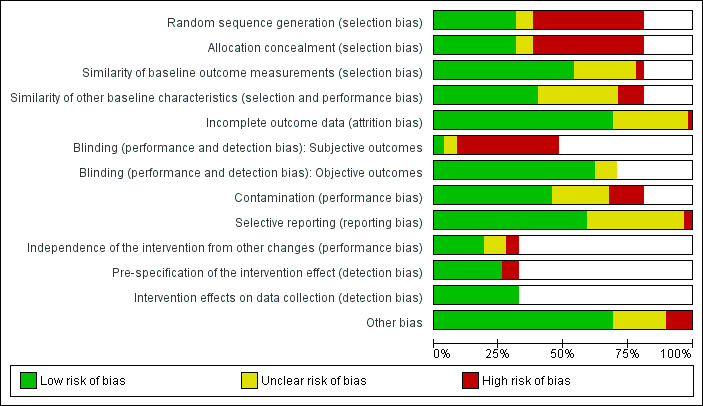
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
7.
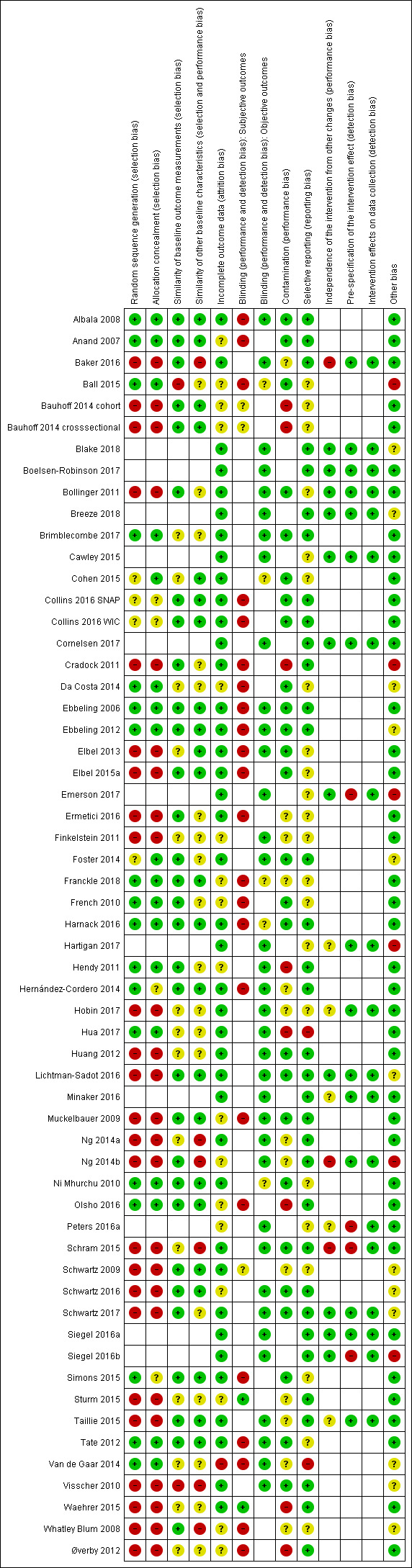
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation sequence generation and allocation sequence concealment (selection bias)
Selection bias is minimised if an allocation sequence is generated with a truly random process (allocation sequence generation), and if the forthcoming allocation is effectively concealed from those involved in enrolment into the trial (allocation sequence concealment). Following Cochrane guidance, we classified all CBA studies and all NRCTs as being at high risk of bias in both domains. For the 22 RCTs included in our review, risks of bias in the two domains varied across studies, as discussed in the following two paragraphs. We discuss random sequence generation in the first paragraph, and allocation sequence concealment in the following one.
Of the 22 RCTs included in our review, 18 report using methods for allocation sequence generation which are considered truly random, and which we classified as low risk (EPOC 2013b): 12 studies describe the use of a random‐number generator (Albala 2008; Ball 2015; Ebbeling 2006; Ebbeling 2012; Franckle 2018; Harnack 2016; Hernández‐Cordero 2014; Hua 2017; Ni Mhurchu 2010; Olsho 2016; Simons 2015; Tate 2012); three studies report using the flip of a coin (Da Costa 2014; French 2010; Van de Gaar 2014); one study reports allocating assignments by choosing units contained in separate opaque envelopes (Brimblecombe 2017), one study reports using a central, automated randomisation service (Anand 2007), and one study reports using random‐number tables from a statistics textbook (Hendy 2011). Four RCTs did not report details on allocation sequence generation, and were classified as being at unclear risk of bias (Cohen 2015; Collins 2016 SNAP; Collins 2016 WIC; Foster 2014).
Eighteen out of 22 RCTs in this review reported methods for allocation sequence concealment which we classified as low risk (EPOC 2013b), including the following: six RCTs in which allocation was by institution and was performed on all units at the start of the study (Cohen 2015; Da Costa 2014; Foster 2014; French 2010; Hua 2017; Van de Gaar 2014); three RCTs which used a centralised randomisation scheme (Anand 2007; Ball 2015; Ebbeling 2012); one RCT which used sealed opaque envelopes (Brimblecombe 2017); and eight RCTs which reported some other form of concealment (Albala 2008; Ebbeling 2006; Franckle 2018; Harnack 2016; Hendy 2011; Ni Mhurchu 2010; Olsho 2016; Tate 2012). Four RCTs did not report details on allocation sequence concealment, and were classified as being at unclear risk of bias (Collins 2016 SNAP; Collins 2016 WIC; Hernández‐Cordero 2014; Simons 2015).
Baseline similarity of outcome measures and other participant and provider characteristics (selection bias)
In RCTs, randomisation of a sufficiently large number of participants generally ensures that the intervention and control groups are comparable at baseline. In non‐randomised study designs, as well as in RCTs with small sample sizes or imperfect randomisation procedures, relevant baseline differences between the intervention and control groups may exist. In the EPOC‐adapted Cochrane ‘Risk of bias’ tool, similarity of baseline outcome measures and similarity of other participant and provider characteristics are assessed separately. We discuss the two domains in the following two paragraphs.
Baseline outcome measures were assessed in all 47 included studies which used controlled designs. Based on the data provided by the studies’ published reports, we judged the risk of bias in this domain to be low for 31 studies, unclear for 14 studies, and high for two studies (see Figure 7).
Most studies assessed and reported some other baseline characteristics of participants and providers, most commonly demographic and socio‐economic measures. Most studies adjusted for observed baseline differences in their statistical analyses. We judged some allocation procedures used in non‐randomised studies to be likely to produce unobserved baseline differences between the intervention and control groups. This included three studies in which schools self‐selected into the intervention or control group (Øverby 2012; Visscher 2010; Whatley Blum 2008), and one study in which schools with a pre‐existing collaboration with the investigators served as the intervention group, while additional schools were recruited as controls (Ermetici 2016). In total, we judged the risk of bias due to differences in baseline characteristics (other than baseline outcome measures) to be low for 23 studies, unclear for 18 studies, and high for six studies (see Figure 7).
Completeness of outcome data (attrition bias)
Attrition (dropout) or exclusion of participants during the course of a study can lead to bias if participants who drop out or are excluded from the intervention group differ systematically from those who drop out or are excluded from the control group. A related problem arises in repeat cross‐sectional studies, in which participants are not followed up individually but are redrawn from the population at each time point. In such studies, bias can arise when sampling methods differ, or when other factors differentially affect representativeness of the sample in the intervention and control groups at baseline and follow‐up. The following three paragraphs discuss, respectively, studies with individual follow‐up, repeat cross‐sectional studies, and studies using electronic sales data not linked to individual participants.
Five studies with individual follow‐up reported relevant attrition, and conducted per protocol analyses. Of these, we judged seven to be at unclear risk of bias (Anand 2007; Ball 2015; Franckle 2018; Hendy 2011; Muckelbauer 2009; Olsho 2016; Whatley Blum 2008), and one to be at high risk of bias (Van de Gaar 2014). One study conducted intention‐to‐treat analyses, but reported substantial attrition (54%), with dropouts being significantly different from those staying in the study in several characteristics (Da Costa 2014). We judged this study to be at unclear risk of bias.
We judged repeat cross‐sectional studies as being at unclear risk of bias due to doubts if representativeness was consistently ensured in all study groups and for all assessments (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; French 2010; Øverby 2012; Schwartz 2016; Sturm 2015).
Two studies using electronic sales data from restaurants report that only restaurants for which complete or relatively complete data were available were included in the analyses, without specifying why data were missing from those excluded from the analysis (Finkelstein 2011; Peters 2016a). One study on the effects of industry self‐regulation used household beverage purchasing data provided by the commercial Nielsen Homescan database, and notes that these data could be linked only imperfectly to the units of analysis in the intervention and control groups, resulting in incomplete outcome data for both groups (Ng 2014b). We judged these studies to be at unclear risk of bias in this domain. We judged all remaining studies to be at low risk of bias in this domain.
Blinding (performance bias and detection bias)
In studies on environmental interventions participants and intervention personnel can generally not be blinded to the intervention they receive or deliver. However, performance bias can be minimised if participants and intervention personnel are not aware that they are part of a systematic study. Detection bias is generally of less concern for objective outcomes, and in studies using routinely‐ collected data. By contrast, behavioural co‐interventions can reinforce social desirability bias in the intervention group, and therefore increase the risk for detection bias when outcomes are subjective and self‐reported. We therefore assessed bias due to lack of blinding separately for objective and subjective outcomes. The next paragraph discusses studies reporting objective outcomes, and the subsequent paragraph discusses studies reporting subjective outcomes.
Thirty‐seven studies reported objective outcomes, for which we judged the risk of bias to be low. Objective outcomes were in most cases automatically recorded electronic sales data, or anthropometric measures recorded by trained personnel using standardised protocols. Three studies used sales data collected with supermarket loyalty cards, which may have been used selectively by participants. We judged these outcomes as objective but as being at unclear risk of bias (Ball 2015; Franckle 2018; Ni Mhurchu 2010). One study used grocery receipts collected from participants, which is described as an objective outcome measure by the study authors, and which we judged to be at unclear risk of bias due to the possibility that participants turned in grocery receipts selectively (Harnack 2016). One study, in which participants were not blinded but were not likely to be aware of their assignment to the intervention and control groups, used outcome data collected through observation by trained observers following a standardised protocol. The study does not report if observers were blinded. We classified this outcome as objective, and at unclear risk of bias due to lack of blinding (Cohen 2015).
Twenty‐three studies reported subjective, self‐reported outcomes, for which we judged the risk of bias to be high. Five studies used subjective but routinely‐collected data, which we judged to be at low (Sturm 2015; Waehrer 2015) or at unclear risk of bias (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Schwartz 2009).
Protection against contamination (performance bias)
Contamination occurs when the control group partially or fully receives the intervention intended for the intervention group, or alternative interventions with similar effects. In studies on environmental interventions, the control group may be partially exposed to the intervention due to geographical proximity, or other reasons specific to the intervention in question.
We classified the risk of bias due to contamination as unclear in 13 studies. In one of these studies, study authors note that participants in the Iintervention and control groups interacted, and that the general nutrition counselling received by the control group may have motivated control participants to change their beverage intake (Hernández‐Cordero 2014). One study on reduced availability of SSB in schools notes that availability of SSB decreased considerably in control schools too, possibly due to several state‐wide policies implemented at the same time but independent of the intervention (Whatley Blum 2008). In one study on the effects of changes in school nutrition policies, four out of six included schools had the same food service director (Schwartz 2009). One study included school and community components, and we judged contamination to be possible in the case of the community components (Van de Gaar 2014). One study on menu‐board calorie labelling used geographically adjacent regions as intervention and control sites, and noted a significant decrease in average drink calories per transaction in both intervention and control groups (Finkelstein 2011). In one study on vending machine redesign with a behavioural co‐intervention, study authors explicitly state that contamination was likely due to geographical proximity of intervention and control schools (Ermetici 2016). In one study on trade and investment liberalisation in Bolivia, which used Peru as control country, study authors note that after the intervention was implemented SSB exports from Bolivia to Peru increased, and hypothesised that the intervention might have had regional effects which spilled over to the control country (Baker 2016). In two studies on industry self‐regulation, we judged contamination to be likely due to intervention characteristics (Ng 2014a; Ng 2014b). In one study on urban planning restrictions on new fast‐food restaurants which used geographically adjacent parts of one city and county as intervention and control sites, we judged contamination to be likely due to the potential mobility of residents (Sturm 2015). In three supermarket‐based studies we judged the risk of bias due to contamination as unclear as customers in the intervention and control group may have interacted (Franckle 2018), the same customers may have visted intervention and control supermarkets (Hobin 2017), and some control supermarkets may have implemented part of the intervention (Taillie 2015).
We judged eight studies to be at high risk of bias due to contamination. These include one study on reduced availability of SSB in schools where the intervention and control groups were overlapping, and substantial parts of the control group may have received similar interventions (Cradock 2011). Two further studies on reduced availability of SSB in schools note that parts of the control group were exposed to a similar intervention, and that baseline collection partly took place after the intervention had begun, and that this might have biased results towards null (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional). In one study on vending machine redesign which included labelling and point‐of‐purchase promotions, vending machines assigned to the intervention and control groups were located on the same university campus, and were therefore possibly frequented by the same customers, making contamination likely (Hua 2017). One study on changes to a government food benefit programme notes that parts of the control group were likely to have received the intervention, and that this might have biased results towards the null (Waehrer 2015). One study on fruit provision schemes in schools notes that some control schools implemented similar schemes during the study period (Øverby 2012). One study on food benefits with incentives randomised participants individually, but included intervention components implemented at the community level (Olsho 2016). In one study on small prizes for the selection of healthier beverages in school cafeterias children in the intervention and control groups were interacting, and favourable changes were observed in both groups (Hendy 2011). We rated all remaining studies to be at low risk of bias in this domain.
Selective outcome reporting (reporting bias)
Selective outcome reporting occurs when not all outcomes which were assessed in a study are reported in publications. Following Cochrane guidance (EPOC 2013b), we classified studies as being at low risk of bias when all outcomes mentioned in the Methods section were reported, and when we did not identify further reasons for suspecting selective outcome reporting. This was the case for 34 studies. By contrast, we classified 22 studies as being at unclear risk of bias, and two studies as being at high risk of bias in this domain (Hua 2017; Van de Gaar 2014). We provide details on these in the 'Risk of bias' tables in the section on Characteristics of included studies.
Independence of the intervention from other changes (performance bias)
In ITS studies performance bias due to confounding can arise when changes unrelated to the intervention occur during the study period and influence outcomes. Underlying temporal trends (secular changes) can be taken into account in the analysis of ITS studies, but discrete events or trends setting in during the study period can bias the effect estimates, even if appropriate analyses were performed. We judged five ITS studies to be at unclear risk of bias ( Hartigan 2017; Hobin 2017; Minaker 2016; Peters 2016a; Taillie 2015), and three ITS studies to be at high risk of bias for this domain (Baker 2016; Ng 2014b; Schram 2015). We judged all remaining ITS studies to be at low risk of bias for this domain.
Prespecification of the shape of the intervention effect (detection bias)
Detection bias can arise in ITS studies when the shape of the intervention effect is not prespecified, and when the point of analysis is not the point of intervention. We judged four ITS studies to be at high risk of bias (Emerson 2017; Peters 2016a; Schram 2015; Siegel 2016b), and all remaining ITS studies to be at low risk of bias for this domain.
Intervention effects on data collection (detection bias)
In ITS studies detection bias can arise when the intervention influences data collection. We found no evidence that this was the case in any of the included ITS studies, and judged them to be at low risk of bias for this domain.
Other potential sources of bias
In 13 studies with a control group we identified additional sources for risks of bias. These include four studies which used clusters as units of allocation, but do not report if this was taken into account in their analyses (Da Costa 2014; Van de Gaar 2014; Visscher 2010; Whatley Blum 2008). Two studies note that the data sources used may have been imperfect measures for the outcomes of interest (Lichtman‐Sadot 2016; Schwartz 2017). One study on improved availability of low‐calorie alternatives to SSB at home included multiple assessments and various measures to improve adherence and limit attrition (Ebbeling 2012). In this study, study authors note that the intensity of the intervention and the study protocol, rather than the provision of low‐calorie beverages per se, may have led to lifestyle changes which affected body weight (Ebbeling 2012). In one study data were not collected in parallel in the intervention and control groups, and data collection methods differed substantially (Cradock 2011). In one study data were self‐reported, and study authors note that participants might have misinterpreted certain survey questions (Schwartz 2009). In one study using a quasi‐experimental stepped‐wedge cross‐over design results may have been biased by underlying temporal trends (Schwartz 2016).One study notes that implementation fidelity was low for the beverage‐specific intervention components (Foster 2014). One study on industry self‐regulation estimated effects on calories from beverages sold as difference between observed trends and a best‐fit counterfactual. This counterfactual assumed that the outcome measure would fall to zero within a few years, which seems to be an implausible assumption, and would bias the results towards the null (Ng 2014b). One study on financial incentives for purchasing low‐calorie beverages implemented through supermarket loyalty reports both purchasing data collected through loyalty cards and self‐reported consumption data, with large discrepancies between the two, which suggests that these outcome measure may not have been reliable proxies for actual consumption (Ball 2015).
In five ITS studies without a control group, we identified additional sources for risks of bias. We judged these studies to be at high risk of bias in this domain. In two studies reported effect sizes may have been influenced by underlying trends, which were not taken into account in the analyses (Emerson 2017; Siegel 2016b; ). In two studies compensatory SSB purchases from points of sale not covered by the study may have influenced the results (Blake 2018, Breeze 2018). In one study the statistical method is not well described, casting some doubt on its appropriateness for an ITS analysis (Hartigan 2017).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9
We present the effects of interventions separately for the eight intervention areas covered by this review, namely:
A. Labelling interventions (eight studies);
B. Nutrition standards in public institutions (18 studies);
C. Economic tools (seven studies);
D. Advertisement regulation (no studies);
E. Whole food supply interventions (three studies);
F. Retail and food service interventions (seven studies);
G. Action across sectors (eight studies);
H. Home‐based interventions (seven studies).
The ‘Summary of findings’ tables provide an overview of the effects on primary outcomes by intervention type, as well as details of our assessment of the certainty of the evidence with GRADE. An effect direction plot (Thomson 2013) displaying the direction of reported effects on direct and indirect measures of SSB intake is shown in Figure 8. Table 10, Table 11 and Table 12 present data on effects on primary outcomes for each included study. In the following sections we provide a narrative summary of the studies contributing data to each of the comparisons, and of the effects on primary and secondary outcomes.
8.
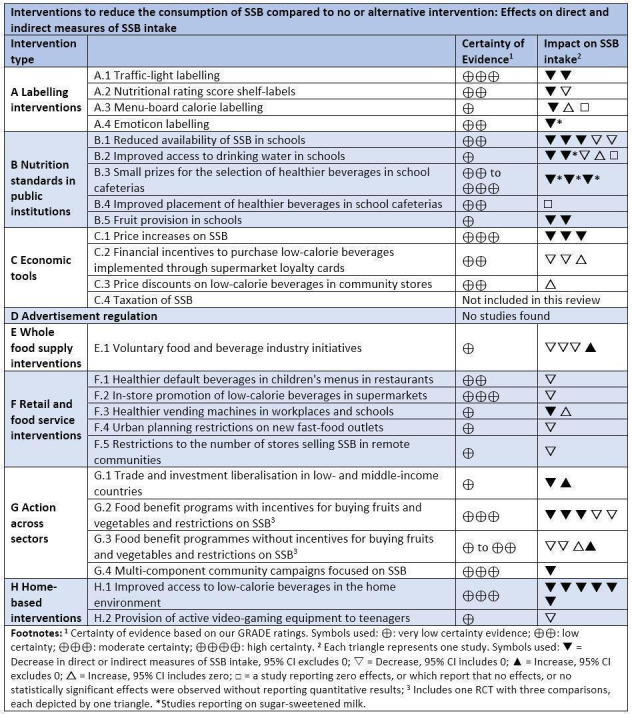
Effect direction plot showing the direction of reported effects on direct and indirect measures of SSB intake
2. Diet‐related anthropometric measures and health outcomes.
| Additional Table 2: Diet‐related anthropometric measures and health outcomes |
Ebbeling 2006:
|
Ebbeling 2012:
|
Hernández‐Cordero 2014:
|
Muckelbauer 2009:
|
Schwartz 2016:
|
Tate 2012:
|
Van de Gaar 2014:
|
BMI: body mass index
3. Adverse outcomes and unintended consequences.
| Additional Table 3: Adverse outcomes and unintended consequences |
Note: In this table, we present data on the following outcome categories:
|
Albala 2008:
|
Anand 2007:
|
Baker 2016:
|
Ball 2015:
|
Bauhoff 2014 cohort and Bauhoff 2014 crosssectional
|
Blake 2018
|
Boelsen‐Robinson 2017
|
Bollinger 2011
|
Breeze 2018
|
Brimblecombe 2017
|
Cawley 2015
|
Cohen 2015
|
Collins 2016 SNAP and Collins 2016 WIC
|
Cornelsen 2017
|
Cradock 2011
|
Da Costa 2014
|
Ebbeling 2006
|
Ebbeling 2012
|
Elbel 2013
|
Elbel 2015a
|
Emerson 2017
|
Ermetici 2016
|
Finkelstein 2011
|
Foster 2014
|
Franckle 2018
|
French 2010
|
Harnack 2016
|
Hartigan 2017
|
Hendy 2011
|
Hernández‐Cordero 2014
|
Hobin 2017
|
Hua 2017
|
Huang 2012
|
Lichtman‐Sadot 2016
|
Minaker 2016
|
Muckelbauer 2009
|
Ng 2014a
|
Ng 2014b
|
Ni Mhurchu 2010
|
Olsho 2016
|
Øverby 2012
|
Peters 2016a
|
Schram 2015
|
Schwartz 2009
|
Schwartz 2016
|
Schwartz 2017
|
Siegel 2016a
|
Siegel 2016b
|
Simons 2015
|
Sturm 2015:
|
Taillie 2015:
|
Tate 2012:
|
Van de Gaar 2014:
|
Visscher 2010:
|
Waehrer 2015:
|
Whatley Blum 2008:
|
BMI: body mass index; SE: standard error
We also assessed whether there were any differential effects for groups with varying levels and forms of disadvantage based on the PROGRESS‐Plus framework.
Overall, the included studies covered a broad and diverse range of participants from a variety of residential, ethnic, occupational, educational and socio‐economic backgrounds, as well as participants of all ages, and participants with normal weight, overweight and obesity. Thirteen studies were focused on socially‐disadvantaged participants, and nine studies report subgroup analyses by indicators of social disadvantage. We present details in Appendix 14. Overall, no clear pattern of differences in effectiveness by social disadvantage emerges from the evidence in this review. There is, however, some evidence that interventions can be effective in groups exposed to varying degrees and forms of social disadvantage. In addition, eight studies report subgroup analyses by sex or gender, four studies included only or predominately female participants, and two studies included mainly male participants. We present details in Appendix 14. Overall, the studies in this review do not provide evidence for a consistent moderation of intervention effects by gender.
A. Labelling interventions
We found eight eligible studies on labelling interventions, including:
A.1 Traffic‐light labelling (Boelsen‐Robinson 2017; Hartigan 2017);
A.2 Nutritional rating score shelf labels in supermarkets (Cawley 2015; Hobin 2017);
A.3 Menu‐board calorie labelling in chain restaurants and cafés (Bollinger 2011; Elbel 2013; Finkelstein 2011);
A.4 Emoticon labelling in school cafeterias (Siegel 2016a).
A.1 Traffic‐light labelling
Description of studies contributing data to this comparison
We included two ITS studies on traffic‐light labelling of beverages, in which beverages were labelled as red, yellow and green according to their nutritional value (Boelsen‐Robinson 2017; Hartigan 2017). In both studies a number of co‐interventions were performed.
In Boelsen‐Robinson 2017, traffic‐light labelling was applied and the share of green‐labelled beverages among all beverages offered was increased. The intervention was implemented in all 37 vending machines located on the premises of one large not‐for‐profit hospital in Melbourne, Australia. The analysis is based on electronic sales data collected during a 30‐month baseline period and a 12‐month intervention phase. The number of beverage items sold each month at baseline was 3774. Participants were hospital staff, patients and visitors.
In Hartigan 2017, traffic‐light labelling was applied and healthier beverages were placed at eye level in cafeteria coolers and vending machines, and educational and promotional activities including point‐of‐sale posters explaining the traffic‐light system were performed. The study was set in a large not‐for‐profit hospital in San Diego, USA, and the intervention was implemented in all locations selling beverages in that hospital. The analysis is based on electronic sales data collected during a three‐month baseline period and a 16‐month intervention phase. The average monthly number of beverage transactions in the main cafeteria was 25,000 (this number includes hot beverages, which were not labelled and not included in the analyses). Participants were hospital staff, patients and visitors.
SSB sales (two ITS studies, moderate‐certainty evidence)
Boelsen‐Robinson 2017 reports that baseline sales of red‐labelled beverages (mainly SSB) were 2343 items/months, or 62% of all beverage items sold through vending machines on hospital premises. One year after the intervention was implemented, the number of red‐labelled beverages sold decreased by −56% (95% confidence interval (CI) −67 to −45), and the volume of red‐labelled beverages sold decreased by −61% (95% CI −73 to −49) compared to a counterfactual scenario based on pre‐intervention trends adjusted for seasonal effects and autocorrelation. The total volume of red‐labelled beverage sales was 1263 l/month at baseline, and decreased by −61% (95% CI −73 to −49). The total amount of sugar in all beverages sold was 129 kg/month at baseline, and decreased by −69% (95% CI −82 to −56). For the number of red‐labelled beverage items outcome data are also shown graphically, illustrating that the steepest reduction occurred at the time point when the intervention was implemented, and that the reduction persisted throughout the follow‐up period of one year.
Hartigan 2017 reports that the share of sold beverage items labelled red (mainly SSB) decreased from 56% at baseline to 32% at the end of the data collection period, i.e. 15 months post‐intervention (P < 0.001), from which we calculated a decrease of −25 percentage points. The study does not report the absolute number of red‐labelled beverages sold at baseline or post‐intervention. The study does not report if baseline trends and seasonality were taken into account in the analyses, and a graphical representation of the data suggests that the share of red‐labelled beverages may have already been declining at baseline. Underlying trends may therefore have contributed to the observed effects.
Adverse outcomes: total revenue and sales (two ITS studies, low‐certainty evidence)
Decreasing revenue or profits from beverage sales are a potential adverse outcome of labelling interventions. Boelsen‐Robinson 2017 reports that overall vending‐machine revenue from foods and beverages decreased by −21% (95% CI −29 to −12) at 12 months post‐implementation, compared to the counterfactual, and that the reduction was similar for foods and drinks considered separately (data not shown in the study). Hartigan 2017, by contrast, reports that average total monthly sales revenue from all beverages was USD 34,624 at baseline, USD 35,390 during the 12‐month intervention period, and USD 34,955 during the four‐month post‐intervention period, and study authors conclude that revenue remained constant (no statistical analyses shown in the study).
Secondary outcomes: sales of green‐labelled beverages
Boelsen‐Robinson 2017 reports that baseline sales of green‐labelled beverages were 645 items/month, or 17% of all beverage items sold through vending machines on hospital premises. One year after the intervention was implemented, the number of green‐labelled beverages sold increased by 22% (95% CI 4 to 40) compared to the counterfactual. Hartigan 2017 reports that the share of green‐labelled beverage items sold increased from 12% at baseline to 38% at the end of the data collection period, i.e. 15 months post‐intervention (P < 0.001), from which we calculated an increase of 26 percentage points. The caveats about the influence of underlying trends noted for the share of red‐labelled beverages reported by Hartigan 2017 also apply to this outcome.
A.2 Nutritional rating score shelf labels in supermarkets
Description of studies contributing data to this comparison
We included one ITS study (Cawley 2015) and one CBA study (Hobin 2017) on nutritional rating score shelf labels in supermarkets. Both studies examined the effects of the Guiding Stars nutrition rating system. In this system, a rating score ranging from zero to three stars is calculated for foods and beverages by an algorithm based on nutrient density per 100 kcal. Vitamins, minerals, omega‐3 fatty acids, fibre, and whole grains increase the score, and trans‐ and saturated fats as well as added sodium and sugar decrease the score. The rating is displayed on the shelf tag next to the price. Products which do not contain nutrients, such as bottled water, are not rated and not labelled. In addition, in both studies a limited number of educational activities were performed, including distribution of brochures and display of aisle signage.
In Cawley 2015, the Guiding Stars system was applied and all products, including those receiving zero stars, were labelled. The intervention was implemented in 168 supermarkets belonging to one supermarket chain in North‐Eastern USA. The analysis is based on electronic sales data collected during a 19‐month baseline period and a 16‐month intervention phase. The number of food and beverage items sold each week was approximately 12 million (data shown graphically only). Participants were supermarket customers.
In Hobin 2017, the Guiding Stars system was applied, and products receiving one to three stars (but not those receiving zero stars) were labelled. The study is based on data from 126 supermarkets belonging to three supermarket chains owned by one company, all located in Ontario, Canada. The intervention was implemented in 44 supermarkets belonging to one of the three supermarket chains. In the remaining 82 supermarkets, which served as controls, implementation was delayed until after the end of the study. The analysis is based on electronic sales data collected during a 2½‐month baseline period and a seven‐month intervention phase. The mean number of transactions (defined as the number of customers purchasing any food or beverage) per store and day was 2763. Participants were supermarket customers.
SSB sales (one ITS and one CBA study, low‐certainty evidence)
Cawley 2015 reports that the number of units of SSB with zero stars sold decreased by −27.3% at 16 months. For SSBs with any number of stars, results were almost identical (−27.4%), reflecting the fact that almost all SSBs receive zero stars in the Guiding Stars system (Cawley 2015; Guiding Stars 2018). The study does not report the absolute number of units of SSB sold at baseline or post‐intervention, and does not provide a confidence interval or P value for the estimate of the effect on SSB sales. However, it reports that in the average food and beverage category, the number of less nutritious, zero‐star‐rated items sold each week decreased by −3183 units/week (95% CI −5454 to −913; P = 0.006) or −8.31% (95% CI −13.50 to −2.80; P = 0.004), and that SSBs were among the food and beverage categories for which the decrease was most pronounced. Estimates are based on the comparison with a counterfactual, which took baseline trends and seasonality into account.
Hobin 2017 reports that the share of beverages with zero stars (including most SSBs) decreased (coefficient estimate: −0.026, standard error (SE): 0.006; P < 0.001) at seven months compared to the control supermarkets which did not implement the intervention. The study does not report the absolute numbers of beverages sold at baseline or follow‐up.
Adverse outcomes: total sales and revenue, compensatory consumption (one ITS and one CBA study, low‐certainty evidence)
Cawley 2015 reports that total sales (i.e. of both nutritious and less nutritious items) in the average food and beverage category decreased by −3637 units/week (95% CI −5961 to −1313; P = 0.002), or by −4.9% (95% CI −9.7 to 0.07; P = 0.05) at 16 months. Different statistical models were used to estimate absolute and relative changes, which explains why effects reached statistical significance for absolute but not for relative changes. Hobin 2017 reports that at seven months total revenue increased (coefficient estimate: 0.042, SE: 0.013, P < 0.01), as did the number of products sold per transaction (coefficient estimate 0.016, SE: 0.005, P < 0.01) and the price per transaction (coefficient estimate: 0.013, SE: 0.002, P < 0.001).
Compensatory consumption, whereby reduced consumption of one type of unhealthy food or beverage is accompanied by a compensatory increase in consumption of other types of unhealthy foods and beverages, is a potential adverse outcome of nutrition interventions. Cawley 2015 reports that in the average food and beverage category, the number of zero‐star‐rated items sold each week decreased by −3183 units/week (95% CI −5454 to −913; P = 0.006) or −8.31% (95% CI −13.50 to −2.80; P = 0.004). Hobin 2017 reports that the average star rating of all products sold increased from 1.22 to 1.24 on a three‐star scale, with higher numbers indicating improved healthfulness (P < 0.001, coefficient estimate 0.014, SE 0.003). Thus none of the studies provides evidence for compensatory purchases of other unhealthy foods and beverages.
Secondary outcomes: sales of alternatives to SSB and target group perceptions
Hobin 2017 reports that the share of beverages with three stars (indicating healthfulness) decreased (coefficient estimate: −0.038, SE: 0.039, P > 0.05) at seven months. Regarding target group perceptions, Hobin 2017 reports results from a customer survey showing that "6 months after implementation, a modest proportion of consumers were aware of, understood, and trusted the Guiding Stars system in intervention supermarkets with the labelling intervention, and a small but significant proportion of consumers reported using this system when making decisions about food purchases. (…) [C]onsumers strongly supported the use of nutrition labelling systems in supermarkets."
A3. Menu‐board calorie labelling in chain restaurants and cafés
Description of studies contributing data to this comparison
We included one controlled ITS study (Bollinger 2011) and two CBA studies (Elbel 2013; Finkelstein 2011) on menu‐board calorie labelling in chain restaurants and cafés. All three studies examine the effect of mandatory calorie‐labelling laws passed by states and cities in the USA, which required chain restaurants and cafés to post the number of calories contained in foods and beverages on menu boards.
Bollinger 2011 is based on electronic transaction data from all 222 Starbucks cafés located in New York City, where calorie labelling became mandatory in 2008, as well as on data from all 94 Starbucks cafés located in Boston and Philadelphia, which served as controls. Data were collected during a three‐month baseline period and an 11‐month intervention phase, and cover more than 100 million transactions. Participants were customers of Starbucks.
Elbel 2013 used receipts collected from customers of 23 McDonald’s and Burger King restaurants in Philadelphia, where calorie labelling became mandatory in 2010, and Baltimore, which served as control. At baseline, receipts were collected from 599 customers in Philadelphia, and from 433 customers in Baltimore. Four months after the intervention was implemented receipts from 570 customer in Philadelphia and from 481 customers in Baltimore were collected. Participants were adults aged 18 to 64 years who were recruited by the researchers while entering participating restaurants. The sample was predominantly black and lower‐educated.
Finkelstein 2011 is based on electronic transaction data from seven restaurants belonging to Taco Time, a Mexican‐style quick‐service restaurant chain, located in King County, Washington State, USA, where calorie labelling became mandatory in 2009, as well as on data from seven restaurants belonging to the same chain located in adjacent counties, which served as controls. Data were collected during a 12‐month baseline period and a 12‐month intervention phase. The average number of monthly transactions per restaurant was 11,592 in King County and 10,194 in control counties. Participants were Taco Time customers.
Beverage calories per transaction (one ITS and two CBA studies, very low‐certainty evidence)
Bollinger 2011 reports that beverage calories per transaction decreased by −0.3% (P < 0.01) at 11 months, and notes that this effect, while statistically significant, may lack practical relevance due to its small size. Elbel 2013 reports that the intervention had no effect on beverage calories per transaction at four months (data not shown in the study). Unadjusted data from Elbel 2013 indicate that beverage calories per transaction increased from 203 kcal at baseline to 308 kcal at four months in the intervention group, and from 306 kcal at baseline to 368 kcal at four months in the control group (these data are reported in Taksler 2014, a secondary publication to Elbel 2013). Finkelstein 2011 reports that beverage calories per transaction increased by 0.9 kcal (95% CI −1.4 to 3.2) at six months and by 1.7 kcal (95% CI −1.5 to 4.9) at 12 months. All three studies conclude that menu‐board calorie labelling has no relevant effects on beverage calories per transaction.
Adverse outcomes: total revenue, frequency of fast‐food restaurant visits, compensatory consumption, and stakeholder discontent (one ITS and two CBA studies, very low‐certainty evidence)
Bollinger 2011 reports that there was no statistically significant effect on total store revenue (regression coefficient: 0.005, SE: 0.004, P > 0.05). Elbel 2013 notes that the self‐reported number of fast‐food restaurant visits increased by 0.9 visits/week (P = 0.07).
None of the three studies provides evidence for compensatory consumption. Bollinger 2011 reports that calories from foods and beverages per transaction decreased from 247 kcal to 232 kcal, or by −6.0% (95% CI −6.2 to −5.8). Elbel 2013 reports that calories from foods and beverages per transaction decreased by −3.8 kcal/transaction (95% CI −125 to 119). Finkelstein 2011 reports that calories from foods and beverages per transaction increased by 18.5 kcal/transaction (95% CI −11 to 48) at 12 months.
Regarding stakeholder discontent, Bollinger 2011 reports that "[t]he NYC Board of Health first voted in the law in 2006, but legal challenges from the New York State Restaurant Association delayed its implementation until mid‐2008."
Secondary outcomes: implementation costs and target group perceptions
Bollinger 2011 reports that the cost of compliance with the intervention was approximately USD 2000 per store. Elbel 2013 reports that the share of residents who reported noticing calorie information increased by 33 percentage points (P < 0.001).
A4. Emoticon labelling in school cafeterias
Description of studies contributing data to this comparison
We included one ITS study on emoticons on healthier beverages in school cafeterias (Siegel 2016a). In this study, green, smiley‐faced emoticons were placed on plain white fat‐free milk in school cafeterias, to encourage students to choose this type of milk rather than sugar‐sweetened, chocolate‐flavoured milk, which was also available. In a second study phase, small prizes were given to students selecting healthier foods and beverages. Data from this second study phase are not included in this review, as the follow‐up period did not meet our inclusion criteria. The study is based on electronic cafeteria sales data from two elementary schools in Cincinnati, USA. Data were collected during a two‐month baseline period and a four‐month intervention phase. Between 186 and 278 students used the cafeterias each day. Most students were African‐American and received free school meals, i.e. were from relatively low‐income families.
Sugar‐sweetened milk selection (one ITS study, low‐certainty evidence)
Based on data provided by the corresponding author of Siegel 2016a, we calculated that the share of students selecting sugar‐sweetened, chocolate‐flavoured milk decreased by −15.7 percentage points (95% CI −27.4 to −4.0; P = 0,0113; t‐value: −2625, level change) without a significant trend change following the introduction of the intervention. We provide further details on the statistical model used for our analysis in Appendix 11.
Adverse outcomes: effects on total milk selection (one ITS study, very low‐certainty evidence)
Siegel 2016a reports that there was no statistically significant effect on the share of students selecting any milk (white or chocolate), which was 93% at baseline and 95% during the four‐month intervention phase (no statistical analyses shown).
Secondary outcomes: implementation costs and share of students selecting white milk
Siegel 2016a reports that the intervention "was low cost and easy to implement." Moreover, it reports that the share of students selecting plain white fat‐free milk (the main alternative to sugar‐sweetened milk offered in the cafeterias) was 7% at baseline, and increased to 18% during the four‐month intervention phase (P < 0.001).
B. Nutrition standards in public institutions
We found 18 studies on nutrition standards in public institutions, including studies on:
B.1 Reduced availability of SSB in schools (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Cradock 2011; Huang 2012; Lichtman‐Sadot 2016; Schwartz 2009; Whatley Blum 2008);
B.2 Improved access to drinking water in schools (Elbel 2015a; Muckelbauer 2009; Schwartz 2016; Van de Gaar 2014; Visscher 2010);
B.3 Small prizes for the selection of healthier beverages in school cafeterias (Hendy 2011; Emerson 2017; Siegel 2016b);
B.4 Improved placement of healthier beverages in school cafeterias (Cohen 2015);
B.5 Fruit provision in schools (Øverby 2012; Da Costa 2014).
B.1 Reduced availability of SSB in schools
Description of studies contributing data to this comparison
We included seven studies on interventions limiting the availability of SSB in schools, including six CBA studies (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Cradock 2011; Huang 2012; Schwartz 2009; Whatley Blum 2008) and one controlled ITS study (Lichtman‐Sadot 2016).
The studies examine interventions implemented in the USA between 2004 and 2009. Five studies examine the effects of mandatory government regulation (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Cradock 2011; Huang 2012; Lichtman‐Sadot 2016), one study examines the effects of a government pilot project (Schwartz 2009), and one study the effects of a pilot project initiated by the investigators (Whatley Blum 2008). Five studies assess effects on overall SSB intake by students (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Cradock 2011; Schwartz 2009; Whatley Blum 2008), and three studies assess effects on compensatory SSB purchases or intake outside school (Huang 2012; Lichtman‐Sadot 2016; Schwartz 2009).
Bauhoff 2014 cohort and Bauhoff 2014 crosssectional are CBA studies which examine the effects of a school nutrition policy implemented in the Los Angeles Unified School District in 2004 in elementary, middle and high schools on SSB intake by high‐school students. They use SSB intake data from the routinely‐conducted California Healthy Kids Survey collected in spring 2004, shortly after the policy took effect, as well as in spring 2006, two years post‐intervention. They compare data for Los Angeles with data for a synthetic control group of matched and re‐weighted school districts in the rest of California, which were exposed to less stringent state‐wide school nutrition standards which applied to elementary and middle schools, but not to high schools. In Bauhoff 2014 cohort, the number of survey participants contributing data at baseline was 1810 in the intervention group and 13,386 in the control group. At follow‐up it was 701 and 17,000 respectively. In Bauhoff 2014 crosssectional the number of survey participants contributing data at baseline was 1451 in the intervention group and 11,720 in the control group, and at follow‐up 701 and 11,851 respectively. The sample was ethnically diverse (approximately 65% were Hispanic, 10% white, 5% black) and 60% of students received free school lunches, i.e. were from relatively low‐income families.
Cradock 2011 is a CBA study which examines the effects of school nutrition standards mandated by the Boston School Committee, which took effect in public schools in Boston in fall 2004. It compares SSB intake in Boston with national trends, using data for 2004 (pre‐intervention) and 2006 (two‐year post‐intervention) from the Boston Youth Survey and the National Health and Nutrition Examination Survey (NHANES), two routinely‐conducted nutrition surveys. The number of survey participants contributing data at baseline was 895 in the intervention group and 1196 in the control group; at follow‐up it was 1138 and 1233 respectively. In the intervention group 37% of students were black, 39% Hispanic, and 13% white, and 74% received free or reduced‐price school meals.
Schwartz 2009 is a CBA study which examines the effects of a government pilot project conducted by the Connecticut State Department of Education, for which three middle schools in Connecticut volunteered to implement nutrition guidelines limiting the availability of SSB. The investigators identified three matched control schools, and collected SSB intake data from students by asking teachers to distribute questionnaires to their students before and one year after the guidelines were implemented. The number of participants was 501 at baseline and 495 at follow‐up. A broad range of ethnic and socio‐economic groups was represented among the participants.
Whatley Blum 2008 is a NRCT which examines the effects of a pilot trial initiated by the study authors. In this study, seven high schools in villages and small towns in Maine, USA, volunteered either as intervention schools, which reduced the availability of SSB on school premises, or as control schools which did not change beverage offerings. Data from 456 students were included in analyses. Data were collected before and one year after the intervention by administering a food frequency questionnaire to a convenience sample of students, who were recruited through posters, public announcements and presentations in selected classes. Ninety‐eight per cent of participants were white.
Huang 2012 is a CBA study which examines the effects of a state‐wide ban on SSB and diet beverages in public schools, implemented in July 2006 in Connecticut on compensatory SSB purchases outside school by households with school‐aged children in Hartford, Connecticut. It is based on commercially available household‐level purchasing data provided by the market research firm Nielsen, and uses a triple‐difference approach by comparing purchasing levels before and after the intervention, by households with and without school‐aged children, and by households living in Hartford and households living in Atlanta, Houston, Miami and Kansas City, which did not implement restrictions on SSB in schools during the study period. Data for February to May 2006 are used as pre‐intervention data, and data for February to May 2007 as post‐intervention data. The number of households contributing data was 81 in the intervention group (households with school‐aged children living in Hartford) and 3104 in the control group (all other households) at baseline and at follow‐up.
Lichtman‐Sadot 2016 is a controlled ITS study which examines the effects of restrictions on the availability of SSB in schools implemented in 46 school districts in the USA between January 2004 and December 2009 on compensatory SSB purchases outside school by households with school‐aged children. Like Huang 2012, it is based on household‐level purchasing data provided by Nielsen, and uses a triple‐difference approach comparing purchasing trends before and after the intervention, by households with and without school‐aged children, and by households living in schools districts which implemented restrictions on the availability of SSB in schools during the study period and households living in school districts which did not implement new restrictions during the study period. Quarterly data were used, covering the period from 2004 to 2009. The total number of households in the sample was 10,308, including 7517 household living in school districts which implemented new restrictions on the availability of SSB in schools during the study period.
Total SSB intake (five CBA studies, low‐certainty evidence)
Cradock 2011 reports that total SSB intake decreased by −99 ml/day (95% CI −173 to −26) at two years. Whatley Blum 2008 reports that total SSB intake decreased by −14 ml/day (95% CI −69 to 41) at nine months. Bauhoff 2014 cohort and Bauhoff 2014 crosssectional report effects on the share of female and male students consuming more than 0, 1, 2, 3 or 4 servings of SSB a day (see Analysis 1.1 and Analysis 1.2). For the number of students consuming any SSB we were able to pool results for male and female students, and calculated that the share of students consuming any SSB decreased by −4 percentage points (95% CI −10 to 2) in the cohort analysis (Bauhoff 2014 cohort), and by −10 percentage points (95% CI −17 to −3) at two years in the repeat cross‐sectional analysis (Bauhoff 2014 crosssectional). The study author concludes that SSB intake decreased significantly at the upper end of the SSB intake distribution for female students, and at the lower end of the SSB intake distribution for male students. Schwartz 2009 reports that consumption of beverages excluded by nutrition standards (mainly SSB) in schools decreased (ß = −0.23, P < 0.05) at 12 months.
1.1. Analysis.
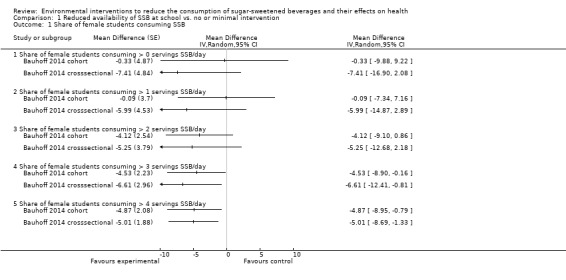
Comparison 1 Reduced availability of SSB at school vs. no or minimal intervention, Outcome 1 Share of female students consuming SSB.
1.2. Analysis.
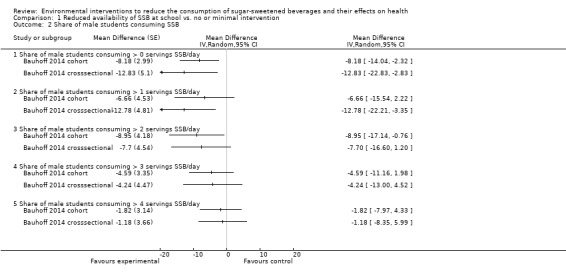
Comparison 1 Reduced availability of SSB at school vs. no or minimal intervention, Outcome 2 Share of male students consuming SSB.
Adverse outcomes: compensatory SSB purchases outside school (two CBA and one ITS study, very low‐ to low‐certainty evidence), body dissatisfaction and advertisement exposure (one CBA study each, very low‐certainty evidence)
Huang 2012 reports that SSB purchases outside school by households with school‐aged children decreased by −13 ml/day (95% CI −137 to 112) at six months. Lichtman‐Sadot 2016 reports that during a 36‐month follow‐up period SSB purchases outside school increased by 36 ml/day (95% CI 13 to 60) in households with high‐school‐aged children, decreased by −20 ml/day (95% CI −50 to 10) in households with middle‐school‐aged children, and decreased by −2 ml/day (95% CI −47 to 44) in households with elementary‐school‐aged children (see Figure 9; Analysis 1.3). Schwartz 2009 reports that consumption of beverages excluded by nutrition standards (mainly SSB) outside school decreased (ß = −0.18, P < 0.05) at 12 months.
9.
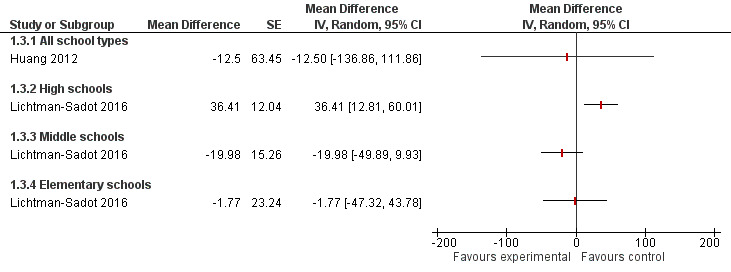
Analysis 1.3: Effects of reduced availability of SSB at school on SSB purchases outside school by households with school‐aged children [ml/day].
1.3. Analysis.
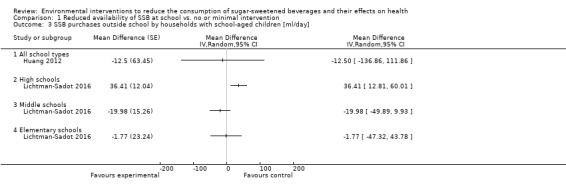
Comparison 1 Reduced availability of SSB at school vs. no or minimal intervention, Outcome 3 SSB purchases outside school by households with school‐aged children [ml/day].
Schwartz 2009 reports that there were no statistically significant effects on body dissatisfaction and dieting behaviour at 12 months (data shown narratively only in the study). Huang 2012 reports that exposure to advertisement for SSB did not increase (data shown graphically only in the study).
Secondary outcomes: consumption of alternatives to SSB, financial impact on schools, and target group perceptions
Schwartz 2009 reports that water and 100% fruit juice intake increased in schools (ß = 0.33, P < 0.05) but not outside school (data shown graphically only) at 12 months. Whatley Blum 2008 reports that diet beverage intake decreased by −16 ml/day (95% CI −50 to 19), and that fruit juice intake decreased by −60 ml/day (95% CI −115 to −5) at nine months. Whatley Blum 2008 reports that consumption of milk (including plain and sugar‐sweetened milk) decreased by −43 ml/day (95% CI −124 to 38).
Whatley Blum 2008 reports that "[b]ased on anecdotal financial data for the schools participating in the study, there appeared to be no negative financial impact on the intervention schools from reducing and/or eliminating the availability of SSB and diet soda." Regarding target group perceptions, Davee 2005 (a secondary publication of Whatley Blum 2008) reports that “anecdotal evidence showed that the responses to the change in the nutrition environment by faculty, staff, and students were mixed. (…) Comments were made about (…) the perceived lack of food and beverage choices.”
B.2 Improved access to drinking water in schools
Description of studies contributing data to this comparison
We included five studies on improved access to drinking water in schools, including two CBA studies (Elbel 2015a; Schwartz 2016), two NRCTs (Muckelbauer 2009; Visscher 2010) and one cluster‐RCT (Van de Gaar 2014).
Elbel 2015a is a CBA study examining the effects on SSB, water and milk intake of water jets, which were installed in the cafeterias of public schools in New York City as part of a government programme. Nine schools, which were scheduled to receive a water jet in November 2010, were recruited by the New York Department of Health and Mental Hygiene, and researchers identified 10 matched control schools which were not scheduled to received a water jet during the study period. Data on beverage intake were collected with a questionnaire which was distributed to students by their classroom teachers, at baseline and at three months post‐intervention. At baseline, the number of participants was 849 in the intervention group and 665 in the control group, and at follow‐up it was 800 and 585 respectively. In addition, milk‐ and water‐taking by students in the school cafeterias were observed by trained observers at baseline and at three months post‐intervention. In a subset of 12 schools additional follow‐up cafeteria observations were performed at 10 months post‐intervention. The sample was ethnically diverse (approximately 20% were African American, 40% were Hispanic and 25% white), and approximately half qualified for free or reduced‐price school meals.
Schwartz 2016 is a CBA examining the effects of the same programme as Elbel 2015a – the installation of water jets in public schools in New York City – on student body weight and school cafeteria milk purchases. It is based on data from 1227 schools, including 483 schools which received a water jet during the study period, which lasted from June 2008 to August 2013, and 744 schools which did not receive a water jet during this period. It used a stepped‐wedge design, in which all schools started as control schools, and crossed over to the intervention group once they received a water jet. Body weight data are from the New York FITNESSGRAM survey, a routinely‐administered annual school health examination, and includes 3,319,083 observations on 1,065,562 students. Data on school cafeteria milk purchases are from an administrative database maintained by the New York City Department of Education. The sample was 37% black, 37% Hispanic, and 14% white, and 85% received free or reduced‐price school lunches.
Muckelbauer 2009 is a NRCT which examines the effects of water fountains installed in schools, distribution of re‐usable water bottles to students and a behavioural co‐intervention on SSB, water and juice intake, and student body weight. Seventeen public elementary schools in socially‐deprived neighbourhoods in Dortmund, a medium‐sized post‐industrial city in Germany, received water fountains, and 16 schools in the neighbouring city of Essen served as controls. The behavioural co‐intervention included organised water bottle fill‐ups and classroom lessons on water‐related themes. Beverage intake data were collected with a student questionnaire, and body weight was assessed by trained healthcare professionals at baseline and at 10 months post‐intervention. Participants were followed up individually, and data from 2950 students were included in the analysis.
Visscher 2010 is a NRCT which examines the effects on SSB sales in schools of the installation of water fountains in school cafeterias. Three secondary schools in Zwolle, a medium‐sized city in the Netherlands, received water fountains, and three schools in the same city served as controls. Data are reported for a six‐week baseline period and a three‐month intervention phase. The study does not report how data were collected. In total, 5909 students attended the participating schools.
Van de Gaar 2014 is a cluster‐RCT which examines the effects of a multicomponent ‘water campaign’ intervention on SSB and water intake, as well as student body weight. The intervention included the provision of water in water jugs in classrooms throughout the school day, distribution of water bottles to students, ‘water breaks’ during physical education lessons, and a number of promotional and educational activities. Two elementary schools in multi‐ethnic, socially‐deprived neighbourhoods in Rotterdam, the Netherlands, received the intervention, and two schools in matched neighbourhoods in the same city served as controls. Beverage intake data were collected with student and parent questionnaires, and body weight data were collected by trained personnel with a standardised protocol at baseline and at 13 months post‐intervention. Moreover, trained observers collected data on the number of students bringing SSB to school at baseline and at 13 months post‐intervention. In total, data on 1009 students were analysed. The study reports that the sample included participants with various ethnic backgrounds, including Dutch (approximately 25%), Surinamese/Antillean (approximately 30%), and Moroccan/Turkish (approximately 27%).
SSB consumption (one CBA study, two NRCTs and one cluster‐RCT, very low‐certainty evidence)
Elbel 2015a reports that there was no statistically significant effect on SSB intake at three months (data not shown in the study). Muckelbauer 2009 reports that SSB intake at 10 months decreased by −20 ml/day (95% CI −60 to 20) among participants with foreign‐born parents or grandparents, but remained stable among participants without foreign‐born parents or grandparents (effect estimate ±0 ml/day, 95% CI −60 to 60) (these data are reported in Muckelbauer 2010, a secondary publication to Muckelbauer 2009). Van de Gaar 2014 reports that SSB intake at 13 months decreased by −190 ml/day (95% CI −280 to −100). Van de Gaar 2014 also reports that the share of students bringing SSB to school decreased (odds ratio (OR) 0.5, 95% CI 0.4 to 0.7) and that the share of students consuming SSB every day decreased (OR 0.8, 95% CI 0.5 to 1.3) at 13 months. Based on data for individual schools reported by Visscher 2010, we calculated that SSB sales decreased by −3.6 ml/day/student across the three schools of the intervention group, and by −4.3 ml/day/student across the three schools in the control group (intervention effect +0.7 ml/day/student, no statistical analyses reported by study authors). SSB sales by student varied considerably across the three schools of the intervention and control groups and across the reported time points. We judged this effect size to be below the threshold of public health relevance, and equivalent to no effect.
Sugar‐sweetened milk consumption (one CBA study, very low‐certainty evidence)
Schwartz 2016 reports that consumption of sugar‐sweetened milk intake decreased by −3 ml/day (95% CI −5 to −1) during a five‐year follow‐up period.
Body weight (one NRCT, one CBA study, one cluster‐RCT, very low‐certainty evidence)
Muckelbauer 2009 reports that z‐BMI decreased by −0.00 (95% CI −0.04 to 0.04), and that the share of students with overweight or obesity decreased (OR 0.69, 95% CI 0.48 to 0.99) at 10 months.
Schwartz 2016 reports that z‐BMI decreased by −0.02 (95% CI −0.03 to −0.00), and that the share of students with overweight or obesity decreased by −1.2 percentage points (95% CI −1.9 to −0.5) for boys, and by −0.6 percentage points (95% CI −1.3 to 0.1) for girls during a five‐year follow‐up period. The share of students with obesity decreased by −0.5 percentage points (95% CI −1.0 to 0.1) for boys, and by −0.2 percentage points (95% CI −0.7 to 0.4) for girls during a five‐year follow‐up period.
Van de Gaar 2014 reports that non‐standardised BMI increased by 0.26 kg/m2 (95% CI 0.11 to 0.41) and that the share of students with overweight or obesity increased (OR 1.27, 95% CI 0.78 to 2.07) at 11 months.
Elbel 2015a and Visscher 2010 did not assess effects on body weight.
Adverse outcomes: total milk intake (two CBA studies, very low‐certainty evidence)
Schwartz 2016 reports that total milk intake decreased by −3 ml/day (95% CI −6 to −1) during a five‐year follow‐up period. Elbel 2015a reports that the number of milk‐taking events per 100 students decreased by −7 events (P = 0.17) at three months and by −4 events (P = 0.24) at 10 months.
Secondary outcomes: consumption of alternatives to SSB, intervention costs, and target group perceptions
Elbel 2015a reports that water‐taking events per 100 students visiting the school cafeteria increased by 22 events (P < 0.01) at three months and by 19 events (P < 0.01) at 12 months. Muckelbauer 2009 reports that water intake increased by 220 ml/day (95% CI 140 to 280), and that juice intake decreased by −20 ml/day (95% CI −40 to 20) at 10 months. Schwartz 2016 reports that low‐fat and skim white milk intake decreased by −0.07 ml/day (95% CI −2.4 to 2.2). Van de Gaar 2014 reports that water intake increased by 30 ml/day (95% CI −30 to 90) at 13 months.
Muckelbauer 2009 reports that initial costs per water fountain were approximately EUR 2500 and maintenance costs 13 EUR/year/student. Schwartz 2016 reports that initial costs per water fountain were approximately USD 1000.
Regarding target group perceptions, Elbel 2015a reports that "[t]here were no differences between comparison and intervention schools in students’ opinions about water before and after water jet installation. In the intervention schools, after water jets were introduced, 55% of students said they liked the taste of tap water, 56% said it was safe to drink, and 53% said the tap was healthy with no change from their opinions before the water jets were introduced. Overall, 80% said they noticed the water jet in the cafeteria. (…) Of those reporting that they noticed it, a series of additional questions were asked. Approximately 64% said they used it ‘every day‘ or ‘occasionally‘ with no difference between age groups, and 59% liked the taste of the water that came from the machine.“ Visscher 2010 reports that "[c]anteen keepers mentioned that pupils were enthusiastic about the free water coolers and that the water tasted better than the water tapped from the taps in the toilets."
B.3 Small prizes for the selection healthier beverages in school cafeterias
Description of studies contributing data to this comparison
We included two ITS studies (Emerson 2017; Siegel 2016b) and one RCT (Hendy 2011) on interventions in which children having lunch in the cafeterias of elementary schools received small prizes for selecting healthier beverages.
In Hendy 2011, children in the intervention group received token rewards for selecting healthy beverages (defined as skim milk, 1% or 2% low‐fat white milk, 100% fruit juice, and water) instead of unhealthy beverages (defined as SSB, sugar‐sweetened flavoured milk, and whole plain milk). Children in the control group received rewards for showing ‘good citizenship behaviours’, such as talking quietly during meals and keeping their meal area clean. Research assistants and parent volunteers punched a star‐shaped hole in the children’s nametag each time a child showed a desired behaviour, and once a week children could trade 10 stars for a small reward, such as pens, notebooks, modelling clay or stickers. Data were collected by trained observers, who recorded children’s beverage choices during three days each week at baseline and throughout the three‐month intervention phase. Beverage outcome data on 252 children were included in the analyses. Participants were 1st to 4th grade elementary‐school children, and the intervention was implemented in one school located in a small town in Pennsylvania, USA. Over 95% of participants were white.
Emerson 2017 and Siegel 2016b examined an intervention called ‘Power Plate’, implemented in two separate sets of schools. In this intervention, healthy food and beverage items (plain fat‐free milk, fruits, vegetables, and main dishes with whole grain) offered in the school cafeteria were labelled with green, smiley‐faced emoticons, and students who selected a ‘Power Plate’, i.e. a meal consisting only of healthy food and beverage items, received small prizes. Prizes were distributed on the first day of the intervention, and then on every Tuesday and Thursday during the intervention phase, and included bracelets, stickers and temporary tattoos. The main alternative to plain fat‐free milk available in the school cafeterias was sugar‐sweetened, chocolate‐flavoured milk. SSBs were not available in the school cafeterias. Both studies assess effects on sugar‐sweetened and plain milk consumption based on cafeteria cash register data collected at baseline and throughout the study period.
Emerson 2017 was implemented in three elementary schools in Norwood, a small city in Massachusetts, USA, which were attended by 960 students, of whom approximately 60% participated in the school lunch programme and were thus exposed to the intervention. Seventy‐one per cent of participants were white, 13% black, and 10% Hispanic, and 73% were below 130% of the national poverty line. The length of follow‐up was 20 months (October 2014 to May 2016), with 56 weeks of data collection.
Siegel 2016b was implemented in eight public elementary schools in a low‐income, majority‐minority inner city district of Cincinnati, Ohio, USA, which were attended by 3001 students, an unspecified number of whom participated in the school lunch programme and were exposed to the intervention. More than 95% of students were below 130% of the national poverty line. Follow‐up was four to eight months for seven out of eight participating schools, and two to three months for the remaining school.
In one of the eight schools included in Siegel 2016b food waste, i.e. the percentage of white milk selected but not consumed by students, was assessed in addition to the outcomes mentioned above. Food waste data were collected by trained observers from 111 students during one day at baseline and from 96 students during one day during the intervention phase (no exact date provided), and is reported in Hudgens 2017 (a secondary publication to Siegel 2016b). Results for food waste are based on an uncontrolled before‐after (UBA) analysis.
Unhealthy beverage and sugar‐sweetened milk consumption (one RCT and two ITS studies, low‐ to moderate‐certainty evidence)
Hendy 2011 reports that the number of meals with unhealthy beverages (defined as sugar‐sweetened milk, SSB, and whole plain milk) selected by children decreased by −3.5 a week in the intervention group, and by −0.5 a week in the control group during a three‐month intervention phase (P = 0.000; the total number of meals served each week was six, and the most popular beverage at baseline was sugar‐sweetened chocolate milk). Only healthy beverage selection was recorded directly, and effect estimates for unhealthy beverage selection are based on the assumption that the share of children not having any beverage for lunch was approximately 1% and therefore negligible. Effect estimates for unhealthy beverage selection are not reported in the study’s published report, but were calculated by us based on the above information, which was provided to us by the study’s corresponding author.
Siegel 2016b reports that chocolate‐milk purchases decreased by −0.12 servings/day (P < 0.001, representing a decrease of −17%) during the follow‐up period. Emerson 2017 reports that chocolate‐milk purchases decreased from 0.82 servings/day to 0.70 servings/day (P < 0.001) during a 20‐month follow‐up period, from which we calculated a decrease of −0.12 servings/day.
Adverse outcomes: total milk intake and food waste (two ITS studies, very low‐certainty evidence)
Siegel 2016b reports that total milk purchases decreased by −0.03 servings/day (P < 0.001). Emerson 2017 reports that total milk purchases increased from 0.92 servings/day to 0.96 servings/day (P < 0.001) during a 13‐month follow‐up period, from which we calculated an increase by 0.04 servings/day.
Hudgens 2017 (a secondary publication to Siegel 2016b) reports that food waste (i.e. the share of total milk selected but not consumed by students) increased from 67% to 72% from before to after intervention, from which we calculated an increase by 5 percentage points (P = 0.275, length of follow‐up not reported). Hendy 2011 reports that food waste could not be assessed as beverages were served in opaque cartons, but notes that “nearly 100% of children open[ed] and dr[a]nk from their chosen cartons."
Secondary outcomes: intervention costs, alternative beverage selection, and target group perceptions
Hendy 2011 reports that the intervention was “relatively low in cost at two U.S. dollars per child per month of application.” Siegel 2016b and Emerson 2017 report that the intervention was low‐cost (no quantitative data reported).
Hendy 2011 reports that the number of meals with healthy beverages (defined as skim milk, 1% or 2% low‐fat white milk, 100% fruit juice, and water) selected by children increased by 3.46 a week in the intervention group, and by 0.52 a week in the control group during a three‐month intervention phase (P = 0.000; the number of meals served per week was six). Siegel 2016b reports that plain fat‐free milk purchases increased by 0.09 servings/day (P < 0.001) during the follow‐up period. Emerson 2017 reports that plain milk selection increased from 0.10 servings/day to 0.26 servings/day (P < 0.001) during a 13‐month follow‐up period, from which we calculated an increase by 0.16 servings/day.
Regarding target group and stakeholder perceptions, Hendy 2011 reports that “[t]he program has received high acceptability ratings from children and parents in past research, with a mean rating of 2.9 on a three‐point scale for children, and a mean rating of 4.4 on a five‐point scale for parents (...), and the present study documented a mean rating of 3.8 on a five‐point scale for school staff.”
B.4 Improved placement of healthier beverages in school cafeterias
Description of studies contributing data to this comparison
We included one cluster‐RCT examining the effects of improved placement of healthier beverages in school cafeterias (Cohen 2015). In this study, six out of 14 elementary and middle schools which had participated in an earlier study by the same investigators were randomly selected to receive a ‘smart café’ intervention. As part of this intervention, white low‐fat milk was placed prominently in front of sugar‐sweetened milk to encourage its consumption. Sugar‐sweetened and white milk selection was recorded by trained observers at baseline and at three to four months follow‐up. The schools were located in urban, low‐income school districts in Massachusetts, USA, and the total number of students in the study was 2638. More than 80% of participants were Hispanic, and eligible for free or reduced‐price school meals.
Selection and consumption of sugar‐sweetened milk (one cluster‐RCT, low‐certainty evidence)
Cohen 2015 reports that there was no statistically significant change (data not shown in the study) in the selection and consumption of sugar‐sweetened milk.
Adverse outcomes: stakeholder discontent (one cluster‐RCT, very low‐certainty evidence)
Cohen 2015 reports that the intervention "met with substantial resistance from teachers, who were concerned that younger students were having trouble accessing the less prominently displayed sugar‐sweetened milk."
Secondary outcomes: selection and consumption of white milk
Cohen 2015 reports that there was no statistically significant change (data not shown) in the selection and consumption of white milk.
B.5 Fruit provision in schools
Description of studies contributing data to this comparison
We included one cluster‐RCT (Da Costa 2014) and one CBA study (Øverby 2012) examining the effects of fruit provision in schools on SSB intake by students.
In Da Costa 2014, students received weekly deliveries of seasonal fruit, and were exposed to a number of promotional and educational activities focused on fruit consumption. SSB intake was assessed with student questionnaires at baseline and at nine‐month follow‐up. The study was conducted in 20 public high schools in Florianopolis and Recife, Brazil, and data on 2155 students were included in the intention‐to‐treat analyses.
Øverby 2012 examines the effects of two different types of fruit provision schemes, namely a fruit subscription programme (with parental payment) and a free fruit provision scheme (without parental payment). In both schemes students received one piece of fruit or vegetable each day they attended school. SSB and diet beverage intake were assessed with student questionnaires at baseline and at six‐year follow‐up. The study was conducted at 27 elementary schools in the Hedmark and Telemark counties in Norway. Data were contributed by 1488 students at the baseline assessment, and by 1339 students at the follow‐up assessment.
SSB consumption (one cluster‐RCT and one CBA study, very low‐certainty evidence)
Da Costa 2014 reports that SSB intake decreased (P = 0.003, data shown in the study not intelligible to review authors) at nine months follow‐up. Øverby 2012 reports that SSB intake measured with an unhealthy snack frequency score decreased by −1.4 in the free‐fruit provision group, by −1.1 in the fruit subscription group, and by −0.7 in the control group (P = 0.002 for time*group interaction) at six‐year follow‐up. These data were provided to us by the study authors.
Secondary outcomes: diet beverage intake
Øverby 2012 reports that diet beverage intake measured with an unhealthy snack frequency score increased by 0.1 in the free‐fruit provision group, by 0.5 in the fruit subscription group, and by 0.5 in the control group (P = 0.11 for time*group interaction) at six‐year follow‐up.
C. Economic tools
We included seven studies on economic tools other than taxation, including studies on:
C.1 Price increases on SSB (Blake 2018; Breeze 2018; Cornelsen 2017);
C.2 Financial incentives to purchase low‐calorie beverages implemented through supermarket loyalty cards (Franckle 2018; Ball 2015; Ni Mhurchu 2010);
C.3 Price discounts on low‐calorie beverages in community stores (Brimblecombe 2017).
C.1 Price increases on SSB
Description of studies contributing data to this comparison
We included three ITS studies on price increases on SSB (Blake 2018; Breeze 2018; Cornelsen 2017).
In Blake 2018, prices of red‐labelled beverages (including SSB and sugar‐sweetened milk, as well as fruit juices larger than 250 ml per unit) sold in a convenience store were raised by 20%, and leaflets explaining the intervention were given to customers inquiring about the price increase. Effects on sales of red‐, amber‐ and green‐labelled beverages, as well as on total beverage revenue were assessed with routinely‐collected sales data during a 122‐week (approx. 28 months) baseline period and a 17‐week intervention phase. The intervention was implemented in one convenience store located on the premises of a public hospital in Melbourne, Australia.
In Breeze 2018, prices of SSB sold in public leisure centres were raised by GBP 0.20 (approximately EUR 0.23 or USD 0.27), equivalent to a price increase of 11% to 25%. Further intervention components included “staff training in order to deliver face to face awareness of the scheme with customers; publicity in local and national media; publicity within venues including posters, billboards and drinks stickers in café and vending areas." Effects on sales of SSB, diet beverages, water and fruit juice, and total cold beverage sales were assessed with routinely‐collected sales data during an 18‐month baseline period and a 12‐month intervention phase. The intervention was implemented in seven public leisure centres in Sheffield, UK.
In Cornelsen 2017, prices of SSB sold in chain restaurants were raised by GBP 0.10 (approximately EUR 0.11 or USD 0.14), equivalent to a price increase of 3% to 4%. In addition, a number of non‐fiscal intervention components were implemented, including the following: a reorganisation of the beverage menu into two sections, one for SSB and one for alternatives to SSB; the addition of a short text to the SSB section of the menu explaining the price increase and that its proceeds would be used to support a children's health charity; the addition of fruit spritzers (100% fruit juice mixed with water) to the menu; and the airing of a documentary on the health effects of sugar on national TV. Effects on the sales of SSB and alternatives to SSB were evaluated with electronic sales data during a 12‐week baseline and a six‐month intervention phase. The intervention was implemented in 37 restaurants belonging to the restaurant chain Jamie’s Italian, located in 27 cities in the UK.
SSB sales (three ITS studies, moderate‐certainty evidence)
Cornelsen 2017 reports that the number of on‐menu SSB units sold per customer decreased by −11% (95% CI −17 to −4) at three months and by −9% (95% CI −15 to −3) at six months. The number of off‐menu SSB units (which could be requested by customers but were not listed on the menu) sold per customer decreased by −8% (95% CI −16 to 0.3) at three months and by −4% (95% CI −10 to 2) at six months.
Blake 2018 reports that the number of red‐labelled beverage units sold (including SSB and sugar‐sweetened milk) decreased by −25% (95% CI −29 to −20), and that the volume of red‐labelled beverages sold decreased by −28% (95% CI −32 to −23) at four months. Moreover, the study reports that the total sugar content of all beverages sold decreased by −24% (95% CI −27 to −18), and that the total calorie content of all beverages sold decreased by −23% (95% CI −29 to −17) at four months.
Breeze 2018 reports that the volume of SSB sold per attendance, i.e. each person visiting one of the leisure centres on a given occasion, decreased from 16 ml to 11 ml, equivalent to a decrease by −27% (95% CI −59 to −3) at 12 months. The number of SSB units sold per attendance decreased from 0.043 to 0.030, or by −31% (95% CI −59 to −4) at 12 months.
Our pooled effect estimate based on data from all three studies is that SSB sales decreased by −19% (95% CI −33 to −6) at four to 12 months, with relevant subgroup differences according to the magnitude of the price increase (see Figure 10; Analysis 2.1). Graphical inspection of the forest plot and the I2 statistic of the overall analysis (89%) indicate substantial statistical heterogeneity, which may be explained by differences in the magnitude of price increase, and by differences in population, intervention delivery and context.
10.
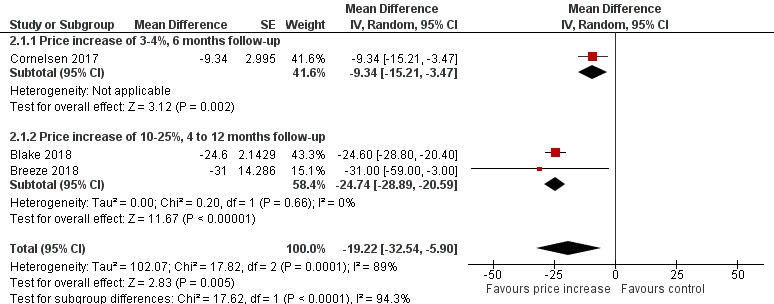
Analysis 2.1: Effects of price increase on SSBon units of SSB sold [% change, 4 to 12 months follow‐up].
2.1. Analysis.
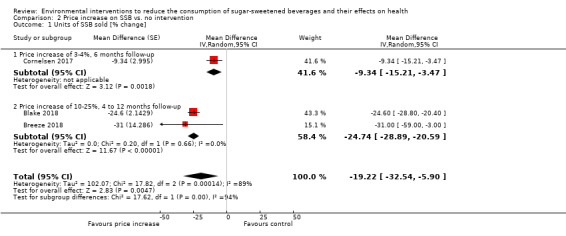
Comparison 2 Price increase on SSB vs. no intervention, Outcome 1 Units of SSB sold [% change].
Adverse outcomes: total beverage sales and revenue from beverages (two ITS studies, low‐certainty evidence), target group discontent and stakeholder concerns (one ITS study, low‐certainty evidence)
Blake 2018 reports that total revenue from beverage sales decreased by −10% (95% CI −14 to −7) at four months. Breeze 2018 reports that total cold beverage unit sales decreased from 0.1 per attendance to 0.095 per attendance, or by −5% (P > 0.05) at 12 months.
Blake 2018 reports that “while the majority of surveyed customers agreed with the intervention, 39% disagreed that the store should continue with higher prices, and 29% of surveyed customers disagreed that higher prices are generally a good way to reduce community consumption of sugary beverages. (…) The issue of customer complaints was a strong sub‐theme from the qualitative interviews of store and hospital staff. Interviewees indicated that only a small proportion of customers provided negative feedback. They reported that the majority of complaints referred to a perception of choice removal, concerns that prices were unreasonably high, and desires for forewarning of price changes. All four staff interviewees perceived that there were fewer complaints as the intervention progressed, and that many customers were able to recognize the potential community health benefits of the intervention.” Blake 2018 also reports that “[a]lthough one staff member was concerned about a negative impact on customer purchases and profitability, there was an overall perception that the intervention was business neutral (…). However, ongoing concerns about customer perceptions of the store and the long‐term impact on the business were expressed by all staff interviewees (…). At the end of the 17‐week initial intervention, with concern about need to meet contractual obligations to buyers’ groups, including use of multi‐buys (eg, 2‐for‐1 deals) on red beverages, the price differential was partially discontinued.”
Secondary outcomes: sales of alternative beverages, target group perceptions
Cornelsen 2017 reports that the number of units of diet cola served per customer decreased by −7% (95% CI −12 to −3) and that the number of units of bottled water served per customer decreased by −7% (95% CI −11 to −2). The study notes that data on the sale of alternatives to SSB may be incomplete, as data on orders of tap water, which was served for free and advertised prominently on the reorganised beverage menu, were not recorded.
Blake 2018 reports that volume sales of amber‐labelled beverages, including diet beverages and 100% fruit juice in serving sizes less than 250 ml, decreased by −27% (95% CI −40 to −16) at four months. Sales of green‐labelled beverages, including water and plain low‐fat milk, increased by 27% (95% CI 14 to 40) at four months.
Breeze 2018 reports that unit sales of diet beverages increased from 0.026 units to 0.033 units per attendance, or by 27% (95% CI 6 to 48) at 12 months. Unit sales of water increased from 0.019 units per attendance to 0.020 units, or by 7% (P > 0.05).
Regarding target group perceptions, Blake 2018 reports that “15% of customers noticed the price difference and 61% supported the intervention. (…) 30% of surveyed customers agreed that the price differential had changed their purchases, or would do so if they had been aware of it.”
C.2 Financial incentives to purchase low‐calorie beverages implemented through supermarket loyalty cards
Description of studies contributing data to this comparison
We included three RCTs on financial incentives to purchase low‐calorie beverages, implemented through supermarket loyalty cards (Ball 2015; Franckle 2018; Ni Mhurchu 2010).
In Ball 2015, a price discount of 20% was applied to bottled water and diet beverages when participants used their supermarket loyalty cards to make purchases at the participating supermarkets. Price discounts were not visible at point‐of‐purchase, but participants received a list of discounted items. Effects on purchases of SSB, water and diet beverages were assessed based on electronic sales data collected through the participants’ loyalty cards at baseline, during a three‐month intervention phase and during an additional three‐month post‐intervention phase, during which no price discounts were applied. In addition, self‐reported beverage intake was assessed with a validated questionnaire at baseline and at three and six months. Data from 574 adult female customers of one supermarket chain in Melbourne, Australia were included in the analyses reported in this review. Forty‐four per cent of participants were from low socio‐economic status areas, and 50% did not have tertiary education. The study also evaluated the effects of a nutrition skills‐building intervention, which we did not include in this review.
In Franckle 2018, participants who refrained from buying any red‐labelled beverages (mainly SSBs) at the participating supermarket using their loyalty card during a given month in the intervention phase received a USD 25 supermarket gift voucher. Effects on the number of red‐labelled beverages purchased each month, and the share of participants purchasing one or more red‐labelled beverage each month were assessed with electronic sales data collected through the participants’ loyalty cards at baseline and during the five‐month intervention period. In addition, effects on the share of participants reporting consumption of one or more red‐labelled beverage a week were assessed with a beverage frequency questionnaire at baseline and at five months. One hundred and forty‐eight adult customers of one supermarket in Chelsea, a small city adjacent to Boston, Massachusetts, USA, were included in the study. Most participants were women, and of Hispanic/Latino ethnicity.
In Ni Mhurchu 2010, a price discount of 12.5% was applied to bottled water and diet beverages when participants used their supermarket loyalty cards to make purchases at the participating supermarkets. Price discounts were not visible at point‐of‐purchase, but participants received a list of discounted items. Effects on average energy density of beverages purchased were assessed based on electronic sales data collected through the participants’ loyalty cards at baseline, during a six‐month intervention phase and during an additional six‐month post‐intervention phase, during which no price discounts were applied. Data from 1028 adult customers of one supermarket chain in the Lower North Island region of New Zealand were included in the analyses reported in this review. Most participants were women, 23% were Māori and 9% Pacific Islanders, and approximately equal numbers of participants were from low‐ and high‐income households. The study also evaluated the effects of an education skill‐building intervention, which we did not include in this review.
SSB consumption and purchases (three RCTs, low‐certainty evidence)
Ball 2015 reports that SSB purchases increased by 55 ml/day (95% CI −7 to 117) and self‐reported SSB intake increased by 10 ml/day (95% CI 0 to 20) at three months. Ni Mhurchu 2010 reports that energy density of beverages purchased decreased by −0.1 MJ/kg (95% CI −0.4 to 0.2) at six months. Franckle 2018 reports that the number of red‐labelled beverages purchased each month decreased by −0.14 beverage items/month (95% CI −0.8 to 0.6). These data were provided to us by the study authors. Franckle 2018 reports that the share of participants who purchased any red‐labelled beverage decreased by −9 percentage points a month (P = 0.002), and the share of participants reporting consuming any red‐labelled beverage each week decreased significantly (−23% in the intervention group versus −2% in the control group, P = 0.01) during the five‐month intervention period.
Adverse outcomes: purchases of less‐healthy products (one RCT, low‐certainty evidence)
Ni Mhurchu 2010 reports that purchases of all less‐healthy products (including foods and beverages) increased by 0.07 kg/week (95% CI −0.15 to 0.29) at six months, and by 0.05 kg/week (95% CI −0.18 to 0.27) at 12 months (including six months additional follow‐up without intervention).
Secondary outcomes: implementation cost, target group perceptions, and water and diet beverage intake
Ball 2015 reports that the total cost of providing the three‐month‐long intervention was AUD 158 (approximately USD 117 or EUR 100) per household. Franckle 2018 reports that the costs of the incentive programme, excluding overhead costs, was USD 5.3/month (approximately EUR 4.7/month) per participant randomised to the intervention group.
Olstad 2016 (the process evaluation of Ball 2015) reports that "[p]articipants indicated limited appreciation for, and use of beverage (…) discounts." Ni Mhurchu 2010 reports that “[o]f the 166 (40%) participants randomly assigned to receive discounts who only sometimes or never bought discounted foods, the reason given by most (52%) was that it took too long to sort through the list [of discounted foods and beverages]". Franckle 2018 reports that participants in the intervention group “were significantly more likely to report noticing changes in the supermarket beverage aisles during the intervention period (58 % v. 30 %, P = 0.003) and were less likely to report buying red beverages at other supermarkets during the study period (15 % v. 39 %, P = 0.004).”
Ball 2015 reports that bottled water purchases increased by 29 ml/day (95% CI −12 to 70), self‐reported bottled and tap water intake decreased by −24 ml/day (95% CI −133 to 85), diet beverage purchases increased by 11 ml/day (95% CI −29 to 51) and self‐reported diet beverage intake increased by 7 ml/day (95% CI −7 to 21).
C.3 Price discounts on low‐calorie beverages in community stores
Description of studies contributing data to this comparison
We included one cluster‐RCT on price discounts on low‐calorie beverages in remote community stores (Brimblecombe 2017). In this study, a price discount of 20% was directly applied at the point of purchase to bottled water and diet beverages, and advertised with promotional signs. The study used a cluster‐randomised stepped‐wedge design, in which 20 stores were allocated randomly to receive the intervention, staggered at eight‐week intervals. Effects on SSB, water and diet beverage sales were collected through electronic sales data during an 11‐month baseline period, a six‐month intervention phase, and an additional six‐month post‐intervention phase during which no discounts were applied. Each store was located in a separate very remote, socio‐economically deprived Indigenous community (i.e. settlement) in the Northern Territory of Australia, and was the only commercial source for foods and beverages within 20 km. The total population of the 20 communities included in the study was 8515.
SSB consumption (one cluster‐RCT, low‐certainty evidence)
Brimblecombe 2017 reports that SSB intake per capita increased by 6% (95% CI −3 to 15) during the six‐month intervention period, and by 6% (95% CI −7 to 21) during the additional five‐month follow‐up period. SSB intake was 365 g/capita/day at baseline.
Adverse outcomes: total calories purchased (one cluster‐RCT, low‐certainty evidence)
Brimblecombe 2017 reports that "[t]here have been concerns that total calories purchased might increase with price subsidies on healthy foods thereby potentially negating health gains. Our findings add to this evidence because we observed increases (albeit non‐significant) in the volume of other food purchases and increases in energy and sodium (due to its ubiquity in the food supply) during and after the price discount. Similar increases in purchases were observed for both healthy and less healthy food groups."
Secondary outcomes: water and diet beverage intake
Brimblecombe 2017 reports that bottled water intake per capita increased by 18% (95% CI 1 to 37) during the six‐month intervention period, and by 12% (95% CI −11 to 41) during the additional five‐month follow‐up period, and that diet beverage intake per capita increased by 5% (95% CI −6 to 18) during the six‐month intervention period, but decreased by −8% (95% CI −23 to 10) during the additional five‐month follow‐up period. At baseline, bottled water intake was 44 ml/per capita/day, and diet beverage intake was 63 ml/per capita/day.
D. Advertisement regulation
We did not find any eligible studies on advertisement regulation.
E. Whole food supply interventions
E.1 Voluntary food and beverage industry initiatives to improve the nutritional quality of the whole food supply
Description of studies contributing data to this comparison
We included one CBA study (Ng 2014a) and two controlled ITS studies (Ng 2014b; Taillie 2015) on voluntary food and beverage industry initiatives aiming to improve the nutritional quality of the whole food supply.
Ng 2014a and Ng 2014b examine the effects of the Healthy Weight Commitment Foundation Market Place Pledge. As part of this pledge, 16 major food and beverage manufacturers in the USA vowed to engage in a variety of activities with the aim of “reducing or controlling calories while preserving or enhancing the overall nutrition of healthier product options” (quoted in Ng 2014a). In particular, the 16 companies which signed the pledge promised to collectively reduce, between 2007 and 2015, the energy content of their total sales in the USA by 1.5 trillion calories. Ng 2014a examines the effects of this pledge on the total energy content of beverages sold, measured in kcal/capita/day, at baseline and at four years, comparing brands produced by companies which participated in the pledge with national beverage brands produced by companies which did not participate in the pledge, as well as with private‐label brands (also known as generic brands or unbranded products). The analysis is based on sales data provided by the market research firm Nielsen through the Nielsen Scantrack database. Ng 2014b examines the effects of the pledge on calories from SSB purchased by households with children aged two to 18 years during a seven‐year baseline period and during a four‐year intervention phase, comparing trends for purchases from companies participating in the pledge with purchases from companies not participating in the pledge. The analysis is based on data from the Nielsen Homescan database, with data on 61,126 households included in the analyses.
Taillie 2015 examines the effects of Walmart’s Healthier Food Initiative on SSB sales by Walmart in the USA. As part of this initiative, Walmart announced a number of measures to help consumers make healthier food and beverage purchases, including front‐of‐package nutrition labelling, price reductions on healthier items, and a reduction of added sugars by 10% in key product categories. The study examines effects on SSB purchases as a share of total consumer packaged‐good purchases by comparing trends during an 11‐year baseline period (2000 to 2011) and during a three‐year intervention phase (2011 to 2013) for Walmart and a set of other chain retailers, which were chosen as a comparison group. Participants were members of households covered by the Nielsen Homescan longitudinal data set (a nationally representative data set covering consumer packaged‐goods purchases in the USA). Eighty‐six per cent of participants were non‐Hispanic white, and 7% were below the national poverty line.
Energy from beverages sold, SSB purchases and SSB sales (one CBA and two ITS studies, very low‐certainty evidence)
Ng 2014a reports that the energy content of beverages (including SSB) sold by companies participating in the Healthy Weight Commitment Foundation Pledge decreased by −14 kcal/per capita/day compared to a decrease by −3 kcal/per capita/day for national‐brand companies not participating in the pledge at four years, and a decrease by −14 kcal/per capita/day for private‐label brands. (Study authors note that some private‐label brands covered by the analysis were produced by companies participating in the Healthy Weight Commitment Foundation Pledge; the comparison with national‐brand companies not participating in the pledge may therefore be the better comparison). Ng 2014a also reports that SSB sales by companies participating in the Healthy Weight Commitment Foundation Pledge decreased by −7 kcal/per capita/day at four years (no P values or CIs reported, data for the control group not reported).
Ng 2014b reports that SSB purchases from companies participating in the Healthy Weight Commitment Foundation Pledge measured in kcal/household/day decreased less than expected, based on pre‐intervention trends during a four‐year follow‐up period in both the intervention and control groups (P < 0.001, results shown graphically only, see appendix figure C3 of Ng 2014b; for SSB purchases the study does not report a direct numerical comparison between the intervention and control groups).
Taillie 2015 reports that after the implementation of Walmart’s Healthier Food Initiative the percentage volume of SSB purchased from Walmart decreased more steeply than expected, based on pre‐intervention trends (P < 0.01, results shown graphically only, see appendix exhibit 3 of Taillie 2015), and more than for other chain retailers during a three‐year follow‐up period (results shown graphically only).
F. Retail and food service interventions
We included seven studies on retail and food service interventions, including studies on:
F.1 Healthier default beverages in children’s menus in restaurants (Peters 2016a);
F.2 In‐store promotion of low‐calorie beverages in supermarkets (Foster 2014);
F.3 Healthier vending machines in workplaces and schools (Ermetici 2016; Hua 2017; French 2010);
F.4 Urban planning restrictions on new fast‐food outlets (Sturm 2015);
F.5 Restrictions to the number of stores selling SSB in remote communities (Minaker 2016).
F.1 Healthier default beverages in children’s menus in restaurants
Description of studies contributing data to this comparison
We included one ITS study on healthier default beverages in children's menus in restaurants (Peters 2016a). In this study, the default beverage sold as part of the children’s menus was changed from SSB to low‐fat milk, water, or 100% fruit juices (at baseline, SSBs were the only beverages available as part of the children’s menus; estimates reported by the study are therefore based on the comparison of 100% of customers selecting SSB versus the percentage of customers selecting the healthier beverages once they became available and were offered as default). After the intervention was implemented, SSBs were still available, but had to be actively requested by customers. The share of children’s menus sold with healthier beverages, i.e. beverages other than SSB, were assessed at baseline and at four, five and six years post‐intervention with electronic sales data. The intervention was implemented in 145 quick‐service and table‐service restaurants located in the Walt Disney World theme park in Orlando, USA.
SSB purchases (one ITS study, low‐certainty evidence)
Peters 2016a reports that the acceptance rate for healthy beverage defaults in children’s menus was 66% at four years and 68% at six years, implying that the share of children’s menus served with SSB decreased by −66 percentage points at four years and by −68 percentage points at six years (no P values or CIs reported for the pre‐post‐comparison).
F.2 In‐store promotion of low‐calorie beverages in supermarkets
Description of studies contributing data to this comparison
We included one cluster‐RCT on in‐store promotion of low‐calorie beverages in supermarkets (Foster 2014). In this study, a variety of in‐store promotion techniques commonly used in supermarkets were applied to increase sales of water and diet beverages, including improved placement, multiple facings, call‐out signs and shelf runners, and secondary placements at end caps and on dead‐space stacks. Effects on weekly sales of SSB, water and diet beverages from in‐aisle shelves and check‐out coolers were assessed with electronic sales data during a three‐month baseline period and a six‐month intervention phase. The study was conducted in eight supermarkets belonging to two supermarket chains and located in urban, low‐income, high‐minority neighbourhoods in Philadelphia and Wilmington, USA, four of which were randomly selected to receive the intervention.
SSB sales (one cluster‐RCT, moderate‐certainty evidence)
Foster 2014 reports that in‐aisle SSB sales decreased by −11 l/day (95% CI −63 to 40) per participating supermarket, and check‐out cooler SSB sales decreased by −2 units/day (95% CI −5 to 1) per participating supermarket.
Secondary outcomes: financial measures, water and diet beverage sales
Foster 2014 reports that products promoted by the intervention were “cost neutral or cost less for the consumer and profit‐neutral or more profitable for grocers compared with other top‐selling products in the category.” Foster 2014 reports that in‐aisle bottled water sales increased by 7 l/day (95% CI −48 to 62) and in‐aisle diet beverage sales decreased by −2 l/day (95% CI −10 to 6), and that check‐out cooler bottled water sales increased by 3 units/day (95% CI 1 to 9) and check‐out cooler diet beverage sales increased by 0.2 units/day (95% CI −1 to 2) per participating supermarket.
F.3 Healthier vending machines in workplaces and schools
Description of studies contributing data to this comparison
We included an NRCT (Ermetici 2016) and two cluster‐RCTs (French 2010; Hua 2017) on healthier vending machines in workplaces and schools.
In Ermetici 2016, the nutritional quality of foods and beverages offered in vending machines in schools was improved, and “[a]n agreement was reached with the vending machine supplier to keep prices as low as possible and to dedicate part of the proceeds to childhood health promotion initiatives.” The healthier beverages offered in the vending machines included drinkable yogurt, fruit juices and smoothies without added sugars. Study authors report that the products offered in the redesigned vending machines contained on average 60 kcal and 14 g of added sugars per 100 g less than the traditional vending machines. In addition, educational posters promoting healthy diets, water consumption and physical activity were posted. Data from 462 students were included in analyses. Effects on SSB intake were assessed with a questionnaire at baseline and at two years. The study was implemented in six middle schools in Milan, Italy, of which three served as controls. Most participants were white, and fewer than 5% belonged to ethnic minorities.
French 2010 examines the effects of increasing the availability of diet beverages by 50% and of lowering their price by at least 10% in vending machines located in two bus garages, which were chosen randomly from a set of four garages, all belonging to one urban transit company. A behavioural co‐intervention was also implemented, which included healthy eating challenges, and self‐weighing programmes. Effects on SSB consumption among garage employees were assessed at baseline and at 18 months with a self‐administered questionnaire, which was completed by 1094 employees at baseline and by 1065 at follow‐up. The garages were located in Minneapolis, USA. Most participants (73%) were bus drivers while 16% were bus maintenance staff, 56% were obese, and 79% were men.
Hua 2017 examined the effects of three different interventions targeting water and diet beverages, namely improved availability and placement, price reductions of 30% to 50%, and point‐of‐purchase promotional signage. Effects on sales of healthier beverages were assessed at baseline and during a five‐month intervention phase. The intervention was implemented in 28 beverage‐vending machines located on the premises of a university in Connecticut, USA, which were randomly allocated to one of eight conditions in a 2x2x2 factorial design.
SSB consumption (two cluster‐RCTs and one NRCT, very low‐certainty evidence)
French 2010 reports that SSB consumption increased by 14 ml/day (P > 0.05) at 18 months follow‐up. Ermetici 2016 reports that SSB consumption frequency decreased by −1.1 times/week (95% CI −1.5 to −0.7) among normal‐weight participants, and by −0.8 times/week (95% CI −1.5 to −0.1) among participants with overweight and obesity at two years follow‐up. Hua 2017 does not report effects on mean sales of SSB or healthier alternatives to SSB, but conducted post hoc analyses of the best‐selling beverages pre‐ and post‐intervention, and reports that “there was an overall shift toward healthier purchasing. (…) [W]hereas three of the top‐five best‐selling beverages preintervention were sold in 20‐oz bottles, none of the top five best‐selling beverages postintervention were sold in 20‐oz bottles aside from water.” We found it difficult to judge on the basis of this description and the list of best‐selling beverages provided by study authors if the overall effect of the intervention on SSB sales was positive or negative.
