Abstract
We analyzed CIBMTR data to evaluate the incidence of non-relapse mortality (NRM) and association with overall survival (OS) for Bacterial blood stream infections (BSIs) occurring within 100 days of alloHCT in 2 different phases: pre/peri engraftment (BSI very early phase, BSI-VEP) and BSI post engraftment (BSI occurring between 2 weeks after engraftment and Day100, late early phase, BSI-LEP). Of 7,128 alloHCT patients, 2,656 (37%) had ≥1 BSI by day100. BSI-VEP, BSI-LEP, BSI-Both constituted 56% (n=1492), 31% (n=824), and 13% (n=340) of total BSI, respectively. Starting in 2009 we observed a gradual decline in BSI incidence through 2012 (61% to 48%). Patients with BSI-VEP were more likely to receive a myeloablative conditioning (MAC) regimen with total body irradiation (TBI). NRM was significantly higher in patients with any BSI (RR 1.82 95CI 1.63–2.04 for BSI-VEP, RR 2.46, 95%CI 2.05–2.96 for BSI-LEP, and RR 2.29, 95%CI 1.87–2.81 for BSI-Both) compared with those without BSI. OS was significantly lower in patients with any BSI compared with patients without BSI (RR 1.36, 95%CI 1.26–1.47 for BSI-VEP; RR 1.83, 95%CI 1.58–2.12 for BSI-LEP: RR 1.66, 95%CI 1.43–1.94 for BSI-Both). BSIs within day100 after alloHCT are common and remain a risk factor for mortality.
Keywords: Bacterial stream infections, allogeneic hematopoietic cell transplantation, engraftment, mortality
Introduction
Bacterial blood stream infections (BSIs) are common after allogeneic hematopoietic cell transplantation (alloHCT), occurring in 20 to 45% of patients.1–7 The main predisposing factor for pre-engraftment BSI are mucosal injury (mucosal barrier injury laboratory-confirmed bloodstream infection, MBI- LCBI)8 or the presence of an indwelling central catheter (central line-associated BSI, CLABSI)9. Higher incidence of BSI has been reported for umbilical cord blood (UCB),6,10 or bone marrow7 allografts (compared with peripheral blood), unrelated donors1,6 (compared with related), HLA-mismatched donors11 (compared with mismatched), myeloablative conditioning12 (compared with nonmyeloablative conditioning) and advanced leukemia1. In addition, graft-versus-host disease (GVHD),5 and steroid use,13,14 have been associated with higher BSI incidence. In single center studies, BSI is associated with increased mortality at 1 year after alloHCT.6,11,14,15
We analyzed the registry data from the Center for International Blood and Marrow Transplant Research (CIBMTR) to assess the impact of early BSI (by day 100) on transplant outcomes including overall survival (OS), non-relapse mortality (NRM), disease-free survival (DFS) and relapse at 1 year after alloHCT. Two BSI time-frames were examined: pre/peri-engraftment phase [Very Early Phase (VEP)], and post-engraftment phase, 2 weeks after engraftment through day 100 [Late Early Phase (LEP)]. Transplant outcomes for patients with BSI-VEP, BSI-LEP, and both BSIs were compared with patients without BSI.
Material and Methods
Study Population
The study population included all patients receiving first alloHCT for acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), and myelodysplastic syndrome (MDS) in pediatric and adult patients between January 2008 and December 2012. Grafts from related (including haploidentical) and unrelated (URD) donors were included. Graft sources included bone marrow (BM), peripheral blood stem cells (PBSC), and UCB. T cell depleted grafts were also included. Patients who had a prior alloHCT were excluded.
Data Source
The CIBMTR is a voluntary working group of more than 450 transplantation centers worldwide that contribute detailed data on consecutive hematopoietic cell transplants to a statistical center located at the Medical College of Wisconsin in Milwaukee and the National Marrow Donor Program (NMDP) Coordinating Center in Minneapolis. Participating centers are required to report all transplantations consecutively; compliance is monitored by onsite audits. The CIMBTR maintains an extensive database of detailed patient-, transplant-, and disease-related information, and prospectively collects data longitudinally with yearly follow-ups. Observational studies conducted by the CIBMTR are performed in compliance with HIPAA regulations as a public health authority and also in compliance with all applicable federal regulations pertaining to the protection of human research participants, as determined by a continuous review by the Institutional Review Boards of NMDP and the Medical College of Wisconsin. The CIBMTR collects data at two levels: Transplant Essential Data (TED) and Comprehensive Report Form (CRF) data. TED data include disease type, age, gender, pre-transplant disease stage and chemotherapy-responsiveness, date of diagnosis, graft type (bone marrow- and/or blood-derived stem cells), conditioning regimen, post-transplant disease progression and survival, development of a new malignancy and cause of death. All CIBMTR centers contribute TED data. CRF data are collected on a subset of registered patients, selected by weighted randomization. CRF data include more detailed disease and pre- and post-transplant clinical information, including infection data. TED and CRF level data are collected pre-transplant, 100 days and six months post-HCT and annually thereafter or until death. This analysis includes only CIBMTR CRF data.
Infection Data
Data for infections are captured on the CRF using an organism code, site of infection, and date of infection. BSI was defined as the isolation of a bacterial pathogen from the blood/buffy coat obtained from peripheral blood or a central venous catheter. Patients from 50 centers (n=268) were excluded from the analysis due to the center reporting 100% of patients with BSI, 0% of patients with BSI, or 100% of BSI due to coagulase negative Staphylococcus spp. BSI was considered “recurrent” if there was at least 7 days between the dates of reported infection for the same organism. Data regarding antibacterial prophylaxis, treatment and infection severity are not collected in the registry and, therefore, unavailable for analyses.
Definitions
Bacterial BSI was analyzed from day −10 (D-10) through 100 days after transplant (D100). BSI reported after D100 was not included in the analyses. Based on onset of BSI relative to neutrophil recovery, BSIs were grouped into pre/peri- and post-neutrophil engraftment. Pre/peri-engraftment or very early phase (“BSI-VEP”) BSI was defined as infection occurring between D-10 through 14 days after neutrophil engraftment. Post-engraftment or late early phase (“BSI-LEP”) BSI was defined as infection occurring between 15 days after neutrophil engraftment until D100. Patients with both BSI-VEP and BSI-LEP were designated as “BSI-Both”. Patients who did not develop any BSI by D100 are defined as “no BSI” and served as the control population. Recurrent bacterial infections required a minimum of 7 days between cultures with the same organism reported. Neutrophil engraftment was defined as the first of 3 consecutive days with an absolute neutrophil count ≥ 500/mm3. Platelet engraftment was defined as a platelet count ≥20,000/mm3 without platelet transfusions in the prior 7 days. Acute and chronic GVHD was scored by standard criteria.16–18 The use of growth factors between day −3 through day 15 post-transplant was collected.
