Abstract
Objective:
To test whether two interventions promote interest in diabetes prevention among women with a history of gestational diabetes mellitus (GDM), who face high lifetime risk for diabetes.
Research Design and Methods:
We designed an email outreach message promoting an existing preventive lifestyle program. The message incorporated values affirmation, a theory-based intervention that can improve openness to health information but typically relies on a writing exercise less practical in healthcare settings. In a 3-arm randomized study, 237 women with elevated BMI and a history of GDM were randomized to read an outreach message containing either no affirmation (control) or one of two affirmations, streamlined to remove the typical writing exercise: either a values affirmation prompting reflection on any personal value, or a parenting affirmation prompting reflection on caregiving-related values. Outcomes included demonstrating interest in the lifestyle program (seeking information about it or intending to join) and seeking publicly-available health information about diabetes prevention.
Results:
Compared to control, participants randomized to the values affirmation more frequently demonstrated interest in the lifestyle program (59.0% vs. 74.4%; adjusted relative risk [95% CI]: 1.31 [1.04–1.66]) and sought information about diabetes prevention (59.0% vs. 73.4%; 1.22 [0.97–1.54]). The parenting affirmation yielded no significant differences in either outcome.
Conclusions:
A streamlined values affirmation, designed for feasibility in a healthcare setting, can promote interest in diabetes prevention among women at high-risk. Research is needed to evaluate its effects on diabetes prevention program enrollment and clinical outcomes.
Keywords: Diabetes mellitus, gestational diabetes, preventive health services, health communication, self-affirmation
Introduction
Up to 14% of pregnant women in the U.S. experience gestational diabetes mellitus (GDM), or glucose intolerance identified during pregnancy.1 Compared to women without this common complication, women with a history of GDM face 7-fold increased risk for developing diabetes later in life.2 Elevated BMI increases this risk.3 Screening for GDM is universal, which presents a prime opportunity to identify patients at high-risk for diabetes and promote lifestyle programs for weight management, healthy eating, and physical activity to prevent diabetes after delivery.4
In healthcare settings, population management tools such as electronic health records (EHRs), disease registries, and secure patient-provider email systems offer a platform to promote preventive programs among the high-risk patients most likely to benefit from them. Yet participation in diabetes prevention programs is persistently low: over half report participation rates of less than 20%.5 A critical barrier is that health promotion outreach is often least effective among those for whom it is most relevant, leading to dismissal or avoidance of preventive health information.6–8 Indeed, women with history of GDM often perceive themselves as healthy and discount their diabetes risk once pregnancy is over.9
Self-affirmation theory provides an explanation for this paradox by asserting that people are naturally motivated to maintain their self-integrity, or a sense of themselves as adaptively adequate.8,10 The possibility of being at risk for disease can prompt avoidance of health information because it threatens a self-perception of adequacy.6,11 Based on this theory, an intervention known as values affirmation has been shown to increase openness to threatening health information. The intervention typically involves an exercise in which people write about important personal values unrelated to the threat, such as religion or relationships.12 Against the backdrop of a broadened view of the self and its psychological resources, the threatening health message evokes less defensiveness.8 Recent meta-analyses show that values affirmation interventions can improve acceptance of health information, intentions to engage in health behaviors, and health behaviors themselves.13–15 However, with notable exceptions,16,17 most values affirmation interventions have been tested in student or non-clinical samples rather than truly at-risk populations. Moreover, values affirmation interventions typically rely on a writing exercise that is less practical in busy healthcare settings and likely burdensome for wide-scale adoption.
Therefore, our goal in the “Patients Engaged in Prevention” (PEP) study was to create and test a values affirmation intervention, feasible in clinical settings, to promote interest in preventive lifestyle programs among women with elevated BMI and a recent history of GDM. We used an intervention mixed methods study design18 including 2 phases: 1) a quantitative and qualitative development phase to design an affirmation intervention that does not rely on any writing, followed by 2) a randomized study to test its effectiveness in promoting women’s interest in diabetes prevention. Outcomes of the randomized study included demonstrating interest in an existing health system-based lifestyle program (i.e., seeking information about it or intending to join) and seeking publicly-available health information about diabetes prevention.
Research Design and Methods
Setting and Participants
Kaiser Permanente Northern California (KPNC) is an integrated healthcare delivery system whose 4 million members include 24% of the surrounding Northern California population.19 Participants were racially and ethnically diverse women recruited approximately 4 years after an index GDM pregnancy, who met initial eligibility criteria: current absence of recognized diabetes, confirmed via EHR and the KPNC diabetes registry;20 elevated BMI (25–40 kg/m2, or 23–40 kg/m2 if Asian);21 age 18–50 years; no current pregnancy; and ability to communicate in English. The Kaiser Foundation Research Institute Human Subjects Committee approved this research.