Adverse outcomes: total revenue (one cluster‐RCT, low‐certainty evidence)
Hua 2017 reports that "the control machines and machines that had product guidelines and price changes both had small but significant decreases in revenue (‐$156.10 and ‐$593.55, respectively; P < 0.05)."
Secondary outcomes: bottled water sales and intervention costs
Hua 2017 reports that bottled water became one of the five top‐selling beverages post‐intervention (data not shown in the study). Ermetici 2016 reports that “[a]lternative healthier vending machines did not cost more than the previous ones."
F.4 Urban planning restrictions on new fast‐food outlets
Description of studies contributing data to this comparison
We included one CBA study on urban planning restrictions on new fast‐food outlets (Sturm 2015). This study examines the effects of a zoning regulation that restricted the opening or expansion of stand‐alone fast‐food restaurants in parts of South Los Angeles on SSB intake, comparing South Los Angeles with the rest of the City of Los Angeles and Los Angeles County. The analysis is based on data from the California Health Interview Survey, a routinely‐conducted population‐level nutrition survey. Data were collected approximately one year before and two to three years after the intervention. The baseline sample size was 467 in the intervention group and 15,420 in the control group, and the sample size of the last follow‐up assessment was 535 in the intervention group and 11,286 in the control group. The area in which the intervention was implemented was low‐income and ethnically diverse.
SSB intake frequency (one CBA study, very low‐certainty evidence)
Sturm 2015 reports that SSB intake frequency decreased by between −0.9 (P > 0.05, difference‐in‐difference estimate for the comparison between South Los Angeles and other parts of Los Angeles City) and −0.3 (P > 0.05, difference‐in‐difference estimate for the comparison between South Los Angeles and other parts of Los Angeles County). The study does not report which scale or measure was used to assess intake frequency.
F.5 Restrictions in the number of stores selling SSB in remote communities
Description of studies contributing data to this comparison
We included one ITS study (Minaker 2016) on restrictions in the number of stores selling SSB in remote communities. Minaker 2016 examines the effect of the discontinuation of the sale of SSB from one out of three stores selling SSB in small rural community. Effects on community‐wide sales of SSB are assessed with electronic sales data from all three stores selling SSB in that community. Reported effects are based on an ITS analysis comparing a 20‐month baseline period with an eight‐month intervention phase, controlling for underlying trends and seasonality. The study was conducted in Baddeck, a community with approximately 800 permanent residents located on Cape Breton Island, Nova Scotia, Canada.
SSB sales (one ITS study, very low‐certainty evidence)
Minaker 2016 reports that community‐wide SSB sales decreased by CAD −95/day (95% CI −217 to 28) (approximately USD −73 or EUR −62) during the eight‐month intervention period, based on an ARIMA model controlling for ARIMA‐defined seasonality. In an alternative model controlling for the summer peak, community‐wide SSB sales decreased by CAD −51/day (95% CI −166 to 65) (approximately USD −39 or EUR −34) during the eight‐month intervention period.
Adverse outcomes: compensatory SSB sales in remaining stores (one ITS study, very low‐certainty evidence)
SSB sales in the two stores which continued selling SSB were assessed to examine switching behaviour, i.e. compensatory SSB purchases in the stores that did not implement the intervention. Minaker 2016 reports that in store 1, SSB sales increased by CAD 3/day (95% CI −93 to 99) (approximately USD 2 or EUR 2), and that in store 2, SSB sales decreased by CAD −17/day (95% CI −54 to 21) (approximately USD −13 or EUR −11) during the eight‐month intervention period.
G. Action across sectors
We included eight studies on action across sectors, including studies on:
G.1 Trade and investment liberalisation in low‐ and middle‐income countries (Baker 2016; Schram 2015);
G.2 Government food benefit programmes with incentives to buy fruit and vegetables and restrictions on SSB purchases (Collins 2016 WIC; Harnack 2016; Olsho 2016);
G.3 Government food benefit programmes without incentives and restrictions (Collins 2016 SNAP; Waehrer 2015);
G.4 Multicomponent community campaigns focused on SSB (Schwartz 2017).
G.1 Trade and investment liberalisation in low‐ and middle‐income countries
Description of studies contributing data to this comparison
We included two controlled ITS studies on trade and investment liberalisation in low‐ and middle‐income countries (Baker 2016; Schram 2015).
Baker 2016 examines the effects of a free‐trade agreement between Peru and the USA ratified in 2006 and enforced from 2009 onwards on SSB and bottled water sales in Peru. The analysis is based on data provided by the market research firm Euromonitor for a 10‐year baseline period (pre‐enforcement) and a four‐year intervention phase (post‐enforcement), both for Peru and Bolivia, which served as a matched comparison country. The study reports results for ITS analyses controlling for underlying trends as well as gross domestic product (GDP) and population growth.
Schram 2015 examines the effects of Vietnam’s accession to the World Trade Organization (WTO) on retail sales of SSB in that country. Vietnam joined the WTO in 2007, and WTO rules applying to the beverage sector were implemented in Vietnam in 2010. The analysis is based on data provided by the market research firm Euromonitor for a 10‐year baseline period (pre‐implementation, 1999 ‐ 2009) and a four‐ year intervention phase (post‐implementation, 2010 ‐ 2013), both for Vietnam and the Philippines, which served as a matched comparison country. The study reports results for ITS analyses controlling for underlying trends as well as GDP and population growth.
SSB sales (two ITS studies, very low‐certainty evidence)
Schram 2015 reports that retail sales of SSB increased by 13 ml/per capita/day (95% CI 10 to 15) and that the annual growth rate of retail sales of SSB manufactured by foreign companies increased by 12 percentage points (95% CI 9 to 16) at four years post‐implementation. Baker 2016 reports that the annual rate of change in volume sales per capita of SSB (called ‘carbonates’ in the study) decreased by −1.4 percentage points (95% CI −2.5 to −0.4) at four years post‐enforcement. The annual rate of change in volume sales per capita of sugar from SSB decreased by −1.0 percentage points (95% CI −1.9 to −0.06) at four years post‐enforcement. The annual rate of change in volume sales per capita of sports and energy drinks increased by 0.3 percentage points (P > 0.05, SE 0.8) at four years post‐enforcement.
Secondary outcomes: bottled water sales
Baker 2016 reports that the annual rate of change in bottled water sales increased by 0.6 percentage points (95% CI −0.01 to 1.3) at four years post‐enforcement.
G.2 Government food benefit programmes with incentives and restrictions
Description of studies contributing data to this comparison
We included three RCTs on government food benefit programmes with incentives for buying fruit and vegetables and restrictions on the purchase of SSB (Collins 2016 WIC; Harnack 2016; Olsho 2016). Collins 2016 WIC and Harnack 2016 compare benefits with incentives and restrictions to no intervention, and Olsho 2016 compares benefits with incentives to benefits without incentives.
Collins 2016 SNAP and Collins 2016 WIC report results of the Summer Electronic Benefit Transfers for Children (SEBTC) project, which examined the effects of monetary transfers to low‐income households with children on children’s food security and nutritional intake. Participating households were randomised to receive USD 60 a month, USD 30 a month, or no benefit during three months in summer, when children do not have access to meals served in schools. The intervention was implemented in 28 intervention sites across the USA, which chose one of two different modes of delivery. In half of the sites, benefits were delivered through Supplemental Nutritional Assistance Program (SNAP) electronic benefit transfer (EBT) cards. The remaining sites used Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) EBT cards for intervention delivery. Benefits delivered through SNAP EBT cards could be used to purchase a wide range of foods and beverages, including SSB. Benefits delivered through WIC EBT cards could be used to purchase only a limited set of healthy foods and beverages specifically selected to meet the nutritional needs of children, excluding SSB. We considered these to be two different interventions and studies, which we labelled Collins 2016 SNAP and Collins 2016 WIC. We present results for Collins 2016 WIC in this section, and results for Collins 2016 SNAP in the section on ‘Government food benefit programmes without incentives and restrictions’. Collins 2016 SNAP included 25,150 participants, and Collins 2016 WIC included 18,207 participants. Participants were households with school‐aged children with incomes below 185% of the national poverty level. Outcomes were assessed with food‐frequency questionnaires at baseline and during the intervention (no exact dates reported). The intervention was implemented during four consecutive years, 2011 to 2014, but data on sugar‐sweetened beverage intake were collected in 2012 and 2013 only.
In Harnack 2016, participants received monetary transfers, designed to be similar to the Supplemental Nutritional Assistance Program (SNAP) food benefit programme in the USA, with restrictions on the purchase of SSB, candy and sweet baked goods as well as incentives for fruit and vegetable purchases equivalent to 30% of the purchasing price of these. Lower‐income adults were randomised to one of four study arms (control, incentives, restrictions, and incentives with restrictions). Data from 265 individuals were included in analyses. Effects on SSB intake was assessed with three unannounced 24‐hour dietary recall telephone interviews at baseline and at three months. Effects on SSB purchases were assessed by collecting grocery receipts at baseline and during a three‐month intervention phase. Purchasing data are reported in French 2017, a secondary publication to Harnack 2016. Participants were low‐income residents of Minneapolis‐St. Paul, Minnesota, USA.
Olsho 2016 reports results of the Healthy Incentives Pilot (HIP) project, in which 55,095 households participating in SNAP were randomly allocated in a 1:6 ratio to the intervention and control groups. Participants in the intervention group received a 30% rebate on fruits and vegetables purchased with SNAP benefits, which was credited to their SNAP EBT accounts and could be spent on any SNAP‐eligible foods and beverages. Participants in the control group continued to receive their normal SNAP benefits without rebates. A random sample of 2784 adult household members were selected for data collection, of which 2009 completed at least one follow‐up assessment and were included in the analyses. Dietary intake data were collected with 24‐hour dietary recall interviews at baseline and at four to six and nine to 11 months follow‐up. All participants were SNAP‐eligible, i.e. had incomes below 130% of the national poverty line, and lived in Hampden County, Massachusetts, USA.
SSB consumption and purchases (three RCTs, moderate‐certainty evidence)
Collins 2016 WIC reports that intake of sugar from SSB decreased by −5 g/day (95% CI −8 to −3) for the comparison of USD 60 versus no USD benefit a month, decreased by −1 g/day (95% CI −3 to 2) for the comparison of USD 60 versus USD 30 benefit a month, and decreased by −5 g/day (95% CI −8 to −2) for the comparison of USD 30 versus no USD benefit a month.
Harnack 2016 reports that at three months SSB intake decreased by −180 ml/day (95% CI −338 to −22) with incentives, by −108 ml/day (95% CI −266 to 50) with restrictions, and by −180 ml/day (95% CI −338 to −22) with incentives and restrictions. Moreover, SSB purchases decreased by USD −0.2/day (95% CI −0.3 to −0.04) with incentives, by USD −0.4/day (95% CI −0.6 to −0.3) with restrictions, and by USD −0.3/day (95% CI −0.5 to −0.2) with incentives and restrictions.
Olsho 2016 reports that energy intake from SSB decreased by −5 kcal/day/person (95% CI −21 to 11), and that sugar intake from SSB decreased by −1 g/day/person (95% CI −5 to 2) at four to nine months. These data were provided to us by the study’s corresponding author.
Adverse outcomes: stigma and alcoholic beverage intake (one RCT, very low to low‐certainty evidence)
Olsho 2017 (a secondary publication to Olsho 2016) reports that “the (…) evaluation found no evidence of increased stigma associated with rebate use. This may be because in most settings [the project] was implemented automatically via electronic cash registers.”
Bartlett 2014 (a secondary publication to Olsho 2016) reports that alcoholic beverage intake increased by 0.08 drinks/day (95% CI 0.01 to 0.15) at four to nine months. Study authors note that this result may have been driven by several outliers in the second follow‐up assessment, who reported more than eight alcoholic drinks in the prior 24 hours.
Secondary outcomes: target group and stakeholder perceptions, programme costs, and share of participants usually drinking non‐fat or low‐fat milk
Olsho 2017 (a secondary publication to Olsho 2016) reports that “participant satisfaction with the program was high, with the great majority indicating they would like to keep participating if [the project] were to continue.” Moreover, the study reports that “[m]ore than a third of HIP participants in the early implementation survey and almost a quarter in the late implementation survey said they had not heard of [the project]. Nearly a third reported that [the project] was hard to understand or that they did not know how [the project] worked, and focus group participants exhibited substantial confusion about rebate mechanics.” In addition, the study reports that "few retailers reported problems during the pilot. The most common problems and questions,which were reported by stores without integrated electronic cash registers, concerned identifying (…) eligible items and identifying customers participating in the pilot who could earn incentives."
Collins 2016 WIC reports that in 2012 (one of the two years in which an economic evaluation of the programme was done), programme costs were USD 184 per child, including USD 62 administrative costs and USD 122 benefit costs. The study reports that administrative costs could be expected to be lower if the programme were to be scaled up and implemented as an ongoing programme.
Bartlett 2014 (a secondary publication to Olsho 2016) reports that “[t]otal costs for implementing [the project], including the incentives earned by (…) participants, were USD 4.4 million. The majority of the costs (55%) were incurred for system design, development, and testing for both EBT and retailer system changes. Retailer recruitment and participant notification and training accounted for an additional 14% of implementation costs. General administrative expenses for management and oversight (…) accounted for 16%. Most of the remaining 10% of costs were incurred in support of the evaluation. Incentive payments to (…) participants over the course of the pilot represented the smallest proportion of total costs ‐ just 6%.”
Collins 2016 WIC reports that the share of participants usually drinking non‐fat or low‐fat milk decreased by −1% (95% CI −4 to 1) for the comparison of USD 60 versus no USD benefit a month, increased by 0.5% (95% CI −1 to 2) for the comparison of USD 60 versus USD 30 benefit a month, and decreased by −2% (95% CI −5 to 1) for the comparison of USD 30 versus no USD benefit a month.
G.3 Government food benefit programmes without incentives and restrictions
Description of studies contributing data to this comparison
We included one RCT (Collins 2016 SNAP) and one CBA study (Waehrer 2015) on government food benefit programmes without incentives and restrictions. Collins 2016 SNAP was part of a larger study described in the section on ‘Government food benefit programmes with incentives and restrictions’.
Waehrer 2015 examines the effects of the changes to the SNAP food benefit programme in the USA mandated by the American Recovery and Reinvestment Act of 2009, which involved an increase in the amount of the average monthly benefit as well as an expansion in the coverage of the benefit programme. The study is based on a repeat cross‐sectional analysis of SSB intake data provided by the National Health and Nutrition Examination Survey (NHANES), a nationally representative health and nutrition survey in the USA. It included all adult NHANES participants who had two days of dietary recall data recorded during the 2007 to 2008 study cycle (providing pre‐intervention data), or during the 2009 to 2010 study cycle (providing post‐intervention data). NHANES participants enrolled in SNAP, as well as participants with incomes less than 150% of the federal poverty level, were considered to be SNAP‐eligible and served as the intervention group, while participants with incomes greater than 150% but less than 250% of the federal poverty level, which were considered ‘nearly SNAP‐eligible’, served as the control group. In total, the study is based on a sample of 2844 participants.
SSB consumption (Collins 2016 snap, moderate‐certainty evidence)
Collins 2016 SNAP reports that intake of sugar from SSB decreased by −0.5 g/day (95% CI −2 to 1) for the comparison of USD 60 versus no USD benefit a month, increased by 1 g/day (95% CI −1 to 3) for the comparison of USD 60 versus USD 30 benefit a month, and decreased by −2 g/day (95% CI −4 to 1) for the comparison of USD 30 versus no USD benefit a month.
SSB consumption (Waehrer 2015, very low‐certainty evidence)
Waehrer 2015 reports that median SSB intake increased by 34 kcal/day (95% CI 7 to 60) at eight months (triple interaction between SNAP, ARRA and a low education indicator, controlling for total energy intake, as reported in Table 8 of the study’s primary report). In an alternative model, not controlling for total energy intake, SSB intake increased by 26 kcal/day (SE 13, P < 0.01).
Secondary outcomes: share of participants usually drinking non‐fat or low‐fat milk, programme costs
Collins 2016 SNAP reports that the share of participants usually drinking non‐fat or low‐fat milk decreased by −0.04% (95% CI −2 to 2) for the comparison of USD 60 versus no USD benefit a month, increased by 0.2% (95% CI −1 to 2) for the comparison of USD 60 versus USD 30 benefit a month, and decreased by −0.2% (95% CI −2 to 2) for the comparison of USD 30 versus no USD benefit a month.
Collins 2016 SNAP reports that in 2012 (one of the two years in which an economic evaluation of the programme was done), programme costs were USD 214 per child, including USD 58 administrative costs and USD 156 benefit costs. The study reports that administrative costs could be expected to be lower if the programme were to be scaled up and implemented as an ongoing programme.
G.4 Multi‐component community campaigns focused on SSB
Description of studies contributing data to this comparison
We included one controlled ITS study on a multicomponent community campaign aiming to reduce SSB intake (Schwartz 2017). This study examines the effects of a three‐year community campaign co‐ordinated by a non‐governmental organisation, which aimed to reduce SSB intake by addressing all levels of the social ecological model. Intervention components included a mass media campaign, an online tool called the Better Beverage Finder, and community outreach. During the campaign, a number of policy changes were introduced, including a state‐wide policy removing SSB from childcare facilities, a local school nutrition policy improving the healthfulness of foods and beverages served in schools, and a policy requiring healthy vending machines in government facilities. The study is based on an analysis of SSB sales data provided by a commercial market research company. Data were collected during a 12‐month baseline period and a three‐year intervention phase, both in 15 supermarkets located in the intervention area and in 17 matched comparison supermarkets located outside the intervention area. Results are based on ITS analyses controlling for weekly temperature and product prices, among others. The intervention was implemented in Howard County, Maryland, USA.
SSB sales (one ITS study, moderate‐certainty evidence)
Schwartz 2017 reports that regular soda sales per product and store decreased by −19.7% in the intervention group and increased by 0.8% in the control group during the three‐year intervention period, equivalent to a net decrease of −1.6 l/day (95% CI −2.0 to −1.2) per product and store. Moreover, Schwartz 2017 reports that beverage sales per product and store decreased by −0.4 l/day (95% CI −1.5 to 0.7) for sports drinks, and by −1.5 l/day (95% CI −2.0 to −0.9) for fruit drinks during the three‐year intervention period.
Secondary outcomes: diet beverage sales
Schwartz 2017 reports that diet beverage sales per product and store decreased by −0.3 l/day (95% CI −0.8 to 0.1) during a three‐year intervention period.
H. Home‐based interventions
We included seven studies on home‐based interventions, including studies on:
H.1 Improved access to low‐calorie beverages in the home environment (Albala 2008; Anand 2007; Ebbeling 2006; Ebbeling 2012; Hernández‐Cordero 2014; Tate 2012);
H.2 Provision of active video gaming equipment to teenagers (Simons 2015).
H.1 Improved access to low‐calorie beverages in the home environment
Description of studies contributing data to this comparison
We included six RCTs on improved access to low‐calorie beverages in the home environment (Albala 2008; Anand 2007; Ebbeling 2006; Ebbeling 2012; Hernández‐Cordero 2014; Tate 2012).
In Albala 2008 participants in the intervention group received weekly home deliveries of flavoured, low‐fat milk without added caloric sweeteners as well as dietary advice on SSB consumption. One serving (200 ml) of milk a day was provided per participant, and this allotment was increased when siblings lived in the same household, or when the allotment was found insufficient based on discussions with the participants’ caretakers. Control participants received no intervention. Participants were children aged eight to 10 years with overweight or obesity and a baseline consumption of at least two servings of SSB a day, living in Soprole, San Bernado, Chile. Data from 93 children were included in analyses. SSB intake was assessed with a food frequency questionnaire, and body weight was assessed by certified clinic personnel, both at baseline and at four months follow‐up.
In Anand 2007 participants in the intervention group received weekly home deliveries of two 18‐litre containers and 24 bottles (size not specified) of drinking water, as well as dietary counselling. Participants in the control group received a nutrition and physical activity guide. Participants were 57 two‐parent families with at least one child, living in an Aboriginal reserve in Ontario, Canada. Baseline body weight and SSB consumption were not inclusion criteria; baseline BMI was 35 kg/m2 in the intervention group and 33 kg/m2 in the control group, and baseline SSB intake was 462 ml/day and 533 ml/day respectively. Data from 159 individuals living in 51 households were included in analyses. Beverage intake was assessed with one 24‐hour dietary recall interview at baseline and at six months.
In Ebbeling 2006 participants in the intervention group received weekly home deliveries of four servings (360 ml each) of non‐caloric beverages a day, as well as dietary counselling focused on beverages. Beverage deliveries included water and diet beverages, and were adapted to participants’ preferences. Control participants received no intervention. Participants were 103 healthy teenagers aged 13 to 18 years with a baseline consumption of at least one serving (360 ml) of SSB a day, living in Boston, Massachusetts, USA. Body weight was not an inclusion criterion, and mean baseline BMI was 26 kg/m2 in the intervention group and 25 kg/m2 in the control group. Beverage intake was assessed with a 24‐hour multiple‐pass dietary recall interview, and body weight was assessed with a standardised protocol, both at baseline and at six months. Sixty‐four per cent of participants were non‐white, and 17% lived in subsidised housing.
In Ebbeling 2012 participants in the intervention group received weekly home deliveries of bottled water and diet beverages (four servings a day for each participant, plus two servings a day for each additional household member, adapted to participants’ preferences), as well as dietary counselling focused on beverages. Control participants received no intervention. Participants were teenagers (mean age 15 years) with overweight or obesity and a baseline consumption of at least one serving (360 ml) of SSB or 100% fruit juice a day, living in Boston, Massachusetts, USA. Data from 217 teenagers were included in analyses. Beverage intake was assessed with a 24‐hour dietary recall interview, and body weight was assessed by a trained dietitian following a standardised protocol, at baseline, after a one‐year intervention phase and after one year of additional follow‐up without intervention. The sample was ethnically and socio‐economically diverse.
In Hernández‐Cordero 2014 participants in the intervention group received bi‐weekly deliveries of two to three litres of bottled water a day, as well as dietary counselling focused on beverages. Participants in the control group received general dietary counselling. Participants were 240 women aged 18 to 44 years with overweight or obesity and a baseline SSB intake of at least 250 kcal/day, living in Cuernavaca, Mexico. Beverage intake was assessed with a 24‐hour dietary recall interview, and body weight was assessed by trained research staff following a standardised protocol, at baseline and at 3, 6 and 9 months. A broad range of occupational and educational groups were represented among the participants.
In Tate 2012 participants in the two intervention groups received either water or diet beverages (four servings of 355 to 500 ml per participant and day, plus two servings for each additional household member, adapted to participants’ preferences), as well as dietary counselling focused on beverages. Beverages were provided to participants at monthly group meetings for transportation to their homes. Participants in the control group received general weight‐loss counselling.
Participants were 318 adults aged 18 to 65 years with overweight or obesity and a baseline consumption of at least 280 kcal/day of caloric beverages, living in the Raleigh‐Durham area in North Carolina, USA. Beverage intake was assessed with a 24‐hour dietary recall interview, and body weight was assessed with a standardised protocol, at baseline and at three and six months. The sample was ethnically and socio‐economically diverse.
SSB consumption (six RCTs, moderate‐certainty evidence)
Our pooled effect estimate, based on data from Albala 2008, Anand 2007, Ebbeling 2006, Ebbeling 2012 and Hernández‐Cordero 2014, is that SSB intake decreased by −413 ml/day (95% CI −684 to −143; 816 participants) at four to 12 months (see Analysis 3.1; Figure 11). Graphical inspection of the forest plot and the I2 statistic (96%) indicate substantial statistical heterogeneity, which may be explained by differences in population, intervention delivery and context.
3.1. Analysis.
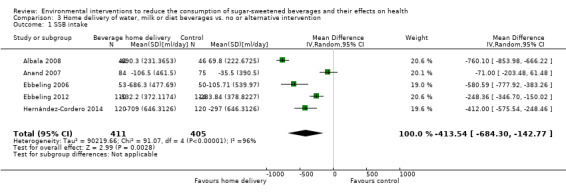
Comparison 3 Home delivery of water, milk or diet beverages vs. no or alternative intervention, Outcome 1 SSB intake.
11.
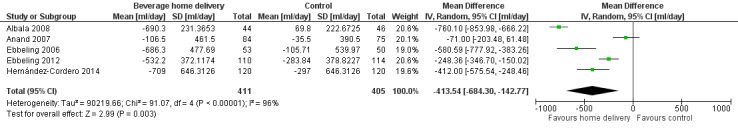
Analysis 3.1: Effects of home delivery of water, milk or diet beverages on SSB intake [ml/day].
Tate 2012 reports that energy intake from beverages decreased by −83 kcal/day (95% CI −125 to −42) at six months in the group receiving bottled water compared to the control group, and by −92 kcal/day (95% CI −133 to −51) in the group receiving diet beverages compared to the control group. Based on these data, we calculated that in the two intervention groups considered together compared to the control group, energy intake from beverages decreased by −88 kcal/day (95% CI −124 to −51) at six months.
(Tate 2012 does not report SSB intake with an outcome measure that could be converted to ml/day, and was therefore not included in Analysis 3.1) . Ebbeling 2012 reports that SSB intake decreased by −248 ml/day (95% CI −347 to −150) at 12 months (this effect estimate is included in the pooled analysis presented above), and by −142 ml/day (95% CI −240 to −44) at 24 months, including 12 months without intervention.
Body weight: comparison of improved access to non‐caloric beverages with no intervention (two RCTs, high‐certainty evidence)
Ebbeling 2006 reports that BMI decreased by −0.14 kg/m2 (95% CI −0.54 to 0.26) at six months in the full sample, and by −0.75 kg/m2 (95% CI −1.43 to −0.07) among participants in the upper baseline‐BMI tertile (BMI ≥ 25.6 kg/m2). Ebbeling 2012 reports that BMI decreased by −0.57 kg/m2 (95% CI −1.12 to −0.01) at 12 months, and by −0.29 kg/m2 (95% CI −1.07 to 0.49) after 12 months of additional follow‐up without intervention.
Body weight: comparison of improved access to non‐caloric beverages with general weight‐loss counselling (two RCTs, low‐certainty evidence)
Hernández‐Cordero 2014 reports that BMI decreased by −0.17 kg/m2 (95% CI −0.6 to 0.2) at nine months. Our pooled effect estimate with data from Hernández‐Cordero 2014 and Tate 2012 is that waist circumference decreased by −0.83 cm (95% CI −3.65 to 1.98; 2 studies; 558 participants; Analysis 3.3) and that body weight decreased by −1.11 kg (95% CI −3.56 to 1.34; 2 studies; 558 participants; Analysis 3.2) at six to nine months. Tate 2012 reports data for participants receiving diet beverages and participants receiving water separately, and finds similar effects for both groups. For our pooled analysis, we used data from both groups, as described in Appendix 11.
3.3. Analysis.
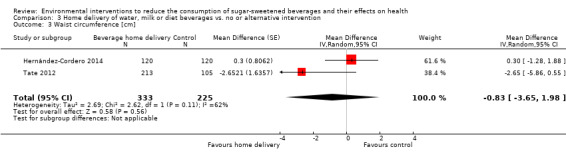
Comparison 3 Home delivery of water, milk or diet beverages vs. no or alternative intervention, Outcome 3 Waist circumference [cm].
3.2. Analysis.
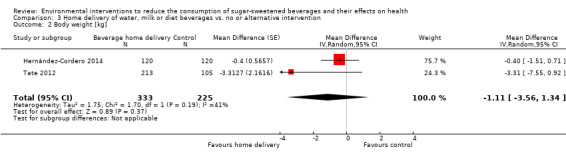
Comparison 3 Home delivery of water, milk or diet beverages vs. no or alternative intervention, Outcome 2 Body weight [kg].
Body weight: comparison of improved access to milk with no intervention (one RCT, moderate‐certainty evidence)
Albala 2008 reports an increase in BMI z‐score by 0.02 (95% CI −0.04 to 0.08), an increase in body weight by 0.44 kg (95% CI −0.28 to 1.16), a decrease in percentage body fat by −0.42 percentage points (95% CI −0.12 to 0.28), a decrease in total fat mass by −0.05 kg (95% CI −0.5 to 0.4), a decrease in trunk fat mass by −0.08 kg (95% CI −0.3 to 0.2), an increase in lean mass by 0.3 kg (95% CI 0.01 to 0.6), an increase in bone mass by 0.01 kg (95% CI −0.02 to 0.04), and an increase in height by 0.1 cm (95% CI −0.2 to 0.5) at 16 weeks follow‐up. These effect estimates were calculated by us based on changes from baseline reported by the study for the intervention and control groups.
Adverse outcomes
Albala 2008, Ebbeling 2006 and Ebbeling 2012 report that no serious adverse effects were observed related to study participation. Hernández‐Cordero 2014 reports that "[t]wenty‐two participants from the [IG] reported an adverse event during the intervention. The most common adverse events reported were tiredness, nausea, stress, or frequent urge to urinate."
Secondary outcomes: intake of alternatives to SSB
Albala 2008 reports that milk intake increased by 428 ml/day (95% CI 348 to 508) and diet beverage intake increased by 275 ml/day (95% CI 174 to 376) at 16 weeks. Anand 2007 reports that water intake increased by 200 ml/day (95% CI 28 to 372) at six months, and Hernández‐Cordero 2014 reports that water intake increased by 971 ml/day (95% CI 703 to 1239) at nine months follow‐up. Ebbeling 2012 reports that diet beverage intake increased by 207 ml/day (95% CI 112 to 303) and unsweetened beverage intake increased by 284 ml/day (95% CI 187 to 381) at 12 months follow‐up. Tate 2012 reports that diet beverage intake in the intervention group receiving home deliveries of diet beverages increased by 669 ml/day (95% CI 650 to 688) compared to the control group at six‐month follow‐up.
Secondary outcomes: metabolic parameters and nutrient intake
Hernández‐Cordero 2014 reports a decrease in fasting plasma glucose by −0.5 mg/dl (95% CI −7 to 6), a decrease in HBA1c by −0.05 % (95% CI −0.13 to 0.03), a decrease in plasma triglycerides by −16 mg/dl (95% CI −44 to 11), an increase in total cholesterol by 5 mg/dl (95% CI −19 to 29), an increase in LDL cholesterol by 5 mg/dl (95% CI −7 to 17), an increase in HDL cholesterol by 2 mg/dl (95% CI −2 to 6), an increase in systolic blood pressure by 2 mmHg (95% CI −2 to 6), an increase in diastolic blood pressure by 0.5 mmHg (95% CI −3 to 4), a decrease in serum osmolality by −1 mOsm/kg (95% CI −10 to 7), and a decrease in urine osmolality by −134 mOsm/kg (95% CI −246 to −22) at nine months. These effect estimates were calculated by us based on changes from baseline reported by the study for the intervention and control groups. Albala 2008 reports an increase in calcium intake by 657 mg/day (95% CI 578 to 737) at 16 weeks.
H.2 Provision of active video‐gaming equipment to teenagers
Description of studies contributing data to this comparison
We included one RCT on the provision of active video‐gaming equipment to teenagers (Simons 2015). Participants in the control group received no intervention. Participants were teenagers aged 12 to 17 years who played at baseline at least two hours non‐active video games a week, living in Amsterdam, Amersfoort, Leiden and Breda, the Netherlands. Data from 262 teenagers were included in analyses. SSB intake was assessed with a questionnaire at baseline and at 1, 4 and 10 months. Sixty‐nine per cent of participants were pursuing higher education, 83% were of Dutch ethnic origin, and 91% were boys.
SSB consumption (one RCT, very low‐certainty evidence)
Simons 2015 reports that the share of participants consuming more than 1400 ml SSB a day decreased (OR 0.71, 95% CI 0.36 to 1.41) at 10 months.
Adverse outcomes
Simons 2015 reports that at 10 months "1/5 of the intervention group reported having experienced an injury (the most frequently mentioned injuries were bruises or strained muscles/tendons) while playing [active] video games."
Secondary outcomes: costs and target group perceptions
Simons 2015 reports that the active video‐gaming equipment used in the study cost approximately EUR 50 per participant. Regarding target group perceptions, Simons 2015 reports that “results also indicate that the current commercially available active video games cannot (yet) truly compete with non‐active video games because the intervention group participants told us that they preferred playing non‐active video games and thought that the active video games were boring.”
Discussion
Summary of main results
Results of the search
We identified 14,488 unique records, and assessed 1030 full texts for eligibility. We found 58 studies meeting our inclusion criteria, including 22 RCTs, 3 NRCTs, 14 CBA studies, and 19 ITS studies, with a total of 1,180,096 participants. The median length of follow‐up was 10 months. The studies included children, teenagers and adults, and were implemented in a variety of settings, including schools, retailing and food service establishments. We judged most studies to be at high or unclear risk of bias in at least one domain, and most studies used non‐randomised designs. The studies examine a broad range of interventions, and we present results for these separately. Effects on direct and indirect measures of SSB intake are summarised in Table 1 and in the effects direction plot shown in Figure 8.
Labelling interventions
We found moderate‐certainty evidence from two ITS studies that traffic‐light labelling in worksite cafeterias and vending machines is associated with decreased SSB sales (Boelsen‐Robinson 2017; Hartigan 2017). We also found low‐certainty evidence from one ITS and one CBA study that nutritional rating score shelf‐labels in supermarkets are associated with decreased SSB sales (Cawley 2015; Hobin 2017). We found low‐certainty evidence from one ITS study that emoticon labelling in school cafeterias is associated with decreased sales of sugar‐sweetened milk (Siegel 2016a). One controlled ITS and two CBA studies examined the effects of menu‐board calorie labelling in chain restaurants and cafés on mean beverage calories per transaction, with variable direction of reported effects (Bollinger 2011; Elbel 2013; Finkelstein 2011). Reported effects on total sales and revenue varied (Boelsen‐Robinson 2017; Bollinger 2011; Cawley 2015; Hartigan 2017; Hobin 2017).
Nutrition standards in public institutions
We found low‐certainty evidence from five CBA studies that reduced availability of SSB in schools is associated with decreased total SSB intake by students (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Cradock 2011; Schwartz 2009; Whatley Blum 2008). We found very low‐ to low‐certainty evidence from one controlled ITS and two CBA studies that reduced availability of SSB in schools may be associated with increased compensatory SSB consumption outside school among high‐school students (Lichtman‐Sadot 2016), but not among elementary‐ and middle‐school children (Huang 2012; Lichtman‐Sadot 2016; Schwartz 2009). Very low‐certainty evidence from one CBA study suggests that reduced availability of SSB in schools does not affect body dissatisfaction or dieting behaviour (Schwartz 2009).
Very low‐certainty evidence from one CBA study and three NRCTs suggests that improved availability of drinking water in schools may be associated with decreased SSB intake of students (Elbel 2015a; Muckelbauer 2009; Van de Gaar 2014; Visscher 2010). Very low‐certainty evidence from one CBA study and two NRCTs suggests that improved availability of drinking water in schools may affect the body weight of students, but the direction of reported effects varied (Muckelbauer 2009; Schwartz 2016; Van de Gaar 2014). We also found very low‐certainty evidence from one CBA study and one NRCT that improved availability of drinking water in schools is associated with decreased total milk intake of students (Elbel 2015a; Schwartz 2016).
We found low‐ to moderate‐certainty evidence from two ITS studies and one RCT that small prizes and token rewards for the selection of plain milk in elementary school cafeterias are associated with decreased selection of sugar‐sweetened milk (Emerson 2017; Hendy 2011; Siegel 2016b). Very low‐certainty evidence from the two ITS studies suggests that total milk selection may be affected, but the direction of reported effects varied (Emerson 2017; Siegel 2016b). Very low‐certainty evidence from one study suggests that the intervention may be associated with an increase in food waste, i.e. in the share of milk selected but not consumed by children (Siegel 2016b).
Low‐certainty evidence from one cluster‐RCT suggests that improved placement of plain milk in school cafeterias is not associated with statistically significant changes in the selection and consumption of sugar‐sweetened and plain milk (Cohen 2015).
We found very low‐certainty evidence from one cluster‐RCT and one CBA study that fruit provision in schools may be associated with decreased SSB consumption by students (Da Costa 2014; Øverby 2012).
Economic tools
We found moderate‐certainty evidence from three ITS studies that price increases for SSBs in chain restaurants, leisure centres and convenience stores are associated with decreasing SSB sales (Blake 2018; Breeze 2018; Cornelsen 2017). Low‐certainty evidence from two ITS studies indicates that price increases for SSBs are associated with decreased total beverage sales and revenue (Blake 2018; Breeze 2018), and one study provides low‐certainty evidence on target group discontent and stakeholder concerns (Blake 2018).
Low‐certainty evidence from three RCTs suggests that financial incentives for the purchase of low‐calorie beverages implemented through supermarket loyalty cards may affect SSB sales, but the direction of reported effects varied (Ball 2015; Franckle 2018; Ni Mhurchu 2010). Low‐certainty evidence from one cluster‐RCT indicates that price discounts on low‐calorie beverages in remote indigenous community stores are associated with increased SSB sales, and increased sales of total energy and sodium (Brimblecombe 2017).
Advertisement and marketing regulation
We did not find any eligible studies on advertisement and marketing regulation.
Whole food supply interventions
Very low‐certainty evidence from two controlled ITS and one CBA study suggests that voluntary industry initiatives to improve the nutritional quality of the whole food supply may affect SSB sales and purchases, but the direction of reported effects varied (Ng 2014a; Ng 2014b; Taillie 2015).
Retail and food service interventions
We found low‐certainty evidence from one ITS study that healthier default beverages in children’s menus in chain restaurants are associated with decreased SSB sales (Peters 2016a). Moderate‐certainty evidence from one cluster‐RCT indicates that in‐store promotion of low‐calorie beverages is associated with decreased SSB sales (Foster 2014).
Very low‐certainty evidence from two NRCTs suggests that improved availability of healthier beverages in worksite and school vending machines may affect SSB intake, but the direction of reported effects varied (Ermetici 2016; French 2010). We found very low‐certainty evidence from one CBA study that urban planning restrictions on new fast‐food restaurants may be associated with decreased SSB intake frequency (Sturm 2015). Very low‐certainty evidence from one ITS study suggests that restrictions in the number of stores selling SSB in remote communities may be associated with decreased community‐wide SSB sales (Minaker 2016).
Action across sectors
Very low‐certainty evidence from two controlled ITS studies suggests that trade and investment liberalisation in low‐ and middle‐income countries may affect SSB sales, but the direction of reported effects varied (Baker 2016; Schram 2015).
We found moderate‐certainty evidence from three RCTs that government food benefit programmes with incentives to purchase fruits and vegetables and restrictions on SSB purchases are associated with decreased SSB consumption and purchases (Collins 2016 WIC; Harnack 2016; Olsho 2016). Very low‐ to low‐certainty evidence from one RCT with three comparisons and one CBA study indicates that government food benefit programmes without incentives and restrictions on specific foods and beverages may affect SSB intake, but the direction of reported effects varied (Collins 2016 SNAP; Waehrer 2015). Low‐certainty evidence from one RCT suggests that incentives to buy fruits and vegetables with government food benefits may not affect stigma, but may be associated with increased alcoholic beverage intake (Olsho 2016).
We found moderate‐certainty evidence from one controlled ITS study that multicomponent community campaigns focused on SSB are associated with decreased SSB sales (Schwartz 2017).
Home‐based interventions
We found moderate‐certainty evidence from six RCTs that improved access to low‐calorie beverages in the home environment is associated with decreased SSB intake (Albala 2008; Anand 2007; Ebbeling 2006; Ebbeling 2012; Hernández‐Cordero 2014; Tate 2012). High‐certainty evidence from two RCTs indicates that improved access to low‐calorie beverages in the home environment is associated with decreased body weight among overweight and obese teenagers with a high baseline consumption of SSB (Ebbeling 2006; Ebbeling 2012). Low‐certainty evidence from two RCTs suggests that improved access to low‐calorie beverages in the home environment combined with dietary counselling focused on beverages may be associated with a larger decrease in body weight among adults than general low‐intensity weight‐loss counselling (Hernández‐Cordero 2014; Tate 2012). Three of these studies report that no serious adverse events occurred (Albala 2008; Ebbeling 2006; Ebbeling 2012), and one study reports adverse events including tiredness, nausea, stress, and frequent urge to urinate among some participants (Hernández‐Cordero 2014).
We found very low‐certainty evidence from one RCT that provision of active video‐gaming equipment to teenagers may be associated with decreased SSB intake, as well as with an increased risk for minor injuries such as bruises and strained muscles and tendons (Simons 2015).
Overall completeness and applicability of evidence
We used an extensive search strategy, and did not exclude studies based on publication status or language. We did, however, conduct searches in English only, and note that 47 of the 58 included studies were conducted in anglophone countries. It is possible that we missed eligible studies published in languages other than English. Moreover, we used database search filters to exclude editorials and case reports from our search in MEDLINE, and to restrict our search in Embase to articles, conference abstracts and reports. Using these search filters is now discouraged by Cochrane, as it can reduce the sensitivity of searches (Cochrane 2018). It is possible that we missed eligible studies as a result.
We included a broad range of different interventions potentially affecting consumption of SSB and its effects on health. However, we did not include studies on taxation of SSB and on behavioural (educational) interventions, as these are covered by existing or ongoing reviews. Furthermore, we did not find any eligible studies on a number of approaches which have been proposed for reducing the consumption of SSB or its effects on health, including the following:
Advertisement and marketing regulations (Hennessy 2015; McDarby 2018; Velazquez 2014).
Portion and package size reductions (Flood 2006; John 2017; Mantzari 2017).
Warning labels (Donnelly 2018; Lee 2018; Roberto 2016; Schillinger 2016; VanEpps 2016).
Reformulation (Luger 2018).
National strategies to improve the quality of the whole food supply (Bryden 2013; Jones 2016).
Upstream interventions targeting the food production system, such as the reduction of subsidies for and the regulation of the production of sugar and other caloric sweeteners (Glickman 2013; Siegel 2016c).
Improved availability and access to healthier beverages in small neighbourhood shops, such as corner stores or bodegas (Dannefer 2012; Nau 2018; Ortega 2016).
We included only studies conducted in real‐world settings (excluding studies conducted in research laboratories and virtual environments), with a combined length of intervention and follow‐up of at least three months and with at least 20 individuals in the intervention and control groups. The studies included in this review cover a broad range of settings, including schools (20 studies), supermarkets and other retailing establishments (12 studies), restaurants (six studies) and participants’ homes (seven studies), among others. Twenty‐three of the included studies were implemented at a policy‐level, i.e. at the level of political jurisdictions such as states or municipalities. This strengthens our confidence that, overall, results are applicable to a variety of real‐world settings, and are scalable to a population level.
For a number of intervention types, however, the evidence in this review is limited to specific settings, specific modes of delivery, or specific populations. Both studies on traffic‐light labelling, for example, were implemented in hospitals (Boelsen‐Robinson 2017; Hartigan 2017). The only study on menu‐board calorie labelling at low risk of bias examined cafés belonging to one chain in New York City (Bollinger 2011). Similarly, all three studies on financial incentives to purchase low‐calorie beverages in supermarkets were implemented through supermarket loyalty cards, which may have influenced effectiveness (Ball 2015; Franckle 2018; Ni Mhurchu 2010). Five of the six studies on improved access to low‐calorie beverages in the home environment included only individuals with overweight and obesity. Results of these studies may not be generalisable to other settings, modes of delivery or populations.
Thirty‐eight of the 58 studies included in our review were conducted in the USA, and for a number of intervention types, all or almost all studies are from the USA, including limits to the availability of SSB in schools (seven out of seven studies), labelling (seven out of eight studies), and whole food supply interventions (three out of three studies). Results may not be generalisable to other countries and world regions.
Only four studies were conducted in low‐ and middle‐income countries, including two studies on trade and investment agreements (Baker 2016; Schram 2015), and one each on improved access to water at home (Hernández‐Cordero 2014) and fruit provision in schools (Da Costa 2014). For the remaining 21 intervention types covered by this review all studies eligible for inclusion were from high‐income countries. Globally, the highest levels of per capita SSB consumption have been reported for middle‐income countries (Singh 2015), where resources to respond to the resulting disease burden are often limited. Research conducted in low‐ and middle‐income countries may be necessary to identify approaches which are viable and effective in such contexts (Ebrahim 2013).
In many countries, SSB consumption is higher among disadvantaged population groups than among the general population (Ogden 2011). The studies in this review provide only limited evidence on the potential moderation of intervention effects by social disadvantage, as discussed in detail in Appendix 14. Interventions may or may not be more or less effective among disadvantaged population groups than among the general population.
Few studies gave systematic consideration to contextual and implementation factors, including barriers to and enablers of implementation. Such information can, however, be important for sustained and scaled‐up implementation. Similarly, only a few studies systematically examined target group and stakeholder perceptions, which can be essential for mobilising and sustaining public and political support. Process evaluations and mixed‐methods approaches, used by several studies in our review, can help to generate evidence on such aspects. In Blake 2018, for example, interviews with store staff and managers revealed that the perception of declining sales, and contractual obligations with suppliers, contributed to the partial discontinuation of the intervention after five months. In Foster 2014, interviews with supermarket employees revealed that implementation fidelity was low, as stocking of beverages was not done by supermarket employees but by suppliers, who were not invested in the intervention. In Boelsen‐Robinson 2017, interviews with stakeholders showed that strong executive support was crucial for sustained implementation.
Only seven studies reported effects on body weight outcomes, and with a few exceptions most studies do not explicitly discuss the possibility of adverse outcomes and unintended consequences. Moreover, many studies used indirect measures for SSB consumption, such as sales data. Sales data may be considered more reliable than self‐reported intake data, which are known to be prone to a number of biases, including social desirability bias and recall bias. However, sales data collected within the specific setting in which interventions are implemented are a proxy for actual consumption, and compensatory consumption of SSB acquired from other sources may occur, as reported by Lichtman‐Sadot 2016 for limits on the availability of SSB in high schools.
We found a number of studies which did not fulfill the inclusion criteria of this review, but which may provide relevant information on how interventions examined in this review can be scaled up. These include, among others, studies on skill‐building interventions targeting school staff, aiming to enable them to change the school environment in order to change behaviours of students (Foster 2010; Haerens 2007; Levy 2012a), as well as similar interventions targeting child‐care centre staff (Jones 2015; Korwanich 2008). We classified these studies as ‘indirect environmental change’ interventions, and list them as such in the Characteristics of excluded studies tables.
Certainty of the evidence
Most of the studies included in our review (39 of 58) used non‐randomised designs, and for most of the intervention types covered by our review (13 of 24) we found only non‐randomised studies. Following GRADE, our initial confidence in the certainty of the effects was therefore low for most intervention types and most outcomes. In addition, most studies, including several of those using randomised designs, were at high or unclear risk of bias in additional domains. Furthermore, we downgraded the level of evidence for imprecision in all cases in which the 95% confidence interval of all or most of the available effect estimates included zero. We downgraded the certainty of the evidence for indirectness in cases in which all or most of the available effect estimates referred to indirect measures of SSB intake, such as calories from beverages per transaction, or energy density of beverages sold.
As detailed in the section on Implications for research in the conclusions, a number of approaches could contribute to lifting the level of evidence to moderate or high certainty for the different intervention types, by reducing risks of bias and by improving precision, consistency and directness. These include the following approaches, among others:
the use of randomised study designs, including cluster‐RCTs, and of relatively more sophisticated non‐randomised study designs, such as controlled ITS studies and designs with synthetic control groups.
reliable, validated data collection methods.
optimal use of existing data sources, including commercial sales and purchasing data.
pre‐registration and other methods for prespecifying key methodological aspects of study conduct.
In addition, there is general concern that the value of some less bias‐prone non‐randomised study designs, such as controlled ITS studies and studies with well‐matched synthetic control groups, may not be appropriately reflected in the assessment of the certainty of evidence with GRADE. Recent developments within the GRADE Working Group may enable a more appropriate assessment of the certainty of evidence delivered through these study designs: all non‐randomised studies can start the GRADE assessment as high, provided sophisticated ‘Risk of bias’ tools matching specific study types are then used to evaluate their risks of bias (Schünemann 2018). So far, ROBINS‐I, a newly developed ‘Risk of bias’ tool, is available to assess the risks of bias in cohort studies (Sterne 2016); similar tools for other study designs are under development (University of Bristol 2018).
Potential biases in the review process
Key steps of the review process, including study selection, data extraction and ‘Risk of bias’ assessment, were duplicated by two review authors working independently, thus reducing the risk for review author bias or error. In conducting our review, we followed our published protocol, which prespecified key methodological aspects, including eligibility criteria and primary and secondary outcomes. We made a number of changes to the review’s methodology after we had published the protocol, and provide details on and the rationale for these changes in the section on Differences between protocol and review.
As explained in the section on Overall completeness and applicability of evidence, we used an extensive search strategy, but conducted searches in English only, and used search filters based on article type. We may have missed eligible studies as a result.
In a number of cases we found it difficult to decide unambiguously if studies met the criteria for inclusion in our review. Criteria which proved difficult to apply in some cases include the criterion that cluster‐RCTs, cluster‐NRCTs and CBA studies must include at least two intervention and two control sites, and the requirement that interventions must include at least one direct environmental intervention component. We provide further details on these issues in the section on Differences between protocol and review. For a number of studies, we could not clearly establish eligibility based on the published reports. In these cases, we contacted study authors, but could not always establish contact or acquire the necessary information.
Reporting bias was a major concern. Most studies included in this review were conducted retrospectively with routinely‐collected data, and do not provide information on trial registration, protocol availability or the prespecification of outcomes and analyses, and do not state explicitly that analyses were conducted as planned and that all important aspects of the study were reported. In such circumstances it is possible that studies which do not show promising (i.e. positive, statistically significant or otherwise interesting results) are aborted early on in the research process, or are not published. We used reporting on primary outcomes as one eligibility criterion for studies, which limits our ability to ascertain the extent of reporting bias. Even when studies are published, reporting of results may be selective. Among the few studies that did report registration, we found reasons to suspect selective outcome reporting in some cases, as detailed in the section on Assessment of risk of bias in included studies.
Following our published protocol, we included studies reporting indirect measures of SSB consumption, including measures that are not specific to SSB, such as beverage calories per transaction (Bollinger 2011; Elbel 2013; Finkelstein 2011) and energy density of beverages sold (Ni Mhurchu 2010). Depending on the context, such outcome measures may be influenced by factors other than SSB purchases or intake, including, among others, the fat content of dairy beverages. Most of these studies showed no effects. It is possible that SSB‐specific outcome measures, if reported, would have shown different effects.
As explained in the section on Overall completeness and applicability of evidence, our inclusion criteria implied a focus on real‐world evidence. While this strengthened the external validity of the findings of our review, it also led to the exclusion of a considerable number of studies conducted in controlled experimental settings, as well as studies on one‐off experiments or with short follow‐up periods. Including such studies may have strengthened the internal validity of the evidence in our review, and may have shifted the overall body of evidence towards increased effectiveness.
We used the EPOC‐adapted Cochrane ‘Risk of bias’ tool to assess risks of bias of individual studies, and GRADE to assess the overall certainty of evidence. When assessed with the Cochrane ‘Risk of bias’ tool, evidence from non‐randomised studies always starts as low‐certainty evidence in GRADE. While there are a number of factors which can justify the upgrading of the level of evidence, methodological strengths of the studies in question are not among them. As a consequence, the strengths of relatively less bias‐prone non‐randomised study designs, such as controlled ITS studies and studies with well‐matched synthetic control groups, may not be appropriately reflected in our assessment of the certainty of evidence with GRADE. At the time when we started to work on this review, the EPOC‐adapted Cochrane ‘Risk of bias’ tool was the recommended ‘Risk of bias’ assessment tool for non‐randomised studies in Cochrane Reviews. In the meantime ROBINS‐I, a more sophisticated tool, has been developed (Schünemann 2018). Using ROBINS‐I may have allowed us to better account for the relative strengths and weaknesses of different non‐randomised study designs, both in the ‘Risk of bias’ assessment of individual studies and in the assessment of the certainty of evidence with GRADE.
Agreements and disagreements with other studies or reviews
In a literature search updated on 25 May 2018 we identified six systematic reviews on interventions to reduce the consumption of SSB, including five that are focused on children and adolescents (Abdel Rahman 2017; Avery 2015; Lane 2016; Vercammen 2018; Vézina‐Im 2017), and one which includes interventions targeting all age groups (Vargas‐Garcia 2017). In addition, we identified seven non‐systematic reviews on interventions to reduce the consumption of SSB (Arsenault 2017; Dooley 2017; Evans 2017; Pomeranz 2012; Scharf 2016; Tipton 2015; Yoshida 2018).
There is substantial variation in the focus, the search strategies, the eligibility criteria and various other methodological aspects used by the six existing systematic reviews and our review. Accordingly, the overlap among the studies included in these reviews is small. Counting the studies included in our review, a total of 180 unique studies are included in the seven reviews, of which 148 studies are included in only one of the seven reviews. Eleven of the 58 studies included in our review are also included in one of the existing systematic reviews, including studies on improved access to low‐calorie beverages in the home environment, as well as studies on reduced availability of SSB and improved access to water in schools. There was no overlap in the remaining 21 intervention types covered by our review.
Most of the 123 studies included in one of the existing reviews but not in our review were on behavioural interventions (77 studies), used ineligible study designs (14 studies), did not meet our criteria for follow‐up (11 studies) or sample size (three studies), did not meet the EPOC criteria for their study design (eight studies), or did not report on any of our primary outcomes (six studies). Details on these studies are provided in the Characteristics of excluded studies tables. We briefly summarise the results of the six existing systematic reviews in the following paragraphs.
Abdel Rahman 2017 included 16 RCTs on behavioural interventions targeting children aged four to 16 years, including 12 school‐based and four home‐ or community‐based interventions. It found a trend towards reduced SSB consumption which approached statistical significance in a meta‐analysis of two school‐based interventions, and reports that this was in line with results reported by six of the remaining school‐based interventions, which could not be meta‐analysed. Of the four home‐ and community‐based studies, two showed statistically significant reductions in SSB intake, while two did not. Meta‐analyses of two studies reporting the prevalence of overweight and obesity and of three studies reporting BMI z‐scores did not show statistically significant effects on body weight. Review authors conclude that behavioural interventions conducted in schools may possibly reduce SSB intake, but may be insufficient to limit excessive weight gain.
Avery 2015 included eight controlled trials targeting children and adolescents aged two to 18 years with a sample size of at least 100 participants and a follow‐up of six months or more. It reports that six of the eight included studies reported statistically significant effects on SSB intake. Moreover, in the three studies providing replacement drinks as well as in three of the five educational interventions, significant effects on body weight were observed. Review authors conclude that schools‐based educational interventions can be effective in reducing SSB intake and body weight, in particular when combined with environmental intervention components.
Lane 2016 included 55 experimental and quasi‐experimental studies on behavioural and environmental interventions targeting children aged three to 18 years. It reports that statistically significant reductions of SSB intake were found in 11 of 21 studies on behavioural interventions, in 14 of 18 studies on environmental interventions, and in 11 of 16 studies combining behavioural and environmental components. Besides intervention effectiveness, the review examines intervention reach, adoption, implementation and maintenance, and finds that reporting on these aspects is poor, limiting their ability to assess the external validity of the findings reported by included studies.
Vargas‐Garcia 2017 included 40 controlled studies on behavioural or environmental interventions reporting effects on SSB or water intake with volumetric measures, such as ml/day. The review conducts meta‐analyses and reports that interventions were effective in reducing SSB intake in children (−76 ml/day, 95% CI −105 to −46, P < 0.01, 23 studies) and in adolescents (−66 ml/day, 95% CI −130 to −2, P = 0.04, 4 studies) but not in adults (−12 ml/day, 95% CI −44 to 18, P = 0.16, 12 studies). It also suggests that modelling and demonstrating the desired behaviour is a successful behaviour change technique for the reduction of SSB consumption, and that interventions in the home environment may be more effective than school‐based interventions.
Vercammen 2018 included 27 randomised and non‐randomised studies on interventions to reduce SSB consumption in children aged 0 to five years that were conducted in high‐income countries and published between 2000 and 2017. Review authors classified 17 of the 27 studies as successful, defined as studies that reported statistically significant decreases in SSB intake for at least one follow‐up assessment and one type of SSB. It concludes that in this age range, preschool and day care may be suitable settings, and that in‐person individual education, changes to the physical access to beverages, and provider training show particular promise as strategies to reduce SSB intake.
Vézina‐Im 2017 included 36 controlled and uncontrolled studies on behavioural and environmental school‐based interventions targeting adolescents aged 12 to 17 years. It reports that statistically significant reductions of SSB intake were found in 13 of 20 studies on behavioural interventions, in nine of 10 studies on environmental interventions, and in four of six studies combining behavioural and environmental components. Review authors conclude that most school‐based interventions are effective in reducing SSB consumption among adolescents, and suggest that environmental interventions may be more effective than behavioural ones.
Overall, the results of the six existing systematic reviews indicate that environmental interventions can contribute to reductions in SSB intake, and are thus in line with the findings of our review.
Authors' conclusions
Implications for practice.
The evidence included in this review shows that effective, scalable interventions exist, addressing sugar‐sweetened beverage (SSB) consumption at a population level. Based on the findings of this review, we tentatively suggest that this may include:
interpretative nutrition labelling, such as traffic‐light and nutritional rating score labelling;
interventions limiting the availability of SSB in schools;
price increases on SSB;
healthier default beverages in children’s menus in chain restaurants;
emoticon labels and small prizes for the selection of healthier beverages in elementary‐school cafeterias;
in‐store promotion of healthier beverages in supermarkets;
government food benefit programmes with incentives to purchase fruits and vegetables and restrictions on purchasing SSB;
multicomponent community campaigns focused on SSB;
and interventions improving access to low‐calorie beverages in the home environment of participants with overweight and obesity and a high baseline consumption of SSB.
Our confidence in the certainty of effects, however, is low to moderate for most of these interventions and in relation to most outcomes, and true effects may be substantially different from those reported in this review. Further approaches to reduce the consumption of SSB exist, and may be effective, but the evidence in this review does not allow clear conclusions about their effects.
Given the uncertainty of the evidence, it is important that the existing evidence base is strengthened. Intervention implementation should therefore be accompanied by evaluations using appropriate study designs and high‐quality study conduct. Practitioners can seek co‐operation with researchers for this purpose. A number of studies included in our review are based on such models, including co‐operations between researchers and public officials (Breeze 2018; Elbel 2015a; Schwartz 2016), civil society (Schwartz 2017) and private businesses (Blake 2018; Bollinger 2011; Cawley 2015; Cornelsen 2017; Foster 2014; Hobin 2017).
When examining the existing evidence, policy‐makers and practitioners should consider that in public health, the effects of interventions in the real world can rarely be established conclusively by conducting trials in controlled research settings (Rutter 2017). Generating meaningful evidence on public health interventions generally requires that policy‐makers and practitioners take action based on limited and imperfect evidence, and implement interventions while ensuring that these are evaluated, and reviewed and adapted once stronger evidence on population‐level effects emerges (Ludwig 2009; Rutter 2017).
A large number and variety of factors are associated with and may potentially influence SSB consumption, and SSBs are consumed on a variety of occasions and in many locations (Mazarello Paes 2015). This implies that there may be no single intervention which, taken alone, is sufficiently effective to lower population‐level SSB consumption to recommended levels. Given the complexity of factors influencing food and beverage consumption, each single approach may have only limited impact, and a variety of approaches, targeting a variety of contextual factors, settings, and population groups may be necessary (Cawley 2016; Rutter 2012; Rutter 2017).
The interventions examined in this review were implemented by a variety of agents, including local, regional and national governments, researchers, civil society organisations, and private enterprises of various sizes and sectors. This underlines that a variety of agencies have a role to play in improving population‐level nutrition and reducing overweight and obesity, and that this objective involves multi‐sectoral, and multi‐level engagement and co‐operation.
Implications for research.
The evidence included in this review was limited in quality, quantity and scope. Regarding quality, reporting bias was a major concern. Most studies in this review did not provide information on trial registration, protocol availability or prespecification of outcomes and analyses. Only one study explicitly states that the study’s published report does not omit any important aspects of the study and that discrepancies from the study as planned were explained (Cornelsen 2017). One further study explicitly states that all analyses were planned a priori and all outcomes which were examined are reported (Harnack 2016). Future studies, including those conducted with routinely‐collected data after the intervention has been implemented, should be prospectively registered, outcomes and analyses should whenever possible be prespecified in publicly‐available protocols, and differences between protocol and study should be made transparent. Declarations like those made by Cornelsen 2017 and Harnack 2016 can further strengthen confidence that results are not biased by selective outcome reporting.
Researchers should strive to make use of study designs that minimise the risks of bias. RCTs may not always be feasible for population‐level health interventions, or may not constitute the best use of available resources. However, a number of alternatives exist that are generally superior to the simple pre‐post comparisons of single data points used in many uncontrolled before‐after studies. This includes interrupted‐time‐series designs controlling for underlying temporal trends, as used by Blake 2018, Boelsen‐Robinson 2017, Breeze 2018 and Cornelsen 2017. Interrupted‐time‐series designs can be strengthened further by the inclusion of control groups, as done by Bollinger 2011 and Lichtman‐Sadot 2016. Another possible approach is the use of synthetic control groups, i.e. of composite control groups selected and re‐weighted to maximise similarity with the intervention group at baseline, as done by the Bauhoff 2014 studies. Further methods which can be used to minimise bias arising from baseline imbalances include selection of units of control based on minimal Euclidian distance, as done by Elbel 2015a and Elbel 2013. Researchers with content‐related expertise in public health and nutrition may need to co‐operate with methodologists, or with researchers from other disciplines, such as economics, to make optimal use of such methods.
Even in studies using strong study designs, bias can arise when unreliable data collection methods are used for outcome assessment. Self‐reported dietary intake data are known to be prone to a variety of biases, in particular when used for the evaluation of interventions in which participants and outcome assessors are not blinded and have interests in the outcome of the assessment. While no method for the assessment of dietary intake is perfect, some methods, such as 24‐hour dietary recall, are generally considered to be more reliable for the assessment of differences in mean intake levels between groups than others, such as food frequency questionnaires (National Cancer Institute 2018). A considerable number of studies in our review use routinely‐collected electronic sales data for outcome assessment, which is objective and therefore less prone to the reporting biases typical of self‐reported data. By contrast, effect estimates based on SSB sales data can be biased when switching behaviour occurs, i.e. when participants switch to alternative sources of SSB in reaction to the intervention. In some cases it may be possible to limit bias due to switching by using commercial sales data sets which cover a large variety of sources of SSB, as done for example by Lichtman‐Sadot 2016 and Huang 2012, or by collecting sales data from all sources of SSB within a given community, as done by Minaker 2016. In some cases it may be feasible to collect both electronic sales data and self‐reported dietary intake data. Researchers should therefore strive to use recommended and validated methods for the assessment of self‐reported dietary intake, and comprehensive electronic sales data for the assessment of SSB sales, or ideally both, to allow for triangulation.
Pilot trials based on interventions implemented in selected settings, and with a small number of participants, may produce results that are internally valid, but which are of limited generalisability. Studies evaluating large‐scale interventions on the basis of small and unrepresentative samples may be prone to sampling bias. In some cases it may be possible to strike a balance between internal and external validity by evaluating large‐scale policy interventions with data from publicly or commercially available data sets that attempt to achieve representativeness at a city, state or national level. This may include commercial sales and purchasing data provided by market research firms, such as the Nielsen Scantrack data used by Ng 2014a and Taillie 2015, the Nielsen Homescan data used by Lichtman‐Sadot 2016, Huang 2012, and Ng 2014b, and the Euromonitor International Passport Global Market Information data used by Baker 2016 and Schram 2015. It may also include population‐level health and nutrition monitoring data, such as the NHANES data used by Cradock 2011, the California Healthy Kids Survey data used by the Bauhoff 2014 studies, and the New York FITNESSGRAM data used by Schwartz 2016. Besides the benefits of larger sample sizes and improved representativeness, some of these data sets, including the NHANES and the Nielsen data, are based on data collection, processing and analysis methods that may be more reliable than the methods used by many studies which collect their own data.
The evidence in this review is also limited in quantity and scope, as detailed in the section on Overall completeness and applicability of evidence. For a number of intervention types, the available evidence is limited to specific settings, populations, and modes of delivery. Most studies were conducted in high‐income countries. We found no studies on a number of potentially relevant intervention types, such as advertisement regulation, portion and package size reduction, and reformulation. Only few studies provide information on barriers to and enablers of implementation, as well as on target group and stakeholder perceptions, which can be important for sustained and scaled‐up implementation. Few studies give systematic consideration to the possibility of adverse outcomes and unintended consequences, and most studies are focused on short‐term outcomes such as SSB consumption rather than body weight.
Further studies should build on the existing evidence base and strengthen it by using better study designs with appropriate sample sizes, more reliable and direct outcome measures and longer follow‐up periods. The evidence base should be expanded with studies on intervention types, settings, populations and modes of delivery not yet covered sufficiently. Future studies should give more systematic consideration to contextual and implementation factors, including target group and stakeholder perceptions, and to the possibility of adverse outcomes and unintended consequences. This includes studies on interventions initiated and implemented by researchers. In addition, as noted in the section on Implications for practice, co‐operation with policy‐makers and practitioners from a variety of sectors can be sought to evaluate real‐world interventions.
Notes
There are no published notes.
Acknowledgements
We would like to acknowledge the substantial and generous contributions made by the members of our Review Advisory Group, who helped to inform the Background section and the parameters of the review at protocol stage. Several members also reviewed the draft review or selected sections thereof. The members of the Review Advisory Group were María Eugenia Bonilla‐Chacín (World Bank), Karen Hofman (University of Witwatersrand, South Africa), Artur Furtado (European Commission), Mark Lawrence (Deakin University, Australia), Cintia Lombardi (Pan American Health Organization), Rebecca Muckelbauer (Charité – Universitätsmedizin Berlin, Germany), Modi Mwatsama (UK Health Forum, United Kingdom), Sohyun Park (U.S. Centers for Disease Control and Prevention, United States), Ludovic Reveiz (Pan American Health Organization), and Marc Suhrcke (University of York, United Kingdom).
We would also like to acknowledge the helpful contributions by the Cochrane Public Health editorial team, including Lorainne Tudor Car (methodologist), Reza Yousefi Nooraie and Ruth Dundas (statistical editors), Patrick Condron and Valerie Wells (search specialists), Kate Cahill (copy editor), Hilary Thomson (sign‐off editor), Jodie Doyle (managing editor) and Solange Durao (contact editor). We are grateful to Qëndresë Daka and Samuel Muli for their assistance with title and abstract screening.
Appendices
Appendix 1. List of abbreviations
| List of Abbreviations | |
| BMI | Body mass index |
| CBA | Controlled before‐after study |
| CDC | U.S. Centers for Disease Control and Prevention |
| CG | Control group |
| CI | Certainty interval |
| CICI | Context and Implementation of Complex Interventions |
| EPOC | Cochrane Effective Practice and Organization of Care |
| GDP | Gross domestic product |
| GRADE | Grading of Recommendations Assessment, Development and Evaluation |
| IG | Intervention group |
| ITS | Interrupted‐time‐series study |
| NNS | Non‐nutritive sweetener |
| NRCT | Non‐randomised controlled trial |
| RCT | Randomised controlled trial |
| RMS | Repeated measures study |
| SSB | Sugar‐sweetened beverage |
| TIDieR | Template for Intervention Description and Replication |
| UBA | Uncontrolled before‐after study |
| USDA | U.S. Department of Agriculture |
| WHO | World Health Organization |
| zBMI | BMI z‐score |
Appendix 2. Review Advisory Group
We formed a Review Advisory Group (RAG), as recommended by Cochrane policies (Cochrane 2011). RAG members were policy advisers, researchers, and civil society representatives with extensive and diverse experience in a number of relevant fields. We sent the protocol and review draft to all RAG members, who provided feedback to ensure the review would meet its intended goal of assessing the effectiveness of SSB interventions in a systematic and comprehensive way, and that the review will appropriately inform policy. The members of our RAG are listed below.
| Members of the Review Advisory Group | |
| Government and International Organizations | |
| Dr. María Eugenia Bonilla‐Chacín | World Bank, Health, Nutrition and Population Global Practice |
| Mr. Artur Furtado | European Commission, Directorate General for Health and Food Safety, Directorate for Public Health, Health Determinants Unit |
| Dr. Cintia Lombardi | Pan American Health Organization/World Health Organization Regional Office for the Americas, Department of Noncommunicable Diseases and Mental Health |
| Dr. Sohyun Park | US Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity |
| Dr. Ludovic Reveiz | Pan American Health Organization/World Health Organization Regional Office for the Americas, Department of Knowledge Translation and Evidence Knowledge Management, Bioethics and Research Office |
| Academia | |
| Prof. Karen Hofman | South Africa Medical Research Council Wits/Agincourt unit, PRICELESS SA, University of Witwatersrand School of Public Health, Johannesburg, South Africa |
| Prof. Mark Lawrence | Deakin University, Institute for Physical Activity and Nutrition, School of Exercise and Nutrition Sciences, Burwood, Australia |
| PD Dr. Rebecca Muckelbauer | Charité ‐ Universitätsmedizin Berlin, Institute for Public Health, Berlin, Germany, and Federal Joint Committee (Healthcare) (Gemeinsamer Bundesausschuss), Berlin, Germany |
| Prof. Marc Suhrcke | University of York, Centre for Health Economics, United Kingdom |
| Civil society | |
| Ms. Modi Mwatsama | UK Health Forum, London, United Kingdom |
Appendix 3. Beverage categories considered in this review
| Beverage categories considered in this review | |||||
| Beverage category | Beverage type | Definition | Examples | Status in our review | Covered by the search strategy |
| Beverages with added caloric sweeteners | Sugar‐sweetened beverages (SSB) | Non‐alcoholic, non‐dairy beverages with added caloric sweeteners | Carbonated and/or caffeinated soft drinks (sodas), fruit juices with less than 100% fruit content and added sugar, sugar‐sweetened energy and sports drinks, sugar‐sweetened vitamin waters and flavoured waters, and sugar‐sweetened coffee and tea | Main intervention target, primary outcome | Yes |
| Sugar‐sweetened milk | Dairy‐based beverages with added caloric sweeteners | Flavoured milk and other dairy drinks (including fortified soy beverages and milk‐based coffee drinks) with added sugar | Additional intervention target, primary outcome | Yes | |
| Low‐calorie alternatives to SSB | Beverages without added sweeteners | Beverages without added sweeteners and recommended by dietary guidelines | Plain water, unsweetened tea and coffee, low‐fat or fat‐free unsweetened milk (including fortified soy beverages), beverages prepared by adding 100% fruit juice to carbonated or uncarbonated water without adding additional caloric sweeteners | Preferred alternative to SSB, secondary outcome | Yes |
| Diet beverages | Beverages sweetened mainly or exclusively with non‐nutritive sweeteners (NNS) | Diet soda, sports drinks, coffe, tea, low‐fat or fat‐free milk and flavoured water, when sweetened mainly or exclusively with NNS | Additional alternative to SSB, secondary outcome | Yes | |
| Other beverages | 100% fruit juice | 100% fruit juice without added sweeteners | ‐ | Secondary outcomes (not the primary focus of this review, but reported if any effects on consumption are discussed in the included studies) | No |
| Full‐fat milk | Full‐fat milk without added sweeteners | ‐ | No | ||
| Alcoholic beverages | Any beverage containing alcohol with or without added sweeteners | ‐ | No | ||
Appendix 4. Logic model
Our logic model, which guided our data extraction, analysis and interpretation, is shown in Figure 19.
12.
Logic model of interventions to reduce the consumption of SSB
Appendix 5. The EPOC algorithm used for the classification of study designs
See Figure 20
13.
Algorithm for the classification of study designs. Reproduced with permission from EPOC 2013a.
Appendix 6. References used for forward and backward citation searches
Appendix 7. Search log of the initial search
We conducted searches on 27 ‐ 28 June 2016.
| Name of database | Search syntax | No. of hits |
| MEDLINE | SeeAppendix 8 | 4547 |
| Embase | SeeAppendix 8 | 4517 |
| CENTRAL | SeeAppendix 8 | 1263 |
| Social Science Citation Index (through Web of Science Core Collection) |
The following search parameters were used: · Topic: (sugar‐sweetened beverage) · Research areas: ( NUTRITION DIETETICS OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH ) · Document types: ( ARTICLE OR ABSTRACT OR OTHER OR CLINICAL TRIAL OR BOOK OR MEETING OR UNSPECIFIED ) · Timespan: All years |
1494 |
| SCOPUS |
The following search parameters were used: · Title, abstract, keywords: sugar‐sweetened beverage · Time: all years to present · Document types: all document types · Subject areas: health sciences , social sciences & humanities |
1397 |
| LILACS (Literatura Latino‐Americana e do Caribe em Ciências da Saúde) | The following search syntax was used (through the Virtual Health Library Regional Portal search interface): (tw:("sugar‐sweetened‐beverages")) OR (tw:("sugar‐sweetened‐beverage")) OR (tw:("soft drink")) OR (tw:("soft drinks")) | 263 |
| SciELO Citation Index (Thomson Reuter regional database for Latin America, Spain, Portugal, the Caribbean and South Africa) | The following search syntax was used (through the Thomson Reuter Web of Science search interface): “TOPIC: (sugar‐sweetened beverages) or TOPIC: (soft drinks)” | 250 |
| Google Scholar | The following search syntax was used: allintitle: ("sugar‐sweetened beverages" OR "sugar‐sweetened beverage" OR "soft drink" OR "soft drinks") AND (trial OR intervention OR RCT OR study) | 161 |
| Open Grey | The following search syntax was used: “sugar‐sweetened beverages” OR “sugar‐sweetened beverage” OR "soft drinks" OR “soft drink” | 70 |
| Trials Register of Promoting Health Interventions (TRoPHI) |
The following search parameters were used: · What type of study does this report describe: trial (non‐randomised) OR RCT · Focus of the report: cardiovascular OR diabetes OR healthy eating OR obesity OR oral health · Type(s) of intervention: environmental modification OR incentives OR legislation OR regulation OR resource access OR service access · Freetext (All but Authors): beverage* OR drink* OR water* |
42 |
| EPPI‐Centre database of health promotion research (Bibliomap) |
The following search parameters were used: · What type of study does this report describe: intervention OR outcome evaluation OR process evaluation OR RCT OR trial · Focus of the report: cardiovascular OR diabetes OR healthy eating OR obesity OR oral health · Type(s) of intervention: environmental modification OR incentives OR legislation OR regulation OR resource access OR service access · Freetext: beverage OR beverages OR drink OR drinks OR water |
11 |
| Cited‐studies search | We used Scopus to search for studies citing previously published systematic and non‐systematic reviews on SSB interventions (n=14) as well as primary studies on SSB interventions identified in our scoping literature search (n=10). | 1337 |
| Reference list hand‐searching | We used Scopus to search for studies cited by previously published systematic and non‐systematic reviews on SSB interventions (n=14) as well as primary studies on SSB interventions identified in our scoping literature search (n=10). | 854 |
| Sum (before de‐duplication) | 16114 | |
| No. of duplicates removed in EndNote | 5644 | |
| No. of duplicates removed in Mendeley | 1065 | |
| Sum (after de‐duplication) | 9395 | |
Appendix 8. Results of the initial search in MEDLINE, Embase and CENTRAL
MEDLINE search strategy and results of the initial search
The search syntax has been developed for use with the Ovid search interface. We conducted the initial search on 27 June 2016 in the database Ovid MEDLINE(R) 1946 to June Week 3 2016.
| Beverage search set (containing terms related to SSB and low‐calorie alternatives to SSB, as well as to nutritive and nonnutritive sweeteners): | ||
| # | Search terms | Results |
| 1 | Carbonated Beverages/ | 2274 |
| 2 | Drinking Water/ | 4255 |
| 3 | Carbonated Water/ | 32 |
| 4 | Energy Drinks/ | 389 |
| 5 | (SSB or SSBs or sugar‐sweetened beverage or sugar‐sweetened beverages or lemonade or lemonades or softdrink or softdrinks).kf. | 153 |
| 6 | (SSB or SSBs or cola or lemonade* or drinking water).ti,ab. | 40739 |
| 7 | ((sugar or sugar‐sweetened or sugarsweetened or sugary or carbonated or caffein* or fizzy or diet* or cal or calorie or caloric or energy or soft or sport* or sweet* or fructose* or sucrose* or corn syrup or HFCS) adj2 (drink* or beverage* or soda or milk)).ti,ab. | 10765 |
| 8 | ((tea or coffee or milk or dairy or water or soda) adj2 (flavour* or flavor* or ice* or sugar* or sweet*)).ti,ab. | 4048 |
| 9 | (soda adj10 (consumption or intake or sales or drink* or beverage* or sugar* or sweet*)).ti,ab. | 538 |
| 10 | ((water or soda) adj2 (fountain* or cooler* or dispenser* or chiller* or bottled or vending or filter*)).ti,ab. | 2143 |
| 11 | Dietary Sucrose/ | 3477 |
| 12 | exp Agents, sweetening/ and (beverage* or drink* or soda*).ti,ab. | 4214 |
| 13 | or/1‐12 | 60954 |
| Intervention search set (containing terms related to intervention types, intervention areas and study designs): | ||
| # | Search terms | Results |
| 14 | Nutrition Policy/ | 7604 |
| 15 | exp School Health Services/ | 20408 |
| 16 | exp Occupational Medicine/ | 23055 |
| 17 | Food Labeling/ | 2802 |
| 18 | Product labelling/ | 2049 |
| 19 | Consumer Health Information/ | 2544 |
| 20 | Health Literacy/ | 2768 |
| 21 | Portion Size/ | 183 |
| 22 | Serving Size/ | 17 |
| 23 | Food Dispensers, Automatic/ | 292 |
| 24 | exp Nutritive Value/ | 12350 |
| 25 | (intervention* or policy or policies or prevention or preventive or school* or lifestyle* or (community adj1 (project or involvement))).ti,ab. | 1304387 |
| 26 | (labelling or labeling or affordability or incentive* or advertisment* or advertising or marketing or (water adj2 (availability or provision))).ti,ab. | 184676 |
| 27 | exp Clinical Studies/ | 295831 |
| 28 | (randomized controlled trial or controlled clinical trial or multicenter study or pragmatic clinical trial).pt. | 641962 |
| 29 | (random* or RCT* or controlled trial* or controlled stud* or controlled design or interrupted time series or "before and after" or "before‐and‐after" or pretest posttest or pretest‐posttest).ti,ab. | 962532 |
| 30 | or/14‐29 | 2714397 |
| Outcome search set (containing terms related to intervention outcomes): | ||
| # | Search terms | Results |
| 31 | ((consumption or intake) adj2 (water or soda or lemonade or SSB or SSBs or sugar‐sweetened beverage*)).ti,ab. | 10000 |
| 32 | Drinking/ | 13079 |
| 33 | exp Overweight/ | 169125 |
| 34 | exp Body Weight Change/ | 57391 |
| 35 | Nutritional Status/ | 34771 |
| 36 | exp Energy Intake/ | 39380 |
| 37 | Food Preferences/ | 11281 |
| 38 | exp Diabetes Mellitus/ | 351858 |
| 39 | (weight* or bodyfat or obes* or overweight* or adiposity or BMI or zBMI or body mass index or skinfold thickness or diabetes or prediabetes or hyperglyc?emia or glucose tolerance or insulin resistance or HBA1c or cardiovascular or hypertension or hyperlipidemia or dyslipidemia or hyperuric?emia or caries or dental decay or dental erosion or ((fat or fatness) adj1 (body or visceral or skin or abdominal))).ti,ab. | 1686986 |
| 40 | or/31‐39 | 1869668 |
| Search set to exclude animal studies and non‐eligible study designs: | ||
| # | Search terms | Results |
| 41 | exp Animals/ not humans/ | 4265395 |
| 42 | exp Veterinary Medicine/ | 23182 |
| 43 | exp Animal Experimentation/ | 7989 |
| 44 | (editorial or case reports or in vitro).pt. | 2187382 |
| Joint search sets: | ||
| # | Search terms | Results |
| 45 | or/41‐44 | 6429115 |
| 46 | 13 and 30 and 40 | 5774 |
| 47 | 46 not 45 | 4547 |
Embase search strategy and results of the initial search
The search syntax has been developed for use with the Ovid search interface. We conducted the initial search on 27 June 2016 in the database Ovid Embase 1974 to 2016 Week 26. Please note that the search terms # 1 ‐ 3 were introduced erroneously into the search string. They have no influence on the results of the search, and can be ignored.
| Beverage search set (containing terms related to SSB and low‐calorie alternatives to SSB, as well as to nutritive and non‐nutritive sweeteners) | ||
| # | Search terms | Results |
| 1 | carbonated beverages/ | 2230 |
| 2 | carbonated water/ | 58 |
| 3 | 1 or 2 | 2286 |
| 4 | carbonated beverage/ | 2628 |
| 5 | carbonated water/ | 58 |
| 6 | drinking water/ | 36371 |
| 7 | energy drink/ | 1015 |
| 8 | sports drink/ | 466 |
| 9 | (SSB or SSBs or sugar‐sweetened beverage or sugar‐sweetened beverages or lemonade or lemonades or softdrink or softdrinks).kw. | 565 |
| 10 | (SSB or SSBs or cola or lemonade* or drinking water).ti,ab. | 57197 |
| 11 | ((sugar or sugar‐sweetened or sugarsweetened or sugary carbonated or caffein* or fizzy or diet* or cal or calorie or caloric or energy or soft or sport* or sweet* or fructose* or sucrose* or corn syrup or HFCS) adj2 (drink* or beverage* or soda or milk)).ti,ab. | 14359 |
| 12 | ((tea or coffee or milk or dairy or water or soda) adj2 (flavour* or flavor* or ice* or sugar* or sweet*)).ti,ab. | 5536 |
| 13 | (soda adj10 (consumption or intake or sales or drink* or beverage* or sugar* or sweet*)).ti,ab. | 790 |
| 14 | ((water or soda) adj2 (fountain* or cooler* or dispenser* or chiller* or bottled or vending or filter*)).ti,ab. | 3202 |
| 15 | ((corn syrup or nonutritive sweetener or nutritive sweetener) and (beverage* or drink* or soda*)).ti,ab. | 207 |
| 16 | or/4‐15 | 88721 |
| Intervention search set (containing terms related to intervention types, intervention areas and study designs) | ||
| # | Search terms | Results |
| 17 | portion size/ | 1181 |
| 18 | nutritional health/ | 5375 |
| 19 | nutrition education/ | 3174 |
| 20 | cariogenic diet/ | 1057 |
| 21 | glycemic load/ | 1051 |
| 22 | glycemic index/ | 3691 |
| 23 | exp school health service/ | 19882 |
| 24 | (intervention* or policy or policies or prevention or preventive or school* or lifestyle* or (community adj1 (intervention or project or involvement))).ti,ab. | 1884249 |
| 25 | (labelling or labeling or affordability or incentive* or advertisment* or advertising* or marketing or (water adj2 (availability or provision))).ti,ab. | 233933 |
| 26 | (random* or RCT* or controlled trial* or controlled stud* or controlled design or interrupted time series or "before and after" or "before‐and‐after" or pretest posttest or pretest‐posttest).ti,ab. | 1408492 |
| 27 | or/17‐26 | 3236230 |
| Outcome search set (containing terms related to intervention outcomes) | ||
| # | Search terms | Results |
| 28 | ((consumption or intake) adj2 (water or soda or lemonade or SSB or SSBs or sugar‐sweetened beverage*)).ti,ab. | 13772 |
| 29 | drinking/ | 18852 |
| 30 | exp obesity/ | 373230 |
| 31 | weight gain/ | 78814 |
| 32 | weight change/ | 9446 |
| 33 | weight control/ | 4770 |
| 34 | weight reduction/ | 126927 |
| 35 | caloric intake/ | 46735 |
| 36 | food preference/ | 11142 |
| 37 | diabetes mellitus/ | 446198 |
| 38 | impaired glucose tolerance/ | 22404 |
| 39 | (weight* or bodyfat or obes* or overweight* or adiposity or BMI or zBMI or body mass index or skinfold thickness or diabetes or prediabetes or hyperglyc?emia or insulin resistance or glucose tolerance or HBA1c or cardiovascular or hypertension or hyperlipidemia or dyslipidemia or hyperuric?emia or caries or dental decay or dental erosion or ((fat or fatness) adj1 (body or visceral or skin or abdominal))).ti,ab. | 2493203 |
| 40 | or/28‐39 | 2753070 |
| Joint search sets | ||
| # | Search terms | Results |
| 41 | 16 and 27 and 40 | 7131 |
| Search set to exclude animal studies and non‐eligible study designs | ||
| # | Search terms | Results |
| 42 | limit 41 to human | 5047 |
| 43 | limit 42 to (article or conference abstract or conference paper or report) | 4517 |
CENTRAL (Cochrane Central Register of Controlled Trials) search strategy and results of the initial search
The search syntax has been developed for use with the Ovid search interface. It uses both the controlled vocabulary of MEDLINE (the Medical Subject Headings, or MeSH terms) and the controlled vocabulary of Embase (the EMTREE thesaurus). We ran the initial search on 27 June 2016 in the database Cochrane Central Register of Controlled Trials (CENTRAL) May 2016.
| Beverage search set (containing terms related to SSB and low‐calorie alternatives to SSB, as well as to nutritive and non‐nutritive sweeteners) | ||
| # | Search terms | Results |
| 1 | Carbonated Beverages/ | 127 |
| 2 | Drinking Water/ | 44 |
| 3 | Carbonated Water/ | 3 |
| 4 | Energy Drinks/ | 37 |
| 5 | (SSB or SSBs or sugar‐sweetened beverage or sugar‐sweetened beverages or lemonade or lemonades or softdrink or softdrinks or carbonated beverage or carbonated water or drinking water or energy drink or sports drink).kw. | 171 |
| 6 | (SSB or SSBs or cola or lemonade* or drinking water).ti,ab. | 562 |
| 7 | ((sugar or sugar‐sweetened or sugarsweetened or sugary carbonated or caffein* or fizzy or diet* or cal or calorie or caloric or energy or soft or sport* or sweet* or fructose* or sucrose* or corn syrup or HFCS) adj2 (drink* or beverage* or soda or milk)).ti,ab. | 1459 |
| 8 | ((tea or coffee or milk or dairy or water or soda) adj2 (flavour* or flavor* or ice* or sugar* or sweet*)).ti,ab. | 441 |
| 9 | (soda adj10 (consumption or intake or sales or drink* or beverage* or sugar* or sweet*)).ti,ab. | 51 |
| 10 | ((water or soda) adj2 (fountain* or cooler* or dispenser* or chiller* or bottled or vending or filter*)).ti,ab. | 103 |
| 11 | Dietary Sucrose/ | 248 |
| 12 | exp Agents, sweetening/ and (beverage* or drink* or soda*).ti,ab. | 422 |
| 13 | or/1‐12 | 2785 |
| Intervention search set (containing terms related to intervention types, intervention areas and study designs) | ||
| # | Search terms | Results |
| 14 | Nutrition Policy/ | 228 |
| 15 | exp School Health Services/ | 1056 |
| 16 | exp Occupational Medicine/ | 63 |
| 17 | Food Labeling/ | 63 |
| 18 | Product labelling/ | 38 |
| 19 | Consumer Health Information/ | 87 |
| 20 | Health Literacy/ | 160 |
| 21 | Portion Size/ | 24 |
| 22 | Serving Size/ | 4 |
| 23 | Food Dispensers, Automatic/ | 6 |
| 24 | exp Nutritive Value/ | 762 |
| 25 | (portion size or nutritional health or nutrition education or cariogenic diet or glycemic load or glycemic index or school health service).kw. | 618 |
| 26 | (labelling or labeling or affordability or incentive* or advertisment* or advertising or marketing or (water adj2 (availability or provision))).ti,ab. | 3402 |
| 27 | (labelling or labeling or affordability or incentive* or advertisment* or advertising or marketing).ti,ab. | 3368 |
| 28 | (randomized controlled trial or controlled clinical trial or multicenter study).pt. | 478600 |
| 29 | (random* or RCT* or controlled trial* or controlled stud* or controlled design or interrupted time series or "before and after" or "before‐and‐after" or pretest posttest or pretest‐posttest).ti,ab. | 495529 |
| 30 | or/14‐29 | 668853 |
| Outcome search set (containing terms related to intervention outcomes) | ||
| # | Search terms | Results |
| 31 | ((consumption or intake) adj2 (water or soda or lemonade or SSB or SSBs or sugar‐sweetened beverage*)).ti,ab. | 505 |
| 32 | Drinking/ | 463 |
| 33 | exp Overweight/ | 8964 |
| 34 | exp Body Weights/ and "Measures"/ | 7 |
| 35 | exp Body Weight Change/ | 5361 |
| 36 | Nutritional Status/ | 1699 |
| 37 | exp Energy Intake/ | 4077 |
| 38 | Food Preferences/ | 568 |
| 39 | exp Diabetes Mellitus/ | 16359 |
| 40 | (drinking or obesity or weight gain or weight change or weight control or weight reduction or caloric intake or food preference or diabetes mellitus or impaired glucose tolerance).kw. | 16760 |
| 41 | (weight* or bodyfat or obes* or overweight* or adiposity or BMI or zBMI or body mass index or skinfold thickness or diabetes or prediabetes or hyperglycemia or insulin resistance or HBA1c or cardiovascular or hypertension or hyperlipidemia or hyperuricemia or caries or dental decay or dental erosion or ((fat or fatness) adj1 (body or visceral or skin or abdominal))).ti,ab. | 130381 |
| 42 | or/31‐41 | 138658 |
| Joint search sets | ||
| # | Search terms | Results |
| 43 | 13 and 30 and 42 | 1263 |
Appendix 9. Search log of the search update
We cnducted searches on 29 January 2018. Note that ScieELO, Google Scholar, Open Grey and Bibliomap were included in our original search, but not in our search update,
Database searches
| Name of database | Search syntax | No. of hits |
| MEDLINE | The search update was conducted in the databases Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R) 1946 to January 24, 2018. We used the same search strategy as for the original search, but restricted the search to studies published since the original search by adding the the filter "limit to yr=2016‐2018". | 1210 |
| Embase | The search update was conducted on January 29, 2018 in the database Embase 1974 to 2018 January 26. We used the same search strategy as for the original search, but restricted the search to studies published since the original search by adding the the filter "limit to yr=2016‐2018". Note that a number of EMTREE search terms were changed on January 1, 2018 (including ‘weight gain’, which was changed to ‘body weight gain’; ‘weight change’, changed to ‘body weight change’; ‘weight control’, changed to ‘body weight control’; ‘weight reduction’, changed to ‘body weight loss’). We did not consider these changes in our search update, and may have missed relevant articles as a result. | 1175 |
| CENTRAL | The search update was conducted on January 29, 2018 in the database Cochrane Central Register of Controlled Trials December 2017. We used the same search strategy as for the original search, but restricted the search to studies published since the original search by adding the the filter "limit to yr=2016‐2018". | 238 |
| Social Science Citation Index (through Web of Science Core Collection) |
The following search parameters were used: · Topic: sugar‐sweetened beverage* · Timespan = 2016 ‐ 2018 |
408 |
| SCOPUS | The following search syntax was used: TITLE‐ABS‐KEY ( sugar‐sweetened AND beverage* ) AND PUBYEAR > 2015 AND ( SUBJAREA ( econ ) OR SUBJAREA ( medi ) OR SUBJAREA ( psyc ) OR SUBJAREA ( soci ) OR SUBJAREA ( dent ) OR SUBJAREA ( heal ) OR SUBJAREA ( mult ) ) AND ( LIMIT‐TO ( DOCTYPE , "ar" ) OR LIMIT‐TO ( DOCTYPE , "re" ) OR LIMIT‐TO ( DOCTYPE , "ip" ) ) | 582 |
| LILACS (Literatura Latino‐Americana e do Caribe em Ciências da Saúde) | The following search syntax was used (through the Virtual Health Library Regional Portal search interface): (tw:(sugar‐sweetened‐beverages)) OR (tw:(sugar‐sweetened‐beverage)) OR (tw:(soft drink)) OR (year_cluster:(soft drinks)) AND (year_cluster:(2016‐2018)) | 13 |
| SciELO Citation Index (Thomson Reuter regional database for Latin America, Spain, Portugal, the Caribbean and South Africa) | Not included in the search update | |
| Google Scholar | Not included in the search update | |
| Open Grey | Not included in the search update | |
| Trials Register of Promoting Health Interventions (TRoPHI) |
The following search parameters were used: · What type of study does this report describe: trial (non‐randomised) OR RCT · Focus of the report: cardiovascular OR diabetes OR healthy eating OR obesity OR oral health · Type(s) of intervention: environmental modification OR incentives OR legislation OR regulation OR resource access OR service access · YEAR: > 2015 |
4 |
| EPPI‐Centre database of health promotion research (Bibliomap) | Not included in the search update | |
| Snowballing Round V (cited‐studies search and reference list hand‐searching) | We used Scopus to search for studies citing and studies cited by previously published reviews on SSB interventions as well as primary studies on SSB interventions identified after August 14, 2016 (the date when snowballing round IV was conducted) (n=44). | 3173 |
| Sum (before de‐duplication) | 6797 | |
| No. of duplicates removed in EndNote | 3416 | |
| Sum (after de‐duplication) | 3378 | |
Trial register searches
For clinicaltrials.gov we used the advanced search interface, and used the search syntax “(sugar‐sweetened beverage) OR SSB OR soda” to run searches in the following fields:
Condition or disease
Other terms
Intervention/treatment
Title/Acronym
Outcome Measure
The search yielded 646 records, which we collated and de‐duplicated in MS Excel. After de‐duplication, 282 unique records remained.
