Abstract
Objective
Research investigating long-term effects of childhood sexual abuse (CSA) on mental health for men is vastly underdeveloped. This study strengthened the knowledge base by examining: (a) long-term trajectories of depressive symptoms for men with and without a history of CSA, and (b) moderating effects of social support over time.
Method
We analyzed multiple waves of data from the Wisconsin Longitudinal Study. The sample (N = 2,451) consisted of men with histories of CSA and a stratified, randomly sampled comparison group. Growth curve modeling was employed for analyses.
Results
After controlling for demographic, parental, and health factors, men with CSA histories had greater depressive symptoms than those with no history of CSA. For both groups, depressive symptoms decreased over time; slope patterns did not differ. We found a significant moderating effect of social support on the relationship between CSA and depressive symptoms.
Discussion
This innovative, population-based, longitudinal study demonstrated that CSA can undermine mental health for men across the life span and into old age. Social support appears to mitigate these deleterious effects. In early, middle, and late adulthood, practitioners should assess for CSA and strengthen support resources for male survivors.
Keywords: Adverse childhood experiences, Complex trauma, Male survivors, Social support, Wisconsin Longitudinal Study
Epidemiological research suggests that childhood sexual abuse (CSA) is a serious public health issue affecting both men and women. Although prevalence rates vary depending on methodological considerations, approximately 20% of women and 8% of men worldwide experienced some form of sexual abuse during childhood (Pereda, Guilera, Forns, & Gómez-Benito, 2009). CSA is related to a litany of long-term outcomes such as mental health disorders (Papilla, Buebbers, Ogloff, Cutajar, & Mullen, 2016), substance abuse (Tonmyr & Shields, 2017), interpersonal conflict (Kennedy & Prock, 2016), physical health problems (Gilbert et al., 2009), and others. Emerging research indicates that some problems (e.g., bodily pain, mental illness, physical disabilities) extend across the life course and into old age (Draper et al., 2008; Talbot et al., 2009). However, most empirical studies on the long-term effects of CSA have been based on female samples (Gilbert et al., 2009); as a result, the knowledge base on boys/men who experienced CSA is vastly under-developed.
Although all survivors of CSA face formidable obstacles to reporting and disclosure, boys/men face some unique barriers including impaired masculine identity, internalized homophobia, and gender-based stigma (O’Leary & Barber, 2008; Easton, Saltzman, & Willis, 2014). Delayed disclosure, lack of support services, and lack of training among health care providers (Easton, 2013; Easton et al., 2014; Gruenfeld, Willis, & Easton, 2017) may undermine assessment and treatment of men with histories of CSA. These constraints may be especially harmful for male survivors of CSA in later life, thereby increasing their isolation and susceptibility to mental health issues such as depression.
The current study examined long-term effects of CSA on depressive symptoms for men in middle and late adulthood. The investigation used an integrated theoretical framework of complex trauma theory (Van der Kolk, 1996) and life course perspective (Elder & Johnson, 2003). Based on three-waves of data from the Wisconsin Longitudinal Study, we examined trajectories of depressive symptoms for survivors and investigated protective effects of social support. Results will enhance our understanding of mental health for male survivors across the life course and inform intervention strategies to reduce suffering among this population.
Literature Review
Integrated Theoretical Framework
Complex trauma theory posits that post-traumatic stress disorder (PTSD), adopted in the 1980s primarily in response to returning war veterans, does not fully capture clinical pathologies faced by many trauma survivors (Van der Kolk, 1996). Complex psychological trauma results from “…exposure to severe stressors that: (a) are repetitive or prolonged, (b) involve harm or abandonment by caregivers or other ostensibly responsible adults, and (c) occur at developmentally vulnerable times in the victim’s life, such as early childhood or adolescence” (Ford & Courtois, 2009, p. 13). Traumatic events such as child abuse involve interpersonal violation, victimization, betrayal, stigma, and shame (Briere & Spinazzola, 2005) and often co-occur with other environmental stressors (Ford & Courtois, 2009) that can augment psychological suffering for victims.
While PTSD is conceptualized as a specific triad of anxiety symptoms (i.e., re-experiencing, avoidance, hyperarousal) in response to specific external stimuli, complex trauma survivors experience a broader range of symptoms that are pervasive, chronic, and manifest themselves in multiple ways (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013). Complex trauma impairs various aspects of functioning, including: regulation of mood, attention or consciousness, self-perception, relations with others, and systems of meaning (Van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005). Across these domains, feelings of despair, hopelessness, shame, guilt, permanent damage, and suicide—all elements of depressive disorders—are common for survivors (Van der Kolk et al., 2005).
The inclusion of life course perspective (LCP; Elder & Johnson, 2003) into complex trauma theory enhances and compliments our understanding of CSA’s long-term effects. As a multidisciplinary framework, LCP examines how “…chronological age, relationships, common life transitions, and social change shape people’s lives from birth to death” (Hutchison, 2011, p. 8). These factors can set people on trajectories, long-term patterns of stability and change within different aspects of a person’s life (e.g., work, family, health; Elder & Johnson, 2003; Hutchison, 2011). Developmental risk factors, such as CSA, can undermine positive trajectories of physical and mental health decades after event occurrence (Hutchison, 2011). Importantly, LCP suggests that living a linked or interdependent life provides individuals with social support that can buffer them from harmful outcomes due to traumatic events. Through different forms (e.g., emotional, instrumental, appraisal, informational; Berkman, Glass, Brissette, & Seeman, 2000), social support is often exchanged across generations and more available within broader family and friendship networks (Hutchison, 2011).
Empirical Research on CSA
Although research on the short-term effects of CSA on mental health is well-developed, there is a small but growing literature on the long-term mental health effects in early or emerging adulthood (Maniglio, 2009). The majority of previous research is based on all-female samples (e.g., McGuigan & Middlemiss, 2005; Coles, Lee, Taft, Mazza, & Loxton, 2015). Studies with mixed-gender samples have found that a history of CSA is related to depression for both male and female college students (Cantón-Cortés, Cortés, & Cantón, 2012) and adults under 50 years of age (Turner & Lloyd, 1995). A cross-sectional study of 497 adult men with histories of CSA (mean age = 50.4 years) found elevated rates of mental distress, including symptoms of depression (Easton, 2014). Other cross-sectional studies with population-based samples of men have found that CSA is related to depression in middle or late adulthood (Easton & Kong, 2017; Turner, Taillieu, Cheung, & Afifi, 2017). In one of the few longitudinal studies, Fergusson, McLeod, and Horwood (2013) found that both men and women with histories of CSA had higher rates of depression at age 30 compared to adults with no CSA history.
