Abstract
Background/Aims
Liver fibrosis is a chronic liver injury affecting numerous individuals in the world, and efforts have been exercised for introducing a non-invasive method to evaluate the stages of liver fibrosis, which can be used instead of invasive methods, such as a liver biopsy. Various glycoproteins have been suggested by many investigators as indicators of liver fibrosis. This study aimed to compare the diagnostic accuracy of serum laminin, fibronectin, and hyaluronic acid levels in the assessment of liver fibrosis for discriminating patients from healthy subjects.
Materials and Methods
We searched the English language literature to identify relevant studies regarding the role of glycoproteins in the assessment of liver fibrosis, using the following electronic databases: Medline, PubMed central, web of knowledge (ISI), Scopus, Google scholar, Springer, and Science Direct from 1981 to 2016. The key words used for searching were “glycoproteins”, “laminin”, “hyaluronic acid”, “fibronectin”, “diagnostic accuracy”, “assessment”, “liver fibrosis”, “cirrhosis”, “liver biopsy”, “grading”, and “staging”. The statistical data relevant for the diagnostic accuracy were extracted and analyzed using the summary receiver operating characteristic curves.
Results
The diagnostic accuracy among the glycoproteins involved in this study were compared, and the area under curves for serum levels of laminin, hyaluronic acid, and fibronectin, as indicators of diagnostic accuracy, were 0.89, 0.82, and 0.73, respectively.
Conclusion
It can be concluded that when liver biopsy is contraindicated, the serum levels of laminin, hyaluronic acid, and fibronectin can be considered screening tests as well as additional clinically useful tools for the evaluation of liver fibrosis.
Keywords: Diagnostic accuracy, fibronectin, hyaluronic acid, laminin, liver fibrosis
INTRODUCTION
Liver fibrosis is a chronic liver injury characterized by the accumulation of extracellular matrix (ECM), including noncollagenous glycoproteins (1,2). Hyaluronic acid, laminin, fibronectin, merosin, tenascin, and nidogen are the main glycoproteins involved in liver functions (3). To the best of our knowledge, most researches to date have focused on the role of hyaluronic acid, laminin, and to some extent fibronectin in the assessment of liver fibrosis (4–6). Therefore, in this study, we chose to focus on these three glycoproteins as well.
The non-collagenous glycoprotein laminin is synthesized by hepatic stellate cells (HSC) and deposited in the liver’s basement membrane. It has been found that there is a good correlation between serum laminin levels and liver fibrosis development (4–6). Laminin has been introduced as one of the main basement membrane glycoproteins of the liver (6,7) firstly identified in a murine fibrosarcoma, the Engelbreth Holm-Swan tumor, by Timpl and Martin in 1979 (8). Laminin is a large complex structure (about 850 kDa) including three chains of α1 (about 440 kDa), β1, and γ1 (each about 200 kDa) proteins. These chains create a characteristic cross-shaped asymmetrical structure intertwined by disulphide bridges. The laminin receptors can be found on the surface of many cells, for instance, platelets, muscle cells, neutrophils, endothelial cells, and hepatocytes (8). Laminin has important roles in biological functions, including cellular adhesion and binding to collagens and glycoaminoglycans as matrix constituents (7), cytoskeleton maintenance (9), and fibrogenesis mechanisms related to hepatic fibrosis. It has been reported that serum laminin can reflect the activity of liver fibrosis (10).