For the International Clinical Trials Registry Platform (ICTRP) we used the advanced search interface, and used the search syntax “sugar‐sweetened beverage OR SSB OR soda” to run searches in the following fields (with synonyms, all recruitment status):
Title
OR Condition
OR Intervention
The search resulted in 171 hits.
Based on the search, we identified two completed studies eligible for inclusion in our review (Collins 2016 SNAP; Collins 2016 WIC), which we found through clinicaltrials.gov. Moreover, we identified 10 ongoing studies which we judged likely to meet our eligibility criteria upon completion. We present details of these in Characteristics of ongoing studies. We found eight of these through our search in clincialtrials.gov, and two through our search in the ICTRP.
We ran trial register searches on 21 June 2018.
Appendix 10. Data extraction form
We developed and used an electronic data extraction form in MS Excel for data extraction, containing the following item.s
General Information:
Study ID
Study title
Supporting documents
Date of extraction
Extractor
-
Publication type:
Journal article (peer reviewed)
Report (grey literature)
Other
If report or other type of publication, please provide details
Copy of the funding, conflict of interest (coi) and/or acknowledgements section
-
Funding source of study:
Public
Private (Industry)
Private (Other)
Other
Potential conflict of interest from funding? (Yes, No, or Unclear; if yes or unclear, please specify)
Other potential conflict of interest (COI)? (Yes, No, or Unclear; if yes or unclear, please specify)
Has the study been registered? (Yes, No, or Unclear; if yes, please specify by providing the trial registry and the trial ID)
Corresponding author and correspondence address
Study eligibility:
-
Intervention:
Are any of the intervention's main components intended to, or potentially suitable to limit the health effects of SSB consumption, or to increase the consumption of low‐calorie alternatives to SSB? (Yes or No)
Definition of SSB used in the study / type of SSB targeted by the intervention
Definition of alternatives to SSB used in the study / type of alternative beverage targeted by the intervention:
Is the intervention an environmental intervention, i.e. is it trying to permanently alter the environment in which individuals make beverage choices? (Yes or No)
Any further relevant comments regarding the eligibility of the intervention
Does the intervention satisfy the inclusion criteria? (Yes or No)
-
Level of implementation:
What was the level of implementation of the intervention? (Policy or Setting‐based intervention)
-
Study design:
What is the design of the study? (RCT, NRCT, CBA, ITS, UBA, or Other; if other, please specify)
In case the study design is a NRCT, CBA or ITS, does it fulfil the EPOC criteria? (Yes, No, or Not applicable)
Comment on adherence to EPOC criteria
Does the study design satisfy the inclusion criteria? (Yes or No)
Any further relevant comments regarding the eligibility of the study design
-
Outcomes:
Does the study assess any of the primary outcomes?
Do the outcomes reported satisfy the inclusion criteria? (Yes or No)
Any further relevant comments regarding the eligibility of the outcome measures
-
Further exclusion criteria:
-
Is any of the following exclusion criteria fulfilled?
The intervention is implemented in a laboratory
The intervention is implemented in a virtual setting
The follow‐up period is fewer than three months (In this review, the follow‐up period is defined as the time span between the start of the intervention and the last outcome assessment)
There are less than 20 individuals in the intervention or control group
The study is a clinical trial on the physiological effects of SSB
Is one or more of the above exclusion criteria fulfilled? (Yes or No)
Any further relevant comments regarding the above mentioned exclusion criteria
-
-
Summary of study eligibility:
Regarding the study design, intervention, outcomes and further exclusion criteria, does the study meet all inclusion criteria? (Yes or No)
Any further relevant comments regarding the study eligibility, including uncertainties or concerns
Timing:
Start of the study (i.e. the date of the baseline assessment)
End of the study (i.e. the date of the last outcome assessment)
Start of the intervention (i.e. the start date of the implementation of the first intervention component)
End of the intervention (i.e. the date when the last intervention component was discontinued; in case the intervention was not discontinued within the study period, enter the last reported date instead)
Duration of the intervention (i.e. the time span from the start of the intervention to the end of the intervention)
Total duration of the follow‐up (i.e. the time span from the start of the intervention to the date of the last outcome assessment)
Was there an additional follow‐up period after the end of the intervention? (I.e. was the total follow‐up period longer than the duration of the intervention?) (Yes or No)
If yes, duration of the additional follow‐up after the end of the intervention
Any other relevant information regarding intervention timing?
Study design:
Unit of randomisation or control (allocation by individuals or clusters/groups)
Unit of analysis
Is the unit of randomisation or control the same as the unit of analysis? (Yes, No, or Unclear)
If yes, was this taken into account in the analysis? (Yes, No, or Unclear)
Details on unit of randomisation, control and analysis issues, and on the way how these were taken into account in the analysis
Total number of persons in all intervention and control groups at baseline (or total number randomised for RCTs)
Number of individuals in each intervention and control group (for cluster trials, include the number of individuals and the number of clusters)
Mode of analysis (Intention‐to‐treat, Per protocol, or Unclear =
Please provide details on the mode of analysis (e.g. on attempts to impute missing data)
Was a subgroup analysis done? (Yes or No; if yes, please provide details)
Is any information on moderators or mediators of effectiveness discussed in the study? (Yes or No; if yes, please provide details)
Was a power calculation done? (Yes or No; if yes, please provide details)
Participants:
-
General Characteristics:
General description of the participants (e.g. school children aged 7‐12 in four schools in Chicago)
Was the intervention targeted at specific age categories? (No, Children, Teenagers, Adults, or Other)
Details on the age of the participants
List of all inclusion and exclusion criteria for study participation (in case of cluster‐randomised studies include details both for clusters and for individuals within clusters)
-
Recruitment:
How were potential participants approached and invited to participate?
Where were participants recruited from?
-
Baseline assessment:
How were baseline differences between study groups assessed?
List any baseline differences found
Was baseline body weight of participants higher than the average of their population? (Yes or No)
Details on the baseline weight status of the participants
Did participants have at baseline any existing medical conditions or physiological risk factors other than overweight or obesity? (Yes or No)
Details on the baseline health status of the participants (Yes or No)
Was the baseline SSB consumption of participants higher than the average of their population?
Details on the baseline SSB consumption of the participants
Representativeness of the sample
-
Equity considerations (PROGRESS‐Plus framework):
Place of residence
Race or ethnicity
Occupation
Gender
Religion
Education
Socio‐economic status
Social capital
Any other information of potential relevance to equity considerations (e.g. disability)
Any other relevant data regarding participant characteristics
Intervention and Comparison:
How many groups were assessed in total?
What was the comparison? (No intervention, Behavioural intervention only, Minimal intervention, or Other)
Further comments on the comparison
If there are several intervention groups, or if the comparison was a minimal, behavioural or alternative intervention, the following section should be copy‐pasted and used for each intervention or active control group.
Intervention:
-
Description of the intervention (TIDieR framework):
BRIEF NAME: The name or phrase that describes the intervention
WHY: The rationale, theory, or goal of the elements essential to the intervention
WHAT (Materials): The physical or informational materials used in the intervention
WHAT (Procedures): The procedures, activities, and/or processes used in the intervention
WHO PROVIDED: The expertise, background and training of intervention providers
HOW: The modes of delivery of the intervention (e.g. face‐to‐face, or by internet or telephone)
WHERE: The type(s) of location(s) where the intervention occurred
WHEN and HOW MUCH: The schedule, duration, intensity or dose of the intervention
TAILORING: Any personalisation, titration or adaption of the intervention to individual participants
MODIFICATIONS: Modification of the intervention during the study
HOW WELL (planned): Strategies for the assessment and maintenance of intervention adherence or fidelity
HOW WELL (actual): Extent of the intervention adherence or fidelity
-
Categorisation of the intervention:
-
What type of intervention was performed? (not applicable for the intervention groups):
Labelling
Limits to the availability of SSB
Improved access to low‐calorie alternatives to SSB
Pricing
Advertisement / marketing
Nutritional content / reformulation
Food system intervention
Other
If other, please specify
-
What type of behavioural co‐intervention (or control intervention) performed?
None
Behavioural co‐intervention (information / awareness‐raising)
Behavioural co‐intervention (nutrition advice and counselling for at‐risk individuals)
Behavioural co‐intervention (skills‐building)
Other
If other, please specify
-
In the following section, information on all primary and secondary outcomes will be extracted. It will be copy‐pasted in case more than one outcome is reported.
Outcomes:
-
Select the outcome that was assessed:
-
Primary outcomes:
Direct and indirect measures of SSB intake (e.g. the amount of SSB consumed or purchased in ml/day/person, energy intake from SSB and total energy intake in kcal/day/person)
Diet‐related anthropometric measures (e.g. BMI, waist circumference, waist‐to‐hip ratio, body weight change, incidence and prevalence of overweight and obesity, body composition or total body fat)
Diet‐related health outcomes other than body weight (e.g. incidence and prevalence of pre‐diabetes and diabetes, insulin resistance, blood lipids and blood pressure, incidence of dental caries and other indicators of oral health)
Any reported adverse outcomes or unintended consequence (e.g. compensatory behaviour, reduced fluid intake and dehydration, reduced intake of essential nutrients, body image changes, unhealthy dietary practices, unhealthy weight control, perceived reduction of freedom of choice and other forms of target group and stakeholder dissatisfaction, negative effects on employment or other adverse economic consequences).
-
Secondary outcomes:
Measure of financial and economic viability and sustainability (e.g. costs, cost‐effectiveness, return on investment, and staff time requirements)
Diet‐ and nutrition‐related psychosocial variable (e.g. perceived dietary self‐efficacy, general self‐efficacy, health‐related and general and quality of life)
Measure for target group and stakeholder perceptions of the intervention (e.g. satisfaction with the intervention, satisfaction with the way the intervention was implemented, support for the continuation of the intervention)
-
Exact description of the outcome
How the outcome was assessed
By whom the outcome was assessed
Has the assessment tool or measurement method been validated? (Yes, No, or Unclear)
Details on the validation of the assessment tool or measurement method
Has the assessment tool or measurement method been used as validated? (Yes, No, or Unclear)
Details on whether the validation of the assessment tool or measurement method has been used as validates
Is the assessment or measurement repeated on the same individuals or redrawn from the population for each time point? (Yes, No, or Unclear)
Description of the time points at which the outcome was measured
Description of the time points at which the outcome was analysed
Description of the statistical method applied
Description of any methods used for adjustment
Number of participants in group and attrition rate
Reasons for attrition, if provided
Baseline, Follow‐up and Post‐intervention means of the intervention group and the control or comparison (Including variance measure and indication of whether measures are adjusted or not, and indication of significant differences were shown)
Effect estimate, if given (e.g. odds ratio, risk ratio, regression coefficients)
Narrative summary of results for this outcome
Adverse outcomes or unintended consequences:
-
Does the study mention whether adverse outcomes or unintended consequences occurred? (This includes adverse or unintended consequences on the broader context, such as employment effects)
Yes (study states explicitly that there were no adverse outcomes)
Yes (study states explicitly that there were adverse outcomes)
No (study does not mention whether adverse outcomes were observed or not)
Details of the statement of adverse outcomes or unintended consequences
Does the study provide any information on how information on possible adverse outcomes was collected? (e.g. through a critical incident reporting system, anonymous feedback options, explicit screening for adverse outcomes in the process evaluation, etc) (Yes, No, or Unclear)
Were any precautions made to avoid adverse outcomes or unintended consequences? (Yes, No, or Unclear)
Any information on adverse outcomes or unintended consequences not captured above
Attribution of outcomes:
-
Does the study provide information on the possibility of attributing specific outcomes to specific intervention components? (e.g. whether some intervention components were more effective than others)
Yes (Attribution is possible)
Yes (Attribution is not possible)
No (No information provided)
Details on attribution of outcomes
Context and implementation (CICI framework)
Context:
Which geographical aspects could influence the intervention, its implementation, its population reach and its effectiveness?
Which epidemiological aspects could influence the intervention, its implementation, its population reach and its effectiveness?
Which socio‐cultural aspects could influence the intervention, its implementation, its population reach and its effectiveness?
Which socio‐economic aspects could influence the intervention, its implementation, its population reach and its effectiveness?
Which political aspects could influence the intervention, its implementation, its population reach and its effectiveness? (This may include policies not assessed in the study but implemented in parallel or in close sequence).
Which legal aspects could influence the intervention, it implementation, its population reach and its effectiveness?
Which ethical aspects could influence the intervention, it implementation, its population reach and its effectiveness?
(Note: Setting aspects, which are also part of the CICI framework, are already captured by the TIDeR framework, and are therefore not duplicated here).
-
Implementation:
Which funding measures and mechanisms are applied and how do these mechanisms and processes enable or limit implementation?
In which policy field was the intervention implemented? (Education, Health care, Consumer protection, Food safety, Media and marketing regulation, or Other)
In which sector was the intervention implemented? (Public sector, Private not‐for‐profit, Private for profit, or Other)
What was the mode of implementation? (Pilot trial by researchers, Voluntary action by private actors other than industry (e.g. non‐governmental organizations, philanthropy), Mandatory government regulation, Industry self‐regulation, Public‐private partnership, or Other)
Was resource‐intensity or cost‐effectiveness of the intervention discussed by the authors? Were resource‐intensity and cost‐effectiveness considerations in the study development?
Was sustainability discussed by the authors? (i.e. whether the intervention is likely to persist after the end of the study period) Was sustainability a consideration in the study development?
Was political viability and sustainability discussed by the authors? (i.e. the ease of political implementation, and the likelihood that the intervention is reversed after the end of the study due to political reasons) Was political viability and sustainability a consideration in the study development?
Were barriers to implementation before and during the intervention discussed by the authors? Were barriers to implementation a consideration in the study development?
Was scalability discussed by the authors? (i.e. whether the intervention is suitable to be implemented on a larger scale) Was scalability a consideration in the study development?
Was generalisability discussed by the authors? (i.e. whether the intervention is suitable to be implemented in other contexts with similar results) Was generalisability a consideration in the study development?
Appendix 11. Choice of statistical model, data, comparison or outcome measures
Following our published protocol, we attempted to extract and report data for the most adjusted models reported by primary studies, and on all comparisons and outcome measures reported by primary studies which fulfilled the inclusion criteria specified in our protocol. The following table provides details on studies reporting multiple models, data sources, comparisons or outcome measures.
| Choice of statistical model, data, comparison or outcome measures |
| Baker 2016 reports results for two statistical models, including one using the date of ratification (2006) as point of intervention and analysis, and one using the date of enforcement (2009) as point of intervention and analysis. For the outcomes of interest to this review results of both models result in similar effect estimates, and we report post‐enforcement analyses, as reported in the abstract of the study’s primary report. We considered the beverage category of 'carbonates' as closest to our definition of SSB. |
| Ball 2015 had four arms (control, price reduction, skills building, and price reduction combinded with skills building). We report data for the comparison control versus price reduction only. |
| Bauhoff 2014 cohort, Bauhoff 2014 crosssectional report two analyses, labelled 'cohort' and 'cross‐sectional' by the study author. Both are CBA analyses by the EPOC definition used in this review. Neither of the two analyses is clearly superior to the other. The data used in the two analyses and the analytical approach differ substantially, which is why we included them as two separate studies. The study reports effects on the share of male and female students consuming more than 0, 1, 2, 3 or 3 servings of SSB per day. Data for the share of male and female students consuming any serving of SSB per day is reported in a format that allowed us to combine the two subgroups, and to derive an effect estimate for student of both sexes. We use this effect estimate as primary outcome measure, which we report in the abstract and the 'Summary of findings' table. |
| Bollinger 2011 reports analyses based on two different datasets, one including all transactions from all participating stores (labelled 'transaction data' by the study authors), and one including only data from customers owning and using a Starbucks loyality card (labelled 'cardholder data'). For the primary outcome of interest to this review ‐ effects on calories from beverages per transaction ‐ we report effects based on the transaction data set, as it is larger and more representative than the cardholder data set. For effects by indicators of social disadvantage we report results from the model using the cardholder data, as it includes additional sociodemographic characteristics of participants. |
| Brimblecombe 2017 had three arms (price discounts, a combination of price discounts and nutrition education, and no intervention). We report data for the comparison price discounts versus no price discounts only. |
| Cohen 2015 reports on two separate interventions: a 'chef intervention', in which schools received a professional chef to improve school meal palatability, and a 'smart café intervention', in which choice architecture techniques were used to increase the consumption of healthier foods and beverages in school cafeterias. We include and report data on the smart café intervention only. |
| Cornelsen 2017 reports effects on two groups of SSB: on‐menu SSB, which were listed on the restaurant menu, and off‐menu SSB, which could be requested by customers but were not listed on the menu. We report effects on both groups of SSB, but follow the study authors in considering effects on on‐menu SSB as the primary outcome for effects on SSB. |
| Ebbeling 2012 reports data for 12 months follow‐up, and for 24 months follow‐up, which includes 12 months without intervention (the intervention ended after 12 months). For primary outcomes we report data for both follow‐up assessments, and for secondary outcomes we report data for the first follow‐up assessment only. In the abstract and 'Summary of findings' table we report data for the first follow‐up assessment. |
| Ermetici 2016 reports data on anthropometric measures. We did not include and do not report these, due to confounding by the non‐beverage‐specific intervention components used in this study. |
| French 2010 reports self‐reported SSB intake data and SSB vending‐machine sales data. For the latter data are available only for follow‐up, but not for baseline. We therefore include and report the self‐reported intake data only. |
| Lichtman‐Sadot 2016reports three statistical models: difference‐in‐difference (DD) analyses based on the comparison of treated versus untreated school districts; DD analyses based on the comparison of treated versus untreated households; and difference‐in‐difference‐in‐difference (DDD) analyses, which make use of both comparisons. We report results for the DDD analyses, as these control for the largest set of possible confounders. |
| For community‐wide SSB sales, Minaker 2016 reports results from two ARIMA models, one controlling for the summer peak in SSB sales and the other controlling for ARIMA‐defined seasonality. Neither of the two models is described as clearly superior to the other, and both models yield similar results. We therefore report results from both models. In the ‘Summary of Findings’ tables, we report the more conservative of the two estimates. |
| Ng 2014a reports two comparisons: a comparison of companies participating in the Healthy Weight Commitment Foundation (HWCF) Pledge with national‐brand companies not participating in the pledge; and a comparison of HWCF companies with private label brands. Study authors note that some private‐label brands covered by the analysis were produced by companies participating in the HWCF Pledge. The comparison with national‐brand companies not participating in the pledge may therefore be the better comparison. We report both comparisons in the review text; in the abstract and the ‘Summary of findings’ tables, however, we report only the comparison with national‐brand companies not participating in the pledge. |
| Schram 2015 reports results for two statistical models, including one using the date of accession (2007) as point of intervention and analysis, and one using the date of implementation (2010) as point of intervention and analysis. For the outcomes of interest to this review, results of both models result in similar effect estimates, and we report post‐implementation analyses, as reported in the abstract of the study’s primary report. |
| For body weight outcomes reported by Schwartz 2016, we used data from the models with student‐level fixed effects, which are described as the more conservative model by the study authors. For beverage outcomes reported by Schwartz 2016, we used data from the models with year fixed effects and school‐level fixed effects, i.e. the most adjusted model. |
| Simons 2015 reports results for two models. We report results for model 2, which adjusted for baseline outcome value, age, sex, ethnicity and adolescent educational level, and was thus the more adjusted model. We also report results for the 10‐months follow‐up. |
| The published reports of Siegel 2016a did not report data in a form that allowed inclusion in our review. We contacted the study's corresponding author, and received the necessary data. Based on the data which we received, we compiled a data set with 11 data points for the pre‐intervention period and 45 data points for the post‐intervention period. We assessed the rate of choclate‐milk consumption (number of milks selected devided by number of students) as the dependent variable of interest. We assumed an impact model showing an immediate negative change at the point of intervention introduction, with the possibility of a positive trend change approaching pre‐intervention levels. In the re‐analysis, we build a segmented linear regression model including the following explanatory variables:
Due to data and information limitations, no additional cofounders were included in the impact model. The model showed a significant level change of −15,7 percentage points (−27.4 to −4,0 percentage points; P = 0.0113; t‐value: −2.625) without a significant trend change following the introduction of the intervention (0.037 percentage points/day (−0.19 to +0.26 pecentage points/day); t‐value: 0.316; P value: 0.75) |
| Sturm 2015 reports two comparisons: South Los Angeles (the intervention area) compared to other parts of Los Angeles City, and South Los Angeles compared to other parts of Los Angeles County. In our review, we report both comparisons. In the 'Summary of findings' tables, we report the comparison between South Los Angeles and other parts of Los Angeles City only, as this seems to be the more closely matched comparison. |
| Taillie 2015 reports two ITS analyses: one which uses the official start date of the intervention (2011) as the point of analysis and one using an earlier date (2007) as the point of analysis. The rationale for this is that while the intervention was announced publicly in 2011, Walmart reports that implementation of some parts of the initiative had already begun in the preceding years. For the outcomes of interest to this review both models yield similar results. We therefore report results for the analyses using the official start date of the intervention as the point of analysis. |
| Tate 2012 reports data for three study arms, including one group which received home deliveries of water, one group which received home deliveries of diet beverages, and one group which received no intervention. For effects on anthropometric outcomes and energy intake from beverages we combined the two intervention groups. For this purpose, we used the RevMan calculator to derive standard deviations from the 95% CI reported in the study; subsequently we used the RevMan calculator to combine the two study arms. For effects on diet beverage intake we report data for the comparison between the comparison group and the group receiving diet beverages. |
| For Van de Gaar 2014, we used data from the parent report, as it is described by the study authors as more reliable than the children report. (Quote: "The parent reported SSB consumption is probably more reliable and is supported by similar findings in the observations.") |
| Waehrer 2015 reports results for two analyses, one using a more educated, and one using a less educated sample of NHANES participants. We report in our review results from the model using the less‐educated sample, as these are described by the study authors as the best approximation of the real effects. (Quote: "To further minimize the effect of compositional changes in SNAP participants, we also estimate the effects of SNAP expansion among those with a high school or lower education. If the less‐educated group of low‐income individuals faces a tighter food budget and is therefore more likely to enroll in SNAP even at the pre‐ARRA benefit levels than those with higher education, the DD estimates for this group should more closely approximate the effect of higher SNAP benefits on dietary outcomes separate from any compositional changes due to expanded participation in the program"). The study reports results for models controlling for total energy intake, and for models not doing so. We report in our review results from both models. In the ‘Summary of findings’ tables, we report results from the models controlling for total energy intake, as these are the ones highlighted by the study authors in the text of the study’s primary report. |
Appendix 12. Conversion factors for unit conversions
To convert effect sizes reported in non‐standard units to SI units we used, whenever possible, conversion factors reported by primary studies , partly in conjunction with standard conversion factors derived from the literature (see tables below). For studies conducted in the USA which did not report specific conversion factors, we assumed a serving size for SSB of 12 oz, based on serving sizes reported in Ebbeling 2006, Ebbeling 2012, Cradock 2011 and Whatley Blum 2008. For studies conducted in Canada we used standard serving sizes reported by the Canadian Food Inspection Agency, namely 355 ml for SSB and 500 ml for water (Canadian Food Inspection Agency 2018). For all other studies we used either specific conversion factors reported by the primary studies or standard conversion factors for SI units (see tables below). To convert teaspoons of sugar to grams of sugar we assumed that 1 teaspoon of sugar equals 4.2 grams of sugar (MSUE 2013).
| Conversion factors derived from primary studies | ||
| Study ID | Conversion factor | Quote from text |
| Cradock 2011 | 1 serving = 12 oz | Quote: "The magnitude of the decline in consumption of sugar‐sweetened beverages after the policy change in Boston Public Schools corresponds to approximately 45 kcals per day, assuming there are 150 kcals per 12‐oz serving" |
| Ebbeling 2006 | 1 serving = 12 oz = 360 ml 1 serving of SSB = 630 kJ = 150 kcal | Quote: "Because each 360‐mL (12‐fl oz) serving of SSB contains 630 kJ (150 kcal), and total SSB consumption was reduced by 82% in the intervention group, we calculate that BMI decreased on average by 0.26 kg/m2 for every serving per day of SSB that was displaced" |
| Ebbeling 2012 | 1 serving = 12 oz | Quote: "We enrolled 224 adolescents (...) who reported consuming at least one serving (12 oz) per day of sugar‐sweetened beverages or 100% fruit juice." |
| Foster 2014 | 1 oz = 29.6 mL | Quote: "Conversion factor: 1 oz = 29.6 mL" |
| Huang 2012 | 1 oz = 29.6 ml | Quote: "In the top panel, we compare soft drink purchases measured in ounces (oz) (1 oz = 0.296 l) of the treatment group in Connecticut and in non‐experimental DMAs, before and after the implementation of the soft drink ban in Connecticut." |
| Muckelbauer 2009 | 1 glass = 200 ml | Quote: "The prevalence of overweight (...), BMI SD scores, and beverage consumption (in glasses per day; 1 glass was defined as 200 mL) self‐reported in 24‐hour recall questionnaires, were determined before (baseline) and after the intervention." |
| Whatley Blum 2008 | 1 serving = 12 oz | Quote: "It is also plausible that baseline consumption of SSB was too low, and therefore the impact of reducing school SSB was minimal. Indeed, only boys consumed more than 1 serving/day (12 oz/d) of SSB." |
| Standard conversion factors | ||
| Unit 1 | Unit 2 | Conversion |
| kJ | kcal | 1 kJ = 0.239006 kcal |
| kcal | kJ | 1 kcal = 4.184 kJ |
| US fluid ounce (oz) | ml | 1 oz = 29.5735 ml |
| ml | US fluid ounce (oz) | 1 ml = 0.033814 oz |
| 1 g of SSB | 1 ml of SSB | 1g of SSB = 0.970874 ml |
| 1 g of milk | 1 ml of milk | 1g of milk = 0.970874 ml |
| 1 g of water | 1 ml of water | 1 g of water = 1 ml |
| 1 g of diet beverages | 1 ml of diet beverages | 1 g of diet beverages = 1 ml |
| 1 half‐pint | 1 ml | 1 half‐pint = 236.588 ml |
| 1 teaspoon sugar | 1 g sugar | 1 teaspoon sugar = 4.2 g sugar |
Appendix 13. Contact with study authors
As specified in our protocol, we contacted the corresponding authors of potentially eligible studies in cases in which missing data on study characteristics or outcome measures precluded study inclusion or limited the use of a study. The table shown below provides details on all such attempts to obtain or clarify data.
In the following cases we included studies in our review, and contacted study authors to obtain additional information:
Studies reporting that no, or no statistically significant effects on direct or indirect measures of SSB intake were observed without reporting exact effect estimates or underlying data (Elbel 2013; Elbel 2015a).
Studies reporting effects on direct and indirect measures of SSB intake in a non‐standard format, e.g. as share of participants consuming more than 0, 1, 2, 3 or 4 servings of SSB per day (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional), as share of participants consuming or purchasing any SSB (Franckle 2018), or as changes to the top five best‐selling beverages (Hua 2017).
Studies reporting that participants, or participating clusters, were allocated randomly to the intervention and control group without providing information on the procedures used for random sequence generation and concealment (Anand 2007; Cohen 2015; Collins 2016 SNAP; Collins 2016 WIC; Ebbeling 2006; Foster 2014; Harnack 2016).
In the following cases we contacted study authors, but did not include studies in our review unless we received sufficient information to justify inclusion:
Studies reporting effects on direct or indirect measures of SSB intake as part of aggregate, non‐beverage specific outcomes, such as unhealthy snack consumption scores, energy intake from foods and beverages considered together, or purchases or consumption of red‐labelled (i.e. unhealthy) foods and beverages considered together (Brunello 2014; Kral 2016, Lawman 2015; Øverby 2012; Safdie 2013; Sturm 2013; Sutherland 2010; Thorndike 2016).
Studies which we could not unambigiously classify as either ITS or UBA studies based on the information provided in the studies’ published reports (Bleich 2014; Butler 2011; Ferguson 2016; Levy 2012a; Peters 2016a).
Studies reporting on interventions which we could not unambigiously classify as either behavioural or environmental, based on the information provided in the studies’ published reports (Carriedo 2013; Sichieri 2013; Van de Gaar 2014).
Studies reporting on interventions for which the information provided in the studies’ published reports did not allow us to unambigiously establish if they entailed direct environmental change as part of the intervention (Gittelsohn 2010a; Gittelsohn 2010b; Gittelsohn 2013).
Studies on interventions targeting SSB which reported data only for alternatives to SSB, but not for SSB (Hendy 2011; Lee‐Kwan 2015; Wolfenden 2015).
Studies for which the information provided in the studies’ published reports did not allow us unambigiously to establish if they met our inclusion criteria for the length of intervention (Patel 2016) or study design (Marcus 2009).
Studies on interventions similar to interventions included in our review which collected but did not report data on direct or indirect measures of SSB intake (Klerman 2014; Olsho 2016).
We also contacted the authors of a number of ITS studies to obtain data for re‐analyses (Jue 2012; Siegel 2016a; Siegel 2016b).
We contacted the corresponding authors of all primary studies, provided them with a list of studies included in this review, and asked if they were aware of additional studies which we might have missed in our search strategy. We also contacted the contact persons of all ongoing studies identified in our searches of trial registers and asked if any other public information besides the register entry, such as a published protocol, a conference abstract, or a working paper with preliminary results, were available.
| Contact with study authors |
| Attempts to obtain or clarify data |
| Anand 2007: We contacted the corresponding author (Sonia Anand) to obtain additional information on the allocation procedure. We received the information that randomisation was performed by a central, automated randomisation service. We therefore judged the study to be at low risk of bias for random sequence generation and concealment. |
| Bauhoff 2014 cohort, Bauhoff 2014 crosssectional: We contacted the corresponding author (Sebastian Bauhoff) to obtain additional data on SSB consumption, as the study reports effects on the share of students consuming more than 0, 1, 2, 3 or 4 servings of SSB a day, but not on the mean intake level in servings/day or a similar measure. We successfully established contact, but have not received the additional data. |
| Bleich 2014: We contacted the corresponding author (Sarah Bleich) to clarify if the study fulfills our criteria for the definition of an ITS study. Based on the information received, as well as on the data reported in the study’s primary report, we classified the study as a uncontrolled before‐after (UBA) study and did not include it in our review. |
| Brunello 2014: We contacted the corresponding author (Maria de Paola) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Butler 2011: We contacted the corresponding author (Rosalind Butler) to clarify if the study fulfills our criteria for the definition of an ITS study. We were unable to establish contact, and based on the data reported in the study’s primary report we classified the study as a UBA study and did not include it in our review. |
| Carriedo 2013: We contacted the corresponding author (Anabelle Bonvecchio Arenas) to clarify the extent to which the intervention included environmental intervention components. We were unable to establish contact, and did not include the study in our review. |
| Cohen 2015: We contacted the corresponding author (Juliana Cohen) to obtain additional information on the allocation procedure. We did not receive an answer to this inquiry, and rated the study's risk of bias as 'unclear' in the domain of random sequence generation and concealment. |
| Collins 2016 SNAP, Collins 2016 WIC: We contacted the corresponding author (Jacob Klerman) to obtain additional information on the allocation procedure. We did not receive an answer to this inquiry, and rated the study's risk of bias as 'unclear' in the domain of random sequence generation and concealment. |
| Ebbeling 2006: We contacted the corresponding author (David Ludwig) to obtain additional information on the allocation procedure. We received the information that a random‐number generator was used to create the allocation sequence, which was concealed until an enrolment list had been obtained from earch participating school. We therefore judged the study to be at low risk of bias for random sequence generation and concealment. |
| Elbel 2013: We contacted the corresponding author (Brian Elbel) to obtain additional data on beverage purchases, as the study reports that no statistically significant effects on calories from beverages per transaction were observed, without showing data. We successfully established contact, but have not received the data. |
| Elbel 2015a: We contacted the corresponding author (Brian Elbel) to obtain additional data on SSB consumption, as the study reports that no statistically significant effects on SSB intake were observedm without showing data. We successfully established contact, but have not received the data. |
| Ferguson 2016: We contacted the corresponding author (Megan Ferguson) to clarify if the study design meets our criteria for an ITS study. We received the information that the study compared data for the same four months in the pre‐ and post‐intervention year, thus adjusting for temporal variation but not for underlying trends. We therefore classified the study as a UBA study, and did not include it in our review. |
| Foster 2014: We contacted the corresponding author (Gary Foster) to obtain additional information on the allocation procedure. We did not receive an answer to this inquiry, and rated the study's risk of bias as 'unclear' in the domain of random sequence generation and concealment. |
| Franckle 2018: We contacted the corresponding author (Rebecca Franckle) to obtain additional data on SSB consumption, as the study reports only the share of participants consuming or purchasing any SSB (assessed and reported separately for each of the three intervention months), but not the mean consumption level or other standard measures of SSB intake. We received data on intake frequencies and effect estimates for the number of red‐labeled beverages purchased per month, which we included in our review. |
| Gittelsohn 2013,Gittelsohn 2010a,Gittelsohn 2010b: We contacted the corresponding author (Joel Gittelsohn) to obtain additional information on intervention delivery and data collection. Based on the information received, as well as on the data reported in the studies’ published reports, we classified the studies as indirect environmental change interventions, and did not include them in our review. |
| Harnack 2016: We contacted the corresponding author (Lisa Harnack) to obtain additional information on the allocation procedure. We successfully established contact and received the information that a random‐number generator was used to create the allocation sequence, and that participants were enrolled and randomised in waves. We therefore judged the study to be at low risk of bias for random sequence generation and concealment. |
| Hendy 2011: We contacted the corresponding author (Helen Hendy) to obtain data on SSB consumption, as the study reports data on healthy beverages (defined by the study as skim milk, 1% or 2% low‐fat white milk, 100% fruit juice, or water), but not on healthy beverages (defined in the study as sugar‐sweetened milk, whole plain milk, soda, and artificial fruit drinks). We successfully established contact and received the information that SSB and sugar‐sweetened milk were among the beverages available to children, that the share of children not consuming any beverage for lunch was negligible (approx. 1%), that close to all children who did not select a healthy beverage selected an unhealthy beverage, and that sugar‐sweetened milk was by far the most popular unhealthy beverage. We therefore included the study being on an intervention targeting sugar‐sweetened milk, and calculated changes in the share of students selecting unhealthy beverages based on the data on healthy beverage selection reported by the study's primary report. We also asked for additional information on the randomisation procedure, which is not described in detail in the study’s published report, and received the answer that participants were listed in alphabetical order and then randomly assigned to the intervention and control groups with a table of random numbers from a statistics textbook, with odd numbers assigned to one group, and even numbers assigned to the other group. We classified the study as being at low risk of bias for random sequence generation and concealment. |
| Hua 2017: We contacted the corresponding author (Jeannette R. Ickovics) to obtain additional data on SSB sales, as the study reports only sales of healthy beverages, and changes to the top five best‐selling beverages, but not mean or total sales or other standard measures of SSB sales. We were unable to establish contact. |
| Jue 2012: We contacted the corresponding author (Jane Jue) to obtain additional data on SSB intake required for an ITS re‐analysis for the three intervention phases considered together. We successfully established contact, but have not received the data. We therefore did not include the study, as our inclusion criterion regarding the minimum length of intervention and follow‐up is not met for the intervention, as reported in the study’s published report. |
| Klerman 2014: We contacted the corresponding author (Jacob Klerman) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Kral 2016: We contacted the corresponding author (Tanja V.E. Kral) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Lawman 2015: We contacted the corresponding author (Hannah G. Lawman) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Lee‐Kwan 2015: We contacted the corresponding author (Seung Hee Lee‐Kwan) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Levy 2012a: We contacted the corresponding author (Douglas Levy) to clarify if the study fulfills our criteria for the definition of an ITS study. Based on the information received, as well as on the data reported in the study’s primary report, we classified the study as a UBA study and did not include it in our review. |
| Marcus 2009: We contacted the corresponding author (Claude Marcus) to obtain additional data on how effects on SSB intake were assessed. We received the information that SSB intake was assessed only at follow‐up and not as baseline, as it was not part of the initial study plan. We therefore did not include the study in our review. |
| Olsho 2016: We contacted the corresponding author (Lauren Olsho) to inquire if SSB outcome data were available. We received the required information, and included the study in our review. |
| Øverby 2012: We contacted the corresponding author (Ellen Tufte Bere) to obtain additional data on SSB intake, as the study reports data only for an aggregate ‘unhealthy snack consumption score’, which includes SSB, candy and potato chips. We received the required data, and included the study in our review. |
| Patel 2016: We contacted the corresponding author (Anisha Patel) to obtain additional data on the timing of data collection and intervention delivery. We successfully established contact and received the information that baseline data collection took place from 27 February 2013 to 14 March 2013 and follow‐up data collection occurred between 9 May 2013 and 20 June 2013. Based on this information and data reported in the study’s published report, we concluded that the timespan between the start of the intervention and the last outcome assessment was less than three months. We therefore did not include the study in our review. |
| Peters 2016a: We contacted the corresponding author (John C Peters) to clarify details about study design and data collection. We received the information that at baseline, no other beverages than SSB were available in the restaurants which implemented the intervention, and that sales data were incomplete for the first three years post‐intervention, but that no information on the reasons for this incompleteness was available. We included the study, but judged it to be at high risk of bias in the domain of missing data, and at unclear risk of bias in the domain of selective outcome reporting. |
| Safdie 2013: We contacted the corresponding author (Juan A Rivera) to inquire if SSB outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Sichieri 2009: We contacted the corresponding author (Rosely Sichieri) to clarify the extent to which the intervention included environmental intervention components. We were unable to establish contact, and did not include the study in our review. |
| Siegel 2016a,Siegel 2016b: We contacted the corresponding author (Robert Siegel) to obtain additional data on sugar‐sweetened milk intake required for an ITS re‐analysis. We successfully established contact and received the required data. |
| Sturm 2013: We contacted the corresponding author (Roland Sturm) to obtain data on beverage purchases, as the study’s published report gives data only for the aggregate categories of healthy/unhealthy foods and beverages, but not for beverages separately. We successfully established contact and received the information that running separate analyses for beverages would require substantial resources, and would not be possible outside a funded project. We therefore did not include the study in our review. |
| Sturm 2015: We contacted the corresponding author (Aiko Hattori) to clarify the interpretation of the SSB outcome data. The study provides numercial values for dietary intake frequencies, but does not specify the time frame to which these refer, and if they refer to items consumed, or consumption occasions. We were unable to establish contact. |
| Sutherland 2010: We contacted the corresponding author (Lisa A Sutherland) to inquire if beverage‐specific outcome data were available. We were unable to establish contact, and did not include the study in our review. |
| Thorndike 2016: We contacted the corresponding author (Douglas Levy) to obtain data on beverage consumption, as the study reports data on foods and beverages considered together only. We successfully established contact and received data on purchases of green‐labelled beverages. In a second email sent at a later time point, we asked if data on purchases of red‐labelled beverages were available, and if the percentage changes reported in the study's published report refer to percent, or to percentage point changes in the share of differently‐labelled beverages. We did not receive an answer to this second inquiry, and did not include the study. |
| Van de Gaar 2014: We contacted the corresponding author (Vivian van de Gaar) to clarify the extent to which the intervention included environmental intervention components. Based on the information received, as well as on the data reported in the study’s published reports, we classified the intervention as an environmental intervention with a behavioural co‐intervention, and included the study in our review. |
| Wolfenden 2015: We contacted the corresponding author (Luke Wolfenden) to obtain data on SSB consumption, as the study reports data on the aggregate category of non‐sugar‐sweetened beverages only. We successfully established contact, but did not receive the data. |
Appendix 14. Subgroup and sensitivity analyses
Subgroup and sensitivity analyses by social disadvantage
Nine studies reported subgroup analyses by social disadvantage. Of these, four report that they did not find statistically significant differences in intervention effects by subgroup (Ball 2015; Ebbeling 2006; Elbel 2013; Van de Gaar 2014); one study reports that the intervention was more effective in socially‐disadvantaged participants (Øverby 2012), and one study reports that it was less effective in such groups (Bollinger 2011). Ebbeling 2012 reports that decreases in BMI reached statistical significance in Hispanic but not in non‐Hispanic participants, and that a significant effect modification according to ethnic group for changes in BMI and body weight was found. However, study authors note that these results must be interpreted cautiously, given the small number of Hispanic participants in this study. Ni Mhurchu 2010 reports that subgroup analyses found variation in effectiveness by ethnicity but not by income or education, but cautions that these may be false‐positive and false‐negative findings. Muckelbauer 2009 reports that SSB intake decreased in participants with foreign‐born parents or grandparents, but not in participants with native‐born parents and grandparents; by contrast, BMI decreased in participants with native‐born parents and grandparents, but not in participants with foreign‐born parents or grandparents.
Thirteen studies were focused on disadvantaged participants. Of these, six reported significant associations with decreases in direct or indirect measures of SSB intake (Collins 2016 WIC; Franckle 2018; Harnack 2016; Siegel 2016a; Siegel 2016b; Van de Gaar 2014), four reported associations with decreases in SSB intake which did not reach statistical significance (Collins 2016 SNAP; Foster 2014; Muckelbauer 2009; Sturm 2015), and two reported increases in SSB intake (Brimblecombe 2017; Waehrer 2015), which reached statistical significance in one study (Waehrer 2015). One study focused on sugar‐sweetened milk reports that no significant effects on sugar‐sweetened milk intake were observed, without showing further results (Cohen 2015). This is broadly consistent with the overall pattern of effects reported in the included studies.
Subgroup and sensitivity analyses by sex or gender
Eight studies report subgroup analyses by sex or gender (Bauhoff 2014 cohort; Bauhoff 2014 crosssectional; Bollinger 2011; Ebbeling 2006; Ermetici 2016; Elbel 2013; Schwartz 2009; Schwartz 2016). Of these, three studies report that no statistically significant differences in effects between female and male participants were observed (Ebbeling 2006; Elbel 2013; Ermetici 2016). Bauhoff 2014 cohort and Bauhoff 2014 crosssectional report that SSB intake decreased significantly at the upper end of the SSB intake distribution for female students, and at the lower end of the SSB intake distribution for male students. Bollinger 2011 reports that calories from foods and beverages per transaction decreased significantly more in female than in male participants (calories from beverages only are not reported separately by gender). Schwartz 2009 reports subgroup analyses by gender only for one of its outcomes – body dissatisfaction and dieting behaviour – and reports that effects did not differ significantly by gender. Schwartz 2016 reports that when using a coservative estimation strategy, effects on z‐BMI and prevalence of overweight reached statistical significance in boys but not in girls, and that observed effects were larger for boys than for girls for all body weight outcomes and in all statistical models.
Four studies included only or predominately female participants, of which two reported statistically significant effects on direct or indirect measures of SSB intake (Franckle 2018; Hernández‐Cordero 2014), while two did not (Ball 2015; Ni Mhurchu 2010). Two studies included mainly male participants, and one found an increase in SSB consumption (French 2010) while the other found a decrease (Simons 2015), which did not reach statistical significance.
Data and analyses
Comparison 1. Reduced availability of SSB at school vs. no or minimal intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Share of female students consuming SSB | 2 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 1.1 Share of female students consuming > 0 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Share of female students consuming > 1 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Share of female students consuming > 2 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Share of female students consuming > 3 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Share of female students consuming > 4 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Share of male students consuming SSB | 2 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 2.1 Share of male students consuming > 0 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Share of male students consuming > 1 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Share of male students consuming > 2 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Share of male students consuming > 3 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Share of male students consuming > 4 servings SSB/day | 2 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 SSB purchases outside school by households with school‐aged children [ml/day] | 2 | Mean Difference (Random, 95% CI) | Totals not selected | |
| 3.1 All school types | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 High schools | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Middle schools | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Elementary schools | 1 | Mean Difference (Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Price increase on SSB vs. no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Units of SSB sold [% change] | 3 | Mean Difference (Random, 95% CI) | ‐19.22 [‐32.54, ‐5.90] | |
| 1.1 Price increase of 3‐4%, 6 months follow‐up | 1 | Mean Difference (Random, 95% CI) | ‐9.34 [‐15.21, ‐3.47] | |
| 1.2 Price increase of 10‐25%, 4 to 12 months follow‐up | 2 | Mean Difference (Random, 95% CI) | ‐24.74 [‐28.89, ‐20.59] |
Comparison 3. Home delivery of water, milk or diet beverages vs. no or alternative intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SSB intake | 5 | 816 | Mean Difference (IV, Random, 95% CI) | ‐413.54 [‐684.30, ‐142.77] |
| 2 Body weight [kg] | 2 | 558 | Mean Difference (Random, 95% CI) | ‐1.11 [‐3.56, 1.34] |
| 3 Waist circumference [cm] | 2 | 558 | Mean Difference (Random, 95% CI) | ‐0.83 [‐3.65, 1.98] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Albala 2008.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 93 Length of intervention: 16 weeks |
|
| Participants |
General description of participants: Healthy, overweight and obese children living in Soprole, San Bernardo, Chile Age: Children (aged 8 ‐ 10 years, prepubertal) Inclusion criteria: "BMI greater than the 85th percentile for sex and age; Prepubertal (ie, Tanner Stage 1); Reported consuming at least 2 servings/day of SSBs" Exclusion criteria: "Serious underlying medical condition; Lactose intolerance; Allergy to milk protein" Recruitment: "We enrolled 98 children (...) with the assistance of teachers and staff at 2 schools" Weight status at baseline: Overweight and obese (BMI > the 85th percentile for sex and age was an inclusion criterion. At baseline, mean BMI was 22.5 in the intervention and 22.3 in the control group; mean baseline BMI z score was 1.74 in the intervention group, and 1.64 in the control group) SSB consumption at baseline: Consumption of at least 2 servings/day of SSBs was an inclusion criterion; at baseline, mean SSB consumption was 742 g/day in the intervention group, and 802 g/day in the control group Equity considerations: N/R |
|
| Interventions |
Intervention: Home delivery of low‐fat, flavoured, unsweetened or minimally sweetened milk beverages (Quote: "A nutritionist visited the homes of children in the intervention group weekly to deliver the milk beverages (…). We selected flavored milk beverages to increase the likelihood that children would consume what was delivered to them. Each individually packaged portion (200 mL, approx. 200 g) provided 80 kcal, 8 g protein, 3 g fat, 11 g carbohydrate, and 320 mg Ca. (…) To avoid competition between the subject and siblings for the milk beverages, the number of portions delivered to each home was based on household size. We provided 1 serving/d for each sibling in the household and offered additional servings if this allotment was not adequate on the basis of discussions with the mother") Behavioural co‐intervention: Dietary counselling (Quote: "A nutritionist visited the homes of children in the intervention group weekly to (…) provide instructions to the family about consuming the delivered beverages, and encourage parents to remove SSBs from their homes. (…) Children were counseled to drink 3 portions per day of the milk beverages and not to consume SSBs; no additional nutrition education regarding other foods or beverages was provided. Moreover, they were encouraged to take the milk beverages to school for consumption during lunch. (…) All members of each household were encouraged to support the subject by not drinking SSBs") Control: No intervention (Quote: "We gave no instructions regarding food or beverage choices to subjects in the control group and had no contact with them, other than to conduct assessments") |
|
| Outcomes |
Measures of SSB intake: SSB intake (g/d), assessed with a food‐frequency questionnaire at baseline and 16 weeks Measures of intake of alternatives to SSB: Milk and diet beverage intake (g/d), assessed with a food‐frequency questionnaire at baseline and 16 weeks Anthropometric measures: Weight, height, BMI, BMI z score, percentage body fat, total fat mass, trunk fat mass, lean mass, bone mass, assessed by certified clinic personnel at baseline and 16 weeks Adverse outcomes: The study does not report how data on adverse outcomes were collected, but states that none were observed Other outcomes: Total energy intake (kcal/d), protein intake (g/day), calcium intake (mg/d), assessed with a food‐frequency questionnaire at baseline and 16 weeks |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: Chile Year(s) when implemented: 2004 ‐ 2005 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "DSL is the author of a book on childhood obesity (Ending the Food Fight: Guide Your Child to a Healthy Weight in a Fast Food/Fake Food World). None of the other authors reported any conflicts of interest" Funding: "Supported by grant TW006818 from the Fogarty International Center, National Institutes of Health" Trial registration: ClinicalTrials.gov number NCT00149695 Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study statistician randomly assigned each eligible child to the intervention or control group using a computer‐generated set of random numbers. Random assignment was stratified by height‐for‐age z score" |
| Allocation concealment (selection bias) | Low risk | Quote: "The sequence of random numbers was concealed from personnel conducting recruitment until after the group assignment" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | No significant differences in anthropometric measures were found at baseline. Diet beverage intake was significantly different between study groups at baseline, and SSBs were borderline significantly different; however, this was taken into account in the analysis. Quote: "Multiple linear regression was used to analyze change scores for study outcomes. We included group as an indicator independent variable, age and sex as obligatory covariates, and a group x sex interaction term in the analytic model" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Study groups were similar across all baseline characteristics which were assessed. However, only a limited number of characteristics besides the outcome measurements were assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The retention rate was high and an intention‐to‐treat analysis was performed. Quote: "According to the intention‐to‐treat principle, we included data from the 93 subjects who completed follow‐up assessments irrespective of compliance with study protocols during the intervention period. Of the 48 children who were randomly assigned to the control group, 1 girl developed type 2 diabetes mellitus and was dismissed from the study, and another girl was lost to follow‐up" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Outcome data on beverage consumption was self‐reported, and participants were not blinded |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but anthropometric measurements were assessed by certified clinic personnel who were masked to group assignment |
| Contamination (performance bias) | Low risk | Interaction between participants in the IG and CG cannot be ruled out, as they were recruited from the same schools. However, it is unlikely that the control group received the intervention, i.e. beverage deliveries |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in the Methods section are reported in the Results section, and no important outcomes one would expect in such a study are missing. However, the clinical trial registry mentions three secondary outcomes which are not mentioned in the published report (blood glucose, blood insulin and serum lipids) |
| Other bias | Low risk | No other concerns |
Anand 2007.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 51 households Number of individuals: 159 Length of intervention: 6 months |
|
| Participants |
General description of participants: 2‐parent families with at least 1 child living in an Aboriginal reserve in Ontario, Canada Age: All ages Inclusion criteria: "Eligible households on the Six Nations Reserve had to be comprised of a male and/or female parent with at least one child living in the same household, and all individuals between 5 and 70 years of age (including grandparents) were eligible." Exclusion criteria: "Households were excluded if they: a) were not willing to have the health counsellor visit their homes, b) had a planned absence from the Reservation for >1 month during the intervention, or c) had a planned break‐up of the household in the coming year. Individual exclusion criteria are listed elsewhere [Reference to a webpage which could not be located]" Recruitment: N/R Weight status at baseline: Body weight was not an inclusion criterion; the mean baseline BMI of the adults participants was 35 in the intervention and 33 in the control group SSB consumption at baseline: Baseline SSB consumption was not an inclusion criterion; baseline SSB and juice consumption was 1.3 servings/day in the intervention and 1.5 servings/day in the control group Equity considerations: "The Six Nations people may be disproportionately affected by obesity because of their rapid change from a physically active to a relatively sedentary lifestyle, as well as their dietary transition from lower energy non‐processed to energy‐dense processed foods, all of which is compounded by the relatively low socio‐economic status of this community" |
|
| Interventions |
Intervention: Home delivery of water (The intervention included "two 18 L containers of filtered spring water, and 24 bottles of spring water provided to intervention households/week") Behavioural co‐intervention: Dietary counselling (The intervention included "a regular home visit by Aboriginal health counsellors who were trained to assess and set dietary and physical activity goals for each household member") Control: Minimal intervention (Quote: "Usual care families received Canada’s Food Guide to Healthy Eating and Canada’s Physical Activity Guide to Healthy Active Living") |
|
| Outcomes |
Measures of SSB intake: Servings of SSB ("soda pop and juice") per day, assessed through 1 x 24‐hour dietary recall at baseline and 6 months Measures of intake of alternatives to SSB: Servings of bottled or distilled water per day, assessed through 1 x 24‐hour dietary recall at baseline and 6 months Anthropometric measures: Assessed in the study but not included in our review, due to confounding by non‐beverage‐specific intervention components Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: Canada Year(s) when implemented: 2005 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "Canadian Institutes of Health Research (CIHR) Grant number: MCT 64076" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study's published report does not provide details on the methods used for randomisation, but the study's statistician provided us with the information that randomisation was performed by a central, automated randomisation service |
| Allocation concealment (selection bias) | Low risk | See explanation above |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline differences in the outcomes of interest to us (beverages) were small and were taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Differences in baseline characteristics of household seem to be small (see table 2 of the study's primary report) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Results are based on a per‐protocol analysis, but attrition was low (< 10%) and similar in the intervention and control group. Quote: "[O]utliers total kcals <200 or >10,000 and those missing baseline or 6‐month data were excluded" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Blinding was not possible, and the outcomes of interest to us were self‐reported |
| Contamination (performance bias) | Low risk | Neighbours could have spread the word about the intervention, but it seems unlikely that the control group received the intervention (home delivery of beverages) |
| Selective reporting (reporting bias) | Low risk | There was a study protocol (not published), and the outcomes reported correspond with the outcomes in the Methods section, and the Methods section clearly distinguishes primary and secondary outcomes |
| Other bias | Low risk | No other concerns |
Baker 2016.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: Quote: "A natural experiment study design was adopted since the intervention (ratification of a US‐FTA) is not amenable to experimental manipulation, and it was possible to compare an intervention country (one that had ratified a US‐FTA) and a control country (one that had not). The control country was matched to the intervention country against economic, demographic and trade indicators reported in the literature to effect soft drink consumption, including population and income growth (…). We also wanted to include a TPP country in the analysis to demonstrate what has previously happened in the country as a consequence of trade liberalization, thereby providing a richer understanding of the context in which the TPP will operate. Against these criteria Peru was selected as the intervention country and Bolivia as the control country" Number of clusters or sites: 2 countries Number of individuals: Peru (the intervention country) had, in 2013, a population of 30 million. Bolivia, the control country, had a population of 10 million Length of intervention: 4 ‐ 6 years (from enforcement and ratification onwards, respectively) |
|
| Participants |
General description of participants: Inhabitants of Peru Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: Quote: "Obesity is a pressing public health concern in Peru and Bolivia where rates of adult obesity are high, 15.7 and 17.9 % respectively" SSB consumption at baseline: Baseline (2006) SSB consumption was approx. 50 l/capita/year in Peru (the IG) and 45 l/capita/year in Boliva (the CG) Equity considerations: N/R |
|
| Interventions |
Intervention: A bilateral trade and investment agreement. (Quote: "The US‐Peru FTA [free trade agreement], which is similar to the preceding NAFTA and CAFTA agreements, resulted in the preferential elimination of tariffs on soft‐drink imports (previously 25 %), as well as stronger protections for US investors, and strengthened intellectual property rights") Behavioural co‐intervention: None reported Control: No intervention. (Quote: "[W]e adopted a natural experiment design to quantify the effects of the US‐Peru FTA, ratified in 2006 and enforced in 2009, in contrast to Bolivia, a suitably matched country having no such agreement, on Peru’s soft drink market") |
|
| Outcomes |
Measures of SSB intake: Rate of change in SSB, and sports and energy drinks sales in litre per capita, and in sugar from soft drinks in kg per capita, assessed continuously throughout the study period with data from the commercial Euromonitor International Passport Global Market Information database Measures of intake of alternatives to SSB: Rate of change in bottled water and juice sales in litre per capita, assessed continuously throughout the study period with data from the commercial Euromonitor International Passport Global Market Information database Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes per‐capita sales of sports and energy drinks increased (see above) Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Low‐ and middle‐income countries Sector: Trade and investment policy Country: Peru Year(s) when implemented: 2006 ‐ 2009 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "The authors declare that they have no competing interests" Funding: "SF and PB are supported by funding from an Australian Research Council Discovery Project, “Trade policy: Maximising benefits for nutrition, food security, human health and the economy” (DP130101478). RL is an investigator on the same Project but does not receive funding from it, and is supported through the Canada Research Chairs program" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | For the outcomes of interest to us, baseline trends were similar for Bolivia and Peru (see table 4 of the study's primary report) |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | As discussed by the study authors, Peru and Bolivia differed in a number of relevant ways, which may have influenced investment, production, trade, marketing and consumption patterns, including population size, GDP per capita, general trade and FDI intensity, and other demographic, cultural, political and economic factors. The analysis did adjust for GDP and population growth, but not for other factors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | While the commercially available Euromonitor sales figures are not perfect, they are generally considered reliable, and there is no evidence that problems regarding incomplete outcome data affected the 2 countries differently |
| Blinding (performance and detection bias) Objective outcomes | Low risk | The outcome data (Euromonitor sales data) can be considered objective |
| Contamination (performance bias) | Unclear risk | While trade and investment rules did evolve in Bolivia, too, no major free trade agreement with the US was concluded at the time of the study. The study does, however, note that the US‐Peru FTA may also have affected Bolivia Quote: "Interestingly we also observed an increase, albeit small, in soft drink imports into Bolivia from Peru following enforcement, suggesting the US‐Peru FTA may have had regional effects on soft drink sales" |
| Selective reporting (reporting bias) | Low risk | The study has not been registered and there is no protocol available; however, given that some of the authors have taken in past publications a critical stance towards trade liberalisation, and that they found in this study positive effects strengthens confidence that outcomes were not reported selectively |
| Independence of the intervention from other changes (performance bias) | High risk | Study authors note that a number of factors not attributable to the intervention may have affected outcomes. Quote: "[I]t is important to note that the study design makes it difficult to draw inferences and the results may simply reflect changes in the strategic decisions made by soft‐drink manufacturers in response to consumer demand for different products rather than changes in FDI in‐flows and production resulting from the FTA. Others have also acknowledged the difficulty of separating the effects of trade liberalization from other social and economic influences on food markets and consumer behaviour" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | Study authors discuss the difficulties of establishing a clear time point when the intervention occurred, and report results both for the time point when the free trade agreement was ratified, and for the time point when it was enforced. In both cases, the point of analysis is the point of intervention. Quotes: "Another challenge in using the natural experiment design in this analysis was to determine where to introduce the intervention time‐point. For example, although the US‐Peru FTA was ratified in 2006 and enforced in 2009, changes in soft‐drink markets may have occurred earlier when, for example, the Office of the US Trade Representative notified US Congress of the Government’s intention to initiate negotiations with Peru in November 2003, with negotiations beginning in May 2004. Because this may have enhanced US investor confidence in Peru (a so‐called ‘market signal’) trade and investment flows may have begun as early as 2004. The staggered timing of the agreement and associated processes (e.g. notification of intent to congress → negotiation → ratification → enforcement) made it difficult to define a single intervention time‐point. For these reasons we included two time‐points in our models: 2006 as the ratification year and 2009 as the enforcement year" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns |
Ball 2015.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 574 Length of intervention: 3 months (+ 6 months additional follow‐up after the end of the intervention) |
|
| Participants |
General description of participants: Female, adult customers of Coles supermarkets in Melbourne, Australia Age: Adults (age 18 to 60 years was an inclusion criterion, mean age was 44 years in the CG and 43 in the IG) Inclusion criteria: Quote: "Women were required to either hold or be willing to obtain a Coles store loyalty (FlyBuys) card, which was provided to shoppers at no cost, and use this card when they shopped at Coles supermarkets over the 9‐mo study period. Additional eligibility criteria were that women were aged between 18 and 60 y; the main household shopper; able to speak, read, and write English and provide written informed consent to participate; willing to give information about total household income; willing to have their Coles sales data collected and analyzed; and the only woman in their household taking part in the study" Exclusion criteria: N/R Recruitment: Quote: "Coles and Loyalty Pacific Pty Ltd. (FlyBuys) staff (...) composed the sampling pool from which a random sample of 5000 was drawn for a recruitment mailing to participants’ home addresses. At the same time, a media release that targeted local newspapers was undertaken in catchment areas to encourage additional participation" Weight status at baseline: N/R SSB consumption at baseline: Self‐reported intake of SSB at baseline was 13 ml/day in the CG and 13 ‐ 25 ml/day in the 2 IGs. SSB purchases at baseline were 115 ml/day in the IG and 93 ‐ 102 ml/day in the 2 IGs Equity considerations: Quote: "The sample was close to evenly split according to catchment area (44% from low–socioeconomic status and 55% from high–socioeconomic status areas) and educational level (50% tertiary educated). The majority (71%) of women were married, and 53% of women had at least one child living at home. (...) Supplementary analyses were conducted to determine whether intervention effects were moderated by socioeconomic position (by testing 3‐way interaction terms, intervention by time by educational level/household income). Results (data not shown) indicated no strong evidence of moderation by education or income (i.e., intervention effects were consistent across women with low and high education for all 19 outcomes at times 2 and 3 and across low‐ and high‐income women for all time 2 outcomes and all but 3 time 3 outcomes)." 27% of participants in the CG and 25% in the IG were not born in Australia, and 100% were women |
|
| Interventions |
Intervention: A 20% price reduction on water and low‐calorie beverages implemented through a supermarket loyalty card scheme. (Quote: "[P]articipants in the price‐reduction intervention arm received a 20% price discount on target items, which was applied at the checkout on swiping their FlyBuys card at any Coles store for a 3‐mo period. Participants were sent a list of discounted items (all fruit and vegetables, including fresh, tinned, and frozen, and diet or low‐calorie carbonated beverages or water) at the start of the intervention and midway through the intervention period. This discount was applied over and above any other usual store discounts. Low‐calorie carbonated beverages were included in the discount because carbonated beverages are among the most popular and affordable beverage for Australian consumers with average prices per liter below those of other nonalcoholic beverages") Behavioural co‐intervention: None. (The study had 4 arms: control, price reduction, skills building, and price reduction plus skills building. We report data on the comparison control versus price reduction only) Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Purchases of SSB assessed continuously throughout the study period with electronic sales data, and self‐reported intake of SSB assessed at baseline, at 3 months (the end of the intervention) and after 6 months additional follow‐up Measures of intake of alternatives to SSB: Purchases of water and diet beverages assessed continuously throughout the study period with electronic sales data, and self‐reported intake of water and diet beverages assessed at baseline, at 3 months (the end of the intervention) and after 6 months additional follow‐up Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes an increase in the self‐reported intake of SSB in the IG (see above) Other outcomes: Intervention costs, assessed with a comprehensive economic evaluation, reported in a separate publication |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: Australia Year(s) when implemented: 2013 ‐ 2014 Mode of implementation: Pilot trial by researchers in co‐operation with a supermarket chain Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "None of the authors reported a conflict of interest related to the study" Funding: "The Supermarket Healthy Eating for Life study was supported by a National Health & Medical Research Council Project Grant (594767). KB is supported by a National Health & Medical Research Council Principal Research Fellowship (1042442). SM is supported by an Australian Research Council Future Fellowship (FT100100581). LG is supported by a National Health & Medical Research Council Early Career Fellowship (1035100). (...) Coles supermarkets and the National Heart Foundation of Australia provided in‐kind support for this study" Trial registration: Retrospectivly registered at Current Controlled Trials Registry, Trial ID ISRCTN39432901, www.isrctn.com/ISRCTN39432901 Protocol availability: Published as a separate paper |
|
| Notes | This study had 4 arms (control, price reduction, skills building, price reduction plus skills building). We report data on the comparison control versus price reduction only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A total of 642 women were randomly assigned to one of 4 conditions by using a computer‐generated block‐randomization sequence produced and implemented by an independent statistician that involved blocks of 4 and 8 in varying combinations stratified by supermarket catchment area" |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment was enabled via the secure storage of the randomization sequence separately from the participant database, which was accessible only by the data manager and statistician. Eligible participants were added to the database by the research fellows and assistants who were blinded to the allocation sequence. Only after the baseline survey had been completed and returned with signed consent did the data manager allocate participants to study arms" |
| Similarity of baseline outcome measurements (selection bias) | High risk | Baseline beverage outcome measurements differed substantially ‐ purchase and consumption data differed by up to 100% between the CG and the 2 IGs of interest. While this was taken into account in the analysis, the large magnitude of the differences suggest that there might have been unobserved baseline differences for which adjustment was not possible. Quote: "Values of sugar‐sweetened beverage purchasing were highly variable at baseline with highest values in the control group; subsequent increases in intervention groups could have reflected a regression to the mean" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | CG and IG were compared for socioeconomic status, country of birth, education level, marital status, household annual income, and number of children at home. Substantial differences are notable across all characteristics. The statistical models used did control for most demographic variables, but not for household size: Quote: "[P]urchasing was assessed at the household level, and these servings may have been spread across multiple individuals. It was difficult to adjust for household size in these analyses because some households had a single loyalty card, whereas other households had multiple cards that may or may not have been linked" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was approximately 10%, and the analysis was per‐protocol. Baseline beverage purchases and consumption were systematically different among those who were lost to follow‐up compared to those who stayed in the study: Quote: "At baseline, participants who were excluded from compared with those included in the analysis reported lower intakes of (…) tap water (4.4 ± 3.0 compared with 5.5 ± 3.1 servings/d, respectively) and purchased fewer (…) diet beverages (159.6 ± 340.2 compared with 513.6 ± 1324.7 mL/wk, respectively) and more nondiet beverages (1302.2 ± 2496.1 compared with 691.7 ± 1416.0 mL/wk, respectively)" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded to the intervention, and consumption data is self‐reported |
| Blinding (performance and detection bias) Objective outcomes | Unclear risk | Participants were not blinded to the intervention, and purchasing data could be manipulated by the participants (purchasing data were collected through supermarket loyalty cards, which had to be swiped at the checkout at each visit to a supermarket, and which might have been used selectively. Participants reported in the process evaluation surveys to have made purchases for other persons than themselves. Furthermore, it is possible that participants made stocking purchases during the intervention period to benefit additionally from the price reductions) |
| Contamination (performance bias) | Low risk | It seems unlikely that the CG received the price reduction intervention |
| Selective reporting (reporting bias) | Unclear risk | The trial was registered, but only retrospectively. The protocol was published prior to its implementation, and mentions total grocery shopping purchases (collected through FlyBuys loyalty cards) as an outcome, which is not reported in the primary report. In particular, reporting on certain potential adverse outcomes, e.g. compensatory behaviour, might be incomplete due to confidentiality agreements. Quote: "Our agreement with industry partners did not permit us to analyze substitution effects (i.e., whether and how the discount affected the purchasing of nontargeted products)" |
| Other bias | High risk | The methods used for outcome assessment seem to have been unreliable, as shown by the huge discrepancies between self‐reported beverage consumption and beverage purchases ‐ e.g. in the whole sample at baseline, participants seem to have purchased only 53% of the bottled water they consumed at Coles supermarkets, while they seem to have consumed only 13% of the SSB they bought there. The study authors raise doubts about the reliability of the self‐reported data, and in the process evaluation it is mentioned that participants reported that even with the discount, beverages were more expensive at Coles supermarkets than in other shops, which is why they bought their beverages primarily from other sources. Study authors also mention the possibility that FlyBuy cards were not used for all purchases. Neither the purchasing data from the FlyBuys cards nor the self‐reported consumption data therefore seem to be sufficiently reliable |
Bauhoff 2014 cohort.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: The intervention site was the Los Angeles Unified School District (which implemented a district‐wide school nutrition policy in July 2004), which is compared with a synthetic control group constructed as a weighted combination of several control districts from the rest of California which did not implement such a policy during the study period Number of clusters or sites: In total, data from 133 middle schools and 77 high schools were used in the study (see table 2 of the study's primary report). How many schools contributed data to the analyses included in this review is not reported Number of individuals: This was a repeat cross‐sectional analysis. At baseline, 15,196 students were included, and at follow‐up 17,701 students were included (both sexes, cohort analysis, as reported in table 4 of the study's primary report) Length of intervention: Approximatly 24 months |
|
| Participants |
General description of participants: Middle and high school students in Los Angeles, USA Age: Children and teenagers (12 ‐ 15 years of age) Inclusion criteria: Students participating in the California Healthy Kids Survey (CHKS), a representative state‐wide cohort study (the study's primary report does not provide details on the methods used by this survey, but provides relevant references) Exclusion criteria: Students outside the age range of 12 ‐ 15 years Recruitment: N/R Weight status at baseline: At baseline, 46% of participants were overweight or obese and 18% were obese SSB consumption at baseline: At baseline, between 61% and 74% of participants reported consuming at least 1 serving of SSB a day Equity considerations: The IG was a representative sample of middle and high school students living in Los Angeles, California, USA. Both sexes (49% female), and a variety of ethnic backgrounds were represented (65% Hispanic, 10% white, 5% black); 60% of students received a free school lunch (i.e. were from lower‐income families) and 76% of the schools were title 1 schools (i.e. schools with an above‐average share of lower‐income students) |
|
| Interventions |
Intervention: Reduced availability of SSB at school. (Quote: "This paper evaluates the impact of an early nutrition policy, Los Angeles Unified School District’s food‐and‐beverage standards of 2004. (...) The policy limits beverages to unsweetened soft drinks and juice blends with at least 50% juice. It allows only low‐fat milk, and imposes serving size restrictions on electrolyte drinks; added sweeteners are also limited for these types of beverages") Behavioural co‐intervention: None reported Control: Minimal intervention (Control districts were exposed to less stringent state‐wide school nutrition standards. Quote: "The state of California implemented a less comprehensive beverage standard, Senate Bill SB 677, in July, 2004. The regulations prohibited added sweeteners and required that juice blends contain at least 50% juice. This was the first school nutrition policy in the state and only applied to elementary and middle schools") |
|
| Outcomes |
Measures of SSB intake: Percentage of students consuming more than 0, 1, 2, 3 or 4 servings of SSB a day, assessed at baseline (spring 2004) and 24 months (spring 2006) with questionnaires administered as part of the California Healthy Kids Survey Measures of intake of alternatives to SSB: Percentage of students consuming 0, 1, 2, 3 or 4 servings of milk (any kind, including sugar‐sweetened milk) a day, assessed at baseline (spring 2004) and 24 months (spring 2006) with questionnaires administered as part of the California Healthy Kids Survey Anthropometric measures: Assessed in the study but not included in our review due to confounding by non‐beverage‐specific intervention components Adverse outcomes: None included in this review Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Middle and high schools Sector: Education Country: USA Year(s) when implemented: 2004 ‐ 2005 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "I have no conflicts of interest to declare" Funding: N/R Trial registration: N/R Protocol availability: N/R |
|
| Notes | The data used for this analysis partially overlaps with the data used in Bauhoff 2014 crosssectional, and is reported in the same paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | SSB consumption was slightly higher among boys in the CG than in the IG, but almost identical among girls in the 2 groups (see table 4 of the study's primary report). Moreover, this was taken into account in the analysis. Quote: "I estimate a transparent two‐period difference‐in‐difference using 'synthetic' control groups, combinations of several control districts that are reweighted to minimize imbalance between treatment and control areas on a defined set of covariates and pre‐intervention outcomes" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | There were some differences between the intervention and control schools (see table 1 and table 4 of the study's primary report), but these were small, and were taken into account in the analysis (see quote above) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The data used were not collected for the present study, but as part of a general repeat cross‐sectional population health monitoring survey. While there is no indication that intervention and control districts were differently affected by sampling errors at baseline and at follow‐up, it is unclear to what extent the data are representative of the districts included in the IG and CG. Quote: "Note that the data are an unbalanced panel because an individual school’s data may be redacted or missing, and that the CHKS is administered to a changing sample of schools" |
| Blinding (performance and detection bias) Subjective outcomes | Unclear risk | Participants were not blinded, and the outcomes are self‐reported, i.e. not assessed blindly. The data were not collected for the present study, and data collection was therefore not necessarily perceived to be connected to the changes in the school food and beverage policies. However, the intervention, as well as possible behavioural co‐interventions, may still have led to social desirability bias in the IG |
| Contamination (performance bias) | High risk | Contamination is likely, and would have biased the results towards null. Quote: "The estimates for soda must be treated with caution since the pre‐policy data were collected in Spring 2004, after the beverage policy was already in place. Also, the post‐policy data are from Spring 2006; at that time, students who were exposed to the (ineffective) state beverage policy in middle school grade 8 during 2004/5 school year have entered the control high schools. These issues should bias the results toward finding no effect" |
| Selective reporting (reporting bias) | Unclear risk | All important outcomes reported in the Methods section are reported in the Results section. However, given that this was a post hoc analysis of secondary data, with no study protocol is publicly available, we cannot rule out selective outcome reporting. Moreover, no overall measure for mean SSB intake is reported (such as mean intake in servings/day), but only the percentage of male and female students consuming more than 0, 1, 2, 3 and 4 servings of SSB/day |
| Other bias | Low risk | No other concerns |
Bauhoff 2014 crosssectional.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: See Bauhoff 2014 cohort Number of clusters or sites: In total, data from 77 high schools were used in this study (see table 2 of the study's primary report). How many schools contributed data to the analyses included in our review is not reported Number of individuals: This was a repeat cross‐sectional analysis. At baseline, 13,171 students were included, and at follow‐up 12,552 students were included (both sexes, repeat cross‐sectional analysis, as reported in table 4 of the study's primary report) Length of intervention: See Bauhoff 2014 cohort |
|
| Participants |
General description of participants: High school students in Los Angeles, USA All other items: See Bauhoff 2014 cohort |
|
| Interventions | See Bauhoff 2014 cohort | |
| Outcomes | See Bauhoff 2014 cohort | |
| Context and implementation | See Bauhoff 2014 cohort | |
| Declarations | See Bauhoff 2014 cohort | |
| Notes | The data used for this analysis partially overlap with the data used in Bauhoff 2014 cohort, and are reported in the same paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | See Bauhoff 2014 cohort. |
| Allocation concealment (selection bias) | High risk | See Bauhoff 2014 cohort. |
| Similarity of baseline outcome measurements (selection bias) | Low risk | See Bauhoff 2014 cohort. |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | See Bauhoff 2014 cohort. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | See Bauhoff 2014 cohort. |
| Blinding (performance and detection bias) Subjective outcomes | Unclear risk | See Bauhoff 2014 cohort. |
| Contamination (performance bias) | High risk | See Bauhoff 2014 cohort. |
| Selective reporting (reporting bias) | Unclear risk | See Bauhoff 2014 cohort. |
| Other bias | Low risk | See Bauhoff 2014 cohort. |
Blake 2018.
| Methods |
Design: ITS study Timing: Prospective Allocation to group: N/A (ITS study without control group) Number of clusters or sites: 1 convenience store located in 1 public hospital Number of individuals: The number of customers using the store which implemented the intervention is not reported; the mean number of beverage units sold each week was 1538 a week at baseline Length of intervention: 17 weeks |
|
| Participants |
General description of participants: Customers of a convenience store located on the premises of a public hospital in Melbourne, Australia Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: At baseline, approximately 300 litres of SSB a week were sold at the convenience store which implemented the intervention (equivalent to approximately 40% of all beverage sales) Equity considerations: Among the sub‐sample of participants who completed the customer exit survey, 24% were from areas belonging to the most disadvantaged socio‐economic index tertile; 61% were female, 51% were hospital staff or students and 19% were hospital patients; 82% were adults aged 25 to 64 years |
|
| Interventions |
Intervention: Price increase on SSB of 20%. Quote: "Beverages were classified using a traffic‐light system from the Healthy Choices guidelines from the Victorian Department of Health and Human Services.20 The categories were 'red' ('limit,' eg, sugary soft drinks, juices >250 mL), 'amber' ('choose carefully,' eg, diet soft drinks), and 'green' ('best choices,' eg, water). This classification system considers the macronutrient and energy content of beverages for different beverage categories (…). Prices of red beverages were increased by 20%, while amber and green beverage prices were unchanged for 17 weeks (...). For example, 450‐mL bottles of a popular brand of nondiet soft drink increased from $3.90 to $4.50 Australian dollars, while the equivalent diet soft drink remained at $3.90. Customers were not explicitly informed of the price increases; however, price tags were displayed next to beverages and researchers provided store staff with flyers to give to customers who inquired about the intervention. The flyer detailed the purpose of the intervention and relevant hospital staff contact details. Researchers monitored intervention fidelity weekly through visual inspection of beverage price tags. Prices of red beverages in vending machines surrounding the store were also increased by 20% (…)" Behavioural co‐intervention: None (but see quote above) Control: N/A (ITS study without control group) |
|
| Outcomes |
Measures of SSB intake: Units and volume of red‐labelled beverages sold, as well as total sugar and calorie content of all beverages sold, assessed continuously throughout the study period with routinely‐collected sales data Measures of intake of alternatives to SSB: Units and volume of amber‐ and green‐labelled beverages sold, assessed continuously throughout the study period with routinely‐collected sales data Anthropometric measures: N/R Adverse outcomes: Total beverage revenue, assessed continuously throughout the study period with routinely collected sales data, and target group discontent and stakeholder concerns, assessed with a customer survey and semi‐structured interviews with store staff and managers after the end of the intervention Other outcomes: Stakeholder perceptions, assessed with semi‐structured interviews at the end of the intervention period |
|
| Context and implementation |
Setting: Convenience stores Sector: Retailing Country: Australia Year(s) when implemented: 2015 Mode of implementation: Voluntary action by for‐profit private businesses Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Statement of potential conflict of interest: K. Corben is employed within the health service where the intervention took place. No potential conflict of interest was reported by the remaining authors." Funding: "Funding/support: This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors. M. R. Blake received an International Congress of Dietetics LEAP (Leadership, Evidence and Advancing Practice) travel grant from the Dietitians’ Association of Australia to present findings of the project at the International Congress of Obesity 2016. M. R. Blake is supported by an Australian Government Research Training Program Scholarship and a Monash University Departmental Scholarship. K. Backholer is supported by a National Heart Foundation Post‐Doctorial Research Fellowship. K. Corben is employed by the health service where the policy was implemented. T. Boelsen‐Robinson is supported by an Australian Government Research Training Program Scholarship. C. Palermo is supported by Monash University Department of Nutrition and Dietetics. A. Peeters is supported by a National Health and Medical Research Council fellowship and Deakin University. C. E. Stevenson is supported by Deakin University. E. Lancsar is supported by an Australian Research Council (ARC) fellowship." Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study is based on routinely collected sales data, which are likely to be close to complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes (sales data) are objective |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section, and which one might expect in a study of this kind are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | The intervention may not have been independent of other changes; however, the clear, step‐shaped effects occurring immediately after the start of the intervention and the sophisticated ITS methods used by the study authors strengthen our confidence that the observed effects are at least partially attributable to the intervention |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention was the point of analysis |
| Intervention effects on data collection (detection bias) | Low risk | The study is based on routinely‐collected sales data. The intervention is unlikely to have affected data collection |
| Other bias | Unclear risk | Seasonality was taken into account; however, compensatory SSB purchases from other sources may have occurred. Quotes: "Each sales data outcome (volume, number of items, and revenue) was analyzed using single‐group interrupted time series analyses to control for pre‐intervention trends, autocorrelation in sales data, and seasonal fluctuations. (...) [I]t was not possible to determine whether customers compensated by buying cheaper‐priced red beverages from other retailers, such as the hospital cafeteria. Additional research should investigate the effect of SSB price increases on overall dietary intake, taking account of possible food and beverage substitutions" |
Boelsen‐Robinson 2017.
| Methods |
Design: ITS Timing: Prospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 37 vending machines Number of individuals: N/R (the analysis is based on transaction data not linked to individual participants) Length of intervention: 1 year |
|
| Participants |
General description of participants: Staff, patients, and visitors using vending machines in a large public hospital in Melbourne, Australia Age: All ages Inclusion criteria: All vending machines located on the premises of the hospital implementing the intervention were included Exclusion criteria: N/R Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: N/R |
|
| Interventions |
Intervention: Traffic‐light labelling and improved availability of healthier beverages in vending machines. (Quote: "The health service adopted the Healthy Choices: food and drink guidelines for Victorian public hospitals (Healthy Choices), which guides health services to reduce the proportion of unhealthy food and beverages available for sale, and increase the availability of healthy options. These guidelines classify food and beverages into ‘red’, items that should be limited, ‘amber’, items to be chosen carefully, and ‘green’, the best choices. Classification is based on nutrients such as saturated fat, sugar, sodium, fibre, and energy content. Consistent with these guidelines, following policy implementation by the health service, the proportion of ‘red’ items available in each vending machine across the health service was no more than 20% of displayed products, ‘green’ made up at least 50% of displayed products, and ‘amber’ contributed the remaining. There was basic communication at point‐of‐sale as to the meaning of the classification, and items were labelled with their classification. All products were coded by an accredited dietician at the health service. These classifications were obtained and used in this study") Behavioural co‐intervention: None reported Control: N/A (ITS without control group) |
|
| Outcomes |
Measures of SSB intake: Number of beverages labelled red or amber sold, assessed continuously throughout the study period with routinely‐collected itemised sales data Measures of intake of alternatives to SSB: Number of beverages labelled green sold, assessed continuously throughout the study period with routinely‐collected itemised sales data Anthropometric measures: N/R Adverse outcomes: Total revenue from beverages, assessed continuously throughout the study period with routinely‐collected itemised sales data Other outcomes: Stakeholder perceptions, assessed with qualitative interviews towards the end of the study period |
|
| Context and implementation |
Setting: Hospital Sector: Health care Country: Australia Year(s) when implemented: 2011 ‐ 2012 Mode of implementation: Voluntary action by a public hospital Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Conflict of interest statement: TBR, KB, MB, CP, and AP report no conflict of interest. KC is employed by the health service where the policy was implemented" Funding: "Sources of support: TBR is supported by a Monash University Australian Postgraduate Award (APA). KB is supported by a National Heart Foundation Doctorial Research Fellowship (Grant number: PH 12 M6824). KC is employed by the health service where the policy was implemented. MB is supported by a Monash University APA and a Monash University Departmental Scholarship. CP is supported by Monash University Department of Nutrition and Dietetics. AP is supported by a National Health and Medical Research Council fellowship (Grant number: GNT1045456) and Deakin University. This project was supported in part by VicHealth" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were itemised electronic sales data, and can be assumed to be complete. Quote: "Itemised, monthly sales data from all 37 vending machines from 30 months prior to, and 12 months post‐policy implementation was obtained from the supplier." However, researchers could not "measure compensatory purchasing behavior", and mention that there were other in‐hospital locations where SSB were available |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported. For green and amber beverages only relative changes are reported, and for red beverages absolute changes are reported only graphically. However, the study also reports the total number of items sold and revenue from all items targeted by the intervention |
| Independence of the intervention from other changes (performance bias) | Low risk | Due to their magnitude and the clear, step‐shaped correlation with the time point when the intervention was implemented, it seems unlikely that the effects can be explained by other factors than the intervention. At the time point when the new stocking and labelling rules were introduced, a number of other changes took place, which can, however, be considered part of the intervention. Quote: "As part of the policy implementation the vending services were publicly tendered in a competitive process. Respondents were required to demonstrate their capacity to comply with Healthy Choices, as well as submitting a proposal regarding commission rates and other factors. The supplier who was appointed offered higher commission rates than previously, and also changed the location and size of some vending machines within the health service" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of analysis was the point of intervention. Quote: "The intervention was modelled to commence 1st April 2012" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection. Quote: "Itemised, monthly sales data from all 37 vending machines from 30 months prior to, and 12 months post‐policy implementation was obtained from the supplier" |
| Other bias | Low risk | No other concerns ‐ in particular, seasonality was taken into account. Quote: "Seasonal effects and autocorrelation up to 12 months prior were adjusted for" |
Bollinger 2011.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: The intervention site was New York City, which implemented a city‐mandated calorie‐labelling policy in 2008, and the control sites were Boston and Philadelphia, which did not implement such a policy during the study period Number of clusters or sites: 316 coffee shops located in 3 cities and belonging to 1 coffee shop chain Number of individuals: N/R (the main analysis, which we report in this review, was done with transaction data not linked to individual participants; the analysis is based on 118,480 observations, each constituting 1 unique store‐day combination) Length of intervention: 11 months |
|
| Participants |
General description of participants: Customers of the coffee shop chain Starbucks in New York City (the IG), and Boston and Philadelphia (the CG), USA Age: All ages Inclusion criteria: Any transaction at a Starbucks company store in New York City, Boston and Philadelphia during the study period Exclusion criteria: N/R Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: "Although the anonymous transaction data contain no information about the demographics of the consumers who made each transaction, we do know the store location of each transaction, and census data provide us with zip‐level demographics. Using this information, we find that the decrease in calories per transaction was larger in zips with higher income and in zips with more education (i.e., more people with college degrees). (...) We find that individuals who averaged more than 250 calories per transaction prior to calorie posting reacted to calorie posting by decreasing calories per transaction by 26 percent ‐ dramatically more than the 6 percent average reduction for all consumers" |
|
| Interventions |
Intervention: Menu‐board calorie labelling in chain restaurants. (Quote: "The mandatory calorie posting law in NYC requires all chains (with 15 or more units nationwide) to display calories for every item on all menu boards and menus in a font and format that is at least as prominent as price. Health department inspectors verify the posting, and restaurants may be fined up to $2,000 per restaurant location for noncompliance. The NYC Board of Health first voted in the law in 2006, but legal challenges from the New York State Restaurant Association delayed its implementation until mid‐2008. The litigation process gave restaurants a couple of years to anticipate the introduction of the new law and created uncertainty around the date at which enforcement would commence. In early May 2008, it was reported that restaurants in NYC were being given citations for noncompliance. However, fines were not imposed until late July 2008. Starbucks commenced calorie posting in their NYC stores on April 1, 2008. They were one of the first chains to start posting and, as best we can tell, other chains were close behind") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Total calories from beverages per transaction, assessed continuously throughout the study period with transaction data provided by Starbucks Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: Starbucks' revenue, assessed continuously throughout the study period with transaction data provided by Starbucks Other outcomes: Total calories from foods per transaction, and total calories from foods and beverages combined per transaction, assessed continuously throughout the study period with transaction data provided by Starbucks |
|
| Context and implementation |
Setting: Cafés Sector: Food service Country: USA Year(s) when implemented: 2009 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "We are very grateful to Starbucks for providing us with the data used in this study. We have no consulting relationship with Starbucks ‐ the findings in this study are completely independent of Starbuck’s interest" Funding: N/R Trial registration: N/R Protocol availability: N/R |
|
| Notes | We report results from the cardholder and the transaction data, but include only the latter in our primary analyses, as they are based on a larger and more representative data set | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline outcome measurement differences existed, but were small (see table 1 of the study's primary report). These were taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Outcomes were measured at baseline, and while differences exist, they are small (see table 1 of the study's primary report). Quote: "Qualitatively (...) it appears that Boston and Philadelphia are reasonable controls for NYC. (...) Beverage offerings are the same in all Starbucks and there is some variation in food items" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study used routinely‐collected sales data, which can be assumed to be complete, as stated clearly by the study. Quotes: "First, we observe every transaction at Starbucks company stores in NYC from January 1, 2008 to February 28, 2009, with mandatory calorie posting commencing on April 1, 2008. To control for other factors affecting transactions, we also observe every transaction at Starbucks company stores in Boston and Philadelphia, where there was no calorie posting. (...) Our transaction data cover all 222 Starbucks locations in NYC, and all 94 Starbucks locations in Boston and Philadelphia" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were objective (routinely‐collected sales data) |
| Contamination (performance bias) | Low risk | The study clearly states that there were no calorie postings in the control locations. Quote: "To control for other factors affecting transactions, we also observe every transaction at Starbucks company stores in Boston and Philadelphia, where there was no calorie posting" |
| Selective reporting (reporting bias) | Unclear risk | No protocol predefining outcomes and analyses is provided; moreover, comprehensive confidentiality agreements with Starbucks may have given room for selective outcome reporting |
| Independence of the intervention from other changes (performance bias) | Low risk | Given the controlled design, it seems unlikely that the observed effects were substantially affected by other changes than the intervention. Study authors examine and assess a number of potential confounding factors, including prices, changes to product offerings, and seasonal effects. Quote: "[T]here are a few reasons why other factors are unlikely to confound our findings. First, the time path of estimates shown in Figure 2 indicates the reduction in calories occurred immediately following calorie posting on April 1, 2008. Hence, any other differential change in NYC relative to the controls that could explain this pattern must have occurred at almost the same time. That seems unlikely. Second, the estimated effect of calorie posting based on the cardholder data is primarily identified by within individual variation over time. (...) Fourth, as a robustness check, we include day‐of‐week dummies and holiday dummies that differ for NYC and the controls, finding no difference in the estimates. If we also drop the observations for holidays (and allow day‐of‐week dummies to be different for NYC and the controls) the estimates are unchanged" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of analysis is the point of intervention |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns ‐ in particular, seasonality was taken into account in the analysis |
Breeze 2018.
| Methods |
Design: ITS study Timing: Retrospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 7 leisure centres Number of individuals: The median number of persons attending each of the 7 leisure centres was 42,324 a month (range 11,916 to 108,393) Length of intervention: 12 months |
|
| Participants |
General description of participants: Attenders of public leisure centres, which included facilities such as swimming pools, gyms, and other training facilities, located in Sheffield, UK Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: At baseline, on average 15.8 ml of SSB were sold per attendance (i.e. each visit of 1 person at 1 of the leisure centres) Equity considerations: Quotes: "The policy has been evaluated in leisure centre venues across Sheffield serving a broad social spectrum. (...) . Sheffield City Trust attracts a high proportion of customers from lower socioeconomic groups due to the location of venues, suggesting that the policy can be effective in more hard to reach groups. Given the breadth of facilities on offer, the study population includes representation from wide age ranges, gender mix and black and minority ethnic groups. (…) The impact of the policy on non‐SSB options were highly variable across venues with almost no substitution observed for Concord and ICE Sheffield (comprising lower socioeconomic status and younger attendees respectively) but much higher in Ponds Forge in the city centre and Hillsborough suggesting that the response to the policy and impact on revenues are likely to be highly dependent on the population demographics. (…) The overall and substitution effects varied between venues and product types, suggesting that consumers of drinks specifically marketed for children were more likely to reduce consumption and switch to alternatives. The very large price elasticity for these products may suggest that the policy is more effective for young people and, more specifically, when parents are purchasing drinks for their children" |
|
| Interventions |
Intervention: A price increase on SSB of approximately 11‐25% accompanied by promotional and educational activities. Quote: "In July 2016 Sheffield City Trust (SCT) introduced a comprehensive sugar sweetened drink strategy to improve customer health outcomes at all of its Sheffield leisure facilities including: £0.20 ($0.27, €0.23) increase on price of all drinks containing 5mg of sugar per 100ml or more directly applied to all products in leisure centre venues enforced by a central catering team (approximately 11%‐25% of product prices); Staff training in order to deliver face to face awareness of scheme with customers; Publicity in local and national media; Publicity within venues including posters, billboards and drinks stickers in café and vending areas" Behavioural co‐intervention: Awareness‐raising and education (see quote above) Control: N/A (ITS without control group) |
|
| Outcomes |
Measures of SSB intake: Total volume, and units of SSB sold per attendance, assessed continuously throughout the study period with routinely‐collected sales data Measures of intake of alternatives to SSB: Units of cold drinks excluding SSB, of diet beverages, and of water and fruit juice, assessed continuously throughout the study period with routinely‐collected sales data Anthropometric measures: N/R Adverse outcomes: Total beverage sales, assessed continuously throughout the study period with routinely‐collected sales data Other outcomes: N/R |
|
| Context and implementation |
Setting: Public leisure centres Sector: Other Country: United Kingdom Year(s) when implemented: 2016 Mode of implementation: Mandatory government regulation (city‐level regulation) Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "PB, RP, EG, and AB have no conflicts of interest. RW is an employee of Sheffield City Trust. This does not alter our adherence to PLOS ONE policies on sharing data and materials" Funding: "The study was funded by the Medical Research Council (MC_PC_15062). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study is based on routinely‐collected sales data, which are likely to be complete. Quote: "We obtained data on sales of cold drinks at all venues from January 2015 to July 2017. Cold drinks sales at cafes and vending machines within venues were included but sales data for hot drinks and other confectionary were not available" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes (sales data) are objective |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section, and all outcomes one might expect from a study of this kind are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | The absence of pre‐existing trends in SSB sales during the baseline period, and in the venues not affected by the intervention suggests that observed effects are attributable to the intervention and not to other changes. Quote: "Other changes are occurring concurrent with the tax, including anticipation of a national tax on SSB, health campaigns about sugar sweetened beverages, and anti‐obesity programs may contribute to the demand for SSB in the leisure centre venues. The study did not identify any pre‐existing trends in SSB in the pre‐tax period. From our analysis of venues not affected by the policy it is clear that a similar reduction in SSBs were not observed in the post‐policy period. The affected and unaffected venues were not randomly allocated, which means it is not possible to conclusively state that the changes observed are solely due to the new policy" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The shape of the intervention was prespecified, and the point of intervention was the point of analysis. Quote: "It was hypothesised that the intervention would have an immediate impact on sales on initiation of the policy and would maintain effectiveness over time. Investigations of the data suggested that sales per attendance were relative stable over the study period, i.e. no gradual increases or decreases over time and time trend covariates for month and year were not significantly associated with demand. Therefore, the model assumed no time trend in sales over time and a level change in SSB sales per visitor with no lag" |
| Intervention effects on data collection (detection bias) | Low risk | The study is based on routinely‐collected sales data. Quote: "Each month the total numbers of cold drinks sold were extracted by product from routine monitoring of product sales used by the catering team for accounting and stock control purposes" |
| Other bias | Unclear risk | Seasonality was taken into account; however, it is possible that compensatory SSB sales outside the leisure centres occurred. Quotes: "Average monthly rainfall was included to describe environmental factors. Seasonality was adjusted for to account for seasonal changes in sales and because there was an unbalanced distribution of months before and after the intervention. (...) [I]t has not been possible to evaluate how the policy has affected purchasing behaviour outside of these venues. It is possible that some customers delayed the purchase of SSBs and visited other retail outlets to avoid paying the higher price. This explanation is less likely to apply to customers choosing to substitute for non‐SSB products. Given that we observed a large increase in non‐SSB consumption and overall sales did not decrease significantly, we believe that there would be limited delayed purchases of SSB products outside the venues which might mitigate the effectiveness of the policy" |
Brimblecombe 2017.