Not all studies on CSA and depression, however, have generated consistent results. For example, two studies (Spataro, Mullen, Burgess, Wells, & Moss, 2004; Cutajar et al., 2010) found associations between CSA and psychopathology in early adulthood for male and female participants, including psychosis, anxiety, personality, and substance abuse disorders. Results from both studies also indicated a relationship between CSA and major affective disorders for the entire sample, but gender subanalyses did not find support of the relationship for male participants. These findings may be related to systematic bias due to data source (i.e., Victorian Psychiatric Case Registry), which included only inpatient cases from Australian public health facilities (Spataro et al., 2004; Cutajar et al., 2010). Additional methodological choices may also have contributed to divergent findings in the literature, including: lost cases due to linkage problems (between forensic medical records and the registry), lack of controls during matching (e.g., health status, income, education, marital status), and limited age range of participants. To address inconsistencies in the extant literature, more research is needed that focuses on men in middle and late life using more robust methodological approaches.
Complex trauma theory posits that environmental context can compound effects of a single traumatic stressor such as CSA (Ford & Courtois, 2009). For boys/men, CSA commonly co-occurs with other forms of childhood maltreatment, such as physical abuse and neglect, as well as household dysfunction (Dong et al., 2004; Easton, 2014; Easton & Kong, 2017; Turner et al., 2017). Mounting evidence suggests that a class of early life stressors, adverse childhood experiences (ACE; Felitti et al., 1998), is related to long-term mental health problems including depression in the general population (Cavanaugh, Petras, & Martins, 2015). In previous research with Wisconsin Longitudinal Study (Springer, Sheridan, Kuo, & Carnes, 2007; Springer, 2009), scholars examined effects of childhood physical abuse on adult physical and mental health, controlling for other childhood adversities and family background.
Based on the concept of linked and interdependent lives, LCP contends that social support from significant relationships can mitigate negative effects of traumatic experiences (Hutchison, 2011). A well-developed body of empirical literature has established that social support has beneficial effects on health for older adults (e.g., Thomas, 2010). More specifically, Marriott, Hamilton-Giachritsis, and Harrop (2014) analyzed 50 peer-reviewed studies with survivors of CSA and found that social support indicators were associated with resilient outcomes (e.g., lack of psychopathology). Some studies with all (or predominantly) female samples of CSA survivors have demonstrated that supportive relationships facilitate healing (Glaister & Abel, 2001), promote resilience (Valentine & Feinauer, 1993), and protect against psychological disorders (Collishaw et al., 2007). Musliner and Singer (2014) found that parental (i.e., warmth, relationship satisfaction) and friend support (i.e., number of close friends) reduced the odds of depression for adult survivors, but only in case when the sexual abuse was committed by someone other than a parent or caregiver. Among a large sample of men with histories of CSA, Easton (2014) found that a specific form of social support (i.e., positive response to disclosure of CSA) was related to lower levels of mental distress, including depressive symptoms.
Current Study
Overall, our current understanding of life course effects of CSA on depression for men is extremely limited. Most previous studies have employed cross-sectional designs, which prohibits the analysis of depression levels across time. Other research has been based on data collected from samples comprised primarily (or exclusively) of female survivors of CSA and/or survivors in early or young adulthood. Our literature review did not identify studies that examined depression in late life. Furthermore, little is known about factors (e.g., social support) that may explain why some men who experienced sexual abuse have better mental health outcomes than other CSA survivors (Maniglio, 2009). To address these gaps in the literature, the current study examined male survivors of CSA in middle and late adulthood, investigating their trajectories of depressive symptoms across two decades using a population-based, longitudinal data set. To accurately assess the long-term effect of CSA, we created a matched-comparison group based on sociodemographic characteristics, considered effects of childhood environment, and examined the potential moderating influence of social support on the relationship between CSA and depressive symptoms for this population, all distinctive contributions to the literature.
Methods
Data Source
The Wisconsin Longitudinal Study (WLS) is a long-term population-based study of a random sample of 10,317 men and women who graduated from Wisconsin high schools in 1957 and 5,823 of their siblings. After the first interview in 1957, graduates were re-interviewed at subsequent time points by telephone and mailed questionnaires: 1975 (35–36 years of age), 1993 (53–54 years), 2004 (64–65 years), and 2011 (71–72 years). Data was also collected from a randomly selected sibling of each graduate in four corresponding waves (1977, 1994, 2005, 2011). Because only the last three waves contain variables of interest, our study used data from graduates and siblings in 1993–1994 (Wave 1), 2004–2005 (Wave 2), and 2011 (Wave 3).
High retention rates characterize the WLS. In the 1993 data set, for example, 87.2% of surviving graduates (n = 8,493) completed the telephone survey and 80.9% of the telephone sample (n = 6,875) completed the mail survey. In the 1994 data set, 4,778 surviving siblings completed the telephone survey and 84.5% of siblings (n = 4,039) completed the mail survey. Across all waves, the overall response rate for surviving graduates was 73.8% for the telephone survey (for additional information on WLS retention rates, see WLS [n.d.]).
Study Sample
In order to examine trajectories of depressive symptoms over time and compare long-term patterns between men with and without histories of CSA, this study utilized data from three waves of the WLS. Two groups were created using a pooled sample of 5,013 respondents (3,145 graduates; 1,868 siblings) from the Wave 2 data set, which included data on early life adversities. A total of 129 respondents reported having experienced sexual abuse during childhood. From the remaining 4,884 respondents, we used stratified random sampling to select a comparison group (i.e., no history of CSA) that had similar sociodemographic characteristics with the CSA group. Using a matched comparison group is valuable because it reduces confounding bias when comparing abused and nonabused groups, important considerations when evaluating relationships between CSA and negative outcomes in later life (Bolen, 2001; Osborne, 2008).
