Abstract
Objective
To provide anatomical and morphometric basis of the posterior cruciate ligament's tibial insertions in order to assist the creation of anatomical tibial tunnels, in the ligament surgical reconstruction.
Material and methods
The topographic anatomy and morphometry of the posterior cruciate ligament's anterolateral and posteromedial bundles’ tibial insertions were analyzed in 24 anatomical knee pieces. The pieces were photographed by a digital camera and the images obtained were studied by the software ImageJ, where the bundles’ insertion areas were measured in square millimeters, and the length of structures and the distances between significant points were measured in millimeters.
Results
In 54.2% of the knees the insertion’ shape was concave; in most pieces (41.6%) the form of insertion was oval. The average posterior cruciate ligament's tibial insertion total area was 88.33 ± 21.66 mm2; the average anterolateral bundle's tibial insertion area was 46.79 ± 14.10 mm2 and it was 41.54 ± 9.75 mm2 for the posteromedial bundle.
Conclusions
The anterolateral bundle has a tibial insertion area larger than the posteromedial bundle; the insertion areas of those bundles in our study, were smaller than the ones found in the literature. The variations in the posterior cruciate ligament's tibial insertion area suggest that there should be an indication for anatomical reconstructions of this ligament using single or double tibial tunnels according to individual characteristics.
Keywords: Tibia, Posterior cruciate ligament, Orthopedic procedures
1. Introduction
The posterior cruciate ligament (PCL) originates from the lateral face of the medial femoral condyle (MFC) and crosses the knee joint in the posterior, lateral and distal directions. The PCL is inserted in the posterior and proximal tibia in the intercondylar area and extends into the adjacent posterior tibial surface for several millimiters.1, 2
The PCL is split into two functional bundles; the anterolateral bundle (ALB) and the posteromedial bundle (PMB). The ALB is tight at flexion, while the PMB is tight at extension.2
In addition, the PCL is the primary stabilizer of the knees because it provides the central rotational axis3 and responds to 95% of the posterior displacement of the tibia over the femor.4 It also limits the varus and valgus as well as the external rotation of this joint.5
PCL lesions alter the articular kinematics, which results in medial or generalized femorotibial osteoarthosis approximately 25 years after the lesion.6
In order to obtain articular stability and prevent secondary arthrosis, surgical treatment of these lesions for active patients is frequently indicated. Surgical reconstruction, however, requires thorough knowledge of anatomy to correctly place the graft.7
Our study was aimed at providing anatomical and morphometric details of tibial insertions of the PCL to help surgeons find the perforation points of the anatomical tibial tunnels during surgical reconstruction.
2. Materials and Methods
We studied the topographic anatomy and morphometry of tibial insertions of the PCL in 24 anatomical knee pieces, 12 on the right and 12 on the left. They were separate, and all of the articular cartilage and anterior and posterior cruciate ligaments were intact.
Preparation of the pieces before dissection was as follows: fixation with 10% formaldehyde, conservation in a mixture of 2.5% phenol, 2.5% formaldehyde, and 1%sodium chloride, and storage of the pieces in liquid glycerin for 60 days.
Initially, the synovial covering of the PCL, the fibrous expansions and the meniscofemoral ligaments were carefully removed (Fig. 1). Each bundle was then delicately removed with a scalpel, with a #11 blade, and dissection tweezers, and its limits were marked with small points of ink. In this manner, the bone insertions of the AL and PM bundles in the proximal tibia could be delimited.
Fig. 1.