| Methods |
Design: Cluster‐RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 20 communities with 1 store each Number of individuals: 8515 (The analysis is based on sales data not linked to individual participants; the estimated total population of the intervention communities was 8515, and we follow the study authors in using this figure as proxy for the total number of participants. Quote: "Whole population RCTs assessing point‐of‐sale interventions are diffi cult to do because of the risk of contamination from adjacent retailers. The Northern Territory of Australia provides a unique and ideal trial location because communities are sparsely located and community stores are the main food source for most people. In this context, store‐level purchasing is a powerful proxy of community‐level diet. (…) We derived per capita daily estimates by using Australian census estimates of usual residence by Indigenous location including Indigenous and non‐Indigenous status'") Length of intervention: 24 weeks (+ 24 weeks additional follow‐up after the end of the intervention) |
|
| Participants |
General description of participants: Customers of community stores in very remote Indigenous communities in the Northen Territory of Australia. Age: All ages Inclusion criteria: Quote: "Communities (the equivalent of small towns) were eligible if they were located in very remote regions of the Northern Territory (...). Other eligibility criteria were that each community had a population more than 100 people, the community store was managed by either of the two store associations ALPA or OBS, and no other food outlet was present within 20 km" Exclusion criteria: N/R Recruitment: Quote: "20 communities (...) met the eligibility criteria, were invited to participate, and consented to participate" Weight status at baseline: N/R SSB consumption at baseline: At baseline, SSB sales per capita were 354 ml/day, and 58% of all beverages purchased in the community stores were SSB Equity considerations: Quote: "Communities (...) were eligible if they were located in very remote regions of the Northern Territory, where access to goods and services is severely restricted and extreme socioeconomic disadvantage is concentrated. (...) Indigenous Australians are one of the most disadvantaged populations in Australia and have a burden of disease 2‐3 times that of non‐Indigenous Australians. Around 37% of this disease burden is preventable by reducing exposure to modifiable risk factors, such as dietary factors, which account for 10% of the total disease burden and 15% of the health gap between Indigenous and non‐Indigenous Australians. (...) The generalisability of these study findings to other extremely disadvantaged populations needs consideration. With regards to generalisation to remote Indigenous Australia, the communities were spread across the Northern Territory. 44% of Indigenous Australians who live in very remote parts of Australia are located in the Northern Territory and the population distribution by age and gender of the 20 study communities matched that of the broader remote Indigenous population. There are communities and small rural and remote non‐Indigenous townships in Australia and internationally that experience similar degrees of social disadvantage and issues of food affordability for whom these findings are relevant" |
|
| Interventions |
Intervention: A 20% price reduction for bottled water and diet beverages, and point‐of‐purchase promotion. (Quote: "A 20% price discount on all fresh and frozen fruit and vegetables (excluding frozen potato products), all bottled water, and all artificially sweetened soft drinks was applied at the point of sale and the discount promoted in stores. The value of the price discount was reimbursed to the store associations using Australian National Health and Medical Research Council research funding. Promotional materials (large pull‐up banner, price tickets [shelf talkers], shelf stripping, and fridge stickers) were developed by an expert working group and made available to stores within 2 weeks of intervention commencement") Behavioural co‐intervention: None (The study had 3 arms: Price discounts only, a combination of price discounts and nutrition education, and no intervention; we report data for the comparison price discounts vs no price discounts only) Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Percentage change in the amount of SSB (ml/capita/day) purchased, assessed continuously throughout the study period with store sales data Measures of intake of alternatives to SSB: Percentage change in the amount of bottled water and diet beverages (ml/capita/day) purchased, assessed continuously throughout the study period with store sales data Anthropometric measures: N/R Adverse outcomes: Substitution effects, and effects on overall food and beverage sales, assessed continuously throughout the study period with store sales data Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Community stores in remote Indigenous communities Sector: Retailing Country: Australia Year(s) when implemented: 2013 ‐ 2014 Mode of implementation: Pilot trial by researchers in co‐operation with not‐for‐profit community stores Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "We declare no competing interests." Funding: "The SHOP@RIC study was funded by the Australian National Health and Medical Research Council (NHMRC; grant number 1024285). JB is supported by a National Heart Foundation (NHF) Future Leader Fellowship (grant number 100085). MF is supported by a NHMRC Postgraduate Scholarship (grant number 10390774). SCL is supported by NHMRC project grant (grant number 1106632). MM is supported by a NHMRC Centre for Research Excellence grant (grant number 1041020) in Obesity Policy and Food Systems. KB is supported by a NHMRC Principal Research Fellowship (grant number 1042442). AJL is supported by a NHMRC senior research fellowship. NHMRC Program Grant (631947) provided some salary support for the study" Trial registration: Retrospectively registered at Australian New Zealand Clinical Trials Registry, registration number ACTRN12613000694718 Protocol availability: Protocol published as separate publication |
|
| Notes | The study had 3 arms (price discounts, a combination of price discounts and nutrition education, and no intervention). We report data for the comparison price discounts versus no price discounts only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study states that allocation was random and done by the team statistician, but does not state explicitly how the allocation sequence was generated. However, given that assignment was done by choosing stores contained in separate opaque envelopes, this is unlikely to have introduced bias. Quote: "Before commencement, all communities were randomly allocated by the team statistician to a fixed framework (...). A store from each of the ALPA and OBS group of stores (contained in separate opaque envelopes) was selected, and stores in turn continued to be consecutively allocated to the fixed store set framework, starting with the first store slot in the first store set, until all stores had been allocated" |
| Allocation concealment (selection bias) | Low risk | All stores were allocated to their study arm at the start of the study, and allocation was done by choosing stores contained in separate opaque envelopes (see quote above) |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | This was a stepped‐wedge design, and all stores received the intervention, but at different time points. The study does not report if stores receiving the intervention later (i.e. serving as controls for longer) differed from those receiving it earlier |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | See comment above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The analysis is based on routinely‐collected sales data, and it seems unlikely that incomplete outcome data substantially biased results |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcome data were objective. Quote: "Sales data is objective. The price discount was automatically applied at the store level, and therefore was not reliant on study participants redeeming the discount at point of purchase" |
| Contamination (performance bias) | Low risk | It seems unlikely that contamination substantially biased results. Quotes: "All stores were located 20 km or more from another food outlet with 13 stores located more than 50 km away. (...) Whole population RCTs assessing point‐of‐sale interventions are difficult to do because of the risk of contamination from adjacent retailers. The Northern Territory of Australia provides a unique and ideal trial location because communities are sparsely located and community stores are the main food source for most people. In this context, store‐level purchasing is a powerful proxy of community‐level diet" |
| Selective reporting (reporting bias) | Low risk | Full results for all foods and beverages sold in the intervention stores are reported |
| Other bias | Low risk | No other concerns ‐ in particular, seasonality was taken into account. Quote: "The study design allowed for temporal variation to be accounted for such as seasonal effect, which was particularly strong for water purchases in our study" |
Cawley 2015.
| Methods |
Design: ITS Timing: Retrospective Allocation to group: N/A (ITS study without control group) Number of clusters or sites: 168 supermarkets belonging to 1 supermarket chain Number of individuals: N/R (the analysis is based on transaction data not linked to individual participants) Length of intervention: 16 months |
|
| Participants |
General description of participants: Customers of Hannaford Supermarkets, a supermarket chain in the north‐east USA Age: All ages Inclusion criteria: All supermarkets belonging to Hannarford Supermarkets, a regional supermarket chain in the north‐east USA Exclusion criteria: See Inclusion criteria Recruitment: N/R Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: N/R |
|
| Interventions |
Intervention: Nutrition rating shelf labels in supermarkets (Quote: "The nutrition information system of interest is Guiding Stars, developed by Hannaford Supermarkets. Analogous to the three‐star approach recommended by the Institute of Medicine, Guiding Stars assigned scores of zero, one, two or three stars (with three stars being the most nutritious) to specific branded food items based on an independent published algorithm that takes into account vitamins, minerals, fibre and whole grains (which raise the score), as well as saturated fat, trans‐fat, cholesterol, added sodium and added sugars (which lower the score). A shelf tag beneath the product displays the number of stars assigned to that food item; one star indicates good nutritional value, two indicates better nutritional value and three indicates the best nutritional value. This information is displayed on the shelf tag in the following way. If the food item did not meet the nutritional criteria for even one star then the shelf label shows an outline of a running man with the words ‘No Guiding Stars’ in an arc over his head. In contrast, the shelf labels for nutritious food items display the running man in solid blue (not just an outline), with the relevant number of large gold stars in an arc over his head. (...) More than 60 000 food items are rated. The few that are not rated include new items (not yet rated), seasonal items (not consistently available) and items such as dried spices, dried coffee/tea and bottled water, which have no energy or nutrient content") Behavioural co‐intervention: A limited number of educational activities. (Quote: "To facilitate shopper use of the information, educational materials about the programme are available throughout the supermarket in the form of brochures, signs and kiosks") Control: N/A (ITS study without control group) |
|
| Outcomes |
Measures of SSB intake: Percentage change of units of SSB with any, zero and 1 ‐ 3 stars sold, assessed continuously throughout the study period with routinely‐collected transaction data Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: Total sales, assessed continuously throughout the study period with routinely‐collected transaction data Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: USA Year(s) when implemented: 2006 ‐ 2007 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Conflict of interest: None" Funding: "The study was supported by the National Institutes of Health (NIH; grant number 1RC1HD063370‐01). The NIH had no role in the design, analysis or writing of this article" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were routinely‐collected sales data. There is no indication that data were not complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Unclear risk | All outcomes mentioned in the Methods section are reported. However, no trial registration is reported, and no information on the availability of a study protocol is provided. Data were provided by the supermarket to the researchers after the intervention took place, and some potentially relevant aspects can not be assessed with the data as they are reported. Quote: "A limitation of the data is that sales are not separately reported for items with one, two and three stars; only for all starred items collectively. The data set does not contain any information about unit sales of unrated items" |
| Independence of the intervention from other changes (performance bias) | Low risk | It seems possible that outside events influenced the results. However, the controls for linear time trends which were included in the ITS analyses strengthen our confidence that these did not substantially bias the effect estimates. Quote: "The main limitation of the present study is the lack of a control group, which restricts our ability to control for the influence of events that occurred around the time of the introduction of the nutrition rating system. (...) One might be concerned that macroeconomic changes could bias these results; e.g. if during an economic downturn people buy fewer low‐nutrient energy‐dense treats. However, our data span 2005–2007, which is before the financial crisis of late 2008 and the ensuing Great Recession; thus, macroeconomic fluctuations are unlikely to bias these results. One might also be concerned that the supermarket chain made other changes at the same time as the nutrition guidance system that influenced shopping patterns, but the supermarket chain reports that it made no other changes to store marketing or merchandising strategies at the time of implementation. Still, it remains possible that some other change took place after September 2006 but before the end of 2007 that influenced shopping decisions as concern more nutritious and less nutritious foods. For example, there may have been an increase in media coverage of the health risks of less nutritious, energy‐dense foods. To allow researchers to difference away the effects of such unobserved factors that may change over time, future studies should include control groups" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention is the point of analysis. Quote: "The regressor of interest is an indicator variable that equals 1 if the week in question is after the implementation of the nutrition rating system (i.e. after September 2006)" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns ‐ in particular, seasonality was taken into account in the analysis. Quote: "All models control for indicator variables for week of year to control for seasonality and a linear time trend" |
Cohen 2015.
| Methods |
Design: Cluster‐RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 14 schools Number of individuals: 2638 Length of intervention: 3 ‐ 4 months (for the smart café intervention, i.e. the intervention of interest to this review) |
|
| Participants |
General description of participants: Elementary and middle school students in Massachusetts, USA Age: Children (average age 12 years, age range 8 to 17 years) Inclusion criteria: Students in grades 1 ‐ 8 attending a participating school and receiving a school meal on a study day Exclusion criteria: Students bringing a lunch from home on a study day or not eating lunch in the cafeteria on a study day Recruitment: Quote: "All students in grades 3 through 8 were given consent forms and surveys requesting demographic information (ie, sex, race/ethnicity, and date of birth). Students in grades 1 through 8 were also recruited using passive consent procedures (no identifying information was collected). The present study focuses primarily on the students with active consents. Consenting students participated if they received a school lunch on a study day (schools had closed campuses)" Weight status at baseline: N/R SSB consumption at baseline: Quote: "[At baseline, m]ost students selected sugar‐sweetened milk (76.0%‐79.1%), with only 9.2% to 9.6% of students taking white milk, and approximately 70% of the milk was consumed overall" Equity considerations: The intervention took place in urban, low‐income school districts. Quote: "Among 2638 students participating in the MEALS Study with active consents (38.4% of eligible participants), approximately half of the participants were female (range, 50.7%‐ 56.0%), and 82.2% to 90.3% were Hispanic. Students were on average 11.5 years old (age range, 8.0‐16.6 years). The percentage of students eligible for free or reduced‐price meals ranged from 86.9% to 95.0%. The student demographics were similar among those with active consents and the general population in participating schools" |
|
| Interventions |
Intervention: Prominent placement of white milk in front of chocolate milk in school cafeterias. (Quote: "The smart café intervention consisted of multiple modifications to the school cafeteria, incorporating choice architecture strategies. A list of previously successful techniques was presented to the participating school districts, and the modifications that both districts agreed on were implemented (the smart café intervention was the same in all schools). (...) To encourage white milk selection, it was placed prominently in front of sugar‐sweetened milk (eg, chocolate milk). All the modifications were simultaneously present and applied daily by existing food service staff for 4 months until the postintervention data collection period. These modifications were monitored regularly by study staff to ensure consistent implementation") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Percentage of students selecting sugar‐sweetened milk, assessed at baseline and at 3‐4 months follow‐up by trained observers following a standardized protocol Measures of intake of alternatives to SSB: Percentage of students selecting white milk, assessed at baseline and at 3 ‐ 4 months follow‐up by trained observers following a standardised protocol Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary and middle schools Sector: Education Country: USA Year(s) when implemented: 2011 ‐ 2012 Mode of implementation: Pilot trial by researchers in co‐operation with a private non‐profit organisation Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Conflict of Interest Disclosures: None reported" Funding: "This study was funded by a grant from Arbella Insurance. Dr Cohen is supported by grant R25 CA 098566 from the Nutritional Epidemiology of Cancer Education and Career Development Program. (...) The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication" Trial registration: ClinicalTrials.gov number NCT02309840 Protocol availability: Published as supplement to the study's primary report |
|
| Notes | The primary report of Cohen 2015 reports on 2 separate interventions: a 'chef intervention', in which schools received a professional chef to improve school meal palatability; and a 'smart café intervention', in which choice architecture techniques were used to increase the consumption of healthier foods and beverages (including white milk) in school cafeterias. We included and report data only on the smart café intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reports that allocation was random, but does not state how the allocation sequence was generated and if it was concealed. Quote: "2 chef schools and 4 control schools were randomly assigned to receive the smart café intervention. The remaining 6 schools continued as controls" |
| Allocation concealment (selection bias) | Low risk | Allocation was by institution (school), and was done at the beginning of the smart café intervention |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | The study does not provide data on baseline beverage consumption separately for the IG and CG |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline differences in socio‐demographic characteristics and baseline outcome measures (other than beverage intake) were assessed and reported, and used for adjustment in the statistical analysis |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete outcome data are mainly a problem for the participants with active consent (for these, attrition was > 60%) ‐ participants with passive consent were redrawn from the student body at each assessment, and it does not seem likely that attrition or other sources of missing outcome data were a problem in this case. While not explicitly stated in the study, results on SSB and white milk selection seem to be based on all students, including those with passive consent only |
| Blinding (performance and detection bias) Objective outcomes | Unclear risk | It is unclear to what degree students were aware of their status as intervention or control; they were certainly aware of the fact that their food and beverage intake was recorded. It is also unclear if the research assistants who did the recording were blinded to the intervention/control status of the individual schools. Quote: "At the beginning of each lunch period, an announcement was made reminding students of the study and that participation was voluntary. After students selected their meals, research assistants standing discreetly by the cafeteria line exits recorded the foods and the tray number. Students with active consents were asked to include their name on their tray" |
| Contamination (performance bias) | Low risk | Allocation was by institution (schools), and it seems unlikely that the CG received the intervention |
| Selective reporting (reporting bias) | Unclear risk | All primary outcomes as described in the protocol are reported; however, for milk consumption the study only reports that no significant effects were observed, and does not provide numerical data |
| Other bias | Low risk | No other concerns |
Collins 2016 SNAP.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 14 sites (2011 ‐ 2014, SNAP only, as reported in Exhibit 1.3, page 31 of the study's primary report) Number of individuals: 25,150 children (2012 ‐ 2013, SNAP only, as reported in Exhibit 4.M, page 143 of the study's primary report) Length of intervention: 2 years (The intervention was implemented during 4 consecutive years, 2011 ‐ 2014, but data on sugar‐sweetened beverage intake were collected in 2012 and 2013 only) |
|
| Participants |
General description of participants: Households with school‐aged children qualifying for free or reduced school meals living in 10 states and Indian Tribal Organisations in the US Age: School‐aged children (pre‐kindergarten to 12th grade) Inclusion criteria: Quote: "The SEBTC [Summer Electronic Benefit Transfer for Children] benefit was provided to households with children who were, in the prior school year, in pre‐kindergarten through 12th grade and certified for free or reduced‐price (FRP) school meals in the school food authorities (SFAs) that participated in the demonstration. All households with at least one child certified for FRP in a participating SFA and who gave consent were included in the demonstration" Exclusion criteria: N/R Recruitment: Quote: "To obtain household consent in the demonstration and evaluation, grantees could choose either an active consent process (i.e., requiring guardians to return consent materials if they desired to be part of the demonstration) or a passive consent process (i.e., requiring guardians to return a pre‐addressed letter if they desired to be excluded). Several grantees in active consent sites had difficulty getting enough guardians to read and return consent forms to meet numbers needed for the demonstration and evaluation. The active consent process is analogous to having households apply for SEBTC, should it be a pilot or an ongoing program" Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: The intervention targeted children qualifying for free or reduced‐price school meals, i.e. at children from lower‐income families. Quote: "Given the rules for participation in the demonstration, it would be expected that households in SEBTC would be relatively more disadvantaged compared to the general population of households with school‐age children. In fact, 71 percent of households in the evaluation had monthly incomes below FPL [federal poverty level] (...). In terms of other household characteristics, the largest group of respondents to the household survey identified themselves as non‐Hispanic white (41.3 percent), with the next largest group being Hispanic (27.3 percent), and then non‐Hispanic black (22.6 percent). In addition, approximately one‐quarter of respondents did not complete high school, approximately one‐third completed high school (or GED [General Educational Development Test]), approximately one‐third had some college, and less than 10 percent had at least a four‐year degree" |
|
| Interventions |
Intervention: Monetary transfers to low‐income households with children, which could be used to purchase foods and beverages including SSB (following the rules of the Supplemental Nutrition Assistance Program, SNAP). Quote: "In the summers of 2011 and 2012, for households that were randomly selected, a value of $60 per eligible child per month was provided on an EBT [electronic benefit transfer] card when schools were not in session (prorated for partial summer months). In 2013, FNS [Food and Nutrition Service, a division of the US Department of Agriculture] added a third demonstration year and consenting households were randomly selected to receive either the $60 monthly benefit per eligible child or a $30 monthly benefit per child. (...) Benefits for SEBTC followed the general program rules of either the SNAP or WIC, depending upon the model selected by the grantee. Consequently, in the sites using the SNAP EBT systems to deliver SEBTC, participants could redeem benefits for SNAP‐eligible foods at any SNAP‐authorized retailer in the nation” Behavioural co‐intervention: None, but some sites provided a limited amount of nutrition information. Quote: "After households received their EBT cards and were issued benefits, grantees provided support to families as families attempted to use their cards. All grantees used new or existing help‐lines to respond to questions. In addition, half the grantees provided other supports to families, including SEBTC‐specific websites, a Facebook page where the grantee posted program updates and healthy recipes, and Hunger Helpline numbers to assist households with finding SFSP sites" Control: No or alternative intervention. Quote: "In the summers of 2011 and 2012, for households that were randomly selected, the value of SEBTC was $60 per eligible child per month; other households received no SEBTC benefit. In 2013, there were two benefit levels; households were randomly selected to receive either a $60 monthly benefit per eligible child benefit or a $30 monthly benefit per child per month benefit" |
|
| Outcomes |
Measures of SSB intake: Sugar from SSB, assessed with a food‐frequency questionnaire based on the National Health and Nutrition Examination Survey (NHANES) Multifactor Diet Screener at baseline and during the intervention Measures of intake of alternatives to SSB: Share of participants usually drinking non‐fat or low‐fat milk, assessed with a food‐frequency questionnaire based on the National Health and Nutrition Examination Survey (NHANES) Multifactor Diet Screener at baseline and during the intervention Anthropometric measures: N/R Adverse outcomes: N/R Other outcomes: Total added sugar intake |
|
| Context and implementation |
Setting: Social Policy Sector: Food assistance programmes Country: USA Year(s) when implemented: 2011 ‐ 2014 Mode of implementation: Government pilot project Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "No financial disclosures were reported by the authors of this paper" Funding: "The 2010 Agriculture Appropriations Act (P.L. 111‐80) authorized and provided funding for USDA to implement and rigorously evaluate the Summer Food for Children Demonstrations" Trial registration: ClinicalTrials.gov registration NCT02877147 Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study report that allocation was random, but does not provide details on allocation sequence generation and concealment. Quote: "[T]he evaluation team randomly assigned households in participating sites in 2011, 2012, and 2013. (...) Households that had one or more children certified for FRP meals and consented were randomly assigned either to a benefit group that received the SEBTC benefit or to a non‐benefit group that did not in 2011 and 2012, or to one of the two benefit groups with different levels of benefits in 2013" |
| Allocation concealment (selection bias) | Unclear risk | See quote above |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "Observation of field operations and comparisons of baseline characteristics support the belief that the randomly‐assigned groups used in the evaluation are equivalent. (See Appendix 3, Exhibits 4.E–4.H for baseline means of food security; household characteristics (e.g., household size, household composition, number of children; household income); respondent characteristics (i.e., race/ethnicity, education level); and participation in nutrition assistance programs (e.g., SNAP, WIC, NSLP, SBP) in each year stratified by treatment condition))" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | See quote above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was similar across treatment conditions, and intention‐to‐treat analyses were performed. Quote: "Overall response rates in summer 2012 were 73 percent; in 2013 the summer response rate was 88 percent. Response rates were similar across treatment condition (a four percentage point difference in 2012 and virtually no difference in 2013) (...). In addition, all analyses used weights that adjusted for the sampling approach and for the differences in survey response rates associated with measured differences in household characteristics. Finally, crossover (i.e., households receiving benefits other than what was intended based on their randomization status) was minimal ‐ well under 0.1%; hence, households were analyzed according to their random assignment status even when crossover occurred (i.e., an intention‐to‐treat analysis was conducted)" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and outcomes are self‐reported |
| Contamination (performance bias) | Low risk | It is unlikely that the IG received the intervention |
| Selective reporting (reporting bias) | Low risk | Analysis plans were prespecified, and all outcomes mentioned in the Methods section are reported |
| Other bias | Low risk | No other concerns |
Collins 2016 WIC.
| Methods |
Design: See Collins 2016 SNAP Timing: See Collins 2016 SNAP Allocation to group: See Collins 2016 SNAP Number of clusters or sites: 14 sites (2011 ‐ 2014, WIC only, as reported in Exhibit 1.3, page 31 of the study's primary report) Number of individuals: 18,207 children (2012 ‐ 2013, WIC only, as reported in Exhibit 4.M, page 143 of the study's primary report) Length of intervention: See Collins 2016 SNAP |
|
| Participants | See Collins 2016 SNAP | |
| Interventions |
Intervention: Monetary transfers to low‐income households with children, which could be used to purchase a limited range of foods and beverages, excluding SSB (following the rules of the Special Supplemental Nutrition Program for Women, Infants, and Children, WIC). Quote: "In the summers of 2011 and 2012, for households that were randomly selected, a value of $60 per eligible child per month was provided on an EBT [electronic benefit transfer] card when schools were not in session (prorated for partial summer months). In 2013, FNS [Food and Nutrition Service, a division of the US Department of Agriculture] added a third demonstration year and consenting households were randomly selected to receive either the $60 monthly benefit per eligible child or a $30 monthly benefit per child. (...) Benefits for SEBTC followed the general program rules of either the SNAP or WIC, depending upon the model selected by the grantee. (…) [A]s in the main WIC program, in the sites using the WIC EBT system to deliver SEBTC, participants could redeem benefits only for a limited set of foods and only at WIC‐authorized retailers. The SEBTC WIC package was specified by FNS based on existing WIC food packages for preschool children, but adjusted to accommodate the nutritional needs of the older (i.e., school age) children participating in SEBTC. For both the $60 and $30 packages, grantees implementing the WIC approach also worked with FNS to customize the package to meet the tastes of the local population and so that the foods and amounts in the package would fit within the expected cost considering local food costs and availability of items in the SEBTC WIC package (e.g., some sites substituted whole grain tortillas for whole wheat bread)" Behavioural co‐intervention: See Collins 2016 SNAP Control: See Collins 2016 SNAP |
|
| Outcomes | See Collins 2016 SNAP | |
| Context and implementation | See Collins 2016 SNAP | |
| Declarations | See Collins 2016 SNAP | |
| Notes | See Collins 2016 SNAP | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | See Collins 2016 SNAP |
| Allocation concealment (selection bias) | Unclear risk | See Collins 2016 SNAP |
| Similarity of baseline outcome measurements (selection bias) | Low risk | See Collins 2016 SNAP |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | See Collins 2016 SNAP |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | See Collins 2016 SNAP |
| Blinding (performance and detection bias) Subjective outcomes | High risk | See Collins 2016 SNAP |
| Contamination (performance bias) | Low risk | See Collins 2016 SNAP |
| Selective reporting (reporting bias) | Low risk | See Collins 2016 SNAP |
| Other bias | Low risk | See Collins 2016 SNAP |
Cornelsen 2017.
| Methods |
Design: ITS Timing: Retrospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 37 restaurants Number of individuals: N/A (the analysis is based on routinely‐collected sales data not linked to individual participants) Length of intervention: 24 weeks |
|
| Participants |
General description of participants: Customers of restaurants belonging to the Jamie's Italian chain in 27 cities in the UK Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: At baseline, the mean number of SSBs sold per customer was 0.17, and SSBs were the most commonly purchased non‐alcoholic beverage Equity considerations: N/R |
|
| Interventions |
Intervention: A price increase on SSB in chain restaurants with accompanying menu changes and further activities. (Quote: "On the 1 September 2015, Jamie’s Italian, a national chain of UK restaurants, added a £0.10 levy to the price of non‐alcoholic SSBs sold within them. The prelevy price of SSBs ranged from £2.60 to £3.25 (excluding the levy), thus addition of the levy equated to a price increase of 3.1%–3.8%. Other non‐alcoholic beverages were similar in price, ranging from £2.00 and £3.95. In combination with the introduction of the levy, Jamie’s Italian reorganised the non‐alcoholic beverage menu into two sections: SSBs and other beverages (juices, bottled waters and diet cola). In addition, fruit spritzers (fruit juice mixed with water) were added to the main non‐alcoholic beverage menu. Text (…) on the SSB section of the non‐alcoholic beverage menu explained the decision to implement the levy and that proceeds from the levy would go directly to a Children’s Health Fund that offered grants for children’s health initiatives. Introduction of the levy was supported by a Channel 4 television documentary ‘Jamie’s Sugar Rush’, first broadcast on 3 September 2015. Thus, the levy can be seen as a complex ‘intervention’ comprising a fiscal component (a price rise) in combination with other non‐fiscal components that could plausibly help reduce purchases of SSBs") Behavioural co‐intervention: A television documentary on sugar (see quote above) Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Mean number of on‐ and off‐menu SSBs sold per customer, assessed continuously throughout the study period with routinely‐collected electronic sales data Measures of intake of alternatives to SSB: Mean number of bottled water, diet beverages, and juices sold per customer, assessed continuously throughout the study period with routinely‐collected electronic sales data Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Restaurants Sector: Food service Country: UK Year(s) when implemented: 2015 ‐ 2016 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Competing interests: None declared" Funding: "This study was funded by the UK National Institute of Health Research (PHR 15/124/01) and the UK Medical Research Council (MRC Strategic Skills Fellowship to LC). JA and MW are funded by the Centre for Diet and Activity Research (CEDAR), a UKCRC Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were routinely‐collected itemised electronic point‐of‐sale sales data, and are described as complete. However, no data on tap water orders were collected, as these were served for free and not registered, and "[a] further 1.3% of all drinks sold during the study period were excluded as they did not fit the categories above (eg, slim‐line tonics, smoothies and cordial drinks)" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Low risk | Quote: "The evaluative study was conceived postimplementation of the levy. The authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. SC confirms that the manuscript is an honest, accurate and transparent account of the study being reported; no important aspects of the study have been omitted; and any discrepancies from the study as planned have been explained" |
| Independence of the intervention from other changes (performance bias) | Low risk | Quote: "Our analyses show a step decrease in number of SSBs sold per customer, and sensitivity analyses suggests this decrease occurred at time of implementation. This locates our observed changes at the point of the intervention’s introduction and strengthens the case for it being the likely explanation for our observed changes, rather than a general secular decline or as a result of other unobserved external factors" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention is the point of analysis: Quote: "As the implementation date (1 September 2015) of the levy fell in the middle of a 4‐week accounting period, data for that period were split into 2‐week periods to allow for the specification of an exact implementation date in analyses. (...) Changes in non‐alcoholic beverage sales associated with the intervention in the ITS were modelled as an immediate step change in the log‐transformed number of beverages sold per customer. The step change was defined as a categorical variable equal to zero before implementation (up to 31 August) and one afterwards. This assumes an immediate and stable effect of the intervention. We did not analyse changes in trends as the postintervention period was too short for meaningful interpretation" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | Analyses adjusted for seasonality: Quote: "Estimates using weekly data were adjusted for time trend in number of beverages sold per customer and estimates using 4 weekly data additionally adjusted for quarterly seasonal effects" |
Cradock 2011.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: Quote: "This quasi‐experimental evaluation study design contrasted local trends in consumption of sugar‐sweetened beverages, measured before and after the policy change was implemented, with national trends in consumption among high‐school–aged adolescents" Number of clusters or sites: This was a repeat cross‐sectional analysis. In the IG students from 17 high schools were sampled at baseline, and students from 18 high schools were sampled at follow‐up. In the CG, data were not collected at the cluster level Number of individuals: This was a repeat cross‐sectional analysis. At baseline, 895 students were included in the IG, and 1196 in the CG. At follow‐up, 1138 students were included in IG, and 1233 in the CG (see tables 1 and 3 of the study's primary report). Length of intervention: 2 years (in the IG, baseline data collection took place from February to April 2004, and follow‐up data collection from February to April 2006. In the control group, baseline data were collected in 2003 ‐ 2004, and follow‐up data in 2005 ‐ 2006) |
|
| Participants |
General description of participants: High‐school students in grades 9 through 12 in Boston, USA Age: Teenagers (no details on the age reported; IG participants were 9th to 12th grade students, and CG participants were aged 15 ‐ 19 years) Inclusion criteria: Quote: "Students [in the IG] with complete data on demographic covariates and consumption of sugar‐sweetened beverages were included in this analysis" Exclusion criteria: Quote: "We excluded from analysis [of participants in the CG] data from respondents who self‐identified as 'other' race/ethnicity because of the small sample size" Recruitment: The study is based on data from the Boston Youth Survey conducted by the City of Boston and the Harvard Youth Violence Prevention Center, as well as on nationally representative data from the National Health and Nutrition Examination Survey conducted by the National Center for Health Statistics in the USA. The study's primary report does not provide details on recruitment, but includes references to relevant publications Weight status at baseline: N/R SSB consumption at baseline: Baseline SSB consumption was 607 ml/day in the IG, and 618 ml/day in the CG Equity considerations: Quote: "The student body [in the IG] is diverse: 37% of students are black, 39% are Hispanic, 13% are white, and 9% are Asian, and approximately 74% of students are eligible for free or reduced‐price meals" |
|
| Interventions |
Intervention: Reduced availability of SSB at schools. (Quote: "In Boston, a policy that restricts the sale of sugar‐sweetened beverages in vending and à la carte settings was approved by the Boston School Committee in June 2004 and initiated with the fall 2004 school year. The new Boston Public Schools Snack and Beverage Policy and subsequent detailed implementation guidelines required that beverages sold in schools or on school grounds adhere to the Massachusetts à la Carte Food and Beverage Standards to Promote a Healthier School Environment published by Massachusetts Action for Healthy Kids. The beverage guidelines specifically precluded the sale of soft drinks, fruit drinks (ie, non–100% vegetable or fruit juice beverages), and sports drinks anywhere in school buildings or on school campuses and had specifications that limited other beverage serving sizes") Behavioural co‐intervention: Nutrition education and awareness‐raising (Quote: "The passage of the Boston Public Schools beverage policy was the beginning of more widespread focus on promoting more healthful foods and beverages in Boston and Boston schools. For example, further initiatives included the implementation of nutrition‐related curricula in middle and primary schools and interdepartmental committees and collaborations charged with monitoring implementation and acceptance of related policy guidelines. Awareness‐raising activities in the Boston Public Schools system included a presentation of the new policy guidelines to principals before implementation, parent workshops on healthful snack choices, dissemination of pamphlets to teachers and school staff detailing alternatives for fundraising, and a brochure for school administrators and teachers entitled Healthy Beverages and Snack News. Boston city officials also negotiated new procurement contracts with vendors who would supply the new more healthful options to schools, and school vending machines were stocked with water and 100% juice instead of sugar‐sweetened beverages") Control: No, minimal or alternative intervention (the study compares trends in Boston (the IG) with nationally representative data from NHANES) |
|
| Outcomes |
Measures of SSB intake: Intake of SSB in servings/day, assessed through a 7‐day dietary recall (IG) and a 24‐hour dietary recall (CG), at baseline and 2 years post‐intervention Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: Substitution effects, assessed by noting that total SSB intake (including SSB intake outside school) decreased after access to SSB at school was restricted (Quote: "Boston’s results also suggest that youth may not compensate for in‐school restrictions on sugar‐sweetened beverages by increasing consumption outside of school") Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2004 ‐ 2006 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This work was supported by cooperative agreement nos. U48/DP000064 and 1U48DP001946 (including the Nutrition and Obesity Policy Research and Evaluation Network) from the Centers for Disease Control and Prevention; a Steps to a Healthier US grant to the Boston Public Health Commission; and the Robert Wood Johnson Foundation (nos. 260639, 61468, and 66284)" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline outcome measurements were similar (baseline SSB consumption was 607 ml/day in the IG, and 618 ml/day in the CG) |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Baseline differences were substantial. Differences in observed baseline characteristics were taken into account in the analysis, but unobserved baseline differences seem likely. Quote: "We used linear regression analysis to examine changes in mean servings per day of sugar‐sweetened beverages between 2004 and 2006, adjusting for potential differences in student composition. In regression models, we estimated change in consumption via an indicator variable identifying surveys completed in 2006 (postpolicy change; 2004 survey was reference), controlling for respondents’ sex, grade, race/ethnicity, and primary neighborhood of residence" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | This was a repeat‐cross‐sectional analysis, samples were chosen to ensure representativeness, and missing data seem unlikely to have substantially affected the results. Quote: "In 2004 and 2006, respectively, 3.5% and 2.8% of respondents were missing data on consumption of sugar‐sweetened beverages. (...) Regression analysis including covariates for age, sex, and race/ethnicity (non‐Hispanic white, non‐Hispanic black, and Mexican American) accounted for potential differences in the sample population demographics across the 2 survey periods" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Outcomes were self‐reported, and participants were not blinded |
| Contamination (performance bias) | High risk | The IG and CG were overlapping, and it is likely that parts of the CG received the intervention. This would have biased the observed effects towards null. Other cities and states in the USA, forming part of the CG, may have implemented policies aimed at reducing the consumption of SSB during the study period |
| Selective reporting (reporting bias) | Low risk | All results mentioned in the Methods section are reported. No outcome measures one would expect in a study of this kind are missing |
| Other bias | High risk | Data were not collected in parallel in the IG and CG, and data collection methods differed substantially. Quote: "Furthermore, NHANES and Boston Youth Survey estimates of consumption of sugar‐sweetened beverages are not directly comparable because of differences in wording and data collection methods" |
Da Costa 2014.
| Methods |
Design: Cluster‐RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 20 schools Number of individuals: 2155 Length of intervention: 9 months |
|
| Participants |
General description of participants: Evening‐class students in public high schools in Florianopolis and Recife, Brazil Age: Teenagers and young adults (age range 15 to 24 years) Inclusion criteria: N/R Exclusion criteria: N/R Recruitment: N/R Weight status at baseline: The baseline prevalence of overweight was 17% in the CG and 19% in the IG in Florianopolis, and 26% in the CG and 31 in the IG in Recife SSB consumption at baseline: Mean SSB consumption (days per weeks on which any SSB is consumed) was 3 in both the IG and CG Equity considerations: In the IG, 59% of participants were female, 46% were working and 40% were white; in the CG, 53% were female, 48% were working, and 44% were white |
|
| Interventions |
Intervention: Fruit provision in schools. (Quote: "The following components made up the intervention and measures to promote healthy eating habits with an emphasis on increased fruit and vegetable consumption: a) The food education and physical education component: food and vegetable posters, four newsletters for the entire school community and the project website; b) Environmental and organizational change component: weekly distribution of three types of seasonal fruit during school lunch; c) Personnel engagement and training: with school employees, emphasizing the choice of healthy foods, in addition to the purchase, cleaning and provision fruits during class breaks") Behavioural co‐intervention: Nutrition education and skills building (see quote above) Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB intake, assessed at baseline and at 9 months follow‐up with a validated questionnaire "administered in a classroom by a trained team of undergraduate and graduate Physical Education students" Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: High schools Sector: Education Country: Brazil Year(s) when implemented: 2006 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This study was financed by Healthy Lifestyles, the Healthy People Project of the International Life Sciences Institute Research Foundation (ILSI RF), Pan American Health Organization (PAHO), and the US Centers for Disease Control and Prevention (CDC). We also received financial assistance from CNPq (Ministry of Science and Technology, Brazil), Universidade Federal de Santa Catarina (UFSC), and Universidade de Pernambuco (UPE)" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Next, we randomly assigned the schools in each pair to the control or intervention group by flipping a coin" |
| Allocation concealment (selection bias) | Low risk | Allocation was by institution (school), and allocation was done at the start of the study |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | The way data on SSB intake are presented does not allow clear conclusions regarding baseline differences. Table 2 of the study's primary report suggests that SSB intake was identical across all measurements (IG versus CG and pre‐ versus post‐intervention); this, however, seems to contradict the statement from the study text that there was a significant effect on SSB intake |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Baseline characteristics differed substantially between IG and CG, and it is not clear if these were taken into account in the analyses on which the study's conclusions about SSB intake are based |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analyses were intention‐to‐treat, but attrition was high (54%) and dropouts differed from those remaining in the study. Quote: "Participants and dropout students differed according to their gender, work status and use of illicit drugs" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and outcomes are self‐reported |
| Contamination (performance bias) | Low risk | Quote: "Contamination of the CG is also highly unlikely, considering the type of intervention used, as well as the little contact expected between the groups due to the profile of the population investigated" |
| Selective reporting (reporting bias) | Unclear risk | The way data on soft drink consumption is presented does not allow clear conclusions regarding the magnitude of effects. Important information on how data was collected and analysed is missing. Reporting may be selective |
| Other bias | Unclear risk | This was a cluster‐RCT, and it is not reported if clustering was taken into account in the analysis |
Ebbeling 2006.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 103 Length of intervention: 25 weeks |
|
| Participants |
General description of participants: Teenagers consuming at least 360 mL SSB per day living in Boston, Massachusetts, USA Age: Teenagers (an age of 13 to 18 years was an eligibility criterion, and mean age was 16 years) Inclusion criteria: Quote: "We enrolled 103 adolescents (47 males and 56 females), aged 13 to 18 years, who reported consuming at least 1 serving (ie, 360 mL or 12 fl oz) per day of SSB (ie, soft drinks, juice drinks containing <100% juice, punches, lemonades, iced teas, and sports drinks). Each subject lived predominantly in 1 household (ie, no more than 1 weekend every 2 weeks in a secondary household)." Exclusion criteria: Quote: "We excluded those who were currently dieting for the purpose of weight loss or taking prescription medications that might affect body weight. We also did not enroll those who reported smoking at least 1 cigarette in the past week or were diagnosed as having a major medical illness or eating disorder. To decrease the likelihood of enrolling individuals with eating disorders or undernutrition, we excluded those with a BMI below the 25th percentile" Recruitment: "Recruitment and screening of subjects were conducted in collaboration with a local high school that provided mailing lists and space for obtaining measurements. Packets containing an invitation letter and informed consent and assent documents were sent to parents of all students enrolled at the school" Weight status at baseline: Body weight at baseline was not an inclusion criterion, and mean BMI at baseline was 26 kg/m2 in the IG and 25 kg/m2 in the CG. Study authors did a sub‐group analysis according to weight status SSB consumption at baseline: Consumption of at least 360 mL per day of SSB was an inclusion criterion. Mean energy intake from SSB at baseline was 1466 kJ/day in the intervention and 1596 kJ/day in the control group Equity considerations: Participants lived in Boston, USA, included 65% non‐white participants, and 18% participants residing in subsidized housing. Quote: "The results of our pilot study were not materially affected by gender, race or ethnicity, age, household income, household size, physical activity, or television viewing" |
|
| Interventions |
Intervention: Home‐delivery of non‐caloric beverages (Quote: "The intervention group received weekly home deliveries of noncaloric beverages for 25 weeks. The target number of individual beverage servings (ie, 360 mL or 12 fl oz per referent serving) delivered to each home was based on household size: 4 servings per day for the subject and 2 servings per day for each additional member of the household. This extra allotment was provided to avoid competition between the subject and family members for the beverages. We distributed an order form to each household for selecting beverage preferences from a wide variety of options (eg, bottled water and “diet” beverages including soft drinks, iced teas, lemonades, and punches). The beverage order form listed options in units, based on manufacturer packaging. The units contained bundles of 4 to 6 cans or bottles, with volumes ranging from 300 to 720 mL (10–24 fl oz) per can or bottle. The target number of delivered servings, specified above, was approximately equal to 5 units per week for the subject and 3 units per week for each additional member of the household. A regional supermarket delivery service filled the orders and delivered the beverages, with research staff coordinating and monitoring the process") Behavioural co‐intervention: Dietary counselling focused on beverages ("We instructed subjects to drink the noncaloric beverages delivered to their homes and not to buy or drink SSBs. In addition, we offered advice on how to choose noncaloric beverages when not at home. (...) Written instructions regarding beverage consumption were mailed to subjects at the beginning of the intervention period. We also contacted each household by telephone during the first week of the intervention to speak with the subject and a parent. This telephone contact provided an opportunity to reinforce instructions, answer questions, and address concerns. Thereafter, we contacted each subject by telephone on a monthly basis throughout the intervention period to assess satisfaction with beverage choices and deliveries, discuss beverage consumption, and provide motivational counseling") Control: No intervention (Quote: "We asked subjects in the control group to continue their usual beverage consumption habits throughout the 25‐week intervention period. They received weekly home deliveries of noncaloric beverages for 4 weeks after completion of follow‐up measurements, as a benefit for having participated in the study") |
|
| Outcomes |
Measures of SSB intake: Energy intake from SSB (kJ/day) as change from baseline, assessed through multiple‐pass dietary recall at baseline and 25 weeks Measures of intake of alternatives to SSB: Non‐caloric beverage intake (ml/day) as change from baseline, assessed through multiple‐pass dietary recall at baseline and 25 weeks Anthropometric measures: Mean BMI as change from baseline, assessed through a standardized diagnostic protocol at baseline and 25 weeks Adverse outcomes: The study does not report how data on adverse outcomes were collected, but states that none were observed Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: USA Year(s) when implemented: 2003‐2004 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The authors have indicated they have no financial relationships relevant to this article to disclose" Funding: "This study was supported by grants R01 DK63554 and K01 DK62237 from the National Institute of Diabetes and Digestive Kidney Diseases, the Charles H. Hood Foundation, and grant M01 RR02172 awarded by the National Institutes of Health to support the General Clinical Research Center at Children's Hospital Boston" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | We contacted the study's corresponding author for additional information on the randomization procedure, which is not described in detail in the study's published report, and received the information that a computer random number generator was used to create the list of assignments. Quote: "To determine the experimental groups, we used a computer random number generator to prepare a list of assignments, mixed in random order. These were concealed until an enrollment list had been obtained from each participating school. We then juxtaposed the participant list with the assignment list to define the groups" |
| Allocation concealment (selection bias) | Low risk | Quote: "To avoid any bias in the enrollment procedure, personnel conducting recruitment were masked to sequence" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "There were no significant group differences between intervention and control subjects in (...) anthropometrics (weight, height, and BMI). Likewise, the groups did not differ in baseline levels of daily EISSB [energy intake from SSB], noncaloric beverage intake, physical activity, television viewing, or total media time" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Quote: "There were no significant group differences between intervention and control subjects in demographics (gender, race, ethnicity, age, household income, and household size)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was not attrition |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Dietary intake was self‐reported, and blinding of participants was not possible (interviewers were, however, masked to group assignment) |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but the outcome (BMI) was objective and assessed based on a standardized clinical protocol |
| Contamination (performance bias) | Low risk | It is unlikely that the CG received the intervention |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section are reported; moreover, the study reports all outcomes one would generally expect in such a study. However, no information on study registration is provided |
| Other bias | Low risk | No other concerns |
Ebbeling 2012.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 217 Length of intervention: 12 months (+ 12 months additional follow‐up after the end of the intervention) |
|
| Participants |
General description of participants: Teenagers consuming at least 360 ml SSB of 100% fruit juice a day, and with a BMI at or above the 85th percentile for sex and age, living in Boston, Massachusetts, USA Age: Teenagers (mean age was 15 years) Inclusion criteria: Quote: "Enrolled in grade 9 or 10 (or entering grade 9 or 10, if recruited during the summer); BMI ≥ 85th percentile for sex and age; Residing in predominately one household (no more than one weekend every 2 weeks in a secondary household), with access to a working telephone; Consumption of 12 fluid ounces or more of sugar‐sweetened beverages (including 100% fruit juice) per day" (quote from the study protocol) Exclusion criteria: Quote: "Siblings participating in the study; Intention to change location of residence during the 2 years post‐randomization; Plans to be away from home for 5 weeks or longer during the study period; Physician diagnosis of a major medical illness or eating disorder; Chronic use of any medication that may affect body weight or composition; Current smoking (1 cigarette in the past week); Physical, mental, or cognitive handicaps that prevent participation" (quote from the study protocol) Recruitment: Quote: "We use a multifaceted screening, recruitment, and enrollment strategy. Collaboration with six area high schools to advertise the study to students is our primary method of recruitment. To enhance enrollment, we also recruit from a pediatric dental clinic and use flyers posted in locations other than schools (e.g., community clinics, libraries, community centers) and newspaper or Internet advertisements" Weight status at baseline: Overweigth and obese (a BMI at or above the 85th percentile for sex and age was an inclusion criterion; at baseline, in the IG 36% were overweight and 64% were obese, and in the CG 39% were overweight and 61% were obese) SSB consumption at baseline: Consumption of 12 fluid ounces or more of sugar‐sweetened beverages (including 100% fruit juice) a day was an inclusion criterion. Mean SSB consumption at baseline was 1.7 servings/day in the intervention and control group Equity considerations: Participants were adolescents living in Boston, USA. The sample was ethnically diverse (approximately 24% black, 22% Hispanic, 35% non‐Hispanic white, 17% multiple or other), and high‐, middle‐ and low‐income households were represented in roughly equal parts |
|
| Interventions |
Intervention: Home delivery of low‐calorie beverages (Quote: "The 1‐year intervention consisted of home delivery of noncaloric beverages (e.g., bottled water and 'diet' beverages) every 2 weeks") Behavioural co‐intervention: Dietary counselling focused on beverages (The intervention included "monthly motivational telephone calls with parents (30 minutes per call), and three check‐in visits with participants (20 minutes per visit). Written intervention messages with instructions to drink the delivered beverages and not to buy or drink sugar‐sweetened beverages were mailed to participants. Unsweetened water was recommended over artificially sweetened beverages. Discussions during telephone calls and check‐in visits focused exclusively on beverage consumption, with no attention to other dietary behaviors or to physical activity") Control: No intervention (Quote: "We mailed $50 supermarket gift cards to participants in the control group at 4 and 8 months as a retention strategy but did not provide instructions on what to purchase with the cards") |
|
| Outcomes |
Measures of SSB intake: SSB intake (servings/day) and energy intake from SSB (kcal/day), assessed through 24‐hour dietary recall at baseline, 1 year (the end of the intervention) and 2 years (1 year after the end of the intervention) Measures of intake of alternatives to SSB: Intake of fruit juice, unsweetened beverages and artificially sweetened beverages (servings/day), reported separately, assessed through 24‐hour dietary recall at baseline, 1 year (the end of the intervention) and 2 years (1 year after the end of the intervention) Anthropometric measures: BMI, assessed by a trained dietitian following a standardised diagnostic protocol at baseline, 1 year (the end of the intervention) and 2 years (1 year after the end of the intervention) Adverse outcomes: Data on adverse outcomes were collected during motivational phone calls which were conducted at various time points during the study period with the parents of participating teenagers Other outcomes: Total energy intake (kcal/day) and sugar intake (g/day), assessed through 24‐hour dietary recall at baseline, 1 year (the end of the intervention) and 2 years (1 year after the end of the intervention) |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: USA Year(s) when implemented: 2007 ‐ 2011 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: None (the study report has no COI section but refers to disclosure forms published online; these did not indicate any relationship deemed relevant by the review authors) Funding: "Supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK073025 and K24DK082730, to Dr. Ludwig) and from the National Center for Research Resources to the Boston Children's Hospital General Clinical Research Center (M01RR02172), the Harvard Catalyst Clinical and Translational Science Center (UL1RR025758), and the New Balance Foundation. The observational study was supported by grants from the National Institute of Child Health and Human Development (HD30780), the Centers for Disease Control and Prevention (1U48DP001946), and the Robert Wood Johnson Foundation (66284)" Trial registration: ClinicalTrials.gov number NCT00381160 Protocol availability: Publicly available online as supplement to the published report |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from the published protocol: "We use specialized software to generate a stratified random sequence of assignments" |
| Allocation concealment (selection bias) | Low risk | Quote from the published protocol: "Upon confirmation of eligibility, the system retrieves the next assignment from the stored sequence (...) and transmits that assignment to unmasked intervention personnel for further action" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "At baseline, there were no significant differences between the experimental and control groups with regard to demographic characteristics (...) or other variables" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | See quote above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quotes: "The retention rate for study participants was 97% at 1 year and 93% at 2 years (...), with no significant difference between groups in the percentage of participants available at 2 years for assessment of the primary outcome (P=0.29). (...) Missing values for BMI were conservatively imputed by assuming that the participant's BMI z score was unchanged from baseline and calculating BMI at the appropriate later age from national norms. Other methods for treating missing data, including use of the immediately preceding BMI z score, produced similar results" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Dietary intake was self‐reported, and blinding of participants was not possible. Quote: "Subjects and staff implementing the beverage delivery are not masked to group assignment" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but the outcome (BMI) was objective and assessed based on a standardised clinical protocol. Personnel who assessed study outcomes was blinded. Quote: "All personnel who assess study outcomes are masked to group assignment" |
| Contamination (performance bias) | Low risk | It seems unlikely that a relevant degree of contamination occurred. Quote from the published protocol: "Given (...) concern for contamination between experimental and control groups, only one child per family is enrolled in the study" |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcomes mentioned in the protocol are reported |
| Other bias | Unclear risk | Quote: "However, we recognize that the intensity of the intervention, rather than provision of noncaloric beverages per se, may have led to salutary changes in other behaviors, such as decreased television viewing, and that these changes may affect body weight" |
Elbel 2013.
| Methods |
Design: CBA Timing: Prospective Allocation to group: Quote: "Consumers’ changes in fast‐food purchasing behaviors were examined in Philadelphia before and after calorie labeling was implemented, and these outcomes were simultaneously compared to consumer purchases in a comparison city that did not implement labeling. Baltimore was selected as the city most comparable to Philadelphia by calculating Euclidean distances between Philadelphia and each of the largest 100 US cities using standardized city‐level measures derived from Census 2000 data, including population size, poverty, unemployment, education, race/ethnicity, and income measures" Number of clusters or sites: 23 restaurants located in 2 cities and belonging to 2 fast‐food chains Number of individuals: 1032 at baseline, and 1051 at follow‐up (this was a repeat cross‐sectional analysis, in which participants were redrawn from the population at each time point) Length of intervention: 4 months |
|
| Participants |
General description of participants: Customers of the 2 fast‐food restaurant chains McDonalds and Burger King in Philadelphia (the IG) and Baltimore (the CG), USA Age: Adults (participants were roughly evenly distributed by age group, see table 1 of the study's primary report) Inclusion criteria: See recruitment Exclusion criteria: See recruitment Recruitment: Restaurant‐level (quote): "For the consumer survey fast food restaurants in Philadelphia and Baltimore were matched based on the comparability of ZIP code level demographics. Based on the top matches two of the largest fast food chains in the US were selected: McDonald’s and Burger King. Initially 28 restaurants were selected; as some managers asked not to survey their customers, the final sample was from 23 of them." Customer‐level (quote): "Research staff stood outside the busiest doorway of each fast food restaurant during lunch (approximately 11:30 am‐2:30 pm) or dinner (approximately 5:00 pm‐8:00 pm) hours, and approached every customer appearing 18 years and older by asking them to bring their itemized receipt back to us in exchange for $2. Any customer aged 18‐64 with any food or beverage purchased was eligible; older consumers were excluded as they are most likely to be on a special diet. For customers who returned with their receipt, research staff asked a short series of questions" Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: "Sample members were roughly evenly distributed by age, with slightly more males (51‐56%, depending on city and time period) than females. The sample was predominantly Black (70%), and the majority of sample members had a high school education or lower" |
|
| Interventions |
Intervention: Menu‐board calorie labelling in chain restaurants. (Quotes: "Researchers sought to determine whether a city‐mandated policy requiring calorie labeling at fast food restaurants was associated with consumer awareness of labels, calories purchased and fast food restaurant visits. No restaurants in the study presented calories on their menu board before the labeling regulation officially began (though calories may have been on food wrappers, tray liners or other less prominent places), and all restaurants in Philadelphia adopted this policy afterwards") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Mean calories from beverages purchased per fast‐food restaurant visit, assessed by customer intercept and receipt collection at baseline and 4 months Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes that the number of fast‐food restaurant visits, assessed with a random‐digit‐dialled landline telephone survey of residents within the city limits of Philadelphia and Baltimore at baseline and 4 months, increased in some subgroups Other outcomes: Mean calories from foods and beverages purchased per fast‐food restaurant visit, assessed by customer intercept and receipt collection at baseline and 4 months |
|
| Context and implementation |
Setting: Fast‐food restaurants Sector: Food service Country: USA Year(s) when implemented: 2009 ‐ 2010 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "Disclosure: The authors have no competing interests" Funding: N/R Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Average total calories purchased per transaction were different between the IG and CG, even after adjustment (weighting) for covariates (see table 4 of the study's primary report). For average beverage calories purchased per transaction (the primary outcome of interest to this review) baseline measurements are not reported. Quote: "Because of the imperfect covariate balance by case status and time period (...), the sample was weighted via inverse probability of treatment weights" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baltimore was selected as comparison city based on measures such as population size, poverty, unemployment, education, race/ethnicity, and income measures, and the sites for the consumer receipt survey were matched based on ZIP code‐level demographics. Quotes: "Baltimore was selected as the city most comparable to Philadelphia by calculating Euclidean distances between Philadelphia and each of the largest 100 US cities using standardized city‐level measures derived from Census 2000 data, including population size, poverty, unemployment, education, race/ethnicity, and income measures. (...) For the consumer survey fast food restaurants in Philadelphia and Baltimore were matched based on the comparability of ZIP code‐level demographics. Based on the top matches two of the largest fast food chains in the US were selected: McDonald's and Burger King" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | This was a repeat cross‐sectional analysis, the same data collection procedures were used at baseline and follow‐up in the IG and CG and it seems unlikely that the intervention substantially affected data collection. Quote: "An important limitation of this study is the possibility of selection bias, in terms of restaurants chosen or consumers who choose to take part in the survey. While data were not collected on consumer survey response rates, other studies have reported 60% participation. Any bias should be addressed by using the same data collection procedures before and after labeling, and in both cities" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and data on the frequency of fast‐food restaurant visits are self‐reported only |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but the assessment method can be considered objective. Quotes: "This examination of responses to calorie labeling in fast food restaurants includes objective receipt data from a diverse sample of individuals. (...) Consumers could have purchased differently as a result of the survey or incentive ($2), but given that the data collection procedures were consistent across all periods and locations this should not influence the impact estimates" |
| Contamination (performance bias) | Low risk | While not explicitly discussed by the study authors, it seems unlikely that contamination substantially affected results |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or published protocol is mentioned, but all outcome measures mentioned in the Methods section are reported. For the outcome of interest for this review (total calories from beverages per transaction) only the non‐significance of results is reported |
| Other bias | Low risk | No other concerns |
Elbel 2015a.
| Methods |
Design: CBA Timing: Prospective Allocation to group: Allocation of schools to the IG depended on administrative decisions outside the control of the investigators, which took schools' expressed interest and technical requirements for water jet installation into account. Matched comparison schools were chosen by the investigators and allocated to the CG. Quote: "We identified all schools within the New York City school district that were scheduled to receive a water jet in November 2010 (based on expression of interest by the school and having appropriate electrical outlets to support the machine) for inclusion in the study (n = 22). Principals in 10 of these schools were reached by the Department of Health and Mental Hygiene and agreed to be part of the study. We then created a pool of other New York City public elementary, middle, and high schools not scheduled to receive a water jet in the 2010–2011 school year, matched by grade level to the participating schools" Number of clusters or sites: 19 schools Number of individuals: The total number of students attending the 19 schools was 21,657, and the number of students participating in the student survey was 1515 at baseline and 1385 at follow‐up Length of intervention: 3½ months |
|
| Participants |
General description of participants: Students at schools in New York City, ranging from kindergarten to 12th grade Age: Children and teenagers (no details on the age range reported; participants of the student survey, with which part of the data were collected, were 5th to 11th grade students) Inclusion criteria: For the student survey, students from the 5th, 8th and 11th grades were included. No particular criteria were applied for the cafeteria observations Exclusion criteria: N/R Recruitment: Quote: "The surveys were administered by the students’ classroom teachers (...). To the best of our knowledge, no teachers refused to distribute the survey, and all students that were administered a survey completed the survey" Weight status at baseline: Not reported for the study participants, but study authors note that "[i]n New York City, the obesity rate among young children (kindergarten through 8th grade) is nearly 21%" SSB consumption at baseline: N/R Equity considerations: Quote: "Approximately half of the students at the participating schools qualified for free or reduced‐price meals (…). A range of races/ethnicities was represented; intervention schools had 21% African American students, 41% Hispanic students, 25% White students, and 11% Asian American students. About half of the students were female. The demographics of the comparison schools were similar. Participating schools were somewhat larger on average than NYC schools, and had more White and fewer African American students" |
|
| Interventions |
Intervention: Improved access to drinking water at school. (Quote: "To meet the city’s goal of increasing student water consumption, in 2010 the Fund for Public Health in New York, an arm of the New York City Department of Health and Mental Hygiene, received funding to provide 'water jets' (drinking water dispensers) to 140 schools across the city from the Communities Putting Prevention to Work grant from the Centers for Disease Control and Prevention. Water jets are large, clear plastic jugs with push levers that dispense cooled, aerated tap water (similar to slushy machines found in convenience stores) that are placed near the lunch line in the school cafeteria. (…) The water jets were installed with no other school‐based activities to promote water drinking; disposable cups were available next to the jet at all schools. We note that New York City water is delivered from sources in upstate New York essentially lead‐free, but because lead introduction is possible from pipes, water in schools is periodically tested") Behavioural co‐intervention: None Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Average student‐reported number of glasses of SSB drunk the day before the survey, assessed at baseline and at 3 months with a survey which was "based on modified questions from the Youth Physical Activity and Nutrition Survey" Measures of intake of alternatives to SSB: Water‐taking events per 100 students in attendance at the school cafeteria on the day of observation from water jets or pre‐existing cafeteria water sources, and milk‐taking events per 100 students, assessed at baseline, at month 3 and month 4, by trained observers following a standardised protocol; Percentage of students reporting drinking water at lunch on most days, average student‐reported number of glasses of water drunk the day before the survey, and percentage of students reporting drinking milk at lunch on most days, assessed at baseline and at month 3 with a survey which was "based on modified questions from the Youth Physical Activity and Nutrition Survey" Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes stakeholder discontent (see below), and a decrease in milk intake (see above) Other outcomes: Target group perceptions, assessed among students at month 3 with a "set of questions regarding the jet (...). These included whether they noticed the water jet, how often they used it, where the water in the jet comes from, whether they liked the taste of the water, whether the water is safe, and whether they drink more water now that the jet is there." Stakeholder perceptions, assessed among cafeteria managers at month 3 by "trained interviewer from the Department of Health and Mental Hygiene [who] conducted structured interviews with the cafeteria managers in each intervention school. The interviews included a mix of quantitative and open‐ended questions about their experiences with the water jets, implementation and maintenance, and student interaction with the jets" |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2010 ‐ 2011 Mode of implementation: Mandatory government regulation and public investment Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This study was funded by the Centers for Disease Control and Prevention (Nutrition and Obesity Policy Research and Evaluation Network supplement to 1U48DP001904‐01) and the National Institutes of Health (award R01HD070739). (...) The funding sources played no role in the study design; collection, analysis, or interpretation of data; writing of the article; or decision to submit the article for publication" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline outcome measurements were similar (see table 3, 4 and 5 of the study's primary report) |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | IG and CG schools were matched using the Euclidean distance, considering "the following publicly available school characteristics for each school: grades served, total student population, percentage of students below the poverty level, and percentage of Black, Asian, and Hispanic students. (...) The demographics of the comparison schools were similar. (...) Demographic information for schools was provided by the Department of Education for the year 2009. Significance testing was conducted between the intervention schools and the comparison schools; no differences were significant" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 IG school crossed over to the CG on the first day of the intervention implementation due to water spillage, and no other dropouts or cross‐overs are reported. For the 10‐month follow‐up data study authors report that results for an intention‐to‐treat analysis were not significantly different from results of the per‐protocol analysis |
| Blinding (performance and detection bias) Subjective outcomes | High risk | By the nature of the intervention, participants and observers could not be blinded, and outcome measures were self‐reported |
| Contamination (performance bias) | Low risk | Allocation was by institution (schools), and it is unlikely that control schools received the intervention |
| Selective reporting (reporting bias) | Unclear risk | For SSB and fruit juice consumption the study's published report only states that there were no significant effects, and does not provide pre‐ and post‐intervention means |
| Other bias | Low risk | No other concerns |
Emerson 2017.
| Methods |
Design: ITS Timing: Prospective Allocation to group: N/A (ITS without a control group) Number of clusters or sites: 3 schools Number of individuals: 960 (of which approximately 60% participated in the school lunch programme, i.e. the intervention) Length of intervention: 20 months (October 2014 to May 2016), with 56 weeks of data collection |
|
| Participants |
General description of participants: Elementary school children in Norwood, USA Age: Children (elementary school students, grade k to 6; no age details reported) Inclusion criteria: N/R (all children attending the participating schools who had lunch in the cafeteria were included) Exclusion criteria: N/R Recruitment: N/R Weight status at baseline: N/R SSB consumption at baseline: At baseline, 82% of children chose chocolate milk for lunch, and 10% plain milk Equity considerations: 71% of students were white, 13% black, and 10% Hispanic; 47% were girls, and 73% were low‐income, defined as less than 130% of the poverty level. Quote: "[T]he Norwood City School District (…) has a diverse and economically broad student body" |
|
| Interventions |
Intervention: Small prizes for the selection of plain, fat‐free milk instead of chocolate milk. (Quote: "Green 'smiley‐faced' emoticons were placed by preferred food items (fruits, vegetables, plain fat free milk and entrée with whole grain) and signs were posted explaining the PP [Power Plate, i.e. a meal consisting of plain fat free milk, an entrée with whole grain, fresh fruit and fresh vegetables or a salad] on the first day of the intervention (…). Small prizes were given students selecting the PP on Tuesdays and Thursdays once the intervention began. On the first day of the intervention, a small prize, such as a bracelet, was distributed to students who selected the PP") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Rate of children choosing chocolate milk, assessed continuously throughout the study period with cash register data Measures of intake of alternatives to SSB: Rate of children choosing plain fat‐free milk, assessed continuously throughout the study period with cash register data Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary schools Sector: Education Country: USA Year(s) when implemented: 2015 ‐ 2017 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The authors declare no conflict of interest" Funding: "The project described was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number 1UL1TR001425‐01" Trial registration: N/R Protocol availability: N/R |
|
| Notes | Note that figure 2 of the study’s primary publication (Emerson 2017) shows only data for the first part of the study. According to the study’s text, the intervention lasted considerably longer than suggested by figure 2, namely until May 2016, with 56 weeks of data collection. Quote: “The PPP was resumed for all three schools in September 2015 during the second academic year of the program and continued through the end of May2016. Thus the intervention lasted for 56 weeks with a 3‐week gap at the beginning of the 2nd academic year during weeks 23 to 26. Cafeteria cash register receipt data was collected for one month prior to the PPP intervention and then throughout the entire intervention period.” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data are unlikely to bias results ‐ the routinely‐collected sales data can be assumed to be close to complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Unclear risk | For chocolate and plain milk selection, only numerical data are reported; temporal trends can therefore be assessed only for Power Plate selection, which is only an indirect measure for chocolate and plain milk selection. Apart from this, there is no indication that outcomes were reported selectively. Outcome data on all food and beverage items targeted by the intervention, and mentioned in the Methods section, are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | A number of other factors may have influenced the outcomes, but it is unlikely that they explain the existence and the direction of the effect. Quote: "Events are annotated [in the graph showing white milk selection over time] such as baseline period, when the PP was initiated and events that may have influenced the effectiveness of the program such as cafeteria staff changes at the Sharpsburg School or when the school dietary interns who helped run program left for summer break" |
| Pre‐specification of the intervention effect (detection bias) | High risk | The point of analysis is the point of intervention; the results reported in the study are, however, not based on a classical ITS analysis |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection. Quote: "Purchase data obtained from cash register receipts were supplied by the Food Services Department of Norwood City School District" |
| Other bias | High risk | While the graphical presentation of results strengthens our confidence that effects were due to the intervention, and cannot be explained with underlying temporal trends, these were not taken into account in analyses. In 1 of the 3 intervention schools, chocolate milk purchases seem to have reverted to baseline levels towards the end of the study period. The authors conduct a statistical process management (SPM) analysis, which differs from classical ITS analyses. Seasonality may have influenced outcomes, but it is unlikely that it explains the existence and direction of the effect. Quote: "Even though the dates of introduction are staggered, the effect is similar at each school suggesting that time of year is not a factor in PP selection" |
Ermetici 2016.
| Methods |
Design: NRCT Timing: Prospective Allocation to group: "Three schools (262 adolescents) were chosen as the intervention schools because of previous collaboration with educational initiatives of our Institute, not related to nutrition and carried out with different pupils. Three other socio‐demographically matched schools (225 adolescents) were chosen as a comparison group" Number of clusters or sites: 6 schools Number of individuals: 462 Length of intervention: 2 years |
|
| Participants |
General description of participants: Students in middle schools in Milan, Italy Age: Teenagers (age range 11 to 15 years, median age 12.5 years) Inclusion criteria: N/R Exclusion criteria: Quote: "Exclusion criteria were applied only for individuals with conditions interfering with anthropometric measurements, such as severe malformation" Recruitment: N/R Weight status at baseline: 24% of participants in the IG and CG were overweight at baseline, and 7% were obese SSB consumption at baseline: At baseline, mean SSB consumption (times per week) was 2.6 in the IG and 2.7 in the CG Equity considerations: Quote: "The schools were all in a limited area of about 20 square kilometers with a high degree of urbanization and about 10% of public green areas. (...) Most of the pupils attending the schools were Caucasian, with less than 5% of ethnic minorities including Asians, Arabs, and South Americans. The annual average income of the households was about 35,000 euros (about 38,000 dollars). The parental educational levels included mainly middle‐school and high‐school certificates." 49% of participants were female |
|
| Interventions |
Intervention: Healthier vending machines (as part of a multicomponent intervention). (Quote: "In the intervention group schools, all traditional vending machines were replaced with machines containing healthy foods and beverages, including fresh fruit and vegetables, dried fruit, fruit juices, smoothies without added sugar, and drinkable yogurt, all from local farms, carefully evaluated by our expert nutritionist team. On the basis of a comparative analysis of nutritional facts, the products selected for the alternative healthy vending machines contained per 100 g an average of 60 less kilocalories, 14 g less added sugars, 0.1 g less salt, 1 g less saturated fats, and 1.4 g higher fiber, compared with the traditional vending machines. An agreement was reached with the vending machine supplier to keep prices as low as possible and to dedicate part of the proceeds to childhood health promotion initiatives. No other food and drink sources were available inside the schools, except for tap water. Students were free to bring food or drinks from home. Educational posters adapted from The Healthy Eating Plate conveying messages promoting healthy diet, water consumption, and daily exercise were posted in schools. The schools were asked to create more opportunities for exercise during breaks. Pupils were allowed to leave their classrooms and walk in the corridors or outdoor play areas, for a total of one additional hour a week of movement") Behavioural co‐intervention: Nutrition education (Quote: "Sixteen health‐promoting group lessons by expert nutritionists over two‐school‐years were included in the curriculum. Students were given an easy textbook developed by our nutritionist team as a support to school lessons and as a tool for involving parents. Automated text messages promoting a healthy diet and daily exercise were sent to the students and their parents three times a week throughout the two school years including school vacations. Text messages were sent close to meal times to encourage constructive debate in each family. Students were given a pedometer (PE320‐BL, Oregon Scientific Italia Srl) to encourage them to be physically active. A re‐usable BPA‐free TRITANtm water bottle was supplied to encourage water consumption") Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB intake (times/week), assessed with a "simple self‐completion questionnaire designed by the Italian National Institute of Health, adapted from a validated international standard questionnaire targeting adolescents" at baseline and 2‐year follow‐up Measures of intake of alternatives to SSB: N/R Anthropometric measures: Assessed in this study but not included in our review due to confounding by non‐beverage specific intervention components Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Cost of the intervention per student (no details on how and when this outcome was assessed provided) |
|
| Context and implementation |
Setting: Schools Sector: Education Country: Italy Year(s) when implemented: 2009 ‐ 2011 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Disclosure: The authors declare no conflict of interest" Funding: "Funding agencies: This study was partially sustained by IRCCS Policlinico San Donato Ricerca Corrente Fund" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a NRCT, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a NRCT, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline outcome measurements were similar, and differences were tested for significance (all were non‐significant) |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Study authors report that the IG and CG schools were similar with regard to a number of characteristics at baseline. However, the way schools were allocated to the IG and CG may have lead to unobserved differences. In particular,study authors hypothesise that motivation to participate differed between IG and CG. Quotes: "Although previous collaborations with the schools assigned to the intervention group in the present study were not inherent to nutritional education and were carried out with different students, the possibility of a different motivation between the intervention and control schools cannot be excluded. (...) The characteristics of the schools of the intervention and the control groups were sufficiently homogeneous, on the basis of previous reports of the Italian National Institute of Statistics. The schools were all in a limited area of about 20 square kilometers with a high degree of urbanization and about 10% of public green areas. The access to green areas as well as to fast food outlets and food stores was similar for all the schools" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A per‐protocol analysis was done, but attrition was low (only 5 our of 487 students until year 2) |
| Blinding (performance and detection bias) Subjective outcomes | High risk | The outcome of interest to us (SSB intake) was self‐reported only, and the students' responses to the questionnaire are likely to have been influenced by the student's knowledge that they were part of the study, in particular due to the fact that an intensive behavioural co‐intervention was performed |
| Contamination (performance bias) | Unclear risk | The authors discuss contamination, but it is unclear how this might have occurred. Quote: "It was almost impossible to prevent cross‐contamination of the intervention between schools placed in a geographically limited area" |
| Selective reporting (reporting bias) | Unclear risk | It is not reported if outcomes were prespecified or not, or if the trial was registered or if a protocol was published. No data on a number of potentially relevant outcomes (e.g. prevalence of overweight and obesity at follow‐up, consumption of water and other alternatives to SSB, vending machine sales etc) are reported |
| Other bias | Low risk | No other concerns |
Finkelstein 2011.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: All restaurants belonging to 1 quick‐service restaurant chain, Taco Time Northwest, located in King County, which implemented calorie labelling, were the IG, and restaurants belonging to the same chain but located outside King County were the CG. Quote: "Fourteen stores were included in the analysis. These include all seven stores located in counties adjacent to King County and whose data were available in the company database for the entire period of analysis and a randomly selected subset of 21 King County stores that also had complete sales and transactions data for the study period" Number of clusters or sites: 14 restaurants located in 2 counties and belonging to 1 fast‐food chain Number of individuals: N/R (the analysis is based on transaction data not linked to individual participants; the mean number of monthly transactions per restaurant was 10,773, and the total number of restaurants was 14) Length of intervention: 12 months (including 6 months during which calories were posted only on menu boards inside the restaurants, and 6 months during which calories were additionally posted on drive‐through menu boards) |
|
| Participants |
General description of participants: Customers of Taco Time restaurants, a Mexican‐style quick‐service restaurant chain, in the state of Washington, USA Age: All ages Inclusion criteria: See allocation to group Exclusion criteria: N/R Recruitment: N/R Weight status at baseline: N/R SSB consumption at baseline: Average drink calories per transaction were 84 in the IG, and 102 in the CG, and the baseline share of diet drinks among all drinks sold was 45% in the IG, and 39% in the CG Equity considerations: Quote: "It is worth noting that even before the King County law went into effect, on average, customers of the King County locations were eating healthier than customers outside King County. Seattle is known to be a health conscious city, so this result is not surprising" |
|
| Interventions |
Intervention: Menu‐board calorie labelling in chain restaurants. (Quote: "King County’s menu‐labeling law went into effect on August 1, 2008, and became mandatory (fınes imposed) on January 1, 2009. The legislation states that restaurants that are part of chains with 15 or more outlets nationwide and have annual gross sales of at least $1 million must provide nutrition labels (calories, saturated fat, carbohydrates, and sodium) for all standard food and beverage items at the point of purchase. Quick‐service restaurants are required to display calories on menu boards or on signs adjacent to menu boards and must make information on carbohydrate, sodium, saturated fat, and daily recommended caloric intake readily available in pamphlets, brochures, or posters. Additionally, restaurants were required to post calories on drive‐through menu boards beginning in August 1, 2009. This latter requirement is signifıcant given that drive‐through orders represent more than 70% of revenue for many fast‐food outlets") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Average drink calories per transaction, assessed continuously throughout the study period with routinely‐collected transaction data Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Average food and drink calories per transaction, assessed continuously throughout the study period with routinely‐collected transaction data |
|
| Context and implementation |
Setting: Fast‐food restaurants Sector: Food service Country: USA Year(s) when implemented: 2009 ‐ 2010 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "No fınancial disclosures were reported by the authors of this paper" Funding: "This research was funded by an internal grant from Duke‐NUS Graduate Medical School" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Average drink calories per transaction were considerably lower in the IG (83.8 kcal/transaction) than in the CG (102.4 kcal/transaction) at baseline. The share of diet beverages among all beverages sold was significantly higher in the IG (45.4%) than in the CG (39.4%). While this was taken into account in the analysis, it may be a sign of unobserved baseline differences which may have biased the results. Quote: "Moreover, whereas 45.4% of transactions involved a low‐calorie drink in King County, this fıgure was 39.4% for restaurants outside King County. These differences, which were signifıcant, explain why average calories per transaction were greater in stores outside King County and may explain the lack of effect of the legislation; King County patrons already were consuming healthier options" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Apart from outcome measures, no baseline characteristics are reported. The significant differences in baseline outcome measurements may hint at differences in unobserved baseline characteristics, which may have biased results |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study reports that only restaurants for which complete transaction data were available were included in the analysis. It is not reported for how many restaurants this was not the case, and why transaction data for these were missing. Quote: "Fourteen stores were included in the analysis. These include all seven stores located in counties adjacent to King County and whose data were available in the company database for the entire period of analysis and a randomly selected subset of 21 King County stores that also had complete sales and transactions data for the study period" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcome data were objective (routinely‐collected transaction data) |
| Contamination (performance bias) | Unclear risk | Control restaurants were located in counties adjacent to King County, where the intervention restaurants were located. The same customers may have frequented intervention and control restaurants. In both the IG and the CG. Average drink calories per transaction ‐ the outcome of interest to this review ‐ decreased significantly between baseline and follow‐up, which may be a sign of contamination |
| Selective reporting (reporting bias) | Unclear risk | No trial registration is reported, and no study protocol is publicly available. The transaction data may have allowed a number of additional analyses which are not reported, including the effect of the legislation on the share of diet beverages among all beverages sold, for which only baseline but no follow‐up data is reported |
| Other bias | Low risk | No other concerns |
Foster 2014.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: 8 supermarkets Number of individuals: N/A (The analysis is based on routinely‐collected sales data not linked to individual participants) Length of intervention: 6 months |
|
| Participants |
General description of participants: Customers of supermarkets in low‐income, high‐minority urban neighbourhoods in Philadelphia and Wilmington, USA Age: All ages Inclusion criteria: Quote: "Supermarkets were the unit of randomization, intervention, and analysis. Two chains were approached about the study: Brown’s Super Stores Inc (Shoprite) (n = 11 stores) and The Fresh Grocer (n = 8 stores). On the basis of st atistics from Policy Map and the US Census, 8 stores (4 in each chain) met the following eligibility criteria: located in a low‐ to moderate income census tract, located in an area of below‐average supermarket density, or located in an area having a supermarket customer base with >50% living in a low‐income census tract" Exclusion criteria: See inclusion criteria Recruitment: See inclusion criteria Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: "All stores were located in urban, high‐minority, low‐income neighborhoods" (For further details see inclusion criteria) |
|
| Interventions |
Intervention: Point‐of‐purchase promotion of healthier beverages in supermarkets. (Quote: "Intervention stores (n = 4) received a 6‐mo intervention to increase the purchase of recommended healthier items in 5 food and beverage categories. The intervention consisted of 4 major marketing strategies used across all categories, with placement as the dominant strategy and promotion as the secondary strategy. Strategies included 1) multiple facings: increased the number of facings of the recommended products; 2) prime placement: placed recommended products at arm/eye level and in the middle of the category aisle and reordered types of milk so that 2% milk was located on the left‐hand side of the dairy case followed by 1%, skim and then whole milk; 3) signage: placed call‐out signs with the recommended product’s name and price, and shelf runners below recommended products; and 4) secondary placement: mimicked shelf strategies (1 and 2) in all secondary placements (end caps, dead space stacks, etc). In addition, other strategies were used as appropriate to the category, including 5) cross promotion (cereal and beverages only): displayed recommended products in 2 product categories together, through dead space stacks and end caps (eg, cereal and bananas, soda and water); and 6) taste‐testing (milk only): offered free samples of recommended products to increase shoppers’ exposure to healthier options (1 d/mo for 2–3 h). It is important to note that the strategies were 'stealth' with regard to health or nutrition claims, there were no prompts to buy one product instead of another, and there were no reductions in the price of the targeted products. The overall approach was to simply increase the visibility of, and access to, healthier options through increased number and optimal placement of the recommended products, signage, and taste‐testing. The specific strategies used for each product category in the intervention stores are described in Table 12 [of the study’s primary report]. The intervention strategies were developed in consultation with supermarket operators and managers and were implemented by store staff, rather than the research team. Planograms, which are visual representations of where specific products are placed on the supermarket shelves, were created for each category and store to promote consistency through the intervention period") Behavioural co‐intervention: None (but see quote above) Control: No intervention (Quote: "Control stores (n = 4) received no intervention and served as assessment‐only controls") |
|
| Outcomes |
Measures of SSB intake: Weekly sales of SSB, assessed throughout the study period with routinely‐collected sales data Measures of intake of alternatives to SSB: Weekly sales of bottled water, diet beverages, and skim, 1% and 2% milk, assessed throughout the study period with routinely‐collected sales data Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Target group perceptions, assessed with focus‐group discussions at baseline, and stakeholder perceptions, assessed with informal discussions |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: USA Year(s) when implemented: 2011 ‐ 12 Mode of implementation: Pilot trial by researchers in co‐operation with private supermarkets Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "During the time of the study, GDF served on the scientific advisory boards of the United Health Group, ConAgra Food, and Tate & Lyle. GDF is currently the Chief Scientific Officer at Weight Watchers International. JB is an owner of Brown’s Super Stores Inc. PJB is an owner of The Fresh Grocer. None of the other authors declared any conflicts of interest" Funding: "Supported by grants 68237 and 68201 from the Robert Wood Johnson Foundation and grant 310128 from the USDA" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study states that allocation was random, but does not report how the allocation sequence was generated and if it was concealed. Quote: "Eight supermarkets (4 from each chain) were divided into 4 matched pairs (...). The randomization allocation sequence was created by a statistician and implemented by a research coordinator. Within each pair, the stores were randomly assigned to intervention or control" |
| Allocation concealment (selection bias) | Low risk | Allocation was by institution (supermarket), and done at the start of the study |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Some differences in baseline outcomes measurements exist, but confidence intervals overlap and differences were taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | The percentage of customers below the poverty line, and the percentage of ethnic minority customers, were considerably lower in control than in intervention stores |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Routinely‐collected supermarket sales data were used as an outcome measure. The study does not mention that sales data for any of the assessment period or targeted beverages were missing |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were objective (routinely‐collected sales data) |
| Contamination (performance bias) | Low risk | Allocation was by institution (supermarkets), and it seems unlikely that the CG received the intervention |
| Selective reporting (reporting bias) | Low risk | All outcome measures mentioned in the Methods section are reported, and complete sales data for all food and beverage types targeted in the intervention are presented |
| Other bias | Unclear risk | Quote: "The study also had several limitations, including (...) lower than ideal implementation within the 2 beverage product categories" |
Franckle 2018.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 148 Length of intervention: 5 months |
|
| Participants |
General description of participants: Customers of a supermarket in Chelsea, a small city adjacent to Boston, Massachusetts, USA Age: Adults (a minimum age of 18 was an inclusion criterion) Inclusion criteria: Quote: "Participants were recruited from a medium‐sized Chelsea supermarket of 6000 ft2 (˜557 m2) and approximately 30 % of the total store sales were made with SNAP electronic benefit transfer cards. To be included in the study, customers had to be 18 years or older, speak either Spanish or English, have at least one child under the age of 18 years living in the household, and report purchasing at least half of their monthly groceries at the study supermarket. Employees of the store were excluded" Exclusion criteria: N/R Recruitment: Quote: "Study staff fluent in Spanish and English recruited customers after they entered the store during weekdays between 09.00 and 17.00 hours in January 2014. When the customer consented to participate, he or she was informed about the study ‘loyalty card’ that would provide them with a 5 % discount on all store purchases during the entire study period. The loyalty card included the study participant’s name, and each card had a barcode that was scanned at the checkout and linked the participant’s purchases in the supermarket sales database" Weight status at baseline: N/R SSB consumption at baseline: Quote: "[At baseline, t]he vast majority (94 % of the intervention group and 87 % of the control group) reported consuming at least one SSB (that met criteria for a red label in the study traffic‐light system, including soda, juice drinks, energy drinks, powdered mixes and sweetened teas) once weekly or more" Equity considerations: Quote: "The majority were female and identified as White race and Hispanic/Latino ethnicity. Study participants were predominantly Central American, with the most frequently reported countries of origin being El Salvador, Honduras and Guatemala" |
|
| Interventions |
Intervention: Financial incentives for not purchasing beverages labelled red (predominately SSB) in a supermarket. (Quote: "All beverages sold in the store (750 different items), including powder mixes (when prepared as directed), were categorized as red, yellow or green based on similar criteria used for the Boston Public Health Commission’s ‘Rethink your drink’ campaign. (…) Following the two‐month baseline period, traffic‐light shelf labels were posted for each beverage item in the store to indicate if the beverage was a healthy (green), less healthy (yellow) or unhealthy (red) choice. (…) Intervention group participants received five monthly letters during the intervention period (April–August 2014). The initial monthly letter (April) explained what the red, yellow and green supermarket beverage labels represented and how the participant could earn a $US 25 incentive each month (in the form of a supermarket gift card) by refraining from purchasing any red‐labelled beverages at the store. Each subsequent monthly letter (May–August) provided feedback identifying any red‐labelled beverage purchases they made in the previous month and notified them if they earned the $US 25 gift card. Each of the monthly letters also included a graphic of the in‐store traffic‐light labels, brief targeted beverage education and a healthy beverage recipe (e.g. seltzer water with fruit). The beverage education topics for each month were: (i) juice and juice drinks; (ii) sports drinks; (iii) milk and flavoured milk; (iv) coffee and tea; and (v) powdered drinks. These topics were chosen based on findings from previous focus groups with non‐participant store customers that demonstrated customers were aware that soda was unhealthy, but they had gaps in knowledge about the healthfulness of other sugary beverages, particularly juice, juice drinks and powdered mixes. Each letter reminded the participant to use their loyalty card to receive the 5 % store discount. The supermarket gift card could be used for all groceries available in the store, except for tobacco products. The store did not sell alcohol") Behavioural co‐intervention: None (but see quote above about nutrition information provided to participants) Control: Alternative intervention. (Quote: "The control group participants received monthly letters with general nutrition information in the form of the MyPlate.gov graphic (http://www.choosemyplate.gov/). Each letter also included a healthy eating tip (e.g. fruit and fibre) and a healthy meal recipe (e.g. beans and brown rice). Control letters did not provide any information about beverages or about the in‐store traffic‐light labels. Each control letter also reminded participants to use their loyalty card to receive the 5 % store discount.") Note: Control group participants were also exposed to the traffic‐light labelling implemented in the supermarket |
|
| Outcomes |
Measures of SSB intake: Share of participants purchasing ≥ 1 red‐labelled beverage a month, assessed continuously throughout the study period with loyalty card sales data, and share of participants reporting consumption of ≥ 1 red‐ or yellow‐labelled beverage a week, assessed at baseline and 5 months follow‐up with a beverage frequency questionnaire; number of red‐labelled beverages purchases a month, assessed continuously throughout the study period with loyalty card sales data (data provided to us by study authors) Measures of intake of alternatives to SSB: Share of participants reporting consumption of ≥ 1 green‐labelled beverages a week, assessed at baseline and 5 months follow‐up with a beverage frequency questionnaire Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: An estimate of the incentive programme cost per household, based on the total cost of monthly incentives divided by the total number of participants, and target group perceptions assessed with a participant exit survey |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: USA Year(s) when implemented: 2014 Mode of implementation: Pilot trial by researchers in co‐operation with a private for‐profit supermarket Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Conflict of interest: None" Funding: "The project was supported by the Harvard Clinical and Translational Science Center, from the National Center for Advancing Translational Science (grant number 8 UL1 TR000170‐05); and the National Institutes of Health (R.L.F., grant numbers T32 DK 007703, T32 HL 098048). A.N.T. was supported in part by a grant from the Carney Family Foundation. The funders had no role in the design, analysis or writing of this article" Trial registration: ClinicalTrials.gov number NCT01990508 Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The Stata statistical software package was used to randomize participants 1:1 to intervention or control in blocks of 8, to assure that the number of individuals in each arm was roughly equal" |
| Allocation concealment (selection bias) | Low risk | Quote: "Study participants and investigators were blinded to the randomization assignment during the baseline data collection months (February and March 2014) and all participants were notified of their group assignment in April 2014" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | The CG had lower levels of SSB purchase and consumption at baseline (see table 1 of the study's primary report), but differences are smaller than the calculated intervention effects, and were taken into account in the analysis. Quote: "A generalized least‐squares model with subject‐specific random effects was used to assess differences by study arm in trends of the monthly probability of purchasing any red beverages during intervention period, controlling for baseline red beverage purchases and SNAP use" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline characteristics were similar, and differences were taken into account in the analysis. Quote: "There were no significant differences in baseline characteristics between the intervention and control group participants, except for self‐reported SNAP use at baseline (66 % of the intervention group v. 49 % of the control group, P=0.04)" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was similar across study groups, but substantial, and the analysis was per‐protocol. No systematic differences between dropouts and participants remaining in the study were found. Quote: "A total of 214 store customers were randomized to the intervention or control group. There were sixty‐six participants who never picked up (n = 31) or who never used (n = 35) the study loyalty card. Therefore, 148 customers (n = 77 in the intervention group and n = 71 in the control group) were included in the final analyses. (...) We found no differences in participant characteristics between those who were randomized but never picked up their cards (n = 31), those who were randomized and picked up their cards but never used them (n = 35), and those who picked up their cards (n = 183) and were included in our analyses" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were blinded during baseline data collection, but not during the intervention, and SSB consumption data are self‐reported |
| Blinding (performance and detection bias) Objective outcomes | Unclear risk | Participants were not blinded, and purchasing data could be manipulated by the participants (purchasing data were collected through supermarket loyalty cards, which may have been used selectively) |
| Contamination (performance bias) | Unclear risk | While it is unlikely that CG participants received the financial incentives, they did see the traffic‐light labels and it is possible that were indirectly exposed to the behavioural co‐intervention through contact with IG participants, who were recruited from the same communities and frequented the same supermarket |
| Selective reporting (reporting bias) | Unclear risk | The study was prospectively registered, and the prespecified primary and secondary outcome (SSB purchases and consumption) are reported only indirectly and in a non‐standard form. The study's published report provides only the share of participants purchasing or consuming any red‐labelled beverages, but not the mean purchase or consumption level. Data on the number of red‐labelled beverages purchased per month were provided to us by the study's corresponding author |
| Other bias | Low risk | No other concerns |
French 2010.