Consistent with WLS researchers who relied on matched comparison groups (e.g., Song, Floyd, Seltzer, Greenberg, & Hong, 2010; Seltzer, Floyd, Song, Greenberg, & Hong, 2011), we used age and education as stratification variables. We first examined variable distribution among the CSA group to determine strata levels. By comparing the number of people in each stratum between the CSA and comparison groups, we derived a matching ratio of 1:18. Respondents were then randomly selected from each stratum based on the ratio, creating a comparison group of 2,322 respondents. A series of t tests and χ2 tests confirmed that there were no significant group differences on age, marital status, educational attainment, household income, and health status based on Wave 2 data. Our final study sample consisted of 2,451 men. The abused group (n = 129) constituted 5.3% of the study sample.
Measures
Key variables were measured repeatedly over three waves, except for childhood abuse/adversities.
Depressive symptoms
Depressive symptoms were evaluated using the 20-item Center for Epidemiologic Studies Depression scale (CES-D) (Radloff, 1977). This scale has been widely used to assess later-life depression (Haringsma, Engels, Beekman, & Spinhoven, 2004). Items ask about frequency of common depressive symptoms such as depressed mood, feeling worthless/hopeless, and loss of appetite. Response choices ranged from zero to seven, indicating number of days each symptom was experienced in the past week. Responses were averaged to produce a total score (range = 0–7); higher scores indicated higher levels of depressive symptoms. The square root was taken to adjust skewness.
Sexually abused in childhood
CSA history was assessed using four self-reported items included in the Wave 2 data collection: “Up-until 18, to what extent (a) did your father have oral, anal, or vaginal sex with you against your wishes?; (b) did any other person have oral, anal, or vaginal sex with you against your wishes?; (c) did your father treat you in way that you consider sex abuse?; (d) did any other person treat you in way that you consider sex abuse?” Response choices were based on a four-point Likert scale: not at all (a), a little (b), some (c), and a lot (d). A new variable for sexual abuse was then created; respondents who answered a little, some, or a lot on any of the four items were coded as having been sexually abused during childhood (yes = 1; no = 0).
Childhood adversities
The number of childhood adversities was measured with items that corresponded with major categories within the Adverse Childhood Experiences (ACE; Center for Disease Control and Prevention, 2016). WLS contained items for seven ACE categories: emotional abuse, physical abuse, neglect, family dysfunction, parental divorce, witnessing domestic violence, and living with a household member with a substance problem. For example, one item asked: “Up until you were 18, how often did you see a parent or one of your brothers or sisters get beaten at home.” Response choices were based on a 5-point Likert scale ranging from never (1) to very often (5). For each item, responses of often (4) and very often (5) were recoded into yes (1) and summed to produce a total count of the number of adversities (range = 0–7).
Social support
Two items measured social support: “Is there a person in your (a) family, including a spouse, with whom you can really share your very private feelings and concerns?”; (b) friend with whom you can really share your very private feelings and concerns?” Item responses (yes= 1; no = 0) were summed to create a total score which ranged from 0 to 2.
Control variables
Sociodemographic characteristics, including birth year, marital status (married, nonmarried), self-rated health condition (good/excellent, very poor/poor/fair), educational attainment (years), annual household income, and childhood background (level of father’s education, rural background) were controlled in the analyses. Marital status, self-rated health condition, and household income variables were measured across three waves and were treated as time varying; birth year, educational attainment, and childhood background variables were treated as time invariant.
Analytic Strategy
Growth curve modeling techniques were employed to explore the trajectory of changes in depressive symptoms through mid- and late adulthood between CSA and non-CSA groups (Trickett, Noll, & Putnam, 2011; Panik, 2014). We included two levels: Level 1 was time (age) and Level 2 was individual (i.e., respondents). Age was mean-centered at 60 years. Because there were few graduate and sibling pairs (n = 150), we did not introduce a third level to control for family effect; instead, we added childhood environmental factors (i.e., father’s education, rural background) as covariates. The first goal was to estimate age trajectories of depressive symptoms between adults who experienced CSA and those who did not (Models 1–3 in Table 2). Next, depressive symptoms were regressed on social support (Model 4 in Table 2). Cross-level interaction effects were then estimated to evaluate whether effects of social support moderated the relationship between CSA and depressive symptoms (Model 5 in Table 2).
Table 2.
Two-level Growth Curve Models Predicting Depressive Symptoms
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Intercept (β0) | |||||
| Intercept (γ00) | 0.76*** | 1.03*** | 1.03*** | 1.02*** | 1.02*** |
| Sexually abused (γ01) | 0.06* | 0.04 | 0.04 | 0.04 | |
| Childhood adversities (γ02) | 0.04*** | 0.03*** | 0.03*** | ||
| Education (γ03) | −0.01 | −0.01 | −0.01 | −0.01 | |
| Father’s education (γ04) | 0.001 | 0.001 | 0.001 | 0.002 | |
| Rural background (γ05) | −0.04* | −0.03* | −0.03* | −0.03* | |
| Birth year (γ06) | 0.01*** | 0.01*** | 0.01** | 0.01** | |
| Agea (β1) | |||||
| Intercept (γ10) | −0.003*** | −0.004*** | −0.004*** | −0.004*** | −0.004*** |
| Sexually abused (γ11) | 0.004 | 0.004 | 0.004 | 0.003 | |
| Social support (β2) | |||||
| Intercept (γ20) | −0.07*** | −0.06*** | |||
| Sexually abused (γ21) | −0.07* | ||||
| Married (β3) | |||||
| Intercept (γ30) | −0.08*** | −0.08*** | −0.08*** | −0.08*** | |
| Good or excellent health (β4) | |||||
| Intercept (γ40) | −0.22*** | −0.22*** | −0.22*** | −0.22*** | |
| Household income (β5) | |||||
| Intercept (γ50) | −0.0002*** | −0.0002*** | −0.0002*** | −0.0002*** | |
| Variance components | |||||
| Level-1 variance (σ2) | 0.27 | 0.27 | 0.27 | 0.27 | 0.27 |
| Level-2 intercept variance (τ00) | 0.29*** | 0.27*** | 0.27*** | 0.27*** | 0.27*** |
| Level-2 age slope variance (τ11) | 0.01*** | 0.01*** | 0.01*** | 0.01*** | 0.01*** |
Note: aAge was mean-centered at age 60. Analyses were conducted using 20 imputed data sets.