Fibronectin is a multifunctional glycoprotein of the ECM with a high molecular weight. It has been reported that there is a negative correlation between serum fibronectin level and liver fibrosis (11,12). Fibronectin is mainly secreted and synthesized by endothelial cells, Kupffer cells, and hepatocytes and can be found on the cell surface, blood, and bodily fluids. Fibronectin is involved in many biological functions, such as immunity, platelet aggregation, cell adhesion, and blood coagulation (13). Plasma fibronectin is one of the most abundant matrix proteins in the normal liver and is synthesized by hepatocytes. Plasma fibronectin comprises a major part of the low-density matrix in the subendothelial space of Disse connecting the hepatocytes. However, cellular fibronectin (cFn) can be detected in the liver at very low levels. A wide range of pathogenic mechanisms may result in liver damage, including autoimmune diseases, genetic disorders, viral infection, disorders of uncertain etiology, those attributed to systemic disease, and toxic insult. The hepatic sinusoidal endothelial cells (SECs) are activated in response to injury and increase the production of cFn. As this event occurs in the earliest stages of liver damage, it would thereby be helpful in the earlier detection of harmful stimuli. Similar studies have reported that fibronectin is significant in the early stages of liver fibrosis and acts as a chemotactic for collagen-producing cells providing a skeleton for collagen formation (14). Therefore, the fibronectin serum level increases with the advancement of liver fibrosis but finally decreases in patients with cirrhosis due to hepatic dysfunction (15).
Hyaluronic acid is a glycosaminoglycan found in the ECM, synthesized by HSC, and degraded by the SECs (16). Hyaluronic acid is a linear chain, non-sulfated, high molecular weight glycosaminoglycan present in the extracellular, pericellular, and intracellular spaces and various body parts in different concentrations, sizes, and shapes. Hyaluronic acid is composed of hexuronic and amino sugar with acetyl groups ((1→3)-β-D-GlcNAc-(1→4)-β-D-GlcA) for which the liver is the major tissue for the removal and synthesis of that. In normal conditions, the hyaluronic acid uptake and degradation occur in the hepatic SECs, and a decrease in hepatic removal or increase in production results in an increase in serum hyaluronic acid. Therefore, the serum hyaluronic acid level has had a reliable clinical application in liver diseases, including hepatitis B and C viruses (HBV and HCV), alcoholic or non-alcoholic steatohepatitis, and hepatic immune disease, and it has been reported that serum hyaluronic acid level is significantly higher in patients with liver diseases and particularly those with cirrhosis (16,17). In this study, we aimed to compare the diagnostic accuracy of serum laminin, fibronectin, and hyaluronic acid as glycoproteins involved in the assessment of liver fibrosis and to discriminate patients from healthy subjects.
MATERIALS AND METHODS
To identify the relevant studies, considering the consent of the participants and approval of Ethics Committee, we searched the English language literature regarding the role of glycoproteins in the assessment of liver fibrosis, Firstly, the following electronic databases were searched to identify relevant studies from 1981 to 2016: Medline, PubMed central, Scopus, Google scholar, Springer, and Science Direct. The key search words used were: “glycoprotein,” “laminin,” “hyaluronic acid,” “fibronectin,” “diagnostic accuracy,” “assessment,” “liver fibrosis,” “cirrhosis,” “liver biopsy,” “grading,” and “staging.” The number of searches for some of the main keywords in various databases can be seen in Table 1. Secondly, the titles and abstracts were reviewed and selected based on certain criteria mentioned subsequently. Studies were excluded from the review if the abstract provided did not fulfill the primary objective or if the full-text was not available. In the following step, a manual retrieval of references cited in the selected articles was performed to find additional, potentially relevant, publications. Finally, all selected papers were read for primary evaluation and for minimizing the risk of bias. The checklist of the method of “Assessing the Methodological Quality of Systematic Reviews (AMSTAR)” (18) was followed carefully and discussed with both co-authors of this article.
Table 1.