| Methods |
Design: Cluster‐RCT (included as a NRCT in our GRADE assessment due to the small number of randomised units) Timing: Prospective Allocation to group: Random Number of clusters or sites: 4 bus garages Number of individuals: The analysis is based on repeat cross‐sectional data, and the number of participants was 1094 at baseline and 1065 at follow‐up Length of intervention: 18 months |
|
| Participants |
General description of participants: Employees of a bus garage in Minneapolis, USA Age: Adults (age range 19 to 79 years, average age 47 years) Inclusion criteria: Quote: "All garage employees who worked at each of the four garages were eligible to complete the evaluation measures" Exclusion criteria: N/R Recruitment: Quote: "Participants were recruited using a variety of methods, including paycheck distribution fliers, signs posted in the garages, fliers distributed at health fair events, information in employee newsletters, and instant text messaging on the buses. Participants received a $20 incentive for completing the behavioral measurement survey and for having their height and weight measured by trained research staff” Weight status at baseline: Mean BMI at baseline was 32 kg/m2 in the IG, and 33 kg/m2 in the CG SSB consumption at baseline: Self‐reported intake of SSB at baseline was 216 ml/day (0.6 servings/day) in both the IG and the CG Equity considerations: "Seventy‐three percent of the employees who completed the surveys were bus drivers; 16% were bus maintenance staff; 8% other jobs (such as dispatchers); and 3% were managers. Seventynine percent of the employees were men, with an average age of 47 years (age range 19 to 79 years). Sixty‐three percent were white. Forty‐nine percent had completed high school/vocational school or had less education, and 43% reported annual household incomes before taxes of <$50,000. Most workers had been employed with the transit company ≥6 years, and about one third had been working with the transit company 15 years or longer. Overall, the prevalence obesity among the transit workers was very high. The average body mass index was 32.3 kg/m2, and 56% were obese (body mass index ≥30 kg/m2)" |
|
| Interventions |
Intervention: Improved availability and price reductions for healthy beverages in vending machines. (Quote: "The two key components of the vending intervention were to increase the availability and to lower the prices of healthier food and beverage choices in the vending machines at the two intervention garages. (…) Healthy vending choices were defined separately for the different types of foods and beverages available in the vending machines (ie, beverages, snacks, and entrees). All vending machine foods and beverages were classified as healthful or not according to nutrition criteria for calories ((…) beverages 50 calories or fewer); (…). Examples of healthy and unhealthy items include the following: (…) 3) beverage: diet soft drink versus regular soft drink. (…) Planagrams (product placement maps for each machine) were created for both intervention and control garage vending machines. Vending machine service personnel were trained by the research staff to stock the machines according to the specific planagram for each vending machine. Vending machine service personnel were instructed to stock the control garage vending machines according to the control machine planagrams to ensure that the control garage vending machines continued to offer the same items throughout the intervention and to prevent contamination of the vending machine intervention across garages. The number of rows in each machine for healthy products was negotiated in advance with the vending machine service company and remained constant for the 18‐month period. Prices for the healthy food and beverage items were also programmed into the machines at the start of the study and remained constant throughout the intervention period. The goal of the vending intervention was to make 50% of the available vending offerings meet healthy criteria and to price these items 10% lower than the usual price for the item. (…) Vending route service staff received a small monthly financial incentive for maintaining accurate product placement in the garage vending machines for which they were responsible for servicing") Behavioural co‐intervention: A limited number of promotional activities. Quote: "Taste‐testing activities were conducted with the garage advisory groups before the selection of the new vending products" Control: No intervention. Quote: "Control garage vending machines continued to offer the same items as before the study and did not change items during the intervention period" |
|
| Outcomes |
Measures of SSB intake: Intake of SSB in ml/day, assessed at baseline and at 18 months with a self‐administered survey which "was adapted from two existing instruments for which validity has been evaluated" Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Worksites Sector: Public transport Country: USA Year(s) when implemented: 2005 ‐ 2007 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The authors declare that there are no conflicts of interest" Funding: "The research was funded with a grant from the National Institutes of Health NIH R01 HL 079478" Trial registration: N/R Protocol availability: N/R |
|
| Notes | This study reports self‐reported SSB intake data and objective vending machine sales data. For the latter, data are available only for follow‐up, but not for baseline. We have therefore included the self‐reported intake data only. Given the small number of randomised units, randomisation may not have been sufficient to attain baseline comparability of the IG and CG. We therefore included the study as a NRCT in our GRADE assessment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The four bus garages were paired on physical characteristics (urban location and number of employees) and then randomized within pairs to intervention or comparison conditions by the toss of a coin" |
| Allocation concealment (selection bias) | Low risk | Allocation was by institution (bus garage), and allocation was done at the start of the study |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Reported baseline intake of SSB was identical in the 2 groups (216 ml/day or 0.6 servings/day) |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Baseline characteristics other than outcome measures are not reported separately for the IG and the CG. Differences in baseline characteristics can therefore not be assessed |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Survey participants were redrawn each time from the study population, and the method used for the selection (40 participants were enrolled at each garage on first‐come‐first‐served basis) does not guarantee representativeness. The intervention may have changed the motivation of drivers to volunteer for the survey, which could lead to differences in the representativeness of the sample in the control and the intervention group at follow‐up |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded and SSB intake was self‐reported. The behavioural co‐interventions may have reinforced social desirability bias |
| Contamination (performance bias) | Low risk | The only pathway for contamination would have been through interaction between staff from the different sites. However, most of the intervention components were aimed at the physical environment in the garages; behavioural components were relatively small |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol is mentioned, and it is not reported if outcomes were prespecified or not. Data on vending machine sales are reported only for follow‐up, and not for baseline |
| Other bias | Low risk | No other concerns |
Harnack 2016.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 265 Length of intervention: 12 weeks |
|
| Participants |
General description of participants: Low‐income households in Mineapaulis‐St. Paul, USA Age: Adults and their families (average age of adult household members enrolled in the study was 45 years) Inclusion criteria: Quote: "[S]tudy eligibility criteria were established with the aim of recruiting adults in households that were near eligible for SNAP or eligible for SNAP but not currently participating. Criteria included: (1) not currently participating in SNAP; (2) household income less than or equal to 200 percent of the federal poverty level, or participating in a government program, such as the Diversionary Work Program, which automatically qualifies household for SNAP in Minnesota; and (3) adult in household most responsible for food shopping is able to read and speak English and is willing to participate" Exclusion criteria: N/R Recruitment: Quote: "Recruitment was carried out in the Minneapolis–St Paul, Minnesota metropolitan area by posting study fliers in community locations in neighborhoods with a high poverty rate; distributing fliers through food pantries; and referrals from organizations that serve lower income households. Respondents were screened for eligibility and scheduled for a clinic visit if eligible and interested in participating" Weight status at baseline: 57% of participants were obese at baseline, and 24% were overweight but not obese SSB consumption at baseline: Baseline SSB consumption of participants was 0.9 servings/day in the CG and 0.9 ‐ 1.2 servings/day in the 3 IGs Equity considerations: Quote: "Most participants were female with an average age of 44.5 years. African Americans comprised 52.7% (n = 139) of the sample followed by those who self‐identified as white (29.2%; n = 77) or biracial (13.3%; n = 35). Most were either overweight (24.0%; n = 62) or obese (57.4%; n = 148). Household food security was low (34.0%; n = 90) or very low (46.0%; n = 122) for most. Ten percent of participants reported currently participating in WIC. Thirty‐seven percent reported using an emergency source of food (eg, food pantry) in the past month. About one‐half reported participating in SNAP in the past. Demographic factors were similar across experimental conditions" |
|
| Interventions |
Intervention: Monetary transfers, modelled to be similar to the Supplemental Nutritional Assistance Program (SNAP) food benefit programme in the USA, with restrictions on SSB purchases and incentives for fruit and vegetable purchases. (Quote: "[Participants] were randomized to 1 of 4 experimental conditions (…). Restriction: sugar sweetened beverages, candies, and sweet baked goods were selected for restriction in the restriction and the incentive plus restriction arms because these food categories are leading contributors to discretionary calories in the American diet and contribute minimally to vitamin and mineral intake. Financial incentives: fruit and vegetable intake is insufficient for 44% and 42% of SNAP participants respectively, hence these food categories were selected for incentivizing in the incentive and incentive plus restriction arms. The incentive was 30% of purchase price, and the amount was based on previous research. After random assignment to condition, a meeting was scheduled to orient the participant to his or her assigned experimental arm. While complete blinding was impossible, we did not share the experimental details of the study with participants; they were blind to other conditions. The participant was given a debit card and told the dollar amount to be added to the card every 4 weeks over the 12‐week experimental period (3 deposits). The amount placed on the card every 4 weeks was the average benefit amount provided by SNAP in Minnesota’s Hennepin and Ramsey counties to those with the same household size as the participant ($152 monthly for a household of 1, $277 monthly for household of 2, $401 monthly for household of 3, etc). Verbal and written instructions were provided regarding allowable and non allowable purchases. The food purchase receipt collection procedures (weekly submission of all food purchase receipts) were reviewed, with a focus on the role they play in monitoring compliance with food purchase rules and determining the incentive amount. On a weekly basis the amount of incentive earned for purchasing eligible fruits and vegetables was calculated from the receipts; the incentive amount was added to the participant’s debit card; and a text or email was sent to the participant notifying her or him of the incentive amount added to their card") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Intake of SSB, assessed at baseline and 3 months follow‐up with 3 unannounced 24‐hour dietary recalls each conducted over the telephone by trained and certified interviewers using an established protocol, and weekly SSB purchases, assessed continuously throughout the study period with grocery receipts collected from study participants Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Households Sector: Social security/public food benefit programmes Country: USA Year(s) when implemented: 2013 ‐ 2015 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Conflict of Interest Disclosure: Dr Beatty reports grants from National Institutes of Health during the conduct of the study. No other disclosures are reported" Funding: "Funding/Support: Funding was provided by the National Institute for Diabetes and Digestive and Kidney Disease (R01DK098152)" Trial registration: ClinicalTrials.gov number NCT02643576 Protocol availability: The study protocol has been published as supplementary material to the study's primary report |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | We contacted the corresponding author Lisa Harnack to obtain additional information on the randomisation procedure, which is not described in detail in the study's published report. We received the information that a random‐number generator was used to create the allocation sequence, and that participants were enrolled and randomised in waves |
| Allocation concealment (selection bias) | Low risk | See comment above ‐ given that participants were enrolled and randomised in waves it seems unlikely that lack of allocation concealment introduced bias |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline SSB consumption of participants was 0.9 servings/day in the CG to 1.1/1.2 servings/day in the 2 IGs. Baseline SSB purchases were similar across all study arms, and 95% CI intervals overlap. Baseline differences were not taken into account in the analysis, but this seems justified. Quote: "Because no confounding was expected as a result of randomization and the distribution of potential confounders appeared to be similar across experimental conditions (...) no covariates were included in the final models" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | While not stated explicitly, it seems likely that all participants were handled by the same providers (i.e. research staff who provided participants with the study‐specific debit cards and the required training and assessment). It seems unlikely that baseline differences in provider characteristics introduced bias. Certain baseline differences in demographic characteristics of participants existed, but these were small and not statistically significant |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was low, and an intention‐to‐treat analysis was done with all participants for whom follow‐up data were available (including those who did not receive the intervention). Quotes: "Sixteen participants (6%) had their debit card funds discontinued owing to noncompliance with experimental procedures. Similar numbers were discontinued from each experimental condition (...). (...) Those with only 1 dietary recall at baseline or follow‐up (n = 14) were excluded from analyses in which food or nutrient intake was the outcome of interest because a single recall is a poor representation of usual intake owing to high day‐to‐day variation in diet. (...) The analytic sample was restricted those with ≥3 weeks of food purchase receipts at baseline and ≥9 weeks during the follow‐up period (n = 252 of 279 randomized: see Fig. 1). The reason for the minimum number of weeks of receipt criterion was due to concerns that only two weeks of receipts would not validly represent usual food purchasing in this low‐income sample. The number of participants excluded from the analysis due to not meeting the minimum number of receipts did not differ meaningfully by treatment group assignment" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Self‐reported food and beverage intake data: Participants in the IGs received detailed instruction, training and feedback on what to buy and what not to buy with the debit cards they received as part of the intervention, i.e. they were clearly aware of the fact that they should consume less SSB, and this might have increased social desirability bias in the IG, leading to under‐reporting of SSB intake. Quote: "In this study blinding was impossible, however participants are most likely to have been unaware of the other arms. We do not believe that knowledge of the allocated intervention would have introduced bias" |
| Blinding (performance and detection bias) Objective outcomes | Unclear risk | Grocery receipt data: Participants were not blinded, and the data collection method (analysis of food purchase receipts), while described as objective by the study authors, depended on collaboration by the study participants. Some bias due to lack of blinding is possible. Quote: "Limitations include the methodological weaknesses inherent in the receipt collection methodology. No objective measure exists of the true total number of receipts that participants should turn in to the research staff. It is possible that participants may have omitted receipts for small purchases such as a single drink or candy item. Participants may have selectively turned in the receipts for which the study debit card was capable of tracking and omitted other receipts from foods purchased with their own money. By contrast, a strength of the receipt data is its potentially lower reactivity compared with the assessment of individual dietary intake using a verbally reported 24‐h dietary intake interview. Food purchase receipts are an objective measure of food purchases, do not rely on participant memory, and may be less affected by social desirability responding." |
| Contamination (performance bias) | Low risk | Due to the way the intervention was implemented it seems unlikely that there was a relevant degree of contamination |
| Selective reporting (reporting bias) | Low risk | Quote: "All analyses were planned a priori and all outcomes examined are reported herein" |
| Other bias | Low risk | No other concerns |
Hartigan 2017.
| Methods |
Design: ITS Timing: Prospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 1 Hospital Number of individuals: N/R (the analysis is based on sales data not linked to individual participants) Length of intervention: 12 months (+ 4 months additional follow‐up after the end of the intervention; it is unclear if all intervention components were discontinued or only the behavioural co‐intervention) |
|
| Participants |
General description of participants: Employees, physicians, patients, and visitors of Rady Children’s Hospital, San Diego, California, US Age: All ages (no age details reported) Inclusion criteria: N/R Exclusion criteria: N/R Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: N/R |
|
| Interventions |
Intervention: Traffic‐light labelling and repositioning of beverages in vending machines and cafeteria coolers, and elimination of SSB from room service menus. (Quote: "After consideration of the formative research findings and the employee survey, the Advisory team decided to decrease SSB options, increase non‐SSB options, and focus the intervention on educating employees about making healthy drink choices. The team decided to use a similar stoplight approach to that outlined in the Healthy Beverage Toolkit published by the Boston Public Health Commission, whereby all drinks are color coded as 'red', 'yellow', or 'green' based on sugar content. This intervention was named 'Rethink Your Drink' and was implemented over 12 months and evaluated to determine its effectiveness to reduce sales of SSBs relative to non‐SSBs. (…) The stoplight labeling system was chosen to emphasize education with drinks labeled as red (high in sugar or SSBs defined as having over 12 grams of sugar per 12 ounces), yellow (low in sugar or artificially sweetened defined as having 6 to 12 grams of sugar per 12 ounces or containing artificial sugar), or green (no added sugar and no sweeteners defined as having 0 to 5 grams of sugar per 12 ounces). In addition, some drinks were identified as “other” and included beverages into which sugar could be added after purchasing and therefore were not coded by color. These drinks were mostly hot beverages, including coffee, tea, and hot water. The hospital’s Communications Department designed a customized stoplight graphic to be used on all collateral materials based on the criteria established. (...) Environmental changes included repositioning all beverages in coolers in the cafeteria and vending machines so that green drinks were placed at eye level and red drinks placed at the bottom. Also, color‐coded labels were added to the cafeteria coolers corresponding with the drinks on each shelf. Policy changes included eliminating SSBs from room service menus—although they were provided on request. (…) The intervention took place at the main hospital cafeteria, delicatessen, hospital Grab & Go, Starbucks cart, and patient room service") Behavioural co‐intervention: Educational and promotional activities. (Quote: "The RYD educational intervention included flyers and point of sale education posters describing the traffic light system (...), tabletop tents, and an education handout designed for children. Displays included green beverage tastings, a display that included a wheelbarrow holding 40 pounds of sugar (annual sugar intake for a person drinking one daily SSB), and a handmade interactive electronic display where customers could guess what color certain beverages were (...). Displays and drink demonstrations were rotated on a quarterly basis to different areas of the hospital (main cafeteria, delicatessen, hospital lobby, and entrance to the acute care pavilion)" Control: N/A (ITS without control group) |
|
| Outcomes |
Measures of SSB intake: Monthly red and yellow beverage sales (total number of items, and percentage of all beverage items), assessed throughout the study period with sales data collected through cashiers Measures of intake of alternatives to SSB: Monthly green beverage sales (total number of items, and percentage of all beverage items), assessed throughout the study period with sales data collected through cashiers Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes a decrease in total monthly revenue from all beverages sold Other outcomes: Average total monthly revenue from all drinks, assessed throughout the study period with sales data collected through cashiers |
|
| Context and implementation |
Setting: A private not‐for‐profit hospital Sector: Health care Country: USA Year(s) when implemented: 2013 ‐ 2014 Mode of implementation: Voluntary initiative by private not‐for‐profit actors/pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "Of note, this intervention was planned and implemented by a small working group with no dedicated staff and very limited resources. This study was unfunded outside of the time and effort of the RCHSD [hospital] staff" (No further details provided) Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The data collection method as described in the paper appears reliable, and precautions were taken to ensure its reliability. Quote: "Another strength of this study was the ability to collect objective sales and revenue data over an extended period of time as a result of permanent modifications of cash registers to recode beverage sales data" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Unclear risk | Outcome data on all 3 beverage groups which were targeted is reported. However, only percentage changes from baseline are reported, not absolute values |
| Independence of the intervention from other changes (performance bias) | Unclear risk | Figure 3 of the study's primary report suggests that the percentage of red beverages was already decreasing, and the percentage of green beverages increasing before the intervention was implemented in September, and that the change after the start of the intervention was not stepwise, but at least partially a continuation of the baseline trend. It is not clear if this was taken into account in the analysis |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention is the point of analysis |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | High risk | Based on figure 3 of the study's primary report, seasonality seems not to have substantially affected the direction of the observed effects. However, the statistical method is not well described, casting some doubt on its appropriateness for an ITS analysis |
Hendy 2011.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random (Quote: "After one month of baseline records, children were randomly assigned to one of the two study groups for three months of reward conditions") Number of clusters or sites: 1 elementary school Number of individuals: Beverage outcome data on 252 children were included in the analyses. Length of intervention: 3 months |
|
| Participants |
General description of participants: Children in an elementary school in a small town in Pennsylvania, USA Age: Participants were 1st to 4th grade elementary school children Inclusion criteria: Quote: "Of the 457 children who attended the 1st–4th grades at some time during the KCP application, data from 382 (83.6%) children were included in statistical analyses of the present report only if they had been a student at the school throughout the program, and only if they did not have severe disabilities that would make it difficult for them to understand the program" Exclusion criteria: See quote above Recruitment: N/R Weight status at baseline: Quote: "Of the total 382 children in the present study, 341 (89.3%) had BMI% scores available, with 11 (3.2%) being underweight with BMI% scores less than the 10th percentile, with 210 (61.6%) being average‐weight with BMI% scores between the 10th and 85th percentile, and with 120 (35.2%) being at risk for overweight or obesity with BMI% scores above the 85th percentile" SSB consumption at baseline: Not reported in the study's published report; based on information provided to us by the corresponding author, the most popular beverage at baseline was sugar‐sweetened chocolate‐flavoured milk Equity considerations: Quote: "[T]he present Kids' Choice Program (KCP) was conducted with a sample of school‐aged children from a small‐town in eastern Pennsylvania and with mostly Caucasian children. Future KCP applications could be examined in schools with more regional and ethnic diversity (...)". Participants were over 95% white, and included 211 boys and 171 girls. Children with severe disabilities were excluded |
|
| Interventions |
Intervention: Token rewards for children choosing healthy beverages during school lunch. (Quote: "The Kid’s Choice Program (KCP) was developed as an easy‐to‐use and relatively inexpensive school‐based intervention to improve well‐documented changes in children’s weight management behaviors. (…) The KCP includes three simple school procedures: (1) children wear nametags during school lunch and recess; (2) star‐shaped holes are punched into the nametags when children exhibit small amounts of specific weight management behaviors, with at least two choices being available for each behavior; (3) Reward Days are presented once each week when children can trade their stars for small prizes. (…) Reward Days were offered each week so children could trade 10 stars for one small prize (pens, fancy pencils, notebooks, modeling clay, puzzles, banks, toy gliders, stickers, water bottles, playing cards, jump ropes, stuffed animals, balls, silly hats, etc.). A large table was set up in the corner of the lunch room with large plastic bins containing a selection of five or six prizes. During the last 10 min of the lunch period for each grade, children were called by classroom to line up along the edge of the lunchroom to approach the table and trade their 10 stars for a prize of their choice. Children were given new nametags each week, but allowed to keep leftover stars toward the next week’s Reward Day") Behavioural co‐intervention: None reported Control: Alternative intervention (Quote: "The control group (...) received stars punched into their nametags for each of three ‘Good Citizenship Behaviors’ that included talking quietly during meals, keeping their meal area clean, and respecting others by not touching them or their things" |
|
| Outcomes |
Measures of SSB intake: The average number of days per week (= 6 days) in which children chose an unhealthy beverage (defined as SSB, sugar‐sweetened milk, and whole plain milk) for lunch, assessed by trained observers on 3 days each week during baseline and continuously throughout the 3‐month intervention phase Measures of intake of alternatives to SSB: The average number of days per week (= 6 days) in which children chose a low‐fat and low‐sugar healthy drink (defined as skim milk, 1% or 2% low‐fat white milk, 100% fruit juice, or water) for lunch, assessed by trained observers on 3 days each week during baseline and continuously throughout the 3‐month intervention phase Anthropometric measures: Assessed in the study but not included in this review due to confounding by non‐beverage‐specific intervention components Adverse outcomes: None reported Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary schools Sector: Education Country: USA Year(s) when implemented: N/R Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: N/R (the study's primary report does not contain a COI section) Funding: "This research was supported by grants from Penn State University. We thank the student research team members from Psychology 494 of Penn State Schuylkill for supply preparation, data collection, and data processing. For their support, we also express appreciation to the school board, superintendent, school staff, and parent volunteers of Schuylkill Haven Area Elementary Center, with special thanks to Rene Reese, Nurse Cheryl Wagner, Melanie Wade, Wally Haus, and Alberta Hudson" Trial registration: N/R Protocol availability: N/R |
|
| Notes | The study's published report shows data on healthy beverages (defined as skim milk, 1% or 2% low‐fat white milk, 100% fruit juice, or water) only. We contacted the corresponding author, who informed us that the share of children not consuming any beverage for lunch was negligible (approx. 1%), and that it can therefore be assumed that close to all children who did not select a healthy beverage selected 1 defined as unhealthy (including sugar‐sweetened milk, whole plain milk, soda, and artificial fruit drinks). She confirmed that sugar‐sweetened milk was by far the most popular beverage at baseline. We therefore included the study as a study of an intervention targeting sugar‐sweetened beverages | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | We contacted the study's corresponding author for additional information on the randomisation procedure, which is not described in detail in the study’s published report. We received the answer that participants were listed in alphabetical order and then randomly assigned to the IG and CG with a table of random numbers from a statistics textbook, with odd numbers assigned to 1 group, and even numbers assigned to the other group |
| Allocation concealment (selection bias) | Low risk | See explanation above |
| Similarity of baseline outcome measurements (selection bias) | Low risk | The difference in HDRINK between the control and intervention groups at baseline seems to have been minimal (see figure 1b of the study's primary report) |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Participant characteristics other than baseline outcome measurements are not reported for the IG and CG separately, and may have been different between groups if randomisation was not perfect. Differences in baseline provider characteristics are unlikely, as the 2 interventions (the KCP and the control intervention) were delivered by the same team of research assistants and parent volunteers |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was substantial (32%) and is not reported separately for the CG and IG. Analyses are per protocol. Only healthy beverage selection was recorded directly, and effect estimates for unhealthy beverage selection are based on the assumption that the share of children not having any beverage for lunch was approximately 1% and therefore negligible (this information was provided to us by the study’s corresponding author) |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were assessed blindly. Quote: "Lunch observers were kept blind as to children’s group assignments as they completed their lunchtime datasheets, which were then handed over to other research assistants who walked down the lunch tables, flipped over each child’s nametag to read the small print showing each child’s group assignment, and punched stars into the child’s nametag according to how many of the ‘Good Citizenship Behaviors’ or ‘Good Health Behaviors’ were recorded on the datasheet" |
| Contamination (performance bias) | High risk | Contamination is likely, and would have reduced observed effect sizes. Quote: "As in previous one month KCP applications (...), the present study found that the KCP‐targeted behaviors (FVFIRST, HDRINK, and EXERCISE) showed improvements lasting throughout the three‐month application, both for children who received the program directly (the KCP group), and for children who only observed it being applied to their classmates (the control group" |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported in the Results section |
| Other bias | Low risk | No other concerns |
Hernández‐Cordero 2014.
| Methods |
Design: RCT Timing: Prospective Allocation to group: "Assignments to each of the 24 blocks within the groups were made by random numbers generated with Microsoft Office Excel. (...) The randomization was done by the statistician of the group (...) and the treatment allocation by the project manager" Number of clusters or sites: N/A Number of individuals: 240 Length of intervention: 9 months |
|
| Participants |
General description of participants: Adult women with a BMI between 25 and 40 with a baseline SSB intake of at least 250 kcal/day, living in Cuernacava, Mexico Age: Adults (age range 18 ‐ 44 years, mean age 33 years) Inclusion criteria: Quote: "Young adult women aged >18‐<45 y; BMI >25 and <39; Consume at least 250 calories per day from caloric beverage; Women planning to live in the study area over the next year; Willingness to participate in the required evaluations; Women have given their consent to participate" Exclusion criteria: Quote: "[R]eport losing >5% of current body weight in the previous 6 months; report to be on a diet to reduce weight at the time of recruitment; report pregnancy during the previous 6 months or if they are lactating at the time of recruitment or they are planning to become pregnant in the following 12 months; report current treatment for any medical condition that could impact metabolic function (e.g., diabetes mellitus, cancer, etc.); history of myocardial infarction or heart surgery such as bypass or angioplasty; report taking any type of medication that could affect metabolism, energy intake or change body weight (e.g., hypothyroidism); report hospitalization for psychiatric problems prior year to the enrollment period; report being on a regime to increase muscle mass or taking anabolics; excessive consumption of alcoholic beverages, defined as 21 or more drinks per week" Recruitment: Quote: "Participants were recruited in Cuernavaca, Mexico, between April 2009 and November 2010, through an advertisement campaign" Weight status at baseline: Overweight and obese (a BMI between 25 and 40 was an inclusion criterion; at baseline, 47% of participants in the IG were overweight and 53% were obese. In the CG, 45% were overweight and 55% were obese SSB consumption at baseline: A baseline SSB intake of at least 250 kcal/day was an inclusion criterion. Mean baseline SSB consumption was 1127 ml/day in the intervention group, and 1094 ml/day in the control group Equity considerations: Participants lived in Cuernacava, Mexico. A broad range of occupational and educational groups were represented among the participants |
|
| Interventions |
Intervention: Home delivery of water (Quote: "To ensure water availability, the IG women received bottled water at home and/or picked it up every 2 wk. We provided 2–3 L of water per participant per day with 1 additional L/d to account for possible consumption by other family members" Behavioural co‐intervention: Dietary counseling focused on water (Quote: "Women of both groups participated in monthly face‐to‐face meetings with a dietitian and a psychologist (1 set for each group) either individually or in a group (2–10 participants each") Control: Dietary counselling only, not focused on beverages (Quote: "The IG and CG groups met separately and received equal attention. For ethical reasons, after final measurements, the CG group participated in an extra meeting with regard to water and SSB intake") |
|
| Outcomes |
Measures of SSB intake: SSB intake in ml/day, kcal/day, and % of total kcal/day, assessed through 24‐hour dietary recall at baseline, 3, 6 and 9 months Measures of intake of alternatives to SSB: Water intake in ml/day, assessed through 24‐hour dietary recall at baseline, 3, 6 and 9 months Anthropometric measures: BMI, percentage body fat and waist circumference, assessed by trained research staff using a standardised clinical protocol at baseline, 3, 6 and 9 months Adverse outcomes: Data on adverse outcomes were collected during contacts with participants during the study period (Quote: "We closely monitored the development of any adverse event (any symptom or safety concern requiring medical attention reported by a participant during a contact). Participants reporting potential adverse events were referred to the project s physician") Other outcomes: Total energy intake in kcal/d assessed through 24‐hour dietary recall at baseline, 3, 6 and 9 months; plasma lipids and glucose, and systolic and diastolic blood pressure, assessed at baseline, 3, 6 and 9 months; HbA1c, serum and urine osmolality, assessed at baseline and 9 months |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: Mexico Year(s) when implemented: 2010 ‐ 2011 (no exact dates provided) Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "None of the authors consulted with the Danone Research Center, but some of the authors received grants to conduct clinical studies (S. Barquera), grants for epidemiologic analyses/talks on beverage patterns at the British Nutrition Society (B. Popkin), or partial support for sabbatical research at the University of North Carolina at Chapel Hill (S. Hernandez‐Cordero). S. Rodrıguez‐Ramirez, M. A. Villanueva‐Borbolla, T. González de Cossio, and J. Rivera Dommarco, no conflicts of interest" Funding: "Supported in part by a grant from the Danone Research Center to the National Institute of Public Health, Cuernavaca, Mexico, which provided water for the intervention and partially supported S.H.‐C. s research sabbatical at the University of North Carolina at Chapel Hill. The Danone Research Center had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation or approval of the manuscript" Trial registration: ClinicalTrials.gov number NCT01245010 Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Women fulfilling all selection criteria (n = 240) were randomly assigned to either of the treatment groups through blocked randomization. Assignments to each of the 24 blocks within the groups were made by random numbers generated with Microsoft Office Excel" |
| Allocation concealment (selection bias) | Unclear risk | No information provided if the allocation sequence was concealed. Quote: "The randomization was done by the statistician of the group (...) and the treatment allocation by the project manager " |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline outcome measurements were similar (see tables 1 – 3 of the study's primary report) |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline characteristics were similar (see tables 1 – 3 of the study's primary report) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Results are based on an intention‐to‐treat analysis, and missing data were imputed. Quotes: "The potential effect of a low retention rate is selection bias, which we minimized by using an ITT analysis in our main analysis. (...) For continuous variables, the Markov–Monte Carlo method was used to impute missing data, generating 10 imputations." |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Dietary intake was self‐reported, and blinding of participants was not possible |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but the outcome (BMI) was objective and assessed based on a standardised clinical protocol |
| Contamination (performance bias) | Unclear risk | Quote: "Despite our requests that [IG] participants not discuss the intervention with the [CG] participants, contamination from the [IG] to the [CG] group is possible, which would make both groups very similar and affect the intervention results. The nutrition counseling that both groups received did not address weight loss or changes in beverage consumption patterns but instead covered general topics, such as sodium intake, fat content in the diet (unsaturated vs. saturated), and including vegetables in the diet. Nevertheless, it is possible that women in the EP group were motivated by joining this weight‐loss study and decided to modify some behaviors that are related to a healthier lifestyle (e.g., increasing water intake or reducing SSBs, topics that received extensive media coverage in Mexico during this period). We adhered to strict attention control limits for both groups" |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in the trial registry are reported |
| Other bias | Low risk | No other concerns |
Hobin 2017.
| Methods |
Design: Controlled ITS Timing: Prospective Allocation to group: Allocation to group depended on the intervention start date, which was determined by factors outside the control of the investigators. Quote: "In Ontario, Canada, Loblaw operates 345 supermarkets under 13 supermarket banners, including Loblaws, Zehrs, and Real Canadian Superstore (Superstore). Loblaw first implemented the Guiding Stars system in all Loblaws supermarkets in Ontario in August 2012, and all other Loblaw supermarket banners (eg, Zehrs, Superstore) in Ontario in March 2013, prior to implementing the system across all Loblaw supermarkets in Canada in September 2014. (…) Since Loblaw first implemented the Guiding Stars system in the Loblaws supermarket banner in Ontario, it enabled a pretest‐posttest design with a control group. Transaction data were acquired from Loblaw for all Loblaws (intervention condition) and Zehrs and Superstore (control conditions) supermarkets in Ontario, Canada both before and after the Guiding Stars system was implemented in Loblaws supermarkets. (…) Researchers did not have any involvement or control over the implementation of the Guiding Stars system in supermarkets" Number of clusters or sites: 126 supermarkets belonging to 3 supermarket chains (including 38 supermarkets from 1 chain which were included in the robustness checks only) Number of individuals: N/R (the analysis is based on transaction data not linked to individual participants) Length of intervention: 7 months |
|
| Participants |
General description of participants: Customers of Loblaw, Zehrs and Real Canadian Superstore supermarkets in Ontario, Canada Age: All ages Inclusion criteria: All supermarkets belonging to the Loblaw, Zehrs and Real Canadian Superstore chains in Ontario, Canada Exclusion criteria: See Inclusion criteria Recruitment: N/R Weight status at baseline: Not reported for the overall sample; however, in a subsample of customers participating in a customer survey approx. 50% reported being overweight or obese SSB consumption at baseline: N/R Equity considerations: Quote: "The geographic areas served by these Loblaw supermarkets across Ontario range from urban to rural areas with a median income of $59,017 (SD = $24,033), an employment rate of 59.3% (SD = 16.0), and 13.1% without a secondary school diploma" |
|
| Interventions |
Intervention: Nutrition rating shelf labels in supermarkets. (Quote: "Guiding Stars is a US‐based system that was adapted for Canada by an independent scientific panel with no associations to the grocery or food industry, and is administered by the Guiding Stars Licensing Company. The Guiding Stars system rates the vast majority of foods, both fresh and packaged, based on nutritional quality. However, alcohol, medical foods, natural health products, infant formula, and food items containing fewer than 5 calories per manufacturer‐specified serving size (eg, water and tea) are not rated under the Guiding Stars system. The underlying algorithm generates scores for fresh and packaged food and beverage products based on nutrient density per 100 kcal. Points are credited for vitamins, minerals, omega‐3 fatty acids, fiber, and whole grains, and points are debited for trans and saturated fats and added sodium and sugars; scores are then translated into ratings of 0 to 3 stars. Products earning ratings of 1 to 3 stars have the corresponding star symbols displayed on the shelf tag beside the price. Zero‐star items that do not meet the nutritional requirements for a star rating do not receive a rating or symbol on the label. With the exception of not labelling products earning a 0‐star rating, the Guiding Stars system is consistent with the National Academies’ recommendations for a well‐designed FOP nutrition label, and it has the potential to help consumers make more informed and nutritious food choices. (…) Researchers did not have any involvement or control over the implementation of the Guiding Stars system in supermarkets") Behavioural co‐intervention: A limited number of educational activities. (Quote: "In‐store educational and promotional materials, including brochures and aisle signage, were displayed as the Guiding Stars system rolled out across supermarkets") Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Share of beverages with 0, 1, 2, or 3 stars sold, assessed continuously throughout the study period with routinely‐collected transaction data Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Total revenues, number of products per transaction, and price per product purchased, assessed continuously throughout the study period with routinely‐collected transaction data |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: USA Year(s) when implemented: 2012 ‐ 2013 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were reported" Funding: "This work was supported by the Canadian Institutes for Health Research (CIHR). Additional support was provided by the Propel Centre for Population Health Impact, Public Health Ontario, CIHR Applied Public Health Chairs (to DH and LR), and a Banting Postdoctoral Fellowship Award (to LV)" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Baseline differences are not reported for beverages separately, only for foods and beverages considered together. For these the average star rating was considerably lower for the control than for the intervention supermarkets ‐ the baseline differences were larger than the size of the intervention's effect (see figure 2 of the study's primary report). However, this was taken into account, and the robustness checks conducted by the study authors further strengthen our confidence that the direction of the observed effects was not due to baseline differences (quotes see below) |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Baseline differences in the demographic profile of supermarket customers, and possibly also of supermarkets themselves, existed, but the robustness checks conducted by study authors strengthen our confidence that these did not substantially affect the direction of effects, and the statistical models accounted for time invariant differences across stores. Quotes: "According to Loblaw, Zehrs and Superstore supermarkets in Ontario are appropriate comparisons for Loblaws supermarkets as they are the most comparable Loblaw supermarket banners in terms of customer demographics, product profiles, and store layout. (...) In a series of robustness checks, the analysis approach was repeated (...). All of these analyses produced similar results as in the main specifications. Finally, to ascertain that the results are not due to the difference in levels of the main dependent variables and the assumption of proportional effects that comes with the use of a log model, the specifications using levels instead of logs were analyzed, producing similar results" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study used routinely‐collected electronic sales data, which can be assumed to be complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were objective (routinely‐collected sales data) |
| Contamination (performance bias) | Unclear risk | It seems unlikely that control supermarkets received the intervention, or parts of the intervention, during the study phase. However, it is possible that shoppers did not always shop at the same store; the fact that there was no blinding means that behaviours of shoppers in the control supermarkets may have been influenced by the intervention in intervention supermarkets |
| Selective reporting (reporting bias) | Unclear risk | All outcomes mentioned in the Methods section are reported. However, no trial registration is reported, and no information on the availability of a study protocol is provided. Data were provided by the supermarket after the intervention took place. Outcome reporting may be selective |
| Independence of the intervention from other changes (performance bias) | Unclear risk | It is clear from figures 2 and 3 that several changes in the wider geographic area were influencing the outcomes. However, given that the study was controlled with data from the control supermarkets, these other changes were likely accounted for |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The analysis point was the point of intervention. Additionally, the effect was estimated for the entire period; this, as opposed to testing for abrupt changes, seems appropriate for such an intervention which may need some time to gain traction and to influence the behaviour of shoppers |
| Intervention effects on data collection (detection bias) | Low risk | Routine transaction data were used |
| Other bias | Low risk | No other concerns |
Hua 2017.
| Methods |
Design: Cluster‐RCT Timing: Prospective Allocation to group: Quote: "The researchers used a random number generator to randomly assign vending machines into one of eight different conditions in a 2×2×2 factorial design that manipulated availability of healthier products, pricing, and/or promotional signage" Number of clusters or sites: 28 beverage‐vending machines (in addition to 28 food‐vending machines, which do not contribute data to the results included in this review) Number of individuals: N/R (the analysis is based on anonymous transaction data not linked to individual participants) Length of intervention: 5 months |
|
| Participants |
General description of participants: Students, staff and visitors of Yale University, USA, using beverage‐vending machines located in dormitories, libraries, administrative buildings, and department buildings with classrooms Age: All ages (no age details reported) Inclusion criteria: Quote: "Snack and beverage machines that were co‐located in a single location were included" (no further details provided) Exclusion criteria: N/R Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: Not reported for individual participants, but the study reports that "[t]he best‐selling beverages preintervention were Diet Coke (Coca‐Cola Company) (20 oz and 12 oz), Coke (Coca‐Cola Company) (20 oz and 12 oz), and Coke Zero (Coca‐Cola Company) (20 oz)" Equity considerations: Not reported explicitly, but the study's primary report seems to imply that the intervention took place at Yale University in New Haven, Connecticut, implying a socio‐economically privileged sample |
|
| Interventions |
Intervention: Vending machine redesign, including improved availability and lower prices for healthier beverages and promotional signs. (Quote: "Beverage guidelines were adapted from the New York City Agency Food Standards guidelines for vending machines. Healthier beverages included water and other beverages with 25 kcal/8 oz (eg, unsweetened iced tea or diet carbonated beverages). Based on New York City standards, these beverages made up at least 75% of available products, with the remaining 25% of products permitted to include regular, 8‐oz sodas placed in the bottom row. (…) Beverage machines randomized to the price intervention sold water for $1 (instead of the prestudy price of $1.50 to $2). (…) [B]everage machines randomized to the promotional sign intervention received one or two of two stickers, depending on condition (...): '$1 Water' or 'Rethink your drink'") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Change in best‐selling beverages, assessed continuously throughout the study period through routinely‐collected sales data Measures of intake of alternatives to SSB: Change in best‐selling beverages, assessed continuously throughout the study period through routinely‐collected sales data Anthropometric measures: N/R Adverse outcomes: Target group discontent in the case of 2 vending machines (no further details provided on how and when this outcome was assessed) Other outcomes: Revenue made in vending machines, and total number of products sold, assessed continuously throughout the study period through routinely‐collected sales data |
|
| Context and implementation |
Setting: University campus Sector: Higher education Country: USA Year(s) when implemented: 2015 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "No potential conflict of interest was reported by the authors" Funding: "Funding/Support: None to report" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The researchers used a random number generator to randomly assign vending machines into one of eight different conditions" |
| Allocation concealment (selection bias) | Low risk | Allocation was by vending machine, and allocation was done at the start of the study |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Baseline outcome measurements differed substantially across vending machines, and no means for study groups are reported. It is unclear if this was taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | All vending machines were served by the same provider, but apart from the outcome measurements no other baseline characteristics are reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 2 (out of 56) vending machines dropped out due to customer dissatisfaction, but were included in the intention‐to‐treat analyses. Sales data from the vending machines were probably close to complete. It seems unlikely that incomplete outcome data substantially influenced the results |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were objective (routinely‐collected sales data) |
| Contamination (performance bias) | High risk | All vending machines were located on the same university campus, and it is likely that vending‐machine customers, who were students, faculty and staff, did not always use the same vending machine, and were exposed to all 3 interventions in varying degrees. In particular with regard to the promotional signs and the re‐organisation of the beverage‐vending machines, this might have biased results towards null |
| Selective reporting (reporting bias) | High risk | Only outcomes for healthy beverages (but not for unhealthy beverages) are reported, even though it can be assumed that data on those were also routinely collected through the sales data system of the vending machine supplier |
| Other bias | Low risk | No other concerns |
Huang 2012.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: The study reports results from difference‐in‐difference (DD) analyses for the comparison of treated versus untreated designated marketing areas (DMAs) and for the comparison of treated versus untreated households. It also reports difference‐in‐difference‐in‐difference (DDD) estimates, which make use of both comparisons. Allocation to treated versus untreated DMAs was based on a regulatory review conducted by the study authors. (Quote: "Connecticut banned soft drink in all public schools, effective from 1 July 2006. The Hartford DMA in Connecticut therefore serves as the experimental DMA in our research design. Based on our comprehensive regulatory review, we select Atlanta, Houston, Miami and Kansas City as the non‐experimental DMAs. To our knowledge, these cities have no state, city or school district‐level soda bans in place.") Allocation to treated versus untreated households was based on demographic data provided as part of the outcome data set by the commercial market research firm Nielsen. Households with children aged 6 ‐ 18 years are assumed to be exposed to the school‐based intervention examined in this study, and households without children in this age range are assumed to be unexposed to the intervention and serve as controls Number of clusters or sites: 3185 households from 5 designated marketing areas (see table 4 of the study's primary report) Number of individuals: N/R (the analysis is done at the level of households; the household size in the IG and the CGs varied between 1.9 and 4.2 individuals per household) Length of intervention: 10 months |
|
| Participants |
General description of participants: Households with school‐aged children living in Hartford, Connecticut, USA (the IG), and households without school‐aged children living in the same district as well as households in matched comparison districts (the CG) Age: Children and teenagers (age range 6 ‐ 18 years) Inclusion criteria: Presence of children aged 6 ‐ 18 years in the household Exclusion criteria: N/R Recruitment: The study uses data provided by the commercial market research firm Nielsen (Nielsen Homescan). The study's primary report does not report details on recruitment, but provides references to the primary data set and publications describing its methodology Weight status at baseline: All weight categories (The sample is described as representative at a population level for the intervention area and the 4 control areas. Quote: "Our data consist of a geographically and demographically representative sample of household panel purchases (...) covering three years (...) in 16 geographical markets or designated marketing areas") SSB consumption at baseline: The sample is described as representative at a population level for the intervention area and the 4 control areas. Baseline SSB purchases per household were 658 ml/day in the IG, and between 565 ml/day and 406 ml/day in the CGs Equity considerations: N/R (the sample is, however, described as representative at a population level in the intervention area and the 4 control areas) |
|
| Interventions |
Intervention: Reduced availability of SSB at schools. (Quote: "During our data period, Connecticut implemented a complete ban on all regular and diet soft drink products sold in public schools effective from 1 July 2006") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Monthly purchases of SSB (including regular and diet soda) per household (excluding SSB purchases from restaurants and other food service establishments), assessed monthly during the baseline period and the first 6 months post‐intervention through the commercial Nielsen Homescan data set (the study also reports results for regular and diet soda separately; these data are included in our narrative summary only due to missing data) Measures of intake of alternatives to SSB: Monthly purchases of diet soda per household, excluding SSB purchases from restaurants and other food service establishments, assessed monthly during the baseline period and the first 6 months post‐intervention through the commercial Nielsen Homescan data set (included in our narrative summary only due to missing data) Anthropometric measures: N/R Adverse outcomes: Substitution effects, assessed as primary outcome of the study (see above) and weekly advertisement exposure for SSB (the study hypothesises that an increase in advertisement for SSB might occur as an unintended consequence of SSB bans at school), assessed with commercial advertisement exposure data throughout the study period Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2006 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This project was supported by Agriculture and Food Research Initiative Competitive Grant no. 2010‐65400‐20440 from the USDA National Institute of Food and Agriculture" Trial registration: N/R Protocol availability: N/R |
|
| Notes | For its pre‐post‐intervention comparison, the study collapses the monthly time series data into 2 data points for each of the households in the data set, 1 for the pre‐intervention and 1 for the post‐intervention period. We therefore classified the study as a CBA, and not as a controlled ITS. We report the study's DDD estimates, as these allow for a more comprehensive adjustment for confounding than the DD analyses. Quote: "The third‐level interaction (...) is the DDD estimate of the effect of the soft drink ban on out‐of‐school soda purchases (average monthly volume) for households with children aged 6–18 in Connecticut. It captures the change in volume purchase by households with school‐age children (relative to households without school‐age children) in Connecticut (relative to households in non‐experimental states) during the post‐ban period (relative to pre‐ban period). (...) The DDD specifications control for (...) time‐invariant and time‐varying factors common to all households with or without school‐age children, to all households with school‐age children only and to all households living in Connecticut. It further allows us to control for unobserved factors that are common to these groups of households” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Considerable baseline differences in outcome measurements were found, but were taken into account in the analysis. Quote: "We notice that in both experimental and non‐experimental DMAs [designated marketing areas], the volume purchases are notably lower for both the potential treatment (households with school‐age children) and the control groups. In all panels, the volume purchases by households with school‐age children are higher, but the gap between the potential treatment and control households seems similar in the pre‐ban period across the experimental and non‐experimental DMAs" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | A number of demographic, socioeconomic and economic characteristics of the CG and IG are assessed. Some differences are found, and these are taken into account in the analysis. Quotes: "First, we use pre‐treatment and post‐treatment period fixed effects, as well as month and year fixed effects to capture any trend in soft drink purchases that are common to all DMAs. Second, we use household fixed effects to control for any time‐invariant household‐level differences that could contribute to soft drink consumption" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | While some limitations to the Nielsen Homescan data are discussed in the text, these data are generally considered to be a comparatively reliable source of representative household purchase data. It seems unlikely that incomplete outcome data substantially biased the results. Quote: "We compare the demographics and locations of households who were in the panel during both periods with those who entered late or exit early. We find no statistically significant differences and conclude that sample attrition appears to be random" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | This is a retrospective analysis of routinely‐collected commercial household purchase data, which can be considered objective |
| Contamination (performance bias) | Low risk | Based on the information provided by the study authors it seems unlikely that exposure of the CG to SSB restrictions at school substantially affected the results. Quote: "Credible estimation of treatment effects in our empirical strategy relies on correctly defining a treatment and control groups in our empirical framework. We therefore conducted a comprehensive review of existing policies, using the yearly update and overview provided by the National Conference of State Legislators, cross‐checked available local government and school district information and searched local and national media to detect potential related interventions at the city, school district and school level" |
| Selective reporting (reporting bias) | Low risk | This was a retrospectively‐conducted CBA using routinely‐collected data. All outcomes mentioned in the Methods section are reported in the Results section |
| Other bias | Low risk | No other concerns ‐ the robustness checks in particular suggest that results were not substantially biased by the statistical models. Quote: "Furthermore, the results for our primary variables of interest are robust to any number of specifications including subsets of our additional controls such as including market‐level controls only. In addition, we explored a number of alternative specifications not reported here. Rather than using average monthly purchases, we summed purchases over the school semesters and used monthly purchases with additional month fixed effects. We also classified households as light and heavy soda drinkers to test whether these groups were affected differently by the ban. In addition, we investigated the effect on regular versus diet soda. And finally, we investigated private label versus branded products, as soft drinks available at school are exclusively provided by the leading national‐level brands. However, in all of those specifications, we fail to detect statistically significant treatment effects in the DDD specifications" |
Lichtman‐Sadot 2016.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: The study reports results from difference‐in‐difference analyses for the comparison of treated vs untreated school districts and for the comparison of treated vs untreated households. It reports difference‐in‐difference‐in‐difference estimates, which make use of both comparisons. Quote: "The assignment of treatment status for each household's monthly purchases of soda is determined based on three dimensions: which school district the household belongs to (treated vs. untreated school districts), when the household is observed (before or after treatment), and whether the household has children in the treated school‐level present. This entails the opportunity to utilize a difference‐in‐differences‐in‐differences (triple differences) strategy. The triple differences strategy combines two control groups – households in untreated school districts and untreated households (due to the age of household members) within treated school district boundaries – in one single specification." Allocation to treated vs untreated school districts was based on a review of relevant regulations by the study author, and allocation to treated vs untreated households was based on demographic data provided by the market research firm Nielsen as part of the household‐level purchasing data used for the main analysis Number of clusters or sites: 10,308 households in 46 school districts Number of individuals: N/R (the analysis is done at the level of households; the mean number of individuals per household was 2.3) Length of intervention: 36 months (individual households were on average for 22 months in the sample, but the entire data set covers 12 quarters post‐implementation; see figure 2 of the study's primary report) |
|
| Participants |
General description of participants: Households with school‐aged children living in school districts in the USA which restricted access to SSB at schools during 2004 and 2009 (the IG), and households without school‐aged children and households living in school districts which did not implement new restrictions on SSB at school during 2004 and 2009 (the CG) Age: Children and teenagers (participants were households with elementary, middle or high school‐aged children) Inclusion criteria: Quote: "School districts were targeted for collection of their carbonated beverage policies if they fulfilled either one of two sets of criteria: either the school district covered an entire county and that county had at least 60 households in the 2007 Nielsen Homescan data, or the school district had at least 50,000 students enrolled in it in 2005 and the county where the school district is located had at least 90 households in the 2007 Nielsen Homescan data" Exclusion criteria: Quote: "If details of carbonated beverage restrictions could not be verified sufficiently or produced conflicting information, target school districts were not included in the sample of covered school districts, as including them would likely measure the timing and nature of the treatment with substantial error. Furthermore, if the timing of the policies found for these school districts was between January 2002 and December 2003, these school districts were also excluded from the analysis because the Nielsen data – beginning only in January 2004 – does not capture the initial period after the policy's introduction" Recruitment: The study uses data provided by the market research firm Nielsen, which collects purchasing data from a nationally representative sample of volunteer households across the USA. The study does not report how participants are recruited by Nielsen, but provides references to relevant publications Weight status at baseline: N/R (The study does, however, note that the sample studied may not be representative for the US population. Quote: "Comparing the descriptive statistics between the households in the samples and those in the Nielsen data reveals that the households in the analysis are likely not representative of the entire U.S. population. This raises the question of how much our results can be generalized to household consumption patterns for the general population and compensation in response to carbonated beverage bans in schools. With respect to this, it is reassuring that a robustness check in Table 4 exhibits that the results do not change substantially when adding time‐varying household characteristics. This suggests that the results are not being driven by household characteristics specific to the sample of households in use") SSB consumption at baseline: Mean purchases of SSB per household were 265 ml/day for households with elementary school‐aged children, 312 ml/day for households with middle school‐aged children, and 334 ml/day for households with high school‐aged children Equity considerations: Quote: "The racial composition of the households in our samples is about 16 percent Black and 8 percent Hispanic. Nielsen families excluded from the analysis have lower rates of Blacks and Hispanics, (...) a reflection of the urban nature of our sample of school districts. Roughly 53% of households have a bachelor's degree or higher, and about 11% of households earned less than $10,000 annually per household member while 7% had earned an annual household income exceeding $125,000 during the sample period" |
|
| Interventions |
Intervention: Reduced availability of SSB at school. (Quote: "The term treatment refers to the introduction of a ban on carbonated beverages in a school district for the entire school day during the sample period (2004–2009)") Behavioural co‐intervention: None reported Control: No or minimal intervention. (School districts restricting the sale of carbonated beverages only during part of the school day, and school districts which had passed restrictions at least two years prior to the start of data collection were classified as untreated. Quote: "Many school districts implemented restrictions on the availability of carbonated beverages during part of the school day (...). These restrictions were not considered carbonated beverage restrictions for the construction of the policy data set (...). School districts with restrictions taking place prior to January 2002 are included in the analysis and categorized as untreated. The underlying assumption behind this is that two years is sufficient time for all households in the sample to adapt (at least in terms of purchasing trends) to any past restrictions implemented in their child's school") |
|
| Outcomes |
Measures of SSB intake: Household SSB purchases in ounces/month, assessed continuously by participating households with a barcode scanner at baseline and for up to 36 months post‐intervention Measures of intake of alternatives to SSB: The study reports data on the effects of restrictions of the sale of diet beverages on household purchases of diet beverages. These data are not included in our review as the intervention does not meet our inclusion criteria. No data on the effects of restrictions of the sale of SSB on household purchases of diet beverages is reported Anthropometric measures: N/R Adverse outcomes: Substitution effects, assessed as primary outcome of the study (see above) Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2004 ‐ 2009 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "I am grateful to the U.S. Department of Agriculture, Economic Research Services for providing the Nielsen Homescan data. (…) The research leading to these results has received funding from the People Programme (Marie Curie Actions) of the European Union Seventh Framework Programme (FP7/2007‐2013) under REA grant agreement no. 630714” Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline differences in outcome measurements between treated and untreated households existed (see table 7 of the study's primary report), but were taken into account in the analysis. The controlled ITS design and the large sample size (8146 households in 46 school districts) strengthen our confidence that baseline differences could be sufficiently controlled for with the statistical methods used by the study author. Quote: "The inclusion of the variables (...) for each of the three school‐levels controls for purchasing levels among households with a certain number of children in each of the school‐levels, irrespective of whether the household is treated and when it is observed" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline differences between treated and non‐treated households existed (see table 3 of the study's primary report), but were taken into account in the analysis. The controlled ITS design and the large sample size strengthen our confidence that baseline differences could be sufficiently controlled for. Quote: "Household fixed effects are included to control for unobserved household characteristics (...). Xit controls for time‐varying household characteristics ‐ household size, the presence of children under six years old in the household, whether either household head is 55 or over, whether annual household income is less than $10,000 per household member, and full‐time employment of either household heads. These variables vary annually, when Nielsen updates its surveys of household members’ demographic characteristics. 0j estimates school‐district‐specific linear time trends to account for any changes over time in households’ soda consumption that are specific for households residing within a specific school district’s boundaries" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | While some limitations to the Nielsen Homescan data are discussed in the text, they are still considered to be a comparatively reliable source of representative household purchase data. It seems therefore unlikely that incomplete outcome data substantially biased the results (but note the issues discussed in the domain 'Other risks of bias') |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Contamination (performance bias) | Low risk | The allocation to treated vs non‐treated households was based on the presence of school‐aged children in the household, and it is unlikely that households without school‐aged children were exposed to this school‐based intervention to a substantial extent. The allocation to treated vs non‐treated school districts was based on a comprehensive regulatory review, and the study author took precautions to avoid contamination. Quote: "If details of carbonated beverage restrictions could not be verified sufficiently or produced conflicting information, target school districts were not included in the sample of covered school districts, as including them would likely measure the timing and nature of the treatment with substantial error. Furthermore, if the timing of the policies found for these school districts was between January 2002 and December 2003, these school districts were also excluded from the analysis because the Nielsen data – beginning only in January 2004 – does not capture the initial period after the policy's introduction" |
| Selective reporting (reporting bias) | Low risk | The study report does not mention if the study was registered, or if the study protocol included outcomes that were prespecified. However, the study reports all outcomes mentioned in the Methods section, and all important outcomes which may be expected in a study of this kind, and which could be analysed with the data used, are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | While the intervention may not have been independent of other changes, it is unlikely that the effects shown by the study are explained entirely by these. Quote: "I address the potential for endogeneity of the carbonated beverage restrictions in school districts with three arguments: First, I argue that at least the exact timing of the implementation of these restrictions is unrelated to household preferences in their respective school district. Second, the inclusion of school‐district‐specific linear time trends in the regression specifications should alleviate at least some of the concern for not capturing any pre‐existing trends in households' consumption of carbonated beverages. Last and most importantly, I argue that the triple differences specification alleviates concerns that events/factors/shocks which are correlated with the occurrence of carbonated beverage restrictions in schools but not related to these restriction are driving the results. This is because any such events/factors/shocks would have to differentially affect households with treated high school children within the boundaries of the school district, in comparison to all other households in the school district boundaries" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention was the point of analysis. Quote: "The triple differences specification (...) includes separate dummies for each quarter before and after the restriction implementation. While the post‐treatment estimates assess whether the treatment effect varies over time, the pre‐treatment coefficient estimates are extremely useful for detecting whether any pre‐existing trends in treated households’ soda consumption existed prior the introduction of the carbonated beverage ban" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Unclear risk | The study author notes that some types of purchases which are potentially relevant for the study's research question may not be covered reliably by the Nielsen Homescan data. This may have biased the observed effects towards null. Quote: "It is important to note that food purchases from restaurants or vending machines are not documented. In addition, while small purchases from convenience stores should be documented by the household, these purchases are generally omitted from most households’ scanning activity. Thus, for the most part, the data does not document any beverage purchases students make in school and it very likely does not capture beverage purchases students make on their way to/from school or while on lunch breaks off campus" |
Minaker 2016.
| Methods |
Design: ITS Timing: Retrospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 1 pharmacy (in which the intervention was implemented) and 2 further stores selling SSB Number of individuals: N/A (the study is based on routinely‐collected sales data not linked to individual customers) Length of intervention: 8 months |
|
| Participants |
General description of participants: Residents and visitors of Baddeck, a small rural community on Cape Breton Island, Nova Scotia, Canada Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: "Baddeck is a rural small town (population approximately 800 year‐round residents) on Cape Breton Island in Nova Scotia. Baddeck is a popular tourist destination in the summer months, and throughout the year functions as a service center for the surrounding, sparsely populated county. The nearest urban municipality is Sydney, Nova Scotia (population 31,597), 80 km away (about an hour’s drive). The community nutrition environment in Baddeck includes twelve restaurants (several of which are only open seasonally), and three food stores including the pharmacy" |
|
| Interventions |
Intervention: Removal of SSB from 1 out of 3 stores selling SSB in a small, remote community. (Quote: "This study examines an intriguing example of a recent retailer‐led restrictive RFE [retail food environment] intervention in the province of Nova Scotia, Canada. In September 2014, a pharmacist made national and regional news by removing all sweet beverages from his pharmacy’s shelves. When questioned about his objectives, the pharmacist commented, ‘It made no sense to me. Just in good conscience, we just couldn’t continue selling’") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Weekly community‐wide sales of SSB in Canadian dollars, assessed continuously throughout the study period with routinely‐collected sales data Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not (but community‐wide sales of SSB are assessed as a measure of switching behaviour among stores within the community) Other outcomes: None included in this review |
|
| Context and implementation |
Setting: A rural community pharmacy Sector: Retailing Country: Canada Year(s) when implemented: 2014 Mode of implementation: Pilot trial by researchers in co‐operation with a private pharmacy Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Competing interests: LMM, NN, SA, CLM, BEC, and DLO have no financial disclosures and no competing interests to declare. GM is employed by Atlantic Pharmasave" Funding: "LMM, NN, and SA acknowledge the support of the Canadian Cancer Society Research Institute [Major Program Grant #701019] to the Propel Centre for Population Health Impact, which funded the study. CLM holds a Canadian Institute of Health Research Grant. DLO is supported by a Canadian Institutes of Health Research Fellowship" Trial registration: N/R Protocol availability: N/R |
|
| Notes | We report results from the ARIMA model, as this model is described as the most‐adjusted one by the study authors. Quote: "Although several analytical options exist to analyse time series data, our interrupted time series data were most appropriately analysed using autoregressive integrated moving average (ARIMA) models. These models attempt to account for all aspects of data series autocorrelation, and are appropriate for repeated measures data assessed at equal intervals" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The outcome data were routinely‐, automatically‐collected sales data, so it is likely that they are close to complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported in the Results section, and based on how data collection and assessment are described it seems likely that SSB sales were indeed the only outcome which was assessed |
| Independence of the intervention from other changes (performance bias) | Unclear risk | The paper notes that the composition of the customer base of the 3 stores in Baddeck (the intervention community) is fluctuating seasonally (e.g. permanent residents versus visitors), which could potentially affect the observed effect sizes. Quote: "In addition, the relatively short follow‐up time precluded an analysis of CSD [carbonated soft drinks] during a summer peak in which the policy was in place, when a different type of consumer (namely tourists) would have comprised a greater proportion of people purchasing CSD [carbonated soft drinks]" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of analysis is the point of intervention |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns |
Muckelbauer 2009.
| Methods |
Design: NRCT Timing: Prospective Allocation to group: Schools in 1 city (Dortmund, Germany) served as intervention sites, and schools in another city (Essen, Germany) served as control. Quote: "Schools in Dortmund represented the intervention group and schools in Essen the control group. For each city, 20 schools were selected randomly" Number of clusters or sites: 33 schools Number of individuals: 2950 Length of intervention: 10 months |
|
| Participants |
General description of participants: Elementary school children in deprived neighbourhoods in Dortmund and Essen, Germany Age: Childen (mean age 8.3 years) Inclusion criteria: School‐level (quote): "Schools were eligible for participation if they were located in deprived areas, as defined with the following criteria: unemployment rate of >15%, proportion of social welfare recipients of >5%, and proportion of non‐German residents of >5%, as indicated by the local public authorities." Student‐level: Parental consent Exclusion criteria: N/R Recruitment: N/R Weight status at baseline: The prevalence of overweight was 23% at baseline in the IG and 26% in the CG. Mean baseline BMI SDS was 0.23 in the IG and 0.30 in the CG SSB consumption at baseline: At baseline, SSB consumption was 260 ml/day in the IG and CG Equity considerations: Quote: "The study population comprised children attending the second and third grades of elementary schools in deprived neighborhoods of 2 neighboring cities, namely, Dortmund and Essen, Germany. Both cities have a population of ∼600 000 and are located in the Ruhr Area, a conglomerate of formerly industrial cities. (...) From a public health perspective, it is of importance that this intervention was effective in a deprived population, in which the prevalence of obesity was up to 3 times greater than that among children of a higher socioeconomic background.” A secondary analysis showed that the intervention was more effective in children without migration background (i.e. children whose parents and grandparents were born in Germany). Quote: "After intervention, the risk of being overweight was reduced in the IG compared to the CG among non‐MIG [i.e. children without migration background] (odds ratio = 0.51, 95% confidence interval (CI): 0.31–0.83), but not among MIG children (odds ratio = 1.02, 95% CI: 0.63–1.65)" |
|
| Interventions |
Intervention: Improved access to drinking water at school. (Quote: "In each IG school, 1 water fountain (Sodamaster‐Aquatower 200; IONOX‐Wassertechnologie, Obertraubling, Germany), or 2 for schools with 150 participants, was installed. The fountains provided cooled, filtered, plain or optionally carbonated water. In addition, each child received a plastic water bottle (500 mL). (...) In month 5 after the baseline assessment, each participant received a new water bottle with an improved handling design") Behavioural co‐intervention: Organised water bottle fill‐ups and nutrition education focused on water. (Quote: "[T]eachers were encouraged to organize filling of the water bottles each morning for all children in the corresponding classes. The educational intervention consisted of four 45‐minute classroom lessons dealing with the water needs of the body and the water circuit in nature. At the beginning of the study, teachers received a booklet with the prepared curriculum and necessary materials to implement the lessons in the formal school curriculum. The lessons were developed by using the results of empirical teaching research and were intended to improve the constructs of intention, attitudes, and perceived behavioral control, on the basis of the theory of planned behavior. Three months after the beginning of the study, teachers introduced a motivation unit (ie, booster sessions) that used a goal‐setting strategy to reach a sustained increase in water consumption by giving quantitative targets and feedback") Control: No intervention (Quote: "CG schools did not receive any intervention") |
|
| Outcomes |
Measures of SSB intake: SSB intake, assessed with a 24‐hour recall questionnaire that was self‐completed under teachers’ supervision at baseline and 10 months Measures of intake of alternatives to SSB: Water and juice intake, assessed with a 24‐hour recall questionnaire that was self‐completed under teachers’ supervision at baseline and 10 months Anthropometric measures: Prevalence of overweight and BMI SD‐Scores, assessed by trained healthcare professionals at baseline and 10 months Adverse outcomes: The study does not report how data on adverse outcomes were collected, but states that none were observed Other outcomes: Target group and stakeholder perceptions and uptake, assessed with interviews and questionnaires and by reading the integrated flow meters at baseline and at 6 control visits during the intervention period |
|
| Context and implementation |
Setting: Schools Sector: Education Country: Germany Year(s) when implemented: 2006 ‐ 2007 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The authors have indicated they have no financial relationships relevant to this article to disclose" Funding: "This trial was carried out by the Research Institute of Child Nutrition Dortmund (Dortmund, Germany), and was supported by grant 05HS026 from the German Federal Ministry of Food, Agriculture, and Consumer Protection. Intervention materials (water fountains, bottles, and lesson booklets) were provided by the Association of the German Gas and Water Industries. Ms Muckelbauer and Mr Libuda received research funding from grant 05HS026 from the German Federal Ministry of Food, Agriculture, and Consumer Protection" Trial registration: ClinicalTrial.gov number NCT00554294 Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a NRCT, and allocation to the IG and CG was not random. Quote: "Schools in Dortmund represented the intervention group (IG) and schools in Essen the control group (CG). For each city, 20 schools were selected randomly" |
| Allocation concealment (selection bias) | High risk | This was a NRCT, and allocation was not random and not concealed (see quote above) |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "The IG and CG did not differ in baseline characteristics regarding prevalence of overweight, BMI SDS, gender, age, and migrational background. Water and soft drink consumption levels at baseline were similar in the IG and the CG, but the level of juice consumption was slightly higher in the IG than in the CG" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline characteristics were assessed and similar (see table 1 of the study's primary report) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | A per‐protocol analysis was performed, and the attrition rate was higher in the CG than in the IG (1 control school withdrew, stating time requirements for data collection), but baseline characteristics of dropouts and non‐dropouts were similar, and overall attrition was in an acceptable range. For the questionnaire data a substantial number of participants (33%) were excluded due to implausible values. Quote: "Of 3190 children screened at baseline, a total of 2950 children (92%) were also measured at the follow‐up assessment and were considered for analysis. Dropouts (n = 240) were similar to analyzed participants with respect to the prevalence of overweight (24.6% vs 24.5%; P = .741), mean BMI SDS (0.26 vs 0.26; P = .807), mean age (8.27 vs 8.30 years; P = .574), proportion of boys (50.4% vs 50.2%; P = .772), and proportion of children with migrational background (42.1% vs 44.3%; P = .568). (...) Overall, 1987 (67%) of 2950 analyzed children (IG: 65%; CG: 70%) had plausible questionnaires on beverage consumption at both baseline and follow‐up assessments" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and social desirability bias, which might have been reinforced by the behavioural components of the intervention, may have biased the results for beverage intake data, which was self‐reported |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Body weight outcomes were objective, and assessed by trained health professionals following a standardised protocol |
| Contamination (performance bias) | Low risk | Intervention and control schools were located in different cities, and it is unlikely that contamination substantially affected results |
| Selective reporting (reporting bias) | Low risk | The trial was registered after the start but before the end of the study, and all important outcomes mentioned in the Methods section are reported |
| Other bias | Low risk | No other concerns |
Ng 2014a.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: The IG were companies which self‐selected to participate in the Healthy Weight Commitment Foundation Market Place Pledge (the intervention), and the CG were companies not participating in this Pledge for which data were available from the Nielsen Scantrack database. Quote: "Nielsen Scantrack data from 2007 and 2012 were used to track the total caloric sales in the U.S., and caloric sales from three mutually exclusive brand categories: HWCF [Healthy Weight Commitment Foundation] brands; non‐HWCF national brands; and private labels ([PLs], also known as store or generic brands, produced by HWCF or non‐HWCF companies, but controlled by retailers). (…) To distinguish the mutually exclusive proportion of calories from HWCF companies, non‐HWCF companies, and PL, all foods and beverages were classified according to our best understanding of brands and product lines. This included identifying brands/product lines manufactured and sold by each of the 16 companies annually during the period from 2007 to 2012 to determine when sales, purchases/acquisitions or mergers, introductions/product launches, or discontinuations of brands/product lines by each of the HWCF companies occurred" Number of clusters or sites: N/A Number of individuals: N/A (The analysis is based on commercial sales data not linked to individual participants) Length of intervention: 4 years |
|
| Participants |
General description of participants: Consumers of consumer‐packaged goods in the USA Age: All ages Inclusion criteria: N/R (but references to relevant secondary publications are provided) Exclusion criteria: See inclusion criteria Recruitment: See inclusion criteria Weight status at baseline: N/R (But the sample is described as nationally representative of the US general population) SSB consumption at baseline: See weight status Equity considerations: See weight status |
|
| Interventions |
Intervention: Food and beverage industry self‐regulation. (Quote: "The HWCF [Healthy Weight Commitment Foundation Marketplace Pledge] is a national, multi‐year effort designed to help reduce obesity ‐ especially childhood obesity ‐ by 2015. In the marketplace, HWCF’s focus is on 'reducing or controlling calories while preserving or enhancing the overall nutrition of healthier product options.' Using 2007 as a baseline year, 16 HWCF food‐manufacturing companies pledged to collectively sell 1.5 trillion fewer calories from the marketplace by 2015, with an interim goal of 1 trillion calories by 2012. The 1.5 trillion target was based on the estimated HWCF share (25% of total energy consumed in the U.S.) of the published estimates of the calorie gap needed to prevent excessive weight gain among the nation’s children and adolescents aged 2–18 years, assuming that both dietary/caloric intake and physical activity/energy expenditure should have an equal role in reducing obesity. The Robert Wood Johnson Foundation stepped forward to fund a rigorous, independent evaluation of the HWCF marketplace pledge to assess its impact on the numbers of calories sold and purchased in the U.S., and consumed by the nation’s children and adolescents") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Average daily calories (kcal/per capita/day) from beverages, assessed with commercial sales and purchasing data (Nielsen Scantrack and Homescan) at baseline and at 4 years follow‐up Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Food and beverage companies Sector: Food and beverage industry Country: USA Year(s) when implemented: 2008 ‐ 2012 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "Shu Wen Ng and Meghan M. Slining have not consulted with or been a part of any conflicting relationship with the 16 HWCF companies evaluated in this project. Barry M. Popkin has been a co‐investigator of one RCT funded by Nestle’s Water USA but has never consulted for them. He has a gift from Kraft and Gerber Foods to co‐fund the dietary intake portion of the National Nutrition and Health Survey 2011–2012 conducted in Mexico by the National Institute of Public Health, Mexico" Funding: "The work presented in this paper was supported by funds from the Robert Wood Johnson Foundation (RWJF) for the Healthy Weight Commitment Foundation Evaluation project (Grant Nos. 67506, 68793, and 70017) and the Carolina Population Center (Grant No.5R24 HD050924). (...) Shu Wen Ng, Meghan M. Slining, and Barry M. Popkin are funded by grants from NIH and RWJF" Trial registration: N/R Protocol availability: The study's protocol has been prospectively published as a separate paper (Slining 2013) |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Beverage calories sold per capita per day differed considerably across the 3 brand categories at baseline (75 kcal/per capita/day for HWCF brands, 122 kcal/per capita/day for non‐HWCF national brands, and 76 for private‐label brands). These differences were taken into account in the analysis, but given their magnitude they may hint at unobserved baseline differences and may have given rise to bias |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | The Nielsen Scantrack data, which is the main data source for the analysis, does not contain information about the individuals that products were sold to, but it seems likely that there were systematic differences between individuals buying predominantly HWCF products and those buying mainly non‐HWCF products. Moreover, while not discussed explicitly by the study authors, it can be assumed that HWCF companies were systematically different from non‐HWCF companies at baseline, since they self‐selected into the HWCF group, and were major, mainly multinational companies, whereas the group of non‐HWCF companies contains a large, diverse set of food and beverage companies. In addition, major changes took place during the time of the study, including the economic crisis of 2007 ‐ 2009, which may have affected the 3 brand categories and their respective customers differently |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Concerning data collection, incomplete outcome data seems to be adequately addressed by the sophisticated methodology used for the Nielson Scantrack and Homescan data, which is generally considered to be comparatively reliable. Concerning data analysis, study authors seem to have taken precautions to minimise problems arising from incomplete or imperfectly matched outcome data. Quote: "The Scantrack data contain information on the weekly dollar sales and units sold of all UPC transactions at participating grocery, drug, and mass‐merchandisers in 2007 and 2012. These are point‐of‐sale data and do not include information about the individuals or households that products were sold to. Sampling limitations and representativeness are offset by using the Nielsen Homescan data. Nielsen Homescan data from 2007 and 2012 were used to track total caloric purchases and caloric purchases by U.S. households from each of the three brand categories. The Homescan data contain detailed UPC‐level information about household food purchases brought into the home and cover all UPC transactions from all outlet channels, including grocery, drug, mass‐merchandise, club, supercenter, and convenience stores" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | The outcome data (Nielsen Scantrack data) can be considered objective |
| Contamination (performance bias) | Unclear risk | Contamination is likely, in particular between HWCF brands and private‐label brands, and would have biased results towards null |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes mentioned in the Methods section are reported in the Results section, and very detailed results for all food and beverage groups as defined in the Nielsen Homescan data set are provided in the study's appendix |
| Other bias | Low risk | No other concerns |
Ng 2014b.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: See Ng 2014a Number of clusters or sites: 61,126 households Number of individuals: N/R (the analysis is done at the level of households) Length of intervention: 4 years |
|
| Participants |
General description of participants: Households with children aged 2 ‐ 18 years, living in the USA Age: All ages (however, only households with at least 1 child aged 2 ‐ 18 years were included) Inclusion criteria: Households with at least 1 child aged 2 ‐ 18 years for which data were available from the Nielsen Homescan database were included. References to publications providing details on the methods used by Nielsen Homescan, a commercial market research firm, are provided Exclusion criteria: See inclusion criteria Recruitment: See inclusion criteria Weight status at baseline: N/R (But the sample is described as nationally representative of US households with children) SSB consumption at baseline: See weight status Equity considerations: See weight status |
|
| Interventions |
Intervention: See Ng 2014a Behavioural co‐intervention: See Ng 2014a Control: See Ng 2014a |
|
| Outcomes |
Measures of SSB intake: Kcal/per capita/day from carbonated soft drinks purchased by households with children, assessed continuously throughout the study period with commercial household‐level consumer purchase data (Nielsen Homescan data) Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Food and beverage companies Sector: Food and beverage industry Country: USA Year(s) when implemented: 2008 ‐ 2012 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: See Ng 2014a Funding: See Ng 2014a Trial registration: See Ng 2014a Protocol availability: See Ng 2014a |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Beverage calories purchased per household per day were similar across the 3 brand categories at baseline (62 kcal/household/day for HWCF brands, 67 kcal/household/day for non‐HWCF national brands, and 69 kcal/household/day for private‐label brands). These differences were taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | It seems possible that households purchasing predominantly HWCF brands were systematically different from households purchasing mainly non‐HWCF name brands and private‐label products. The Nielsen Homescan data set contains information on sociodemographic and socio‐economic parameters, and these data were used for adjustment in the ITS analysis, but not in the unadjusted CBA comparison. No data on baseline differences are reported. The study acknowledges that the portfolio of HWCF and non‐HWCF companies may have been different at baseline, and affected differently by concurrent trends. Quote: "A basic approach to assess the HWCF pledge would be to compare how the absolute and relative calories purchased changed in the pre‐pledge period compared to the post‐pledge period, and how these varied for HWCF products versus non‐HWCF products. However, this approach assumes that the portfolio of HWCF and non‐HWCF products are similar and comparable, (...),and that other factors (e.g., economy, prices, sociodemographic composition) would not affect purchases of HWCF versus non‐HWCF products differentially" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Incomplete and imperfectly‐matched outcome data may have affected the effect estimates. Quote: "For this paper, identification of HWCF products in each year was based on information on the brand and manufacturer of each Universal Product Code (UPC) provided by Nielsen Homescan. This approach differed from that used in the previous paper because it was not possible to reliably or consistently find information about the sales, acquisitions, joint manufacturing, or shared distributions of brands from the 16 HWCF companies going back to 2000. Additionally, it was not possible to apply the inclusion and exclusion criteria to reliably distinguish those products considered to belong to the HWCF companies across 13 years of data in a logical manner given mergers, acquisitions, and changes in distribution agreements across the companies" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | The outcome data (Nielsen Scantrack data) can be considered objective |
| Contamination (performance bias) | Unclear risk | Contamination is likely, in particular between HWCF brands and private‐label brands, and would have biased results towards null |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes mentioned in the Methods section are reported in the Results section, and very detailed results for all food and beverage groups as defined in the Nielsen Homescan data set are provided in the study's appendix |
| Independence of the intervention from other changes (performance bias) | High risk | Authors point out that there are various demand and supply‐side factors which occurred independently of the intervention and that could have contributed to less energy‐dense products offered and sold |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The Healthy Weight Commitment Foundation (HWCF) declared 2007 to be the base year for its pledge, and the point of analysis is the turn of the year 2007/2008. While the pledge was publicly announced only in 2009, HWCF companies may have started earlier with relevant measures. It therefore seems appropriate to consider the turn of the year 2007/2008 also as the point of intervention |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | High risk | The results of the calculation of the best‐fit counterfactual seem unrealistic, as they imply that calories purchased as beverages from HWCF brands would fall to zero by 2013 (2012 for carbonated soft drinks, see Figure FA and Appendix Figure C3a of the study's primary report). However, it should also be acknowledged that attempts to ensure reproducibility, integrity and quality were made: Quote: "To ensure the highest scientific integrity and quality, an independent Evaluation Advisory Committee of eminent scholars provided scientific review and advice. A critical dimension of all work is reproducibility in decisions regarding the methods and metrics used" |
Ni Mhurchu 2010.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Quote: "Eligible participants were randomly assigned to 1 of the following 4 intervention arms: price discounts on healthier supermarket foods, tailored nutrition education promoting purchase of healthier supermarket foods, a combination of price discounts and tailored nutrition education, or control (no intervention)" Number of clusters or sites: N/A Number of individuals: 1028 Length of intervention: 6 months (+ 6 months additional follow‐up after the end of the intervention) |
|
| Participants |
General description of participants: Adult customers of supermarkets in the Lower North Island region of New Zealand who were the main shoppers of their households Age: Adults (age ≥ 18 years was an inclusion criterion, mean age was between 43 and 45 years in the 4 study groups) Inclusion criteria: Quote: "Trial eligibility criteria were as follows: age ≥18 y, the main household shopper, a regular shopper at participating stores, and either a registered user of the Shop 'N Go system or willing to sign up and use the system for the duration of the trial" Exclusion criteria: N/R Recruitment: Quote: "Recruitment took place over 9 mo beginning in February 2007. Recruitment methods and outcomes have been described in detail previously. Strategies used were mail‐outs to a random selection of customers who were registered to use the Shop 'N Go system and in‐store and community‐based recruitment targeted to Māori and Pacific shoppers. (...) Initial contact with potential participants was either by telephone for those who received a mailed invitation to participate in the trial or face‐to‐face for those who were approached in‐store or in the community" Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote 1: "The population was moderately diverse and included higher proportions of priority populations [Māori (23%) and Pacific (9%)] than would be expected on the basis of their representation in the population (15% and 7%, respectively). Most participants were women (which reflected their frequent role as main household shoppers), and there were approximately equal numbers of participants from high‐ and low‐income households. However, the study population was relatively well educated compared with the general New Zealand population, and a high proportion (85%) self‐rated their knowledge of nutrition and healthy eating as ‘moderate‘ or ‘a lot.‘ Thus, although findings should be applicable to a reasonably socioeconomically diverse population, it is likely the study population had a higher level of baseline nutrition knowledge and interest than average." Quote 2: "There was an association of price discounts with healthy food purchasing (0.79 kg/week increase; 95% CI 0.43 to 1.16) that varied by ethnicity (p=0.04): European/other 1.02 kg/week (n=755; 95% CI 0.60 to 1.43); Pacific 1.20 kg/week (n=101; 95% CI 0.06 to 2.34); Māori −0.15 kg/week (n=248; 95% CI −1.10 to 0.80). This association of price discounts with healthy food purchasing did not vary by household income or education. (...) While a statistically significant variation by ethnicity in the effect of price discounts on food purchasing was found, the authors caution against a causal interpretation due to likely biases (eg, attrition) that differentially affected Māori and Pacific people. The study highlights the challenges in generating valid evidence by social groups for public health interventions" |
|
| Interventions |
Intervention: A 12.5% price reduction for water and low‐calorie beverages implemented through a supermarket loyalty card scheme. (Quote: "The price discount intervention consisted of an automatic 12.5% price reduction on all eligible healthier food products, and discounts were available only to study participants in the discount intervention groups. Choice of discount level was pragmatic because a 12.5% price discount is equivalent to removal of the goods and services tax (GST), which is applied to all consumer products (including all foods) in New Zealand. Foods eligible for price discounts were core foods (excluding chocolate, potato chips, sports supplements, baby foods, etc) that met Tick program criteria. Participants who were randomly assigned to receive discounts were mailed a printed list of discounted foods at regular intervals throughout the study, and discounts were implemented when Shop ’N Go cards were scanned at checkouts during the intervention period") Behavioural co‐intervention: None (2 of the 4 study arms received a tailored nutrition education programme; data for these 2 arms are not included in our review) Control: No intervention (Quote: "Eligible participants were randomly assigned to 1 of the following 4 intervention arms: (...) or control (no intervention)" |
|
| Outcomes |
Measures of SSB intake: Energy density (MJ/kg) of beverages purchase, assessed continuously throughout the study period with electronic sales data at 6 and 12 months Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Target group perceptions, assessed with a comprehensive process evaluation using a variety of methods |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: New Zealand Year(s) when implemented: 2007 ‐ 2009 Mode of implementation: Pilot trial by researchers in co‐operation with a private supermarket chain Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "There is no conflict of interest" Funding: "This study was funded primarily by the Health Research Council of New Zealand and the National Heart Foundation of New Zealand. The Cancer Society of New Zealand also provided some financial support" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available, but methods and results of a pilot study on which the study is based were published as a separate publication |
|
| Notes | This study had 4 arms (price discounts, tailored nutrition education, a combination of price discounts and tailored nutrition education, and no intervention). In our review, we report only data for the 2‐way comparison price discounts versus no price discounts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated blocked randomization was used, with stratification by ethnicity (...) and household income pretax" |
| Allocation concealment (selection bias) | Low risk | Quote: "Treatment assignment codes were not available to investigators or research staff at any point during the study" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Re the outcome which is relevant for our review (energy density of beverages) baseline outcome measurements were similar. Baseline differences were taken into account in the analysis. Quote: "Prespecified potential confounding factors adjusted for in the regression model were baseline measures of food and nutrients, ethnicity, household income, age, and sex" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | This was an individually randomised controlled trial, and participants from all groups frequented the same 8 supermarkets; baseline demographics were similar between the CG and the IGs. Quote: "Baseline characteristics were similar between participants assigned to the 4 intervention groups" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was similar and relatively low (approx. 10%) across all study groups, and analysis was intention‐to‐treat without imputation. Those who were lost to follow‐up were different from those who remained in the study, but given the low attrition rate and the intention‐to‐treat analysis this seems unlikely to have substantially affected the results. Quote: "Those lost to follow‐up were younger on average (mean age: 33 y) and differed by ethnicity (70% Maori and Pacific) compared with those who continued to provide shopping data." Moreover, it seems likely that displacement shopping was a not serious problem, given the results of the sensitivity analysis: "[W]e conducted sensitivity analyses of the effect of price discounts on healthier food purchases in subgroups of the intervention population that we predicted would be less prone to displacement shopping (...). In all cases, the main study findings were replicated in the predefined 'more internally valid' study subgroups, and there were no clear differences in purchases between these subgroups and those more likely to undertake displacement shopping" |
| Blinding (performance and detection bias) Objective outcomes | Unclear risk | Participants were not blinded, and purchasing data are described as objective by the study authors but could be manipulated by the participants (purchasing data were collected through supermarket loyalty cards, which may have been used selectively) |
| Contamination (performance bias) | Low risk | It seems unlikely that the CG received the price reduction intervention |
| Selective reporting (reporting bias) | Unclear risk | The Methods section implies that data on all food and beverage items purchased by the participants were collected. However, only results on healthy items, and 1 specific beverage category (milk and milk products), as well as average energy density of the beverages purchased are reported |
| Other bias | Low risk | The study authors acknowledge the possibility of chance positive findings for nutrient outcomes, since for these results were inconsistent, and no positive effects were found for the average of all products; however, since for the average energy density of beverages the effect was not significant, this is not relevant for this review |
Olsho 2016.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Random Number of clusters or sites: N/A Number of individuals: 2009 adult household heads Length of intervention: 9 ‐ 11 months |
|
| Participants |
General description of participants: Households participating in the Supplemental Nutrition Assistance Program (SNAP), living in Hampden County, Massachusetts, USA Age: All ages Inclusion criteria: Quote: "The Massachusetts Department of Transitional Assistance (DTA) screened all 55,300 SNAP households with a residential or mailing address within Hampden County for eligibility. Child only cases—households that did not include $1 member aged $16 eligible to serve as the SNAP head of household—were not eligible for the HIP; nor were SNAP participants who signed benefits over to residential or treatment facilities. The DTA provided the study team with administrative case file records for the 55,095 SNAP households in Hampden County that met eligibility criteria as of mid‐July 2011" Exclusion criteria: See quote above Recruitment: See quote above Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: " The pilot was implemented (…) in Hampden County (…). Located in western Massachusetts, the county is a mix of urban, rural, and suburban areas with 55,095 SNAP households in July 2011. Hampden County has the lowest median household income in the State. Massachusetts, like the rest of the country, is in the midst of an obesity epidemic, and residents in the western region have the highest rates of obesity and related chronic illness" |
|
| Interventions |
Intervention: Rebates on fruits and vegetables as part of a government food benefit programme (Quote: "During the 12‐month pilot in 2011–2012, HIP [Healthy Incentives Pilot] participants received a 30% rebate for purchases of targeted fruits and vegetables (TFVs) at participating retailers, using SNAP [Supplemental Nutrition Assistance Program] benefits. The rebate was credited to participants’ EBT accounts at time of purchase and could be spent on any SNAP‐eligible foods and beverages. Eligible TFVs included fresh, frozen, canned, and dried fruits and vegetables without added sugars, fats, oils, or salt (with some exceptions). White potatoes, dried beans and peas, and 100% fruit juice were excluded. TFVs are the same categories of fruits and vegetables eligible for the Special Supplemental Nutrition Program for Women, Infants, and Children voucher") Behavioural co‐intervention: Limited promotional activities (Quote: "For HIP to affect purchase decisions, participants needed to know about the program and how it worked. However, to avoid disappointing or confusing non‐HIP participants, promotional efforts were intentionally limited. The Department of Transitional Assistance developed direct mailings for HIP participants, including simple, colorful brochures. Receipts issued to HIP participants in stores with electronic cash registers included HIP rebate earning totals. Late in the evaluation, the Department of Transitional Assistance developed signage for use by HIP retailers. Even then, to avoid confusing non‐HIP participants, the signage was designed to identify HIP‐eligible foods without explicitly referencing the rebate; for example, by quoting the slogan ‘It’s HIP to be healthy!’ adjacent to the HIP logo, without mention of the rebate itself") Control: Government food benefits without rebates on fruits and vegetables (Quote: "The HIP evaluation randomly selected 7,500 SNAP households to receive the rebate on eligible SNAP purchases; the other 47,595 SNAP households in Hampden County were ineligible for the rebate, continuing to receive SNAP benefits as usual") |
|
| Outcomes |
Measures of SSB intake: SSB calories ( in kcal/day/person), and added sugar from SSB (in teaspoons/day/person), assessed with a 24‐hour dietary recall at baseline (1 ‐ 3 months prior to implementation), as well as at 4 ‐ 6 and 7 ‐ 9 months after the start of the intervention Measures of intake of alternatives to SSB: None reported Anthropometric measures: None reported Adverse outcomes: Stigma, assessed with a comprehensive process evaluation, and intake of alcoholic beverages, assessed with a 24‐hour dietary recall at baseline (1 ‐ 3 months prior to implementation), as well as at 4 ‐ 6 and 7 ‐ 9 months after the start of the intervention Other outcomes: Target group and stakeholder perceptions, assessed with focus‐group discussions, interviews, and surveys; programme costs, assessed with a comprehensive process evaluation |
|
| Context and implementation |
Setting: Social Policy Sector: Food assistance programmes Country: USA Year(s) when implemented: 2011 ‐ 2012 Mode of implementation: Government pilot project Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "None of the authors reported a conflict of interest related to the study" Funding: "Supported by the Food and Nutrition Service, USDA, contract number AG‐3198‐D‐10‐0044" Trial registration: ClinicalTrials.gov NCT02651064 Protocol availability: www.fns.usda.gov/sites/default/files/study_plan.pdf |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "With the use of blocked random assignment, the study team selected 7500 SNAP households to participate in the HIP (the HIP group). Twelve household‐level blocking cells were created by completely cross‐classifying eligible SNAP households by geography (3 levels: Springfield, Chicopee/Holyoke, and Hampden County remainder); household size (2 levels: 1‐person and $2‐ person); and sex of household head (2 levels: male‐headed and female‐headed). With the use of PROC SURVEYSELECT in SAS (version 9.3), the study team selected HIP participants who reflected target totals within each blocking cell via simple random sampling without replacement. The remaining 47,595 eligible SNAP households in Hampden County (the non‐HIP group) continued to receive SNAP benefits as usual, without earning the HIP rebate" |
| Allocation concealment (selection bias) | Low risk | See quote above |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "Study participants included in the final analytic sample (n = 2009) were similar between the HIP and non‐HIP groups, both in baseline demographic characteristics (Table 1) and baseline nutritional profile (Table 2)" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | See quote above |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The analysis was per‐protocol, but attrition was in an acceptable range (28%) and similar across groups. Quotes: "2784 adults (1388 HIP, 1396 non‐HIP) completed baseline interviews; data were analyzed for 2009 adults (72%) who also completed >= follow‐up interview. (...) Post hoc tests confirmed that attrition from the SNAP did not significantly differ between the HIP and non‐HIP groups. (...) There were some statistically significant differences between sampled persons who were or were not included in the final analytic sample (implementation wave, geography, sex of household head; sex, age, race/ethnicity, disability status, and marital status of sample respondent; Supplemental Table 1), and between those who did or did not complete >=1 follow‐up interview (perceived barriers to grocery shopping; Supplemental Table 2). These losses to follow‐up did not introduce imbalance across the HIP and non‐HIP groups. All analyses incorporated sampling weights that accounted for survey nonresponse and attrition from the SNAP" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and outcomes are self‐reported |
| Contamination (performance bias) | High risk | Participants were randomised individually to receiving the discounts or not, which limited the possibilities for providing information on the programme at the point‐or‐purchase. In providing such information, those implementing the intervention attempted to strike a balance between sufficiently informing the HIP recipients about the intervention, and not confusing non‐HIP recipients, who were also SNAP recipients. Contamination could have been in both directions: 1. through the public information materials the control group found out about the intervention and changed shopping habits; 2. the intervention group did not understand the intervention well enough, thus did not 'fully receive' it. There is indeed some indication that a substantial portion of IG participants did not receive, or did not understand the information necessary to participate in and respond to the intervention. As the study authors explain, this may have influenced the observed effects. Quote: "More than a third of HIP participants in the early implementation survey and almost a quarter in the late implementation survey said they had not heard of HIP. Nearly a third reported that HIP was hard to understand or that they did not know how HIP worked, and focus group participants exhibited substantial confusion about rebate mechanics. These factors probably diluted HIP impacts (...)." This would have biased results downwards |
| Selective reporting (reporting bias) | Low risk | All important outcomes mentioned in the trial register entry, the study protocol, and the Methods section are reported |
| Other bias | Low risk | No other concerns |
Peters 2016a.