*p < .05. **p < .01. ***p < .001.
The level-1 equation for Model 5 can be expressed as: Yij = β0j + β1j(age)ij +β2j (social support)ij +β3j (married)ij +β4j (good/excellent health)ij +β5j (household income)ij + rij. Yij indicated depressive symptoms at age i of person j and β0j as the level-1 intercept. In addition to the intercept (β0j), the effect of age (β1j) was modeled as random to assess how age trajectories varied by individual characteristics. The effect of abuse history was the focus of this study.
The level-2 equation for Model 5 can be expressed as:
β 1j = γ10 + γ11 (sexually abused)j + μ1j
β 2j = γ20 + γ21 (sexually abused)j
β 3j = γ30
β 4j = γ40
β 5j = γ50
Data analyses were conducted using STATA 14. Assump tions for multilevel regression modeling, including normality and homoscedasticity, were met. In terms of missing information, 50.1% of cases provided complete data across three waves. To address missing values, we conducted multiple imputation using the ICE procedure based on all the variables used in the analyses and generated 20 imputed datasets. The strategy of multiple imputation then deletion was used for the dependent variable.
Results
Table 1 presents descriptive characteristics of the study sample as well as grand means for subgroups. The average age of respondents across the three waves was approximately 63 years (SD = 8.65). On average, respondents indicated that they had completed fourteen years of education (i.e., high school graduate with some college education) and that their fathers had completed ten years (i.e., less than high school graduate). Mean household income was $74,124 (SD = 78,912). Respondents experienced, on average, 0.70 childhood adversities (SD = 1.18). Across waves, most respondents reported that they were married (77.8%) and in good or excellent health (70.0%). Almost one-third of respondents (29.7%) reported that they lived in rural areas during childhood.
Table 1.
Descriptive Statistics of Key Variables
| Variable | Total sample (N = 2,451) | Sexually abused in childhood (CSA, N = 129) | Non-CSA (N = 2,322) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Depressive symptomsa | 0.73 (0.71) | 0.88 (0.83) | 0.72 (0.70) |
| Social supporta | 1.47 (0.66) | 1.46 (0.72) | 1.47 (0.65) |
| Childhood adversitiesb,c | 0.70 (1.18) | 1.45 (1.82) | 0.66 (1.11) |
| Agea | 62.88 (8.65) | 62.86 (8.40) | 62.88 (8.66) |
| Years of educationb | 14.44 (2.67) | 14.58 (2.68) | 14.43 (2.67) |
| Years of father’s educationb | 10.05 (3.56) | 9.80 (3.58) | 10.06 (3.56) |
| Household income ($)a | 74,124.21 (78,912.13) | 77,248.56 (82,868.54) | 73,949.32 (78,688.26) |
| % | % | ||
| Marrieda,d | 77.75 | 73.90 | 77.96 |
| Good or excellent healtha,e | 70.03 | 63.82 | 70.37 |
| Rural backgroundb,f | 29.66 | 27.13 | 29.80 |
Note: Values are reported prior to data transformation and multiple imputation. CSA = Childhood sexual abuse.
aTime-varying variables were repeatedly measured across the three waves; the grand mean values are shown. bTime-invariant variables were measured at Wave 1. cChildhood adversities was a count of the types of childhood stressors. dMarried: 1 (married), 0 (nonmarried). eGood health: 1 (good or excellent health), 0 (very poor, poor, or fair health). fRural background: 1 (grew up in rural areas), 0 (grew up in nonrural areas).
Growth Curve Models
Parameter estimates of growth curve analyses are shown in Table 2. In the null model (not shown), average depressive symptoms across all individuals and waves were 0.75 (p < .001) which corresponds to 0.87 in terms of the value prior to the square-root transformation. As age was added in Model 1, average depressive symptoms were 0.76 (p < .001). Level-2 intercept variance was statistically significant (p < .001), indicating individual differences in the dependent variable across respondents. The fixed effect of age was also statistically significant (γ10 = −0.003, p < .001). This γ10 coefficient is equal to −0.05 in terms of depressive symptoms prior to the square-root transformation. The random effect of age slope (τ11) was statistically significant (p < .001), indicating significant variations in how depressive symptoms change as respondents age across waves.
CSA was added in Model 2 and was statistically significant, indicating that adults who experienced sexual abuse had greater depressive symptoms than those who did not (γ01 = 0.06, p < .05). This γ01 coefficient is equal to 0.25 in terms of depressive symptoms prior to the square-root transformation. Given the units of measurement in the depression scale, this finding signifies a noticeable clinical effect of heightened frequency of depressive symptoms due to CSA (Baguley, 2009). However, cross-level interaction between CSA and age was not statistically significant; thus, how depressive symptoms change across waves (i.e., rate of change) was not different between men with and without CSA histories. Level-2 variances of intercept and age slope were statistically significant (p < .001). Model 2 also included time-invariant (i.e., years of education, father’s education, rural background, birth year) and time-varying (i.e., marital status, self-reported health status, household income) covariates. Rural background was negatively associated with depressive symptoms (γ05 = −0.04, p < .05). Birth year was positively associated with our outcome (γ06 = 0.01, p < .001), indicating that being born earlier was associated with lower levels of depressive symptoms. Three time-varying covariates—marital status, health status, and household income—were negatively associated with depressive symptoms (γ30 = −0.08; γ40 = −0.22; γ50 = −0.0002, ps < .001, respectively).
Model 3 added childhood adversities. Each additional childhood adversity was positively associated with depressive symptoms (γ02 = 0.04, p < .001). This γ02 coefficient is equal to 0.20 in terms of depressive symptoms prior to the square-root transformation, also indicating a noticeable clinical effect. In this model, CSA was no longer significant. To examine how social support is associated with depressive symptoms over time, we added the main effect of social support (grand-mean centered) in Model 4. Results showed that social support was negatively associated with depressive symptoms for the overall sample (γ20 = −0.07, p < .001).
