Abstract
Objective
Describe the knee anterolateral ligament (ALL) and establish its anatomical marks of origin and insertion.
Methods
Dissection of the anterolateral aspect of the knee was performed in six cadavers. After isolation of the ALL, its lenght, width and thickness were measured as its places of origin and insertion. The ALL origin was documented in relation to the lateral collateral ligament (LCL) origin and the insertion was documented in relation to the Gerdy tubercle, fibullar head and lateral meniscus. After the first two dissections, the ligament was removed and sent to histologycal analysis.
Results
The ALL was clearly identified in all knees. Its origin in the lateral epycondile was on average 0.5 mm distal and 2.5 mm anterior to the LCL. In the tibia, two insertions were observed, one in the lateral meniscus and another in the proximal tibia, about 4.5 mm distal to the articular cartilage, between the Gerdy tubercle and the fibullar head. The average measures obtained were: 35.1 mm lenght, 6.8 mm width and 2.6 mm thickness. In the ligament histological analysis, dense connective tissue was observed.
Conclusion
The ALL is a constant structure in the knee anterolateral region. Its origin is anterior and distal to the LCL origin. In the tibia, it has two insertions, one in the lateral meniscus and another in the proximal tibia between the Gerdy tubercle and the fibullar head.
Keywords: Anterior cruciate ligament/anatomy & histology, Cadaver, Dissection, Knee
Resumo
Objetivo
Descrever o ligamento anterolateral (LAL) do joelho e estabelecer seus pontos anatômicos de origem e inserção e suas medidas.
Métodos
Foram feitas dissecções da região anterolateral do joelho em seis cadáveres. Após isolamento do LAL, medidas de comprimento, espessura e largura foram feitas, assim como seus locais de origem e inserção. A origem do LAL foi documentada com base na sua distância ântero-posterior e proximal- distal em relação à origem do ligamento colateral lateral. A inserção foi documentada com base no tubérculo de Gerdy, a cartilagem do planalto tibial lateral e o menisco lateral. Nas duas primeiras dissecções, o ligamento foi removido e enviado para análise histológica.
Resultados
O LAL foi observado com clareza nas dissecções de todos os seis joelhos. Sua origem no epicôndilo lateral apresentou uma média 0,5 mm distal e 2,5 mm anterior à origem do LCL. Na tíbia foram observadas duas inserções, uma mais proximal no menisco lateral e outra mais distal entre o tubérculo de Gerdy e a cabeça da fíbula, cerca de 4,5 mm distal à cartilagem articular da tíbia. As medidas encontradas do ligamento foram: comprimento médio de 35,1 mm, largura média de 6,8 mm e espessura média de 2,6 mm. Na análise histológica dos ligamentos foi observada presença de tecido conectivo denso.
Conclusão
O LAL do joelho é uma estrutura constante na região anterolateral. Sua origem no fêmur é anterior e distal à origem do LCL. Na tíbia, apresenta duas inserções, no menisco lateral e entre o tubérculo de Gerdy e a cabeça da fíbula.
Palavras-chave: Cadáver, Dissecação, Joelho, Ligamento cruzado anterior/anatomia & histologia
Introduction
Anterior cruciate ligament (ACL) injuries are among the pathological conditions most frequently seen in the Brazilian and worldwide orthopedics literature, with an incidence of approximately 200,000 reconstructions per year in the United States.1, 2 Many advances in treating these injuries have already been achieved, including extra-articular reconstruction, intra-articular reconstruction using an open approach, intra- articular reconstruction through isometric arthroscopy and, most recently, anatomical reconstruction techniques, with discussions between single-band and double-band procedures.3
The advances in surgical techniques have come from surgeons’ dissatisfaction with some clinical results obtained independently from adequate intra-articular reconstruction. It has been observed that not all patients behave in a similar manner. There are patients with residual knee instability even after technically adequate surgery, which justifies constantly undertaking intensive searches for improvement within this field of knee surgery.3
Despite significant improvement in residual anterolateral instability through the advent of anatomical single or double-band reconstructions, instead of transtibial isometric reconstructions, prospective series have demonstrated residual instability in around 7% of the cases, using the pivot-shift test. A positive result from this test is considered to be significantly correlated with worse postoperative functional results.4, 5, 6
Recently, some authors proposed that structures adjacent to the anterolateral joint capsule, and more specifically the anterolateral ligament (ALL) of the knee, may be involved in the genesis of rotational instability, given that its reconstruction is not envisaged in intra-articular reconstructions.7, 8 This stimulated us to evaluate the presence of this structure and details of its anatomy, and whether it histologically corresponds to a ligament. This first step is fundamental for future evaluations such as biomechanical tests and for surgical reconstructions.