| Methods |
Design: ITS Timing: Retrospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 145 restaurants Number of individuals: N/A (the analysis is based on routinely‐collected sales data not linked to individual participants) Length of intervention: 6 years |
|
| Participants |
General description of participants: Visitors to Walt Disney World quick‐service and table‐service restaurants located in the Walt Disney theme park in Orlando, USA Age: Children (age range 3 to 9 years) Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R (However, the study notes that prior to the start of the intervention, SSBs were the only beverage available as part of the kids' menus targeted by the intervention) Equity considerations: N/R |
|
| Interventions |
Intervention: Change of the default beverage served with children's menus at chain restaurants. (Quote: "Beginning in October 2006, the Walt Disney Company changed the default side item and beverage offered with all complete kids’ lunch and dinner meals (including those offering healthy and classic entrées) served in its domestic US theme parks and resorts. Prior to this date, kids’ meals were served with french fries and a regular soft drink as the default side and beverage. Default choices were changed to servings of fruit (…) or vegetables (…) while beverage choices changed to low‐fat milk, water, or 100% juice (apple, orange, or fruit punch). Customers could substitute french fries or a soft drink upon request. In other words, they could opt out of the healthy side and beverage defaults. Pricing for kids’ meals with healthy defaults was the same as for meals with french fries and soft drink. Point‐of‐sale picture boards displaying the meals showed only the meal with the healthy default items, though all potential substitutes were listed on the menu board. (...) Menu changes were introduced without any substantial public relations campaign, avoiding a potentially negative consumer response if consumers perceived that healthy items may not taste as good or be as fun or if consumers perceived that the use of healthy defaults threatened their freedom, resulting in consumers intentionally opting out of the healthy defaults in order to counteract this perceived threat. This allowed consumers to become accustomed to the new offerings before the changes were deliberately brought to the public’s attention. (...) Prior to implementation of the healthy defaults, french fries and a soft drink were the only available options. (...) [T]herefore, the separate effects of offering healthy items as defaults from the effects of adding healthy items to the menu as opt‐in choices cannot be determined") Behavioural co‐intervention: None (Quote: "Menu changes were introduced without any substantial public relations campaign, avoiding a potentially negative consumer response if consumers perceived that healthy items may not taste as good or be as fun or if consumers perceived that the use of healthy defaults threatened their freedom, resulting in consumers intentionally opting out of the healthy defaults in order to counteract this perceived threat. This allowed consumers to become accustomed to the new offerings before the changes were deliberately brought to the public’s attention") Control: N/A (ITS without control group) |
|
| Outcomes |
Measures of SSB intake: Share of customers accepting healthy beverage defaults as part of the kids' menus, assessed at baseline and at years 4, 5 and 6 post‐intervention with routinely‐collected sales data Measures of intake of alternatives to SSB: See above Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Restaurants Sector: Food service (private for profit) Country: USA Year(s) when implemented: 2006 ‐ 2012 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "This work was supported by the Walt Disney Company and by the National Institutes of Health (grant no. DK48520). The Walt Disney Company and the National Institutes of Health had no role in the design, analysis, or writing of this article. Full disclosure: JH is a consultant for the Walt Disney Company and for McDonalds; KA is a consultant for the Walt Disney Company" Funding: See COI Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data for the first 3 years post‐intervention are missing, and data for the remaining years are described as "relatively complete" by the study authors. Study authors note that for the table‐service restaurants (TSR) in the sample, beverage purchase data was incomplete due to the way sales data were collected. Quotes: "Data were analyzed for three fiscal years for which Disney had relatively complete point‐of‐sale data at WDW. (…) At TSRs, Disney had incomplete data on beverage purchases because they are not always entered as individual sales (as are entrées) in this restaurant format. For example, TSRs offer water with all meals in addition to any other beverage, and these servings of water are not recorded with the beverage numbers. Because of this, the percentage of consumers who opted in to the healthy beverage option at TSR locations does not include consumers who consumed water as their beverage" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study. The study reports that "[m]enu changes were introduced without any substantial public relations campaign, avoiding a potentially negative consumer response if consumers perceived that healthy items may not taste as good or be as fun or if consumers perceived that the use of healthy defaults threatened their freedom, resulting in consumers intentionally opting out of the healthy defaults in order to counteract this perceived threat. This allowed consumers to become accustomed to the new offerings before the changes were deliberately brought to the public’s attention" |
| Selective reporting (reporting bias) | Unclear risk | It is not reported if the study was registered, if a protocol is available, or if analyses were prespecified. Data were provided by Walt Disney with the understanding that only certain outcomes are reported. This may have introduced bias. Quotes: "Disney did not have complete data for Disneyland, located in Anaheim, California; therefore, Disneyland is not part of this analysis. (…) Although raw sales data were provided for this analysis, access to these data was provided with the understanding that only the percentages of different kids’ meal items sold, as a function of the total meal items sold, would be published. Likewise, WDW [World Disney World] did not provide data for the number of children who visited the park for fiscal years 2010–12 or the absolute number of kids’ meal items sold during that period. Reporting percentages is not uncommon in the literature because of the proprietary nature of absolute numerical data for commercial businesses. In such cases where a company will not provide absolute numerical sales, the general convention has been to report differences in terms of percentages instead of as absolute numbers. Such an approach is common in health economics and psychology" |
| Independence of the intervention from other changes (performance bias) | Unclear risk | At baseline, no healthy beverages were offered. This implies that without the intervention (the introduction of healthy beverage defaults) the outcome (healthy beverage default acceptance rates) would have been zero. Quote: "Prior to implementation of the healthy defaults, french fries and a soft drink were the only available options. Therefore, these estimates compare the nutritional values based on 100% of individuals selecting french fries and soft drink defaults versus the percent of individuals in this sample who actually selected the healthy defaults once they were implemented." It is, however, possible that other developments occurring during the study period, such as increasing public awareness of health risks associated with SSB consumption, and secular trends towards healthier beverage choices, influenced the magnitude of the observed effects |
| Pre‐specification of the intervention effect (detection bias) | High risk | The intervention was implemented in October 2006, but no data are available for the first 3 years post‐intervention. That is, the point of intervention is not the point of analysis, and no prespecification of the shape of the intervention effect is reported |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns |
Schram 2015.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: Quote: "A natural experiment occurred on 11 January 2007 when Vietnam joined the WTO. (...) To identify the impact of the trade agreement on SSCB [sugar‐sweetened carbonated beverages] sales we compare the intervention group, Vietnam, with a control group that was not similarly exposed but was similar in other respects. Here, a neighboring country, the Philippines, serves as the control. It had early engagement in trade relations with the United States, joined the WTO in 1995, and did not experience a marked change in FDI from 1999 to 2013, but it has a similar demographic profile and GDP per capita as Vietnam ($4700 and $4000, respectively)" Number of clusters or sites: 2 countries Number of individuals: Vietnam (the intervention country) had, in 2017, a population of 94 million. The Philippines, the control country, had a population of 106 million Length of intervention: 4 years (post‐implementation) |
|
| Participants |
General description of participants: Inhabitants of Vietnam Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: Baseline retail sales of SSB were 1.9 l/per capita/year in Vietnam (the IG), and 28.7 l/per capita/year in the Philippines (the CG). Equity considerations: N/R |
|
| Interventions |
Intervention: A bilateral trade and investment agreement with the USA and accession to the WTO. (Quote: "A natural experiment occurred on 11 January 2007 when Vietnam joined the WTO. As part of the agreement, Vietnam began a process of liberalizing its markets to allow greater entry by foreign owned companies through foreign direct investment (FDI); although market access commitments specific to SSCBs [sugar‐sweetened carbonated beverages] were only fully implemented as of 2009. The impacts of Vietnam’s WTO accession may have been enhanced by a bilateral agreement it entered into with the US in 2001 which largely paralleled its WTO commitments, permitting US companies access to services relevant to the beverage sector just weeks before remaining WTO members" (Further details are provided in table 1 of the study's primary report) Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Retail sales of sugar‐sweetened carbonated beverages (SSCB), in litres per capita per year, and growth rate of retail sales of SSCB manufactured by foreign companies, in per cent per year, assessed continuously throughout the study period with data from the commercial Euromonitor Database Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes an increase in the per capita retail sales of sugar‐sweetened carbonated beverages Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Low‐ and middle‐income countries Sector: Trade and investment policy Country: Vietnam Year(s) when implemented: 2007 ‐ 2013 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "The authors declare that they have no competing interests" Funding: "AS was supported by a Canadian Institutes for Health Research Michael Smith Foreign Study Supplement award. DS and AR are supported by a Wellcome Trust Investigator Award. This project was partially supported by funding from an Australian Research Council Discovery Project, “Trade policy: Maximising benefits for nutrition, food security, human health, and the economy” (DP130101478)" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Differences in outcome measurements at baseline were taken into account in the analysis, but were large (approx. 5 times as big as the intervention effect shown by the statistical models employed). Quote: "Average per capita sales of SSCBs in Vietnam rose from 1.9 L (95 % CI: 1.6 to 2.2) to 3.9 L (95 % CI: 3.4 to 4.3) post‐intervention. Over the same period per capita sales in the Philippines dropped from 28.7 L (95 % CI: 28.4 to 29.0) to 26.1 L (95 % CI: 25.6 to 26.6)" |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | While the study authors argue that Vietnam and the Philippines are similar demographically and have a similar GDP per capita, they also point out that their trade and investment policies have been very different for a long time (i.e. at baseline). There are also important political, economic and sociocultural differences between the 2 countries, for which the study design cannot control |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study uses commercially‐available Euromonitor sales figures, which were considered by the review authors to be a comparatively reliable source of data. There is no indication that problems of incomplete outcome data affected the IG and CG differently |
| Blinding (performance and detection bias) Objective outcomes | Low risk | The outcome data (Euromonitor sales data) can be considered objective |
| Contamination (performance bias) | Low risk | While trade and investment rules did evolve in the Philippines too, it did not accede to the WTO at the time of the study. Contamination would have reduced any observed effect, which strengthens our confidence that the effects which were observed are not due to contamination bias |
| Selective reporting (reporting bias) | Low risk | The study has not been registered and there is no protocol available. However, all outcomes mentioned in the Methods section are reported, and the study authors report that they altered their analysis plan after an initial examination of the data, and explain their rationale for doing so, which strengthens our confidence that outcomes were not reported selectively |
| Independence of the intervention from other changes (performance bias) | High risk | The study authors note that a number of factors not attributable to the intervention may have affected outcomes. Quotes: "[T]here may have been one or more significant events that took place in Vietnam that may equally or better explain our findings that were outside of the knowledge and control of the researchers. (...) Other factors that may contribute to a country’s investment climate include political and economic stability, infrastructure, wages, corporate tax structures, tax incentives for FDI (...) and proximity to main markets (...). To our knowledge there were no considerable changes in these factors in Vietnam during our intervention period. Attributing specific patterns in FDI to trade and investment agreements is challenging with even the most sophisticated econometric techniques; this is due in part to the long‐term implementation periods of these agreements which make it challenging to capture all FDI activity attributable to the agreement and the difficulty in obtaining disaggregated FDI data due to confidentiality provisions" |
| Pre‐specification of the intervention effect (detection bias) | High risk | The study authors discuss the difficulties of establishing a clear time point when the intervention occurred, and report results both for the time point when the free trade agreement was ratified, and for the time point when it was enforced. In the statistical model the point of analysis was time‐lagged by 1 year. It is not reported if this was prespecified. Quotes: "Deciding where to introduce the time of intervention is also complicated. Our intervention period of 2009, although capturing almost all liberalization we identified as relevant to SSCBs, did not account for the full implementation of commitments incidental to manufacturing, which did not take effect until 1 January 2010. (...) The DID models utilized the average of annual per capita sales estimates over the pre‐ and post‐intervention years. In order to detect changes in sales we time‐lagged the intervention point one year after liberalization of the SSCB market access commitments to allow time for the effects of the new investment commitments to take place. Thus the intervention year is considered to be 2009 with the effects of the intervention beginning to take effect in 2010, making our pre‐intervention period inclusive of the years 1999–2009, and the post‐intervention period inclusive of the years 2010–2013 (with the exception of sales data by foreign and domestic companies, which were only available post 2004)" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns |
Schwartz 2009.
| Methods |
Design: CBA Timing: Prospective Allocation to group: Quote: "[I]ntervention schools applied to the [Connecticut State Department of Education] to participate in the snack study. The comparison schools were chosen to match the intervention schools as closely as possible. In two cases, the comparison school was another middle school in the same town, with the same food service director. In the third case, there was only one middle school in the town, so a middle school from a town within the same economic reference group was invited to participate" Number of clusters or sites: 6 schools Number of individuals: 495 Length of intervention: 1 year |
|
| Participants |
General description of participants: Students at middle schools in Connecticut, USA Age: Children and teenagers (no age range reported) Inclusion criteria: N/R Exclusion criteria: N/R Recruitment: Quote: "During the spring of the school year preceding the intervention, baseline Year 1 data were collected in each of the six middle schools through surveys administered by health or family consumer science teachers to all the students they had in class at the time of data collection (N = 501). During the spring of the intervention year, the same teachers were contacted and the same measures were administered to their current classes (N = 495)" Weight status at baseline: N/R SSB consumption at baseline: Information on baseline SSB intake is reported graphically only (see figure 1 of the study's primary report). The mean frequency of SSB consumption at baseline was 2 on a scale from 1 ("I never eat this food at home/school") to 4 ("I eat this food at home/school everyday) Equity considerations: A broad range of ethnic, demographic and socio‐economic groups was represented among the participants (approximately 55% were white, 25% Hispanic, 15% black and 4% Asian American; 35% were eligible for free or reduced school meals; 13% were on special education and 2% on gifted and talented programmes) |
|
| Interventions |
Intervention: Reduced availability of SSB at school. (Quote: "The intervention consisted of having the schools follow a set of snack guidelines for all foods sold at school during the school day (i.e., cafeteria a la carte, vending, and fundraisers). (...) Each school had the ability to choose its own array of snacks and beverages within the guidelines. The only beverages that met the standards were water, milk, and 100% juice. Intervention schools removed beverages such as sugar‐sweetened teas, sports drinks, and fruit drinks") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Frequency rating of SSB consumption at school and at home, based on a rating from 1 (never), 2 (rarely), 3 (sometimes) and 4 (always), assessed at baseline and 1 year with a "questionnaire entitled Snack Foods Eaten at School and Home [which] was developed for the present study to assess intake of the foods and beverages targeted by the intervention" Measures of intake of alternatives to SSB: Frequency rating of water and 100% fruit juice consumption at school and at home, based on a rating from 1 (never), 2 (rarely), 3 (sometimes) and 4 (always), assessed at baseline and 1 year with a questionnaire (see quote above) Anthropometric measures: N/R Adverse outcomes: Percentage of students reporting their weight as the right amount, too much or too little, reporting a desire to weigh more, less or have weight stay about the same, and percentage of students reporting to be currently dieting, assessed with the School‐Based Nutrition Monitoring Questionnaire (SBNMQ) at baseline and at 1 year Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2004 ‐ 2005 Mode of implementation: Government pilot project Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This research was supported by the Rudd Center for Food Policy and Obesity at Yale University. Connecticut’s Healthy Snack Project was funded through a 2003‐2005 Team Nutrition Training Grant from the U.S. Department of Agriculture to the Connecticut State Department of Education" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Data on baseline outcome measurements are reported graphically only (figure 1 and 2 of the study's primary report), and are similar across study groups. Quotes: "EBNS [excluded by nutrition standards] Beverages: No differences were found based on condition or year. (...) MNS [meeting nutrition standards] Beverages: Reports of consumption of water and 100% juice did not differ based on condition or year. (...) No difference in water or juice consumption at home based on condition was found" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Schools were matched for a number of relevant variables, and analyses adjusted for remaining differences. Quotes: "The comparison schools were chosen to match the intervention schools as closely as possible. In two cases, the comparison school was another middle school in the same town, with the same food service director. In the third case, there was only one middle school in the town, so a middle school from a town within the same economic reference group was invited to participate. (...) To ensure that our comparison schools were equivalent to the intervention schools on key variables, we conducted analyses to compare the two groups of schools using data from published Connecticut Strategic School Profiles. We included the following variables: percentage of (a) students eligible for free/reduced price meals, (b) students with non‐English home language, (c) students above entry grade who attended this school the previous year, (d) students in a gifted and talented program, and (e) students in special education. A multivariate analysis of variance followed by pairwise comparisons of each variable individually indicated no difference between the groups (F (1, 4) = 1.1, p = .61). (...) Despite the lack of statistical differences between the intervention and comparison schools, there was a large range among the schools of the percentage of students who qualified for free and reduced meals (from a minimum of 7% to a maximum of 62%). To address this, all analyses statistically controlled for the percentage of students eligible for free/reduced lunch within each school" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None of the 6 schools in the study dropped out, and survey participants were redrawn from the student population at baseline and follow‐up. No response rate for the repeat cross‐sectional data collection is reported, but there is no indication that sampling variation introduced substantial bias |
| Blinding (performance and detection bias) Subjective outcomes | Unclear risk | It is unclear to what extent participants (i.e. school children and teachers administering the survey questionnaires) were blinded to the intervention ‐ they certainly noted that the choice of foods and beverages available at school changed, but it is unclear to what degree they realised that this was part of a planned intervention and study |
| Contamination (performance bias) | Unclear risk | Contamination cannot be ruled out as 2 of the intervention and control schools were located in the same town and had the same food director, which would have biased results towards null. |
| Selective reporting (reporting bias) | Unclear risk | For beverage consumption outcomes only beta coefficients from the regression analyses are reported numerically, pre‐ and post‐intervention means are presented only graphically. For weight perception outcomes, only the non‐significance of changes is reported, without any more specific data. For beverage consumption outcomes only aggregate data for beverage groups are reported, which is explained by the study authors as follows: Quote: "A fourth limitation of the present study concerns multiplicity of testing. Because there were many beverage and snack options available and all children were not expected to make changes in their purchasing behavior for all categories, we needed to examine each group of items separately. We did cluster the individual items into subgroups to minimize the problem of multiple tests, but the risk of Type I error remains" |
| Other bias | Unclear risk | Data were self‐reported, and as the study authors discuss in detail in the limitations section, students might have misinterpreted certain survey questions. In particular, this might have obscured relevant effects on compensatory behaviour (i.e. beverage consumption outside school), for which the study found no relevant effect. The same applies to weight perception outcomes: Quote: "A third limitation is the lack of a comprehensive and detailed assessment of body dissatisfaction and unhealthy dieting and eating behaviors. It is possible that there were changes due to the intervention that our measure was not sensitive enough to detect. Future research examining the hypothesis that school‐based interventions may increase weight preoccupation and dieting behaviors in a negative way should use measures that can detect subtle changes and distinguish between appropriate attempts to eat healthfully and inappropriate extreme dieting behaviors (such as fasting or purging)" |
Schwartz 2016.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: The study used a stepped‐wedge design in which schools received water jets (i.e. the intervention) at different time points during a 5‐year period, and crossed over from the CG to the IG at the moment when they received the water jet. The timing of water jet installation in each school depended on factors outside the control of the investigators. Quote: "Water jets were not randomly assigned, but spread across a large number of schools as part of a district initiative. (...) Interviews with district‐ and school‐level personnel suggest the specific timing of water jet adoption by a school reflects the interaction of opportunity, convenience, and happenstance, rather than systematic targeting" Number of clusters or sites: 1227 schools Number of individuals: 1,065,562 Length of intervention: 5 years |
|
| Participants |
General description of participants: Students at public elementary and middle schools in New York City, US Age: Children and teenagers (the exact age range is not reported) Inclusion criteria: Students attending public elementary and middle schools in New York City participating in the New York FITNESSGRAM survey, an routinely administered annual school health examination. Quote: "New York schools have conducted the New York FITNESSGRAM annually for all students in kindergarten through 12th grade since the 2005‐2006 academic year as part of the standards‐based physical education program" Exclusion criteria: Quote: "We excluded charter and special education schools from our sample. We also excluded schools (in a given year) where less than 50% of students participated in the New York FITNESSGRAM (only 1.6% of kindergarten through eighth‐grade student observations) and students with missing New York FITNESSGRAM data (4.1 % of students in schools not dropped owing to low New York FITNESSGRAM coverage)" Recruitment: See inclusion criteria Weight status at baseline: At baseline, 39% of students in the IG and CG were overweight or obese, and 21% of students in the IG and CG were obese SSB consumption at baseline: N/R Equity considerations: Both sexes were equally represented among the participants in the IG, as were a variety of ethnicities (37% black, 37% Hispanic, 14% white, 12% Asian). 11.3% were foreign‐born, 12% had limited English proficiency, 12.1% were on special education, and 85% received free or reduced‐price school lunches (i.e. were from lower‐income families) |
|
| Interventions |
Intervention: Improved access to drinking water at school (Quote: "In 2009, New York’s Department of Health and Mental Hygiene and Department of Education launched an intervention to increase access to drinking water at lunchtime by placing ‘water jets’ in school cafeterias. Water jets are electrically cooled, large, clear jugs with a push lever for fast dispensing that give students access to clean New York tap water. Water jet machines both chill the water and oxygenate it to keep it tasting fresh and cost approximately $1000 per machine. Plastic disposable cups are also provided by schools for use with the water jet machines") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Number of half‐pints of fat‐free chocolate milk purchased per student per year, assessed continuously during the study period with data from an administrative data base maintained by the New York City Department of Education Office of School Food Measures of intake of alternatives to SSB: Number of half‐pints of low‐fat and skim white milk purchased per student per year, assessed continuously during the study period with data from an administrative data base maintained by the New York City Department of Education Office of School Food Anthropometric measures: Mean z BMI, percentage of overweight, and percentage of obese, assessed annually with data from the New York FITNESSGRAM data base. Data were collected by physical education teachers trained in measurements protocols Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes that a reduction in total milk intake was observed (see above) Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2008 ‐ 2013 Mode of implementation: Government regulation and public investment Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "Conflict of Interest Disclosures: None reported" Funding: "This project was supported by award 1R01HD070739 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. (...) The sponsor played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Quote: "In the 2007‐2008 academic year, water jet schools had similar percentages of overweight students (38.9% vs 39.2%) and obese students (21.1% vs 21.4%) than non–water jet schools" (baseline differences for milk consumption are not reported) |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Quote: "Overall, schools with water jets (n = 374) were not systematically different than those without (n = 482) on baseline characteristics. (...) However, water jet schools did have different percentages of Asian, special education, and foreign born students than non–water jets schools (P < .05). Differences were small in magnitude" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Body weight outcome observations were excluded for schools which had a FITNESSGRAM coverage of less than 50% in the respective year, i.e. which assessed the body weight of fewer than 50% of their students. The study does not report if average FITNESSGRAM coverage differed between IG and CG |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Outcomes were objective |
| Contamination (performance bias) | Low risk | Allocation was by institution (school), and it seems unlikely that a substantial number of schools in the CG installed water jets independently from the programme run by the New York Department of Education (i.e. before the scheduled date, and before they crossed over to the IG) |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported, and the choice of outcomes is well‐justified, making it unlikely that outcomes with positive results were selected, and those with negative results dropped from the analysis in a post hoc manner |
| Other bias | Unclear risk | This study used a complex quasi‐experimental stepped‐wedge cross‐over design. Results may have been biased by underlying temporal trends |
Schwartz 2017.
| Methods |
Design: controlled ITS Timing: Prospective Allocation to group: "The method IRI [the market research firm hired by the investigators] used to test advertising campaigns is the Matched Market Test. The Matched Market Test measures sales for the target (ie, advertised) brand and the other brands in the category for 52 weeks before the campaign begins. Sales are assessed in stores located where the advertising campaign is planned (the test market) and a set of control stores in another location that have been identified as the best match during the previous 52 weeks for sales of the target brand and category (the control market). To identify the control market, IRI considers qualitative and quantitative factors and avoids markets where other tests have recently occurred that may affect sales. The details of the statistics used in the matching protocol are proprietary, but the concepts are described in the marketing literature. To identify the best‐matched control stores, IRI examined beverage sales for each category of interest during the 52 weeks from May 29, 2011, to May 20, 2012, in HC [Howard County, the intervention area] supermarkets. These data were compared with a sample of 326 supermarkets that included the same HC chains and were in the same region of the country. From that pool, IRI identified a set of 17 stores in southeastern Pennsylvania that provided the best match. The HC stores were from 6 large supermarket chains, and all of the final sample in the contiguous state were drawn from 4 of those chains" Number of clusters or sites: 32 supermarkets Number of individuals: N/A (the study is based on commercial sales data not linked to individual participants) Length of intervention: 3 years |
|
| Participants |
General description of participants: Residents of Howard County, Maryland, USA Age: All ages Inclusion criteria: N/A Exclusion criteria: N/A Recruitment: N/A Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: Quote: "In 2012, HC [Howard County, the intervention area] had a population of 299 430 and a median income of $108 844, and 95.1% of residents had at least a high school diploma. In contrast, in 2012 the comparison counties were somewhat bigger (population 350 637 people), had a substantially lower median income ($53 713), and had a lower rate of residents with at least a high school diploma (86.2%). The racial/ethnic profile of the 2 sets of communities also differed. The HC schools were substantially more racially and ethnically diverse, with a mean of 37.5% white, 28.2% black, 16.0% Asian, and 11.7% Hispanic students. The schools around the comparison stores had a mean of 74.0% white, 7.1% black, 4.4% Asian, and 13.0% Hispanic students. In sum, HC residents were wealthier, more educated, and more racially and ethnically diverse than the residents near the comparison stores" |
|
| Interventions |
Intervention: A multi‐component community campaign. (Quote: "In 2012, the Horizon Foundation and several community partners planned a multicomponent campaign to reduce sugary drink consumption in HC [Howard County]. The official launch occurred in December 2012, and campaign activities have taken place since 2013. The initiative was designed to address all levels of the social ecological model. Table 1 details the many components of the campaign, which promoted change at the interpersonal, organizational, community, and policy levels. Through extensive community outreach, a range of partners were engaged, including faith‐based groups, businesses, the county school system, child care providers, local government agencies, pediatricians, and the health care system. The present analysis of sales data did not involve human subjects and was deemed exempt from institutional review board approval by the University of Connecticut. Howard County Unsweetened targeted beverages that contained any type of added sugar and encouraged people to move away from sugary drinks and toward those lower in sugar and calories (defined as better beverages). The sugary drinks most frequently identified in campaign materials through pictures and words were regular soda, sports drinks, and fruit drinks. Sweetened flavored waters,sweetened teas, and sweet hot beverages (eg, flavored coffee drinks) were also included in some communications. The beverage most often promoted was water, including bottled, plain tap, and tap water flavored with pieces of whole fruit, vegetables, and herbs. Diet soda was not addressed explicitly by the campaign, although it was designated as a better choice in the Better Beverage Finder. One hundred percent juice was also designated as a better beverage; however, materials included the caveat that portion size matters and provided age‐appropriate limits. During the 3‐year period, the media campaign alone reached more than 576000 nonunique county residents and created 17 million impressions through cable and broadcast television advertising, television advertising, digital marketing advertising, direct mail, outdoor and facility advertising, and social media. The campaign also benefited from significant additional earned media in response to the public discourse surrounding the proposed policy changes. In this context, earned media is the free publicity gained through publication of online and print news stories. Successful policy changes during the study period included a state‐wide policy removing sugary drinks from childcare facilities, a local school wellness policy that required healthier food and drinks to be served during the school day and in vending machines, and a healthy vending policy for all county government property. Residents of HC were also exposed to media coverage of Maryland state wide campaigns to remove the sales tax from bottled water and a bill to require a healthy default beverage in children’s meals in restaurants" Behavioural co‐intervention: The intervention included a number of behavioural intervention components (see quote above) Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Regular soda, fruit and sports drinks sales per product per store per week, assessed continuously throughout the study period with commercial sales data Measures of intake of alternatives to SSB: Diet beverage and 100% fruit juice sales per product per store per week, assessed continuously throughout the study period with commercial sales data Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Various Sector: Various Country: USA Year(s) when implemented: 2013 ‐ 2015 Mode of implementation: Pilot trial by researchers in co‐operation with private non‐profit organisations Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "Conflict of Interest Disclosures: Mr Schneider reports serving as Chief Program Officer of the Horizon Foundation. Ms Highsmith Vernick reports serving as the president and chief executive officer of the Horizon Foundation. Dr Appel reports serving on the board of directors of the Horizon Foundation. No other disclosures were reported" (The Horizon Foundation is the non‐profit organization which implemented the intervention) Funding: "Funding/Support: This study was supported by grants from the Horizon Foundation, the Robert Wood Johnson Foundation, and the Rudd Foundation" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a controlled ITS, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Outcome measurements were similar in the IG and CG at baseline. Quote: "Figure 1 illustrates the match between HC (test market) and comparison (control market) stores at baseline for regular soft drink volume sales per $1 million all‐commodity volume. The similar level and pattern of sales during the 52 weeks indicate that the HC and comparison stores are a good match" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | There were some baseline differences between IG and CG. Quote: "In 2012, HC had a population of 299 430 and a median income of $108 844, and 95.1% of residents had at least a high school diploma. In contrast, in 2012 the comparison counties were somewhat bigger (population 350 637 people), had a substantially lower median income ($53 713), and had a lower rate of residents with at least a high school diploma (86.2%). The racial/ethnic profile of the 2 sets of communities also differed. The HC schools were substantially more racially and ethnically diverse, with a mean of 37.5% white, 28.2% black, 16.0% Asian, and 11.7% Hispanic students. The schools around the comparison stores had a mean of 74.0% white, 7.1% black, 4.4% Asian, and 13.0% Hispanic students. In sum, HC residents were wealthier, more educated, and more racially and ethnically diverse than the residents near the comparison stores" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The analysis is based on commercial scanner data, which can be assumed to be complete (but see the issues discussed in the domain 'Other risks of bias') |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcome measures are objective |
| Contamination (performance bias) | Low risk | It seems unlikely that the CG received the intervention in comparable form |
| Selective reporting (reporting bias) | Low risk | The study design was prospective, and all outcomes mentioned in the Methods section are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | The intervention may not have been independent of other changes; however, the clear difference in the control group, and the marked trend shift after the start of the intervention suggest that the observed effects are not entirely due to concurrent events or trends |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of intervention was the point of analysis |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Unclear risk | The outcome measures may be an imperfect measure for the actual SSB intake of the target population. Quote: "We requested data for all 17 full‐service chain supermarkets in the county, but 2 retailers would not release data, leaving a sample of 15 HC stores. We purchased scanner data for the top‐selling brands from the 3 largest beverage companies (Coca‐Cola Co, PepsiCo, and Dr Pepper Snapple Group) in the regular soda (13 brands), sports drink (2 brands), and diet soda (7 brands) categories. We also purchased data for the brands with the highest sales in the 100% juice (4 brands) and fruit drink (6 brands) categories. (...) [T]hese data do not tell us what people are drinking instead of the brands included in the study. The beverage industry is transforming quickly, and new products are introduced each year. We focused on the best‐selling major brands within each category to ensure we could measure the same products each year. However, HC consumers may have shifted to beverages from small companies that are marketed as healthy alternatives, such as organic sodas or low‐sugar iced teas. Future work should follow the sales of these smaller brands in the HC and comparison stores to determine whether consumers are shifting to other products and, in turn, how sugar intake from beverages has changed" |
Siegel 2016a.
| Methods |
Design: ITS Timing: Prospective Allocation to group: N/A (ITS without control group) Number of clusters or sites: 2 schools Number of individuals: Quote: "The number of students purchasing lunch ranged from 186 to 278 per day" Length of intervention: 4 months |
|
| Participants |
General description of participants: Elementary school children in Cincinnati, USA Age: Children (no age details reported; participants attended grades k to 6) Inclusion criteria: N/R (All children having lunch at the 2 school cafeterias where the intervention was implemented were exposed to the intervention) Exclusion criteria: N/R Recruitment: N/R Weight status at baseline: N/R SSB consumption at baseline: N/R (However, at baseline, on average 87% of children chose chocolate milk in the school cafeteria, and 7.4% selected white milk) Equity considerations: "FD [Frederick Douglass Elementary School, where the intervention was implemented] is an inner city school with grades k through 6 and,at the time of the intervention, had an enrollment of 297 children of whom 50.5% were female, 92.7% African American and 98.1% free lunch eligible" |
|
| Interventions |
Intervention: Labelling of white milk with a green smiley face emoticon. (Quote: "Signs with ‘Green Smiley Face’ emoticons were placed next to PWFFM [plain white fat free milk], fruits, vegetables (including a salad bar), and the main entrée to encourage the purchase of healthful foods. A cafeteria staff worker explained the intervention to students on the first day of the intervention and intermittently throughout the study period") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Percentage of children selecting chocolate milk (among all children having lunch at the cafeteria), assessed continuously throughout the study period with cafeteria sales data Measures of intake of alternatives to SSB: Percentage of children selecting plain white fat‐free milk (among all children having lunch at the cafeteria), assessed continuously throughout the study period with cafeteria sales data Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes that total milk sales (see above), which might have been adversely affected by the intervention, did not decrease Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary schools Sector: Education Country: USA Year(s) when implemented: 2013 ‐ 2014 Mode of implementation: Pilot trial by researchers in co‐operation with a public school Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The authors have no conflicts of interest to disclose" Funding: "The study was not supported by a grant" Trial registration: N/R Protocol availability: N/R |
|
| Notes | Besides the labelling intervention, this study examined a second intervention (small prizes for the selection of healthier foods and beverages), which was implemented in a second study phase, following the first study phase during which only the labelling intervention was implemented. Data from this second study phase are not included in this review, as the follow‐up period did not meet our inclusion criteria. The published reports of this study did not report data in a form that allowed inclusion in our review. We contacted the study's corresponding author, and received the necessary data. Details on the statistical model used for our analysis is provided in Appendix 11 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data are unlikely to bias results ‐ the routinely‐collected sales data can be assumed to be close to complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Low risk | There is no indication that outcomes were reported selectively. Outcome data on all food and beverage items targeted by the intervention, and mentioned in the methods section, are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | It seems unlikely that other changes occurred exactly at the same time as the intervention which could have produced such a marked and clearly timed change in consumption patterns |
| Pre‐specification of the intervention effect (detection bias) | Low risk | The point of analysis is the point of intervention |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | No other concerns |
Siegel 2016b.
| Methods |
Design: ITS Timing: Prospective Allocation to group: N/A (ITS without a control group) Number of clusters or sites: 8 schools Number of individuals: 3001 students attended the participating schools; the number of students frequenting the school cafeteria, i.e. participating in the intervention, is not reported Length of intervention: 4 ‐ 8 months for 7 out of 8 participating schools, and 2 ‐ 3 months for the remaining school |
|
| Participants |
General description of participants: Elementary school children in Cincinnati, US Age: Children (elementary school students, grade k to 6; no age details reported) Inclusion criteria: N/R (all children attending the participating schools who had lunch in the cafeteria were exposed to the intervention) Exclusion criteria: N/R Recruitment: Quote: "The schools selected were at the recommendation of the CPS [Cincinnati Public Schools District] Community Learning Center Coordinator" Weight status at baseline: N/R SSB consumption at baseline: At baseline, 0.73 servings of chocolate milk were selected per child per day Equity considerations: The study was set in a low‐income, majority‐minority inner city district of Cincinnati, Ohio, USA. Quote: "Greater than 95% of students in all of these schools [participating in the study] were below 130% of the U.S. poverty level and were eligible for free lunch because of the CPS [Cincinnati Public Schools District] district’s overall demographics" |
|
| Interventions |
Intervention: Small prizes for the selection of plain, fat‐free milk instead of chocolate milk. (Quote: "Green ‘smiley‐faced’ emoticons were placed by preferred food items (fruits, vegetables, plain fat free milk and entrée with whole grain) and signs were posted explaining the PP [Power Plate, i.e. a meal consisting of plain fat free milk, an entrée with whole grain, fresh fruit and fresh vegetables or a salad] on the first day of the intervention (…). Small prizes were given students selecting the PP on Tuesdays and Thursdays once the intervention began. On the first day of the intervention, a small prize, such as a bracelet, was distributed to students who selected the PP. On all other PP prize days, either temporary tattoos or stickers were given to students who selected the PP by school volunteers") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Chocolate milk servings sold per student per day, assessed continuously throughout the study period with cash register data Measures of intake of alternatives to SSB: Plain fat‐free milk servings sold per student per day, assessed continuously throughout the study period with cash register data Anthropometric measures: N/R Adverse outcomes: Food waste (estimated percentage of plain milk selected but not consumed by children in the school cafeteria), assessed at baseline and for 1 day during the intervention phase (no exact date provided) by trained observers following a standardised protocol Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary schools Sector: Education Country: USA Year(s) when implemented: 2015 ‐ 2016 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article" Funding: "The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The project described was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number 1UL1TR001425‐01" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data are unlikely to bias results ‐ the routinely‐collected sales data can be assumed to be close to complete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Selective reporting (reporting bias) | Low risk | There is no indication that outcomes were reported selectively. Outcome data on all food and beverage items targeted by the intervention, and mentioned in the Methods section, are reported |
| Independence of the intervention from other changes (performance bias) | Low risk | It seems unlikely that other changes occurred at exactly the same time as the intervention which could have produced such a marked and clearly timed change in consumption patterns |
| Pre‐specification of the intervention effect (detection bias) | High risk | The point of analysis is the point of intervention; the results reported in the study are, however, not based on a classical ITS analysis |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | High risk | While the graphical presentation of results strengthens our confidence that effects were due to the intervention, and cannot be explained with underlying temporal trends, these were not taken into account in analyses. The authors conduct a statistical process management (SPM) analysis, which differs from classical ITS analyses. By contrast, seasonality seems unlikely to have influenced outcomes, as both the pre‐ and post‐intervention phase were in winter |
Simons 2015.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Quote: "The adolescents were randomly assigned to the intervention group or control group after baseline assessment by the researcher or a research assistant using a pre‐determined computer‐generated block randomization list with blocks of 100" Number of clusters or sites: N/A Number of individuals: 262 Length of intervention: 10 months |
|
| Participants |
General description of participants: Adolescents spending 2 hours or more a week with non‐active video games, living in cities in the Netherlands Age: Teenagers (age range 12 to 17 years, mean age 14 years) Inclusion criteria: Quote: "The inclusion criteria were as follows: The adolescent played ≥ 2 hours of non‐active video games per week. The adolescent played active video games less than once per week. The adolescent was physically and mentally able to play active video games (based on self‐report). The adolescent had access to a PlayStation 3 at home. The family did not have a Move upgrade for the PlayStation 3. The adolescent lived in the same home as the participating family members at least 4 days per week (to enable sufficient access to the Move video games provided as part of the intervention, see below). At least one other family member (parent or sibling aged 8–18 years old) was willing to participate in the study (i.e., complete the questionnaires)" Exclusion criteria: See inclusion criteria Recruitment: Quote: "Recruitment of adolescents takes place in four cities in the Netherlands: Amsterdam, Amersfoort, Leiden and Breda. Advertisements are posted on game websites, game magazines, Facebook, newsletter for PlayStation owners and local papers, and announcements are made on local radio. In addition, local health organizations (GGD) and municipalities in the four cities collaborate by providing addresses of families with a child aged 12–16 years old. In Leiden all families with a 12–16 years old child receive an invitation letter, and in Amsterdam, Breda and Amersfoort we make a selection based on postal code areas covering neighborhoods with a relatively low social economic status. Also, flyers are distributed in schools and popular places for gaming adolescents (e.g. game shops, music stores). Interested adolescents and families can provide their contact details on our project website or send it by mail. The interested families are contacted by email and asked to complete an online questionnaire to assess further inclusion criteria. Next, eligible families receive information about participation and an informed consent form that they have to fill in prior to the baseline measure. Then, families receive information about the baseline online questionnaires and an invitation for the adolescent’s baseline assessment" Weight status at baseline: Mean BMI was 21 kg/m2 in the IG and 20 kg/m2 in the CG at baseline. Baseline prevalence of overweight and obesity was 25% in the IG and 19% in the CG SSB consumption at baseline: At baseline, 73% of the participants in the IG and 76% of the participants in the CG reported consuming more than 1400 ml SSB a week Equity considerations: Recruitment focused on neighbourhoods with a relatively low socio‐economic status; 69% of participants were pursuing higher education, 83% were of Dutch ethnic origin, and 91% were boys. Quote from the protocol: "In Leiden all families with a 12–16 year‐old child receive an invitation letter, and in Amsterdam, Breda and Amersfoort we make a selection based on postal code areas covering neighborhoods with a relatively low social economic status" |
|
| Interventions |
Intervention: Provision of active video gaming equipment. (Quote: "The adolescents assigned to the intervention group received a PlayStation Move upgrade package to play the active video games on a PlayStation 3 console in their homes. The PlayStation Move uses a handheld motion controller wand, a motion‐capture PlayStation Eye camera that tracks the player’s position and inertial sensors in the wand that detect its motion. Thus, every movement of the player is mimicked on‐screen in the game. The following active video games were provided during the intervention: Sport Champions, Move Fitness, Start the Party and Medieval Moves, Dance Star Party and Sorcery") Behavioural co‐intervention: None reported Control: No intervention (Quote: "Adolescents in the control group were asked to continue their normal gaming behavior. They received PlayStation Move starter packs at the end of the study as an incentive for their participation. Further, they received a small gift (e.g., a magazine, lanyard, or pen) as an incentive after participation at each measure moment") |
|
| Outcomes |
Measures of SSB intake: Percentage of participants reporting more than 1400 ml SSB consumption a week, assessed with questionnaires at baseline and at 4 and 10 months follow‐up Measures of intake of alternatives to SSB: N/R Anthropometric measures: Assessed in this study but not included in our review due to confounding by non‐beverage‐specific intervention components Adverse outcomes: Potential adverse effects were assessed with a comprehensive process evaluation at 1, 2, 4 and 10 months follow‐up Other outcomes: Target group perceptions, assessed with a comprehensive process evaluation at 1, 2, 4 and 10 months follow‐up |
|
| Context and implementation |
Setting: Participants' homes Sector: Leisure time entertainment Country: The Netherlands Year(s) when implemented: 2012 ‐ 2013 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "Competing interests: The authors declare that they have no financial relationships relevant to this article. Sony Benelux provided the PlayStation Move packages and video games for the study participants, but did not have any role in the design, conduct or analysis of the study" Funding: "This work was supported by a grant from The Netherlands Organization for Health Research and Development (http://www.zonmw.nl/nl/)(grant number: 120520012). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Sony Benelux provided the PlayStation Move packages and video games for the study participants, but did not have any role in the design, data collection, and analysis, decision to publish or preparation of the manuscript" Trial registration: "Registered at the Nederlands Trial Register at trialregister.trialregister.nl/trialreg/admin/rctview.asp?TC=3228 Protocol availability: Published as a separate paper referenced in the study's primary report |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The adolescents were randomly assigned to the intervention group or control group after baseline assessment by the researcher or a research assistant using a pre‐determined computer‐generated block randomization list with blocks of 100" |
| Allocation concealment (selection bias) | Unclear risk | The study does not state if the allocation sequence was concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | The outcome of interest to us (SSB consumption) was similar in the IG (73% consuming more than 1400 ml/week) and in the CG (76% consuming more than 1400 ml/week). The statistical model adjusted for baseline outcome measurements. Quote: "In addition to the model that was adjusted for baseline (model 1), we also constructed a second model that was additionally adjusted for demographics (age, sex, ethnicity and adolescent educational level) (model 2)" |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Baseline demographics were similar, and were taken into account in the analysis (see quote above) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was low (about 3%), similar in the IG and the CG, and participants lost to follow‐up were not systematically different from the remaining ones. Quote: "Missing data analyses revealed that the adolescents who missed one or more anthropometric measurements (n = 30) did not differ in age, sex, educational level or ethnicity from the adolescents with complete anthropometric data (n = 240). Further, the adolescents who missed one or more questionnaire measurement (n = 42) did not differ in age, sex, educational level or ethnicity from the adolescents with complete questionnaire data (n = 228)" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and outcomes are self‐reported |
| Contamination (performance bias) | Low risk | The CG received the intervention (i.e. the active video‐gaming equipment) delayed by 10 months ‐ it seems unlikely that a considerable number of individuals in the CG purchased the equipment during the waiting time. Quote: "One adolescent in the control group reported having a PlayStation Move at baseline but not during the follow‐up measurements. At T10m one additional adolescent in the control group reported having a PlayStation Move application. (...) The process evaluation did not provide any reason to believe that the adolescents in the control group bought Move packages themselves and began playing (more) active video games" |
| Selective reporting (reporting bias) | Unclear risk | It is not clear why the SSB consumption data were dichotomised, and this is not mentioned in the trial register entry or the published protocol |
| Other bias | Low risk | No other concerns |
Sturm 2015.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: Quote: "The intervention group is respondents living in South Los Angeles, that is, the area targeted by the Fast‐Food Ban (...). The comparison groups are either respondents living in other parts of the city of Los Angeles (...) or living in other parts of Los Angeles County" Number of clusters or sites: An unspecified number of fast‐food restaurants in parts of South Los Angeles (including Baldwin Hills, Leimert Park, and portions of South Los Angeles and Southeast Los Angeles) (the IG), and in other parts of the city of Los Angeles and Los Angeles County (the CG) Number of individuals: This was a repeat cross‐sectional analysis, and the baseline sample size was 467 in the IG and 15,420 in the CG; the follow‐up sample size was 535 in the IG and 11,286 in the CG Length of intervention: 3 ‐ 4 years (no exact dates for follow‐up data collection reported) |
|
| Participants |
General description of participants: Residents of the city of Los Angeles and Los Angeles County, USA Age: Adults (all age groups were exposed to the intervention, but data were collected only from adults aged 18 years or older) Inclusion criteria: Quote: "Diet and obesity measures come from the 2007, 2009, and 2011–2012 waves of the California Health Interview Survey (CHIS), a random‐digit‐dial telephone survey of California’s non‐institutionalized population. We use the restricted files that identify a survey respondent’s residential address. In the three waves, a total of 141,597 adults ages 18 years and older were interviewed. The sampling weights provided by CHIS account for unequal sampling probabilities and non‐response. We exclude pregnant women (0.5%), respondents whose information was provided through a proxy interview (0.5%), and residents of areas defined as rural (1.7%)" Exclusion criteria: See inclusion criteria Recruitment: See inclusion criteria Weight status at baseline: Mean BMI was 29.9 in the IG at baseline, and 26.7 and 26.3 in the 2 CGs. Baseline prevalence of obesity was 32% in the IG and 17% and 22% in the CGs. Baseline prevalence of overweight and obesity combined was 63% in the IG and 57% and 55% in the CGs SSB consumption at baseline: Baseline intake frequency of soft drinks was 3.23 in the IG, and 2.3 and 2.1 in the 2 control groups (unclear if these numbers refer to servings/day or some other unit) Equity considerations: The area in which the intervention was implemented (South Los Angeles) is described as relatively low‐income and as having a high proportion of minority inhabitants. Quotes: "There is a widespread belief that low‐income or minority neighborhoods have an overconcentration of fast food chains. This belief was enshrined in the justification for the interim regulation (...) Prior to the regulation, South Los Angeles had more small retail stores, but not more (if anything fewer) large fast‐food restaurants than wealthier areas of Los Angeles per capita. Consistent with the business structure, residents in South LA also had a higher consumption of discretionary calories from candy, cookies, and soda" |
|
| Interventions |
Intervention: A zoning regulation that restricts opening or expanding stand‐alone fast‐food restaurants. (Quote: "The Los Angeles Fast‐Food Ban was introduced as a draft ordinance in the Los Angeles City Council in 2007 and after an extended debate was passed unanimously in July 2008. It became effective on September 14, 2008, initially as a temporary ordinance, but the City Council made it a permanent amendment to the city’s General Plan in December 2010. Despite its nickname, the policy is a zoning regulation that restricts opening or expanding a ‘stand‐alone fast‐food restaurant’ in Baldwin Hills, Leimert Park, and portions of South Los Angeles and Southeast Los Angeles; the paper refers to this area as South Los Angeles. Fast‐food restaurants are defined as ‘any establishment which dispenses food for consumption on or off the premises, and which has the following characteristics: a limited menu, items prepared in advance or prepared or heated quickly, no table orders, and food served in disposable wrapping or containers.’ The regulation prevents new drive‐through windows, new stand‐alone fast food restaurants, or expanding floor space. It does not affect interior remodeling or exterior changes that do not increase the floor space. For example, a fast food restaurant that shares a building in a strip mall would not be subject to the regulation") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: Intake frequency of soft drinks (excluding diet drinks), assessed with data from the California Health Interview Survey, a routine population health survey, at baseline and 3 ‐ 4 years follow‐up" Measures of intake of alternatives to SSB: N/R Anthropometric measures: Assessed in this study but not included in our review due to confounding by non‐beverage specific intervention components Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Fast‐food restaurants Sector: Food service/urban planning Country: USA Year(s) when implemented: 2008 ‐ 2012 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This project was supported by grant no. 1R03CA173040‐01 from the National Cancer Institute" Trial registration: N/R Protocol availability: N/R |
|
| Notes | See section on 'Potential biases in the review process' for a discussion of issues related to the minimum number of intervention and control sites | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Baseline outcome measurements differed substantially (baseline intake frequency of SSB was 3.23 in the IG, and 2.3 and 2.1 in the 2 control groups). While this was taken into account in the analysis, it may hint at unobserved baseline differences. Quote: "We assess crosssectional differences between areas and difference‐in‐differences (DID, whether secular changes in diet or obesity in South Los Angeles differ from secular changes in other areas)" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | There were differences in baseline characteristics, which were taken into account in the analysis. However, given the magnitude of differences it seems plausible that unobserved baseline differences may have existed, which could not be adjusted for. Quote: "Our main statistical analysis uses regression analysis to address potentially confounding variables at the individual and neighborhood level (including socio‐demographic changes that may differ across areas): gender, age, race/ethnicity, household size, annual household income, education, and marital status at the individual level; population density, median household income, and proportion of non‐Hispanic Whites of residential census tract from the 2010 Census as neighborhood‐level covariates" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data were repeat‐cross‐sectional. While precautions were taken to ensure representativeness of the sample at each time point, representativeness may not be given at the neighbourhood level. Quote: "Diet and obesity measures come from the 2007, 2009, and 2011–2012 waves of the California Health Interview Survey (CHIS), a random‐digit‐dial telephone survey of California’s non‐institutionalized population. We use the restricted files that identify a survey respondent’s residential address. In the three waves, a total of 141,597 adults ages 18 years and older were interviewed. The sampling weights provided by CHIS account for unequal sampling probabilities and non‐response. We exclude pregnant women (0.5%), respondents whose information was provided through a proxy interview (0.5%), and residents of areas defined as rural (1.7%)" |
| Blinding (performance and detection bias) Subjective outcomes | Low risk | This study is based on a retrospective analysis of routinely‐collected population health monitoring data. Bias due to lack of blinding is unlikely |
| Contamination (performance bias) | Unclear risk | Given the potential mobility of residents between the different parts of Los Angeles, contamination seems possible |
| Selective reporting (reporting bias) | Low risk | The study does not provide information on trial registration or the public availability of a protocol, but all outcomes mentioned in the Methods sections, and all outcomes which one would expect in a study of this kind are reported |
| Other bias | Low risk | No other concerns |
Taillie 2015.
| Methods |
Design: Controlled ITS Timing: Retrospective Allocation to group: The study compared sales data from Walmart, which self‐committed to a 'Healthier Food Initiative', with data from other chain retailers for which data were available. Quote: "We conducted counterfactual simulations by comparing the projected pre‐implementation trends in the nutrient profile of Walmart packaged food purchases to the observed post‐implementation trends in that profile. We examined whether those results varied using the official launch date of the initiative or a date indicated by the data as the cut‐off between the pre‐ and post‐implementation periods. We also compared trends at Walmart to concurrent trends in packaged food purchases at other chain retailers (grocery stores, supermarkets, and supercenters with at least ten locations) to examine whether the healthier food initiative was associated with any changes above and beyond industry trends" Number of clusters or sites: 1 company in the IG + an unspecified number of companies in the CG Number of individuals: N/A (The analysis is done on the level of households; Quote:"Household‐quarter observations were included for sample households that shopped (...) at Walmart (n= 1,212,803) or other chain retailers (n= 2,521,128) for at least two quarters") Length of intervention: 3 years (when January 2011 is taken as the start of the intervention) |
|
| Participants |
General description of participants: A nationally representative sample of customers of Walmart and other chain retailers living in the USA Age: All ages Inclusion criteria: N/R (but references to relevant secondary publications are provided) Exclusion criteria: See inclusion criteria Recruitment: See inclusion criteria Weight status at baseline: N/R SSB consumption at baseline: N/R Equity considerations: In the IG (i.e. among Walmart customers) at baseline 86% of participants were non‐Hispanic white, 5% were Hispanic, and 8% were non‐Hispanic black; 27% had high‐school education or less, 32% some college education, and 40% higher education; 7% were below the national poverty level |
|
| Interventions |
Intervention: Walmart's Healthier Food Initiative, a voluntary industry initiative. (Quote: "In 2011 Walmart announced a healthier food initiative with the stated intent of helping consumers make healthier food purchases. The initiative included a front‐of‐package labeling system to identify items that met certain nutrition criteria and strategic price reductions on healthier items. To improve the healthfulness of the food available, the initiative also had the following goals: to eliminate trans fat, reduce sodium by 25 percent, and reduce added sugar by 10 percent in key product categories by 2015. Walmart’s website suggests that these goals were to be achieved through the reformulation of products, but reductions in key nutrients across these product categories could also be achieved through the introduction of new products or the removal of other products") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB sales as share of total sales, assessed continuously throughout the study period with commercial household‐level consumer purchase data (Nielsen Homescan data) Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Supermarkets Sector: Retailing Country: USA Year(s) when implemented: 2008 ‐ 2013 Mode of implementation: Industry self‐regulation/voluntary industry action Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "Funding for this study came from the Robert Wood Johnson Foundation (Grant Nos. 67506, 68793, 70017, and 71837), the National Institutes of Health (Grant No. R01DK098072), and the Carolina Population Center (Grant Nos. R24 HD050924 and T32 HD007168)" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Percentage volume of sales from SSB (the outcome measure reported in this review) is reported graphically only, but seems to be similar at baseline for Walmart (i.e. the intervention group) and other chain retailers (the comparison group) (see this study's primary report appendix exhibit 3a and 5a) |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | Study authors provide justification for their choice of other chain retailers as comparison for Walmart. Demographic and socio‐economic characteristics of Walmart and other chain retailers customers are reported and similar. Quote: "To understand whether shifts in the nutrient profile of Walmart packaged food purchases were above and beyond industry trends, we also examined changes in packaged food purchases from other chain retailers, which are the most comparable group of stores given their size and product assortment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | While the Nielsen Homescan data used in this study are not without limitations, they are generally considered to provide relatively reliable estimates for population‐level purchasing behaviour |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but outcomes are objective, and outcome data were collected independently of the intervention and study |
| Contamination (performance bias) | Unclear risk | It seems possible that some of the other chain retailers serving as controls implemented similar interventions, as noted by the study authors. Quote: "[S]ince 2011, three of the US’ largest grocers have implemented “healthier foods initiatives” (HFIs) intended to improve the healthfulness of foods consumers purchase" |
| Selective reporting (reporting bias) | Low risk | This was a retrospectively‐conducted controlled ITS using routinely‐collected data. All outcomes mentioned in the Methods section are reported in the results section |
| Independence of the intervention from other changes (performance bias) | Unclear risk | Study authors explain that a number of factors not attributable to the intervention may have influenced the outcomes of interest. However, the use of a control group strengthens our confidence that the observed effects cannot be fully explained by these. Quote: "Possibly these changes simply reflect a shift in the public attitudes towards SSBs as a result of public health campaigns about the potential health consequences of SSBs ‐ although such a shift in awareness would have likely resulted in a downwards shift in SSB purchases at other chain retailers; as well, which we did not see" |
| Pre‐specification of the intervention effect (detection bias) | Low risk | Study authors provide justification for conducting analyses using, respectively, 2007 and 2011 as start date for the intervention. For the outcome of interest to this review both analyses yield similar results. Quotes: "The final challenge is determining the appropriate baseline period against which to measure these changes: since in a natural experiment, investigators do not implement an intervention but observe variation in response to natural events, it is not always obvious when the intervention occurred. In the present example, although Walmart formally announced their HFI in January of 2011, much of their online marketing suggests an earlier start date (i.e. “between 2008 and 2011 we removed 1.5 million pounds of salt across the commercial bread category”). (…) Thus, for all models, we examined both 2011 and 2007 as potential healthier food initiative initiation dates, since 2011 was Walmart’s stated initiation date and 2007 was the second most plausible date, given the 2008 date indicated in some of Walmart’s marketing materials. Using these start dates, we tested the shape of the trend. In the energy models, we found that when we used the 2011 start date, a quadratic trend provided the best fit (based on model R2 and visual inspection). In contrast, when we used the 2007 start date, a linear trend provided the best fit. For the sodium model, a linear trend provided the best fit for the 2011 start date, while a quadratic term provided the best fit for the 2007 start date. Models with the appropriate terms were used for the remainder of the analyses" |
| Intervention effects on data collection (detection bias) | Low risk | Data were collected routinely and independently of the intervention and the study. It is unlikely that the intervention affected data collection |
| Other bias | Low risk | There is no reason to assume that seasonality was a problem, or that other potential sources of bias existed |
Tate 2012.
| Methods |
Design: RCT Timing: Prospective Allocation to group: Quote: "Eligible participants were randomly assigned as cohorts after baseline measures by using a computer‐generated random‐numbers method by the project coordinator with allocation concealed from the participants and investigators until randomization was revealed to the study participants at the initial group session" Number of clusters or sites: N/A Number of individuals: 318 Length of intervention: 6 months |
|
| Participants |
General description of participants: Overweight or obese adults consuming at least 280 kcal/d of caloric beverages, living in the Raleigh‐Durham area in North Carolina, USA Age: Adults (aged 18 ‐ 65 years) Inclusion criteria: Quote: "18‐65 years of age; body mass index (BMI) between 25.0‐49.9 kg/m2; subject consumes at least 280 calories per day from caloric beverages" Exclusion criteria: Quote: "[R]eport losing >5% of current body weight in the previous 6 months; report participating in a research project involving weight loss or physical activity in the previous 6 months, as these proximal experiences may impact the results of this study. Additionally, report current participating in any other research studies whose results could be compromised by or in which participation could compromise this research study. (Participation in a research study that would not affect or be affected by this study is allowed.); report pregnancy or lactation during the previous 6 months, or planned pregnancy in the next 6 months; report taking medication that could affect metabolism or change body weight (e.g., synthroid); report hospitalization for psychiatric problems during the prior year; report major psychiatric diagnoses and organic brain syndromes; report heart problems, chest pain, cancer within the last 5 years; being treated by a therapist for psychological issues or problems with psychotropic medications; report behaviors that indicate probable alcohol dependence as assessed by the Rapid Alcohol Problems Screen (RAPS4‐QF); unwilling to change intake of beverages during the study period; plan to move from the area during the study period, and/or unable to attend monthly group meetings; report not having adequate transportation to the study center that would allow transport of study supplies back to the subject's home; report not being able to attend group meetings on Monday or Tuesday evenings" Recruitment: Quote: "We recruited, enrolled, and followed participants between May 2008 and January 2010 at UNC–Chapel Hill, North Carolina" (no further information provided) Weight status at baseline: Overweight or obese (a BMI between 25 and 50 was an inclusion criterion; mean baseline BMI was 37 in the CG and 38 in both IGs) SSB consumption at baseline: Intake of at least 280 kcal/d of caloric beverages was an inclusion criterion; SSB consumption at baseline is not reported, only energy intake from beverages in general, which was 320 kcal/day in the control group, 390 kcal/day in the diet beverage group, and 327 kcal/day in the water group Equity considerations: Participants lived in the Raleigh‐Durham area in North Carolina, USA. A variety of ethnic groups (approximately 55% were black, 40% were white, and 5% other), educational groups (approximately 7% high school or less, 40% some college, and 53% college graduate or beyond) and both sexes (85% female and 15% males) were represented |
|
| Interventions |
Intervention: Provision of water and diet beverages to participants at monthly group meetings, for transportation to their homes (Quote: “Both of the intervention groups received noncaloric beverages [water or noncaloric sweetened ('diet') beverages] (…). On the basis of previous research, four 355–500‐mL (12–16 oz) single‐serving beverages per person per day were provided to ensure availability, with 2 additional servings per day to account for family members’ occasional consumption, although this was discouraged. Participants in the Water group could choose any combination of bottled still and nonsweetened sparkling water. Similarly, participants in the DB group were provided any combination of noncaloric sweetened beverages of their choice, including carbonated, noncarbonated, noncaffeinated, and caffeinated beverages. Both the Water and DB groups were given beverages at their monthly treatment group meeting“) Behavioural co‐intervention: Dietary counselling focused on beverages (Quote: "Both of the intervention groups received (…) monthly group behavioral counseling to promote adherence to beverage substitution. The recommendations for each of these groups were identical except for the substituted beverage. Participants were encouraged to replace ≥2 servings (≥200 kcal) per day of caloric beverages with either water or DBs [diet beverages]") Control: General weight‐loss counselling (Quote: "The AC group was designed to equate treatment contact time and attention, monthly weigh‐ins, and weekly monitoring to facilitate study of the additional benefit of beverage change. This group, called 'Healthy Choices', attended monthly group sessions of identical length to the beverage groups. They were weighed and given general weight‐loss information (eg, instructed to read product labels, increase vegetable consumption, control portions, and increase physical activity); they were not given weight‐loss calorie‐reduction or physical activity goals. They were not encouraged to change beverage intake (beverages were not mentioned during the lessons or group sessions) and were not provided with beverages") |
|
| Outcomes |
Measures of SSB intake: Total energy intake from beverages (kcal/d), assessed through 24‐hour dietary recall at baseline, 3 and 6 months Measures of intake of alternatives to SSB: Water and diet beverage intake (g/d), assessed through 24‐hour dietary recall at baseline, 3 and 6 months (reported in the 2‐arm comparison presented in Piernas 2013 only) Anthropometric measures: Weight (kg) and waist circumference (cm), assessed with a standardised clinical protocol at baseline, 3 and 6 months Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: Total energy intake from solid foods (kcal/d), assessed through 24‐hour dietary recall at baseline, 3 and 6 months; blood glucose (mg/dl), systolic and diastolic blood pressure, and urine osmolality, assessed at baseline, 3 and 6 months |
|
| Context and implementation |
Setting: Participants' homes Sector: Health care Country: USA Year(s) when implemented: 2008 ‐ 2010 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "None of the authors has or had any conflicts of interest. Nestle´ Waters USA had no involvement in the study design, conduct, or preparation and review of this manuscript" Funding: "Supported by an investigator‐initiated research grant to University of North Carolina from Nestle´ Waters USA. Water was provided by Nestlé Waters USA" Trial registration: ClinicalTrials.gov number NCT01017783 Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | We combined the 2 outcome categories 'water' and 'beverages with low calorie sweeteners' and report these outcomes both separately and as combined outcome. For the data reported in the 3‐arm comparison we combined the 2 intervention arms to create a 2‐arm comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible participants were randomly assigned as cohorts after baseline measures by using a computer‐generated random‐numbers method by the project coordinator" |
| Allocation concealment (selection bias) | Low risk | Quote: "[A]llocation [was] concealed from the participants and investigators until randomization was revealed to the study participants at the initial group session" |
| Similarity of baseline outcome measurements (selection bias) | Low risk | For weight, waist circumference and blood pressure, baseline outcome measurements were similar. Energy intake from beverages differed between groups, but confidence intervals overlap |
| Similarity of other baseline characteristics (selection and performance bias) | Low risk | No significant differences in baseline characteristics between the 3 groups were observed (see table 1 of the study's primary report) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was low (approx. 15%) and similar across groups. Results are based on an intention‐to‐treat analysis with imputed data, and we conducted a sensitivity analysis for imputation. Quote: "For continuous variables, the Markov Monte Carlo method was used to impute missing data by generating a total of 10 imputations. Results from the imputations were combined by using PROC MIANALYZE in SAS. In a secondary analysis of study completers, results were consistent with the findings of the multiple imputation analysis except with respect to BP [blood pressure]" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Dietary intake was self‐reported, and blinding of participants was not possible |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but the outcomes (body weight and waist circumference) were objective and assessed based on a standardised clinical protocol |
| Contamination (performance bias) | Low risk | Contamination seems unlikely. Quote: "After the participants’ specific substitution group was revealed, the substitution for the other study group was not revealed, and the controls were not informed of either substitution until all cohorts were completed" |
| Selective reporting (reporting bias) | Unclear risk | The trial was registered towards the end of the study, and no published protocol is available. SSB consumption and BMI were inclusion criteria and assessed, but are not reported in the main 3‐arm comparison (the study does, however, report energy intake in kcal/day, waist circumference and body weight in kg as outcomes). The study does not report if outcomes were prespecified or not, and there are some differences between the outcomes listed as primary and secondary outcomes in the trial registry and those reported in the study reports |
| Other bias | Low risk | No other concerns |
Van de Gaar 2014.
| Methods |
Design: Cluster‐RCT (included as a NRCT in our GRADE assessment due to the small number of randomised units) Timing: Prospective Allocation to group: Quote: "A total of four schools, located in four different non adjacent neighbourhoods in Rotterdam, the Netherlands, were matched in pairs of two. (...) One of the schools in the school pair was then allocated to either the intervention or control condition by the flip of a coin" Number of clusters or sites: 4 schools Number of individuals: 1009 Length of intervention: 13 months |
|
| Participants |
General description of participants: Children attending elementary school in multi‐ethnic, socially‐deprived neighbourhoods in Rotterdam, the Netherlands Age: Children (age range 6 ‐ 12 years) Inclusion criteria: School‐level (Quote: "The matched schools had a roughly equal number of pupils, had pupils of similar socio‐economic status, and had a similar prevalence of overweight. On the basis of these criteria, we were able to select only six school pairs from the 80 schools that were eligible for the study. These pairs were then approached based on convenience, in the knowledge that a school pair could only be included in the study if both schools in the pair provided consent and a maximum of two school pairs in total could be included in the study." Student‐level (quote): "At the four participating schools, all children in grades 2 to 7 (aged 6‐12 years) were invited to participate, as were their parents") Exclusion criteria: N/R Recruitment: Schools were "approached on convenience" (quote); how students were approaches is not reported Weight status at baseline: The combined prevalence of overweight and obesity at baseline was 25.1% in the CG and 21.6% in the IG (based on the observation report, see table 2 of the study's primary report) SSB consumption at baseline: Baseline SSB consumption based on a survey among the parents of participating children was 760 ml/day in the IG and 850 ml/day in the CG. Based on a survey among the participants themselves it was 1310 ml/day in the IG and 1500 ml/day in the CG Equity considerations: The intervention was performed in neighbourhoods described as socially deprived and ethnically diverse. Approximately 25% of participants had a Dutch ethnic background, 30% Surinamese/Antillean, 27% Moroccan/Turkish, and 20% Other/Missing. Quotes: "The water campaign is an intervention tailored to children (...) and their families who live in multi‐ethnic, socially more deprived neighbourhoods; populations who remain disproportionately affected by childhood overweight. (...) [T]he local government intervention‐development team decided to focus the water campaign on Turkish and Moroccan families. These families form a large group of non‐Western immigrants in the study area, a group disproportionately affected by childhood overweight. (...) [W]hen we explored whether such tailoring of the water campaign specifically to these minorities improved the effects seen among these children, we were unable to detect significant differences in intervention effect between children of Turkish and Moroccan background and children from other ethnic backgrounds (p > 0.05 in all three data sets; data not shown)" |
|
| Interventions |
Intervention: Improved access to drinking water at school. (Intervention components included "[p]rovision of free water at school throughout the day; Taking a water break during physical education lessons; Provision of free water bottles by community organizations during summer activities") Behavioural co‐intervention: Educational and promotional activities based on social marketing techniques. (Behavioural intervention components included the following: "Special event: water campaign kick‐off ‘Drinking water is fun!’; Use of promotional material: posters ‘Water is the best thing I can give to my child!’ Activity for children: Pimp up your water bottle; Activity for parents: Pimp up your water jug; Water theme week, including [the following] activities for children: special educational water lessons, fun games such as happy families, board and card games involving water consumption, and a special water show provided by children’s role models. [Activities for] parents: storytelling about promoting water consumption, different fun games involving water consumption and other aspects of water, including a water magazine for mothers; and promotion by water ambassadors") Control: No intervention. (Quote: "The intervention and control schools continued with their regular health promotion programme, the effective school‐based curriculum ‘Enjoy Being Fit’") |
|
| Outcomes |
Measures of SSB intake: Average SSB consumption in l/day and servings/day, and percentage of participants consuming SSB every day, assessed through a questionnaire completed by participants and their parents at baseline and 13 months; and percentage of participants bringing SSB to school, assessed by trained observers on 1 randomly‐chosen day at baseline and 15 months Measures of intake of alternatives to SSB: Average water consumption in l/day and servings/day, and percentage of participants consuming water every day, assessed through a questionnaire completed by participants and their parents at baseline and 13 months Anthropometric measures: Mean BMI, and combined prevalence of overweight and obesity, assessed by trained personnel with a standardised protocol at baseline and 15 months Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not, but notes an increase in the BMI in the IG compared to the CG (see above) Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: The Netherlands Year(s) when implemented: 2011 ‐ 2012 Mode of implementation: Pilot trial by researchers in co‐operation with local government Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "All authors (VM van de Gaar, W Jansen, A van Grieken, GJJM Borsboom, S Kremers and H Raat) declare that they have no competing interests" Funding: "This study is funded by a grant from the major funding body ZonMw, the Netherlands Organization for Health Research and Development, project no. 50‐50102‐96‐015. This study is part of the Dutch project CIAO, which stands for Consortium Integrated Approach Overweight. Within CIAO, several studies are being conducted that investigate the different components of the EPODE approach. This study reflects on the component ‘social marketing’. The publication of this study was supported by a grant of the Netherlands Organization for Scientific Research (NWO)" Trial registration: Registered at the Nederlands Trial Register at trialregister.nl/trialreg/admin/rctview.asp?TC=3400 Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | Given the small number of randomised units, randomisation may not have been sufficient to attain baseline comparability of the IG and CG. We therefore included Van de Gaar 2014 as a NRCT in our GRADE assessment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "One of the schools in the school pair was then allocated to either the intervention or control condition by the flip of a coin" |
| Allocation concealment (selection bias) | Low risk | Allocation was by institution (school), and allocation was done at the start of the study |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Important baseline outcome measurement imbalances were present. The combined prevalence of overweight and obesity based on the observation report was 25.1% in the CG and 21.6% in the IG, and the share of students bringing SSB to school was 69% in the IG and 80% in the CG. Based on the parent report, baseline SSB consumption was 769 ml/day in the IG and 850 ml/day in the CG. While baseline differences were taken into account in the analysis, adjustment may not have been complete. Quote: "In all analyses, outcome measures were adjusted for baseline SSB values, several socio‐demographic characteristics (grade, gender and ethnic background of the child and educational level of the caregiver) and child’s weight status at baseline. This was done by also entering them as independent variables" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Potentially relevant baseline differences between the IG and CG were observed. The share of participants with Dutch ethnic background based on the parent report was 29% in the CG and 41% in the IG, and the share of parents with higher education was 50% in the CG and 55% in the IG. While baseline differences were taken into account in the analysis, adjustment may not have been complete. These differences, and the large differences in baseline outcome measurements, may hint at relevant differences in unobserved baseline characteristics of the IG and CG |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The analysis was per‐protocol. Participants lost to follow‐up differed significantly from those who stayed in the study, and it is unclear to what extent there was different attrition in the IG and CG. Quotes: "Only complete case analyses were performed, meaning we analysed data only from children whose data from both time points was complete. (...) The non‐response of parents to the parent questionnaire (complete case analyses only possible for 35%) is another limitation of this study. (...) We were able to conduct non‐response analyses for the variables gender, grade and ethnic background of the child. Parents of children who participated in the study were more often parents of children in the lower grades (p < 0.001) and of children with a Dutch ethnic background (p < 0.001) as compared to parents lost to follow‐up. Children who completed a questionnaire were more often children in the lower grades (p < 0.001) and children with a Dutch ethnic background (p = 0.007) as compared to children lost to follow‐up. Children who were observed were more often children with a non‐Dutch ethnic background (p < 0.001) as compared to children lost to follow‐up. Non‐response analyses were also conducted for the condition variable. Here we saw a difference between the intervention and control conditions in parents of children who participated in the study compared to parents lost to follow‐up (p = 0.006) and for children who underwent observation compared to children lost to follow‐up (p = 0.014)" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants and data collectors were not blinded, and the intensive behavioural co‐intervention may have introduced a relevant degree of social desirability bias. Quotes: "Blinding of participants and data collectors was not possible since the water campaign’s activities were visible at the intervention schools and throughout the neighbourhoods. (...) [R]esearch has shown that parents are more prone to reporting socially desirable answers compared to children. This could also partly explain the fact that SSB consumption reported by children was higher than that reported by parents" |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but body weight outcomes are objective, and were assessed by trained personnel with a standardised protocol |
| Contamination (performance bias) | Unclear risk | Contamination (in particular through the community component) is possible, and would have biased results towards null |
| Selective reporting (reporting bias) | High risk | The trial registry entry for this study (www.trialregister.nl/trialreg/admin/rctview.asp?TC=3400) mentions 3 potentially important outcomes which are not reported in the study: waist circumference, snack consumption and intake of fruit. Moreover, results on the prespecified primary outcome (BMI) and the first of the 4 prespecified secondary outcomes (water consumption) are not reported in the Results section of the paper, but only in the annexe, with a short reference in the Discussion section of the paper. For the first of the 4 secondary outcomes prespecified in the trial registry entry the study's primary report states explicitly that it was not an outcome Quote: "Although the intervention was aimed at reducing the intake of children’s SSB consumption by promoting the intake of water, water consumption was not an outcome measure of our study") |
| Other bias | Unclear risk | The unit of analysis was not the unit of control, and it is unclear to what extent this was taken into account in the analysis. Quote: "A further limitation is the small number of clusters (i.e. four), which inhibited multi‐level analyses but was countered by adding the ‘school pair’ variable in the analyses." For the beverage intake data it is not reported if the questionnaires which were used were validated (for the anthropometric measures standardised measurement protocols were used) |
Visscher 2010.
| Methods |
Design: NRCT Timing: Prospective Allocation to group: The allocation procedure is not explicitly described, but allocation depended on school characteristics. Quote: "[S]ix school locations were willing to participate. However, two of them could only be included as control schools, due to technical reasons and worries about spilling of water. Intervention schools were matched to these two control schools by educational level. Of the two remaining schools the school with the most pupils was selected as a control school" Number of clusters or sites: 6 schools Number of individuals: 5909 (according to table 1 of the study's primary report), 5866 (according to the abstract) Length of intervention: 3 months |
|
| Participants |
General description of participants: Secondary school students in Zwolle, a medium‐sized city in the Netherlands Age: Children and teenagers (age range 12 to 19 year, average age 14 years) Inclusion criteria: Quote: "Eligible schools had to meet the following inclusion criteria: i) preparatory secondary vocational level had to be offered, ii) sugar‐sweetened beverages had to be offered in school canteens, iii) at least 100 pupils had to be exposed to the school canteen" Exclusion criteria: See allocation to group Recruitment: Quote: "As part of the systematic approach we started inviting few schools only, in our city of Zwolle, a town in the northern part of the Netherlands with 114,635 inhabitants, until we found six participating schools, with at least a few including a relatively lower form of education. (...). Nine secondary schools (out of 15 school locations) met [the] inclusion criteria and received a letter of invitation with information about the intervention. They were contacted by phone subsequently. Two schools were not interested in participating, since they already were involved in another project aiming at improving healthy behaviour, and one school was not interested because of the expected extra work load. The remaining six school locations were willing to participate" Weight status at baseline: N/R SSB consumption at baseline: SSB sales at school at baseline were 17.9 ml/day/student in the IG and 25 ml/day/student in the CG. 3 months after the end of the intervention, a survey was conducted in participating schools showing a mean self‐reported SSB intake of 582 ml/day for boys and 275 ml/day for girls. Equity considerations: 2 of the intervention schools and all 3 control schools offered "a relatively lower form of education", and all schools offered a "preparatory secondary vocational level" |
|
| Interventions |
Intervention: Improved access to drinking water at school. (Quote: "The intervention consisted of placing water coolers in school canteens, providing free water to pupils, without any communication such as lessons or media messages. (...) At the three intervention schools, the water coolers were placed next to every vending machine. The coolers were installed one week before the intervention period, but left inoperable until the first day of intervention. At the first day of the intervention period, free water bottles were handed out, that pupils could use to refill at the water cooler. A local water distribution company provided the water coolers and water bottles") Behavioural co‐intervention: None. (Quote: "It was on purpose that information was not provided since the aim was to study the effect of changing one single environmental factor in secondary schools on sugar‐sweetened beverage sales") Control: No intervention. (Quote: "In the three control schools no water coolers were placed, and no bottles were provided") |
|
| Outcomes |
Measures of SSB intake: SSB (including sport drinks) sales in the school canteen and the vending machines present in the canteen, assessed with sales data (no further details reported) at baseline and 4 x 3 ‐ 4 week periods during the intervention (in total, the intervention lasted 3 months) Measures of intake of alternatives to SSB: Water taken from the water coolers, which had been installed as part of the intervention, assessed on the first day and every Friday during the intervention period with the waterflow meters attached to the water coolers Anthropometric measures: N/R Adverse outcomes: Leakage and misuse, assessed through observation by the investigators at baseline and on 1 day every 3 ‐ 4 weeks during the intervention period Other outcomes: Target group use of the water coolers, assessed through observation by the investigators at baseline and on 1 day every 3 ‐ 4 weeks during the intervention period |
|
| Context and implementation |
Setting: Schools Sector: Education Country: The Netherlands Year(s) when implemented: 2006 ‐ 2007 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: "The author(s) declare that they have no competing interests. The water distribution company Vitens had provided the water coolers and water bottles for free but had no influence on the design of the study nor on the analyses and interpretation of the results" Funding: "This study was supported by The Ministry of Health, Welfare and Sport. (...) Cooperation of Mr. Marcel Lips from Vitens and their free provision of water coolers and water bottles is gratefully acknowledged" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | High risk | There were substantial differences in baseline beverage consumption levels (table 2 of the study's primary report). It is unclear if this was taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | Control and intervention schools differed in a number of relevant observed characteristics, hinting at potential unobserved differences. Quote: "The remaining six school locations were willing to participate. However, two of them could only be included as control schools, due to technical reasons and worries about spilling of water. Intervention schools were matched to these two control schools by educational level. Of the two remaining schools the school with the most pupils was selected as a control school" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses are based on sales data, and there is no indication that these were incomplete |
| Blinding (performance and detection bias) Objective outcomes | Low risk | Participants were not blinded, but water consumption and SSB sales were measured with objective measures |
| Contamination (performance bias) | Low risk | It is unlikely that control schools received the intervention |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported, and while not stated explicitly, the wording suggests that they have been prespecified |
| Other bias | Unclear risk | Allocation was by institution (school), but SSB sales (the primary outcome) fluctuated widely between the pre‐intervention and the 4 intervention measurement periods, with no explanation provided which could account for these variations (see table 3 of the study's primary report) |
Waehrer 2015.
| Methods |
Design: CBA Timing: Retrospective Allocation to group: Quote: "Following the approach of Nord and Prell, we estimate difference‐in‐difference (DD) models comparing differences in pre‐post ARRA [American Recovery and Reinvestment Act] diets for SNAP [Supplemental Nutritional Assistance Program] eligible respondents (rather than participants) compared to those for ineligible respondents (rather than non‐participants) with incomes just greater than 150% but less than 250% of the federal poverty threshold. This group has been used as a comparison for SNAP‐eligibles in recent studies and have been treated as ‘nearly SNAP‐eligible households’ by Nord and Prell. While respondents in this income range are likely to be more economically secure than those who are eligible, many are still considered low‐income for public health insurance programs. For example, 250% FPL [federal poverty level] is used to define Medicaid and Children’s Health Insurance Program eligibility in 13 states while another 11 states have higher limits of at least 300% FPL for these programs. At the same time, respondents with incomes in the 150–250% FPL range are unlikely to receive SNAP benefits even in states with broad‐based categorical eligibility. Since a large percentage of SNAP‐eligible households do not participate in SNAP, the DD approach will underestimate the effect of the increase in benefits on SNAP participants but is a valid intent‐to‐treat effect" Number of clusters or sites: N/A Number of individuals: 2844 Length of intervention: Approximately 8 months |
|
| Participants |
General description of participants: Low‐income individuals living in the USA Age: Adults (aged 18 years or older was an inclusion criterion) Inclusion criteria: Quote: "In this study, we identify SNAP [Supplemental Nutritional Assistance Program] eligible respondents as those with gross household income less than 150% of the federal poverty threshold for that household size. (…) Finally, we also define SNAP eligibles to include those with incomes higher than the 150% threshold who report current receipt of SNAP benefits. Our sample includes SNAP‐eligible NHANES [National Health and Nutrition Examination Survey] respondents who had two days of dietary recall data recorded between the official start of the recession in October 2007 and December 2010. Since youth have access to food from school meal programs, we focus our analysis on those aged 18 and over, yielding a sample of 2844 eligible adults" Exclusion criteria: See inclusion criteria Recruitment: The study is based on data provided by the National Health and Nutrition Examination Survey (NHANES), a nationally representative health and nutrition survey in the USA. The study does not report details of recruitment procedures used by NHANES, but provides references to relevant secondary publications Weight status at baseline: Mean baseline BMI was 29 kg/m2 in the IG and CG SSB consumption at baseline: Mean baseline caloric intake from SSB was 178 kcal/day in the IG, and 131 kcal/day in the CG Equity considerations: In the full sample of the IG at baseline, 42% of participants were male, 48% were white, 15% non‐Hispanic black, and 32% Hispanic; 46% had less than high school education, 27% had high school education, 21% some college education and 6% were college graduates. 43% were employed. See inclusion criteria for further details |
|
| Interventions |
Intervention: An increase in the amount and expansion in the coverage of the Supplemental Nutritional Assistance Program (SNAP) food benefit programme in the USA, mandated by the American Recovery and Reinvestment Act of 2009 (ARRA). (Quote: "As part of the ARRA, SNAP benefits were increased by a constant dollar amount according to household size. This increase is equivalent to a 13.6% increase in the maximum allotment for that household size, with proportionally greater increases for families receiving less than the maximum allotment. Also, the 3 month time limits on program participation by jobless, working‐age adults with no children was relaxed. In 2009, the average monthly SNAP benefit was $125 per person, up nearly 22.6% from $102 in 2008. (…) SNAP benefits may not be used on ready‐to‐eat hot meals or in restaurants. In 2013, the average monthly SNAP benefit was approximately $275 per household") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB intake in kcal/day, assessed at baseline and at approx. 8 months post‐intervention with data from the National Health and Nutrition Examination Survey (NHANES), a nationally‐representative health and nutrition survey in the USA Measures of intake of alternatives to SSB: N/R Anthropometric measures: N/R Adverse outcomes: The study does not report if adverse outcomes occurred or not, but notes an increase in caloric intake from SSB in the IG Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Households Sector: Social security/public food benefit programmes Country: USA Year(s) when implemented: 2009/2010 Mode of implementation: Mandatory government regulation Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "This research was partly funded through a Research Innovation and Development Grant in Economics (RIDGE) Grant No. 59‐5000‐0‐0013 from the U.S. Department of Agriculture’s (USDA) Economic Research Service administered through the Institute for Research on Poverty (IRP) at the University of Wisconsin‐Madison" Trial registration: N/R Protocol availability: N/R |
|
| Notes | We report in our review results from the model using the less‐educated sample, as these are described by the study authors as the best approximation of the real effects. Quote: "To further minimize the effect of compositional changes in SNAP participants, we also estimate the effects of SNAP expansion among those with a high school or lower education. If the less‐educated group of low‐income individuals faces a tighter food budget and is therefore more likely to enroll in SNAP even at the pre‐ARRA benefit levels than those with higher education, the DD estimates for this group should more closely approximate the effect of higher SNAP benefits on dietary outcomes separate from any compositional changes due to expanded participation in the program" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Baseline outcomes measures (in particular daily energy intake from SSB) were significantly different between groups, but the statistical models used seem to have fully adjusted for this. However, given their magnitude some bias still seems possible. Quotes: "[P]re‐ARRA SSB consumption for SNAP‐eligible respondents is 178 calories per day, significantly higher than 131 calorie consumption of those ineligible for SNAP. (...) Models controlling for total energy intake (in logarithms) reveal that pre‐ARRA, SNAP‐eligibles consume a significantly larger share of total calories from SSBs" |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Baseline characteristics of participants differed substantially, and were taken into account in the analysis. However, given their magnitude some bias still seems possible. Quote: "Models also control for age, gender, education (high school/ged; some college; college grad; missing education), employment status, race/ethnicity, the ratio of household income to federal poverty threshold, household size, family structure (divorced/separated/widowed/never married, missing marital status), quarterly time trend, and state fixed effects" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The NHANES data is generally considered to be relatively reliable, and it seems unlikely that incomplete outcome data differently affected the control and intervention group at pre‐ and post‐intervention |
| Blinding (performance and detection bias) Subjective outcomes | Low risk | This study is based on a retrospective analysis of routinely‐collected population health monitoring data. Bias due to lack of blinding is unlikely |
| Contamination (performance bias) | High risk | The definition of the intervention group led to an expected 'misclassification' for part of the group. Authors explain that this would have biased effects towards the null |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported. The study does not report if analyses and outcomes were prespecified, and no protocol or trial registration are mentioned. There is no indication that outcomes were reported selectively |
| Other bias | Low risk | No other concerns |
Whatley Blum 2008.
| Methods |
Design: CBA Timing: Prospective Allocation to group: Quote: "High schools volunteered as intervention schools (n = 4), with an aim to eliminate and/or reduce SSB and diet soda, or as control schools (n =3), which made no changes in beverages offered in a la carte and vending programs for 1 school year" Number of clusters or sites: 7 schools Number of individuals: 456 Length of intervention: 9 months |
|
| Participants |
General description of participants: High‐school students in small cities in Maine, USA Age: Adolescents (mean age 16 years) Inclusion criteria: Quote: "Only students in grades 9‐11 were eligible, because students had to be available over 2 school years" Exclusion criteria: N/R Recruitment: Quote: "A convenience sample of students was recruited through presentations in selected classes (eg, physical education, health education, home economics, and science), as well as through posters and announcements on the public address system of the schools. (...) Students were offered a $10 gift certificate to a sporting goods store for each year of participation" Weight status at baseline: N/R SSB consumption at baseline: Baseline mean SSB intake among girls was 284 ml/day in the IG and 295 ml/day in the IG, and among boys it was 418 ml/day in the IG and 468 ml/day in the CG Equity considerations: Participants were residents of small communities (2500 to 23,000 inhabitants, median household income (USD 28,390 to USD 56,491) in Maine, USA. 97.8% were white; approximately 70% were girls |
|
| Interventions |
Intervention: Reduced availability of SSB at school. (Quote: "High schools volunteered as intervention schools (..) with an aim to eliminate and/or reduce SSB and diet soda, offered in a la carte and vending programs for 1 school year. (...) Indeed, diet soda was eliminated [from 1,3 % to 0,0 %], and SSB was reduced to a small percentage of total beverages ([from 44,1% to] 3.6%) in the intervention schools") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB intake in servings/day, assessed with a food‐frequency questionnaire at baseline and 9 months Measures of intake of alternatives to SSB: Intake of diet soda, milk and juice in servings/day, assessed with a food‐frequency questionnaire at baseline and 9 months Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Schools Sector: Education Country: USA Year(s) when implemented: 2004 ‐ 2006 Mode of implementation: Pilot trial by researchers Level of implementation: Setting‐based intervention |
|
| Declarations |
COI: No information provided by study authors (the study's primary report does not contain a COI section) Funding: "The Centers for Disease Control and Prevention provided funding for this study (grant 03022)" Trial registration: N/R Protocol availability: Protocol mentioned in the report but not publicly available |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a NRCT, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a NRCT, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Low risk | Baseline beverage consumption of students is reported and similar (see table 2 of the study's primary report) |
| Similarity of other baseline characteristics (selection and performance bias) | High risk | Schools self‐selected into the IG and CG, which is likely to produce unobserved baseline differences between the 2 groups. Beverage availability differed between IG and CG at baseline. Quotes: "High schools volunteered as intervention schools (n = 4), with an aim to eliminate and/or reduce SSB and diet soda, or as control schools (n =3), which made no changes in beverages offered in a la carte and vending programs for 1 school year. (...) The availability of beverages in the intervention and control schools at baseline was not perfectly matched; the intervention schools had less SSB and diet soda, and more milk, juice, and water available as compared to the control schools. These baseline differences may have influenced the beverage consumption patterns of subjects" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | A per‐protocol analysis was done, and attrition was substantial (approx. 22%) in both the CG and IG |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants and providers were not blinded, and outcomes were self‐reported. Quotes: "[L]etters were sent home to inform students and their parents of upcoming changes in the vending and à la carte programs. (...) Subjects were asked to complete the youth food frequency questionnaire for what they ate and drank over the past 30 days" |
| Contamination (performance bias) | Unclear risk | The study authors indicate that there may have been contamination. Quotes: "Although control schools did not aim to change the availability of beverages in their food venues, there was a decrease of 9.4% in SSB availability. This decrease in availability of SSB could have contributed to the overall decrease in the control subjects’ SSB consumption. Taken together, these data may be a reflection of the social environment. That is, at the time of the study, at least 3 statewide policy initiatives were being discussed regarding healthful food choices in Maine public schools. For example, the Maine Department of Education was proposing a statewide rule that would eliminate food of minimal nutritional value, such as soda and candy, from being available to students in all public schools. Discussions around these initiatives were widely publicized and may have influenced food and beverage consumption of all Maine citizens. Furthermore, these discussions may have influenced the control schools’ decision to offer fewer SSB (eg, soda) in school food venues" |
| Selective reporting (reporting bias) | Unclear risk | No trial registration is reported. A study protocol is mentioned in the report but is not publicly available. Students completed a food‐frequency questionnaire which covered both foods and beverages, but only beverage outcome data are reported, and it is unclear if the data for food intake was published elsewhere |
| Other bias | Unclear risk | The unit of control (schools) and the unit of analysis (students) are not the same, and it is not reported if this was taken into account in the analysis |
Øverby 2012.
