Abstract
Objective
To evaluate outcomes of 229 idiopathic clubfeet (ICF) treated using the Ponseti method, from 2001 to 2011, comparing two groups with different follow-ups.
Method
155 patients (229 ICF) were treated separated in two groups: Group I: 72 patients (109 ICF – 47.6%) with a follow up of 62 to 128 months (mean of 85). Group II: 83 patients (120 ICF – 52.4%) with a follow up of 4 to 57 months (mean of 33.5). We have considered satisfactory outcomes for cases which correction of all deformed components, without surgery.
Results
Mean age for the initial assessment was 5.4 months in Group I and 3.2 in Group II. Satisfactory outcomes were obtained in 85.4% in Group I and 97.5% in Group II. Mean cast placements were 9.5 in Group I and 7 in Group II. 67% were submitted to percutaneous Achilles tenotomy in Group I and 65% in Group II. Deformity relapses, when using abducted braces, occurred in 41 (37.6%) feet from Group I; 11 were treated surgically. In Group II, 17 feet relapsed (14.1%); three of them were submitted to surgery.
Conclusion
The method was successful in both groups, in low number of complications. The results were statistically superior in Group II when deformity correction, cast placements, relapses and surgery indication.
Keywords: Clubfoot, Congenital abnormalities, Foot deformities
Resumo
Objetivo
Avaliar os resultados do tratamento de 229 pés tortos congênitos idiopáticos (PTC) pelo método de Ponseti, de 2001 a 2011, com a comparação de dois grupos com diferentes tempos de seguimento.
Métodos
Foram tratados 155 pacientes (229 PTC) divididos em dois grupos: Grupo I: 72 pacientes (109 PTC – 47,6%) com seguimento de 62 a 128 meses (média de 85). Grupo II: 83 pacientes (120 PTC – 52,4%) com seguimento de quatro a 57 meses (média de 33,5). Consideramos resultados satisfatórios para casos que apresentaram correção de todos os componentes da deformidade sem necessidade de cirurgias.
Resultados
A idade média ao início do tratamento foi de 5,4 meses no grupo I e 3,2 no grupo II. Os resultados foram satisfatórios em 85,4% dos pés no grupo I e em 97,5% no grupo II. A média do número de gessos trocados foi de 9,5 no grupo I e de sete no grupo II. Fizemos a tenotomia percutânea do calcâneo em 67% dos pés do grupo I e 65% do grupo II. A recidiva das deformidades, quando do uso da órtese de abdução, ocorreu em 41 (37,6%) pés do grupo I; desses, 11 foram operados. No grupo II, recidivaram 17 (14,1%) pés; desses, três evoluíram para cirurgia.
Conclusão
O método foi eficaz em ambos os grupos, com baixo número de complicações. Os resultados foram estatisticamente superiores no grupo II quando analisados correção das deformidades, número de gessos, recidivas e indicação cirúrgica.
Palavras-chave: Anormalidades congênitas, Deformidades do pé, Pé torto
1. Introduction
Idiopathic congenital clubfoot (CCF) is the most important musculoskeletal malformation at birth1, 2 and may present as the following deformities: pes equinus, hindfoot varus, forefoot cavus or adduction of the mid and forefoot.3, 4, 5, 6, 7, 8 Its incidence is approximately one to two cases per 1,000 live births, and it is three times more common among males.2, 9, 10
Several factors such as genetic predisposition,11 gestational abnormalities9 and a variety of histological abnormalities12 seem to be related to its genesis. Nonetheless, its true cause remains unknown.13, 14, 15
The objective in treating this pathological condition is to achieve pain-free plantigrade feet with good mobility and without the need for special footwear.5, 16, 17 There are records of conservative treatment dating from 400 BC, performed by Hippocrates, by means of manipulation followed by immobilization.9 The treatment evolved over time, but the principle remained the same, with correction of the deformities based on the plasticity of the tissues involved.9 Several studies published from the middle of the 20th century onwards promoted surgical treatment,18, 19 and this trend predominated until the end of the 1990s.
