Case.
A 26-year-old female was involved in a motor vehicle accident as a belted driver after losing control at highway speeds and rolling multiple times into a ditch. There was a prolonged extrication and due to inclement weather conditions, the patient was unable to be evacuated by air ambulance. She was transferred by EMS to a peripheral hospital before expedited transfer to a tertiary trauma centre was possible.
Primary resuscitation & imaging
At the time of transfer to a tertiary care centre, she was stable without any other injuries. Her pelvis was stable and a focused trauma ultrasound exam revealed no evidence of intra-abdominal fluid. As per advanced trauma life support (ATLS) protocol, a Foley catheter was inserted without difficulty and frank hematuria was seen. She underwent an initial computed tomography (CT) abdomen/pelvis, which demonstrated (among other non-operative injuries):
-- Multiple pelvic fractures, including a comminuted left sacrum fracture extending to the left sacro-iliac (SI) joints and multiple left inferior and superior pubic rami fractures.
-- A potential extraperitoneal bladder rupture with hemoperitoneum.
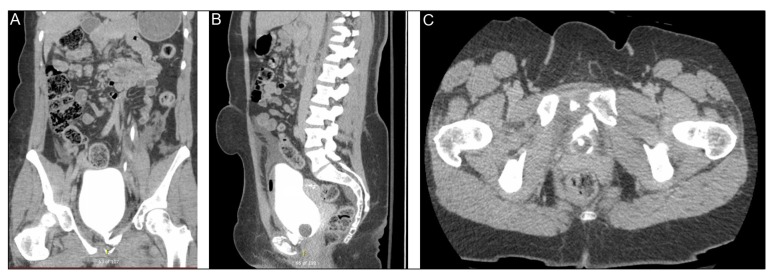
A CT cystogram was ordered, which showed a defect in the left anteroinferior bladder wall measuring approximately 0.8 cm (axial) and 1.3 cm (sagittal). There was a small amount of extraluminal contrast extending through this defect. On imaging review, it was not felt to be involving the bladder neck. There was an intermediate density fluid in the pelvis surrounding the bladder, extending superiorly and abutting the colon and a loop of small bowel (Fig. 1).
Introduction
Bladder trauma can be classified based on injury etiology: blunt, penetrating, iatrogenic, or spontaneous rupture. Bladder injury is described anatomically as being either intraperitoneal (15–30%), extraperitoneal (40–60%), or mixed (10–25%).1 The most superior aspect (dome) of the bladder is closely related to the peritoneum and anchored by the urachus to the anterior abdominal wall.2 During filling, the dome of the bladder expands superiorly and its muscle fibres are progressively stretched with urinary filling. If there is a sudden compression by a blunt force on a maximally filled bladder, an isolated intraperitoneal bladder rupture can occur.
By contrast, extraperitoneal injury is usually associated with the posterior bladder wall and fibrous attachments, including the pubovesical ligament, puboprostatic fascia in men, superior fascia, and inferior fascia. Surrounding the bladder and bony fascial attachments, there is anteroinferior and lateral loose areolar connective tissue known as the potential “space of Retzius.”2 Laceration of the bladder by bony spicules or from compression during pelvic fracture can lead to a bladder rupture that directly communicates with the anterior arch of the pelvis. Blunt external trauma to the bladder usually occurs due to rapid acceleration-deceleration forces stressing the fascial attachments of the bladder to the pelvis and horizontal tearing near fascial connections. Common mechanisms of trauma include motor vehicle accidents, falls, and crush injuries. The vast majority of cases of bladder trauma occur with other pelvic injuries.3
The case presented here involves an extraperitoneal bladder injury due to blunt injury with a concomitant pelvic fracture. Approximately 12% of trauma patients have a pelvic ring injury. Additionally, injury to intra-abdominal or pelvic organs occurs in 3–6% of patients with pelvic fractures and 15% with severe pelvic fractures.3,4 A retrospective review of 31 380 patients with pelvic fractures found that those who sustained an associated genitourinary injury concurrent with their pelvic fracture had increased morbidity and morbidity compared to pelvic fracture alone.4
Diagnosis of intra and extraperitoneal bladder injuries can be challenging due to often vague and non-specific presentation; up to 23% of all bladder and urethral injuries associated with pelvic fracture are missed at initial evaluation. 5 Classic signs and symptoms of a bladder injury following blunt trauma include gross hematuria; suprapubic pain; extravasation of urine into the perineum, scrotum, and thighs; and lower abdominal bruising.6–9 Intraperitoneal bladder rupture can result in an elevated serum creatinine from reabsorption of urine in the peritoneal cavity.
