Abstract
Objective
To study the anatomy of the oblique popliteal ligament, as regards its dimensions, expansion and anatomical relationships.
Methods
Eleven cadaver knees were dissected in order to study the anatomy and take measurements of anatomical structures and relationships of the oblique popliteal ligament. The dissection was for posterior access to the proper exposure of the oblique popliteal ligament, the semimembranosus muscle and its expansions. For measurement of dimensions, 40 × 12 needles were used for marking the specific points and a caliper. The angles were calculated using the software ImagePro Plus®.
Results
The distance from the origin of the oblique popliteal ligament to the tibial plateau was 7.4 mm, the thickness at its origin was 7.3 mm, length was 33.6 mm and the tibial plateau angle 34.8°. The length of the expansion of the proximal oblique popliteal ligament was 39.2 mm, thickness 7.8 mm and angle of the oblique popliteal ligament with its expansion 32.2°.
Conclusion
The oblique popliteal ligament is thick, rises in the semimembranosus and protrudes proximally forming an acute angle with the joint interline, crossing the popliteal fossa. In some cases it has a proximal expansion.
Keywords: Anatomy, Cadaver, Knee
Resumo
Objetivo
Estudar a anatomia do ligamento poplíteo oblíquo no que se refere às suas dimensões, expansões e relações anatômicas.
Métodos
Onze joelhos de cadáveres foram dissecados com o intuito de se estudar a anatomia e fazer medições das estruturas e das relações anatômicas do ligamento poplíteo oblíquo. A dissecção foi por acesso posterior até a exposição adequada do ligamento poplíteo oblíquo, do músculo semimembranoso e de suas expansões. Para aferição das medidas, foram usados agulhas 40 × 12 na marcação dos pontos específicos e um paquímetro. Os ângulos foram calculados com o auxílio do software ImagePro Plus®.
Resultados
A distância da origem do ligamento poplíteo oblíquo ao platô tibial foi de 7,4 mm, a espessura na sua origem foi de 7,3 mm, o comprimento foi de 33,6 mm e o ângulo com o platô tibial foi de 34,8°. O comprimento da expansão proximal do ligamento poplíteo oblíquo foi de 39,2 mm, a espessura foi de 7,8 mm e o ângulo do ligamento poplíteo oblíquo com sua expansão foi de 32,2°.
Conclusão
O ligamento poplíteo oblíquo é espesso, nasce no músculo semimembranoso, projeta-se proximalmente, forma um ângulo agudo com a interlinha articular e cruza a fossa poplítea. Em alguns casos apresenta uma expansão proximal.
Palavras-chave: Anatomia, Cadáver, Joelho
Introduction
The oblique popliteal ligament (OPL) is one of the five insertions of the semimembranosus muscle and forms part of the posterior anatomy of the knee.1, 2, 3 This ligament crosses the popliteal fossa from medial to lateral and is considered to be primary limiter of genu recurvatum and thus avoid hyperextension of the knee.4
The posterior anatomy of the knee consists of a network of structures and has uniquely complex biomechanics. Controlling knee hyperextension due to soft-tissue genu recurvatum is one of the functions of the posterior structures, especially the OPL. Hyperextension may alter gait and may lead to difficulty in walking across uneven ground.
Despite the great importance of the posterior structures of the knee, including the OPL, few studies in the literature have given emphasis to these structures, because no techniques for reconstructing them have been described.
The aim of this study was to examine the anatomy of the OPL with regard to its dimensions, expansions and anatomical relationships.
Materials and methods
This study was conducted in the Department of Anatomy of the Biological Sciences Sector of the Federal University of Paraná, in April and May 2011. Eleven knees from cadavers were dissected with the aims of studying their anatomy and making measurements on the structures and on the anatomical relationships of the OPL.
The inclusion criteria specified that only knees from cadavers with undamaged posterior structures, including the joint capsule, without previous arthrotomy, should be used. Eleven knees fulfilled the criteria. The dissection was performed by means of posterior access and was done such that sufficient exposure of the semimembranosus muscle, the OPL and their expansions was obtained. All the knees were conserved in 10% formol.
To make the measurements, 40 × 12 needles and metal calipers (Aero Space – 150 mm) were used to mark out specific points.5 Measurements were made of the distance from the origin of the OPL to the tibial plateau (O-P), the thickness of the OPL at its origin (Th-O), the length of the OPL (L), the thickness of the semimembranosus muscled at the point where the OPL arises (Th-S), the thickness of the OPL at the origin of its proximal expansion (Th-OPL-Exp), the thickness of the proximal expansion of the OPL (Th-Exp) and the length of the proximal expansion of the OPL (L-Exp).