For many years, in our service, the protocol for CCF treatment followed the plaster cast method proposed by Kite, with modifications. Feet that remained uncorrected or that presented relapse underwent surgery with broad postero- mediolateral release of soft tissues, by means of the Cincinnati segmented access route.20 However, despite the initially satisfactory results from surgery, we observed that over the course of time, many of these feet developed joint stiffness, hypertrophic scarring, relapse and hypo or hypercorrection of the deformity. This led us to question the real value of the method used.
In the 1990s, conservative treatment started to regain emphasis subsequent to the studies by Ponseti5, 6 presenting late results from CCF treatment using this author's method. This consisted of less aggressive and practically closed treatment with satisfactory results, thus significantly reducing the use of extensive surgery.5, 6, 21, 22, 23, 24
After personal contact with Professor Ponseti in 2001 and then learning his method, we started to use it at our service.
The aim of the present study was to analyze the results from treating CCF using the Ponseti method. We divided our patients into two groups, according to the different lengths of follow-up, and we sought to evaluate the influence of the age at the start of the treatment, the number of changes of plaster cast used to correct the deformity, the need (or not) for calcaneal tenotomy and occurrences of relapse and complications.
This study was initially submitted for analysis to the Medical Research Ethics Committee, and was approved under the number 374/11.
2. Methods
We retrospectively analyzed 155 patients (229 feet) with a diagnosis of idiopathic CCF, who were treated at the University Hospital of Taubaté and in the private clinic of one of the authors, between 2001 and 2011.
The patients were divided into two groups, according to the length of follow-up of the treatment. The first group (GI) was formed by cases with follow-up of more than 60 months. This accounted for 109 feet and its mean length of follow-up was 85 months (range: 62-128).
The second group (GII) comprised 120 feet, with a mean length of follow-up of 33.5 months (range: 4-57). Male gender was more prevalent in both groups (GI: 69%; GII: 83%) and unilateral impairment occurred in 52% of the patients, with the right side predominating.
We used the classification proposed by Dimeglio, in a simplified form.10 This is based on hindfoot and forefoot flexibility and is divided into four types of feet: type I is characterized by flexible hindfoot and forefoot; type II has a rigid hindfoot and flexible forefoot; in type III, only the forefoot is rigid; and in type IV, both are rigid. Thus, before treatment, our CCF cases presented as follows, in GI: Dimeglio type I – 9 feet, type II – 72, type III – 1 and type IV – 26; and in GII: type I – 15 feet, type II – 62, type III – 4 and type IV – 39. CCF type II predominated in both study groups (GI: 67%; GII: 52.6%).
Patients with neurological, syndromic and teratogenic clubfoot and those whose clubfoot was associated with other malformations were excluded from this study.
In accordance with the protocol for the method, which does not place value on radiographs of the feet,5, 6 these were not requested routinely, except in cases in which we suspected that other associated abnormalities were present.
3. Ponseti method
At the first consultation, detailed palpation of the foot was performed and the anatomical relationships between the bones were identified. This was followed by gentle manipulation and immobilization in a plaster cast. During the manipulation, it was sought to promote stretching of the soft tissues and thus facilitate correction of the deformity.
The entire limb was firstly padded by means of a double tubular mesh. The plaster cast was constructed in two stages; in the first, the most proximal portion of the limb was immobilized and the knee was kept flexed at 90 degrees; and in the second, after a maneuver to correct the deformities, the plaster cast was terminated distally (Fig. 1). All of the bones distal to the talus were rotated and lateralized below the talus, while this bone remained fixed in the wrappings of the ankle. The manipulation was started using the thumb, which functioned as a fulcrum positioned over the lateral portion of the head of the talus, while counterpressure was exerted on the first metatarsal and medial cuneiform bones.
Figure 1.

Plaster cast from groin to foot: Ponseti method.