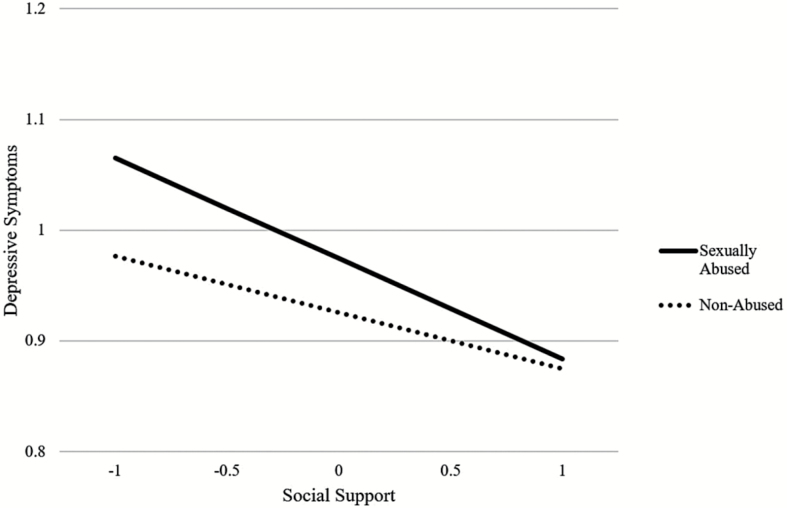
To examine moderating effects of social support in the association between CSA and depressive symptoms, Model 5 added cross-level interactions between CSA and social support. Results showed that the conditional grand mean of depressive symptoms was 1.02 when other predictors were zero or at their mean (γ00 = 1.02, p < .001). Childhood adversities were positively associated with depressive symptoms (γ02 = 0.03, p < .001). CSA was not statistically significant and there were no significant cross-level interactions between CSA and age. The cross-level interaction between CSA and social support, however, was statistically significant. As shown in Figure 1, the level of social support significantly moderated the association between CSA and depressive symptoms (γ21 = −0.07, p < .05). The coefficient γ21 corresponds to −0.26 in terms of depressive symptoms prior to the square-root transformation. This indicates that higher levels of social support may protect against the damaging effects of CSA in terms of depressive symptoms for men in middle and late adulthood.
Figure 1.
Cross-level interaction between social support and sexual abuse in childhood (Model 5).
Discussion
The central aim of this study was to examine effects of CSA on mental health trajectories using data from a population-based, random sample of men in middle and late adulthood. After controlling for sociodemographic, health, and childhood background factors, we found that men who reported being sexually abused in childhood experienced higher levels of depressive symptoms in their fifties, sixties and seventies compared to men without histories of CSA. This finding is congruent with our integrated theoretical framework of complex trauma theory (Van der Kolk, 1996) and life course perspective (Elder & Johnson, 2003), which suggests that the effects of traumatic stressors in early life can reverberate across the life span. The results of this study extend findings from previous studies with male survivors of CSA that used cross-sectional designs (e.g., Easton & Kong, 2017; Turner et al., 2017) and build on the limited number of longitudinal studies (e.g., Fergusson et al., 2013). This finding is inconsistent with prior studies that did not establish a link between CSA and depression for male survivors (Spataro et al., 2004; Cutajar et al., 2010). However, differences in results may be due to methodological limitations of those studies (e.g., data source, matching process, limited age range). Our findings suggest that CSA may indeed put male survivors at risk for depression in the second half of their lives. Based on this knowledge, physicians and mental health practitioners who serve men in midlife and late life should incorporate CSA into assessment protocols, thus increasing opportunities for intervention and treatment of residual effects of early life trauma.
Complex trauma theory also suggests that early environmental stressors can augment suffering for survivors (Ford & Courtois, 2009). As expected, the number of childhood stressors (beyond CSA) was associated with depressive symptoms. Thus, witnessing domestic violence or living with someone with a substance abuse problem during childhood is related to distal mental health, as supported by previous literature in the general population (Cavanaugh et al., 2015) and, more specifically, among men with histories of CSA (Easton, 2014; Easton & Kong, 2017; Turner et al., 2017). Although the number of childhood adversities pose risks to mental health for all men across the life course, their co-occurrence with CSA underscores the need to assess and address them in clinical practice with CSA survivors.
Interestingly, results indicated that the effect of CSA became statistically non-significant when the variable for childhood stressors was added to the model. There are several possible explanations for this finding. It is possible that environmental context (i.e., number of childhood adversities) is the most potent predictor of long-term mental health and thus masked the effects of CSA. Another possibility is that the cumulative effects of multiple types of childhood stressors may be more important than any one form of abuse or neglect. A third interpretation is that subsequent life stressors may mediate the relationship between CSA and depressive symptoms. Among sexually abused children, those who are exposed to additional life adversities later in childhood, adolescence, or adulthood may be at increased risk of mental health problems across the life course.
Yet another interpretation could be based on limitations associated with WLS items, which assessed CSA with a restricted range of sexual abuse behaviors. Thus, WLS may underestimate the number of men in the sample that actually experienced CSA, a possibility supported by the small number of men in the abused subsample (n = 129). Due to the measure, men with actual sexual abuse histories may have been included in the comparison group, a problem recognized by other researchers (Spataro et al., 2004; Cutajar et al., 2010) and one that may have suppressed the effects of CSA. Relatedly, the WLS items did not assess characteristics of CSA such as severity. According to complex trauma theory, shame and psychological injury may be more pronounced with more severe sexual abuse (e.g., penetrative abuse committed over a long period of time by a biological relative). These possibilities underscore the need for more research that explores the distinct contributions of specific types of childhood adversities on long-term mental health, which is discussed below.
Relatedly, we examined the rate of change for depressive symptoms for men with and without histories of CSA. For both groups, there was a small (but statistically significant) decline in the level of depressive symptoms across the waves of data. We then compared the rate of change (i.e., slope) of the abused group to the non-abused group and found that the difference was not statistically significant. These findings are consistent with the few existing studies of men with histories of CSA (e.g., Easton, 2014) in which age was a protective factor in cross-sectional analyses. Although mental health screening services are needed for men throughout the second half of their lives, early prevention and interventions services in midlife seem especially important.