Search results of main keywords in various databases
| Keywords | Medline | PubMed central | Scopus | Google scholar | Springer | Science Direct |
|---|---|---|---|---|---|---|
| Glycoprotein | 1648 | 316199 | 290351 | 1610000 | 384 | 290351 |
| Laminin | 98 | 48433 | 50410 | 346000 | 380 | 50410 |
| Hyaluronic acid | 421 | 23122 | 36998 | 294000 | 4512 | 36998 |
| Fibronectin | 308 | 80529 | 82951 | 725000 | 810 | 82951 |
| Liver fibrosis | 3136 | 151178 | 133810 | 1900000 | 2685 | 133813 |
| Cirrhosis | 7385 | 299832 | 153855 | 1130000 | 221 | 153858 |
| Liver biopsy | 2214 | 310432 | 202684 | 1910000 | 2948 | 202688 |
Statistical analysis
For comparing the diagnostic accuracy of these glycoproteins, the relevant data were firstly summarized. Thereafter, to compare the diagnostic accuracies of glycoproteins, including laminin, fibronectin, and hyaluronic acid, according to the Joanna Briggs Institute Reviewers’ manual 2015 (19), pooled sensitivity, specificity, and summary receiver operating characteristic (ROC) curves were calculated using the MetaDiSk version 1.4 (Clinical Biostatistics Unit, Ramón y Cajal Hospital, Madrid, Spain).
RESULTS
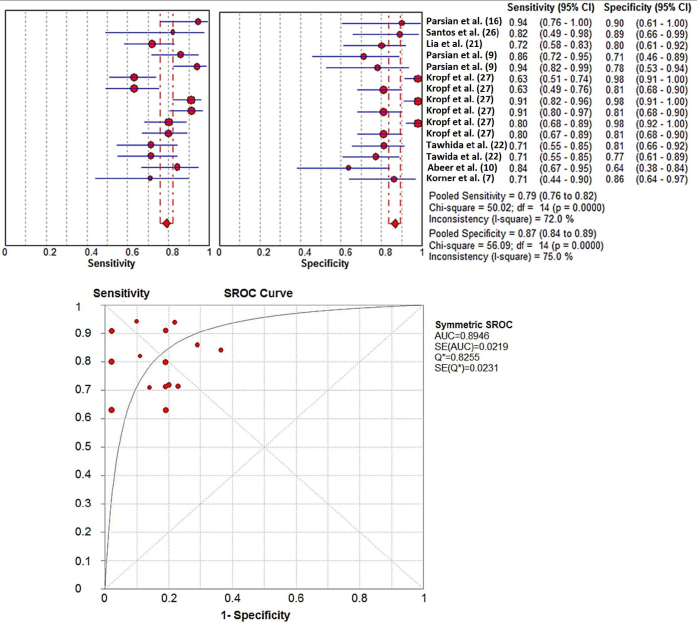
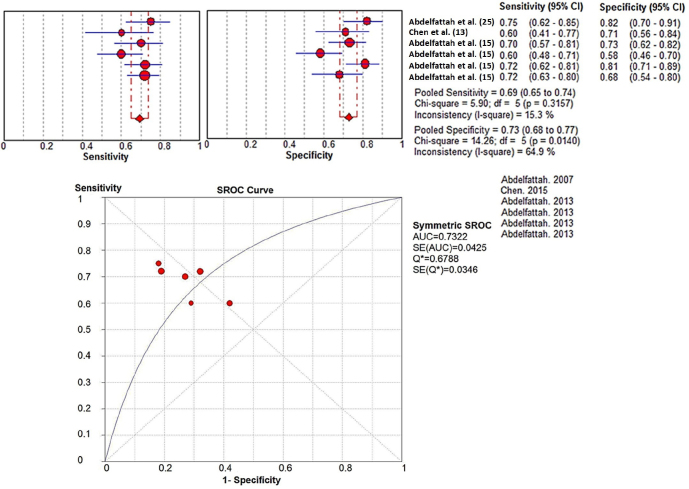
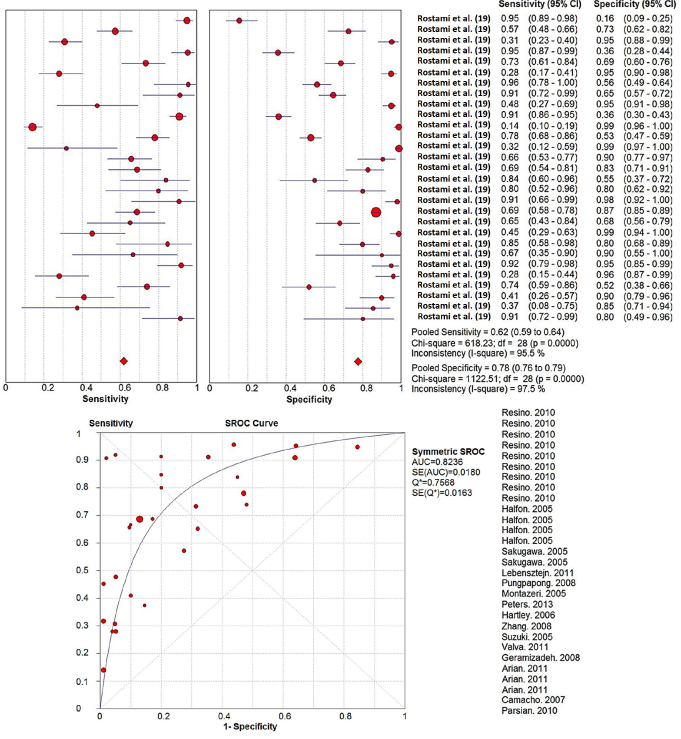
According to the studies in literature, the diagnostic accuracy of laminin and fibronectin in the assessment of liver fibrosis is summarized in Tables 2 and 3, respectively. For hyaluronic acid, the relevant data were used from the review paper by Rostami et al. (20). To compare the diagnostic accuracies of these glycoproteins in the assessment of liver fibrosis, the pooled sensitivity, specificity, and summary ROC curve was calculated accordingly (Figures 1–3).
Table 2.
The clinical application of serum laminin concentration in the assessment of liver fibrosis
| Etiology | N | Stage | Cut off | AUC | Se. (%) | Sp. (%) | NPV (%) | PPV (%) | Conclusion | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
| Hepatitis B and C | 38 | Fibrosis/cirrhosis | 2.6 U/mL (591 ng/mL) | 71 | 86 | 80 | Serum laminin can be considered a prognostic marker in liver cirrhosis. | (7) | ||
