Abstract
Background
Few studies have evaluated the years of life lost (YLL) and productivity loss due to Sudden Unexpected Death (SUD). The burden of SUD on society is undetermined due to lack of population- based studies and comprehensive adjudication methods.
Objective
We estimated YLL and productivity loss from SUD in working age adults and compared it with leading causes of death in the United States.
Methods:
We screened all out of hospital deaths among people 20–64 in Wake County, North Carolina from 2013 to 2015 to adjudicate SUDs. We extrapolated Wake County incidence to estimate the age and sex standardized rate of SUD in the United States. YLL was calculated based on the remaining life expectancy of the victims. Incorporating market and housekeeping value estimated the present value of lifetime productivity loss due to SUD.
Results:
SUD incidence rates in the US adults 20–64 were 49.3 (95%CI: 41.2–58.3) and 21.7 (95%CI: 16.5–27.8) per 100000 among men and women, respectively. SUD resulted in the loss of 2 million years of life, accounting for 10.0% of YLL from all causes of death. Among natural causes of death, YLL from SUD was only lower than that from all cancers combined and heart disease. Lifetime productivity loss due to SUD was about $51 billion, exceeding productivity loss from any individual cancer.
Conclusion:
Sudden unexpected death is an important source of YLL and productivity loss among adults 20–64. Such high burden on society justifies prioritizing health policies and interventions toward preventing sudden unexpected death.
Keywords: Sudden Unexpected Death, Mortality Rate, Years of Potential Life Lost, Economic Value of Life
Introduction
Sudden death accounts for 180000 to 450000 deaths in the US yearly. (1, 2) Incidence of sudden death has not greatly declined despite the known reduction in total cardiovascular mortality. (3) The wide range in estimates of sudden death may be due to different criteria chosen for sudden death. The World Health Organization (WHO) defines sudden death as a witnessed death within 1 hour of symptoms onset or unwitnessed deaths within 24 hours of being observed alive and without symptoms. (4) However, this commonly used definition fails to include potential cases in which the precise time or etiology of death cannot be determined. (5, 6)
Although there is no consensus in literature on a common term and definition, Sudden Unexpected Death (SUD) in our study encompass all types of sudden death that are not attributed to trauma, suicide, etc or other apparent natural expected causes of death in adults. (7) The growing prevalence of risk factors such as obesity and diabetes may lead to an increase in SUD incidence in the coming years. (5) Although SUD occurs at all ages, the burden and productivity loss of SUD is not equal across age/sex groups, necessitating indices other than mortality rate to show the impact of SUD on society. (8, 9)
Years of life lost (YLL) is an indicator of premature mortality that takes into account the age at death in addition to the incidence in a way that more weight is given to deaths in the younger age. (10) Therefore, it summarizes age-specific mortality rates in an index that can be used to show social and economic consequences associated with mortality. (11, 12) Productivity loss is a measure that can be used to show the magnitude of a disease mortality in terms of an economic estimation. Although it does not show all the cost associated with a health problem, it can provide insight to the possible economic gain through preventive measures. (13, 14)
In this study, we aimed to calculate incidence of SUD in Wake County, North Carolina (NC), an ethnically diverse community with a population of about one million and to estimate the mortality rate, YLL, and productivity loss due to sudden unexpected death in the United States.
Methods
We used data from Sudden Unexpected Death in North Carolina (SUDDEN) project, a population-based study on all adjudicated out of hospital sudden unexpected deaths in Wake County, NC. The detailed methods and design of the SUDDEN project and data acquisition have been previously described. (15, 16) In summary, all out of hospital deaths ages 20–64 years in Wake County, NC from March 2013 to February 2015 were identified by performing an electronic query of the Emergency Medical Services (EMS) patient care reporting software (ESO Solutions V 4.8, Austin, Texas). Two trained research assistants used the information from EMS scene report, medical examiner, toxicology and autopsy reports (if available) to exclude nonresidents, residents of correctional facilities, non-natural causes of death such as trauma, suicide/homicide, and unintentional injuries. After the initial screening, medical records within the last five years were obtained through a systematic process for all cases. Finally, a majority decision by three cardiologists at University of North Carolina at Chapel Hill unaffiliated with the study reviewed all the available information to make the final SUD adjudication.
Population demographic data in 2014, including age and sex, were obtained for Wake County and the US population from the United States Census Bureau. (17) We considered sex-specific age groups of 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, and 60–64. The absolute incidence of SUD during the two-year study period was divided by two to estimate the average annual incidence. For each age/sex group, the incidence rate of SUD in Wake County was calculated by dividing the SUD incidence by the 2014 Wake population in that group. The SUD incidence rate of Wake County was subsequently age and sex standardized based on the 2014 US population. Sex-specific and overall national SUD incidence among 20–64 year olds was estimated by multiplying the standardized rates by the US population. The gamma distribution formula (18) was used to construct 95% confidence intervals for the US SUD incidence rates.