This maneuver promoted supination of the forefoot and aligned the first metatarsal bone (which was in a verticalized and pronated position), and thus corrected the cavus deformity of the foot.5, 6, 21, 22 During this manipulation, it was sought to achieve simultaneous realignment of the calcaneal-cuboid, talonavicular and talocalcaneal joints, with special attention to the talonavicular joint. The plaster cast was changed every week, in a progressive sequence based on correction of the inversion and gain of abduction.
Pronation of the forefoot needed to be avoided and the calcaneus was not touched, thereby not making a mistake that frequently occurs with other techniques.
When no gain was obtained through the correction and the equin us deformity r emained r esistant, percutaneous tenotomy of the calcaneus was performed under general anesthesia in a surgical environment. Using a No. 3 cable scalpel and a No. 11 blade, a short transverse incision was made medially to laterally, anterior and parallel to the tendon. At this moment, the scalpel was rotated through 90 degrees and the cutting edge was positioned against the tendon, which was then sectioned using light pressure. Usually only one 5.0 mononylon stitch was needed to suture the incision.
After the tenotomy, we did not observe any resistance to correction of the equinus, and the foot easily achieved the desired dorsiflexion. The foot was then immobilized in a plaster cast brace from the groin to the foot, which was kept in place for three weeks.
After removal of the surgical plaster cast, with the foot corrected, an abduction brace with a transverse bar of Denis Browne type was introduced, with the boots positioned at 45 degrees of abduction to the normal foot and 70 degrees to the corrected CCF, with 10 degrees of dorsiflexion (Fig. 2).
Figure 2.
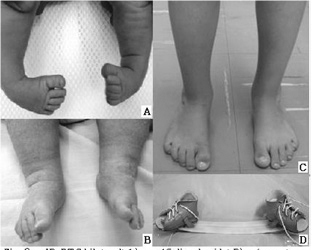
JB, bilateral CCF. A) at age of 15 days; B) after sixth plaster cast; C) at age of four years; D) Denis Browne splint.
The protocol for using the abduction brace consisted of 23 hours of use per day for the first four months, followed by 12 hours overnight for the next four years.
In the event of recurrence of the deformity during the stage of using the abduction brace, placement of a series of plaster casts started again, until complete correction of the deformity was achieved. There could even be the need for tenotomy of the calcaneus again.
To assess the results, the clinical and functional appearance of the feet was used. We considered the results to be satisfactory if the feet presented correction of all the components of the deformity (equinus, cavus, varus and adduction) and were seen to be plantigrade and flexible. On the other hand, the results were considered to be unsatisfactory if the CCF persisted with some degree of deformity or recurrence, even after new changes of plaster cast and use of splints, and if a surgical procedure was required to correct the residual deformities.
The adults responsible for the patients were advised regarding the need to adhere to the consultation schedule and particularly to using the abduction brace, for the treatment to be successful. In addition, for GII, we introduced an explanatory group class about the method, for the parents, which was given before the consultations.
The statistical analysis was performed by a professional qualified in this field. To compare the categorical variables between the groups, the chi-square test was used; and for continuous variables, the Mann-Whitney test. The significance level used was 5% (p-value ≤ 0.05).
4. Results
The children's mean age at the start of the treatment, for the entire sample, was 4.2 months. Comparing the two study groups, although the mean age was lower among the GII patients (3.2 months versus 5.4 months in GI), this difference did not present any statistical influence on the results (p = 0.13).
The mean length of follow-up in GI was 85 months (minimum of 62 and maximum of 128); while in GII, it was 33.5 months (minimum of 4 and maximum of 57).