To recruit diverse women with a recent (but not necessarily immediate) history of GDM, we derived the cohort of potentially eligible participants from the GEM (“Gestational diabetes’ Effects on Moms”) cluster-randomized trial.22 GEM had identified all 2,480 women diagnosed with GDM in a 1-year period from 2011–2012 across all of KPNC’s medical facilities, which had been randomized to a usual care arm (22 facilities) or intervention arm (22 facilities). As part of routine care offered by the Kaiser Permanente Regional Perinatal Service Center, women in facilities assigned to the GEM intervention arm had been offered an optional telephone-based lifestyle program directly after their index GDM pregnancy. Half of those (i.e., approximately one-quarter of the total GEM sample) participated in the optional program, which ended at 6 months postpartum. As GEM was a pragmatic trial evaluating a program delivered on behalf of the health system, no consent was required to participate in its evaluation. However, as part of a related survey,22 many women provided contact and demographic information used here to recruit a diverse sample of participants with similarly recent histories of GDM.
Intervention Development
Methods and results for an intervention development phase are reported in the supplementary materials. Briefly, we conducted a survey and 6 focus groups approximately 4 years after participants’ index GDM pregnancy.23 Results led us to develop two affirmations. The first was a standard values affirmation prompting participants to reflect on a personal value, e.g., religion or relationships, unrelated to the threatening health domain. Importantly, this affirmation was consistent with interventions found to be effective in previous research which broaden the self-concept beyond the threatened domain.8 Second, given its importance to the target population of women with young children, we developed an exploratory parenting affirmation that prompted participants to reflect on values related to caregiving. Both affirmations were streamlined in the form of instructions encouraging participants to reflect on their core values, without any writing.
We conducted a 3-arm randomized study to test whether the values and parenting affirmations, as compared to a no affirmation control condition, promoted participants’ interest in a health system-based lifestyle program for weight management, healthful eating, and physical activity. The study setting, ethical approval, participant identification, and eligibility criteria are as described above in Phase 1, with the exception that participants recruited in Phase 1 were not eligible for Phase 2. Prospective participants received email invitations to participate in an online study and were offered $15 for their participation. Consenting participants completed a baseline survey to assess demographic characteristics, current weight, presence of diagnosed pre-diabetes, and attainment of national guidelines for accruing ≥150 minutes of moderate- to vigorous-intensity physical activity per week.24 The baseline survey also assessed intention to join a health system-based lifestyle program using an item adapted from Klein et al.:25 “In the next month, how likely are you to join a Kaiser Permanente program to eat better, be more active, or manage your weight?” (5-point scale, dichotomized as likely vs. unlikely).
Following the baseline survey, participants were randomized by research staff to either the values affirmation, parenting affirmation, or no affirmation control condition in a 1:1:1 ratio. We used a covariate adaptive randomization procedure (minimization method)26–28 to ensure between-condition balance on participant characteristics assessed prior to the baseline survey via GEM or EHR data: GEM treatment arm (usual care and intervention), BMI category (< 30 and ≥ 30 kg/m2), race/ethnicity (minority and White), and educational level (< 4-year college degree [e.g., high school or 2-year college degree] and ≥ 4-year college degree). Investigators and data analysts were blind to condition assignment. One month post-baseline, participants received a link to read the outreach message corresponding to their assigned condition and complete an outcomes survey.
Outreach message.
All participants were asked to “read the following secure email message, which a Kaiser Permanente member like you might receive from her doctor on kp.org,” the health system’s secure patient-provider email system. The main text of the outreach message was identical across conditions and written at an 8th grade reading level. It described “Wellness Coaching,” a healthy lifestyle program accessible to all adult KPNC members at no cost, which offers 1-on-1 telephone sessions focused on health behaviors critical to diabetes prevention (e.g., weight management, healthy eating, and physical activity).29 The message included information which could be perceived as threatening by this group of at-risk participants, i.e., it described women’s risk for type 2 diabetes due to their history of GDM and noted that this risk is especially high among those from racial/ethnic minority groups. The main text of the outreach message also addressed multiple potential determinants of engaging in preventive programs. Determinants were drawn from the validated Theoretical Domains Framework, a synthesis of behavior change theories, and linked to specific behavior change techniques (Table 1).30 The message ostensibly originated from participants’ personal physician, a credible source of information, to increase positive social influence.23
Table 1.