Therefore, the objective of the present study was to describe the ALL of the knee and establish its anatomical points of origin and insertion, in relation to other anatomical structures in the region and their measurements.
Materials and methods
For the present anatomical study, six cadavers from the death verification service of the city of São Paulo (SVOC), which is attached to the University of São Paulo (USP), were used. There were four male cadavers and two female cadavers, of mean age 61.3 years (range: 49 to 72), mean weight 65.7 kg (range: 43 to 80) and mean height 1.70 m (range: 1.57 to 1.81).
None of the cadavers selected had any history of previous infections or surgery in the knee region or adjacent tissues that could in any way change the anatomy of the region. One cadaver was excluded from the study at the outset because it presented a previous fracture in the distal region of the femur, which had been fixed by means of a plate and screws through an anterolateral route in the knee.
Firstly, the skin and subcutaneous tissue were dissected, and this was followed by tenotomy of the quadriceps tendon at its muscle-tendon junction, medial parapatellar opening of the retinaculum and osteotomy of the anterior tuberosity of the tibia in order to access the anterolateral region of the knee without violating the adjacent extra-articular soft tissues. Part of the retropatellar fat of the region was resected to view the area better. The iliotibial tract was deinserted at the Gerdy tubercle, and tenotomy was performed on the biceps at the fibular head.
The tendon of the popliteal muscle and the lateral collateral ligament (LCL) were carefully isolated so as not to reach the origin of the ALL in the region of the lateral epicondyle (Fig. 1).
Fig. 1.
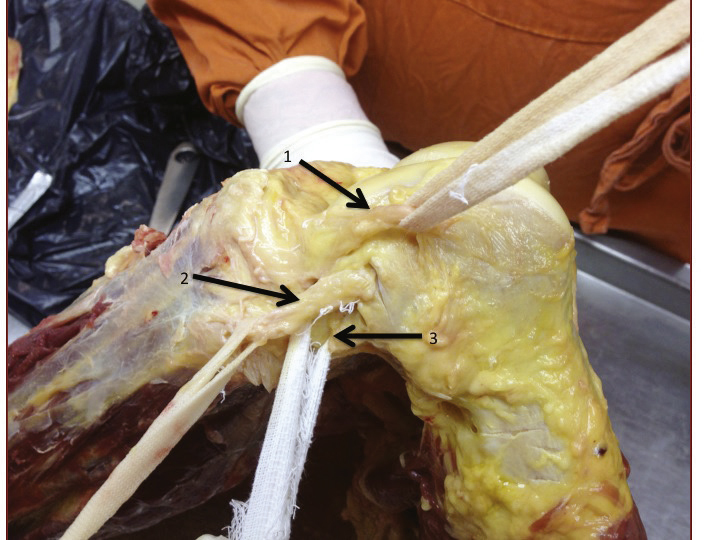
Lateral view of the left knee of a cadaver with isolation of the anterolateral ligament of the knee (arrow 1), lateral collateral ligament (arrow 2) and tendon of the popliteal muscle (arrow 3).
After isolating the posterolateral structures, a capsular thickening in the anterolateral region of the knee that was compatible with the ALL of the knee could clearly be seen.
All the dissections were performed in accordance with the same protocol.
After the ALL had been isolated and identified, length, thickness and width measurements were made using a digital pachymeter (150 mm [6”] DC-60 Western) with precision of approximately 0.03 mm. In addition, the sites of origin and insertion were documented. The origin of the ALL was documented based on the anteroposterior and proximal- distal distances from the origin of the LCL. The insertion was documented based on the most lateral portion of the Gerdy tubercle, the cartilage of the lateral tibial plateau and the lateral meniscus.
In the first two dissections, the ligament was removed en bloc together with its origins in the femur and tibia and was sent for analysis at the anatomical pathology laboratory of the Institute of Orthopedics and Traumatology, Hospital das Clínicas, USP School of Medicine (IOT-HC-FMUSP).