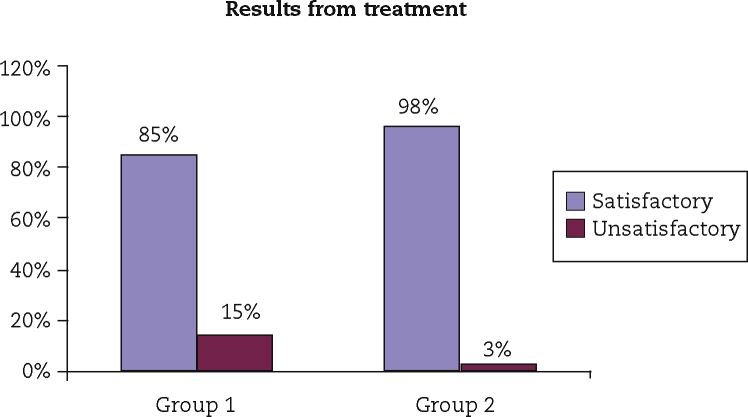
The results classified as satisfactory showed a statistically significant correlation with the length-of-follow-up groups: 97.5% in GII versus 85.3% in GI (p = 0.0008) (Fig. 3). In evaluating the 209 CCFs treated using this method, the results were seen to be significant in 91.2%.
Figure 3.
Results from treatment using Ponseti method.
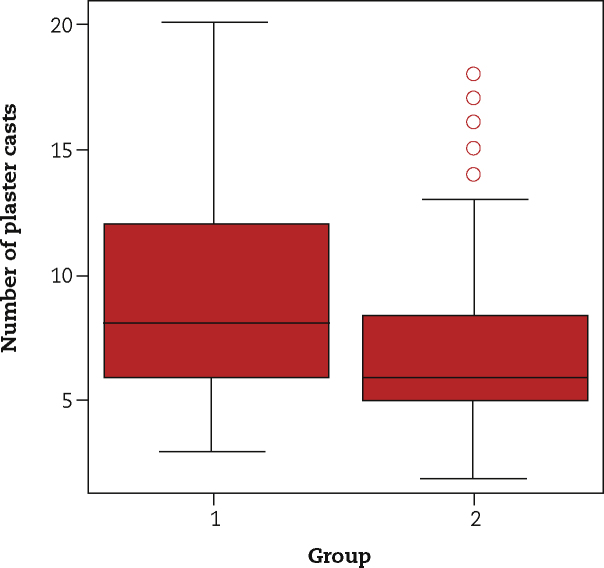
The mean number of plaster casts among the entire CCF sample was 8.1. In correlating this variable between the groups, a significant difference was observed, such that while 9.5 casts were used in GI, only 7 were used in GII (p < 0.0001) (Fig. 4).
Figure 4.
Number of plaster casts.
The feet that, over the course of the changes of plaster cast, continued to present residual equinus after correction of the other deformities underwent percutaneous tenotomy of the calcaneus. The two groups presented similar percentages regarding the need for tenotomy, such that 73 feet (67%) in GI were thus treated and 78 (65%) in GII, without any statistical difference (p = 0.75).
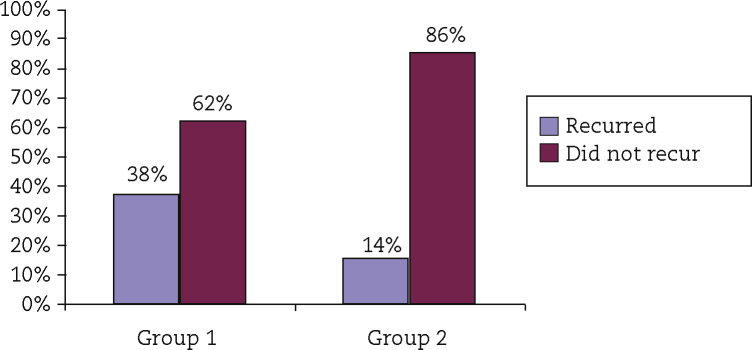
In GI, 41 feet (37.6%) showed recurrence and underwent additional plaster cast changes. However, in GII, this percentage was significantly lower: 17 feet (14.2%) presented a component of the deformity and were put into plaster casts again (p < 0.0001) (Fig. 5).
Figure 5.