| Hepatitis B and C and AIH patients (severe vs. mild liver fibrosis). | 62 | F0-6 | 92.5 ng/mL | 0.879 | 86 | 71 | 69 | 87 | When liver biopsy is contraindicated, serum laminin levels may be useful as an additional non-invasive tool for liver fibrosis evaluation. | (9) |
| Hepatitis B and C and AIH patients (with liver fibrosis vs. without liver fibrosis) | 52.0 ng/mL | 0.974 | 94 | 78 | 86 | 91 | ||||
| Hepatitis B | 50 | F01234 | 107.5 ng/mL | 84.2 | 63.6 | 70 | 80 | Serum laminin levels could be clinically useful serum markers for predicting significant fibrosis in patients, especially when liver biopsy is contraindicated. | (10) | |
| Chronic hepatitis B | 35 | F0-6 | 64.0 ng/mL | 0.986 | 94.3 | 90 | 90 | 94.3 | Serum laminin levels can be considered an additional clinical tool for assessment of liver fibrosis, where it is impossible to perform liver biopsy. | (16) |
| Chronic hepatitis B | 87 | F ≥ 2 | 132.7 ng/mL | 0.815 | 71.9 | 80 | 60 | 87.2 | Serum laminin levels showed a positive correlation with liver fibrosis stages and would clinically be a useful serum marker for predicting significant fibrosis in patients, when liver biopsy is contraindicated. | (22) |
| Hepatitis B and C virus | 80 | Cirrhosis (F6) | 63.7 ng/mL | 0.76 | 71.4 | 81 | 73.9 | 78.9 | Serum laminin level could be used in reducing liver biopsy rates but cannot replace it. | (23) |
| Fibrosis (F>2) | 60.9 ng/mL | 0.82 | 71.4 | 77.1 | 72.9 | 75.7 | ||||
| Patient with NAFLD | 30 | F 0-4 | 282 ng/ml | 82 | 89 | 89 | 82 | Serum laminin levels may identify patients with NAFLD and fibrosis and can be considered indicators for liver biopsy. | (27) | |
| Healthy subjects | 146 | Fibrosis | 330 ng/mL | 63 | 98 | 72 | 97 | Determination of laminin cannot replace conventional diagnostic methods, and the clinical value of measuring serum laminin as a screening test for this kind of hepatic disease is not known. | (28) | |
| Patients with non hepatic diseases | 112 | Fibrosis | 63 | 81 | 68 | 77 | ||||