Life expectancy of each age/sex group was obtained from 2014 CDC National Vital Statistics Report. (19) We estimated YLL due to SUD by multiplying the estimated age/sex group specific SUD incidence by the US population’s group-specific expected remaining years of life. For example, for men ages 45–49, the CDC estimates an average of 34.2 years before death, and we estimate a SUD incidence of about 3851 per year for men ages 45–49. Thus, YLL for men aged 45–49 is estimated to be 34.2*3851, which represents about 130,000 years of life lost nationally attributable to SUD. For each age group, 10,000 Monte Carlo simulation replications were conducted using the binomial distribution of the Wake County SUD rates. The 2.5th and 97.5th percentiles of the simulated results were used to calculate the 95% uncertainty interval.
We used the estimates by Grosse and colleagues to calculate the lifetime productivity loss related to SUD, in which the market compensation and household production are used to estimate present value of lifetime productivity of a person by 3% discount rate, age group and gender. Lifetime productivity loss in each gender/age group was calculated by multiplying the mortality rate by estimated individual lifetime productivity. (13) All analyses were conducted with Microsoft Excel 2016 and SAS 9.4.
The CDC WONDER database report was used to identify the leading causes of death, and to obtain cause-specific and overall incidence of death by age/sex group in 2014 among individuals ages 20–64 in the US. (20) The overall YLL for all causes of death as well as the proportion of each cause was calculated. The leading causes of death were compared with SUD in terms of mortality rate, YLL, and productivity loss in different age groups.
Results
The population of Wake County in 2014 was 998,691 with about 67% White, 20% African- American and 6% Asian. United States population in 2014 was 318,857,056 with about 73% white, 13% African American and 5% Asian.
We estimated that approximately 67,390 SUDs (95% uncertainty interval: 45,655–89,408) occur annually among the adults ages 20–64 in the United States. The age and sex adjusted incidence rate for SUD among 20–64 years old was 35.1 per 100,000 (95% CI: 30.3–40.4). The rate among men was twice that of women (49.3 vs. 21.7 per 100,000). Three leading causes of death in adults 20–64 were all cancers combined, heart diseases, and unintentional injuries. In both genders, age adjusted rate of SUD was more than half of the mortality rate for heart diseases and was greater than any individual cancer, chronic lower respiratory diseases, diabetes mellitus, and cerebrovascular disease (Table 1).
Table 1-.
Incidence, years of life lost and mortality rate due to sudden unexpected death and leading causes of death among men and women aged 20–64 in United States.
| Male | Female | |||||
|---|---|---|---|---|---|---|
| Deaths | Years of Life Lost | Mortality Rate per 100000 | Deaths | Years of Life Lost | Mortality Rate per 100000 | |
| Sudden unexpected death* | 46580 | 1355685 | 49.3 (41.2–58.3) |
20811 | 648437 | 21.7 (16.5–27.8) |
| All cancers | 93095 | 2497763 | 98.5 | 82869 | 2571238 | 86.6 |
| Lung cancer | 23880 | 608116 | 25.3 | 18521 | 539631 | 19.3 |
| Colorectal Cancer | 9536 | 264425 | 10.1 | 6673 | 210409 | 7.0 |
| Prostate Cancer | 3090 | 74704 | 3.3 | - | - | - |
| Female Breast Cancer | - | - | - | 16559 | 530515 | 17.3 |
| Heart Disease | 85825 | 2397783 | 90.8 | 37802 | 1188932 | 39.5 |
| Unintentional injuries | 55942 | 2178365 | 59.2 | 24104 | 992072 | 25.2 |
| Chronic Lower Respiratory Disease | 11201 | 290301 | 11.9 | 10937 | 321925 | 11.4 |
| Diabetes Mellitus | 13726 | 386931 | 14.5 | 8583 | 270948 | 9.0 |
| Cerebrovascular Disease | 11195 | 314244 | 11.8 | 8274 | 260975 | 8.6 |
Sudden unexpected death data are extrapolated based on SUDDEN project.
Data for other causes of deaths are obtained from CDC WONDER database by using following International Classification of Diseases (ICD) 10 codes: C00-C97 for all cancers, C34 for lung cancer, C18-C20 for colorectal cancer, for C61 prostate cancer, C50 for female breast cancer, I00-I09, I11,I13, I20-I51 for heart disease, V01-X59,Y85-Y86 for unintentional injuries, J40-J47 for chronic lower respiratory disease, E10-E14 for diabetes mellitus, I60-I69 for cerebrovascular disease.