Statistics
Patient-, disease-, and transplant –related factors were compared between groups using the Chi-square test for categorical variables and Wilcoxon two-sample testing for continuous variables. Time-dependent variables (neutrophil and platelet engraftment and acute GVHD) occurring after transplant and prior to d100 are descriptive only since these events occurred variably by patient in relation to the bacterial BSI event that categorized the cohorts. Probabilities of OS and DFS were calculated using the Kaplan-Meier estimator. Values for relapse and NRM were generated using cumulative incidence estimates to account for competing risks. Because the patient populations are determined by an event occurring (or not) by D100, we performed univariate analyses for both the entire population from the time of transplant (D0) as well as a left-truncated analysis for only those patients alive at D100 (data not shown). As trends and statistical significance for all events were the same, this manuscript reports the results for the entire population unless otherwise specified. A Cox model for the entire population was fit to determine factors important for OS, DFS, relapse, and NRM and the main effect variable was the time-dependent variable of no BSI (reference) versus BSI-VEP versus BSI-LEP versus BSI-both forced into every model. The proportional hazards assumption was checked; when violated, the co-variate was included as a time-dependent covariate. Center effect was tested using the score test of Commenges and Andersen.19 If there is found to be a center effect, then the results are adjusted accordingly to account for this. Variables examined in the multivariable models included: age (≤ 20 years vs 21 – 40 years vs 41 – 50 years vs >60 years); Karnofsky performance status (≥ 90% vs <90%); Disease stage (AML/ALL early (CR1) vs AML/ALL intermediate (≥CR2) vs AML/ALL Advanced (relapsed/refractory), vs MDS early (RA, RARS, RCMD, RCMD/RS) vs MDS Advanced (RAEB1, RAEB2)); HCT-CI (0 vs 1 – 2 vs ≥3); donor/recipient CMV serostatus (both negative vs any positive); Conditioning intensity (myeloablative vs non-myeloablative/reduced intensity); Donor/HLA-Match (HLA-identical sibling vs 8/8 unrelated vs mismatched unrelated vs UCB vs other [mismatched related/Haploidentical or unrelated with HLA missing]); ATG/Campath use (no vs yes); GVHD prophylaxis (calcineurin inhibitor [CNI]+ methotrexate ± others vs. CNI + mycophenylate mofetil ± others vs. T-cell depletion [in vivo or ex vivo] vs. Other); and year of HCT (2008 – 2009 vs 2010 – 2012). Due to clinical suspicion of an impact of acute GVHD and its therapy on the development of BSI and transplant outcomes, separate Cox models were fit forcing in the co-variate of development of acute GVHD at any time, aGVHD occurring prior to the development of the BSI, and without acute GVHD in the model. Important co-variates, relative risks, and statistical significance were unchanged between these three models for all transplant outcomes; therefore, the models shown do not include acute GVHD.
Results:
Blood stream infections (BSIs)
Of total 7,128 alloHCT, 2,656 (37%) had ≥1 BSI by D100 (Table 1). Of these 2,656 patients, 1891 (71%) had one BSI [762 (66%) by one single organism and 129 (5%) by >1 organisms (polymicrobial)] and 765 (29%) had >1 BSIs. (Figure 1 and Supplemental Table 1). BSI-VEP comprised 56% of total BSI (n=1492); BSI-LEP or BSI-Both comprised 31% (n=824) and 13% (n=340), respectively.
Table 1.
Comparison of clinical characteristics among the four patient groups.
| Characteristic | BSI-VEP Total n(%) | BSI-LEP Total n(%) | BSI-Both Total n(%) | No BSI Total n(%) | P-Value |
|---|---|---|---|---|---|
| Number of patients | 1,492 | 824 | 340 | 4,472 | |
| Number of centers | 165 | 138 | 105 | 177 | |
| Gender, Male | 836 (56) | 446 (54) | 187 (55) | 2,483 (56) | 0.840 |
| Age, years median (range) | 42 (<1–75) | 46 (<1–79) | 42 (1–74) | 49 (<1–78) | <0.001 |
| ≤10 | 214 (14) | 93 (11) | 56 (16) | 405 ( 9) | |
| 11–20 | 179 (12) | 98 (12) | 40 (12) | 338 ( 8) | |
| 21–30 | 162 (11) | 84 (10) | 31 ( 9) | 430 (10) | |
| 31–40 | 163 (11) | 87 (11) | 30 ( 9) | 452 (10) | |
| 41–50 | 222 (15) | 120 (15) | 58 (17) | 725 (16) | |
| 51–60 | 327 (22) | 175 (21) | 75 (22) | 1,064 (24) | |
| >60 | 225 (15) | 167 (20) | 50 (15) | 1,058 (24) | |
| KPS | 0.915 | ||||
| <90 | 470 (32) | 265 (32) | 103 (30) | 1,392 (31) | |
| 90–100 | 995 (67) | 541 (66) | 233 (69) | 2,996 (67) | |
| Missing | 27 ( 2) | 18 ( 2) | 4 ( 1) | 84 ( 2) | |
| HCT-CI | 0.530 | ||||
| 0 | 650 (44) | 353 (43) | 140 (41) | 1,927 (43) | |
| 1 | 224 (15) | 114 (14) | 55 (16) | 649 (15) | |
| 2 | 159 (11) | 91 (11) | 44 (13) | 536 (12) | |
| ≥3 | 433 (29) | 321 (30) | 95 (28) | 1,263 (28) | |
| Missing | 26 ( 2) | 13 ( 2) | 6 ( 2) | 97 ( 2) | |
| Conditioning intensity | <0.001 | ||||
| Myeloablative | 1,207 (81) | 617 (75) | 276 (81) | 3,149 (70) | |