Intervention content of the Patients Engaged in Prevention (PEP) study: Theory-based behavioral determinants, linked behavior change techniques, and outreach message excerpts
| Behavioral determinants | Behavior change technique |
Message excerpt | |||||
|---|---|---|---|---|---|---|---|
| Capability | Opportunity | Motivation | |||||
| Knowledge | Social influences | Environmental context & resources | Social role & identity | Beliefs about capabilities | Beliefs about consequences | ||
| ✓* | Self-affirmation (Valued self-identity) |
I invite you to take a few moments, right now, to think about what’s most important to you in your life. Whether you value your independence, religion or spirituality, or relationships with family and friends, what is it about that value that means the most to you? | |||||
| ✓† | Self-affirmation (Valued self-identity) |
I invite you to take a few moments, right now, to think about why parenting or caregiving might be an important part of your life. Whether it’s the closeness you share, the special moments you create, or the chance to positively impact your loved ones, what is it about being a parent or caregiver that means the most to you? | |||||
| ✓ | ✓ | Identification of self as role model | Simple changes…are one way to be a positive role model | ||||
| ✓ | Information about social consequences | [Caring] for yourself now can help you nurture and enjoy your growing family for years to come; stay strong for the people who depend on you | |||||
| ✓ | ✓ | Information about health consequences | [Lifestyle changes] are one way to…reduce your chances of getting diseases like diabetes | ||||
| ✓ | ✓ | ✓ | Salience of consequences | [Coaches] help women who had [GDM] lower their high risk for getting diabetes—a risk that’s especially high for Asian, Pacific Islander, African American, Latina, and Native American women | |||
| ✓ | Verbal persuasion about capability | Joining [the program] is easy | |||||
| ✓ | Focus on past success | Just as you partnered with your doctors and nurses to have the healthiest pregnancy possible, you can now partner with a wellness coach | |||||
| ✓ | Credible source | Free program helps you & your family thrive: A message on behalf of your doctor [subject line of message ostensibly sent by personal physician via patient-provider email system] | |||||
| ✓ | Social support | [The program is] supportive; Coaches…[help] members find their own motivation | |||||
| ✓ | Instruction on how to perform a behavior | Visit [link to program website]…Book appointment online [link] or call [number] | |||||
| ✓ | ✓ | Information about social and environmental consequences | There’s no cost to participate [inform recipient about financial resources required] | ||||
Note: Content applies to all conditions unless otherwise noted.
Values affirmation condition only.
Parenting affirmation condition only.
Conditions.
The main text of the outreach message was preceded by either the values affirmation, the parenting affirmation, or no affirmation (control). Participants in the values affirmation condition were presented with two sentences prompting reflection on core personal values; those in the parenting affirmation condition were presented with two sentences prompting reflection on values related to caregiving. Participants in the no affirmation control condition were presented only with the main text of the outreach message.
Outcomes.
Participants completed outcome measures after viewing the outreach message in their assigned condition. First, we assessed whether participants demonstrated interest in the health system-based lifestyle program described in the outreach message. This was a composite of whether participants a) intended to join a lifestyle program (as described above at baseline, dichotomized as likely vs. unlikely); or b) sought information about it (“After completing this survey, would you like to receive more information about Wellness Coaching, a free Kaiser Permanente program to help members eat better, be more active, and manage their weight?”; yes vs. no). For those who responded yes to the latter, a link to the program website appeared onscreen immediately after completion of the survey. Across conditions we observed a significant association between seeking information about the program and intention to join: Compared to those who did not seek information, those who sought information about the lifestyle program had over 20-fold higher odds of intending to join a program, adjusted for intentions at baseline (adjusted odds ratio 27.71 [95% CI 6.5 to 117.93]). Given this association and evidence that self-affirmation influences distal target behaviors,14 intentions and information seeking were combined into the composite outcome of demonstrated interest in a lifestyle program, which corresponded to a positive response on either indicator.
Second, we assessed whether participants sought publicly available health information about diabetes prevention from the National Institutes of Health, or NIH (“After completing this survey, would you like to receive information from the National Institutes of Health about preventing diabetes for women who have had gestational diabetes?”; yes vs. no). Again, for participants who responded yes, the requested link appeared onscreen immediately after survey completion. The website contained information on diabetes risk after GDM and preventive advice from the National Diabetes Education Program, a public health information service jointly sponsored by the NIH and the Centers for Disease Control and Prevention.
Process Measures.
We examined steps in the process of behavior change in response to health messages.13,14 As an indication of whether participants attended to the message, we assessed how much of the message participants had read with a single item on a 6-point scale (dichotomized as none/almost none/some vs. most/almost all/all of the message). We assessed participants’ acceptance of the message using 3 indices developed in prior research: 1) persuasiveness (12 items, e.g., extent to which the message was “persuasive,” “memorable,” “applicable to my life”; α =.91);31,32 2) derogation (4 items, e.g., extent to which the message was “misleading,” “exaggerated”; α =.73);33,34 and 3) threat (7 items, e.g., “The message made me feel [upset, guilty]”; α =.90).34,35 Message acceptance items were rated on 7-point scales from not at all (1) to very (7), with higher mean scores corresponding to greater persuasiveness, derogation, or threat. As an indication of the degree to which participants were affirmed, we assessed self-integrity using a 5-item measure (e.g., “On the whole, I am a capable person”; α = .90) modified with the scale’s author to exclude 3 items more relevant to moral than adaptive adequacy.36 Items were rated on a 7-point scale from strongly disagree (1) to strongly agree (7), with higher mean scores corresponding to greater self-integrity. Additional qualitative data collection and results are described in the supplementary materials.