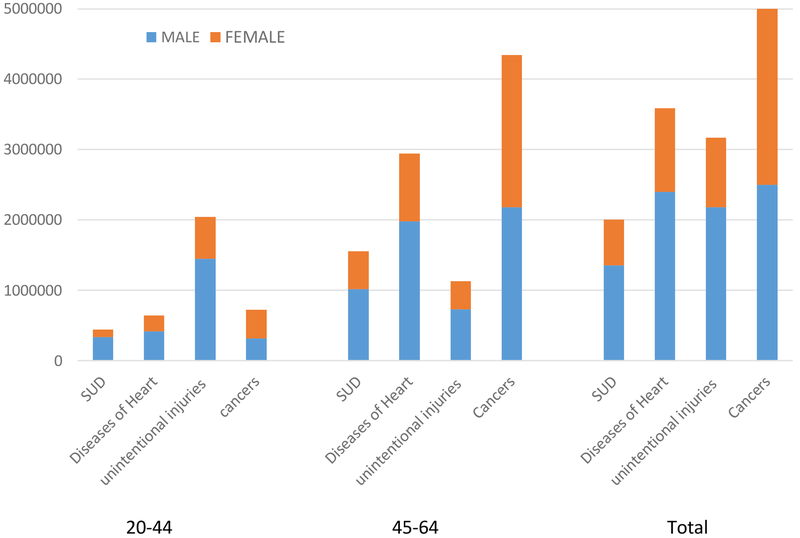
In total, more than 2 million years were lost due to SUD among adults 20–64 years of age (95 % uncertainty interval: 1.41–2.65). In men, SUD caused loss of 1.36 million years (95% uncertainty interval: 0.96–1.75) accounting for 10.8% of all cause YLL in men (12.57 million years). This was more than twice the YLL due to lung cancer, the most fatal cancer in men. Among women, YLL due to SUD was 0.65 million years (95% uncertainty interval: 0.42–0.90) accounting for 7.7% of all cause YLL in women (8.38 million years). Among those older than 45, SUD is the third leading cause of YLL after heart disease, and all cancers combined, exceeding unintentional injuries. Among victims younger than 45, YLL from SUD is lower than that from unintentional injuries, but it remains the third leading cause among males, surpassing all cancers combined (Figure 1).
Figure 1-.
Years of life lost from SUD and leading causes of death among adults aged 20–44 and 45–64
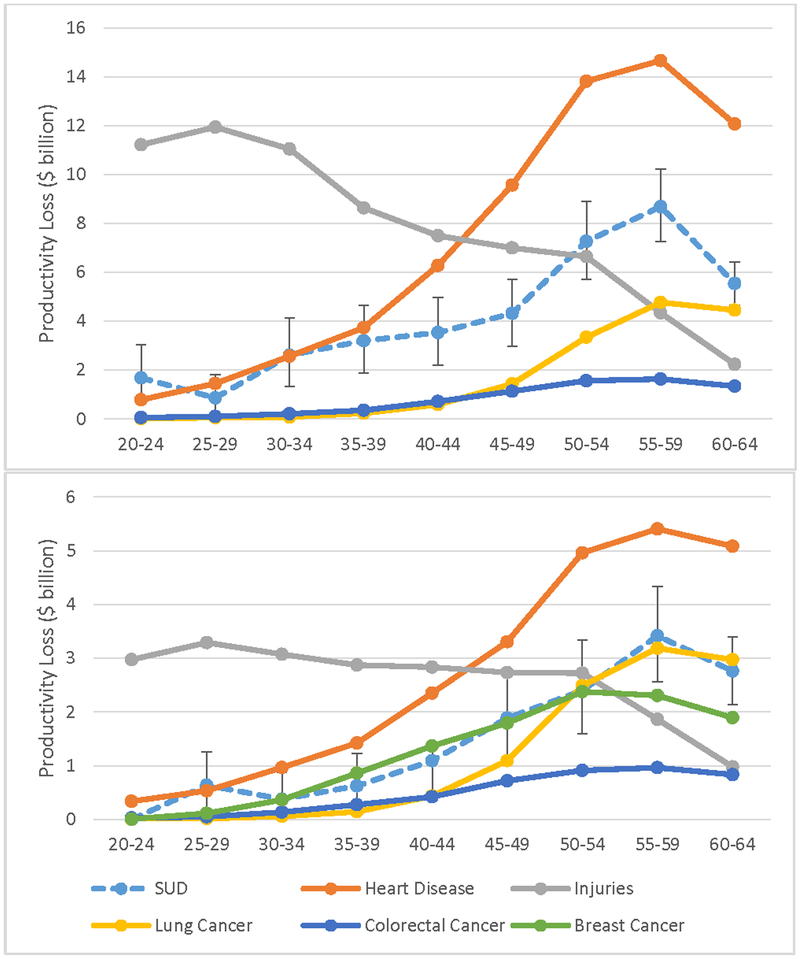
Lifetime productivity loss from SUD among 20–64 years old in 2014 was about 51 billion dollars. (2007 $US values) Being a direct product of deaths, lifetime productivity loss was higher in men compared to women. SUD was an important contributor to lifetime productivity loss in all age groups resulting in loss of 9.7 and 3.4 billion dollars among men and women only in the age group of 55–59 (Figure 2).