| RIC/NMA | 285 (19) | 207 (25) | 64 (19) | 1,323 (30) | |
| TBI dose | <0.001 | ||||
| No TBI | 664 (45) | 430 (52) | 156 (46) | 2,480 (55) | |
| ≤1200 cGy | 454 (30) | 265 (32) | 110 (32) | 1,297 (29) | |
| >1200 cGy | 374 (25) | 129 (16) | 74 (22) | 695 (16) | |
| Disease status at HCT | <0.001 | ||||
| AML/ALL Early | 596 (40) | 325 (39) | 132 (39) | 1,908 (43) | |
| AML/ALL Intermediate | 378 (25) | 192 (23) | 88 (26) | 884 (20) | |
| AML/ALL Advanced | 254 (17) | 115 (14) | 57 (17) | 613 (14) | |
| MDS Early | 95 ( 6) | 70 ( 8) | 26 ( 8) | 415 ( 9) | |
| MDS Advanced | 156 (10) | 119 (14) | 34 (10) | 630 (14) | |
| Missing | 13 (<1) | 3 (<1) | 3 (<1) | 22 (<1) | |
| Time to AlloHCT, median (range), months | 7 (<1–313) | 7 (<1–173) | 7 (1–224) | 6 (<1–291) | 0.059 |
| Donor age, in decades | <0.001 | ||||
| UCB | 593 (40) | 210 (25) | 113 (33) | 918 (21) | |
| Related donor | 366 (25) | 211 (26) | 87 (26) | 1,454 (33) | |
| 18–20 | 43 ( 3) | 28 ( 3) | 8 ( 2) | 148 ( 3) | |
| 21–30 | 193 (13) | 157 (19) | 43 (13) | 857 (19) | |
| 31–40 | 118 ( 8) | 98 (12) | 34 (10) | 479 (11) | |
| 41–50 | 96 ( 6) | 63 ( 8) | 38 (11) | 321 ( 7) | |
| 51–60 | 28 ( 2) | 24 ( 3) | 4 ( 1) | 97 ( 2) | |
| Missing | 55 ( 4) | 33 ( 4) | 13 ( 4) | 198 ( 4) | |
| Donor-recipient sex match | 0.799 | ||||
| Male-Male | 522 (35) | 269 (33) | 108 (32) | 1,554 (35) | |
| Male-Female | 359 (24) | 231 (28) | 88 (26) | 1,128 (25) | |
| Female-Male | 310 (21) | 174 (21) | 78 (23) | 909 (20) | |
| Female-Female | 292 (20) | 145 (18) | 63 (19) | 851 (19) | |
| Missing | 9 (<1) | 5 (<1) | 3 (<1) | 30 (<1) | |
| Donor-recipient CMV status | 9 (<1) | 5 (<1) | 3 (<1) | 30 (<1) | <0.001 |
| +/+ | 291 (20) | 179 (22) | 77 (23) | 1,043 (23) | |
| +/− | 98 ( 7) | 49 ( 6) | 27 ( 8) | 418 ( 9) | |
| −/+ | 646 (43) | 328 (40) | 142 (42) | 1,627 (36) | |
| −/− | 441 (30) | 256 (31) | 85 (25) | 1,307 (29) | |
| Both missing | 16 ( 1) | 12 ( 1) | 9 ( 3) | 77 ( 2) | |
| Graft type | <0.001 | ||||
| Bone marrow | 239 (16) | 114 (14) | 52 (15) | 662 (15) | |
| PBSC | 660 (44) | 500 (61) | 175 (51) | 2,892 (65) | |
| Umbilical Cord blood | 593 (40) | 210 (25) | 113 (33) | 918 (21) | |
| Donor/recipient HLA match | <0.001 | ||||
| Umbilical Cord blood | 593 (40) | 210 (25) | 113 (33) | 918 (21) | |
| HLA-identical siblings | 337 (23) | 196 (24) | 78 (23) | 1,379 (31) | |
| Matched/Mismatched related | 5 (<1) | 2 (<1) | 3 (<1) | 20 (<1) | |
| Haplo-identical | 24 ( 2) | 13 ( 2) | 6 ( 2) | 55 ( 1) | |
| 8/8 unrelated | 382 (26) | 277 (34) | 85 (25) | 1,558 (35) | |
| 7/8 unrelated | 114 ( 8) | 98 (12) | 42 (12) | 401 ( 9) | |
| <=6/8 unrelated | 10 (<1) | 5 (<1) | 7 ( 2) | 27 (<1) | |
| Unrelated (HLA match information missing) | 27 ( 2) | 23 ( 3) | 6 ( 2) | 114 ( 3) | |
| ATG/Alemtuzumab as conditioning/GVHD prophy | 0.240 | ||||
| ATG alone | 442 (30) | 244 (30) | 102 (30) | 1,367 (31) | |
| Alemtuzumab alone | 36 ( 2) | 9 ( 1) | 11 ( 3) | 89 ( 2) | |
| No ATG or Alemtuzumab | 1,014 (68) | 571 (69) | 227 (67) | 3,016 (67) | |
| GVHD prophylaxis | <0.001 | ||||
| CSA/TAC + MTX ± others | 659 (44) | 411 (50) | 159 (48) | 2,398 (54) | |
| CSA/TAC + MMF ± others | 541 (36) | 297 (36) | 128 (38) | 1,393 (31) | |
| CSA/TAC + others | 166 (11) | 66 ( 8) | 31 ( 9) | 392 ( 9) | |
| CSA/TAC alone | 52 ( 3) | 20 ( 2) | 9 ( 3) | 145 ( 3) | |
| SIRO +/− others (Not TAC/CSA) | 3 (<1) | 1 (<1) | 0 | 15 (<1) | |
| ATG/ Alemtuzumab only | 0 | 0 | 0 | 7 (<1) | |
| Ex vivo T-cell depletion | 29 ( 2) | 10 ( 1) | 2 (<1) | 26 (<1) | |
| CD34 selection | 19 ( 1) | 2 (<1) | 5 ( 1) | 48 ( 1) | |
| Cyclophosphamide | 20 ( 1) | 15 ( 2) | 5 ( 1) | 81 ( 2) | |
| Other GVHD prophylaxis | 3 (<1) | 2 (<1) | 1 (<1) | 17 (<1) | |
| G-CSF, GM-CSF use, yes | 901 (60) | 498 (60) | 205 (60) | 2,379 (53) | <0.001 |
| Supplemental IVIG, yes | 712 (48) | 389 (47) | 191 (56) | 1,766 (39) | <0.001 |
| Year of AlloHCT | <0.001 | ||||
| 2008 | 448 (30) | 248 (30) | 121 (36) | 1,194 (27) | |
| 2009 | 410 (27) | 240 (29) | 97 (29) | 1,073 (24) | |
| 2010 | 284 (19) | 158 (19) | 56 (16) | 837 (19) | |
| 2011 | 177 (12) | 98 (12) | 42 (12) | 642 (14) | |
| 2012 | 173 (12) | 80 (10) | 24 ( 7) | 726 (16) |
Abbreviations: AlloHCT, allogeneic hematapoietic cell transplantation; ALC, absolute lymphocyte count; ANC, absolute neutrophil count; ATG, anti-thymocyte globulin; BSI, blood stream infections; CMV, cytomegalovirus; CSA, cyclosporine; G-CSF, granulocyte-colony forming factor; GM-CSF, granulocyte,monocyte- colony forming factor; GVHD, graft-versus-host disease; HCT-CI, Hematopoietic cell transplant comorbidity index; HLA, human leukocyte antigens; IVIG, intravenous immunoglobulin; KPS, Karnofsky Performance score; LEP, late early phase; MMF, mycophenolate mofetil; MTX, methotrexate; NMA, non-myeloablative; PBSC, peripheral blood stem cells; RIC, reduced-intensity conditioning; SIRO, sirolimus; TAC, tacrolimus; TBI, total body irradiation WBC, white blood cells; ; VEP, very early phase
Figure 1.