Number of recurrences.
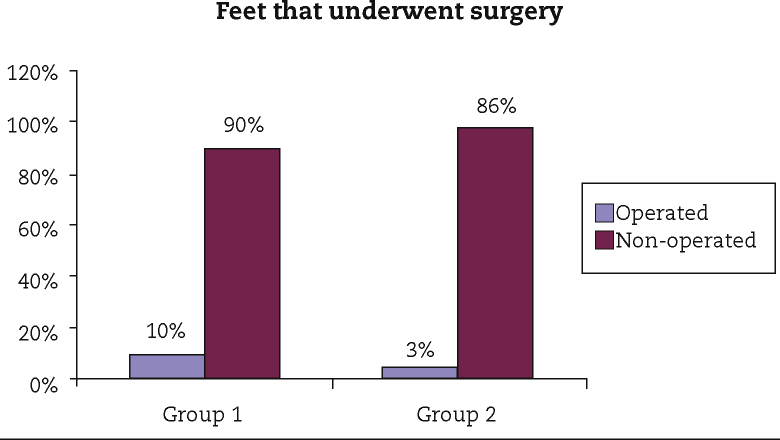
After new treatments for relapses, some feet still persisted with some degree of deformity. In correlating this variable with the groups studied, this number was also significantly smaller in GII, comprising three feet (2.5%), versus eleven feet (10.1%) in GI.These feet underwent surgical treatment (p = 0.01) (Fig. 6).
Figure 6.
Number of surgical procedures.
Complications occurred in seven feet in each group, in similar manners (p = 0.85). In GI, three presented residual edema, two had contact dermatitis and two had excessive bleeding at the tenotomy site; in GII, two feet presented residual edema, four had dermatitis and one had excessive bleeding (Table 1).The excessive bleeding was resolved by removing the plaster case and applying local compression; after observing that hemostasis had been reached, a new plaster cast was placed.
Table 1.
Complications.
| Group 1 | Group 2 | |
|---|---|---|
| Dermatitis | 02 | 04 |
| Bleeding | 02 | 01 |
| Residual edema | 03 | 02 |
5. Discussion
The Ponseti method, which was published in 1963,21 was disparaged by orthopedic surgeons at that time because of the high number of recurrences over the short term. However, with improvements to the method, it regained space as a therapeutic option for CCF in the 1990s, with good long-term results shown by the original author.5, 6 Today, most services that treat this pathological condition start their approach towards CCF by using this method, because of its simplicity, effectiveness and drastically reduced need for extensive surgery.3, 5, 23, 24 On the other hand, it has been observed that, over the long term, patients who underwent surgical treatment with extensive release developed painful and stiff feet presenting under or overcorrection and lower muscle strength.24, 25 Moreover, these patients were liable to present the complications inherent to surgery, such as superficial and deep infection, skin necrosis and hypertrophic scar tissue.
Although our GII patients presented lower mean age at the start of the treatment than our GI patients (3.2 versus 5.4 months), this difference did not influence the results. It is known that CCF treatment should be started as early as possible, i.e. at ages when the tissue structures of the foot present greater plasticity. Studies have recommended that the approach should begin within the first 15 days of life.24, 26 We believe that the higher mean age among our patients occurred because our institution is a regional referral hospital for CCF treatment and thus the children came to us already at a greater age than is recommended.
In the past, since the great majority of feet evolved to surgical correction, authors at that time sought methods for evaluating the results such that there would be a single language, with the objective of emphasizing the clinical, functional and radiological aspects of the feet.10, 27 In these and other studies on surgical treatment of CCF, we applied the evaluation method proposed by Lehman for analysis on the results.10, 20, 27 However, currently, the Ponseti method does not place value on radiology but, rather, the functional and clinical characteristics of the foot. All the deformities of the foot need to be corrected and, if any recurrences appear, serial plaster casts should again be applied until a new correction is achieved, with or without the need for new tenotomy of the calcaneus. If these feet continue to present deformity, more extensive surgery will then be indicated and the result from these CCFs using the Ponseti method will be considered to be unsatisfactory.5, 6, 21, 22, 23, 24
Herzenberg et al.24 suggested that it would be necessary to assess their results from CCF treatment over the long term. We therefore divided our cases into two groups, according to their length of follow-up: GI with a mean of seven years and GII with 3.5 years, in order to analyze the results better and search for factors that might have led to improvement or worsening of the results, as well as assessing the learning curve for the method.