| Healthy subjects | 146 | Cirrhosis | 91 | 98 | 92 | 98 | ||||
| Patients with non hepatic diseases | 112 | Cirrhosis | 91 | 81 | 91 | 83 | ||||
| Healthy subjects | 146 | All | 80 | 98 | 83 | 97 | ||||
| Patients with non hepatic diseases | 112 | All | 80 | 81 | 80 | 81 |
N: number of cases, AUC: area under the curve; Se: Sensitivity; Sp: Specificity; NPV: Negative predictive value; PPV: Positive predictive value; NAFLD: non-alcoholic fatty liver disease
Table 3.
The clinical application of serum fibronectin concentration in the assessment of liver fibrosis
| Etiology | N | Stage | Cut off | AUC | Se. (%) | Sp. (%) | NPV (%) | PPV (%) | Conclusion | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
| Chronic hepatitis B | 78 | 135 ng/mL | 0.66 | 60 | 71 | 71 | 60 | Decreased serum fibronectin concentrations in patients with ACHBLF were correlated to inflammation and hepatic injury. However, because of low specificity, the use of fibronectin is limited as an independent prognostic indicator. | (13) | |
| HCV | 145 | F0-F4 | >380 ng/mL | 70 | 73 | 77 | 64 | In this study, a novel index fibronectin discriminate score (FDS) based on albumin, fibronectin, and APRI was provided. The FDS predicted liver fibrosis with a higher degree of accuracy than fibronectin. | (15) | |
| Estimation group | > 415 ng/mL | 60 | 58 | 44 | 59 | |||||
| 180 | >380 ng/mL | 72 | 81 | 75 | 79 | |||||
| Validation group | F0-F4 | > 415 ng/mL | 72 | 68 | 52 | 84 | ||||
| HCV | 126 | F0-F3 | 0.78 | 75 | 82 | Serum fibronectin showed satisfactory reproducibility and could be used for the differentiation of HCV infected patients with liver fibrosis from those with non-fibrosis. | (26) |
N: number of cases, AUC: area under the curve; Se: sensitivity; Sp: specificity; NPV: negative predictive value; PPV: positive predictive value; ACHBLV: acute-on-chronic hepatitis B liver failure; HCV: hepatitis B virus
Figure 1.
Summary ROC for serum laminin level in the assessment of liver fibrosis
Figure 2.
Summary ROC for serum fibronectin level in the assessment of liver fibrosis
Figure 3.