Statistical Analysis.
Analyses using SAS 9.3 (Cary, NC) followed adapted intent-to-treat procedures by including all eligible participants who completed the intervention and outcomes survey and thus were exposed to the outreach message in their assigned condition, regardless of how much of the message they read. We excluded 13 ineligible participants who reported at baseline that they either were not parents of a child <18 years or were already participating in a lifestyle program. The analytic sample size of 237 yielded 80% power to detect a pairwise difference in mean self-integrity score of at least .45 standard deviation units, which does not reflect the potential added precision resulting from covariate adjustment (2-sided t-test, α=.05). To compare each affirmation to the control condition, we used analysis of covariance and log binomial models to estimate relative risks (RRs). Analyses adjusted for variables used in the randomization scheme, i.e., GEM treatment arm, BMI category, race/ethnicity, and education.37 Analysis of the composite outcome, which incorporated participants’ intentions at follow-up, further adjusted for intentions at baseline. Additionally, because half of the GEM-derived sample had been offered a lifestyle program as part of optional routine care 4 years earlier, directly after their index GDM pregnancy, we conducted sensitivity analyses by including an interaction term for GEM treatment arm by assigned condition; and, if significant, by repeating the main analysis stratified by GEM treatment arm.
Results
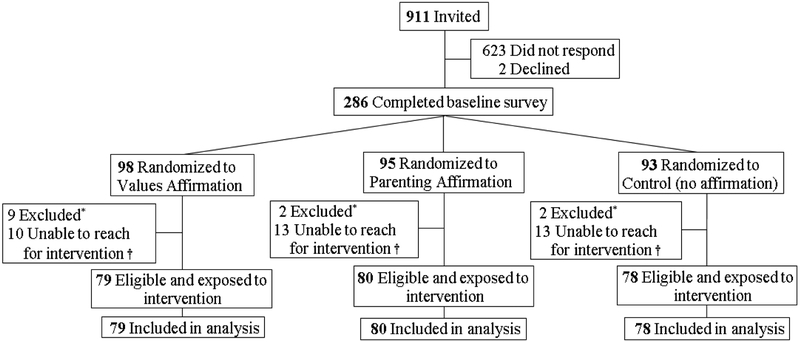
Figure 1 shows the flow of participants through the study. The number of eligible participants who could not be reached for the intervention (i.e., who were not exposed to the outreach message in their assigned condition) did not differ across conditions (n = 10 [10.2%], 13 [13.7%], and 13 [10.2%] in the values, parenting, and affirmation conditions, respectively; P = .80). Baseline characteristics of the analytic sample likewise were comparable across conditions (Table 2).
Figure 1.
Flow of participants through the Patients Engaged in Prevention (PEP) study
*Not parents of a child <18 years or already in a program (not mutually exclusive). †Not exposed to assigned condition
Table 2.
Baseline characteristics by condition among participants with a history of gestational diabetes: The Patients Engaged in Prevention (PEP) study
| Condition | ||||||
|---|---|---|---|---|---|---|
| Values affirmation (n = 79) |
Parenting affirmation (n = 80) |
Control (n = 78) |
||||
| Mean | SD | Mean | SD | Mean | SD | |
| Age, years | 38.1 | 5.0 | 37.7 | 5.0 | 37.7 | 4.5 |
| BMI (kg/m2)* | 30.2 | 5.5 | 31.4 | 6.7 | 31.2 | 7.0 |
| n | % | n | % | n | % | |
| Racial/ethnic origin | ||||||
| Asian/Pacific Islander† | 28 | 35.4 | 29 | 36.3 | 28 | 35.9 |
| Latina | 11 | 13.9 | 11 | 13.8 | 12 | 15.4 |
| Non-Hispanic White | 31 | 39.2 | 28 | 35.0 | 27 | 34.6 |
| Other‡ | 9 | 11.4 | 12 | 15.0 | 11 | 14.1 |
| Educational level | ||||||
| < 4-year college degree | 32 | 40.5 | 33 | 41.3 | 35 | 44.9 |
| ≥ 4-year college degree | 47 | 59.5 | 47 | 58.8 | 43 | 55.1 |
| Household income | ||||||
| < $50,000 | 8 | 10.1 | 12 | 15.0 | 17 | 21.8 |
| $50,000 to $99,999 | 28 | 35.4 | 23 | 28.8 | 21 | 26.9 |
| ≥ $100,000 | 31 | 39.2 | 36 | 45.0 | 30 | 38.5 |
| Missing | 12 | 15.2 | 9 | 11.3 | 10 | 12.8 |
| Employment status | ||||||