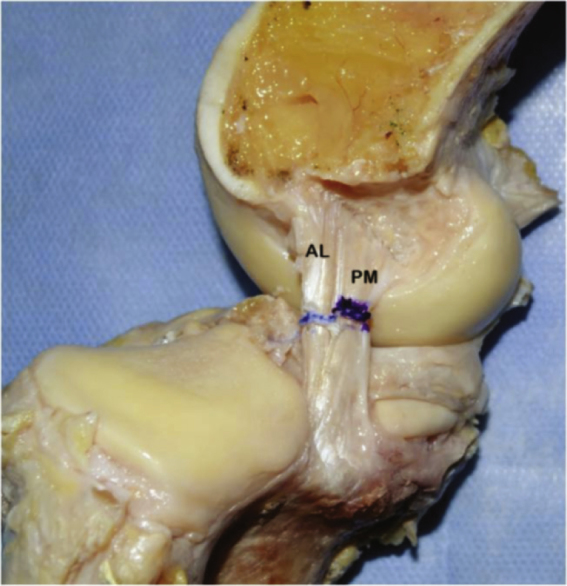
View of the anterolateral (a) and posteromedial (b) bundles of the cruciate ligament and its insertion after removing the meniscofemoral ligaments.
After the details of the tibial insertions of the AL and PM bundles of the PCL were macroscopically observed, a Canon EOS Rebel T1i digital camera and reference marker were used to photograph all of the pieces. (Fig. 2)
Fig. 2.
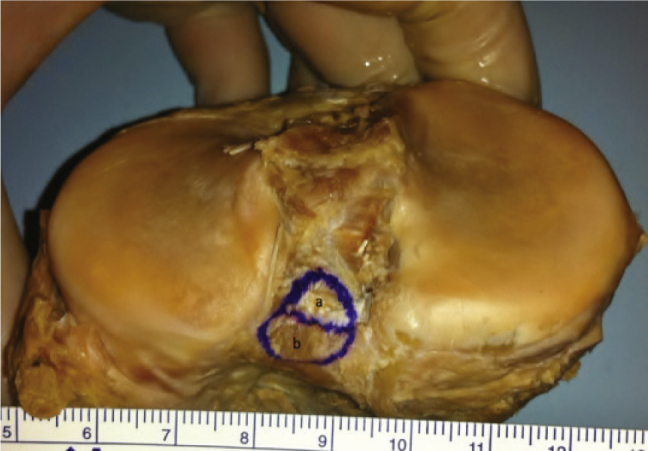
Macroscopic aspect of the tibial insertion areas of the anterolateral (a) and posteromedial (b) bundles of the posterior cruciate ligament in the posterior tibial intercondylar area of a right knee and the reference marker.
The ImageJ program was used to measure the insertion area of the bundles in square millimeters, and the distances between the significant points were measured in millimeters.
3. Results
The insertion of the PM bundle was distal and medial to the insertion of the AL bundle. In the macroscopic analysis, we noted topographic and geometric variations in the tibial insertions of the PCL.
In 13 knees (54.2%), the shape of the insertions was concave; eight pieces (33.3%) were planar, and three pieces (12.5%) presented a convex insertion area.
Regarding the geometric shape of the insertions of the PCL, we noted an oval shape in 10 knees, a square shape in eight knees (33.3%), and a trapezoidal (25%) shape in six dissected pieces.
Table 1 shows the measurement of the insertion areas of the AL and PM bundles, the length and width of these bundles, the distances between their insertion centers and the shortest distance between the articular cartilage edge and the insertion centers of the AL and PM bundles. The corresponding standard deviations and the variations between the lowest and highest values are also provided.
Table 1.
Quantitative measures of the tibial insertion of the posterior cruciate ligament.