Clinical prediction of extraperitoneal bladder rupture with a pubic fracture requiring open reduction internal fixation (ORIF) includes gross hematuria/microscopic hematuria with >30 RBC/HPF, diastasis of pubic symphysis >1 cm (10-fold increased risk), and fracture of the obturator ring with displacement >1 cm (3-fold increased risk). Specific physical exam should include examination of the pelvis, assessment of pelvic stability, and digital rectal examination.10
Clinicians should be aware that certain pelvic fractures have a greater risk of bladder injury. Lateral compression fractures and pubic symphysis diathesis injuries are most commonly associated with bladder injury.11 Clinical widening of the sacroiliac (SI) joint >1 cm, symphysis pubis >1 cm, and any documented sacral fractures can also be associated with bladder injury. A widened pubic symphysis or SI joint has a sensitivity of 75% for bladder injury, however, the positive predictive value is only 20%.4 Acetabular fractures are rarely associated with bladder injuries.
Identification of a coexisting bladder injury is important, as it should be promptly managed with urinary drainage by either suprapubic or urethral catheterization. Importantly, the time span from initial injury to ORIF for pelvic fracture may be greater than 10 days from initial trauma; it is important to appropriately drain the urine during this time period to reduce the risk of colonization of the pelvic hematoma.12 The indications for bladder imaging are listed in Table 1.
Table 1.
Indications for imaging of the bladder
| Absolute indications | Blunt or penetrating external trauma with gross hematuria and a known pelvic fracture |
| Relative indications | Blunt external trauma with microscopic hematuria >30 RBC/HPF |
| Penetrating injury to buttocks, pelvis or lower abdomen with any degree of microscopic hematuria. | |
| Widening of pubic symphysis >1 cm and/or widening of obturator ring >1 cm. |
Bladder imaging in the trauma setting
Retrograde cystography
Retrograde filling of bladder is carried out until the patients experience discomfort (assuming they are conscious). In an otherwise healthy patient with no history of bladder reconstruction or significant urological history, 350 cc is adequate. A plain-film, full-bladder anterior-posterior film, and drainage film are taken. Extraperitoneal extravasation may show a classic “flame sign.”1 Extra and intraperitoneal bladder ruptures may be differentiated by the presence of contrast outlining the loops of bowel (diagnostic of an intraperitoneal injury). To prevent false-negatives, the bladder must be adequately filled and post-void films must be taken to visualize any extravasation of contrast that may be hidden behind the fully distended bladder.12 If the bladder is underfilled, smaller defects may be temporarily occluded by omentum or blood clots.13 When properly performed, a retrograde cystogram is nearly 100% sensitive for detecting rupture.
Computed tomography (CT) cystography
Conventional intravenous CT abdomen/pelvis will miss 40% of bladder ruptures.1,13 A CT cystogram involves retrograde filling of the bladder with contrast to a volume of 350 mL. Drainage films are not required due to the axial nature of the images. Antegrade filling of contrast after administration of intravenous contrast and clamping the urinary catheter is discouraged, as it does not allow adequate distention for proper bladder evaluation.6,14,15 When properly performed, CT cystography has a high sensitivity and specificity for detecting evidence of rupture (95–99% and 95–100%, respectively).16,17
Focused assessment with sonography for trauma (FAST) exam
In the setting of a critically ill patient, CT cystogram or plain-film cystogram may delay essential treatment, as retrograde dye administration can be technically challenging or there may be a delay until the imaging is interpreted.18 The use of bedside ultrasonography with intravesical saline instillation may assist in early diagnosis of bladder rupture; however, reliability is dependent on the bedside ultrasonographer’s experience. Experienced centres report sensitivity of 90% with a positive predictive value of 100%. A FAST exam is considered positive if there is a small, contracted bladder with peri-vesicle fluid accumulation that is visible with real-time administration of saline.18,19
Imaging recommendations from national guidelines
The American Urological Association (AUA)20 recommends bladder imaging for all patients with pelvic fractures and gross hematuria. Either plain-film or CT retrograde cystography are appropriate, as both show similar sensitivity and specificity for detecting bladder injuries in experienced centres. Similarly, the European Association of Urology (EAU)21 recognizes the role of both CT and plain-film cystography as reasonable modalities for diagnosing bladder injuries, however, they favour CT cystogram due to its ability to diagnose injuries beyond the bladder. While ultrasonography may be useful in the future, it is currently not recommended as a diagnostic test.