| Full-time | 50 | 63.3 | 45 | 56.3 | 48 | 61.5 |
| Part-time or student | 12 | 15.2 | 9 | 11.3 | 10 | 12.8 |
| Not employed outside the home | 17 | 21.5 | 26 | 32.5 | 20 | 25.6 |
| Married/living with partner | 70 | 88.6 | 76 | 95.0 | 67 | 85.9 |
| Children in household | ||||||
| 1 | 16 | 20.3 | 15 | 18.8 | 12 | 15.4 |
| 2 | 36 | 45.6 | 35 | 43.8 | 40 | 51.3 |
| ≥ 3 | 27 | 34.2 | 30 | 37.5 | 26 | 33.3 |
| Meets physical activity recommendations* | 14 | 17.7 | 21 | 26.3 | 13 | 16.7 |
| Pre-diabetes | 25 | 31.6 | 31 | 38.8 | 29 | 37.2 |
| Hypertension | 15 | 19.0 | 15 | 18.8 | 7 | 9.0 |
| GEM treatment arm | ||||||
| Usual care | 42 | 53.2 | 42 | 52.5 | 41 | 52.6 |
| Intervention | 37 | 46.8 | 38 | 47.5 | 37 | 47.4 |
| Intention to participate in a lifestyle program (% likely) | 16 | 20.3 | 17 | 21.3 | 22 | 28.2 |
GEM: Gestational Diabetes’ Effects on Moms trial.
n = 1 missing.
n = 1 Pacific Islander.
n = 14 African American, 15 multiethnic, and 3 unknown.
Baseline characteristics were comparable across conditions (P-values ≥ .14).
As shown in Table 3, exposure to the streamlined values affirmation promoted participants’ interest in preventive programs. Compared to control, those randomized to the values affirmation more frequently demonstrated interest in a lifestyle program (59.0% vs. 74.4%; RR 1.31 [95% CI 1.04 to 1.66]; P = .02) and more frequently sought NIH information about diabetes prevention (59.0% vs. 73.4%; RR 1.22 [0.97 to 1.54]; P = .09), although the latter did not reach significance. In contrast, as compared to control, those randomized to the parenting affirmation demonstrated interest in a lifestyle program (59.0% vs. 67.5%; RR 1.19 [0.94 to 1.50]; P = .15) and sought information about diabetes prevention (59.0% vs. 62.5%; RR 1.05 [0.82 to 1.36]; P = .69) at more similar rates.
Table 3.
Effects of condition on outcomes and process measures, with proportions and adjusted relative risks (RRs) or adjusted means and standard errors, among participants with a history of gestational diabetes: The Patients Engaged in Prevention (PEP) study
| Condition | |||||||
|---|---|---|---|---|---|---|---|
| Values affirmation | Parenting affirmation | Control | Values affirmation vs. control |
Parenting affirmation vs. control |
|||
| Outcomes | % (n) | % (n) | % (n) | RR (95% CI) | P-value | RR (95% CI) | P-value |
| Demonstrated interest in lifestyle program*† | 74.4 (58) | 67.5 (54) | 59.0 (46) | 1.31 (1.04, 1.66) | .02 | 1.19 (0.94, 1.50) | .15 |
| Sought information about diabetes prevention | 73.4 (58) | 62.5 (50) | 59.0 (46) | 1.22 (0.97, 1.54) | .09 | 1.05 (0.82, 1.36) | .69 |
| Process measures | % (n) | % (n) | % (n) | RR (95% CI) | P | RR (95% CI) | P |
| Attended to message | 76.0 (60) | 86.3 (69) | 68.0 (53) | 1.12 (0.92, 1.37) | .26 | 1.27 (1.06, 1.51) | < .01 |
| Mean (SE) | Mean (SE) | Mean (SE) | F-statistic | P-value | F-statistic | P-value | |
| Message acceptance | |||||||
| Persuasiveness† | 5.12 (0.12) | 5.13 (0.12) | 5.01 (0.12) | 0.42 | .52 | 0.47 | .49 |
| Derogation† | 1.86 (0.12) | 2.01 (0.12) | 1.72 (0.12) | 0.73 | .39 | 3.00 | .08 |
| Threat | 1.49 (0.09) | 1.46 (0.09) | 1.45 (0.09) | 0.10 | .75 | 0.01 | .93 |
| Self-integrity | 5.52 (0.12) | 5.67 (0.12) | 5.38 (0.12) | 0.67 | .42 | 3.00 | .08 |
All analyses adjusted for randomization variables (i.e., GEM treatment arm, body mass index, race/ethnicity, and education).