We achieved satisfactory results in both groups, with a significant difference such that GII was better (97.5% versus 85.3%). Ponseti reported an 89% success rate using this technique in some studies.12, 28 Other authors, in recently published papers, have shown results better than 90%.16, 24, 26
We believe that the higher frequency of satisfactory results in GII may be related to evolution of the learning curve, the shorter follow-up and better adherence to treatment among the children, due to good availability of information and the explanatory class on the method that was given to their parents.
In relation to the number of plaster casts used to correct the deformity, we found that on average there was a decline, which went from 9.5 in GI to 7 in GII, with statistical significance. This corroborates what was found by Herzenberg et al.,24 who also reported a mean of seven plaster casts. However, other studies have shown even lower means, like five plaster casts.22, 26 This decline in the number of plaster casts provides evidence of improvement in the way in which the method is implemented.
The number of tenotomy procedures on the calcaneus during the treatment was practically the same between the groups (67% GI; 65% GII). Likewise, Chu et al.26 also demonstrated a low percentage of tenotomy procedures (57%). However, most studies have reported rates greater than 80%.5, 6, 22, 24, 28 Ponseti himself performed this on more than 90% of the feet.5 Scher et al.22 analyzed the need for tenotomy of the calcaneal tendon and concluded that it did not worsen the results in comparison with the non-tenotomized feet. The main criterion for indicating tenotomy was lack of passive dorsiflexion of the foot of up to 15 degrees, after the plaster cast sequence. Despite our lower percentage of tenotomy procedures, we observed that this did not influence the results, which were in line with what we saw in the literature.
Both groups presented relapses, but with different presentations in terms of frequency (GI: 37.6%; GII: 14.2%). This clearly demonstrated the influence of continual practice of the method and patient adherence, on better performance. The Iowa group defined recurrence as the reappearance of any of the components of the deformity: cavus, adduction, varus or equinus.29 In the literature, non-adherence to treatment is cited as a factor that is important with regard to recurrence, with reported rates of up to 51%.29 This was clear from our sample, with evident diminution of recurrence in the second group, in which interactive classes for the adults responsible for our patients were instituted. Among the feet in which some deformity persisted, eleven (10.1%) in GI and three (2.5%) in GII underwent surgical treatment. Herzenberg et al.24 reported that there was a need for early surgery in 3% to 6% of the relapsed feed. Studies have shown that using the Ponseti method again, early on in the recurrence, is able to significantly diminish the recurrence and surgical treatment rates.30
In the current literature, it is emphasized that recurrences are unrelated to the severity of the deformities of the feet at the start of the treatment, or to the number of plaster casts used for correction. However, the authors are unanimous with regard to adherence to treatment: use of an abduction brace is the proper preventive method. Dobbs reported that failure to adhere to using the brace was the main cause of relapses in treating CCFs.30
Complications arose in both groups, and even presented the same absolute numbers: seven each, as already mentioned. The spectrum of these complications did not present any variation, with cases of excessive bleeding at the tenotomy site, residual edema and dermatitis. There was only a difference in terms of the learning curve between GI and GII. For us, this raised the point that these are complications that could occur in any series, independent of familiarity with the method. In 2004, Dobbs reported that 2% (four feet) presented excessive bleeding, in a retrospective study on 200 feet treated using the Ponseti method, which underwent percutaneous tenotomy.23 In our sample, this problem occurred in two feet in GI and one foot in GII.