A.Patients with BSI per documented bacteria involved in BSI-VEP (left column) and BSI-LEP (middle column) and BSI-Both (right column) within 100 days (presented as %). Most of the BSI in VEP and LEP are composed of CoNS, Enterobacteriaceae, and other GPC.
B.Patients with BSI divided by episodes and single organism or polymicrobial infections. 63% of patients had no BSI whereas 9% of patients had ≥ 2 BSI.
The median time to first BSI-VEP was 7 days (range, D-1 to D74); and the median time to first BSI-LEP was 58 days (range, D21 to D100) (Table 2). Staphylococcus species (spp.) were the most common bacteria, and coagulase negative Staphylococcus (CoNS) accounted for over a quarter (n=647; 28%) of the infections reported (Figure 1A, Supplemental Table 1).
Table 2.
Description of time dependent variables of engraftment and acute GVHD among the four groups.
| Variable | VEP-BSI | LEP-BSI | Both-BSI | No BSI |
|---|---|---|---|---|
| Number of patients | 1,492 | 824 | 340 | 4,472 |
| Days to first BSI (range) | 7 (<1–74) | 58 (21–100) | 8 (<1–36) | |
| Time to ANC >500, n(%) | ||||
| Yes | 1,299 (87) | 824 | 340 | 4,321 (97) |
| No | 188 (13) | 0 | 0 | 138 ( 3) |
| Missing | 5 (<1) | 0 | 0 | 13 (<1) |
| Time to ANC >500 days (range) | 17 (<1–99) | 15 (<1–42) | 16 (1–50) | 15 (<1–111) |
| Platelet engraftment >20 ×109/L, n(%) | ||||
| Yes | 1,103 (74) | 721 (88) | 277 (81) | 4,049 (91) |
| No | 368 (25) | 96 (12) | 57 (17) | 395 ( 9) |
| Missing | 21 ( 1) | 7 (<1) | 6 ( 2) | 28 (<1) |
| Time to platelet >20×109/L, days (range) | 27 (1–180) | 20 (<1–293) | 26 (1–640) | 19 (<1–753) |
| aGVHD, n(%) | ||||
| Yes | 546 (37) | 433 (53) | 195 (57) | 1,673 (37) |
| No | 940 (63) | 387 (47) | 141 (41) | 2,783 (62) |
| Missing | 6 (<1) | 4 (<1) | 4 ( 1) | 16 (<1) |
| Time to aGVHD diagnosis, days (range) | 28 (7–175) | 27 (7–176) | 26 (7–168) | 29 (7–178) |
| Median follow-up of survivors, months (range) | 60 (3–87) | 60 (3–81) | 60 (12–85) | 59 (3–87) |
Abbreviations: aGVHD, acute graft-versus-host disease; ANC, absolute neutrophil count; cGVHD, chronic graft-versus-host disease; VEP, very early phase; LEP, late early phase
Of note, for the entire population the cumulative incidence by day 100 of fungal infection (any reported) was 8% and that of viral infections (any reported) was 44%. Because of the issues of timing of 3 time-dependent variables (BSI vs. fungal vs. viral) for infection and the added complication of the time-dependent of aGVHD, this was not statistically compared across the BSI groups.
Comparison of Factors Amongst BSI Groups
Patients with no BSI were older, had more early stage disease at the time of alloHCT, were more likely to receive a reduced-intensity conditioning (RIC) regimen with an HLA-identical sibling PBSC donor using tacrolimus and methotrexate for GVHD prophylaxis, and were less likely to receive TBI-based conditioning or post-transplant granulocyte colony stimulating factor (GCSF) (Table 1). Patients with BSI-VEP were more likely to receive a myeloablative conditioning (MAC) regimen with total body irradiation (TBI) (Table 1). White blood cell count (WBC), absolute neutrophil count (ANC) at the time of alloHCT, or history of clinically significant fungal infection prior to alloHCT were similar across the 4 groups.
Table 2 reports the time-dependent events of engraftment and GVHD among the four BSI-defined, patient cohorts. As cohorts were defined by BSI developing before neutrophil engraftment and/or by D100 and platelet engraftment and acute GVHD generally occurred prior to D100, it is not possible to formally compare by univariate analysis the cumulative incidence of acute GVHD and platelet engraftment across the cohorts. When assessing only patients who were alive at 100 days, the cumulative incidence of chronic GVHD was similar at 1 year for the four cohorts [BSI-VEP: 45% (42 – 48%) vs BSI-LEP: 43% (39 – 47%) vs BSI-both: 44% (38 – 50%) vs no BSI: 46% (45 – 48%); p = .2007].
Survival
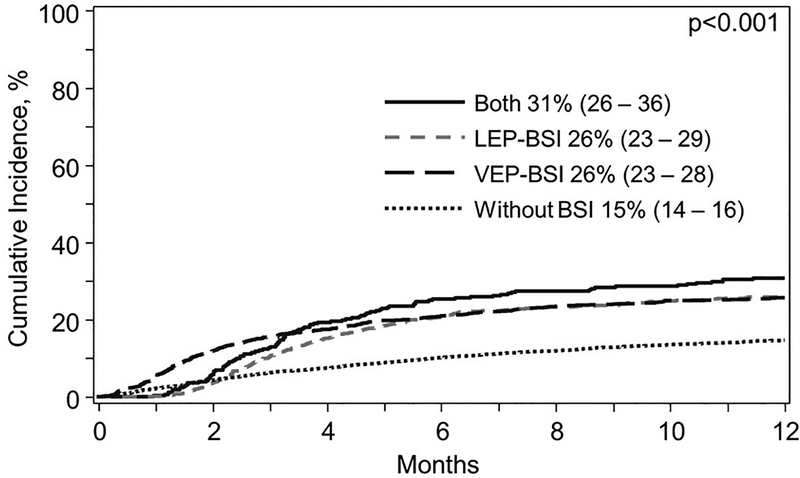
NRM was significantly higher in patients with any BSI compared with those with no BSI in multivariable analyses (Table 3, Figure 2). NRM was lower for BSI-VEP compared with BSI-LEP (HR, 0.74; 95% CI: 0.57–0.97, p=0.003) and BSI-Both (HR, 0.80; 95% CI: 0.67–1.0, p=0.03).
Table 3.