Analysis further adjusted for baseline intentions to participate in lifestyle program.
n=1 missing.
In sensitivity analyses, the GEM treatment arm by condition interaction was not significant for the first outcome, demonstrated interest in a lifestyle program (P = .72). The interaction was significant for the second outcome, seeking NIH information about diabetes prevention (P = .02). Subsequent analyses stratified by GEM treatment arm indicated that, as compared to control, both the values affirmation (46.3% vs. 73.8%; RR 1.58 [95% CI 1.08 to 2.32]; P = .02) and parenting affirmation (46.3% vs. 69.1%; RR 1.51 [1.02 to 2.23]; P = .04) improved information seeking behavior for those who had been in the GEM usual care arm. In contrast, neither the values affirmation (73.0% vs. 73.0%; RR 0.96 [0.73 to 1.27]; P = .78) nor the parenting affirmation (73.0% vs. 55.3%; RR 0.76 [0.54 to 1.07]; P = .11) improved information seeking for those who had been in the GEM intervention arm.
Process measures showed that, as compared to control, participants randomized to the values affirmation attended to the message at similar rates (68.0% vs. 76.0%; RR 1.12 [95% CI 0.92 to 1.37]; P = .26). In contrast, as compared to control, those randomized to the parenting affirmation more frequently attended to the message (68.0% vs. 86.3%; RR 1.27 [1.06 to 1.51]; P < .01; Table 3). All other process measures were comparable across conditions (Table 3).
Discussion
In this randomized study, women at high risk for diabetes were 31% more likely to demonstrate interest (i.e., seek information or intend to participate) in a health system-based preventive lifestyle program after being exposed to a streamlined values affirmation. Given that most diabetes prevention programs report participation rates of less than 20%,5 innovative strategies are needed to promote such programs to the high-risk patients who may benefit from them most. This study adds to the evidence base for theory-driven, empirically-tested interventions capable of promoting patients’ interest in preventive programs.
As compared to an active control condition, the streamlined values affirmation developed here increased the proportion of participants who demonstrated interest in a preventive program by 25%; it also increased the proportion who sought NIH information about diabetes prevention by 24%, although the latter did not reach statistical significance. We observed these effects despite finding that participants randomized to the values affirmation reported no differences in attention to or acceptance of the outreach message as compared to control, nor differences in self-integrity. Like others, this study leaves unanswered questions about the mechanisms by which values affirmation interventions influence intention and behavior.14 Research is needed to identify mediators responsible for such outcomes, particularly in adult (vs. student) samples.13
Despite garnering greater attention to the outreach message, participants randomized to an exploratory parenting affirmation demonstrated no significant differences in outcome and process measures as compared to control, with only a slight, non-significant difference in self-integrity. Parents may consider family as a domain in which they are usually able to excel and feel in control; and being a good parent as a domain important to their identity, despite also being a source of negative feedback (Fotuhi O, Cohen GL, unpublished observations, 2013). Family-related affirmations thus may engender negative as well as positive reactions.38 The values affirmation may have been better able to invoke positive aspects of the self, uncomplicated by the “double edged sword” of parenting. Although it seems intuitive to affirm parenting, it may backfire since it is in the domain of threat, narrowing people’s focus on the provoking threat.8 Because parenting is relevant to pregnancy, and pregnancy was the source of increased diabetes risk due to GDM, this may have dampened the parenting affirmation’s impact.
The brief and “passive” affirmation tested here yielded results consistent with those of more writing-intensive values affirmation interventions shown to improve diabetes risk assessment, physical activity, and patient-provider communication.16,17,39 Given its simplicity, the intervention described here—a simple two-sentence affirmation without the typical writing exercise, embedded in an outreach message feasible for large-scale distribution via email—may be practical to implement in health systems equipped for population-based outreach. Future research could examine whether additional modalities (e.g., text message) or repeated outreach could enhance the effectiveness of this intervention by increasing exposure to affirming content.
Study strengths include the randomized design; active comparison group; and clinically important sample. Additional strengths include our use of theory to develop the affirmations and the main text of the outreach message; and our use of a standard taxonomy of behavior change techniques to document intervention content. Limitations include, first, that the outreach message was lengthy (given inclusion of multiple behavior change techniques) and was situated in a research context rather than an actual encounter with a physician. A shorter, interactive message delivered directly from a physician could have greater impact; this could be examined in future research. Second, this initial study did not examine actual program participation, given the limited scope and sample size. Third, the streamlined values affirmation did not impact self-integrity—perhaps due to using a streamlined affirmation, rather than a traditional writing-based affirmation. Yet the affirmation was designed to reduce threat, which leads to defensive disengagement; and results indicate the affirmation had its intended impact of reducing disengagement. Controlled studies should determine whether the streamlined affirmation actually leads to greater reflection on values; and whether its mechanism of action differs from that of a writing-based affirmation. A final consideration is that the study participants were previously identified in GEM, a pragmatic trial among women diagnosed with GDM in a 1-year period (rather than a traditional trial among research volunteers). However, we balanced GEM treatment arm across conditions and controlled for it in analyses. We further tested for interactions between GEM treatment arm and condition as assigned here. We found no evidence that the GEM intervention arm primed participants’ receptivity to the affirmations tested here. Instead, it was among those who had been in the GEM usual care arm—a “naïve” subgroup not previously offered a lifestyle program after their index GDM pregnancy—that the affirmations improved NIH information seeking by over 50%. Larger studies should confirm these effects in other patient populations and healthcare settings.