The angles of the OPL with the tibial plateau (A-P) and of the OPL with its expansion (A-Exp) were calculated with the aid of the ImagePro Plus® software, version 4.5 for Windows (Media Cybernetics, Inc., USA) (Fig. 1).
Fig. 1.
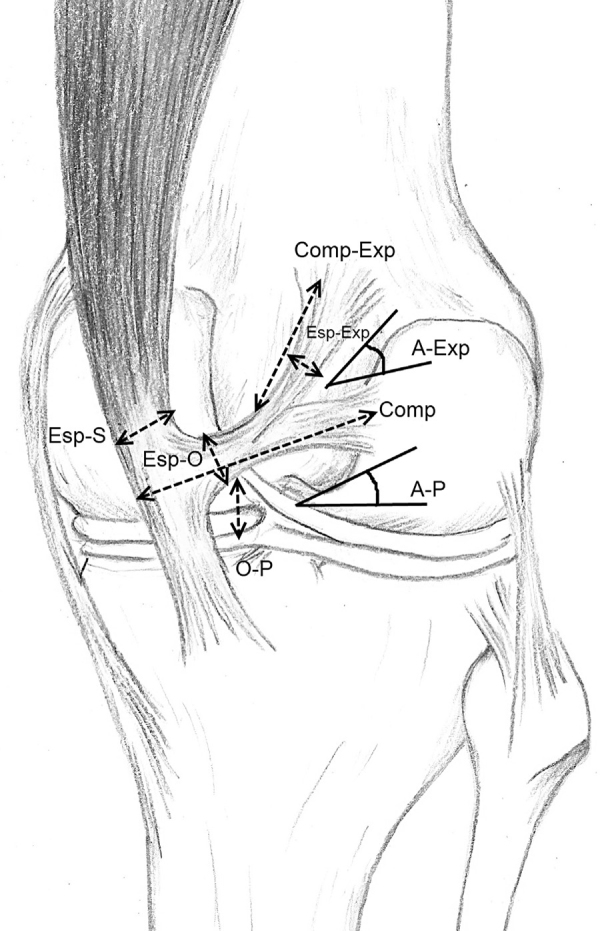
Anatomy of the oblique popliteal ligament. A-Exp, angle of the OPL with its expansion; A-P, angle of the OPL with the tibial plateau; L, length of the OPL; L-Exp, length of the proximal expansion of the OPL; Th-Exp, thickness of the proximal expansion of the OPL; Th-OPL-Exp, thickness of the OPL at the origin of its proximal expansion; Th-O, thickness of the OPL at its origin; Th-S, thickness of the semimembranosus at the point at which the OPL arises from it; O-P, distance from the origin of the OPL to the tibial plateau.
Results
The mean and standard deviation results from the measurements made are presented in Table 1.
Table 1.
Means and standard deviations for the anatomical structures of the oblique popliteal ligament.
| O-P | Th-O | L | A-P | Th-S | Th-OPL-Exp | Th-Exp | L-Exp | A-Exp | |
|---|---|---|---|---|---|---|---|---|---|
| Mean | 7.4 | 7.4 | 33.6 | 34.8 | 11.4 | 5.2 | 7.8 | 39.2 | 32.2 |
| Standard deviation | 2.0 | 2.0 | 4.8 | 8.0 | 2.0 | 2.5 | 3.3 | 7.2 | 6.6 |
O-P, distance from the origin of the OPL to the tibial plateau; Th-O, thickness of the OPL at its origin; L, length of the OPL; A-P, angle of the OPL with the tibial plateau; Th-S, thickness of the semimembranosus at the point at which the OPL arises from it; Th-OPL-Exp, thickness of the OPL at the origin of its proximal expansion; Th-Exp, thickness of the proximal expansion of the OPL; L-Exp, length of the proximal expansion of the OPL; A-Exp, angle of the OPL with its expansion; SD, standard deviation.
Proximal expansion of the OPL, with a mean length of 39 ± 7 mm (L-Exp), was observed in four of the eleven cases. It was found to be absent in the other seven anatomical specimens (Fig. 1).
Discussion
Unlike studies on the medial, lateral and central pivot structures of the knee, anatomical and biomechanical studies on the OPL are rare. This lack of interest probably comes from the fact that no technique for reconstructing this structure has been described.
The OPL is the main structure of the so-called posterior semimembranosus complex of the knee and the importance of this structure is emphasized both by its dimensions and by its biomechanical importance. In a descriptive laboratory study, dissections were performed on 20 fresh specimens and structures that would possibly limit hyperextension were sectioned. Independent of the order of the sectioning done, after sectioning the OPL there was an increased in hyperextension of 2.5 degrees. It was concluded that this structure was the main limiter of hyperextension and soft-tissue genu recurvatum.4
In the present study, it was observed that the OPL is a structure that originates together with the tendon of the semimembranosus muscle, and that its insertion in the posterior capsule of the knee is together with the lateral condyle, thereby forming an angle of 34.8° with the medial plateau, with a path from distally medial to proximally lateral.