| Methods |
Design: CBA Timing: Prospective Allocation to group: The study compares schools which implemented 2 different types of fruit provision schemes with schools that did not implement such schemes during the study period. Quote: "Initially, Hedmark and Telemark counties were chosen [as intervention sites] because the subscription program was about to start in these 2 counties in the school year 2001–2002. (...) In September 2001, no schools had any organized school fruit program. In September 2008, 5 schools participated in the free school fruit program (...), 10 schools participated in the subscription program, and 12 schools did not participate in any official school fruit program (...) [T]he subscription schools were self‐selected" Number of clusters or sites: 27 schools Number of individuals: 1488 (baseline assessment), 1339 (follow‐up assessment) Length of intervention: 6 years |
|
| Participants |
General description of participants: Students at elementary schools in Hedmark and Telemark, Norway Age: Children (age range 10 to 12 years) Inclusion criteria: N/R Exclusion criteria: N/R Recruitment: Quote: "In 2001, 48 schools from Hedmark and Telemark counties (24 schools in each county) were randomly selected and invited to participate in the research project Fruits and Vegetables Make the Marks (...). Nineteen schools from each county agreed to participate. All sixth‐ and seventh‐graders (ages 10–12 y) in these 38 schools were invited to take part in a questionnaire survey. These 38 schools were contacted again in 2008 and invited to once more participate in a similar survey. At that time, 27 schools—14 in Hedmark and 13 in Telemark—agreed to participate, and all sixth‐ and seventh‐graders in these 27 schools were invited to take part in the survey. Pupils from these 27 schools, from both 2001 and 2008, constitute the study sample of the current study" Weight status at baseline: N/R SSB consumption at baseline: At baseline, participants in the IG and CG reported consuming SSB on average 7 times a week Equity considerations: "[A] significant time x parental educational level interaction was observed (P = 0.01), and the decrease in frequency of unhealthy snack consumption was greater for children of parents without a higher education (from 7.3 times/wk in 2001 to 4.7 times/wk in 2008) than for children of parents with higher education (from 5.9 to 4.1 times/wk, respectively). Stratified on parental educational level, the effect of the school fruit programs was significant in reducing the frequency of unhealthy snack consumption for children of parents without higher education (time x group P = 0.004), but not significant for children of parents with higher education (time x group: P = 0.32)" |
|
| Interventions |
Intervention: A fruit subscription programme (with parental payment) and free fruit provision (without parental payment) at public schools. (Quote: "Among the initiatives is an FV [fruit and vegetable] subscription program for grades 1–10 that was initiated in 1996 and was made nationwide in 2003. Furthermore, from autumn 2007, an official free fruit program (without parental payment) was implemented in all secondary elementary schools (8th–10th grades) and combined schools (1st–10th grades). The pupils who subscribe or are a part of the free fruit program receive a piece of fruit or a carrot each school day") Behavioural co‐intervention: None reported Control: No intervention |
|
| Outcomes |
Measures of SSB intake: SSB intake (times per week), assessed with a non‐validated questionnaire at baseline and 6 years follow‐up Measures of intake of alternatives to SSB: Diet beverage intake (times per week), assessed with a non‐validated questionnaire at baseline and 6 years follow‐up Anthropometric measures: N/R Adverse outcomes: The study does not report how data on adverse outcomes were collected, and if adverse outcomes were observed or not Other outcomes: None included in this review |
|
| Context and implementation |
Setting: Elementary schools Sector: Education Country: Norway Year(s) when implemented: 2001 ‐ 2007 Mode of implementation: Government programme Level of implementation: Policy‐level intervention |
|
| Declarations |
COI: "KIK has been employed since 2006 by the Norwegian Directorate of Health, which is partially responsible for implementing the national school fruit programs. EB and NCØ had no conflicts of interest" Funding: "Supported by the Norwegian Research Council (both the 2001 and 2008 studies)" Trial registration: N/R Protocol availability: N/R |
|
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Allocation concealment (selection bias) | High risk | This was a CBA, and allocation was not random and not concealed |
| Similarity of baseline outcome measurements (selection bias) | Unclear risk | Baseline SSB consumption data provided by the authors show differences which are substantial compared with the observed effect sizes (± 0.33 compared with an effect size of −0.69). It is not clear if these were taken into account in the analysis |
| Similarity of other baseline characteristics (selection and performance bias) | Unclear risk | Schools self‐selected into the IG and CG, which may have produced unobserved baseline differences. Quote: "A limitation of the study was the nonrandomization of the different groups. The Free Fruit 08 groups constitute all combined schools (with grades 1–10), and the subscription schools were self‐selected. The pupils attending the different types of schools may have been different, even though that was not likely. Data presented in Table 2 indicate no baseline differences between the groups regarding the frequency of consumption of unhealthy snacks. The trends and results reported in this study are clear, and a potential group effect was expected to be small" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition at the school level was substantial (approximately 30%), which raises some doubts about possible bias, even though the authors undertook analyses to check if schools for which follow‐up data were missing were different at baseline from those that remained in the study sample. Quote: "To conduct a school attrition analysis, pupils at the 27 schools in the study sample were compared with those of the 11 schools participating in 2001 but not in 2008, regarding sex, parental educational level, and unhealthy snacks at school and all day. A t test was used for continuous variables and chi‐square statistics for the categorical variables. No significant differences between the study sample and pupils at schools not participating in 2008 were observed" |
| Blinding (performance and detection bias) Subjective outcomes | High risk | Participants were not blinded, and outcomes are self‐reported |
| Contamination (performance bias) | High risk | Contamination is likely, and would have biased results towards null Quote: "A second limitation of the study was that some schools now organize their own school fruit programs. School fruit has been a hot topic in Norway over recent years, possibly because of long‐term sustained public efforts. Within the No program 08 group, one of the schools had their own free fruit program; therefore, the results presented in this study may have underestimated the association between introducing a school fruit program and the observed reduction in frequency of reported intake of unhealthy snacks" |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the Methods section are reported |
| Other bias | Low risk | No other concerns |
BMI: body mass index; CG: control group; IG: intervention group; N/A: not assessed; N/R: not reported
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alaimo 2013 | Indirect environmental change intervention |
| Alaimo 2015 | Indirect environmental change intervention |
| Alberti 2010 | EPOC criteria not fulfilled (ITS with fewer than 3 data points before the intervention); study focus was on milk rather than SSB |
| Allan 2015 | EPOC criteria not fulfilled (cross‐over cluster‐RCT with 1 intervention and 1 control site); follow‐up too short (the intervention phase lasted 6 weeks) |
| Ames 2016 | Behavioural intervention focused on SSB; ineligible setting (research laboratory) |
| Andersen 2016 | In this study, participants received either water or 1 of 3 different types of protein drinks; the aim was to compare these, and not to displace SSB consumption |
| Anttila 2015 | Ineligible study design (UBA study) |
| Anzman‐Frasca 2015 | Ineligible study design (UBA study) |
| Bacardi‐Gascon 2012 | Behavioural intervention |
| Bae 2012 | EPOC criteria not fulfilled (ITS study with 1 pre‐intervention data point only) |
| Baidal 2017 | Behavioural intervention partly focused on SSB |
| Baranowski 2000 | Intervention not focused on beverages, no beverage‐specific outcome data reported |
| Baranowski 2003 | Study size too small; behavioural intervention not focused on SSB |
| Barlow 2017 | Ineligible outcomes (no beverage‐specific outcome data reported) |
| Barlow 2018 | Ineligible outcomes (no beverage‐specific outcome data reported) |
| Barr 2000 | Behavioural intervention focused on milk |
| Bayer 2009 | Indirect environmental change intervention |
| Beck 2017 | Behavioural intervention focused on SSB |
| Beets 2014 | Ineligible study design (UBA study) |
| Beets 2016 | Indirect environmental change intervention |
| Beinert 2017 | Behavioural intervention partly focused on SSB |
| Bender 2014 | Behavioural intervention; Follow‐up too short |
| Bender 2016 | No direct environmental intervention component |
| Bergen 2006 | Follow‐up too short (7 weeks) |
| Bjelland 2011 | Behavioural intervention partly focused on SSB |
| Bleich 2012 | Follow‐up too short (9 weeks); EPOC criteria not fulfilled (4 study arms with 1 intervention site each) |
| Bleich 2014 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before the intervention); follow‐up too short (each intervention phase lasted 3 weeks followed by a 2‐week washout phase) |
| Bleich 2017 | EPOC criteria not fulfilled (ITS study with1 pre‐intervention data point only) |
| Block 2010 | EPOC criteria not fulfilled (cluster‐NRCT with 1 intervention and1 control site); follow‐up too short (each intervention phase lasted 4 weeks) |
| Bogart 2011 | Follow‐up too short (5 weeks); EPOC criteria not fulfilled (cluster‐NRCT with 1 control site only) |
| Boone‐Heinonen 2011 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before and after the intervention) |
| Brandstetter 2012 | Behavioural intervention partly focused on SSB |
| Branscum 2013 | Behavioural intervention partly focused on SSB |
| Brown 2009 | Ineligible study design (UBA study) |
| Bruerd 1996 | Behavioural intervention focused on SSB |
| Brunello 2014 | No beverage‐specific outcome data available |
| Bruun 2015 | Clinical trial in which participants received SSB; study size too small (fewer than 20 individuals in each study arm) |
| Bryden 2013 | Ineligible study design (review article) |
| Burrows 2012 | Intervention not focused on beverages, no beverage‐specific outcome data reported |
| Butler 2011 | Ineligible study design (UBA study) |
| Caljouw 2014 | Ineligible setting (research laboratory); Follow‐up too short (less than 1 day) |
| Campbell 2013 | Behavioural intervention |
| Campos 2015 | Clinical trial in which participants received SSB; study size too small (fewer than 20 individuals in each study arm) |
| Campos 2017 | Clinical trial in which 1 group of participants received SSB |
| Carriedo 2013 | Behavioural intervention focused on water (the intervention may have included some environmental components; however, we were unable to contact the study authors for clarification) |
| Casazza 2006 | Behavioural intervention not focused on SSB |
| Chen 2009 | Behavioural intervention focused on SSB |
| Chen 2010 | Behavioural intervention focused on SSB |
| Chi 2016 | Clinical trial in which 1 group of participants received SSB |
| Chin 2008 | Indirect environmental change intervention |
| Choi 2017 | EPOC criteria not fulfilled (ITS with no clear time point when the intervention occurred) |
| Cloutier 2015 | Behavioural intervention partly focused on SSB |
| Collins 2014 | Behavioural intervention partly focused on SSB |
| Cordeira 2012 | Behavioural intervention partly focused on SSB |
| Cox 2012 | Clinical trial in which participants received SSB; follow‐up too short (10 weeks) |
| Cullen 2006 | Ineligible study design (SSB consumption data is based on a UBA analysis); unclear to what extent SSBs were targeted by the intervention (we contacted study authors for clarification, and confirmed that only some SSBs were removed from the cafeterias) |
| Cullen 2008 | Ineligible study design (UBA); intervention not focused on SSB |
| Cummins 2014 | EPOC criteria not fulfilled (CBA study with 1 intervention and control site only) |
| Cunha 2013 | Behavioural intervention partly focused on SSB |
| Daniels 2014 | Behavioural intervention partly focused on SSB |
| Dannefer 2012 | Ineligible study design (UBA study) |
| Davis 2007 | Study size too small; behavioural intervention not focused on SSB |
| De Bourdeaudhuij 2015 | Indirect environmental change intervention |
| De Moraes 2017 | Behavioural intervention focused on SSB |
| De Ruyter 2014 | Clinical trial in which 1 group of participants received SSB |
| De Souza 2013 | Indirect environmental change intervention |
| Delpier 2013 | Ineligible study design (UBA); behavioural intervention focused on SSB |
| Dennis 2010 | Behavioural intervention focused on water (in this study, participants in both the intervention and the control group received bottled water, and participants in the intervention group additionally received the instruction to consume 500 ml water prior to each meal; the study thus tested if advice about pre‐meal water intake is beneficial, and is thus a behavioural intervention study by our definition) |
| Donnelly 2018 | Follow‐up too short (2 weeks for each condition, 10 weeks in total), ineligible study design (UBA analysis) |
| Doymaz 2009 | Behavioural intervention focused on SSB; Follow‐up too short (2 weeks) |
| Drewnowski 2017 | Ineligible study design (UBA study) |
| Dubuy 2014 | Behavioural intervention partly focused on SSB |
| Duncan 2011 | Behavioural intervention not focused on SSB |
| Elbel 2009 | Ineligible outcomes |
| Elbel 2011 | Follow‐up too short (4 weeks) |
| Elbel 2015b | EPOC criteria not fulfilled (CBA study with 1 intervention and 1 control site only) |
| Elder 2014 | Follow‐up too short (8 weeks) |
| Ezendam 2007 | Behavioural intervention partly focused on SSB |
| Ezendam 2012 | Behavioural intervention partly focused on SSB |
| Ferguson 2016 | ineligible study design (UBA study) |
| Fernandes 2009 | Behavioural intervention partly focused on SSB |
| Fernandes 2012 | Ineligible study design (UBA study) |
| Fiechtner 2016 | Ineligible study design (repeat cross‐sectional observational study) |
| Folta 2013 | Behavioural intervention partly focused on SSB |
| Foster 2010 | Indirect environmental change intervention |
| Franks 2017 | Follow‐up too short (the intervention phase of interest to this review ‐ the water affordance intervention ‐ lasted only 3 weeks) |
| French 2011 | Behavioural intervention not focused on SSB |
| French 2015 | Study size too small (only 15 participants in the control group) |
| Fung 2013 | Ineligible study design (UBA); intervention partly focused on SSB |
| Garipagaoglu 2009 | Behavioural intervention partly focused on SSB |
| Geliebter 2013 | EPOC criteria not fulfilled (cluster‐NRCT with 1 intervention and control site only) |
| Giles 2012 | Ineligible outcomes (water intake only) |
| Gittelsohn 2010a | Indirect environmental change intervention |
| Gittelsohn 2010b | Indirect environmental change intervention |
| Gittelsohn 2013 | Indirect environmental change intervention |
| Goldberg 2015 | Behavioural intervention focused on SSB |
| Gomez 2013 | Behavioural intervention focused on SSB |
| Gostin 2014 | Ineligible study design (case study) |
| Goto 2013 | Follow‐up too short (5 days) |
| Greece 2017 | EPOC criteria not fulfilled (NRCT with 1 intervention and 1 control site only) |
| Griffin 2015 | Behavioural intervention focused on SSB |
| Haddock 2014 | Clinical trial testing the hypothesis that green tea extract added to a diet beverage increases weight loss; participants received fortified diet beverages, but not with the aim of displacing SSB consumption |
| Haerens 2007 | Indirect environmental change intervention |
| Han‐Markey 2012 | Ineligible study design (UBA study) |
| Hanks 2014 | Ineligible study design (UBA study) |
| Hebden 2014 | Behavioural intervention partly focused on SSB |
| Hedrick 2015 | Behavioural intervention focused on SSB |
| Hodgson 2013 | Clinical trial in which 1 group of participants received low‐calorie beverages (black tea), but not with the aim of displacing SSB |
| Hoeft 2016 | Behavioural intervention partly focused on SSB |
| Holmes 2012 | Ineligible study design (beverage outcome data are based on UBA analyses) |
| Hoppu 2010 | Indirect environmental change intervention |
| Iaia 2017 | Behavioural intervention partly focused on SSB |
| James 2004 | Behavioural intervention focused on SSB |
| Jancey 2014 | Behavioural intervention partly focused on SSB |
| Jensen 2012 | Ineligible study design (UBA study) |
| John 2017 | Ineligible setting (research laboratory), follow‐up too short (one‐off experiment) |
| Jones 2015 | Indirect environmental change intervention |
| Jones 2016 | Ineligible study design (case study/UBA study) |
| Jue 2012 | Follow‐up too short (4 weeks for each of the 5 intervention phases) |
| Kansagra 2015 | Ineligible study design (case study) |
| Keast 2015 | Follow‐up too short (6 weeks) |
| Keita 2014 | Behavioural intervention |
| Keller 2016 | Clinical trial in which participants received SSB; study size too small (fewer than 20 individuals in each study arm) |
| Kenney 2015 | Follow‐up too short (3 weeks) |
| Kerr 2016 | Behavioural intervention not focused on SSB |
| Kim 2013 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before and after the intervention) |
| Kipping 2014 | Behavioural intervention not focused on SSB |
| Klerman 2014 | No beverage‐specific outcome data available |
| Klesges 2010 | Behavioural intervention not focused on SSB |
| Klohe‐Lehman 2007 | Behavioural intervention |
| Kobel 2014 | Behavioural intervention not focused on SSB |
| Kobel 2016 | Behavioural intervention partly focused on SSB |
| Kocken 2012 | Follow‐up too short (each intervention phase lasted 3 to 6 weeks, and is analysed separately) |
| Korwanich 2008 | Indirect environmental change intervention |
| Kral 2016 | No beverage‐specific outcome data available |
| Kubik 2011 | Ineligible study design (cross‐sectional study) |
| Kubik 2013 | Ineligible outcome (availability of SSB but not of direct or indirect measures of SSB intake) |
| Lahlou 2015 | Follow‐up too short (the intervention phase of interest to this review ‐ the water affordance intervention ‐ lasted only 3 weeks) |
| Lao 2011 | Follow‐up too short (8 weeks); behavioural intervention not focused on SSB |
| Laurence 2007 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before and after the intervention) |
| Lawman 2015 | Ineligible study design (UBA study) |
| Lee 2018 | Ineligible study design (simulation study) |
| Lee‐Kwan 2015 | No beverage‐specific outcome data available |
| Leung 2014 | Ineligible study design (UBA); intervention not focused on SSB |
| Levy 2012a | EPOC criteria not fulfilled (RMS with fewer than 3 data points before the intervention) |
| Levy 2012b | Indirect environmental change intervention |
| Lo 2008 | Behavioural intervention focused on SSB |
| Loeb 2017 | Follow‐up too short (less than 1 day) |
| Looney 2012 | Behavioural intervention partly focused on SSB |
| Looney 2014 | Behavioural intervention not focused on SSB; study size too small |
| Loughridge 2005 | EPOC criteria not fulfilled (cluster‐NRCT with 1 intervention site per study arm) |
| Lowe 2010 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before and after the intervention) |
| Lowndes 2012 | Clinical trial in which 1 group of participants received sugar‐sweetened milk |
| Luehrmann 2014 | Follow‐up too short (8 weeks) |
| Luger 2018 | Ineligible study design (UBA study) |
| Lumeng 2017 | Behavioural intervention |
| Luoto 2012 | Ineligible outcomes (water intake only) |
| Madjd 2015 | In this study, participants received water with the aim of displacing consumption of diet beverages; the study's aim is to compare water and diet beverages, not SSB |
| Malbon 2012 | Behavioural intervention |
| Mantzari 2017 | Follow‐up too short (4 weeks) |
| Marcus 2009 | Ineligible outcomes (data on SSB is available only for post‐intervention, not for baseline) |
| Maupome 2010 | Indirect environmental change; EPOC criteria not fulfilled (cluster‐NRCT with 1 control site only) |
| McDarby 2018 | Follow‐up too short (less than 1 day) |
| McGoldrick 2006 | Ineligible study design (no intervention study) |
| Mendez 2017 | Ineligible study design (longitudinal association study) |
| Morley 2018 | Behavioural intervention focused on SSB |
| Morris 2016 | Behavioural intervention |
| Mozaffarian 2010 | Ineligible study design (UBA); intervention not focused on SSB |
| Namba 2013 | Ineligible outcomes (items offered is the only outcome measure, no sales or consumption data) |
| Nanney 2016 | Ineligible study design (cross‐sectional study) |
| Nau 2018 | Ineligible study design (modelling study) |
| Neumark‐Sztainer 2010 | Behavioural intervention not focused on SSB |
| Nezami 2018 | Behavioural intervention focused on SSB |
| Nollen 2014 | Behavioural intervention partly focused on SSB |
| Nyström 2017 | Behavioural intervention |
| Okuno 2010 | Clinical trial in which 1 group of participants received SSB |
| Olvera 2010 | Behavioural intervention not focused on SSB |
| Ortega 2016 | Ineligible study design (UBA study) |
| Ostbye 2012 | Behavioural intervention not focused on SSB; no direct environmental intervention component |
| Patel 2011 | Follow‐up too short (7 weeks); ineligible outcomes (water consumption only) |
| Patel 2016 | ineligible outcomes (water intake only) |
| Pbert 2013 | Behavioural intervention not focused on SSB |
| Peters 2016b | In this study, participants received water with the aim of displacing consumption of diet beverages; the study's aim is to compare water and diet beverages, not SSB |
| Pinket 2016 | Indirect environmental change intervention |
| Policastro 2017 | Follow‐up too short (7 weeks) |
| Raynor 2012 | Behavioural intervention not focused on SSB |
| Reid 2014 | Clinical trial in which 1 group of participants received SSB; Follow‐up too short (1 month) |
| Reinhold 2015 | Behavioural intervention focused on SSB |
| Roberto 2016 | Ineligible study design (online survey) |
| Rodriguez‐Cano 2015 | Behavioural intervention not focused on SSB |
| Rogers 2013 | Ineligible study design (UBA); intervention not focused on SSB |
| Rogus 2017 | EPOC criteria not fulfilled (CBA study with 1 intervention and control site only) |
| Rosario 2013 | Behavioural intervention partly focused on SSB |
| Rosenkranz 2010 | No direct environmental intervention component |
| Rosi 2017 | Indirect environmental change; EPOC criteria not fulfilled (cluster‐NRCT with 1 control site only) |
| Sacks 2011 | Follow‐up too short (10 weeks) |
| Safdie 2013 | No beverage‐specific outcome data available |
| Sanchez‐Vaznaugh 2010 | Intervention not focused on beverages, no beverage‐specific outcome data reported |
| Sanchez‐Vaznaugh 2015 | Intervention not focused on beverages, no beverage‐specific outcome data reported |
| Schroeder 2015 | Behavioural intervention partly focused on SSB |
| Seah 2018 | Follow‐up too short (11 weeks) |
| Shahril 2013 | Behavioural intervention not focused on SSB; follow‐up too short (10 weeks) |
| Shamah 2012 | Indirect environmental change intervention |
| Shuster 1992 | Behavioural intervention focused on SSB |
| Sichieri 2009 | Behavioural intervention focused on SSB |
| Sichieri 2013 | Behavioural intervention focused on SSB |
| Siega‐Riz 2011 | Indirect environmental change intervention |
| Simon 2013 | Ineligible study design (not an intervention study) |
| Singh 2009 | Indirect environmental change intervention |
| Singhal 2010 | Behavioural intervention partly focused on SSB |
| Skouteris 2016 | Behavioural intervention |
| Smit 2016 | Behavioural intervention focused on water |
| Smith 2014 | Follow‐up too short (1 month) |
| Sobko 2011 | Ineligible outcomes (data on SSB were collected post‐intervention only) |
| Song 2009 | Indirect environmental change intervention |
| Stettler 2014 | Behavioural intervention focused on SSB |
| Steyn 2015 | Indirect environmental change intervention |
| Storey 2010 | Ineligible study design (UBA study); no clearly‐defined intervention |
| Story 2012 | Indirect environmental change intervention |
| Strauss 2011 | Indirect environmental change intervention |
| Strippel 2010 | Behavioural intervention |
| Sturm 2013 | Intervention not focused on beverages, no beverage‐specific outcome data reported |
| Sutherland 2010 | Ineligible study design (UBA study) |
| Swinburn 2014 | Indirect environmental change intervention |
| Taljaard 2013 | Clinical trial in which 1 group of participants received SSB |
| Taylor 2007 | Behavioural intervention partly focused on SSB |
| Teufel 1998 | Ineligible study design (UBA); behavioural intervention partly focused on SSB |
| Thiele 1989 | Behavioural intervention focused on SSB |
| Thompson 2008 | Behavioural intervention partly focused on SSB |
| Thorndike 2012 | EPOC criteria not fulfilled (CBA study with 1 intervention and 2 control sites) |
| Thorndike 2016 | Ineligible outcomes (purchases of healthy beverages only) |
| Thow 2015 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before and after the intervention) |
| Toxqui 2016 | Follow‐up too short (8 weeks) |
| Trinies 2016 | Ineligible outcomes |
| Tucker 2011 | Behavioural intervention partly focused on SSB |
| Tyhurst 2015 | Behavioural intervention focused on SSB |
| Utter 2011 | Indirect environmental change intervention |
| Van Grieken 2014 | Behavioural intervention partly focused on SSB |
| Van Grieken 2017 | Behavioural intervention |
| Van Walleghen 2007 | Ineligible setting (research laboratory); Follow‐up too short (less than 1 day) |
| VanEpps 2016 | Ineligible study design (online survey) |
| Vargas 2011 | Behavioural intervention partly focused on SSB |
| Veitch 2011 | Indirect environmental change intervention |
| Velazquez 2014 | Ineligible study design (UBA study) |
| Verbestel 2013 | Behavioural intervention |
| Vermeer 2010 | Ineligible outcomes (purchase intentions only, not actual purchases or consumption); follow‐up too short (less than 1 day) |
| Vien 2017 | Ineligible setting (research laboratory); follow‐up too short (less than 1 day); clinical trial in which 1 group of participants received SSB |
| Vitolo 2012 | Behavioural intervention partly focused on SSB |
| Vázquez‐Durán 2016 | Behavioural intervention focused on SSB |
| Wang 2006 | Indirect environmental change intervention |
| Wang 2016 | Behavioural intervention focused on SSB |
| Wansink 2014 | Ineligible study design (UBA study) |
| Ward 2008 | Indirect environmental change intervention |
| Wardle 2000 | ineligible study design (UBA study); ineligible setting (research laboratory) |
| Watt 2009 | Behavioural intervention |
| Weber‐Gasparoni 2013 | Behavioural intervention |
| Wennhall 2005 | Behavioural intervention |
| Wescott 2012 | EPOC criteria not fulfilled (ITS study with fewer than 3 data points before the intervention) |
| Whatley Blum 2011 | Ineligible outcomes (availability of SSB, not direct or indirect measures of SSB intake); ineligible study design (UBA study) |
| Williamson 2013 | Indirect environmental change intervention |
| Willis 2014 | Behavioural intervention |
| Wilson 2015 | Ineligible study design (UBA study) |
| Winett 1999 | Behavioural intervention partly focused on SSB |
| Wing 2015 | Behavioural intervention partly focused on SSB |
| Wofford 2013 | Ineligible study design (UBA); behavioural intervention partly focused on SSB |
| Wolfenden 2015 | Ineligible outcomes (water intake only) |
| Wong 2017 | Behavioural intervention focused on SSB |
| Woodward‐Lopez 2010 | Ineligible study design (UBA); intervention partly focused on SSB |
| Wordell 2012 | In the 6 schools in this study, SSB had been eliminated 3 years prior to the start of the intervention, in which the ban on SSB was extended to 100% fruit juice and diet beverages. The study evaluates the additional effects of banning 100% fruit juice and diet beverages. As none of the 2 falls under our definition of SSB this study does not fulfil the first inclusion criterion |
| Wright 2016 | Ineligible outcomes (water intake only) |
| Xu 2015 | Indirect environmental change intervention |
| Yildirim 2013 | No direct environmental intervention component |
| Yon 2014 | Ineligible study design (UBA study) |
| Zizzo 2016 | Ineligible setting (virtual supermarket) |
| Zoellner 2013 | Behavioural intervention focused on SSB |
| Zoellner 2016 | Behavioural intervention focused on SSB |
CBA: controlled before‐after; ITS: interrupted time series; UBA: uncontrolled before‐after study
Characteristics of ongoing studies [ordered by study ID]
Ayala 2016.
| Trial name or title | A restaurant‐based intervention to promote sales of healthy children’s menu items: the Kids’ Choice Restaurant Program cluster randomized trial |
| Methods | RCT, 8 restaurants |
| Participants | Restaurant customers |
| Interventions | Improved availability of healthier beverages in restaurants |
| Outcomes | Food and beverage sales |
| Starting date | 2013 |
| Contact information | Guadalupe X. Ayala, San Diego State University, ayala@mail.sdsu.edu |
| Completion date | 2015 |
| Notes | None |
Kajons 2018.
| Trial name or title | Thirsty? Choose Water! The effect of behavioural interventions and water stations on water consumption in secondary schools: A two‐by‐two factorial randomised controlled trial. |
| Methods | RCT, 8100 participants, 60 schools |
| Participants | Secondary school students |
| Interventions | Improved availability of water at schools |
| Outcomes | Water and SSB intake |
| Starting date | 2017 |
| Contact information | Mrs Niki Kajons, Health Promotion Service, Central Coast Local Health District, New South Wales, Australia, Nicole.Kajons@health.nsw.gov.au |
| Completion date | 2019 |
| Notes | None |
NCT02877823.
| Trial name or title | A community‐based, family navigator intervention to improve cardiometabolic health of Medicaid‐insured youth identified through an antipsychotic medication preauthorization program |
| Methods | RCT, 360 participants |
| Participants | Children and teenagers |
| Interventions | Improved availability of low‐calorie beverages in the home environment |
| Outcomes | BMI z‐score, SSB consumption (among others) |
| Starting date | 2016 |
| Contact information | Gloria Reeves, University of Maryland, College Park, US, greeves@som.umaryland.edu |
| Completion date | 2020 |
| Notes | None |
NCT02914821.
| Trial name or title | Do taxes reduce the purchasing of soda? |
| Methods | NRCT, 50 participants |
| Participants | Adult cafeteria customers |
| Interventions | Price increases on SSB |
| Outcomes | SSB sales, beverage calories purchases, unsweetened beverage sales, changes in types of beverages purchased |
| Starting date | 2016 |
| Contact information | Grant Donnelly, Marketing Department, Harvard University, donnelly.177@osu.edu |
| Completion date | 2018 |
| Notes | None |
NCT02996422.
| Trial name or title | Appalachians Together Restoring the Eating Environment (Appal‐TREE): advancing sustainable CBPR interventions to improve healthy diet in rural Appalachian children |
| Methods | NRCT, 1360 participants |
| Participants | Middle‐ and high‐school students and their parents |
| Interventions | Improved access to drinking water at school |
| Outcomes | Beverage consumption, beverage sales (among others) |
| Starting date | 2016 |
| Contact information | Mark Swanson, University of Kentucky, mark.swanson@uky.edu |
| Completion date | 2021 |
| Notes | None |
NCT0306927.
| Trial name or title | Home intervention for reducing sugary drinks and obesity in Hispanic women‐infants |
| Methods | RCT, 214 participants |
| Participants | Mother‐child dyads |
| Interventions | Improved availability of low‐calorie beverages in the home environment |
| Outcomes | Maternal BMI, infant weight‐for‐length |
| Starting date | 2017 |
| Contact information | Michael I. Goran, University of Southern California, goran@usc.edu |
| Completion date | 2020 |
| Notes | None |
NCT03069274.
| Trial name or title | Impact of a randomized school‐based intervention on sugar‐sweetened beverage intake substitution by water to prevent excessive weight in Mexican scholars |
| Methods | RCT, 314 participants |
| Participants | Elementary school students |
| Interventions | Improved access to drinking water at school |
| Outcomes | Change in drinking habits |
| Starting date | 2015 |
| Contact information | Lilia Castillo Martinez, Medical Rearch Investigator, Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran, lilia.castillom@incmnsz.mx |
| Completion date | 2016 |
| Notes | None |
NCT03181971.
| Trial name or title | The impact of the school water access on child food and beverage intake and obesity |
| Methods | RCT, 1742 participants, 26 schools |
| Participants | Elementary school children |
| Interventions | Improved access to drinking water at school |
| Outcomes | BMI z‐score, total caloric intake |
| Starting date | 2016 |
| Contact information | Anisha Patel, University of California, San Francisco, US, Anisha.Patel@ucsf.edu |
| Completion date | 2021 |
| Notes | None |
NCT03431051.
| Trial name or title | The impact of workplace food and beverage choices on health and wellness |
| Methods | NRCT, 700 participants |
| Participants | Adults hospital employees |
| Interventions | Decreased availability of SSB at workplaces |
| Outcomes | Abdominal adiposity, BMI, SSB intake |
| Starting date | 2017 |
| Contact information | Jamey Schmidt, Director, Clinical Research, California Pacific Medical Center Research Institute, SchmidJ@cpmcri.org |
| Completion date | 2021 |
| Notes | None |
NCT03518151.
| Trial name or title | Women's Responses to Adjusted Product Placement and its Effects on Diet ‐ 1 (WRAPPED1) |
| Methods | NRCT, 150 participants |
| Participants | Adult female supermarket customers |
| Interventions | Removal of SSB from supermarket checkout coolers and replacement with bottled water |
| Outcomes | Dietary quality score (among others) |
| Starting date | 2016 |
| Contact information | None provided |
| Completion date | 2017 |
| Notes | We failed to contact authors of this study due to a lack of contact information in the trial register entry |
Oi 2018.
| Trial name or title | A cluster randomised controlled trial to evaluate the efficacy of a secondary school intervention in reducing sugar‐sweetened beverage consumption |
| Methods | RCT, 1260 participants |
| Participants | Secondary school students |
| Interventions | Reduced availability of SSB and improved availability of water at schools |
| Outcomes | SSB intake, energy intake from SSB, BMI (among others) |
| Starting date | 2017 |
| Contact information | Ms Rachel Sutherland, Hunter New England Population Health, Wallsend, Australia, Rachel.Sutherland@hnehealth.nsw.gov.au |
| Completion date | 2018 |
| Notes | None |
BMI: body mass index
Differences between protocol and review
Objectives
We reworded the Objectives in line with Cochrane guidelines recommending that all prespecified primary outcomes are mentioned in the Objectives. We therefore now mention that the review also aims to assess effects on the consumption of sugar‐sweetened milk. We also reworded the Objectives to make clear that the review also includes interventions that were not exclusively and explicitly targeted at SSB, but may affect SSB consumption.
Criteria for considering studies for this review
We applied all inclusion and exclusion criteria prespecified in the published protocol. However, during the screening process we found that for a number of these further clarification and specification were needed to decide on ambiguous cases. We provide relevant details in the following sections.
Multicomponent interventions
In our published protocol, we stated that we would exclude interventions that combine components to reduce the consumption of SSB with broader components to improve diet or increase physical activity, as it would be difficult to attribute effects to the environmental or policy intervention of interest. In conducting our review, we interpreted this criterion as applying only to multicomponent interventions for which the description of the intervention, the way it was implemented, or the reported outcome data do not allow a clear attribution of effects. By contrast, we did include studies on multicomponent interventions reporting direct or indirect measures of SSB intake.
Clinical trials
In our published protocol we specified that we would exclude studies in which participants are administered SSB or alternatives to SSB as part of clinical trials on the physiological effects of SSB consumption, as these studies provide only limited evidence on the feasibility and effectiveness of public health interventions aimed at reducing SSB intake among free‐living individuals outside controlled research settings. We anticipated in our protocol that this may include studies in which participants consume predefined amounts of beverages under supervision, or in which bottled beverages are delivered for free to the homes of participants with additional measures taken to ensure and monitor compliance. In the light of the studies we found we interpreted this criterion as follows: we excluded all studies in which one group of participants received SSB as part of the intervention, regardless of the mode of implementation. Furtherrmore, we excluded feeding studies, i.e. studies in which predefined amounts of beverages (SSB or any alternative to SSB) are consumed by participants in clinical or research settings, such as study centres or research laboratories. By contrast, we included studies in which low‐calorie alternatives to SSB (but not SSB) were delivered to the homes of participants with the aim of displacing baseline SSB consumption by changing the home environment. We decided to include this set of studies after finding three studies (Anand 2007; Ebbeling 2012; Hernández‐Cordero 2014) which rely on home delivery of water and other low‐calorie beverages, while being framed as community‐based or home‐based public health interventions. In particular in contexts with a high prevalence of obesity and related diseases, and a high baseline consumption of SSB, improved access to drinking water and other low‐calorie beverages at the household level may indeed be a viable public health strategy, or at least not one which can be dismissed outright without closer consideration. In our interpretation of results we paid special attention to the resource‐intensity of these interventions, their public health implications and their potential applicability at a population level, including relevant limitations.
Interventions aiming at indirect environmental change
In our published protocol, we specified that we would include environmental interventions, including environmental interventions with behavioural co‐interventions, while we would exclude purely behavioural interventions. We defined environmental interventions as interventions which target the environment, physical, socio‐economic, socio‐cultural or legal, in which individuals make food and beverage choices, aiming to alter this environment in a permanent way. By contrast, we defined behavioural interventions as interventions targeting the dietary preferences, knowledge, attitudes, motivations, skills and abilities of individuals, as well as their subjective perception of social norms on food and beverage consumption.
During our screening process we found a number of studies which targeted the preferences, knowledge, attitudes, motivations, skills and abilities of individuals, with the aim of enabling these individuals to implement environmental changes in their specific settings. This included, among others, skill‐building and counselling interventions targeting school staff, aiming to enable them to change the school environment in order to change the behaviours of students. In these studies, we considered the environmental change to be an outcome, rather than a part of the intervention itself. Based on the definitions used in our protocol, we therefore excluded these studies. However, we note that some of these studies can be considered as effectiveness trials, or as implementation studies aiming to explore the ways in which the interventions examined in our review can be scaled up and implemented at a population level. They therefore provide potentially valuable evidence for policy‐makers.
Cluster trials with fewer than two intervention and control sites
Following Cochrane EPOC guidance we specified in our published protocol that we would include only cluster‐RCTs, NRCTs and CBA studies with at least two intervention and two control sites.
There are several possible definitions of what constitutes an intervention and a control site. More specifically, the term may refer either to the level of implementation, or to the level of allocation. For the purposes of our review, we chose the first option.
This distinction matters for several studies included in our review, such as Muckelbauer 2009. This is a study in which 32 schools were randomly selected among eligible primary schools located in two cities within the same urban agglomeration (the German cities of Dortmund and Essen, both in the Ruhr area). Allocation to the intervention and control group was non‐random, using a geographic allocation criterion: schools in Dortmund were allocated to the intervention group, and schools in Essen to the control group. Intervention schools received water fountains, and control schools no intervention. Following our definition of the term intervention and control site as referring to the level of implementation (rather than the level of allocation) we considered schools (rather than cities) to be the intervention and control sites, and included the study. Similar issues arose in the case of Cradock 2011, Elbel 2013 and Sturm 2015.
Our rationale for choosing this interpretation of the term 'intervention and control site' is the following: any non‐random allocation procedure can be a source of bias, and some non‐random allocation procedures may carry a higher risk of bias than others. However, allocation procedures using geographical criteria, as in the example above, are not necessarily more prone to bias than other commonly‐used non‐random allocation procedures, such as allocation based on pre‐existing co‐operation with the investigators, as was done in Ermetici 2016. The risk of bias arising from non‐random allocation procedures is taken into account in the 'Risk of bias' assessment done for all included studies. Singling out one specific non‐random allocation procedure, which is not necessarily more prone to bias than others, as a reason to exclude the respective studies altogether from a review that includes NRCTs does not seem justified in light of the intention of the relevant EPOC guidance.
Types of studies
We added the specification that we included both studies that collected data on individual participants, and studies based on data not linked to individual participants, such as sales or transaction data.
Types of interventions
In our published protocol we stated that we would consider interventions that are intended to reduce the consumption of SSB and sugar‐sweetened milk, or their adverse effects on health, or to increase the consumption of low‐calorie alternatives to SSB, implemented at an environmental level. In the review, we reworded this sentence to clarify that we included studies that have potential effects on the consumption of SSB or sugar‐sweetened milk, regardless of the intentions of those planning, deciding upon or implementing the intervention. We also removed the words ‘or to increase the consumption of low‐calorie alternatives to SSB’ from the sentence, as the consumption of low‐calorie alternatives to SSB was not one of the prespecified primary outcomes of the review.
Types of outcome measures
In our protocol, we listed ‘diet‐related anthropometric measures‘ and ‘diet‐related health outcomes (other than body weight)’ as two separate primary outcomes. For simplicity and clarity, we combined these two outcome categories and formed a new one, which we called ‘diet‐related anthropometric measures and health outcomes’.
In our protocol, we did not provide a justification for our decision to use the reporting of primary outcomes as an inclusion criterion. We added information on this at the review stage.
In our protocol, we had not listed the consumption of beverages other than SSB as a secondary outcome. By contrast, the wording of the review’s Objectives, as presented in the protocol, implied that we would assess effects on consumption levels of both SSB and alternatives to SSB. We therefore added ‘consumption of beverages other than SSB’ to the list of secondary outcomes.
In our protocol, we specified that for reformulation interventions that report effects on SSB consumption levels, at least one additional primary outcome (i.e. either diet‐related anthropometric measures and health outcomes, or any adverse outcome or unintended consequence) would be needed to justify inclusion. We dropped this specification from the review, as we did not find any study for which this was of relevance.
Search methods for identification of studies
In our protocol, we specified that for eligible studies in languages other than English, French, Spanish, Italian or German we would attempt to arrange for translation. We dropped this from the review as we did not find any eligible studies in languages other than English.
In our protocol, we stated that we would search the website of the U.S. National Institutes of Health. We dropped this, as we did not perform such a search.
We added the specification that ScieELO, Google Scholar, Open Grey and Bibliomap were included in our original search, but not in our 2018 search update, as these databases contributed relatively few studies which we did not also identify through the remaining databases, while proving relatively time‐consuming to search.
Assessment of risk of bias in included studies
We reworded the domains of the EPOC‐adapted Cochrane 'Risk of bias' tool, using the wording used in the most recent edition of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017a). We also reorganised the presentation of the domains to clarify that for controlled ITS studies we applied both the domains for controlled study designs and the domains for ITS studies.
In the protocol we specified that if we found relevant conflicts of interest we would conduct sensitivity analyses. We dropped this specification, given the small number of studies which we could include in meta‐analysis.
Measures of treatment effect
In our protocol, we stated that we would use the standardised mean difference (SMD) as the preferred measure of treatment effect for continuous outcome measures. Given the small number of studies within each intervention category, and the difficulties of interpreting the SMD, we decided to use the mean difference (MD) instead.
In our protocol, we stated that we would report energy in both joules and calories. We decided to report energy in calories only, to improve readability.
In our protocol, we did not specify how to proceed in cases where studies report several alternative measures for the same group of outcomes. We added information on the procedures applied in such cases to the subsection on Measures of treatment effect in the Methods section, clearly stating that we added this information after the publication of the protocol.
Definition of minimal patient‐relevant differences
In our protocol, we did not define minimal patient‐relevant differences, i.e. thresholds for the clinical or public health relevance of reported effect sizes. We have added a subsection on this issue to the Methods section.
Unit of analysis issues
In our protocol, we stated that where possible, we would re‐analyse data for cluster trials that have not taken clustering into account in their analysis. We included three studies (Da Costa 2014; Van de Gaar 2014; Whatley Blum 2008) which used a cluster design but did not report if clustering was taken into account in the analyses. In view of difficulties with obtaining the required data and in order not to delay the publication of the review, we decided not to attempt a re‐analysis. Furthermore, we specified in our protocol that individually‐randomised controlled trials and cluster‐RCTs would be combined in the same meta‐analyses or harvest plots, but would be clearly identified. We dropped this specification from the review as we did not identify any intervention category with both cluster‐ and individually‐randomised trials.
Dealing with missing data
In our protocol we stated that in cases in which missing data on study characteristics or outcome measures precluded study inclusion or limited the use of a study at further stages of the review, we would contact the corresponding author. We have added further information on the criteria which we used to decide if study authors should be contacted or not.
We also specified in the protocol that we would examine the effect of including results from studies without intention‐to‐treat analysis by performing a sensitivity analysis for high or unclear risks of bias in the selective outcome reporting domain. We dropped this specification, given the small number of studies which we could include in meta‐analysis.
Data synthesis
We specified in our protocol that we would run separate meta‐analyses for (i) RCTs, NRCTs and cluster‐RCTs, provided these had been adjusted for clustering, (ii) ITS and RMS, and (iii) CBA studies. We dropped this specification from our review, as all studies which could be included in meta‐analysis were individually‐randomised RCTs.
We stated in our protocol that we would use harvest plots for a graphical representation of results. We subsequently questioned the added value of harvest plots in the presence of detailed 'Summary of findings' tables, and decided not to produce such plots. We did, however, create an effect direction plot (Thomson 2013) to present the direction of reported effects on direct and indirect measures of SSB intake in graphical form.
Classification of interventions with the NOURISHING framework
We used the NOURISHING framework to classify interventions, as indicated in our protocol. In addition to the seven environmental intervention areas covered by the NOURISHING framework we introduced an eighth category for interventions implemented in the home environment. These interventions fulfilled the eligibility criteria for inclusion in our review, but could not be readily assigned to one of the intervention areas of the NOURISHING framework.
Classification of interventions as policy‐ or setting‐based interventions
In our published protocol, we specified that we would classify interventions only as policy‐level when they were implemented at the level of a geographically‐defined political or administrative unit, and when the original studies reporting on them evaluated their effects at the same level (e.g. by analysing the effects of a national school nutrition policy on the SSB consumption of school children in that country). We dropped the second part of this specification, as we found, in the light of the included studies, that the level of implementation of an intervention is of greater importance for the classification than the level of evaluation.
Subgroup analysis and investigation of heterogeneity
In our protocol we stated that we would consider performing separate meta‐analyses, or creating separate harvest plots, for studies assessing interventions implemented: at the policy or at the setting level; with or without behavioural co‐interventions; targeted at SSB, sugar‐sweetened milk, beverages with NNS or at beverages without added sweeteners; implemented in high‐, middle‐ or low‐income countries; targeted at the general population or at disadvantaged populations. We dropped this specification, given the small number of studies which we could include in meta‐analysis, as well as our decision not to use harvest plots.
For one intervention type and one outcome measure (effects of price increases on SSB on SSB sales) we conducted a post hoc subgroup analysis (not prespecified in our protocol) according to the level of the price increase, i.e. the intensity of the intervention. We did this in order to assess whether a dose‐response gradient existed.
Sensitivity analysis
In our protocol we specified that we would examine how the time frame of the outcome measurement, the unit of analysis, the risk of bias and the existence of relevant conflicts of interest affect results by conducting separate meta‐analyses or by creating separate harvest plots. We further specified that we would consider conducting an intra‐cluster correlation value sensitivity analysis for cluster trials. We dropped this specification given the small number of studies which we could include in meta‐analysis, as well as our decision not to use harvest plots.
Certainty of evidence
Following updated GRADE guidance (Hultcrantz 2017), we replaced the phrase ‘quality of evidence’ with ‘certainty of evidence’, and revised the relevant definitions.
In our protocol, we stated that we would use GRADE for rating the body of evidence for all critical and important outcomes, as defined with the help of our Review Advisory Group. We changed this, and now specify that we applied GRADE to all primary outcomes only. We did not apply GRADE to target group and stakeholder perceptions, nor to measures of economic and financial sustainability and viability (unless classified as adverse outcomes). The reason is that for these outcomes, most included studies reported only qualitative or anecdotal evidence, which limited our ability to apply GRADE.
We added the specification that our assessment of the certainty of effect estimates refers to the existence and the direction of effects, and not to the exact effect sizes reported by individual studies. We also added the specification that we considered cluster‐RCTs in which the number of randomised units was four or fewer as equivalent to NRCTs.
Wording
In our protocol, we used the term ‘beverages with NNS’ to denote beverages sweetened with non‐nutritive sweeteners. In our review, we decided to use the term ‘diet beverages’ instead, as this term is more commonly used in the literature and more easily understood by the more general readership.
Contributions of authors
PvP drafted the protocol with support from JMS, JB, LKB, LMP, SP, CH, HH and ER. PvP developed the search strategy and conducted the searches. PvP, JMS, JB, LKB, LMP and SP selected studies, extracted data, and assessed the risks of bias of included studies. PvP entered data into Review Manager 5, conducted the analyses, graded the evidence, and drafted the manuscript. JMS double‐checked data entry, data analysis, and evidence grading. ER provided methodological support on all stages of the review process. All authors contributed to the interpretation of results, read and commented on drafts, and approved the final version.
Sources of support
Internal sources
-
LMU University of Munich, Germany.
Provided support for PvP, JMS, JB, LKB, LMP, SP, and ER.
-
Technical University Munich, Germany.
Provided support for PvP, CH, and HH.
-
University College London, UK.
Provided support for LKB.
-
Bavarian Office for Health and Food Safety, Germany.
Provided support for JMS.
External sources
No sources of support supplied
Declarations of interest
PvP, JMS, JB, LKB, LMP, SP: None known.
CH is a member of the scientific advisory board of 4sigma, a consultancy working primarily for health insurance companies. She has been involved in the preparation of a systematic review on Associations between single nucleotide polymorphisms and macronutrient intake (PROSPERO: CRD42015025738), partly funded by an institutional grant from the consumer products company Amway GmbH.
HH has received honoraria for membership on scientific advisory boards of Weight Watchers, NovoNordisk and Boehringer Ingelheim. His institution has received grants from Riemser Pharma, Amway GmbH and Certmedica, a producer of slimming products. HH has received honoraria for membership on scientific advisory boards of Nestle and Danone, providing advice on recommendations regarding the nutritional content of breakfast meals and dairy products.
ER: None known.
New
References
References to studies included in this review
Albala 2008 {published data only}
- Albala C, Ebbeling CB, Cifuentes M, Lera L, Bustos N, Ludwig DS. Effects of replacing the habitual consumption of sugar‐sweetened beverages with milk in Chilean children. American Journal of Clinical Nutrition 2008;88(3):605‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anand 2007 {published data only}
- Anand SS, Davis AD, Ahmed R, Jacobs R, Xie C, Hill A, et al. A family‐based intervention to promote healthy lifestyles in an aboriginal community in Canada. Canadian Journal of Public Health 2007;98(6):447‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2016 {published data only}
- Baker P, Friel S, Schram A, Labonte R. Trade and investment liberalization, food systems change and highly processed food consumption: A natural experiment contrasting the soft‐drink markets of Peru and Bolivia. Globalization and Health 2016;12(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ball 2015 {published data only}
- Ball K, McNaughton SA, Ha ND, Gold L, Ni Mhurchu C, Abbott G, et al. Influence of price discounts and skill‐building strategies on purchase and consumption of healthy food and beverages: outcomes of the Supermarket Healthy Eating for Life randomized controlled trial. American Journal of Clinical Nutrition 2015;101(5):1055‐64. [DOI] [PubMed] [Google Scholar]
- Ball K, McNaughton SA, Ni Mhurchu C, Andrianopoulos N, Inglis V, McNeilly B, et al. Supermarket Healthy Eating for Life (SHELf): protocol of a randomised controlled trial promoting healthy food and beverage consumption through price reduction and skill‐building strategies. BMC Public Health 2011;11(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olstad DL, Ball K, Abbott G, McNaughton SA, Ha ND, Ni Mhurchu C, et al. A process evaluation of the Supermarket Healthy Eating for Life (SHELf) randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauhoff 2014 cohort {published data only (unpublished sought but not used)}
- Bauhoff S. The effect of school district nutrition policies on dietary intake and overweight: a synthetic control approach. Economics and Human Biology 2014;12:45‐55. [DOI] [PubMed] [Google Scholar]
Bauhoff 2014 crosssectional {published data only (unpublished sought but not used)}
- Bauhoff S. The effect of school district nutrition policies on dietary intake and overweight: a synthetic control approach. Economics and Human Biology 2014;12:45‐55. [DOI] [PubMed] [Google Scholar]
Blake 2018 {published data only}
- Blake MR, Peeters A, Lancsar E, Boelsen‐Robinson T, Corben K, Stevenson CE, et al. Retailer‐led sugar‐sweetened beverage price increase reduces purchases in a hospital convenience store in Melbourne, Australia: a mixed methods evaluation. Journal of the Academy of Nutrition and Dietetics 2018;118(6):1027‐36. [DOI] [PubMed] [Google Scholar]
Boelsen‐Robinson 2017 {published data only}
- Boelsen‐Robinson T, Backholer K, Corben K, Blake MR, Palermo C, Peeters A. The effect of a change to healthy vending in a major Australian health service on sales of healthy and unhealthy food and beverages. Appetite 2017;114:73‐81. [DOI] [PubMed] [Google Scholar]
Bollinger 2011 {published data only}
- Bollinger B, Leslie P, Sorensen A. Calorie posting in chain restaurants. American Economic Journal: Economic Policy 2011;3(1):91‐128. [Google Scholar]
Breeze 2018 {published data only}
- Breeze P, Womack R, Pryce R, Brennan A, Goyder E. The impact of a local sugar sweetened beverage health promotion and price increase on sales in public leisure centre facilities. PLOS One 2018;13(5):e0194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brimblecombe 2017 {published data only}
- Brimblecombe J, Ferguson M, Chatfield MD, Liberato SC, Gunther A, Ball K, et al. Effect of a price discount and consumer education strategy on food and beverage purchases in remote Indigenous Australia: a stepped‐wedge randomised controlled trial. Lancet Public Health 2017;2(2):e82‐95. [DOI] [PubMed] [Google Scholar]
- Brimblecombe J, Ferguson M, Liberato SC, Ball K, Moodie ML, Magnus A, et al. Stores Healthy Options Project in Remote Indigenous Communities (SHOP@RIC): a protocol of a randomised trial promoting healthy food and beverage purchases through price discounts and in‐store nutrition education. BMC Public Health 2013;13:744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capewell S, Lloyd‐Williams F. Promotion of healthy food and beverage purchases: are subsidies and consumer education sufficient?. Lancet Public Health 2018;2(2):e59‐60. [DOI] [PubMed] [Google Scholar]
Cawley 2015 {published data only}
- Blumberg FB, Broihier K, Duncan A, Fitzpatrick K, Fisher L, Nobel J. Regarding the paper ‘The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods’ by Cawley et al. Public Health Nutrition 2014;18(12):2283‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Sweeney MJ, Sobal J, Just DR, Kaiser HM, Schulze WD, et al. Authors’ response: Regarding the paper ‘The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods’ by Cawley et al. Public Health Nutrition 2014;18(12):2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Sweeney MJ, Sobal J, Just DR, Kaiser HM, Schulze WD, et al. The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods. Public Health Nutrition 2015;18(1):8‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2015 {published data only}
- Cohen JF, Richardson SA, Cluggish SA, Parker E, Catalano PJ, Rimm EB. Effects of choice architecture and chef‐enhanced meals on the selection and consumption of healthier school foods: a randomized clinical trial. JAMA Pediatrics 2015;169(5):431‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JF, Smit LA, Parker E, Austin SB, Frazier AL, Economos CD, et al. Long‐term impact of a chef on school lunch consumption: findings from a 2‐year pilot study in boston middle schools. Journal of the Academy of Nutrition and Dietetics 2012;112(6):927‐33. [DOI] [PubMed] [Google Scholar]
- Patel MS, Volpp KG. Nudging students toward healthier food choices—applying insights from behavioral economics. JAMA Pediatrics 2015;169(5):425‐6. [DOI] [PubMed] [Google Scholar]
Collins 2016 SNAP {published data only}
- Collins AM, Briefel R, Klerman JA, Wolf A, Rowe G, Logan C, et al. Summer Electronic Benefit Transfer for Children (SEBTC) Demonstration: Summary Report. U.S. Department of Agriculture 2016. [clinicaltrials.gov/ct2/show/NCT02877147]
- Collins AM, Klerman JA. Improving nutrition by increasing Supplemental Nutrition Assistance Program benefits. American Journal of Preventive Medicine 2017;52(2 Supplement 2):S179‐85. [DOI] [PubMed] [Google Scholar]
- Klerman JA, Collins AM, Olsho LE. Improving nutrition by limiting choice in the Supplemental Nutrition Assistance Program. American Journal of Preventive Medicine 2017;52(2 Supplement 2):S171‐8. [DOI] [PubMed] [Google Scholar]
- Schwartz MB. Moving beyond the debate over restricting sugary drinks in the Supplemental Nutrition Assistance Program. American Journal of Preventive Medicine 2017;52(2 Supplement 2):S199‐205. [DOI] [PubMed] [Google Scholar]
Collins 2016 WIC {published data only}
- Collins AM, Briefel R, Klerman JA, Wolf A, Rowe G, Logan C, et al. Summer Electronic Benefit Transfer for Children (SEBTC) Demonstration: Summary Report. U.S. Department of Agriculture 2016. [clinicaltrials.gov/ct2/show/NCT02877147]
Cornelsen 2017 {published data only}
- Cornelsen L, Mytton OT, Adams J, Gasparrini A, Iskander D, Knai C, et al. Change in non‐alcoholic beverage sales following a 10‐pence levy on sugar‐sweetened beverages within a national chain of restaurants in the UK: interrupted time series analysis of a natural experiment. Journal of Epidemiology and Community Health 2017;71(11):1107‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cradock 2011 {published data only}
- Cradock AL, McHugh A, Mont‐Ferguson H, Grant L, Barrett JL, Wang YC, et al. Effect of school district policy change on consumption of sugar‐sweetened beverages among high school students, Boston, Massachusetts, 2004‐2006. Preventing Chronic Disease 2011;8(4):A74. [PMC free article] [PubMed] [Google Scholar]
Da Costa 2014 {published data only}
- Costa FF, Assis MA, Gonzalez‐Chica D, Bernardo C, Barros MV, Nahas MV, et al. Effect of school‐based intervention on diet in high school students. Revista Brasileira de Cineantropometria & Desempenho Humano 2014;16:36‐45. [Google Scholar]
- Nahas MV, Barros MV, Assis MA, Hallal PC, Florindo AA, Konrad L. Methods and participant characteristics of a randomized intervention to promote physical activity and healthy eating among Brazilian high school students: The Saude na Boa project. Journal of Physical Activity and Health 2009;6(2):153‐62. [DOI] [PubMed] [Google Scholar]
- Silva KS, Barros MV, Barbosa FV, Garcia LM, Wanderley JR, Beck CC, et al. Implementation of the “Saúde na Boa” intervention: process evaluation and characteristics of participants and dropouts. 2014 2014;16:12. [Google Scholar]
Ebbeling 2006 {published data only}
- Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar‐sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics 2006;117(3):673‐80. [DOI] [PubMed] [Google Scholar]
Ebbeling 2012 {published data only}
- Caprio S. Calories from soft drinks — do they matter?. New England Journal of Medicine 2012;367(15):1462‐3. [DOI] [PubMed] [Google Scholar]
- Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, et al. A randomized trial of sugar‐sweetened beverages and adolescent body weight. New England Journal of Medicine 2012;367(15):1407‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2013 {published data only (unpublished sought but not used)}
- Elbel B, Mijanovich T, Dixon LB, Abrams C, Weitzman B, Kersh R, et al. Calorie labeling, fast food purchasing and restaurant visits. Obesity (Silver Spring) 2013;21(11):2172‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taksler GB, Elbel B. Calorie labeling and consumer estimation of calories purchased. International Journal of Behavioral Nutrition and Physical Activity 2014;11(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2015a {published data only (unpublished sought but not used)}
- Elbel B, Mijanovich T, Abrams C, Cantor J, Dunn L, Nonas C, et al. A water availability intervention in New York City public schools: influence on youths' water and milk behaviors. American Journal of Public Health 2015;105(2):365‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Emerson 2017 {published data only (unpublished sought but not used)}
- Emerson M, Hudgens M, Barnes A, Hiller E, Robison D, Kipp R, et al. Small prizes increased plain milk and vegetable selection by elementary school children withoug adversely affecting total milk purchase. Beverages 2017;3(1):14. [Google Scholar]
- Siegel R, Lockhart MK, Barnes AS, Hiller E, Kipp R, Robison DL, et al. Small prizes increased healthful school lunch selection in a Midwestern school district. Applied Physiology, Nutrition and Metabolism 2016;41(4):370‐4. [DOI] [PubMed] [Google Scholar]
Ermetici 2016 {published data only}
- Ermetici F, Zelaschi RF, Briganti S, Dozio E, Gaeta M, Ambrogi F. Association between a school‐based intervention and adiposity outcomes in adolescents: the Italian “EAT” Project. Obesity 2016;24(3):687‐95. [DOI] [PubMed] [Google Scholar]
Finkelstein 2011 {published data only}
- Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast‐food chain in King County, Washington. American Journal of Preventive Medicine 2011;40(2):122‐7. [DOI] [PubMed] [Google Scholar]
Foster 2014 {published data only}
- Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low‐income, ethnically diverse neighborhoods: a randomized controlled trial. American Journal of Clinical Nutrition 2014;99(6):1359‐68. [DOI] [PubMed] [Google Scholar]
Franckle 2018 {published and unpublished data}
- Franckle RL, Levy DE, Macias‐Navarro L, Rimm EB, Thorndike AN. Traffic‐light labels and financial incentives to reduce sugar‐sweetened beverage purchases by low‐income Latino families: a randomized controlled trial. Public Health Nutrition 2018;21(8):1426‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2010 {published data only}
- Escoto KH, French SA. Unhealthy and healthy weight control behaviours among bus operators. Occupational Medicine (Lond) 2012;62(2):138‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Hannan PJ, Harnack LJ, Mitchell NR, Toomey TL, Gerlach A. Pricing and availability intervention in vending machines at four bus garages. Journal of Occupational and Environmental Medicine 2010;52:S29‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SA, Harnack LJ, Hannan PJ, Mitchell NR, Gerlach AF, Toomey TL. Worksite environment intervention to prevent obesity among metropolitan transit workers. Preventive Medicine 2010;50(4):180‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harnack 2016 {published data only}
- French SA, Rydell SA, Mitchell NR, Michael OJ, Elbel B, Harnack L. Financial incentives and purchase restrictions in a food benefit program affect the types of foods and beverages purchased: Results from a randomized trial. International Journal of Behavioral Nutrition and Physical Activity 2017;14(127):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnack L, Oakes J, Elbel B, Beatty T, Rydell S, French S. Effects of subsidies and prohibitions on nutrition in a food benefit program: A randomized clinical trial. JAMA Internal Medicine 2016;176(11):1610‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz MB. Incentive and restriction in combination ‐ make food assistance healthier with carrots and sticks. JAMA Internal Medicine 2016;176(11):1619‐20. [DOI] [PubMed] [Google Scholar]
Hartigan 2017 {published data only}
- Hartigan P, Patton‐Ku D, Fidler C, Boutelle KN. Rethink your drink: reducing sugar‐sweetened beverage sales in a children’s hospital. Health Promotion Practice 2017;18(2):238‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hendy 2011 {published and unpublished data}
- Hendy HM. 8 ‐ School‐based interventions to improve children’s food choices: the Kid’s choice program. In: Kilcast David, Angus Fiona editor(s). Developing Children's Food Products. Woodhead Publishing, 2011:140‐59. [Google Scholar]
- Hendy HM, Williams KE, Camise TS. Reduce Child Obesity: A Guide to Using the Kid's Choice Program in School and at Home. Plymouth, United Kingdom: R&L Education, 2013. [Google Scholar]
- Hendy HM, Williams KE, Camise TS. "Kids Choice" School lunch program increases children's fruit and vegetable acceptance. Appetite 2005;45(3):250‐63. [DOI] [PubMed] [Google Scholar]
- Hendy HM, Williams KE, Camise TS. Kid's Choice Program improves weight management behaviors and weight status in school children. Appetite 2011;56(2):484‐94. [DOI] [PubMed] [Google Scholar]
- Hendy HM, Williams KE, Camise TS, Alderman S, Ivy J, Reed J. Overweight and average‐weight children equally responsive to "Kids Choice Program" to increase fruit and vegetable consumption. Appetite 2007;49(3):683‐6. [DOI] [PubMed] [Google Scholar]
Hernández‐Cordero 2014 {published data only}
- Hernández‐Cordero S, Barquera S, Rodríguez‐Ramirez S, Villanueva‐Borbolla MA, Cossio TG, Dommarco JR, et al. Substituting water for sugar‐sweetened beverages reduces circulating triglycerides and the prevalence of metabolic syndrome in obese but not in overweight Mexican women in a randomized controlled trial. Journal of Nutrition 2014;144(11):1742‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández‐Cordero S, González‐Castell D, Rodríguez‐Ramirez S, Villanueva‐Borbolla MA, Unar M, Barquera S, et al. Design and challenges of a randomized controlled trial for reducing risk factors of metabolic syndrome in Mexican women through water intake. Salud Publica de Mexico 2013;55(6):595‐606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández‐Cordero S, Popkin BM. Impact of a water intervention on sugar‐sweetened beverage intake substitution by water: a clinical trial in overweight and obese Mexican women. Annals of Nutrition and Metabolism 2015;66:22‐5. [DOI] [PubMed] [Google Scholar]
- Rodríguez‐Ramirez S, González de Cosio T, Mendez MA, Tucker KL, Mendez‐Ramirez I, Hernández‐Cordero S, et al. A water and education provision intervention modifies the diet in overweight Mexican women in a randomized controlled trial. Journal of Nutrition 2015;145(8):1892‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hobin 2017 {published data only}
- Hobin E, Bollinger B, Sacco J, Liebman E, Vanderlee L, Zuo F, et al. Consumers’ response to an on‐shelf nutrition labelling system in supermarkets: evidence to inform policy and practice. Milbank Quarterly 2017;95(3):494‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hua 2017 {published data only (unpublished sought but not used)}
- Hua SV, Kimmel L, Emmenes M, Taherian R, Remer G, Millman A, et al. Health promotion and healthier products increase vending purchases: a randomized factorial trial. Journal of the Academy of Nutrition and Dietetics 2017;117(7):1057‐65. [DOI] [PubMed] [Google Scholar]
Huang 2012 {published data only}
- Huang R, Kiesel K. Does limited access at school result in compensation at home? the effect of soft drink bans in schools on purchase patterns outside of schools. European Review of Agricultural Economics 2012;39(5):797‐820. [Google Scholar]
Lichtman‐Sadot 2016 {published data only}
- Lichtman‐Sadot S. Does banning carbonated beverages in schools decrease student consumption?. Journal of Public Economics 2016;140:30‐50. [Google Scholar]
Minaker 2016 {published data only}
- Minaker LM, Olstad DL, MacKenzie G, Nguyen N, Azagba S, Cook BE, et al. An evaluation of the impact of a restrictive retail food environment intervention in a rural community pharmacy setting. BMC Public Health 2016;16(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Muckelbauer 2009 {published data only}
- Giraudeau B, Ravaud P. Random sampling alone does not make a randomized trial. Comment on 'Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial'. https://pediatrics.aappublications.org/content/123/4/e661.comments#random‐sampling‐alone‐does‐not‐make‐a‐randomized‐trial (accessed 1 April 2019).
- Muckelbauer R, Gortmaker SL, Libuda L, Kersting M, Clausen K, Adelberger B, et al. Changes in water and sugar‐containing beverage consumption and body weight outcomes in children. British Journal of Nutrition 2016;115(11):2057‐66. [DOI] [PubMed] [Google Scholar]
- Muckelbauer R, Libuda L, Clausen K, Kersting M. Approaches for the prevention of overweight through modified beverage consumption in the elementary school setting: The "trinkfit" study. [German]. Bundesgesundheitsblatt ‐ Gesundheitsforschung ‐ Gesundheitsschutz 2011;54(3):339‐48. [DOI] [PubMed] [Google Scholar]
- Muckelbauer R, Libuda L, Clausen K, Kersting M. Long‐term process evaluation of a school‐based programme for overweight prevention. Child: Care, Health and Development 2009;35(6):851‐7. [DOI] [PubMed] [Google Scholar]
- Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obesity Facts 2009;2(5):282‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muckelbauer R, Libuda L, Clausen K, Toschke A M, Reinehr T, Kersting M. Immigrational background affects the effectiveness of a school‐based overweight prevention program promoting water consumption. Obesity (Silver Spring) 2010;18(3):528‐34. [DOI] [PubMed] [Google Scholar]
- Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics 2009;47(4):S27‐34. [DOI] [PubMed] [Google Scholar]
Ng 2014a {published data only}
- Lavizzo‐Mourey R, Orleans CT, Marks JS. Cutting calories: trillions at a time. American Journal of Preventive Medicine 2014;47(4):e7‐e8. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D. The Healthy Weight Commitment Foundation trillion calorie pledge: lessons from a marketing ploy?. American Journal of Preventive Medicine 2014;47(4):e9‐e10. [DOI] [PubMed] [Google Scholar]
- Ng SW, Slining MM, Popkin BM. The Healthy Weight Commitment Foundation Pledge: calories sold from U.S. consumer packaged goods, 2007–2012. American Journal of Preventive Medicine 2014;47(4):508‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slining MM, Ng SW, Popkin BM. Food companies’ calorie‐reduction pledges to improve U.S. diet. American Journal of Preventive Medicine 2013;44(2):174‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ng 2014b {published data only}
- Ng SW, Popkin BM. The Healthy Weight Commitment Foundation pledge: calories purchased by U.S. households with children, 2000‐2012. American Journal of Preventive Medicine 2014;47(4):520‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ni Mhurchu 2010 {published data only}
- Blakely T, Mhurchu CN, Jiang Y, Matoe L, Funaki‐Tahifote M, Eyles H C, et al. Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomised, controlled trial. Journal of Epidemiology and Community Health 2011;65(10):902‐8. [DOI] [PubMed] [Google Scholar]
- Eyles H, Jiang Y, Ni Mhurchu C. Use of household supermarket sales data to estimate nutrient intakes: a comparison with repeat 24‐hour dietary recalls. Journal of The American Dietetic Association 2010;110(1):106‐10. [DOI] [PubMed] [Google Scholar]
- Le HN, Gold L, Abbott G, Crawford D, McNaughton SA, Mhurchu CN, et al. Economic evaluation of price discounts and skill‐building strategies on purchase and consumption of healthy food and beverages: The SHELf randomized controlled trial. Social Science & Medicine 2016;159:83‐91. [DOI] [PubMed] [Google Scholar]
- Ni Mhurchu C, Blakely T, Funaki‐Tahifote M, McKerchar C, Wilton J, Chua S, et al. Inclusion of indigenous and ethnic minority populations in intervention trials: challenges and strategies in a New Zealand supermarket study. Journal of Epidemiology and Community Health 2009;63(10):850‐5. [DOI] [PubMed] [Google Scholar]
- Ni Mhurchu C, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. American Journal of Clinical Nutrition 2010;91(3):736‐47. [DOI] [PubMed] [Google Scholar]
Olsho 2016 {published and unpublished data}
- Abt Associates Inc. Healthy Incentives Pilot: updated study plan. fns‐prod.azureedge.net/sites/default/files/study_plan.pdf 2011 (accessed 10 July 2018).
- Bartlett S, Klerman J, Olsho L, Logan C, Blocklin M, Beauregard M, et al. Evaluation of the Healthy Incentives Pilot (HIP): Final Report. Prepared by Abt Associates for the U.S. Department of Agriculture, Food and Nutrition Service. mafoodsystem.org/media/resources/pdfs/PilotFinalReport.pdf (accessed 28 August 2018).
- Klerman JA, Bartlett S, Wilde P, Olsho L. The short‐run impact of the Healthy Incentices Pilot program on fruit and vegetable intake. American Journal of Agricultural Economics 2014;96(5):1372‐82. [Google Scholar]
- Olsho LE, Klerman JA, Bartlett SH, Logan CW. Rebates to incentivize healthy nutrition choices in the Supplemental Nutrition Assistance Program. American Journal of Preventive Medicine 2017;52(2 Supplement 2):S161‐70. [DOI] [PubMed] [Google Scholar]
- Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot. American Journal of Clinical Nutrition 2016;104(2):423‐35. [DOI] [PubMed] [Google Scholar]
- Wilde P, Klerman JA, Olsho LE, Bartlett S. Explaining the impact of USDA's Healthy Incentives Pilot on different spending outcomes. Applied Economic Perspectives and Policy 2016;38(4):655‐72. [Google Scholar]
Peters 2016a {published data only}
- Peters JC, Beck J, Lande J, Pan Z, Cardel M, Ayoob K, et al. Using healthy defaults in Walt Disney World Restaurants to improve nutritional choices. Journal of the Association for Consumer Research 2016;1(1):92‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schram 2015 {published data only}
- Schram A, Labonte R, Baker P, Friel S, Reeves A, Stuckler D. The role of trade and investment liberalization in the sugar‐sweetened carbonated beverages market: a natural experiment contrasting Vietnam and the Philippines. Globalization and Health 2015;11(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwartz 2009 {published data only}
- Schwartz MB, Novak SA, Fiore SS. The impact of removing snacks of low nutritional value from middle schools. Health Education & Behavior 2009;36(6):999‐1011. [DOI] [PubMed] [Google Scholar]
Schwartz 2016 {published data only}
- Schwartz AE, Leardo M, Aneja S, Elbel B. Effect of a school‐based water intervention on child body mass index and obesity. JAMA Pediatrics 2016;170(3):220‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner L, Hager E. The power of a simple intervention to improve student health ‐ just add water. JAMA Pediatrics 2016;170(3):199‐200. [DOI] [PubMed] [Google Scholar]
Schwartz 2017 {published data only}
- Schwartz MB, Schneider GE, Choi YY, Li X, Harris J, Andreyeva T, et al. Association of a community campaign for better beverage choices with beverage purchases from supermarkets. JAMA Internal Medicine 2017;177(5):666‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siegel 2016a {published and unpublished data}
- Siegel RM, Anneken A, Duffy C, Simmons K, Hudgens M, Lockhart KM, et al. Emoticon use increases plain milk and vegetable purchase in a school cafeteria without adversely affecting total milk purchase. Clinical Therapeutics 2015;37(9):1938‐43. [DOI] [PubMed] [Google Scholar]
- Siegel RM, Hudgens M, Annekin A, Simmons K, Shelly J, Bell I, et al. A two‐tiered school cafeteria intervention of emoticons and small prizes increased healthful food selection by over 300%. International Journal of Food and Nutritional Science 2016;5(3):e‐ISSN: 2320‐7876. [Google Scholar]
Siegel 2016b {published data only (unpublished sought but not used)}
- Hudgens ME, Barnes AS, Lockhart MK, Ellsworth SC, Beckford M, Siegel RM. Small prizes improve food selection in a school cafeteria without increasing waste. Clinical Pediatrics 2017;56(2):123‐6. [DOI] [PubMed] [Google Scholar]
- Siegel RM, Geoppinger R, Emerson MM, Barnes A, Shelly J, Crumpton M, et al. Small prizes to improve food selection in inner city elementary schools. Journal of Pediatrics and Child Nutrition 2016;3(2):1‐6. [Google Scholar]
Simons 2015 {published data only}
- Simons M, Brug J, Chinapaw MJ, Boer M, Seidell J, Vet E. Replacing non‐active video gaming by active video gaming to prevent excessive weight gain in adolescents. PLoS One 2015;10(7):e0126023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons M, Chinapaw MJ, Bovenkamp M, Boer MR, Seidell JC, Brug J, et al. Active video games as a tool to prevent excessive weight gain in adolescents: rationale, design and methods of a randomized controlled trial. BMC Public Health 2014;14(1):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sturm 2015 {published data only}
- Sturm R, Hattori A. Diet and obesity in Los Angeles County 2007‐2012: is there a measurable effect of the 2008 "Fast‐Food Ban"?. Social Science & Medicine 2015;133:205‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taillie 2015 {published data only}
- Taillie SL, Ng SW, Popkin BM. Can a food retailer‐based healther foods initiative improve the nutrient profile of US packaged food purchases? A case study of Walmart, 2000‐2013. Health Affairs 2015;34(11):1869‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tate 2012 {published data only}
- Piernas C, Tate DF, Wang X, Popkin BM. Does diet‐beverage intake affect dietary consumption patterns? Results from the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. American Journal of Clinical Nutrition 2013;97(3):604‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate DF, Turner‐McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. American Journal of Clinical Nutrition 2012;95(3):555‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner‐McGrievy G, Wang X, Popkin BM, Tate DF. Tasting profile affects adoption of caloric beverage reduction in a randomized weight loss intervention. Obesity Science and Practice 2016;2(4):392‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van de Gaar 2014 {published data only}
- Blanchette LM, Gaar VM, Raat H, French J, Jansen W. The development of the “Water Campaign”: combining social marketing and intervention mapping. Journal of Social Marketing 2016;6(4):318‐34. [Google Scholar]
- Gaar V, Jansen W, Grieken A, Borsboom G, Kremers S, Raat H. Effects of an intervention aimed at reducing the intake of sugar‐sweetened beverages in primary school children: a controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2014;11(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaar VM, Grieken A, Jansen W, Raat H. Children's sugar‐sweetened beverages consumption: associations with family and home‐related factors, differences within ethnic groups explored. BMC Public Health 2017;17(1):195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaar VM, Grieken A, Jansen W, Raat H. Children’s sugar‐sweetened beverages consumption: associations with family and home‐related factors, differences within ethnic groups explored. BMC Public Health 2017;17(1):195. [DOI] [PMC free article] [PubMed] [Google Scholar]
Visscher 2010 {published data only}
- Visscher TL, Hal WC, Blokdijk L, Seidell JC, Renders CM, Bemelmans WJ. Feasibility and impact of placing water coolers on sales of sugar‐sweetened beverages in Dutch secondary school canteens. Obesity Facts 2010;3(2):109‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waehrer 2015 {published data only}
- Waehrer G, Deb P, Decker SL. Did the 2009 American Recovery and Reinvestment Act affect dietary intake of low‐income individuals?. Economics and Human Biology 2015;19:170‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whatley Blum 2008 {published data only}
- Davee AM, Blum JE, Devore RL, Beaudoin CM, Kaley LA, Leiter JL, et al. The vending and a la carte policy intervention in Maine public high schools. Preventing Chronic Disease 2005;2:A14. [PMC free article] [PubMed] [Google Scholar]
- Whatley Blum JE, Davee AM, Beaudoin CM, Jenkins PL, Kaley LA, Wigand DA. Reduced availability of sugar‐sweetened beverages and diet soda has a limited impact on beverage consumption patterns in Maine high school youth. Journal of Nutrition Education and Behavior 2008;40(6):341‐7. [DOI] [PubMed] [Google Scholar]
Øverby 2012 {published and unpublished data}
- Bere E, Hilsen M, Klepp KI. Effect of the nationwide free school fruit scheme in Norway. British Journal of Nutrition 2010;104(4):589‐94. [DOI] [PubMed] [Google Scholar]
- Bere E, Klepp KI, Øverby NC. Free school fruit: can an extra piece of fruit every school day contribute to the prevention of future weight gain? A cluster randomized trial. Food and Nutrition Research 2014;58:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bere E, Velde SJ, Småstuen MC, Twisk J, Klepp KI. One year of free school fruit in Norway ‐ 7 years of follow‐up. International Journal of Behavioral Nutrition and Physical Activity 2015;12(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bere E, Veierød MB, Bjelland M, Klepp K‐I. Free school fruit—sustained effect 1 year later. Health Education Research 2006;21(2):268‐75. [DOI] [PubMed] [Google Scholar]
- Bere E, Veierød MB, Skare Ø, Klepp KI. Free school fruit ‐ sustained effect three years later. International Journal of Behavioral Nutrition and Physical Activity 2007;4:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Øverby NC, Klepp K‐I, Bere E. Introduction of a school fruit program is associated with reduced frequency of consumption of unhealthy snacks. American Journal of Clinical Nutrition 2012;96(5):1100‐03. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alaimo 2013 {published data only}
- Alaimo K, Oleksyk SC, Drzal NB, Golzynski DL, Lucarelli JF, Wen Y, et al. Effects of changes in lunch‐time competitive foods, nutrition practices, and nutrition policies on low‐income middle‐school children's diets. Childhood Obesity 2013;9(6):509‐23. [DOI] [PubMed] [Google Scholar]
Alaimo 2015 {published data only}
- Alaimo K, Oleksyk S, Golzynski D, Drzal N, Lucarelli J, Reznar M, et al. The Michigan Healthy School Action Tools process generates improvements in school nutrition policies and practices, and student dietary intake. Health Promotion Practice 2015;16(3):401‐10. [DOI] [PubMed] [Google Scholar]
Alberti 2010 {published data only}
- Alberti PM, Perlman SE, Nonas C, Hadler J, Choe J, Bedell F, et al. Effects of switching from whole to low‐fat/fat‐free milk in public schools ‐ New York City, 2004‐2009. Morbidity and Mortality Weekly Report 2010;59(3):70‐3. [PubMed] [Google Scholar]
Allan 2015 {published data only}
- Allan JL, Johnston M, Campbell N. Snack purchasing is healthier when the cognitive demands of choice are reduced: a randomized controlled trial. Health Psychology 2015;34(7):750‐5. [DOI] [PubMed] [Google Scholar]
Ames 2016 {published data only}
- Ames SL, Wurpts IC, Pike JR, MacKinnon DP, Reynolds KR, Stacy AW. Self‐regulation interventions to reduce consumption of sugar‐sweetened beverages in adolescents. Appetite 2016;105:652‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 2016 {published data only}
- Andersen LB, Arnberg K, Trolle E, Michaelsen KF, Bro R, Pipper CB, et al. The effects of water and dairy drinks on dietary patterns in overweight adolescents. International Journal of Food Sciences and Nutrition 2016;67(3):314‐24. [DOI] [PubMed] [Google Scholar]
Anttila 2015 {published data only}
- Anttila J, Rytkönen T, Kankaanpää R, Tolvanen M, Lahti S. Effect of national recommendation on sweet selling as an intervention for a healthier school environment. Scandinavian Journal of Public Health 2015;43(1):27‐34. [DOI] [PubMed] [Google Scholar]
Anzman‐Frasca 2015 {published data only}
- Anzman‐Frasca S, Mueller MP, Sliwa S, Dolan PR, Harelick L, Roberts SB, et al. Changes in children's meal orders following healthy menu modifications at a regional US restaurant chain. Obesity 2015;23(5):1055‐62. [DOI] [PubMed] [Google Scholar]
Bacardi‐Gascon 2012 {published data only}
- Bacardi‐Gascon M, Perez‐Morales ME, Jimenez‐Cruz A. A six month randomized school intervention and an 18‐month follow‐up intervention to prevent childhood obesity in Mexican elementary schools. Nutricion Hospitalaria 2012;27(3):755‐62. [DOI] [PubMed] [Google Scholar]
Bae 2012 {published data only}
- Bae SG, Kim JY, Kim KY, Park SW, Bae J, Lee WK. Changes in dietary behavior among adolescents and their association with government nutrition policies in Korea, 2005‐2009. Journal of Preventive Medicine and Public Health 2012;45(1):47‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baidal 2017 {published data only}
- Baidal JW, Nelson C, Perkins M, Colchamiro R, Leung‐Strle P, Kwass JA, et al. Childhood obesity prevention in WIC: outcomes of the MA‐CORD study. Journal of Pediatric Gastroenterology and Nutrition 2017;65:S196. [Google Scholar]
Baranowski 2000 {published data only}
- Baranowski T, Davis M, Resnicow K, Baranowski J, Doyle C, Lin LS, et al. Gimme 5 fruit, juice, and vegetables for fun and health: outcome evaluation. Health Education and Behavior 2000;27(1):96‐111. [DOI] [PubMed] [Google Scholar]
Baranowski 2003 {published data only}
- Baranowski T, Baranowski JC, Cullen KW, Thompson DI, Nicklas T, Zakeri IF, et al. The Fun, Food, and Fitness Project (FFFP): the Baylor GEMS pilot study. Ethnicity and Disease 2003;13(1):S1 30‐9. [PubMed] [Google Scholar]
Barlow 2017 {published data only}
- Barlow P, McKee M, Basu S, Stuckler D. Impact of the North American Free Trade Agreement on high‐fructose corn syrup supply in Canada: a natural experiment using synthetic control methods. Canadian Medical Association Journal 2017;189(26):E881‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barlow 2018 {published data only}
- Barlow P, McKee M, Stuckler D. The Impact of U.S. Free Trade Agreements on calorie availability and obesity: a natural experiment in Canada. American Journal of Preventive Medicine 2018;54(5):637‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barr 2000 {published data only}
- Barr SI, McCarron DA, Heaney RP, Dawson‐Hughes B, Berga SL, Stern J, et al. Effects of increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. Journal of The American Dietetic Association 2000;100(7):810‐7. [DOI] [PubMed] [Google Scholar]
Bayer 2009 {published data only}
- Bayer O, Kries R, Strauss A, Mitschek C, Toschke AM, Hose A, et al. Short‐ and mid‐term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster‐randomized trial. Clinical Nutrition 2009;28(2):122‐8. [DOI] [PubMed] [Google Scholar]
Beck 2017 {published data only}
- Beck AL, Fernandez A, Rojina J, Cabana M. Randomized controlled trial of a clinic‐based intervention to promote healthy beverage consumption among latino children. Clinical Pediatrics 2017;56(9):838‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beets 2014 {published data only}
- Beets MW, Tilley F, Weaver RG, Turner‐McGrievy GM, Moore JB. Increasing fruit, vegetable and water consumption in summer day camps‐‐3‐year findings of the healthy lunchbox challenge. Health Education Research 2014;29(5):812‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beets 2016 {published data only}
- Beets MW, Turner‐McGrievy B, Weaver RG, Huberty J, Moore JB, Ward DS, et al. Intervention leads to improvements in the nutrient profile of snacks served in afterschool programs: a group randomized controlled trial. Translational Behavioral Medicine 2016;6(3):329‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Beinert 2017 {published data only}
- Beinert C, Hernes S, Haugen M, Overby NC. No long‐term effect of a 2‐days intervention on how to prepare homemade food, on toddlers' skepticism for new food and intake of fruits and vegetables and sweet beverages: a randomized, controlled trial. BMC Research Notes 2017;10(1):607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bender 2014 {published data only}
- Bender MS, Clark MJ, Gahagan S. Community engagement approach: developing a culturally appropriate intervention for Hispanic mother‐child dyads. Journal of Transcultural Nursing 2014;25(4):373‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bender 2016 {published data only}
- Bender MS, Santos GM, Villanueva C, Arai S. Development of a mobile phone‐based weight loss lifestyle intervention for Filipino Americans with type 2 diabetes: Protocol and early results from the PilAm Go4Health randomized controlled trial. JMIR Research Protocols 2016;5(3):e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergen 2006 {published data only}
- Bergen D, Yeh MC. Effects of energy‐content labels and motivational posters on sales of sugar‐sweetened beverages: stimulating sales of diet drinks among adults study. Journal of The American Dietetic Association 2006;106(11):1866‐9. [DOI] [PubMed] [Google Scholar]
Bjelland 2011 {published data only}
- Bjelland M, Bergh IH, Grydeland M, Klepp KII, Andersen LF, Anderssen SA, et al. Changes in adolescents' intake of sugar‐sweetened beverages and sedentary behaviour: results at 8 month mid‐way assessment of the HEIA study‐‐a comprehensive, multi‐component school‐based randomized trial. International Journal of Behavioral Nutrition and Physical Activity 2011;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bleich 2012 {published data only}
- Bleich SN, Herring BJ, Flagg DD, Gary‐Webb TL. Reduction in purchases of sugar‐sweetened beverages among low‐income black adolescents after exposure to caloric information. American Journal of Public Health 2012;102(2):329‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bleich 2014 {published data only (unpublished sought but not used)}
- Bleich SN, Barry CL, Gary‐Webb TL, Herring BJ. Reducing sugar‐sweetened beverage consumption by providing caloric information: How black adolescents alter their purchases and whether the effects persist. American Journal of Public Health 2014;104(12):2417‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bleich 2017 {published data only}
- Bleich SN, Wolfson JA, Jarlenski MP. Calorie changes in large chain restaurants from 2008 to 2015. Preventive Medicine 2017;100:112‐6. [DOI] [PubMed] [Google Scholar]
Block 2010 {published data only}
- Block JP, Chandra A, McManus KD, Willett WC. Point‐of‐purchase price and education intervention to reduce consumption of sugary soft drinks. American Journal of Public Health 2010;100(8):1427‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bogart 2011 {published data only}
- Bogart LM, Elliott MN, Uyeda K, Hawes‐Dawson J, Klein DJ, Schuster MA. Preliminary healthy eating outcomes of SNaX, a pilot community‐based intervention for adolescents. Journal of Adolescent Health 2011;48(2):196‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boone‐Heinonen 2011 {published data only}
- Boone‐Heinonen J, Gordon‐Larsen P, Kiefe CI, Shikany JM, Lewis CE, Popkin BM. Fast food restaurants and food stores ‐ Longitudinal associations with diet in young to middle‐aged adults: the CARDIA study. Archives of Internal Medicine 2011;171(13):1162‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brandstetter 2012 {published data only}
- Brandstetter S, Klenk J, Berg S, Galm C, Fritz M, Peter R, et al. Overweight prevention implemented by primary school teachers: a randomised controlled trial. Obesity Facts 2012;5(1):1‐11. [DOI] [PubMed] [Google Scholar]
Branscum 2013 {published data only}
- Branscum P, Sharma M, Wang LL, Wilson BR, Rojas‐Guyler L, Leigh Wang L, et al. A true challenge for any superhero: an evaluation of a comic book obesity prevention program. Family & Community Health 2013;36(1):63‐76. [DOI] [PubMed] [Google Scholar]
Brown 2009 {published data only}
- Brown DM, Tammineni SK. Managing sales of beverages in schools to preserve profits and improve children's nutrition intake in 15 Mississippi schools. Journal of The American Dietetic Association 2009;109(12):2036‐42. [DOI] [PubMed] [Google Scholar]
Bruerd 1996 {published data only}
- Bruerd B, Jones C. Preventing baby bottle tooth decay: eight‐year results. Public Health Reports 1996;111(1):63‐5. [PMC free article] [PubMed] [Google Scholar]
Brunello 2014 {published data only (unpublished sought but not used)}
- Brunello G, Paola M, Labartino G. More apples fewer chips? The effect of school fruit schemes on the consumption of junk food. Health Policy 2014;118(1):114‐26. [DOI] [PubMed] [Google Scholar]
Bruun 2015 {published data only}
- Bruun JM, Maersk M, Belza A, Astrup A, Richelsen B. Consumption of sucrose‐sweetened soft drinks increases plasma levels of uric acid in overweight and obese subjects: a 6‐month randomised controlled trial. European Journal of Clinical Nutrition 2015;69(8):949‐53. [DOI] [PubMed] [Google Scholar]
Bryden 2013 {published data only}
- Bryden A, Petticrew M, Mays N, Eastmure E, Knai C. Voluntary agreements between government and business—A scoping review of the literature with specific reference to the Public Health Responsibility Deal. Health Policy 2013;110(2–3):186‐97. [DOI] [PubMed] [Google Scholar]
Burrows 2012 {published data only}
- Burrows T, Morgan PJ, Lubans DR, Callister R, Okely T, Bray J, et al. Dietary outcomes of the healthy dads healthy kids randomised controlled trial. Journal of Pediatric Gastroenterology and Nutrition 2012;55(4):408‐11. [DOI] [PubMed] [Google Scholar]
Butler 2011 {published data only (unpublished sought but not used)}
- Butler R, Tapsell L, Lyons‐Wall P. Trends in purchasing patterns of sugar‐sweetened water‐based beverages in a remote Aboriginal community store following the implementation of a community‐developed store nutrition policy. Nutrition and Dietetics 2011;68(2):115‐9. [Google Scholar]
Caljouw 2014 {published data only}
- Caljouw SR, Wijck R. Is the glass half full or half empty? How to reverse the effect of glass elongation on the volume poured. PLoS One 2014;9(10):e109374. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2013 {published data only}
- Campbell KJ, Lioret S, McNaughton SA, Crawford DA, Salmon J, Ball K, et al. A parent‐focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics 2013;131(4):652‐60. [DOI] [PubMed] [Google Scholar]
Campos 2015 {published data only}
- Campos V, Despland C, Brandejsky V, Kreis R, Schneiter P, Chiolero A, et al. Sugar‐ and artificially sweetened beverages and intrahepatic fat: a randomized controlled trial. Obesity 2015;23:2335‐9. [DOI] [PubMed] [Google Scholar]
Campos 2017 {published data only}
- Campos V, Despland C, Brandejsky V, Kreis R, Schneiter P, Boesch C, et al. Metabolic effects of replacing sugar‐sweetened beverages with artificially‐sweetened beverages in overweight subjects with or without hepatic steatosis: a randomized control clinical trial. Nutrients 2017;9(3):1‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carriedo 2013 {published data only (unpublished sought but not used)}
- Carriedo A, Bonvecchio A, Lopez N, Morales M, Mena C, Theodore FL, et al. Use of social marketing to increase water consumption among school‐age children in Mexico City. Salud Publica de Mexico 2013;55:S388‐96. [PubMed] [Google Scholar]
Casazza 2006 {published data only}
- Casazza K. nts. A Computer Based Approach to Improve the Dietary and Physical Activity Patterns of a Diverse Group of Adolesce [Dissertation. Miami: Florida International University, 2006. [Google Scholar]
Chen 2009 {published data only}
- Chen L, Appel LJ, Loria C, Lin Pao‐Hwa H, Champagne CM, Elmer PJ, et al. Reduction in consumption of sugar‐sweetened beverages is associated with weight loss: The PREMIER trial. American Journal of Clinical Nutrition 2009;89(5):1299‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2010 {published data only}
- Chen L, Caballero B, Mitchell DC, Loria C, Lin Pao‐Hwa H, Champagne CM, et al. Reducing consumption of sugar‐sweetened beverages is associated with reduced blood pressure a prospective study among United States adults. Circulation 2010;121(22):2398‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chi 2016 {published data only}
- Chi DL, Zegarra G, Vasquez HE, Castillo JL, Milgrom P, Roberts MC, et al. Milk sweetened with xylitol: a proof‐of‐principle caries prevention randomized clinical trial. Journal of Centistry for Children 2016;83(3):152‐60. [PMC free article] [PubMed] [Google Scholar]
Chin 2008 {published data only}
- Chin A, Paw MJ, Singh AS, Brug J, Mechelen W. Why did soft drink consumption decrease but screen time not? Mediating mechanisms in a school‐based obesity prevention program. International Journal of Behavioral Nutrition and Physical Activity 2008;5:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2017 {published data only}
- Choi SK, Frongillo EA, Blake CE, Thrasher JF. Korean adolescents' energy intake of selected foods by eating place from 1998 to 2012 during implementation of two national school nutrition policies. Journal of Hunger and Environmental Nutrition 2017 [Epub ahead of print]. [DOI: 10.1080/19320248.2017.1337534] [DOI]
Cloutier 2015 {published data only}
- Cloutier MM, Wiley J, Huedo‐Medina T, Ohannessian M, Grant A, Hernandez D, et al. Outcomes from a pediatric primary care weight management program: Steps to Growing Up Healthy. Journal of Pediatrics 2015;167(2):372‐7.e1. [DOI] [PubMed] [Google Scholar]
Collins 2014 {published data only}
- Collins CE, Dewar DL, Schumacher TL, Finn T, Morgan PJ, Lubans DR. 12 Month changes in dietary intake of adolescent girls attending schools in low‐income communities following the NEAT Girls cluster randomized controlled trial. Appetite 2014;73:147‐55. [DOI] [PubMed] [Google Scholar]
Cordeira 2012 {published data only}
- Cordeira KL. Effects of a Health Advocacy Program to Promote Physical Activity and Nutrition Behaviors among Adolescents: an Evaluation of the Young Leaders for Healthy Change Program [Masters Thesis]. Houston, Texas: University of Texas, 2012. [Google Scholar]
Cox 2012 {published data only}
- Cox CL, Stanhope KL, Schwarz JM, Graham JL, Hatcher B, Griffen SC, et al. Consumption of fructose‐sweetened beverages for 10 weeks reduces net fat oxidation and energy expenditure in overweight/obese men and women. European Journal of Clinical Nutrition 2012;66(2):201‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cullen 2006 {published data only}
- Cullen KW, Watson K, Zakeri I, Ralston K. Exploring changes in middle‐school student lunch consumption after local school food service policy modifications. Public Health Nutrition 2006;9(6):814‐20. [DOI] [PubMed] [Google Scholar]
Cullen 2008 {published data only}
- Cullen KW, Watson K, Zakeri I. Improvements in middle school student dietary intake after implementation of the Texas Public School Nutrition Policy. American Journal of Public Health 2008;98(1):111‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cummins 2014 {published data only}
- Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Affairs 2014;33(2):283‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cunha 2013 {published data only}
- Cunha DB, Souza B, Pereira RA, Sichieri R. Effectiveness of a randomized school‐based intervention involving families and teachers to prevent excessive weight gain among adolescents in Brazil. PLoS One 2013;8(2):e57498. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daniels 2014 {published data only}