Results
The ALL was clearly seen in the dissections on all of the six knees studied (Fig. 2). Its origin in the lateral epicondyle presented variation in the cases studied. In two cases, the origin was proximal to the LCL (Fig. 3); in three cases, distal to the LCL (Fig. 4); and in one case, at the same level as the LCL. The mean was 0.5 mm distally, with a range from 2 mm proximally to 3 mm distally to the origin of the LCL. In all cases, the origin of the ALL was anterior to the origin of the LCL, with a mean of 2.5 mm anteriorly (range: 2 mm to 4 mm) (Table 1, Table 2).
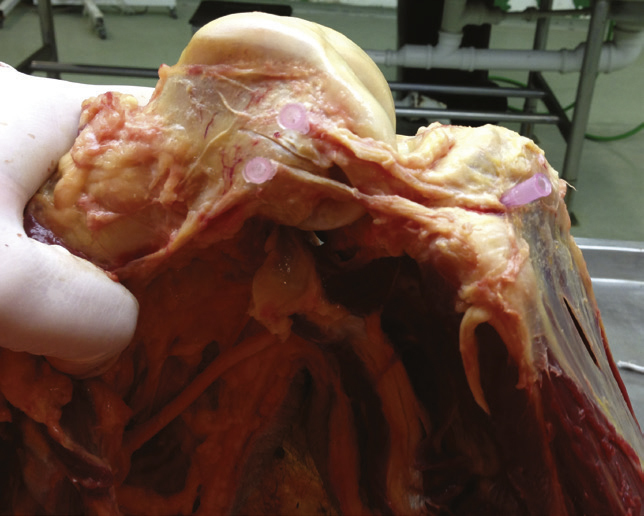
Fig. 2.

Lateral view of the knee showing anterolateral ligament anteriorly to the lateral collateral ligament.
Fig. 3.

Origin of the anterolateral ligament proximally to the origin of the lateral collateral ligament.
Fig. 4.
Origin of the anterolateral ligament distally to the origin of the lateral collateral ligament.
Table 1.
Anthropometric measurements on the cadavers and lengths, widths and thicknesses of the anterolateral ligaments in the knees studied.
| Knee | Sex | Age (years) | Side | Weight (kg) | Height (mm)) | Length (mm)) | Thickness (mm) | Width (mm) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 68 | D | 80 | 1.73 | 33 | 3 | 7 |
| 2 | M | 49 | D | 75 | 1.64 | 34 | 3 | 7 |
| 3 | M | 72 | E | 72 | 1.67 | 36 | 2 | 6 |
| 4 | F | 70 | E | 66 | 1.81 | 37 | 3 | 7 |
| 5 | F | 55 | E | 58 | 1.57 | 35 | 3 | 7 |
| 6 | M | 54 | D | 43 | 1.79 | 36 | 2 | 7 |
| Mean ± SD | 61.3 ± 9.79 | 65.7 ± 13.5 | 1.7 ± 0.09 | 35.1 ± 1.47 | 2.6 ± 0.51 | 6.8 ± 0.4 |
Table 2.
Measurements of the origin of the anterolateral ligament in relation to the lateral collateral ligament in the femur and measurements of its insertion in relation to the tibial joint cartilage.
| Knee | Origin anteriorly to LCL in the femur (mm) | Origin proximally-distally to the LCL in the femur (mm) | Insertion distally to the tibial cartilage tibial (mm) |
|---|---|---|---|
| 1 | 2 | 0 | 4 |
| 2 | 2 | 1 | 5 |
| 3 | 2 | 2 | 5 |
| 4 | 3 | -1 | 3 |
| 5 | 2 | -3 | 4 |
| 6 | 4 | -2 | 6 |
| Mean ± SD | 2.5 ± 0.83 | -0.5 ± 1.87 | 4.5 ± 1.04 |
In the tibia, the insertion of the ALL was constant. Two important insertions of the ligament were observed: one, more proximally in the lateral meniscus, in the peripheral portion of the transition between the anterior cornu and the body (Fig. 5); and the other, more distally, between the Gerdy tubercle and the fibular head (Fig. 6), around 4.5 mm distally to the tibial joint cartilage (ranging from 3 mm to 6 mm from this anatomical marker.
Fig. 5.

Insertion of the anterolateral ligament in the lateral.
Fig. 6.