A second aim of the study was to investigate the possible moderating effect of social support on the relationship between CSA and depressive symptoms. As posited by LCP (Hutchison, 2011) and consistent with general literature (e.g., Taylor & Lynch, 2004), social support was negatively related to depressive symptoms across the waves for the entire sample. However, our results found support for an interaction between social support and CSA. That is, the negative effects of CSA on depression appear to weaken at higher levels of social support for men, an important finding that is similar to literature conducted primarily with female survivors of CSA (Valentine & Feinauer, 1993; Glaister & Abel, 2001; Collishaw et al., 2007). In supplementary analysis, however, the social support did not moderate the relationship between childhood adversities and depressive symptoms. Having supportive relationships may help men with histories of CSA disclose their past abuse experiences and facilitate meaning-making, both of which have positive mental health effects for this population (Easton, 2014). Mental health practitioners should evaluate the size, strength, and quality of social support networks in clinical work with men with CSA histories.
Strengths and Limitations
Based on an integrated theoretical framework, this investigation of the effects of CSA on mental health trajectories of men had many strengths. The longitudinal design allowed for comparison of levels as well as rates of change for depressive symptoms in middle and late life. Use of a population-based data set, a stratified, random comparison group, an extensive set of control variables, and advanced statistical procedures increased the rigor of the study and represented improvements over previous research. As called for by Maniglio (2009), identification of malleable, protective mechanisms (i.e., social support) can inform innovative practice interventions.
Nonetheless, study limitations must be considered when interpreting results. First, results from the geographically-bound WLS may not be generalizable to all segments of the U.S. population, especially racial and ethnic minorities. The WLS is largely representative of older White American high school graduates (Herd, Carr, & Roan, 2014). However, it is possible that CSA may affect mental health trajectories differently among African American, Latino, and other diverse communities, particularly because Wisconsin, compared to the nation at-large, is a relatively homogenous state in terms of race and ethnicity. These issues should be examined in future studies with more heterogeneous samples that are representative of recent cohorts of high school graduates in the United States.
Second, CSA was measured with a few retrospective, self-reported items at Wave 2 and generated a small subsample of abuse survivors (n = 129). Despite careful attention in creating and matching the larger comparison group in accordance with previous WLS scholarship, the design of CSA items may have led to under-reporting of sexual abuse due to factors such as stigma, denial, definitional issues, gender or generational norms, or psychological health, thereby suppressing results. Additionally, previous research has found that some characteristics of CSA, such as duration (Easton, Renner, & O’Leary, 2013) and force by abuser (Easton et al., 2013; Easton, 2014), have been linked to worse psychological, long-term outcomes. More nuanced measures of CSA in future studies that include indicators of severity and generate more balanced subgroups would enhance our understanding.
Third, the measure of social support focused on potential support from a family member or friend. It is possible that actual support might play a more important role in preventing or mitigating depressive symptoms among survivors. Future investigations could include measures of types (e.g., emotional, instrument; Berkman et al., 2000) and characteristics (e.g., frequency, duration, in-person/electronic) of social support. More specifically, relational or marital satisfaction may be an important form of support to mitigate depression among CSA survivors and worthy of further examination in men (Feinauer, Callahan, & Hilton, 1996). It would also be helpful to assess social interactions related to trauma processing (e.g., disclosure), which often are critical to well-being for CSA survivors (Easton, 2013; Easton, 2014).
Directions for Future Research
Beyond these methodological suggestions, researchers should pursue related topics to advance our understanding of CSA and late life mental health. For example, a multicohort, longitudinal study would help elucidate whether there are generational differences in terms of the experience of CSA and its effects. The current study focused on high school graduates (and siblings) in the late 1950s; it would be interesting to investigate and compare trajectories of later graduates. Also, future studies should explore the relationship between CSA and other childhood adversities. In this study, CSA fell below significance when we included childhood adversities in models. Parsing out the individual, cumulative, and interactive effects of these different types of abuse and neglect would increase knowledge of early life course trauma. More research into how CSA may be related to subsequent stressors or adversities that unfold later in childhood, adolescence, and adulthood would expand our knowledge. Last, more intervention research with older adults with histories of CSA, such as organizing support groups, targeted psychoeducation campaigns, or clinical treatment modalities, is sorely needed. The most important implication of our results was that CSA and childhood adversities should be included in clinical assessments with older men. Scholarship is needed to identify the most effective means of gathering sensitive information from men in their fifties and older and delivering services that alleviate psychological suffering within this population.
Funding
The primary support for this work was by the National Institute on Aging of the National Institutes of Health (R03AG048768). The study was also partially supported by the Institute on Aging at Boston College (Aging Research Incentive Grant) and the National Institute on Aging Grant T32 AG049676 to The Pennsylvania State University.
Conflict of Interest
None reported.
Author Contributions
S. D. Easton planned the study, supervised data analysis, and wrote the paper. J. Kong helped plan the study, performed all statistical analyses, and wrote major sections of the paper. Both M. Gregas and C. Shen helped develop the statistical analysis plan, reviewed statistical analyses, and assisted in revising the paper. K. Shafer reviewed statistical analyses and helped revise the paper.
Acknowledgments
The authors are grateful for the advice and guidance from Dr. Jan Greenberg (School of Social Work) and Dr. Jieun Song (Waisman Center) at the University of Wisconsin-Madison and for assistance with manuscript preparation from Mr. Robert Hasson.