- Daniels LA, Mallan KM, Battistutta D, Nicholson JM, Meedeniya JE, Bayer JK, et al. Child eating behavior outcomes of an early feeding intervention to reduce risk indicators for child obesity: the NOURISH RCT. Obesity (Silver Spring) 2014;22(5):E104‐11. [DOI] [PubMed] [Google Scholar]
Dannefer 2012 {published data only}
- Dannefer R, Williams DA, Baronberg S, Silver L. Healthy bodegas: increasing and promoting healthy foods at corner stores in New York City. American Journal of Public Health 2012;102(10):e27‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2007 {published data only}
- Davis JN, Ventura EE, Alexander KE, Salguero LE, Weigensberg MJ, Crespo NC, et al. Feasibility of a home‐based versus classroom‐based nutrition intervention to reduce obesity and type 2 diabetes in Latino youth. International Journal of Pediatric Obesity 2007;2(1):22‐30. [DOI] [PubMed] [Google Scholar]
De Bourdeaudhuij 2015 {published data only}
- Bourdeaudhuij I, Verbestel V, Henauw S, Maes L, Huybrechts I, Marild S, et al. Behavioural effects of a community‐oriented setting‐based intervention for prevention of childhood obesity in eight European countries. Main results from the IDEFICS study. Obesity Reviews 2015;16:30‐40. [DOI] [PubMed] [Google Scholar]
Delpier 2013 {published data only}
- Delpier T, Giordana S, Wedin BM. Decreasing sugar‐sweetened beverage consumption in the rural adolescent population. Journal of Pediatric Health Care 2013;27(6):470‐8. [DOI] [PubMed] [Google Scholar]
De Moraes 2017 {published data only}
- Moraes MM, Mediano MF, Souza RA, Moura AS, Veiga GV, Sichieri R. Discouraging soft drink consumption reduces blood glucose and cholesterol of Brazilian elementary students: secondary analysis of a randomized controlled trial. Preventive Medicine 2017 July; Vol. 100:223‐8. [DOI: 10.1016/j.ypmed.2017.04.035] [DOI] [PubMed]
Dennis 2010 {published data only}
- Dennis EA, Dengo AL, Comber DL, Flack KD, Savla J, Davy KP, et al. Water consumption increases weight loss during a hypocaloric diet intervention in middle‐aged and older adults. Obesity 2010;18(2):300‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Ruyter 2014 {published data only}
- Ruyter JC, Olthof MR, Katan MB. A trial of sugar‐free or sugar‐sweetened beverages and body weight in children. New England Journal of Medicine 2014;367(15):1397‐406. [DOI] [PubMed] [Google Scholar]
De Souza 2013 {published data only}
- Souza RA, Mediano MF, Souza AM, Sichieri R. Reducing the use of sugar in public schools: a randomized cluster trial. Revista de Saude Publica 2013;47(4):666‐74. [DOI] [PubMed] [Google Scholar]
Donnelly 2018 {published data only}
- Donnelly GE, Zatz LY, Svirsky D, John LK. The effect of graphic warnings on sugary‐drink purchasing. Psychological Science 2018; Vol. 29, issue 8:1321‐33. [DOI: 10.1177/0956797618766361] [DOI] [PMC free article] [PubMed]
Doymaz 2009 {published data only}
- Doymaz S, Neuspiel DR. The influence of pediatric resident counseling on limiting sugar‐sweetened drinks in children. Clinical Pediatrics 2009;48(7):777‐9. [DOI] [PubMed] [Google Scholar]
Drewnowski 2017 {published data only}
- Drewnowski A, Michels S, Leroy D. The impact of crunchy wednesdays on happy meal fruit orders: analysis of sales data in France, 2009–2013. Journal of Nutrition Education and Behavior 2017;49(3):236‐40.e1. [DOI] [PubMed] [Google Scholar]
Dubuy 2014 {published data only}
- Dubuy V, Cocker K, Bourdeaudhuij I, Maes L, Seghers J, Lefevre J, et al. Evaluation of a real world intervention using professional football players to promote a healthy diet and physical activity in children and adolescents from a lower socio‐economic background: a controlled pretest‐posttest design. BMC Public Health 2014;14:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duncan 2011 {published data only}
- Duncan S, McPhee JC, Schluter PJ, Zinn C, Smith R, Schofield G. Efficacy of a compulsory homework programme for increasing physical activity and healthy eating in children: the healthy homework pilot study. International Journal of Behavioral Nutrition and Physical Activity 2011;8:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2009 {published data only}
- Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low‐income people in New York City. Health Affairs 2009;28(6):w1110‐21. [DOI] [PubMed] [Google Scholar]
Elbel 2011 {published data only}
- Elbel B, Gyamfi J, Kersh R. Child and adolescent fast‐food choice and the influence of calorie labeling: a natural experiment. International Journal of Obesity 2011;35(4):493‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2015b {published data only}
- Elbel B, Moran A, Dixon LB, Kiszko K, Cantor J, Abrams C, et al. Assessment of a government‐subsidized supermarket in a high‐need area on household food availability and children's dietary intakes. Public Health Nutrition 2015;18(15):2881‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elder 2014 {published data only}
- Elder JP, Holub CK, Arredondo EM, Sanchez‐Romero LM, Moreno‐Saracho JE, Barquera S, et al. Promotion of water consumption in elementary school children in San Diego, USA and Tlaltizapan, Mexico. Salud Publica de Mexico 2014;56:s148‐56. [DOI] [PubMed] [Google Scholar]
Ezendam 2007 {published data only}
- Ezendam NP, Oenema A, Looij‐Jansen PM, Brug J. Design and evaluation protocol of "FATaintPHAT", a computer‐tailored intervention to prevent excessive weight gain in adolescents. BMC Public Health 2007;7:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ezendam 2012 {published data only}
- Ezendam NP, Brug J, Oenema A. Evaluation of the web‐based computer‐tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Archives of Pediatrics & Adolescent Medicine 2012;166(3):248‐55. [DOI] [PubMed] [Google Scholar]
Ferguson 2016 {published data only (unpublished sought but not used)}
- Ferguson M, O'Dea K, Holden S, Miles E, Brimblecombe J. Food and beverage price discounts to improve health in remote Aboriginal communities: mixed method evaluation of a natural experiment. Australian and New Zealand Journal of Public Health 2016;41(1):32‐7. [DOI] [PubMed] [Google Scholar]
Fernandes 2009 {published data only}
- Fernandes PS, Bernardo CO, Campos RM, Vasconcelos FA. Evaluating the effect of nutritional education on the prevalence of overweight/obesity and on foods eaten at primary schools. Journal of Pediatrics (Rio de Janeiro) 2009;85(4):315‐21. [DOI] [PubMed] [Google Scholar]
Fernandes 2012 {published data only}
- Fernandes MM. Effect of the Supplemental Nutrition Assistance Program SNAP on frequency of beverage consumption among youth in the United States. Journal of the Academy of Nutrition and Dietetics 2012;112(8):1241‐6. [DOI] [PubMed] [Google Scholar]
Fiechtner 2016 {published data only}
- Fiechtner L, Kleinman K, Melly SJ, Sharifi M, Marshall R, Block J, et al. Effects of proximity to supermarkets on a randomized trial studying interventions for obesity. American Journal of Public Health 2016;106(3):557‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Folta 2013 {published data only}
- Folta SC, Kuder JF, Goldberg JP, Hyatt RR, Must A, Naumova EN, et al. Changes in diet and physical activity resulting from the shape up Somerville community intervention. BMC Pediatrics 2013;13(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2010 {published data only}
- Foster GD, Linder B, Baranowski T, Cooper DM, Goldberg L, Harrell JS, et al. A school‐based intervention for diabetes risk reduction. New England Journal of Medicine 2010;363(5):443‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franks 2017 {published data only}
- Franks B, Lahlou S, Bottin JH, Guelinckx I, Boesen‐Mariani S. Increasing water intake in pre‐school children with unhealthy drinking habits: a year‐long controlled longitudinal field experiment assessing the impact of information, water affordance, and social regulation. Appetite 2017;116:205‐14. [DOI] [PubMed] [Google Scholar]
French 2011 {published data only}
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take action ‐ a group‐randomized trial. Obesity 2011;19(10):2082‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2015 {published data only}
- French SA, Sherwood NE, JaKa MM, Haapala JL, Ebbeling CB, Ludwig DS. Physical changes in the home environment to reduce television viewing and sugar‐sweetened beverage consumption among 5‐to 12‐year‐old children: a randomized pilot study. Pediatric Obesity 2015;11(5):e12‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fung 2013 {published data only}
- Fung C, McIsaac JL, Kuhle S, Kirk S F, Veugelers PJ. The impact of a population‐level school food and nutrition policy on dietary intake and body weights of Canadian children. Preventive Medicine 2013;57(6):934‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garipagaoglu 2009 {published data only}
- Garipagaoglu M, Sahip Y, Darendeliler F, Akdikmen O, Kopuz S, Sut N. Family‐based group treatment versus individual treatment in the management of childhood obesity: randomized, prospective clinical trial. European Journal of Pediatrics 2009;168(9):1091‐9. [DOI] [PubMed] [Google Scholar]
Geliebter 2013 {published data only}
- Geliebter A, Ang I, Bernales‐Korins M, Hernandez D, Ochner CN, Ungredda T, et al. Supermarket discounts of low‐energy density foods: Effects on purchasing, food intake, and body weight. Obesity 2013;21(12):E542‐8. [DOI] [PubMed] [Google Scholar]
Giles 2012 {published data only}
- Giles CM, Kenney EL, Gortmaker SL, Lee RM, Thayer JC, Mont‐Ferguson H, et al. Increasing water availability during afterschool snack: evidence, strategies, and partnerships from a group randomized trial. American Journal of Preventive Medicine 2012;43(3, Supplement 2):S136‐42. [DOI] [PubMed] [Google Scholar]
Gittelsohn 2010a {published data only (unpublished sought but not used)}
- Gittelsohn J, Vijayadeva V, Davison N, Ramirez V, Cheung LW, Murphy S, et al. A food store intervention trial improves caregiver psychosocial factors and children's dietary intake in Hawaii. Obesity (Silver Spring) 2010;18:S84‐90. [DOI] [PubMed] [Google Scholar]
Gittelsohn 2010b {published data only}
- Gittelsohn J, Song HJ, Suratkar S, Kumar MB, Henry EG, Sharma S, et al. An urban food store intervention positively affects food‐related psychosocial variables and food behaviors. Health Education and Behavior 2010;37(3):390‐402. [DOI] [PubMed] [Google Scholar]
Gittelsohn 2013 {published data only}
- Gittelsohn J, Kim EM, He S, Pardilla M. A food store‐based environmental intervention is associated with reduced BMI and improved psychosocial factors and food‐related behaviors on the Navajo nation. Journal of Nutrition 2013;143(9):1494‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldberg 2015 {published data only}
- Goldberg JP, Folta SC, Eliasziw M, Koch‐Weser S, Economos CD, Hubbard KL, et al. Great Taste, Less Waste: a cluster‐randomized trial using a communications campaign to improve the quality of foods brought from home to school by elementary school children. Preventive Medicine 2015;74:103‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomez 2013 {published data only}
- Gomez P, Mariani SB, Lambert JL, Monrozier R. A water intervention program to improve fluid intakes among French women. Nutrition Today 2013;48(4):S40‐2. [Google Scholar]
Gostin 2014 {published data only}
- Gostin LO, Reeve BH, Ashe M. The historic role of boards of health in local innovation: New York City's soda portion case. JAMA 2014;312(15):1511‐2. [DOI] [PubMed] [Google Scholar]
Goto 2013 {published data only}
- Goto K, Waite A, Wolff C, Chan K, Giovanni M. Do environmental interventions impact elementary school students' lunchtime milk selection?. Applied Economic Perspectives and Policy 2013;35(2):360‐76. [Google Scholar]
Greece 2017 {published data only}
- Greece JA, Feld S, DeJong W, Cozier YC, Quatromoni PA. Effects of a school‐based intervention on middle school children's daily food and beverage intake. Health Behavior and Policy Review 2017;4(1):24‐36. [Google Scholar]
Griffin 2015 {published data only}
- Griffin TL, Jackson DM, McNeill G, Aucott LS, Macdiarmid JI. A brief educational intervention increases knowledge of the sugar content of foods and drinks but does not decrease intakes in scottish children aged 10‐12 years. Journal of Nutrition Education and Behavior 2015;47(4):367‐73.e1. [DOI] [PubMed] [Google Scholar]
Haddock 2014 {published data only}
- Haddock CK, Poston WS, Lagrotte C, Klotz AA, Oliver TL, Vander Veur SS, et al. Findings from an online behavioural weight management programme provided with or without a fortified diet beverage. British Journal of Nutrition 2014;111(2):372‐9. [DOI] [PubMed] [Google Scholar]
Haerens 2007 {published data only}
- Haerens L, Bourdeaudhuij I, Maes L, Vereecken C, Brug J, Deforche B. The effects of a middle‐school healthy eating intervention or adolescents' fat and fruit intake and soft drinks consumption. Public Health Nutrition 2007;10(5):443‐9. [DOI] [PubMed] [Google Scholar]
- Haerens L, Deforche B, Maes L, Cardon G, Stevens V, Bourdeaudhuij I. Evaluation of a 2‐year physical activity and healthy eating intervention in middle school children. Health Education Research 2006;21(6):911‐21. [DOI] [PubMed] [Google Scholar]
Hanks 2014 {published data only}
- Hanks AS, Just DR, Wansink B. Chocolate milk consequences: a pilot study evaluating the consequences of banning chocolate milk in school cafeterias. PLoS One 2014;9(4):e91022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Han‐Markey 2012 {published data only}
- Han‐Markey TL, Wang L, Schlotterbeck S, Jackson EA, Gurm R, Leidal A, et al. A public school district's vending machine policy and changes over a 4‐year period: implementation of a national wellness policy. Public Health 2012;126(4):335‐7. [DOI] [PubMed] [Google Scholar]
Hebden 2014 {published data only}
- Hebden L, Cook A, Ploeg HP, King L, Bauman A, Allman‐Farinelli M. A mobile health intervention for weight management among young adults: a pilot randomised controlled trial. Journal of Human Nutrition and Dietetics 2014;27(4):322‐32. [DOI] [PubMed] [Google Scholar]
Hedrick 2015 {published data only}
- Hedrick VE, Davy BM, Myers EA, You W, Zoellner JM. Changes in the healthy beverage index in response to an intervention targeting a reduction in sugar‐sweetened beverage consumption as compared to an intervention targeting improvements in physical activity: results from the Talking Health trial. Nutrients 2015;7(12):10168‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodgson 2013 {published data only}
- Hodgson JM, Croft KD, Woodman RJ, Puddey IB, Fuchs D, Draijer R, et al. Black tea lowers the rate of blood pressure variation: a randomized controlled trial. American Journal of Clinical Nutrition 2013;97(5):943‐50. [DOI] [PubMed] [Google Scholar]
Hoeft 2016 {published data only}
- Hoeft KS, Barker JC, Shiboski S, Pantoja‐Guzman E, Hiatt RA. Effectiveness evaluation of Contra Caries Oral Health Education Program for improving Spanish‐speaking parents' preventive oral health knowledge and behaviors for their young children. Community Dentistry and Oral Epidemiology 2016;44(6):564‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Holmes 2012 {published data only}
- Holmes AS, Estabrooks PA, Davis GC, Serrano EL. Effect of a grocery store intervention on sales of nutritious foods to youth and their families. Journal of the Academy of Nutrition and Dietetics 2012;112(6):897‐901. [DOI] [PubMed] [Google Scholar]
Hoppu 2010 {published data only}
- Hoppu U, Lehtisalo J, Kujala J, Keso T, Garam S, Tapanainen H, et al. The diet of adolescents can be improved by school intervention. Public Health Nutrition 2010;13(6):973‐9. [DOI] [PubMed] [Google Scholar]
Iaia 2017 {published data only}
- Iaia M, Pasini M, Burnazzi A, Vitali P, Allara E, Farneti M. An educational intervention to promote healthy lifestyles in preschool children: a cluster‐RCT. International Journal of Obesity 2017;41(4):582‐90. [DOI] [PubMed] [Google Scholar]
James 2004 {published data only}
- James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ 2004;328(7450):1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jancey 2014 {published data only}
- Jancey JM, Dos Remedios Monteiro SM, Dhaliwal SS, Howat PA, Burns S, Hills AP, et al. Dietary outcomes of a community based intervention for mothers of young children: a randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2014;11:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 2012 {published data only}
- Jensen CD, Sato AF, McMurtry CM, Hart CN, Jelalian E. School nutrition policy: an evaluation of the Rhode Island healthier beverages policy in schools. Infant, Child, and Adolescent Nutrition 2012;4(5):276‐82. [Google Scholar]
John 2017 {published data only}
- John LK, Donnelly GE, Roberto CA. Psychologically informed implementations of sugary‐drink portion limits. Psychological Science 2017;28(5):620‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2015 {published data only}
- Jones J, Wyse R, Finch M, Lecathelinais C, Wiggers J, Marshall J, et al. Effectiveness of an intervention to facilitate the implementation of healthy eating and physical activity policies and practices in childcare services: A randomised controlled trial. Implementation Science 2015;10(1):1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2016 {published data only}
- Jones A, Magnusson R, Swinburn B, Webster J, Wood A, Sacks G, et al. Designing a healthy food partnership: lessons from the Australian food and health dialogue. BMC Public Health 2016;16:651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jue 2012 {published data only (unpublished sought but not used)}
- Jue JJ, Press MJ, McDonald D, Volpp KG, Asch DA, Mitra N, et al. The impact of price discounts and calorie messaging on beverage consumption: A multi‐site field study. Preventive Medicine 2012;55(6):629‐33. [DOI] [PubMed] [Google Scholar]
Kansagra 2015 {published data only}
- Kansagra SM, Kennelly MO, Nonas CA, Curtis CJ, Van WG, Goodman A, et al. Reducing sugary drink consumption: New York City's approach. American Journal of Public Health 2015;105(4):e61‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keast 2015 {published data only}
- Keast RS, Swinburn BA, Sayompark D, Whitelock S, Riddell LJ. Caffeine increases sugar‐sweetened beverage consumption in a free‐living population: a randomised controlled trial. British Journal of Nutrition 2015;113(2):366‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keita 2014 {published data only}
- Keita AD, Risica PM, Drenner KL, Adams I, Gorham G, Gans KM. Feasibility and acceptability of an early childhood obesity prevention intervention: results from the healthy homes, healthy families pilot study. Journal of Obesity 2014;2014:378501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keller 2016 {published data only}
- Keller J, Kahlhofer J, Peter A, Bosy‐Westphal A. Effects of low versus high glycemic index sugar‐sweetened beverages on postprandial vasodilatation and inactivity‐induced impairment of glucose metabolism in healthy men. Nutrients 2016;8(12):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kenney 2015 {published data only}
- Kenney EL, Gortmaker SL, Carter JE, Howe MC, Reiner JF, Cradock AL. Grab a cup, fill it up! an intervention to promote the convenience of drinking water and increase student water consumption during school lunch. American Journal of Public Health 2015;105(9):1777‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerr 2016 {published data only}
- Kerr DA, Harray AJ, Pollard CM, Dhaliwal SS, Delp EJ, Howat PA, et al. The connecting health and technology study: a 6‐month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2013 {published data only}
- Kim K, Park SM, Oh KW. The impact of nutritional policy on socioeconomic disparity in the unhealthy food intake among Korean adolescents. Appetite 2013;71:388‐95. [DOI] [PubMed] [Google Scholar]
Kipping 2014 {published data only}
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348:g3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klerman 2014 {published data only}
- Klerman JA, Bartlett S, Wilde P, Olsho L. The short‐run impact of the Healthy Incentives Pilot Program on fruit and vegetable intake. American Journal of Agricultural Economics 2014;96(5):1372‐82. [Google Scholar]
Klesges 2010 {published data only}
- Klesges RC, Obarzanek E, Kumanyika S, Murray DM, Klesges LM, Relyea GE, et al. The Memphis Girls' health Enrichment Multi‐site Studies (GEMS): an evaluation of the efficacy of a 2‐year obesity prevention program in African American girls. Archives of Pediatrics & Adolescent Medicine 2010;164(11):1007‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klohe‐Lehman 2007 {published data only}
- Klohe‐Lehman M, Freeland‐Graves J, Clarke KK, Cai G, Voruganti VS, Milani T, et al. Low‐income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1‐to‐3‐year‐old children. Journal of the American College of Nutrition 2007;26(3):196‐208. [DOI] [PubMed] [Google Scholar]
Kobel 2014 {published data only}
- Kobel S, Wirt T, Schreiber A, Kesztyus D, Kettner S, Erkelenz N, et al. Intervention effects of a school‐based health promotion programme on obesity related behavioural outcomes. Journal of Obesity 2014;2014(476230):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kobel 2016 {published data only}
- Kobel S, Lammle C, Wartha O, Kesztyus D, Wirt T, Steinacker JM. Effects of a randomised controlled school‐based health promotion intervention on obesity related behavioural outcomes of children with migration background. Journal of Immigrant and Minority Health 2016;19(2):254‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kocken 2012 {published data only}
- Kocken PL, Eeuwijk J, Kesteren NM, Dusseldorp E, Buijs G, Bassa‐Dafesh Z, et al. Promoting the purchase of low‐calorie foods from school vending machines: a cluster‐randomized controlled study. Journal of School Health 2012;82(3):115‐22. [DOI] [PubMed] [Google Scholar]
Korwanich 2008 {published data only}
- Korwanich K, Sheiham A, Srisuphan W, Srisilapanan P. Promoting healthy eating in nursery schoolchildren: a quasi‐experimental intervention study. Health Education Journal 2008;67(1):16‐30. [Google Scholar]
Kral 2016 {published data only}
- Kral TV, Bannon AL, Moore RH. Effects of financial incentives for the purchase of healthy groceries on dietary intake and weight outcomes among older adults: A randomized pilot study. Appetite 2016;100:110‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kubik 2011 {published data only}
- Kubik MY, Lytle LA, Farbakhsh K. School and district wellness councils and availability of low‐nutrient, energy‐dense vending fare in minnesota middle and high schools. Journal of The American Dietetic Association 2011;111(1):150‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kubik 2013 {published data only}
- Kubik MY, Davey C, Nanney MS, MacLehose RF, Nelson TF, Coombes B. Vending and school store snack and beverage trends: Minnesota secondary schools, 2002‐2010. American Journal of Preventive Medicine 2013;44(6):583‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lahlou 2015 {published data only}
- Lahlou S, Boesen‐Mariani S, Franks B, Guelinckx I. Increasing water intake of children and parents in the family setting: a randomized, controlled intervention using installation theory. Annals of Nutrition & Metabolism 2015;66:26‐30. [DOI] [PubMed] [Google Scholar]
Lao 2011 {published data only}
- Lao LS. Evaluation of a Social Networking Based SNAP‐Ed Nutrition Curriculum on Behavior Change [Thesis]. University of Rhode Island, 2011. [Google Scholar]
Laurence 2007 {published data only}
- Laurence S, Peterken R, Burns C. Fresh Kids: the efficacy of a Health Promoting Schools approach to increasing consumption of fruit and water in Australia. Health Promotion International 2007;22(3):218‐26. [DOI] [PubMed] [Google Scholar]
Lawman 2015 {published data only}
- Lawman HG, Vander Veur S, Mallya G, McCoy TA, Wojtanowski A, Colby L, et al. Changes in quantity, spending, and nutritional characteristics of adult, adolescent and child urban corner store purchases after an environmental intervention. Preventive Medicine 2015;74:81‐5. [DOI] [PubMed] [Google Scholar]
Lee 2018 {published data only}
- Lee BY, Ferguson MC, Hertenstein DL, Adam A, Zenkov E, Wang PI, et al. Simulating the impact of sugar‐sweetened beverage warning labels in three cities. American Journal of Preventive Medicine 2018;54(2):197‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee‐Kwan 2015 {published data only}
- Lee‐Kwan SH, Bleich SN, Kim H, Colantuoni E, Gittelsohn J. Environmental intervention in carryout restaurants increases sales of healthy menu items in a low‐income urban setting. American Journal of Health Promotion 2015;29(6):357‐64. [DOI] [PubMed] [Google Scholar]
Leung 2014 {published data only}
- Leung CW, Cluggish S, Villamor E, Catalano PJ, Willett WC, Rimm EB. Few changes in food security and dietary intake from short‐term participation in the Supplemental Nutrition Assistance Program among low‐income Massachusetts adults. Journal of Nutrition Education and Behavior 2014;46(1):68‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2012a {published data only (unpublished sought but not used)}
- Levy DE, Riis J, Sonnenberg LM, Barraclough SJ, Thorndike AN. Food choices of minority and low‐income employees: a cafeteria intervention. American Journal of Preventive Medicine 2012;43(3):240‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2012b {published data only}
- Levy TS, Ruan CM, Castellanos CA, Coronel AS, Aguilar AJ, Gomez Humarn IM. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Health 2012;12(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lo 2008 {published data only}
- Lo E, Coles R, Humbert ML, Polowski J, Henry CJ, Whiting SJ. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutrition Research 2008;28(3):144‐50. [DOI] [PubMed] [Google Scholar]
Loeb 2017 {published data only}
- Loeb KL, Radnitz C, Keller K, Schwartz MB, Marcus S, Pierson RN, et al. The application of defaults to optimize parents' health‐based choices for children. Appetite 2017;113:368‐75. [DOI] [PubMed] [Google Scholar]
Looney 2012 {published data only}
- Looney SM, Raynor HA. Are changes in consumption of "Healthy" foods related to changes in consumption of "Unhealthy" foods during pediatric obesity treatment?. International Journal of Environmental Research and Public Health 2012;9(4):1368‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Looney 2014 {published data only}
- Looney SM, Raynor HA. Examining the effect of three low‐intensity pediatric obesity interventions: A pilot randomized controlled trial. Clinical Pediatrics 2014;53(14):1367‐74. [DOI] [PubMed] [Google Scholar]
Loughridge 2005 {published data only}
- Loughridge JL, Barratt J. Does the provision of cooled filtered water in secondary school cafeterias increase water drinking and decrease the purchase of soft drinks?. Journal of Human Nutrition and Dietetics 2005;18(4):281‐6. [DOI] [PubMed] [Google Scholar]
Lowe 2010 {published data only}
- Lowe MR, Tappe KA, Butryn ML, Annunziato RA, Coletta MC, Ochner CN, et al. An intervention study targeting energy and nutrient intake in worksite cafeterias. Eating Behaviour 2010;11(3):144‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowndes 2012 {published data only}
- Lowndes J, Kawiecki D, Pardo S, Nguyen V, Melanson KJ, Yu Z, et al. The effects of four hypocaloric diets containing different levels of sucrose or high fructose corn syrup on weight loss and related parameters. Nutrition Journal 2012;11:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luehrmann 2014 {published data only}
- Luehrmann P, Simpson F, Sickinger S, Fuchs T, Dohnke B. Impact of the provision of mineral water on the drinking behavior of students. Ernahrungs Umschau 2014;61(6):M298‐305. [Google Scholar]
Luger 2018 {published data only}
Lumeng 2017 {published data only}
- Lumeng JC, Miller AL, Horodynski MA, Brophy‐Herb HE, Contreras D, Lee H, et al. Improving self‐regulation for obesity prevention in Head Start: a randomized controlled trial. Pediatrics 2017;139(5):1‐12. [DOI] [PubMed] [Google Scholar]
Luoto 2012 {published data only}
- Luoto J, Mahmud M, Albert J, Luby S, Najnin N, Unicomb L, et al. Learning to dislike safe water products: results from a randomized controlled trial of the effects of direct and peer experience on willingness to pay. Environmental Science & Technology 2012;46(11):6244‐51. [DOI] [PubMed] [Google Scholar]
Madjd 2015 {published data only}
- Madjd A, Taylor M A, Delavari A, Malekzadeh R, Macdonald IA, Farshchi HR. Beneficial effects of replacing diet beverages with water on type 2 diabetic obese women following a hypo‐energetic diet: A randomized, 24‐week clinical trial. Diabetes, Obesity and Metabolism 2017;19(1):125‐32. [DOI] [PubMed] [Google Scholar]
- Madjd A, Taylor MA, Delavari A, Malekzadeh R, Macdonald IA, Farshchi HR. Effects on weight loss in adults of replacing diet beverages with water during a hypoenergetic diet: a randomized, 24‐wk clinical trial. American Journal of Clinical Nutrition 2015;102(6):1305‐12. [DOI] [PubMed] [Google Scholar]
Malbon 2012 {published data only}
- Malbon, CA. Examining the Influence of an Online Health Behaviour Support Tool for High School Aged Youth [MSc Dissertation]. University of Victoria (Canada), 2012. [Google Scholar]
Mantzari 2017 {published data only}
- Mantzari E, Holl GJ, Pechey R, Jebb S, Marteau TM. Impact of bottle size on in‐home consumption of sugar‐sweetened beverages: a feasibility and acceptability study. BMC Public Health 2017;17(1):304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marcus 2009 {published data only (unpublished sought but not used)}
- Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, Ekelund U. A 4‐year, cluster‐randomized, controlled childhood obesity prevention study: STOPP. International Journal of Obesity 2009;33(4):408‐17. [DOI] [PubMed] [Google Scholar]
Maupome 2010 {published data only}
- Maupome G, Karanja N, Ritenbaugh C, Lutz T, Aickin M, Becker T. Dental caries in American Indian toddlers after a community‐based beverage intervention. Ethnicity & Disease 2010;20(4):444‐50. [PMC free article] [PubMed] [Google Scholar]
McDarby 2018 {published data only}
- McDarby F, O'Hora D, O'Shea D, Byrne M. Taking the sweetness out of the 'Share a Coke' marketing campaign: the influence of personalized labelling on elementary school children's bottled drink choices. Pediatric Obesity 2018;13(1):63‐9. [DOI] [PubMed] [Google Scholar]
McGoldrick 2006 {published data only}
- McGoldrick, KA. Sweetened Beverage Consumption of Peel Adolescents: Nutritional Correlates and Influence of the School and Neighbourhood Food Environments [MSc Dissertation]. University of Waterloo, 2006. [Google Scholar]
Mendez 2017 {published data only}
- Mendez LA, Loopstra R, McKee M, Stuckler D. Is trade liberalisation a vector for the spread of sugar‐sweetened beverages? A cross‐national longitudinal analysis of 44 low‐ and middle‐income countries. Social Science & Medicine 2017;172:21‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morley 2018 {published data only}
- Morley BC, Niven PH, Dixon HG, Swanson MG, McAleese AB, Wakefield MA. Controlled cohort evaluation of the LiveLighter mass media campaign's impact on adults' reported consumption of sugar‐sweetened beverages. BMJ Open 2018;8(4):e019574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2016 {published data only}
- Morris H, Skouteris H, Edwards S, Rutherford L, Cutter‐Mackenzie‐Knowles A, O'Connor A, et al. Feasibility of conducting a randomized trial to promote healthy eating, active play and sustainability awareness in early childhood curricula. Early Child Development and Care 2016;186(11):1752‐64. [Google Scholar]
Mozaffarian 2010 {published data only}
- Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an organizational intervention designed to improve snack and beverage quality in YMCA after‐school programs. American Journal of Public Health 2010;100(5):925‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Namba 2013 {published data only}
- Namba A, Auchincloss A, Leonberg BL, Wootan MG. Exploratory analysis of fast‐food chain restaurant menus before and after implementation of local calorie‐labeling policies, 2005‐2011. Preventing Chronic Disease 2013;10:E101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nanney 2016 {published data only}
- Nanney MS, MacLehose R, Kubik MY, Davey CS, Coombes B, Nelson TF. Recommended school policies are associated with student sugary drink and fruit and vegetable intake. Preventive Medicine 2014;62:179‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanney MS, MacLehose RF, Kubik MY, Davey CS, O'Connell MJ, Grannon KY, et al. School obesity prevention policies and practices in Minnesota and student outcomes: a longitudinal cohort study. American Journal of Preventive Medicine 2016;51(5):656‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nau 2018 {published data only}
- Nau C, Kumanyika S, Gittelsohn J, Adam A, Wong MS, Mui Y, et al. Identifying financially sustainable pricing interventions to promote healthier beverage purchases in small neighborhood stores. Preventing Chronic Disease 2018;15:E12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neumark‐Sztainer 2010 {published data only}
- Neumark‐Sztainer DR, Friend SE, Flattum CF, Hannan PJ, Story MT, Bauer KW, et al. New moves‐preventing weight‐related problems in adolescent girls: A group‐randomized study. American Journal of Preventive Medicine 2010;39(5):421‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nezami 2018 {published data only}
- Nezami BT, Ward DS, Lytle LA, Ennett ST, Tate DF. A mHealth randomized controlled trial to reduce sugar‐sweetened beverage intake in preschool‐aged children. Pediatric Obesity 2018;13(11):668‐76. [DOI: 10.1111/ijpo.12258] [DOI] [PubMed] [Google Scholar]
Nollen 2014 {published data only}
- Nollen NL, Hutcheson T, Carlson S, Rapoff M, Goggin K, Mayfield C, et al. Development and functionality of a handheld computer program to improve fruit and vegetable intake among low‐income youth. Health Education Research 2013;28(2):249‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nollen NL, Mayo MS, Carlson SE, Rapoff MA, Goggin KJ, Ellerbeck EF. Mobile technology for obesity prevention: A randomized pilot study in racial‐ and ethnic‐minority girls. American Journal of Preventive Medicine 2014;46(4):404‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nyström 2017 {published data only}
- Nyström CD, Sandin S, Henriksson P, Henriksson H, Trolle‐Lagerros Y, Larsson C, et al. Mobile‐based intervention intended to stop obesity in preschool‐aged children: the MINISTOP randomized controlled trial. American Journal of Clinical Nutrition 2017;105(6):1327‐35. [DOI] [PubMed] [Google Scholar]
Okuno 2010 {published data only}
- Okuno M, Kim MK, Mizu M, Mori M, Mori H, Yamori Y. Palatinose‐blended sugar compared with sucrose: different effects on insulin sensitivity after 12 weeks supplementation in sedentary adults. International Journal of Food Sciences and Nutrition 2010;61(6):643‐51. [DOI] [PubMed] [Google Scholar]
Olvera 2010 {published data only}
- Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community‐based mother‐daughter healthy lifestyle intervention for low‐income Latino families. Obesity 2010;18:S102‐4. [DOI] [PubMed] [Google Scholar]
Ortega 2016 {published data only}
- Ortega AN, Albert SL, Chan‐Golston AM, Langellier BA, Glik DC, Belin TR, et al. Substantial improvements not seen in health behaviors following corner store conversions in two Latino food swamps. BMC Public Health 2016;16(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ostbye 2012 {published data only}
- Ostbye T, Krause KM, Stroo M, Lovelady CA, Evenson KR, Peterson BL, et al. Parent‐focused change to prevent obesity in preschoolers: results from the KAN‐DO study. Preventive Medicine 2012;55(3):188‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2011 {published data only}
- Patel AI, Bogart LM, Elliott MN, Lamb S, Uyeda KE, Hawes‐Dawson J, et al. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Preventing Chronic Disease 2011;8(3):A60. [PMC free article] [PubMed] [Google Scholar]
Patel 2016 {published data only (unpublished sought but not used)}
- Patel AI, Grummon AH, Hampton KE, Oliva A, McCulloch CE, Brindis CD. A trial of the efficacy and cost of water delivery systems in San Francisco bay area middle schools, 2013. Preventing Chronic Disease 2016;13:E88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pbert 2013 {published data only}
- Pbert L, Druker S, Gapinski MA, Gellar L, Magner R, Reed G, et al. A school nurse‐delivered intervention for overweight and obese adolescents. Journal of School Health 2013;83(3):182‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peters 2016b {published data only}
- Peters JC, Beck J, Cardel M, Wyatt HR, Foster G D, Pan Z, et al. The effects of water and non‐nutritive sweetened beverages on weight loss and weight maintenance: A randomized clinical trial. Obesity 2016;24(2):297‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters JC, Wyatt HR, Foster GD, Pan Z, Wojtanowski AC, Vander Veur SS, et al. The effects of water and non‐nutritive sweetened beverages on weight loss during a 12‐week weight loss treatment program. Obesity 2014;22(6):1415‐21. [DOI] [PubMed] [Google Scholar]
Pinket 2016 {published data only}
- Pinket AS, Lippevelde W, Bourdeaudhuij I, Deforche B, Cardon G, Androutsos O, et al. Effect and process evaluation of a cluster randomized control trial on water intake and beverage consumption in preschoolers from six european countries: the Toybox‐study. PLoS One 2016;11(4):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Policastro 2017 {published data only}
- Policastro P, Palm T, Schwartz J, Chapman G. Targeted calorie message promotes healthy beverage consumption better than charity incentive. Obesity (Silver Spring) 2017;25(8):1428‐34. [DOI] [PubMed] [Google Scholar]
Raynor 2012 {published data only}
- Raynor HA, Osterholt KM, Hart CN, Jelalian E, Vivier P, Wing RR. Efficacy of US paediatric obesity primary care guidelines: two randomized trials. Pediatric Obesity 2012;7(1):28‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reid 2014 {published data only}
- Reid M, Hammersley R, Duffy M, Ballantyne C. Effects on obese women of the sugar sucrose added to the diet over 28 d: a quasi‐randomised, single‐blind, controlled trial. British Journal of Nutrition 2014;111(3):563‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinhold 2015 {published data only}
- Reinhold MM. Exploring the Reach and Representativeness of Participants Enrolled in a Behavioral Intervention Targeting Sugar‐Sweetened Beverage Consumption [Thesis]. Virginia Polytechnic Institute and State University, 2015. [Google Scholar]
Roberto 2016 {published data only}
- Roberto CA, Wong D, Musicus A, Hammond D. The influence of sugar‐sweetened beverage health warning labels on parents' choices. Pediatrics 2016;137(2):1‐12. [DOI] [PubMed] [Google Scholar]
Rodriguez‐Cano 2015 {published data only}
- Rodriguez‐Cano A, Mier‐Cabrera J, Balas‐Nakash M, Muñoz‐Manrique C, Legorreta‐Legorreta J, Perichart‐Perera O. Dietary changes associated with improvement of metabolic syndrome components in postmenopausal women receiving two different nutrition interventions. Menopause 2015;22(7):758‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rogers 2013 {published data only}
- Rogers VW, Hart PH, Motyka E, Rines EN, Vine J, Deatrick DA. Impact of Let's Go! 5‐2‐1‐0: a community‐based, multisetting childhood obesity prevention program. Journal of Pediatric Psychology 2013;38(9):1010‐20. [DOI] [PubMed] [Google Scholar]
Rogus 2017 {published data only}
- Rogus S, Athens J, Cantor J, Elbel B. Measuring micro‐level effects of a new supermarket: do residents within 0.5 mile have improved dietary behaviors?. Journal of the Academy of Nutrition and Dietetics 2017;118(6):1037‐46. [DOI] [PubMed] [Google Scholar]
Rosario 2013 {published data only}
- Rosario R, Araujo A, Oliveira B, Padrao P, Lopes O, Teixeira V, et al. Impact of an intervention through teachers to prevent consumption of low nutrition, energy‐dense foods and beverages: a randomized trial. Preventive Medicine 2013;57(1):20‐5. [DOI] [PubMed] [Google Scholar]
Rosenkranz 2010 {published data only}
- Rosenkranz RR, Behrens TK, Dzewaltowski DA. A group‐randomized controlled trial for health promotion in girl scouts: Healthier troops in a SNAP (Scouting Nutrition & Activity Program). BMC Public Health 2010;10:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosi 2017 {published data only}
- Rosi A, Zerbini C, Pellegrini N, Scazzina F, Brighenti F, Lugli G. How to improve food choices through vending machines: The importance of healthy food availability and consumers’ awareness. Food Quality and Preference 2017;62:262‐9. [Google Scholar]
Sacks 2011 {published data only}
- Sacks G, Tikellis K, Millar L, Swinburn B. Impact of 'traffic‐light' nutrition information on online food purchases in Australia. Australian and New Zealand Journal of Public Health 2011;35(2):122‐6. [DOI] [PubMed] [Google Scholar]
Safdie 2013 {published data only}
- Safdie M, Levesque L, Gonzalez‐Casanova Is, Salvo D, Islas A, Hernández‐Cordero S, et al. Promoting healthful diet and physical activity in the Mexican school system for the prevention of obesity in children. Salud Publica de Mexico 2013;55:357‐73. [DOI] [PubMed] [Google Scholar]
Sanchez‐Vaznaugh 2010 {published data only}
- Sanchez‐Vaznaugh EV, Sánchez BN, Baek J, Crawford PB. 'Competitive' food and beverage policies: are they influencing childhood overweight trends?. Health Affairs 2010;29(3):436‐46. [DOI] [PubMed] [Google Scholar]
Sanchez‐Vaznaugh 2015 {published data only}
- Sanchez‐Vaznaugh EV, Sánchez BN, Crawford PB, Egerter S. Association between competitive food and beverage policies in elementary schools and childhood overweight/obesity trends differences by neighborhood socioeconomic resources. JAMA Pediatrics 2015;169(5):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schroeder 2015 {published data only}
- Schroeder N, Rushovich B, Bartlett E, Sharma S, Gittelsohn J, Caballero B. Early obesity prevention: a randomized trial of a practice‐based intervention in 0‐24‐month infants. Journal of Obesity 2015;2015:795859. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seah 2018 {published data only}
- Seah SS, Rebello SA, Tai BC, Tay Z, Finkelstein EA, Dam RM. Impact of tax and subsidy framed messages on high‐ and lower‐sugar beverages sold in vending machines: a randomized crossover trial. International Journal of Behavioral Nutrition and Physical Activity 2018;15(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shahril 2013 {published data only}
- Shahril MR, Wan Dali WP, Lua PL. A 10‐week multimodal nutrition education intervention improves dietary intake among university students: Cluster randomised controlled trial. Journal of Nutrition and Metabolism 2013;2013:658642. [DOI: 10.1155/2013/658642] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shamah 2012 {published data only}
- Shamah LT, Morales RC, Amaya CC, Salazar CA, Jiménez AA, Méndez GHI. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Health 2012;12(1):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shuster 1992 {published data only}
- Shuster J, Jenkins A, Logan C, Barnett T, Riehle R, Zackson D, et al. Soft drink consumption and urinary stone recurrence: a randomized prevention trial. Journal of Clinical Epidemiology 1992;45(8):911‐6. [DOI] [PubMed] [Google Scholar]
Sichieri 2009 {published data only (unpublished sought but not used)}
- Sichieri R, Paula Trotte A, Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutrition 2009;12(2):197‐202. [DOI] [PubMed] [Google Scholar]
Sichieri 2013 {published data only}
- Sichieri R, Yokoo EM, Pereira RA, Veiga GV. Water and sugar‐sweetened beverage consumption and changes in BMI among Brazilian fourth graders after 1‐year follow‐up. Public Health Nutrition 2013;16(1):73‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siega‐Riz 2011 {published data only}
- Siega‐Riz AM, Ghormli L, Mobley C, Gillis B, Stadler D, Hartstein J, et al. The effects of the HEALTHY study intervention on middle school student dietary intakes. International Journal of Behavioral Nutrition and Physical Activity 2011;8:7. [DOI: 10.1186/1479-5868-8-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2013 {published data only}
- Simon PA, Lightstone AS, Baldwin S, Kuo T, Shih M, Fielding JE. Declines in sugar‐sweetened beverage consumption among children in Los Angeles County, 2007 and 2011. Preventing Chronic Disease 2013;10:E131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2009 {published data only}
- Singh AS, Chin AP, Brug J, Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school‐based program on body composition and behavior. Archives of Pediatrics & Adolescent Medicine 2009;163(4):309‐17. [DOI] [PubMed] [Google Scholar]
Singhal 2010 {published data only}
- Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school‐based multi‐component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. European Journal of Clinical Nutrition 2010;64(4):364‐73. [DOI] [PubMed] [Google Scholar]
Skouteris 2016 {published data only}
- Skouteris H, Hill B, McCabe M, Swinburn B, Busija L. A parent‐based intervention to promote healthy eating and active behaviours in pre‐school children: evaluation of the MEND 2‐4 randomized controlled trial. Pediatric Obesity 2016;11(1):4‐10. [DOI] [PubMed] [Google Scholar]
Smit 2016 {published data only}
- Smit CR, Leeuw RN, Bevelander KE, Burk WJ, Buijzen M. A social network‐based intervention stimulating peer influence on children's self‐reported water consumption: a randomized control trial. Appetite 2016;103:294‐301. [DOI] [PubMed] [Google Scholar]
Smith 2014 {published data only}
- Smith LH, Holloman C. Piloting "Sodabriety": A school‐based intervention to impact sugar‐sweetened beverage consumption in rural Appalachian high schools. Journal of School Health 2014;84(3):177‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sobko 2011 {published data only}
- Sobko T, Svensson V, Ek A, Ekstedt M, Karlsson H, Johansson E, et al. A randomised controlled trial for overweight and obese parents to prevent childhood obesity‐‐Early STOPP (STockholm Obesity Prevention Program). BMC Public Health 2011;11:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Song 2009 {published data only}
- Song H, Gittelsohn J, Kim M, Suratkar S, Sharma S, Anliker J. A corner store intervention in a low‐income urban community is associated with increased availability and sales of some healthy foods. Public Health Nutrition 2009;12(11):2060‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stettler 2014 {published data only}
- Stettler N, Wrotniak BH, Hill DL, Kumanyika SK, Xanthopoulos MS, Nihtianova S, et al. Prevention of excess weight gain in paediatric primary care: beverages only or multiple lifestyle factors. The Smart Step Study, a cluster‐randomized clinical trial. Pediatric Obesity 2014;10(4):267‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steyn 2015 {published data only}
- Steyn NP, Villiers A, Gwebushe N, Draper CE, Hill J, Waal M, et al. Did HealthKick, a randomised controlled trial primary school nutrition intervention improve dietary quality of children in low‐income settings in South Africa?. BMC Public Health 2015;15(1):948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Storey 2010 {published data only}
- Storey M. The shifting beverage landscape. Physiology & Behavior 2010;100(1):10‐4. [DOI] [PubMed] [Google Scholar]
Story 2012 {published data only}
- Story M, Hannan PJ, Fulkerson JA, Rock BH, Smyth M, Arcan C, et al. Bright start: description and main outcomes from a group‐randomized obesity prevention trial in American Indian children. Obesity 2012;20(11):2241‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Strauss 2011 {published data only}
- Strauss A, Herbert B, Mitschek C, Duvinage K, Koletzko B. TigerKids: successful health promotion in preschool settings. Bundesgesundheitsblatt ‐ Gesundheitsforschung ‐ Gesundheitsschutz 2011;54(3):322‐9. [DOI] [PubMed] [Google Scholar]
Strippel 2010 {published data only}
- Strippel H. Effectiveness of structured comprehensive paediatric oral health education for parents of children less than two years of age in Germany. Community Dental Health 2010;27(2):74‐80. [PubMed] [Google Scholar]
Sturm 2013 {published data only}
- Sturm R, An R, Segal D, Patel D. A cash‐back rebate program for healthy food purchases in South Africa: results from scanner data. American Journal of Preventive Medicine 2013;44(6):567‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sutherland 2010 {published data only}
- Sutherland LA, Kaley LA, Fischer L. Guiding Stars: The effect of a nutrition navigation program on consumer purchases at the supermarket. American Journal of Clinical Nutrition 2010;91(4):1090S‐4S. [DOI] [PubMed] [Google Scholar]
Swinburn 2014 {published data only}
- Swinburn B, Malakellis M, Moodie M, Waters E, Gibbs L, Millar L, et al. Large reductions in child overweight and obesity in intervention and comparison communities 3 years after a community project. Pediatric Obesity 2014;9(6):455‐62. [DOI] [PubMed] [Google Scholar]
Taljaard 2013 {published data only}
- Taljaard C, Covic NM, Graan AE, Kruger HS, Smuts CM, Baumgartner J, et al. Effects of a multi‐micronutrient‐fortified beverage, with and without sugar, on growth and cognition in South African schoolchildren: a randomised, double‐blind, controlled intervention. British Journal of Nutrition 2013;110(12):2271‐84. [DOI] [PubMed] [Google Scholar]
Taylor 2007 {published data only}
- Taylor RW, McAuley KA, Barbezat W, Strong A, Williams SM, Mann JI. APPLE Project: 2‐y findings of a community‐based obesity prevention program in primary school‐age children. American Journal of Clinical Nutrition 2007;86(3):735‐42. [DOI] [PubMed] [Google Scholar]
Teufel 1998 {published data only}
- Teufel NI, Ritenbaugh CK. Development of a primary prevention program: insight gained in the Zuni Diabetes Prevention Program. Clinical Pediatrics 1998;37(2):131‐41. [DOI] [PubMed] [Google Scholar]
Thiele 1989 {published data only}
- Thiele MC, Boushey CJ. Soft drink consumption among Yup'ik Eskimo teenagers. Alaska Medicine 1989;31(1):1‐3. [PubMed] [Google Scholar]
Thompson 2008 {published data only}
- Thompson JL, Allen P, Helitzer DL, Qualls C, Whyte AN, Wolfe VK, et al. Reducing diabetes risk in American Indian women. American Journal of Preventive Medicine 2008;34(3):192‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorndike 2012 {published data only}
- Thorndike AN, Riis J, Sonnenberg LM, Levy DE. Traffic‐light labels and choice architecture promoting healthy food choices. American Journal of Preventive Medicine 2014;46(2):143‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2‐phase labeling and choice architecture intervention to improve healthy food and beverage choices. American Journal of Public Health 2012;102(3):527‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorndike 2016 {published data only}
- Thorndike AN, Riis J, Levy DE. Social norms and financial incentives to promote employees' healthy food choices: a randomized controlled trial. Preventive Medicine 2016;86:12‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thow 2015 {published data only}
- Thow AM, Sanders D, Drury E, Puoane T, Chowdhury SN, Tsolekile L, et al. Regional trade and the nutrition transition: opportunities to strengthen NCD prevention policy in the Southern African Development Community. Global Health Action 2015;8:28338. [DOI] [PMC free article] [PubMed] [Google Scholar]
Toxqui 2016 {published data only}
- Toxqui L, Vaquero MP. An intervention with mineral water decreases cardiometabolic risk biomarkers. a crossover, randomised, controlled trial with two mineral waters in moderately hypercholesterolaemic adults. Nutrients 2016;8(7):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trinies 2016 {published data only}
- Trinies V, Chard AN, Mateo T, Freeman MC. Effects of water provision and hydration on cognitive function among primary‐school pupils in Zambia: a randomized trial. PLOS One 2016;11(3):e0150071. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tucker 2011 {published data only}
- Tucker S, Lanningham‐Foster L, Murphy J, Olsen G, Orth K, Voss J, et al. A school based community partnership for promoting healthy habits for life. Journal of Community Health 2011;36(3):414‐22. [DOI] [PubMed] [Google Scholar]
Tyhurst 2015 {published data only}
- Tyhurst M. Application of The Theory of Planned Behavior in a Randomized Control Trial Targeting Sugar‐Sweetened Beverage Intake and Physical Activity in Southwest Virginia. Virginia Polytechnic Institute and State University, 2015. [Google Scholar]
Utter 2011 {published data only}
- Utter J, Scragg R, Robinson E, Warbrick J, Faeamani G, Foroughian S, et al. Evaluation of the Living 4 Life project: a youth‐led, school‐based obesity prevention study. Obesity Reviews 2011;12:51‐60. [DOI] [PubMed] [Google Scholar]
VanEpps 2016 {published data only}
- VanEpps EM, Roberto CA. The influence of sugar‐sweetened beverage warnings. American Journal of Preventive Medicine 2016;51(5):664‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Grieken 2014 {published data only}
- Grieken A, Renders CM, Veldhuis L, Looman CW, Hirasing RA, Raat H. Promotion of a healthy lifestyle among 5‐year‐old overweight children: health behavior outcomes of the 'Be active, eat right' study. BMC Public Health 2014;14:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Grieken 2017 {published data only}
- Grieken A, Vlasblom E, Wang L, Beltman M, Boere‐Boonekamp MM, L'Hoir MP, et al. Personalized web‐based advice in combination with well‐child visits to prevent overweight in young children: cluster randomized controlled trial. Journal of Medical Internet Research 2017;19(7):e268. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Walleghen 2007 {published data only}
- Walleghen EL, Orr JS, Gentile CL, Davy BM. Pre‐meal water consumption reduces meal energy intake in older but not younger subjects. Obesity 2007;15(1):93‐9. [DOI] [PubMed] [Google Scholar]
Vargas 2011 {published data only}
- Vargas IC, Sichieri R, Sandre‐Pereira G, Veiga GV. Evaluation of an obesity prevention program in adolescents of public schools. Revista de Saude Publica 2011;45(1):59‐68. [DOI] [PubMed] [Google Scholar]
Vázquez‐Durán 2016 {published data only}
- Vázquez‐Durán M, Orea‐Tejeda A, Castillo‐Martínez L, Cano‐García Á, Téllez‐Olvera L, Keirns‐Davis C. A randomized control trial for reduction of caloric and non‐caloric sweetened beverages in young adults: Effects in weight, body composition and blood pressure. Nutricion Hospitalaria 2016;33(6):1372‐8. [DOI] [PubMed] [Google Scholar]
Veitch 2011 {published data only}
- Veitch J, Singh A, Stralen MM, Mechelen W, Brug J, Chinapaw MJ. Reduction in sugar‐sweetened beverages is not associated with more water or diet drinks. Public Health Nutrition 2011;14(8):1388‐93. [DOI] [PubMed] [Google Scholar]
Velazquez 2014 {published data only}
- Velazquez CE, Pasch KE. Attention to food and beverage advertisements as measured by eye‐tracking technology and the food preferences and choices of youth. Journal of the Academy of Nutrition and Dietetics 2014;114(4):578‐82. [DOI] [PubMed] [Google Scholar]
Verbestel 2013 {published data only}
- Verbestel V, Coen V, Winckel M, Huybrechts I, Maes L, Bourdeaudhuij I. Prevention of overweight in children younger than 2 years old: a pilot cluster‐randomized controlled trial. Public Health Nutrition 2013;17(6):1384‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vermeer 2010 {published data only}
- Vermeer WM, Steenhuis IHM, Leeuwis FH, Bos Arian ER, Boer M, Seidell JC. Portion size labeling and intended soft drink consumption: the impact of labeling format and size portfolio. Journal of Nutrition Education and Behavior 2010;42(6):422‐6. [DOI] [PubMed] [Google Scholar]
Vien 2017 {published data only}
- Vien S, Luhovyy BL, Patel BP, Panahi S, Khoury D, Mollard RC, et al. Pre‐ and within‐meal effects of fluid dairy products on appetite, food intake, glycemia, and regulatory hormones in children. Applied Physiology, Nutrition, and Metabolism 2017;42(3):302‐10. [DOI] [PubMed] [Google Scholar]
Vitolo 2012 {published data only}
- Vitolo MR, Bortolini GA, Campagnolo PD, Hoffman DJ. Maternal dietary counseling reduces consumption of energy‐dense foods among infants: a randomized controlled trial. Journal of Nutrition Education and Behavior 2012;44(2):140‐7. [DOI] [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang Y, Tussing L, Odoms‐Young A, Braunschweig C, Flay B, Hedeker D, et al. Obesity prevention in low socioeconomic status urban African‐american adolescents: study design and preliminary findings of the HEALTH‐KIDS Study. European Journal of Clinical Nutrition 2006;60(1):92‐103. [DOI] [PubMed] [Google Scholar]
Wang 2016 {published data only}
- Wang ML, Lemon SC, Clausen K, Whyte J, Rosal MC. Design and methods for a community‐based intervention to reduce sugar‐sweetened beverage consumption among youth: H2GO! study. BMC Public Health 2016;16(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wansink 2014 {published data only}
- Wansink B, Hanks AS. Calorie reductions and within‐meal calorie compensation in children's meal combos. Obesity 2014;22(3):630‐2. [DOI] [PubMed] [Google Scholar]
Ward 2008 {published data only}
- Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and physical activity in child care ‐ results from an environmental intervention. American Journal of Preventive Medicine 2008;35(4):352‐6. [DOI] [PubMed] [Google Scholar]
Wardle 2000 {published data only}
- Wardle J, Huon G. An experimental investigation of the influence of health information on children's taste preferences. Health Education Research 2000;15(1):39‐44. [DOI] [PubMed] [Google Scholar]
Watt 2009 {published data only}
- Watt RG, Tull KI, Hardy R, Wiggins M, Kelly Y, Molloy B, et al. Effectiveness of a social support intervention on infant feeding practices: randomised controlled trial. Journal of Epidemiology and Community Health 2009;63(2):156‐62. [DOI] [PubMed] [Google Scholar]
Weber‐Gasparoni 2013 {published data only}
- Weber‐Gasparoni K, Warren JJ, Reeve J, Drake DR, Kramer KW, Marshall TA, et al. An effective psychoeducational intervention for early childhood caries prevention: part II. Pediatric Dentistry 2013;35(3):247‐51. [PMC free article] [PubMed] [Google Scholar]
Wennhall 2005 {published data only}
- Wennhall I, Martensson EM, Sjunnesson I, Matsson L, Schroder U, Twetman S. Caries‐preventive effect of an oral health program for preschool children in a low socio‐economic, multicultural area in Sweden: results after one year. Acta Odontologica Scandinavica 2005;63(3):163‐7. [DOI] [PubMed] [Google Scholar]
Wescott 2012 {published data only}
- Wescott RF, Fitzpatrick BM, Phillips E. Industry self‐regulation to improve student health: quantifying changes in beverage shipments to schools. American Journal of Public Health 2012;102(10):1928‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whatley Blum 2011 {published data only}
- Whatley Blum JE, Beaudoin CM, O'Brien LM, Polacsek M, Harris DE, O'Rourke KA. Impact of Maine's statewide nutrition policy on high school food environments. Preventing Chronic Disease 2011;8(1):A19. [PMC free article] [PubMed] [Google Scholar]
Williamson 2013 {published data only}
- Williamson DA, Han H, Johnson WD, Martin CK, Newton RL Jr. Modification of the school cafeteria environment can impact childhood nutrition. Results from the Wise Mind and LA Health studies. Appetite 2013;61(1):77‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Willis 2014 {published data only}
- Willis TA, George J, Hunt C, Roberts KP, Evans CE, Brown RE, et al. Combating child obesity: impact of HENRY on parenting and family lifestyle. Pediatric Obesity 2014;9(5):339‐50. [DOI] [PubMed] [Google Scholar]
Wilson 2015 {published data only}
- Wilson AL, Bogomolova S, Buckley JD. Lack of efficacy of a salience nudge for substituting selection of lower‐calorie for higher‐calorie milk in the work place. Nutrients 2015;7(6):4336‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winett 1999 {published data only}
- Winett RA, Roodman AA, Winett SG, Bajzek W, Rovniak LS, Whiteley JA. The effects of the Eat4Life Internet‐based health behavior program on the nutrition and activity practices of high school girls. Journal of Gender, Culture, and Health 1999;4(3):239‐54. [Google Scholar]
Wing 2015 {published data only}
- Wing YK, Chan NY, Yu MW, Lam SP, Zhang J, Li SX, et al. A school‐based sleep education program for adolescents: a cluster randomized trial. Pediatrics 2015;135(3):e635‐43. [DOI] [PubMed] [Google Scholar]
Wofford 2013 {published data only}
- Wofford L, Froeber D, Clinton B, Ruchman E. Free afterschool program for at‐risk African American children: findings and lessons. Family and Community Health 2013;36(4):299‐310. [DOI] [PubMed] [Google Scholar]
Wolfenden 2015 {published data only (unpublished sought but not used)}
- Wolfenden L, Kingsland M, Rowland BC, Dodds P, Gillham K, Yoong SL, et al. Improving availability, promotion and purchase of fruit and vegetable and non sugar‐sweetened drink products at community sporting clubs: a randomised trial. International Journal of Behavioral Nutrition and Physical Activity 2015;12(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wong 2017 {published data only}
- Wong JM, Ebbeling CB, Robinson L, Feldman HA, Ludwig DS. Effects of advice to drink 8 cups of water per day in adolescents with overweight or obesity: a randomized clinical trial. JAMA Pediatrics 2017;171(5):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Woodward‐Lopez 2010 {published data only}
- Woodward‐Lopez G, Gosliner W, Samuels SE, Craypo L, Kao J, Crawford PB. Lessons learned from evaluations of California's statewide school nutrition standards. American Journal of Public Health 2010;100(11):2137‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wordell 2012 {published data only}
- Wordell D, Daratha K, Mandal B, Bindler R, Butkus SN. Changes in a middle school food environment affect food behavior and food choices. Journal of the Academy of Nutrition and Dietetics 2012;112(1):137‐41. [DOI] [PubMed] [Google Scholar]
Wright 2016 {published data only}
- Wright J, Dzodzomenyo M, Fink G, Wardrop NA, Aryeetey GC, Adanu RM, et al. Subsidized sachet water to reduce diarrheal disease in young children: a feasibility study in Accra, Ghana. American Journal of Tropical Medicine and Hygiene 2016;95(1):239‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2015 {published data only}
- Xu F, Ware RS, Leslie E, Tse LA, Wang Z, Li J, et al. Effectiveness of a randomized controlled lifestyle intervention to prevent obesity among Chinese primary school students: CLICK‐Obesity Study. PLoS One 2015;10(10):e0141421. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildirim 2013 {published data only}
- Yildirim M, Singh AS, Velde SJ, Stralen MM, MacKinnon DP, Brug J, et al. Mediators of longitudinal changes in measures of adiposity in teenagers using parallel process latent growth modeling. Obesity 2013;21(11):2387‐95. [DOI] [PubMed] [Google Scholar]
Yon 2014 {published data only}
- Yon BA, Johnson RK. Elementary and middle school children's acceptance of lower calorie flavored milk as measured by milk shipment and participation in the National School Lunch Program. Journal of School Health 2014;84(3):205‐11. [DOI] [PubMed] [Google Scholar]
Zizzo 2016 {published data only}
- Zizzo DJ, Parravano M, Nakamura R, Forwood S, Suhrcke M. The impact of taxation and signposting on diet: an online field study with breakfast cereals and soft drinks. Working Papers 131, Centre for Health Economics, University of York 2016.
Zoellner 2013 {published data only}
- Zoellner J, Cook E, Chen Y, You W, Davy B, Estabrooks P. Mixed methods evaluation of a randomized control pilot trial targeting sugar‐sweetened beverage behaviors. Open Journal of Preventive Medicine 2013;3(1):51‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zoellner 2016 {published data only}
- Zoellner JM, Hedrick VE, You W, Chen Y, Davy BM, Porter KJ, et al. Effects of a behavioral and health literacy intervention to reduce sugar‐sweetened beverages: a randomized‐controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Ayala 2016 {published data only}
- Ayala GX, Castro IA, Pickrel JL, Williams CB, Lin SF, Madanat H, et al. A restaurant‐based intervention to promote sales of healthy children's menu items: The Kids' Choice Restaurant Program cluster randomized trial. BMC Public Health 2016;16(250):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kajons 2018 {published data only}
- Kajons N, David M, Gowland‐Ella J, Lewis P, Batchelor S. Thirsty? Choose Water! Behavioural interventions and water stations in secondary schools a two‐by‐two factorial randomised controlled trial. BMC Public Health 2018;18(1):788. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02877823 {published data only}
- NCT02877823. Improving cardiometabolic health of youth on antipsychotic medication [Reeves G]. clinicaltrials.gov/ct2/show/NCT02877823 (first received 24 August 2016).
NCT02914821 {published data only}
- NCT02914821. Do taxes reduce the purchasing of soda? [John, L]. clinicaltrials.gov/ct2/show/NCT02914821 (first received 26 September 2016).
NCT02996422 {published data only}
- NCT02996422. Appalachians Together Restoring the Eating Environment: improving healthy diet in rural Appalachian Kentucky [Swanson M]. clinicaltrials.gov/ct2/show/NCT02996422 (first received 19 December 2016).
NCT0306927 {published data only}
- NCT03069274. Sugar‐sweetened beverage intake substitution by water to prevent overweight in Mexican children [Castillo Martinez L]. clinicaltrials.gov/ct2/show/NCT03069274 (first received 03 March 2017).
NCT03069274 {published data only}
- NCT03069274. Sugar‐sweetened beverage intake substitution by water to prevent overweight in Mexican children [Castillo Martinez L]. clinicaltrials.gov/ct2/show/NCT03069274 (first received 3 March 2017).
NCT03181971 {published data only}
- NCT03181971. School water access, food and beverage intake, and obesity [Anisha Patel]. clinicaltrials.gov/ct2/show/NCT03181971 (first received 09 June 2017).
NCT03431051 {published data only}
- NCT03431051. The Impact of workplace food and beverage choices on health and wellness [Schmidt J]. clinicaltrials.gov/ct2/show/NCT03431051 (first received 13 February 2018).
NCT03518151 {published data only}
- NCT03518151. Women's Responses to Adjusted Product Placement and Its Effects on Diet ‐ 1 (WRAPPED1) (WRAPPED1) [University Hospital Southampton]. clinicaltrials.gov/ct2/show/NCT03518151 (first received 08 May 2018).
Oi 2018 {published data only}
- Ooi J Y, Sutherland R, Nathan N, Yoong S L, Janssen L, Wrigley J, et al. A cluster randomised controlled trial of a sugar‐sweetened beverage intervention in secondary schools: Pilot study protocol. Nutrition and Health 2 August 2018 [Epub ahead of print]:260106018791856. [DOI: 10.1177/0260106018791856] [DOI] [PubMed]
Additional references
AAP 2015
- American Academy of Pediatrics. Snacks, sweetened beverages, added sugars, and schools. Pediatrics 2015;135(3):575‐3. [DOI] [PubMed] [Google Scholar]
Abdel Rahman 2017
- Abdel Rahman A, Jomaa L, Kahale LA, Adair P, Pine C. Effectiveness of behavioral interventions to reduce the intake of sugar‐sweetened beverages in children and adolescents: a systematic review and meta‐analysis. Nutrition Reviews 2017;76(2):88‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Adams 2009
- Adams J, Zask A, Dietrich U. Tooty Fruity Vegie in Preschools: an obesity prevention intervention in preschools targeting children's movement skills and eating behaviours. Health Promotion Journal of Australia 2009;20(2):112‐9. [DOI] [PubMed] [Google Scholar]
Andreyeva 2011
- Andreyeva T, Kelly IR, Harris JL. Exposure to food advertising on television: associations with children's fast food and soft drink consumption and obesity. Economics and Human Biology 2011;9(3):221‐33. [DOI] [PubMed] [Google Scholar]
Armstrong 2011
- Armstrong R, Waters E, Doyle J, editor(s). Chapter 21: Reviews in public health and health promotion. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Arno 2016
- Arno A, Thomas S. The efficacy of nudge theory strategies in influencing adult dietary behaviour: A systematic review and meta‐analysis. BMC Public Health 2016;16(1):676. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arsenault 2017
- Arsenault BJ, Lamarche B, Despres JP. Targeting overconsumption of sugar‐sweetened beverages vs. overall poor diet quality for cardiometabolic diseases risk prevention: Place Your Bets!. Nutrients 2017;9(6):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Auerbach 2018
- Auerbach BJ, Dibey S, Vallila‐Buchman P, Kratz M, Krieger J. Review of 100% fruit juice and chronic health conditions: implications for sugar‐sweetened beverage policy. Advances in Nutrition 2018;9(2):78‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Avery 2015
- Avery A, Bostock L, McCullough F. A systematic review investigating interventions that can help reduce consumption of sugar‐sweetened beverages in children leading to changes in body fatness. Journal of Human Nutrition and Dietetics 2015;28:52‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Backholer 2016
- Backholer K, Sarink D, Beauchamp A, Keating C, Loh V, Ball K, et al. The impact of a tax on sugar‐sweetened beverages according to socio‐economic position: a systematic review of the evidence. Public Health Nutrition 2016;19(17):3070‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bassett 2008
- Bassett MT, Dumanovsky T, Huang C, Silver LD, Young C, Nonas C, et al. Purchasing behavior and calorie information at fast‐food chains in New York City, 2007. American Journal of Public Health 2008;98(8):1457‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bes‐Rastrollo 2013
- Bes‐Rastrollo M, Schulze MB, Ruiz‐Canela M, Martinez‐Gonzalez MA. Financial conflicts of Interest and reporting bias regarding the association between sugar‐sweetened beverages and weight gain: a systematic review of systematic reviews. PLoS Medicine 2013;10(12):e1001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bleich 2015
- Bleich SN, Wolfson JA. Trends in SSBs and snack consumption among children by age, body weight, and race/ethnicity. Obesity (Silver Spring) 2015;23(5):1039‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bleich 2018
- Bleich SN, Vercammen KA. The negative impact of sugar‐sweetened beverages on children's health: an update of the literature. BMC Obesits 2018;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borges 2017
- Borges MC, Louzada M, Sá TH, Laverty AA, Parra DC, Garzillo JM, et al. Artificially sweetened beverages and the response to the global obesity crisis. PLOS Medicine 2017;14(1):e1002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyland 2016
- Boyland EJ, Nolan S, Kelly B, Tudur‐Smith C, Jones A, Halford JC, et al. Advertising as a cue to consume: a systematic review and meta‐analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. American Journal of Clinical Nutrition 2016;103(2):519‐33. [DOI] [PubMed] [Google Scholar]
Budd 2015
- Budd N, Cuccia A, Jeffries JK, Prasad D, Frick KD, Powell L, et al. B'More healthy: Retail rewards ‐ Design of a multi‐level communications and pricing intervention to improve the food environment in Baltimore City. BMC Public Health 2015;15(1):283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Byrne 2011
- Byrne S, Niederdeppe J. Unintended consequences of obesity prevention messages. In: Cawley J editor(s). The Oxford Handbook of the Social Science of Obesity. Oxford: Oxford University Press, 2011:752‐71. [Google Scholar]
Cabrera Escobar 2013
- Cabrera Escobar MA, Veerman JL, Tollman SM, Bertram MY, Hofman KJ. Evidence that a tax on sugar sweetened beverages reduces the obesity rate: a meta‐analysis. BMC Public Health 2013;13:1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Canadian Food Inspection Agency 2018
- Canadian Food Inspection Agency. Serving Sizes and Reference Amounts. inspection.gc.ca/food/labelling/food‐labelling‐for‐industry/nutrition‐labelling/nutrition‐facts‐table/eng/1389198568400/1389198597278?chap=2 2018 (accessed 28 August 2018).
Cantu‐Jungles 2017
- Cantu‐Jungles TM, McCormack LA, Slaven JE, Slebodnik M, Eicher‐Miller HA. A meta‐analysis to determine the impact of restaurant menu labeling on calories and nutrients (ordered or consumed) in U.S. adults. Nutrients 2017;9(10):1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cassady 2012
- Cassady BA, Considine RV, Mattes RD. Beverage consumption, appetite, and energy intake: what did you expect?. American Journal of Clinical Nutrition 2012;95(3):587‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cawley 2016
- Cawley J. Does anything work to reduce obesity? (Yes, modestly). Journal of Health Politics, Policy and Law 2016;41(3):463‐72. [DOI] [PubMed] [Google Scholar]
CDC 2010
- CDC. The CDC Guide to Strategies for Reducing the Consumption of Sugar Sweetened beverages. stacks.cdc.gov/view/cdc/51532 (accessed 1 December 2018).
CDC 2014
- CDC. Increasing Access to Drinking Water in Schools. www.cdc.gov/healthyschools/npao/pdf/water_access_in_schools_508.pdf (accessed 1 December 2018).
CDC 2015
- Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. Social Ecological Model. www.cdc.gov/cancer/nbccedp/sem.htm (accessed 31 March 2019).
Chi 2013
- Chi DL. Reducing Alaska Native paediatric oral health disparities: a systematic review of oral health interventions and a case study on multilevel strategies to reduce sugar‐sweetened beverage intake. International Journal of Circumpolar Health 2013;72:21066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane 2011
- Cochrane Public Health Group. Guide for developing a Cochrane protocol. ph.cochrane.org/resources‐and‐guidance (accessed 1 November 2015).
Cochrane 2018
- Cochrane Methods. Methodological Expectations of Cochrane Intervention Reviews (MECIR). community.cochrane.org/mecir‐manual (accessed 28 August 2018).
Cochrane Campbell Methods Group 2011
- Ueffing E, Tugwell P, Welch V, Petticrew M, Kristjansson E, for the Campbell and Cochrane Equity Methods Group. Equity checklist for systematic review authors. equity.cochrane.org/sites/equity.cochrane.org/files/uploads/equitychecklist2011.pdf (accessed 1 October 2015).
Cope 2009
- Cope MB, Allison DB. White hat bias: examples of its presence in obesity research and a call for renewed commitment to faithfulness in research reporting. International Journal of Obesity 2009;34(1):84‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crockett 2018
- Crockett RA, King SE, Marteau TM, Prevost AT, Bignardi G, Roberts N, et al. Nutritional labelling for healthier food or non‐alcoholic drink purchasing and consumption. Cochrane Database of Systematic Reviews 2018, Issue 2. [DOI: 10.1002/14651858.CD009315.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cuffey 2015
- Cuffey J, Beatty TK, Harnack L. The potential impact of Supplemental Nutrition Assistance Program (SNAP) restrictions on expenditures: a systematic review. Public Health Nutr 2015;19(17):3216‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daniels 2010
- Daniels MC, Popkin BM. Impact of water intake on energy intake and weight status: a systematic review. Nutrition Reviews 2010;68(9):505‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
DGE 2015
- Deutsche Gesellschaft für Ernährung. What should children drink? [Presseinformation: Was sollen Kinder trinken?]. www.dge.de/presse/pm/was‐sollen‐kinder‐trinken/. Deutsche Gesellschaft für Ernährung, (accessed 1 November 2015).
Dooley 2017
- Dooley D, Moultrie NM, Sites E, Crawford PB. Primary care interventions to reduce childhood obesity and sugar‐sweetened beverage consumption: food for thought for oral health professionals. Journal of Public Health Dentistry 2017;77:S104‐s127. [DOI] [PubMed] [Google Scholar]
Drewnowski 2014
- Drewnowski A, Rehm CD. Consumption of added sugars among US children and adults by food purchase location and food source. American Journal of Clinical Nutrition. 2014;100(3):901‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dumanovsky 2011
- Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: Cross sectional customer surveys. BMJ (Online) 2011;343:d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ebrahim 2013
- Ebrahim S, Pearce N, Smeeth L, Casas JP, Jaffar S, Piot P. Tackling non‐communicable diseases in low‐ and middle‐income countries: is the evidence from high‐income countries all we need?. PLoS Medicine 2013;10(1):e1001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2012
- Elbel B, Cantor J, Mijanovich T. Potential effect of the New York City policy regarding sugared beverages. New England Journal of Medicine 2012;367(7):680‐1. [DOI] [PubMed] [Google Scholar]
EPOC 2013a
- Effective Practice, Organisation of Care (EPOC). What study designs should be included in an EPOC review? EPOC resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services. 2013. Online: epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 1 October 2015).
EPOC 2013b
- Effective Practice, Organisation of Care (EPOC). How to prepare a risk of bias table for reviews that include more than one study design. EPOC resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services. 2013. Online: epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 1 October 2015).
EPOC 2015
- Effective Practice, Organisation of Care (EPOC). Suggested risk of bias criteria for EPOC reviews. EPOC resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services 2015. Online: epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 1 October 2015).
EU 2018
- EU High Level Group on Nutrition and Physical Activity. Opinion of the High Level Group on Nutrition and Physical Activity on Added Sugars. ec.europa.eu/health/sites/health/files/nutrition_physical_activity/docs/hlg_opinion_addedsugars_school_fruitvegetablesmmilkscheme_en.pdf (accessed 26 August 2018).
European Commission 2007
- European Commission. White paper on a strategy for Europe on nutrition, overweight and obesity related health issues. ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/nutrition_wp_en.pdf. EU Commission, (accessed 1 October 2015).
Evans 2003
- Evans T, Brown H. Road traffic crashes: operationalizing equity in the context of health sector reform. International Journal of Injury Control and Safety Promotion 2003;10(1‐2):11‐2. [DOI] [PubMed] [Google Scholar]
Evans 2017
- Evans CE. Sugars and health: a review of current evidence and future policy. Proceedings of the Nutrition Society 2017;76(3):400‐7. [DOI] [PubMed] [Google Scholar]
FAO/WHO 2014
- Food, Agriculture Organization of the United Nations. World Health Organization. Rome Declaration on Nutrition. www.fao.org/3/a‐ml542e.pdf 2014.
Fernandes 2016
- Fernandes AC, Oliveira RC, Proenca RP, Curioni CC, Rodrigues VM, Fiates GM. Influence of menu labeling on food choices in real‐life settings: A systematic review. Nutrition Reviews 2016;74(8):534‐48. [DOI] [PubMed] [Google Scholar]
Fitch 2012
- Fitch C, Keim KS. Position of the Academy of Nutrition and Dietetics: use of nutritive and nonnutritive sweeteners. Journal of the Academy of Nutrition and Dietetics 2012;112(5):739‐58. [DOI] [PubMed] [Google Scholar]
Fletcher 2010
- Fletcher JM, Frisvold D, Tefft N. Taxing soft drinks and restricting access to vending machines to curb child obesity. Health Affairs (Millwood) 2010;29(5):1059‐66. [DOI] [PubMed] [Google Scholar]
Flood 2006
- Flood JE, Roe LS, Rolls BJ. The effect of increased beverage portion size on energy intake at a meal. Journal of the American Dietetic Association 2006;106(12):1984‐90; discussion 1990‐1. [DOI] [PubMed] [Google Scholar]
French 2003
- French SA, Story M, Fulkerson JA, Gerlach AF. Food environment in secondary schools: a la carte, vending machines, and food policies and practices. American Journal of Public Health 2003;93(7):1161‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gakidou 2017
- Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafati C, Abbas KM, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990‐2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1345‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gamburzew 2016
- Gamburzew A, Darcel N, Gazan R, Dubois C, Maillot M, Tomé D, et al. In‐store marketing of inexpensive foods with good nutritional quality in disadvantaged neighborhoods: Increased awareness, understanding, and purchasing. International Journal of Behavioral Nutrition and Physical Activity 2016;13(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glickman 2013
- Glickman D, Veneman A. The essential role of food and farm policy in improving health. Health Affairs 2013;32(9):1519‐21. [DOI] [PubMed] [Google Scholar]
Gortmaker 2015
- Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, et al. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Affairs (Millwood) 2015;34(11):1932‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grech 2015
- Grech A, Allman‐Farinelli M. A systematic literature review of nutrition interventions in vending machines that encourage consumers to make healthier choices. Obesity Reviews 2015;16(12):1030‐41. [DOI] [PubMed] [Google Scholar]
Greenwood 2014
- Greenwood DC, Threapleton DE, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. Association between sugar‐sweetened and artificially sweetened soft drinks and type 2 diabetes: systematic review and dose‐response meta‐analysis of prospective studies. British Journal of Nutrition 2014;112(5):725‐34. [DOI] [PubMed] [Google Scholar]
Grummon 2014
- Grummon A, Hampton K, Oliva A, Brindis C, Patel A. Water Works: A Guide to Improving Water Access and Consumption in Schools to Improve Health and Support Learning. waterinschools.org/pdfs/WaterWorksGuide2014.pdf (accessed 1 December 2018).
Guiding Stars 2018
- Guiding Stars. Guiding Stars Food Finder. food.guidingstars.com/ (accessed 30 November 2018).
Hauner 2012
- Hauner H, Bechthold A, Boeing H, Brönstrup A, Buyken A, Leschik‐Bonnet E, et al. Evidence‐based guideline of the German Nutrition Society: carbohydrate intake and prevention of nutrition‐related diseases. Annals of Nutrition and Metabolism 2012;60 (Suppl 1):1‐58. [DOI] [PubMed] [Google Scholar]
Heise 2016
- Heise TL, Katikireddi SV, Pega F, Gartlehner G, Fenton C, Griebler U, et al. Taxation of sugar‐sweetened beverages for reducing their consumption and preventing obesity or other adverse health outcomes. Cochrane Database of Systematic Reviews 2016, Issue 8. [DOI: 10.1002/14651858.CD012319] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hennessy 2015
- Hennessy M, Bleakley A, Piotrowski JT, Mallya G, Jordan A. Sugar‐sweetened beverage consumption by adult caregivers and their children: the role of drink features and advertising exposure. Health Education & Behavior 2015;42(5):677‐86. [DOI] [PubMed] [Google Scholar]
Higgins 2017a
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Higgins 2017b
- Higgins JP, Deeks JJ, Altman DG, editor(s). Chapter 16: Special topics in statistics. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
Hollands 2015
- Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Lewis HB, Wei Y, et al. Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Database of Systematic Reviews 2015, Issue 9. [DOI: 10.1002/14651858.CD011045] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsiao 2013
- Hsiao A, Wang YC. Reducing sugar‐sweetened beverage consumption: evidence, policies, and economics. Current Obesity Reports 2013;2(3):191‐9. [Google Scholar]
Hu 2013
- Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar‐sweetened beverage consumption will reduce the prevalence of obesity and obesity‐related diseases. Obesity Reviews 2013;14(8):606‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2014
- Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta‐analysis of prospective studies. Atherosclerosis 2014;234(1):11‐6. [DOI] [PubMed] [Google Scholar]
Hultcrantz 2017
- Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al. The GRADE Working Group clarifies the construct of certainty of evidence. Journal of Clinical Epidemiology 2017;87:4‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
IHME 2018
- Institute for Health Metrics and Evaluation. GBD Compare. www.healthdata.org/data‐visualization/gbd‐compare. I, (accessed 26 July 2018).
Imamura 2015
- Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta‐analysis, and estimation of population attributable fraction. BMJ 2015;351:h3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
INFORMAS 2015
- University of Auckland. International Network for Food and Obesity / non‐communicable diseases Research, Monitoring and Action Support (INFORMAS). www.fmhs.auckland.ac.nz/en/soph/global‐health/projects/informas.html (accessed 1 October 2015).
Johnson 2009
- Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009;120(11):1011‐20. [DOI] [PubMed] [Google Scholar]
Johnson 2015
- Johnson BJ, Hendrie GA, Golley RK. Reducing discretionary food and beverage intake in early childhood: a systematic review within an ecological framework. Public Health Nutrition 2015;19(9):1684‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2014
- Jones NR, Conklin AI, Suhrcke M, Monsivais P. The growing price gap between more and less healthy foods: analysis of a novel longitudinal UK dataset. PLoS One 2014;9(10):e109343. [1932‐6203: (Electronic)] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ker 2010
- Ker K, Edwards PJ, Felix LM, Blackhall K, Roberts I. Caffeine for the prevention of injuries and errors in shift workers. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD008508] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kiszko 2014
- Kiszko KM, Martinez OD, Abrams C, Elbel B. The influence of calorie labeling on food orders and consumption: a review of the literature. Journal of Community Health 2014;39(6):1248‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kit 2013
- Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL. Trends in sugar‐sweetened beverage consumption among youth and adults in the United States: 1999‐2010. American Journal of Clinical Nutrition 2013;98(1):180‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lane 2016
- Lane H, Porter K, Estabrooks P, Zoellner J. A systematic review to assess sugar‐sweetened beverage interventions for children and adolescents across the socioecological model. Journal of the Academy of Nutrition and Dietetics 2016;116(8):1295‐307.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2011
- Levy DT, Friend KB, Wang YC. A review of the literature on policies directed at the youth consumption of sugar sweetened beverages. Advances in Nutrition 2011;2(2):182S‐200S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberato 2014
- Liberato SC, Bailie R, Brimblecombe J. Nutrition interventions at point‐of‐sale to encourage healthier food purchasing: A systematic review. BMC Public Health 2014;14(1):919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liira 2014
- Liira J, Verbeek JH, Costa G, Driscoll TR, Sallinen M, Isotalo LK, et al. Pharmacological interventions for sleepiness and sleep disturbances caused by shift work. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD009776] [DOI] [PMC free article] [PubMed] [Google Scholar]
Litman 2018
- Litman EA, Gortmaker SL, Ebbeling CB, Ludwig DS. Source of bias in sugar‐sweetened beverage research: a systematic review. Public Health Nutrition 2018;21(12):2345‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Long 2015
- Long MW, Tobias DK, Cradock AL, Batchelder H, Gortmaker SL. Systematic review and meta‐analysis of the impact of restaurant menu calorie labeling. American Journal of Public Health 2015;105(5):e11‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorenc 2014
- Lorenc T, Oliver K. Adverse effects of public health interventions: a conceptual framework. Journal of Epidemiology and Community Health 2014;68(3):288‐90. [DOI] [PubMed] [Google Scholar]
Ludwig 2002
- Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 2002;287(18):2414‐23. [DOI] [PubMed] [Google Scholar]
Ludwig 2009
- Ludwig DS, Brownell KD. Public health action amid scientific uncertainty: The case of restaurant calorie labeling regulations. JAMA 2009;302(4):434‐5. [DOI] [PubMed] [Google Scholar]
Luger 2017
- Luger M, Lafontan M, Bes‐Rastrollo M, Winzer E, Yumuk V, Farpour‐Lambert N. Sugar‐sweetened beverages and weight gain in children and adults: a systematic review from 2013 to 2015 and a comparison with previous studies. Obesity Facts 2017;10(6):674‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lundh 2017
- Lundh A, Lexchin J, Mintzes B, Schroll JB, Bero L. Industry sponsorship and research outcome. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.MR000033.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
MacLean 2009
- MacLean L, Edwards N, Garrard M, Sims‐Jones N, Clinton K, Ashley L. Obesity, stigma and public health planning. Health Promotion International 2009;24(1):88‐93. [DOI] [PubMed] [Google Scholar]
Maersk 2012
- Maersk M, Belza A, Holst JJ, Fenger‐Gron M, Pedersen SB, Astrup A, et al. Satiety scores and satiety hormone response after sucrose‐sweetened soft drink compared with isocaloric semi‐skimmed milk and with non‐caloric soft drink: a controlled trial. European Journal of Clinical Nutrition. 2012/01/19 2012; Vol. 66, issue 4:523‐9. [DOI] [PubMed]
Malik 2010a
- Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar‐sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010;121(11):1356‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malik 2010b
- Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar‐sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta‐analysis. Diabetes Care 2010;33(11):2477‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malik 2013
- Malik VS, Pan A, Willett WC, Hu FB. Sugar‐sweetened beverages and weight gain in children and adults: a systematic review and meta‐analysis. American Journal of Clinical Nutrition 2013;98(4):1084‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malik 2015
- Malik VS, Hu FB. Fructose and cardiometabolic health: what the evidence from sugar‐sweetened beverages tells us. Journal of the American College of Cardiology 2015;66(14):1615‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mazarello Paes 2015
- Mazarello Paes V, Hesketh K, O'Malley C, Moore H, Summerbell C, Griffin S, et al. Determinants of sugar‐sweetened beverage consumption in young children: a systematic review. Obesity Reviews 2015;16(11):903–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKetin 2014
- McKetin R, Coen A. The effect of energy drinks on the urge to drink alcohol in young adults. Alcoholism: Clinical and Experimental Research 2014;38(8):2279‐85. [DOI] [PubMed] [Google Scholar]
Mello 2008
- Mello MM, Pomeranz J, Moran P. The interplay of public health law and industry self‐regulation: The case of sugar‐sweetened beverage sales in schools. American Journal of Public Health 2008;98(4):595‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2014
- Miller PE, Perez V. Low‐calorie sweeteners and body weight and composition: a meta‐analysis of randomized controlled trials and prospective cohort studies. American Journal of Clinical Nutrition 2014;100(3):765‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moise 2011
- Moise N, Cifuentes E, Orozco E, Willett W. Limiting the consumption of sugar sweetened beverages in Mexico's obesogenic environment: a qualitative policy review and stakeholder analysis. Journal of Public Health Policy 2011;32(4):458‐75. [DOI] [PubMed] [Google Scholar]
Moynihan 2014
- Moynihan PJ, Kelly SA. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. Journal of Dental Research 2014;93(1):8‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mozaffarian 2017
- Mozaffarian D. Conflict of interest and the role of the food industry in nutrition research. JAMA 2017;317(17):1755‐6. [DOI] [PubMed] [Google Scholar]
MSUE 2013
- MSUE. How to convert grams of sugars into teaspoons. Michigan State University Extension 2013; Vol. msue.anr.msu.edu/news/how_to_convert_grams_of_sugars_into_teaspoons.
Muckelbauer 2013
- Muckelbauer R, Sarganas G, Gruneis A, Muller‐Nordhorn J. Association between water consumption and body weight outcomes: a systematic review. American Journal of Clinical Nutrition 2013;98(2):282‐99. [DOI] [PubMed] [Google Scholar]
Nakhimovsky 2016
- Nakhimovsky SS, Feigl AB, Avila C, O'Sullivan G, Macgregor‐Skinner E, Spranca M. Taxes on sugar‐sweetened beverages to reduce overweight and obesity in middle‐income countries: a systematic review. PLoS One 2016;11(9):e0163358. [DOI] [PMC free article] [PubMed] [Google Scholar]
National Cancer Institute 2018
- National Cancer Institute. Recommendations on Potential Approaches to Dietary Assessment for Different Research Objectives Requiring Group‐level Estimates. dietassessmentprimer.cancer.gov/approach/table.html (accessed 22 June 2018).
Nestle 2015
- Nestle M. Sodas. Soda Politics. Oxford: Oxford University Press, 2015:11‐22. [Google Scholar]
Nikolaou 2015
- Nikolaou CK, Hankey CR, Lean ME. Calorie‐labelling: does it impact on calorie purchase in catering outlets and the views of young adults?. International Journal of Obesity (London) 2015;39(3):542‐5. [DOI] [PubMed] [Google Scholar]
O'Dea 2005
- O'Dea JA. Prevention of child obesity: ‘First, do no harm’. Health Education Research 2005;20(2):259‐65. [DOI] [PubMed] [Google Scholar]
O'Neill 2014
- O'Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology 2014;67(1):56‐64. [DOI] [PubMed] [Google Scholar]
Ogden 2011
- Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005–2008. National Center for Health Statistics Data Brief. Hyattsville, MD: National Center for Health Statistics, No. 71, August 2011:1‐8.
Onufrak 2014
- Onufrak SJ, Park S, Sharkey JR, Sherry B. The relationship of perceptions of tap water safety with intake of sugar‐sweetened beverages and plain water among US adults. Public Health Nutrition 2014;17(1):179‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ouzzani 2016
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan ‐ a web and mobile app for systematic reviews. Systematic Reviews 2016;5(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2014
- Park S, Onufrak S, Sherry B, Blanck HM. The relationship between health‐related knowledge and sugar‐sweetened beverage intake among US adults. Journal of the Academy of Nutrition and Dietetics 2014;114(7):1059‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2010
- Patel AI, Cabana MD. Encouraging healthy beverage intake in child care and school settings. Current Opinion in Pediatrics 2010;22(6):779‐84. [DOI] [PubMed] [Google Scholar]
Patel 2018
- Patel AI, Moghadam SD, Freedman M, Hazari A, Fang ML, Allen IE. The association of flavored milk consumption with milk and energy intake, and obesity: a systematic review. Preventive Medicine 2018;111:151‐62. [DOI] [PubMed] [Google Scholar]
Peeters 2018
- Peeters A. Obesity and the future of food policies that promote healthy diets. Nature Reviews. Endocrinology 2018;14:430–7. [DOI] [PubMed] [Google Scholar]
Pfadenhauer 2017
- Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, et al. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implementation Science 2017; Vol. 12, issue 1:1‐17. [DOI] [PMC free article] [PubMed]
Pomeranz 2012
- Pomeranz JL. Advanced policy options to regulate sugar‐sweetened beverages to support public health. Journal of Public Health Policy 2012;33(1):75‐88. [DOI] [PubMed] [Google Scholar]
Popkin 2016
- Popkin BM, Hawkes C. Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes and Endocrinology 2016;4(2):174‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poppitt 2015
- Poppitt SD. Beverage consumption: are alcoholic and sugary drinks tipping the balance towards overweight and obesity?. Nutrients 2015;7(8):6700‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powell 2014
- Powell LM, Wada R, Persky JJ, Chaloupka FJ. Employment impact of sugar‐sweetened beverage taxes. American Journal of Public Health 2014;104(4):672‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Public Health England 2015
- Public Health England. Sugar reduction. The evidence for action. www.gov.uk/government/uploads/system/uploads/attachment_data/file/470179/Sugar_reduction_The_evidence_for_action.pdf (accessed 1 November 2015).
Quirmbach 2018
- Quirmbach D, Cornelsen L, Jebb SA, Marteau T, Smith R. Effect of increasing the price of sugar‐sweetened beverages on alcoholic beverage purchases: an economic analysis of sales data. Journal of Epidemiogly and Community Health 2018;72(4):324–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramos Salas 2015
- Ramos Salas X. The ineffectiveness and unintended consequences of the public health war on obesity. Canadian Journal of Public Health 2015;106(2):e79‐81. [DOI] [PubMed] [Google Scholar]
Roberto 2015
- Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet 2015;385(9985):2400‐9. [DOI] [PubMed] [Google Scholar]
Rutter 2012
- Rutter H. The single most important intervention to tackle obesity. Internal Journal of Public Health 2012;57(4):657‐8. [DOI] [PubMed] [Google Scholar]
Rutter 2017
- Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood D T, et al. The need for a complex systems model of evidence for public health. Lancet 2017;390(10112):2602‐4. [DOI] [PubMed] [Google Scholar]
Sacco 2017
- Sacco J, Lillico HG, Chen E, Hobin E. The influence of menu labelling on food choices among children and adolescents: A systematic review of the literature. Perspectives in Public Health 2017;137(3):173‐81. [DOI] [PubMed] [Google Scholar]
Sadeghirad 2016
- Sadeghirad B, Duhaney T, Motaghipisheh S, Campbell NR, Johnston BC. Influence of unhealthy food and beverage marketing on children's dietary intake and preference: a systematic review and meta‐analysis of randomized trials. Obesity Reviews 2016;17(10):945‐59. [DOI] [PubMed] [Google Scholar]
Scharf 2016
- Scharf RJ, DeBoer MD. Sugar‐sweetened beverages and children's health. Annual Reviews of Public Health 2016;37:273‐93. [DOI] [PubMed] [Google Scholar]
Schillinger 2016
- Schillinger D, Jacobson MF. Science and public health on trial: Warning notices on advertisements for sugary drinks. JAMA 2016;316(15):1545‐6. [DOI] [PubMed] [Google Scholar]
Schünemann 2018
- Schünemann HJ, Cuello C, Akl EA, Mustafa RA, Meerpohl JJ, Thayer K, et al. GRADE Working Group. GRADE guidelines: 18. How ROBINS‐I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Journal of Clinical Epidemiology 2018; Vol. S0895‐4356, issue 17:31031‐4. [DOI: 10.1016/j.jclinepi.2018.01.012] [DOI] [PMC free article] [PubMed]
Siegel 2016c
- Siegel KR, McKeever Bullard K, Imperatore G, Kahn HS, Stein AD, Ali MK, et al. Association of higher consumption of foods derived from subsidized commodities with adverse cardiometabolic risk among US adults. JAMA Internal Medicine 2016;176(8):1124‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2015
- Singh GM, Micha R, Khatibzadeh S, Shi P, Lim S, Andrews KG, et al. Global, regional, and national consumption of sugar‐sweetened beverages, fruit juices, and milk: a systematic assessment of beverage intake in 187 countries. PLoS One 2015;10(8):e0124845. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sonntag 2015
- Sonntag D, Schneider S, Mdege N, Ali S, Schmidt B. Beyond food promotion: a systematic review on the influence of the food industry on obesity‐related dietary behaviour among children. Nutrients 2015;7(10):8565‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stephens 2013
- Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. Journal of Cardiovascular Nursing 2013;28(4):320‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stern 2014
- Stern D, Piernas C, Barquera S, Rivera JA, Popkin BM. Caloric beverages were major sources of energy among children and adults in Mexico, 1999‐2012. Journal of Nutrition 2014;144(6):949‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M. ROBINS‐I: a tool for assessing risk of bias in non‐randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2017
- Sterne JA, Egger M, Moher D, Boutron I, editor(s). Chapter 10: Addressing reporting biases. In: Higgins JP, Churchill R, Chandler J, Cumpston MS, editor(s), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Swinburn 2011
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378(9793):804‐14. [DOI] [PubMed] [Google Scholar]
Thomson 2013
- Thomson HJ, Thomas S. The effect direction plot: visual displayof non‐standardised effects across multiple outcome domains. Research Synthesis Methods 2013;4:95‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tipton 2015
- Tipton JA. Reducing sugar‐sweetened beverage intake among students: school‐based programs and policies that work. NASN School Nurse 2015;31(2):102‐10. [DOI] [PubMed] [Google Scholar]
Tugwell 2010
- Tugwell P, Petticrew M, Kristjansson E, Welch V, Ueffing E, Waters E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ 2010;341:c4739. [DOI] [PubMed] [Google Scholar]
University of Bristol 2018
- University of Bristol. Ongoing work on ROBINS‐I. www.bristol.ac.uk/population‐health‐sciences/centres/cresyda/barr/riskofbias/robins‐i/ongoing/ (accessed 27 August 2018).
USDA 2015a
- U.S. Department of Health and Human Services, U.S. Department of Agriculture. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. health.gov/dietaryguidelines/2015‐scientific‐report/. Washington, D.C.: U.S. Department of Health and Human Services, U.S. Department of Agriculture, (accessed 27 August 2018).
USDA 2015b
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. health.gov/dietaryguidelines/2015/ (accessed 1 June 2016).
Van der Horst 2007
- Horst K, Oenema A, Ferreira I, Wendel‐Vos W, Giskes K, Lenthe F, et al. A systematic review of environmental correlates of obesity‐related dietary behaviors in youth. Health Education Research 2007;22(2):203‐26. [DOI] [PubMed] [Google Scholar]
Van der Horst 2008
- Horst K, Timperio A, Crawford D, Roberts R, Brug J, Oenema A. The school food environment associations with adolescent soft drink and snack consumption. American Journal of Preventive Medicine 2008;35(3):217‐23. [DOI] [PubMed] [Google Scholar]
Van Hook 2012
- Hook J, Altman CE. Competitive food sales in schools and childhood obesity: A longitudinal study. Sociology of Education 2012;85(1):23‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vargas‐Garcia 2017
- Vargas‐Garcia EJ, Evans CE, Prestwich A, Sykes‐Muskett BJ, Hooson J, Cade JE. Interventions to reduce consumption of sugar‐sweetened beverages or increase water intake: evidence from a systematic review and meta‐analysis. Obesity Reviews 2017;18(11):1350‐63. [DOI] [PubMed] [Google Scholar]
Vartanian 2007
- Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta‐analysis. American Journal of Public Health 2007;97(4):667‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vercammen 2018
Vericker 2013
- Vericker TC. Limited evidence that competitive food and beverage practices affect adolescent consumption behaviors. Health Education & Behavior 2013;40(1):19‐23. [DOI] [PubMed] [Google Scholar]
Verloigne 2012
- Verloigne M, Lippevelde W, Maes L, Brug J, Bourdeaudhuij I. Family‐ and school‐based correlates of energy balance‐related behaviours in 10‐12‐year‐old children: a systematic review within the ENERGY (EuropeaN Energy balance Research to prevent excessive weight Gain among Youth) project. Public Health Nutrition 2012;15(8):1380‐95. [DOI] [PubMed] [Google Scholar]
Vodopivec‐Jamsek 2012
- Vodopivec‐Jamsek V, Jongh T, Gurol‐Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007457.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vos 2016
- Vos MB, Kaar JL, Welsh JA, Horn LV, Feig DI, Anderson CA, et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American Heart Association. Circulation 2016;134:1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vézina‐Im 2017
- Vézina‐Im LA, Beaulieu D, Belanger‐Gravel A, Boucher D, Sirois C, Dugas M, et al. Efficacy of school‐based interventions aimed at decreasing sugar‐sweetened beverage consumption among adolescents: a systematic review. Public Health Nutrition 2017;20(13):2416‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
WCRFI 2015
- World Cancer Research Fund International. NOURISHING framework. www.wcrf.org/int/policy/nourishing‐framework (accessed 1 October 2015).
WHO 2013
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases. www.who.int/nmh/events/ncd_action_plan/en/. WHO, (accessed 1 October 2015).
WHO‐EURO 2014
- World Health Organization Regional Office for Europe. European Food and Nutrition Action Plan 2015–2020. www.euro.who.int/__data/assets/pdf_file/0008/253727/64wd14e_FoodNutAP_140426.pdf (accessed 1 November 2015).
Wolf 2008
- Wolf A, Bray GA, Popkin BM. A short history of beverages and how our body treats them. Obesity Reviews 2008;9(2):151‐64. [DOI] [PubMed] [Google Scholar]
Yoshida 2018
- Yoshida Y, Simoes EJ. Sugar‐sweetened beverage, obesity, and type 2 diabetes in children and adolescents: policies, taxation, and programs. Current Diabetes Reports 2018;18(6):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Von Philipsborn 2016
- Philipsborn P, Stratil JM, Burns J, Busert LK, Pfadenhauer LM, Polus S, et al. Environmental interventions to reduce the consumption of sugar‐sweetened beverages and their effects on health. Cochrane Database of Systematic Reviews 2016, Issue 7. [DOI: 10.1002/14651858.CD012292] [DOI] [PMC free article] [PubMed] [Google Scholar]