In sum, a streamlined values affirmation, designed to be feasible for large-scale implementation in a clinical setting, can promote interest in programs to prevent diabetes among women with elevated BMI and a history of GDM. Future research is needed to evaluate whether benefits translate into changes in actual diabetes prevention program enrollment, program retention, and clinical outcomes.
Supplementary Material
Acknowledgments:
The authors thank the study participants as well as Alyce Adams, PhD and Julie Schmittdiel, PhD, Division of Research, Kaiser Permanente Northern California, for their input on the manuscript.
Funding: This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (grant K01 DK099404) and the Agency for Healthcare Research and Quality (grant R01 HS019367). SDB and AF also received support from National Institute of Diabetes and Digestive and Kidney Diseases grant P30 DK092924. The authors collected, analyzed, and interpreted the data and drafted the manuscript independently from the sponsors.
Footnotes
Disclosures: The authors declare they have no relevant conflicts of interest to disclose.
Prior presentations: Portions of this study were presented at the 39th Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine, April 11–14, 2018, New Orleans, LA.
References
- 1.Ferrara A, Hedderson MM, Quesenberry CP, et al. Prevalence of gestational diabetes mellitus detected by the National Diabetes Data Group or the Carpenter and Coustan plasma glucose thresholds. Diabetes Care. 2002;25(9):1625–1630. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy L, Casas JP, Hingorani AD, et al. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet. 2009;373:1773–1779. [DOI] [PubMed] [Google Scholar]
- 3.Kim C Maternal outcomes and follow-up after gestational diabetes mellitus. Diabet Med. 2014;31(3):292–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93(12):4774–4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aziz Z, Absetz P, Oldroyd J, et al. A systematic review of real-world diabetes prevention programs: Learnings from the last 15 years. Implement Sci. 2015;10(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessels LTE, Ruiter RAC, Jansma BM. Increased attention but more efficient disengagement: Neuroscientific evidence for defensive processing of threatening health information. Health Psychol. 2010;29(4):346–354. [DOI] [PubMed] [Google Scholar]
- 7.van ‘t Riet J, Ruiter RAC. Defensive reactions to health-promoting information: an overview and implications for future research. Health Psychology Review. 2013;7(sup1):S104–S136. [Google Scholar]
- 8.Cohen GL, Sherman DK. The psychology of change: Self-affirmation and social psychological intervention. Annu Rev Psychol. 2014;65:333–371. [DOI] [PubMed] [Google Scholar]
- 9.Hamel MS, Werner EF. Interventions to Improve Rate of Diabetes Testing Postpartum in Women With Gestational Diabetes Mellitus. Curr Diab Rep. 2017;17(2):7. [DOI] [PubMed] [Google Scholar]
- 10.Steele CM. The psychology of self-affirmation: Sustaining the integrity of the self In: Advances in experimental social psychology, Vol. 21: Social psychological studies of the self: Perspectives and programs. San Diego, CA, US: Academic Press; 1988:261–302. [Google Scholar]
- 11.Kessels LTE, Ruiter RAC, Brug J, et al. The effects of tailored and threatening nutrition information on message attention. Evidence from an event-related potential study. Appetite. 2011;56(1):32–38. [DOI] [PubMed] [Google Scholar]
- 12.McQueen A, Klein WMP. Experimental manipulations of self-affirmation: A systematic review. Self and Identity. 2006;5(4):289–354. [Google Scholar]
- 13.Sweeney AM, Moyer A. Self-affirmation and responses to health messages: A meta-analysis on intentions and behavior. Health Psychol. 2015;34(2):149–159. [DOI] [PubMed] [Google Scholar]
- 14.Epton T, Harris PR, Kane R, et al. The impact of self-affirmation on health-behavior change: A meta-analysis. Health Psychol. 2015;34(3):187–196. [DOI] [PubMed] [Google Scholar]
- 15.Ferrer RA, Cohen GL. Reconceptualizing self-affirmation with the Trigger and Channel framework: Lessons from the health domain. Personality and Social Psychology Review. 2018. (in press). [DOI] [PubMed] [Google Scholar]
- 16.Peterson JC, Charlson ME, Hoffman Z, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med. 2012;172(4):329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Havranek EP, Hanratty R, Tate C, et al. The effect of values affirmation on race-discordant patient-provider communication. Arch Intern Med. 2012;172(21):1662–1667. [DOI] [PubMed] [Google Scholar]
- 18.Creswell JW. A concise introduction to mixed methods research. Thousand Oaks, California: SAGE; 2015. [Google Scholar]
- 19.Gordon NP. Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011–12 California Health Interview Survey. 2015; http://www.dor.kaiser.org/external/chis_non_kp_2011/. Accessed July 6, 2015.