References
- Berkman L. F. Glass T. Brissette I. & Seeman T. E (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine (1982), 51, 843–857. doi:10.1016/S0277-9536(00) [DOI] [PubMed] [Google Scholar]
- Baguley T. (2009). Standardized or simple effect size: What should be reported?British Journal of Psychology (London, England: 1953), 100, 603–617. doi:10.1348/000712608X377117 [DOI] [PubMed] [Google Scholar]
- Bolen R. M. (2001). Child sexual abuse: Its scope and our failure. New York, NY: Kluwer Academic/Plenum. [Google Scholar]
- Briere J. & Spinazzola J (2005). Phenomenology and psychological assessment of complex posttraumatic states. Journal of Traumatic Stress, 18, 401–412. doi:10.1002/jts.20048 [DOI] [PubMed] [Google Scholar]
- Cantón-Cortés D., Cortés M. R., & Cantón J (2012). The role of traumagenic dynamics on the psychological adjustment of survivors of child sexual abuse. European Journal of Developmental Psychology, 9, 665–680. doi:10.1080/17405629.2012.660789 [Google Scholar]
- Cavanaugh C. E. Petras H. & Martins S. S (2015). Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Social Psychiatry and Psychiatric Epidemiology, 50, 1257–1266. doi:10.1007/s00127-015-1024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (2016). Adverse Childhood Experiences (ACEs). Retrieved from http://www.cdc.gov/violenceprevention/acestudy/. [Google Scholar]
- Cloitre M., Garvert D. W., Brewin C. R., Bryant R. A., & Maercker A (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4,1–12. doi:10.3402/ejpt.v4i0.20706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles J. Lee A. Taft A. Mazza D. & Loxton D (2015). Childhood sexual abuse and its association with adult physical and mental health: Results from a national cohort of young Australian women. Journal of Interpersonal Violence, 30, 1929–1944. doi:10.1177/0886260514555270 [DOI] [PubMed] [Google Scholar]
- Collishaw S. Pickles A. Messer J. Rutter M. Shearer C. & Maughan B (2007). Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect, 31, 211–229. doi:10.1016/j.chiabu.2007.02.004 [DOI] [PubMed] [Google Scholar]
- Cutajar M. C. Mullen P. E. Ogloff J. R. Thomas S. D. Wells D. L. & Spataro J (2010). Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse & Neglect, 34, 813–822. doi:10.1016/j.chiabu.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Dong M., Anda R. F., Felitti V. J., Dube S. R., Williamson D. F., Thompson T. J., … Giles W. H(2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28, 771–784. doi:10.1016/j.chiabu.2004.01.008 [DOI] [PubMed] [Google Scholar]
- Draper B., Pfaff J. J., Pirkis J., Snowdon J., Lautenschlager N. T., Wilson, I., & Almeida, O. P.; Depression and Early Prevention of Suicide in General Practice Study Group. (2008). Long-term effects of childhood abuse on the quality of life and health of older people: Results from the Depression and Early Prevention of Suicide in General Practice Project. Journal of the American Geriatrics Society, 56, 262–271. doi:10.1111/j.1532-5415.2007.01537.x [DOI] [PubMed] [Google Scholar]
- Easton S. D. (2013). Disclosure of child sexual abuse among adult male survivors. Clinical Social Work Journal, 41, 344–355. doi:10.1007/s10615-012-0420-3 [Google Scholar]
- Easton S. D. (2014). Masculine norms, disclosure, and childhood adversities predict long-term mental distress among men with histories of child sexual abuse. Child Abuse and Neglect, 38, 243–251. doi:10.1016/j.chiabu.2013.08.020 [DOI] [PubMed] [Google Scholar]
- Easton S. D., & Kong J (2017). Mental health indicators fifty years later: A population-based study of men with histories of child sexual abuse. Child Abuse and Neglect, 63, 273–283. doi:10.1016/j.chiabu.2016.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton S. D., Renner L. M., & O’Leary P (2013). Suicide attempts among men with histories of child sexual abuse: Examining abuse severity, mental health, and masculine norms. Child Abuse and Neglect, 37, 380–387. doi:10.1016/j.chiabu.2012.11.007 [DOI] [PubMed] [Google Scholar]
- Easton S. D., Saltzman L. & Willis D (2014). “Would you tell under circumstances like that?”: Barriers to disclosure for men who were sexually abused during childhood. Psychology of Men and Masculinity, 15, 460–469. doi:10.1037/a0034223 [Google Scholar]
- Elder G. H., & Johnson M. K (2003). The life course and aging: Challenges, lessons, and new directions. In Settersten R., Jr (Ed.), Invitation to the life course: Toward new understandings of later life (pp. 49–81). Amityville, NY: Baywood Publishing Co. [Google Scholar]
- Feinauer L. L., Callahan E. H., & Hilton H. G (1996). Positive intimate relationships decrease depression in sexually abused women. American Journal of Family Therapy, 24, 99–106. doi:10.1080/01926189608251023 [Google Scholar]
- Felitti V. J., Anda R. F., Nordenberg D., Williamson D. F., Spitz A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fergusson D. M. McLeod G. F. & Horwood L. J (2013). Childhood sexual abuse and adult developmental outcomes: Findings from a 30-year longitudinal study in New Zealand. Child Abuse & Neglect, 37, 664–674. doi:10.1016/j.chiabu.2013.03.013 [DOI] [PubMed] [Google Scholar]
- Ford J. D., & Courtois C. A (2009). Defining and understanding complex trauma and complex traumatic stress disorders. Treating complex traumatic stress disorders: An evidence-based guide (pp. 13–30). New York, NY: Guildford Press. [Google Scholar]
- Gilbert R., Widom C. P., Browne K., Fergusson D., Webb E., & Janson S (2009). Burden and consequences of child maltreatment in hi-income countries. Lancet, 373, 68–81. doi:10.1016/S01406736(08)61706–7 [DOI] [PubMed] [Google Scholar]
- Glaister J. A. & Abel E (2001). Experiences of women healing from childhood sexual abuse. Archives of Psychiatric Nursing, 15, 188–194. doi:10.1053/apnu.2001.25419 [DOI] [PubMed] [Google Scholar]
- Gruenfeld L., Willis D., & Easton S. D (2017)“A very steep climb”: Therapists’ perspectives on barriers to disclosure of childhood sexual abuse experiences for men. Journal of Child Sexual Abuse, 26, 731–751. doi:10.1080/10538712.2017.1332704 [DOI] [PubMed] [Google Scholar]
- Haringsma R. Engels G. I. Beekman A. T. & Spinhoven P (2004). The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. International Journal of Geriatric Psychiatry, 19, 558–563. doi:10.1002/gps.1130 [DOI] [PubMed] [Google Scholar]