| Mean and Standard Deviation | Variation | |
|---|---|---|
| Area (mm2) | ||
| Posterior Cruciate Ligament | 88.33 ± 21.66 | (52.00 - 136.00) |
| Anterolateral Bundle | 46.79 ± 14.10 | (25.32 - 83.68) |
| Posteromedial Bundle | 41.54 ± 9.75 | (22.65 - 59.00) |
| Length (mm) | ||
| Anterolateral Bundle | 5.66 ± 1.18 | (4.22 - 9.15) |
| Posteromedial Bundle | 5.47 ± 1.23 | (4.03 - 9.62) |
| Width (mm) | ||
| Anterolateral Bundle | 7.20 ± 1.18 | (5.25 - 10.34) |
| Posteromedial Bundle | 8.08 ± 1.34 | (5.74 - 11.02) |
| Distance between the Insertion Centers of the Anterolateral Bundle and the Posteromedial Bundle (mm) | 6.67 ± 1.00 | (4.23 - 7.98) |
| Shortest Distance (mm) between the Articular Cartilage Edge of the Medial Plateau and the | ||
| Anterolateral Bundle Center | 9.79 ± 2.08 | (5.78 - 15.49) |
| Posteromedial Bundle | 11.04 ± 2.25 | (8.22 - 17.32) |
| Shortest Distance (in mm) between the Articular Cartilage Edge of the Medial Plateau and the | ||
| Anterolateral Bundle | 7.30 ± 1.73 | (4.76 - 10.71) |
| Posteromedial Bundle | 8.59 ± 1.63 | (5.28 - 11.27) |
4. Discussion
The inappropriate placement of tunnels when reconstructing the PCL may result in graft shortening or stretching with flexion and subsequent failure.8
This study was aimed at describing the shape, location and measurement of the tibial insertions of the PCL to assist the surgeon in creating anatomic femoral tunnels during the surgical reconstruction of this ligament.
Regarding the descriptive anatomy, we verified that the PCL is inserted in the posterior intercondylar fossa, the AL bundle is inserted in its superolateral aspect, and the PM bundle is inserted in the inferomedial part of this fossa. Moorman et al.9 described the site of the tibial insertion as a ‘PCL facet’.
In our study, the geometric shape of the tibial insertions of the PCL was varied, although it was oval in most cases (41.6%). Sheps et al.10 described it as a trapezoidal shape; according to Harner et al.7 and Dargel et al.,11 the tibial insertion is rectangular.
Edwards et al.12 studied 39 cadaver knees. The images from digital photographs of the tibial insertions of the PCL were analyzed with software. We obtained the following measurements for the mean length and width of the AL bundle insertion: 8 ± 2 mm and 9 ± 2 mm, respectively; the mean length and width of the PM bundle insertion were 6 ± 1 mm and 10 ± 2 mm, respectively.
According to Tajima et al.,13 the mean length and width of the AL bundle insertion were 7.8 ± 1.5 mm and 9.2 ± 1.6 mm, respectively, and the mean length and width of the PM bundle insertion were 9.4 ± 1.4 mm and 15.0 ± 2.7 mm, respectively.
Of the measurements in our study, only the length of the AL bundle insertion was greater than the values reported by Edwards et al.;12; the other values were lower than the those reported by both Edwards et al. and Tajima et al.13
Also, in our study, we noted that the mean area of the AL bundle insertion, 46.79 ± 14.10 mm2, was greater than the mean area of the PM bundle insertion, 41.54 ± 9.75 mm2.
Harner et al.7 also reported that the mean area of AL bundle insertion was greater than that of the PM bundle (AL = 70 ± 26 mm2 and PM = 62 ± 17 mm2).
On the other hand, according to Tajima et al.13 and Takahashi et al.,14 the mean area of the PM bundle insertion was greater than the mean area of the AL bundle insertion.
We also determined the shortest distance, in millimeters, between the edges of the articular cartilages of the lateral and medial tibial condyles and the AL and PM bundle centers, which were 7.30 ± 1.73 mm and 8.59 ± 1.63 mm, respectively.
In our study, the center of the PCL bundle insertions was more proximal than traditionally recommended for surgical reconstruction of this ligament. According to Christel,15 the guide pin used to create the tibial tunnel should be centered in the PCL tibial insertion, 15 mm below the articular line, i.e., in a more distal position than the one we found in our anatomic study.