Summary ROC for serum hyaluronic level in the assessment of liver fibrosis (data from Rostami et al. (20))
DISCUSSION
According to literature, hepatitis has been the main reason of liver fibrosis particularly in the developing countries (10). HBV is highly prevalent worldwide with an estimated 350 million people affected. This disease is a serious form of liver inflammation due to the infection caused by the virus (21). According to the studies performed on HBV patients, laminin can be a clinically beneficial serum marker for estimating significant fibrosis, particularly when liver biopsy is contraindicated. The studies have shown that elevated laminin serum levels as ECM components indicate a chronic liver injury consequence, which leads to architectural changes in the liver parenchyma and eventually liver fibrosis (10,16,22). The most elevated serum laminin levels were found in the cirrhotic group (F=4), and the cutoff point of 60.9 ng/mL showed a sensitivity and specificity of 71.4% and 77.1%, respectively, in the assessment of significant fibrosis. Additionally, it was reported by Tawhida et al. (23) that serum laminin concentration could be useful in decreasing the need for liver biopsy, but not to replace liver biopsy. Other researchers have reported that a serum cutoff value of 52.0 ng laminin/mL gives a reliable sensitivity, positive predictive value, and negative predictive value for discriminating the various liver fibrosis stages. A significant positive correlation was also observed between serum laminin level and liver fibrosis stages (4,9). Other results indicated that the serum laminin concentration significantly increased with the level of hepatic fibrosis (16,22,24). Parsian et al. (16) reported that in HBV patients, the development of inflammation and liver fibrosis would be accompanied by the impairment of liver endothelial cell function and a decrease in laminin degradation, eventually leading to an increase in serum laminin level. With regard to fibronectin, it has been reported in the Chen et al. (13) study that the decrease of serum fibronectin level is correlated with acute-on-chronic hepatitis B liver failure (ACHBLF), but due to the lack of area under the curve (AUC), sensitivity, and specificity, this glycoprotein cannot be considered an independent prognostic indicator for the assessment of liver fibrosis. The role of hyaluronic acid in the assessment of liver fibrosis in HBV patients also has been reported by Rostami et al. (20).
HCV is also a common disease affecting approximately 130 million people worldwide with most being chronically infected (25). It is evident that HCV can infect liver cells, leading to severe inflammation with serious complications (9). In the Tawhida et al. (23) study of hepatitis C patients, it was indicated that the laminin serum concentration was considerably higher in HBV patients in comparison with the control group. The laminin serum level in patients with HCV was 68.9±2.5, HBV was 57.0±4.8, and control subjects was 45.5±2.4 (p<0.000). El-Mezayen et al. (25) indicated that the serum laminin level increased in accordance with liver fibrosis stages, and the AUC of 0.71 was obtained for the discrimination of patients with severe liver fibrosis from those with mild fibrosis. Therefore, the serum laminin level could be considered a reliable and additional non-invasive tool for the evaluation of liver fibrosis. With regard to the fibronectin, Abdelfattah et al. (26) reported that the AUC, sensitivity, and specificity was 0.78, 75%, and 82%, respectively. They concluded that serum fibronectin may be useful for discriminating patients with liver fibrosis from others in HCV patients. Abdelfattah et al. (15) defined a novel index based on fibronectin, APRI, and albumin as the fibronectin discriminant score (FDS). The results showed good accuracy with AUC of 0.90 for the FDS cutoff value of >0.35 and AUC of 0.86 for FDS of >0.55. They concluded that by using the FDS index, liver fibrosis could be predicted with a high degree of accuracy leading to a lower number of liver biopsies. Santos et al. (27) and Kropf et al. (28) also found similar findings, which are presented in Table 1.
In conclusion, according to the studies on the role of glycoproteins as an indicator for the assessment of liver fibrosis stages and calculated summary ROC, it can be concluded that laminin, hyaluronic acid, and fibronectin with AUC of 0.8946, 0.8236, and 0.7332, respectively, can be considered reliable non-invasive glycoproteins for discriminating the patients with liver fibrosis from the healthy ones and the assessment of liver fibrosis stages. However, further studies are needed particularly for the fibronectin to be introduced as a reliable indicator, which can replace liver biopsy. In addition, the serum levels of these glycoproteins can be considered screening tests and additional clinically useful tools for the liver fibrosis assessment when liver biopsy is contraindicated. It can be also suggested that by defining an index considering these glycoproteins as a combined indicator, there is a higher chance for improving the diagnostic accuracy of glycoproteins in the assessment of liver fibrosis in future.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the local ethics committee.