Figure 2-.
Productivity loss due to SUD and leading causes of death in different age groups in 2014 among a) men b) women aged 20–64 (95% uncertainty interval for SUD is shown in the figure.)
Discussion
In this study, we estimated the incidence of SUD and compared the associated burden with the leading causes of death in the US among men and women ages 20–64. The high burden of SUD on public health and economic productivity is neither calculated nor reported separately in public health studies. The Global Burden of Disease Project has published YLL due to different causes of death from the International Classification of Diseases (ICD) codes. (21) However, since SUD is reported under different ICD codes that cannot be aggregated easily, its burden cannot be shown using a single code or combined outcome. This concern underscores the importance of relying on sources other than death certificates to monitor incidence and harm to productivity from SUD in society. Because there is no national surveillance registry for sudden unexpected death, our estimates of YLL and productivity loss from SUD in a diverse population are valuable.
The estimated age and sex adjusted rate of SUD in men and women was 49.3 per 100000 (95% CI: 41.2–58.3) and 21.7 per 100000 (95% CI: 16.5–27.8) respectively. YLL due to SUD in people aged 20–65 years, accounted for 10.8% and 7.7% of all YLL in men and women, respectively. Premature mortality from SUD was associated with an estimated productivity loss of 51 billion dollars (2007 $US value), which exceeded that associated with any individual cancer. After Employment Cost Index adjustment (22), this number increases to approximately $59 billion in 2014 dollars.
Despite the important reduction in cardiovascular mortality over the past decades, the incidence of out of hospital cardiac arrest remained unacceptably high. (23) According to a meta-analysis by Berdowski and colleagues, the rate of out of hospital cardiac arrest in North America is higher compared to Europe, Asia and Australia (54.6 vs. 35, 28.3 and 44 respectively). (24) The survival rate for out of hospital cardiac arrest is very unfavorable with about 5 percent finally being discharged from hospital. (25) Reported improved survival in some studies should be interpreted with caution, considering the methodological and adjudication differences. (26) Limiting victims to those who received resuscitative efforts or those reported by selected health facilities in various studies may underestimate mortality in population. (27–29) The high national prevalence, poor prognosis and different estimates of incidence highlights the need for a reliable monitoring of SUD to guide preventive and therapeutic measures.
Our study has some limitations. One important limitation is collection of data from a single county. Also, we were not able to adjust by ethnicity; however, racial diversity of Wake County provided us with a good representative sample for the US population. In addition, we used the lifetime productivity loss estimates for the past decade; however, this data provided the most recent available estimates and newer data are not likely to change the comparisons. We excluded people younger than 20 and older than 65, so our results only reflect this age group of population. A strength of our study is that we did not exclude cases based on presumed etiology of SUD and we did not limit adjudication to causes of death provided in death certificates, which are prone to misclassification.
Conclusion
Sudden unexpected death is a major contributor to years of life lost in the US. High societal burden of sudden unexpected death necessitates allocating more resources toward addressing this public health problem. An extensive registry of ethnically diverse and representative population is needed to measure the health burden and impact of sudden unexpected death and evaluate the real life effectiveness of preventive measures.
Acknowledgments:
The Wake County EMS Data System supports, maintains, and monitors EMS service delivery, patient care, and disaster preparedness for the Wake County, NC community at large. This manuscript has been reviewed by Wake County EMS Data System investigators for scientific content and consistency of data interpretation with previous Wake County EMS Data System publications.
We would like to thank the North Carolina Office of the Chief Medical Examiner, SUDDEN team of researchers, and the North Carolina Translational and Clinical Sciences Institute at University of North Carolina at Chapel Hill.