In this type of reconstruction, the graft may present an acute bend, known as a killer turn, around the proximal tibia, which may lax it. This would explain failures in restoring posterior laxity during the procedure.16 The creation of more proximal tunnels, according to the anatomic insertions of the PCL bundles verified in our study, may prevent these failures.
In our study, the total area of the PCL, 88.33 mm2, was smaller than that reported by other authors. Approximately 85% was the area of the knees was evaluated by Dargel et al.11, and the area of the knees evaluated by Tajima et al. was only 36%.13
Tajima et al.13 evaluated 21 unpaired cadaver knees. The tibial insertions were studied by three-dimensional laser photography and analyzed by specific software. The means of the insertion areas of the AL and PM bundles were 93.1 ± 16.6 mm2 and 150.8 ± 31.0 mm2, respectively. Takahashi et al., 14 evaluated 33 tibias using photographs with measurement scales and analyzed them using a computer. The means of the insertion areas of the AL and PM bundles obtained in this study were 46.7 ± 15.6 mm2 and 115.8 ± 54.6 mm2, respectively.
Dargel et al.11 examined 30 pairs of formalin-fixed knees whose tibial insertions of the PCL were marked with an emulsion of radiopaque barium sulfate, radiographed and evaluated using image processing software. The authors reported that the mean of the tibial insertion area of the PCL was 110.4 ± 36.7 mm2 for left knees and 103.9 ± 28.46 mm2 for right knees.
Tajima et al.13 addressed the difference between their findings and those present in the literature and state that the difference resulted from the inclusion of the peripheral fibers of the PCL, especially those of the PM bundle, which are more extensively inserted in the periosteum of the distal tibia.
Contrary to the aforementioned research, our study utilized careful dissection to limit the analysis to the ligament body itself at the site of the PCL tibial insertion.
In the present study and also in other publications, we have noted a high standard deviation for the mean of the PCL insertion areas in the tibia, with variations between 17% and 44% of the mean area. This is possibly a result of substantial differences between the individual measurements of the evaluated samples.
Because the mean of the total insertion area of the PCL in our study was 88.33 mm2, this area was 66.67 mm2 when subtracting the standard deviation and 109.99 mm2 after the addition of the standard deviation. Using these values, we calculated the diameter necessary for the tibial bone tunnel, which is to be filled in with a graft, to cover the total insertion area of the PCL.
Because the diameter is equal to two times the square root of the area divided by pi, a tibial tunnel of 10.60 mm in diameter would be necessary to occupy the mean area of PCL tibial insertion. For the smallest area, a tunnel 9.21 mm in diameter would be necessary, and for the largest area, a tunnel 11.83 mm in diameter would be required, which is greater than the size of the single tunnels normally used. Contrary to our study, Sheps et al.,10 considers the PCL tibial insertion area sufficiently large to allow the placement of two independent tunnels. The variations found in our study suggest that the creation of single or double tibial tunnels in the anatomic tunnels is indicated based on the individual.
Our study has some limitations. Due to the great anatomic variation found, our sample size of 24 knees may be small. In addition, the photographs of the PCL tibial insertions taken with a digital camera do not provide a three-dimensional view of the ligament insertion.
5. Conclusions
We confirm that the PCL has two bundles of tibial insertion, the AL and the PM bundles, and the AL bundle has an insertion area greater than that of the PM bundle. In our study, the insertion areas of these bands were smaller than those reported in the literature.
The insertion center of the PCL bundles was more proximal than what is commonly recommended for surgical reconstruction of this ligament. The creation of more proximal tunnels, with respect to the anatomic insertions of the PCL bundles, may avoid the phenomenon known as killer turn and loosening of the graft used for reconstruction of the transtibial tunnels.
The size variations in the insertion area of the PCL of the studied knees suggest that there the use single or double tibial tunnels for anatomical reconstruction of this ligament may be indicated according to individual characteristics.
Conflict of Interest
The authors have no conflicts of interest to declare in association with this paper.