Multivariate analyses for non-relapse mortality, disease-free survival, and overall survival RR, relative risk; CI, confidence interval
| Non-Relapse Mortality | Disease-Free Survival | Overall Survival | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | N | RR (99% CI) | P-Value | Overall P-Value | RR (99% CI) | P-Value | Overall P-Value | RR (99% CI) | P-Value | Overall P-Value |
| BSI | ||||||||||
| No BSI | 4,472 | 1.00 | <0.0001 | 1.00 | <0.0001 | 1.00 | <0.0001 | |||
| VEP | 1,493 | 1.82 (1.63–2.04) | <0.0001 | 1.24 (1.15–1.34) | <0.0001 | 1.36 (1.26–1.47) | <0.0001 | |||
| LEP | 824 | 2.46 (2.05–2.96) | <0.0001 | 1.53 (1.35–1.74) | <0.0001 | 1.83 (1.58–2.12) | <0.0001 | |||
| BOTH | 339 | 2.29 (1.87–2.81) | <0.0001 | 1.49 (1.30–1.71) | <0.0001 | 1.66 (1.43–1.94) | <0.0001 | |||
| Age at HCT, years | ||||||||||
| ≤20 | 1,423 | 1.00 | <0.0001 | 1.00 | 1.00 | <0.0001 | ||||
| 21–40 | 1,439 | 1.75 (1.44–2.11) | <0.0001 | 1.28 (1.13–1.45) | 0.0001 | <0.0001 | 1.40 (1.23–1.60) | <0.0001 | ||
| 41–50 | 1,125 | 1.98 (1.57–2.51) | <0.0001 | 1.35 (1.20–1.52) | <0.0001 | 1.56 (1.36–178) | <0.0001 | |||
| 51–60 | 1,641 | 2.17 (1.74–2.71) | <0.0001 | 1.44 (1.25–1.66) | <0.0001 | 1.76 (1.54–2.02) | <0.0001 | |||
| >60 | 1,500 | 2.52 (2.00–3.10) | <0.0001 | 1.59 (1.36–1,86) | <0.0001 | 2.02 (1.76–2.33) | <0.0001 | |||
| KPS at HCT | ||||||||||
| ≥90 | 4,765 | 1.00 | 0.0010 | 1.00 | 0.0018 | 1.00 | 0.0001 | |||
| <90 | 2,230 | 1.18 (1.05–1.32) | 0.0039 | 1.18 (1.08–1.30) | 0.0005 | 1.20 (1.10–1.31) | <0.0001 | |||
| Missing | 133 | 1.38 (1.09–1.74) | 0.0067 | 1.14 (0.94–1.38) | 0.1978 | 1.20 (0.99–1.44) | 0.0574 | |||
| Disease-Disease stage variable | ||||||||||
| AML/ALL Early | 2,961 | 1.00 | <0.0001 | 1.00 | <0.0001 | 1.00 | <0.0001 | |||
| AML/ALL Intermediate | 1,542 | 1.06 (0.92–1.23) | 0.4336 | 1.17 (1.08–1.26) | 0.0001 | 1.17 (1.08–1.26) | 0.0002 | |||
| AML/ALL Advanced | 1,039 | 1.27 (1.06–1.53) | 0.0100 | 2.06 (1.89–2.25) | <0.0001 | 2.07 (1.88–2.27) | <0.0001 | |||
| MDS Early | 606 | 1.32 (1.10–1.58) | 0.0027 | 0.87 (0.78–0.96) | 0.0087 | 1.00 (0.87–1.14) | 0.9747 | |||
| MDS Advanced | 939 | 1.44 (1.24–1.68) | <0.0001 | 1.20 (1.10–1.32) | 0.0001 | 1.31 (1.19–1.44) | <0.0001 | |||
| Missing | 41 | 1.48 | 0.1703 | 1.28 (0.82–1.99) | 0.2831 | 1.25 (0.83–1.88) | 0.2955 | |||
| HCT-CI | ||||||||||
| 0 | 3,070 | 1.00 | 0.0012 | 1.00 | 0.0003 | 1.00 | <0.0001 | |||
| 1–2 | 1,872 | 1.09 (0.95–1.24) | 0.2121 | 1.06 (0.97–1.15) | 0.1914 | 1.07 (0.98–1.17) | 0.1097 | |||
| ≥3 | 2,044 | 1.27 (1.12–1.43) | 0.0001 | 1.14 (1.06–1.23) | 0.0004 | 1.21 (1.12–1.31) | <0.0001 | |||
| Missing | 142 | 1.05 (0.69–1.59) | 0.8137 | 0.78 (0.62–0.98) | 0.0302 | 0.78 (0.61–0.99) | 0.0453 | |||
| Donor/recipient HLA match | ||||||||||
| HLA-identical siblings | 1,990 | 1.00 | <0.0001 | 1.00 | <0.0001 | 1.00 | <0.0001 | |||
| 8/8 unrelated | 2,302 | 1.26 (1.09–1.45) | 0.0017 | 0.97 (0.90–1.06) | 0.5015 | 1.03 (0.95–1.13) | 0.4696 | |||
| ≤7/8 unrelated | 704 | 2.12 (1.78–2.53) | <0.0001 | 1.22 (1.09–1.36) | 0.0007 | 1.31 (1.16–1.48) | <0.0001 | |||
| Cord blood | 1,834 | 2.15 (1.83–2.53) | <0.0001 | 1.23 (1.09–1.38) | 0.0007 | 1.46 (1.29–1.64) | <0.0001 | |||
| Other | 298 | 1.60 (1.28–2.02) | <0.0001 | 1.15 (0.97–1.37) | 0.1040 | 1.26 (1.04–1.52) | 0.0161 | |||
| Conditioning regimen intensity | ||||||||||
| Myeloablative | 1.0000 | <0.0001 | ||||||||
| RIC/NMA | 1.24 (1.12–1.37) | |||||||||
| Donor/Recipient CMV status | ||||||||||
| −/− | 2,089 | 1.00 | 0.0035 | 1.00 | 0.0032 | |||||
| Any positive | 4,925 | 1.26 (1.10–1.43) | 0.0008 | 1.13 (1.05–1.22) | 0.0008 | |||||
| Missing | 114 | 1.11 (0.75–1.65) | 0.6035 | 1.07 (0.86–1.34) | 0.5438 | |||||
| Year of HCT | ||||||||||
| 2008–2009 | 1.00 | 0.0046 | ||||||||
| 2010–2012 | 0.91 (0.85–0.97) | 0.0046 | ||||||||
Figure 2.
NRM curve for VEP-BSI vs. LEP-BSI vs Both VEP- and LEP-BSI vs. No BSI), starting day 100 after transplant. Patients with no BSI had a lower NRM.
DFS was lower for BSI-VEP, BSI-LEP or BSI-both compared with no BSI; and BSI-LEP or BSI-Both had the lowest DFS among these groups. Relapse was similar among the 4 groups.