Treatment
Conservative care
For patients with an uncomplicated extraperitoneal injury and pelvic fracture, a large bore (≥16 French) catheter for 2–3 weeks without surgical intervention is the treatment of choice, as many of these injuries will heal without operative intervention. A seven-day course of antibiotics should be started immediately to prevent secondary infection of the extraperitoneal fluid collections from the inevitable bacteriuria that is associated with an indwelling catheter.1 Cystography to confirm defect closure should be performed prior to removing the catheter.
Operative management
Extraperitoneal bladder injury in the setting of ORIF for pelvic fracture requires immediate catheterization since fracture repair may be delayed several days.22 Immediate surgical repair of an extraperitoneal bladder injury is appropriate in the setting of intravesical bone spicules, rectal or vaginal laceration, and bladder neck injuries in order to minimize the risks of fistula formation, abscess, urine leak, and incontinence. Immediate repair may also be considered for patients undergoing exploratory laparotomy or internal fixation of their pelvic fracture to minimize urine contamination of orthopedic hardware.9 Surgical repair involves two-layer (mucosa-detrusor) primary vesicorraphy with an absorbable suture followed by the placement of a large bore Foley catheter to ensure drainage.23 A transvesical approach may be useful, as it can be difficult to identify an extraperitoneal bladder rupture from outside the bladder. It may be necessary to resect devitalized mucosa or detrusor muscle, although extensive mobilization of the bladder should be avoided to minimize the risk of vascular and neurological injuries to the bladder. An important potential complication of a bladder rupture with a pelvic fracture (even in the absence of operative repair) is peripheral nerve injury with resulting bladder dysfunction. This may lead to lifelong voiding dysfunction and may be more common with delayed repair and significant pelvic fractures.24
It is up to the operating surgeon’s judgement if both urethral and suprapubic catheters are necessary. The routine use of both a suprapubic and a urethral catheter may increase morbidity and delay hospital discharge.20 The AUA guidelines recommend against routine placement of a suprapubic catheter following repair of bladder injury.20 The decision to use double bladder drainage should be based on the complexity of the bladder repair, whether there is an associated urethral injury/bladder neck injury, coexisting severe neurological injuries, and the degree of hematuria at the end of the case.8,25,26 Catheter removal should be considered after 14–21 days and should be preceded by repeat bladder imaging.
Orthopedic hardware and the type of urinary catheter
Orthopedic management of unstable pelvic fractures includes external and/or internal pelvic fixation to control bleeding, immobilization of fragments, pain reduction, and facilitating mobility for rehabilitation.27 In general, internal fixation of unstable pelvic fractures is preferred. External fixation is used for temporary fixation of the pelvis when patients are hemodynamically unstable and require other life-saving treatment prior to definitive management of the pelvic fracture. However, this is associated with a high complication rate, such as pin site infections (50%), osteomyelitis (7%), and case reports of bladder herniation and entrapment due to closed reduction of pubic symphysis disruption.28–31
There are no prospective studies addressing the issues of combined orthopedic-genitourinary injury. However, given the elevated infection risk associated with prosthetic material used in orthopedic surgery, urologists may consider primary surgical repair of uncomplicated bladder injuries to reduce likelihood of colonized urine infecting orthopedic hardware (EAU guideline, Grade B recommendation).21 A recent retrospective cohort study of 45 patients compared conservative management (catheter drainage alone) with concurrent primary repair of bladder injury in the setting of pelvic fractures managed with internal fixation. Overall, the authors showed an increased rate of infected hardware in patients managed conservatively compared to those receiving concurrent bladder repair at time of orthopedic surgery (33.3% vs. 5.6%; p=0.047). The rate of hardware infection with suprapubic catheterization compared to urethral catheterization was not significantly different between the two groups.
Management options from national guidelines
In any patient with penetrating trauma or intraperitoneal injuries, both the AUA and EAU agree on the need for emergency exploration and repair regardless of presence of pelvic fracture.20,21 For patients with an uncomplicated extraperitoneal injury, conservative care with catheter drainage and followup imaging is the treatment of choice for most injuries.
The AUA recommends considering surgical repair in uncomplicated extraperitoneal bladder injuries that fail to resolve after four weeks of conservative management or immediate repair of patients with complex factors (previously discussed). The advantage of conservative management is the potential to avoid or defer the morbidity associated surgical intervention; therefore, if the patient is going to have an operation for another indication (in this case orthopedic fixation or repair of other injuries), the urologist should consider repairing the bladder injury at that time.