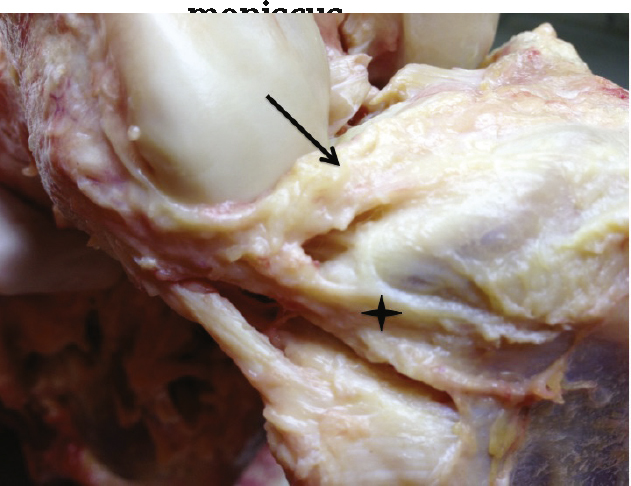
Insertion of the anterolateral ligament between the Gerdy tubercle and the fibular head (asterisk), distally to the insertion in the lateral meniscus (arrow).
The measurements found in the ligament were: mean length of 35.1 mm (range: 33 to 37); mean width of 6.8 mm (range: 6 to 7); and mean thickness of 2.6 mm (range: 2 to 3).
In the anatomopathological analysis on the two ligaments examined, dense connective tissue similar to ligament tissue was seen to be present.
Discussion
The motivation for the present study was to investigate the anatomy of the ALL and to enable deeper studies on anterolateral knee instability. We consider it important to invest in this line of research because the current ACL reconstruction techniques do not achieve complete eradication of the rotary instability after the surgery. Along this line, we intended to perform imaging examinations and correlate these with joint instability patterns and with biomechanical studies on cadavers.4, 9
The presence of an extra-articular structure responsible for the anterolateral rotational stability of the knee might explain why intra-articular reconstructions alone are not always sufficient to stabilize the rotational movements of the knee.8
The structure found, which was described recently by Vincent et al.8 in an anatomical study on cadavers and was analyzed biomechanically by Mônaco et al.7 using navigation, also on cadavers, may be important and possibly crucial for this correction. Placing value on the anterolateral structures for the genesis of ACL reconstruction is not a recent trend, but with the evolution of intra-articular reconstructions, it was being left aside.10, 11 Recently, it was demonstrated that performing lateral extra-articular tenodesis in association with intra-articular reconstruction of the ACL using a single band might be superior to intra-articular ACL reconstruction with a double band, from a rotational point of view, which emphasizes the importance of these extra-articular structures.12
In our study, the structure found was constant in all the knees studied, with length, width and thickness measurements that were similar between the cases and close to those in the recent literature.8
The only finding that was not constant was the origin of the ALL in the femur, in the region of the epicondyle. In all the cases, the origin was found anteriorly to the origin of the LCL, but there was no constancy with regard to its positioning proximally or distally to the LCL. In two cases, the origin of the ALL was shown to be proximal to the LCL and the ligament followed a more oblique course. In three cases, the ligament was found distally to the LCL, with a more vertical course. Vincent et al.8 found that all ten ligaments of their series had origins that were distal to the LCL. This difference may be explained by difficulty in separating the structures at the site, use of different dissection techniques or possibly the presence of superficial and deep layers with slight differences in their origins.
The insertion of the ALL in the meniscus was also constant in all the cases. There was difficulty in viewing any clear separation between the meniscal fibers and the insertion of the ligament. Thus, there may have been some participation by the ALL in the genesis of the lateral meniscal lesions and, likewise, the lateral meniscal lesions may have had a relationship with anterolateral rotational instability of the knee, through impairment of the insertion.
The second insertion of the ALL, in the proximal region of the tibia, may have been related to a Segond fracture, and this fracture may have represented a bone avulsion of the tibia in the region where the ALL was inserted, and not of the iliotibial band, the oblique anterior band of the LCL or the meniscotibial ligament, as was assessed previously.13, 14
In the histopathological analysis, the finding of dense connective tissue confirmed that a true ligament was present at this location, and not just a capsular thickening.
One criticism of the present study is the small number of cases, even though the sample size was similar to those of anatomical dissection studies on other knee ligaments in the recent literature.15 Nonetheless, this study is important since it is the first on this topic in the Brazilian literature and because of the scarcity of similar descriptions in the worldwide literature.