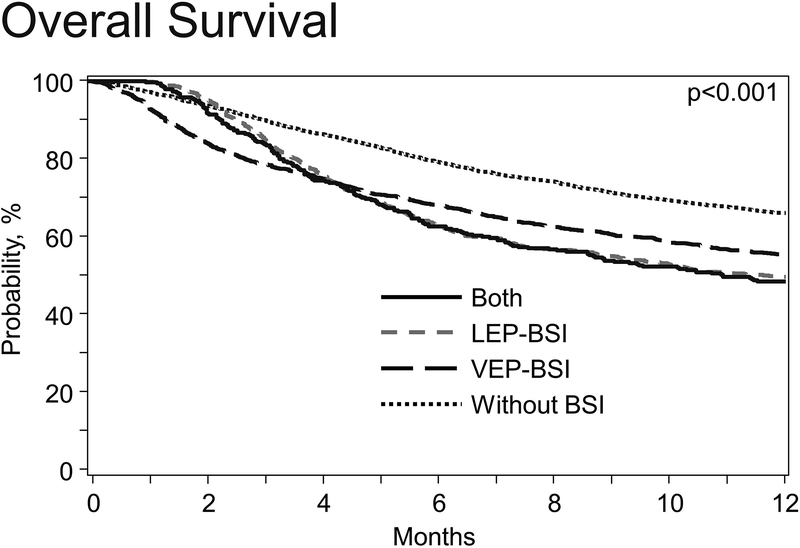
OS was significantly lower in patients with any BSI compared with patients without BSI (Table 3, Figure 3). However, OS was higher for BSI-VEP compared with BSI-LEP (HR, 0.74; 95%CI: 0.62–0.90, p<0.0001) and BSI-Both (HR, 0.82; 95%CI: 0.64–1.06, p=0.008). Besides infections, graft failure or organ failure were more important in BSI-VEP patients whereas GVHD was more common in BSI-LEP and BSI-Both as a cause of NRM. (Supplemental Table 2). Of note, in all subgroups, relapse was the most common cause of death.
Figure 3.
OS curve for VEP-BSI vs. LEP-BSI vs Both VEP- and LEP-BSI vs. No BSI), starting day 100 after transplant. Patients with LEP-BSI and Both-BSI especially had worse OS.
In multivariate analyses, additional factors associated with higher NRM and lower OS were older age, lower KPS, higher HCT-CI score (≥3), advanced acute leukemia, CMV seropositivity in either the donor or the recipient, use of alternative donor (HLA-mismatched URD, UCB or other donor) and earlier transplantation (Table 3). In addition, MDS was associated with a higher NRM.
Discussion:
We analyzed the CIBMTR registry data to assess the impact of early BSI (by D100) on long term (by D365) transplant outcomes. Our cohort consists of >7,000 patients from 181 Centers who received alloHCT between from 2008 through 2012. This is to our knowledge the largest analysis examining the impact of BSI after HCT in the contemporary era. Our main findings are that 1) Patients with BSI by D100 after alloHCT had increased NRM and lower OS compared with patients without BSI. 2) BSI-LEP was associated with increased NRM compared with no BSI or BSI-VEP.
Consistent with single center studies3,20, the majority of BSI occurred in the pre/peri engraftment phase (i.e., BSI-VEP). However, the risk for mortality was higher for patients with BSI-LEP and for patients with both BSI-VEP and BSI-LEP. Interestingly, both in univariate and multivariable analyses, the increased NRM was similar for those with BSI-LEP and the cohort with both BSI-VEP and BSI-LEP. We postulate that differences in mortality could be partially explained by different risk factors and causative organisms between VEP and LEP BSIs. Patients with BSI-VEP were more likely to have received MAC that are associated with more severe and protracted mucosal injury and longer time to neutrophil engraftment. As a result, BSI-VEP were predominantly caused by pathogens found in gastrointestinal (GI) flora BSI (e.g., Enterobacteriaceae spp., anaerobes). In contrast, patients with BSI-LEP were more likely to have received RIC regimens associated with later onset GVHD. BSI-LEP were predominantly caused by skin organisms (e.g., coagulase-negative Staphylococci, CoNS) suggesting possibly related to central venous catheter (CVC) use. While in general skin organisms are associated with low pathogenity (with exception of S. aureus) such organisms may be a surrogate marker of increased morbidity and more frequent utilization of health care centers. Alternatively, although difficult to prove, it is possible that monitoring and reacting to patients may vary once neutrophil engraftment occurs. As patients are generally no longer hospitalized following neutrophil engraftment, there may be less vigilance resulting in some delay in treatment leading to increased mortality. Additional possible factors that may contribute to this increased NRM for the BSI-LEP cohort including issues of drug-resistance, increased degrees of immunosuppression, and/or patient deconditioning at time of BSI are unanswerable within the CIBMTR dataset.
Gudiol et al found that early-onset BSI was mainly related to the presence of neutropenia, mucositis and CVC, whereas late-onset BSI mainly affected severely immunosuppressed alloHCT recipients with GVHD and corticosteroids.21 In our cohort, only 44% of BSI-VEP compared to 61% of BSI-LEP occurred following PBSC transplantation. PBSC transplantation is associated with more rapid neutrophil engraftment and increased GVHD compared to marrow allografts.22,23 In a recent prospective study comparing rates of infections between marrow and peripheral blood HCT from unrelated donors, 47.9% (95% CI, 41.5 to 53.9) of BM allograft recipients had infections compared with 32.8% (95% CI, 27.1 to 38.7) of PBSC allograft recipients (p=0.002). Faster neutrophil engraftment after PBSC transplantation may at least partially explain these findings.7
Acute GVHD is a recognized risk factor for late BSI after alloHCT.14,24,25 Low rates of post engraftment BSI and associated mortality have been reported after ex vivo T cell depletion, presumably due to lower incidence of GVHD.26 GVHD prevention and treatment contribute to the immune compromise in alloHCT patients. However, both the event of infection and the event of GVHD have variable onset relative to transplant and are intertwined in transplant outcomes. As this analysis sought to examine the impact of bacterial BSI occurring by day 100 on transplant outcomes, the event of aGVHD was examined both as an event prior to infection or at any time relative to infection in multivariable models (data not shown). Notably, there was no difference in significant variables allowing the reporting of a multivariable model focused on infection impact. Therefore, our results suggest that the increased NRM for patients with BSI-LEP or BSI-both are driven by the infection and not concomitant aGVHD alone.
Organisms of BSI differed between the two phases. Streptococcus spp., Enterobacteriaceae, and Enterococcus faecium comprised one third of total BSI-VEP. In contrast, Streptococcus spp. and Enterobacteriaceae were less frequent in BSI-LEP. CoNS comprised 25% and 33% of BSI-VEP and BSI-LEP respectively. The frequency of VRE was similar across the two phases. Similar epidemiology has been reported from single center studies26,6. Interestingly, we observed a trend toward decrease in all BSI over the years of this study, 2008 through 2012. A number of advances in supportive care or transplant practices (e.g., more RIC alloHCT) may have had an impact on the incidence of BSI and potentially BSI associated mortality. This is in the same line with improved outcomes and decreased NRM after alloHCT over time.27
Growth factor and supplemental intravenous immunoglobulin (IVIG) use are common for various reasons after alloHCT.28,29 In this study, we found that both GCSF and IVIG were used significantly higher in patients with any BSI compared to patients without BSI. Although counterintuitive, there was likely selection bias with use of these adjunctive preventative measures among sicker patients, i.e patients who are high risk to develop infections (such as UCB transplantation or ATG use) or already had infection29–31. Furthermore, the administration of post-transplant growth factor use and IVIG are only captured as given or not, without timing in regards to the infection.