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.Y., H.P.; Design - S.Y., H.P.; Supervision - S.Y., H.P.; Resources - S.Y., H.P.; Materials - S.Y., H.P.; Data Collection and/or Processing - S.Y., H.P.; Analysis and/or Interpretation - S.Y., H.P.; Literature Search - S.Y., H.P.; Writing Manuscript - S.Y., H.P.; Critical Reviews - S.Y., H.P.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Yokoyaa Y, Iwatac K, Muragakia Y, et al. Concentration of serum laminin and type IV collagen in liver diseases assayed by a sandwich enzyme-immunoassay using monoclonal antibodies. Clin Chim Acta. 1992;210:109–18. doi: 10.1016/0009-8981(92)90049-V. [DOI] [PubMed] [Google Scholar]
- 2.Kropf J, Gressner A, Tittor W. Logestic regression model for assessing portal hypertension by measuring hyaluronic acid (hyaluronan) and Laminin in serum. Clin Chem. 1991;37:30–5. [PubMed] [Google Scholar]
- 3.Boyer TD, Manns MP, Sanyal AJ. Hepatic Fibrosis and Cirrhosis. Zakim and Boyer’s Hepatology (sixth edition) 2012;Chapter 5:64–85. [Google Scholar]
- 4.Saad EA. Non-invasive Assessment of Liver Fibrosis Using Serum Markers. J Pharm Chem Biol Sci. 2014;2:59–76. [Google Scholar]
- 5.Grigorescu M. Noninvasive Biochemical Markers of Liver Fibrosis. J Gastrointestin Liver Dis. 2006;15:149–59. [PubMed] [Google Scholar]
- 6.Aghcheli K, Parsian H, Qujeq D, et al. Serum hyaluronic acid and laminin as potential tumor markers for upper gastrointestinal cancers. Eur J Intern Med. 2012;23:58–64. doi: 10.1016/j.ejim.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Korner Thomas, Kropf Jurgen, Michael Axel. Serum laminin and hyaluronan in liver cirrhosis: markers of progression with high prognostic value. J Hepatol. 1996;25:684–8. doi: 10.1016/S0168-8278(96)80239-X. [DOI] [PubMed] [Google Scholar]
- 8.Heitor R, Edison RP. Is there a place for serum laminin determination in patients with liver disease and cancer? World J Gastroenterol. 2008;14:3628–32. doi: 10.3748/wjg.14.3628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsian H, Nouri M, Rahimipour A, et al. Comparison of Five Liver Fibrosis Indexes with Serum Levels of Laminin and N Terminal Peptide of Procollagen Type III in Chronic Hepatitis Patients. Tech Open 2011, Liver biopsybook. chapter 22:343–60. [Google Scholar]
- 10.Abeer MH, Yasser SS, Mohamed HI, et al. Could Serum Laminin Replace Liver Biopsy as Gold Standard for Predicting Significant Fibrosis in Patients with Chronic Hepatitis B? Clinical and Histopathological Study. J Asian Sci Res. 2013;3:128–39. [Google Scholar]
- 11.Erturk A, Cure E, Ozkurt Z, et al. Serum fibronectin levels in acute and chronic viral hepatitis patients. Malays J Med Sci. 2014;21:29–36. [PMC free article] [PubMed] [Google Scholar]
- 12.Pujades C, Forsberg E, Enrich C, et al. Changes in cell surface expression of fibronectin and fibronectin receptor during liver regeneration. J Cell Sci. 1992;102:815–20. doi: 10.1242/jcs.102.4.815. [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Shao Z, Yin Z, et al. Fibronectin predicts the outcome of acute-on-chronic hepatitis B liver failure. Int Health. 2015;7:67–72. doi: 10.1093/inthealth/ihu060. [DOI] [PubMed] [Google Scholar]