Funding: The SUDDEN project is funded by individual, private donations, The Heart and Vascular Division of the University of North Carolina at Chapel Hill, and the McAllister Heart Institute. The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 1UL1TR001111. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of interest: We have no conflicts of interest to disclose relevant to this paper or its contents.
References:
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125(4):620–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circulation research. 2015;116(12):1887–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Sudden cardiac death. Report of a WHO Scientific Group. Available at: http://apps.who.int/iris/handle/10665/39554. Accessed February 28, 2018. [PubMed]
- 5.Adabag AS, Luepker RV, Roger VL, Gersh BJ. Sudden cardiac death: epidemiology and risk factors. Nature reviews Cardiology. 2010;7(4):216–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pratt CM, Greenway PS, Schoenfeld MH, Hibben ML, Reiffel JA. Exploration of the precision of classifying sudden cardiac death. Implications for the interpretation of clinical trials. Circulation. 1996;93(3):519–24. [DOI] [PubMed] [Google Scholar]
- 7.Nichols L, Chew B. Causes of sudden unexpected death of adult hospital patients. Journal of hospital medicine. 2012;7(9):706–8. [DOI] [PubMed] [Google Scholar]
- 8.Ackerman M, Atkins DL, Triedman JK. Sudden Cardiac Death in the Young. Circulation. 2016;133(10):1006–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaartjes I, Hendrix A, Hertogh EM, Grobbee DE, Doevendans PA, Mosterd A, et al. Sudden death in persons younger than 40 years of age: incidence and causes. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2009;16(5):592–6. [DOI] [PubMed] [Google Scholar]
- 10.Murray CJ, Lopez AD. Measuring the global burden of disease. The New England journal of medicine. 2013;369(5):448–57. [DOI] [PubMed] [Google Scholar]
- 11.McDonnell S, Vossberg K, Hopkins RS, Mittan B. Using YPLL in health planning. Public health reports (Washington, DC : 1974). 1998;113(1):55–61. [PMC free article] [PubMed] [Google Scholar]
- 12.Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. Jama. 2013;310(6):591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grosse SD, Krueger KV, Mvundura M. Economic productivity by age and sex: 2007 estimates for the United States. Medical care. 2009;47(7 Suppl 1):S94–103. [DOI] [PubMed] [Google Scholar]
- 14.Li C, Ekwueme DU, Rim SH, Tangka FK. Years of potential life lost and productivity losses from male urogenital cancer deaths--United States, 2004. Urology. 2010;76(3):528–35. [DOI] [PubMed] [Google Scholar]
- 15.Mounsey LA, Lin FC, Pursell I, Joodi G, Lewis ME, Nwosu A, et al. Relation of Household Income to Incidence of Sudden Unexpected Death in Wake County, North Carolina. The American journal of cardiology. 2017;119(7):1030–5. [DOI] [PubMed] [Google Scholar]
- 16.Nanavati PP, Mounsey JP, Pursell IW, Simpson RJ Jr., Lewis ME, Mehta ND, et al. Sudden Unexpected Death in North Carolina (SUDDEN): methodology review and screening results. Open heart. 2014;1(1):e000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2016 .Source: U.S. Census Bureau, Population Division. Available at: https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed January 24, 2018
- 18.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Statistics in medicine. 1997;16(7):791–801. [DOI] [PubMed] [Google Scholar]
- 19.Kenneth D, Kochanek MA, Sherry L et al. National vital statistics report, Deaths: Final Data for 2014. Available at https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdf. Accessed January 26, 2018. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999–2016 on CDC WONDER Online Database. Available at http://wonder.cdc.gov/ucd-icd10.html. Accessed on January 24, 2018.
- 21.Naghavi M, Abajobir AA, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1151–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Employment Cost Index Historical Listing. Available at : https://www.bls.gov/web/eci/echistrynaics.pdf. Accessed January 11, 2019.
- 23.Current Burden of Cardiac Arrest in the United States: Report from the Resuscitation Outcomes Consortium 2015 .Available at: http://www.nationalacademies.org/hmd/%20~/media/Files/Report%20Files/2015/ROC.pdf. Accessed January 24, 2018.
- 24.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87. [DOI] [PubMed] [Google Scholar]
- 25.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circulation Cardiovascular quality and outcomes. 2010;3(1):63–81. [DOI] [PubMed] [Google Scholar]
- 26.Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2011;60(8):1–19. [PubMed] [Google Scholar]
- 28.Stecker EC, Reinier K, Marijon E, Narayanan K, Teodorescu C, Uy-Evanado A, et al. Public health burden of sudden cardiac death in the United States. Circulation Arrhythmia and electrophysiology. 2014;7(2):212–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78(2):161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]