Our study has several limitations. Data on antibiotic prophylaxis or treatment or susceptibility (multidrug-resistance) data were not captured in the registry. Lack of this data limits understanding of our ability to impact the outcomes of patients with BSI following HCT; however, because of the large number of centers and patients, it does not lessen the finding that patients with BSI-LEP have inferior outcomes. Ongoing revisions to CIBMTR data collection forms should improve our understanding of antibacterial prophylaxis strategies but detailed data regarding the treatment of common infections is beyond the scope of a transplant registry. Recent studies suggest an association of antibiotic use with GVHD and NRM.32 While a correlation of antibiotic exposures before or after BSI with mortality is beyond the scope of our study it would be interesting to capture in future studies. BSI are not classified using the most updated Centers for Disease Control and Prevention (CDC) definitions (i.e., LCBI: MBI-LCBI or CLABSI) due how the data are gathered. While we acknowledge these limitations inherent to a registry study, our study has several strengths including a robust sample size from 181 centers from diverse geographic locations and reflecting current transplant practices. The inclusion of multiple centers provides a diverse population of all ages, stem cell sources, and transplant types; however, it also results in a small percentage of missing data. Given that it is less than 5% for nearly all pertinent variables, this data is unlikely to change the overall outcomes in this large dataset. It is also likely to minimize over or underreporting biases inherent in single center studies. Uniform definitions were used for data collection stipulated by CIBMTR and long term follow up is ensured.
The comparison of BSI-VEP and BSI-LEP is confounded by the inability to predict prior to transplant into which group a patient will ultimately fall. By definition, a patient can only be in the BSI-LEP group if no BSI-VEP occurred. Similarly, the patient can only be in the “no BSI” group if never developing a BSI in the first 100 days. Furthermore, if a patient dies due to BSI-VEP, they do not live long-enough to become eligible for the “Both” category. However, if one compares only the patients still alive at day 100, valuable data is lost due to early deaths from infection, GVHD, or other causes. Therefore, our analysis and statistical methodology attempts to account for all these issues as meaningfully as possible. Furthermore, our analysis does not seek to imply that a BSI by day 100 is sole reason for inferior survival; instead, we merely demonstrate an association. However, we found no difference in the cumulative incidence of cGVHD for the 4 cohorts when analyzing patients still alive at day 100. Consequently, it may be other consequences of the BSI (i.e. organ dysfunction) or a pre-disposition to later infections (beyond the scope of this analysis) that result in the inferior outcomes for patients with a BSI prior to day 100.
In summary, we show that BSI occurring in each phase by D100 post alloHCT is associated with increased NRM. BSI-LEP was associated with a higher rate of mortality, indicating that neutrophil engraftment was likely critical to the survival of some patients with BSI-VEP, especially the ones who did not develop additional BSI-LEP (i.e., patients with BSI-Both). Therefore, patients after engraftment should continue to be diligently evaluated for BSIs. Further studies should focus on determining the reasons for BSI-LEP, its interaction with changes in gut microbiota and modification of prevention and treatment in these patients.
Supplementary Material
Acknowledgments
CIBMTR Support List
The CIBMTR is supported primarily by Public Health Service Grant/Cooperative Agreement 5U24CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 4U10HL069294 from NHLBI and NCI; a contract HHSH250201200016C with Health Resources and Services Administration (HRSA/DHHS); two Grants N00014-17-1-2388 and N0014-17-1-2850 from the Office of Naval Research; and grants from *Actinium Pharmaceuticals, Inc.; *Amgen, Inc.; *Amneal Biosciences; *Angiocrine Bioscience, Inc.; Anonymous donation to the Medical College of Wisconsin; Astellas Pharma US; Atara Biotherapeutics, Inc.; Be the Match Foundation; *bluebird bio, Inc.; *Bristol Myers Squibb Oncology; *Celgene Corporation; Cerus Corporation; *Chimerix, Inc.; Fred Hutchinson Cancer Research Center; Gamida Cell Ltd.; Gilead Sciences, Inc.; HistoGenetics, Inc.; Immucor; *Incyte Corporation; Janssen Scientific Affairs, LLC; *Jazz Pharmaceuticals, Inc.; Juno Therapeutics; Karyopharm Therapeutics, Inc.; Kite Pharma, Inc.; Medac, GmbH; MedImmune; The Medical College of Wisconsin; *Mediware; *Merck & Co, Inc.; *Mesoblast; MesoScale Diagnostics, Inc.; Millennium, the Takeda Oncology Co.; *Miltenyi Biotec, Inc.; National Marrow Donor Program; *Neovii Biotech NA, Inc.; Novartis Pharmaceuticals Corporation; Otsuka Pharmaceutical Co, Ltd. – Japan; PCORI; *Pfizer, Inc; *Pharmacyclics, LLC; PIRCHE AG; *Sanofi Genzyme; *Seattle Genetics; Shire; Spectrum Pharmaceuticals, Inc.; St. Baldrick’s Foundation; *Sunesis Pharmaceuticals, Inc.; Swedish Orphan Biovitrum, Inc.; Takeda Oncology; Telomere Diagnostics, Inc.; and University of Minnesota. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the U.S. Government.
*Corporate Members
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
References:
- 1.Meyer E, Beyersmann J, Bertz H, Wenzler-Rottele S, Babikir R, Schumacher M et al. Risk factor analysis of blood stream infection and pneumonia in neutropenic patients after peripheral blood stem-cell transplantation. Bone Marrow Transplant 2007; 39(3): 173–178. [DOI] [PubMed] [Google Scholar]
- 2.Hong J, Moon SM, Ahn HK, Sym SJ, Park YS, Park J et al. Comparison of characteristics of bacterial bloodstream infection between adult patients with allogeneic and autologous hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2013; 19(6): 994–999. [DOI] [PubMed] [Google Scholar]
- 3.Mikulska M, Del Bono V, Raiola AM, Bruno B, Gualandi F, Occhini D et al. Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transplant 2009; 15(1): 47–53. [DOI] [PubMed] [Google Scholar]
- 4.Oliveira AL, de Souza M, Carvalho-Dias VM, Ruiz MA, Silla L, Tanaka PY et al. Epidemiology of bacteremia and factors associated with multi-drug-resistant gram-negative bacteremia in hematopoietic stem cell transplant recipients. Bone Marrow Transplant 2007; 39(12): 775–781. [DOI] [PubMed] [Google Scholar]
- 5.Poutsiaka DD, Munson D, Price LL, Chan GW, Snydman DR. Blood stream infection (BSI) and acute GVHD after hematopoietic SCT (HSCT) are associated. Bone Marrow Transplant 2011; 46(2): 300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blennow O, Ljungman P, Sparrelid E, Mattsson J, Remberger M. Incidence, risk factors, and outcome of bloodstream infections during the pre-engraftment phase in 521 allogeneic hematopoietic stem cell transplantations. Transpl Infect Dis 2014; 16(1): 106–114. [DOI] [PubMed] [Google Scholar]
- 7.Young JA, Logan BR, Wu J, Wingard JR, Weisdorf DJ, Mudrick C et al. Infections after Transplantation of Bone Marrow or Peripheral Blood Stem Cells from Unrelated Donors. Biol Blood Marrow Transplant 2016; 22(2): 359–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.See I, Iwamoto M, Allen-Bridson K, Horan T, Magill SS, Thompson ND. Mucosal barrier injury laboratory-confirmed bloodstream infection: results from a field test of a new National Healthcare Safety Network definition. Infect Control Hosp Epidemiol 2013; 34(8): 769–776. [DOI] [PubMed] [Google Scholar]
- 9.Prevention CfDCa. Bloodstream infection event (central line-associated bloodstream infection and non-central line-associated bloodstream infection). http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf 2016.