Footnotes
Research conducted at the Faculdade de Ciências Médicas e da Saúde de Sorocaba, PUC-SP, Sorocaba, SP, Brazil.
References
- 1.Holt B.T., Parks N.L., Engh G.A., Lawrence J.M. Comparison of Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):257–263. doi: 10.1007/s00167-005-0686-x. [DOI] [PubMed] [Google Scholar]
- 2.Girgis F.G., Marshall J.L., Al Monajem A.R.S. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;(106):216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Hughston J.C., Bowden J.A., Andrews J.R., Norwood L.A. Acute tears of the posterior cruciate ligament. Results of operative treatment. J Bone Joint Surg Am. 1980;62(3):438–450. [PubMed] [Google Scholar]
- 4.Butler D.L., Noyes F.R., Grood E.S. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62(2):259–270. [PubMed] [Google Scholar]
- 5.Grood E.S., Stowers S.F., Noyes F.R. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70(1):88–97. [PubMed] [Google Scholar]
- 6.Dejour H., Walch G., Peyrot J., Eberhard P. The natural history of rupture of the posterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot. 1988;74(1):35–43. [PubMed] [Google Scholar]
- 7.Harner C.D., Xerogeanes J.W., Livesay G.A., Carlin G.J., Smith B.A., Kusayama T. The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation. Am J Sports Med. 1995;23(6):736–745. doi: 10.1177/036354659502300617. [DOI] [PubMed] [Google Scholar]
- 8.Saddler S.C., Noyes F.R., Grood E.S., Knochenmuss D.R., Hefzy M.S. Posterior cruciate ligament anatomy and length- tension behavior of PCL surface fibers. Am J Knee Surg. 1996;9(4):194–199. [PubMed] [Google Scholar]
- 9.Moorman C.T., 3rd, Zane S.M., Bansai S., Cina S.J., Wickiewicz T.L., Warren R.F. Tibial insertion of the posterior cruciate ligament: a sagittal plane analysis using gross, histologic, and radiographic methods. Arthroscopy. 2008;24(3):269–275. doi: 10.1016/j.arthro.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 10.Sheps D.M., Otto D., Fernhout M. The Anatomic characteristics of the tibial insertion of the posterior cruciate ligament. Arthroscopy. 2005;21(7):820–825. doi: 10.1016/j.arthro.2005.04.105. [DOI] [PubMed] [Google Scholar]
- 11.Dargel J., Pohl P., Tzikaras P., Koebke J. Morphometric side-to- side differences in human cruciate ligament insertions. Surg Radiol Anat. 2006;28(4):398–402. doi: 10.1007/s00276-006-0107-y. [DOI] [PubMed] [Google Scholar]
- 12.Edwards A., Bull A.M.J., Amis A.A. The Attachments of the fiber bundles of the posterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(3):284–290. doi: 10.1016/j.arthro.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Tajima G., Nozaki M., Iriuchishima T., Ingham S.J., Shen W., Smolinski P. Morphology of the tibial insertion of the posterior cruciate ligament. J Bone Joint Surg Am. 2009;91(4):859–866. doi: 10.2106/JBJS.H.00991. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi M., Matsubara T., Doi M., Suzuki D., Nagano A. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1055–1059. doi: 10.1007/s00167-006-0192-9. [DOI] [PubMed] [Google Scholar]
- 15.Christel P. Basic principles for surgical reconstruction of the PCL in chronic posterior knee instability. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):289–296. doi: 10.1007/s00167-003-0407-2. [DOI] [PubMed] [Google Scholar]
- 16.McAllister D.R., Markolf K.L., Oakes D.A., Young C.R., McWilliams J. A biomechanical comparison of tibial inlay and tibial tunnel posterior cruciate ligament reconstruction techniques: graft pretension and knee laxity. Am J Sports Med. 2002;30(3):312–317. doi: 10.1177/03635465020300030201. [DOI] [PubMed] [Google Scholar]