Better understanding of the anatomy and biomechanics of ligament structures may lead to proposals for new surgical techniques, as has been seen with the medial patellofemoral ligament.16
Studying the ALL opens up a new line of research that involves expansion of the number of dissections on cadavers, biomechanical tests, resonance analysis to assess its presence and correlation with ACL injuries, assessment of its clinical importance and possibly proposals for its repair or reconstruction, as was done with all the other ligaments already studied in the knee.15, 16, 17
Conclusion
The ALL of the knee is a constant structure in the anterolateral region of the knee. Its origin in the femur is anterior to the origin of the LCL and its position on the proximal-distal axis has small variations. In the tibia, it presents two important insertions: in the lateral meniscus and between the Gerdy tubercle and the fibular head.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed in the Medical Investigation Laboratory for the Musculoskeletal System (LIM41), Department of Orthopedics and Traumatology, FMUSP.
References
- 1.Siegel L., Vandenakker-Albanese C., Siegel D. Anterior cruciate ligament injuries: anatomy, physiology, biomechanics, and management. Clin J Sport Med. 2012;22(4):349–355. doi: 10.1097/JSM.0b013e3182580cd0. [DOI] [PubMed] [Google Scholar]
- 2.Frank RN, Verma NN. Graft selection in revision ACL reconstruction. In: Bach BR Jr., Provencher MT, editors. ACL surgery: how to get it right the first time and what to do if it fails. Philadelphia: Elsevier; 2010. p. 217-29.
- 3.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37(2):181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hussein M., van Eck C.F., Cretnik A., Dinevski D., Fu F.H. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40(3):512–520. doi: 10.1177/0363546511426416. [DOI] [PubMed] [Google Scholar]
- 5.Ayeni O.R., Chahal M., Tran M.N., Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767–777. doi: 10.1007/s00167-011-1860-y. [DOI] [PubMed] [Google Scholar]
- 6.Marx R.G. Anatomic double-bundle anterior cruciate ligament reconstruction was superior to conventional single-bundle reconstruction. J Bone Joint Surg Am. 2013;95(4):365. doi: 10.2106/JBJS.9504.ebo804. [DOI] [PubMed] [Google Scholar]
- 7.Monaco E., Ferretti A., Labianca L., Maestri B., Speranza A., Kelly M.J. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 8.Vincent J.P., Magnussen R.A., Gezmez F., Uguen A., Jacobi M., Weppe F. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 9.Hussein M., van Eck C.F., Cretnik A., Dinevski D., Fu F.H. Individualized anterior cruciate ligament surgery: a prospective study comparing anatomic single- and double- bundle reconstruction. Am J Sports Med. 2012;40(8):1781–1788. doi: 10.1177/0363546512446928. [DOI] [PubMed] [Google Scholar]
- 10.Johnston D.R., Baker A., Rose C., Scotland T.R., Maffulli N. Long-term outcome of MacIntosh reconstruction of chronic anterior cruciate ligament insufficiency using fascia lata. J Orthop Sci. 2003;8(6):789–795. doi: 10.1007/s00776-003-0708-9. [DOI] [PubMed] [Google Scholar]
- 11.Garcia R., Jr., Brunet M.E., Timon S., Barrack R.L. Lateral extra- articular knee reconstruction: long-term patient outcome and satisfaction. J South Orthop Assoc. 2000;9(1):19–23. [PubMed] [Google Scholar]
- 12.Monaco E., Labianca L., Conteduca F., De Carli A., Ferretti A. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction?. A CAOS study. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1168–1174. doi: 10.1007/s00167-007-0368-y. [DOI] [PubMed] [Google Scholar]
- 13.Hess T., Rupp S., Hopf T., Gleitz M., Liebler J. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res. 1994;(303):193–197. [PubMed] [Google Scholar]
- 14.Campos J.C., Chung C.B., Lektrakul N., Pedowitz R., Trudell D., Yu J., Resnick D. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381–386. doi: 10.1148/radiology.219.2.r01ma23381. [DOI] [PubMed] [Google Scholar]
- 15.Camanho G.L., Viegas A.C. Estudo anatômico e artroscópico do ligamento femoropatelar medial. Acta Ortop Bras. 2003;11(3):145–149. [Google Scholar]
- 16.Camanho G.L., Bitar A.C., Hernandez A.J., Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23(1):108e1–108e4. doi: 10.1016/j.arthro.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Camanho GL. Função dos ligamentos do joelho: estudo experimental em desarticulação. In: XXII Congresso Brasileiro de Ortopedia e Traumatologia; 1979.