We believe that the better results in GII were influenced by the greater focus given to the parents, regarding the need for adherence to the treatment, by means of an explanatory class on the method, and by improvements in the technique and going beyond the learning curve. There was no difference in the patients’ ages at the start of the treatment. However, the length of follow-up in GII was shorter (33.5 versus 85 months) and it is known that relapses occur more frequently up to the fourth year of life.
Greater length of follow-up is needed for the second group, in which relapses and surgical indications may arise, thus decreasing the number of satisfactory results and increasing the number of surgical indications. Nonetheless, in analyzing all the CCFs in the sample, regardless of the groups, the results from this method were very satisfactory.
6. Conclusion
The method was effective for treating CCF, and satisfactory results were observed in both groups, with low numbers of surgical indications and complications. The results were statistically superior in GII, with regard to correction of the deformities, number of plaster casts applied, recurrences and need for surgical indication.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Work performed in the Foot and Ankle Outpatient Clinic of the Orthopedics and Traumatology Service, Hospital Universitário de Taubaté (HUT), and at Instituto de Ortopedia de Taubaté (IOT), São Paulo, Brazil.
References
- 1.Jowett C.R., Morcuende J.A., Ramachandran M. Management of congenital talipes equinovarus using the Ponseti method: a systematic review. J Bone Joint Surg Br. 2011;93(9):1160–1164. doi: 10.1302/0301-620X.93B9.26947. [DOI] [PubMed] [Google Scholar]
- 2.Herring JB. Congenital talipes equinovarus. In: Tachdjian MO. Tachdjian: pediatric orthopaedics. Philadelphia: Saunders; 2001. p. 922-59.
- 3.Herzenberg J.E., Carroll N.C., Christofersen M.R., Lee E.H., White S., Munroe R. Clubfoot analysis with three-dimensional computer modeling. J Pediatr Orthop. 1988;8(3):257–262. doi: 10.1097/01241398-198805000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Song H.R., Carroll N.C., Neyt J., Carter J.M., Han J., D’Amato C.R. Clubfoot analysis with three-dimensional foot models. J Pediatr Orthop B. 1999;8(1):5–11. [PubMed] [Google Scholar]
- 5.Ponseti I.V. Treatment of congenital club foot. J Bone Joint Surg Am. 1992;74(3):448–454. [PubMed] [Google Scholar]
- 6.Ponseti I.V. Oxford University Press; New York: 1996. Congenital clubfoot: fundamentals of treatment. [Google Scholar]
- 7.Irani R.N., Sherman M.S. The pathological anatomy of clubfoot. J Bone Joint Surg Am. 1963;45:45–52. [Google Scholar]
- 8.McKay D.W. New concept of and approach to clubfoot treatment: section I-principles and morbid anatomy. J Pediatr Orthop. 1982;2(4):347–356. doi: 10.1097/01241398-198210000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Cummings R.J., Davidson R.S., Armstrong P.F., Lehman W.B. Congenital clubfoot. J Bone Joint Surg Am. 2002;84(2):290–308. doi: 10.2106/00004623-200202000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Lara LCR. Tratamento do pé torto congênito idiopático utilizando a técnica de liberação das partes moles póstero-médio-lateral, pela via de acesso de Cincinnati segmentada tese. São Paulo: Escola Paulista de Medicina; 2002.