Similarly, the EAU recognizes that the majority of uncomplicated extraperitoneal bladder ruptures can be managed with catheter drainage alone; however, patients with persistent urine leak on followup imaging, patients undergoing abdominal exploration, or patients presenting with complicating factors may warrant surgical intervention. Additionally, the EAU addresses the growing role of osteosynthetic material in orthopedic surgery. Given the elevated infection risk associated with this material, urologists may want to consider surgical repair of uncomplicated bladder injuries if it is going to be used.
Case followup.
Following initial resuscitation by the trauma service, general surgery, orthopedics, and urology were consulted. The orthopedic team found the patient to be neurovascularly intact and recommended an open reduction internal fixation of her sacrum the next day. There was a simple extraperitoneal bladder injury without any complicating factors and we elected for conservative management overnight with an 18 French foley catheterization.
She underwent an ORIF of her sacrum and pelvis the next day, and after discussions between urology and orthopedics, the decision was made to not repair the bladder, as the hematuria had largely resolved and the bladder laceration was quite small on initial imaging. Her Foley catheter was removed on postoperative day 14 after a negative cystogram. At followup three months postoperatively, there were no urological complications.
Fig. 1.
Computed tomography cystogram of the extraperitoneal bladder injury. (A) Coronal imaging shows extravasation of the intravesical contrast from the left side of the bladder base; (B) sagittal; (C) and coronal views showing a fractured pubic symphysis and anterior extravasation of intravesical contrast.
Footnotes
Competing interests: The authors report no competing personal or financial conflicts.
This paper has been peer reviewed.
References
- 1.Wein AJ, Kavoussi LR, Partin AW, et al. Campbell-Walsh Urology. 11th ed. Philadelphia, PA: Elsevier Saunders; 2016. [Google Scholar]
- 2.Figler B, Edward Hoffler C, Reisman W, et al. Multidisciplinary update on pelvic fracture associated bladder and urethral injuries. Injury. 2012;43:1242–9. doi: 10.1016/j.injury.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 3.Cass AS. The multiple injured patient with bladder trauma. J Trauma. 1984;24:731–4. doi: 10.1097/00005373-198408000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bjurlin MA, Fantus RJ, Mellett MM, et al. Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank. J Trauma. 2009;67:1033–9. doi: 10.1097/TA.0b013e3181bb8d6c. [DOI] [PubMed] [Google Scholar]
- 5.Ziran BH, Chamberlin E, Shuler FD, et al. Delays and difficulties in the diagnosis of lower urologic injuries in the context of pelvic fractures. J Trauma. 2005;58:533–7. doi: 10.1097/01.TA.0000152561.57646.80. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh CH, Chen RJ, Fang JF, et al. Diagnosis and management of bladder injury by trauma surgeons. Am J Surg. 2002;184:143–7. doi: 10.1016/S0002-9610(02)00913-3. [DOI] [PubMed] [Google Scholar]
- 7.Avey G, Blackmore CC, Wessells H, et al. Radiographic and clinical predictors of bladder rupture in blunt trauma patients with pelvic fracture. Acad Radiol. 2006;13:573–9. doi: 10.1016/j.acra.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 8.Parry NG, Rozycki GS, Feliciano DV, et al. Traumatic rupture of the urinary bladder: Is the suprapubic tube necessary? J Trauma. 2003;54:431–6. doi: 10.1097/01.TA.0000053196.19218.4F. [DOI] [PubMed] [Google Scholar]
- 9.Gomez RG, Ceballos L, Coburn M, et al. Consensus statement on bladder injuries. BJU Int. 2004;94:27–32. doi: 10.1111/j.1464-410X.2004.04896.x. [DOI] [PubMed] [Google Scholar]
- 10.Avey G, Blackmore CC, Wessells H, et al. Radiographic and clinical predictors of bladder rupture in blunt trauma patients with pelvic fracture. Acad Radiol. 2006;13:573–9. doi: 10.1016/j.acra.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Cass AS. Diagnostic studies in bladder rupture. Indications and techniques. Urol Clin North Am. 1989;16:267–73. [PubMed] [Google Scholar]