- 14.Erturk A, Cure E, Ozkurt Z, et al. Serum fibronectin levels in acute and chronic viral hepatitis patients. Malays J Med Sci. 2014;21:29–36. [PMC free article] [PubMed] [Google Scholar]
- 15.Abdelfattah MA, Sanaa OA, Ahmed AA, et al. Diagnostic value of fibronectin discriminant score for predicting liver fibrosis stages in chronic hepatitis C virus patients. Ann Hepatol. 2013;12:44–53. [PubMed] [Google Scholar]
- 16.Parsian H, Rahimipour A, Nouri M, et al. Assessment of liver fibrosis development in chronic hepatitis B patients by serum hyaluronic acid and laminin levels. Acta Clin Croat. 2010;49:257–65. [PubMed] [Google Scholar]
- 17.Isman FK, Kucur M, Baysal B, et al. Evaluation of serum hyaluronic acid level and hyaluronidase activity in acute and chronic hepatitis C. J Int Med Res. 2007;35:346–52. doi: 10.1177/147323000703500309. [DOI] [PubMed] [Google Scholar]
- 18.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:1–8. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Jonna Briggs Institute. The systematic review of studies of diagnostic test accuracy. Ann Intern Med. 2015;chapter 2:12–21. [Google Scholar]
- 20.Rostami S, Parsian H. Hyaluronic Acid: From Biochemical Characteristics to its Clinical Translation in Assessment of Liver Fibrosis. Hepat Mon. 2013;13:e13787. doi: 10.5812/hepatmon.13787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McMahon BJ. The Natural History of Chronic Hepatitis B Virus Infection. Hepathology. 2009;49:S45–S55. doi: 10.1002/hep.22898. [DOI] [PubMed] [Google Scholar]
- 22.Lia F, Zhu CL, Zhang H, et al. Role of hyaluronic acid and laminin as serum markers for predicting significant fibrosis in patients with chronic hepatitis B. Braz J Infect Dis. 2012;16:9–14. doi: 10.1016/S1413-8670(12)70267-2. [DOI] [PubMed] [Google Scholar]
- 23.Tawhida Y, Abdel-Ghaffar, Behairy Behairy E, et al. Clinical Benefits of Biochemical Markers of Fibrosis in Egyptian Children with Chronic Liver Diseases. Gastroenterol Res. 2010;3:262–71. doi: 10.4021/gr246w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gressner AM, Tittor W. Serum Laminin-Its concentration Increases with portal hypertension in cirrhotic liver disease. Klin Wochenschr. 1986;64:1240–8. doi: 10.1007/BF01734467. [DOI] [PubMed] [Google Scholar]
- 25.El-Mezayen HA, Habib S, Marzok HF, et al. Diagnostic performance of collagen IV and laminin for the prediction of fibrosis and cirrhosis in chronic hepatitis C patients: a multicenter study. Eur J Gastroenterol Hepatol. 2015;27:378–85. doi: 10.1097/MEG.0000000000000298. [DOI] [PubMed] [Google Scholar]
- 26.Abdelfattah MA, Zahran F, Ismail H, et al. Immunochemical identification and detection of serum fibronectin in liver fibrosis patients with chronic hepatitis C. J Immunoassay Immunochem. 2007;28:331–42. doi: 10.1080/15321810701603476. [DOI] [PubMed] [Google Scholar]
- 27.Santos VN, Leite-Mór MMB, Kondo M, et al. Martins, et al. Serum laminin, type IV collagen and hyaluronan as fibrosis markers in non-alcoholic fatty liver disease. Braz J Med Biol Res. 2005;38:747–53. doi: 10.1590/S0100-879X2005000500012. [DOI] [PubMed] [Google Scholar]
- 28.Kropf J, Gressner MA, Negwer A. Efficacy of serum laminin measurement for diagnosis of fibrotic liver diseases. Clin Chem. 1988;34:2026–30. [PubMed] [Google Scholar]