- Herd P. Carr D. & Roan C (2014). Cohort profile: Wisconsin longitudinal study (WLS). International Journal of Epidemiology, 43, 34–41. doi:10.1093/ije/dys194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchison E. D. (2011). Dimensions of human behavior: The changing life course. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Kennedy A. C., & Prock K. A (2016). “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, and Abuse, 1–16. doi:10.1177/1524838016673601. [DOI] [PubMed] [Google Scholar]
- Maniglio R. (2009). The impact of child sexual abuse on health: A systematic review of reviews. Clinical Psychology Review, 29, 647–657. doi:10.1016/j.cpr.2009.08.003 [DOI] [PubMed] [Google Scholar]
- Marriott C., Hamilton-Giachritsis C., & Harrop C (2014). Factors promoting resilience following childhood sexual abuse: A structured, narrative review of the literature. Child Abuse Review, 23, 17–34. doi:10.1002/car.2258 [Google Scholar]
- McGuigan W. M. & Middlemiss W (2005). Sexual abuse in childhood and interpersonal violence in adulthood: A cumulative impact on depressive symptoms in women. Journal of Interpersonal Violence, 20, 1271–1287. doi:10.1177/0886260505278107 [DOI] [PubMed] [Google Scholar]
- Musliner K. L. & Singer J. B (2014). Emotional support and adult depression in survivors of childhood sexual abuse. Child Abuse & Neglect, 38, 1331–1340. doi:10.1016/j.chiabu.2014.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary P. J. & Barber J (2008). Gender differences in silencing following childhood sexual abuse. Journal of Child Sexual Abuse, 17, 133–143. doi:10.1080/10538710801916416 [DOI] [PubMed] [Google Scholar]
- Osborne J. W. (2008). Best practices in quantitative methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Panik M. J. (2014). Growth curve modeling: Theory and applications. Hoboken, NJ: Wiley. [Google Scholar]
- Papilla N. L., Buebbers S., Ogloff J. R., Cutajar M., & Mullen P. E (2016). The long-term co-occurrence of psychiatric illness and behavioral problems following child sexual abuse. Australian and New Zealand Journal of Psychiatry, 51, 604–613. doi:10.1177/0004867416667232 [DOI] [PubMed] [Google Scholar]
- Pereda N. Guilera G. Forns M. & Gómez-Benito J (2009). The prevalence of child sexual abuse in community and student samples: A meta-analysis. Clinical Psychology Review, 29, 328–338. doi:10.1016/j.cpr.2009.02.007 [DOI] [PubMed] [Google Scholar]
- Radloff S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Seltzer M. M. Floyd F. Song J. Greenberg J. & Hong J (2011). Midlife and aging parents of adults with intellectual and developmental disabilities: Impacts of lifelong parenting. American Journal on Intellectual and Developmental Disabilities, 116, 479–499. doi:10.1352/1944-7558-116.6.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J. Floyd F. J. Seltzer M. M. Greenberg J. S. & Hong J (2010). Long-term effects of child death on parents’ health related quality of life: A dyadic analysis. Family Relations, 59, 269–282. doi:10.1111/j.1741-3729.2010.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spataro J. Mullen P. E. Burgess P. M. Wells D. L. & Moss S. A (2004). Impact of child sexual abuse on mental health: Prospective study in males and females. The British Journal of Psychiatry: The Journal of Mental Science, 184, 416–421. [DOI] [PubMed] [Google Scholar]
- Springer K. W. (2009). Childhood physical abuse and midlife physical health: Testing a multi-pathway life course model. Social Science & Medicine (1982), 69, 138–146. doi:10.1016/j.socscimed.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer K. W. Sheridan J. Kuo D. & Carnes M (2007). Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect, 31, 517–530. doi:10.1016/j.chiabu.2007.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot N. L. Chapman B. Conwell Y. McCollumn K. Franus N. Cotescu S. & Duberstein P. R (2009). Childhood sexual abuse is associated with physical illness burden and functioning in psychiatric patients 50 years of age and older. Psychosomatic Medicine, 71, 417–422. doi:10.1097/PSY.0b013e318199d31b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor M. G. & Lynch S. M (2004). Trajectories of impairment, social support, and depressive symptoms in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 59, S238–S246. doi:10.1093/geronb/59.4.S238 [DOI] [PubMed] [Google Scholar]
- Thomas P. A. (2010). Is it better to give or receive? Social support and the well-being of older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B: 351–357. doi:10.1093/geronb/gbp113 [DOI] [PubMed] [Google Scholar]
- Tonmyr L. & Shields M (2017). Childhood sexual abuse and substance abuse: A gender paradox?Child Abuse & Neglect, 63, 284–294. doi:10.1016/j.chiabu.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Trickett P. K., Noll J. G., & Putnam F. W (2011). The impact of sexual abuse on female development: Lessons from a multigenerational, longitudinal research study. Development and Psychopathology, 23, 453–476. doi:10.1017/S0954579411000174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner R. J., & Lloyd D. A (1995). Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior, 36, 360–376. Retrieved from http://www.jstor.org.proxy.bc.edu/stable/2137325. [PubMed] [Google Scholar]
- Turner S., Taillieu T., Cheung K., & Afifi T. O (2017). The relationship between childhood sexual abuse and mental health outcomes among males: Results from a nationally representative United States sample. Child Abuse & Neglect, 66, 64–72. doi:10.1016/j.chiabu.2017.01.018 [DOI] [PubMed] [Google Scholar]
- Valentine L., & Feinauer L. L (1993). Resilience factors associated with female survivors of childhood sexual abuse. American Journal of Family Therapy, 21, 216–224. doi:10.1080/01926189308250920 [Google Scholar]
- Van der Kolk B. A. (1996). The complexity of adaptation to trauma: Self-regulation, stimulus discrimination, and characterological development. In Van der Kolk B. A., McFarlane A., & Weisaeth L. (Eds.), Traumatic stress (pp. 182–213). New York, NY: Guildford Press. [Google Scholar]
- van der Kolk B. A. Roth S. Pelcovitz D. Sunday S. & Spinazzola J (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18, 389–399. doi:10.1002/jts.20047 [DOI] [PubMed] [Google Scholar]
- Wisconsin Longitudinal Study (WLS) (n.d). Retention and response rates. Retrieved from http://www.ssc.wisc.edu/wlsresearch/documentation/retention/cor1004_retention.pdf. [Google Scholar]