- 12.Berber O, Emeagi C, Perry M, et al. Failure of conventional retrograde cystography to detect bladder ruptures in pelvic trauma. J Orthop Traumatol. 2011;12:57–60. doi: 10.1007/s10195-010-0123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doyle SM, Master VA, McAninch JW. Appropriate use of CT in the diagnosis of bladder rupture. J Am Coll Surg. 2005;200:973. doi: 10.1016/j.jamcollsurg.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Mee SL, McAninch JW, Federle MP. Computerized tomography in bladder rupture: Diagnostic limitations. J Urol. 1987;137:207–9. doi: 10.1016/S0022-5347(17)43954-1. [DOI] [PubMed] [Google Scholar]
- 15.Udekwu PO, Gurkin B, Oller DW. The use of computed tomography in blunt abdominal injuries. Am Surg. 1996;62:56–9. [PubMed] [Google Scholar]
- 16.Deck AJ, Shaves S, Talner L, et al. Computerized tomography cystography for the diagnosis of traumatic bladder rupture. J Urol. 2000;164:43–6. doi: 10.1016/S0022-5347(05)67445-9. [DOI] [PubMed] [Google Scholar]
- 17.Quagliano PV, Delair SM, Malhotra AK. Diagnosis of blunt bladder injury: A prospective comparative study of computed tomography cystography and conventional retrograde cystography. J Trauma. 2006;61:410–21. doi: 10.1097/01.ta.0000229940.36556.bf. discussion 421–2. [DOI] [PubMed] [Google Scholar]
- 18.Karim T, Topno M. Bedside sonography to diagnose bladder trauma in the emergency department. J Emerg Trauma Shock. 2010;3:305. doi: 10.4103/0974-2700.66529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu TS, Pearson TC, Meiners S, et al. Bedside ultrasound diagnosis of a traumatic bladder rupture. J Emerg Med. 2011;41:520–3. doi: 10.1016/j.jemermed.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Morey AF, Brandes S, Dugi DD, et al. Urotrauma: AUA guideline. J Urol. 2014;192:327–35. doi: 10.1016/j.juro.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lynch TH, Martínez-Pieiro L, Plas E, et al. EAU guidelines on urological trauma. Eur Urol. 2005;47:1–15. doi: 10.1016/j.eururo.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 22.Taffet R. Management of pelvic fractures with concomitant urologic injuries. Orthop Clin North Am. 1997;28:389–96. doi: 10.1016/S0030-5898(05)70296-0. [DOI] [PubMed] [Google Scholar]
- 23.Bhatt NR, Merchant R, Davis NF, et al. Incidence and immediate management of genitourinary injuries in pelvic and acetabular trauma: A 10-year retrospective study. BJU Int. 2018;122:126–32. doi: 10.1111/bju.14161. [DOI] [PubMed] [Google Scholar]
- 24.Ter-Grigorian AA, Kasyan GR, Pushkar DY. Urogenital disorders after pelvic ring injuries. Cent European J Urol. 2013;66:352–6. doi: 10.5173/ceju.2013.03.art28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volpe MA, Pachter EM, Scalea TM, et al. Is there a difference in outcome when treating traumatic intraperitoneal bladder rupture with or without a suprapubic tube? J Urol. 1999;161:1103–5. doi: 10.1016/S0022-5347(01)61600-8. [DOI] [PubMed] [Google Scholar]
- 26.Alli MO, Singh B, Moodley J, et al. Prospective evaluation of combined suprapubic and urethral catheterization to urethral drainage alone for intraperitoneal bladder injuries. J Trauma. 2003;55:1152–4. doi: 10.1097/01.TA.0000046255.12137.18. [DOI] [PubMed] [Google Scholar]
- 27.Flint L, Cryer HG. Pelvic fracture: The last 50 years. J Trauma. 2010;69:483–8. doi: 10.1097/TA.0b013e3181ef9ce1. [DOI] [PubMed] [Google Scholar]
- 28.Jain M, Nanda SN, Mohapatra SS, et al. Bladder incarceration following anterior pelvic infix of a traumatic pubic symphysis diastasis treated with immediate open reduction and internal fixation. J Clin Orthop Trauma. 2017;8:S11–6. doi: 10.1016/j.jcot.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bartlett CS, Ali A, Helfet DL. Bladder incarceration in a traumatic symphysis pubis diastasis treated with external fixation: A case report and review of the literature. J Orthop Trauma. 1998;12:64–7. doi: 10.1097/00005131-199801000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Finnan RP, Herbenick MA, Prayson MJ, et al. Bladder incarceration following anterior external fixation of a traumatic pubic symphysis diastasis treated with immediate open reduction and internal fixation. Patient Saf Surg. 2008;2:26. doi: 10.1186/1754-9493-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geracci JJ, Morey AF. Bladder entrapment after external fixation of traumatic pubic diastasis: Importance of followup computed tomography in establishing prompt diagnosis. Mil Med. 2000;165:492–3. doi: 10.1093/milmed/165.6.492. [DOI] [PubMed] [Google Scholar]