- 20.Karter AJ, Ferrara A, Liu JY, et al. Ethnic disparities in diabetic complications in an insured population. J Amer Med Assoc. 2002;287(19):2519–2527. [DOI] [PubMed] [Google Scholar]
- 21.Hsu WC, Araneta MR, Kanaya AM, et al. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care. 2015;38(1):150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrara A, Hedderson MM, Brown SD, et al. The Comparative Effectiveness of Diabetes Prevention Strategies to Reduce Postpartum Weight Retention in Women With Gestational Diabetes Mellitus: The Gestational Diabetes’ Effects on Moms (GEM) Cluster Randomized Controlled Trial. Diabetes Care. 2016;39(1):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown SD, Grijalva CS, Ferrara A. Leveraging EHRs for patient engagement: Perspectives on tailored program outreach. Am J Manag Care. 2017;23(7):e223–e230. [PMC free article] [PubMed] [Google Scholar]
- 24.Kiernan M, Schoffman DE, Lee K, et al. The Stanford Leisure-Time Activity Categorical Item (L-Cat): A single categorical item sensitive to physical activity changes in overweight/obese women. Int J Obes. 2013;37:1597–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein WMP, Lipkus IM, Scholl SM, et al. Self-affirmation moderates effects of unrealistic optimism and pessimism on reactions to tailored risk feedback. Psychology & Health. 2010;25(10):1195–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saghaei M, Saghaei S. Implementation of an open-source customizable minimization program for allocation of patients to parallel groups in clinical trials. J Biomed Sci Eng. 2011;4(11):734–739. [Google Scholar]
- 27.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31(1):103–115. [PubMed] [Google Scholar]
- 28.Scott NW, McPherson GC, Ramsay CR, et al. The method of minimization for allocation to clinical trials. a review. Control Clin Trials. 2002;23(6):662–674. [DOI] [PubMed] [Google Scholar]
- 29.Schmittdiel JA, Adams SR, Goler N, et al. The impact of telephonic wellness coaching on weight loss: A “Natural Experiments for Translation in Diabetes (NEXT-D)” study. Obesity (Silver Spring). 2017;25(2):352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cane J, Richardson M, Johnston M, et al. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol. 2015;20(1):130–150. [DOI] [PubMed] [Google Scholar]
- 31.Updegraff JA, Sherman DK, Luyster FS, et al. The effects of message quality and congruency on perceptions of tailored health communications. J Exp Soc Psychol. 2007;43:249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kreuter MW, Bull FC, Clark EM, et al. Understanding how people process health information: A comparison of tailored and nontailored weight-loss materials. Health Psychol. 1999;18:487–494. [DOI] [PubMed] [Google Scholar]
- 33.Jessop DC, Simmonds LV, Sparks P. Motivational and behavioural consequences of self-affirmation interventions: A study of sunscreen use among women. Psychology & Health. 2009;24(5):529–544. [DOI] [PubMed] [Google Scholar]
- 34.Armitage CJ, Harris PR, Arden MA. Evidence that self-affirmation reduces alcohol consumption: Randomized exploratory trial with a new, brief means of self-affirming. Health Psychol. 2011;30(5):633–641. [DOI] [PubMed] [Google Scholar]
- 35.Witte K Examples of items. 2010; https://www.msu.edu/~wittek/scale.htm. Accessed August 27, 2012.
- 36.Sherman DK, Cohen GL, Nelson LD, et al. Affirmed yet unaware: Exploring the role of awareness in the process of self-affirmation. J Pers Soc Psychol. 2009;97(5):745–764. [DOI] [PubMed] [Google Scholar]
- 37.Raab GM, Day S, Sales J. How to select covariates to include in the analysis of a clinical trial. Control Clin Trials. 2000;21(4):330–342. [DOI] [PubMed] [Google Scholar]
- 38.Charlson ME, Boutin-Foster C, Mancuso CA, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: Rationale, trial design, and methods. Contemp Clin Trials. 2007;28(6):748–762. [DOI] [PubMed] [Google Scholar]
- 39.van Koningsbruggen GM, Das E. Don’t derogate this message! Self-affirmation promotes online type 2 diabetes risk test taking. Psychol Health. 2009;24(6):635–649. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.