In a descriptive anatomical study on the posterior structures of the knee by means of magnetic resonance analysis, a sixth branch of the semimembranosus muscle originating together with the OPL was described. This would have the function of protecting the posterior cornu of the meniscus against traction.6 This structure was not observed in the present study, which is concordant with the study by LaPrade et al.,7 who observed insertion in the meniscofemoral portion of the posterolateral capsule of the knee.
Among the eleven specimens dissected in the present study, it was observed that four of them presented bifurcation of the OPL, thus forming a double insertion, which is described in this study as distal expansion and proximal expansion. In another anatomical study, two lateral insertions of the OPL were described: one in the fabella (cartilaginous or bony), and the other in the meniscofemoral portion of the posterior capsule. However, the prevalences of these expansions were not reported, i.e. whether this is the general rule in all the specimens or whether this occurs in only some of them.7
One of the biggest problems in discussing a study on the OPL is that there is no standard regarding how measurements should be made on this structure, or in relation to the nomenclature of its expansions. Thus, there is a lack of uniformity among the data in the literature, and the capacity for comparison between studies is lost. The data on some measurements obtained in the present study can be compared with those of the study by LaPrade et al.7
At its medial origin, the OPL had a mean thickness of 7.4 mm. On the other hand, LaPrade et al.7 found slightly higher numbers (9.5 mm). Moreover, in evaluating the length of the ligament and the thickness of its lateral insertion, there was greater discordance. In the present study, it was observed that the length of the OPL was approximately 33.6 mm, while in the study by LaPrade this number reached 48 mm. One possible explanation for this is that LaPrade made this measurement on the proximal expansion whereas it was on the distal expansion in the present study. The thickness of the proximal expansion was also divergent. A mean value of 7.8 mm was found in the present study, while LaPrade et al.7 found a value of 4.5 mm.
The thickness of the semimembranosus in its portion from which the tendon of the OPL originates presented very similar values. In the present study, this was 11.4 mm and in the study by LaPrade et al.,7 12 mm. This similarity possibly occurred because this measurement is extremely simple to make and there is little margin for variation between examiners.
Conclusion
The OPL is a thick ligament that arises in the semimembranosus, at 7.4 mm from the tibial plateau, projects proximally, forms an angle of 34.4 degrees with the joint interline and crosses the popliteal fossa. In some cases, it presents proximal expansion.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Fam LPD, et al. Estudo anatômico do ligamento poplíteo oblíquo. Rev Bras Ortop. 2013;48:402–405.
Study conducted at the Biological Sciences Sector of Universidade Federal do Paraná, Curitiba, PR, Brazil.
References
- 1.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 2.Beltran J., Matityahu A., Hwang K., Jbara M., Maimon R., Padron M. The distal semimembranosus complex: normal MR anatomy, variants, biomechanics, and pathology. Skeletal Radiol. 2003;32:435–445. doi: 10.1007/s00256-003-0641-1. [DOI] [PubMed] [Google Scholar]
- 3.Robinson J.R., Sanchez-Ballester J., Bull a M.J., Thomas R., Amis A.A. The posteromedial corner revisited. J Bone Joint Surg. 2004;86:674–681. doi: 10.1302/0301-620x.86b5.14853. [DOI] [PubMed] [Google Scholar]
- 4.Morgan P.M., LaPrade R.F., Wentorf F.A., Cook J.W., Bianco A. The role of the oblique popliteal ligament and other structures in preventing knee hyperextension. Am J Sports Med. 2010;38:550–557. doi: 10.1177/0363546509348742. [DOI] [PubMed] [Google Scholar]
- 5.Stieven-Filho E., Garschangen E.T., Namba M., da Silva J.L.V., Malafaia O., Cunha L.A.M.da. Estudo anatômico das duas bandas do ligamento cruzado anterior com o joelho em 90 graus de flexão. Rev Col Bras Cir. 2011;38:338–342. [PubMed] [Google Scholar]
- 6.Kim Y.C., Yoo W.K., Chung I.H., Seo J.S., Tanaka S. Tendinous insertion of semimembranosus muscle into the lateral meniscus. Surg Radiol Anat. 1997;19:365–369. doi: 10.1007/BF01628503. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., Morgan P.M., Wentorf F.A., Johansen S., Engebretsen L. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Joint Surg Am. 2007;89:758–764. doi: 10.2106/JBJS.F.00120. [DOI] [PubMed] [Google Scholar]