- 11.Dietz F. The genetics of idiopathic clubfoot. Clin Orthop Relat Res. 2002;(401):39–48. doi: 10.1097/00003086-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ippolito E., Ponseti I.V. Congenital club foot in the human fetus. A histological study. J Bone Joint Surg Am. 1980;62(1):8–22. [PubMed] [Google Scholar]
- 13.Heck A.L., Bray M.S., Scott A., Blanton S.H., Hecht J.T. Variation in CASP10 gene is associated with idiopathic talipes equinovarus. J Pediatr Orthop. 2005;25(5):598–602. doi: 10.1097/01.bpo.0000173248.96936.90. [DOI] [PubMed] [Google Scholar]
- 14.Macnicol M.F. The management of club foot: issues for debate. J Bone Joint Surg Br. 2003;85(2):167–170. doi: 10.1302/0301-620x.85b2.14067. [DOI] [PubMed] [Google Scholar]
- 15.Dobbs M.B., Gurnett C.A. Update on clubfoot: etiology and treatment. Clin Orthop Relat Res. 2009;467(5):1146–1153. doi: 10.1007/s11999-009-0734-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Changulani M., Garg N.K., Rajagopal T.S., Bass A., Nayagam S.N., Sampath J. Treatment of idiopathic club foot using the Ponseti method. Initial experience. J Bone Joint Surg Br. 2006;88(10):1385–1387. doi: 10.1302/0301-620X.88B10.17578. [DOI] [PubMed] [Google Scholar]
- 17.Fonseca Filho FF, Ferreira RC, Martins GM. Estado atual do tratamento do pé torto congênito. In: Pardini Junior, Souza JMG, editores. Clínica ortopédica. Rio de Janeiro: Medsi; 2001. p. 283-307.
- 18.Turco V.J. Surgical correction of the resistant club foot. One-stage posteromedial release with internal fixation: a preliminary report. J Bone Joint Surg Am. 1971;53(3):477–497. [PubMed] [Google Scholar]
- 19.McKay D.W. New concept of and approach to clubfoot treatment: Section III--evaluation and results. J Pediatr Orthop. 1983;3(2):141–148. doi: 10.1097/01241398-198305000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Lara L.C., Sodré H. Estudo comparativo entre as técnicas de liberação de partes moles utilizando as vias de acesso de Codivilla e Cincinnati segmentada, no tratamento cirúrgico de pé torto congênito idiopático. Rev Bras Ortop. 1998;33(7):519–523. [Google Scholar]
- 21.Ponseti I.V., Smoley E.N. Congenital clubfoot: the results of treatment. J Bone Joint Surg Am. 1963;45:261–275. [Google Scholar]
- 22.Scher D.M., Feldman D.S., van Bosse H.J., Sala D.A., Lehman W.B. Predicting the need for tenotomy in the Ponseti method for correction of clubfeet. J Pediatr Orthop. 2004;24(4):349–352. doi: 10.1097/00004694-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Dobbs M.B., Gordon J.E., Walton T., Schoenecker P.L. Bleeding complications following percutaneous tendoachilles tenotomy in the treatment of clubfoot deformity. J Pediatr Orthop. 2004;24(4):353–357. doi: 10.1097/00004694-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Herzenberg J.E., Radler C., Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002;22(4):517–521. [PubMed] [Google Scholar]
- 25.Aronson J., Puskarich C.L. Deformity and disability from treated clubfoot. J Pediatr Orthop. 1990;10(1):109–119. [PubMed] [Google Scholar]
- 26.Chu A., Labar A.S., Sala D.A., van Bosse H.J., Lehman W.B. Clubfoot classification: correlation with Ponseti cast treatment. J Pediatr Orthop. 2010;30(7):695–699. doi: 10.1097/BPO.0b013e3181ec0853. [DOI] [PubMed] [Google Scholar]
- 27.Lara L.C.R., Luciano A.P., Barros M.A., Franco Filho N., Feroldi P.C. Avaliação funcional e radiográfica do pé torto congênito tratado cirurgicamente. Rev Bras Ortop. 2007;42(7):217–224. [Google Scholar]
- 28.Laaveg S.J., Ponseti I.V. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980;62(1):23–31. [PubMed] [Google Scholar]
- 29.Haft G.F., Walker C.G., Crawford H.A. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89(3):487–493. doi: 10.2106/JBJS.F.00169. [DOI] [PubMed] [Google Scholar]
- 30.Dobbs M.B., Rudzki J.R., Purcell D.B., Walton T., Porter K.R., Gurnett C.A. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86(1):22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]