- 10.Ballen K, Ahn KW, Chen M, Abdel-Azim H, Ahmed I, Aljurf M et al. Infection Rates among Acute Leukemia Patients Receiving Alternative Donor Hematopoietic Cell Transplantation. Biol Blood Marrow Tr 2016; 22(9): 1636–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poutsiaka DD, Price LL, Ucuzian A, Chan GW, Miller KB, Snydman DR. Blood stream infection after hematopoietic stem cell transplantation is associated with increased mortality. Bone Marrow Transplant 2007; 40(1): 63–70. [DOI] [PubMed] [Google Scholar]
- 12.Kim SH, Kee SY, Lee DG, Choi SM, Park SH, Kwon JC et al. Infectious complications following allogeneic stem cell transplantation: reduced-intensity vs. myeloablative conditioning regimens. Transplant Infectious Disease 2013; 15(1): 49–59. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell AE, Derrington P, Turner P, Hunt LP, Oakhill A, Marks DI. Gram-negative bacteraemia (GNB) after 428 unrelated donor bone marrow transplants (UD-BMT): risk factors, prophylaxis, therapy and outcome. Bone Marrow Transplant 2004; 33(3): 303–310. [DOI] [PubMed] [Google Scholar]
- 14.Dandoy CE, Haslam D, Lane A, Jodele S, Demmel K, El-Bietar J et al. Healthcare Burden, Risk Factors, and Outcomes of Mucosal Barrier Injury Laboratory-Confirmed Bloodstream Infections after Stem Cell Transplantation. Biol Blood Marrow Transplant 2016; 22(9): 1671–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Orasch C, Weisser M, Mertz D, Conen A, Heim D, Christen S et al. Comparison of infectious complications during induction/consolidation chemotherapy versus allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 2010; 45(3): 521–526. [DOI] [PubMed] [Google Scholar]
- 16.Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15(6): 825–828. [PubMed] [Google Scholar]
- 17.Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 2005; 11(12): 945–956. [DOI] [PubMed] [Google Scholar]
- 18.Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant 2015; 21(3): 389–401 e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Commenges D, Andersen PK. Score test of homogeneity for survival data. Lifetime Data Anal 1995; 1(2): 145–156; discussion 157–149. [DOI] [PubMed] [Google Scholar]
- 20.Kikuchi M, Akahoshi Y, Nakano H, Ugai T, Wada H, Yamasaki R et al. Risk factors for pre- and post-engraftment bloodstream infections after allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis 2015; 17(1): 56–65. [DOI] [PubMed] [Google Scholar]
- 21.Gudiol C, Garcia-Vidal C, Arnan M, Sanchez-Ortega I, Patino B, Duarte R et al. Etiology, clinical features and outcomes of pre-engraftment and post-engraftment bloodstream infection in hematopoietic SCT recipients. Bone Marrow Transplant 2014; 49(6): 824–830. [DOI] [PubMed] [Google Scholar]
- 22.Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med 2012; 367(16): 1487–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ustun C, Arslan O, Beksac M, Koc H, Gurman G, Ozcelik T et al. A retrospective comparison of allogeneic peripheral blood stem cell and bone marrow transplantation results from a single center: a focus on the incidence of graft-vs.-host disease and relapse. Biol Blood Marrow Transplant 1999; 5(1): 28–35. [DOI] [PubMed] [Google Scholar]
- 24.Mihu CN, Schaub J, Kesh S, Jakubowski A, Sepkowitz K, Pamer EG et al. Risk factors for late Staphylococcus aureus bacteremia after allogeneic hematopoietic stem cell transplantation: a single-institution, nested case-controlled study. Biol Blood Marrow Transplant 2008; 14(12): 1429–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang CH, Chang FY, Chao TY, Kao WY, Ho CL, Chen YC et al. Characteristics comparisons of bacteremia in allogeneic and autologous hematopoietic stem cell-transplant recipients with levofloxacin prophylaxis and influence on resistant bacteria emergence. J Microbiol Immunol Infect 2016. [DOI] [PubMed] [Google Scholar]
- 26.Almyroudis NG, Fuller A, Jakubowski A, Sepkowitz K, Jaffe D, Small TN et al. Pre- and post-engraftment bloodstream infection rates and associated mortality in allogeneic hematopoietic stem cell transplant recipients. Transpl Infect Dis 2005; 7(1): 11–17. [DOI] [PubMed] [Google Scholar]
- 27.Remberger M, Ackefors M, Berglund S, Blennow O, Dahllof G, Dlugosz A et al. Improved survival after allogeneic hematopoietic stem cell transplantation in recent years. A single-center study. Biol Blood Marrow Transplant 2011; 17(11): 1688–1697. [DOI] [PubMed] [Google Scholar]
- 28.Ueda M, Berger M, Gale RP, Lazarus HM. Immunoglobulin therapy in hematologic neoplasms and after hematopoietic cell transplantation. Blood Rev 2017. [DOI] [PubMed] [Google Scholar]
- 29.Ozcan M, Ustun C, Akcaglayan E, Akan H, Arslan O, Ilhan O et al. Recombinant human granulocyte colony-stimulating factor (rh-G-CSF) may accelerate hematopoietic recovery after HLA-identical sibling allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant 2001; 27(5): 499–505. [DOI] [PubMed] [Google Scholar]
- 30.Engelhard D, Akova M, Boeckh MJ, Freifeld A, Sepkowitz K, Viscoli C et al. Bacterial infection prevention after hematopoietic cell transplantation. Bone Marrow Transplant 2009; 44(8): 467–470. [DOI] [PubMed] [Google Scholar]
- 31.Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Preface. Bone Marrow Transplant 2009; 44(8): 453–455. [DOI] [PubMed] [Google Scholar]
- 32.Shono Y, Docampo MD, Peled JU, Perobelli SM, Velardi E, Tsai JJ et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci Transl Med 2016; 8(339): 339ra371. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.